Adhd and childhood obesity
Are Obesity and ADHD Connected? I Psych Central
Genetic inheritance may link ADHD and obesity. Other underlying factors, such as sleep and eating patterns, may also play a role.
Decades of research have shown a strong link between obesity and attention deficit hyperactivity disorder (ADHD) in children and adults.
A 2019 study suggests that about 70% of adults and 40% of children with ADHD have overweight or obesity than those without ADHD.
While it’s unclear whether people with ADHD have obesity because of ADHD or vice versa, certain factors may contribute to both.
A complex mix of genetics and behavior — such as eating habits, exercise, and sleep patterns — underlies the ADHD and higher BMI connection.
The Centers for Disease Control and Prevention (CDC) defines obesity as:
- an adult body mass index (BMI) of 30 or higher per the adult BMI calculator
- a BMI equal to or above the 95th percentile on the growth chart for height, sex, and age for children or teens
Genetic, environmental, and behavioral patterns seem to play a role in connecting ADHD to a higher BMI.
Genetic and environmental factors
A 2019 narrative review suggests that genetic alterations associated with ADHD may lead to environmental factors resulting in obesity. The review also found that a similar neural substrate may underlie genetic risks for ADHD and a higher BMI.
But researchers note that more research is needed on genetic pathways between ADHD and obesity, including possible differences between the sexes.
A 2020 review examining more than 780,000 mother-child pairs concluded that the children of mothers with overweight before pregnancy might have an increased chance of obesity and ADHD.
Researchers suggested that similar genetic pathways for both conditions and environmental factors, such as dietary habits, likely play a role.
Behavioral factors
Unhealthy eating habits and exercise patterns may be more frequent with ADHD.
This may include behaviors such as:
- skipping breakfast
- late-night snacking
- binge eating (without realizing it)
- missing exercise classes or practice due to time management challenges
In a 2019 study, 105 patients with obesity were categorized and examined for diagnoses of childhood or adulthood ADHD, addiction to food, binge eating, and sleep apnea.
Childhood and adult ADHD diagnoses were connected to food addiction and binge eating. No correlation between sleep apnea and ADHD was found.
If you live with ADHD, you may have greater reward responses or dopamine activation associated with food. This biological factor may lead to overeating.
Excessive daytime sleepiness
Sleep disturbances are common in folks with ADHD. Researchers estimate that about 75% of children and adults with ADHD have sleep problems.
One type that people with ADHD may have is excessive daytime sleepiness. This often features in people with ADHD and obesity, which might strengthen the link between them.
While not much is known about how ADHD connects to sleep disturbances, a 2017 study found that adults and children with ADHD and sleep problems report more severe ADHD symptoms.
Excessive daytime sleepiness is often a symptom of sleep apnea, which is common in people with obesity. A 2017 study noted that 3% to 7% of men and 2% to 5% of women with obstructive sleep apnea have obesity.
Conversely, people with obstructive sleep apnea are more likely to have obesity.
Inflammation
The narrative review suggests that inflammation may link ADHD symptoms and obesity. It suggests that inflammation impacts executive functions — such as attention, organization, and planning — and is a characteristic of obesity.
A 2021 review supports that inflammation contributes to obesity and is the link to obesity-related conditions such as type 2 diabetes.
But longitudinal studies are needed to further examine the connection.
ADHD and childhood obesity
Children with ADHD have a higher chance of obesity or overweight than those without.
A 2022 study using information from the 1993 Pelotol (Brazil) birth cohort concluded that ADHD in childhood (age 11) might predict higher BMIs in adulthood (age 22).
Childhood ADHD symptoms may predict a poor diet quality in children, but a poor diet doesn’t seem to cause childhood ADHD, according to a 2019 study.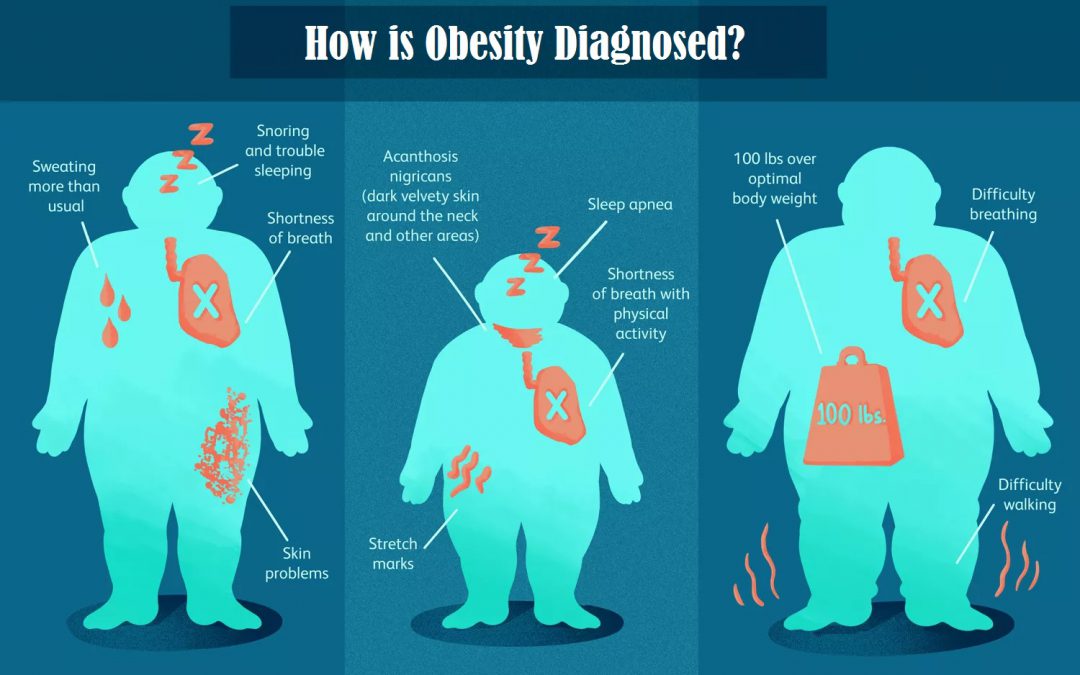
ADHD medication and weight changes
In a 2022 study, nearly 81% of more than 22,000 children with ADHD within the same healthcare system experienced changes in BMI after they started taking ADHD medication.
The researchers found that:
- stimulants led to decreased weight
- antipsychotics and antidepressants led to weight gain
- alpha-agonists led to increased BMI
Researchers suggest that future studies might look at effects over a time period longer than 3 years and across races, ethnic groups, and ADHD subtypes.
A 2015 review found a significant association between obesity and ADHD. It reported that about 70% of adults and 40% of children with ADHD had obesity compared to those without ADHD.
Researchers also found a correlation between ADHD and being overweight — defined in this study as having a BMI greater than or equal to 25 in adults and greater than or a BMI equal to the 85th percentile in children.
