What triggers a bipolar episode
10 Most Common Triggers for Bipolar Mood Episodes
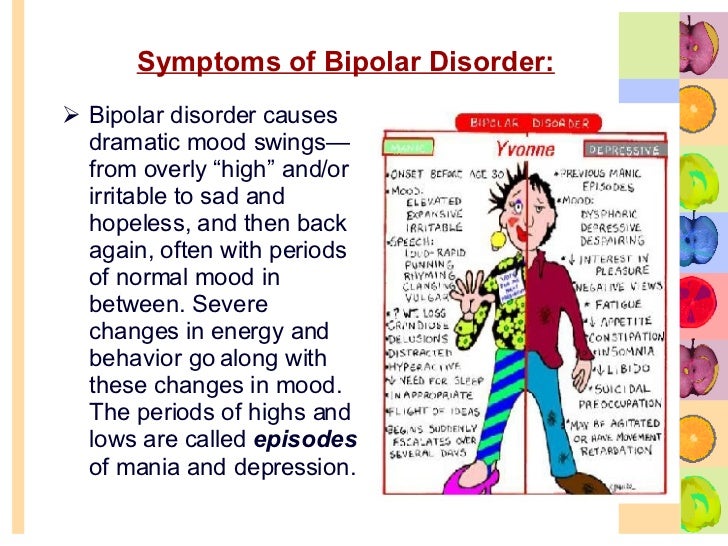
Bipolar disorder is characterized by unusual shifts in mood and energy. These shifts, called “mood episodes,” last at least a week in the case of mania (feeling extremely “up”), and at least two weeks in the case of depression (feeling extremely “down”).
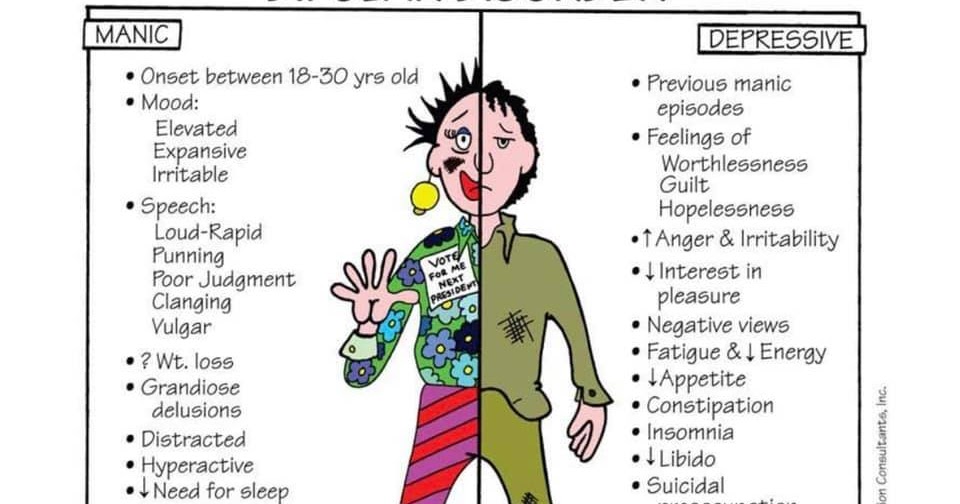
Mania and hypomania share the same symptoms, according to Mayo Clinic, which include:
- Feeling unusually upbeat, euphoric, or irritable, with increased energy
- Elevated mood
- A decreased need for sleep
- Racing thoughts
- Trouble concentrating or distractibility
- Poor judgment
In cases of mania, these symptoms are severe enough to cause significant problems in your day-to-day life. For instance, you might be unable to go to work or school, or you may be compulsively spending money.
Hypomania is considered a less severe form of mania. In cases of hypomania, your daily functioning isn't significantly impacted. For example, you’re usually able to work and socialize.
Symptoms of depression can disrupt people's daily lives, too. According to Mayo Clinic, the symptoms include:
- Sadness
- Emptiness
- Hopelessness
- Tearfulness
- Loss of interest or pleasure in most or all activities
- Sleep issues
- Fatigue
- Guilt
- Difficulty concentrating
- Restlessness or slowed behavior
When mood episodes are severe enough, they can have an even more profound effect on your life. Some episodes of depression and mania are accompanied by loss of reality or psychosis, characterized by hallucinations or delusions. "And unfortunately, suicide is common," says the psychiatrist Jeffrey Bennett, MD, an associate professor of clinical psychiatry at the Southern Illinois University School of Medicine in Springfield.
Suicide deaths are 10 to 30 times more common among people with bipolar disorder than the general population, according to research published in July 2021 in Translational Psychiatry.
What’s more, with recurrent episodes, some people with bipolar disorder may experience less complete periods of remission and a greater likelihood of relapse, either to depression or mania, Dr. Bennett says.
Can these episodes be avoided? Perhaps not. But if you're aware of certain triggers you may find it easier to manage bipolar disorder. Watch out for these common culprits.
Stress
One of the most common bipolar triggers is stress. In a study published in the Journal of Affective Disorders, negative or stressful life events were associated with subsequent mood episodes. It appears that earlier in their course, episodes of depression or mania in bipolar disorder are triggered more often by stressful life events.
While causes of stress are highly individual, certain life events and lifestyle patterns — such as sleep or relationship issues — may act as triggers.
Changes in Sleep Patterns or Lack of Sleep
A change in your sleep pattern is a hallmark symptom of bipolar disorder — but it can also be a trigger.
Shift workers, people who work long and variable hours, and students who are short on sleep are all at risk for a recurrent mood episode related to a lack of sleep. "In addition, travel beyond one's time zone can be another trigger for a mood episode," says Bennett.
Interpersonal and social rhythm therapy (IPSRT) is one of the most effective preventive measures, Bennett says. This treatment approach, available in group as well as individual sessions, helps you develop an orderly life schedule of sleep, diet, and exercise habits to help you more effectively manage your bipolar disorder.
