New types of antidepressants
Newest Antidepressants: Brexanolone, Esketamine, Agomelatine
Antidepressants are medications that can help relieve depression symptoms, like fatigue and emotional numbness.
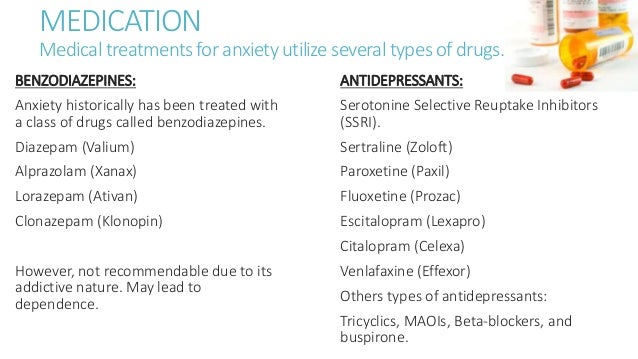
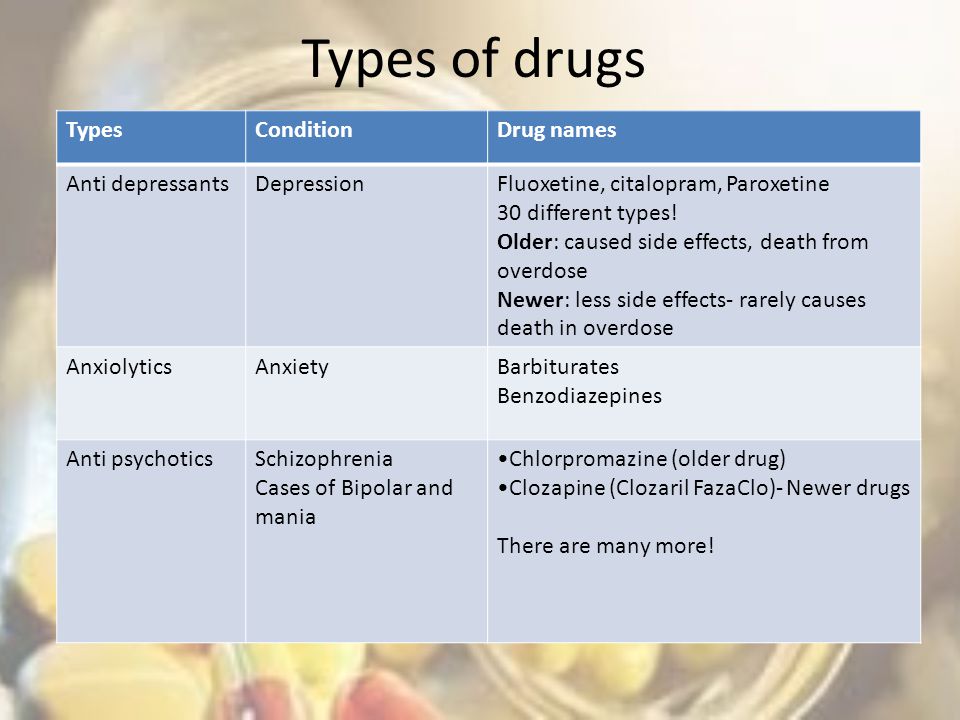
Several different kinds of antidepressants exist, but the most commonly prescribed are selective serotonin reuptake inhibitors (SSRIs).
Fluoxetine (Prozac) entered the market in 1988 as the first SSRI, and for the next 30 years, many experts considered SSRIs the “modern” antidepressant.
In 2019, the Food and Drug Administration (FDA) approved two new antidepressants, brexanolone and esketamine. There’s also been renewed interest in agomelatine, an antidepressant not currently available in the United States.
Read on to learn more about these new antidepressants, including how they compare to SSRIs, their side effects, and how to try them.
In 2019, the FDA approved brexanolone (Zulresso) as the first drug specifically designed to treat moderate to severe postpartum depression (PPD).
Experts consider some SSRIs safe to take while pregnant or nursing, but these medications may not lead to much improvement for several weeks. When you have PPD, symptoms don’t just affect your own well-being — they can also have long-term effects on your bond with your baby.
Brexanolone, however, begins to take effect immediately. According to two randomized clinical trials published in 2018, this medication can significantly reduce PPD symptoms — benefits that held when researchers followed up with participants 30 days after treatment.
Learn more about treatment for postpartum depression.
How it works
Brexanolone raises brain levels of the neurotransmitter gamma aminobutyric acid (GABA).
In a nutshell, GABA dampens the chemical activity in your neurons, almost like a dimmer switch for certain cells.
Scientists aren’t sure exactly how brexanolone treats PPD symptoms, but one theory suggests that with PPD, your GABA levels don’t recover quickly enough from pregnancy to manage your stress. Essentially, cortisol hormones rise unchecked, contributing to symptoms of depression. Brexanolone, then, may offer a “reset” by restoring your GABA levels.
Essentially, cortisol hormones rise unchecked, contributing to symptoms of depression. Brexanolone, then, may offer a “reset” by restoring your GABA levels.
You receive this medication as a one-time IV treatment over the course of 2 and a half days. You’ll remain in your healthcare center for the entire 60-hour treatment for monitoring.
Safety and side effects
Like other drugs that affect GABA levels, brexanolone can cause sedation. Roughly 1 in 4 people experience sedation-related side effects in the first 24 hours of treatment.
You may feel:
- extremely sleepy, even during the day
- unfocused and distractible
- dizzy or faint
Your care team will check on you every 2 hours for extreme symptoms like fainting. If you experience serious side effects, they’ll stop the infusion. Sedation-related symptoms should stop within 15 minutes after the IV infusion stops.
How to get a prescription
You can only receive this treatment from approved healthcare centers, and you’ll need a doctor’s referral to join the treatment program.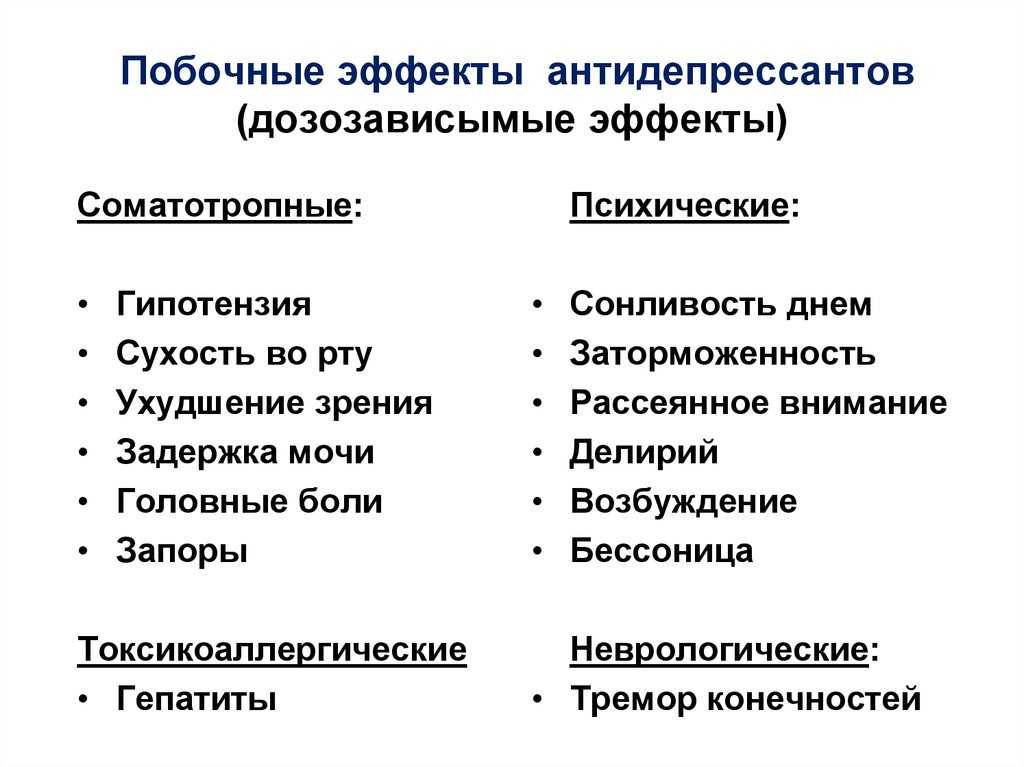
The treatment can cost up to $34,000, though health insurance can help offset some of the cost. Companies like Aetna and Cigna require pre-authorization, so you’ll want to make sure your insurance provider covers the treatment before you check in to your clinic.
Keep in mind, too, that most insurance companies only cover one round of treatment, as research has yet to explore the potential benefits of additional rounds of treatment.
The company that makes brexanolone also offers several financial assistance programs, which could be worth considering if the price tag puts it out of reach.
Esketamine (Spravato) is a chemical cousin of the anesthetic ketamine. The FDA approved esketamine in 2019 to treat treatment-resistant depression, or depression that persists after you try at least two different antidepressant treatments.
During clinical trials, doctors gave participants a nasal esketamine spray or a placebo spray. All participants also took an oral antidepressant they hadn’t tried before.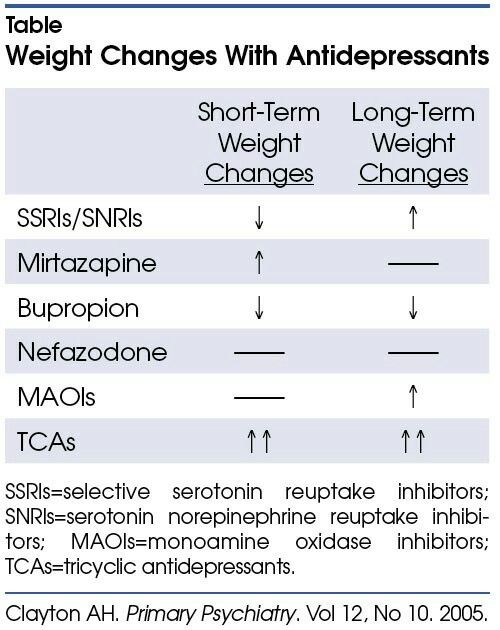 Compared to people who took an oral antidepressant and used a placebo spray, those who used the esketamine spray reported greater symptom relief and longer symptom-free periods.
Compared to people who took an oral antidepressant and used a placebo spray, those who used the esketamine spray reported greater symptom relief and longer symptom-free periods.
How it works
Esketamine sets off a chain reaction of chemicals that ultimately raises your levels of brain-derived neurotrophic factor (BDNF). BDNF helps your neurons make new connections, which in turn enables you to form memories, learn new information, and develop different habits.
Depression typically involves low BDNF levels, and your brain may have difficulty adapting to changes. Esketamine helps restore BDNF levels, along with overall brain plasticity.
As with brexanolone, you have to take esketamine in the presence of a healthcare professional. Your doctor or clinician will give you a dose between 56–84 milligrams (mg), which you spray into your nostrils. You then relax in a chair for 2 hours. Your care team will monitor your blood pressure and heart rate during this time.
This medication works quickly, with many people noticing relief right away. Treatment requires multiple sessions, typically twice a week for the first 28 days and then spaced out over time. The effects usually last until your next dose.
Treatment requires multiple sessions, typically twice a week for the first 28 days and then spaced out over time. The effects usually last until your next dose.
Safety and side effects
In clinical trials, participants tended to report mild to moderate side effects. You may feel sleepy, dizzy, or a bit “out of it” during your treatment session. These side effects often go away within 90 minutes after you take your dose.
On rare occasions, people have reported more severe side effects like:
- vomiting
- anxiety and confusion
- worsening depression or suicidal thoughts
Esketamine can also lead to significant increases in blood pressure during the treatment session, which is why you’ll need monitoring for 2 hours. If you have hypertension or another vascular condition, make sure to tell your doctor before receiving treatment.
How to get a prescription
You can only receive this treatment at an approved healthcare center, so you’ll need to ask your doctor or psychiatrist if you’d like to try esketamine.
The course of treatment instead depends on the severity of your symptoms — and how much you’re able to pay. As of 2021, a standard 56-mg dose of esketamine costs $590, and a large dose of 84 mg costs $885.
The initial month of therapy is often the most expensive since treatment guidelines recommend twice-weekly treatment for the first month. This first month can cost anywhere from $4,800 and $6,800 dollars.
