Will my sex drive come back after antidepressants
Post-SSRI Sexual Dysfunction | RxISK
Written by the RxISK Team. Reviewed by Dr. David Healy.
Last updated: 2022
Contents
- Introduction
- What is post-SSRI sexual dysfunction?
- Symptoms
- Diagnosis
- How common is PSSD?
- How long do sexual side effects last?
- Publications and studies
- Treatment
- Reporting your condition
- Other drugs and conditions
- See also
- References
Introduction
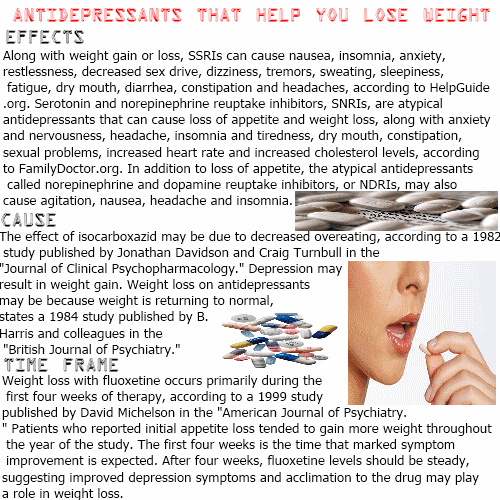
Close to 100% of people who take antidepressants experience some form of sexual side effects.
Most people who take a selective serotonin reuptake inhibitor (SSRI), a serotonin-norepinephrine reuptake inhibitor (SNRI), and some tricyclic antidepressants (clomipramine and imipramine) will feel some degree of genital numbing, often within 30 minutes of taking the first dose.
Commonly used SSRIs include paroxetine (Paxil, Seroxat), fluoxetine (Prozac), sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), and vortioxetine (Trintellix).
Common SNRIs include venlafaxine (Effexor), desvenlafaxine (Pristiq) and duloxetine (Cymbalta).
What is post-SSRI sexual dysfunction?
Post-SSRI sexual dysfunction (PSSD) is an iatrogenic condition which can arise following antidepressant use, in which sexual function does not completely return to normal after the discontinuation of SSRIs, SNRIs and some tricyclic antidepressants.
Some patients develop sexual side effects on antidepressants which either remain in full or don’t resolve completely when the drug is stopped. For others, the condition only appears when they stop the medication or begin to reduce the dosage.
PSSD affects both men and women. It can happen after only a few days exposure to an antidepressant and can persist for months, years, or indefinitely. There is no known cure.
Symptoms
Symptoms of PSSD can include:
- reduced genital sensation
- erectile dysfunction / decreased vaginal lubrication
- difficulty achieving orgasm
- pleasureless or weak orgasms
- decreased libido
- reduced response to sexual stimuli
- decreased or loss of nocturnal erections
- reduced nipple sensitivity
- flaccid glans during erection
Some patients experience a noticeable reduction in tactile sensation – genitals feel like their were exposed to an anesthetic. Others notice a reduction in sexual sensation.
Others notice a reduction in sexual sensation.
Orgasm is experienced with a decreased or loss of pleasurable feeling, often referred to as a pleasureless or muted orgasm. There can also be noticeably weaker muscle contractions.
Cases of premature ejaculation after stopping an SSRI have also been reported [1].
Ancillary non-sexual symptoms may include emotional numbing and cognitive impairment.
Diagnosis
There is no simple test to diagnose PSSD. A diagnosis is made by considering several factors including medication history, onset and profile of the symptoms, and by eliminating other possible causes. Diagnostic criteria were published in 2021 [2].
Quantitative sensory testing (QST) of the penis routinely detects reduced sensitivity in male PSSD patients, but it’s not a widely available test.
While PSSD can often result in lower than normal testosterone levels, this is not responsible for the condition. Restoring hormone levels back to normal with medication fails to resolve the problem.
PSSD is often misdiagnosed as a psychological problem when it is actually pharmacological in origin. Antidepressant sexual side effects are in no way related to depression or any other mental health disorder.
Diagnostic criteria
Necessary
(1) Prior treatment with a serotonin reuptake inhibitor.
(2) An enduring change in somatic (tactile) or erogenous (sexual) genital sensation after treatment stops.
Additional
(3) Enduring reduction or loss of sexual desire.
(4) Enduring erectile dysfunction (males).
(5) Enduring inability to orgasm or decreased sensation of pleasure during orgasm.
(6) The problem is present for ≥3 months after stopping treatment.
There should be
(7) No evidence of pre-drug sexual dysfunction that matches the current profile.
(8) No current medical conditions that could account for the symptoms.
(9) No current medication or substance misuse that could account for the symptoms.
How common is PSSD?
It isn’t known how many people regain 100% of their original sexual function and sensation after using an antidepressant. Based on the available data, PSSD may be quite common.
Based on the available data, PSSD may be quite common.
The condition can vary in severity between individuals. Some people may not realize they are suffering from it. They might have had sexual side effects while on an antidepressant which seemed to resolve when they stopped, but they still notice that their sexual function isn’t the same as it used to be, or that sexual activity feels different.
For example, a patient can find that they can now achieve orgasm after previously being unable to do so while on the medication, but it now feels weaker compared to before using the antidepressants. As they are no longer on the drug, they might think they are imagining it or that it must be due to another reason such as a relationship issue.
PSSD can be extremely distressing to those affected. It can lead to marriage break-up, job loss and suicide. But for some sufferers, the loss of sexual desire means they are no longer interested in sex and are unconcerned that they have the condition.
There is currently no way of determining who will develop PSSD when the drug is stopped or any way to actively prevent it. Stopping an antidepressant gradually (tapering) does not prevent the problem. There is no evidence that adding another drug to an antidepressant to combat sexual side effects eg. bupropion (Wellbutrin) will prevent PSSD when the antidepressant is stopped.
How long do sexual side effects last?
When sexual side effects persist after the antidepressant is stopped, there is no specific timescale for recovery.
Some patients report a certain degree of natural improvement over a period of time – sometimes months or years after stopping the antidepressant. However, many fail to recover to any significant degree with some having had the problem for over 20 years without any improvement.
For some people, PSSD may be permanent.
Publications and studies
In a study by Montejo et al, a group of patients who were experiencing sexual side effects on an SSRI were switched to the dopaminergic antidepressant, amineptine [3].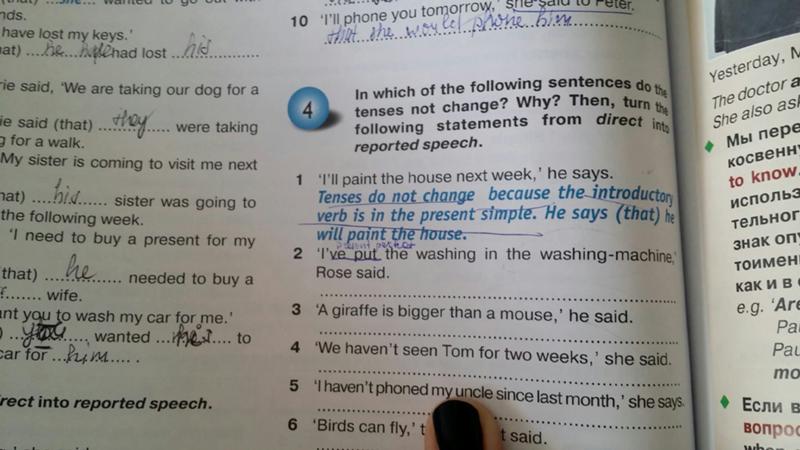 After six months, 55% still had at least some type of sexual dysfunction. This is compared to only 4% in the control group who were treated with amineptine alone and were not exposed to an SSRI.
After six months, 55% still had at least some type of sexual dysfunction. This is compared to only 4% in the control group who were treated with amineptine alone and were not exposed to an SSRI.
Three large placebo controlled studies into the use of SSRIs as a treatment for premature ejaculation found that the ejaculation-delaying effect of the medication persisted for a significant number of participants after the drug was discontinued [4–6].
PSSD was first reported in the medical literature in 2006 [7, 8].
Since 2011, the US Prozac patient information sheet has warned: “Symptoms of sexual dysfunction occasionally persist after discontinuation of fluoxetine treatment” [9].
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) states: “In some cases, serotonin reuptake inhibitor-induced sexual dysfunction may persist after the agent is discontinued” [10].
In response to a petition published in 2018 [11], the European Medicines Agency and Health Canada recommended changes to SSRI and SNRI product labels to include information about persistent sexual dysfunction after stopping the medication.
Since the condition was first reported in 2006, numerous articles involving PSSD have been published [12–40].