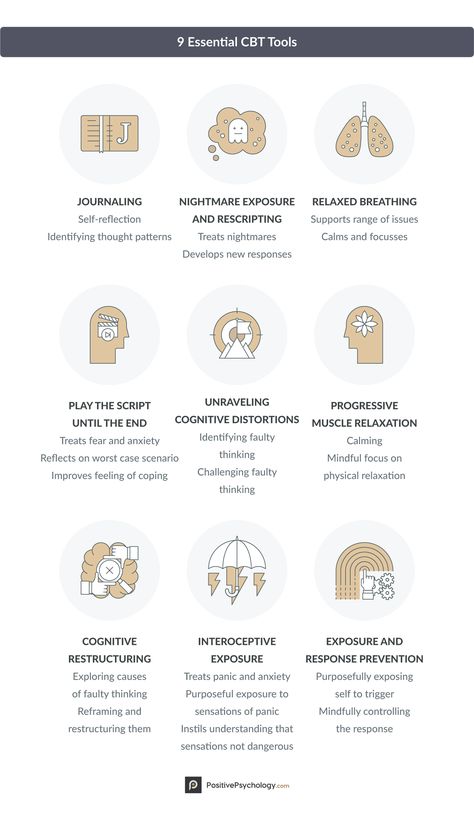
Other forms of therapy, including psychoeducation and cognitive behavioral therapy (CBT), can also be helpful in managing the condition.
Blowout Arguments With Partners, Coworkers, or Friends
Broken relationships are too often the result of untreated bipolar disorder.
But getting into a spat with a loved one can also be a red flag: Your argument could be due to the irritability that often occurs during a manic or depressive episode, or could itself cause stress that becomes a contributing factor for a recurrent episode.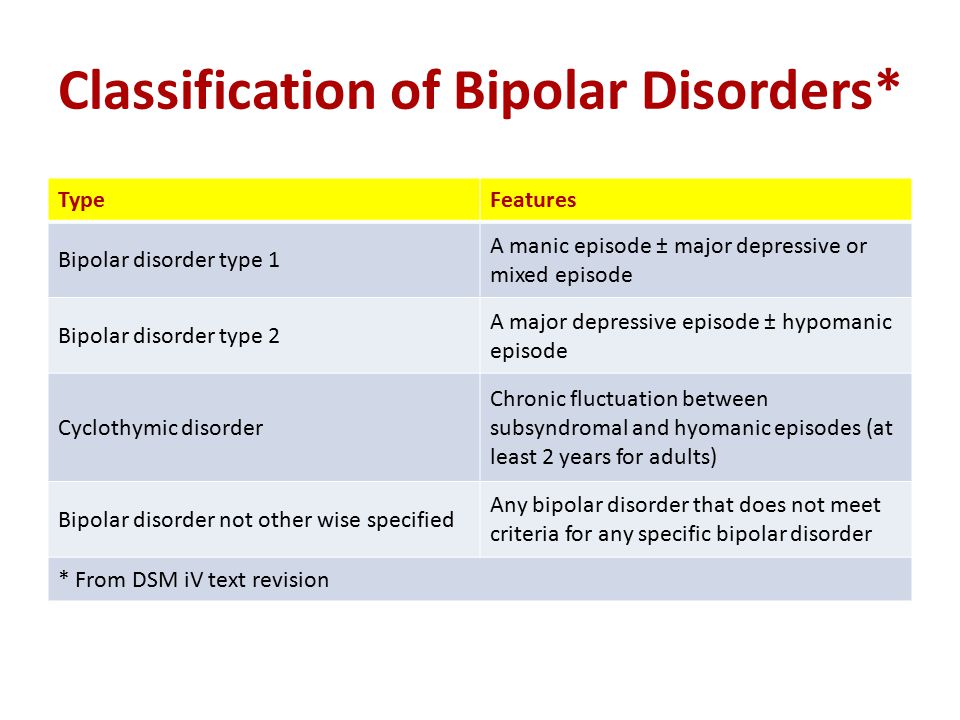
Any type of relationship conflict — whether it’s with your partner, coworker, family member, or friend — can trigger stress and send you over the edge. In another study published in the Journal of Affective Disorders, people with bipolar disorder said negative social experiences were among the events that triggered suicidal thinking for them.
Bad Breakups or Marriage Breakdowns
A number of people with bipolar disorder — especially those with a history of severe manic episodes — experience a breakdown in their marriages. If you’re going through a divorce, working with your therapist through what is often a drawn-out and extremely stressful process can help.
You might consider a durable power of attorney that allows someone else to make major decisions for you, such as financial ones, when you are going through an episode of depression or mania in relation to or during a breakup.
In fact, assigning a durable power of attorney could be useful for anyone who might be experiencing an episode of bipolar disorder.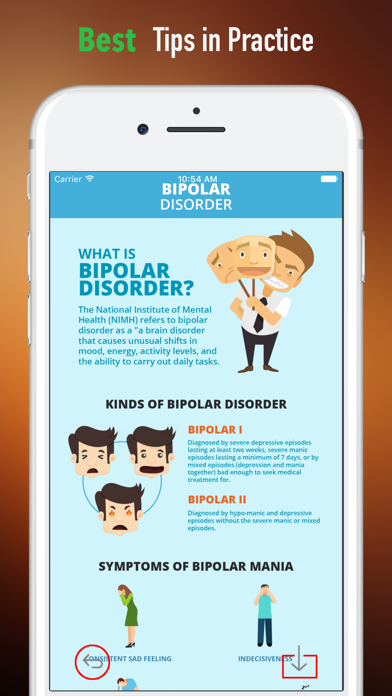
Alcohol Misuse and Drug Intoxication, and the Aftereffects
Misusing drugs and alcohol doesn’t cause bipolar disorder, but it can cause an episode to suddenly occur, or it can worsen the underlying illness. What’s more, about one in five people with bipolar disorder have a substance abuse disorder, according to an analysis of data on young adults with mental illness published in the journal Social Psychiatry and Psychiatric Epidemiology.
Intoxication with drugs such as cocaine and amphetamines can cause or worsen manic symptoms, while the aftereffects of cocaine or alcohol use are associated with worsening depressive symptoms.
Antidepressants, Corticosteroids, and Other Medication
Can antidepressants make you manic?
The treatment of bipolar disorder can trigger episodes of mania by further setting off unstable moods and behaviors. Many psychiatrists say they've seen patients enter a manic phase after starting antidepressants — and some feel uncomfortable prescribing them to people with bipolar disorder.
What should you do about bipolar depression? Until more research is available on long-term safety, Keming Gao, MD, PhD, a professor of psychiatry at Case Western Reserve School of Medicine in Cleveland, and the director of the mood disorders program at the University Hospitals Cleveland Medical Center suggests the following: For bipolar I depression, antidepressants should be used only with a mood stabilizer or stabilizers after symptoms haven't responded to FDA-approved treatment options (such as mood stabilizers).
Dr. Gao says that while some recent studies suggest that antidepressants alone are as effective as lithium taken alone for some people with bipolar II (those who haven't experienced a manic episode), they should never be used alone for bipolar I depression, and patients and doctors should consider discontinuing use of antidepressants once symptoms have improved.