To date, no official guidelines set an ideal length of treatment.
According to the company that produces Spravato, some insurance programs cover most of the cost of esketamine. You’ll only need to pay a $10 copay per session until you hit the benefits cap of $7,150 per year.
Agomelatine (Valdoxan), an oral antidepressant, has been available in some other countries since 2009, though you can’t get this medication in the United States.
You take agomelatine as a 25-mg pill once a day at bedtime. If your depression symptoms don’t respond, a doctor may increase the dose to 50 mg per day.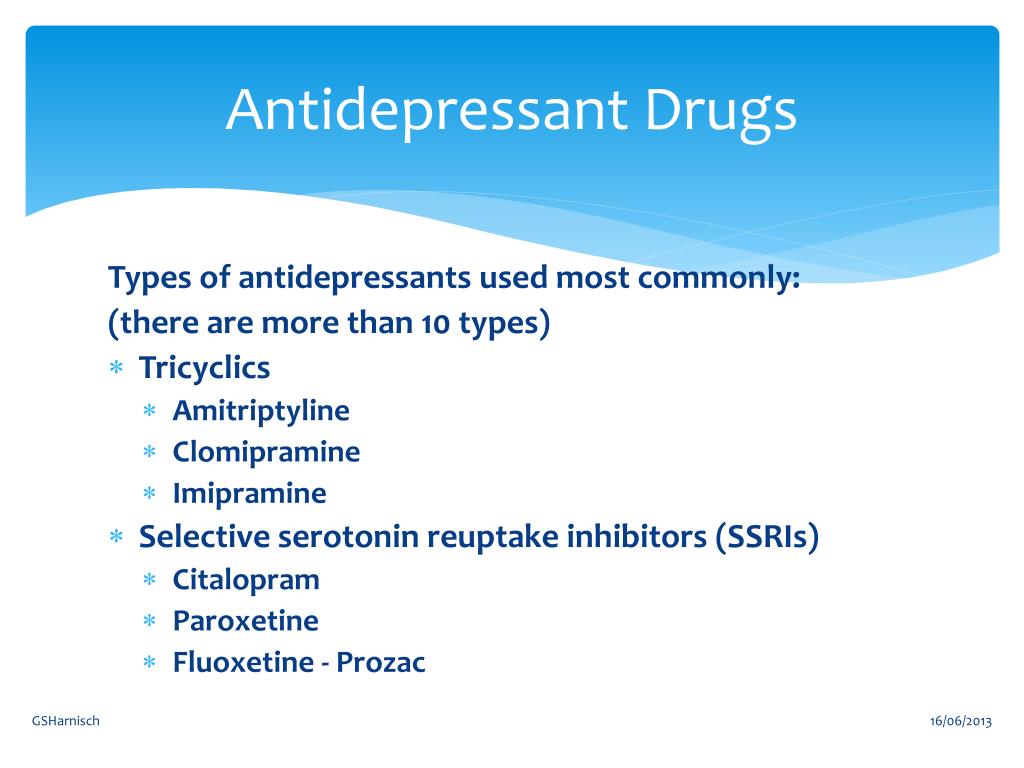
Agomelatine may have particular benefit for depression that:
- involves disruptions in your circadian rhythm (sleep-wake cycle)
- involves anhedonia, or difficulty feeling pleasure
- happens with a health condition, such as Parkinson’s disease or type II diabetes
- happens with seasonal changes
- occurs as part of bipolar disorder
How it works
Agomelatine has two main effects on your brain. It increases activity at melatonin nerve receptors, which helps you sleep. It also decreases activity at specific serotonin receptors and helps increase dopamine and norepinephrine in the frontal cortex.
Increasing melatonin levels can improve sleep-related issues. In a small 2018 study that included 24 young adults, researchers found that the more agomelatine shifted the participants’ circadian rhythms, the more their depression symptoms improved.
Experts don’t yet know exactly how decreasing serotonin fits into the picture.
That said, older animal research from 2014 suggests boosting melatonin and decreasing serotonin binding to receptors simultaneously may help protect newly created neurons by shielding them from the damage caused by chronic stress.
Safety and side effects
Agomelatine may cause:
- nausea and vomiting
- constipation, stomach pain, and diarrhea
- drowsiness or difficulty sleeping
- headaches
But many people only experience mild side effects while taking agomelatine, which may partially explain the renewed interest in this antidepressant.
After all, if you don’t experience severe side effects, you’ll probably feel more inclined to continue taking the medication.
How agomelatine comparesA 2018 review including 522 trials with a total of 116,477 participants compared 21 antidepressants.
When the review authors considered dropout rates specifically due to adverse reactions, they discovered all included antidepressants had a higher dropout rate than the placebo — except agomelatine.
Incidentally, researchers also listed agomelatine as one of seven most effective antidepressants among those studied.
With many antidepressants, you may experience flu-like symptoms if you suddenly stop taking the medication. This phenomenon, called discontinuation syndrome, doesn’t occur with agomelatine. You can easily stop even long-term agomelatine use.
This phenomenon, called discontinuation syndrome, doesn’t occur with agomelatine. You can easily stop even long-term agomelatine use.
So, you might wonder: If this medication works so well, what’s holding up approval in the United States?
Agomelatine does have the potential to cause one very severe side effect: liver toxicity. The medication raises the levels of liver amino acids called transaminases, causing liver damage for up to 4.6% of people who take it. People taking this medication need to have their liver function tested at weeks 3, 6, 12, and 24 of treatment.
Other antidepressants can have a similar impact on your liver, but at much lower rates:
- placebo: 2.1%
- escitalopram (Lexapro): 1.4%
- paroxetine (Paxil): 0.6%
- fluoxetine (Prozac): 0.4%
How to get a prescription
Currently, you can’t get a prescription for agomelatine in the United States or Canada, as regulatory agencies have deemed the risk of liver injury too high to allow the drug on the market.
It’s possible that agomelatine could become more widely available in the future if researchers identify a way to minimize the risk of liver toxicity.
Doctors in Europe and Australia may prescribe this medication.
Brexanolone and esketamine appear to have the most benefit for postpartum depression and treatment-resistant depression, respectively. These medications also come with a high price tag that can make them harder to access.
Agomelatine can effectively treat a wider range of depression subtypes. But it also carries a risk of liver toxicity, and it hasn’t been approved for use in the United States.
To sum up, these medications likely won’t replace SSRIs as the first line of treatment for other types of depression anytime soon. Still, their existence opens up possibilities for future advances in depression treatment.
Emily Swaim is a freelance health writer and editor who specializes in psychology. She has a BA in English from Kenyon College and an MFA in writing from California College of the Arts. In 2021, she received her Board of Editors in Life Sciences (BELS) certification. You can find more of her work on GoodTherapy, Verywell, Investopedia, Vox, and Insider. Find her on Twitter and LinkedIn.
In 2021, she received her Board of Editors in Life Sciences (BELS) certification. You can find more of her work on GoodTherapy, Verywell, Investopedia, Vox, and Insider. Find her on Twitter and LinkedIn.
What Are They and More I Psych Central
New antidepressants have a fresh approach to treating depression and offer options when other medications may not work.
Serotonin reuptake inhibitors (SSRIs) changed the face of depression treatment with their arrival in the 1980s. They offered an improvement over older antidepressants, like tricyclics, because they had fewer side effects.
But since that time, many new developments have been made in antidepressants.
Treatment for depression typically involves a combination of therapy and medication. However, studies show that about one-third of people with depression don’t respond to current medications.
New antidepressants may help fill that gap. The latest antidepressants use new mechanisms to pick up where older antidepressants left off.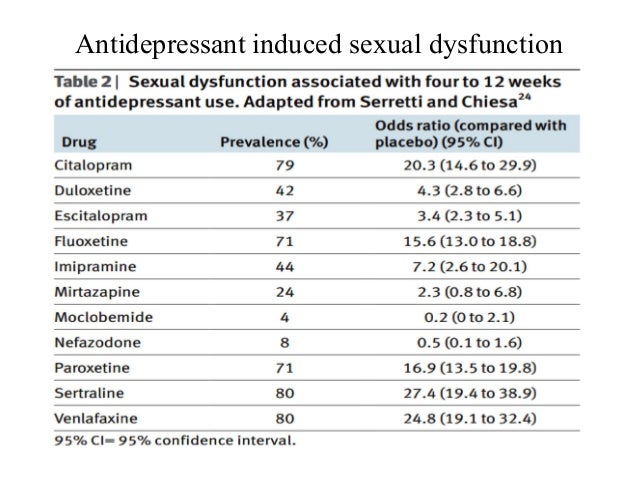
Three new antidepressants are on the market to treat depression:
- brexanolone
- esketamine
- agomelatine
Unlike SSRIs and other antidepressants, these newer medications can start relieving symptoms in a few hours or days instead of a few weeks.
Brexanolone
Approved in 2019 by the Food and Drug Administration (FDA), brexanolone is used to treat postpartum depression in adults who are not pregnant.
How does brexanolone work?
Progesterone and allopregnanolone are hormones that peak in your body during the third trimester of pregnancy. Allopregnanolone is a metabolite (byproduct) of progesterone. After you have your baby, progesterone and allopregnanolone levels drop abruptly and significantly.
Scientists believe that the sudden drop in hormone levels may contribute to postpartum depression.
The exact way brexanolone works is not fully understood. But since it’s a solution of allopregnanolone, it’s thought to help activate gamma-aminobutyric acid (GABA) receptors and raises GABA levels in your brain.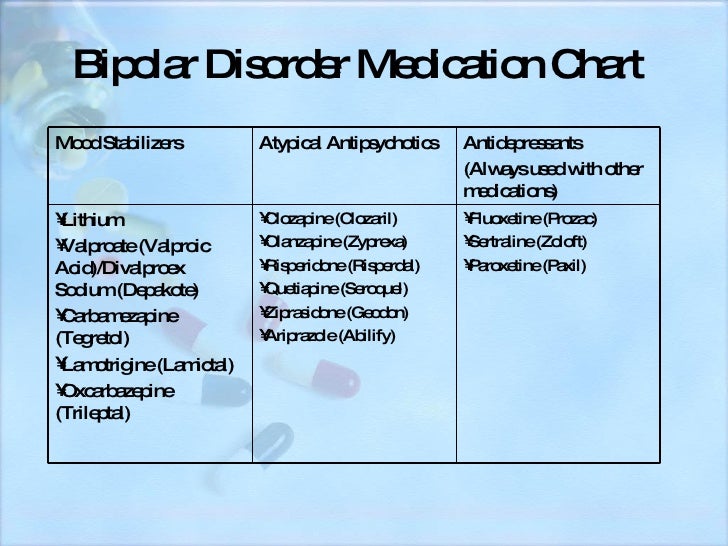 People with depression tend to have lower GABA levels and lower activity in the GABA receptors.
People with depression tend to have lower GABA levels and lower activity in the GABA receptors.
How do you take brexanolone?
Brexanolone is given as an intravenous (IV) infusion for a total of 60 hours (2.5 days). At this time, brexanolone can only be administered in a hospital setting.
You’ll likely start with a low dose, which will gradually increase until your allopregnanolone levels are at what’s typically seen during the third trimester of pregnancy.
During the last 8 hours of the infusion, the dose will gradually be decreased.
What are the side effects of brexanolone?
The most commonly reported side effects of brexanolone include:
- dry mouth
- flushing
- loss of consciousness (passing out)
- sleepiness
What should I watch for while taking brexanolone?
You may lose consciousness while receiving your brexanolone infusion. A healthcare professional will monitor you closely for excessive sleepiness and loss of consciousness.
Like other antidepressants, brexanolone may increase the chance of suicidal thoughts or behaviors in people ages 24 years and younger. It’s recommended that you monitor your symptoms while on this medication.
Esketamine
Esketamine is a new antidepressant drug approved in 2019 by the FDA to treat depression that has not improved with other medications.
It belongs to the class of medications called N-methyl D-aspartate (NMDA) receptor blockers. It’s derived from ketamine — a drug used for anesthesia. This new antidepressant works differently than other commonly prescribed antidepressants.
How does esketamine work?
In clinical studies, scientists discovered that ketamine relieves depression in ways that traditional antidepressants don’t. Compared to other commonly used antidepressants, people who took ketamine showed improvement in depression symptoms within a few hours versus a few weeks.
