Abuse and eating disorders
The Connection Between Eating Disorders and Sexual Violence
Like sexual violence, all forms of disordered eating (such as anorexia, bulimia, and binge eating disorder) can affect anyone at any age. Also like sexual harassment, assault, and abuse, it is critical to combat the stigma, silence, and shame around eating disorders by bringing these issues into the light, acknowledging they are widespread, and uplifting that no one should have to struggle alone. In honor of National Eating Disorder Awareness Week, we’re talking about the intersection of these two critical issues to help illuminate the reality that survivors of trauma including sexual harassment, assault, and abuse are more likely to struggle with eating disorders and other forms of disordered eating.
Why Is It Important?
Understanding the connection between sexual trauma and eating disorders is vital for those working with survivors of sexual assault and individuals recovering from an eating disorder. Offering meaningful support to survivors on their healing journey means seeing them as a whole person and understanding the many ways trauma impacts their daily lives. Similarly, treatment professionals in eating disorder recovery offer. Research finds trauma to be the single greatest factor in the perpetuation of harm and violence — be it sexual violence or disordered eating. Yet, it is still difficult for some to understand the connection between eating disorders and sexual violence. In honor of National Eating Disorder Awareness Week, we’re shining a light on the intersection of these two critical issues
It is important to understand the connection between sexual violence and eating disorders if someone you know is a survivor or struggling with food, exercise, or body image. I’ts also important for service providers to understand this connection in more effective support to survivors as when they recognize and acknowledge how unwanted sexual experiences and trauma can play an underlying role in the development of an eating disorder.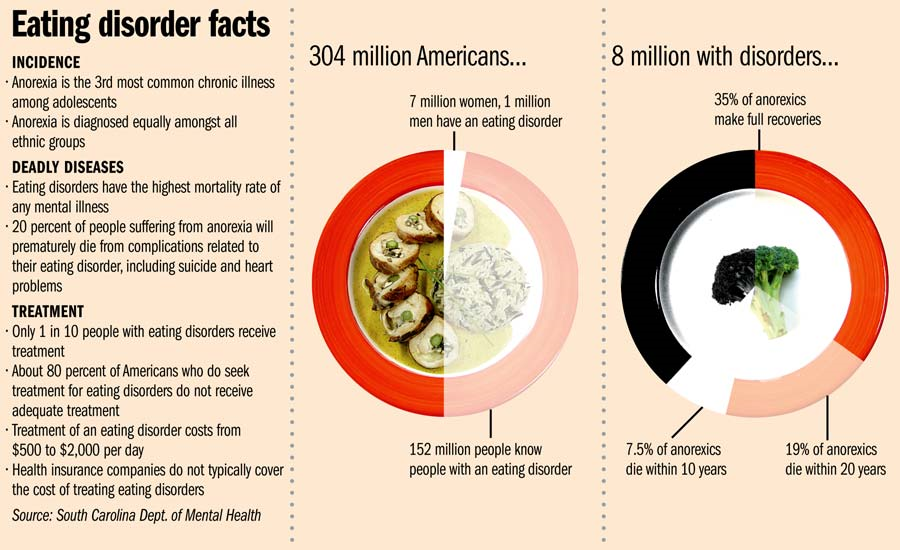 This understanding enables all of us to be more compassionate and supportive of those in our lives by recognizing that an eating disorder is never a choice. At times, there may be visible signs that someone in your life is struggling with an eating disorder, but many times, these behaviors may be hidden. Similarly, a friend or loved one may have disclosed to you their experiences as a survivor and asked for support, but many times, we don’t know the full extent of the struggles those in our lives are carrying. The first step to being able to offer meaningful support is by simply learning more about these issues.
This understanding enables all of us to be more compassionate and supportive of those in our lives by recognizing that an eating disorder is never a choice. At times, there may be visible signs that someone in your life is struggling with an eating disorder, but many times, these behaviors may be hidden. Similarly, a friend or loved one may have disclosed to you their experiences as a survivor and asked for support, but many times, we don’t know the full extent of the struggles those in our lives are carrying. The first step to being able to offer meaningful support is by simply learning more about these issues.