Animal studies
Treatment with fluoxetine has been shown to cause persistent desensitization of 5-HT1A receptors after removal of the SSRI in rats [41]. In another study, the use of a 5-HT1A antagonist was shown to reverse and prevent sexual dysfunction in rats that were being administered with fluoxetine [42]. However, attempts by PSSD patients to manipulate the serotonergic and dopaminergic systems in an effort to resolve the condition have proved unsuccessful.
Rodent studies have shown that treatment with SSRIs at a young age resulted in permanently decreased sexual behavior in adulthood [43–45], with the presence of long-term neurological changes [43]. Maternal exposure to fluoxetine was also found to impair sexual motivation in adult male mice [46].
A systematic review of the literature on persistent sexual dysfunction in animals after early exposure to SSRIs concluded: “Our results showed substantial and lasting effects on sexual behaviour in rats after exposure to an SSRI early in life on important sexual outcomes. ” [47]
” [47]
This raises the question of whether there might be long-term sexual consequences for human offspring exposed to antidepressants either during pregnancy or at a young age.
Animal studies have shown changes in bioelectric cell properties [48] and neuroactive steroids [49] after withdrawal of an SSRI.
Other studies
While on SSRIs, studies have shown side effects to include impaired semen quality and damage to sperm DNA [50–53] as well as issues that are often linked to the endocrine system such as hormone imbalances [54, 55] and breast enlargement [56]. SSRIs have also been found to have effects on sex steroids [57].
Fluoxetine has been classified as a reproductive toxin by the Center for the Evaluation of Risks to Human Reproduction (CERHR), an expert panel at the National Institute of Environmental Health Sciences, part of the National Institutes of Health [58].
Treatment
There is currently no treatment for PSSD.
A number of medications, herbs and related compounds can produce pro-sexual effects in some sufferers. However, the results are generally very limited, inconsistent and can come with their own risks.
However, the results are generally very limited, inconsistent and can come with their own risks.
PDE5 inhibitors often have reduced effectiveness in patients with PSSD.
The PSSD Research Fund was launched on 21 June 2022.
The RxISK Prize of $100,000 USD is offered to anyone who can provide a cure for persistent sexual side effects after stopping antidepressants, finasteride, or isotretinoin.
Reporting your condition
If you are suffering from PSSD, you can report it to us by completing a RxISK Report. Please provide as much detail as possible including the dates that you started and stopped the drug.
You might also want to report your condition to your country’s drug regulator eg. FDA’s MedWatch in the US and MHRA’s Yellow Card Scheme in the UK.
Other drugs and conditions
A number of other medications can also cause persisting sexual side effects after the drug has been stopped:
- Antihistamines that are serotonin reuptake inhibiting
- Ziprasidone – an antipsychotic which is also a serotonin reuptake inhibitor
- Some antibiotics (that may be serotonin reuptake inhibiting) such as tetracycline and doxycycline
- FDA updated the product information for finasteride products in 2011 to warn of persisting sexual side effects after discontinuation of treatment, with further warnings added in 2012 [59].
- Isotretinoin (Accutane) which is used as a treatment for acne [19, 27], and is also serotonin reuptake inhibiting.
The use of SSRIs or SNRIs, and often their withdrawal, has consistently been reported as one of the triggers of persistent genital arousal disorder (PGAD) [11]. This is essentially the opposite of PSSD, causing a relentless sense of arousal and discomfort in the genitals, but without any accompanying feeling of desire.
See also
- PSSD Research Fund
- Research Forum for Enduring Sexual Dysfunction
- PSSD Doctors & Specialists
- PSSD Literature
- Media articles
- Blog posts about sex and medications
- Complex Withdrawal. Hypothesis about protracted withdrawal and PSSD.
References
-
- Adson DE, Kotlyar M. Premature ejaculation associated with citalopram withdrawal. Ann Pharmacother. 2003;37(12):1804-6. PMID 14632589.
- Healy D, Bahrick A, Bak M, Barbato A, Calabrò RS, Chubak BM, et al.
 Diagnostic criteria for enduring sexual dysfunction after treatment with antidepressants, finasteride and isotretinoin. Int J Risk Saf Med. 2022;33(1):65-76. PMID: 34719438.
Diagnostic criteria for enduring sexual dysfunction after treatment with antidepressants, finasteride and isotretinoin. Int J Risk Saf Med. 2022;33(1):65-76. PMID: 34719438. - Montejo AL, Llorca G, Izquierdo JA, Carrasco JL, Daniel E, Pérez-Sola V, et al. Sexual dysfunction with antidepressive agents. Effect of the change to amineptine in patients with sexual dysfunction secondary to SSRI. Actas Esp Psiquiatr (in Spanish). 1999;27(1):23-34. PMID 10380144.
- Safarinejad MR, Hosseini SY. Safety and efficacy of citalopram in the treatment of premature ejaculation: a double-blind placebo-controlled, fixed dose, randomized study. Int J Impot Res. 2006;18(2):164–9. PMID 16107866.
- Arafa M, Shamloul R. Efficacy of sertraline hydrochloride in treatment of premature ejaculation: a placebo-controlled study using a validated questionnaire. Int J Impot Res. 2006;18(6):534–8. PMID 16554853.
- Safarinejad MR. Safety and efficacy of escitalopram in the treatment of premature ejaculation: a double-blind, placebo-controlled, fixed-dose, randomized study.
 J Clin Psychopharmacol. 2007;27(5):444–50. PMID 17873675.
J Clin Psychopharmacol. 2007;27(5):444–50. PMID 17873675. - Csoka AB, Shipko S. Persistent sexual side effects after SSRI discontinuation. Psychother Psychosom. 2006;75(3):187-8. PMID 16636635.
- Bahrick AS. Post SSRI sexual dysfunction. ASAP Tablet. 2006;7(3):2-3,10-11.
- US Prozac product information.
- American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). American Psychiatric Association, 2013. Page 449.
- Healy D. Citizen petition: Sexual side effects of SSRIs and SNRIs. Int J Risk Saf Med. 2018;29(3-4):135-147. PMID 29733031.
- Kauffman RP, Murdock A. Prolonged Post-Treatment Genital Anesthesia and Sexual Dysfunction Following Discontinuation of Citalopram and the Atypical Antidepressant Nefazodone. The Open Women’ Health Journal. 2007;1:1-3.
- Csoka AB, Bahrick A, Mehtonen OP. Persistent sexual dysfunction after discontinuation of selective serotonin reuptake inhibitors. J Sex Med.
 2008;5(1):227-33. PMID 18173768.
2008;5(1):227-33. PMID 18173768. - Bahrick AS. Persistence of sexual dysfunction side effects after discontinuation of antidepressant medications: Emerging evidence. The Open Psychology Journal. 2008;1:42-50.
- Kauffman RP. Persistent Sexual Side Effects after Discontinuation of Psychotropic Medications. Primary Psychiatry. 2008.
- Farnsworth KD, Dinsmore WW. Persistent sexual dysfunction in genitourinary medicine clinic attendees induced by selective serotonin reuptake inhibitors. Int J STD AIDS. 2009;20(1):68–9. PMID 19103903.
- Lareb, Netherlands Pharmacovigilance Center. SSRIs and persistent sexual dysfunction (2012).
- Ekhart GC, van Puijenbroek EP. Does sexual dysfunction persist upon discontinuation of selective serotonin reuptake inhibitors? (In Dutch). Tijdschr Psychiatr. 2014;56(5):336-40. PMID 24838589.
- Hogan C, Le Noury J, Healy D, Mangin D. One hundred and twenty cases of enduring sexual dysfunction following treatment. Int J Risk Saf Med.
 2014;26(2)109-16. PMID 24902508.
2014;26(2)109-16. PMID 24902508. - Waldinger MD, van Coevorden RS, Schweitzer DH, Georgiadis J. Penile anesthesia in Post SSRI Sexual Dysfunction (PSSD) responds to low-power laser irradiation: a case study and hypothesis about the role of transient receptor potential (TRP) ion channels. Eur J Pharmacol. 2015;753:263-8. PMID 25483212.
- Ben-Sheetrit J, Aizenberg D, Csoka AB, Weizman A, Hermesh H. Post-SSRI Sexual Dysfunction: Clinical Characterization and Preliminary Assessment of Contributory Factors and Dose-Response Relationship. J Clin Psychopharmacol. 2015;35(3):273-8. PMID 25815755.
- Reisman Y. Sexual Consequences of Post-SSRI Syndrome. Sex Med Rev. 2017;5(4):429-433. PMID 28642048.
- Bala A, Tue Nguyen HM, Hellstrom WJG. Post-SSRI Sexual Dysfunction: A Literature Review. Sex Med Rev. 2018;6(1):29-34. PMID 28778697.
- Muquebil Ali Al Shaban Rodríguez OW, Álvarez de Morales Gómez-Moreno E, Fernández Fernández J, Fresno García C, del Mar Fernández Fernández M.
