Zoloft off label uses
Off-Label Applications for SSRIs | AAFP
KIMBERLY J. STONE, LCDR, MC, USNR, ANTHONY J. VIERA, LCDR, MC, USNR, AND CHRISTOPHER L. PARMAN, LCDR, MC, USNR
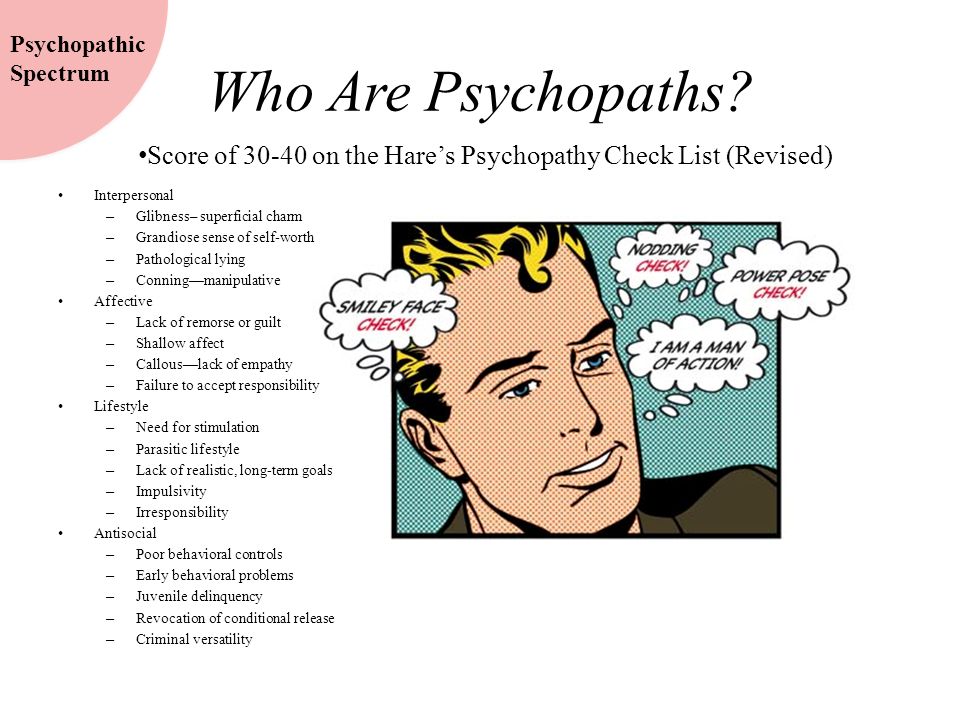
Selective serotonin reuptake inhibitors (SSRIs) are widely used because of their safety, tolerability, and demonstrated efficacy across a broad range of clinical conditions. Medical literature supports the use of SSRIs for the treatment of many conditions outside of the indications approved by the U.S. Food and Drug Administration. SSRIs offer a reasonable alternative to traditional therapy for generalized anxiety disorder. A side effect of SSRIs coincidentally provides therapy for premature ejaculation. SSRIs may reduce the frequency and severity of migraine headaches and are possibly effective in reducing the pain of diabetic neuropathy.
When taken in combination with tricyclic antidepressants, SSRIs offer more potent therapy for fibromyalgia than either agent alone. SSRIs appear to be effective in some patients with neurocardiogenic syncope that is refractory to standard therapies. Clinical experience supported by ongoing research continues to expand on the broad array of therapeutic applications for this class of medication.
Selective serotonin reuptake inhibitors (SSRIs) were initially developed to relieve depression and have become the most commonly prescribed class of antidepressants.1 SSRIs block the reuptake of serotonin at the presynaptic neuron, with minimal or no effect on norepinephrine or dopamine. This narrow mechanism of action confers similarity of efficacy and tolerability with few side effects.1
The following five SSRIs have been approved by the U.S. Food and Drug Administration (FDA) for use in the United States: citalopram (Celexa), fluoxetine (Prozac), fluvoxamine (Luvox), paroxetine (Paxil), and sertraline (Zoloft).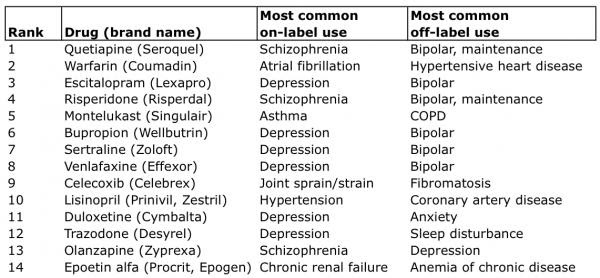 Although the FDA has approved these SSRIs for treatment of a variety of conditions, the medical literature supports their use for a number of “off-label” indications. Off-label use does not imply improper or illegal use.2 The FDA cannot give approval for further indications until it has reviewed new efficacy and safety data provided by the pharmaceutical companies.
Although the FDA has approved these SSRIs for treatment of a variety of conditions, the medical literature supports their use for a number of “off-label” indications. Off-label use does not imply improper or illegal use.2 The FDA cannot give approval for further indications until it has reviewed new efficacy and safety data provided by the pharmaceutical companies.
The use of a well-documented therapy that lacks a specific “labeling” should not be precluded. The decision to prescribe a given medication should be based on the available evidence and a careful consideration of the potential risks and benefits in the context of the individual patient.
This article reviews the use of SSRIs for six conditions commonly managed by family physicians: generalized anxiety disorder, premature ejaculation, migraine headache, diabetic neuropathy, fibromyalgia, and neurocardiogenic syncope (Table 1).3–20
| Condition | Medication and recommended dosages | Efficacy/recommendations | Level of evidence |
|---|---|---|---|
| Generalized anxiety disorder | Fluvoxamine (Luvox), 50 to 300 mg daily 3,4 | Effective; may be a good long-term alternative to benzodiazepines or other anxiolytics | A: RCT |
| Paroxetine (Paxil), 20 to 60 mg daily (generalized anxiety disorder is not an off-label use)5 | — | A: RCT | |
| Premature ejaculation | Paroxetine, 20 mg daily or as needed a few hours before anticipated sexual activity6,7 | Effective; consider as first-line treatment | A: RCT |
| Sertraline (Zoloft), 25 to 50 mg daily or as needed a few hours before anticipated sexual activity6,8,9 | |||
| Fluoxetine (Prozac), 20 mg daily6 | |||
| Migraine headaches (prophylaxis) | Fluoxetine, 20 to 40 mg daily10–12 | May be useful if patient cannot use standard prophylactic agents or if other agents fail; good choice if patient has concomitant depression or other illness treatable with SSRI | A: RCT |
| Diabetic neuropathy | Paroxetine, 40 mg daily13 | Possibly effective; other drugs should be considered first. One meta-analysis found no difference between placebo and SSRIs. One meta-analysis found no difference between placebo and SSRIs. | B: lower quality RCT |
| Fibromyalgia | Fluoxetine, 20 mg daily14,15 | Possibly effective, particularly when combined with amitriptyline (Elavil) | B: lower quality RCT |
| Citalopram (Celexa), 20 to 40 mg daily16,17 | Studies on citalopram showed no significance | B: lower quality RCT | |
| Neurocardiogenic syncope | Paroxetine, 20 mg daily18 | May be useful if standard treatments fail | A: RCT |
| Sertraline, 50 mg daily19 | Has been studied in children | B: nonrandomized, small, prospective trial | |
| Fluoxetine, 20 mg daily20 | — | B: nonrandomized, small, prospective trial |
Generalized Anxiety Disorder
Generalized anxiety disorder (GAD) is one of the most prevalent psychiatric disorders. Benzodiazepines such as diazepam (Valium), alprazolam (Xanax), and clonazepam (Klonopin), which are used to treat GAD, can cause sedation, difficulty concentrating, and other bothersome side effects. Dependence can develop, leading to withdrawal symptoms on discontinuation of these agents. Buspirone (BuSpar), a nonbenzodiazepine anxiolytic that does not lead to dependence, is an effective alternative, but it must be taken three times daily.21
Benzodiazepines such as diazepam (Valium), alprazolam (Xanax), and clonazepam (Klonopin), which are used to treat GAD, can cause sedation, difficulty concentrating, and other bothersome side effects. Dependence can develop, leading to withdrawal symptoms on discontinuation of these agents. Buspirone (BuSpar), a nonbenzodiazepine anxiolytic that does not lead to dependence, is an effective alternative, but it must be taken three times daily.21
SSRIs have been prescribed safely and effectively for mixed anxiety and depression syndromes, as well as for social anxiety.22 Paroxetine may be effective for GAD treatment.5 [evidence level A, randomized controlled trial (RCT)]
In the trial,5 81 patients were randomized to treatment with paroxetine (20 mg daily), imipramine (Tofranil), or the benzodiazepine 2'chlordesmethyldiazepam. The patients had a diagnosis of GAD according to criteria in the Diagnostic and Statistical Manual of Mental Disorders, 4th ed (DSM-IV), a score of at least 18 on the Hamilton Rating Scale for Anxiety (HRSA), and no comorbid psychiatric conditions. The patients ranged from 18 to 65 years of age. Demographics were similar in each group. Sixty-three patients (77.7 percent) completed the study. Using the HRSA to measure response, 68 percent of the patients in the paroxetine group,72 percent in the imipramine group, and 55 percent in the 2'chlordesmethyldiazepam group had at least a 50 percent decrease in HRSA score by the end of the eight-week study. Paroxetine was recently approved by the FDA for GAD treatment.