Understanding Eating Disorders
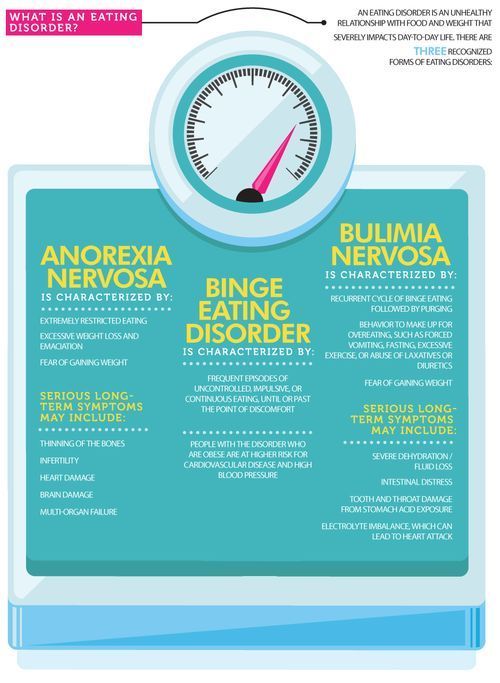
Eating disorders are characterized by extreme attitudes and behaviors surrounding weight and food. For instance, those suffering from bulimia cycle with binges followed by compensatory purging behaviors such as vomiting, abusing laxatives, and over-exercising. Most prevalent are eating disorder behaviors which do not meet the official criteria of any specific condition where an individual struggles with a combination of food restriction, binging, purging, over-exercising, experiencing negative body image and low self-esteem, and having an unhealthy obsession with otherwise healthy eating.
Eating disorders are complex struggles and, although they directly impact behaviors around eating and perceptions of the body, they are most often not directly about food or the desire to appear thinner. Rather, these behaviors serve as coping mechanisms and ways to manage difficult feelings and experiences. Just like sexual violence, eating disorders impact a person’s mental, emotional, and physical wellness. Similarly as with the shame of sexual violence, eating disorders are highly stigmatized and largely regarded to be a gendered issue when they affect all people, of all genders, of all social classes. According to research, “An estimated 10 million men and boys have a diagnosed eating disorder - about a third of all reported cases, according to the National Eating Disorder Association. Yet because the condition is largely seen as a women’s health problem, men often struggle to find help.”
The Connection Between Eating Disorders and Sexual Violence
Statistics indicate that many of the challenges survivors face place them at greater risk for developing an eating disorder and its related symptoms. Specialists call this relationship between eating disorders and sexual trauma “comorbity”— which is the presence of two underlying factors which commonly pair together. Disordered eating is often developed as a coping mechanism as a result of sexual traumas such as rape, molestation, harassment, and other forms of abuse. In fact, research shows that about 30% of patients dealing with disordered eating have also experienced sexual abuse in childhood.
Specialists call this relationship between eating disorders and sexual trauma “comorbity”— which is the presence of two underlying factors which commonly pair together. Disordered eating is often developed as a coping mechanism as a result of sexual traumas such as rape, molestation, harassment, and other forms of abuse. In fact, research shows that about 30% of patients dealing with disordered eating have also experienced sexual abuse in childhood.
Many who experience sexual trauma may develop a sense of disconnection from their body, or a desire to be cut off from their body and the overwhelming emotions they are experiencing. This may come in the form of body shame, hatred, or the urge to self-harm. Many victims and survivors describe feeling a lack of control in the aftermath of their experience of abuse. Controlling behaviors around food and exercise may suppress difficult emotions and provide a temporary sense of control. In these ways and many others, an eating disorder creates distance from painful, uncomfortable feelings and seeks to numb or avoid them.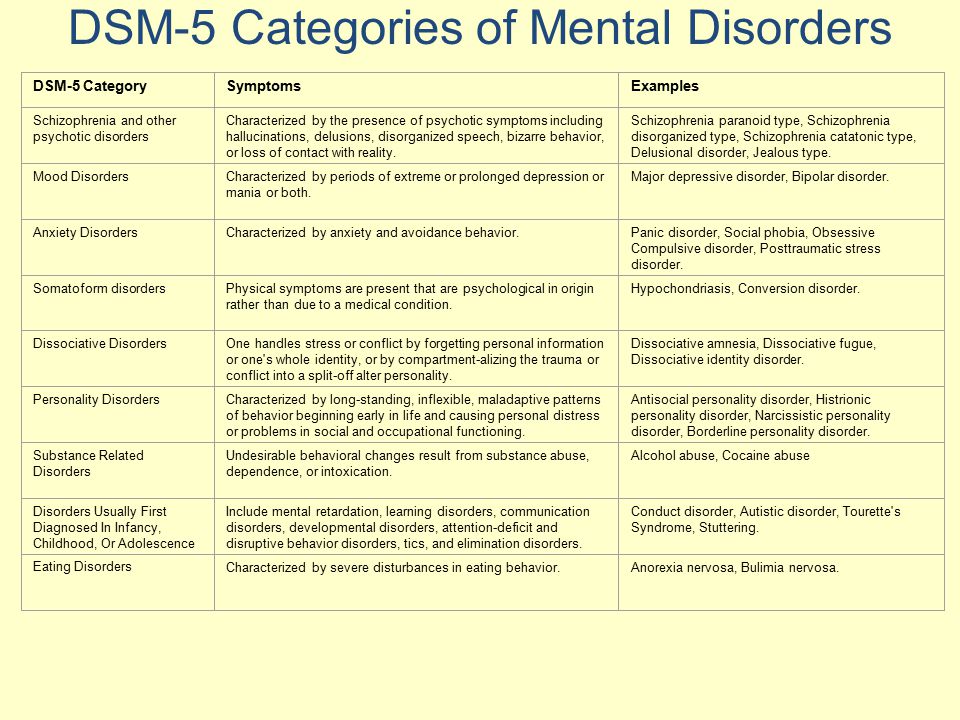
Although eating disorder thoughts and behaviors may be rooted in a desire to preserve and protect oneself, they cause further harm to the body, mind, spirit, and healing process. In fact, eating disorders have the highest mortality rate of any mental illness. Despite many underlying similarities, every survivor is impacted by sexual violence in their own way. People who have not experienced sexual trauma often underestimate the wide range of ways individuals are impacted in the short and long term. These include depression, anxiety, nightmares, flashbacks, chronic pain, substance use, and many other conditions.
