Adhd and magnesium
10 Supplements and Vitamins for ADHD Symptom Control
What ADHD Supplements Improve Symptoms?
Research shows that medication does a good job of managing ADHD symptoms in many children and adults. Still, the thought of starting your eight-year-old son or daughter on a drug, no matter how effective it might be, causes lots of hand-wringing and soul-searching in parents before they agree to do it. There are potential side effects to be considered, along with the fact that ADHD medications don’t work the same way for every child in managing symptoms. So some parents look for other natural remedies for ADHD, such as nutrition, exercise, and supplements, to help their child deal with symptoms.
It is important to understand what a supplement is. A nutritional supplement provides basic nutrients for optimal health and function that you may not be getting from your food. Supplements include vitamins, minerals, proteins, and fats. I don’t include herbal or botanical ingredients, such as ginkgo or St.
John’s wort, in the supplement category. Botanicals are plant-based products that are not necessarily nutrients, but which may have positive effects on health and function.
Now let’s look at the individual ADHD supplements I recommend. Every natural remedy for ADHD mentioned here has some research to support its effectiveness in improving some symptoms.
If possible, I’d consult a physician to help you incorporate supplements into your treatment plan. Managing supplements and other integrative treatments requires expertise. It is difficult for a family to do this on their own.
ADHD Supplement: Omega-3 Fatty Acids
Usually given in the form of fish oil, omega-3s are probably the best-researched supplement for ADHD. Numerous studies, including two meta-analyses, have found benefit in the area of hyperactivity, attention, or impulsivity.
[Get This Free Resource: Everyday Foods Filled with Omega-3s]
Finding the best omega 3 supplement is a different story.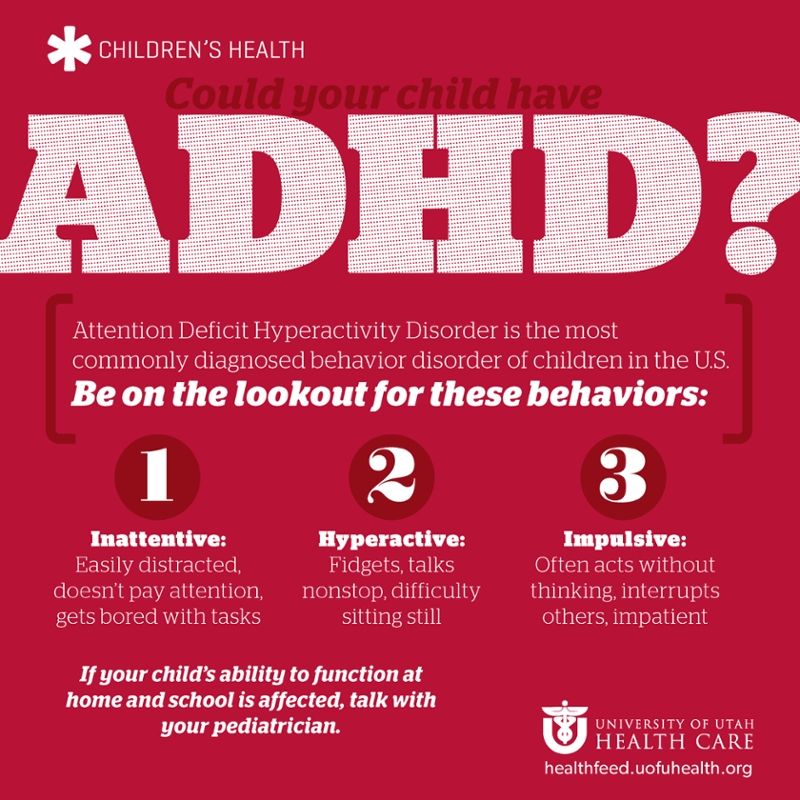 Despite all the studies on omega-3s, questions remain about the optimal dose and how to give it. The important omega-3 fatty acids are EPA and DHA, which are listed on most product labels. I recommend a total of 1,000 mg. of EPA plus DHA (add the two together) for smaller children, 2,000 mg. for adolescents, and 1,500 mg. for those in between. There should be 1.5 to 2 times as much EPA as DHA. Most omega-3 gummies don’t provide these higher levels, so your best option is to give your child capsules or a liquid. For children who are vegetarian, algae oil is available, but it requires large doses to get enough EPA and DHA.
Despite all the studies on omega-3s, questions remain about the optimal dose and how to give it. The important omega-3 fatty acids are EPA and DHA, which are listed on most product labels. I recommend a total of 1,000 mg. of EPA plus DHA (add the two together) for smaller children, 2,000 mg. for adolescents, and 1,500 mg. for those in between. There should be 1.5 to 2 times as much EPA as DHA. Most omega-3 gummies don’t provide these higher levels, so your best option is to give your child capsules or a liquid. For children who are vegetarian, algae oil is available, but it requires large doses to get enough EPA and DHA.
A related supplement is phosphatidylserine. This is a type of molecule derived from fatty acids that plays an important role in cell signaling. A couple of small studies indicate it might be helpful for ADHD. My clinical experience is that the benefits have not been impressive. It can be taken on its own or in conjunction with a fish oil supplement.
ADHD Supplement: Zinc
I recommend zinc for children with ADHD.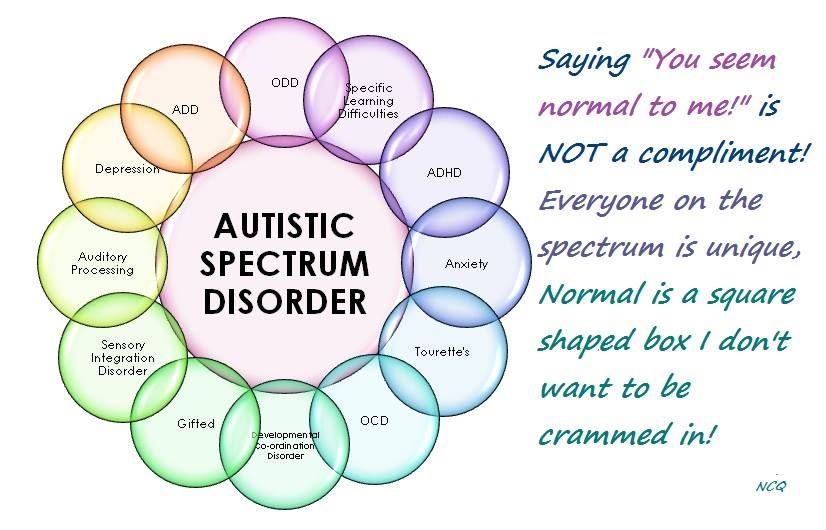 The mineral is not as well researched as omega-3s and iron, but there is some positive research. One study showed that taking zinc with a psychostimulant caused a nearly 40 percent reduction in the amount of the stimulant required to function at optimal levels. Other studies have shown benefits for ADHD symptoms in general. Zinc levels can be measured in the blood, but it is safe to give 20-25 mg. of zinc daily to your child without first doing a blood test.
The mineral is not as well researched as omega-3s and iron, but there is some positive research. One study showed that taking zinc with a psychostimulant caused a nearly 40 percent reduction in the amount of the stimulant required to function at optimal levels. Other studies have shown benefits for ADHD symptoms in general. Zinc levels can be measured in the blood, but it is safe to give 20-25 mg. of zinc daily to your child without first doing a blood test.
ADHD Supplement: Vitamin D
Many American children have abnormally low levels of vitamin D. Newer research shows that children with ADHD have lower vitamin D levels than children without the condition. One study showed that expectant mothers with low vitamin D levels had a higher likelihood of their children having ADHD. There are no studies showing that giving vitamin D to children with ADHD improves their symptoms. Nevertheless, I would check vitamin D levels and supplement if the levels are low or even borderline low.
[Free Resource Here: Guide to Natural ADHD Treatment Options]
ADHD Supplement: Iron
Low levels of the mineral iron can be a significant problem in children with ADHD. Studies have shown that iron is crucial for normal brain function, and that treating with supplemental iron can improve ADHD symptoms.
Before giving an iron supplement to your child, it is important to measure the iron levels in your child’s blood. When doctors measure these in children, they test for hemoglobin and hematocrit — the level of iron in red blood cells. These readings are usually normal in children with ADHD. I recommend that doctors also check the ferritin level, which measures circulating iron. This is often low, or borderline low, in kids with ADHD. One study showed that the average ferritin level in ADHD children was 22 compared with 44 in non-ADHD children.
I recommend supplementing with iron if a child has a ferritin level under 30. It is important to use a chelated iron product, which reduces the problem of constipation or stomachaches.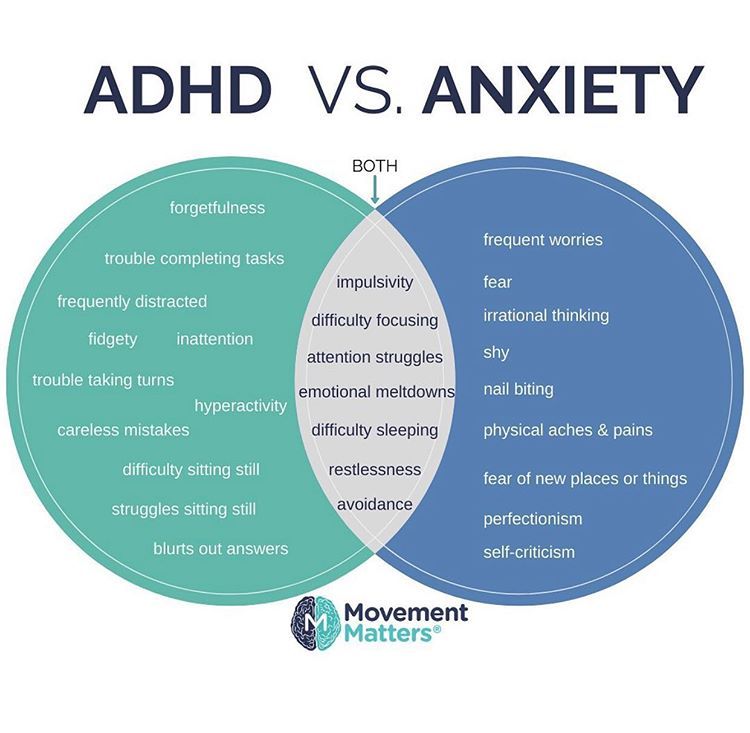 I usually begin with 30-40 mg. of elemental iron a day, and measure ferritin levels again in three to six months.
