Zoloft during pregnancy risks
Antidepressants and Pregnancy: Tips from an Expert
Most pregnant women want to do everything right for their baby, including eating right, exercising regularly and getting good prenatal care. But if you’re one of the many women who have a mood disorder, you might also be trying to manage your psychiatric symptoms as you prepare to welcome your new baby.
It’s common for doctors to tell women with mood disorders to stop taking drugs like antidepressants during pregnancy, leaving many moms-to-be conflicted about giving up the medications that help keep them healthy.
Lauren Osborne, M.D., assistant director of the Johns Hopkins Women’s Mood Disorders Center, talks about why stopping your medication may not be the right approach. She explains how women can — and should — balance their mental health needs with a healthy pregnancy.
Antidepressants and Pregnancy
Women who take antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), during pregnancy may worry about whether the medications can cause birth defects.
There is good news on this front. Osborne says that there is generally no need to taper off medications during pregnancy. “We can say with strong confidence that antidepressants don’t cause birth defects,” says Osborne. She adds that most studies finding a physical effect on babies from antidepressants taken during pregnancy fail to account for the effects of the mother’s psychiatric illness.
In fact, untreated mental illness itself poses risks to a developing fetus. A woman who is depressed is less likely to get good prenatal care and more likely to engage in unhealthy or dangerous behaviors, like smoking and substance abuse. Osborne also says mental illness has direct effects on newborn babies.
“Untreated depression may increase preterm birth or cause low birth weight,” she says. “Babies of depressed moms have higher levels of a hormone called cortisol. This raises a baby’s risk of developing depression, anxiety and behavioral disorders later in life.”
Weighing the Risks
While doctors don’t believe antidepressants cause birth defects, it’s still possible for them to affect the baby. It’s important for a mother and her doctor to know the risks.
It’s important for a mother and her doctor to know the risks.
About 30 percent of babies whose mothers take SSRIs will experience neonatal adaptation syndrome, which can cause increased jitteriness, irritability and respiratory distress (difficulty breathing), among other symptoms. Doctors aren’t sure whether this effect is due to the baby’s withdrawal from the SSRI after birth or exposure to the drug itself before birth.
“It may be distressing and cause pediatricians to run tests, but it will go away,” says Osborne, pointing out that these symptoms also sometimes occur in babies whose mothers don’t take SSRIs.
Common medications women frequently ask about include:
- SSRIs: Some studies link SSRI use with a very rare defect called persistent pulmonary hypertension, which is a condition where babies’ lungs don’t inflate well. “The most recent study looked at 3.8 million women and showed there was no increase in risk to their babies,” says Osborne.

- Paroxetine: Early studies on a small number of patients connected the SSRI paroxetine with cardiac defects in babies. However, these studies didn’t account for smoking, obesity and other risk factors that are more common in women who have depression. Osborne says larger, more recent studies show no such link with cardiac defects. She doesn’t recommend switching medications if paroxetine is the only one that works for you.
- Benzodiazepines: Women should avoid using tranquilizers, such as diazepam, alprazolam and clonazepam, in high doses during pregnancy because they can lead to sedation and respiratory distress in the newborn. You can still use them in small doses for short periods of time. However, Osborne will typically try to get mothers on intermediate-acting options like lorazepam. These medications don’t linger in the baby’s bloodstream like longer-acting forms and aren’t associated with high rates of abuse like shorter-acting forms.

- Valproic acid: This medication treats seizures and bipolar disorder, and does carry significant risk to a developing fetus. Taking valproic acid during pregnancy carries a 10 percent risk of neural tube defects — birth defects that affect the brain or spinal cord, such as spina bifida — as well as risks to the baby’s cognitive development, such as lower IQ. “Valproic acid is the only one I’d never prescribe for pregnant women unless all other treatment had failed,” says Osborne .
Seeing a Reproductive Psychiatrist
If you have a mood disorder, you may benefit from speaking with a reproductive psychiatrist when you are pregnant or thinking about becoming pregnant. Ideally, this should happen when you are planning for pregnancy, although this isn’t always possible. Meeting with a doctor after you become pregnant is not too late.
Osborne says her approach with patients is to limit the number of potentially harmful exposures to the baby. This means considering the number of medications a mother is on, as well as her psychiatric illness.
