Where to go when your depressed
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
Alcohol, Tobacco, and Other Drugs
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Misusing alcohol, tobacco, and other drugs can have both immediate and long-term health effects.The misuse and abuse of alcohol, tobacco, illicit drugs, and prescription medications affect the health and well-being of millions of Americans. NSDUH estimates allow researchers, clinicians, policymakers, and the general public to better understand and improve the nation’s behavioral health. These reports and detailed tables present estimates from the 2021 National Survey on Drug Use and Health (NSDUH).
Alcohol
Data:
- Among the 133.1 million current alcohol users aged 12 or older in 2021, 60.0 million people (or 45.1%) were past month binge drinkers.
 The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH)
The percentage of people who were past month binge drinkers was highest among young adults aged 18 to 25 (29.2% or 9.8 million people), followed by adults aged 26 or older (22.4% or 49.3 million people), then by adolescents aged 12 to 17 (3.8% or 995,000 people). (2021 NSDUH) - Among people aged 12 to 20 in 2021, 15.1% (or 5.9 million people) were past month alcohol users. Estimates of binge alcohol use and heavy alcohol use in the past month among underage people were 8.3% (or 3.2 million people) and 1.6% (or 613,000 people), respectively. (2021 NSDUH)
- In 2020, 50.0% of people aged 12 or older (or 138.5 million people) used alcohol in the past month (i.e., current alcohol users) (2020 NSDUH)
- Among the 138.5 million people who were current alcohol users, 61.6 million people (or 44.4%) were classified as binge drinkers and 17.7 million people (28.8% of current binge drinkers and 12.8% of current alcohol users) were classified as heavy drinkers (2020 NSDUH)
- The percentage of people who were past month binge alcohol users was highest among young adults aged 18 to 25 (31.
 4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH)
4%) compared with 22.9% of adults aged 26 or older and 4.1% of adolescents aged 12 to 17 (2020 NSDUH) - Excessive alcohol use can increase a person’s risk of stroke, liver cirrhosis, alcoholic hepatitis, cancer, and other serious health conditions
- Excessive alcohol use can also lead to risk-taking behavior, including driving while impaired. The Centers for Disease Control and Prevention reports that 29 people in the United States die in motor vehicle crashes that involve an alcohol-impaired driver daily
Programs/Initiatives:
- STOP Underage Drinking interagency portal - Interagency Coordinating Committee on the Prevention of Underage Drinking
- Interagency Coordinating Committee on the Prevention of Underage Drinking
- Talk. They Hear You.
- Underage Drinking: Myths vs. Facts
- Talking with your College-Bound Young Adult About Alcohol
Relevant links:
- National Association of State Alcohol and Drug Abuse Directors
- Department of Transportation Office of Drug & Alcohol Policy & Compliance
- Alcohol Policy Information Systems Database (APIS)
- National Institute on Alcohol Abuse and Alcoholism
Tobacco
Data:
- In 2020, 20.
 7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH)
7% of people aged 12 or older (or 57.3 million people) used nicotine products (i.e., used tobacco products or vaped nicotine) in the past month (2020 NSDUH) - Among past month users of nicotine products, nearly two thirds of adolescents aged 12 to 17 (63.1%) vaped nicotine but did not use tobacco products. In contrast, 88.9% of past month nicotine product users aged 26 or older used only tobacco products (2020 NSDUH)
- Tobacco use is the leading cause of preventable death, often leading to lung cancer, respiratory disorders, heart disease, stroke, and other serious illnesses. The CDC reports that cigarette smoking causes more than 480,000 deaths each year in the United States
- The CDC’s Office on Smoking and Health reports that more than 16 million Americans are living with a disease caused by smoking cigarettes
Electronic cigarette (e-cigarette) use data:
- In 2021, 13.2 million people aged 12 or older (or 4.7%) used an e-cigarette or other vaping device to vape nicotine in the past month.
 The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people).