I usually begin with 30-40 mg. of elemental iron a day, and measure ferritin levels again in three to six months.
Multivitamin/Multimineral for ADHD
It is important that children with ADHD have adequate amounts of a wide range of vitamins and minerals, but until recently, there has been little research suggesting that taking a multivitamin/multimineral was helpful for ADHD. Research indicates that a specific multivitamin/multimineral combination is effective for kids who have ADHD and emotional dysregulation, often displayed by oppositional children.
Daily Essential Nutrients is made by Hardy Nutritionals. In one study, the micronutrients in this formulation reduced impairment and improved inattention, emotional regulation, and aggression. DEN did not improve hyperactive/impulsive symptoms. The downside is that it is expensive, and a child has to take six pills a day. It’s possible that other multivitamins have similar effects, but they have not been well-studied.
ADHD Supplement: Magnesium
This mineral won’t directly improve attention, but it can calm hyperactivity and agitation, which compromise attention.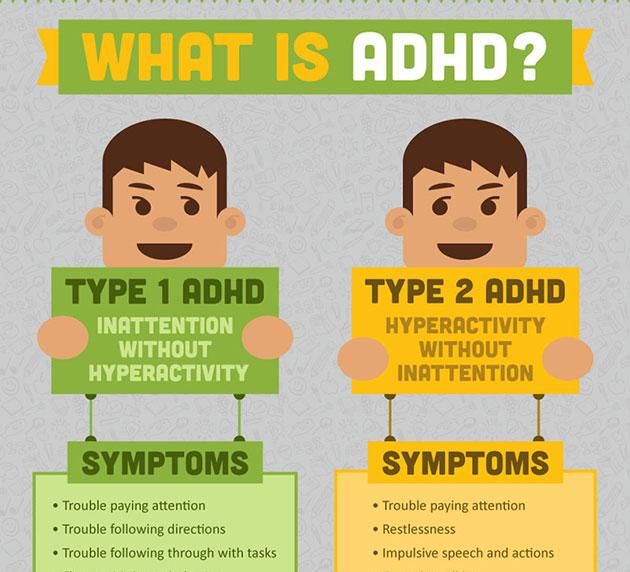 I find magnesium helpful for children who have a “rebound effect” after their stimulant medication wears off. A child can safely take 100-300 mg. of elemental magnesium twice daily in the form of magnesium glycinate, citrate, or chelate. The citrate form tends to lead to loose stools.
I find magnesium helpful for children who have a “rebound effect” after their stimulant medication wears off. A child can safely take 100-300 mg. of elemental magnesium twice daily in the form of magnesium glycinate, citrate, or chelate. The citrate form tends to lead to loose stools.
ADHD Supplement: Inositol
Inositol is found in very small amounts in many foods. In concentrated doses, it helps to counter agitation and anxiety. I recommend 12-18 grams a day divided into two or three doses for adults. The dose for kids would be calculated based on their mass.
ADHD Supplement: Ginkgo Biloba
This herb has been used to improve cognitive function for thousands of years. A couple of small studies have shown that it may be helpful in children with ADHD. A recent double-blind randomized study looked at adding ginkgo to a stimulant that children were already taking. Some children took ginkgo plus a stimulant, while others took a placebo and a stimulant. Those who took the ginkgo had a 35 percent better response rate in terms of improving attention. It had no effect on hyperactivity or impulsivity. I use 60 mg., twice a day, for children.
It had no effect on hyperactivity or impulsivity. I use 60 mg., twice a day, for children.
Bacopa and gotu kola, which are part of Ayurvedic medicine (the traditional medicine of India), have both been used to treat ADHD, but western medicine has done little research on them.
One herb, St. John’s wort, is often recommended for children with ADHD, but research shows that it helps with mood disorders, not ADHD. A study on using St. John’s wort to treat ADHD reached the same conclusion: It did not help. This study was discussed in the June 2008 issue of the Journal of the American Medical Association. View the study abstract.
The ABCs of ADHD Supplements
Among the many questions parents ask me when thinking about natural supplements for ADHD are: How can supplements help? Are they a substitute for ADHD medication, or can they be used together? How long do they take to work? Can they have side effects?
- How do supplements improve attention, impulsivity, or hyperactivity? It is helpful to understand how supplements are researched.
 The most common method is to give either the supplement being studied or a placebo to a person, and see if ADHD symptoms improve. Researchers measure this by looking at ADHD surveys or checklists, filled out by teachers and parents. In most cases, the research shows improvements in attention and focus, hyperactivity, or impulsivity, or all of them. It is hard to predict the effect any single supplement will have on a child.
The most common method is to give either the supplement being studied or a placebo to a person, and see if ADHD symptoms improve. Researchers measure this by looking at ADHD surveys or checklists, filled out by teachers and parents. In most cases, the research shows improvements in attention and focus, hyperactivity, or impulsivity, or all of them. It is hard to predict the effect any single supplement will have on a child. - Will supplements improve symptoms as much as ADHD medication? For the most part, no. ADHD-friendly supplements are helpful, but they do not have the immediate and powerful effect on ADHD symptoms that medication does. It is hard to quantify the effectiveness of these supplements compared to medication. It is worth noting that supplements in general have far fewer side effects than medication, and less potential for severe side effects. I use supplements as part of an integrative treatment plan that includes interventions related to school, parenting, sleep, and exercise.

- How long will it take to see results after starting a supplement? This varies, depending on the supplement and the child. Some families have told me that they saw improvement within days of starting fish oil; other families didn’t see any improvement after a month. I recommend waiting a few months before deciding whether or not supplements are helpful.
- Do supplements have side effects? Some supplements have side effects, but they are milder and less common than the side effects of ADHD stimulants. Iron, for instance, may cause constipation or abdominal pain. It is important to notice any symptoms that occur after starting one or more supplements and consult with your physician.
[Get Free Guide to the Best Vitamins and Supplements for Managing ADHD Symptoms]
Sandy Newmark, M.D., is a member of the ADDitude ADHD Medical Review Panel.
SUPPORT ADDITUDE
Thank you for reading ADDitude. To support our mission of providing ADHD education and support, please consider subscribing. Your readership and support help make our content and outreach possible. Thank you.
Your readership and support help make our content and outreach possible. Thank you.
Previous Article Next Article
Effect of Vitamin D and Magnesium Supplementation on Behavior Problems in Children with Attention-Deficit Hyperactivity Disorder
1. Sadock BJ, Sadock VA. Kaplan & Sadock's Comprehensive Textbook of Psychiatry. 9th ed. London: Williams & Wilkins; 2009. pp. 3561–72. [Google Scholar]
2. Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. Pediatrics. 2015;135:e994–1001. [PubMed] [Google Scholar]
3. Polanczyk GV, Willcutt EG, Salum GA, Kieling C, Rohde LA. ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int J Epidemiol. 2014;43:434–42. [PMC free article] [PubMed] [Google Scholar]
4. Mohammadi MR, Ahmadi N, Salmanian M, Asadian-Koohestani F, Ghanizadeh A, Alavi A, et al. Psychiatric disorders in Iranian children and adolescents. Iran J Psychiatry. 2016;11:87–98. [PMC free article] [PubMed] [Google Scholar]
Mohammadi MR, Ahmadi N, Salmanian M, Asadian-Koohestani F, Ghanizadeh A, Alavi A, et al. Psychiatric disorders in Iranian children and adolescents. Iran J Psychiatry. 2016;11:87–98. [PMC free article] [PubMed] [Google Scholar]
5. Klassen AF, Miller A, Fine S. Health-related quality of life in children and adolescents who have a diagnosis of attention-deficit/hyperactivity disorder. Pediatrics. 2004;114:e541–7. [PubMed] [Google Scholar]
6. Frazier TW, Youngstrom EA, Glutting JJ, Watkins MW. ADHD and achievement: Meta-analysis of the child, adolescent, and adult literatures and a concomitant study with college students. J Learn Disabil. 2007;40:49–65. [PubMed] [Google Scholar]
7. Biederman J, Fried R, Petty C, Mahoney L, Faraone SV. An examination of the impact of attention-deficit hyperactivity disorder on IQ: A large controlled family-based analysis. Can J Psychiatry. 2012;57:608–16. [PubMed] [Google Scholar]
8. Hinshaw SP. Externalizing behavior problems and academic underachievement in childhood and adolescence: Causal relationships and underlying mechanisms. Psychol Bull. 1992;111:127–55. [PubMed] [Google Scholar]
Psychol Bull. 1992;111:127–55. [PubMed] [Google Scholar]
9. Biederman J, Faraone SV. The effects of attention-deficit/hyperactivity disorder on employment and household income. MedGenMed. 2006;8:12. [PMC free article] [PubMed] [Google Scholar]
10. Thapar A, Langley K, Asherson P, Gill M. Gene-environment interplay in attention-deficit hyperactivity disorder and the importance of a developmental perspective. Br J Psychiatry. 2007;190:1–3. [PubMed] [Google Scholar]
11. Mash EJ, Barkley RA. Assessment of Childhood Disorders. 4th ed. New York: Guilford Publications; 2012. [Google Scholar]
