What to do if someone is having a psychotic break
What to Do if a Family Member or Friend Has Psychotic Symptoms
If someone you care about is displaying psychotic symptoms, it can be frightening. Psychosis is a mental state characterized by a break from reality, and it can include delusions or hallucinations. It’s a symptom of serious mental illness, including schizophrenia and bipolar disorder.
Often, the ill person is unaware that the symptoms are unusual or that he or she should seek help. That’s where family members and friends often come in, though the experience can be distressing for them as well.
It’s important to seek help from a mental health professional to deal with psychotic symptoms because early treatment can improve outcomes long term.
Identifying Early Psychotic Symptoms
The earliest phase of a psychotic disorder consists of nonspecific symptoms that can be difficult to recognize as serious, says Karen Graham, MD, medical director at OASIS, a clinic in the Department of Psychiatry at the UNC School of Medicine that treats young people with psychotic disorders and those who are at high risk of developing them. “Many of these symptoms might just seem like fairly typical behavior, especially in teenagers,” Dr. Graham says.
These symptoms include:
- Moodiness
- Sleep difficulty
- Poor performance in school
- Social withdrawal
- Lack of interest
- Lack of enjoyment
Many things can cause these symptoms, including depression, anxiety, drug use, trauma, bullying or teenage angst. But Dr. Graham says “if these symptoms progress to unusual experiences such as thinking others can read your mind, paranoia, misperceiving events, or hearing and seeing things, then the likelihood that the person is developing a psychotic disorder goes up.”
When a teen or young adult withdraws socially, starts to fail at school or work, begins to use drugs or displays other unusual behavior, it’s worth pursuing a mental health evaluation. A good place to start is with your family doctor, the OASIS program or another local mental health center.
Emergency Psychiatric Help for Psychotic Symptoms
Under certain circumstances, it’s important to seek emergency psychiatric help. You can look for signs such as:
You can look for signs such as:
- Expressing thoughts about suicide
- Hearing disturbing voices, especially voices that command suicide or injury to self or others
- Experiencing uncontrollable anxiety
- Exhibiting manic or otherwise bizarre behavior, severe depression, disorientation or extreme confusion
- Reacting unusually to psychiatric medication
- Feeling uncontrollable anger
If the person having these symptoms is already in treatment, contact the clinic or provider immediately. Most mental health centers have 24-hour emergency numbers; it may be a good idea to keep the number handy in case of a crisis.
If your loved one is not receiving psychiatric care and is having an emergency, call 911.
Preparing for Psychiatric Emergencies
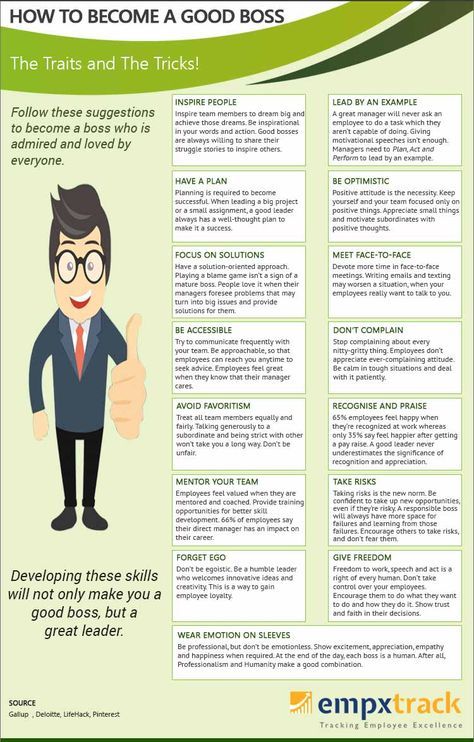
For people with severe and persistent mental illness, it can be helpful to have a plan of action in case of psychiatric emergencies. The person who is ill, family members and caregivers can create the plan together with guidance from a mental health professional.
The plan should allow the person with the illness, in consultation with family members and mental health professionals, to designate who can decide if hospitalization or emergency care is necessary. This allows the person with the illness to have input in the process in advance.