SSRIs may be particularly useful in the treatment of GAD in pediatric patients.3 [evidence level A, RCT] In a multicenter, double-blind trial, 128 children six to 17 years of age with social phobia, separation anxiety disorder, or GAD (as defined by DSM-IV) were randomized to treatment with fluvoxamine or placebo.3 All had received three weeks of psychotherapy without showing improvement. Fluvoxamine was chosen because it was the only SSRI approved by the FDA for use in children in 1996 when the study was designed. Fluvoxamine therapy (at a maximum dosage of 300 mg daily) resulted in a statistically significant decrease in scores on the Pediatric Anxiety Rating Scale compared with placebo. Although this trial was not specific to GAD, it was noted that anxiety disorders in children typically occur together, thereby making it difficult to isolate one disorder for study.
SSRIs seem particularly suited for use in older patients with anxiety disorders.4 [evidence level B, nonrandomized trial] In a small, open-label trial, patients more than 50 years of age with GAD, panic disorder, or obsessive-compulsive disorder were treated with fluvoxamine (median dose, 200 mg daily).4 Twelve of 19 patients (63 percent) completed the 21-week study, with eight of the 12 (66.6 percent) achieving a 50 percent reduction in symptoms as measured by standardized scales. The existence of comorbid depression, as well as the confounding variable of therapy combined with benzodiazepines, were two further limitations of this trial. The authors conclude that randomized, placebo-controlled trials are warranted to study the use of SSRIs for treatment of anxiety disorders in the older population.
Premature Ejaculation
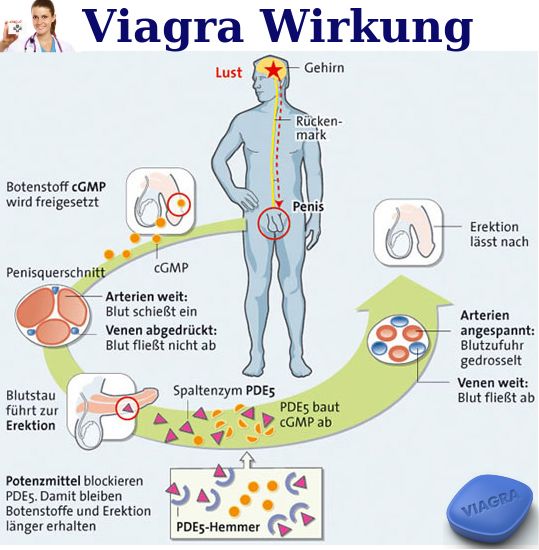
Though premature ejaculation has been overshadowed by recent attention given to erectile dysfunction, it is the most prevalent form of male sexual dysfunction.23 Delayed or inhibited ejaculation, a known side effect of SSRIs, has made SSRIs potentially useful in the treatment of this disorder. The ejaculation-delaying effect was analyzed in a double-blind, placebo-controlled trial completed by 51 men.6 Fluoxetine, sertraline, and paroxetine have been found to increase the latent period of intravaginal ejaculation and therefore to be beneficial in patients who prematurely ejaculate.6 [evidence level A, RCT] Flu-voxamine had the least effect in increasing ejaculatory latency, a difference that was not statistically significant compared with placebo. Citalopram was not studied.
It was demonstrated in a second study6 that SSRI-induced ejaculation delay is probably an effect independent of the baseline ejaculatory latency time.
In a study of 46 men 22 to 63 years of age who prematurely ejaculate (with a baseline mean ejaculatory interval of less than one minute), sertraline increased the ejaculatory interval in a dose-dependent fashion.8 At 25 mg daily, sertraline increased the mean ejaculatory interval to 7.6 minutes with the fewest side effects and with no men experiencing anejaculation. At 50 mg daily, the mean ejaculatory interval increased to 13.1 minutes with four men experiencing ane-jaculation and two men experiencing minor side effects (drowsiness, anorexia, dyspepsia). At 100 mg daily, the mean ejaculatory interval increased to 16.4 minutes, but 10 men experienced anejaculation and two men experienced erectile dysfunction and decreased libido.
Studies also show that SSRIs, particularly sertraline9 and paroxetine,7 can probably be used on an as-needed basis and taken a few hours before anticipated sexual activity. [Reference 9—evidence level B, nonrandomized trial; Reference 7 —evidence level B, randomized crossover trial]
[Reference 9—evidence level B, nonrandomized trial; Reference 7 —evidence level B, randomized crossover trial]
Migraine Headache Prophylaxis
There is fair support for the effectiveness of SSRIs in migraine prophylaxis. Prophylactic treatments for migraine headaches have included tricyclic antidepressants, beta-adrenergic blockers, and calcium channel blockers. These medications are frequently associated with an unfavorable side effect profile and may not be well tolerated by a significant number of patients with migraines. Because most theories of migraine pathophysiology focus on altered serotonergic metabolism, and given the favorable tolerability of SSRIs, the use of SSRIs in migraine prophylaxis has been studied. 10–12,24 While published results are promising, most authors acknowledge that these studies are only preliminary.
Most studies used fluoxetine. Of these, at least four were randomized, double-blind, placebo-controlled studies.10–12,24 Three of these four studies showed a significant decrease (P <. 05) in the frequency and severity of headaches.10–12 [References 10, 11, and 12—evidence level A, RCT] The patients ranged from 18 to 65 years of age, and the minimum frequency of migraines ranged from more than one per month to more than one per week. Daily dosages of fluoxetine ranged from 20 to 40 mg in these studies.