Other drugs that have been linked to manic symptoms include corticosteroids, thyroid medication, and appetite suppressants, says Gao.
A Brand-New Season and Abnormal ‘Clock Genes’
About 20 percent of people with bipolar disorder experience fluctuations in mood when the weather changes. Specifically, they're more likely to undergo seasonal depression during the early winter, and mania or hypomania during the spring or summer, according to a research review published in the Journal of Affective Disorders.
Experts chalk this up to sunlight: Your circadian rhythm, the body’s internal response to changes in a 24-hour day, is affected by the amount of sunlight you get each day. This response is controlled by a complex set of genes commonly referred to as “clock genes.” If some of these genes are abnormal, you could be at risk for seasonal bipolar disorder.
Pregnancy Along With Altered Sleep Patterns and Shifting Hormones
People with bipolar disorder have an elevated risk of a mood episode in the postpartum period — the weeks and months after giving birth — according to research published in the Lancet.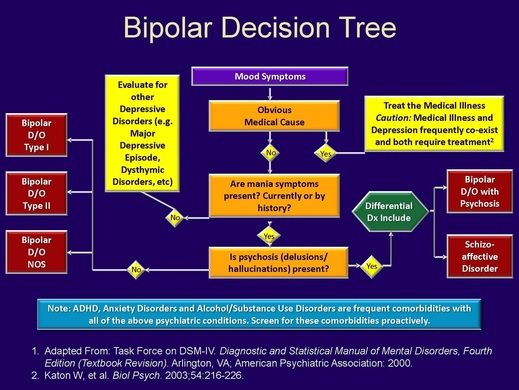
Changing sleep patterns, altered medication prescriptions, and shifting hormones after delivery can combine to serve as risk factors for a postpartum mood or psychotic episode, the researchers wrote.
Bipolar disorder is also strongly associated with postpartum psychosis, a severe mental illness characterized by an inability to respond emotionally to one's newborn, or by thoughts of harming one's baby, according to the Cleveland Clinic.
During your pregnancy, be sure to work with your entire medical team — your bipolar disorder specialists and your ob-gyn — on treatment approaches you can try during and after pregnancy to help prevent postpartum depression, postpartum mania, or postpartum psychosis.
Financial and Emotional Issues Caused by a Job Loss
One of life’s most unpredictable stressors? Losing your job.
And the emotions you may feel about your job loss can be equally unpredictable. People who weren’t satisfied with their work may find it liberating.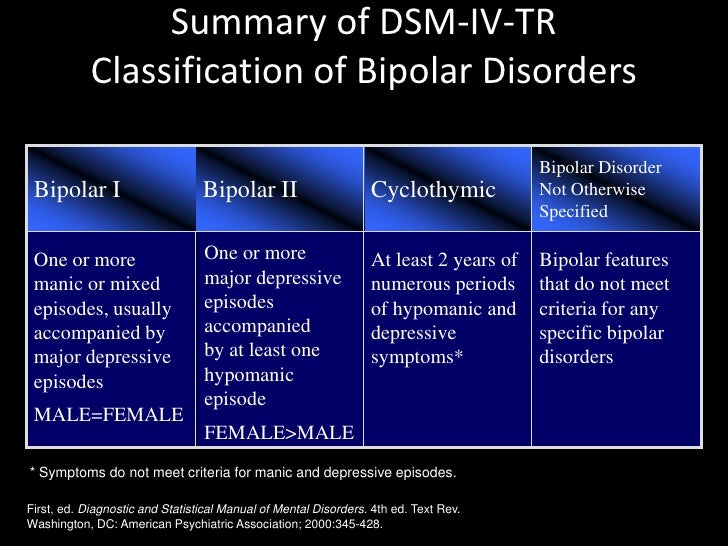 For others, the financial and emotional strains involved can trigger major stress. Either way, the dramatic shift in emotions could trigger a bipolar episode.
For others, the financial and emotional strains involved can trigger major stress. Either way, the dramatic shift in emotions could trigger a bipolar episode.
It may be a good idea to try to put away three to six months' worth of savings to help with the transition in case you lose your job.
The Death of a Loved One and Bereavement
The death of a loved one may be the most stressful life event anyone faces. Many people continue managing bipolar disorder successfully through their mourning, but it may have extreme consequences for others, who can develop “funeral mania,” says Bennett.
This occurs when someone whose bipolar symptoms are stable attends a funeral and develops a manic episode over the course of the following week. The period of bereavement should be one of increased monitoring and heightened support, advises Bennett.
Additional reporting by Christina Vogt.
5 Complementary and Integrative Therapies That Might Help Bipolar Disorder — and 4 to Approach With Caution
By7 Vitamins and Supplements That May Be Helpful for Bipolar Disorder
By7 Triggers That Can Lead to a Bipolar Episode
ByA Therapist Speaks: 5 Common Bipolar Medication Frustrations and How to Safely Manage Them
ByWhat Is Psychosis? Symptoms, Causes, Diagnosis, and Treatment
ByBipolar Disorder: 8 Relationship Tips for Married Couples
By6 Strategies for Self-Care When You Have Bipolar 1 Disorder
ByBiggest Challenges of Bipolar 1 Disorder Manic Episodes (and How to Manage Them)
ByThe 7 Most Effective Ways to Manage Bipolar 1 Disorder
ByA Therapist Speaks: What Is Bipolar Disorder Stigma, and How Can We End It?