The plan should include:
- Emergency phone numbers
- List of medications the person is taking and their doses
- Name of the person’s doctor and case worker, therapist or counselor
- Insurance or related information
- Plan for notifying pertinent health care professionals
- List of family members or other caregivers who should be notified
What to Do if Someone with Psychotic Symptoms Refuses Treatment
Because schizophrenia and other psychotic disorders affect the brain, the person experiencing symptoms often doesn’t recognize them as being unusual and may refuse treatment. If symptoms aren’t too severe and the person refuses treatment, there may be nothing you can do but remain in contact and try to support the person.
Here are some ways to approach someone who refuses treatment:
- Be yourself. This will help the person trust you and perhaps listen to your suggestions.
- Give yourself and the person emotional and physical space. Avoid touching the person without permission, even to give comfort. If the person becomes hostile or aggressive, suggest a cooling-off period, emphasizing that you plan to return to the issue at hand when everyone is calmer. Leave yourself an avenue of escape if the person is agitated.
- Calmly but firmly suggest that you take the person to see a doctor, therapist, case worker or counselor for evaluation. Don’t confront refusals or argue, but rather continue to listen and reiterate your suggestion. It may help to sit or stand beside the person while discussing this, rather than be face-to-face.
- Go with the person to the doctor or mental health center to provide information about when the symptoms started and what medications the person is taking, and to answer any other questions.
 In a crisis, the ill person may not be able to answer these questions clearly, so your input is valuable.
In a crisis, the ill person may not be able to answer these questions clearly, so your input is valuable.
If the person threatens violence or becomes violent, especially if there’s a history of violence, get help from the police as necessary. Remember that your loved one’s illness may cause him or her to act in a way that doesn’t reflect his or her true feelings or wishes.
Involuntary Commitment
In very serious episodes of mental illness, a person may need to be committed involuntarily to a hospital or mental institution.
To involuntarily commit someone in North Carolina, it must be clear that the person is mentally ill and a danger to self or others. “Danger to self or others” includes threats of suicide or suicidal gestures or plans, significant self-injury, threats of violence to others or behaviors that cause harm to others or to property, and a lack of self-care so serious and persistent that injury or disease is likely to result.
If someone displays these behaviors and refuses to seek care, another person may petition the local magistrate for psychiatric evaluation. This involves signing a legal document stating the facts that indicate the person is mentally ill and a danger to self or others. The affidavit must be filed in the magistrate’s office, usually in a local jail. If the magistrate determines there are reasonable grounds for psychiatric evaluation, a custody order will be issued and a law enforcement officer will pick up and transport the person to a mental health center or hospital for examination.
This involves signing a legal document stating the facts that indicate the person is mentally ill and a danger to self or others. The affidavit must be filed in the magistrate’s office, usually in a local jail. If the magistrate determines there are reasonable grounds for psychiatric evaluation, a custody order will be issued and a law enforcement officer will pick up and transport the person to a mental health center or hospital for examination.
If the examining physician recommends inpatient care, the law enforcement officer will take the person to a local psychiatric unit or the state psychiatric hospital, where a second physician will perform an examination and may recommend involuntary commitment. The patient has a right to a court hearing within 10 days and the right to an attorney. The hearing is closed to the public, and court records are kept confidential. If the judge decides the person who was hospitalized does not meet standards for inpatient commitment, the person will be discharged from the hospital, though the judge could still order outpatient commitment.
If you are concerned someone is showing signs of a psychotic disorder, you can call OASIS for advice, or a psychiatric evaluation if appropriate, at (919) 962-1401.
When You Should Call Your Doctor or 911
Written by WebMD Editorial Contributors
If someone you love has schizophrenia, knowing when to call the doctor isn’t always easy -- and you can’t always rely on your loved one to let you know they need help.
During a psychotic episode, they may not know the difference between what’s real and what isn’t. They could see and hear things that aren’t there (hallucinations) or believe something is controlling their thoughts (delusions). They might even think that you’re plotting against them.
This can be scary and upsetting. But stay calm, trust your intuition, and remember that professional help is within reach.
When Should You Call the Doctor?