This means considering the number of medications a mother is on, as well as her psychiatric illness.
“If a woman takes a low dose of many medications and we have time to plan, we’ll try to get that down to a higher dose of fewer medications,” she says. “If a woman is on a low dose and it’s not controlling her illness, then her baby is exposed to both the medication and the illness. In that case, I would increase the medication dosage so her baby isn’t exposed to the illness.”
If your illness is mild, your doctor might recommend getting off medication and replacing it with treatments such as psychotherapy, prenatal yoga or acupuncture to improve your mood.
Ultimately, Osborne says women should weigh the risks of medication against the risk of untreated illness.
“If a particular side effect is extremely rare, it’s still a very rare event even if you double the risk,” she says. Medication risks are typically not greater than those of untreated mental illness. “Switching a woman’s medication is something I do very carefully and reluctantly. ”
”
Sertraline use during pregnancy and the risk of major malformations
. 2015 Jun;212(6):795.e1-795.e12.
doi: 10.1016/j.ajog.2015.01.034. Epub 2015 Jan 28.
Anick Bérard 1 , Jin-Ping Zhao 2 , Odile Sheehy 3
Affiliations
Affiliations
- 1 Research Center, Sainte-Justine Hospital, and Faculty of Pharmacy, University of Montreal, Montreal, Quebec, Canada. Electronic address: [email protected].
- 2 Research Center, Sainte-Justine Hospital, and Faculty of Pharmacy, University of Montreal, Montreal, Quebec, Canada.
- 3 Research Center, Sainte-Justine Hospital, Montreal, Quebec, Canada.
- PMID: 25637841
- DOI: 10.1016/j.ajog.2015.01.034
Anick Bérard et al. Am J Obstet Gynecol. 2015 Jun.
. 2015 Jun;212(6):795.e1-795.e12.
doi: 10.1016/j.ajog.2015.01.034. Epub 2015 Jan 28.
Authors
Anick Bérard 1 , Jin-Ping Zhao 2 , Odile Sheehy 3
Affiliations
- 1 Research Center, Sainte-Justine Hospital, and Faculty of Pharmacy, University of Montreal, Montreal, Quebec, Canada.
 Electronic address: [email protected].
Electronic address: [email protected]. - 2 Research Center, Sainte-Justine Hospital, and Faculty of Pharmacy, University of Montreal, Montreal, Quebec, Canada.
- 3 Research Center, Sainte-Justine Hospital, Montreal, Quebec, Canada.
- PMID: 25637841
- DOI: 10.1016/j.ajog.2015.01.034
Abstract
Objective: Given the current debate and growing public concerns on selective serotonin reuptake inhibitors (SSRIs) and birth defects generated by Food and Drug Administration warnings, we aim to quantify the association between first-trimester exposure to sertraline, a first-line treatment, and the risk of congenital malformations in a cohort of depressed women.
Study design: This was a population-based cohort study in Quebec, Canada, 1998 through 2010. From a cohort of 18,493 depressed/anxious pregnancies, sertraline-exposed, nonsertraline SSRI-exposed, non-SSRI exposed, and unexposed (reference category) women were studied. Major malformations overall and organ-specific malformations in the first year of life were identified. Generalized estimating equation models were used to obtain risk estimates and 95% confidence intervals (CIs). Analyses were adjusted for potential confounders.
Results: Among the 18,493 eligible pregnancies, 366 were exposed to sertraline, 1963 to other SSRIs, and 1296 to non-SSRI antidepressants during the first trimester of pregnancy. Sertraline use was not statistically significantly associated with the risk of overall major malformations when compared to nonuse of antidepressants. However, sertraline exposure was associated with an increased risk of atrial/ventricular defects specifically (risk ratio [RR], 1.34; 95% CI, 1.02-1.76; 9 exposed cases), and craniosynostosis (RR, 2.03; 95% CI, 1.09-3.75; 3 exposed cases). Exposure to SSRIs other than sertraline during the first trimester of pregnancy was associated with craniosynostosis (RR, 2.43; 95% CI, 1.44-4.11; 19 exposed cases), and musculoskeletal defects (RR, 1.28; 95% CI, 1.03-1.58; 104 exposed cases).