05) in the frequency and severity of headaches.10–12 [References 10, 11, and 12—evidence level A, RCT] The patients ranged from 18 to 65 years of age, and the minimum frequency of migraines ranged from more than one per month to more than one per week. Daily dosages of fluoxetine ranged from 20 to 40 mg in these studies.
evidence is limited regarding the use of the other SSRIs in migraine headache treatment. One randomized comparison study of fluvoxamine and amitriptyline (Elavil) showed that fluvoxamine decreased the number of migraine attacks as effectively as amitriptyline.25 [evidence level B, double-blind comparison]
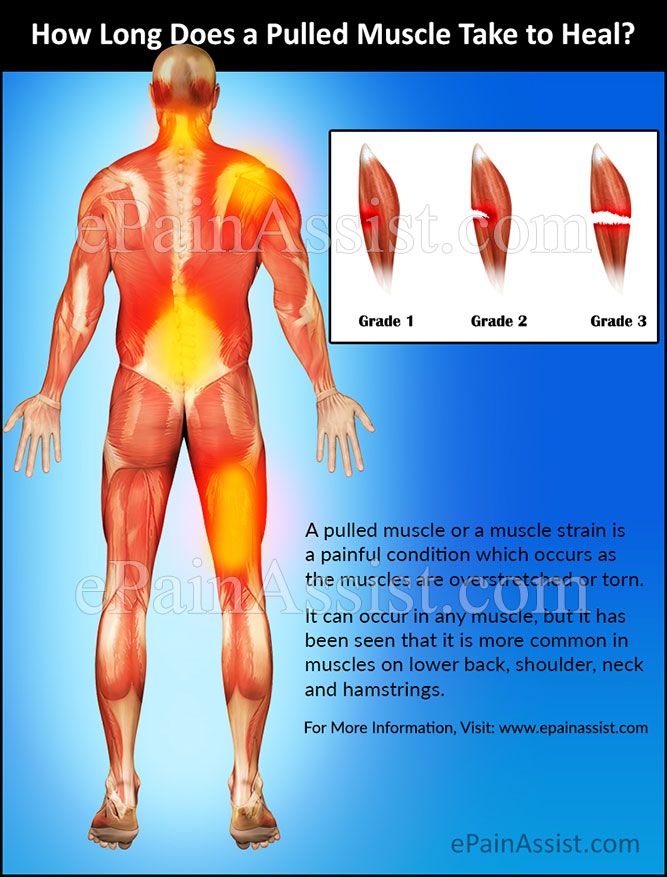
Diabetic Neuropathy
Tricyclic antidepressants are well established as effective therapy for the symptoms of diabetic neuropathy.26,27 Although mexiletine (Mexitil), capsaicin (Zostrix), carbamazepine (Tegretol), and gabapentin (Neurontin) are among other therapies that have been shown to be effective in treating neuropathic pain, no single medication has proved to be consistently effective. 28–31 SSRIs should not be considered as first-line therapy for diabetic neuropathy; the evidence for their use is fair and indicates that SSRIs may be only possibly effective.
28–31 SSRIs should not be considered as first-line therapy for diabetic neuropathy; the evidence for their use is fair and indicates that SSRIs may be only possibly effective.
A randomized, double-blind, crossover study of 29 patients found both imipramine (50 to 75 mg daily) and paroxetine (40 mg daily) to be superior to placebo.13 [evidence level B, lower quality RCT] Imipramine, however, was significantly better than paroxetine for relieving nearly all symptoms, including pain and sleep disturbance.
However, one study did not find SSRIs to be superior to placebo in relieving painful neuropathy.32 [evidence level A, meta-analysis] The meta-analysis of RCTs compared the efficacy and adverse effects of antidepressants and anticonvulsants in treating neuropathic pain, including diabetic neuropathy. Overall, for every three patients treated with a tricyclic antidepressant or an anticonvulsant, one experienced a 50 percent reduction in pain (number needed to treat [NNT] of three). While the authors noted the lack of statistically significant improvement using the pooled data of SSRIs, they thought the data insufficient to “draw a robust conclusion.”32
While the authors noted the lack of statistically significant improvement using the pooled data of SSRIs, they thought the data insufficient to “draw a robust conclusion.”32
Another review of RCTs found SSRIs to be helpful in treating diabetic neuropathy but confirmed that they are not as efficacious as other therapies.33 [evidence level B, nonquantitative systematic review] An NNT of 1.4 was calculated for imipramine, compared with the NNT of 2.4 calculated from other studies of tricyclic antidepressants. The NNT was 1.9 for dextromethorphan (Delsym), 3.3 for carbamazepine, 3.4 for tramadol (Ultram) and levodopa (Larodopa), 3.7 for gabapentin, 5.9 for capsaicin, 6.7 for SSRIs, and 10.0 for mexiletine. It was cautioned that, with the exception of the tricyclic antidepressants, these numbers were calculated on the basis of few trials or small total patient numbers per drug.
Fibromyalgia
Fibromyalgia is the most common rheumatic cause of chronic pain. 34 Medications most commonly prescribed are tricyclic antidepressants, SSRIs, muscle relaxants, simple analgesics, and nonsteroidal anti-inflammatory drugs.35 Pharmacologic therapies have shown only modest benefit at best. A meta-analysis of 49 studies found exercise and cognitive behavior therapy to be more efficacious than pharmacologic treatment alone.36 [evidence level A, meta-analysis] The results of the few RCTs involving SSRIs have been mixed.
34 Medications most commonly prescribed are tricyclic antidepressants, SSRIs, muscle relaxants, simple analgesics, and nonsteroidal anti-inflammatory drugs.35 Pharmacologic therapies have shown only modest benefit at best. A meta-analysis of 49 studies found exercise and cognitive behavior therapy to be more efficacious than pharmacologic treatment alone.36 [evidence level A, meta-analysis] The results of the few RCTs involving SSRIs have been mixed.
Two small trials of citalopram (20 to 40 mg daily) failed to reach significance, although there were subtle trends toward improvements in sleep, pain, and functioning.16,17 [References 16 and 17—evidence level B, lower quality RCTs] A trial of fluoxetine (20 mg daily) did not show significant improvement after six weeks of therapy, but the study was limited by a 43 percent dropout rate from an initially small sample of 42 patients.14 [evidence level B, lower quality RCT]
Conversely, a crossover, placebo-controlled trial comparing fluoxetine (20 mg daily) and amitriptyline (25 mg daily) demonstrated significant improvement in global well-being, pain, and sleep for each medication alone, and further improved efficacy when the two were used in combination.![]() 15 [evidence level B, lower quality RCT] Nineteen of 31 initial participants (61 percent) completed each of four six-week trials separated by two-week washout periods. Significant improvement was noted by 63 percent of those taking the combination compared with 32 percent and 24 percent of patients taking a single agent. The effects were independent of coexistent depression. The study was limited by the dropout rate and has not been duplicated.
15 [evidence level B, lower quality RCT] Nineteen of 31 initial participants (61 percent) completed each of four six-week trials separated by two-week washout periods. Significant improvement was noted by 63 percent of those taking the combination compared with 32 percent and 24 percent of patients taking a single agent. The effects were independent of coexistent depression. The study was limited by the dropout rate and has not been duplicated.
Although the Cochrane Musculoskeletal Group is performing a systematic review to assess the efficacy of SSRIs versus placebo and other antidepressants, it is clear that further study is necessary.37 Currently, SSRIs, with or without tricyclic antidepressants, can be viewed as only possibly effective in patients with unsatisfactory responses to nonpharmacologic therapy.
Neurocardiogenic Syncope
SSRIs appear to be an effective treatment in neurocardiogenic syncope refractory to standard therapies. Neurocardiogenic syncope, or vasovagal syncope, is a common disorder of transient autonomic nervous system dysfunction. 38 Although no definitive treatment for neurocardiogenic syncope exists, standard therapies such as atenolol (Tenormin) and midodrine (ProAmatine) have demonstrated efficacy. Fludrocortisone (Florinef) and increased salt and fluid intake are commonly used as well.38
One randomized, double-blind, placebo-controlled study involved the use of paroxetine in the treatment of neurocardiogenic syncope refractory to standard therapies.18 [evidence level A, RCT] Paroxetine (20 mg daily) was found to significantly improve symptoms in patients refractory to or intolerant of standard treatments. Of the 68 patients in the study, all of whom had a documented positive head-up tilt test initially, 61.8 percent in the paroxetine group versus 38.2 percent in the placebo group had negative tilt table tests after one month. During the approximately two-year follow-up period, spontaneous syncope occurred in 17.6 percent in the paroxetine group compared with 52.9 percent in the placebo group. Paroxetine was generally well tolerated.