 Disfunción sexual persistente tras el tratamiento con inhibidores selectivos de la recaptación de serotonina: a propósito de un caso tras la retirada de paroxetina. Psiquiatría Biológica. 2017;24(2):70-72.
Disfunción sexual persistente tras el tratamiento con inhibidores selectivos de la recaptación de serotonina: a propósito de un caso tras la retirada de paroxetina. Psiquiatría Biológica. 2017;24(2):70-72. - Coskuner ER, Culha MG, Ozkan B, Kaleagasi EO. Post-SSRI Sexual Dysfunction: Preclinical to Clinical. Is It Fact or Fiction? Sex Med Rev. 2018;6(2):217-223. PMID 29463440.
- Giatti S, Diviccaro S, Panzica G, Melcangi RC. Post-finasteride syndrome and post-SSRI sexual dysfunction: two sides of the same coin? Endocrine. 2018;61(2):180-193. PMID 29675596.
- Healy D, Le Noury J, Mangin D. Enduring sexual dysfunction after treatment with antidepressants, 5α-reductase inhibitors and isotretinoin: 300 cases. Int J Risk Saf Med. 2018;29(3-4):125-134. PMID 29733030.
- Calabrò RS, De Luca R, Manuli A, Portaro S, Naro A, Quattrini F. Towards Improving Post-SSRI Sexual Dysfunction by Using Nutriceuticals: Lessons from a Case Study. J Sex Marital Ther. 2019 Jan 14:1-4.
 PMID 30640584.
PMID 30640584. - European Medicines Agency. PRAC recommendations on signals adopted at the 13-16 May 2019 PRAC meeting. Published June 11, 2019. Page 5.
- Healy D, Le Noury J, Mangin D. Post-SSRI sexual dysfunction: Patient experiences of engagement with healthcare professionals. Int J Risk Saf Med. 2019;30(3):167-178. PMID 31450514.
- Healy D. Post-SSRI sexual dysfunction & other enduring sexual dysfunctions. Epidemiol Psychiatr Sci. 2019;29:e55. PMID 31543091.
- Reisman Y. Are There Any Sex/Gender Differences in Post-Selective Serotonin Reuptake Inhibitors (SSRI) Sexual Dysfunction (PSDD)? Curr Sex Health Rep 11, 237–242 (2019).
- Patacchini A, Cosci F. A Paradigmatic Case of Postselective Serotonin Reuptake Inhibitors Sexual Dysfunction or Withdrawal After Discontinuation of Selective Serotonin Reuptake Inhibitors? J Clin Psychopharmacol. 2020 Jan/Feb;40(1):93-95. PMID: 31834096.
- Healy D. Antidepressants and sexual dysfunction: a history.
 J R Soc Med. 2020;113(4):133–135. PMID 31972096.
J R Soc Med. 2020;113(4):133–135. PMID 31972096. - Reisman Y. Post-SSRI sexual dysfunction. BMJ. 2020;368:m754. PMID 32107204.
- Waraich A, Clemons C, Ramirez R, Yih J, Goldstein S, Goldstein I. Post-SSRI sexual dysfunction (PSSD): Ten year retrospective chart review. J Urol. 2020;203(4):e1179.
- Patacchini A, Cosci F. Exposure to serotonin selective reuptake inhibitors or serotonin noradrenaline reuptake inhibitors and sexual dysfunction: Results from an online survey. Int J Risk Saf Med. 2021;32(3):229-242. PMID: 33579876.
- Studt A, Gannon M, Orzel J, Vaughan A, Pearlman AM. Characterizing post-SSRI sexual dysfunction and its impact on quality of life through an international online survey. Int J Risk Saf Med. 2021;32(4):321-329. PMID 34366299.
- Chinchilla Alfaro K, van Hunsel F, Ekhart C. Persistent sexual dysfunction after SSRI withdrawal: a scoping review and presentation of 86 cases from the Netherlands. Expert Opin Drug Saf. 2022 Apr;21(4):553-561.
 Epub 2021 Nov 27. PMID: 34791958.
Epub 2021 Nov 27. PMID: 34791958. - Reisman Y, Jannini TB, Jannini EA. Post-Selective Serotonin Reuptake Inhibitor Sexual Dysfunctions (PSSD): Clinical Experience with a Multimodal Approach. J Mens Health. 2022;18(8):165.
- Raap DK, Garcia F, Muma NA, Wolf WA, Battaglia G, van de Kar LD. Sustained desensitization of hypothalamic 5-Hydroxytryptamine1A receptors after discontinuation of fluoxetine: inhibited neuroendocrine responses to 8-hydroxy-2-(Dipropylamino)Tetralin in the absence of changes in Gi/o/z proteins. J Pharmacol Exp Ther. 1999;288(2):561-7. PMID 9918559.
- Sukoff Rizzo SJ, Pulicicchio C, Malberg JE, Andree TH, Stack GP, Hughes ZA, et al. 5-HT(1A) receptor antagonism reverses and prevents fluoxetine-induced sexual dysfunction in rats. Int J Neuropsychopharmacol. 2009;12(8):1045-53. PMID 19435548.
- Maciag D, Simpson KL, Coppinger D, Lu Y, Wang Y, Lin RC, et al. Neonatal Antidepressant Exposure has Lasting Effects on Behavior and Serotonin Circuitry.
 Neuropsychopharmacology. 2006;31(1):47-57. PMID 16012532.
Neuropsychopharmacology. 2006;31(1):47-57. PMID 16012532. - de Jong TR, Snaphaan LJ, Pattij T, Veening JG, Waldinger MD, Cools AR, et al. Effects of chronic treatment with fluvoxamine and paroxetine during adolescence on serotonin-related behavior in adult male rats. Eur Neuropsychopharmacol 2006;16(1):39-48. PMID 16107310.
- Iñiguez SD, Warren BL, Bolaños-Guzmán CA. Short- and long-term functional consequences of fluoxetine exposure during adolescence in male rats. Biol Psychiatry. 2010 Jun 1;67(11):1057-66. PMID 20172503.
- Gouvêa TS, Morimoto HK, de Faria MJ, Moreira EG, Gerardin DC. Maternal exposure to the antidepressant fluoxetine impairs sexual motivation in adult male mice. Pharmacol Biochem Behav. 2008;90(3):416-9. PMID 18457868.
- Simonsen AL, Danborg PB, Gøtzsche PC. Persistent sexual dysfunction after early exposure to SSRIs: Systematic review of animal studies. Int J Risk Saf Med. 2016;28(1):1-12. PMID 27176752.
- Healy D, LaPalme J, Levin M.
 Post-SSRI Sexual Dysfunction: A Bioelectric Mechanism? Bioelectricity. 2019.
Post-SSRI Sexual Dysfunction: A Bioelectric Mechanism? Bioelectricity. 2019. - Giatti S, Diviccaro S, Cioffi L, Falvo E, Caruso D, Melcangi RC. Effects of paroxetine treatment and its withdrawal on neurosteroidogenesis. Psychoneuroendocrinology. 2021;132:105364. PMID: 34325207.
- Tanrikut C, Schlegel PN. Antidepressant-associated changes in semen parameters. Urology. 2007;69(1):185.e5-7. PMID 17270655.
- Safarinejad MR. Sperm DNA damage and semen quality impairment after treatment with selective serotonin reuptake inhibitors detected using semen analysis and sperm chromatin structure assay. J Urol. 2008;180(5):2124-8. PMID 18804223.
- Koyuncu H, Serefoglu EC, Yencilek E, Atalay H, Akbas NB, Sarıca K. Escitalopram treatment for premature ejaculation has a negative effect on semen parameters. Int J Impot Res. 2011 Nov-Dec;23(6):257-61. PMID 21776003.
- Akasheh G, Sirati L, Noshad Kamran AR, Sepehrmanesh Z. Comparison of the effect of sertraline with behavioral therapy on semen parameters in men with primary premature ejaculation.
 Urology. 2014;83(4):800-4. PMID 24529582.
Urology. 2014;83(4):800-4. PMID 24529582. - Safarinejad MR. Evaluation of endocrine profile and hypothalamic-pituitary-testis axis in selective serotonin reuptake inhibitor-induced male sexual dysfunction. J Clin Psychopharmacol. 2008;28(4):418-23. PMID 18626269.
- Cohen AJ. Antidepressant-Induced Sexual Dysfunction Associated With Low Serum Free Testosterone. Psychiatry Online. 1999.
- Amsterdam JD, Garcia-España F, Goodman D, Hooper M, Hornig-Rohan M. Breast enlargement during chronic antidepressant therapy. J Affect Disord. 1997;46(2):151-6. PMID 9479619.
