Obsessive compulsive control disorder
Obsessive-compulsive disorder (OCD) - Symptoms and causes
Overview
Obsessive-compulsive disorder (OCD) features a pattern of unwanted thoughts and fears (obsessions) that lead you to do repetitive behaviors (compulsions). These obsessions and compulsions interfere with daily activities and cause significant distress.
You may try to ignore or stop your obsessions, but that only increases your distress and anxiety. Ultimately, you feel driven to perform compulsive acts to try to ease your stress. Despite efforts to ignore or get rid of bothersome thoughts or urges, they keep coming back. This leads to more ritualistic behavior — the vicious cycle of OCD.
OCD often centers around certain themes — for example, an excessive fear of getting contaminated by germs. To ease your contamination fears, you may compulsively wash your hands until they're sore and chapped.
If you have OCD, you may be ashamed and embarrassed about the condition, but treatment can be effective.
Symptoms
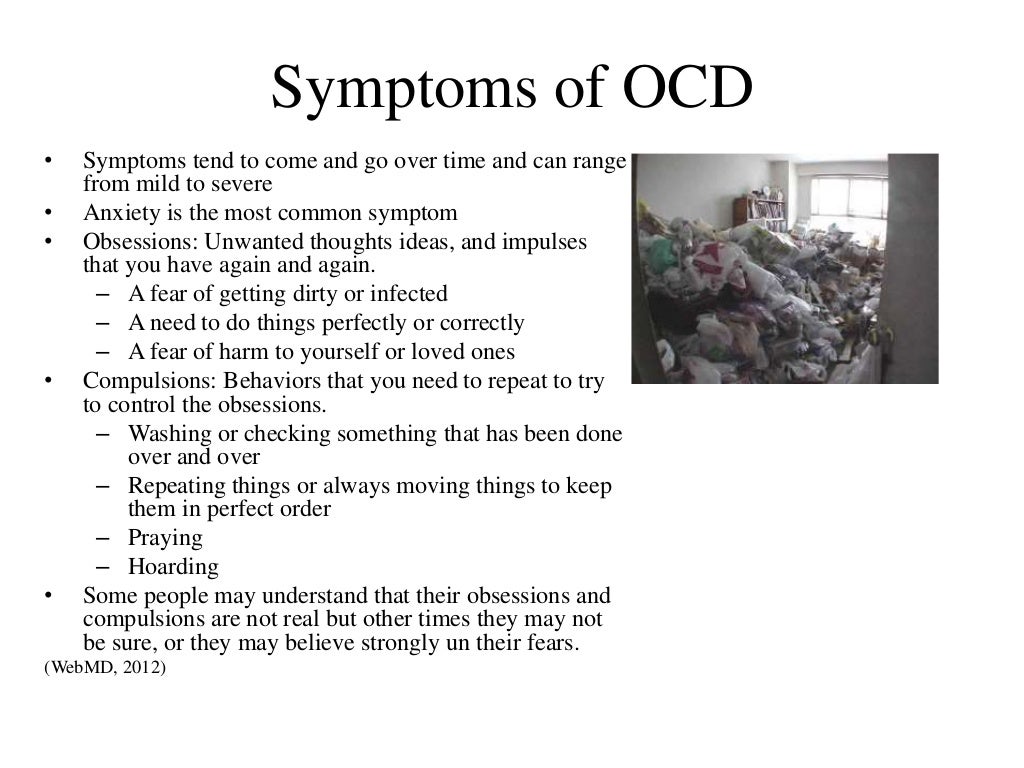
Obsessive-compulsive disorder usually includes both obsessions and compulsions. But it's also possible to have only obsession symptoms or only compulsion symptoms. You may or may not realize that your obsessions and compulsions are excessive or unreasonable, but they take up a great deal of time and interfere with your daily routine and social, school or work functioning.
Obsession symptoms
OCD obsessions are repeated, persistent and unwanted thoughts, urges or images that are intrusive and cause distress or anxiety. You might try to ignore them or get rid of them by performing a compulsive behavior or ritual. These obsessions typically intrude when you're trying to think of or do other things.
Obsessions often have themes to them, such as:
- Fear of contamination or dirt
- Doubting and having difficulty tolerating uncertainty
- Needing things orderly and symmetrical
- Aggressive or horrific thoughts about losing control and harming yourself or others
- Unwanted thoughts, including aggression, or sexual or religious subjects
Examples of obsession signs and symptoms include:
- Fear of being contaminated by touching objects others have touched
- Doubts that you've locked the door or turned off the stove
- Intense stress when objects aren't orderly or facing a certain way
- Images of driving your car into a crowd of people
- Thoughts about shouting obscenities or acting inappropriately in public
- Unpleasant sexual images
- Avoidance of situations that can trigger obsessions, such as shaking hands
Compulsion symptoms
OCD compulsions are repetitive behaviors that you feel driven to perform. These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
These repetitive behaviors or mental acts are meant to reduce anxiety related to your obsessions or prevent something bad from happening. However, engaging in the compulsions brings no pleasure and may offer only a temporary relief from anxiety.
You may make up rules or rituals to follow that help control your anxiety when you're having obsessive thoughts. These compulsions are excessive and often are not realistically related to the problem they're intended to fix.
As with obsessions, compulsions typically have themes, such as:
- Washing and cleaning
- Checking
- Counting
- Orderliness
- Following a strict routine
- Demanding reassurance
Examples of compulsion signs and symptoms include:
- Hand-washing until your skin becomes raw
- Checking doors repeatedly to make sure they're locked
- Checking the stove repeatedly to make sure it's off
- Counting in certain patterns
- Silently repeating a prayer, word or phrase
- Arranging your canned goods to face the same way
Severity varies
OCD usually begins in the teen or young adult years, but it can start in childhood.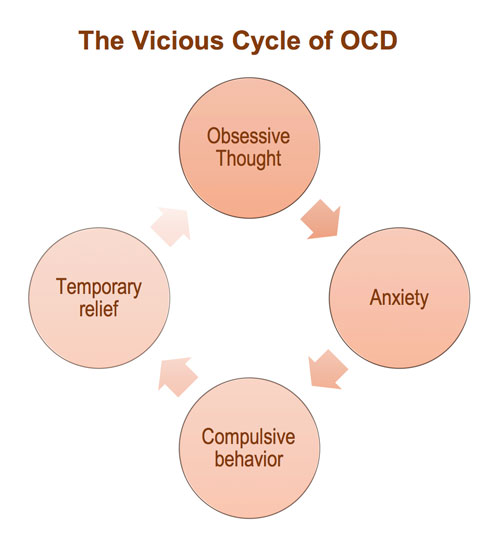 Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
Symptoms usually begin gradually and tend to vary in severity throughout life. The types of obsessions and compulsions you experience can also change over time. Symptoms generally worsen when you experience greater stress. OCD, usually considered a lifelong disorder, can have mild to moderate symptoms or be so severe and time-consuming that it becomes disabling.
When to see a doctor
There's a difference between being a perfectionist — someone who requires flawless results or performance, for example — and having OCD. OCD thoughts aren't simply excessive worries about real problems in your life or liking to have things clean or arranged in a specific way.