Smaller, nonrandomized, prospective studies (two involving pediatric patients) involved the use of sertraline and fluoxetine in the treatment of refractory neurocardiogenic syncope.19,20,39 Each of these agents showed promising results, with most patients having a negative repeat tilt test or remaining symptom-free for at least six months.
Sertraline - StatPearls - NCBI Bookshelf
Continuing Education Activity
Sertraline is a medication used to manage and treat the major depressive disorder, obsessive-compulsive disorder, panic disorder, post-traumatic stress disorder, premenstrual dysphoric disorder, and social anxiety disorder. It is in the SSRI class of medications. This activity outlines the indications, actions, and contraindications for sertraline as a valuable agent in the treatment of major depressive disorder and other disorders. This activity will highlight the mechanism of action, adverse event profile, and other key factors (e.g., off-label uses, dosing, monitoring, relevant interactions) pertinent for members of the interprofessional healthcare team in treating patients with major depressive disorder and related conditions.
Objectives:
Identify the mechanism of action of sertraline.
Describe the adverse effects of sertraline.
Review the appropriate monitoring for sertraline.
Summarize interprofessional team strategies for improving care coordination and communication to advance sertraline and improve outcomes.
Access free multiple choice questions on this topic.
Indications
FDA-approved Indications
Sertraline is an antidepressant used as a first-line treatment of major depressive disorder.[1]
Obsessive-compulsive disorder(OCD)[2]
Panic disorder[3]
Post-traumatic stress disorder(PTSD)[4]
Premenstrual dysphoric disorder
Social anxiety disorder(SAD)
Non-FDA-approved Indications
Binge eating disorder[5]
Body dysmorphic disorder
Bulimia nervosa(BN)[5]
Generalized anxiety disorder(GAD)
Premature ejaculation
Mechanism of Action
Sertraline is an antidepressant medication within the selective serotonin reuptake inhibitors (SSRIs) class. Sertraline is an antidepressant with primarily inhibitory effects on presynaptic serotonin reuptake. This inhibition of serotonin reuptake results in an accumulation of serotonin. Serotonin in the central nervous system plays a role in regulating mood, personality, and wakefulness, which is why blocking serotonin reuptake is beneficial in disorders such as major depression.[1]
Sertraline also has minimal effects on norepinephrine and dopamine uptake, and research has shown that it has more dopaminergic activity than other medications in the same SSRI class. Sertraline's mechanism of action makes it highly efficacious when used in the treatment of various psychiatric conditions.[6][7]
Administration
Available Dosage Form
Sertraline is orally administered once daily in the morning or evening. If the patient experiences somnolence with sertraline, administer it in the evening. The absorption of sertraline may be improved when taken with food.[8] Available dosages in the oral tablet form are 25 mg, 50 mg, 100 mg, in capsules of 150 mg, 200 mg, and solution form 20 mg/ml.
Adult Dosing
Per FDA recommendation, the starting dose for major depressive disorder and obsessive-compulsive disorder is 50 mg once daily. The maintenance dose for depression and obsessive-compulsive disorder is 50 to 200 mg orally once a day. The dosage may be increased at weekly intervals depending on the clinical response.
To treat a premenstrual dysphoric disorder, sertraline can be given continuously (every day) or intermittently (only in the luteal phase of the menstrual cycle, starting sertraline 14 days before the anticipated menstruation dates until the end of menses.
When dosing continuously, start the patient at 50 mg once daily. When not responding optimum, increase the dosage by 50 mg increments per menstrual cycle until the maximum dose of sertraline is 150 mg daily.
When dosing intermittently, start a patient at 50 mg once daily. If not responding optimum, then administer sertraline 50 mg daily for the first three days of dosing and then 100 mg daily during the remaining days of the dosing cycle.
Intermittent dosing is to be repeated with each new cycle.
For treatment of PTSD, PD, and SAD, the starting dose is 25 mg once daily. The sertraline dose increased by 50 mg increments at weekly intervals to a maximum of 200 mg per day. Sertraline dosing is generally once daily, and administration may be at any time of the day.[9]
Special Population
Pregnancy: As per the American College of Obstetricians and Gynecologists, sertraline is Category C medicine.[10]
Breastfeeding Women: Sertraline is preferred among antidepressants in breastfeeding women.[11]
Hepatic Impairment: Sertraline should be used with caution in patients with liver disease, and a lower or less frequent dose is recommended by product labeling.
Renal Impairment: Product labeling does not report any dose adjustment based on the patient's renal function.
Withdrawal
Discontinuation of serotonergic antidepressants may cause adverse reactions, particularly when the discontinuation is abrupt. Symptoms include nausea, diaphoresis, dysphoric mood, irritability, agitation, vertigo, sensory disturbances (e.g., paresthesia, electric shock sensations), tremor, anxiety, confusion, cephalgia, lethargy, emotional lability, sleep disorder, hypomania, tinnitus, and seizures. Therefore, it is preferable to reduce the dosage gradually rather than stop immediately whenever possible.
Adverse Effects
SSRIs, considered a newer class of antidepressants, are better tolerated than tricyclic antidepressants or monoamine oxidase inhibitors. The primary side effects of sertraline include syncope, lightheadedness, diarrhea, nausea, sweating, dizziness, xerostomia, confusion, hallucinations, tremor, somnolence, impotence, a disorder of ejaculation, fatigue, rhinitis, and female sexual disorder.[7]
There is a bleeding risk associated with sertraline, as it may inhibit platelet aggregation.
Sertraline can prolong the QT interval; however, the prolongation is dose-dependent and is very modest. Furthermore, this risk is higher in citalopram rather than sertraline or other SSRIs.[12]
Sertraline may rarely produce symptoms of serotonin syndrome, though this generally happens when combining it with another serotonergic medication. These symptoms include myoclonus, muscle rigidity, diaphoresis, tremor, hyperreflexia, agitated delirium, and hyperthermia.[13]
Sertraline, like other antidepressants, may increase the risk of suicidal ideation and behavior in children, adolescents, and young adults with major depression.
Sertraline use requires caution in patients 65 years and older. It is identified in the Beers Criteria as a high-risk medication in geriatric patients, as it may induce a syndrome of inappropriate antidiuretic hormone or hyponatremia.[14][15]
Sertraline use in the first trimester of pregnancy increases the risk of cardiovascular-related malformations such as atrial and/or ventricular septal defects in infants.[16]
Neonates exposed to sertraline late in the third trimester have been reported with complications requiring prolonged hospitalization, tube feeding, and respiratory support.
Contraindications
Sertraline is contraindicated in patients with documented hypersensitivity to the drug or its components. The coadministration of sertraline with thioridazine, pimozide, or monoamine oxidase inhibitors, including linezolid or methylene blue, is also contraindicated. Patients who are taking other serotonergic medications should receive education regarding the risks of coadministration with sertraline.[17]
Sertraline solution is contraindicated with disulfiram as solution form contains 12% alcohol, and it may cause an alcohol-disulfiram reaction.