It’s not fully understood how esketamine works, but it may work similarly to ketamine. Both medications are NMDA receptor blockers. By blocking NMDA receptors, esketamine triggers the production of glutamate.
Both medications are NMDA receptor blockers. By blocking NMDA receptors, esketamine triggers the production of glutamate.
Glutamate is a chemical in your brain that helps form new brain cell connections. Scientists believe that creating new brain cell connections can help people with depression develop new positive thoughts and behaviors.
How do you take esketamine?
Esketamine comes in a nasal spray. A mental health professional will show you how to use it and how much medication to take. You will likely use esketamine once or twice a week along with another oral antidepressant.
After taking esketamine, a healthcare team will observe you for about 2 hours. They will let you know when it’s safe for you to leave the facility.
What are the side effects of esketamine?
The side effects most commonly seen with esketamine include:
- anxiety
- dizziness
- drowsiness
- feeling detached from yourself
- feeling inebriated
- increased blood pressure
- nausea
- numbness in part of your body
- sluggishness
- vomiting
What should I watch for while taking esketamine?
Esketamine may cause you to feel drowsy or disconnected from yourself, your thoughts, or space and time (dissociation). There’s also a chance that you may become dependent on esketamine. For this reason, esketamine is only administered in a healthcare facility setting.
There’s also a chance that you may become dependent on esketamine. For this reason, esketamine is only administered in a healthcare facility setting.
After taking esketamine, a healthcare professional will monitor you for at least 2 hours for an increase in blood pressure and signs of excessive sleepiness or dissociation. It’s recommended that you avoid driving or operating machinery after taking esketamine for 24 hours.
Like other antidepressants, esketamine may increase the risk of suicidal thoughts and actions in young adults.
Agomelatine
Agomelatine is an antidepressant that works in two unique ways. It blocks serotonin receptors so that you have more serotonin freely available in your brain. It also stimulates melatonin receptors to help you sleep.
Agomelatine is approved to treat depression in Europe and Australia. However, the FDA has not yet approved the medication for use in the United States due to negative results seen in late-stage trials. The possibility of liver damage is also a concern.
New antidepressants open new avenues in depression treatment that haven’t been explored before. However, older antidepressants are still the first choice for antidepressant medication. Here are the five most common antidepressants.
Selective serotonin reuptake inhibitors (SSRIs)
SSRIs remain the most prescribed antidepressants. Fluoxetine (Prozac) was the first SSRI approved by the FDA for the treatment of depression.
Other commonly prescribed SSRIs include:
- citalopram (Celexa)
- escitalopram (Lexapro)
- paroxetine (Paxil)
- sertraline (Zoloft)
Serotonin-norepinephrine reuptake inhibitors (SNRIs)
SNRIs are also frequently prescribed antidepressants. Levomilnacipran (Fetzima) was approved by the FDA in 2013 for depression.
Other commonly used SNRIs include:
- desvenlafaxine (Pristiq)
- duloxetine (Cymbalta)
- venlafaxine (Effexor)
Noradrenergic and specific serotonergic antidepressants (NaSSAs)
Similar to SSRIs and SNRIs, these medications affect serotonin and norepinephrine, but they also block receptors of the stress hormone epinephrine.
They are often prescribed for depression and anxiety, as well as personality disorders. The most commonly used NaSSA is mirtazapine (Remeron).
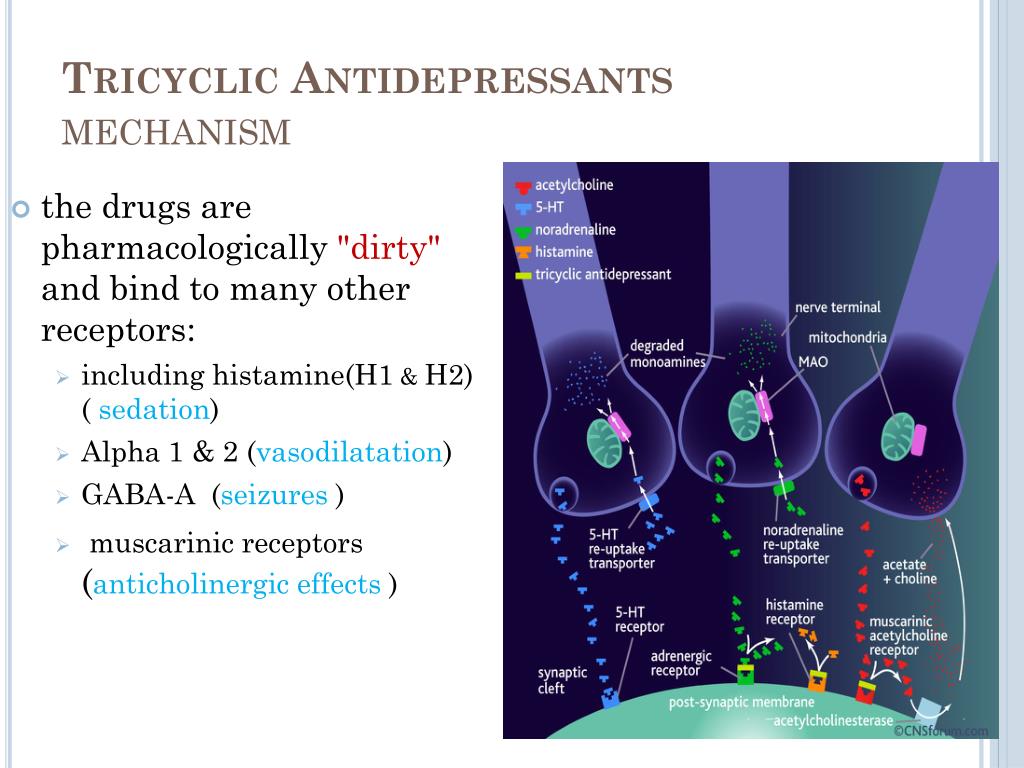
Tricyclic antidepressants (TCAs)
Because TCAs may have some unpleasant side effects, they are less often prescribed for depression. However, TCAs are still used for other conditions, such as trouble sleeping and some types of chronic pain. Commonly used TCAs include:
- amitriptyline (Elavil)
- doxepin (Sinequan)
- imipramine (Tofranil)
- nortriptyline (Pamelor)
Atypical antidepressants
Atypical antidepressants are those that don’t fall into other categories. Each one works slightly differently than other antidepressants and even other atypical antidepressants.
Examples of atypical antidepressants include:
- bupropion (Wellbutrin)
- olanzapine/fluoxetine (Symbax)
- trazodone (Desyrel, Oleptro)
- vortioxetine (Trintellix)
Whether you’re looking for a new depression medication or are thinking of changing from your current treatment, finding the right drug for you can take some time.
Taking steps to learn more about new antidepressants can help you find the right medication for you. Consider reaching out to a mental health professional. They can help guide you when choosing an antidepressant that fits your unique symptoms.
Remember that you do not have to go through depression alone. Help is available. You can check out our “How to Find Mental Health Support” page for a list of mental health resources and hotlines.
Fighting depression: 10 modern drugs
{{if type === 'partner-stocks'}}
{{/if}}
{{/if}} {{each list}}${this} {{if isGorzdrav}}
Delete
{{/if}}
{{/each}} {{/if}} Search by drug, disease, substance: DERMAKOSMETIKA, Nyureksan, Durex, From pain, VoltarenHome
Articles
Fighting depression: 10 modern drugs
Depression is an urgent problem, the number of visits to doctors is growing every year.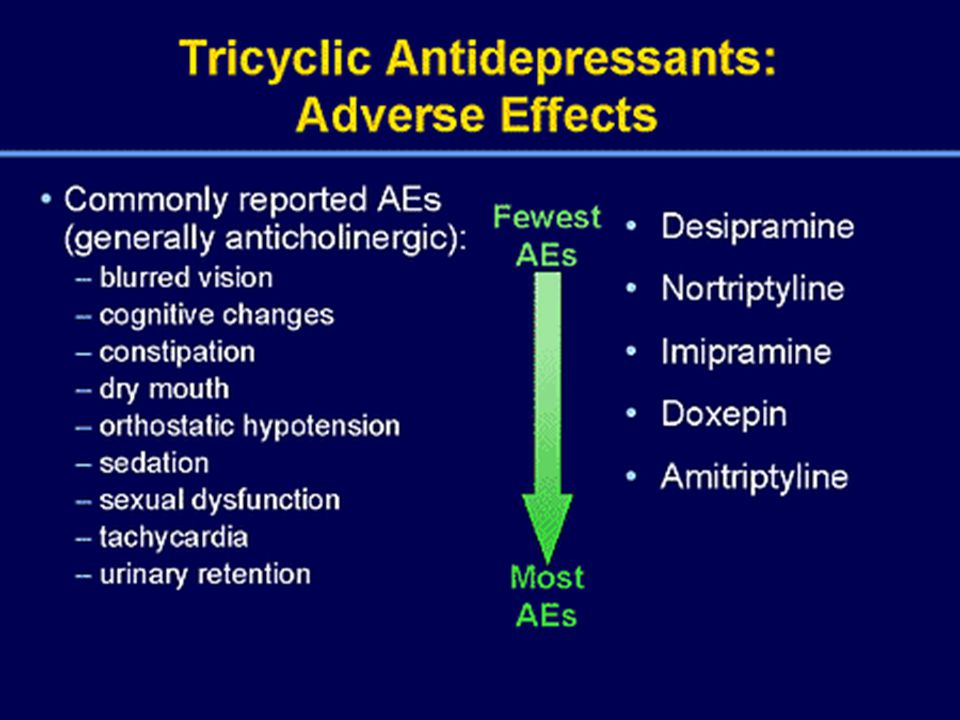 It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
It can be solved by contacting a psychotherapist and taking antidepressants . These are drugs that regulate the production of hormones and biochemical processes in the body. It is strictly forbidden to prescribe them to oneself , as these are complex drugs with certain restrictions, side effects effects . The doctor must authorize their appointment and control the intake. We will tell you which of them are the most effective and common in medicine, how many they have pluses and minuses.