12. Milte CM, Parletta N, Buckley JD, Coates AM, Young RM, Howe PR, et al. Eicosapentaenoic and docosahexaenoic acids, cognition, and behavior in children with attention-deficit/hyperactivity disorder: A randomized controlled trial. Nutrition. 2012;28:670–7. [PubMed] [Google Scholar]
13. Nigg JT, Lewis K, Edinger T, Falk M. Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives. J Am Acad Child Adolesc Psychiatry. 2012;51:86–97. [PMC free article] [PubMed] [Google Scholar]
J Am Acad Child Adolesc Psychiatry. 2012;51:86–97. [PMC free article] [PubMed] [Google Scholar]
14. Arnold LE, Bozzolo H, Hollway J, Cook A, DiSilvestro RA, Bozzolo DR, et al. Serum zinc correlates with parent- and teacher – Rated inattention in children with attention-deficit/hyperactivity disorder. J Child Adolesc Psychopharmacol. 2005;15:628–36. [PubMed] [Google Scholar]
15. Ghanizadeh A. A systematic review of magnesium therapy for treating attention deficit hyperactivity disorder. Arch Iran Med. 2013;16:412–7. [PubMed] [Google Scholar]
16. Goksugur SB, Tufan AE, Semiz M, Gunes C, Bekdas M, Tosun M, et al. Vitamin D status in children with attention-deficit-hyperactivity disorder. Pediatr Int. 2014;56:515–9. [PubMed] [Google Scholar]
17. Kamal M, Bener A, Ehlayel MS. Is high prevalence of Vitamin D deficiency a correlate for attention deficit hyperactivity disorder? Atten Defic Hyperact Disord. 2014;6:73–8. [PubMed] [Google Scholar]
18. Gröber U, Schmidt J, Kisters K. Magnesium in prevention and therapy. Nutrients. 2015;7:8199–226. [PMC free article] [PubMed] [Google Scholar]
Magnesium in prevention and therapy. Nutrients. 2015;7:8199–226. [PMC free article] [PubMed] [Google Scholar]
19. Archana E, Pai P, Prabhu BK, Shenoy RP, Prabhu K, Rao A, et al. Altered biochemical parameters in saliva of pediatric attention deficit hyperactivity disorder. Neurochem Res. 2012;37:330–4. [PubMed] [Google Scholar]
20. Mahmoud MM, El-Mazary AA, Maher RM, Saber MM. Zinc, ferritin, magnesium and copper in a group of Egyptian children with attention deficit hyperactivity disorder. Ital J Pediatr. 2011;37:60. [PMC free article] [PubMed] [Google Scholar]
21. Nogovitsina OR, Levitina EV. Neurological aspect of clinical symptoms, pathophysiology and correction in attention deficit hyperactivity disorder. Zh Nevrol Psikhiatr Im S S Korsakova. 2006;106:17–20. [PubMed] [Google Scholar]
22. Mousain-Bosc M, Roche M, Polge A, Pradal-Prat D, Rapin J, Bali JP, et al. Improvement of neurobehavioral disorders in children supplemented with magnesium-Vitamin B6. I. Attention deficit hyperactivity disorders.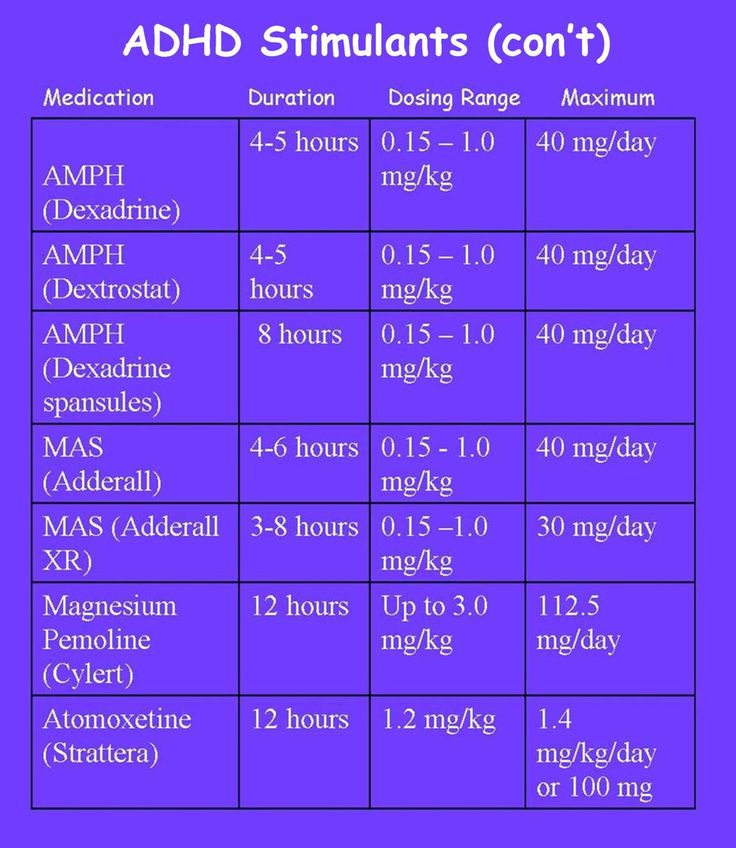 Magnes Res. 2006;19:46–52. [PubMed] [Google Scholar]
Magnes Res. 2006;19:46–52. [PubMed] [Google Scholar]
23. Mousain-Bosc M, Roche M, Rapin J, Bali JP. Magnesium VitB6 intake reduces central nervous system hyperexcitability in children. J Am Coll Nutr. 2004;23:545S–8S. [PubMed] [Google Scholar]
24. Nogovitsina OR, Levitina EV. Effect of MAGNE-B6 on the clinical and biochemical manifestations of the syndrome of attention deficit and hyperactivity in children. Eksp Klin Farmakol. 2006;69:74–7. [PubMed] [Google Scholar]
25. Huss M, Völp A, Stauss-Grabo M. Supplementation of polyunsaturated fatty acids, magnesium and zinc in children seeking medical advice for attention-deficit/hyperactivity problems – An observational cohort study. Lipids Health Dis. 2010;9:105. [PMC free article] [PubMed] [Google Scholar]
26. Starobrat-Hermelin B. The effect of deficiency of selected bioelements on hyperactivity in children with certain specified mental disorders. Ann Acad Med Stetin. 1998;44:297–314. [PubMed] [Google Scholar]
27. El Baza F, AlShahawi HA, Zahra S, AbdelHakim RA. Magnesium supplementation in children with attention deficit hyperactivity disorder. Egypt J Med Hum Genet. 2016;17:63–70. [Google Scholar]
El Baza F, AlShahawi HA, Zahra S, AbdelHakim RA. Magnesium supplementation in children with attention deficit hyperactivity disorder. Egypt J Med Hum Genet. 2016;17:63–70. [Google Scholar]
28. Holick MF. Sunlight and Vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80:1678S–88S. [PubMed] [Google Scholar]
29. Mohammadpour N, Jazayeri S, Tehrani-Doost M, Djalali M, Hosseini M, Effatpanah M, et al. Effect of Vitamin D supplementation as adjunctive therapy to methylphenidate on ADHD symptoms: A randomized, double-blind, placebo-controlled trial. Nutr Neurosci. 2018;21:202–9. [PubMed] [Google Scholar]
30. Al-Daghri NM, Alkharfy KM, Khan N, Alfawaz HA, Al-Ajlan AS, Yakout SM, et al. Vitamin D supplementation and serum levels of magnesium and selenium in type 2 diabetes mellitus patients: Gender dimorphic changes. Int J Vitam Nutr Res. 2014;84:27–34. [PubMed] [Google Scholar]
31. Farhanghi MA, Mahboob S, Ostadrahimi A.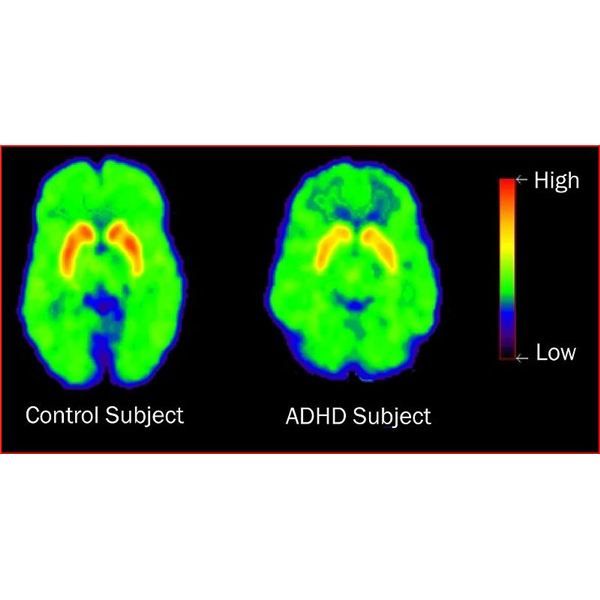 Obesity-induced magnesium deficiency can be treated by Vitamin D supplementation. J Pak Med Assoc. 2009;59:258–61. [PubMed] [Google Scholar]
Obesity-induced magnesium deficiency can be treated by Vitamin D supplementation. J Pak Med Assoc. 2009;59:258–61. [PubMed] [Google Scholar]
32. Deng X, Song Y, Manson JE, Signorello LB, Zhang SM, Shrubsole MJ, et al. Magnesium, Vitamin D status and mortality: Results from US National Health and Nutrition Examination Survey (NHANES) 2001 to 2006 and NHANES III. BMC Med. 2013;11:187. [PMC free article] [PubMed] [Google Scholar]
33. Risco F, Traba ML. Influence of magnesium on the in vitro synthesis of 24,25-dihydroxyvitamin D3 and 1 alpha, 25-dihydroxyvitamin D3. Magnes Res. 1992;5:5–14. [PubMed] [Google Scholar]
34. Risco F, Traba ML, de la Piedra C. Possible alterations of the in vivo 1,25(OH) 2D3 synthesis and its tissue distribution in magnesium-deficient rats. Magnes Res. 1995;8:27–35. [PubMed] [Google Scholar]
35. Holick MF. Vitamin D and health: evolution, biologic functions, and recommended dietary intakes for Vitamin D. Clin Rev Bone Miner Metab.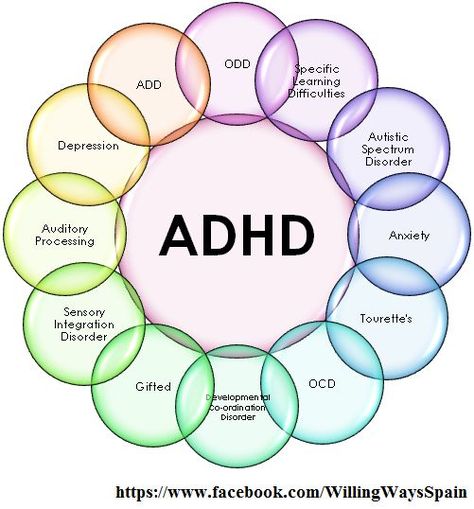 2009;7:2–19. [Google Scholar]
2009;7:2–19. [Google Scholar]
36. Drueke TB, Lacour B. Magnesium homeostasis and disorders of magnesium metabolism. In: Feehally J, Floege J, Johnson RJ, editors. Comprehensive Clinical Nephrology. Philadelphia: Mosby; 2007. pp. 136–8. [Google Scholar]
37. Zhang Z, Peluso MJ, Gross CP, Viscoli CM, Kernan WN. Adherence reporting in randomized controlled trials. Clin Trials. 2014;11:195–204. [PubMed] [Google Scholar]
38. Gianarris WJ, Golden CJ, Greene L. The conners’ parent rating scales: A critical review of the literature. Clin Psychol Rev. 2001;21:1061–93. [PubMed] [Google Scholar]
39. Shahaeian A, Shahim S, Bashash L, Yousefi F. Standardisation, factor analysis and reliability of the conners’ parent rating scales for 6- to 11-years-old children in shiraz. Q J Psychol Stud. 2007;3:97–120. [Google Scholar]
40. Heilskov Rytter MJ, Andersen LB, Houmann T, Bilenberg N, Hvolby A, Mølgaard C, et al. Diet in the treatment of ADHD in children – A systematic review of the literature. Nord J Psychiatry. 2015;69:1–8. [PubMed] [Google Scholar]
Nord J Psychiatry. 2015;69:1–8. [PubMed] [Google Scholar]
41. Peacock G, Amendah D, Ouyang L, Grosse SD. Autism spectrum disorders and health care expenditures: The effects of co-occurring conditions. J Dev Behav Pediatr. 2012;33:2–8. [PubMed] [Google Scholar]
42. Doshi JA, Hodgkins P, Kahle J, Sikirica V, Cangelosi MJ, Setyawan J, et al. Economic impact of childhood and adult attention-deficit/hyperactivity disorder in the United States. J Am Acad Child Adolesc Psychiatry. 2012;51:990–100200. [PubMed] [Google Scholar]
43. Annweiler C, Schott AM, Berrut G, Chauviré V, Le Gall D, Inzitari M, et al. Vitamin D and ageing: Neurological issues. Neuropsychobiology. 2010;62:139–50. [PubMed] [Google Scholar]
44. Armstrong DJ, Meenagh GK, Bickle I, Lee AS, Curran ES, Finch MB, et al. Vitamin D deficiency is associated with anxiety and depression in fibromyalgia. Clin Rheumatol. 2007;26:551–4. [PubMed] [Google Scholar]
45. Kelishadi R, Ataei E, Ardalan G, Nazemian M, Tajadini M, Heshmat R, et al. Relationship of serum magnesium and Vitamin D levels in a nationally-representative sample of Iranian adolescents: The CASPIAN-III study. Int J Prev Med. 2014;5:99–103. [PMC free article] [PubMed] [Google Scholar]
Relationship of serum magnesium and Vitamin D levels in a nationally-representative sample of Iranian adolescents: The CASPIAN-III study. Int J Prev Med. 2014;5:99–103. [PMC free article] [PubMed] [Google Scholar]
Attention deficit hyperactivity disorder: diagnosis, pathogenesis, principles of treatment
00:00
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– The next lecture will be devoted to attention deficit hyperactivity disorder. Professor Zavadenko Nikolai Nikolaevich.