Sertraline therapy should not start within two weeks of discontinuing any monoamine oxidase inhibitor to prevent toxicity with serotonin syndrome.[17]
There is a US black box warning for use in pediatric patients and young adults. Use caution in patients ages 18 to 24 years old due to the risk of an increase in suicidal ideation.[18]
Monitoring
It is essential to monitor patients for unusual changes in behavior, anxiety, suicidality, or any other clinical signs of worsening illness. Regularly evaluate for depression and suicidality, especially when changing the dose of sertraline. Sertraline may also precipitate mania in patients at risk for bipolar disorder. Monitor for symptoms of mania in patients who are started on sertraline, especially if they have a family history of mania or bipolar disorder.[19]
Monitor for abnormal bleeding, adverse effects of medication use, or withdrawal symptoms from abrupt discontinuation in patients taking sertraline. The abnormal bleeding may primarily occur if used concurrently with aspirin, NSAIDs, warfarin, or other anticoagulants, as sertraline may impair platelet aggregation and cause bruising, epistaxis, or hemorrhage.[20]
For geriatric patients, monitor for changes in mental status, and check their sodium concentration regularly due to the risk of SIADH or hyponatremia.
Sertraline is considered safe in patients with a history of myocardial infarction, heart failure, and other cardiac conditions. However, due to the minor effect of QT prolongation, it may benefit the provider to monitor the QT interval with electrocardiograms. [21][22]
Sertraline is also considered safe in pregnancy and with breastfeeding. Although not mandatory, therapeutic drug monitoring may be a consideration to ensure the safety of pregnant patients and infants who may have exposure to the medication.[23][24] When treating pregnant women with sertraline during the third trimester, the physician should consider tapering sertraline in the third trimester by risk-benefit analysis.
Toxicity
The overdose of sertraline is generally well-tolerated. Sertraline toxicity may result in serotonin syndrome, resulting in myoclonus, muscle rigidity, diaphoresis, tremor, hyperreflexia, agitated delirium, and hyperthermia. Treatment of serotonin syndrome requires discontinuing the medication and supportive care. Consider antiemetics (non-serotonergic), benzodiazepines, and standard cooling measures for symptom relief. The patient can also receive serotonin antagonists such as cyproheptadine. If severe toxicity and the patient develops muscular rigidity and hyperthermia with body temperatures higher than 41 degrees C, consider sedation, endotracheal intubation, external cooling, and neuromuscular paralysis. It is important to note that antipyretics are likely not beneficial to patients experiencing hyperthermia due to serotonin syndrome.[25]
Enhancing Healthcare Team Outcomes
Healthcare providers who often prescribe sertraline include primary care physicians, psychiatrists, nurse practitioners, and others, functioning as an interprofessional team. All healthcare team members must follow the patient regularly to monitor the reduction of symptoms or any adverse effects. All providers should know the medication's contraindications, adverse effects, and interactions with other drugs. It is also essential to educate all patients who are prescribed sertraline on the possible adverse effects and the prevention and recognition of toxicity due to sertraline (in combination with other serotonergic drugs). Patient education regarding medication use and compliance will improve outcomes and ensure patient safety.
Patient safety can also be improved when dosing adjustments are considered by health care professionals who are a part of a patient's care team. For example, elderly patients may need dosing adjustments, as they may tolerate lower doses better. In addition, patients with medical conditions affecting their liver may need decreased doses for better tolerability.
Clinicians require vigilance regarding the toxic effects of serotonergic medications and ensure not to prescribe multiple medications that can cause serotonin syndrome, which is possible by preventing polypharmacy and minimizing unnecessary use of these drugs; this is one of the areas where the pharmacist can provide valuable input to the team as they monitor and verify the patient's medication regimen as well as monitor dosing of sertraline and other drugs. Furthermore, should a patient need to be switched to a different serotonergic medication, clinicians and other healthcare team members must ensure that no new medication starts until at least two weeks after the discontinuation of sertraline.[25] Nursing can play a significant role in this type of monitoring, ensuring patient compliance, providing counsel, assessing therapeutic effectiveness, being aware of potential adverse drug reactions, and alerting the team of any concerns. With this type of cohesive interprofessional team coordination can sertraline therapy provide an optimal therapeutic benefit while minimizing adverse events. [Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Cipriani A, La Ferla T, Furukawa TA, Signoretti A, Nakagawa A, Churchill R, McGuire H, Barbui C. Sertraline versus other antidepressive agents for depression. Cochrane Database Syst Rev. 2010 Apr 14;(4):CD006117. [PMC free article: PMC4163971] [PubMed: 20393946]
- 2.
Fenske JN, Schwenk TL. Obsessive compulsive disorder: diagnosis and management. Am Fam Physician. 2009 Aug 01;80(3):239-45. [PubMed: 19621834]
- 3.
Hobgood CD, Clayton AH. Sertraline in the treatment of panic disorder. Drugs Today (Barc). 2009 May;45(5):351-61. [PubMed: 19584964]
- 4.
Buhmann CB, Andersen HS. [Diagnosing and treating post-traumatic stress disorder].
Ugeskr Laeger. 2017 Jun 12;179(24) [PubMed: 28606295]
- 5.
Aigner M, Treasure J, Kaye W, Kasper S., WFSBP Task Force On Eating Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of eating disorders. World J Biol Psychiatry. 2011 Sep;12(6):400-43. [PubMed: 21961502]
- 6.
Kitaichi Y, Inoue T, Nakagawa S, Boku S, Kakuta A, Izumi T, Koyama T. Sertraline increases extracellular levels not only of serotonin, but also of dopamine in the nucleus accumbens and striatum of rats. Eur J Pharmacol. 2010 Nov 25;647(1-3):90-6. [PubMed: 20816814]
- 7.
Sanchez C, Reines EH, Montgomery SA. A comparative review of escitalopram, paroxetine, and sertraline: Are they all alike? Int Clin Psychopharmacol. 2014 Jul;29(4):185-96. [PMC free article: PMC4047306] [PubMed: 24424469]
- 8.
Hicks JK, Bishop JR, Sangkuhl K, Müller DJ, Ji Y, Leckband SG, Leeder JS, Graham RL, Chiulli DL, LLerena A, Skaar TC, Scott SA, Stingl JC, Klein TE, Caudle KE, Gaedigk A.
, Clinical Pharmacogenetics Implementation Consortium. Clinical Pharmacogenetics Implementation Consortium (CPIC) Guideline for CYP2D6 and CYP2C19 Genotypes and Dosing of Selective Serotonin Reuptake Inhibitors. Clin Pharmacol Ther. 2015 Aug;98(2):127-34. [PMC free article: PMC4512908] [PubMed: 25974703]
- 9.
Preskorn SH, Lane RM. Sertraline 50 mg daily: the optimal dose in the treatment of depression. Int Clin Psychopharmacol. 1995 Sep;10(3):129-41. [PubMed: 8675965]
- 10.
ACOG Committee on Practice Bulletins--Obstetrics. ACOG Practice Bulletin: Clinical management guidelines for obstetrician-gynecologists number 92, April 2008 (replaces practice bulletin number 87, November 2007). Use of psychiatric medications during pregnancy and lactation. Obstet Gynecol. 2008 Apr;111(4):1001-20. [PubMed: 18378767]
- 11.
Drugs and Lactation Database (LactMed®) [Internet]. National Institute of Child Health and Human Development; Bethesda (MD): May 15, 2022.
Sertraline. [PubMed: 30000250]
- 12.
Beach SR, Kostis WJ, Celano CM, Januzzi JL, Ruskin JN, Noseworthy PA, Huffman JC. Meta-analysis of selective serotonin reuptake inhibitor-associated QTc prolongation. J Clin Psychiatry. 2014 May;75(5):e441-9. [PubMed: 24922496]
- 13.
Duignan KM, Quinn AM, Matson AM. Serotonin syndrome from sertraline monotherapy. Am J Emerg Med. 2020 Aug;38(8):1695.e5-1695.e6. [PubMed: 31837902]
- 14.