Getting Help
If you or someone you know is struggling with an eating disorder, it’s important to know there is hope. Treatment is available and recovery is possible. The National Eating Disorder Association provides tools for help finding treatment; a network for friends, family, and parents; and tools for screening if you need professional help.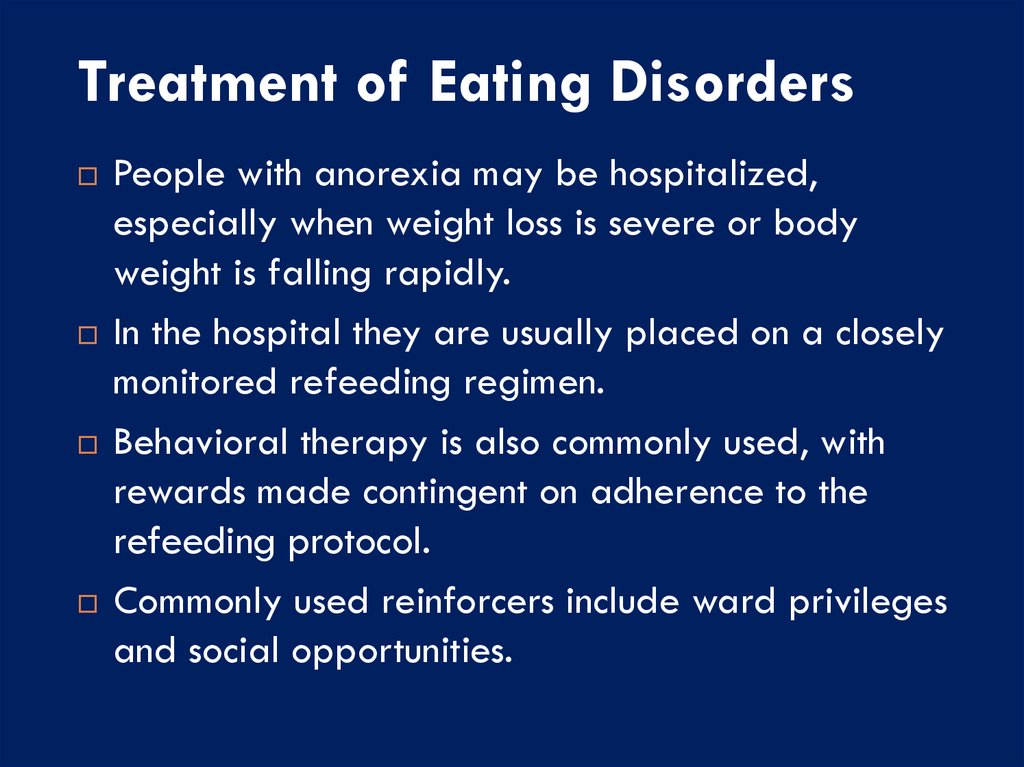
More Resource Hubs
The Eating Disorder Resource Center provides help to people affected by eating disorders through phone, e-mail, and in-person guidance. This includes education, treatment options, resources, and more.
70 Resources to Support Eating Disorder Recovery has organized an array of help topics, including COVID-19 resources, signs and symptoms of eating disorders, understanding different types of eating disorders, treatment and recovery options, free and low-cost resources, where to find a dietitian, where to find mental health counselor or therapists, support groups for eating disorders, books about eating disorder recovery, how to help someone with an eating disorder, and hotlines for immediate help.
Eating Disorder Hope has categorized a list of resources specifically for anorexia, bulimia, and binge eating disorder.