If your obsessions and compulsions are affecting your quality of life, see your doctor or mental health professional.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.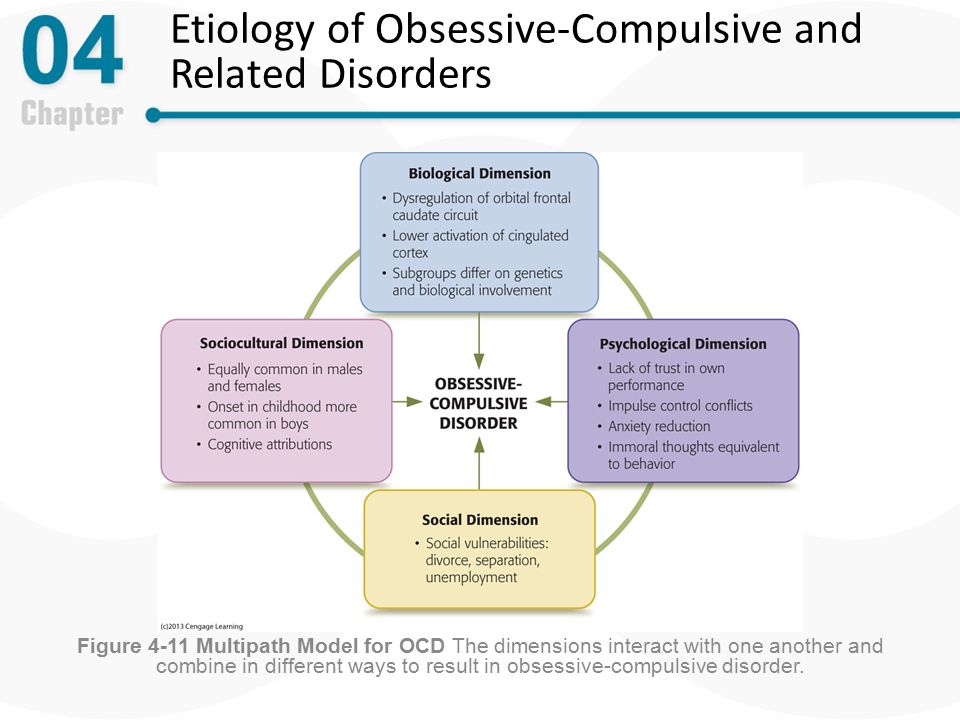 Click here for an email preview.
Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
The cause of obsessive-compulsive disorder isn't fully understood. Main theories include:
- Biology.
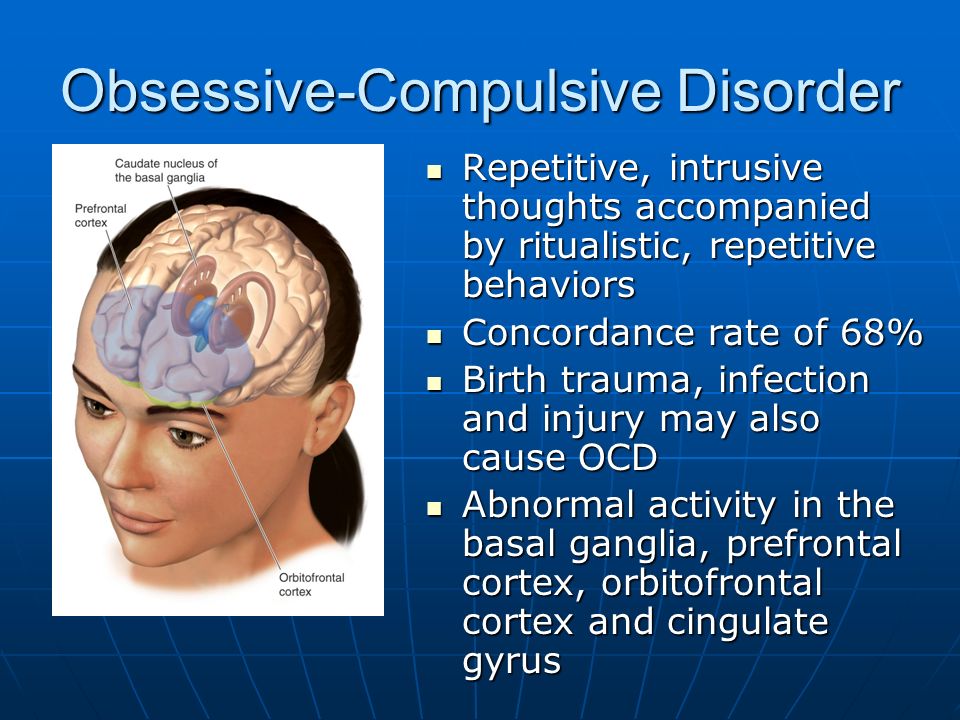 OCD may be a result of changes in your body's own natural chemistry or brain functions.
OCD may be a result of changes in your body's own natural chemistry or brain functions. - Genetics. OCD may have a genetic component, but specific genes have yet to be identified.
- Learning. Obsessive fears and compulsive behaviors can be learned from watching family members or gradually learned over time.
Risk factors
Factors that may increase the risk of developing or triggering obsessive-compulsive disorder include:
- Family history. Having parents or other family members with the disorder can increase your risk of developing OCD.
- Stressful life events. If you've experienced traumatic or stressful events, your risk may increase. This reaction may, for some reason, trigger the intrusive thoughts, rituals and emotional distress characteristic of OCD.

- Other mental health disorders. OCD may be related to other mental health disorders, such as anxiety disorders, depression, substance abuse or tic disorders.
Complications
Problems resulting from obsessive-compulsive disorder may include, among others:
- Excessive time spent engaging in ritualistic behaviors
- Health issues, such as contact dermatitis from frequent hand-washing
- Difficulty attending work, school or social activities
- Troubled relationships
- Overall poor quality of life
- Suicidal thoughts and behavior
Prevention
There's no sure way to prevent obsessive-compulsive disorder. However, getting treatment as soon as possible may help prevent OCD from worsening and disrupting activities and your daily routine.
By Mayo Clinic Staff
Related
Associated Procedures
Obsessive-Compulsive Personality Disorder (OCPD) - Psychiatric Disorders
By
Mark Zimmerman
, MD, Rhode Island Hospital
Last review/revision May 2021 | Modified Sep 2022
View Patient Education
Obsessive-compulsive personality disorder is characterized by a pervasive preoccupation with orderliness, perfectionism, and control (with no room for flexibility) that ultimately slows or interferes with completing a task. Diagnosis is by clinical criteria. Treatment is with psychodynamic psychotherapy, cognitive-behavioral therapy, and selective serotonin reuptake inhibitors (SSRIs).
Diagnosis is by clinical criteria. Treatment is with psychodynamic psychotherapy, cognitive-behavioral therapy, and selective serotonin reuptake inhibitors (SSRIs).
(See also Overview of Personality Disorders Overview of Personality Disorders Personality disorders in general are pervasive, enduring patterns of thinking, perceiving, reacting, and relating that cause significant distress or functional impairment. Personality disorders... read more .)
Because patients with obsessive-compulsive personality disorder need to be in control, they tend to be solitary in their endeavors and to mistrust the help of others.
About 2.1 to 7.9% of the general population are estimated to have obsessive-compulsive personality disorder; it is more common among men.
Familial traits of compulsivity, restricted range of emotion, and perfectionism are thought to contribute to this disorder.