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc. 2019 Apr;67(4):674-694. [PubMed: 30693946]
- 15.
Varela Piñón M, Adán-Manes J. Selective Serotonin Reuptake Inhibitor-Induced Hyponatremia: Clinical Implications and Therapeutic Alternatives. Clin Neuropharmacol. 2017 Jul/Aug;40(4):177-179. [PubMed: 28622213]
- 16.
Shen ZQ, Gao SY, Li SX, Zhang TN, Liu CX, Lv HC, Zhang Y, Gong TT, Xu X, Ji C, Wu QJ, Li D. Sertraline use in the first trimester and risk of congenital anomalies: a systemic review and meta-analysis of cohort studies. Br J Clin Pharmacol. 2017 Apr;83(4):909-922. [PMC free article: PMC5346877] [PubMed: 27770542]
- 17.
Sola CL, Bostwick JM, Hart DA, Lineberry TW. Anticipating potential linezolid-SSRI interactions in the general hospital setting: an MAOI in disguise. Mayo Clin Proc. 2006 Mar;81(3):330-4. [PubMed: 16529136]
- 18.
DeVane CL, Liston HL, Markowitz JS. Clinical pharmacokinetics of sertraline. Clin Pharmacokinet. 2002;41(15):1247-66. [PubMed: 12452737]
- 19.
Leverich GS, Altshuler LL, Frye MA, Suppes T, McElroy SL, Keck PE, Kupka RW, Denicoff KD, Nolen WA, Grunze H, Martinez MI, Post RM. Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers.
Am J Psychiatry. 2006 Feb;163(2):232-9. [PubMed: 16449476]
- 20.
Andrade C, Sandarsh S, Chethan KB, Nagesh KS. Serotonin reuptake inhibitor antidepressants and abnormal bleeding: a review for clinicians and a reconsideration of mechanisms. J Clin Psychiatry. 2010 Dec;71(12):1565-75. [PubMed: 21190637]
- 21.
Glassman AH, O'Connor CM, Califf RM, Swedberg K, Schwartz P, Bigger JT, Krishnan KR, van Zyl LT, Swenson JR, Finkel MS, Landau C, Shapiro PA, Pepine CJ, Mardekian J, Harrison WM, Barton D, Mclvor M., Sertraline Antidepressant Heart Attack Randomized Trial (SADHEART) Group. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002 Aug 14;288(6):701-9. [PubMed: 12169073]
- 22.
O'Connor CM, Jiang W, Kuchibhatla M, Silva SG, Cuffe MS, Callwood DD, Zakhary B, Stough WG, Arias RM, Rivelli SK, Krishnan R., SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial.
J Am Coll Cardiol. 2010 Aug 24;56(9):692-9. [PMC free article: PMC3663330] [PubMed: 20723799]
- 23.
Paulzen M, Goecke TW, Stickeler E, Gründer G, Schoretsanitis G. Sertraline in pregnancy - Therapeutic drug monitoring in maternal blood, amniotic fluid and cord blood. J Affect Disord. 2017 Apr 01;212:1-6. [PubMed: 28129551]
- 24.
Pinheiro E, Bogen DL, Hoxha D, Ciolino JD, Wisner KL. Sertraline and breastfeeding: review and meta-analysis. Arch Womens Ment Health. 2015 Apr;18(2):139-146. [PMC free article: PMC4366287] [PubMed: 25589155]
- 25.
Wang RZ, Vashistha V, Kaur S, Houchens NW. Serotonin syndrome: Preventing, recognizing, and treating it. Cleve Clin J Med. 2016 Nov;83(11):810-817. [PubMed: 27824534]
What you should know about antidepressants
Ekaterina Kushnir
treats anxiety disorder
I have generalized anxiety disorder.
For a long time I coped without pills and other help, but one day I got tired of constant anxiety and began to interfere with my normal life. As a result, I turned to a private psychiatrist.
The doctor prescribed an antidepressant from the SSRI group - these are selective serotonin reuptake inhibitors. Such drugs are the first thing prescribed in the treatment of depression and a number of other conditions, including my illness.
The doctor immediately warned me about some peculiarities associated with taking the drug. Some of them I then felt on myself. I think everyone who plans to be treated with antidepressants should know about them.
At the same time, it should be taken into account that most of the negative effects of therapy are temporary and not dangerous, and if they do not go away, one medicine can be replaced with another. Antidepressants help many people with mental disorders and other illnesses get rid of their symptoms and return to a full life, so you definitely should not be afraid of them. The main thing is to take such drugs when they are really needed: as prescribed by a competent doctor and under his control.
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Fact No. 1
Antidepressants may make symptoms worse at firstAntidepressants can increase anxiety in anxiety disorders, as well as cause irritability and agitation - this is the name for causeless motor arousal, the inability to sit still. It's not dangerous, but rather unpleasant. This condition is sometimes referred to as initial anxiety, that is, the anxiety of starting therapy. Up to 65% of people face it.
Antidepressant-induced anxiety syndrome - a systematic review in the British Journal of Psychiatry
There is also evidence that some classes of antidepressants, including SSRIs, may increase suicidal ideation in depression in young people aged 18 to 24 years. These data are not very reliable, and in older people, the risk of suicide no longer increases and even decreases.
Without treatment, depression is more likely to lead to suicidal thoughts, and in case of anxiety, you just need to prepare for such an effect, then it will be easier to survive the attacks.
The doctor told me that in the first two or three weeks there may be an increase in anxiety, but I did not take it too seriously.
Everything was fine for the first week. After about seven days, I became nervous and irritable. And then I woke up at night and after a while I felt an incomprehensible fear. My heartbeat increased, my head was spinning, my throat was constricted. Because of this, I felt a real panic - I spent the rest of the night fighting terrible thoughts, in the morning I got up completely broken.
/list/antidepressant-myths/
8 myths about antidepressants
I have never had such panic attacks before medication - my anxiety was background, general. I got scared and wrote to the doctor, who reassured me and said that it was not dangerous and would pass soon.
After that, I already expected these panic attacks, immediately tried to relax, calm down, remember that this was just a temporary effect of the drugs. And they ended faster, and then they completely disappeared.
My letter to a psychiatrist. I was scared: I expected an increase in background anxiety, but not panic attacks. I even thought about giving up the medicineFact No. 2
The effect of antidepressant treatment will not be immediateIncrease the dose of antidepressants gradually to reduce side effects. They usually start with the minimum, and then bring it up to the working one. For example, for SSRIs with the active ingredient "sertraline", the working dose is from 100 mg per day. I started taking such a drug with 25 mg, and then gradually, in several steps, under the supervision of a doctor, raised the dose to 100 mg.
SSRI dosage - NHS
What doses of antidepressants will be optimal - an article in The Lancet
The process of reaching a working dose can take from two weeks to a month or more. It depends on the drug and its tolerance. I turned out to be sensitive to the medicine, it was hard for me to survive every increase in dosage: anxiety increased again, there were other side effects that then stopped. However, this is not the case for everyone, sometimes the process goes faster.
The full therapeutic effect, that is, the disappearance or a strong improvement in the symptoms of the disease, occurs some time after reaching the working dosage. As a rule, this is a week or two, although some positive changes may be earlier. For some people, this process stretches for a longer period: 6-12 weeks. Minimum initial doses of drugs usually do not work.
It is better to prepare for the fact that the symptoms of the disease will not disappear in the first weeks of treatment. And remember - this does not always mean that the drug needs to be changed, sometimes you just need to wait or further increase the dosage under the supervision of a doctor.
