Who developed cbt
Cognitive Behavior Therapy - StatPearls
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
StatPearls [Internet].
Show details
Search term
Suma P. Chand; Daniel P. Kuckel; Martin R. Huecker.
Author Information
Last Update: September 9, 2022.
Continuing Education Activity
In the 1960s, Aaron Beck developed cognitive behavior therapy (CBT) or cognitive therapy. Since then, it has been extensively researched and found to be effective in a large number of outcome studies for psychiatric disorders including depression, anxiety disorders, eating disorders, substance abuse, and personality disorders. It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia.
CBT has been adapted and studied for children, adolescents, adults, couples, and families. This activity reviews the efficacy of CBT in both psychiatric and non-psychiatric disorders and the role of the interprofessional team in using it to improve patient outcomes.
Objectives:
Identify the key concepts of cognitive-behavioral therapy.
Describe the indications for cognitive behavioral therapy.
Outline the structure of cognitive behavioral therapy sessions.
Review the clinical significance of cognitive-behavioral therapy and its efficacy in treating common psychiatric illnesses.
Access free multiple choice questions on this topic.
Introduction
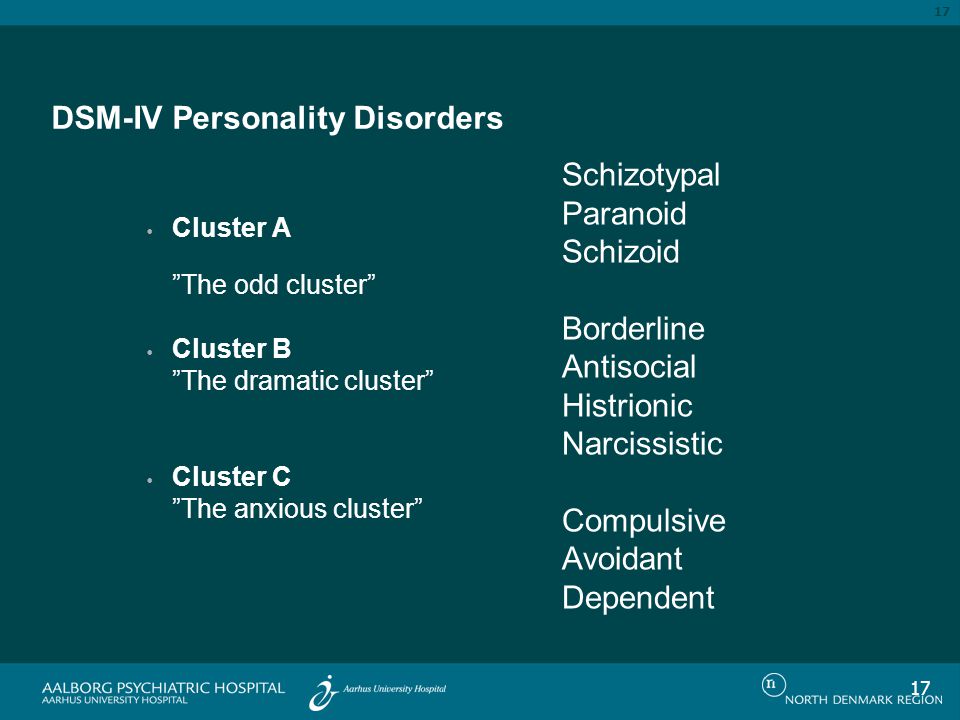
In the 1960s, Aaron Beck developed cognitive behavior therapy (CBT) or cognitive therapy. Since then, it has been extensively researched and found to be effective in a large number of outcome studies for some psychiatric disorders, including depression, anxiety disorders, eating disorders, substance abuse, and personality disorders. It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia. CBT has been adapted and studied for children, adolescents, adults, couples, and families. Its efficacy also has been established in the treatment of non-psychiatric disorders such as irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions.[1][2][3]
It also has been demonstrated to be effective as an adjunctive treatment to medication for serious mental disorders such as bipolar disorder and schizophrenia. CBT has been adapted and studied for children, adolescents, adults, couples, and families. Its efficacy also has been established in the treatment of non-psychiatric disorders such as irritable bowel syndrome, chronic fatigue syndrome, fibromyalgia, insomnia, migraines, and other chronic pain conditions.[1][2][3]
Issues of Concern
Origins of Cognitive Behavior Therapy
The idea for developing this form of psychotherapy took root when Aaron Beck began to notice that his patients with depression often verbalized thoughts that were lacking in validity and noted characteristic “cognitive distortions” in their thinking. His empirical observations led him to start viewing depression not so much as a mood disorder but as a cognitive disorder. Based on his clinical observations and empirical findings, Beck outlined a new cognitive theory of depression. He published Cognitive Therapy for Depression (Beck, Rush, Shaw, and Emery, 1979) after having published a study that evaluated and demonstrated the efficacy of cognitive therapy. The combination of a detailed treatment protocol manual with outcome research was an innovation in psychotherapy practice that had only previously been attempted by behavior therapists in treating discrete behavioral problems. By accomplishing the same feat with a more complex set of clinical interventions that included cognitive, emotional, and behavioral components, Beck pioneered a model for what psychologists many years later defined as an “empirically validated psychological treatment.”
He published Cognitive Therapy for Depression (Beck, Rush, Shaw, and Emery, 1979) after having published a study that evaluated and demonstrated the efficacy of cognitive therapy. The combination of a detailed treatment protocol manual with outcome research was an innovation in psychotherapy practice that had only previously been attempted by behavior therapists in treating discrete behavioral problems. By accomplishing the same feat with a more complex set of clinical interventions that included cognitive, emotional, and behavioral components, Beck pioneered a model for what psychologists many years later defined as an “empirically validated psychological treatment.”