Most of the time your loved one won’t suddenly lose complete control of themselves. You’ll probably notice signs leading up to a psychotic episode.
Symptoms vary, but there are some common ones, including:
- Mistrustful or suspicious beliefs or ideas
- Unexpected outbursts
- Isolation from friends and family
- Noticeable mood changes
- Trouble sleeping
- Bizarre behavior
Call your doctor for advice if your loved one’s mood changes or their thinking seems unusual. If they have stopped taking their medication, but doesn’t seem like they are going to hurt you or anyone else, encourage them to visit the doctor with you.
Additional resources that are helpful include the National Alliance for the Mentally Ill (NAMI) https://nami.org/Home or the Substance Abuse and Mental Health Services Administration (SAMHSA) https://www.samhsa.gov/.
When to Call 911 Instead
If you’re afraid help from your doctor isn’t going to be fast enough, you may need call to 911. To decide when you should call for help, ask yourself these questions:
- Is your loved one threatening to harm themselves or someone else, including you?
- Have they ever attempted suicide before?
- Are they unable to feed or dress themselves?
- Are they living on the streets?
If you answered “yes” to any of these, call 911 or a local emergency number. Some county health departments have crisis units that can assist during a mental health emergency. Don’t try to solve the situation on your own or put yourself at risk.
Some county health departments have crisis units that can assist during a mental health emergency. Don’t try to solve the situation on your own or put yourself at risk.
If you think there’s any chance that they will try to commit suicide, ask someone to stay with them while you call for emergency help.
When to Ask for the Police
Most people with schizophrenia are not violent. But just like you would in any other situation, if you’re scared for your safety, immediately call 911 and ask the dispatcher for the police.
Tell them that your loved one is psychotic, and explain you need help controlling their behavior and getting them medical treatment. Ask the police not to show any weapons when they arrive so they don’t alarm them more.
If possible, someone should stay with you while you wait. And you should also call their doctor right away.
No matter what, remember that you and your loved one deserve to get the help you need quickly, so you can get back on track with their wellness plan.
Nervous breakdown - what it is, causes, symptoms, treatment
Everyone faces stress, but for some people it can develop into a nervous breakdown. What is a nervous breakdown, why does it occur and how does it manifest itself? Especially for Forbes Life, clinical psychologist, co-founder of the YouTalk service Anna Krymskaya talks about the causes, symptoms and consequences of this condition
What is a nervous breakdown
Finished reading here
In the past, the term "nervous breakdown" was often used to refer to various mental disorders, but today there is no such diagnosis in medicine, and a nervous breakdown is not considered a mental illness. The terms “nervous breakdown”, “nervous breakdown” or “emotional breakdown” often describe a condition where a person cannot cope with stress, anxiety and anxiety on their own, cannot function normally in everyday life.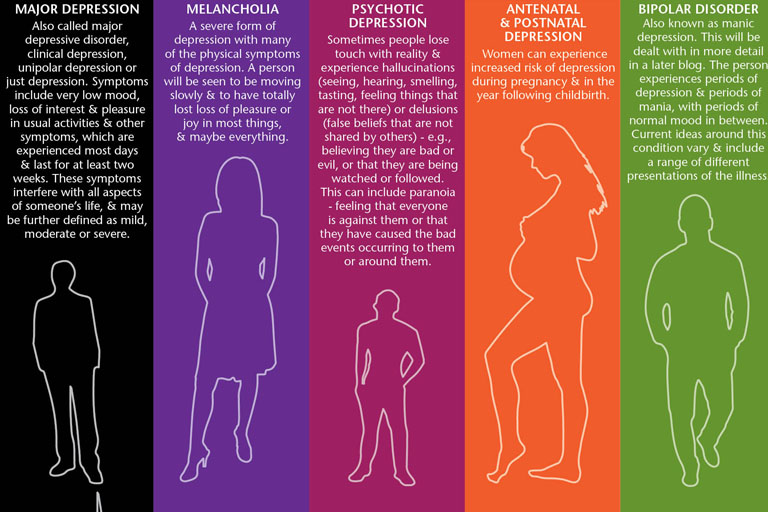
Causes of a nervous breakdown
Although a breakdown is not a mental illness, any other disorder such as PTSD, depression, borderline personality disorder, or etc.), can provoke a breakdown.