Eating Recovery Center hosts a list of recommended websites to help those with eating disorders and their loved ones find trauma-informed online spaces.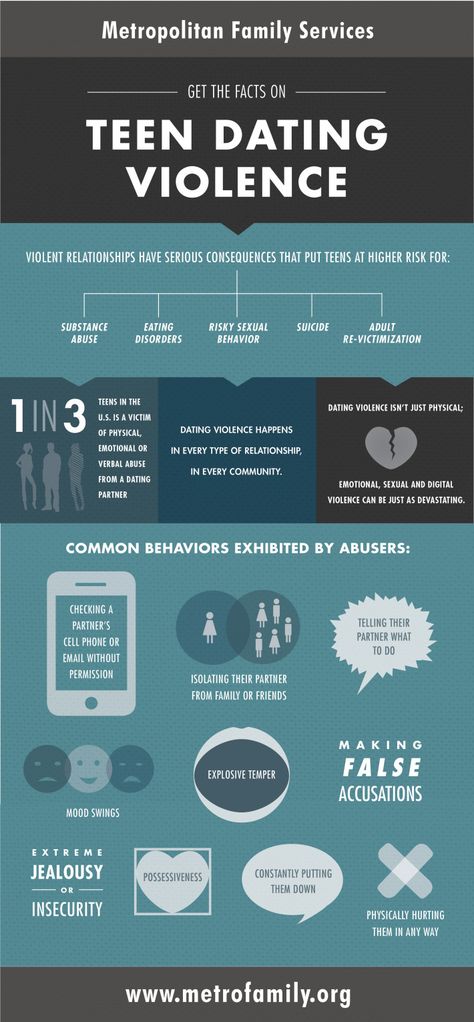
Eating Disorder Therapy LA includes a recommended reading and resource lists to supplement therapy and facilitate the healing process.
National Eating Disorders Collaboration is a treasure trove of great informational and support resources — including a podcast, infographics, publication lists, and more.
The Eating Disorder Foundation showcases a rolodex list of organizations that offer support to those experiencing disordered eating.
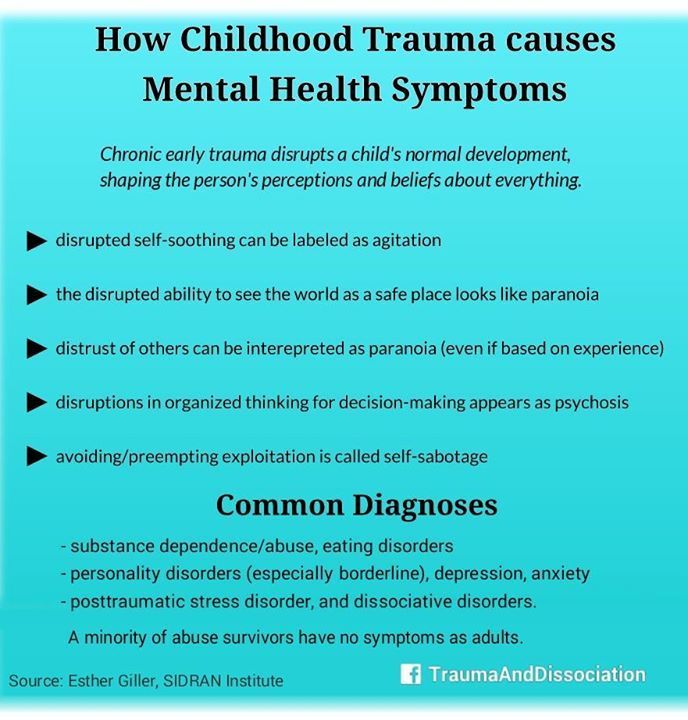
The Role of Childhood Trauma in Eating Disorders
This entry was posted in Youth Mental Health and tagged Childhood Trauma, Eating Disorders on by Cassandra Gibson-Judkins, LCSW.
Millions of people throughout the United States suffer from eating disorders such as Anorexia Nervosa, Binge Eating Disorder (BED), and Bulimia Nervosa. Though it affects both men and women, women are more likely to experience anorexia nervosa (75%) and binge eating disorders (60%).
Several factors can contribute to the onset of an eating disorder, such as genetics and family history. However, one of the most common factors linking eating disorders is a history of childhood trauma. Children who experience emotional, physical, or sexual abuse are more likely to develop psychological issues, including body image and eating disorders.
The Role of Childhood Trauma in Eating Disorders
The link between sexual abuse and eating disorders is well-documented and readily accepted by practitioners. Of particular note, however, is the evolving understanding of other trauma, such as physical and emotional abuse, and the role they can play in the development of an eating disorder. Emotional abuse, for example, can lead to low self-esteem, self-critique, and issues with body image. Eating disorders become a mechanism for maintaining control when a person feels like they none and serve as a way to avoid the emotional trauma head-on.
Trauma can be so severe that it actually disrupts the functioning of the nervous system, to the extent that it is difficult or impossible to regulate their own emotions. Negative behaviors such as binge eating or anorexia become coping mechanisms that keep trauma victims from processing difficult emotions. Much like Post Traumatic Stress Disorder (PTSD), dysregulation of the body’s psychobiological systems results from the exposure to childhood trauma.