Correlations among ADHD subtype, sex, race and ethnicity, and BMI
A 2019 study measured the connection between ADHD type, sex, race and ethnicity, and BMI.
The study looked at a national survey with more than 13,000 people ages 12 to 34 with ADHD and compared the results with those who didn’t have ADHD.
Based on self-reporting, the following conclusions were noted:
- Among those with ADHD inattentive type, European females had higher BMIs.
- ADHD of the primarily hyperactive-impulsive type was associated with higher BMIs among European males and females.
- ADHD of the combined type correlated with higher BMIs for Hispanic American females.
- No ADHD and BMI associations were found for African American males or females or Hispanic American males.
Researchers suggest that the study could not account for these differences. Future studies might consider how sociocultural or genetic differences affect the relationship between ADHD subtype and obesity.
If you have ADHD and are concerned about your BMI, there are strategies you can try lower it.
Consider these tips:
- Set realistic and specific goals.
 If you want to start an exercise routine, instead of trying to work out for 45 minutes to an hour each day, try to walk for 20 to 30 minutes each day. The American Heart Association (AHA) recommends getting at least 150 minutes each week of moderate-intensity exercise. Starting slow can help buildup your endurance, and then you can increase your exercise over time.
If you want to start an exercise routine, instead of trying to work out for 45 minutes to an hour each day, try to walk for 20 to 30 minutes each day. The American Heart Association (AHA) recommends getting at least 150 minutes each week of moderate-intensity exercise. Starting slow can help buildup your endurance, and then you can increase your exercise over time. - Plan your meals. People with ADHD often have trouble staying focused and on task. You might begin a project and forget to eat until you’re overly hungry. This may make you more likely to grab the first thing you can eat, without consideration of calories or fat content. Consider setting aside a time each day to eat. Planning your meals and having them ready to grab can also be helpful.
- Choose healthier options. Focusing on nutrition rather than calorie cutting (particularly for children) might help manage your BMI. Try to avoid processed and sugary foods that increase hyperactivity and weight.
 Consider including more fruits, vegetables, lean meats, and fish.
Consider including more fruits, vegetables, lean meats, and fish. - Practice good sleep hygiene. Getting quality sleep each night can help rejuvenate your body and improve your mood. It might also help you resist the urge to reach for those sugary snacks to stay alert.
- Medication adjustment. If your ADHD medication lists weight gain as a possible side effect, consider talking with a healthcare or mental health professional about adjusting your dose or switching types of medications. They will work with you on what’s best for you and your symptoms.
Does ADHD cause obesity?
No. While research shows a strong association between obesity and ADHD, there’s no evidence that obesity can lead to ADHD or vice versa.
Why are obesity and ADHD often linked?
There’s no direct cause for obesity and ADHD, but contributing factors may include genetics, reward response sensitivity, and different eating and sleep patterns.
Is the connection between ADHD and obesity more likely in children or adults?
The link between obesity and ADHD is stronger in adults but can also be seen in children.
What can you do?
Increasing exercise, improving nutrition, and establishing quality sleep patterns may help with ADHD and high body mass index (BMI).
If you have ADHD and obesity or are overweight, you’re not alone. Research has linked obesity with ADHD for several years.
If you’re concerned and want to lower your BMI, consider a few strategies such as setting weekly or daily goals that are realistic and specific, planning your meals ahead of time, and getting enough sleep.
An accountability partner might also help you sustain your desired habits over time.
It might also help to talk with others who have similar experiences. Unsure where to start? You can check out Psych Central’s page on ADHD resources for help with finding support groups and more.
The Association between ADHD and Obesity: Intriguing, Progressively More Investigated, but Still Puzzling
1. Altfas J.R. Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry. 2002;2:9. doi: 10.1186/1471-244X-2-9. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Altfas J.R. Prevalence of attention deficit/hyperactivity disorder among adults in obesity treatment. BMC Psychiatry. 2002;2:9. doi: 10.1186/1471-244X-2-9. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