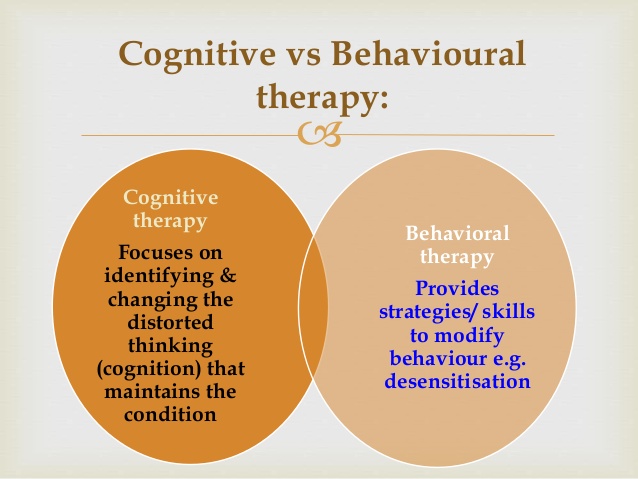
Other clinicians and researchers became interested and began developing CBT treatment protocols and evaluating their efficacy. Specific treatment protocols were developed for some psychiatric disorders. As behavioral strategies were incorporated, the term cognitive therapy changed to cognitive behavior therapy. Today CBT is the most extensively researched of all psychotherapies with several evidence-based treatment protocols.
Today CBT is the most extensively researched of all psychotherapies with several evidence-based treatment protocols.
Cognitive Model
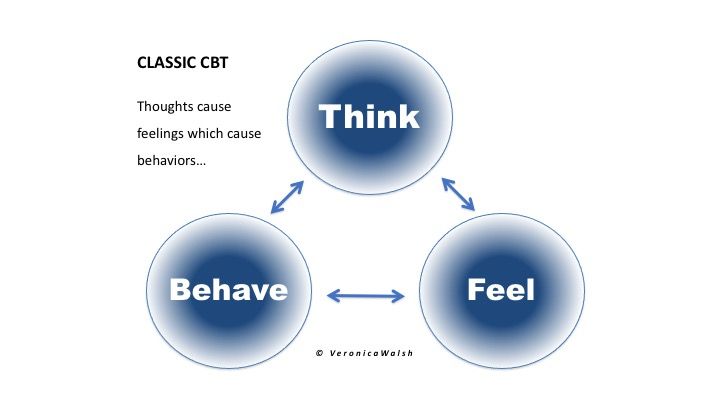
CBT is based on a straightforward, common-sense model of the relationships among cognition, emotion, and behavior.[4][5][6][7]
Three aspects of cognition are emphasized:
Automatic thoughts
Cognitive distortions
Underlying beliefs or schemas
Automatic Thoughts
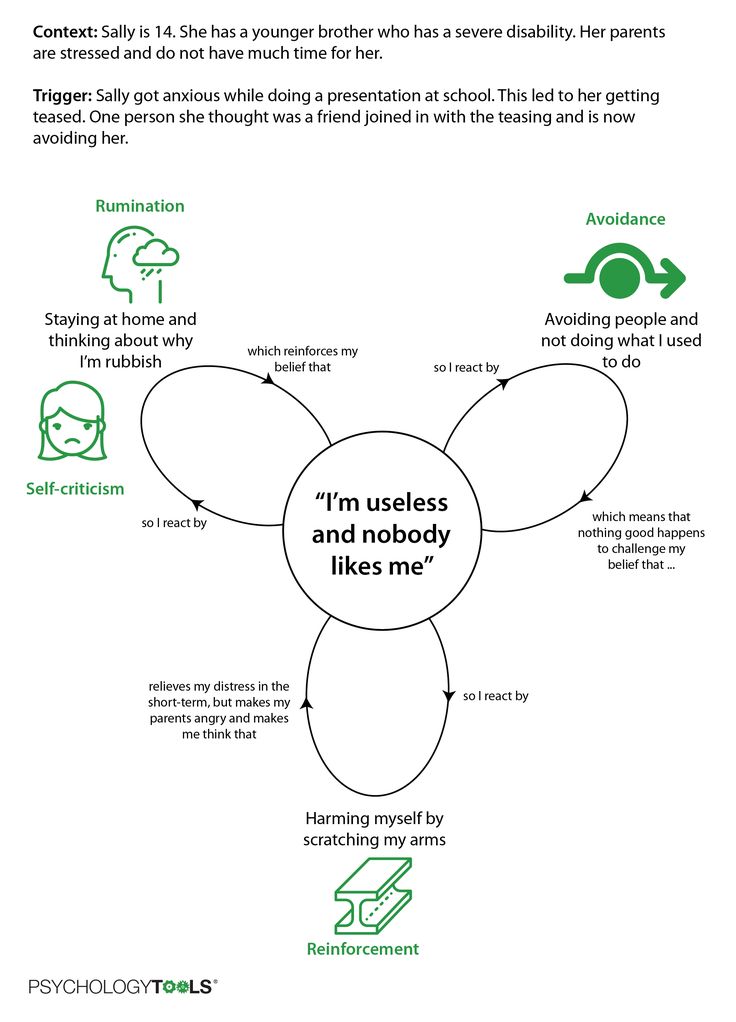
An individual’s immediate, unpremeditated interpretations of events are referred to as automatic thoughts. Automatic thoughts shape both the individual’s emotions and their actions in response to events. For example, a friend may cross you in the hallway and not say hello to you. If you were to have an automatic thought of “he hates me,” or “I have done something to anger him,” it is likely to impact your mood and cause you to feel upset and also to behave in an avoidant manner when you see him next. On the other hand, if you had the automatic thought, “he is in a hurry,” you would not be too concerned, and you would not be avoidant when you were to see him next.