Negative behaviors such as binge eating or anorexia become coping mechanisms that keep trauma victims from processing difficult emotions. Much like Post Traumatic Stress Disorder (PTSD), dysregulation of the body’s psychobiological systems results from the exposure to childhood trauma.
Emotional Abuse and Eating Disorders
Emotional abuse takes the form of continual criticism, insults, or attacks against a child’s character. Over time, these children internalize the criticism, perhaps even believing it to be true. This emotional abuse and its internalization makes children susceptible to eating disorders and dysfunctional behavior. Children who are emotionally abused are just as likely to develop eating disorders as those who experience physical or sexual abuse. A recent study explored the clinical linkages between eating disorders and emotional abuse, noting that emotional invalidation is a core component of the development of eating psychopathology. Emotional abuse poses large risk factors for later eating disorders by creating poor tolerance to distress, stymied emotional development, and problems with emotional inhibition.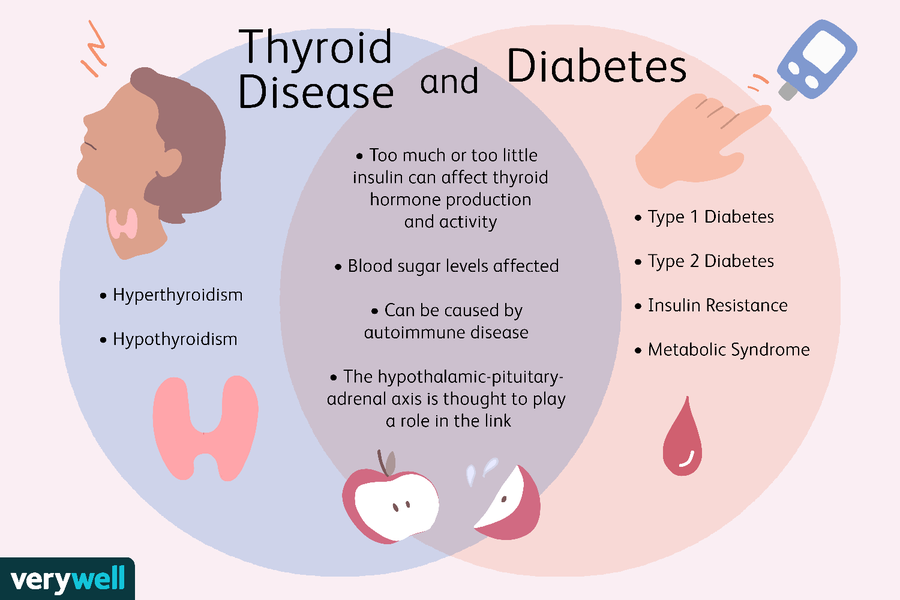 People who bear the brunt of repeated insults or excessive criticism, over time, develop similarly critical view of themselves, which leads to problems with body image that can manifest as anorexia, bulimia, or BED.
People who bear the brunt of repeated insults or excessive criticism, over time, develop similarly critical view of themselves, which leads to problems with body image that can manifest as anorexia, bulimia, or BED.
Sexual Abuse and Eating Disorders
The link between sexual abuse and the psychopathology of eating disorders has been extensively studied, but it is still subject to some debate. A recent review of the literature found that around 30% of eating disordered individuals sampled had experienced childhood sexual trauma or sexual abuse. There are complex associations between the type of trauma, inherent issues in self-regulation, and other risk factors that may make it difficult to pinpoint the exact effect sexual abuse has on the later risk of an eating disorder. Research does indicate, however, that people who experience sexual abuse are slightly more likely to develop bulimia nervosa than anorexia, BED, or other forms of disordered eating.