2. Hanc T., Cortese S. Attention deficit/hyperactivity-disorder and obesity: A review and model of current hypotheses explaining their comorbidity. Neurosci. Biobehav. Rev. 2018;92:16–28. doi: 10.1016/j.neubiorev.2018.05.017. [PubMed] [CrossRef] [Google Scholar]
3. Cortese S., Moreira-Maia C.R., St Fleur D., Morcillo-Penalver C., Rohde L.A., Faraone S.V. Association Between ADHD and Obesity: A Systematic Review and Meta-Analysis. Am. J. Psychiatry. 2016;173:34–43. doi: 10.1176/appi.ajp.2015.15020266. [PubMed] [CrossRef] [Google Scholar]
4. Nigg J.T., Johnstone J.M., Musser E.D., Long H.G., Willoughby M.T., Shannon J. Attention-deficit/hyperactivity disorder (ADHD) and being overweight/obesity: New data and meta-analysis. Clin. Psychol. Rev. 2016;43:67–79. doi: 10.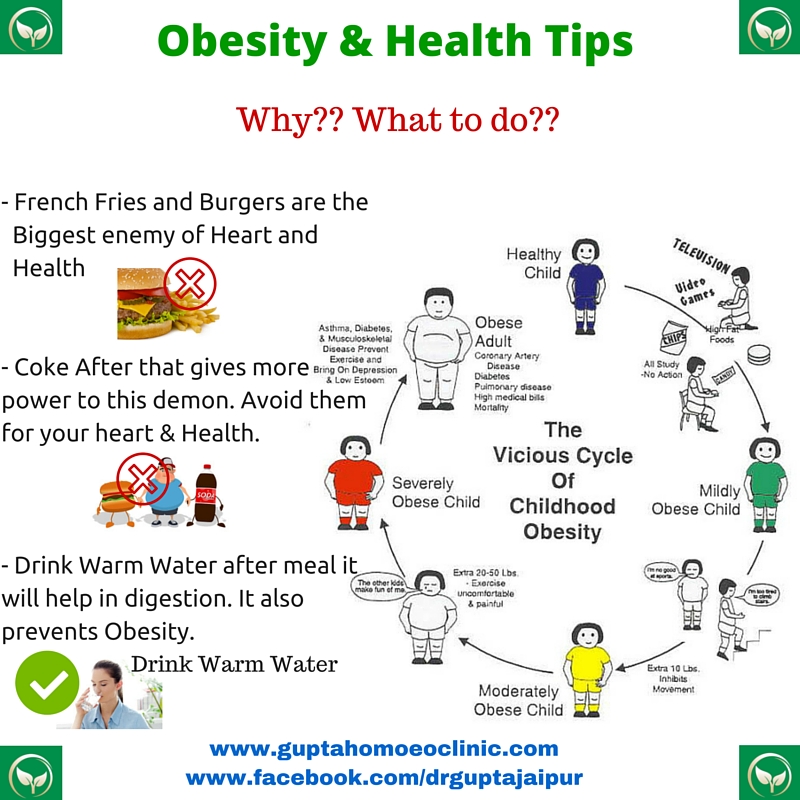 1016/j.cpr.2015.11.005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
1016/j.cpr.2015.11.005. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
5. Inoue Y., Howard A.G., Stickley A., Yazawa A., Gordon-Larsen P. Sex and racial/ethnic differences in the association between childhood attention-deficit/hyperactivity disorder symptom subtypes and body mass index in the transition from adolescence to adulthood in the United States. Pediatr. Obes. 2019;14:e12498. doi: 10.1111/ijpo.12498. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
6. Racicka E., Hanc T., Giertuga K., Brynska A., Wolanczyk T. Prevalence of Overweight and Obesity in Children and Adolescents With ADHD: The Significance of Comorbidities and Pharmacotherapy. J. Atten. Disord. 2018;22:1095–1108. doi: 10.1177/1087054715578272. [PubMed] [CrossRef] [Google Scholar]
7. Cortese S., Ramos Olazagasti M.A., Klein R.G., Castellanos F.X., Proal E., Mannuzza S. Obesity in men with childhood ADHD: A 33-year controlled, prospective, follow-up study. Pediatrics. 2013;131:e1731–e1738. doi: 10.1542/peds.2012-0540. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
doi: 10.1542/peds.2012-0540. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
8. Khalife N., Kantomaa M., Glover V., Tammelin T., Laitinen J., Ebeling H., Hurtig T., Jarvelin M.R., Rodriguez A. Childhood attention-deficit/hyperactivity disorder symptoms are risk factors for obesity and physical inactivity in adolescence. J. Am. Acad. Child Adolesc. Psychiatry. 2014;53:425–436. doi: 10.1016/j.jaac.2014.01.009. [PubMed] [CrossRef] [Google Scholar]
9. Aguirre Castaneda R.L., Kumar S., Voigt R.G., Leibson C.L., Barbaresi W.J., Weaver A.L., Killian J.M., Katusic S.K. Childhood Attention-Deficit/Hyperactivity Disorder, Sex, and Obesity: A Longitudinal Population-Based Study. Mayo Clin. Proc. 2016;91:352–361. doi: 10.1016/j.mayocp.2015.09.017. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
10. Bowling A.B., Tiemeier H.W., Jaddoe V.W.V., Barker E.D., Jansen P.W. ADHD symptoms and body composition changes in childhood: A longitudinal study evaluating directionality of associations.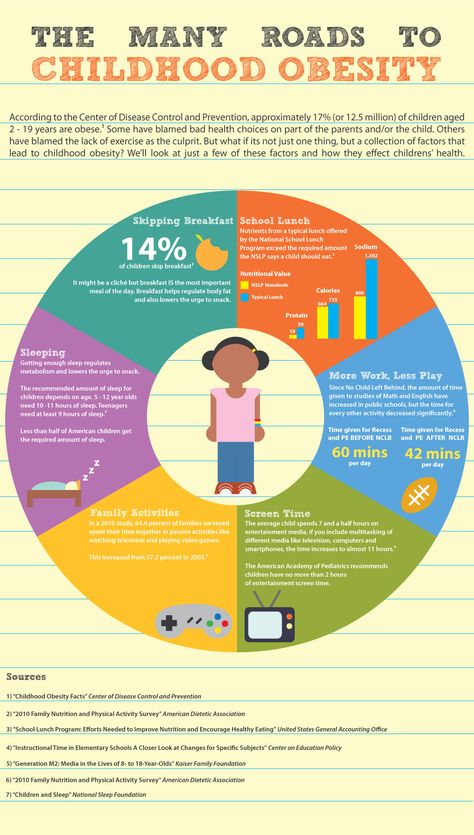 Pediatr. Obes. 2018;13:567–575. doi: 10.1111/ijpo.12288. [PubMed] [CrossRef] [Google Scholar]
Pediatr. Obes. 2018;13:567–575. doi: 10.1111/ijpo.12288. [PubMed] [CrossRef] [Google Scholar]
11. Martins-Silva T., Vaz J.D.S., Hutz M.H., Salatino-Oliveira A., Genro J.P., Hartwig F.P., Moreira-Maia C.R., Rohde L.A., Borges M.C., Tovo-Rodrigues L. Assessing causality in the association between attention-deficit/hyperactivity disorder and obesity: A Mendelian randomization study. Int. J. Obes. 2019 doi: 10.1038/s41366-019-0346-8. [PubMed] [CrossRef] [Google Scholar]
12. Cortese S., Angriman M., Maffeis C., Isnard P., Konofal E., Lecendreux M., Purper-Ouakil D., Vincenzi B., Bernardina B.D., Mouren M.C. Attention-deficit/hyperactivity disorder (ADHD) and obesity: A systematic review of the literature. Crit. Rev. Food Sci. Nutr. 2008;48:524–537. doi: 10.1080/10408390701540124. [PubMed] [CrossRef] [Google Scholar]
13. Cortese S., Vincenzi B. Obesity and ADHD: Clinical and neurobiological implications. Curr. Top. Behav. Neurosci. 2012;9:199–218. doi: 10.1007/7854_2011_154.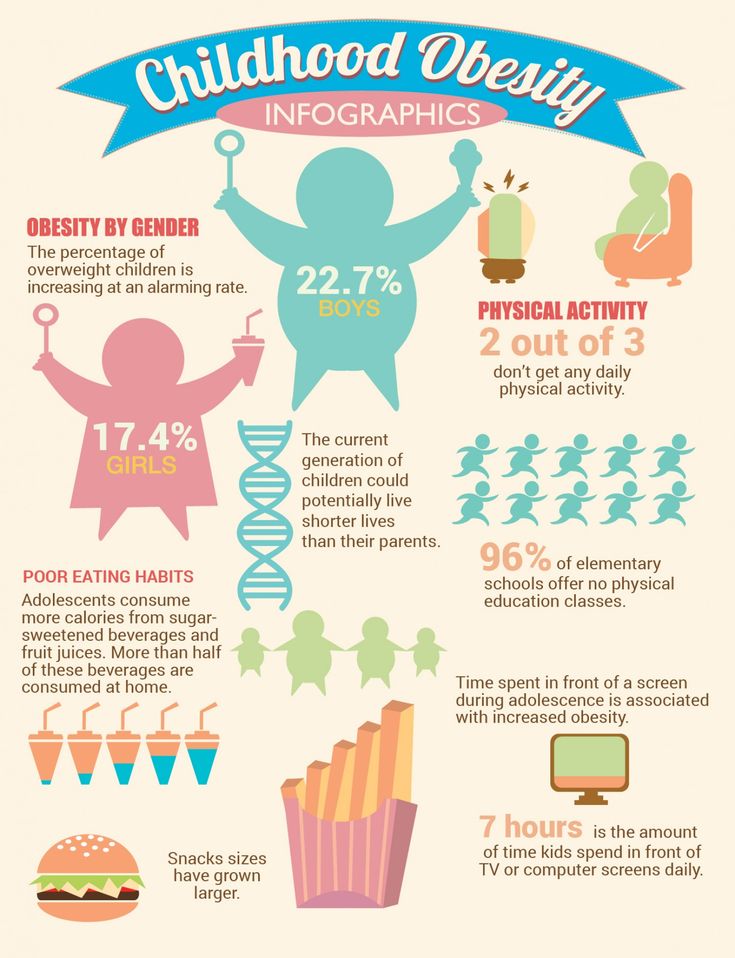 [PubMed] [CrossRef] [Google Scholar]
[PubMed] [CrossRef] [Google Scholar]
14. Chen Q., Kuja-Halkola R., Sjolander A., Serlachius E., Cortese S., Faraone S.V., Almqvist C., Larsson H. Shared familial risk factors between attention-deficit/hyperactivity disorder and overweight/obesity—A population-based familial coaggregation study in Sweden. J. Child Psychol. Psychiatry. 2017;58:711–718. doi: 10.1111/jcpp.12686. [PubMed] [CrossRef] [Google Scholar]
15. Geuijen P.M., Buitelaar J.K., Fliers E.A., Maras A., Schweren L.J.S., Oosterlaan J., Hoekstra P.J., Franke B., Hartman C.A., Rommelse N.N. Overweight in family members of probands with ADHD. Eur. Child Adolesc. Psychiatry. 2019 doi: 10.1007/s00787-019-01331-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