On the other hand, if you had the automatic thought, “he is in a hurry,” you would not be too concerned, and you would not be avoidant when you were to see him next.
CBT is based on the observation that dysfunctional automatic thoughts that are exaggerated, distorted, mistaken, or unrealistic in other ways, play a significant role in psychopathology.
Cognitive Distortions
Errors in logic are quite prevalent in patients with psychological disorders. They lead individuals to erroneous conclusions. Below are some cognitive distortions that are commonly seen in individuals with psychopathology:
Dichotomous thinking: Things are seen regarding two mutually exclusive categories with no shades of gray in between.
Overgeneralization: Taking isolated cases and using them to make wide generalizations.
Selective abstraction: Focusing exclusively on certain, usually negative or upsetting, aspects of something while ignoring the rest.

Disqualifying the positive: Positive experiences that conflict with the individual’s negative views are discounted.
Mind reading: Assuming the thoughts and intentions of others.
Fortune telling: Predicting how things will turn out before they happen.
Minimization: Positive characteristics or experiences are treated as real but insignificant.
Catastrophizing: Focusing on the worst possible outcome, however unlikely, or thinking that a situation is unbearable or impossible when it is just uncomfortable.
Emotional reasoning: Making decisions and arguments based on how you feel rather than objective reality.
“Should” statements: Concentrating on what you think “should” or “ought to be” rather than the actual situation you are faced with or having rigid rules which you always apply no matter the circumstances.
Personalization, blame, or attribution: Assuming you are completely or directly responsible for a negative outcome.
 When applied to others consistently, the blame is the distortion.
When applied to others consistently, the blame is the distortion.
Underlying Beliefs
Underlying beliefs shape the perception and interpretation of events. Belief systems or schemas take shape as we go through life experiences. They are defined as templates or rules for information processing that underlie the most superficial layer of automatic thoughts. Beliefs are understood at two levels in CBT:
Core Beliefs
The central ideas about self and the world
The most fundamental level of belief
They are global, rigid, and overgeneralized
Examples of dysfunctional core beliefs:
Intermediate Beliefs
Consist of assumptions, attitudes, and rules
Influenced in their development by the core beliefs
Examples of dysfunctional intermediate beliefs:
“To be accepted, I should always please others.”
“I should be excellent at everything I do to be considered adequate.
 ”
”“It is best to have as little as possible to do with people.”
Clinical Significance
Cognitive behavior therapy is a structured, didactic, and goal-oriented form of therapy. The approach is hands-on and practical wherein the therapist and patient work in a collaborative manner with the goal of modifying patterns of thinking and behavior to bring about a beneficial change in the patient's mood and way of living his/her life. It is used to help a wide range of problems, and appropriate treatment protocols are applied depending on the diagnosis and problems the patient is facing.[8][9][10][11]
Most psychotherapists who practice CBT personalize and customize the therapy to the specific needs of each patient.
The first step is an assessment of the patient and the initiation of developing an individualized conceptualization of him/her. The conceptualization based on the CBT model is built from session to session and is shared with the patient at an appropriate time later in therapy. The approach to therapy is explained very early at the start of the therapy. The problems patient would like to work on in therapy, and goals for therapy are decided in the first or second session collaboratively. The prioritized problems are worked on first.
The approach to therapy is explained very early at the start of the therapy. The problems patient would like to work on in therapy, and goals for therapy are decided in the first or second session collaboratively. The prioritized problems are worked on first.
The structure of each session:
The session always starts with a brief update and check on mood. This is followed by bridging from the previous session to establish continuity. The agenda of what will be talked about in the session is set up collaboratively, and the homework the patient had to do between the sessions is reviewed before plunging into talking about any problem. Issues on the agenda are talked about punctuated with feedback and summaries. The session ends with setting up further homework and a final summary.
Examples of CBT in practice:
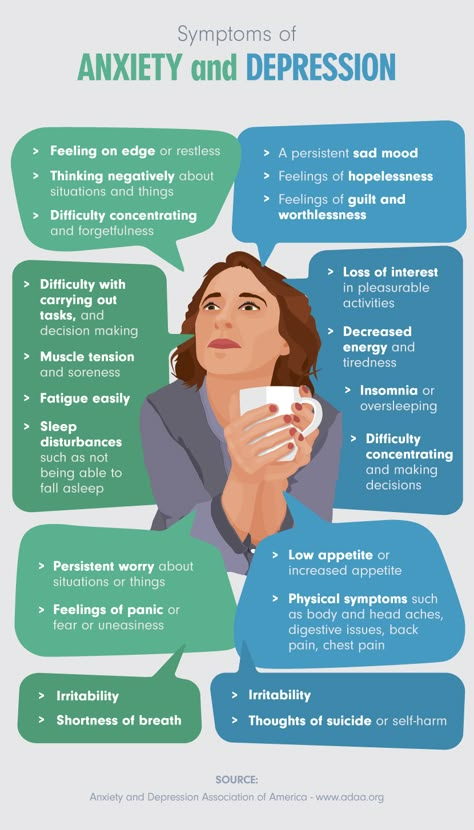