Comorbidities may be present. Patients often also have a depressive disorder Depressive Disorders Depressive disorders are characterized by sadness severe enough or persistent enough to interfere with function and often by decreased interest or pleasure in activities.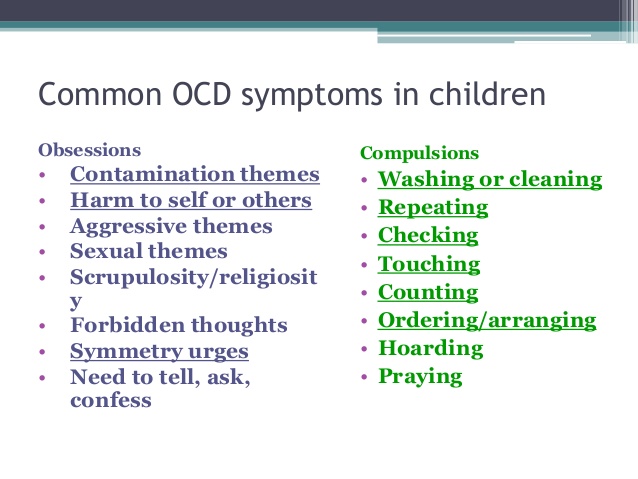 Exact cause is unknown... read more (major depressive disorder or persistent depressive disorder) or an alcohol use disorder Alcohol Toxicity and Withdrawal Alcohol (ethanol) is a central nervous system depressant. Large amounts consumed rapidly can cause respiratory depression, coma, and death. Large amounts chronically consumed damage the liver... read more .
Exact cause is unknown... read more (major depressive disorder or persistent depressive disorder) or an alcohol use disorder Alcohol Toxicity and Withdrawal Alcohol (ethanol) is a central nervous system depressant. Large amounts consumed rapidly can cause respiratory depression, coma, and death. Large amounts chronically consumed damage the liver... read more .
Symptoms of obsessive-compulsive personality disorder may lessen even over a time period as short as 1 year, but their persistence (ie, remission and relapse rates) during the long term are less clear.
In patients with obsessive-compulsive personality disorder, preoccupation with order, perfectionism, and control of themselves and situations interferes with flexibility, effectiveness, and openness. Rigid and stubborn in their activities, these patients insist that everything be done in specific ways.
To maintain a sense of control, patients focus on rules, minute details, procedures, schedules, and lists.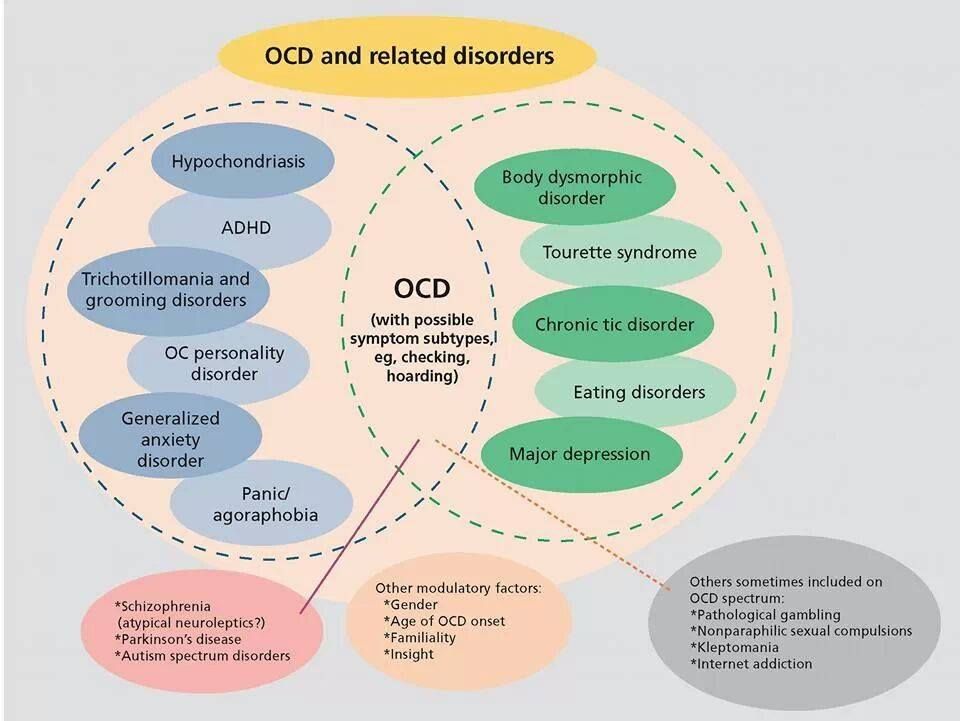 As a result, the main point of a project or activity is lost. These patients repeatedly check for mistakes and pay extraordinary attention to detail. They do not make good use of their time, often leaving the most important tasks until the end. Their preoccupation with the details and making sure everything is perfect can endlessly delay completion. They are unaware of how their behavior affects their coworkers. When focused on one task, these patients may neglect all other aspects of their life.
As a result, the main point of a project or activity is lost. These patients repeatedly check for mistakes and pay extraordinary attention to detail. They do not make good use of their time, often leaving the most important tasks until the end. Their preoccupation with the details and making sure everything is perfect can endlessly delay completion. They are unaware of how their behavior affects their coworkers. When focused on one task, these patients may neglect all other aspects of their life.
Because these patients want everything done in a specific way, they have difficulty delegating tasks and working with others. When working with others, they may make detailed lists about how a task should be done and become upset if a coworker suggests an alternative way. They may reject help even when they are behind schedule.
Patients with obsessive-compulsive personality disorder are excessively dedicated to work and productivity; their dedication is not motivated by financial necessity. As a result, leisure activities and relationships are neglected. They may think they have no time to relax or go out with friends; they may postpone a vacation so long that it does not happen, or they may feel they must take work with them so that they do not waste time. Time spent with friends, when it occurs, tends to be in a formally organized activity (eg, a sport). Hobbies and recreational activities are considered important tasks requiring organization and hard work to master; the goal is perfection.
As a result, leisure activities and relationships are neglected. They may think they have no time to relax or go out with friends; they may postpone a vacation so long that it does not happen, or they may feel they must take work with them so that they do not waste time. Time spent with friends, when it occurs, tends to be in a formally organized activity (eg, a sport). Hobbies and recreational activities are considered important tasks requiring organization and hard work to master; the goal is perfection.
These patients plan ahead in great detail and do not wish to consider changes. Their relentless rigidity may frustrate coworkers and friends.
Expression of affection is also tightly controlled. These patients may relate to others in a formal, stiff, or serious way. Often, they speak only after they think of the perfect thing to say. They may focus on logic and intellect and be intolerant of emotional or expressive behavior.
These patients may be overzealous, picky, and rigid about issues of morality, ethics, and values.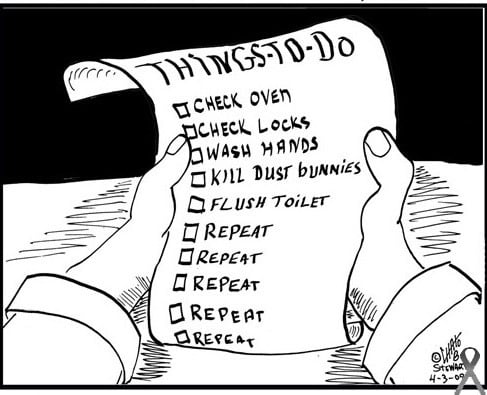 They apply rigid moral principles to themselves and to others and are harshly self-critical. They are rigidly deferential to authorities and insist on exact compliance to rules, with no exceptions for extenuating circumstances.
They apply rigid moral principles to themselves and to others and are harshly self-critical. They are rigidly deferential to authorities and insist on exact compliance to rules, with no exceptions for extenuating circumstances.