However, sertraline exposure was associated with an increased risk of atrial/ventricular defects specifically (risk ratio [RR], 1.34; 95% CI, 1.02-1.76; 9 exposed cases), and craniosynostosis (RR, 2.03; 95% CI, 1.09-3.75; 3 exposed cases). Exposure to SSRIs other than sertraline during the first trimester of pregnancy was associated with craniosynostosis (RR, 2.43; 95% CI, 1.44-4.11; 19 exposed cases), and musculoskeletal defects (RR, 1.28; 95% CI, 1.03-1.58; 104 exposed cases).
Conclusion: Sertraline use during the first trimester of pregnancy was associated with an increased risk of atrial/ventricular defects and craniosynostosis above and beyond the effect of maternal depression. Nonsertraline SSRIs were associated with an increased risk of craniosynostosis and musculoskeletal defects.
Keywords: cardiac defect; craniosynostosis; major congenital malformations; pregnancy; selective serotonin reuptake inhibitor; sertraline.
Copyright © 2015 Elsevier Inc. All rights reserved.
Similar articles
-
Antidepressant use during pregnancy and the risk of major congenital malformations in a cohort of depressed pregnant women: an updated analysis of the Quebec Pregnancy Cohort.
Bérard A, Zhao JP, Sheehy O. Bérard A, et al. BMJ Open. 2017 Jan 12;7(1):e013372. doi: 10.1136/bmjopen-2016-013372. BMJ Open. 2017. PMID: 28082367 Free PMC article.
-
First trimester exposure to paroxetine and risk of cardiac malformations in infants: the importance of dosage.
Bérard A, Ramos E, Rey E, Blais L, St-André M, Oraichi D. Bérard A, et al. Birth Defects Res B Dev Reprod Toxicol. 2007 Feb;80(1):18-27. doi: 10.1002/bdrb.20099. Birth Defects Res B Dev Reprod Toxicol.
 2007. PMID: 17187388
2007. PMID: 17187388 -
First-trimester use of selective serotonin-reuptake inhibitors and the risk of birth defects.
Louik C, Lin AE, Werler MM, Hernández-Díaz S, Mitchell AA. Louik C, et al. N Engl J Med. 2007 Jun 28;356(26):2675-83. doi: 10.1056/NEJMoa067407. N Engl J Med. 2007. PMID: 17596601
-
Sertraline use in the first trimester and risk of congenital anomalies: a systemic review and meta-analysis of cohort studies.
Shen ZQ, Gao SY, Li SX, Zhang TN, Liu CX, Lv HC, Zhang Y, Gong TT, Xu X, Ji C, Wu QJ, Li D. Shen ZQ, et al. Br J Clin Pharmacol. 2017 Apr;83(4):909-922. doi: 10.1111/bcp.13161. Epub 2016 Dec 4. Br J Clin Pharmacol. 2017. PMID: 27770542 Free PMC article. Review.
-
Use of selective serotonin reuptake inhibitors during pregnancy and risk of major and cardiovascular malformations: an update.

Tuccori M, Montagnani S, Testi A, Ruggiero E, Mantarro S, Scollo C, Pergola A, Fornai M, Antonioli L, Colucci R, Corona T, Blandizzi C. Tuccori M, et al. Postgrad Med. 2010 Jul;122(4):49-65. doi: 10.3810/pgm.2010.07.2175. Postgrad Med. 2010. PMID: 20675971 Review.
See all similar articles
Cited by
-
Sickle Cell Disease Association with Premature Suture Fusion in Young Children.
Manrique M, Toro-Tobon S, Bade Y, Paredes-Gutierrez J, Mantilla-Rivas E, Rana MS, Oh AK, Rogers GF. Manrique M, et al. Plast Reconstr Surg Glob Open. 2022 Oct 27;10(10):e4620. doi: 10.1097/GOX.0000000000004620. eCollection 2022 Oct. Plast Reconstr Surg Glob Open. 2022. PMID: 36312905 Free PMC article.
-
Maternal, Fetal, and Child Outcomes of Mental Health Treatments in Women: A Meta-Analysis of Pharmacotherapy.