Anxiety: CBT often focuses on replacing negative automatic thoughts that can occur in generalized anxiety disorder and may be used alone or in combination with medications such as selective serotonin reuptake inhibitors, which are typically first-line as benzodiazepines have a greater risk of adverse outcomes.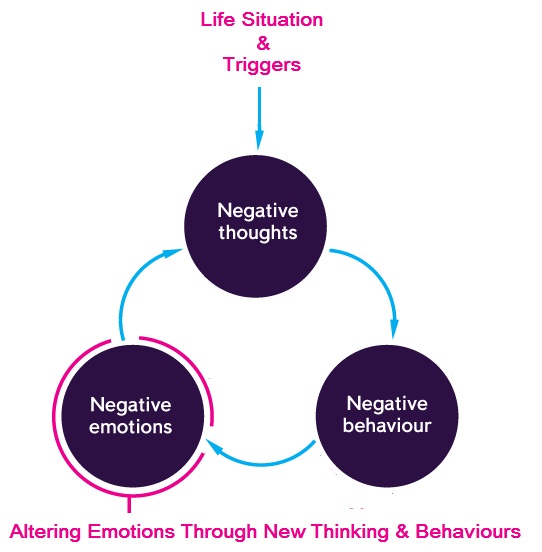 In treating panic disorder, CBT may include desensitization to triggers that provoke anxiety; it is important to note, however, that a potential adverse effect of this technique is a temporary mild increase in anxiety.[12]
In treating panic disorder, CBT may include desensitization to triggers that provoke anxiety; it is important to note, however, that a potential adverse effect of this technique is a temporary mild increase in anxiety.[12]
Depression: In patients with chronic depression, the combination of CBT and antidepressant medication is more effective than either intervention alone. In patients who are no longer taking part in activities that typically bring them pleasure, CBT may initially focus on reinitiating positive activities to overcome inertia.[13]
Attention deficit hyperactivity disorder (ADHD): Behavioral therapy is the initial recommended treatment for children younger than 6 years old, while stimulant medications are the recommended initial intervention for ADHD in children 6 years and older. Behavioral treatments are also recommended for older children, especially if they have a poor response or adverse effects on medication. Behavioral therapy interventions include parent training and behavioral classroom management with a focus on setting clear rules and expectations for the child with appropriate rewards and punishments and daily feedback. [14][15]
[14][15]
Typical CBT treatments involve approximately 60-minute sessions occurring weekly for 8 to 12 weeks.[15]
Enhancing Healthcare Team Outcomes
CBT is a valid and proven form of psychological therapy for a range of mental health disorders. It is important for physicians and nurses to understand that CBT is often used in conjunction with pharmacological therapy to achieve the best outcomes. Moreover, CBT has been shown to provide additional benefits or similar outcomes compared to medication alone. Patients with psychiatric disorders should be referred to a mental health nurse who can educate the patient on treatment options. Primary care physicians are encouraged to develop collaborative relationships with behavior therapists and introduce and monitor the progress of cognitive-behavioral therapy. An interprofessional team approach will result in the best outcomes.[16][17][15]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
van den Berk Clark C, Moore R, Secrest S, Tuerk P, Norman S, Myers U, Lustman PJ, Schneider FD, Barnes J, Gallamore R, Ovais M, Plurad JA, Scherrer JF. Factors Associated With Receipt of Cognitive-Behavioral Therapy or Prolonged Exposure Therapy Among Individuals With PTSD. Psychiatr Serv. 2019 Aug 01;70(8):703-713. [PMC free article: PMC6702958] [PubMed: 31010409]
- 2.
Keefe JR, Chambless DL, Barber JP, Milrod BL. Treatment of anxiety and mood comorbidities in cognitive-behavioral and psychodynamic therapies for panic disorder. J Psychiatr Res. 2019 Jul;114:34-40. [PubMed: 31015099]
- 3.
Zilcha-Mano S, Eubanks CF, Muran JC. Sudden gains in the alliance in cognitive behavioral therapy versus brief relational therapy. J Consult Clin Psychol. 2019 Jun;87(6):501-509. [PMC free article: PMC6533161] [PubMed: 31008637]
- 4.
de Jonge M, Bockting CLH, Kikkert MJ, van Dijk MK, van Schaik DJF, Peen J, Hollon SD, Dekker JJM.
 Preventive cognitive therapy versus care as usual in cognitive behavioral therapy responders: A randomized controlled trial. J Consult Clin Psychol. 2019 Jun;87(6):521-529. [PubMed: 31008635]
Preventive cognitive therapy versus care as usual in cognitive behavioral therapy responders: A randomized controlled trial. J Consult Clin Psychol. 2019 Jun;87(6):521-529. [PubMed: 31008635]- 5.
Tolin DF, Wootton BM, Levy HC, Hallion LS, Worden BL, Diefenbach GJ, Jaccard J, Stevens MC. Efficacy and mediators of a group cognitive-behavioral therapy for hoarding disorder: A randomized trial. J Consult Clin Psychol. 2019 Jul;87(7):590-602. [PubMed: 31008633]
- 6.
Heenan A, Pipe A, Lemay K, Davidson JR, Tulloch H. Cognitive-Behavioral Therapy for Insomnia Tailored to Patients With Cardiovascular Disease: A Pre-Post Study. Behav Sleep Med. 2020 May-Jun;18(3):372-385. [PubMed: 31007057]
- 7.
Janse A, Bleijenberg G, Knoop H. Prediction of long-term outcome after cognitive behavioral therapy for chronic fatigue syndrome. J Psychosom Res. 2019 Jun;121:93-99. [PubMed: 31006534]
- 8.
Webb CA, Stanton CH, Bondy E, Singleton P, Pizzagalli DA, Auerbach RP.
 Cognitive versus behavioral skills in CBT for depressed adolescents: Disaggregating within-patient versus between-patient effects on symptom change. J Consult Clin Psychol. 2019 May;87(5):484-490. [PMC free article: PMC6506214] [PubMed: 30998049]
Cognitive versus behavioral skills in CBT for depressed adolescents: Disaggregating within-patient versus between-patient effects on symptom change. J Consult Clin Psychol. 2019 May;87(5):484-490. [PMC free article: PMC6506214] [PubMed: 30998049]- 9.