For a diagnosis of obsessive-compulsive personality disorder, patients must have
This pattern is shown by the presence of ≥ 4 of the following:
Preoccupation with details, rules, schedules, organization, and lists
A striving to do something perfectly that interferes with completion of the task
Excessive devotion to work and productivity (not due to financial necessity), resulting in neglect of leisure activities and friends
Excessive conscientiousness, fastidiousness, and inflexibility regarding ethical and moral issues and values
Unwillingness to throw out worn-out or worthless objects, even those with no sentimental value
Reluctance to delegate or work with other people unless those people agree to do things exactly as the patients want
A miserly approach to spending for themselves and others because they see money as something to be saved for future disasters
Rigidity and stubbornness
Also, symptoms must have begun by early adulthood.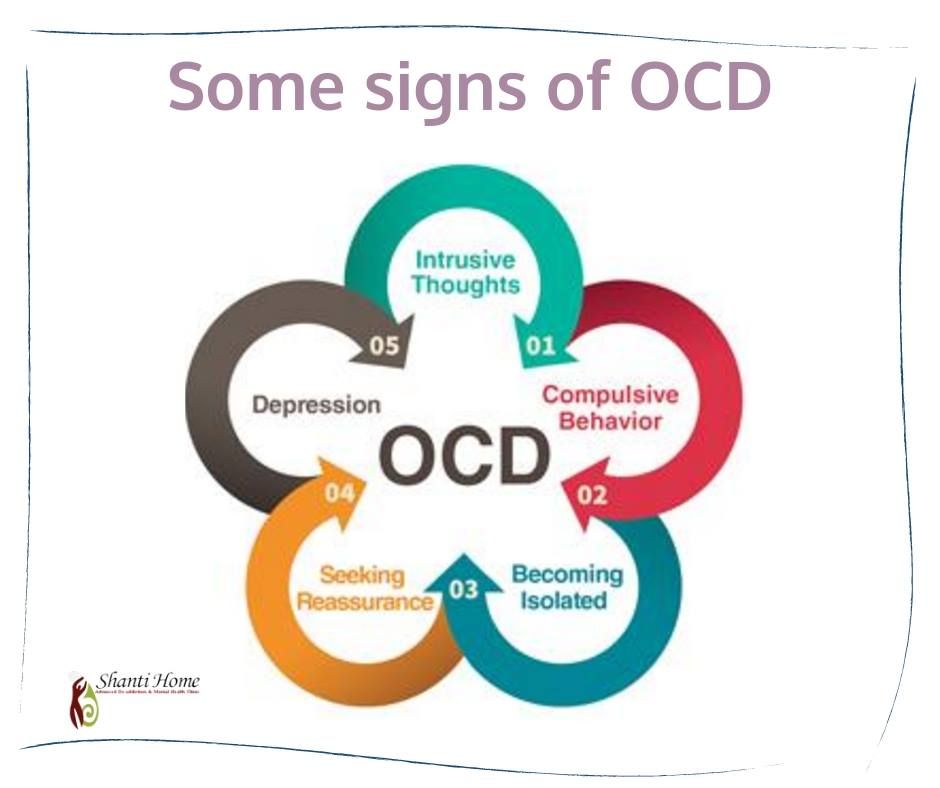
Obsessive-compulsive personality disorder should be distinguished from the following disorders:
Obsessive-compulsive disorder (OCD) Obsessive-Compulsive Disorder (OCD) Obsessive-compulsive disorder (OCD) is characterized by recurrent, persistent, unwanted, and intrusive thoughts, urges, or images (obsessions) and/or by repetitive behaviors or mental acts that... read more : Patients with OCD have true obsessions (repetitive, unwanted, intrusive thoughts that cause marked anxiety) and compulsions (ritualistic behaviors that they feel they must do to reduce their anxiety-related obsessions). Patients with OCD are often distressed by their lack of control over compulsive drives; in patients with obsessive-compulsive personality disorder, the need for control is driven by their preoccupation with order so their behavior, values, and feelings are acceptable and consistent with their sense of self.
Avoidant personality disorder Avoidant Personality Disorder (AVPD) Avoidant personality disorder is characterized by the avoidance of social situations or interactions that involve risk of rejection, criticism, or humiliation.
 Diagnosis is by clinical criteria... read more : Both avoidant and obsessive-compulsive personality disorders are characterized by social isolation; however, in patients with obsessive-compulsive personality disorder, isolation results from giving priority to work and productivity rather than relationships, and these patients mistrust others only because of their potential to intrude on the patients' perfectionism.
Diagnosis is by clinical criteria... read more : Both avoidant and obsessive-compulsive personality disorders are characterized by social isolation; however, in patients with obsessive-compulsive personality disorder, isolation results from giving priority to work and productivity rather than relationships, and these patients mistrust others only because of their potential to intrude on the patients' perfectionism.Schizoid personality disorder Schizoid Personality Disorder (ScPD) Schizoid personality disorder is characterized by a pervasive pattern of detachment from and general disinterest in social relationships and a limited range of emotions in interpersonal relationships... read more : Both schizoid and obsessive-compulsive personality disorders are characterized by a seeming formality in interpersonal relationships and by detachment. However, the motives are different: a basic incapability for intimacy in patients with schizoid personality disorder vs discomfort with emotions and dedication to work in patients with obsessive-compulsive personality disorder.
Psychodynamic psychotherapy
Cognitive-behavioral therapy
Selective serotonin reuptake inhibitors (SSRIs)
General treatment Treatment Personality disorders in general are pervasive, enduring patterns of thinking, perceiving, reacting, and relating that cause significant distress or functional impairment. Personality disorders... read more of obsessive-compulsive personality disorder is similar to that for all personality disorders.
Information about treatment for obsessive-compulsive personality disorder is sparse. Also, treatment is complicated by the patient's rigidity, obstinacy, and need for control, which can be frustrating for therapists.
Psychodynamic therapy and cognitive-behavioral therapy can help patients with obsessive-compulsive personality disorder. Sometimes during therapy, the patient's interesting, detailed, intellectualized conversation may seem psychologically oriented, but it is void of affect and does not lead to change.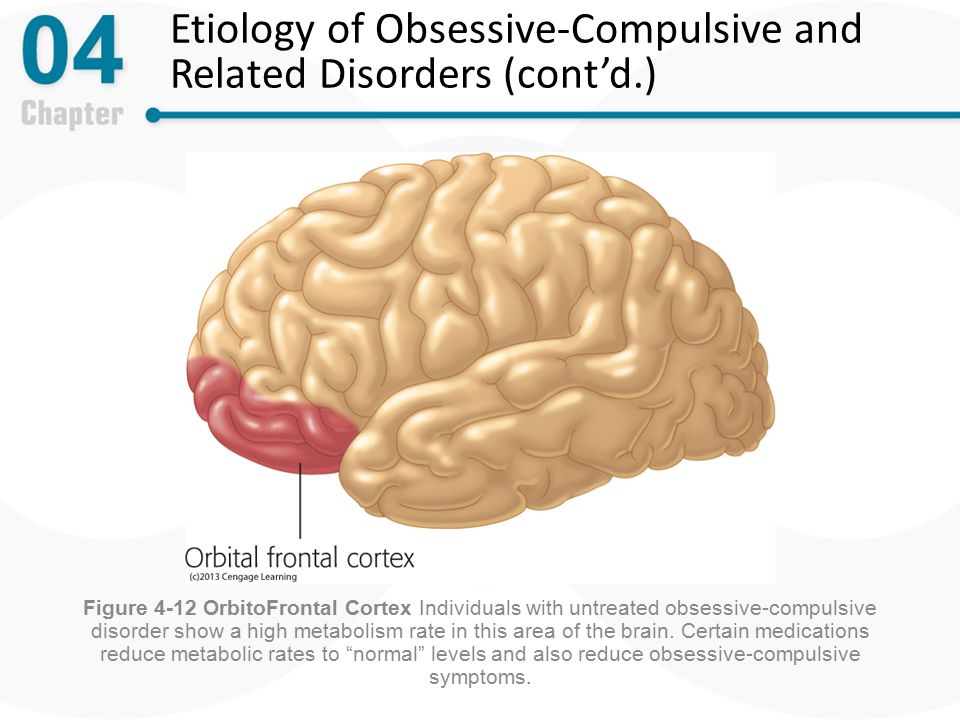
SSRIs Selective Serotonin Reuptake Inhibitors (SSRIs) Several drug classes and drugs can be used to treat depression: Selective serotonin reuptake inhibitors (SSRIs) Serotonin modulators (5-HT2 blockers) Serotonin-norepinephrine reuptake inhibitors... read more may be useful.