Some experts theorize that sexual abuse can cause a person to develop an eating disorder because they believe they need to look a certain way to be considered attractive.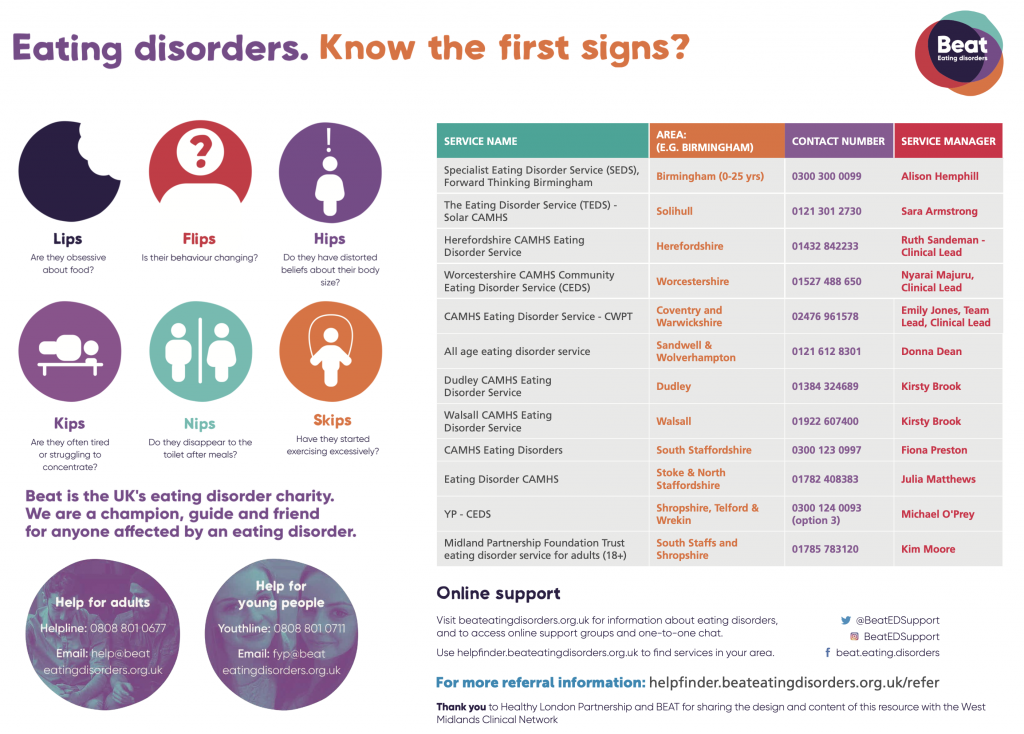 In this manner, a person can seemingly be in control of their lives, but also find an outlet for the emotional pain and turmoil of the sexual trauma.
In this manner, a person can seemingly be in control of their lives, but also find an outlet for the emotional pain and turmoil of the sexual trauma.
In the case of bulimia, there is an inherent symbolism in the etiology of the disorder. For example, bulimic behavior helps a person “purge” the negative feelings associated with the trauma while the food helps fill an emotional void. They both become coping mechanisms that help a person avoid the trauma of their experience; however, it does not provide the answer that the individual needs to heal.
Stress Eating As Disordered Behavior
Though not the same as traditional eating disorders, there has been interesting studies of stress eating and how it can develop in childhood as the result of trauma. For example, a study at the University College London of identical twins found that disordered eating patterns can begin as early as two years old not because of genetics but due to environmental factors. Even in cases where the parents were obese, emotional eating was driven by environment, not genes.
In the study, when confronting stress, some children went for a favorite snack, while others lost their appetite. The parents of the children recognized these behaviors as responses to being upset or anxious. The researchers noted that emotional undereating or overeating in childhood could set the stage for possible disordered eating later in life, when stress naturally increases. A similar study at Huntington University found that the higher the stress level, the more students were likely to eat.
Eating As an Addiction
Modern psychology considers both emotional eating and binge eating as addictive behaviors. Much like illicit drugs, a person who emotionally or binge eats gets a “high” from the experience from increased dopamine levels. Like illicit substances, a person who binge eats will want more or feel like it is never enough. This is called a process addiction: it is marked by a compulsive behavior that eventually becomes a health threat because it leads to obesity and all of its associated health risks.
Emotional eating and stress eating may not be officially designated disorders in the DSM 5, but they both have links to binge eating disorder and trauma. Both can evolve from low self-esteem and cycles of shame, guilt, and overeating. When emotional and binge eating disrupt daily functioning and life quality, it can become Binge Eating Disorder (BED)
Is There a Link Between Eating Disorders and PTSD?
Researchers have found an interesting link between Post Traumatic Stress Disorder (PTSD) and eating disorders. For example, women who present with eating disorders also show signs of PTSD or anxiety disorders as pre-existing or comorbid conditions. Often, the presence of trauma creates anxiety or PTSD, and the eating disorder emerges as a coping mechanism for those symptoms.