Fact No. 3
Another way to mitigate the side effects of antidepressants is to prescribe an additional drug along with them: for example, from the group of tranquilizers. Such drugs may have their own side effects, they should not be taken for a long time. Unlike antidepressants, some of them can be addictive. They are usually appointed for a month, but this period may be shorter or longer.
Antidepressants together with benzodiazepines work better for depression - BMJ magazine
My doctor prescribed a rather mild drug for me. However, he did not suit me. At first, it caused increased drowsiness: during the period of increased anxiety, it went away for a while, but then returned - even with half a pill I turned off and could sleep all day. And if I drank at night, I woke up with difficulty in the morning. The psychiatrist prescribed another medicine, but I could not buy it: the drug was not available in any pharmacy nearby.
As a result, I simply endured all the side effects of therapy - they were unpleasant, but tolerable. When discussing with the doctor, she called this option acceptable if the side effects of the second medicine only worsen the situation.
My prescriptions for drugs. I never used one, because there was no such medicine in pharmaciesFact No. 4
Side effects are not always, but they areModern antidepressants, including SSRIs, are mild and have almost no side effects. Older drugs - tricyclic antidepressants and monoamine oxidase inhibitors - cause more side effects. Doctors usually use them when milder first-line drugs don't work or when they can't be prescribed.
Side effects of antidepressants - the National Health Service of the UK
Side effects of various antidepressants - Uptodate
Side effects of antidepressants and their impact on the treatment of a large depressive disorder - the journal NATURE
STOCE OF RIGHT OF STROTOLNIA 9000 - UPTODATE 9000 effects of antidepressants - advice from the Mayo Clinic staff
Choosing an SSRI drug does not guarantee the absence of side effects - many people tolerate treatment easily, but sometimes a change in drug may be necessary.
The first couple of weeks of taking there is a risk that the state of health will be so-so - it's worth thinking about. It may be worth scheduling the start of therapy on vacation.
I work remotely, and it was easier for me: the first pill was taken on Saturday, I slept through the weekend. Then she continued to work, but refused any additional loads: housework, part-time jobs, training and everything else.
It was hard work: I wanted to sleep, then I began to worry and get distracted. I also had diarrhea, nausea, headaches, tremors, i.e. hand trembling, hot flashes, sweating, palpitations. At night, panic attacks began, in the morning I had difficulty getting up because I was in pain and dizzy.
There are mixed data on how common the side effects of antidepressants are. If we summarize them, then the numbers look something like this:
- nausea - about 25% feel it;
- diarrhea - it happens in 15% of people, and 5%, on the contrary, will have constipation;
- sweating and a feeling of heat occur in about 20% of people;
- sexual dysfunction, decreased libido may occur in 80% of cases;
- insomnia - in 11% of cases;
- headache and dizziness - in about 10-11% of cases;
- weight gain - not all drugs give this effect.
Some, on the contrary, can reduce weight. On my medicine, I lost 2 kilograms in the first month, despite the fact that I quit training due to poor health. True, then they returned back.
It can be seen that most side effects occur in less than half of the cases. In addition, in most cases they pass in the first weeks and are not dangerous.
Side effects not listed above are very rare. I was "lucky", and I faced one such - a decrease in visual acuity. Once in the morning I noticed that I see worse without glasses. A little later, I realized that something was wrong with the glasses.
I wrote to the doctor, she replied that this happens, as a rule, is not dangerous and passes, but it is better to visit an ophthalmologist. I went to the ophthalmologist, everything was fine with my eyes, there was nothing terrible, but my vision really worsened - it was not a subjective feeling. On the right eye, it was -0.5 diopters, it became -0.75, and on the left eye it was -1. 5, and it became -3.5.
I was offered to try changing the drug, but I decided to wait. Vision was then restored. I have not yet gone to the doctor to have it measured, but according to subjective feelings, it is at the same level as before: I am comfortable again in my glasses.
Side effects should not be tolerated - if something greatly worries, scares or interferes with life, it is better to tell the doctor right away. The psychiatrist will be able to determine whether the side effect of the drug is dangerous and whether it is worth continuing to take it. There are several antidepressants of the SSRI group, in addition, there are groups of drugs with a slightly different mechanism of action. As a rule, doctors manage to find a medicine that gives a good effect without side effects.
If there is no danger, the doctor can adjust the dose or increase it more gradually - this often helps to cope with unpleasant effects.
I wrote to the doctor again when my visual acuity decreased Fact No. 5
Antidepressants are not drugs that you can stop drinking as soon as you get better. They are taken for a long time: usually from several months, less often several years.
Anxiety Therapy - UpToDate
For example, for generalized anxiety disorder, the duration of treatment is at least a year. Moreover, the date is not counted from the very beginning, but from the moment when a lasting effect appeared from the pills. In fact, they will have to be drunk for about 1.5 years - it depends on how long it takes to reach the working dosage of the medicine.
The cost of a package of the most famous antidepressant "Zoloft" is about 700 R, enough for about a month. That is, a course of therapy will cost about 10,000 R - maybe more or less, depending on which drug is selected.
Psychotherapy review - UpToDate
Another drug of the same group already costs more than 2000 R per pack. Source: rigla.ru The cost of an appointment with a good psychiatrist in Moscow is 3000-5000 R. At first, you will need to visit him about once every 1-1.5 months, then less often.
You can apply to the psycho-neurological dispensary at the place of residence under compulsory medical insurance - it's free. At the same time, they will not put you on psychiatric registration: it was canceled in 1993. People with disorders that do not threaten their lives or those around them are on consultative and diagnostic care. If you stop going to the doctor, he will not find out what happened: a person seeks help at will.
Psychotherapy, usually cognitive-behavioral, is also commonly prescribed to enhance and sustain the effects of antidepressants. In many cases, it improves the effectiveness of drugs, including depression and generalized anxiety disorder. An appointment with a psychotherapist in Moscow costs an average of 5000 R. For treatment, you will need about 10 sessions or more.
/psychotherapy/
How psychotherapy works
Fact No. 6
Antidepressants do not develop dependence. However, if you abruptly stop drinking them, there will be a withdrawal syndrome. This is felt as electric current discharges while moving or turning the head, headaches, dizziness, insomnia. Many people experience symptoms similar to the flu or an intestinal virus: low fever, diarrhea, general malaise, chills. Often there is anxiety, there are intrusive images.
Withdrawal symptoms after taking serotonin reuptake inhibitors - Journal of Clinical Psychiatry
How difficult it is to stop taking antidepressants - American Psychological Association
Stopping antidepressants in adults - UpToDate
treatment, they should be canceled only under the supervision of a doctor.
Antidepressant withdrawal occurs as gradually as the start of treatment. The dosage is slowly reduced, usually at this time again a cover-up drug is prescribed to alleviate side effects. As a rule, this is the same medicine that was at the beginning of the intake.
Withdrawal is usually harmless and resolves within the first weeks of stopping the drug. Sometimes even within a few days - it still depends on which medicine was prescribed. If severely disturbing symptoms appear during the withdrawal period, you should consult a doctor.
Fact No. 7
If you need to change the drug, everything will start overIt is far from always possible to immediately find the right antidepressant - sometimes the side effects do not go away and you need to take a new one.
Changing antidepressants in adults - UpToDate
Serotonin syndrome - MSD
Most often, it is started again with a small dosage, this delays the process of obtaining the effect of treatment. The new drug may also have side effects - the same or different. We will have to wait again until they pass.
You won't be able to change the drug on your own, since all antidepressants are sold only by prescription - and that's good. Switching from one drug to another can be dangerous if you do not know the characteristics of different groups of drugs.
For example, taking SSRIs is possible only some time after the withdrawal of antidepressants from the group of monoamine oxidase inhibitors - due to the risk of developing serotonin syndrome. This is a potentially fatal condition, accompanied by a change in mental state, high fever, increased muscle tone and other symptoms.