- Jacobsen NW, Hansen CH, Nellemann C, Styrishave B, Halling-Sørensen B. Effects of selective serotonin reuptake inhibitors on three sex steroids in two versions of the aromatase enzyme inhibition assay and in the h395R cell assay. Toxicol In Vitro. 2015;29(7):1729-35. PMID 26162595.
- Hines RN, Adams J, Buck GM, Faber W, Holson JF, Jacobson SW, et al. NTP-CERHR Expert Panel Report on the reproductive and developmental toxicity of fluoxetine.
 Birth Defects Res B Dev Reprod Toxicol. 2004;71(4):193-280. PMID 15334524.
Birth Defects Res B Dev Reprod Toxicol. 2004;71(4):193-280. PMID 15334524. - FDA. Questions and Answers: Finasteride Label Changes.
When an SSRI medication impacts your sex life
The popular medications known as selective serotonin reuptake inhibitors or SSRIs (see box) can help lift people out from under a dark cloud of depression. But there are some side effects from antidepressants, including those that can affect your sex life. In addition to reducing interest in sex, SSRI medications can make it difficult to become aroused, sustain arousal, and reach orgasm. Some people taking SSRIs aren't able to have an orgasm at all. These symptoms tend to become more common with age.
SSRI medications include
|
If you experience any sexual problems while taking an SSRI medication, talk with your doctor or therapist. About 35% to 50% of people with untreated major depression experience some type of sexual dysfunction prior to treatment. So, in some cases, sexual difficulties may stem not from the SSRI, but rather from the underlying depression. If medication is the problem, sexual side effects sometimes subside with time, so it's worth waiting a while to see if problems diminish. This is a particularly good strategy if the medication is easing your depression significantly. But if side effects from antidepressants persist, your doctor or therapist may suggest one of the following strategies, as found in the Harvard Special Health Report Understanding Depression:
Lowering the dose. Sexual side effects may subside at a lower, although still therapeutic, dose.
Scheduling sex. Your medication may produce more pronounced side effects at particular times of the day, for example, within a few hours of taking it. If so, you can try scheduling sexual activity for the time when side effects are least bothersome—or take the drug at a different time.
If so, you can try scheduling sexual activity for the time when side effects are least bothersome—or take the drug at a different time.
Taking a drug holiday. Depending on how long the drug usually remains in your body, you might stop taking it for a few days—for example, before a weekend, if that's when you hope to have sex. This isn't spontaneous, but it can work if you carefully follow your doctor's directions about how to stop and resume your medication. However, there is always a chance that this might cause a relapse, especially if it is one of the drugs that leaves your system relatively rapidly.
Switching to a different drug. Certain antidepressants, such as bupropion (Wellbutrin), and mirtazapine (Remeron) are less likely to cause sexual problems. Bupropion, which affects both norepinephrine and dopamine, can sometimes improve sexual response.
Adding a drug. For some men, taking sildenafil (Viagra) or tadalafil (Cialis) can alleviate SSRI-induced erectile dysfunction. Both men and women may benefit from adding bupropion to their treatment. This medication has been found to counter SSRI-induced sexual dysfunction, boost sexual drive and arousal, and increase the intensity or duration of an orgasm. In some people, the anti-anxiety drug buspirone (BuSpar) may help increase libido and restore the ability to have an orgasm.
Both men and women may benefit from adding bupropion to their treatment. This medication has been found to counter SSRI-induced sexual dysfunction, boost sexual drive and arousal, and increase the intensity or duration of an orgasm. In some people, the anti-anxiety drug buspirone (BuSpar) may help increase libido and restore the ability to have an orgasm.
Meeting with a therapist. Even when physical issues or medication are at the root of sexual problems, psychological issues often become interwoven. For example, a few episodes of erectile dysfunction may cause a man to withdraw from sex and his partner to feel rejected. These issues can lead the couple to retreat further from intimacy. Working with a sex therapist or general therapist can help couples explore their sexual concerns, learn to better communicate, and expand their repertoire of sexual activities.
– By Julie Corliss
Executive Editor, Harvard Heart Letter
What you should know about antidepressants
Ekaterina Kushnir
treats anxiety disorder
I have generalized anxiety disorder.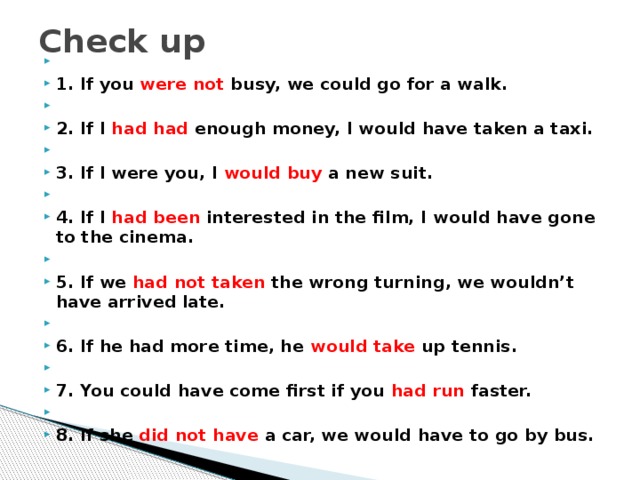
For a long time I coped without pills and other help, but one day I got tired of constant anxiety and began to interfere with my normal life. As a result, I turned to a private psychiatrist.
The doctor prescribed an antidepressant from the SSRI group - these are selective serotonin reuptake inhibitors. Such drugs are the first thing prescribed in the treatment of depression and a number of other conditions, including my illness. nine0003
The doctor immediately warned me about some peculiarities associated with taking the drug. Some of them I then felt on myself. I think everyone who plans to be treated with antidepressants should know about them.
At the same time, it should be taken into account that most of the negative effects of therapy are temporary and not dangerous, and if they do not go away, one medicine can be replaced with another. Antidepressants help many people with mental disorders and other illnesses get rid of their symptoms and return to a full life, so you definitely should not be afraid of them. The main thing is to take such drugs when they are really needed: as prescribed by a competent doctor and under his control. nine0003
The main thing is to take such drugs when they are really needed: as prescribed by a competent doctor and under his control. nine0003
See a doctor
Our articles are written with love for evidence-based medicine. We refer to authoritative sources and go to doctors with a good reputation for comments. But remember: the responsibility for your health lies with you and your doctor. We don't write prescriptions, we make recommendations. Relying on our point of view or not is up to you.
Fact No. 1
Antidepressants may make symptoms worse at firstAntidepressants can increase anxiety in anxiety disorders, as well as cause irritability and agitation - this is the name for causeless motor arousal, the inability to sit still. It's not dangerous, but rather unpleasant. This condition is sometimes referred to as initial anxiety, that is, the anxiety of starting therapy. Up to 65% of people face it. nine0003
Antidepressant-induced anxiety syndrome - a systematic review in the British Journal of Psychiatry
There is also evidence that some classes of antidepressants, including SSRIs, may increase suicidal ideation in depression in young people aged 18 to 24 years. These data are not very reliable, and in older people, the risk of suicide no longer increases and even decreases.
These data are not very reliable, and in older people, the risk of suicide no longer increases and even decreases.
Without treatment, depression is more likely to lead to suicidal thoughts, and in case of anxiety, you just need to prepare for such an effect, then it will be easier to survive the attacks. nine0003
The doctor told me that in the first two or three weeks there may be an increase in anxiety, but I did not take it too seriously.
Everything was fine for the first week. After about seven days, I became nervous and irritable. And then I woke up at night and after a while I felt an incomprehensible fear. My heartbeat increased, my head was spinning, my throat was constricted. Because of this, I felt a real panic - I spent the rest of the night fighting terrible thoughts, in the morning I got up completely broken. nine0003
/list/antidepressant-myths/
8 myths about antidepressants
I have never had such panic attacks before medication - my anxiety was background, general. I got scared and wrote to the doctor, who reassured me and said that it was not dangerous and would pass soon.
I got scared and wrote to the doctor, who reassured me and said that it was not dangerous and would pass soon.
After that, I already expected these panic attacks, immediately tried to relax, calm down, remember that this was just a temporary effect of the drugs. And they ended faster, and then they completely disappeared.
My letter to a psychiatrist. I was scared: I expected an increase in background anxiety, but not panic attacks. I even thought about giving up the medicineFact No. 2
The effect of antidepressant treatment will not be immediateIncrease the dose of antidepressants gradually to reduce side effects. They usually start with the minimum, and then bring it up to the working one. For example, for SSRIs with the active ingredient "sertraline", the working dose is from 100 mg per day. I started taking such a drug with 25 mg, and then gradually, in several steps, under the supervision of a doctor, raised the dose to 100 mg.
SSRI dosage - NHS
What doses of antidepressants will be optimal - an article in The Lancet
The process of reaching a working dose can take from two weeks to a month or more. It depends on the drug and its tolerance. I turned out to be sensitive to the medicine, it was hard for me to survive every increase in dosage: anxiety increased again, there were other side effects that then stopped. However, this is not the case for everyone, sometimes the process goes faster.