Cuijpers P, Noma H, Karyotaki E, Cipriani A, Furukawa TA. Effectiveness and Acceptability of Cognitive Behavior Therapy Delivery Formats in Adults With Depression: A Network Meta-analysis. JAMA Psychiatry. 2019 Jul 01;76(7):700-707. [PMC free article: PMC6583673] [PubMed: 30994877]
- 10.
O'Cleirigh C, Safren SA, Taylor SW, Goshe BM, Bedoya CA, Marquez SM, Boroughs MS, Shipherd JC. Cognitive Behavioral Therapy for Trauma and Self-Care (CBT-TSC) in Men Who have Sex with Men with a History of Childhood Sexual Abuse: A Randomized Controlled Trial. AIDS Behav. 2019 Sep;23(9):2421-2431. [PMC free article: PMC7271561] [PubMed: 30993478]
- 11.
Sahranavard S, Esmaeili A, Salehiniya H, Behdani S.
 The effectiveness of group training of cognitive behavioral therapy-based stress management on anxiety, hardiness and self-efficacy in female medical students. J Educ Health Promot. 2019;8:49. [PMC free article: PMC6432834] [PubMed: 30993142]
The effectiveness of group training of cognitive behavioral therapy-based stress management on anxiety, hardiness and self-efficacy in female medical students. J Educ Health Promot. 2019;8:49. [PMC free article: PMC6432834] [PubMed: 30993142]- 12.
Locke AB, Kirst N, Shultz CG. Diagnosis and management of generalized anxiety disorder and panic disorder in adults. Am Fam Physician. 2015 May 01;91(9):617-24. [PubMed: 25955736]
- 13.
Rupke SJ, Blecke D, Renfrow M. Cognitive therapy for depression. Am Fam Physician. 2006 Jan 01;73(1):83-6. [PubMed: 16417069]
- 14.
Felt BT, Biermann B, Christner JG, Kochhar P, Harrison RV. Diagnosis and management of ADHD in children. Am Fam Physician. 2014 Oct 01;90(7):456-64. [PubMed: 25369623]
- 15.
Coffey SF, Banducci AN, Vinci C. Common Questions About Cognitive Behavior Therapy for Psychiatric Disorders. Am Fam Physician. 2015 Nov 01;92(9):807-12. [PubMed: 26554473]
- 16.
Wu CY, Rodakowski JL, Terhorst L, Karp JF, Fields B, Skidmore ER. A Scoping Review of Nonpharmacological Interventions to Reduce Disability in Older Adults. Gerontologist. 2020 Jan 24;60(1):e52-e65. [PMC free article: PMC7182004] [PubMed: 31002312]
- 17.
Ngamkham S, Holden JE, Smith EL. A Systematic Review: Mindfulness Intervention for Cancer-Related Pain. Asia Pac J Oncol Nurs. 2019 Apr-Jun;6(2):161-169. [PMC free article: PMC6371675] [PubMed: 30931361]
Copyright © 2022, StatPearls Publishing LLC.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.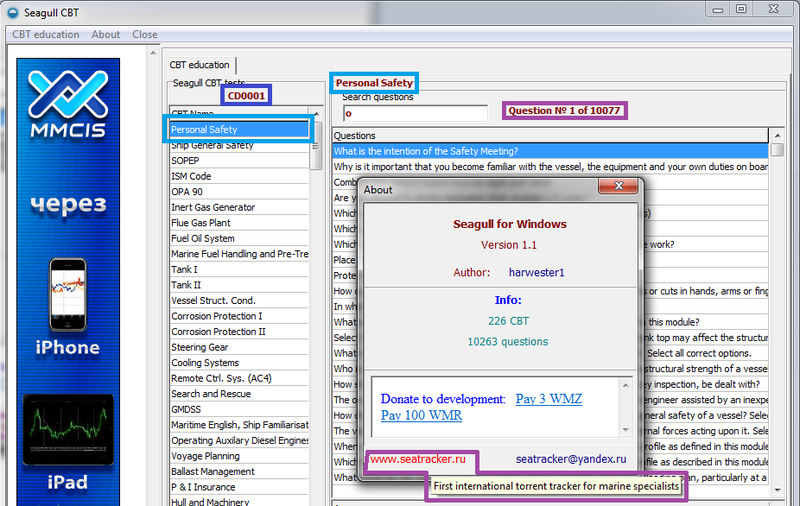
Bookshelf ID: NBK470241PMID: 29261869
The History of Cognitive Behavioural Therapy (CBT)
Posted March 7th, 2022 Written By: Maggie Morrow
Cognitive behavioural therapy (CBT) is a popular psychological treatment which has been shown to be effective in treating common disorders such as anxiety and depression.
CBT is not a new therapy by any means and it has a practical structure which makes it easily measurable. These factors have resulted in a large body of successful clinical trials which, more recently, have secured its position as one of a range of recommended treatments on the NHS.
What is CBT?