By7 Triggers That Can Lead to a Bipolar Episode
Bipolar disorder is a mental health condition that affects millions of people in the United States.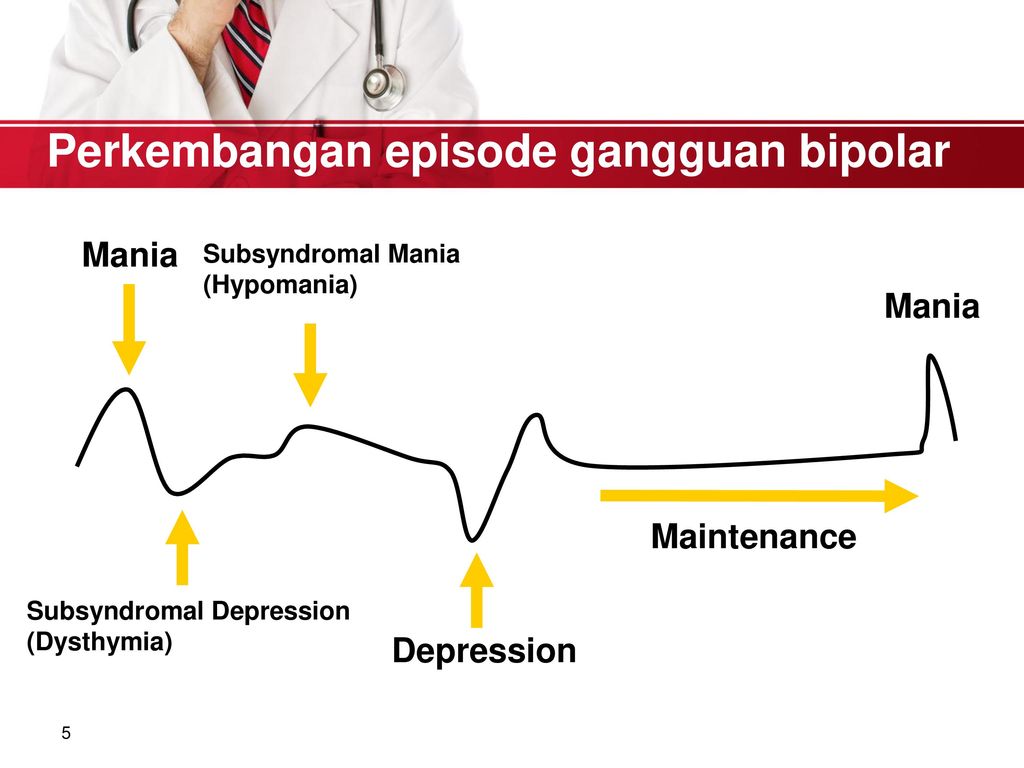 According to the National Institute of Mental Health (NIMH), an estimated 4.4 percent of American adults experience bipolar disorder at some point. There are several types of bipolar disorder, which are characterized as having extreme shifts in mood, energy, and activity levels. Bipolar disorder can affect your ability to think clearly, and the severity and types of symptoms can be different from one person to another.
According to the National Institute of Mental Health (NIMH), an estimated 4.4 percent of American adults experience bipolar disorder at some point. There are several types of bipolar disorder, which are characterized as having extreme shifts in mood, energy, and activity levels. Bipolar disorder can affect your ability to think clearly, and the severity and types of symptoms can be different from one person to another.
Although the exact cause of bipolar disorder is unknown, research is ongoing.
Several key risk factors, such as genes, brain structure and function, and exposure to severe stress could play a role in the frequency, severity, and duration of symptoms, according to the National Alliance on Mental Illness (NAMI).
Certain lifestyle and environmental factors can also trigger or aggravate the extreme highs and lows, known as bipolar episodes, which are a hallmark of the condition. Once you’re aware of these triggers, you can gain better control over your disorder, working closely with your psychiatrist and care team.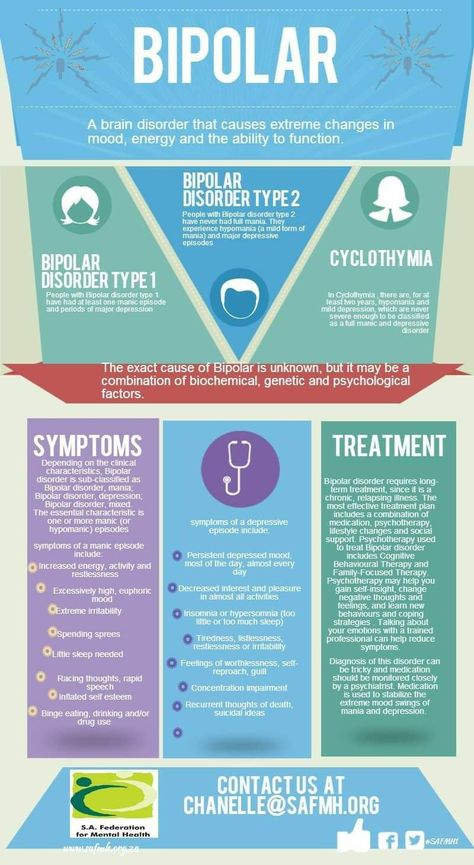
The main difference between bipolar disorder and conditions like unipolar depression is the possibility of experiencing the overly excited state called mania, says Amit Anand, MD, a professor at Harvard Medical School of Medicine in Boston and a leading researcher on mood disorders and behavioral health.
People who are experiencing a manic episode have a cluster of symptoms, which may include an unusually elevated or extremely irritable mood, a decreased need for sleep, rapid speech and racing thoughts, excessive interest in pleasurable activities, or feeling overly important and powerful.
By contrast, during depressive episodes, individuals may experience depressed mood, intense sadness or loss of interest or pleasure in activities, sleep disturbance, fatigue, and trouble concentrating, and they may feel hopeless or worthless, with thoughts of death or suicide.
It is notable that in severe episodes of mania or depression, an individual may also experience psychotic symptoms.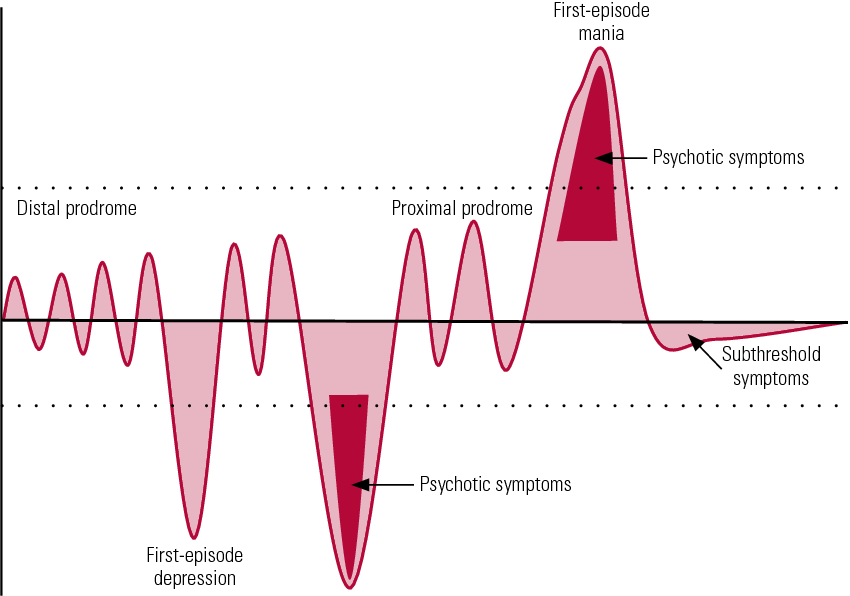
Complicating matters is that it’s possible to experience both symptoms of mania and depression at the same time: This is known as a bipolar episode with mixed features. When this happens, you may feel overly energized while also feeling extremely irritable, sad, hopeless, or empty.