In fact, some research suggests that post-traumatic stress disorder can actually be a mediator between experiencing trauma and developing an eating disorder. For example, a National Women’s Study found than a high percentage or women who experienced an eating disorder also had a diagnosis of PTSD.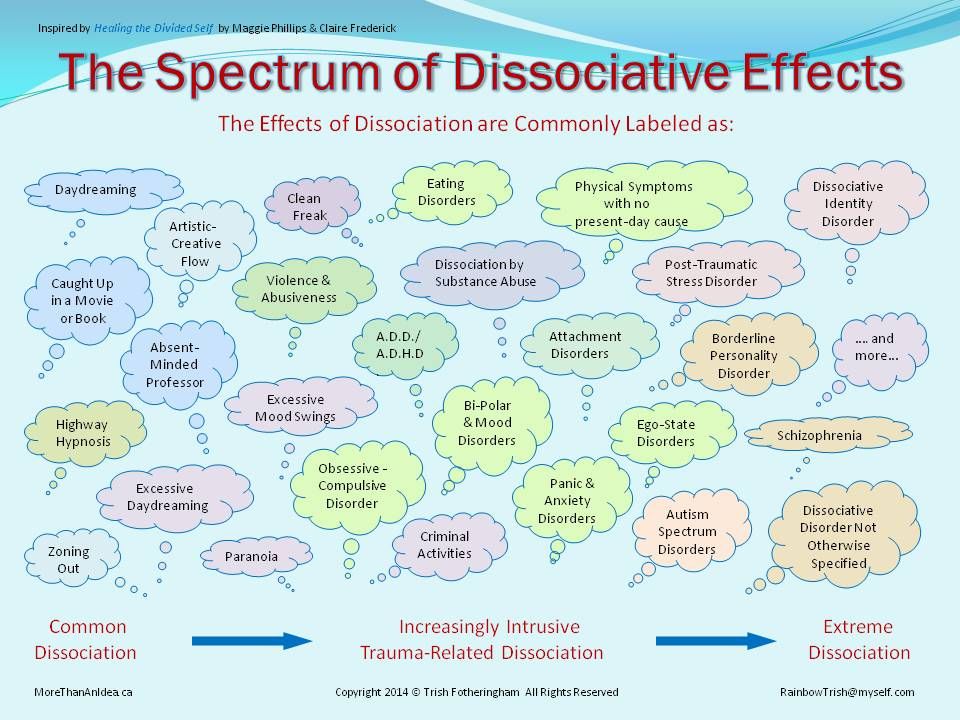 Many survivors of childhood trauma have at least some symptoms of PTSD, suggesting that they have subthreshold manifestations of the disorder.
Many survivors of childhood trauma have at least some symptoms of PTSD, suggesting that they have subthreshold manifestations of the disorder.
At a basic level, there are many commonalities between post-traumatic stress disorder and eating disorders. For example, people with either condition tend to be impulsive and may experience dissociation. It is important to note, however, that the method of dissociation may be different. Binging and purging is a method of dissociating from trauma, as is using illicit drugs or alcohol to escape.
How Eating Disorders Impact Mental Health
Eating disorders have obvious negative health effects. From a physical perspective, a person with an eating disorder may be at higher risk for:
- Obesity
- Malnutrition
- Conditions resulting from micronutrient deficiencies
- Osteoporosis
- Certain types of cancers (for example, esophageal cancer from purging)
Aside from the physical health issues, a person with an eating disorder often has a co-occurring mental health disorder. For example, a person with an eating disorder may have PTSD, depression, anxiety, or other dissociative pathology. To remove themselves even further from the trauma, it is not uncommon for a person with an eating disorder to also have a substance use disorder or alcohol use disorder.
For example, a person with an eating disorder may have PTSD, depression, anxiety, or other dissociative pathology. To remove themselves even further from the trauma, it is not uncommon for a person with an eating disorder to also have a substance use disorder or alcohol use disorder.
Unfortunately, the symptoms of an eating disorder closely mirror those of other disorders. It is essential for mental health professionals to uncover all possible co-occurring mental health and substance abuse issues in order to facilitate a long-term recovery.
Remember that an eating disorder is just one possible method for coping with the trauma of emotional, physical, or sexual abuse. A person may have several different unhealthy coping mechanisms that keep them from confronting the trauma of their childhood experience. Only by addressing the trauma in a healthy way can an individual affected by an eating disorder or co-occurring conditions expect to make a meaningful recovery.
How Can We Treat Eating Disorders?
Treatment of eating disorders is multifaceted. Because of the complex factors involved and the history of childhood trauma, a person cannot simply “stop” binge eating or other disordered eating behavior. Recovering from an eating disorder requires professional intervention, usually with a multidisciplinary team.
Because of the complex factors involved and the history of childhood trauma, a person cannot simply “stop” binge eating or other disordered eating behavior. Recovering from an eating disorder requires professional intervention, usually with a multidisciplinary team.
Eating disorder treatment usually begins at a primary care provider’s office. Often, the first step in receiving treatment is admitting that a problem exists. A primary care provider can help connect each individual with resources in the community, from mental health specialists to support groups that allow people to talk through their trauma.
Once connecting with a mental health specialist, the treatment for the eating disorder and any co-occurring mental health issues can begin. An integrated, trauma-informed approach is essential to facilitating a long-term recovery.