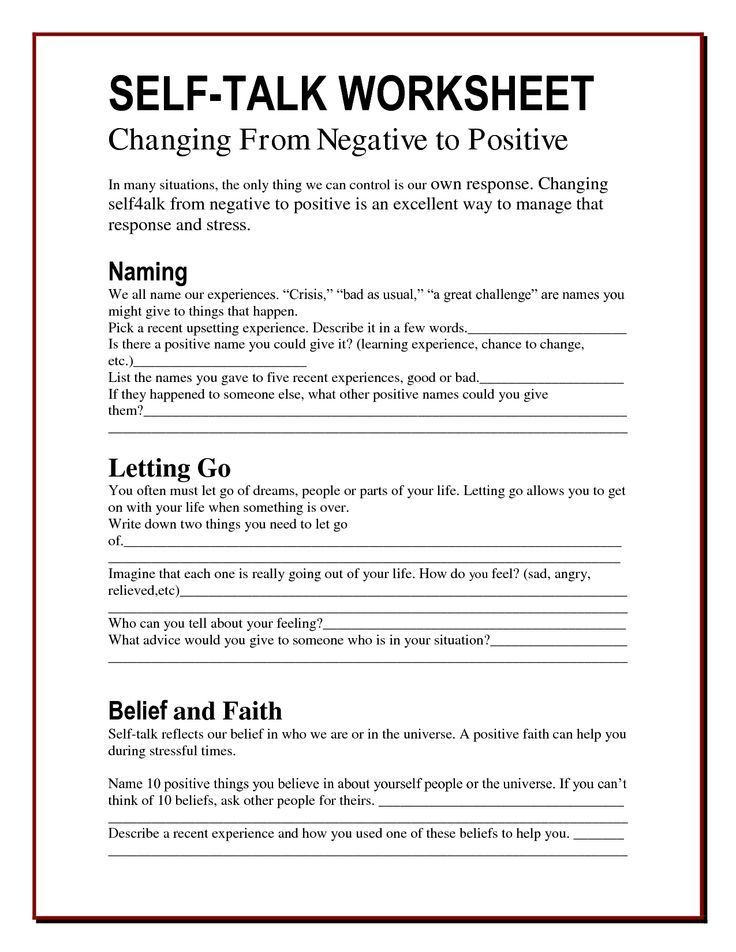
Cognitive behavioural therapy is a type of talking therapy which involves identifying and challenging unhelpful thoughts. It works to help people learn alternative thinking patterns and behaviours which can then improve the way they feel. CBT explores the relationship between feelings, thoughts, and behaviours, and evolved from two distinct schools of psychology: behaviourism and cognitive therapy. Its roots can be traced to these two approaches.
Its roots can be traced to these two approaches.
Behavioural treatment for mental disorders has been around since the early 1900’s. Key proponents like Skinner, Pavlov, and Watson developed theories of change and behavioural treatments. Behaviourism is based on the idea that behaviours can be measured, modelled, and changed.
The first wave of behavioural therapy came about in the 1930/40s in response to the emotional impacts faced by the many WWII veterans returning from war. This need for effective short-term therapy for depression and anxiety coincided with a build up of behavioural research regarding how people learn to behave and react to life situations. Behaviourism offered an alternative to the dominant model of that time, psychoanalysis.
Cognitive Therapy RootsAmerican psychologist Albert Ellis was one of the key figures who developed cognitive therapy. He stressed the importance of thoughts/feelings and behaviours and devised a theory called rational emotive behaviour therapy (REBT) in the 1950s. This is now considered one of the earliest forms of cognitive psychotherapy. It is based on the idea that a person’s emotional distress arises from their thoughts about an event rather than the actual event itself.
This is now considered one of the earliest forms of cognitive psychotherapy. It is based on the idea that a person’s emotional distress arises from their thoughts about an event rather than the actual event itself.
In the 1950s and 1960s, American psychiatrist Aaron T. Beck noticed patterns with his depressed clients. They seemed to hold negative views of self, others and their future, and no matter how much exploration of their past occurred, these negative views did not shift. This led him to start researching whether holding negative views about self, others and the world, might be part of the reason somebody was depressed. Cognitive therapy was up and running.
Automatic Thoughts in Cognitive TherapyBeck understood the importance of the link between thoughts and feelings, and he coined the term “automatic thoughts” to describe the thoughts that pop up in people’s minds. He discovered that although people aren’t always aware of these thoughts, they can learn to identify and report them. He found that people who were upset had negative thoughts that tended to be unrealistic, and by uncovering and challenging these thoughts, long-lasting and positive change can result. In essence, CBT helps people to recognise their thoughts and test them out. This then allows the possibility of finding alternatives and opens up choice.
He found that people who were upset had negative thoughts that tended to be unrealistic, and by uncovering and challenging these thoughts, long-lasting and positive change can result. In essence, CBT helps people to recognise their thoughts and test them out. This then allows the possibility of finding alternatives and opens up choice.
By the 1960s, a number of empirical studies into how cognitions affect behaviours and emotions were carried out. This period became known as the cognitive revolution. It emphasised the role that conscious thinking plays in psychotherapy.
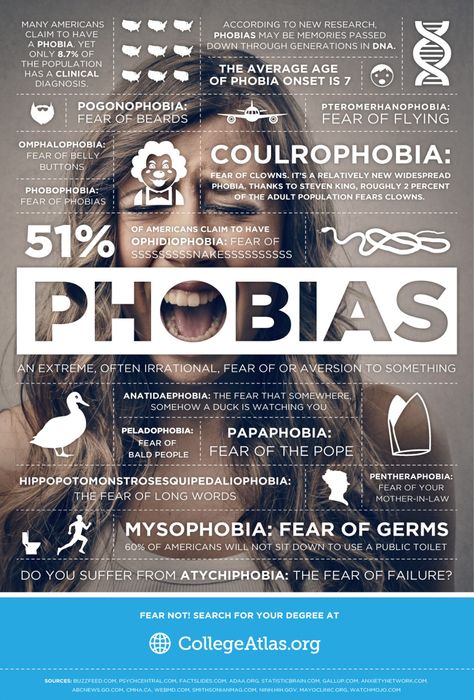
Combining the ApproachesBehavioural therapies were successful in treating a number of conditions, including phobias and anxiety. As the popularity of cognitive therapies began to soar, therapists started to use behavioural techniques and incorporate these to successfully treat disorders. Although each of these schools of thought has a different emphasis, both are concerned with what is happening to the individual in the here and now.