It depends on the drug and its tolerance. I turned out to be sensitive to the medicine, it was hard for me to survive every increase in dosage: anxiety increased again, there were other side effects that then stopped. However, this is not the case for everyone, sometimes the process goes faster.
The full therapeutic effect, that is, the disappearance or a strong improvement in the symptoms of the disease, occurs some time after reaching the working dosage. As a rule, this is a week or two, although some positive changes may be earlier. For some people, this process stretches for a longer period: 6-12 weeks. Minimum initial doses of drugs usually do not work. nine0003
It is better to prepare for the fact that the symptoms of the disease will not disappear in the first weeks of treatment. And remember - this does not always mean that the drug needs to be changed, sometimes you just need to wait or further increase the dosage under the supervision of a doctor.
Fact No.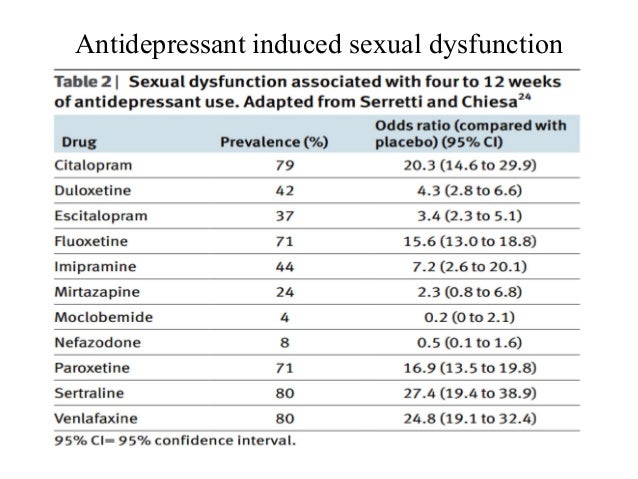 3
3
Another way to mitigate the side effects of antidepressants is to prescribe an additional drug along with them: for example, from the group of tranquilizers. Such drugs may have their own side effects, they should not be taken for a long time. Unlike antidepressants, some of them can be addictive. They are usually appointed for a month, but this period may be shorter or longer. nine0003
Antidepressants together with benzodiazepines work better for depression - BMJ magazine
My doctor prescribed a rather mild drug for me. However, he did not suit me. At first, it caused increased drowsiness: during the period of increased anxiety, it went away for a while, but then returned - even with half a pill I turned off and could sleep all day. And if I drank at night, I woke up with difficulty in the morning. The psychiatrist prescribed another medicine, but I could not buy it: the drug was not available in any pharmacy nearby. nine0003
nine0003
As a result, I simply endured all the side effects of therapy - they were unpleasant, but tolerable. When discussing with the doctor, she called this option acceptable if the side effects of the second medicine only worsen the situation.
My prescriptions for drugs. I never used one, because there was no such medicine in pharmaciesFact No. 4
Side effects are not always, but they areModern antidepressants, including SSRIs, are mild and have almost no side effects. Older drugs - tricyclic antidepressants and monoamine oxidase inhibitors - cause more side effects. Doctors usually use them when milder first-line drugs don't work or when they can't be prescribed. nine0003
Side effects of antidepressants - the National Health Service of the UK
Side effects of various antidepressants - Uptodate
Side effects of antidepressants and their impact on the treatment of a large depressive disorder - the journal NATURE
STRICTIC STRICTION OF REDICAL
. effects of antidepressants - advice from the Mayo Clinic staff
effects of antidepressants - advice from the Mayo Clinic staff
Choosing an SSRI drug does not guarantee the absence of side effects - many people tolerate treatment easily, but sometimes a change in drug may be necessary. nine0003
The first couple of weeks of taking there is a risk that the state of health will be so-so - it's worth thinking about. It may be worth scheduling the start of therapy on vacation.
I work remotely, and it was easier for me: the first pill was taken on Saturday, I slept through the weekend. Then she continued to work, but refused any additional loads: housework, part-time jobs, training and everything else.
It was hard work: I wanted to sleep, then I began to worry and get distracted. I also had diarrhea, nausea, headaches, tremors, i.e. hand trembling, hot flashes, sweating, palpitations. At night, panic attacks began, in the morning I had difficulty getting up because I was in pain and dizzy. nine0003
There are mixed data on how common the side effects of antidepressants are.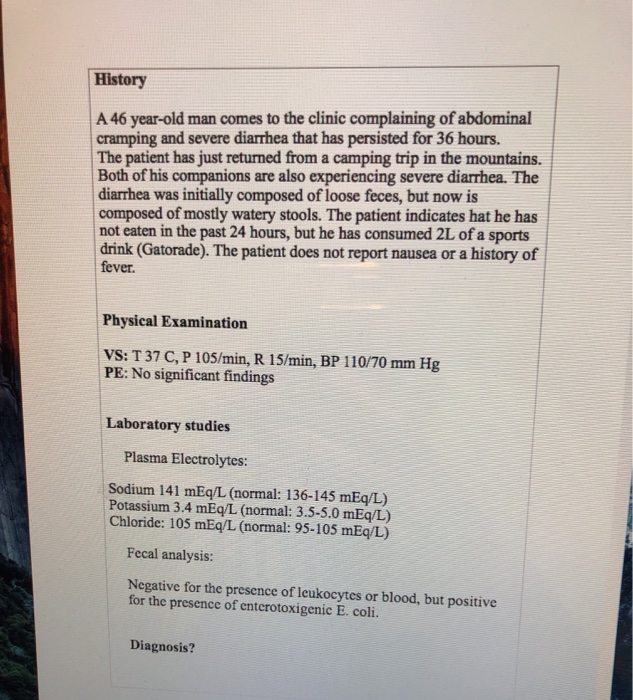 If we summarize them, then the numbers look something like this:
If we summarize them, then the numbers look something like this:
- nausea - about 25% feel it;
- diarrhea - it happens in 15% of people, and 5%, on the contrary, will have constipation;
- sweating and a feeling of heat occur in about 20% of people;
- sexual dysfunction, decreased libido may occur in 80% of cases;
- insomnia - in 11% of cases;
- headache and dizziness - in about 10-11% of cases; nine0100
- weight gain - not all drugs give this effect. Some, on the contrary, can reduce weight. On my medicine, I lost 2 kilograms in the first month, despite the fact that I quit training due to poor health. True, then they returned back.
It can be seen that most side effects occur in less than half of the cases. In addition, in most cases they pass in the first weeks and are not dangerous.
Side effects not listed above are very rare. I was "lucky", and I faced one such - a decrease in visual acuity. Once in the morning I noticed that I see worse without glasses. A little later, I realized that something was wrong with the glasses. nine0003
I was "lucky", and I faced one such - a decrease in visual acuity. Once in the morning I noticed that I see worse without glasses. A little later, I realized that something was wrong with the glasses. nine0003
I wrote to the doctor, she replied that this happens, as a rule, is not dangerous and passes, but it is better to visit an ophthalmologist. I went to the ophthalmologist, everything was fine with my eyes, there was nothing terrible, but my vision really worsened - it was not a subjective feeling. On the right eye, it was -0.5 diopters, it became -0.75, and on the left eye it was -1.5, and it became -3.5.
I was offered to try changing the drug, but I decided to wait. Vision was then restored. I have not yet gone to the doctor to have it measured, but according to subjective feelings, it is at the same level as before: I am comfortable again in my glasses. nine0003
Side effects should not be tolerated - if something greatly worries, scares or interferes with life, it is better to tell the doctor right away. The psychiatrist will be able to determine whether the side effect of the drug is dangerous and whether it is worth continuing to take it. There are several antidepressants of the SSRI group, in addition, there are groups of drugs with a slightly different mechanism of action. As a rule, doctors manage to find a medicine that gives a good effect without side effects.
The psychiatrist will be able to determine whether the side effect of the drug is dangerous and whether it is worth continuing to take it. There are several antidepressants of the SSRI group, in addition, there are groups of drugs with a slightly different mechanism of action. As a rule, doctors manage to find a medicine that gives a good effect without side effects.
If there is no danger, the doctor can adjust the dose or increase it more gradually - this often helps to cope with unpleasant effects. nine0003 I wrote to the doctor again when my visual acuity decreased
Fact No. 5
Antidepressants need to be taken long termAntidepressants are not drugs that you can stop drinking as soon as you get better. They are taken for a long time: usually from several months, less often several years.