Viswanathan M, Middleton JC, Stuebe AM, Berkman ND, Goulding AN, McLaurin-Jiang S, Dotson AB, Coker-Schwimmer M, Baker C, Voisin CE, Bann C, Gaynes BN. Viswanathan M, et al. Psychiatr Res Clin Pract. 2021 May 4;3(3):123-140. doi: 10.1176/appi.prcp.20210001. eCollection 2021 Fall. Psychiatr Res Clin Pract. 2021. PMID: 36101835 Free PMC article. Review.
-
Hypersensitivity of Zebrafish htr2b Mutant Embryos to Sertraline Indicates a Role for Serotonin Signaling in Cardiac Development.
Kent ME, Hu B, Eggleston TM, Squires RS, Zimmerman KA, Weiss RM, Roghair RD, Lin F, Cornell RA, Haskell SE. Kent ME, et al. J Cardiovasc Pharmacol. 2022 Aug 1;80(2):261-269. doi: 10.1097/FJC.0000000000001297. J Cardiovasc Pharmacol. 2022. PMID: 35904815 Free PMC article.
-
Fetal Congenital Cardiac and Vascular Disorders Associated with Sertraline Treatment during Pregnancy: Analysis of FAERS Data.

Hong F, Qiu J, Zhang S, Zhang L. Hong F, et al. Biomed Res Int. 2022 Jul 13;2022:9914931. doi: 10.1155/2022/9914931. eCollection 2022. Biomed Res Int. 2022. PMID: 35872876 Free PMC article.
-
Antidepressants induce toxicity in human placental BeWo cells.
Nabekura T, Ishikawa S, Tanase M, Okumura T, Kawasaki T. Nabekura T, et al. Curr Res Toxicol. 2022 May 6;3:100073. doi: 10.1016/j.crtox.2022.100073. eCollection 2022. Curr Res Toxicol. 2022. PMID: 35602006 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
FGBNU NTsPZ. ‹‹Depression in General Medicine: A Guide for Physicians››
The choice between the need for pharmacotherapy, on the one hand, and the prevention of risks to the health of the fetus or newborn (the risk of congenital malformations, pre- and neonatal complications, etc. ) on the other, is required from the doctor in case of depression that manifests or worsens during the period pregnancy.
) on the other, is required from the doctor in case of depression that manifests or worsens during the period pregnancy.
When deciding on such an alternative (the proportion of benefit to the mother and the potential risk to the child), a number of circumstances are taken into account, including the possibility of a negative impact on the development of the fetus by the mother's severe mental state during pregnancy.
Psychotropic drugs for pregnant women are prescribed if absolutely necessary according to strict clinical indications:
- with pronounced affective manifestations with anxiety, agitation, sleep and appetite disorders, aggravating the somatic condition of pregnant women and women in childbirth;
- with suicidal thoughts and tendencies.
However, in some cases, such as unplanned pregnancy, antidepressants are taken out of ignorance - a depressed woman, not yet aware of the pregnancy, may continue to take psychotropic drugs and be exposed to them.
Penetrating through the placenta or with mother's milk, psychotropic drugs can have an adverse effect on the fetus or newborn. Microsomal enzymes of the fetal liver are less active and are in a lower concentration compared to the liver of adults, which prolongs and enhances the effect of drugs. In the prenatal period, the blood-brain barrier is not yet fully formed and the immature CNS is generally more sensitive to the action of drugs. At the stage of embryogenesis, as well as in the early postnatal (neonatal) period of ontogenesis, the development of these vital structures is not completed, which can enhance the toxic effect of psychotropic drugs on both the fetus and the newborn. Such effects include potentially reversible, dose-dependent effects that may be exacerbated by the fact that metabolic systems have not yet fully formed. The constant use of drugs by a pregnant woman can lead to drug dependence of the fetus and, ultimately, to a withdrawal syndrome in the newborn [Vybornykh D. E., 1996].
E., 1996].
During lactation, taking antidepressants due to the possibility of the neonatal complications listed above is also highly undesirable. The mother should be convinced that in this situation it is more appropriate to feed with donor milk or artificial mixtures.
Differentiation of antidepressants in accordance with the degree of risk of developing toxic effects for infants fed by a mother taking psychotropic drugs of this class is shown in Table. 16.