NOTE: This is the Professional Version. CONSUMERS: View Consumer VersionCopyright © 2023 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Obsessive Compulsive Disorder (OCD): what it is, symptoms, treatment, advice from a doctor Some people develop symptoms during adolescence, although they are usually diagnosed in adults. Obsessive-compulsive disorder can significantly interfere with a fulfilling life, but treatment can help keep it under control.

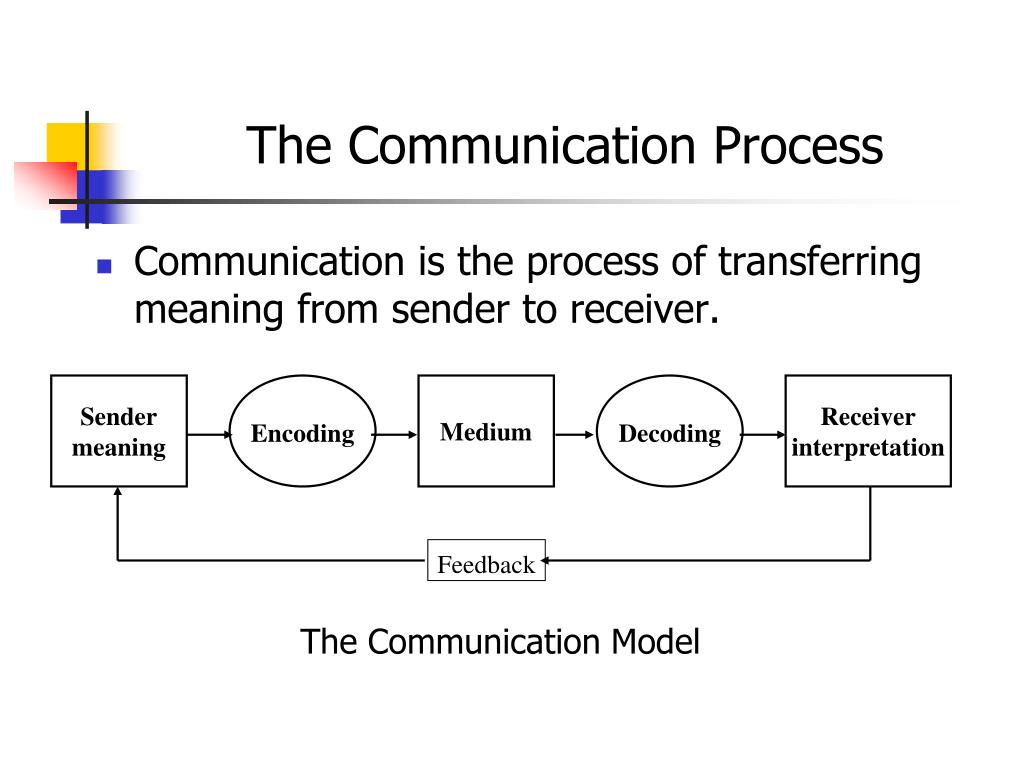
Let's figure out together with experts what are the causes of OCD, what therapeutic and drug methods are used by doctors, and how to behave relatives of a person who has been diagnosed with this disorder.
Contents
- What it is
- Signs and symptoms
- Causes
- Diagnosis
- How to treat
- Advice for relatives 902 support groups
- obsessions - persistent thoughts or impulses, intrusive and unacceptable, causing anxiety;
- compulsions are rituals that are built into the thoughts of a person, he considers it necessary to perform them in response to an obsession.
- present daily;
- are uncontrollable;
- are not enjoyable;
- affect work and social life.
- Checks if the door is locked, if the iron and oven are switched off.
- Unreasonably suspects undiagnosed health conditions such as pregnancy or schizophrenia.
- Afraid of germs, things that can be dirty, constantly cleaning.
- Strives for excessive symmetry and order, feels the need to arrange things in a certain way: by size, colors or alphabet.
- Cannot drive obsessive thoughts and ideas away from himself. Some of them can be violent or disturbing.
- Genetics. If you have OCD in your next of kin—father, mother, brother, and sister—the chances are high that you have it too.
- Structure and function of the brain. In the brain of OCD sufferers, increased activity is recorded in the region of the cortico-striatal-thalamo-cortical loop [5].
- Environment. High levels of stress, increased anxiety can also be a trigger for the development of obsessive-compulsive disorder.
- Concomitant diseases. OCD is often diagnosed in parallel with eating disorders and depression [6].
- Traumatic events. The disorder can be the result of difficult circumstances experienced: psychological and sexual abuse, physical trauma, loss of loved ones.
- Infections. Occasionally, OCD is found in children who have had a streptococcal infection.
 This is called pediatric autoimmune neuropsychiatric disorders.
This is called pediatric autoimmune neuropsychiatric disorders. - Do you experience obsessive thoughts about possible tragic events, death, serious illnesses, fires, accidents?
- Are you concerned about the possibility of contamination with germs and chemicals?
- Do you unnecessarily re-read emails or text messages before or after sending them?
- Are you obsessed with keeping everything in order (cataloging books, perfect stacks of clothes in your closet, sized pencils on your desk)?
- Do you repeat routine activities such as opening a door, putting on your shoes, or getting into bed over and over again until you feel like you've done it "right"?
- Do you have recurring inappropriate thoughts (often of a religious, violent, or sexual nature) that seem intrusive and out of control?
- Do you feel the need to constantly seek confirmation of what you have said or done?
- Do you follow ritualized washing, cleaning or personal grooming habits (eg washing your hands five times in a row)?
- Do you avoid certain colors or numbers because you consider them "unlucky"?
- Do you check your trash before throwing it away to make sure it's clean?
- Do you worry about doing something out of a senseless urge, like pushing a stranger or hitting a loved one?
- Do you check oven handles, door locks and car brakes over and over again in a short period of time?
- Anxiety and Depression Association of America (ADAA) - mental health resources, including conferences of the International OCD Foundation.
There are online support groups for those with the disorder.
- OCD Peers - Virtual support groups (6-10 members) using a HIPAA compliant platform. Video conferences with group mentor, open discussions and agenda. All groups are paid.
- 7 cups - on the platform you can find a volunteer who will be in touch and ready to listen to the problem. This is not a qualified professional, but sometimes speaking out to an attentive listener is just as important as working through a problem with a licensed psychotherapist.
- Support Groups - A free resource with several hundred support groups on a variety of topics, including those for OCD sufferers. Groups are moderated to avoid bullying and inappropriate user reactions.