You do not have to experience mania to have bipolar disorder. Some people may experience a less severe form of mania, known as hypomania. Because the symptoms of hypomania are less severe, they may not cause as many serious problems. And so people experiencing hypomania may not identify anything being wrong, making a bipolar diagnosis more difficult.
Understanding and Managing Bipolar TriggersBipolar episodes can be triggered by lifestyle and environmental factors. Recognizing your triggers and avoiding them, Dr. Anand says, is often a key to managing bipolar disorder and can be an important addition to your treatment by a trained mental health professional.
Here’s a closer look at seven factors that may worsen bipolar symptoms or trigger an episode:
1.
 Stress
StressIn many cases, a major life change or stressful event, such as losing a loved one or having severe financial troubles, can trigger a bipolar episode. How an individual copes with stress can also affect how bipolar disorder progresses.
According to a meta-analysis published in 2017, people with bipolar disorder who were having a relapse of their condition reported experiencing more stressful life events compared with those who were in a more stable mood phase. The researchers concluded that individuals with bipolar disorder tend to be more sensitive to stressors, suggesting that psychosocial treatments are an important component of successfully managing the condition and should be used in addition to mood-stabilizing medications prescribed by a trained psychiatrist.
Psychosocial treatments include psychotherapy and support groups, and education regarding the condition for the individual as well as for loved ones is important so that people can spot the signs of relapse, according to NAMI.
2. Poor Sleep
Lack of sleep is a frequent trigger of bipolar mood episodes, Anand says. Poor sleep or a disruption in normal sleeping patterns, including jet lag, can trigger these intense mood swings. But there is evidence that increased awareness of this elevated risk combined with psychological treatment may help.
In a study published in 2015, researchers treated half of the 58 study participants who had bipolar disorder and insomnia with a bipolar-specific modified form of cognitive behavioral therapy (CBT) that involved incorporating good sleep habits, relaxation, and dim lights at bedtime, and reducing anxiety about sleep into daily routines. The other half of the study participants were given information about how sleep, stress, diet, exercise, and mood are related to each other, but were given no plan or intervention designed to change behavior.
The results were eye-opening: Six months after these interventions, the people who received the CBT approach had experienced just 3.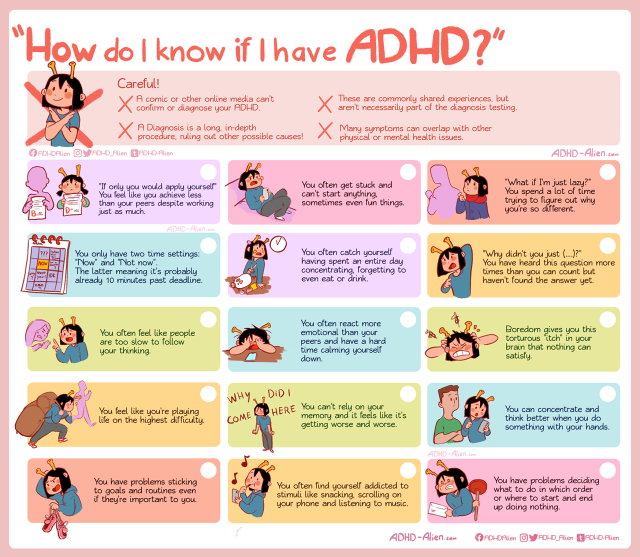 3 days spent in a bipolar episode compared with 25.5 days for those who were given only educational materials. The CBT group also had a lower rate of relapse and less severe insomnia. These results show that it may be beneficial for you to ask your doctor for a plan to ensure you’re getting enough quality sleep if you have bipolar disorder.
3 days spent in a bipolar episode compared with 25.5 days for those who were given only educational materials. The CBT group also had a lower rate of relapse and less severe insomnia. These results show that it may be beneficial for you to ask your doctor for a plan to ensure you’re getting enough quality sleep if you have bipolar disorder.
3. Seasonal Changes
For some people with bipolar disorder, there’s a seasonal pattern to mood episodes. Anand says there’s some evidence that more manias occur during the spring and summer months, while more episodes of depression take place in the fall and winter. But some people experience the opposite, and gender seems to play a role as well.
In a study from 2013 that followed 452 participants with bipolar disorder, the researchers reported that 23 percent of the participants displayed a seasonal pattern in their bipolar episodes — a significant percentage that was consistent with the findings of earlier research. The authors also noted that the participants with seasonal patterns had a significantly higher number of major depressive episodes, and there were differences in the types and timing of episodes based on gender.
Because of these findings — that 1 in 4 people with bipolar disorder display seasonal patterns and also may be at risk for more severe episodes — the researchers concluded that regular screening for seasonal patterns should be an important part of treatment.
A more recent study, from 2019, examined data in over 60,000 people who were admitted to a hospital for a manic, depressive, or mixed featured episode between 2001 and 2014. The authors reported that seasonal patterns in hospitalization rates during manic episodes were evident for both men and women: Women were more likely to experience manic episodes in summer and autumn, depressive episodes in winter, and mixed features in summer; whereas men were more likely to experience manic episodes in summer. Women under age 35 were also more likely to have this seasonal pattern in manic and mixed episodes.
4. Medications
Treatment for bipolar disorder includes psychotropic medications, such as mood stabilizers, antipsychotics, and antidepressants, according to NAMI. But certain types of some antidepressants, such as SSRIs like fluoxetine (Prozac) and sertraline (Zoloft), may worsen bipolar disorder symptoms and possibly even trigger a manic episode in those with undiagnosed bipolar disorder. If you have bipolar disorder, you should not take an antidepressant without also taking a mood stabilizer or an antipsychotic medication, Anand says.
But certain types of some antidepressants, such as SSRIs like fluoxetine (Prozac) and sertraline (Zoloft), may worsen bipolar disorder symptoms and possibly even trigger a manic episode in those with undiagnosed bipolar disorder. If you have bipolar disorder, you should not take an antidepressant without also taking a mood stabilizer or an antipsychotic medication, Anand says.
Additionally, stimulants — a class of medications used to treat conditions like attention deficit hyperactivity disorder (ADHD) — may also trigger a manic episode.