The percentage of people who vaped nicotine was highest among young adults aged 18 to 25 (14.1% or 4.7 million people), followed by adolescents aged 12 to 17 (5.2% or 1.4 million people), then by adults aged 26 or older (3.2% or 7.1 million people). - Among people aged 12 to 20 in 2021, 11.0% (or 4.3 million people) used tobacco products or used an e-cigarette or other vaping device to vape nicotine in the past month. Among people in this age group, 8.1% (or 3.1 million people) vaped nicotine, 5.4% (or 2.1 million people) used tobacco products, and 3.4% (or 1.3 million people) smoked cigarettes in the past month. (2021 NSDUH)
- Data from the Centers for Disease Control and Prevention’s 2020 National Youth Tobacco Survey. Among both middle and high school students, current use of e-cigarettes declined from 2019 to 2020, reversing previous trends and returning current e-cigarette use to levels similar to those observed in 2018
- E-cigarettes are not safe for youth, young adults, or pregnant women, especially because they contain nicotine and other chemicals
Resources:
- Tips for Teens: Tobacco
- Tips for Teens: E-cigarettes
- Implementing Tobacco Cessation Programs in Substance Use Disorder Treatment Settings
- Synar Amendment Program
Links:
- Truth Initiative
- FDA Center for Tobacco Products
- CDC Office on Smoking and Health
- National Institute on Drug Abuse: Tobacco, Nicotine, and E-Cigarettes
- National Institute on Drug Abuse: E-Cigarettes
Opioids
Data:
- Among people aged 12 or older in 2021, 3.
 3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH)
3% (or 9.2 million people) misused opioids (heroin or prescription pain relievers) in the past year. Among the 9.2 million people who misused opioids in the past year, 8.7 million people misused prescription pain relievers compared with 1.1 million people who used heroin. These numbers include 574,000 people who both misused prescription pain relievers and used heroin in the past year. (2021 NSDUH) - Among people aged 12 or older in 2020, 3.4% (or 9.5 million people) misused opioids in the past year. Among the 9.5 million people who misused opioids in the past year, 9.3 million people misused prescription pain relievers and 902,000 people used heroin (2020 NSDUH)
- According to the Centers for Disease Control and Prevention’s Understanding the Epidemic, an average of 128 Americans die every day from an opioid overdose
Resources:
- Medication-Assisted Treatment
- Opioid Overdose Prevention Toolkit
- TIP 63: Medications for Opioid Use Disorder
- Use of Medication-Assisted Treatment for Opioid Use Disorder in Criminal Justice Settings
- Opioid Use Disorder and Pregnancy
- Clinical Guidance for Treating Pregnant and Parenting Women With Opioid Use Disorder and Their Infants
- The Facts about Buprenorphine for Treatment of Opioid Addiction
- Pregnancy Planning for Women Being Treated for Opioid Use Disorder
- Tips for Teens: Opioids
- Rural Opioid Technical Assistance Grants
- Tribal Opioid Response Grants
- Provider’s Clinical Support System - Medication Assisted Treatment Grant Program
Links:
- National Institute on Drug Abuse: Opioids
- National Institute on Drug Abuse: Heroin
- HHS Prevent Opioid Abuse
- Community Anti-Drug Coalitions of America
- Addiction Technology Transfer Center (ATTC) Network
- Prevention Technology Transfer Center (PTTC) Network
Marijuana
Data:
- In 2021, marijuana was the most commonly used illicit drug, with 18.
 7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people).
7% of people aged 12 or older (or 52.5 million people) using it in the past year. The percentage was highest among young adults aged 18 to 25 (35.4% or 11.8 million people), followed by adults aged 26 or older (17.2% or 37.9 million people), then by adolescents aged 12 to 17 (10.5% or 2.7 million people). - The percentage of people who used marijuana in the past year was highest among young adults aged 18 to 25 (34.5%) compared with 16.3% of adults aged 26 or older and 10.1% of adolescents aged 12 to 17 (2020 NSDUH)
- Marijuana can impair judgment and distort perception in the short term and can lead to memory impairment in the long term
- Marijuana can have significant health effects on youth and pregnant women.
Resources:
- Know the Risks of Marijuana
- Marijuana and Pregnancy
- Tips for Teens: Marijuana
Relevant links:
- National Institute on Drug Abuse: Marijuana
- Addiction Technology Transfer Centers on Marijuana
- CDC Marijuana and Public Health
Emerging Trends in Substance Misuse:
- Methamphetamine—In 2019, NSDUH data show that approximately 2 million people used methamphetamine in the past year.
 Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia.
Approximately 1 million people had a methamphetamine use disorder, which was higher than the percentage in 2016, but similar to the percentages in 2015 and 2018. The National Institute on Drug Abuse Data shows that overdose death rates involving methamphetamine have quadrupled from 2011 to 2017. Frequent meth use is associated with mood disturbances, hallucinations, and paranoia. - Cocaine—In 2019, NSDUH data show an estimated 5.5 million people aged 12 or older were past users of cocaine, including about 778,000 users of crack. The CDC reports that overdose deaths involving have increased by one-third from 2016 to 2017. In the short term, cocaine use can result in increased blood pressure, restlessness, and irritability. In the long term, severe medical complications of cocaine use include heart attacks, seizures, and abdominal pain.