Nikolai Nikolaevich Zavadenko , professor, doctor of medical sciences:
– Good afternoon, dear colleagues.
I will talk about the pathogenesis, diagnosis and treatment of attention deficit hyperactivity disorder.
(Slide show).
Attention Deficit Hyperactivity Disorder (or ADHD for short) is the most common neuropsychiatric disorder in childhood. It occurs in school years in 3-7% of children. It is known (this is evidenced by the data of longitudinal studies) that the symptoms weaken as they grow older, but continue to manifest themselves in adolescence and even in adulthood in a fairly large number of patients.
It is known (this is evidenced by the data of longitudinal studies) that the symptoms weaken as they grow older, but continue to manifest themselves in adolescence and even in adulthood in a fairly large number of patients.
(Slide show).
Traditionally, ADHD is considered in our country within the framework of minimal brain dysfunctions. These include two groups of conditions according to the ICD-10 classification. Attention deficit hyperactivity disorder (or hyperkinetic disorder) is presented in section F9: Behavioral and emotional disorders of childhood and adolescence.
The same group of minimal brain dysfunctions includes psychological developmental disorders (section F8), speech developmental disorders, learning disorders (dysgraphia, dyslexia, dyscalculia) and developmental dyspraxia or static-locomotor insufficiency.
(Slide show).
This slide presents the results of our surveys of elementary school students in ordinary Moscow general education schools.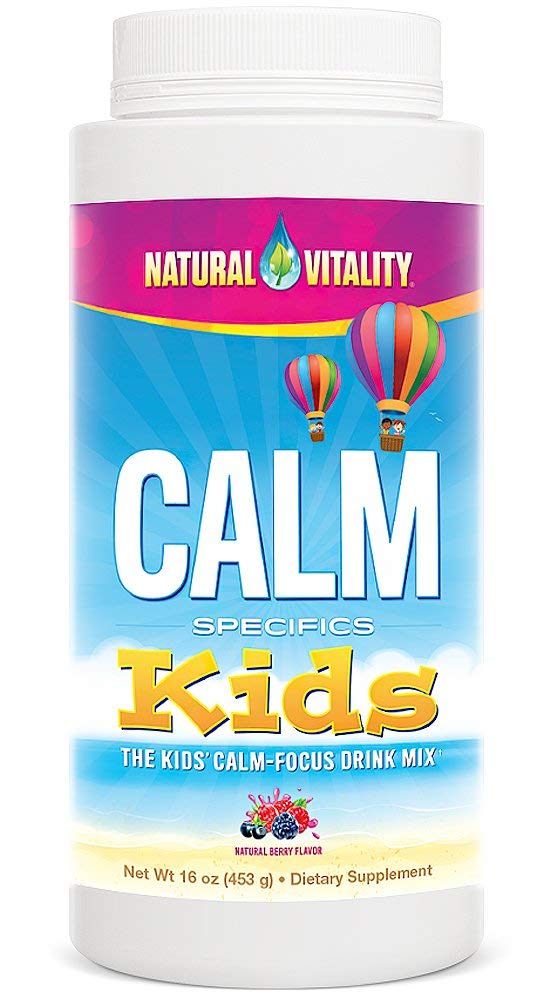 There were 537 children aged 7 to 11 years old. The aim of the study was to identify those children who have manifestations of school maladaptation (difficulties with learning, behavior, emotional control at school).
There were 537 children aged 7 to 11 years old. The aim of the study was to identify those children who have manifestations of school maladaptation (difficulties with learning, behavior, emotional control at school).
Among the examined children, 31.6% had school maladaptation. A significant part of the cases (about half) was determined by just minimal brain dysfunctions. Including ADHD was diagnosed in 7.6% of children. Other forms of minimal brain dysfunction in about 9%.
02:19
(Slide show).
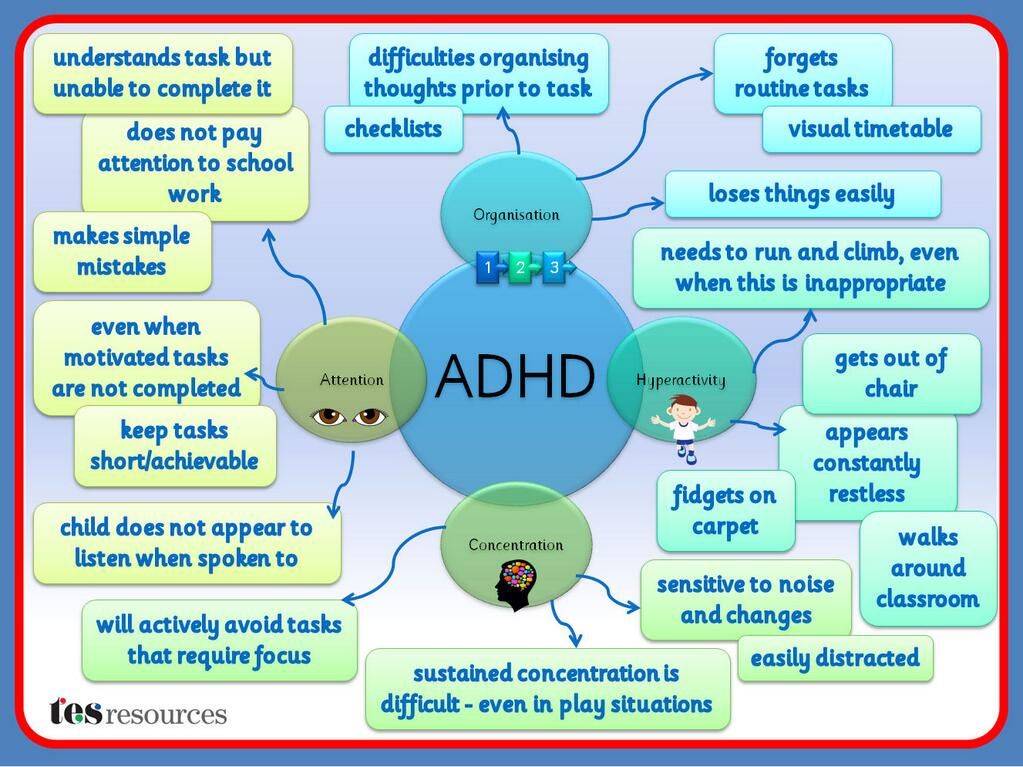
Pathogenesis of ADHD. To date, there is no doubt about the neurobiological nature of this disorder. The condition is due to the delayed development of interconnected brain structures that provide the processes of behavioral inhibition and self-control. They are defined today as the control functions of the brain.
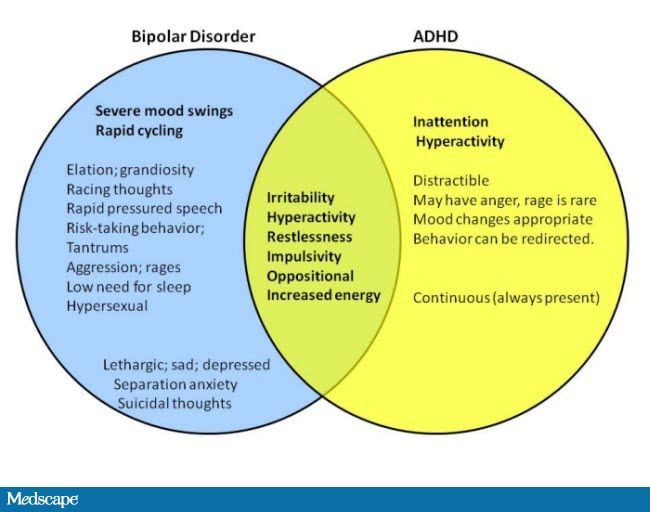
The key symptoms of ADHD are inattention, hyperactivity and impulsivity. The most characteristic symptoms of the disorder are formulated as its diagnostic criteria. 9signs of manifestation of hyperactivity and impulsivity, 9 signs of impaired attention.