What is meant by
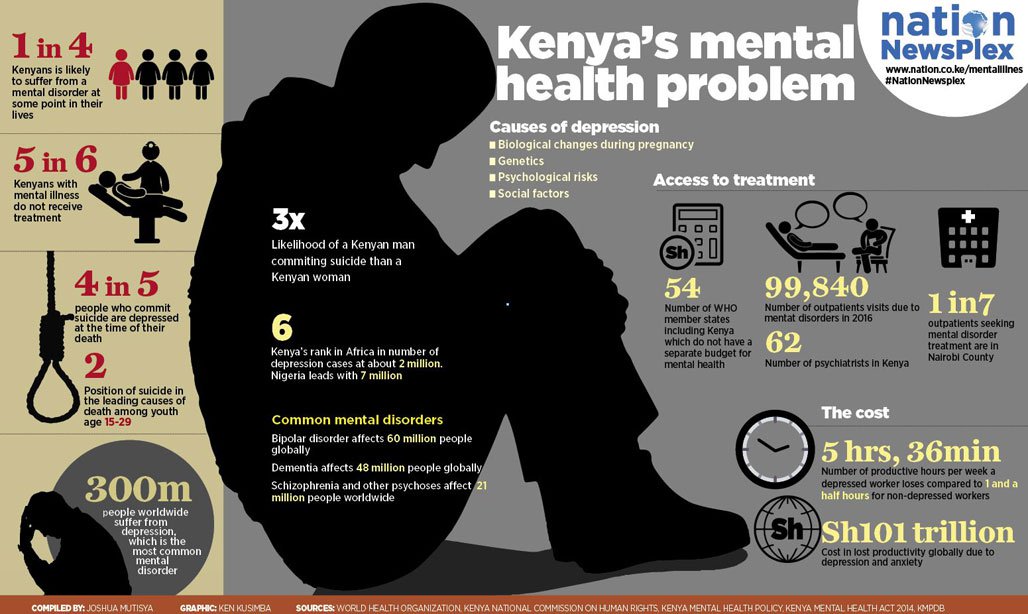
depression Doctors have known it since ancient Greece and Egypt. Hippocrates described it as melancholy - a condition that is accompanied by anxiety, despondency, insomnia, refusal of food, irritability. Most often, the cause is childhood trauma or severe, frequent stress in adulthood. There are many provoking factors: the death of a loved one, deterioration of living conditions, alcoholism, brain diseases.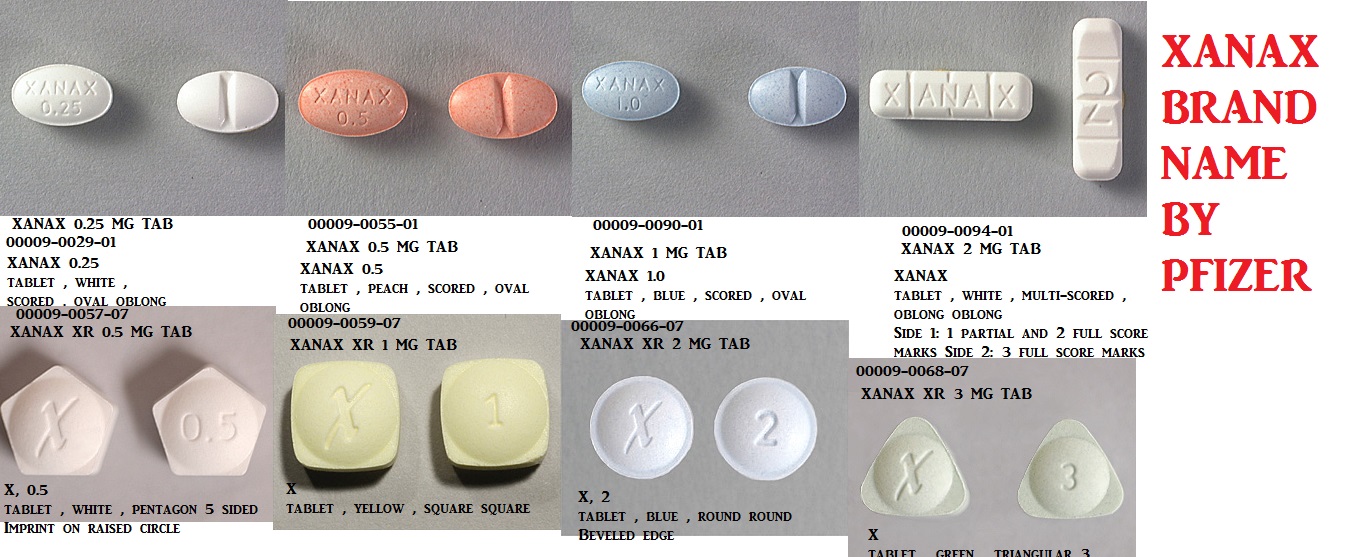 Such cases are referred to as psychogenic depression.
Such cases are referred to as psychogenic depression.
The second type is endogenous. The problem appears not from large external shocks, but because of internal causes. A person is constantly dissatisfied with himself, subjecting himself to criticism. Many patients have panic attacks , haunted by a feeling of fear, anxiety.
How long the period of depression lasts
Many people mistake ordinary periods of low mood for depression. If they do not last long and are quickly replaced by periods of recovery, then we are not talking about a depressive state. The problem is obvious when the symptoms persist for months and dramatically change a person's life. Then you need to see a doctor.
What happens to the body
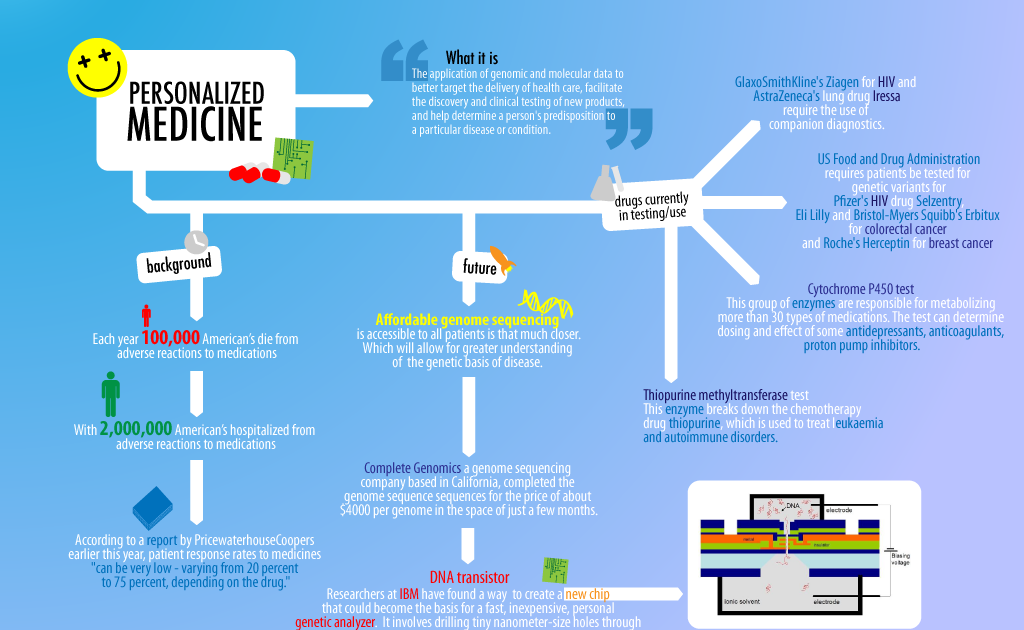
The most common theory is that there is a malfunction of neurotransmitters located in the brain. These substances transmit signals from neuron to neuron and are responsible for a person's mood.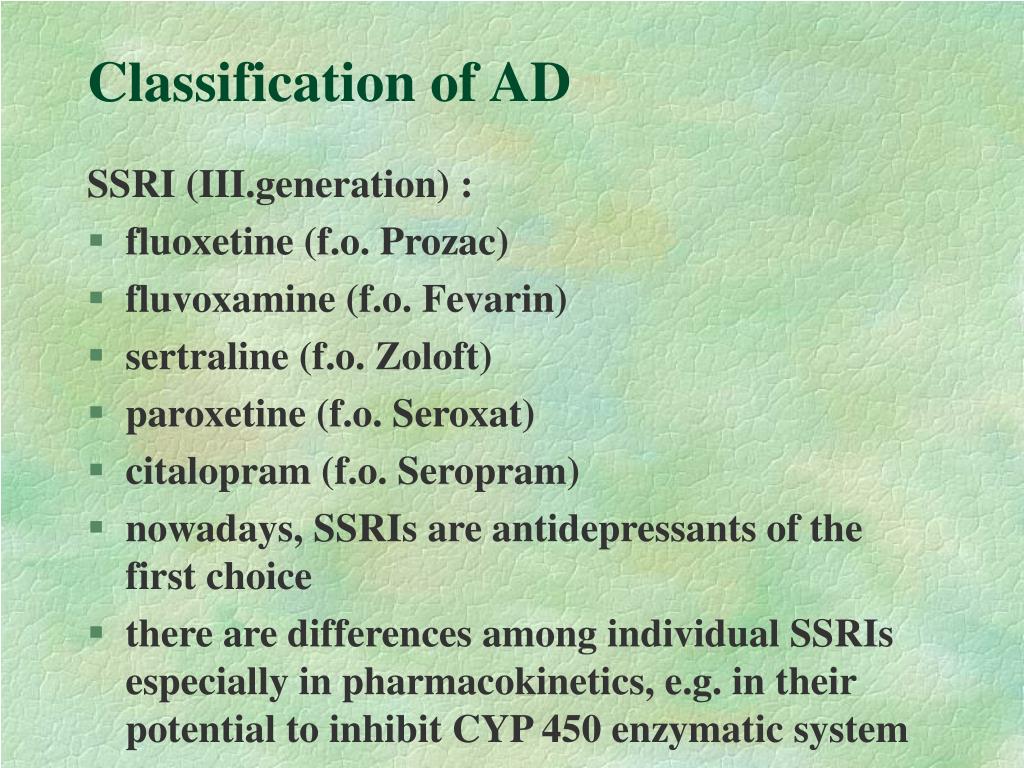 Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
Dysfunction leads to a slowdown in the rate of this transmission and a decrease in the number of neurotransmitters themselves. Serotonin, which is called the "hormone of happiness", suffers the most. For clarity, this biochemical process can be compared, for example, with a drop in blood sugar levels in diabetes mellitus.
How is
treated depressionDepression has been treated in different ways. In the ancient world - emetics and laxatives. In the Renaissance - wine and sunbathing. In the Age of Enlightenment - external stimuli, for example, insects. The 19th century brought new recipes - in particular, a solution of camphor in tartaric acid. The treatment also included the use of drugs, which are now no longer allowed for sale, and some are recognized as narcotic.
Obviously, all these drugs had no effect on increasing the amount of serotonin. And the treatment is precisely to normalize its production. This was done after creating modern antidepressants , which have a minimum of side effects, are safe for the body and are not addictive. These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
These are medicines, whose action is aimed specifically at balancing the disturbed balance of neurotransmitters: serotonin, norepinephrine, dopamine.
Prescription
If a healthy person takes antidepressants , there will be no effect . For a depressed patient, taking them will help:
- improve psychological state;
- get rid of irritability;
- panic fear;
- increase mental and physical activity;
- overcome the dreary mood.
Psychiatrists prescribe antidepressants for chronic back pain, headaches. And also with irritable bowel syndrome, incontinence and other cases when the body stops producing its own painkillers. Medication helps restore pain suppression mechanisms.
These drugs can only be taken with a doctor's prescription, as many of them are strong stimulants. Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Self-administration may cost dearly - the condition may worsen. Only a doctor will correctly calculate how many medicines to take per day. In parallel with the treatment by a psychiatrist, a neurologist, a consultation of a psychotherapist is required.
Precautions
- Prescribed drug start drinking from a small dose - the first couple of days they take a quarter of a tablet. Gradually increase the dose to normal. So the body adapts better. Finish the course by reducing the dose.
- The first effect of appears only 2 weeks after the start of administration. Sustained action - after six months. All this time, you need to take remedy, without making passes, breaks.
-
Products are not combined with melatonin, St. John's wort, products and dietary supplements based on sibutramine, 5-HTP. Their combination can raise serotonin to dangerous levels.
 Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account.
Also, you can not combine them with monoamine oxidase inhibitors, for example, Cipralex. When writing a prescription, the doctor takes these points into account. - Drinking antidepressants is better in parallel with visits to a psychotherapist. If the drugs normalize the biochemical processes in the body, then this doctor will help normalize the psychological state after depression.
The best antidepressants
In medicine, they have long argued that some drugs give only a placebo effect. The purpose of the study was to find out which of them are the most effective and valid . The project involved 116 thousand patients, and its results were published by the authoritative edition of the Lancet. We offer a list of the best.
1. Agomelatine
New generation drug. Agomelatine is used for severe depressive disorders, high levels of anxiety. Enhances the release of dopamine and norepinephrine, stimulates melatonin receptors.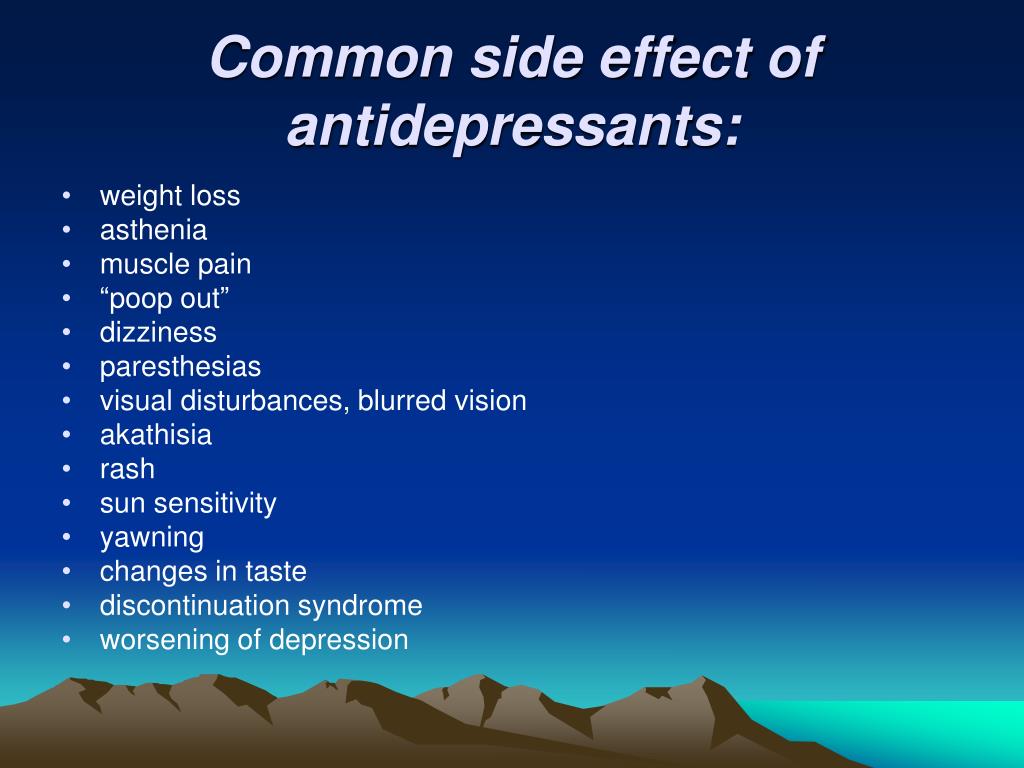 The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
The standard therapeutic dose is 25-50 mg 1 time / day. Helps to restore the normal structure of sleep, get rid of anxiety and panic attacks attacks
Pros
+ Does not adversely affect attention and memory.