- Kratom—In 2019, NSDUH data show that about 825,000 people had used Kratom in the past month. Kratom is a tropical plant that grows naturally in Southeast Asia with leaves that can have psychotropic effects by affecting opioid brain receptors.
 It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
It is currently unregulated and has risk of abuse and dependence. The National Institute on Drug Abuse reports that health effects of Kratom can include nausea, itching, seizures, and hallucinations.
Resources:
- Tips for Teens: Methamphetamine
- Tips for Teens: Cocaine
- National Institute on Drug Abuse
More SAMHSA publications on substance use prevention and treatment.
Last Updated: 01/05/2023
"I'd rather sleep in the evening." How to recognize depression and save your life
At the beginning of this week, sad news came from the city of Karkaraly, Karaganda region: the former member of SuperStar.kz, singer Zhanar Khamitova, died. Earlier, in one of the talk shows, a 30-year-old woman spoke about depression and fear of going on stage, it was also reported that after the divorce, her children stayed with their father in Turkey. Police said they were investigating "incitement to suicide. "
"
Tengrinews.kz correspondent Olga Pastukhova addressed psychotherapist, psychiatrist Zhibek Zholdasova with 5 questions about how to recognize and cure depression. Despite the fact that today this is a very popular diagnosis, according to world statistics, no more than 20-30 percent of patients with depression reach a specialist. Meanwhile, in 80 percent of cases, according to world statistics, suicide is committed by people suffering from severe mental disorders, including depressive ones. There are no exact data for Kazakhstan.
How to recognize depression?
When indifference to everything, unwillingness to communicate, depression last for more than two weeks, then most likely it is depression. This disease can happen to anyone - just like the flu. No one is safe from her.
If a person wakes up in the morning with the thoughts “it would be better to sleep in the evening” and there is a feeling of lengthening the time, then this can be either a mild degree of depression or a manifestation of emotional burnout. Very often people think that depression will go away if you go on vacation or have a holiday. However, such a switch will only help in case of emotional burnout. If you have depression, you need to consult a specialist - a psychotherapist or a psychiatrist.
Very often people think that depression will go away if you go on vacation or have a holiday. However, such a switch will only help in case of emotional burnout. If you have depression, you need to consult a specialist - a psychotherapist or a psychiatrist.
A person can be under the supervision of ordinary doctors for a long time. In some cases, depression is disguised as somatic diseases: osteochondrosis, migraines, abdominal pain, high blood pressure, addiction to alcohol and drugs, and so on. If a patient cannot be diagnosed for a long time or he is overcome by more and more new ailments, then this may be another reason to think about depression. A separate place is occupied by postpartum depression - mental changes can occur after childbirth, miscarriage, abortion or stillbirth in the first two months.
Normally, a person - both a child and an adult - has an instinct for self-preservation. If a person too often gets into unpleasant situations, emergencies, injuries, etc. happen to him, then this is another bell about self-destruction. After all, perhaps, after one of these situations, he will not be saved. We do not know what is the percentage of hidden suicides in those situations that were classified as accidents.
happen to him, then this is another bell about self-destruction. After all, perhaps, after one of these situations, he will not be saved. We do not know what is the percentage of hidden suicides in those situations that were classified as accidents.
Any psychotraumatic situation affects a person either mobilizing or destructive. Normally, stress should mobilize a person. But if a person at a difficult moment was weakened by an illness, for example, the flu, or was left without friendly support - he has no one to call, then he will suffer a new blow of fate harder. And then, instead of mobilization, distress begins - a program of self-destruction of the body.
How can depression lead to suicide?
The algorithm from depressive mood to suicide is as follows.
First comes self-accusation: "Why did I do this and not do this?", "Probably should have said that?". This is followed by self-flagellation and humiliation: "I'm a loser, a loser", "I need to be like this . ..". That is, a person gradually drives himself into a corner. When self-flagellation reaches the limit, thoughts about the aimlessness of life and the desire for death appear: “I am not capable of anything”, “I am not worthy to live in this world”, “I wish a brick fell on my head, I would get a serious illness, I'd get hit by a car to end it."