9signs of manifestation of hyperactivity and impulsivity, 9 signs of impaired attention.
Let's start with a list of manifestations of hyperactivity, since they are already pronounced at preschool age.
• The child is constantly spinning and turning.
• Cannot sit still when necessary.
• He is characterized by excessive and aimless motor activity.
• He cannot play quietly and calmly.
• In constant motion.
• Loquacious.
Hyperactivity is always combined with impulsivity.
• Answers questions without thinking.
• Cannot wait in line.
• Interferes with other people, interrupts them.
I must say that ADHD is characterized by a certain age dynamics. It is the manifestations of hyperactivity that decrease with age, the signs of impulsivity persist.
(Slide show).
As far as attention deficits are concerned, they will become most obvious when the child is being prepared for school or schooling begins.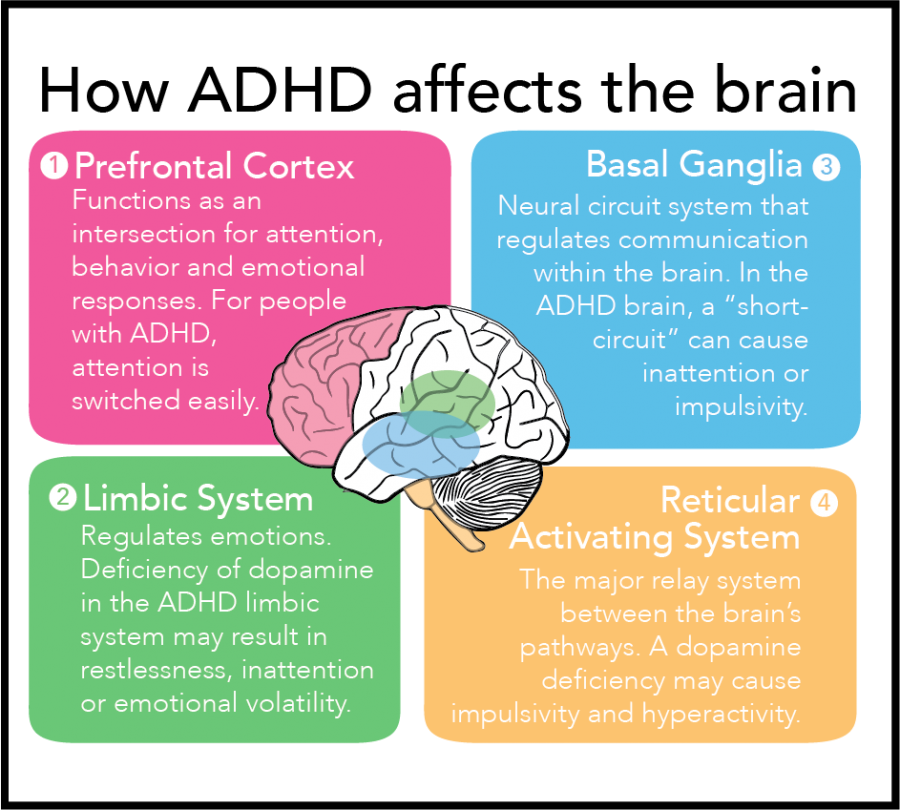 Literally from the first grade of school, the following signs will be very pronounced.
Literally from the first grade of school, the following signs will be very pronounced.
• Does not pay attention to details, makes many mistakes.
• Difficulty paying attention to school and other tasks.
• Does not listen to spoken language.
• Unable to follow instructions, follow through.
• Unable to independently plan and organize tasks.
• Avoids activities that require prolonged mental effort.
• Often loses his belongings.
• Easily distracted.
• Shows forgetfulness.
04:28
(Slide show).
In order for the diagnosis to be substantiated according to ICD-10, which we use in our country, we need to confirm at least 6 symptoms of inattention, 3 signs of hyperactivity and 1 impulsivity.
But there is another internationally recognized DSM-4 classification in the world, the American classification. According to it, the presence of 6 or more symptoms in at least one of two groups will be enough to make a diagnosis: impaired attention or hyperactivity / impulsivity.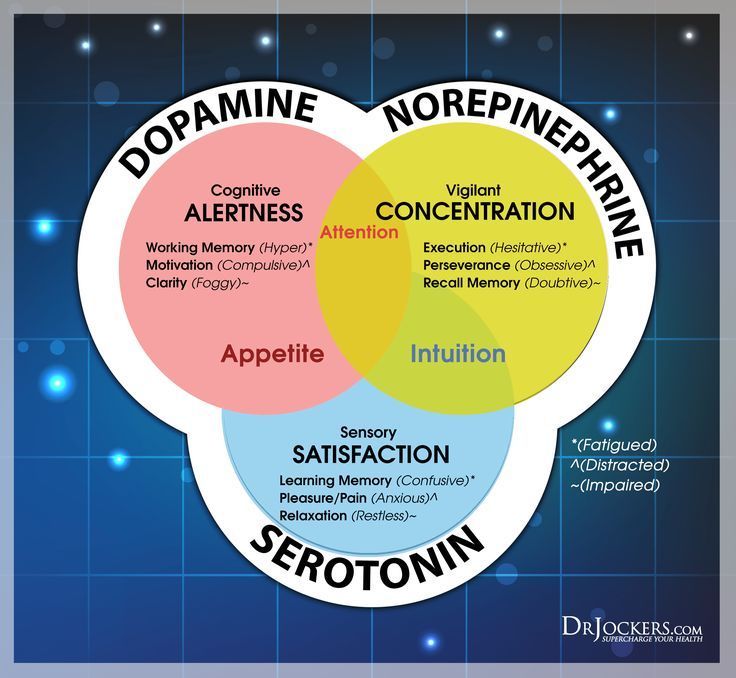
There are additional criteria for ADHD. In particular, the symptoms must be of sufficient duration to occur continuously for at least 6 months.
Age of onset: they first appear before 7 years of age. Characterized by constancy, distribution to all spheres of life. Accordingly, they lead to significant signs of maladaptation in at least two types of environment: at school, at home. It can be public places, sports, leisure time. The violation is quite pronounced. Another important criterion (this is a matter of differential diagnosis) is that other disorders must be excluded.
05:44
(Slide show).
According to the DSM-4 classification, depending on the presence and prevalence of symptoms, 3 forms of ADHD are distinguished:
• combined form. Both groups of symptoms are present. It accounts for 50 to 75% of cases.
• ADHD with predominant attention deficits. 20-30%. This group will mainly be represented by teenagers. And it also often happens that in girls the manifestation of hyperactivity is less pronounced.
• ADHD with a predominance of hyperactivity and impulsivity. This form (15% of cases), on the contrary, is more common in preschool age.
According to the ICD classification, we make a diagnosis - we determine the combined form of ADHD. The ICD-10 classification criteria that we use are more stringent.
(Slide show).
Often there are conditions that mimic ADHD. This is 15-20% of school-age children. They may experience similar phenomena, but their cause is not ADHD at all, but some other violations or even a variant of the norm - individual characteristics of temperament. Including:
• impaired attention, periodic hyperactivity may be present in anxiety disorders - what used to be called neuroses, neurotic reactions in children;
• in case of asthenic syndrome in case of somatic diseases;
• in case of consequences of traumatic brain injury, neuroinfection, intoxication;
• in a number of endocrine diseases, including thyroid pathology;
• for sensorineural hearing loss;
• in a number of forms of epilepsy;
• Tourette's syndrome;
• for a wide range of mental disorders.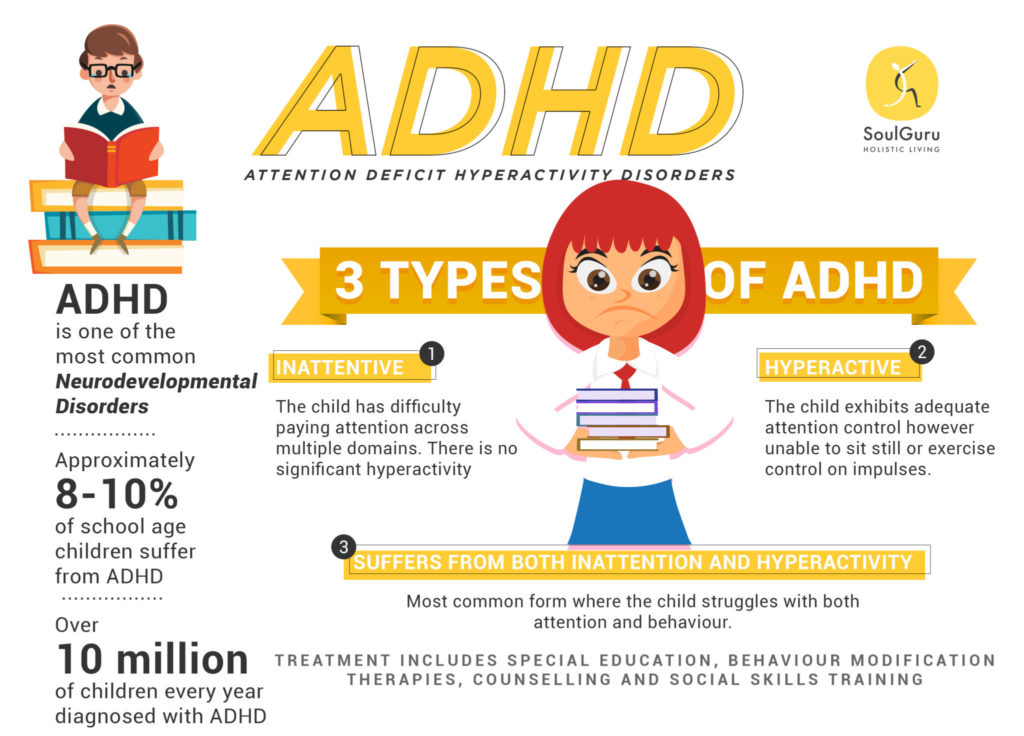
All of these conditions require a differential diagnosis.