+ No lethargy during the day.
+ No sexual deviations.
+ No relation to blood pressure.
+ Do not reduce dosage upon discontinuation.
Cons
— In 1-10% of cases, increased sweating, diarrhea, constipation.
- Possible increased fatigue, drowsiness.
- There are no evidence-based safety studies in people with renal or hepatic insufficiency, therefore, such patients are advised to refrain from taking drugs with active ingredient agomelatine.
2. Amitriptyline
Tricyclic antidepressant. Moreover, the World Health Organization considers Amitriptyline the most reliable in this group. The standard dose is 200-250 mg / day. The action is to block the reuptake of neurotransmitters.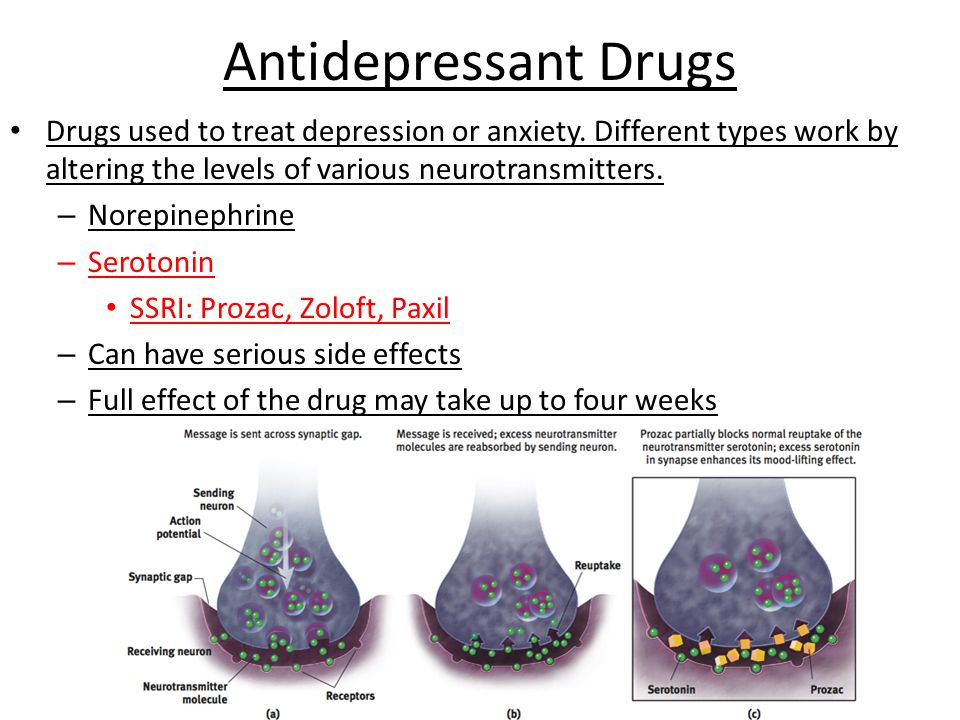 A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
A good remedy for moderate to severe disorders of the endogenous type. Additionally, it has a sedative and hypnotic effect. Effective in the treatment of neuropathic pain, for the prevention of migraine.
Pluses
+ Preparations with active ingredient amitriptyline are inexpensive.
+ High reliability, minimum side effects.
+ Relatively safe during breastfeeding.
Cons
- Possible side effect in the form of blurred vision, dry mouth.
- Lowering blood pressure.
- Some patients experience constipation.
- Drowsiness.
3. Escitalopram
It belongs to the group of modern serotonin reuptake inhibitors (SSRIs). Most often, it is recommended to take for anxiety, panic attacks. It is taken once, the standard dose is 10 mg per day. Escitalopram has a milder effect and is prescribed to patients for whom tricyclic drugs are contraindicated.
Pluses
+ Lasting effect comes after 3 months.
+ Indicated for patients with disorders of the cardiovascular system.
+ Soft action.
Cons
- In some patients, the functions of the gastrointestinal tract are disturbed, which is most often expressed in diarrhea.
- Anxiety may increase during the first 2 weeks, therefore it is recommended to start treatment with low doses and gradually increase them.
- Contraindicated in pregnancy and lactation.
4. Mirtazapine
A drug of the tetracyclic group. Mirtazapine - good stimulant for anxious depressions, has a moderate sedative effect. The average amount is 30 mg / day, it must be consumed once. Usually it is prescribed to patients who lose interest in life, cease to experience joy, pleasure. Effective in the correction of sleep, in particular, early awakenings.
Pros
+ Earlier onset of action than SSRIs (1 week).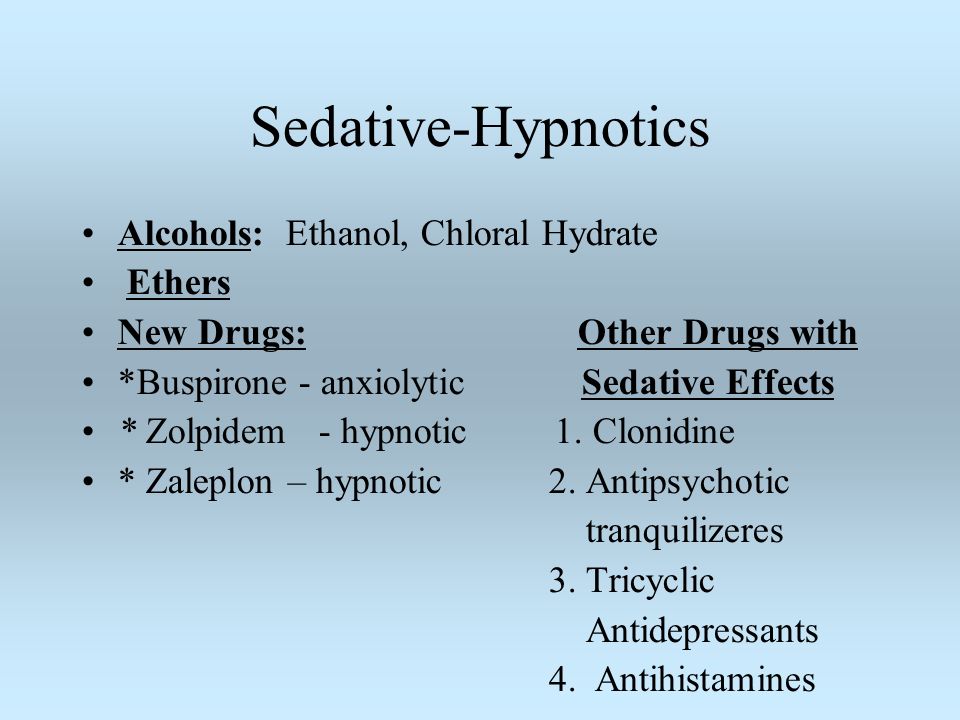
+ Works well with most general medicines.
+ Full effect in 4 weeks.
+ Does not affect sexual function.
Cons
- The active substance mirtazapine is contraindicated in diabetes mellitus, arterial hypotension, increased intraocular pressure.
— During the appointment, you must drive carefully and engage in potentially hazardous types of work.
- 18% of patients experience drowsiness, 15% dry mouth, 5% weight loss. Other side effects occur in 1-3% of cases.
5. Paroxetine
Belongs to the SSRI group, is used most often for severe anxiety, panic, social phobia, nightmares, stress after trauma. Paroxetine can resolve the problems of anxious depression, anxiety-phobic disorders. Take once a day at a dose of 20 mg.
Pros
+ The most powerful stimulant among SSRIs.
+ Anxiety and insomnia pass quickly.
+ Minimal side effects in the form of vomiting, diarrhea.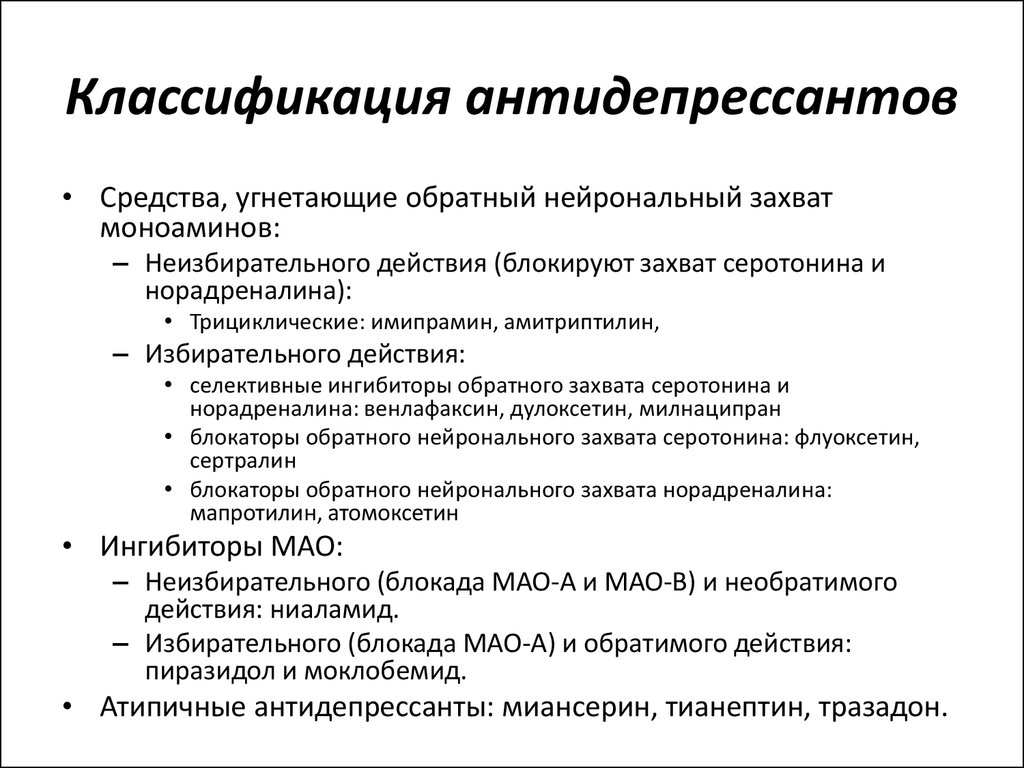
+ Suitable for patients with cardiovascular problems.
Cons
— Not suitable for patients with severe motor, mental inhibition.
- Reduces libido.
- Harmful to the fetus when taken during pregnancy.
6. Fluoxetine
One of the most commonly used antidepressants in the SSRI group. Known as Prozac. Fluoxetine is also known as a good mood stimulant. Patients have a feeling of fear, tension, anxiety, gloomy dislike for others. Depending on the indications, the average daily dose is 20-60 mg.
Pluses
+ There is practically no effect on the work of the heart.
+ Does not cause sedation.
+ Effective for patients with motor retardation and excessive daytime sleepiness.
Cons
- May cause weight loss.
— Hypoglycemia is possible in diabetes mellitus.
- Contraindicated in severe renal impairment.