..". That is, a person gradually drives himself into a corner. When self-flagellation reaches the limit, thoughts about the aimlessness of life and the desire for death appear: “I am not capable of anything”, “I am not worthy to live in this world”, “I wish a brick fell on my head, I would get a serious illness, I'd get hit by a car to end it."
If at this stage you do not seek medical help, then thoughts become suicidal. The thought "I wish I was hit by a car" is transformed into "I'll go and throw myself under the car."
How is depression diagnosed?
The most popular test in clinical practice is the Hamilton scale. A person can go through it himself, calculate the points, and if he shows depression, then seek help. This is a significant aid to clinicians in identifying depression.
But psychiatrists and psychotherapists do not use scales in their work. They ask in great detail about the symptoms. Psychiatry and psychotherapy is the only branch of medicine that does not lend itself to any objective research methods. To diagnose depression, you can’t do, say, an ultrasound or MRI of the brain or a blood test. Will show nothing. Only a subjective, descriptive way of collecting information.
To diagnose depression, you can’t do, say, an ultrasound or MRI of the brain or a blood test. Will show nothing. Only a subjective, descriptive way of collecting information.
It is good if a person comes to an appointment with a specialist together with someone who will confirm and clarify the information. In principle, the diagnosis is made in one visit. If you suspect depression in a loved one, then you can give a test and persuade him to visit a specialist.
Who else can help?
The good news is that today in Kazakhstan not only psychotherapists and psychiatrists, but also therapists (GPs), neuropathologists, and endocrinologists can prescribe antidepressants. According to the order currently in force according to the standard of psychiatric care, general practitioners can treat borderline mental disorders: anxiety, fears, depression.
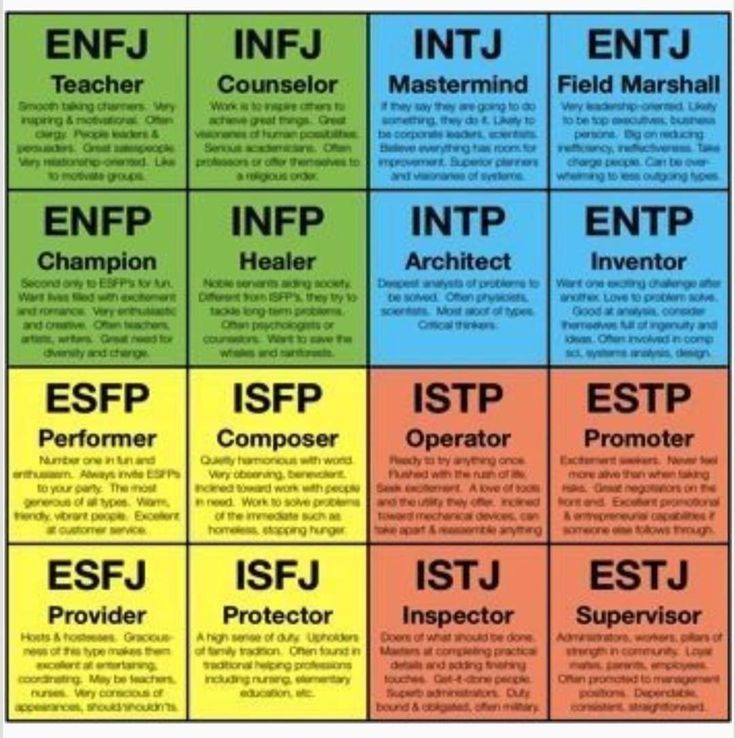
The first step in diagnosing depression for a person can be a psychologist. However, a truly competent specialist always cooperates with a psychiatrist, to whom he will redirect to confirm the diagnosis and prescribe medication. And after that, he will make a plan for his work.
And after that, he will make a plan for his work.
Earlier in an interview with our publication, Zhibek Zholdasova spoke about the difference between a psychologist, psychotherapist and psychiatrist:
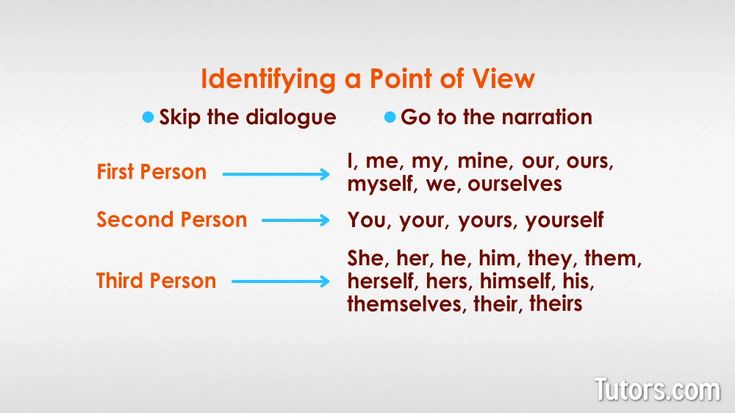
Psychologist helps healthy people to solve issues of emotions, interpersonal relationships, that is, to live better. A psychologist does not write prescriptions or make diagnoses.