Chronic stress can also cause a nervous breakdown, for example, caused by a series of financial difficulties, problems at work and in personal relationships. At risk are people who do not have stress tolerance skills and reliable social support.
You can prevent stress from escalating into a nervous breakdown by “catching” your condition a few weeks before the crisis point
How to understand that you have a nervous breakdown
The signs of a nervous breakdown vary from person to person and depend on the cause. Each organism reacts in its own way. Some symptoms are related to mental state, well-being and changes in behavior. However, physical symptoms are also possible.
Each organism reacts in its own way. Some symptoms are related to mental state, well-being and changes in behavior. However, physical symptoms are also possible.
Psychological symptoms of a nervous breakdown can manifest themselves as:
- acute anxiety that the person cannot cope with on their own;
- a feeling of detachment and disinterest in communicating with friends and relatives, doing the usual things;
- inability to focus and make decisions;
- mood swings - feeling of depression, emotional burnout, outbursts of uncontrollable anger and fear, feeling of helplessness, sobbing and hysteria;
- depersonalization - a state when a person does not feel himself;
- isolation from reality — a person does not distinguish between reality and imagination;
- as well as hallucinations, paranoia (the feeling that someone is watching you), suicidal thoughts and self-harm attempts.

Related material
Physical symptoms include insomnia and restless sleep, fatigue and exhaustion up to the inability to do even normal daily activities, frequent colds, digestive disorders. As well as such physiological manifestations as heart palpitations, discomfort in the chest, a feeling of a coma in the throat, which seems to make it harder to breathe - that is, signs of a panic attack. Some of the symptoms of a nervous breakdown are similar to those of burnout, a state of mental and emotional exhaustion that is often the result of chronic workplace stress.
Photo by Mikhail Nilov PexelsTreatment of a nervous breakdown
There is no universal answer to the question of how to treat a nervous breakdown. Depending on the situation and diagnosis, both a psychiatrist and a psychologist will help to cope with a nervous breakdown - these specialists have a different profile of work, often in the event of a nervous breakdown, the support of both is needed.
A psychiatrist specializes in diagnosing depression, generalized anxiety disorder, post-traumatic disorder and other conditions. If some mental disorder has become the basis for a nervous breakdown, medications can help treat it. Antidepressants and anti-anxiety medications are usually prescribed, but other medication options are available depending on the condition.
Diet, physical activity, and some simple habits can help you through a stressful period.
In terms of psychological help, cognitive behavioral therapy (CBT) is considered the most effective for nervous disorders. This approach helps to identify errors and false attitudes in thinking and interpreting life events, it works effectively for a specific task and in short-term therapy, for example, within 20 sessions. CBT is an important mechanism for the treatment of anxiety disorders of various nature. For a nervous breakdown, cognitive behavioral therapy may include homework, journaling to analyze experiences that occur during the day, refocusing, relaxation, and mindfulness techniques, as well as exposure (intentional encounters with frightening situations in order to reduce fear) and rational-emotive role-playing games. A psychologist should be able to ask open-ended questions correctly, show empathy and give a person the necessary tools that will help them to help themselves in the future.
CBT is an important mechanism for the treatment of anxiety disorders of various nature. For a nervous breakdown, cognitive behavioral therapy may include homework, journaling to analyze experiences that occur during the day, refocusing, relaxation, and mindfulness techniques, as well as exposure (intentional encounters with frightening situations in order to reduce fear) and rational-emotive role-playing games. A psychologist should be able to ask open-ended questions correctly, show empathy and give a person the necessary tools that will help them to help themselves in the future.
What to do to avoid a nervous breakdown
You can prevent stress from developing into a nervous breakdown if you “catch” your condition a few weeks before the crisis point. Try not to overload yourself, find time to replenish resources and slow down.