7. Fluvoxamine
Another SSRI drug.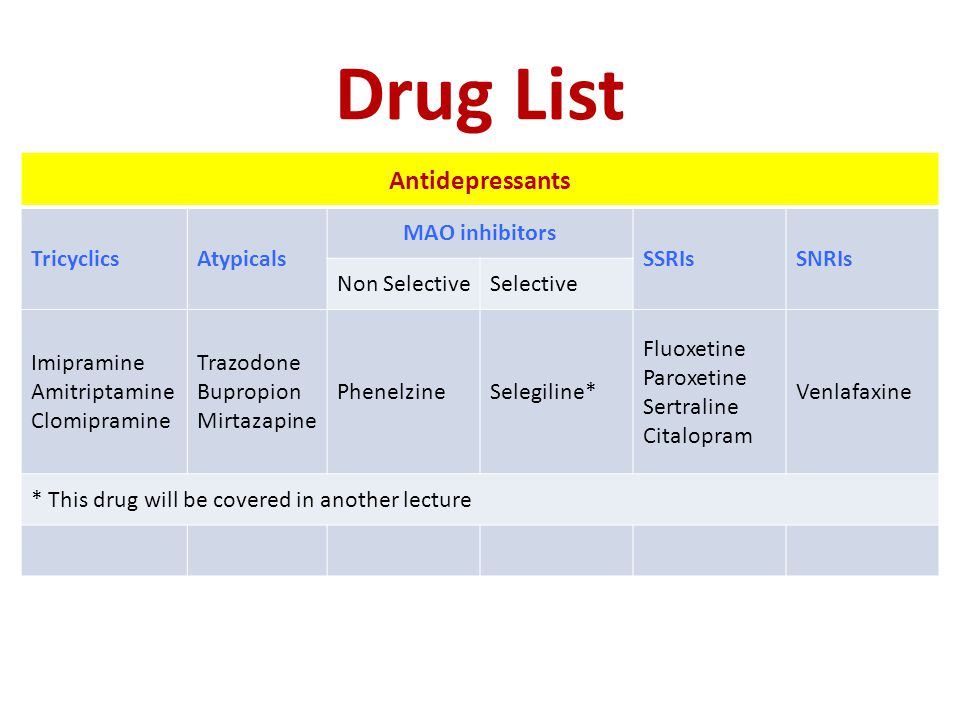 Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Fluvoxamine is similar to Prozac Fluoxetine but is fast acting and may cost cheaper. The effect is in a more active slowing down of the reuptake of serotonin by neurons. It is indicated for depression of various origins, as well as obsessive-compulsive disorders. The average daily dose is 100 mg.
Pros
+ Lower price than traditional Prozac.
+ Faster action than him.
+ Relatively minor side effects (diarrhea, dry mouth, drowsiness).
Cons
- Contraindicated in diabetes.
- Pregnant women - with caution, lactation - prohibited.
- Causes nausea in some patients.
8. Sertraline
One of the widely used and universal drugs of the SSRI group. They treat almost any depressive condition, panic disorder, social phobia. However, in severe clinical cases, sertraline may not be effective enough. The standard dose is 50 mg/day.
Pros
+ No cardiotoxicity.
+ The patient's psychomotor activity does not change.
+ Does not increase body weight.
+ Combines well with other groups of antidepressants.
Cons
— In the first 2 weeks there may be problems with sleep, diarrhea.
- Side effects of a sexual nature.
- Contraindicated in pregnant women.
9. Escitalopram
The drug is classified as an SSRI. Its difference is in its effectiveness in depression, which is accompanied by involuntary movements (tic, tremor, chewing, smacking). Escitalopram is prescribed to patients with panic, anxiety, phobias, obsessive thoughts or actions. The daily dose is 20 mg.
Pluses
+ Effective in tardive dyskinesia.
+ One of the most powerful SSRIs.
+ More pronounced thymoleptic effect (improvement of mood) compared to many antidepressants of the same group.
Cons
- In some patients, anxiety increases within 2 weeks after starting treatment.
— Gastrointestinal disorders, insomnia, agitation are possible.
— Use during pregnancy only in extreme cases, incompatible with feeding.
10. Venlafaxine
Belongs to the SNRI group. In addition to blocking the reuptake of serotonin, venlafaxine has a similar effect on another neurotransmitter, norepinephrine. The medicine is prescribed for depressive conditions of various origins, social phobias, anxiety, panic. Usually take 150 mg per day.
Pros
+ Better tolerated by patients than most tricyclics.
+ More pronounced effect than classic SSRIs.
+ Fewer contraindications.
Cons
- Traditional side effects of most antidepressants: nausea, drowsiness, dry mouth, diarrhea or constipation.
- May increase eye pressure.
- The most severe withdrawal syndrome among antidepressant drugs.
This list is not to be used as a recommendation. In any case, consult your doctor before purchasing. Be healthy!
Modern antidepressants.
 Review
Review In the search for effective remedies for depression, many methods and substances have been tried, from opiates to malariotherapy by Nobel laureate in medicine Julius Wagner-Jauregg [1]. But the real struggle only began in the 1950s. In 1952, iproniazid was invented. Actually, it was intended to fight tuberculosis, but a side effect in the form of an improvement in the mood of depressed patients made me look at the drug in a new way.
What antidepressants should treat. Theories of depression
There are now several biological theories of depression.
Until recently, the most common were those that linked the onset of depression and a lack of production of monoamine neurotransmitters in the human brain: serotonin, norepinephrine, dopamine. The most popular was the serotonin hypothesis. She argued the following: in patients with depression, the production of serotonin is disrupted, if this is corrected, this will allow to overcome depression and various anxiety disorders (of which a person has not just a lot, but a lot).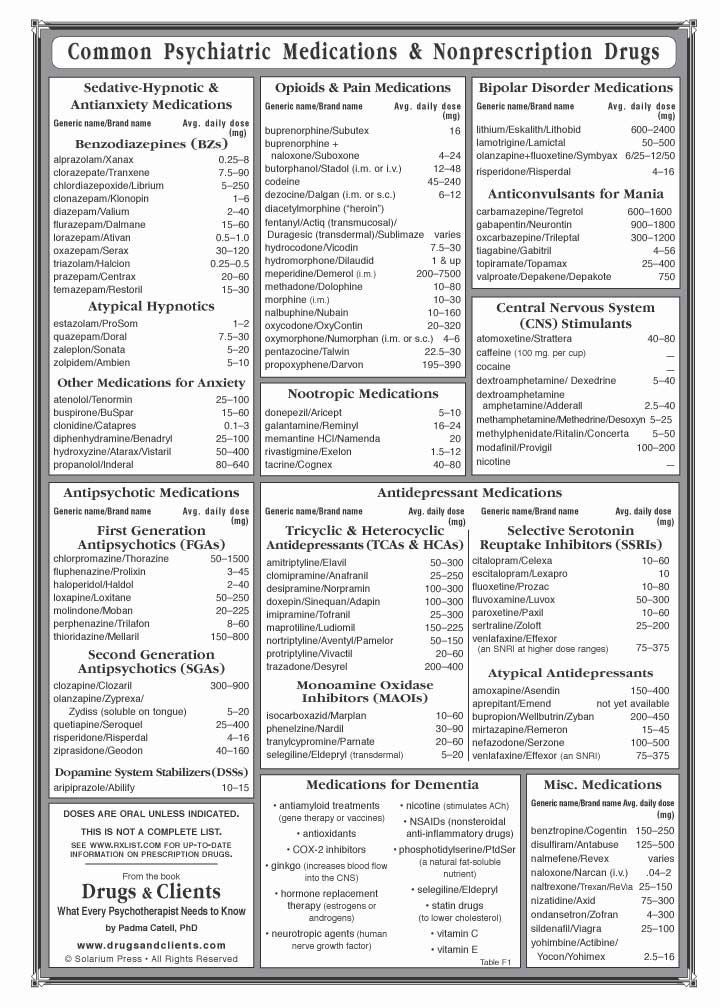
However, science did not stand still, scientists delved deeper and deeper into the human brain and learned more and more about the biological background of human emotions. And the more they learned, the more questions arose about the "monoamine theory" [2].
For example, drugs that block serotonin receptors can belong to completely different classes and have a variety of effects on the human body: the 5HT2 and 5HT3 receptor blocker mirtazapine is an antidepressant, the 5HT2 blocker quetiapine is an antipsychotic. On the other hand, blocker agonists - conditioned depressants - are not. The same LSD, mescaline or psilocybin are not substances that cause a depressive state. In addition, it turned out that such a substance as glutamate plays an important role not only as a neurotransmitter, but also an essential role in the development and functioning of the brain in general [3] There are theories explaining its role in the formation of human emotions, learning processes and aging of the brain [4 ].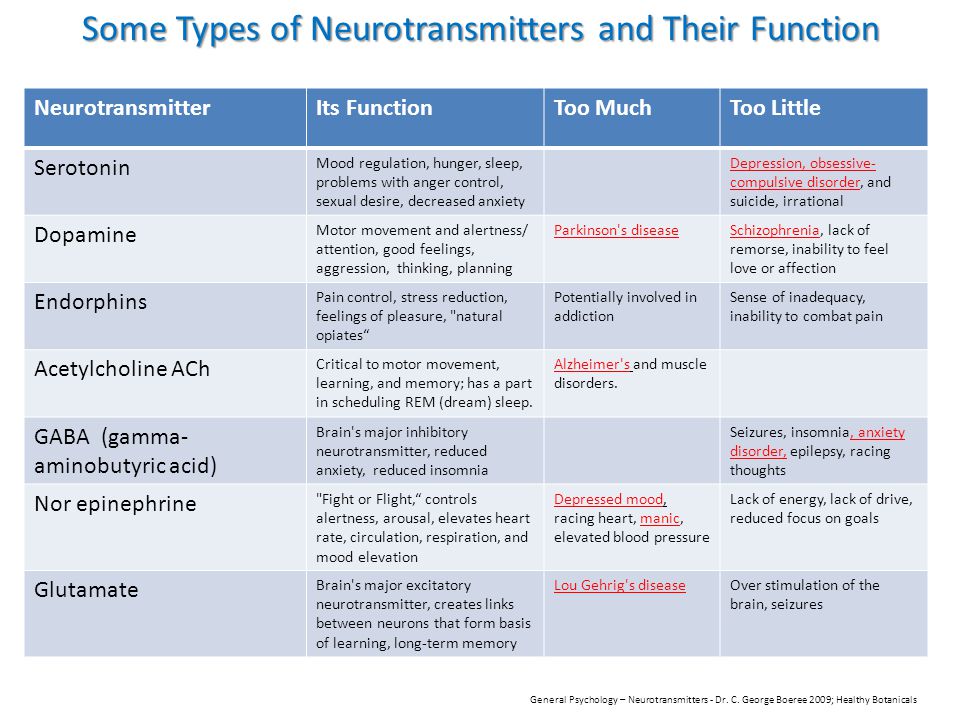
And then they remembered that the brain has such a thing as "neuroplasticity." The theory that the formation of the emotional background of a person is not responsible for any individual neurotransmitter, but as a result of the joint activity of various parts of the brain, quickly began to gain popularity [5]. Its main difference from previous theories is that a decrease or increase in the concentration of serotonin (or any other monoamine) in the synaptic cleft (meaning the gap between two nerve cells) does not in itself lead to the formation of mood, and therefore cannot be responsible for the improvement / worsening mood. More attention began to be paid to the factors of gray matter thinning in depression, the reduction in the branching of nerve cells, and others, for example, those responsible for the growth of neurons and the connections between them. [6]
Types of antidepressants
Although the development of science has a direct impact on the development of antidepressants, many of the currently available were developed at a time when there was simply no talk of any "neuroplasticity".
1. The first of its kind
The first mass "real" synthetic antidepressants developed by pharmaceutical companies were tricyclic drugs - imipramine (first synthesized in 1948, began to be used in large quantities since 1960s), etc. They got their name because of the structure of the molecule - they have three rings in the molecule, although their structure and attached radicals differ.
Trimipramine, a member of the tricyclic antidepressant class.The action of tricyclic antidepressants is based on blocking the reuptake of neurotransmitters (mainly norepinephrine and serotonin) by the presynaptic membrane. As a result, their concentration increases and, as a result, mood should improve.
Particularly active drugs of this group were used to treat severe depression. However, the severe side effects accompanying the treatment, from an increased risk of having a heart attack to provoking epileptic seizures, serious neurological disorders, paranoid conditions, general deterioration in cognitive functions and body condition, along with the development of less toxic and potent drugs, have actually taken these drugs from the mainstream to the sidelines. . For example, in the US and EU they are no longer used as the main antidepressants in the treatment of major depressive conditions.