And there are other types of medications, such as corticosteroids or thyroid medication, that are prescribed for nonpsychiatric conditions but may also lead to hypomanic or manic symptoms, just as other medications may worsen symptoms of depression.
The bottom line: If you have bipolar disorder along with one or more other medical conditions (such as obsessive-compulsive disorder, ADHD, or nonpsychiatric conditions) that is treated with medication, NAMI recommends that you develop a treatment plan with your doctor to best manage all of the conditions and monitor your side effects.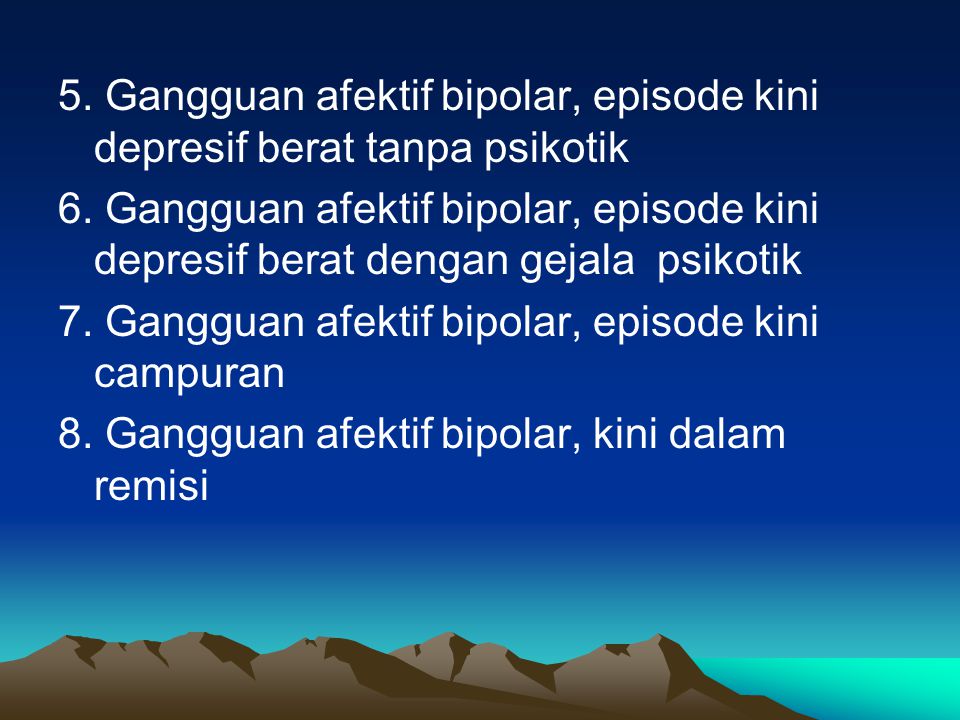
5. Drug and Alcohol Use
Substance misuse is common among people with mental health conditions as a comorbid condition or as a way to cope with their symptoms. In fact, 30 to 50 percent of people with bipolar disorder will develop a substance use disorder, notes the Substance Abuse and Mental Health Services Administration (SAMHSA).
Anand cautions against using drugs or alcohol to “treat” symptoms of the condition. Drinking alcohol or taking drugs, he says, can worsen your bipolar mood swings and lead to an increase in suicidal thoughts or behaviors. As SAMHSA notes, substance use or withdrawal can cause symptoms attributed to bipolar disorder, including agitation, anxiety, paranoia, mania, or depression.
Drinking alcohol in particular can interfere with the metabolism of medications, making you less likely to respond to prescribed treatment, and it may increase the risk of psychiatric hospitalization. That’s why doctors strongly encourage people with bipolar disorder not to self-medicate and instead seek (or continue to get) professional help for management of their bipolar disorder using prescribed medications and psychosocial therapy to manage symptoms.
6. Caffeine
It’s important to note that caffeine is also considered a drug and a stimulant. As such, it may disturb sleep, change sleep patterns,and trigger hypomanic or manic episodes. It can also affect the way your body breaks down the medications you take to treat your condition (like lithium), which can trigger hypomanic or manic episodes, according to a 2021 review of 17 relevant studies. Talk to your doctor about your caffeine consumption and how it may affect your symptoms.
7. Childbirth
The link between childbirth and bipolar disorder has been well-documented in a number of scientific studies. A systematic review from 2016 of nine papers found that the risk for mood disorder episodes increases both during and after pregnancy, and the risk is especially high in the time after childbirth (the postpartum period) in women with bipolar disorder.
And women with a history of bipolar disorder are at especially high risk of postpartum psychosis, according to research published in 2021.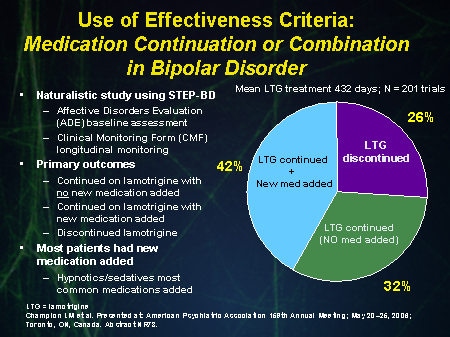 The researchers noted that nearly 50 percent of women with bipolar disorder experienced at least one “mood episode” — for example, a manic, hypomanic, or depressive episode — during pregnancy or within 12 months after childbirth. Hormonal changes associated with pregnancy and the postpartum period for women also increase the risk of mood episodes. Further complicating things: Women often have an interruption to their psychiatric treatment and medications following the birth of a child.
The researchers noted that nearly 50 percent of women with bipolar disorder experienced at least one “mood episode” — for example, a manic, hypomanic, or depressive episode — during pregnancy or within 12 months after childbirth. Hormonal changes associated with pregnancy and the postpartum period for women also increase the risk of mood episodes. Further complicating things: Women often have an interruption to their psychiatric treatment and medications following the birth of a child.
It’s also worth noting that both men and women with bipolar disorder may have episodes triggered by the stress surrounding the birth of a child, coupled with potentially severely disturbed sleep. While there is very limited research examining the effects of a new baby on men, a study from 2017 found that some evidence suggests that fathers with bipolar disorder may have an increased risk of hypomanic episodes after their child is born.
Anticipating Triggers
While it is important to recognize potential triggers for a bipolar episode , it is also essential to keep in mind that episodes can occur even without a trigger. “Bipolar episodes can come out of the blue,” Anand notes.
“Bipolar episodes can come out of the blue,” Anand notes.
Your best plan: Do what you can to manage your stress, get good sleep, avoid using alcohol or other risky substances, and work with your doctor to find the best strategies and treatments to manage your bipolar disorder.