Some simple habits can help you through stressful times. All of them are quite simple, but proven effective. Try to eat a balanced diet that energizes. The diet should be varied, it is worth removing coffee, alcohol and other stimulants from the diet to reduce anxiety and improve sleep. Do not forget about regular physical activity - it can even be small daily walks.
All of them are quite simple, but proven effective. Try to eat a balanced diet that energizes. The diet should be varied, it is worth removing coffee, alcohol and other stimulants from the diet to reduce anxiety and improve sleep. Do not forget about regular physical activity - it can even be small daily walks.
Related material
Relaxation techniques and breathing practices also show high efficiency in dealing with stress. For example, you can use a visualization technique where you create a mental image of a place that calms you, or muscle relaxation, where you first tense and then relax different muscle groups. Try focusing on deep, slow breathing: inhale through your nose for 4 seconds, hold your breath for 7 seconds, and exhale through your mouth for 8 seconds.
If you have a nervous breakdown, you are in a critical condition and urgently need help, you can contact one of these organizations:
+7 (800) 2000-122 - a helpline for children, adolescents and their parents.
+7 (499) 216-50-50 - emergency psychological assistance.
+7 (499) 901-02-01 - assistance to survivors of sexual violence.
+7 (495) 916-30-00 - assistance to survivors of domestic violence (the Violence.net Center is recognized in Russia as a foreign agent).
+7 (800) 101-65-47 - hotline for men.
Postpartum depression
Page 2 of 7
At least one in 10 mothers suffers from postpartum depression. It is one of the most frequent postpartum complications and occurs in 10-13% of women in labor. As a rule, in such cases it is not always possible to make a correct diagnosis, because mothers are reluctant to seek medical help. Psychotic states in the postpartum period occur in no more than 0.1-0. 3% of cases. That is, out of every thousand women who give birth, from 1 to 3 suffer from an even more severe form of depression - postpartum psychosis, in which a woman develops delusions or hallucinations, often accompanied by an obsession with harming herself or the child. The psychotic state significantly impairs the woman's ability to function naturally in family and social life, and also poses a significant risk of committing a suicide attempt. In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
3% of cases. That is, out of every thousand women who give birth, from 1 to 3 suffer from an even more severe form of depression - postpartum psychosis, in which a woman develops delusions or hallucinations, often accompanied by an obsession with harming herself or the child. The psychotic state significantly impairs the woman's ability to function naturally in family and social life, and also poses a significant risk of committing a suicide attempt. In most cases, the postpartum psychotic state requires urgent hospitalization of the patient. Early postpartum depression develops in the first days or weeks after childbirth, and usually lasts from a week to a month. Late postpartum depression usually develops several months after pregnancy. Its duration can be different, but more often it lasts more than a month.
Most often, depression appears 30-35 days after birth and in some cases can last up to 1.5-2 years. However, in most cases, a depressive episode ends spontaneously safely 3-6 months after birth. Symptoms of postpartum depression meet the diagnostic criteria for depressive disorder. The patient has a deterioration in mood, a decrease in energy, activity, the ability to rejoice, have fun, a decrease in interests and difficulty in long-term concentration of attention. Severe fatigue is common, even after minimal effort. As a rule, sleep is disturbed and appetite worsens. Self-esteem and self-confidence are almost always reduced, even in mild forms of the disease. Often there are thoughts of one's own guilt and uselessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.
Symptoms of postpartum depression meet the diagnostic criteria for depressive disorder. The patient has a deterioration in mood, a decrease in energy, activity, the ability to rejoice, have fun, a decrease in interests and difficulty in long-term concentration of attention. Severe fatigue is common, even after minimal effort. As a rule, sleep is disturbed and appetite worsens. Self-esteem and self-confidence are almost always reduced, even in mild forms of the disease. Often there are thoughts of one's own guilt and uselessness. Low mood, which varies little from day to day, does not depend on circumstances and may be accompanied by symptoms such as loss of interest in the environment and the loss of sensations that give pleasure. Typical is awakening in the morning several hours earlier than usual, increased depression in the morning, severe psychomotor retardation, anxiety, loss of appetite, weight loss and decreased libido.
In most cases, postpartum depression remains unrecognized in the initial period.