16. Chen Q., Hartman C.A., Kuja-Halkola R., Faraone S.V., Almqvist C., Larsson H. Attention-deficit/hyperactivity disorder and clinically diagnosed obesity in adolescence and young adulthood: A register-based study in Sweden. Psychol. Med. 2019;49:1841–1849.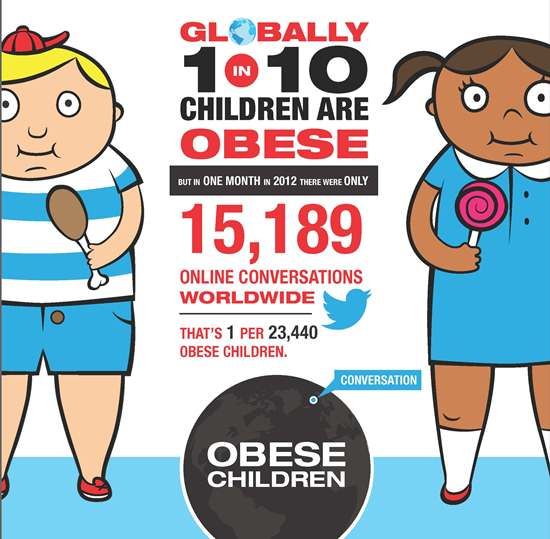 doi: 10.1017/S0033291718002532. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
doi: 10.1017/S0033291718002532. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
17. Demontis D., Walters R.K., Martin J., Mattheisen M., Als T.D., Agerbo E., Baldursson G., Belliveau R., Bybjerg-Grauholm J., Baekvad-Hansen M., et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat. Genet. 2019;51:63–75. doi: 10.1038/s41588-018-0269-7. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
18. Do E.K., Haberstick B.C., Williams R.B., Lessem J.M., Smolen A., Siegler I.C., Fuemmeler B.F. The role of genetic and environmental influences on the association between childhood ADHD symptoms and BMI. Int. J. Obes. 2019;43:33–42. doi: 10.1038/s41366-018-0236-5. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
19. Barker E.D., Ing A., Biondo F., Jia T., Pingault J.B., Du Rietz E., Zhang Y., Ruggeri B., Banaschewski T., Hohmann S., et al. Do ADHD-impulsivity and BMI have shared polygenic and neural correlates? Mol. Psychiatry. 2019 doi: 10.1038/s41380-019-0444-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Psychiatry. 2019 doi: 10.1038/s41380-019-0444-y. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
20. Hanson J.A., Phillips L.N., Hughes S.M., Corson K. Attention-deficit hyperactivity disorder symptomatology, binge eating disorder symptomatology, and body mass index among college students. J. Am. Coll. Health. 2019:1–7. doi: 10.1080/07448481.2019.1583651. [PubMed] [CrossRef] [Google Scholar]
21. Egbert A.H., Wilfley D.E., Eddy K.T., Boutelle K.N., Zucker N., Peterson C.B., Celio Doyle A., Le Grange D., Goldschmidt A.B. Attention-Deficit/Hyperactivity Disorder Symptoms Are Associated with Overeating with and without Loss of Control in Youth with Overweight/Obesity. Child Obes. 2018;14:50–57. doi: 10.1089/chi.2017.0114. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
22. Patte K.A., Davis C.A., Levitan R.D., Kaplan A.S., Carter-Major J., Kennedy J.L. A Behavioral Genetic Model of the Mechanisms Underlying the Link Between Obesity and Symptoms of ADHD. J.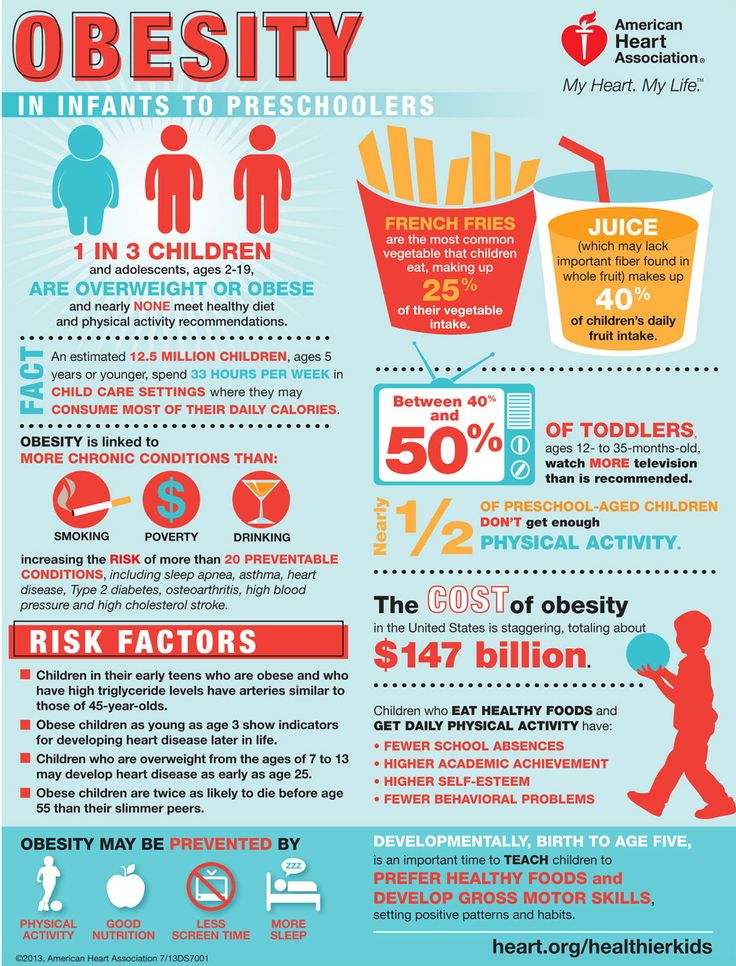 Atten. Disord. 2016 doi: 10.1177/1087054715618793. [PubMed] [CrossRef] [Google Scholar]
Atten. Disord. 2016 doi: 10.1177/1087054715618793. [PubMed] [CrossRef] [Google Scholar]
23. Van der Oord S., Braet C., Cortese S., Claes L. Testing the dual pathway model of ADHD in obesity: A pilot study. Eat Weight Disord. 2018;23:507–512. doi: 10.1007/s40519-017-0375-z. [PubMed] [CrossRef] [Google Scholar]
24. Carter J.C., Stewart D.A., Fairburn C.G. Eating disorder examination questionnaire: Norms for young adolescent girls. Behav. Res. Ther. 2001;39:625–632. doi: 10.1016/S0005-7967(00)00033-4. [PubMed] [CrossRef] [Google Scholar]
25. Rubia K. “Cool” inferior frontostriatal dysfunction in attention-deficit/hyperactivity disorder versus “hot” ventromedial orbitofrontal-limbic dysfunction in conduct disorder: A review. Biol. Psychiatry. 2011;69:e69–e87. doi: 10.1016/j.biopsych.2010.09.023. [PubMed] [CrossRef] [Google Scholar]
26. Fang C.T., Chen V.C., Ma H.T., Chao H.H., Ho M.C., Gossop M. Attentional Bias, “Cool” and “Hot” Executive Functions in Obese Patients: Roles of Body Mass Index, Binge Eating, and Eating Style. J. Clin. Psychopharmacol. 2019;39:145–152. doi: 10.1097/JCP.0000000000001016. [PubMed] [CrossRef] [Google Scholar]
J. Clin. Psychopharmacol. 2019;39:145–152. doi: 10.1097/JCP.0000000000001016. [PubMed] [CrossRef] [Google Scholar]
27. Hanc T., Dmitrzak-Weglarz M., Borkowska A., Wolanczyk T., Pytlinska N., Rybakowski F., Slopien R., Slopien A. Overweight in Boys With ADHD Is Related to Candidate Genes and Not to Deficits in Cognitive Functions. J. Atten. Disord. 2018;22:1158–1172. doi: 10.1177/1087054716676364. [PubMed] [CrossRef] [Google Scholar]
28. Brunault P., Frammery J., Montaudon P., De Luca A., Hankard R., Ducluzeau P.H., Cortese S., Ballon N. Adulthood and childhood ADHD in patients consulting for obesity is associated with food addiction and binge eating, but not sleep apnea syndrome. Appetite. 2019;136:25–32. doi: 10.1016/j.appet.2019.01.013. [PubMed] [CrossRef] [Google Scholar]
29. Tandon P.S., Sasser T., Gonzalez E.S., Whitlock K.B., Christakis D.A., Stein M.A. Physical Activity, Screen Time, and Sleep in Children With ADHD. J. Phys. Act. Health. 2019;16:416–422. doi: 10. 1123/jpah.2018-0215. [PubMed] [CrossRef] [Google Scholar]
1123/jpah.2018-0215. [PubMed] [CrossRef] [Google Scholar]