Additional Reporting by Jessica Migala
Editorial Sources and Fact-Checking
- Bipolar Disorder. National Institute of Mental Health.
- Bipolar Disorder. National Alliance on Mental Illness. August 2017.
- Lex C, Bäzner E, Meyer TD. Does Stress Play a Significant Role in Bipolar Disorder? A Meta-Analysis. Journal of Affective Disorders. January 15, 2017.
- Psychosocial Treatments [PDF]. National Alliance on Mental Illness. March 2015.
- Harvey AG, Soehner AM, Kaplan KA, et al. Treating Insomnia Improves Mood State, Sleep, and Functioning in Bipolar Disorder: A Pilot Randomized Controlled Trial. Journal of Consulting and Clinical Psychology.
 June 2015.
June 2015. - Geoffroy PA, Bellivier F, Scott J, et al. Bipolar Disorder With Seasonal Pattern: Clinical Characteristics and Gender Influences. Chronobiology International. November 2013.
- Fellinger M, Waldhoer T, König D, et al. Seasonality in Bipolar Disorder: Effect of Sex and Age. Journal of Affective Disorders. January 15, 2019.
- Substance Use Disorders. National Alliance on Mental Illness. May 2020.
- An Introduction to Bipolar Disorder and Co-Occurring Substance Use Disorders [PDF]. Substance Abuse and Mental Health Services Administration. 2016.
- Frigerio S, Strawbridge R, Young AH. The Impact of Caffeine Consumption on Clinical Symptoms in Patients With Bipolar Disorder: A Systematic Review. Bipolar Disorders. May 2021.
- Rusner M, Berg M, Begley C. Bipolar Disorder in Pregnancy and Childbirth: a Systematic Review of Outcomes. BMC Pregnancy and Childbirth. October 28, 2016.
- Perry A, Gordon-Smith K, Di Florio A, et al.
 Mood Episodes in Pregnancy and Risk of Postpartum Recurrence in Bipolar Disorder: The Bipolar Disorder Research Network Pregnancy Study. Journal of Affective Disorders. November 1, 2021.
Mood Episodes in Pregnancy and Risk of Postpartum Recurrence in Bipolar Disorder: The Bipolar Disorder Research Network Pregnancy Study. Journal of Affective Disorders. November 1, 2021. - Fisher SD. Paternal Mental Health: Why Is It Relevant? American Journal of Lifestyle Medicine. May–June 2017.
Show Less
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.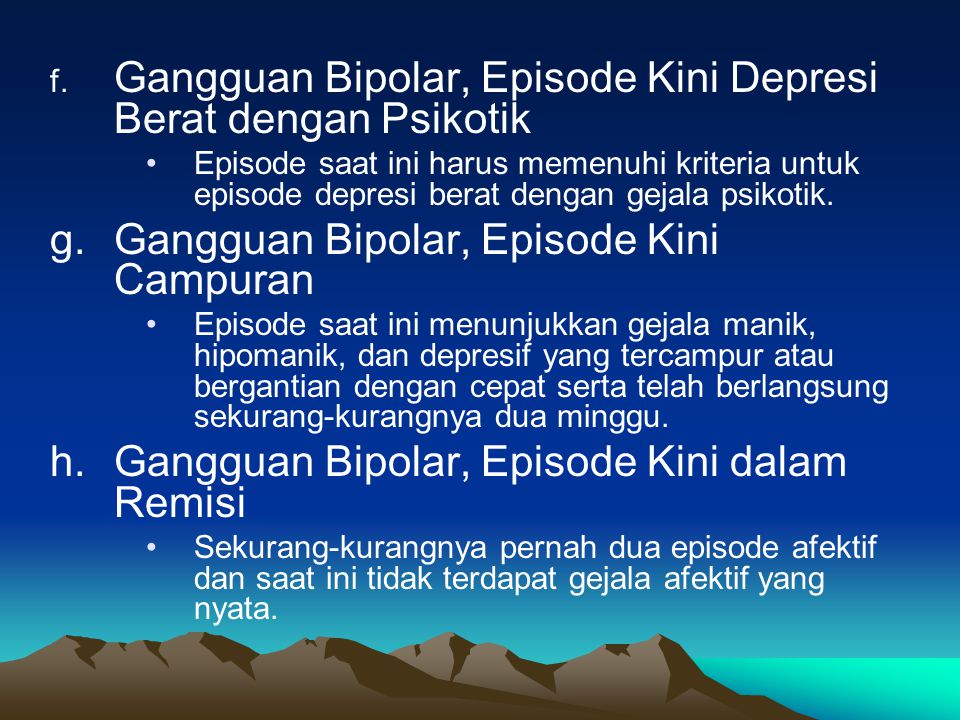
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. They may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
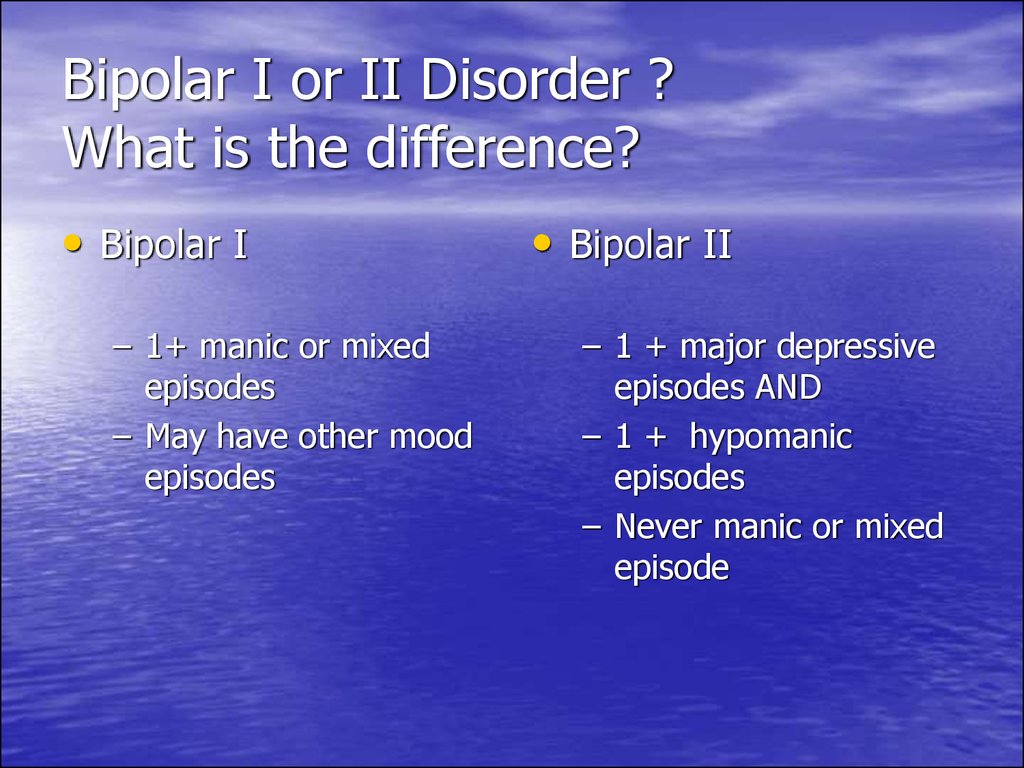
- Bipolar disorder I. You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
- Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.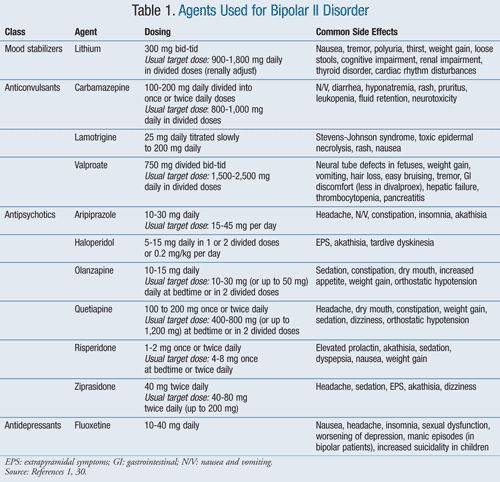
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others. The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships.