- HealthUnlocked - literally "health unlocked" - a resource with forums to support people with various diseases. The ROC topic is moderated not only by the portal administrators, but also by representatives of the International ROC Foundation.
- Sexually aggressive, obscene or "dirty" thoughts when visiting relatives or during interviews.
- Blasphemous thoughts in the church.
- The thought of accidentally hurting or even killing a loved one or child.
- The thought of being naked in public or doing something else ridiculous.
- Mental fear of getting dirty, and then taking this dirt with you.
- Mental repetition of certain numbers, colors, etc. within a few hours, which supposedly should bring good luck or prevent misfortune.
- On an airplane, bus, etc.: mental recitation of "special" verses, proverbs, sayings, songs, which should prevent a possible accident.
- Compulsive washing or cleaning
- Painful desire for order
- Painful desire for control
- Pathological accumulation
- Painful desire for repetition and neutralization
- Genetic predisposition
- Neurobiological factors
- Family Features
- Risk factor - injury
- Personal qualities
What is obsessive-compulsive disorder?
Unsplash
Obsessive-compulsive disorder is a common chronic and long-term condition in which a person has uncontrollable repetitive, obsessive thoughts (ideas) and/or actions (behaviors) [1]. OCD is diagnosed in 1.3% of the world's population [2].
Many people confuse OCD with nail biting or negative thinking. Both can be a sign of the disease, but other diagnostic criteria must be taken into account. The obsession is often that a person considers certain numbers or colors to be "good" or "bad". It happens that the habit with OCD is washing your hands repeatedly after touching something that is considered dirty, infected, dangerous. Although the person does not want to think or do it, he is unable to stop [3].
It happens that the habit with OCD is washing your hands repeatedly after touching something that is considered dirty, infected, dangerous. Although the person does not want to think or do it, he is unable to stop [3].
Vladimir BelovMedical psychologist, child psychologist, consultant suicidologist, leading specialist of the Semeynaya clinic network
“Obsessive Compulsive Disorder is a neuropsychological disorder that always includes two components:
The most common connection between these components is that compulsions are actions whose purpose is to neutralize or reduce the distress caused by obsessions. Rituals include such processes as endless washing of hands, double-checking one's own actions or the state of some objects. For some people, these are specific prayers, rituals when going to work, when returning to an apartment, while waiting for transport.
For some people, these are specific prayers, rituals when going to work, when returning to an apartment, while waiting for transport.
Signs and symptoms of obsessive-compulsive disorder
Unsplash
Obsessions - involuntary thoughts and ideas: "I shook hands with a person and now I can get infected with something." This rumination in itself is perfectly normal, but the person with OCD will wash their hands again and again, unable to get rid of it. This is already a compulsion - an obsessive behavior, an individual unstoppable ritual. In the short term, it reduces anxiety, but the thought returns and the action must be repeated. A person feels that he must do it, while he cannot stop. Everyone has recurring habits or thoughts that recur frequently. But in the case of OCD they are:
It's not unusual to wonder if the curling iron is unplugged.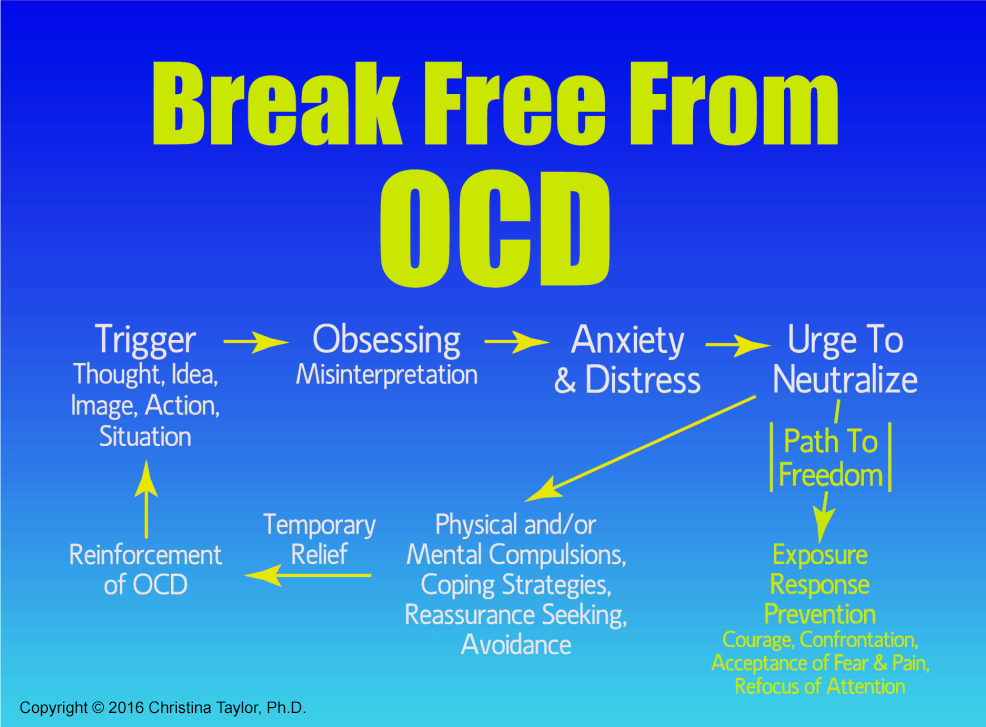 It’s worth worrying if this thought haunts you every day, makes you return home halfway from work and check (more than once, even if you just made sure that the device is not turned on). Obsessive-compulsive disorder comes in many forms, but most cases fall into at least one of the four main categories. The symptoms of OCD are rooted in the person's obsessive behavior. For example, he:
It’s worth worrying if this thought haunts you every day, makes you return home halfway from work and check (more than once, even if you just made sure that the device is not turned on). Obsessive-compulsive disorder comes in many forms, but most cases fall into at least one of the four main categories. The symptoms of OCD are rooted in the person's obsessive behavior. For example, he:
Anastasia AfanasyevaPsychiatrist, psychotherapist, clinical director of the psychological platform Alter
“Intrusive thoughts can occur as part of a variety of disorders, from psychosis to anxiety. To understand what disease these thoughts can be associated with, experts look at how a person treats them. For example, a person in psychosis may not even have a shadow of doubt and discomfort from the fact that the obsessive thought “you can harm your child” is spinning in his head. A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD.
To understand what disease these thoughts can be associated with, experts look at how a person treats them. For example, a person in psychosis may not even have a shadow of doubt and discomfort from the fact that the obsessive thought “you can harm your child” is spinning in his head. A person with OCD cannot have this, he will be frightened by such thoughts, and he will try to do everything to prevent this from happening, for example, remove all sharp objects away from him or not approach the child. Discomfort and the feeling that these thoughts are "inadequate", "wrong" will be an important identifying factor that this is OCD.
People without disorders can also have obsessive thoughts, but normally we quickly cope with them and they do not disturb life, forcing us to rebuild it for ourselves: the thought appeared - the person brushed it off and moved on.
Causes of OCD
Unsplash
Doctors do not give a specific explanation of the causes of the onset and development of OCD. It is most often diagnosed in adolescence and adulthood, with women 1.6 times more likely than men [4]. The factors for the development of the disease include:
It is most often diagnosed in adolescence and adulthood, with women 1.6 times more likely than men [4]. The factors for the development of the disease include:
There is a hypothesis that disturbing deviations developed and persisted in the course of evolution [7]. When people did not have access to modern advances in medicine and hygiene, those who had less contact with a possible source of infection and were constantly on the alert, assessing possible risks and double-checking the safety of food and housing, survived.