Table 16 Risk of developing toxic effects in infants breastfed by mothers taking antidepressants
| Level of risk | ||
| short | average | high |
| Mianserin | SSRI | Doxepin |
| TCAs (majority) | ||
When deciding on the use of antidepressants during pregnancy, it is necessary to take into account data on the risk of teratogenic effects of antidepressants. The teratogenic effects of antidepressants cannot be completely ruled out from laboratory animal data and some very limited clinical observations.
The teratogenic effects of antidepressants cannot be completely ruled out from laboratory animal data and some very limited clinical observations.
There are 3 classes of teratogenicity of psychotropic drugs: class A - no teratogenicity in animals, no studies of the risk of teratogenicity in humans, or teratogenicity in animals has been established, but not in humans;
class B - known to be teratogenic in animals, no risk of teratogenicity in humans, or no risk of teratogenicity in animals or humans;
class B - teratogenicity has been proven, but the benefits associated with prescribing drugs sometimes outweigh the risks (eg, in a life-threatening situation).
The distribution of drugs by teratogenicity classes is presented in Table. 17. Data are given for the first trimester of pregnancy.
Table 17. Distribution of psychotropic drugs by teratogenicity class Psychotropic Drug Directory, 1997]
| Teratogenic class | ||
| BUT | B | AT |
| SSRIs: fluoxetine (Prozac), paroxetine (Paxil), sertraline (Zoloft) | TCAs: imipramine (melipramine), clomipramine (anafranil), desipramine (petylyl), doxepin (sinequan) | TCAs: amitriptyline, nortriptyline |
| Tranquilizers: chlordiazepoxide (Elenium), alprazolam (Xanax), diazepam (Relanium), lorazepam (Ativan), oxazepam (Nozepam) | ||
| Antipsychotics: butyrophenone and phenothiazine derivatives, risperidone | ||
| SSOZS: tianeptine (coaxil)* | Normotimics: lithium preparations | |
| Tranquilizers: clonazepam (antelepsin) | ||
| Antipsychotics: clozapine (azaleptin) | ||
* Due to lack of human teratogenicity data, not recommended for use during pregnancy .
In this aspect, in the treatment of pregnant and lactating mothers, drugs of the group of irreversible MAOIs should be abandoned first of all.
These data show that the risk of a teratogenic effect is minimal with the use of class A drugs. Not found. The results of a meta-analysis, combining a large amount of information, indicate the safety of fluoxetine for intrauterine development of the fetus. Accordingly, the fact of exposure to fluoxetine does not require the termination of psychopharmacological therapy or termination of pregnancy [Addis A., Koren G., 2000]. Some reports, however, indicate that women treated with fluoxetine and TCAs were more likely than in the control group (6.8%) to have spontaneous abortions (13.5 and 12.2%, respectively) [Stokes P. S. , Holtz A., 1997].
According to preliminary data from a 12-month follow-up of children whose mothers took SSRIs (fluoxetine, fluvoxamine, sertraline) during pregnancy or lactation, no adverse effects on the development of the child were registered [Stowe Z. N., 1995; Winn, 1995; Stowe Z. N., Nemeroff S. V., 1996; Yoshida K. et al., 1997; Piontek C. M., 2001].
N., 1995; Winn, 1995; Stowe Z. N., Nemeroff S. V., 1996; Yoshida K. et al., 1997; Piontek C. M., 2001].
The introduction of class B drugs: melipramine-imipramine, anafranil-clomipramine, doxepin-sinequan in animal experiments at doses many times higher than those used in clinical practice may be accompanied by a teratogenic effect. At the same time, at the clinical level, there are currently no convincing data on an increased risk of defects in the embryonic development of the fetus due to the use of these drugs during pregnancy [Puzynski S., 1988]. At the same time, the use of TCAs classified as class B, , i.e., drugs with proven teratogenicity (amitriptyline, nortriptyline), requires special care (justified only in extreme, life-threatening situations for the patient) due to the threat of fetal developmental disorders .