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Bipolar disorder - causes and signs, diagnosis and treatment
Bipolar disorder is a psychopathological disease that manifests itself with sudden changes in mood, alternating episodes of mania and depression. Relapses last weeks and months. Manic-depressive psychosis, as the disease was previously called, if left untreated, can destroy a career, family relationships, and in especially severe cases, lead to suicide.
Relapses last weeks and months. Manic-depressive psychosis, as the disease was previously called, if left untreated, can destroy a career, family relationships, and in especially severe cases, lead to suicide.
The pathological condition occurs with the same frequency in both sexes, the peak falls on the most active age of 15-25 years. Episodes respond well to medication and psychotherapy.
Bipolar personality disorder: symptoms and signs
Mental illness occurs with the change of 2 affective states - depression and mania, which in many manifestations are opposite to each other. The clinical picture depends on the phase of the course:
| Phase | Stages | Symptoms | Phase highlights |
| Manic includes 5 stages | Hypomanic | Increased emotional mood | Emotional instability |
| Sleep problems | |||
| Vigor physical and psychological | |||
| Severe mania | Continuous Jokes | Aggressive-irritable mood or euphoric mood | |
| Outbursts of anger | |||
| Sleep duration 4 hours | |||
| Lots of nonsense ideas | |||
| Manic frenzy | Incomprehensible speech | Sleep disorders - reduced need and duration | |
| Lots of jerky movements | |||
| Motor calming | Physical and mental activity is reduced | ||
| Reactive | Return to normal | ||
| Depression proceeds in 4 stages | Initial | Depression, bad mood | Oppressed, depressed mood |
| By the evening the condition improves | |||
| Sleep disorders | |||
| Growing depression | Increased anxiety | Decreased or absent appetite | |
| Mood deterioration | |||
| Decreased appetite, performance | |||
| Insomnia | |||
| Severe depression | Severe anxiety | Thoughts about the meaninglessness of life, feeling of uselessness | |
| Suicidal thoughts | |||
| Immobility | |||
| Reactive | Symptoms subside and go away |
Causes of bipolar disorder
The disease affects 1.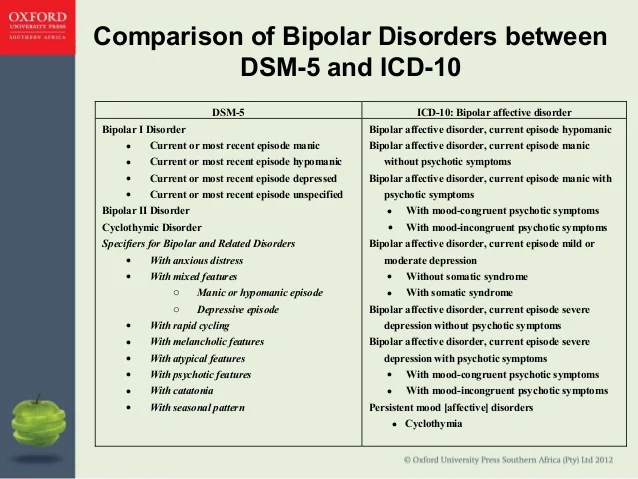 5 to 2.4% of the population. Scientists consider the connection of the disease with such provoking factors:
5 to 2.4% of the population. Scientists consider the connection of the disease with such provoking factors:
- genetic predisposition;
- head injury;
- hormonal imbalance;
- traumatic life events - severe stress, loss.
Motivation for treatment
24/7 emergency care
Top specialists
Quality assurance
Diagnosis of bipolar disorder
Modern flexible diagnostics at the Profi-Detox clinic is the first decisive step on the way to full recovery. With any treatment, specialists begin with a careful thoughtful study of the symptomatic picture, a careful questioning of the patient, and, if necessary, his relatives.
At this stage, the ability of professionals to ask the right questions and make decisions about the choice of tactics is indispensable. For such cases, experienced doctors work in the clinic: a psychiatrist, a neuropathologist, a psychologist, an endocrinologist, a therapist.
To rule out organic pathology, the clinic conducts:
- laboratory tests;
- instrumental diagnostics;
- diagnostic imaging.
Free consultation
+38 (067) 126 04 04
How is bipolar disorder treated?
Patients with bipolar disorder require mandatory medical attention. Since in its absence, an attack of mania or depression can drag on for up to a year or more. In "Profi-Detox" preference is given to proven, modern methods.
The combination of drug therapy with psychotherapeutic and physiological effects is the most effective. Fortunately, bipolar disorder responds well to treatment, and patients return to a productive life within 1-3 months.
In our clinic, the doctor works with the patient individually and chooses specific regimens, timing of medication and dosage. As a rule, the course may include:
- mood stabilizers;
- antidepressants;
- antipsychotics;
- anticonvulsants.
Patient transfer
We arrive at the address within 45 - 60 minutes.
Free consultation
Call and ask any question.