Obsessive Compulsive Disorder Diagnostics
Unsplash
All people from time to time find themselves in stressful situations, many people find it helpful to put things in order at home or in the closet, everyone at least once caught himself thinking that he had not turned off the coffee maker in a hurry to a meeting. It doesn't mean you have OCD. Only a doctor can make an accurate diagnosis. Contact a specialist if the above symptoms directly affect your relationship with yourself and others, steal time, do not allow you to relax and enjoy life.
In society, the attitude towards OCD is often superficial and not serious. It is often perceived as a funny feature of a person. But the worsening symptoms cannot be controlled by willpower alone. OCD can be expressed in varying degrees of obsession, and for many it really does not interfere (and may help maintain cleanliness and keep processes under control), but for others it poses a real threat to normal life [8].
There are specialized tests for obsessive-compulsive disorder. Try to answer several questions in the format "often", "rarely", "never", "always":
If most of the described thoughts and situations appear suspiciously often in your daily life, you should consult a general practitioner. He will conduct a physical examination and order blood tests to make sure that the symptoms are not caused by something else. If OCD is suspected, work with a therapist or psychiatrist to talk about life circumstances, feelings, thoughts, and habits.
How to treat obsessive-compulsive disorder
Shutterstock
There is no specific drug that can completely eliminate the symptoms of OCD. But medication support and additional psychological techniques for working on oneself help to work through this problem and keep it under control.
Psychotherapy
Cognitive Behavioral Therapy allows you to change your thinking patterns. Anastasia Afanasyeva believes that one of the most important techniques when working with OCD is distancing, exposing and challenging thoughts: “Distancing is a group of techniques in which we teach a person with OCD to notice intrusive thoughts, realize their ineffectiveness and switch from thinking about them to current ones. affairs. It is important here not to try to start controlling and “not thinking” these thoughts, as this is unrealistic and causes even more anxiety. Instead, for example, we can imagine that thoughts are like an annoying radio broadcast that cannot be turned off, but is not worth listening to.
Exposure is the conscious exposure to uncomfortable situations in order to gradually learn to endure stress and stop using rituals that reduce anxiety in the moment, such as double-checking, washing hands, avoiding sharp objects.
Challenging and checking the reality of thoughts helps to understand that often a thought is just a thought and not every thought that comes to mind is worth believing. To assess how true this idea is, you can write it down on a piece of paper and give facts for and against its correctness.
Relaxation
Anxiety and obsessive thoughts are inevitably associated with tension in the body. Available meditation techniques, as well as massage and yoga classes, help to consciously look at the circumstances and cope with stress.
Anastasia Afanasyeva:
“In general, working with anxiety disorders always involves homework, as people learn to cope with their anxiety not only in the psychologist's office, but also in situations that arise in everyday life. Mostly it's working with thoughts and changing behavioral strategies that support OCD or reduce anxiety for only a short time.
The most common treatment for OCD involves individual sessions with a psychotherapist. There are practically no therapy protocols with proven efficacy for groups.”
Medicines
When taking drugs, you can achieve a stable remission. The timing of drug treatment will be determined by the attending physician. Do not stop taking antidepressants at the first sign of improvement.
Vladimir Belov:
“First of all, we need both a psychiatrist and a medical psychologist/psychotherapist. Because, on the one hand, cognitive-behavioral therapy is used, which is quite effective and has a lot of scientific evidence: exposure and prevention of reactions and rituals. This program goes on for several months and is combined with drugs. First of all, these are antidepressants - selective serotonin reuptake inhibitors and atypical antipsychotic drugs. Much depends on the condition of the patient and the severity of the process in which he is.
What to do for relatives of an OCD patient
Unsplash
People who live near a person with OCD often find themselves in difficult conditions. They want to help by interrupting the compulsive manifestations of a loved one, which can create an even more stressful situation for him. But it is also not worth closing your eyes to the disease. Psychologists advise updating it, pronouncing the problem. Develop the emotional intelligence of a loved one: let's understand that he can safely talk to you about any of his feelings. Emphasize that you are always ready to listen and help: “I am with you, we will deal with this problem together.”
Anastasia Afanasyeva:
“If someone in your family suffers from OCD, one of the important tasks that you face is to stay out of the anxiety maintenance cycle. For example, one should not encourage the desire for excessive cleanliness, endless washing of clothes, washing hands, constant fruitless visits to doctors, one should not participate in rechecking any facts. You need to understand that this does not help a loved one cope with anxiety, but reinforces a non-working pattern of behavior and serves as proof that such behavior and thoughts are justified.
Forums, support groups for people with OCD
Unsplash
The best option is to contact a trusted doctor and treat according to his recommendations. In addition to medicines and work with a specialist, the fulfillment of independent tasks plays an important role. It is important for people with OCD to talk about the problem and see the support of others. Like-minded forums often help. You can join thematic groups on social networks or contact volunteers:
Share
Materials for Article
Authors
Tags
Irina Rudevich
Obsessive Compulsive Disorder | The CALDA Clinic
Treatment Options: Obsessive-Compulsive Disorder
Approximately 2-3 percent of all people have an obsessive-compulsive disorder at some time in their lives. Among them are many celebrities: “When I am under stress, the same thought constantly revolves in my head, because I am afraid that otherwise something bad will happen,” singer Camila Cabello admits to Cosmopolitan magazine. The star of the musical Mamma Mia, Amanda Seyfried, also openly admits her obsessive-compulsive disorder and explains that she treated him with antidepressants for more than eleven years.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder, formerly also called obsessive-compulsive disorder, is a serious mental illness. Patients perform repetitive unwanted actions and "rituals" accompanied by corresponding negative or dangerous thoughts. The disease usually begins around the age of 20. The first symptoms may also appear during puberty or during childhood. Even healthy people can experience temporary compulsions. For example, many people are familiar with anxious thoughts that arise after leaving the house, such as “Did I turn off the coffee maker, turn off the light, lock the door, etc.?”. Despite the fact that a person knows for sure that everything has been done, he has a short desire to double-check again. Most people manage to calm down in such a situation, and only a few really "bother".
More than just a fad
However, people with obsessive-compulsive disorder are usually quite aware that their obsessive thoughts are far from reality and exaggerated and that obsessive actions are useless or even harmful. However, unlike healthy people, they do not manage to reset this obsession. Patients who try to stop unwanted "rituals" experience a very strong tension that they cannot endure for a long time. Therefore, in order to reduce the internal pressure, they soon return to harmful thoughts and actions. Despite the fact that they are illogical and often quite unpleasant, the patient still returns to obsessive thoughts and compulsive actions again and again in a stereotypical manner for several days a week or even several times a day, often for hours. This creates a vicious circle that is extremely painful for the patient and greatly impairs the quality of his daily life, well-being and performance.
How does OCD manifest itself?
Obsessive-compulsive disorder can manifest itself in obsessive thoughts and/or obsessive actions (compulsions). In most cases, obsessive thoughts and compulsions occur at the same time. Depending on the primary symptoms, obsessive-compulsive disorder is divided into three types:
Obsessive-compulsive disorder. Important features:
- mostly intrusive thoughts or ruminations;
- mostly compulsive actions;
- mixed obsessive thoughts and actions. Obsessive-compulsive disorder with predominance of obsessive thoughts or reflections Intrusive thoughts are usually negative, distressing, and very disturbing to the person. They are often in the form of "mental spirals". In this sense, one can speak of obsessive thoughts. Intrusive thoughts are usually perceived by people as belonging to themselves. At the same time, a person in most cases recognizes the meaninglessness and uselessness of these thoughts. But he can't get rid of them. This can lead to the impossibility of making even simple everyday decisions, since it is necessary to first weigh all possible, including completely irrational, alternatives.