30. Ahn J.S., Min S., Kim M.H. The Role of Uncontrolled Eating and Screen Time in the Link of Attention Deficit Hyperactivity Disorder with Weight in Late Childhood. Psychiatry Investig. 2017;14:808–816. doi: 10.4306/pi.2017.14.6.808. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
31. Cortese S., Konofal E., Dalla Bernardina B., Mouren M.C., Lecendreux M. Does excessive daytime sleepiness contribute to explaining the association between obesity and ADHD symptoms? Med. Hypotheses. 2008;70:12–16. doi: 10.1016/j.mehy.2007.04.036. [PubMed] [CrossRef] [Google Scholar]
32. Weinberg W.A., Brumback R.A. Primary disorder of vigilance: A novel explanation of inattentiveness, daydreaming, boredom, restlessness, and sleepiness. J. Pediatr. 1990;116:720–725. doi: 10.1016/S0022-3476(05)82654-X. [PubMed] [CrossRef] [Google Scholar]
33. Vgontzas A.N., Bixler E.O., Chrousos G.P. Obesity-related sleepiness and fatigue: The role of the stress system and cytokines. Ann. N. Y. Acad. Sci. 2006;1083:329–344. doi: 10.1196/annals.1367.023. [PubMed] [CrossRef] [Google Scholar]
Ann. N. Y. Acad. Sci. 2006;1083:329–344. doi: 10.1196/annals.1367.023. [PubMed] [CrossRef] [Google Scholar]
34. Fliers E.A., Buitelaar J.K., Maras A., Bul K., Hohle E., Faraone S.V., Franke B., Rommelse N.N. ADHD is a risk factor for overweight and obesity in children. J. Dev. Behav. Pediatr. 2013;34:566–574. doi: 10.1097/DBP.0b013e3182a50a67. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
35. Vogel S.W., Bijlenga D., Tanke M., Bron T.I., van der Heijden K.B., Swaab H., Beekman A.T., Kooij J.J. Circadian rhythm disruption as a link between Attention-Deficit/Hyperactivity Disorder and obesity? J. Psychosom. Res. 2015;79:443–450. doi: 10.1016/j.jpsychores.2015.10.002. [PubMed] [CrossRef] [Google Scholar]
36. Turkoglu S., Cetin F.H. The relationship between chronotype and obesity in children and adolescent with attention deficit hyperactivity disorder. Chronobiol. Int. 2019;36:1138–1147. doi: 10.1080/07420528.2019.1622131. [PubMed] [CrossRef] [Google Scholar]
37. Anand D., Colpo G.D., Zeni G., Zeni C.P., Teixeira A.L. Attention-Deficit/Hyperactivity Disorder And Inflammation: What Does Current Knowledge Tell Us? A Systematic Review. Front. Psychiatry. 2017;8:228. doi: 10.3389/fpsyt.2017.00228. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Anand D., Colpo G.D., Zeni G., Zeni C.P., Teixeira A.L. Attention-Deficit/Hyperactivity Disorder And Inflammation: What Does Current Knowledge Tell Us? A Systematic Review. Front. Psychiatry. 2017;8:228. doi: 10.3389/fpsyt.2017.00228. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
38. Cortese S., Angriman M., Comencini E., Vincenzi B., Maffeis C. Association between inflammatory cytokines and ADHD symptoms in children and adolescents with obesity: A pilot study. Psychiatry Res. 2019;278:7–11. doi: 10.1016/j.psychres.2019.05.030. [PubMed] [CrossRef] [Google Scholar]
39. Langrock C., Hebebrand J., Radowksi K., Hamelmann E., Lucke T., Holtmann M., Legenbauer T., Schmidt B., Frank M., Jockel K.H., et al. Thyroid Hormone Status in Overweight Children with Attention Deficit/Hyperactivity Disorder. Horm. Res. Paediatr. 2018;89:150–156. doi: 10.1159/000485620. [PubMed] [CrossRef] [Google Scholar]
40. Ozcan O., Arslan M., Gungor S., Yuksel T., Selimoglu M.A. Plasma Leptin, Adiponectin, Neuropeptide Y Levels in Drug Naive Children With ADHD. J. Atten. Disord. 2018;22:896–900. doi: 10.1177/1087054715587095. [PubMed] [CrossRef] [Google Scholar]
J. Atten. Disord. 2018;22:896–900. doi: 10.1177/1087054715587095. [PubMed] [CrossRef] [Google Scholar]
41. Cortese S., Castellanos F.X. The relationship between ADHD and obesity: Implications for therapy. Expert Rev. Neurother. 2014;14:473–479. doi: 10.1586/14737175.2014.904748. [PubMed] [CrossRef] [Google Scholar]
42. Levy L.D., Fleming J.P., Klar D. Treatment of refractory obesity in severely obese adults following management of newly diagnosed attention deficit hyperactivity disorder. Int. J. Obes. 2009;33:326–334. doi: 10.1038/ijo.2009.5. [PubMed] [CrossRef] [Google Scholar]
43. Williamson T.M., Campbell T.S., Telfer J.A., Rash J.A. Emotion Self-Regulation Moderates the Association Between Symptoms of ADHD and Weight Loss After Bariatric Surgery. Obes. Surg. 2018;28:1553–1561. doi: 10.1007/s11695-017-3037-3. [PubMed] [CrossRef] [Google Scholar]
44. Mocanu V., Tavakoli I., MacDonald A., Dang J.T., Switzer N., Birch D.W., Karmali S. The Impact of ADHD on Outcomes Following Bariatric Surgery: A Systematic Review and Meta-analysis. Obes. Surg. 2019;29:1403–1409. doi: 10.1007/s11695-019-03735-5. [PubMed] [CrossRef] [Google Scholar]
Obes. Surg. 2019;29:1403–1409. doi: 10.1007/s11695-019-03735-5. [PubMed] [CrossRef] [Google Scholar]