CBT continues to evaluate it’s techniques and treatments. This has built up a large body of research about its effectiveness for use with a broad range of psychological issues. It has been shown as an effective form of therapy for treating a range of conditions, including:
- Anxiety
- Panic Disorder
- Depression
- OCD – Obsessive Compulsive Disorder
- Phobias
- Irritable Bowel Syndrome
- Chronic Fatigue
- Eating Disorders
CBT and Other Therapies
Today, a number of therapies blend cognitive and behavioural elements into their approach, including:
- Integrative Psychotherapy
- Reality therapy
- Multimodal therapy
- Eye movement desensitisation and reprocessing
- Cognitive processing therapy
- Acceptance and commitment therapy
- Dialectical behaviour therapy
Further Reading on CBT and Issues it Can Help With
How Cognitive Behavioural Therapy Can Help Treat Anxiety Disorders
How Can Cognitive Behavioural Therapy Help to Treat Depression?
Panic Attacks: How Can Cognitive Behavioural Therapy Help?
Cognitive Distortions and Thinking Errors – How Can CBT Help?
CBT Therapy in London
Like this post? Spread the word!
Cognitive behavioral therapy | PSYCHOLOGIES
On November 1, 2021, Aaron Temkin Beck, an American psychotherapist, professor of psychiatry, who went down in history as the creator of the cognitive-behavioral direction in psychotherapy, died.
"The key to understanding and solving psychological problems lies in the patient's mind," said the psychotherapist. His groundbreaking approach to working with depression, phobias and anxiety disorders has shown good results in therapy with clients and has become popular with professionals around the world. nine0003
What is it?
This method of psychotherapy appeals to consciousness and helps to get rid of stereotypes and preconceived ideas that deprive us of freedom of choice and push us to act according to a pattern.
The method allows, if necessary, to correct the unconscious, "automatic" conclusions of the patient. He perceives them as truth, but in reality they can greatly distort real events. These thoughts often become the source of painful emotions, inappropriate behavior, depression, anxiety disorders, and other illnesses. nine0003
Principle of action
Therapy is based on the joint work of the therapist and the patient. The therapist does not teach the patient how to think correctly, but together with him understands whether the habitual type of thinking helps him or hinders him. The key to success is the active participation of the patient, who will not only work in sessions, but also do homework.
The key to success is the active participation of the patient, who will not only work in sessions, but also do homework.
If in the beginning the therapy focuses only on the symptoms and complaints of the patient, then gradually it begins to affect the unconscious areas of thinking - core beliefs, as well as childhood events that influenced their formation. The principle of feedback is important - the therapist constantly checks how the patient understands what is happening in therapy, and discusses possible errors with him. nine0003
Progress of work
The patient and the psychotherapist find out under what circumstances the problem manifests itself: how “automatic thoughts” arise and how they affect his ideas, experiences and behavior. In the first session, the therapist only listens carefully to the patient, and in the next they discuss in detail the patient's thoughts and behavior in numerous everyday situations: what does he think about when he wakes up? What about breakfast? The goal is to make a list of moments and situations that cause anxiety. nine0003
nine0003
The therapist and patient then plan a program of work. It includes tasks to complete in places or circumstances that cause anxiety - take the elevator, eat dinner in a public place ... These exercises allow you to consolidate new skills and gradually change behavior. A person learns to be less rigid and categorical, to see different facets of a problem situation.
The therapist constantly asks questions and explains points that will help the patient understand the problem. Each session is different from the previous one, because each time the patient moves forward a little and gets used to living without the support of the therapist in accordance with new, more flexible views. nine0003
Instead of "reading" other people's thoughts, a person learns to distinguish his own, begins to behave differently, and as a result, his emotional state also changes. He calms down, feels more alive and free. He begins to be friends with himself and stops judging himself and other people.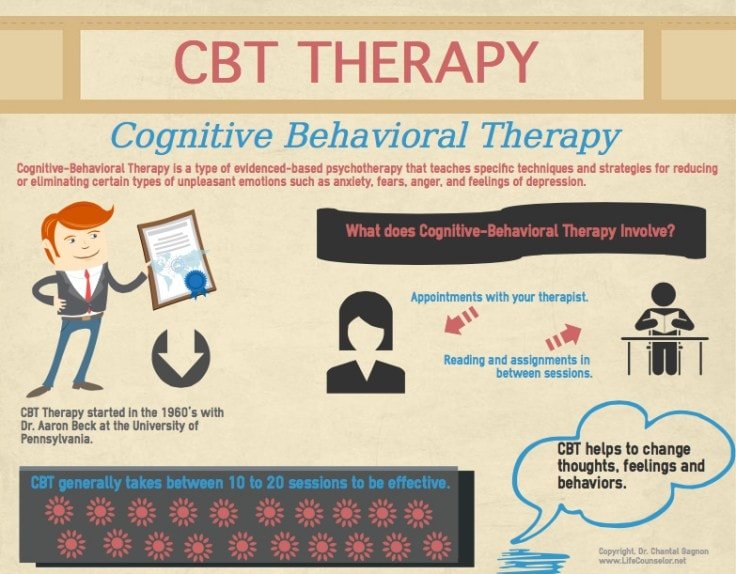
When is it needed?
Cognitive therapy is effective in dealing with depression, panic attacks, social anxiety, obsessive-compulsive disorder and eating disorders. This method is also used to treat alcoholism, drug addiction and even schizophrenia (as a supportive method). At the same time, cognitive therapy is also suitable for dealing with low self-esteem, relationship difficulties, perfectionism, and procrastination. nine0003
It can be used both in individual work and in work with families. But it is not suitable for those patients who are not ready to take an active part in the work and expect the therapist to give advice or simply interpret what is happening.
How long should I have therapy? How much is it?