Anxiety Therapy - UpToDate
For example, for generalized anxiety disorder, the duration of treatment is at least a year. Moreover, the date is not counted from the very beginning, but from the moment when a lasting effect appeared from the pills. In fact, they will have to be drunk for about 1.5 years - it depends on how long it takes to reach the working dosage of the medicine. nine0003
In fact, they will have to be drunk for about 1.5 years - it depends on how long it takes to reach the working dosage of the medicine. nine0003
The cost of a package of the most famous antidepressant "Zoloft" is about 700 R, enough for about a month. That is, a course of therapy will cost about 10,000 R - maybe more or less, depending on which drug is selected.
Psychotherapy review - UpToDate
Another drug of the same group already costs more than 2000 R per pack. Source: rigla.ruThe cost of an appointment with a good psychiatrist in Moscow is 3000-5000 R. At first, you will need to visit him about once every 1-1.5 months, then less often. nine0003
You can apply to the psycho-neurological dispensary at the place of residence under compulsory medical insurance - it's free. At the same time, they will not put you on psychiatric registration: it was canceled in 1993. People with disorders that do not threaten their lives or those around them are on consultative and diagnostic care. If you stop going to the doctor, he will not find out what happened: a person seeks help at will.
If you stop going to the doctor, he will not find out what happened: a person seeks help at will.
Psychotherapy, usually cognitive-behavioral, is also commonly prescribed to enhance and sustain the effects of antidepressants. In many cases, it improves the effectiveness of drugs, including depression and generalized anxiety disorder. An appointment with a psychotherapist in Moscow costs an average of 5000 R. For treatment, you will need about 10 sessions or more. nine0003
/psychotherapy/
How psychotherapy works
Fact No. 6
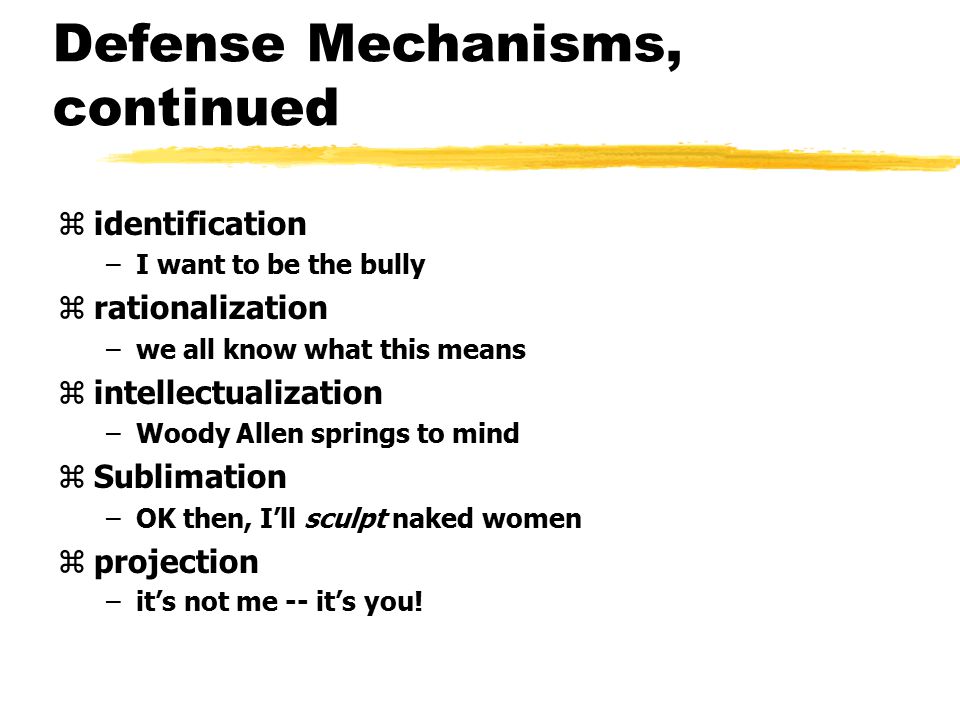
Antidepressants should not be stopped abruptly Antidepressants do not develop dependence. However, if you abruptly stop drinking them, there will be a withdrawal syndrome. This is felt as electric current discharges while moving or turning the head, headaches, dizziness, insomnia. Many people experience symptoms similar to the flu or an intestinal virus: low fever, diarrhea, general malaise, chills. Often there is anxiety, there are intrusive images. nine0003
Often there is anxiety, there are intrusive images. nine0003
Withdrawal symptoms after taking serotonin reuptake inhibitors - Journal of Clinical Psychiatry
How difficult it is to stop taking antidepressants - American Psychological Association
Stopping antidepressants in adults - UpToDate
treatment, they should be canceled only under the supervision of a doctor.
Antidepressant withdrawal occurs as gradually as the start of treatment. The dosage is slowly reduced, usually at this time again a cover-up drug is prescribed to alleviate side effects. As a rule, this is the same medicine that was at the beginning of the intake. nine0003
Withdrawal is usually harmless and resolves within the first weeks of stopping the drug. Sometimes even within a few days - it still depends on which medicine was prescribed. If severely disturbing symptoms appear during the withdrawal period, you should consult a doctor.
Fact No. 7
If you need to change the drug, everything will start over It is far from always possible to immediately find the right antidepressant - sometimes the side effects do not go away and you need to take a new one. nine0003
nine0003
Changing antidepressants in adults - UpToDate
Serotonin syndrome - MSD
Most often, it is started again with a small dosage, this delays the process of obtaining the effect of treatment. The new drug may also have side effects - the same or different. We will have to wait again until they pass.
You won't be able to change the drug on your own, since all antidepressants are sold only by prescription - and that's good. Switching from one drug to another can be dangerous if you do not know the characteristics of different groups of drugs. nine0003
For example, taking SSRIs is possible only some time after the withdrawal of antidepressants from the group of monoamine oxidase inhibitors - due to the risk of developing serotonin syndrome. This is a potentially fatal condition, accompanied by a change in mental state, high fever, increased muscle tone and other symptoms.
If the drug is changed correctly, there will be no dangerous negative effects, so consultation with a doctor is required.
/psychotherapy-search/
How to choose a psychotherapist
Fact No. 8
Among antidepressants there are original drugs and genericsPreparations may be original or generic. Originals are medicines first released by some pharmaceutical company that have passed all clinical trials and checks. Generics are drugs with the same active ingredient from another pharmaceutical company, that is, copied from the original drug.
Theoretically, the action of generics should not differ from the action of original drugs. However, this is possible, since generics may contain other additional substances or the manufacturer may use other raw materials. nine0003
Due to my anxiety, I did not read anything in detail about specific drugs before I bought my first antidepressant in a pharmacy so as not to be scared and not think about taking it. I also didn’t think to ask the doctor about this question.
/list/covid-depression/
Psychoneurological complications after covid: memory problems and depression
As a result, I first bought a generic because it was in stock. Then it turned out that, after all, according to the experience of my psychiatrist, the original drug often gives fewer side effects and is better tolerated. As a result, I changed the generic to the original drug - and, indeed, the side effects softened. nine0003
Then it turned out that, after all, according to the experience of my psychiatrist, the original drug often gives fewer side effects and is better tolerated. As a result, I changed the generic to the original drug - and, indeed, the side effects softened. nine0003
In my subjective opinion, which is supported by some data, in the case of antidepressants and other psychotropic drugs, you should always choose the original medicine. Moreover, the cost of originals and generics is not always very different.