45. Karbasi Amel A., Karbasi Amel S., Erfan A. Effectiveness of Parents-Focused Cognitive-Behavioral Therapy on Attention Deficit Hyperactivity Disorder Symptoms, Obesity and Self-Esteem of Overweight Children with Attention Deficient Hyperactivity Disorder. Adv. Biomed. Res. 2018;7:73. doi: 10.4103/abr.abr_170_17. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
46. Verbeken S., Braet C., Goossens L., van der Oord S. Executive function training with game elements for obese children: A novel treatment to enhance self-regulatory abilities for weight-control. Behav. Res. Ther. 2013;51:290–299. doi: 10.1016/j.brat.2013.02.006. [PubMed] [CrossRef] [Google Scholar]
47. Mayer J.S., Hees K., Medda J., Grimm O., Asherson P., Bellina M., Colla M., Ibanez P., Koch E., Martinez-Nicolas A., et al. Bright light therapy versus physical exercise to prevent co-morbid depression and obesity in adolescents and young adults with attention-deficit / hyperactivity disorder: Study protocol for a randomized controlled trial. Trials. 2018;19:140. doi: 10.1186/s13063-017-2426-1. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Trials. 2018;19:140. doi: 10.1186/s13063-017-2426-1. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
48. Cortese S., Adamo N., Del Giovane C., Mohr-Jensen C., Hayes A.J., Carucci S., Atkinson L.Z., Tessari L., Banaschewski T., Coghill D., et al. Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: A systematic review and network meta-analysis. Lancet Psychiatry. 2018;5:727–738. doi: 10.1016/S2215-0366(18)30269-4. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
49. Mellstrom E., Forsman C., Engh L., Hallerback M.U., Wikstrom S. Methylphenidate and Reduced Overweight in Children With ADHD. J. Atten. Disord. 2018 doi: 10.1177/1087054718808045. [PubMed] [CrossRef] [Google Scholar]
50. Cortese S., Sun S., Zhang J., Sharma E., Chang Z., Kuja-Halkola R., Almqvist C., Larsson H., Faraone S.V. Association between attention deficit hyperactivity disorder and asthma: A systematic review and meta-analysis and a Swedish population-based study. Lancet Psychiatry. 2018;5:717–726. doi: 10.1016/S2215-0366(18)30224-4. [PubMed] [CrossRef] [Google Scholar]
Lancet Psychiatry. 2018;5:717–726. doi: 10.1016/S2215-0366(18)30224-4. [PubMed] [CrossRef] [Google Scholar]
51. Instanes J.T., Klungsoyr K., Halmoy A., Fasmer O.B., Haavik J. Adult ADHD and Comorbid Somatic Disease: A Systematic Literature Review. J. Atten. Disord. 2018;22:203–228. doi: 10.1177/1087054716669589. [PMC free article] [PubMed] [CrossRef] [Google Scholar]
Obesity and diabetes in pregnancy have been linked to an increased risk of ADHD in the child
Pregnant women with obesity and gestational diabetes may be more likely to have a child with attention deficit hyperactivity disorder (ADHD). The combination of these factors almost doubles the chance of having a baby with ADHD, according to a study published in The Journal of Clinical Endocrinology & Metabolism .
During pregnancy, the production of sex hormones and the hormone cortisol increases, which inhibit the action of insulin. This leads to gestational diabetes mellitus (GDM), or gestational diabetes. Studies have shown that GDM is associated with an increased risk of neuropsychiatric disorders in children, such as ADHD. An increase in blood glucose levels can predispose the fetus to stress, chronic inflammation and hypoxia, which can interfere with the development of the child's brain and lead to neurobehavioral disorders. According to data for 2016-2019years, in the United States alone, attention deficit hyperactivity disorder was diagnosed in 6 million children aged 3 to 17 years.
Studies have shown that GDM is associated with an increased risk of neuropsychiatric disorders in children, such as ADHD. An increase in blood glucose levels can predispose the fetus to stress, chronic inflammation and hypoxia, which can interfere with the development of the child's brain and lead to neurobehavioral disorders. According to data for 2016-2019years, in the United States alone, attention deficit hyperactivity disorder was diagnosed in 6 million children aged 3 to 17 years.
Also, one of the factors that have negative consequences for the child is the presence of obesity in the mother. It is one of the main risk factors for neonatal complications, fetal overgrowth, prematurity, as well as adverse consequences for the mental health of the child. Previous studies have described an association between maternal obesity and ADHD in children, and an association has been found in pregnancies complicated by gestational diabetes. About 30 percent of women of reproductive age are obese at their first prenatal visit. In pregnancies complicated by diabetes, this figure rises to 47 percent, and excessive weight gain during pregnancy under these conditions is associated with adverse pregnancy outcomes, such as fetal macrosomia or a large-for-gestational age infant.