. For example, in the US and EU they are no longer used as the main antidepressants in the treatment of major depressive conditions.
Although, due to their low price, they can still be actively used in some places.
In Russia, drugs of this type are still used. These are, for example, drugs based on amitriptyline (commercial name - Amitriptyline Nycomed) or clomipramine (commercial name - Anafranil).
2. The power and toxicity of the first inhibitors
In 1952, the antidepressant iproniazid, a monoamine oxidase (MAO) inhibitor, was invented, which also belongs to the first generation of antidepressants (together with tricyclic ones).
The action of this type of antidepressants is based on the inhibition of MAO, which is contained in the nerve endings, and thereby preventing the destruction of monoamines - serotonin, dopamine, tryptamines, norepinephrine and others. Thus, the drugs help to increase the concentration of monoamines in the synaptic cleft.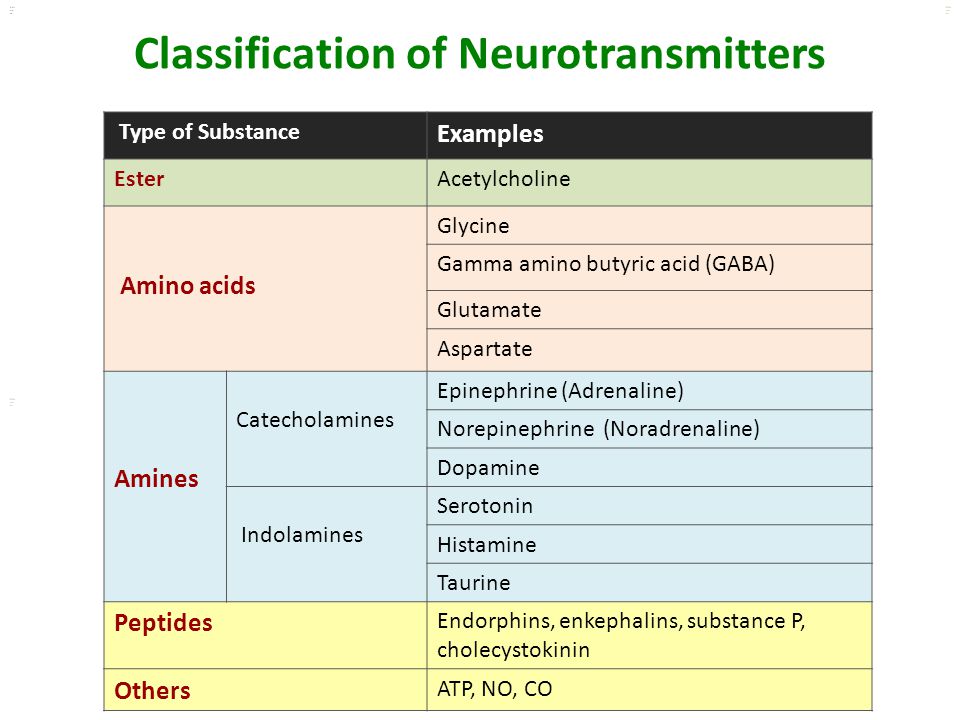
The problem with almost all antidepressants is toxicity and multiple side effects. Especially in non-selective inhibitors that act simultaneously on MAO-A and MAO-B. Iproniazid, due to side effects and high toxicity, has practically ceased to be used as an MAOI.
In addition, the need to follow a specific tyramine diet is a problem. It should be especially strictly adhered to in the case of taking non-selective irreversible MAOIs. The fact is that the simultaneous intake of MAOIs and products "rich in tyramine" can lead to "tyramine syndrome" - the rapid development of a hypertensive crisis. When dieting, you should avoid eating foods such as cheeses, milk, smoked meats (including fish), legumes, wine, vodka, beer and products containing brewer's yeast, as well as spices and cookies.
But these are not the last difficulties. MAOIs do not combine well with a number of drugs due to the suppression of a number of liver enzymes, and these are painkillers, cough and cold drugs, anti-asthma, antihistamines, and others. [7]
MAOIs do not combine well with a number of drugs due to the suppression of a number of liver enzymes, and these are painkillers, cough and cold drugs, anti-asthma, antihistamines, and others. [7]
At the same time, modern MAOIs — moclobemide, pyrazidol, inkazan, befol, selegiline — do not require a diet (however, overdoing it with food containing tyramines is not recommended), they have fewer side effects, they are better tolerated, and their application is wider. However, they are still far from the most popular antidepressants - selective serotonin reuptake inhibitors (SSRIs).
3. Antidepressants take over the masses
So we have reached the most popular antidepressants in the world at the moment - SSRIs. They belong to the second generation, and the most famous of them is, without a doubt, "Prozac" (fluoxetine) of the company Eli Lilly .
The action of drugs of this type (SSRIs) is based, as the name implies, on the inhibition of serotonin reuptake, which leads to an increase in its concentration in the synaptic cleft, with all the consequences.
As the effects of drugs like SSRIs were studied, it became clear that they have side effects, the so-called secondary pharmacological qualities. They affect the capture of norepinephrine and dopamine, stimulate serotonin receptors such as 5-HT2C, etc. Moreover, each of the SSRIs has its own special secondary pharmacological properties.
Popular drugs in this group include fluoxetine, paroxetine, citalopram, escitalopram, sertraline and others. They are present on the market under commercial (trade) names - sertraline is better known under the name "Zoloft", fluoxetine - "Prozac", and escitalopram - "Cipralex".
Unlike first-generation antidepressants, SSRIs are relatively well tolerated, have fewer side effects, and are quite comparable in effect to previous generation drugs.
4. Further development and new types of selective reuptake inhibitors
Further development of drugs based on the inhibition of several neurotransmitters (or other than serotonin) led to the creation of modern antidepressants. These include selective norepinephrine reuptake inhibitors (SNRIs), serotonin and norepinephrine (SNRIs), norepinephrine and dopamine reuptake inhibitors (SNRIs).
These include selective norepinephrine reuptake inhibitors (SNRIs), serotonin and norepinephrine (SNRIs), norepinephrine and dopamine reuptake inhibitors (SNRIs).
The meaning of action is similar to SSRIs - an increase in the concentration of the neurotransmitter (s) in the synaptic cleft. But drugs are easier to tolerate and show better results in the treatment of depression, including severe depression. For example, a number of studies have shown that atomoxetine and reboxetine (SNRIs) are more effective than SSRI drugs in the treatment of severe depression. And drugs of the SNRI group are similar in effectiveness to tricyclic ones, while being easily tolerated and not as toxic as the latter. The most famous of this group are venlafaxine, duloxetine, milnacipran.
If we compare the groups of SSRIs and SSRIs, then, according to a number of studies, the former have more pronounced side effects: problems with the cardiovascular system, with the gastrointestinal tract, with the nervous system.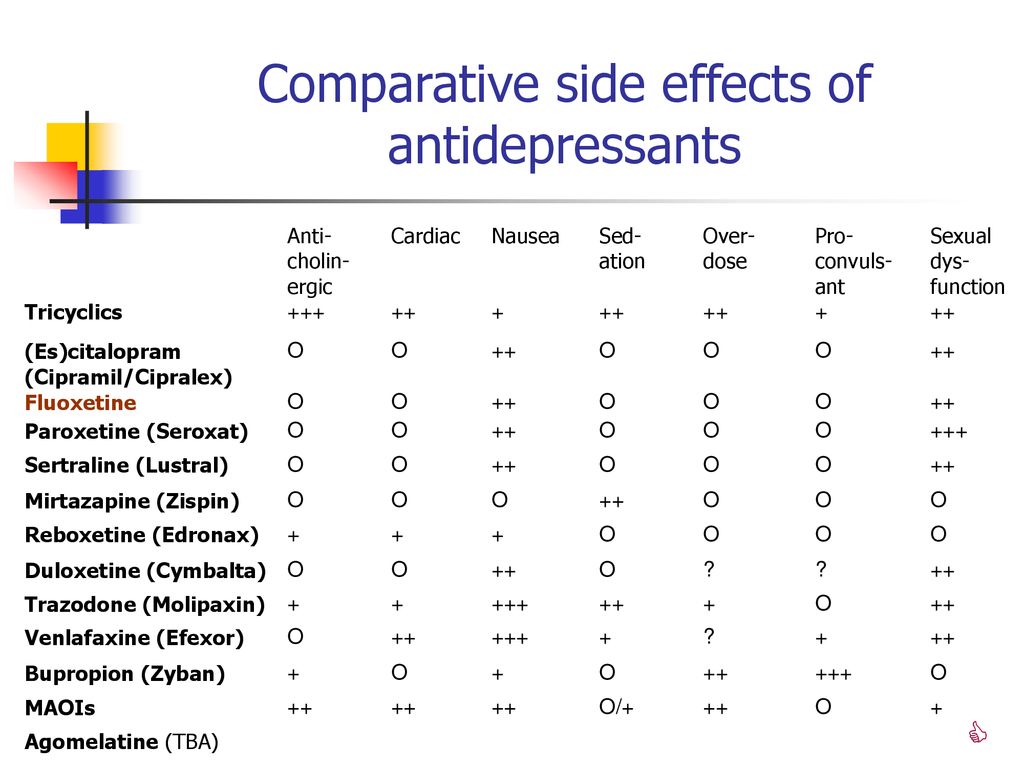 Taking venlafaxine and milnacipran affects the genitourinary system - for example, problems with libido and ejaculation. [8]
Taking venlafaxine and milnacipran affects the genitourinary system - for example, problems with libido and ejaculation. [8]
The SNRIs group includes bupropion, which is actively used in the treatment of apathetic depressions and disorders. This is due to the peculiarities of the drug, which at one time was considered by a number of specialists not as an antidepressant, but as a psychostimulant.
5. Emphasis on the specificity of the action of new drugs
In addition to these types of antidepressants, there are also specific ones (mirtazapine, mianserin), which, by increasing the concentration of norepinephrine and serotonin, block α2-adrenergic receptors. Simultaneously, they block serotonin receptors such as 5-HT2 and 5-HT3, thereby dramatically reducing the side effects for which they are responsible, such as: sexual dysfunction, nausea, vomiting, insomnia, etc.
Mirtazapine's work on blocking α2-adrenergic receptors. From Drugs The Straight Facts, Antidepressants, 2004.
Other drugs, such as trazodone, inhibit reuptake and block serotonin 5-HT2 receptors. As in the previous case, this leads to a decrease in the manifestation of side effects from the use of the drug - sexual disorders, anxiety, insomnia and others.
Some antidepressants have no effect on monoamines at all in terms of reuptake inhibition. The drug agomelatine blocks serotonin 5-HT2C receptors and stimulates melatonin receptors (MT1 and MT2). Blocking serotonin receptors leads to the release of dopamine and norepinephrine, and stimulation of melatonin receptors restores sleep function, often impaired in depression, and eliminates insomnia. Since the drug does not affect other serotonin receptors, does not stimulate the capture of neurotransmitters, it is actually devoid of the side effects of most antidepressants. But there are still some: dizziness, headache, nausea.
Problems of antidepressants and attempts to find solutions to them
A serious scientific problem regarding modern antidepressants, which has been increasingly discussed lately - their effectiveness and various side effects.
A number of analyzes of antidepressant studies have found that, given all available data, including unpublished data, the effectiveness of many drugs can be called into question: in some cases, the result of their use is not better than that obtained in the placebo control group [9]. Some studies claim that SSRI-type antidepressants may increase the risk of suicide in adolescents [10].
Efficacy of different antidepressants compared to placebo. On average, the effect was 42% more effective than the changes observed in the placebo groups [9].As the study of depression and methods of its treatment, it became clear that in mild or moderate forms of it, the most ordinary physical exercises were able to improve the condition of the sick, albeit in the short term. They should not be overestimated, physical exercises have at best a moderate effect [11]. In addition, a depressed person is not easily motivated to exercise.