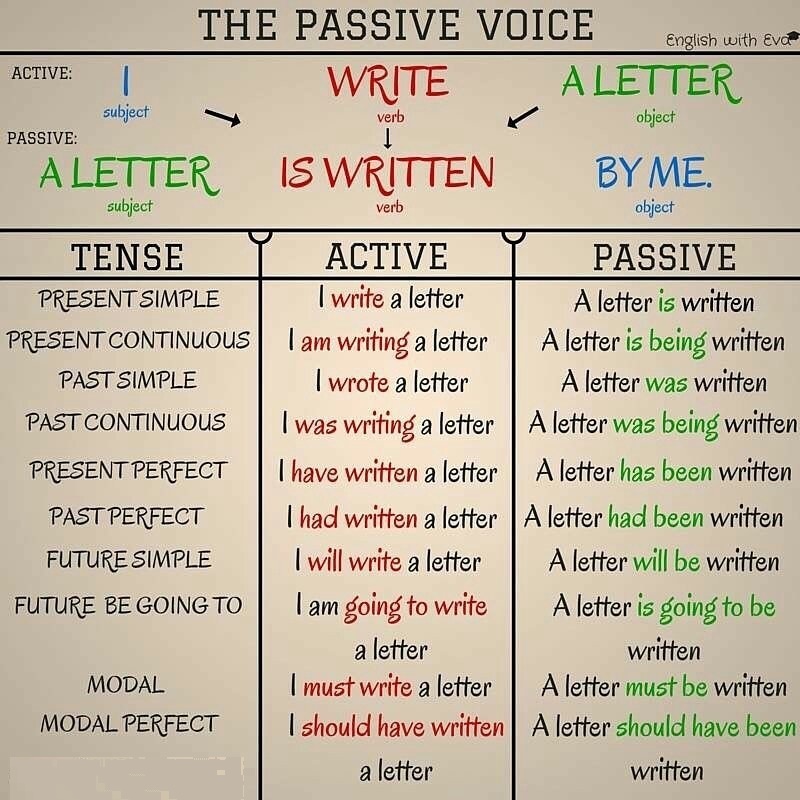
Originals and generics of some SSRIs
| Active ingredient | Original | Original cost | Generics | Cost of generics |
|---|---|---|---|---|
| Sertraline | Zoloft | About 700 R, 100 mg tablets | Serenata, Sirlift | 500-600 R 100mg tablets |
| Escitalopram | Cipralex | 3000 R, tablets 10 mg | "Selektra", "Elycea" | 500-1300 R 10 mg tablets |
| Fluoxetine | Prozac | About 350 R, 20 mg tablets | Profluzak, Fluoxetine | 100-200 R, tablets 20 mg |
CERTRIN
Original
"Zoloft"
Original cost of the original
about 700 r, tablets 100 mg
generics
"Serenata", "Cerelift"
The cost of Jeeneriki
9000 500-600 r. , tablets 100 mg
, tablets 100 mg Escitalopram
Original
Cipralex
Original price
3000 r, tablets 10 mg
generics
“Chektra”, “Elice”
The cost of generics
500-1300 r, tablets 10 mg
Fluoxetine
“Przak”
cost
cost cost
Cost cost cost original
About 350 R, tablets 20 mg
Generics
Profluzak, Fluoxetine
Cost of generics
100—200 R, tablets 20 mg
one remained unclaimedFact No. 9
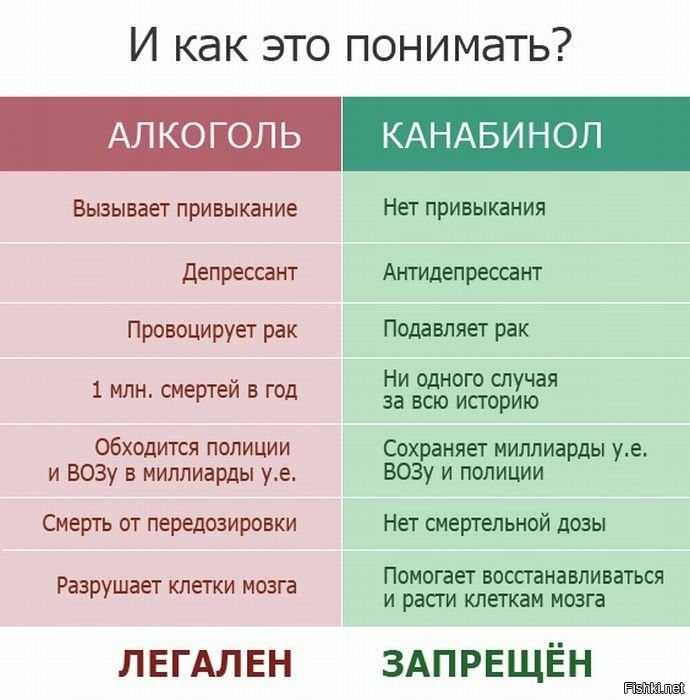
Do not take alcohol along with antidepressantsDrinking alcohol while taking antidepressants may exacerbate unpleasant side effects. Also, alcohol is a depressant, that is, it has the opposite effect, and its intake can adversely affect the results of treatment.
Why you shouldn't mix antidepressants and alcohol - Mayo Clinic
Alcohol is strictly forbidden to drink with some groups of antidepressants, for example, tricyclic antidepressants and monoamine oxidase inhibitors: combination with the latter, for example, can lead to an uncontrolled increase in pressure.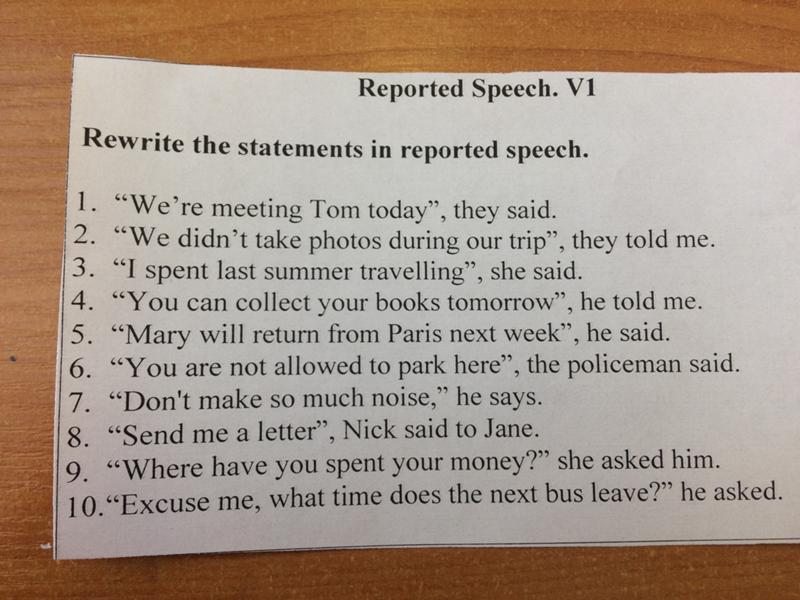 MAO inhibitors in general require a special diet - it is unlikely that a doctor will prescribe such drugs as the first antidepressants, but if necessary, he will issue a list of what is allowed and prohibited. nine0003
MAO inhibitors in general require a special diet - it is unlikely that a doctor will prescribe such drugs as the first antidepressants, but if necessary, he will issue a list of what is allowed and prohibited. nine0003
With other antidepressants, moderate use may not be dangerous and may even pass without consequences, but doctors still recommend abstaining so as not to increase side effects and improve treatment outcome.
The main thing is not to temporarily stop taking the drug in order to drink. This can lead to the development of a withdrawal syndrome.
/trevoga/
How I Treated Generalized Anxiety Disorder under CHI
Fact No. 10
Antidepressants are incompatible with certain drugs and have contraindications nine0017 It is important to tell your doctor what medications you are taking and what chronic illnesses you have. For example, SSRIs may not be suitable for epilepsy and bleeding disorders, and tricyclic antidepressants are usually not prescribed for those who have recently had a heart attack, suffer from glaucoma, or porphyria.
Antidepressant Warnings - NHS
Drug Compatibility Test - Drugs.com
It is also important to be careful if you are about to take any over-the-counter medicine. For example, ibuprofen, which people often take on their own to relieve pain and reduce fever. It should not be taken with SSRIs as it increases the risk of gastrointestinal side effects.
If it is not possible to consult a doctor before taking any medication, carefully read the instructions for it and your antidepressant. It is also worth informing all doctors who prescribe something to you during the therapy period about taking antidepressants. nine0003
Will I lose my libido and become a fat vegetable? Myths about antidepressants that everyone falls for
Surely you have at least once taken an online test that will determine if you have depression in 10 questions. Perhaps even went to a specialist to understand yourself. But as practice shows, when doctors prescribe antidepressants, some patients defiantly refuse, and some, on the contrary, seize any sorrows with them. Both of these behaviors are dangerous. Therefore, KYKY discussed the main myths about pills with Oleg Aizberg, Associate Professor of the Department of Psychiatry and Narcology of the Belarusian Medical Academy of Postgraduate Education. nine0003
Both of these behaviors are dangerous. Therefore, KYKY discussed the main myths about pills with Oleg Aizberg, Associate Professor of the Department of Psychiatry and Narcology of the Belarusian Medical Academy of Postgraduate Education. nine0003
I'm afraid that antidepressants will change my personality, my relatives will no longer recognize me, they will say that I have become a “different person”.
Antidepressants cannot radically change your personality, but they can affect how you experience certain emotions. Adolescents sometimes become more aggressive, and in adults, in 5-10% of cases, emotional sensitivity can be dulled: both bad and good events are experienced as less significant. But patients definitely do not become “vegetables”.
Antidepressants greatly reduce libido. Does that mean I won't want sex at all?
One of the most common side effects of antidepressants is decreased libido. Some data say that this happens to a maximum of 10% of people, others - that it can be in half. But it is not always clear what exactly causes desire to decrease - for example, with depression and anxiety disorders, libido is, in principle, lowered. For some, this side effect can be low desire, and sometimes anorgasmia appears - then it is very difficult for a person to achieve orgasm. There are also cases when a person does not feel his genitals, as if they are numb. But this happens only from antidepressants that affect the exchange of serotonin. nine0003
But it is not always clear what exactly causes desire to decrease - for example, with depression and anxiety disorders, libido is, in principle, lowered. For some, this side effect can be low desire, and sometimes anorgasmia appears - then it is very difficult for a person to achieve orgasm. There are also cases when a person does not feel his genitals, as if they are numb. But this happens only from antidepressants that affect the exchange of serotonin. nine0003
It is important that some people recover their libido over time, even if they continue to take the pills. For others, it remains low, and then this is a reason to stop the drug or switch to another treatment.