In pregnancies complicated by diabetes, this figure rises to 47 percent, and excessive weight gain during pregnancy under these conditions is associated with adverse pregnancy outcomes, such as fetal macrosomia or a large-for-gestational age infant.
Dr. Verónica Perea of the Mutua de Terraza University Hospital, together with colleagues from Spain, studied how GDM and maternal overweight affect the likelihood of developing attention deficit hyperactivity disorder in children later in life, as well as what role this is played by excess weight gain during pregnancy. The cohort study included 1,036 children born in a university hospital from January 1991 to the end of 2008 to mothers with gestational diabetes. 13 percent of them had ADHD. Information about the body mass index (BMI) of women before pregnancy was based on self-report. Among mothers, 1.4 percent were underweight, 52.7 percent were normal, 27.1 percent were overweight, and 18.8 percent were obese. In the last two groups, early diagnosis of GDM (before the 26th week of the term) and insulin therapy during pregnancy were more often observed.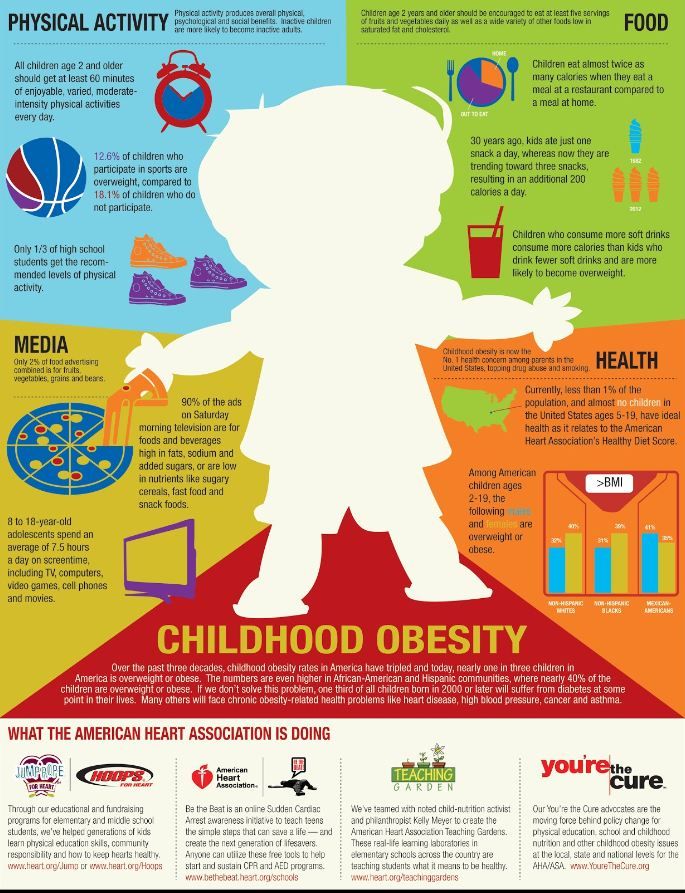
The analysis found that the incidence of ADHD according to maternal BMI was 7.1 percent for underweight women, 11.4 percent for women with normal BMI, 14.2 percent for overweight mothers, and 16.4 percent for obese women (p=0.250). After adjusting (first adjusted model) for year of birth, smoking, maternal age, birth weight, and other factors, maternal obesity showed a higher risk of ADHD (adjusted hazard ratio (HR) = 1.59[95% confidence interval (CI), 1.05-2.41]). When the model (second model) included insulin use during pregnancy and early diagnosis of GDM, the association between obesity and ADHD remained almost unchanged (adjusted HR = 1.66 [95% CI, 1.10-2.67]). But maternal overweight was not associated with attention deficit hyperactivity disorder in either raw data or adjusted models.
Weight gain during pregnancy was not associated with the development of ADHD. At the same time, when analyzing the combined effect of maternal BMI and excessive weight gain during pregnancy, scientists found that children born to mothers who had obesity and excessive weight gain during pregnancy had a greater risk of developing ADHD (adjusted HR = 2.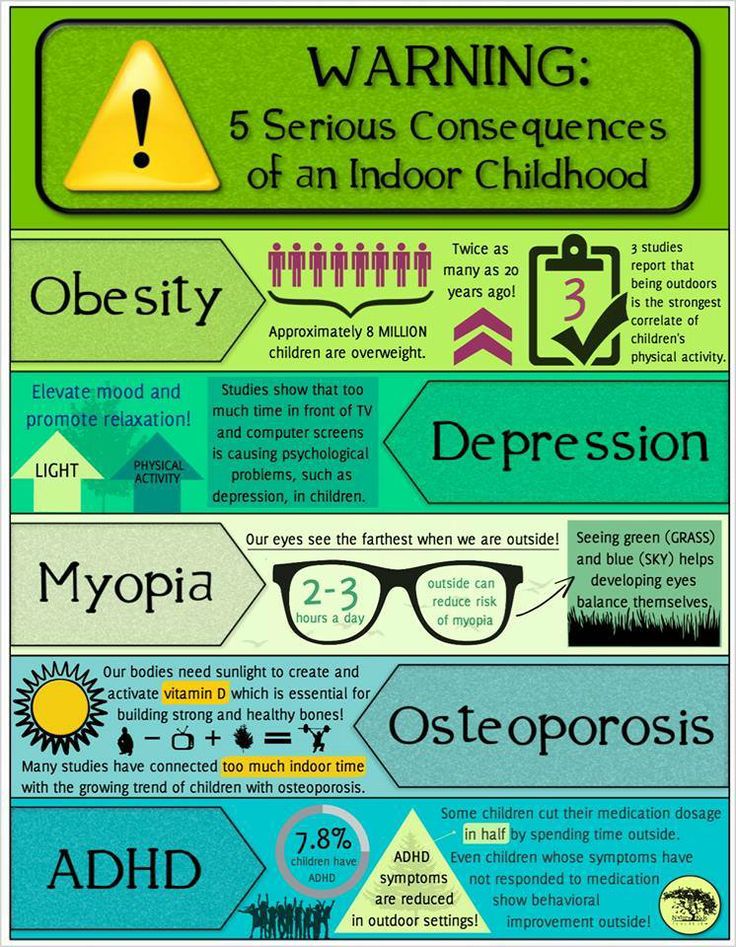 13 [95 percent CI, 1.14–4.01]) than children of non-obese, non-overweight mothers (adjusted HR = 1.36 [95 percent CI, 0.78–2.36]). The same trend was confirmed in the unadjusted and the first adjusted model. However, overweight did not show an association with ADHD, even after including excessive weight gain during pregnancy in the model.