The search and invention of new antidepressants is fueled not only by new data, for example, the discovered effect of interleukins (or cytokines) formed during the inflammatory process on the course of depression [12], but also by a decrease in the effectiveness of antidepressants in large-scale studies.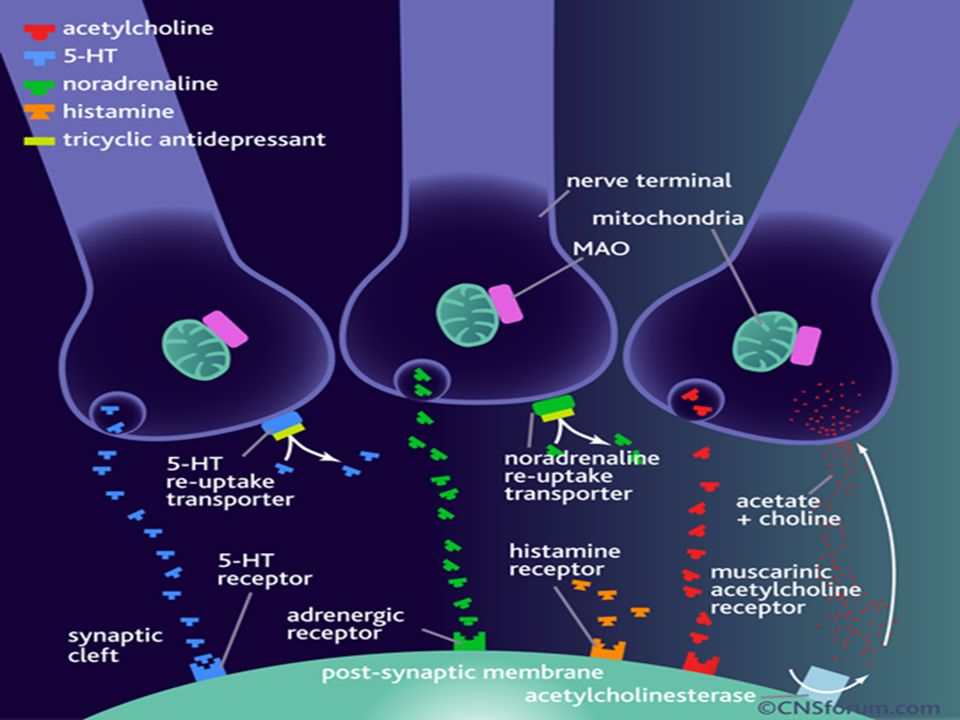 Thus, the large-scale STAR*D study, which studied mainly the latest drugs - bupropion, citalopram, mirtazapine, sertraline, and others - revealed an almost complete lack of difference in the effectiveness of depression treatment between them [13]. And the subsequent ones showed that 30-50% of patients who took antidepressants, the latter practically did not help in the treatment [14]. During the course of taking an antidepressant, its effectiveness decreased [15]. In general, according to clinical studies, about a third of those taking antidepressants achieved a complete remission, a third - they helped, despite the fact that the likelihood of relapse remained constant, and the remaining third did not [16].
Thus, the large-scale STAR*D study, which studied mainly the latest drugs - bupropion, citalopram, mirtazapine, sertraline, and others - revealed an almost complete lack of difference in the effectiveness of depression treatment between them [13]. And the subsequent ones showed that 30-50% of patients who took antidepressants, the latter practically did not help in the treatment [14]. During the course of taking an antidepressant, its effectiveness decreased [15]. In general, according to clinical studies, about a third of those taking antidepressants achieved a complete remission, a third - they helped, despite the fact that the likelihood of relapse remained constant, and the remaining third did not [16].
In the experimental practice of treating depression and depressive conditions, for example, in the USA, in recent years, psychostimulants such as ketamine and its derivatives, one of the most common drugs in Southeast Asia, have been actively used [17]. And when developing new drugs, they are already experimenting with psilocybin (a hallucinogen) [18].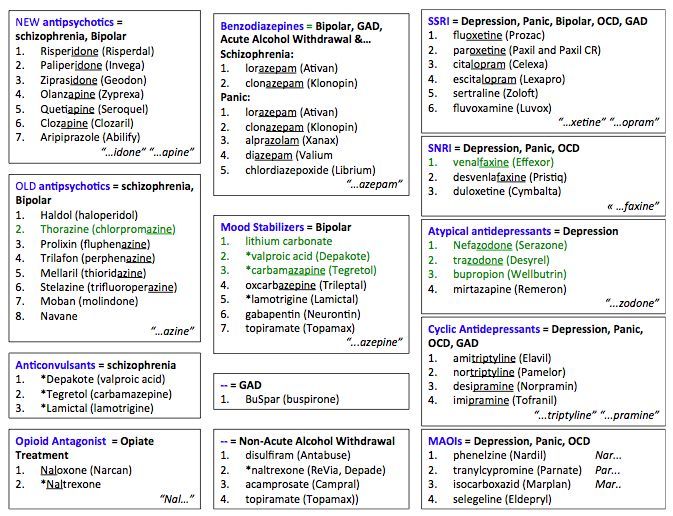 It is probably safe to say that psychopharmacology, having made a circle, has returned to the "basics" and again wants to try to treat depression with narcotic drugs and their derivatives. However, this is in the USA, not in Russia, and so far only experimentally.
It is probably safe to say that psychopharmacology, having made a circle, has returned to the "basics" and again wants to try to treat depression with narcotic drugs and their derivatives. However, this is in the USA, not in Russia, and so far only experimentally.
Conclusion
Despite the active search for an effective and universal cure for depression, it is not yet available, and there are some doubts that it will be created. Especially considering the fact that has been increasingly discussed recently: the term “depression” hides various disorders of various etiologies. Nevertheless, even the available drugs, possibly combined with physical activity, can improve the patient's quality of life and lead - in most cases - to remission.
Literature
[1] Inflammatory illness: Why the next wave of antidepressants may target the immune system, Nature Medicine 23, 1009–1011 (2017), doi:10.1038/nm0917-1009
[2] From Stress to Inflammation and Major Depressive Disorder: A Social Signal Transduction Theory of Depression, Psychol Bull.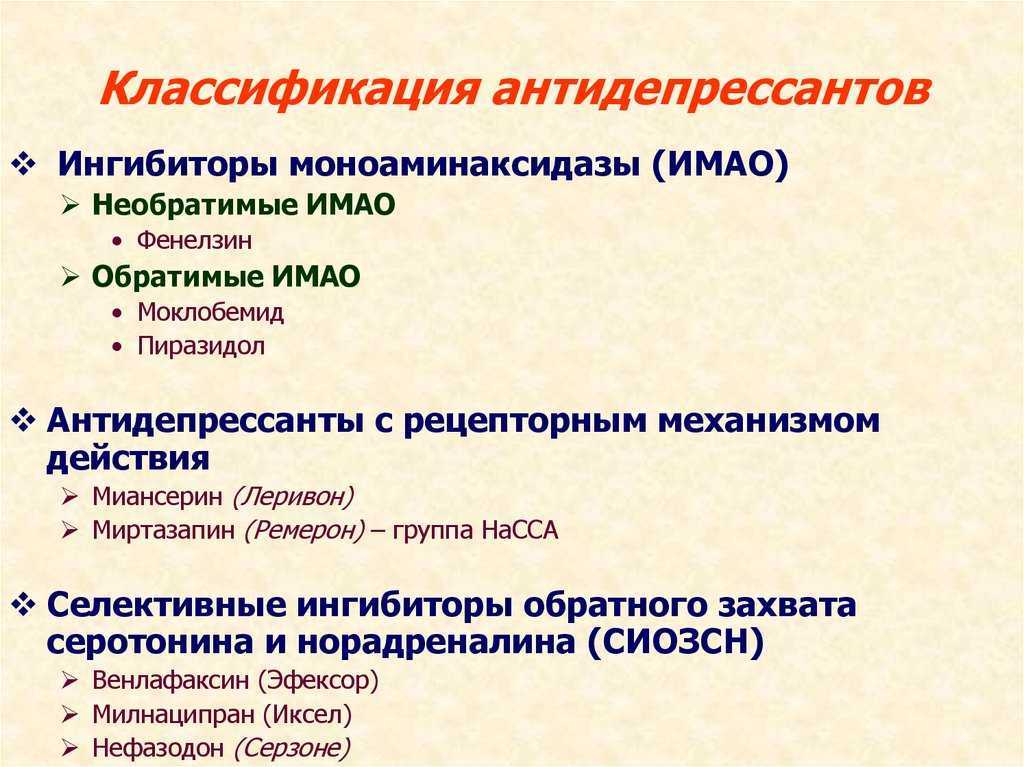 May 2014; 140(3): 774-815. doi:10.1037/a0035302; PATHOPHYSIOLOGY OF DEPRESSION: DO WE HAVE ANY SOLID EVIDENCE OF INTEREST TO CLINICIANS? World Psychiatry. 2010 Oct; 9(3): 155-161.
May 2014; 140(3): 774-815. doi:10.1037/a0035302; PATHOPHYSIOLOGY OF DEPRESSION: DO WE HAVE ANY SOLID EVIDENCE OF INTEREST TO CLINICIANS? World Psychiatry. 2010 Oct; 9(3): 155-161.
[3] Imaging extrasynaptic glutamate dynamics in the brain, PNAS 2010 April, 107 (14) 6526-6531. https://doi.org/10.1073/pnas.0913154107
[4] Glutamate: its role in learning, memory, and the aging brain, July 1993, Volume 111, Issue 4, pp 391-401
[5] Neuronal plasticity : A link between stress and mood disorders, Psychoneuroendocrinology (2009) 34S, S208-S216
[6] Effects of Acute Tryptophan Depletion on Mood and Facial Emotion Perception Related Brain Activation and Performance in Healthy Women with and without a Family History of Depression, Neuropsychopharmacology (2007) 32, 216-224; Role of Brain-Derived Neurotrophic Factor in the Aetiology of Depression, CNS Drugs 2010; 24(1): 1-7; The role of BDNF and its receptors in depression and antidepressant drug action: Reactivation of developmental plasticity. Dev.Neurobiol 2010 Apr;70(5):289-97. doi: 10.1002/dneu.20758.
Dev.Neurobiol 2010 Apr;70(5):289-97. doi: 10.1002/dneu.20758.
[7] Markova I. V., Mikhailov I. B., Nezhentsev M. V. Pharmacology 2nd. - St. Petersburg: Folio, 2001 .; George Arana, Gerald Rosenbaum. Guide to psychopharmacotherapy. Per. from English - Moscow: BINOM Publishing House, 2004 (George Arana, Jerrold Rosenbaum "Handbook of Psychiatric Drug Therapy", 4th ed., 2001)
[8] Serotonin and norepinephrine reuptake inhibitors: pharmacological properties, clinical efficacy and tolerability in comparison with other classes antidepressants. Part 2, Consilium Medicum, 2007, Vol. 2, No. 3.
[9] Antidepressants versus placebo in major depression: an overview. World Psychiatry. 2015 Oct;14(3):294-300. doi: 10.1002/wps.20241. For other data, see Randomized, placebo-controlled trials of antidepressants for acute major depression: thirty-year meta-analytic review. neuropsychopharmacology. 2012 Mar;37(4):851-64. doi: 10.1038/npp.2011.306.
[10] Selective serotonin reuptake inhibitors and risk of suicide: a systematic review of observational studies. CMAJ. 2009 Feb 3; 180(3): 291-297. doi: 10.1503/cmaj.081514
CMAJ. 2009 Feb 3; 180(3): 291-297. doi: 10.1503/cmaj.081514
[11] Exercise for depression. Cochrane Database of Systematic Reviews. Editorial Group: Cochrane Common Mental Disorders Group DOI: 10.1002/14651858.CD004366.pub6 ; Benefits from aerobic exercise in patients with major depression: a pilot study. British Journal of Sports Medicine 2001;35:114-117. ;
[12] Inflammatory mechanisms in major depressive disorder. Curr Opin Psychiatry. 2011 Nov;24(6) : 519-25. doi: 10.1097/YCO.0b013e32834b9db6. ; Antidepressants and Neuroinflammation: Can Antidepressants Calm Glial Rage Down? Mini Rev Med Chem. 2011 Jun;11(7):555-64.
[13] The STAR*D project results: A comprehensive review of findings. Current Psychiatry Reports
December 2007, Volume 9, Issue 6, pp 449-459
[14] Recent Progress in Pharmacological and Non-Pharmacological Treatment Options of Major Depression. Current Pharmaceutical Design6 Volume 12, Issue 4, 2006. doi: 10.2174/138161206775474422;
[15] Early Onset of Selective Serotonin Reuptake Inhibitor Antidepressant Action.