(Slide show).
Pathogenesis of ADHD. As I said, this condition is based on neurobiological factors. These are genetic mechanisms and early organic damage to the central nervous system associated with the pathological course of pregnancy and childbirth.
Genetic mechanisms, early organic damage to the CNS, lead to neurotransmitter disorders. First of all, this concerns two neurotransmitter systems: dopaminergic and noradrenergic. But the production, synthesis of neurotransmitters does not decrease directly, the processes of synaptic transmission suffer.
Social and psychological factors can play an additional negative role. First of all, these are negative intra-family factors. As a result, the child will suffer from the formation of higher mental functions, behavioral deviations and all the clinical symptoms that we have just considered will be noted.
08:29
(Slide show).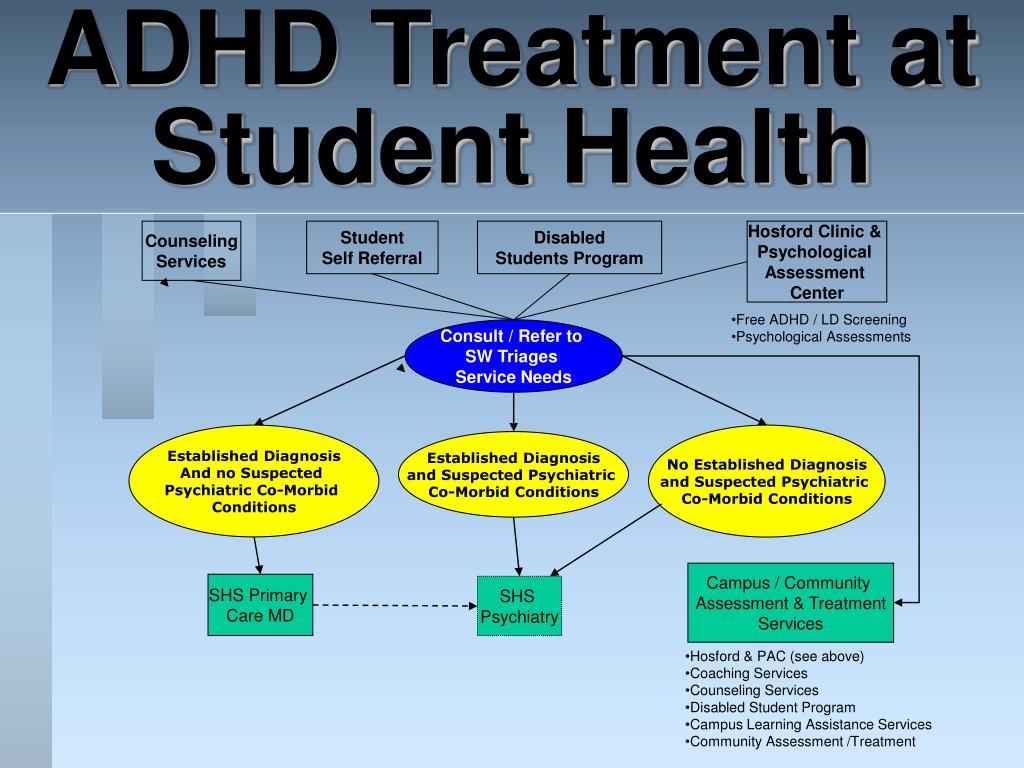
Mechanisms of development of ADHD. If we talk about higher mental functions that suffer in this state and are not sufficiently formed, these are control functions. They are provided by the frontal lobes, primarily their anterior sections, prefrontal structures of the brain.
Prefrontal structures are responsible for control functions and behavioral inhibition. Accordingly, patients with ADHD exhibit executive dysfunction.
Control functions components. It is these aspects of behavior that are affected by Attention Deficit Hyperactivity Disorder.
• Control of attention.
• Braking, containment, impulse control.
• Planning and organization.
• Inner speech.
• Working or random access memory.
• Foresight, forecasting, foresight, which, of course, should be based on a look into the past, a retrospective assessment of past events and miscalculations.
• Choice of priorities.
• Time management also suffers in patients with ADHD.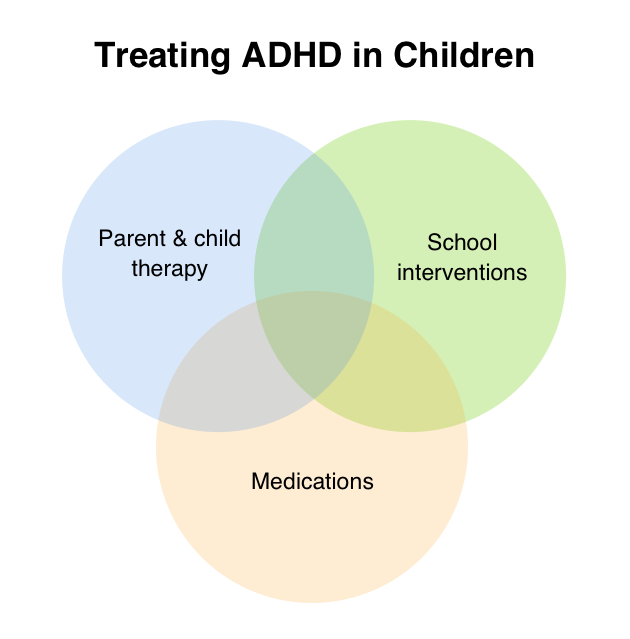
• Change, revision of plans.
• Separation of emotions from real facts.
09:44
(Slide show).
As a result of the influence of these neurobiological factors, the functions of the entire brain system for controlling attention and organizing behavior suffer. This system includes a number of areas of the brain: the associative cortex, basal ganglia, thalamus, cerebellum, prefrontal cortex.
As I said, failures in the functioning of this system, this complex of brain structures result from certain genetic mechanisms and early organic damage to the central nervous system. An additional negative role is played by socio-psychological factors.
Recently, attention has also been drawn to the influence of adverse environmental factors in terms of the pathogenesis of ADHD. This includes the effect of neurotoxicants on the developing brain. The most common of these is such a heavy metal as lead.
The role of nutritional factors is being studied, including the role of unbalanced nutrition and nutritional deficiencies of micronutrients: vitamins, macro- and microelements. Including attention is paid to the lack of magnesium in food.
Including attention is paid to the lack of magnesium in food.
What is the physiological role of magnesium in the central nervous system. This is maintaining the balance of the processes of excitation and inhibition. It affects the activity of neurons and the metabolism of neurotransmitters, is a cofactor for a number of enzymes that regulate neurotransmitter metabolism. In addition, magnesium prevents the accumulation of neurotoxic metals in the brain (in particular, lead, aluminum, nickel, and a number of others) and acts as their antagonist.
(Slide show).
Magnesium deficiency leads to an imbalance in the processes of excitation and inhibition in the brain towards excitation. Accordingly, it can intensify, further exacerbate the manifestation of ADHD symptoms. Magnesium deficiency causes additional disorders of neurotransmitter metabolism that are present in this condition.
Magnesium deficiency in ADHD can be formed due to insufficient intake of this element with food, with an increased need for magnesium during critical periods of growth and development, when exposed to severe physical and neuropsychic stress, and stress. Also, under conditions of environmental stress, lead, nickel and cadmium act as magnesium displacing metals. These mechanisms are currently being actively studied.
Also, under conditions of environmental stress, lead, nickel and cadmium act as magnesium displacing metals. These mechanisms are currently being actively studied.
I must say that in addition to a lack of magnesium in the body, the manifestation of ADHD symptoms can also be affected by zinc, iodine and iron deficiencies.
(Slide show).
Manifestations of magnesium deficiency in the body are:
• increased neuro-reflex excitability with corresponding neurological symptoms;
• asthenia, physical and mental fatigue;
• attention deficit;
• cerebral angiodystonia, which manifests itself in the form of headaches, dizziness, fainting;
• muscle pain and spasms;
• sleep disturbance.
In order to confirm the presence of magnesium deficiency, we must rely on laboratory values. For example, on the content of magnesium in blood serum. Here are indicators that correspond to moderate and severe magnesium deficiency.
13:16
ADHD therapy must be comprehensive. First of all, it should begin with educational work with parents and teachers. Of great importance, of course, is pharmacotherapy. Specialists work with parents to develop skills for raising children with ADHD, and here we also mean parent education and training programs, specially designed programs.
First of all, it should begin with educational work with parents and teachers. Of great importance, of course, is pharmacotherapy. Specialists work with parents to develop skills for raising children with ADHD, and here we also mean parent education and training programs, specially designed programs.
(Slide show).
Good internet resources are available. Here are the names of two Internet sites. Parent organization (meaning parents of patients with ADHD, children and adolescents with ADHD). This organization is called Impulse. A lot of useful information can be found on these sites.
Psychotherapeutic methods are aimed at overcoming difficulties and developing communication skills in children and adolescents with ADHD.
(Slide show).
This book was recently released (last year) by Thera-Wind. It describes the methodology of parent training. Undoubtedly, this technique should be widely adopted in our country.