13 [95 percent CI, 1.14–4.01]) than children of non-obese, non-overweight mothers (adjusted HR = 1.36 [95 percent CI, 0.78–2.36]). The same trend was confirmed in the unadjusted and the first adjusted model. However, overweight did not show an association with ADHD, even after including excessive weight gain during pregnancy in the model.
Thus, the study found that children whose mothers were obese and had gestational diabetes were more likely to be diagnosed with ADHD. Also, the highest risk of the syndrome was observed in the children of those women who had both obesity and high weight gain during the term, while obesity without excessive weight gain during pregnancy was no longer associated with ADHD. Scientists note that since this is a survey study, it is impossible to draw conclusions about causal relationships. Neurologists have previously found that parents of children with ADHD have a higher risk of developing Alzheimer's disease than parents whose children do not suffer from ADHD.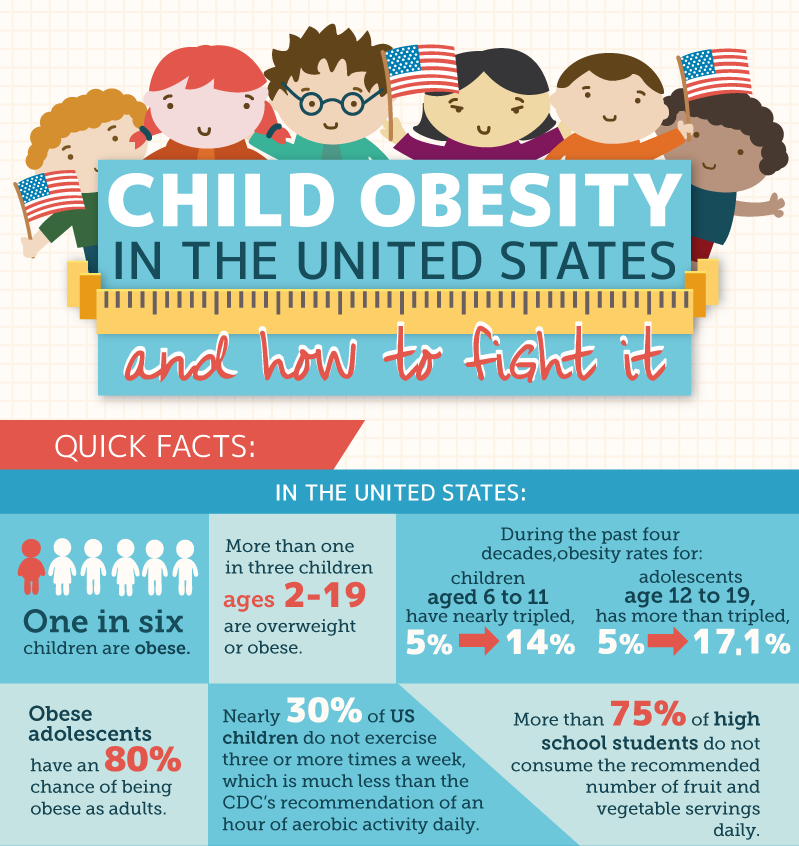
Nadezhda Chekasina
Found a typo? Select the fragment and press Ctrl+Enter.
Attention deficit hyperactivity disorder can cause obesity
Yu.S. Kotikovich
- MORION Publishing House
Summary. Both pathologies have similar genetic, neurobiological and behavioral etiological mechanisms
Attention-deficit/hyperactivity disorder (ADHD) is associated with the development of obesity in women — scientists at the Mayo Clinic, USA, came to this conclusion in the course of a new population-based longitudinal study. The results of the work were published in Mayo Clinic Proceedings.
The prevalence of obesity among children and adults has increased significantly over the past 30 years. In this work, scientists determined that this may be due to changes in the incidence of ADHD. Specialists often lose sight of the facts that indicate an existing relationship between obesity and ADHD, despite the fact that among patients with ADHD the prevalence of obesity is much higher than among healthy people.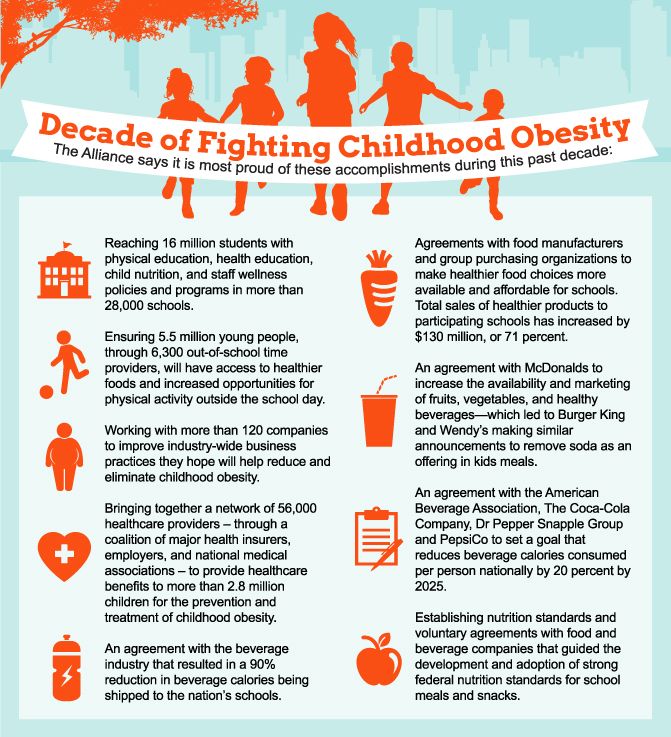 In previous studies, scientists drew attention to the overlap of genetic, neurobiological and behavioral mechanisms for the development of overweight and ADHD. So, the behavioral factor that manifests itself in ADHD as impulsivity and inattention can also be expressed in the form of a lack of regularity in eating. Genetic and neurobiological dysfunctions can be realized through disruptions in the functioning of dopamine systems or the brain's neurotropic factor. Previously, scientists suggested that the similarity of etiological pathways can lead to the parallel development of both obesity and ADHD, and also manifest itself as cognitive hyperstimulation in the first pathology and bouts of overeating in the second.
In previous studies, scientists drew attention to the overlap of genetic, neurobiological and behavioral mechanisms for the development of overweight and ADHD. So, the behavioral factor that manifests itself in ADHD as impulsivity and inattention can also be expressed in the form of a lack of regularity in eating. Genetic and neurobiological dysfunctions can be realized through disruptions in the functioning of dopamine systems or the brain's neurotropic factor. Previously, scientists suggested that the similarity of etiological pathways can lead to the parallel development of both obesity and ADHD, and also manifest itself as cognitive hyperstimulation in the first pathology and bouts of overeating in the second.
The participants in this study were 336 people born between 1976 and 1982 who were diagnosed with ADHD in childhood. Scientists obtained all information about their treatment and anthropometric indicators from medical records. The control group consisted of 665 people without ADHD of the same gender and age.