Psychotherapist is a doctor with a specialization in psychotherapy, he prescribes drugs and carries out psychocorrection. He deals with neurosis and borderline mental disorders, when a person's condition significantly interferes with communication, work and raising children.
Psychiatrist - a more general medical education in mental disorders. Psychiatrists are divided into psychotherapists, narcologists, sex therapists, clinical and medical psychologists. People go to a psychiatrist with impaired attention, thinking, memory, perception, feelings, emotions, behavior and sensations.
A psychiatrist deals with manifestations of a person that help to live in the world around him - to set goals and achieve them.
People with depression who do not reach specialists tend to self-medicate: they seek help from magicians, practice spiritual practices, go to healers and psychics, exorcise genies. But in fact, only a few manage to cope with depression on their own.
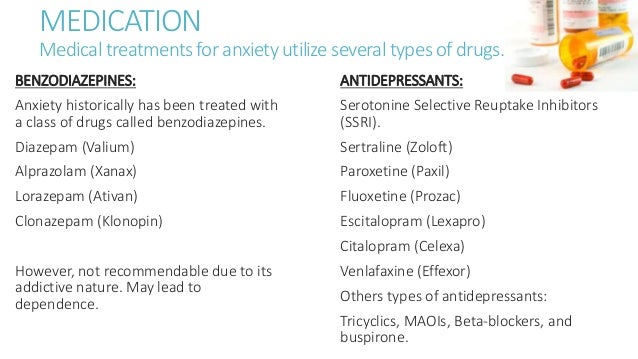
How is depression treated?
The main treatment for depression is antidepressants. Rumors about their harm are a post-Soviet myth: the old drugs did have a number of pronounced side effects. The current generation of antidepressants has a good level of tolerance. There are individual reactions, but by contacting a doctor, you can always change the drug or adjust the dosage.
Drug treatment is prescribed for a course of 5-6 months. The effect of antidepressants appears after a week of taking: a person feels that life has improved, some kind of joy has appeared, sensations have changed, thoughts have become more blissful, not as pessimistic as before. Plus, a visit to a psychologist / psychotherapist is required.
Plus, a visit to a psychologist / psychotherapist is required.
The main treatment for all mental disorders - including depression, anxiety, fears - is psychotherapy. I explain to my patients this way: medicines do not solve problems, they only remove symptoms. This is a kind of crutch that will help to cope with unwanted symptoms, improve the quality of life. It becomes easier to go to work, anxiety goes away, sleep normalizes. A person, in principle, begins to better cope with life, remembers what it is to make plans, and enjoys life.
If the drugs are canceled, but the psychotherapist is not visited, then there is a possibility that the condition will return. Because during the time of taking the medicine, the personality of the person has not changed: the problems that led to this condition have not been solved.
Depression is still stigmatized in our society. Many people do not talk about their condition. Depressive symptoms just cause a person to isolate himself, not to go out anywhere, not to communicate with anyone. To recover, you need to talk about your problems to others, you need to seek help, communication.
Olga Pastukhova
"Psychiatrists should treat depression": three signs of the disease and how to avoid it Therefore, it is not surprising that the theme of World Health Day, which is celebrated on April 7, is depression.