I will gain a lot of weight on antidepressants and then I won't be able to lose it.
Yes, some may gain weight. But it is not known exactly why this happens. During depression, appetite decreases, and when taking pills, it is restored. It turns out that this is more of a weight stabilization, not obesity. Well, gaining 20-30 kilograms on antidepressants will definitely not work. nine0003
Well, gaining 20-30 kilograms on antidepressants will definitely not work. nine0003
I will think about death all the time
A depressed person often has suicidal thoughts. Antidepressants can make them worse, but only in the first two weeks of taking them. But without treatment, the likelihood that a person can commit suicide, on the contrary, only increases.
I don't want to become addicted to pills
Antidepressants are not addictive like sleeping pills, tranquilizers or drugs, which are much more dangerous in this sense. But some drugs can cause withdrawal, which is similar to what addicts experience. Most often, such a reaction is caused by drugs that do not form active metabolites and are rapidly excreted. nine0003
A withdrawal syndrome may occur in a person who has abruptly stopped taking pills. It happens that this happens with a gradual failure, but much less often. And some patients have no withdrawal syndrome at all. In any case, this syndrome resolves within one to four weeks and is not an addiction. It may also happen that after discontinuation of the drug, a relapse of the disease occurs. But, again, this is not a manifestation of dependence.
It may also happen that after discontinuation of the drug, a relapse of the disease occurs. But, again, this is not a manifestation of dependence.
If I take antidepressants, I won't be able to hang out with friends in bars. nine0363
The instructions for antidepressants say that they should not be mixed with alcohol. In rare cases, such a mixture can cause uncontrolled aggression. True, again, it is not yet clear what exactly gives such a result. Sometimes depressed people suppress aggression, and when they drink, it comes out. And then we can assume that the problem is not in antidepressants, but in a person. Another side effect of mixing even small doses of alcohol with antidepressants is increased anxiety. nine0003
If we talk about the combination of drugs with drugs, especially psychostimulants, then this is really dangerous. You can get severe poisoning - convulsions, tachycardia, fever up to 40 degrees, stroke, heart rhythm disturbances. In general, a state similar to an overdose. In this case, the person may be taken to the acute poisoning unit - or he may die. But the new generation of antidepressants, along with booze, do not give the same toxicity as the old generation of antidepressants - here they can be deadly poisonous. nine0003
In this case, the person may be taken to the acute poisoning unit - or he may die. But the new generation of antidepressants, along with booze, do not give the same toxicity as the old generation of antidepressants - here they can be deadly poisonous. nine0003
I will cry all the time
Antidepressants definitely don't have such an effect.
Antidepressants will not solve my problem, they will only mask it.
If a person, instead of going to a psychotherapist, only takes pills, then we can talk about the "masking" of the problem. This is especially true for anxiety disorders. But, unfortunately, there is no clear understanding of whom psychotherapy will help, and who - pills. In Western protocols, they write that the primary method of treatment is psychotherapy, and the secondary is antidepressants. Unless, of course, this is not a severe case. But in practice, most patients are prescribed drugs from the very beginning. This is due to the fact that there are long queues for psychotherapy, and people cannot wait six months without treatment. On the other hand, for some patients, antidepressants are a crutch. If a person has severe depression, then psychotherapy will be impossible without taking antidepressants - the patient simply will not be able to communicate with a psychotherapist. At the same time, one must understand that psychotherapy is not a panacea, there are patients for whom it does not help - just like pills. nine0003
On the other hand, for some patients, antidepressants are a crutch. If a person has severe depression, then psychotherapy will be impossible without taking antidepressants - the patient simply will not be able to communicate with a psychotherapist. At the same time, one must understand that psychotherapy is not a panacea, there are patients for whom it does not help - just like pills. nine0003
I can't work on tablets.
This is an absolute myth. Rather, this can happen when taking antipsychotics, if the drug is chosen incorrectly or the patient takes too much of a dose.
I can manage without antidepressants.
Mental disorders can go away without treatment - the question is when this will happen and what will happen to a person's life. If the patient is categorically against antidepressants, he is recommended psychotherapy. In general, the doctor's task is to inform the patient about the treatment options (antidepressants, psychotherapy, or a combination), their advantages and disadvantages. But there are situations when antidepressants are 100% needed. For example, a person suffers from a severe depressive episode - then not only drugs are needed, but also hospitalization. nine0003
But there are situations when antidepressants are 100% needed. For example, a person suffers from a severe depressive episode - then not only drugs are needed, but also hospitalization. nine0003
If I miss a pill, depression will hit me even more.
If you miss one tablet, nothing bad will happen. "Cover" stronger after a pass can be when taking some antidepressants with a short elimination period. And then the person will feel something like a withdrawal syndrome.
I accidentally drank two - am I overdosing now?
One extra pill won't do anything. The difference between a toxic dose and two pills is too big.
My health will worsen due to antidepressants - for example, my liver will shrink.
No, it's not. The new generation of antidepressants have very few side effects. Even if you take them for many years, it will not affect your health. Ordinary paracetamol is even more dangerous for the liver than antidepressants.
New generation antidepressants are less effective than older ones.
The new generation of antidepressants are as effective as the old, but have fewer side effects. True, older generation drugs can better cope with severe pain, for example. nine0003
If I take pills for a long time, I will have to increase the dosage.
This is rare. Resistance can be from the very beginning, then the person does not respond well to the action of the drug. Why she appears, no one knows. One of the reasons is the progression of the disease. For example, a person has an anxiety disorder for which they are being treated. Suddenly he gets divorced or fired, he experiences severe stress, under the influence of which a relapse occurs.
I'm depressed and have problems at work - I'll take two or three pills to make it easier. nine0363
It is not recommended to do this - it is pointless. Work anxiety and depression have different mechanisms of occurrence, so increasing the dose of antidepressants will not help.
I will always want to sleep.

It happens. If it interferes with normal life, we simply change the drug. But insomnia or nightmares are more common. To get rid of them, we also change the drug. It's not something a person needs to fight.
I will be incontinent.
If this happens, it is very rare.
I'm pregnant, so I can't take antidepressants.
The instructions for many drugs say that you can. If a pregnant woman is depressed, there is a risk that she will eat less and will not regularly go to the gynecologist. Then this depression will smoothly flow into postpartum depression - then the risk increases that the child will lag behind in speech development, because the mother will talk to him less. But there is no evidence that antidepressants cause fetal malformations. There are studies that describe the association of taking antidepressants during pregnancy with an increased incidence of autism spectrum disorders in children born to such mothers. But it is not clear what exactly this association is connected with: either with the mother’s mental disorder, for which she took medication, or with taking antidepressants. In any case, this is a slight increase in risk. nine0003
In any case, this is a slight increase in risk. nine0003
I'd rather drink St. John's wort, because it's a herbal preparation, not some kind of chemistry.
Definitely not. Interacting with other drugs, St. John's wort can make them toxic or, conversely, reduce their effect to zero. Plus, St. John's wort increases the sensitivity of the skin to sunlight, and a person may experience burns. In general, it is more toxic than many antidepressants.
Antidepressants will make me remember information worse or I will get dementia. Even worse, Alzheimer's disease. nine0363
Not exactly. Antidepressants do not reduce memory, this is a myth. And they have no effect on the development of dementia and Alzheimer's disease.
I will have to try a bunch of different pills, because the first time you can not find the right drug.
Optional. For most people, the first drug prescribed is fine. There are patients who find it difficult to find a medicine due to inefficiency or side effects. But it is impossible to know about it in advance.
But it is impossible to know about it in advance.
Antidepressants will cause serotonin syndrome and I will die. nine0363
Yes, they can cause it, but it happens very rarely and without death. The patient may simply have diarrhea, vomiting, a slight increase in body temperature. But this is not the serotonin syndrome with which they end up in intensive care. But if you mix antidepressants with drugs - mephedrone, cocaine, ecstasy and other stimulants - then the case can end in resuscitation or death. Sometimes serotonin syndrome can appear if antidepressants are mixed with other drugs, but they are always written about in the instructions. On a note, St. John's wort also applies to them. nine0003
Antidepressants are not drugs, but a pharmacological conspiracy.
Of course, for pharmaceutical companies, antidepressants are money. But at the same time, antidepressants are medicine. Before they go on sale, drugs undergo clinical trials with placebo. If antidepressants did not show good results, no one would have put them on the market.