Symptoms. Examples of obsessive thoughts
Obsessive-compulsive thoughts are characterized by anxiety, threat, often contradiction and inconsistency with the situation in which the person really is. In particular, mental urges to act are often perceived as extremely frightening and are usually not put into practice.
Typical examples of obsessive thoughts or obsessive impulses
Obsessive-compulsive disorder with predominance of obsessive actions
Obsessive-compulsive disorder can also be characterized by repetitive rituals and actions that the patient cannot avoid. Typical examples:
Fearing possible infections, patients wash their hands many times a day with soap and water, take a shower several times, wipe their skin with hard brushes, constantly wash and change clothes, endlessly clean the apartment, disinfect doorknobs, work surfaces, objects, etc.
Items must be placed, arranged or assembled in a very specific order or manner. They must match a certain size, color, quantity, theme, symmetry, etc. This correspondence is regularly rechecked and infinitely corrected.
The patient constantly checks to see if the door is locked, if the windows are closed, if electrical appliances are turned off, if the faucet is leaking, etc.
Because of the fear of throwing away something important, the patient accumulates everything, even unnecessary items and rubbish. If something is thrown away, there is often a strong urge to search the trash cans to make sure nothing important has been thrown away.
In order to prevent imaginary dangers, catastrophes, etc., the patient is forced to repeat certain actions in a certain amount and in a certain order over and over again. This should help prevent the impending "danger". For example, the patient may forbid himself from touching certain tiles, stones, patterns, and so on. or requires himself to take ten steps back fifty times, say a "special" saying seven times, and so on.
Obsessive-compulsive disorder with obsessive thoughts and actions
In more than 90%, that is, in the vast majority of cases, obsessive thoughts and obsessive actions occur simultaneously. This means that the majority of all patients suffer from obsessive-compulsive disorder, in which there are both painful obsessive-compulsive thoughts and stereotypical compulsive actions.
Obsessive-compulsive disorder: impact on daily life
Obsessive-compulsive disorder is not a quirk of some people who may appear slightly superstitious, overly clean, or especially tidy. This is a serious disease in which people cease to control their thoughts and actions, even if they really want to, and because of which they suffer painfully. It is not uncommon for sufferers to waste several hours a day performing compulsive acts and tormenting themselves with intrusive thoughts. This not only burdens daily life and reduces the patient's ability to work, but also has a huge impact on his social environment, i.e. parents, partners, children, etc. Normal life becomes impossible for long periods of time, causing close family members to leave at some point and marriages to fall apart. In addition to serious psychological and social consequences, there are usually complaints about the physical condition. Serious skin diseases can occur, especially when the disease is accompanied by an obsessive desire to wash and clean.
Causes of OCD
The exact causes of OCD are not yet clearly understood. However, certain factors have been identified that are known to be particularly conducive to the development or maintenance of OCD. As a rule, the development of OKR requires the combination of several factors. The importance of individual factors for each individual patient is individual. The most important risk factors for developing obsessive-compulsive disorder are:
Research shows that heredity does play a role in the development of OCD. Although the disease is not directly transmitted, the risk of a child getting OCD has been shown to increase if one or both parents have OCD. This is also supported by the results of twin studies.
Imaging techniques have also shown that metabolism and brain activity in certain areas of the brain are markedly increased in people with OCD. In particular, it was possible to detect anomalies in the basal ganglia, which, among other things, are responsible for motor processes. In addition, the balance of serotonin is disturbed.
The environment in which a person grows up has a significant impact on the development of personality. A parenting style with high academic demands, strict assessment models, and perfectionist demands, as well as "fearful" parenting methods in which the child is overprotective and constantly protected from all sorts of adversity, can all contribute to the development of obsessive-compulsive disorders.
Also important risk factors for the development of obsessive-compulsive disorders are experienced trauma or mental overload. Excessively stressful events such as violence, abuse, rape, death of a loved one, etc. can unsettle a person and often cause a strong sense of insecurity and insecurity. Understandably, there is also a growing desire for control and security. The performance of "protective", "neutralizing", or "cleansing" compulsions and rituals gives the sufferer a sense of control over a situation in which they would otherwise feel helpless.
Last but not least, individual personality structure also determines to some extent whether a person develops obsessive-compulsive disorder. People who are inherently fearful, vulnerable, unstable, or overly sensitive have a higher risk of developing obsessive-compulsive disorder than confident and calm individuals.
Common comorbidities of obsessive-compulsive disorder
Obsessive-compulsive disorders are often diagnosed together with other mental and dermatological diseases. The most common comorbidities associated with obsessive-compulsive disorder include:
— Depressive moods and depressions
— Eating disorders
— Anxiety disorders
— Social phobias
—Post-traumatic stress disorders0002 -Dermatillomania and trichotillomania
impulse control disorders in which the patient repeatedly scratches, pinches and injures the skin or pulls out hair, eyebrows or eyelashes.
- Dysmorphophobic disorder
distorted perception of one's own body, in which a slight "anomaly" is regarded as a completely disfiguring feature, and there is an excessive concern for an imagined flaw.
- Atopic dermatitis and other skin diseases
eczema occurs mainly in compulsive washing syndrome due to persistent over-irritation of the skin.
What are the treatments for OCD?
People with OCD know that their thoughts, actions, and rituals are irrational, but are unable to deal with them on their own. As a rule, they are very ashamed of this and try their best to hide their suffering from others. Therefore, obsessive-compulsive disorders are often diagnosed very late. On average, it takes 10 years for patients to seek professional help, but periods of 20 to 30 years are also not uncommon. Often patients are forced to see a doctor not even by the obsessive-compulsive disorder itself, but by a concomitant disease, such as severe dermatitis. At this stage, the disease has usually already taken root, and the symptoms have greatly increased both in number and severity.
Complex causes require complex treatment at multiple levels
As with most diseases, it is best to start treatment as early as possible if you have OCD. However, even at an extended stage, very good therapeutic results can still be achieved. The multimodal approach, combining a variety of proven therapeutic options, has proven to be particularly effective. It allows you to accurately recognize many different individual causes of the disease and provide optimal treatment for the patient at every stage and at different levels. In addition, this technique allows you to recognize and effectively eliminate any individually caused physical problems and imbalances and professionally treat all associated diseases.
Modern treatments for obsessive-compulsive disorder have so far mainly involved the use of psychotherapy and psychotropic drugs.
Everything is different with us!
The CALDA concept: Let us help you!
As a client of the CALDA clinic, you are assigned a 1:1 individual therapy based on the CALDA concept, which is tailored specifically to your needs. It is a personalized, highly effective, holistically oriented, ultra-precise therapy: scientifically based methods of classical medicine are combined with specially approved therapies of complementary, traditional Chinese (TCM) and orthomolecular medicine.
Your advantage: Treatment with the CALDA concept works very effectively at different levels of the body and is problem oriented. As a result, amazing results can be achieved in a short time - and often without the use of psychotropic drugs!
CALDA concept
Our motto and guarantee:
we treat the causes, not the symptoms!
If possible, we work without psychotropic drugs!
Our time and all our know-how is an exclusive service for a specific client.