14:29
Complex therapy for ADHD also includes (if possible) control of negative nutritional and environmental factors, limiting the intake of neurotoxic xenobiotics into the child's body.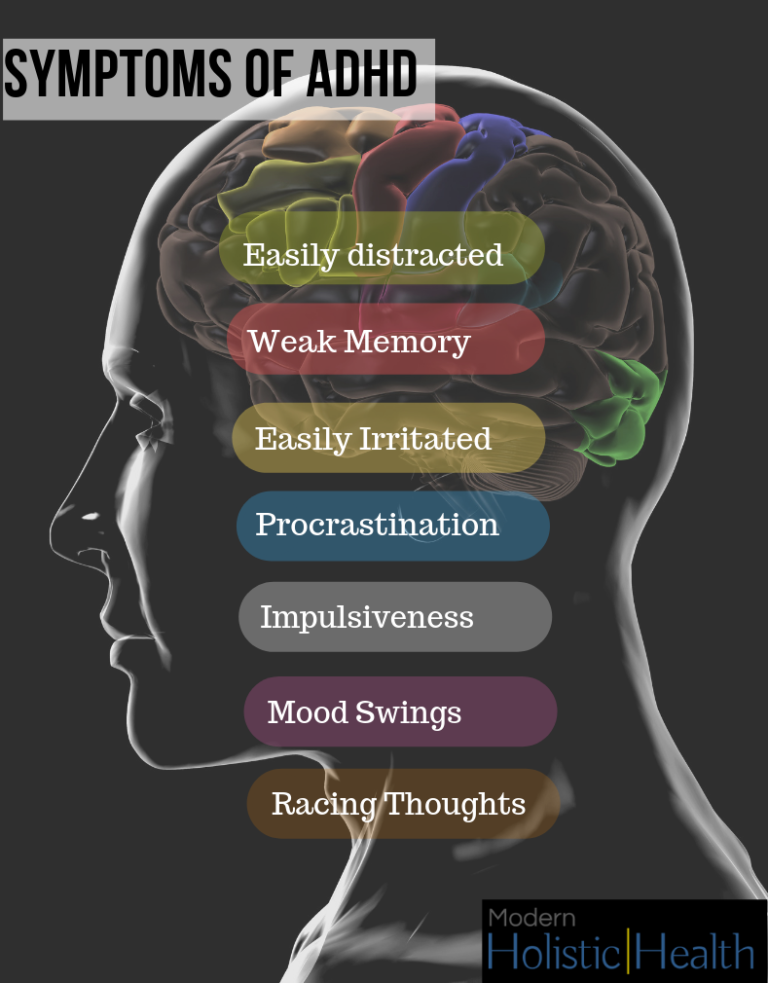 These are lead and other heavy metals, pesticides, food colorings and preservatives.
These are lead and other heavy metals, pesticides, food colorings and preservatives.
Therapy should include micronutrients that help reduce symptoms of ADHD. These are vitamins, macro- and microelements and a whole range of well-known drugs.
(Slide show).
cases where a child's cognitive and behavioral problems cannot be overcome with non-pharmacological methods alone.
Traditionally in our country we use nootropic drugs. There is a wide range of them. In particular, they are very well studied in childhood.
A fairly new and effective drug that has been specifically developed for the treatment of ADHD is Atomoxetine Hydrochloride or Strattera. The drug was registered in Russia in 2005 and is widely used today.
(Slide show).
Nootropic drugs have a pathogenic effect in ADHD. They have a beneficial effect on the insufficiently formed higher mental functions in these patients. Nootropics have a positive effect on metabolic processes in the brain, contribute to the maturation of inhibitory and regulatory systems.
Efficiency in their application we can achieve in 50 - 70% of cases. This efficiency is manifested in the improvement of behavioral characteristics, indicators of motor skills, attention, memory, and other higher mental functions. And also in a certain improvement in the indicators of bioelectrical activity of the brain. For example, according to the EEG.
(Slide show).
Here is a list of nootropics. They are well known/ Include, for example, drugs of the neuropeptide series. Pyrrolidone derivatives, Nootropil (Piracetam). It is considered the ancestor of this group of nootropics. GABA derivatives: domestic drugs Pantogam and Phenibut ) As well as a number of other drugs.
I would like to draw your attention to the last line. The group of nootropic agents also includes neurometabolic agents with nootropic properties. Among them is such a drug as "Magne B6" ("Magne B6"). I would like to dwell on it in more detail.
16:58
It is an optimal combination of magnesium salts and vitamin B6. Magnesium makes up for the lack of a macronutrient in the body, and vitamin B6, pyridoxine, helps the absorption and fixation of magnesium by the cell.
Magnesium makes up for the lack of a macronutrient in the body, and vitamin B6, pyridoxine, helps the absorption and fixation of magnesium by the cell.
Magnesium is an essential trace element involved in many metabolic processes. On the other hand, pyridoxine is necessary for the normal functioning of the nervous system, is a coenzyme of the most important enzymes that act in the nervous tissue, and is involved in the biosynthesis of neurotransmitters. We talked about the fact that magnesium is the same coenzyme, that is, the action of the two components is synergistic.
(Slide show).
These are dosage forms of Magne-B6. From the age of 1 year, an oral solution can be used. It comes in ampoules and contains magnesium lactate. The solution contains mainly magnesium pidolate and magnesium lactate.
The traditional tablet form contains magnesium lactate. A fairly new form of Forte tablet contains magnesium citrate. Tablet forms can be used from the age of 6 years.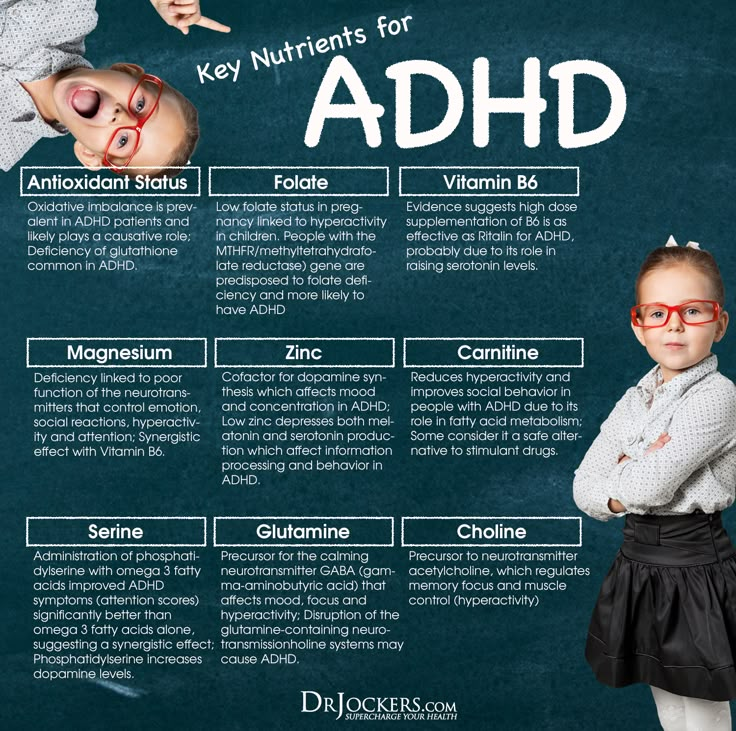
(Slide show).
The effectiveness of the drug in ADHD is due to the synergism of the action of its components. Pyridoxine increases the concentration of magnesium in plasma and erythrocytes, reduces the amount of magnesium excreted from the body, improves the absorption of magnesium in the gastrointestinal tract, its penetration and fixation in cells.
There has been evidence of a positive clinical effect of Magne-B6 in the treatment of those children with ADHD who have been confirmed to have a laboratory magnesium deficiency. These works were published abroad in 1998th year and 2004th.
These investigators administered a combination of magnesium and pyridoxine for several months to patients with ADHD. As a result, regression of symptoms was achieved. Magnesium levels in erythrocytes were monitored and restored to normal values.
19:22
(Slide show).
Russian researchers (in particular, the data of the works of Olga Alekseevna Gromova are presented here) studied the imbalance of macro- and microelements in children with ADHD.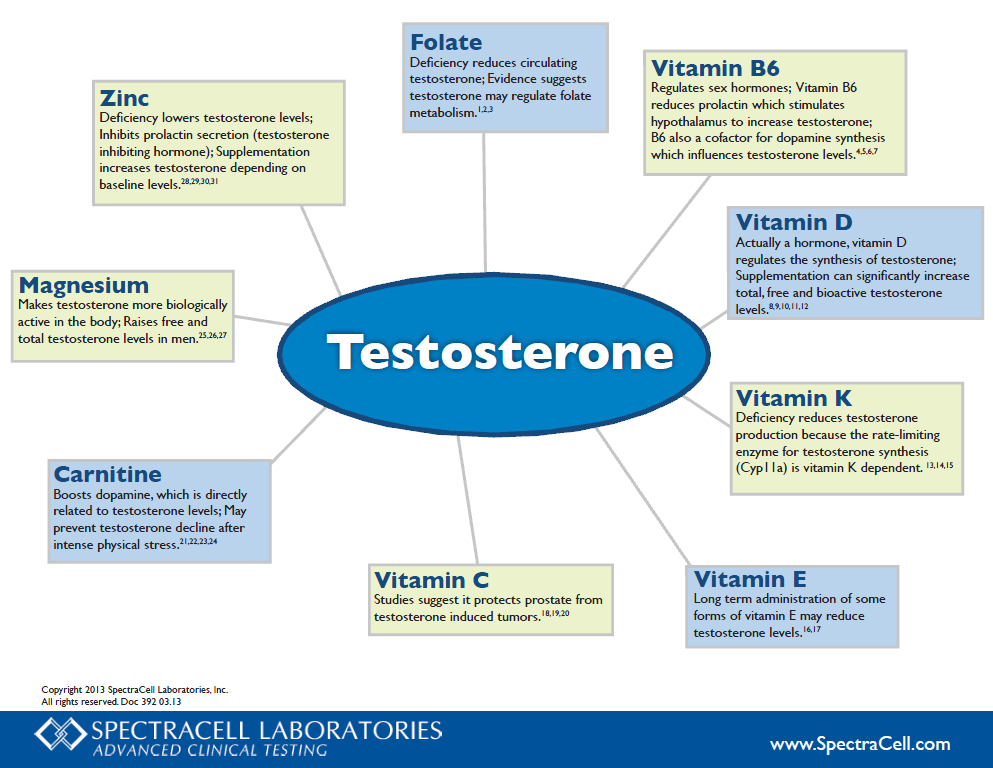 Here in the diagram, the red columns show us the percentage of patients with concentrations of certain macro- and microelements above the upper limit of normal. And the blue columns, on the contrary, are the content below the lower limit of the norm.
Here in the diagram, the red columns show us the percentage of patients with concentrations of certain macro- and microelements above the upper limit of normal. And the blue columns, on the contrary, are the content below the lower limit of the norm.
(Slide show).
The main part of the deviations was accounted for by deficits - this is 70% of cases. Excessive accumulation of elements was determined only in 11% of cases. The core of the deficits were 6 metals: magnesium, zinc, copper, calcium, manganese and cobalt.
I must say that an excess of lead has always correlated with a low level of magnesium. It is very important.
Magnesium deficiency occupied the leading position in the structure of elemental status deviations in patients with ADHD. Its level was below normal in 72% of patients. The level of magnesium in the hair was determined - this approach is also possible. More than 65% of patients had magnesium levels 2 or more times lower than normal.
(Slide show).
The results of therapy with Magne-B6 in patients with ADHD were also published by Russian researchers Nogovitsina and Levitina. Therapy was carried out in 31 patients with ADHD (age from 6 to 12 years) and 20 children of the control group were examined at the same time.