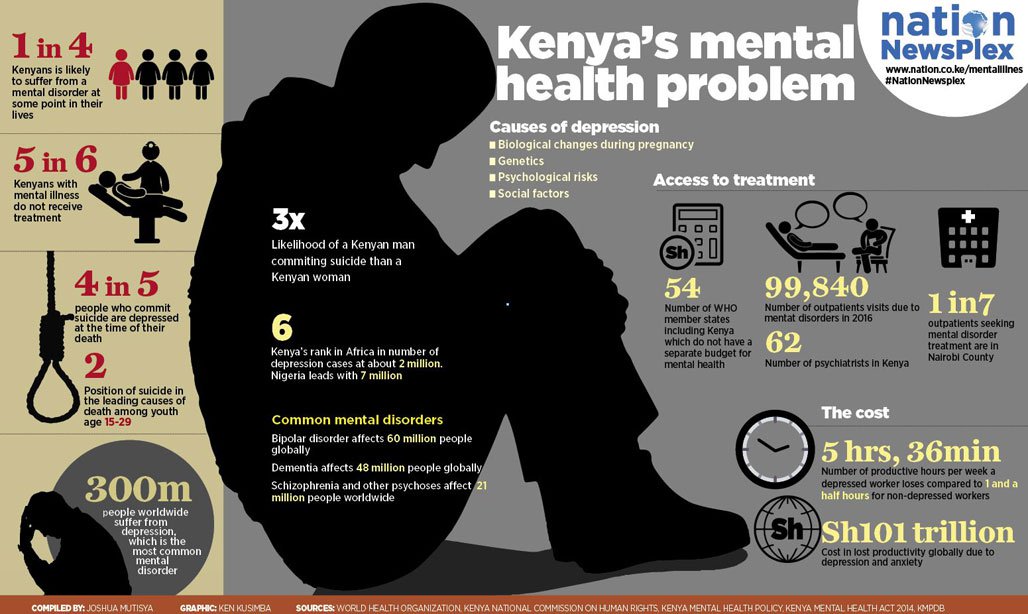
According to the World Health Organization (WHO), depression is one of the leading causes of ill health and disability worldwide. In the 10 years from 2005 to 2015, the number of people with depression increased by more than 18%. "Due to a lack of support, many people with mental disorders do not seek the treatment they need to live healthy and productive lives," the organization said. The WHO is urging countries to increase investment in mental health, reminding that even in high-income countries, about 50% of people with depression do not receive treatment.
Meanwhile, most depressions are treated on an outpatient basis, if the patient turns to a psychiatrist for help in time. This was told to TASS by the chief freelance specialist of the Ministry of Health of the Russian Federation in psychiatry, director of the State Scientific Institute of Forensic and Social Psychiatry. V.P. Serbian Zurab Kekelidze. “Of course, there are chronic, resistant severe conditions when serious measures must be taken,” the expert added.
From 3.7% of the population to 6.5% in different countries - the percentage of people diagnosed with depression. Russia is in the middle of this list - we have about 5.5%
Kekelidze notes that, according to statistics, there are more women diagnosed with depression. However, this may be partly due not to a predisposition to depression, but to the fact that women are more attentive to their health. “They notice deviations faster, see a doctor more often and are more attentively treated,” he said.
Three signs of depression
See also
Tea won't drink itself: what to do so that work doesn't bring you to depression
The chief specialist of the Ministry of Health of the Russian Federation in psychiatry notes that a bad mood is not only from real external causes, but also from a disease called "depression".
"Three main signs are standardly distinguished: a feeling of low mood, motor (motor) retardation, idiotic retardation (when a person feels that it has become harder for him to think, to choose words more slowly, a feeling that he is not thinking about anything)," Kekelidze explained .
In addition to the main signs of depression, there are many varieties: masked (mild depression), seasonal, postpartum, depression that accompanies other somatic conditions - Alzheimer's disease, hypothyroidism and many others.
The psychiatrist advises parents to take a closer look at changes in the child's behavior: sleep disturbances, changes in appetite (stopped eating or eats a lot of sweets) can be early signs of depression.
What prevents Russians from treating depression
In Russia, according to Kekelidze, the problem that not all people with depression receive the necessary treatment is due to the lack of habit of taking care of their health preventively, as well as the fact that people in Russia still For the time being, they are afraid of neuropsychiatric dispensaries, where they try not to go unless absolutely necessary. Not the last role is played by the stigmatization of mental illness - hence the fear of turning to a psychiatrist for help.
However, according to the expert, one should not hope that depression will go away on its own. It is a disease, and like any disease, it must be dealt with by a medical specialist.
Depression should be treated by psychiatrists or psychotherapists. But most people do not go to doctors, they are afraid that they will register
The psychiatrist noted that not every patient needs to be registered with a dispensary, and there are a number of criteria for this. The basis is a danger to oneself and others.
According to the expert, depression is characterized by lack of will, so the worst thing you can advise a depressed person is to tell him "get it together", "pull yourself together." A professional psychiatrist or psychotherapist should say this to the patient, because otherwise the feeling of guilt for "not being able to pull himself together" will grow.