If the drug is changed correctly, there will be no dangerous negative effects, so consultation with a doctor is required.
/psychotherapy-search/
How to choose a psychotherapist
Fact No. 8
Among antidepressants there are original drugs and generics Preparations may be original or generic. Originals are medicines first released by some pharmaceutical company that have passed all clinical trials and checks. Generics are drugs with the same active ingredient from another pharmaceutical company, that is, copied from the original drug.
Theoretically, the action of generics should not differ from the action of original drugs. However, this is possible, since generics may contain other additional substances or the manufacturer may use other raw materials.
Due to my anxiety, I did not read anything in detail about specific drugs before I bought my first antidepressant in a pharmacy so as not to be scared and not think about taking it. I also didn’t think to ask the doctor about this question.
/list/covid-depression/
Psychoneurological complications after covid: memory problems and depression
As a result, I first bought a generic because it was in stock. Then it turned out that, after all, according to the experience of my psychiatrist, the original drug often gives fewer side effects and is better tolerated. As a result, I changed the generic to the original drug - and, indeed, the side effects softened.
In my subjective opinion, which is supported by some data, in the case of antidepressants and other psychotropic drugs, you should always choose the original medicine. Moreover, the cost of originals and generics is not always very different.
Originals and generics of some SSRIs
| Active ingredient | Original | Original cost | Generics | Cost of generics |
|---|---|---|---|---|
| Sertraline | Zoloft | About 700 R, 100 mg tablets | Serenata, Sirlift | 500-600 R 100mg tablets |
| Escitalopram | Cipralex | 3000 R, tablets 10 mg | "Selektra", "Elycea" | 500-1300 R 10 mg tablets |
| Fluoxetine | Prozac | About 350 R, 20 mg tablets | Profluzak, Fluoxetine | 100-200 R, tablets 20 mg |
CERTRALIN
Original
Zoloft
Original cost of the original
about 700 r, tablets 100 mg
generics
"Serenata", "Cerelift"
The cost of generies
9000 500-600 r.Escitalopram
Original
Cipralex
Original cost
3000 r, tablets 10 mg
generics
“Selectra”, “Elice”
The cost of generics
500-1300 r, tablets 10 mg
Fluoxetine
“Przak”
Cost Kene original
About 350 R, tablets 20 mg
Generics
Profluzak, Fluoxetine
Cost of generics
100—200 R, tablets 20 mg
one remained unclaimedFact No. 9
Do not take alcohol along with antidepressantsDrinking alcohol while taking antidepressants may exacerbate unpleasant side effects. Also, alcohol is a depressant, that is, it has the opposite effect, and its intake can adversely affect the results of treatment.
Why you shouldn't mix antidepressants and alcohol - Mayo Clinic
Alcohol is strictly forbidden to drink with some groups of antidepressants, for example, tricyclic antidepressants and monoamine oxidase inhibitors: combination with the latter, for example, can lead to an uncontrolled increase in pressure. MAO inhibitors in general require a special diet - it is unlikely that a doctor will prescribe such drugs as the first antidepressants, but if necessary, he will issue a list of what is allowed and prohibited.
With other antidepressants, moderate use may not be dangerous and may even pass without consequences, but doctors still recommend abstaining so as not to increase side effects and improve treatment outcome.
The main thing is not to temporarily stop taking the drug in order to drink. This can lead to the development of a withdrawal syndrome.
/trevoga/
How I Treated Generalized Anxiety Disorder under CHI
Fact No. 10
Antidepressants are incompatible with certain drugs and have contraindications It is important to tell your doctor what medications you are taking and what chronic illnesses you have. For example, SSRIs may not be suitable for epilepsy and bleeding disorders, and tricyclic antidepressants are usually not prescribed for those who have recently had a heart attack, suffer from glaucoma, or porphyria.
Antidepressant Warnings - NHS
Drug Compatibility Test - Drugs.com
It is also important to be careful if you are about to take any over-the-counter medicine. For example, ibuprofen, which people often take on their own to relieve pain and reduce fever. It should not be taken with SSRIs as it increases the risk of gastrointestinal side effects.
If it is not possible to consult a doctor before taking any medication, carefully read the instructions for it and your antidepressant. It is also worth informing all doctors who prescribe something to you during the therapy period about taking antidepressants.
The supply of Zoloft antidepressant to Russia has been suspended again — RBC
adv.rbc.ru
adv.rbc.ru
adv.rbc.ru
Hide banners
What is your location ?
YesSelect other
Categories
Euro exchange rate on March 25
EUR CB: 82. 39 (-0.75) Investments, 24 Mar, 16:09 Dollar exchange rate on March 25
USD Central Bank: 76.45 (+0.14) Investments, 24 Mar, 16:09
Prigozhin revealed the number of prisoners who completed the contract with PMC Wagner Politics, 11:56
72 Simple Iterations: How an Owner Controls His Business RBC and SberBusiness, 11:51
Medvedev did not see any problems in the possible transition of Russian sports to Asia Sport, 11:30
adv.rbc.ru
adv.rbc.ru
Singapore Prime Minister urged to prevent conflict between China and the United States Politics, 11:27
Medvedev supported the increase in the size of the Russian army Politics, 11:17
American figure skaters win World Championships in ice dancing for the first time in 10 years Sport, 11:04
Volodin called for a ban on the activities of the ICC in Russia Politics, 11:04
Explaining what the news means
RBC Evening Newsletter
Subscribe
How to calculate your credit score and refinance loans RBC and Renaissance Bank, 11:02
Foundations reported a decrease in the number of donations to refugees from Ukraine Society, 11:00
How the life of refugees from Ukraine in Russia has changed Society, 11:00
Ukrainian TV channel replaced the face of a Russian actor Politics, 10:49
Medvedev announced the need to adjust the rules for issuing Fan ID Sport, 10:40
WBA announced the failure of the championship fight between Usyk and Fury Sport, 10:40
"Gazprom" has reduced the pumping of gas through Ukraine Economy, 10:36
adv. rbc.ru
adv.rbc.ru
adv.rbc.ru
Due to production problems, the Zoloft antidepressant (active ingredient sertraline) is temporarily not supplied to Russia. This is not the first time that the supply of this drug has been interrupted: at the beginning of the year, it was out of stock in pharmacies
Photo: Konstantin Kokoshkin / Global look Press
The popular antidepressant Zoloft (the active substance is sertraline) is temporarily not supplied to Russia due to technical problems in production, RIA Novosti was told in the press service of the Russian division of the American company Viatris .
“Due to technical problems at the production site of a third-party manufacturer of the finished product, supplies of the Zoloft drug to the Russian Federation have been temporarily suspended,” they said, noting that problems arose with the supply of the drug in packages of 28 tablets with a dosage of 100 mg and in packs of 14 or 28 tablets with a dosage of 50 mg.
"The reason for the temporary suspension of supplies is not related to the quality, safety or effectiveness of the finished product," RBC was told in the press service of the Russian representative office of Viatris.
adv.rbc.ru
The company is currently evaluating the timing of the suspension of supplies and recommends that patients who are prescribed Zoloft consult with their doctor to find a possible replacement for the drug.
adv.rbc.ru
Zoloft is an antidepressant, a selective serotonin reuptake inhibitor. The active substance sertraline is included in the list of vital and essential drugs (VED).
The drug is popular and widely used by psychiatrists and psychotherapists due to the minimal number of side effects. It has analogues, but the replacement of the drug is very difficult for patients.
Roszdravnadzor notes that since last year in Russia the number of drugs with the active ingredient sertraline has increased by 30%: in total, more than 2 million packages of five trade names have been put on sale since the beginning of the year, including over 958 thousand packages of Zoloft.