The number of meetings depends on the willingness of the client to work, the complexity of the problem and the conditions of his life. Each session lasts 50 minutes. The course of therapy is from 5-10 sessions 1-2 times a week. In some cases, therapy can last longer than six months.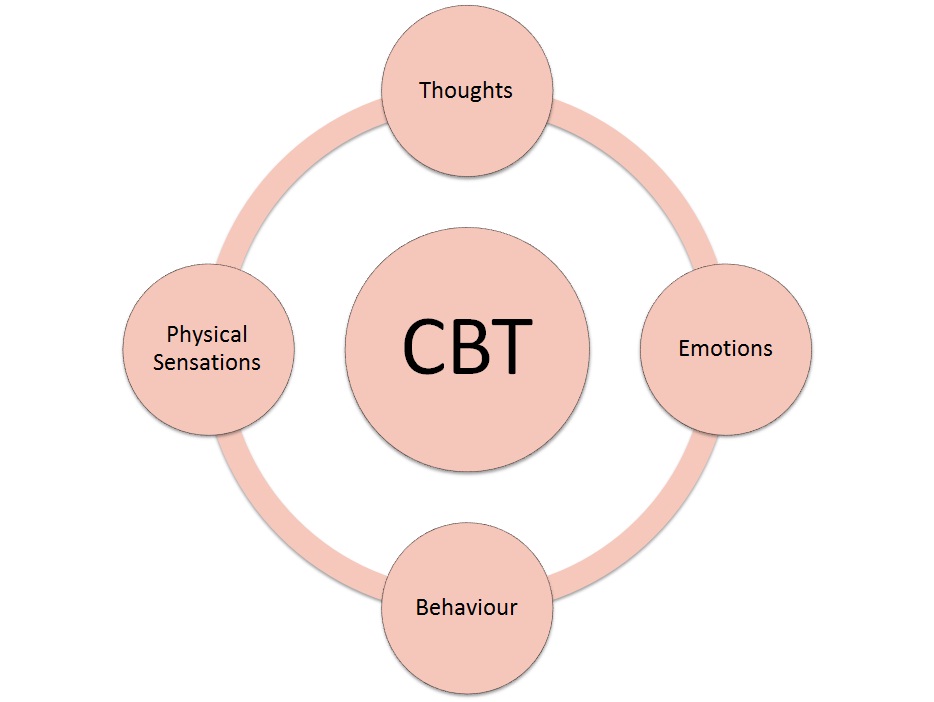 nine0003
nine0003
Aaron Beck died in the USA, the creator of cognitive-behavioral psychotherapy, which is used in the treatment of depression
Dr. Aaron T. Beck with his daughter Judith Beck
Twitter / Institute for Cognitive Psychotherapy and Research
nine0002 At the age of 100, Dr. Aaron T. Beck, a psychotherapist who is considered the "father" of cognitive-behavioral therapy, in particular used in the treatment of depression, died on the morning of November 1.Reported by the Institute for Cognitive Psychotherapy and Research, which Aaron Beck co-founded with his daughter Judith Beck.
The therapist died peacefully at his home in Philadelphia.
“My father dedicated his life to developing and testing treatments to improve the lives of countless people around the world with mental health problems.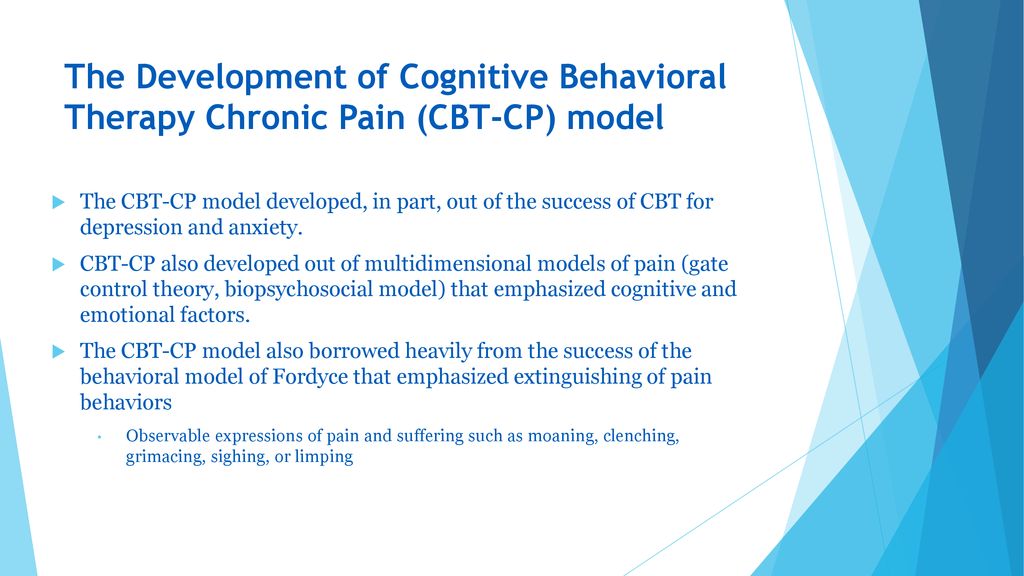 He changed the field of mental health through his own development and research into cognitive behavioral therapy.”, Judith Beck said in a statement.
He changed the field of mental health through his own development and research into cognitive behavioral therapy.”, Judith Beck said in a statement.
What will the scientist be remembered for?
Aaron Beck developed CBT in the 1960s while at the University of Pennsylvania. He created therapies after noticing that his depressed patients often had distorted negative thoughts, also called automatic thoughts ("Nobody loves me", "I will always be a loser"). Beck argued that patients should focus on the thoughts they have here and now, analyze them and change them to improve their lives, writes The Guardian. nine0003
Cognitive Behavioral Therapy emerged as a counterpoint to Freud's psychoanalysis, during which the patient plunges into childhood and searches for hidden internal conflicts. And cognitive therapy analyzes the thoughts that appear now.
Beck refuted Freud's theory that people were depressed because they needed to suffer.