Of great importance for successful therapy is the early detection of depression that manifests during pregnancy. Thanks to this, it is possible to carry out sparing psychopharmacotherapy - the relief of affective disorders at a still undeveloped stage with the help of low doses of medications in short courses.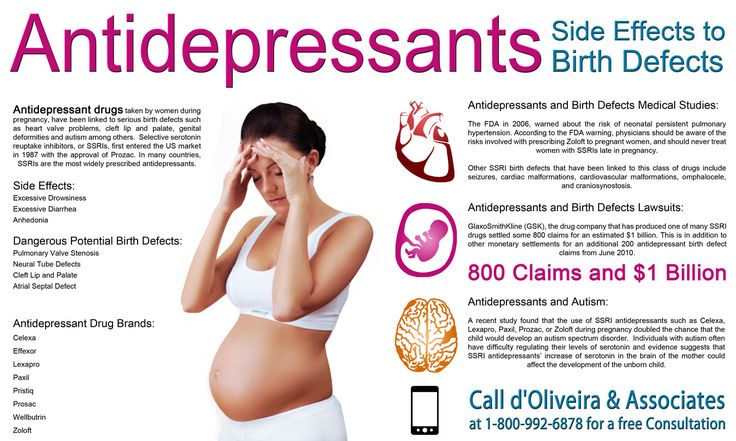 The use of psychotropic drugs in such cases is also the prevention of postpartum depression.
The use of psychotropic drugs in such cases is also the prevention of postpartum depression.
Zoloft pregnancy and lactation - Medum.ru
Pregnancy and lactationPlease note: the use of any drugs, including Zoloft drug, planning and during periods of pregnancy, lactation (breastfeeding) is necessary agree with the attending physician. Women of reproductive potential are advised to undergo pregnancy testing.
Use during pregnancy and lactation
Pregnancy
Controlled studies of the use of sertraline in pregnant women have not been conducted, so the drug should be used in this category of patients only if the expected benefit to the mother outweighs the potential risk to the fetus.
However, in a significant amount of data, there was no evidence of induction of birth defects by sertraline. Animal studies have shown a possible effect of sertraline on reproductive function. This effect is likely due to maternal toxicity caused by the pharmacodynamic effects of sertraline on the fetus.
This effect is likely due to maternal toxicity caused by the pharmacodynamic effects of sertraline on the fetus.
Some neonates whose mothers took sertraline during pregnancy have experienced withdrawal-like symptoms. This phenomenon was also observed when taking other antidepressants of the SSRI group.
Women of childbearing age who are expected to use sertraline should be advised to use effective contraception.
Lactation
Small amounts of sertraline and its metabolite N-desmethylsertraline are found in breast milk. In general, negligible amounts of sertraline were detected in the blood plasma of newborns, with the exception of one case when 50% of the concentration in the mother's blood plasma was found in the blood plasma of the newborn (with no noticeable effect on the health of the newborn). Treatment with this drug during breastfeeding is not recommended. If treatment is still necessary, then it is better to stop breastfeeding.
Neonates whose mothers took Zoloft and other SSRIs or SSRIs during pregnancy have experienced complications requiring additional hospitalization, respiratory support, and tube feeding. features in the third trimester.These newborns may experience the following symptoms: respiratory distress, cyanosis, apnea, convulsions, body temperature instability, feeding difficulties, vomiting, hypoglycemia, hypotension, hypertopus, hyperreflexia, tremor, muscle twitching, irritability, lethargy, prolonged crying, drowsiness and difficulty falling asleep.These symptoms may be associated with direct serotonergic effects or may be symptoms of drug withdrawal.In most cases, these complications begin immediately or soon (
features in the third trimester.These newborns may experience the following symptoms: respiratory distress, cyanosis, apnea, convulsions, body temperature instability, feeding difficulties, vomiting, hypoglycemia, hypotension, hypertopus, hyperreflexia, tremor, muscle twitching, irritability, lethargy, prolonged crying, drowsiness and difficulty falling asleep.These symptoms may be associated with direct serotonergic effects or may be symptoms of drug withdrawal.In most cases, these complications begin immediately or soon (
Newborns whose mothers took SSRIs during pregnancy may also be at increased risk of developing pulmonary hypertension of the newborn (PPHN). PLGN is 5 cases per 1000 pregnancies and is one of the causes of morbidity and mortality in newborns. Several recent epidemiological studies point to an association between SSRIs (including Zoloft) and PLGN .
Fertility
In one of two studies in mice, reduced fertility was noted with sertraline at 80 mg/kg (4 times the maximum recommended human dose on a mg/m basis).