Questioning of parents showed a significant decrease in scores on the scales "anxiety", "impaired attention" and "hyperactivity". Improvement in concentration, accuracy and speed of tasks, a decrease in the number of errors were confirmed during psychological testing.
Positive dynamics on the encephalogram was registered. It was found that the concentration of magnesium in erythrocytes and blood plasma returned to normal after this therapy.
(Slide show).
But in general, replenishment of magnesium deficiency, if the child already has it, should last at least two months. Considering that alimentary deficiency of magnesium occurs most often, when drawing up nutritional recommendations, one should take into account not only the quantitative content of magnesium in foods, but also its bioavailability.
Fresh vegetables, fruits, herbs and nuts are known to be richest in magnesium. When harvesting products for storage, the concentration of magnesium does not decrease so significantly, but its bioavailability drops sharply. This also needs to be taken into account.
It must be taken into account that the deepening of magnesium deficiency in children with ADHD coincides with the period of schooling, that is, from September to May. This refers to the magnesium content in foods. The use of "Magne-B6" is advisable just during the school year.
Thus, the efforts of specialists should be aimed at early detection of ADHD in children. The development and application of complex correction should be carried out in a timely manner, be of an individual nature. Correction, including drug therapy, should have sufficient duration.
Thank you for your attention.
Linking magnesium and children with ADHD
621 views
We talked with Tatyana Vladimirovna Mokina, Candidate of Medical Sciences, neurologist, about the connection between magnesium and children with ADHD.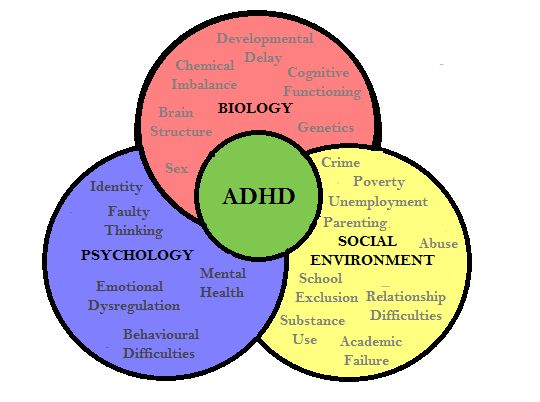
Tatyana Vladimirovna, how can magnesium and, in particular, magnesium baths help children with hyperactivity and attention deficit?
TV. Magnesium deficiency is present in 72% of patients with ADHD, while more than 65% of patients with ADHD have magnesium levels that are 2 or more times lower than normal.
It should be emphasized that the clinical picture of magnesium deficiency and ADHD are manifested by clinically similar symptoms, which is revealed on examination by a neurologist: attention deficit, motor deficit, manifestations of the syndrome of increased neuro-reflex excitability (Chvostek's symptom of 2-3 degrees, Trousseau's symptom, etc. .), cerebral angiodystonia (headaches, dizziness, fainting and lipothymic conditions).
It is known that Mg deficiency leads to such neurological disorders as increased activity of deep tendon reflexes, ataxia, tremor, disorientation, provokes convulsive conditions, nystagmus, paresthesia. These physiological manifestations of magnesium deficiency correspond to the basic components of ADHD, namely behavioral disorders in the form of impulsivity, uncontrollable behavior during stress, attention deficit, and motor deficit manifested in the form of hyperactivity.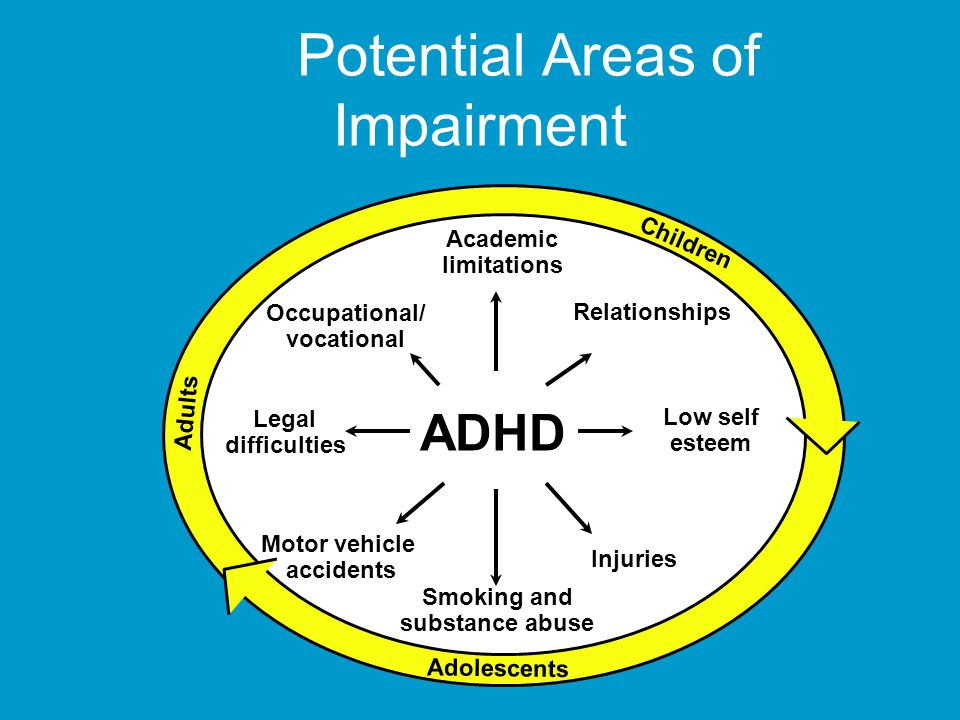
It is noteworthy that an excess of lead has always been combined with a low concentration of magnesium in the hair. This is due to the ability of lead to displace Mg from the body according to the principle of competitive antagonism. As you know, the clinical signs of lead poisoning in children are very similar to those of ADHD. Lead pollution, along with magnesium imbalances, may increase the risk of ADHD in children. A characteristic clinical manifestation of lead intoxication is pronounced hyperactivity, aggressiveness, and "uncontrollability" of children.
Thus, Mg deficiency is specific for attention deficit hyperactivity disorder and can be considered as a characteristic feature of the nosological elemental portrait in children with ADHD. According to Shealy, N deficiency of magnesium can be compensated by transdermal application within 4-6 weeks (Shealy, N. Holy Water, Sacred Oil: The Fountain of Youth; Biogenics Books: New York, NY, USA) and therefore can be considered magnesium baths as one of the ways to treat ADHD.
How does transdermal magnesium work? What reactions at the physiological level does it trigger, and what effect does it have?
TV. Magnesium is not absorbed through the skin into the body. It penetrates no further than the epidermis. But magnesium in transdermal form has a general effect on the body. How does this happen?
The benefits of a magnesia bath on the body are due to the local and general effects that thermal, mechanical and chemical factors have.
Local action of magnesia
Salt baths conduct 1.5 times more heat into the body than regular fresh ones. The resulting heat dilates the vessels of the skin, increasing blood flow, activates the anticoagulant system and reduces the aggregation activity of platelets. Promotes the resorption of inflammation, stimulates the growth of granulation tissue.
Mechanical stimulation of nerve endings by salt particles also leads to the filling of skin vessels with blood. Moreover, the higher the concentration of magnesium sulfate in water, the stronger their irritating effect and the stronger the filling of skin vessels with blood. Increased salt water pressure affects the skin receptors, reducing the excitability and conductivity of nerve endings, which reduces tactile and pain sensitivity. Movements in salt water are less painful, which makes it possible to use baths with magnesia for the treatment of the musculoskeletal system.
Increased salt water pressure affects the skin receptors, reducing the excitability and conductivity of nerve endings, which reduces tactile and pain sensitivity. Movements in salt water are less painful, which makes it possible to use baths with magnesia for the treatment of the musculoskeletal system.
General action of magnesia
Mechanical irritation of skin receptors causes the release of histamine, which dilates capillaries and has a stimulating effect on the whole body. Simultaneously with histamine, acetylcholine is released, which stimulates the vagus nerve, which benefits the entire body.
Irritation of the vagus nerve activates the parasympathetic nervous system, which is responsible for the accumulation of resources, rest, sleep, calmness. As a result, the symptoms of chronic fatigue, stress, and hyperactivity disappear. The action of baths on the autonomic nervous system allows them to be used in the treatment of diseases of the nervous system, rheumatic diseases, etc.
Effects transdermal magnesium
• Deeply cleanses skin pores.
• Increases firmness and smoothness of the skin
• Reduces puffiness.
• Lowers blood pressure.
• Removes excess fluid from the body.
• Eliminates chronic fatigue, gives strength,
• Has a sedative effect.
• Relieves muscle tension and pain.
Are there any special recommendations for use in children?
TV. Care must be taken when using magnesium baths in children: carefully monitor the temperature of the water and the concentration of magnesium. In rare cases, muscle cramps can be observed in case of too long a stay in the bath, therefore, when treating children, it is necessary to monitor the duration of their stay in the bath with magnesium and in no case leave the child alone in the bath. The appearance of any adverse reactions (redness, muscle cramps, diarrhea) indicates the need to reduce the concentration of magnesium in the water.
Tatyana Vladimirovna, thank you for the conversation.
Post Views: 621
Let's get acquainted!
Answer 3 questions and get 5% discount :)
TAKE 1 minute
Let's get acquainted!
Answer 3 questions and get 5% discount :)
TAKE 1 minute
I don't want to meet you and don't need a discount
QUESTION
1/3
YOUR DISCOUNT
1%
Have you tried Epsom salt produced by KAST-EXPO?
Yes, I use a monthly
Yes, several times
is not, I want to try
, I consider for my business
ago
Further
2/3
Your discount
9000 3%For whom do you want to buy magnesium salt?
Personal (adults only)
Family (with children)
Business (online/offline sales)
Gift
Back
Next
QUESTION
3/3
YOUR DISCOUNT
4%
What effect do you expect from English salt?
Reduce weight (fluid withdrawal)
Stress relief
Relax muscles, relieve tension, cramps
Improve adult sleep
For the beauty of skin, hair and nails
sales
I don't expect anything, I just want a discount
Back
Next
Your 5% discount
Promo code 7P2RDQPZ
Is your city Chelyabinsk?
Yes
.