Any number of professionals may be involved in the treatment process for eating disorders: doctors and therapists can help manage the physical and psychological aspects of the disorder, while registered dieticians can provide advice about following a healthy lifestyle filled with enriching, good-for-you foods.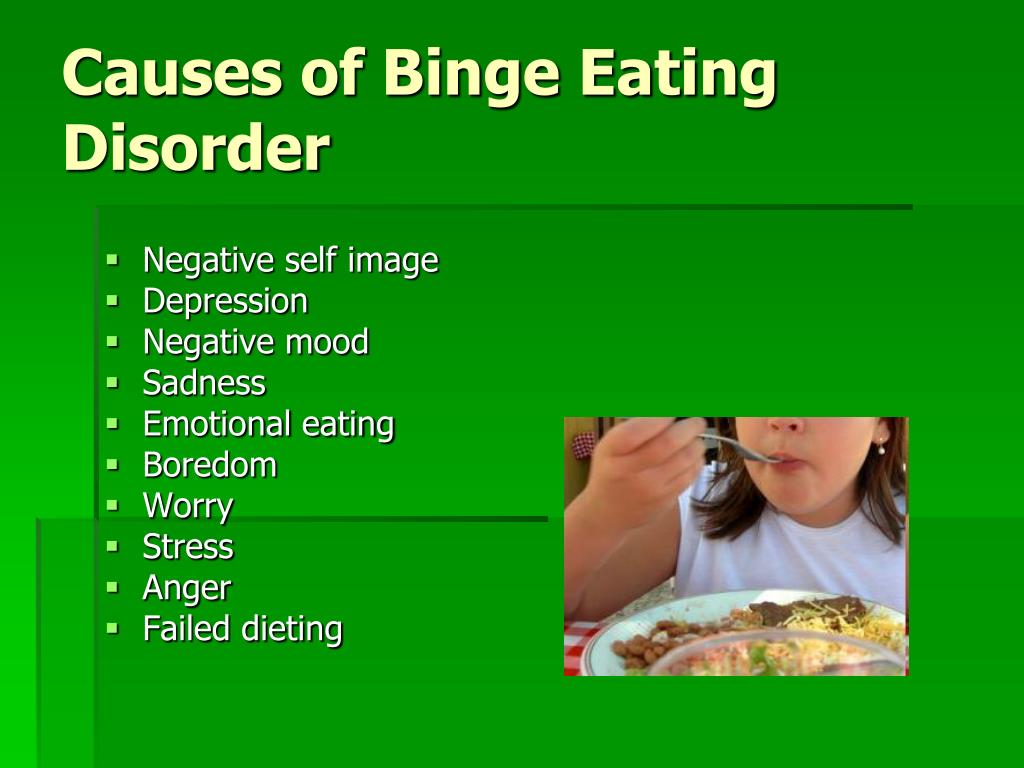 To help assure recovery continues for the long-term, ongoing support in the form of group therapy is essential.
To help assure recovery continues for the long-term, ongoing support in the form of group therapy is essential.
Specifically, the following interventions may be effective in treating eating disorders:
- Cognitive behavioral therapy (CBT). This evidence-based approach helps people challenge and overcome their distorted cognitive perceptions, thereby improving emotional regulation and helping people develop healthy coping mechanism for their problems.
- Residential/Inpatient Treatment. In many cases, inpatient treatment is necessary to help people initially break the cycle of shame and disordered eating.
- Dialectical Behavior Therapy. With a wide body of evidence for treating anorexia, bulimia, and BED, DBT also works to change maladaptive behaviors. Interventions focus on building mindfulness, reacting healthfully to distress, and regulating emotions.
- Support groups and outpatient settings. Ongoing support and safe spaces to talk about trauma and other triggers for disordered eating provides people with the tools they need to sustain recovery.
The Dangers of Untreated Eating Disorders
Eating disorders can be deadly without appropriate intervention. Anorexia, in particular, can kill a person affected due to cardiac arrhythmias, liver failure, kidney failure, and other consequences of malnutrition. A person with bulimia is at higher risk of developing certain types of cancer due to the amount of acid in the esophagus from purging. Obesity, a natural consequence of binge eating disorder, puts people at higher risk of heart attack, stroke, high blood pressure, and cancer.
Long Term Recovery from Eating Disorders
Treatment is available for eating disorders, and it can be incredibly effective. Understand, however, that eating disorders don’t “go away.” Due to their past history, a person recovering from an eating disorder is always susceptible to relapse. That is why it is so important for a person to understand the complex factors and triggers that contribute to their disorder.
Childhood trauma is a common thread in many people who experience eating disorders. On the other hand, it is usually only one facet of the condition. Other complex casualties, such as PTSD and other co-occurring mental health conditions, can also play a role in the development of disordered eating patterns.
On the other hand, it is usually only one facet of the condition. Other complex casualties, such as PTSD and other co-occurring mental health conditions, can also play a role in the development of disordered eating patterns.
Eating disorders can lead to negative physical and mental health effects. Left untreated, individuals experiencing eating disorders are at higher risk for a variety of illnesses and even death. Fortunately, effective treatments are available and consist of integrated psychotherapy, healthy diets, and medication. Mental health professionals, physicians, and peers can all play an integral role in supporting a person’s treatment and recovery.
A multidisciplinary team should use trauma-informed care and evidence-based treatments such as cognitive behavioral therapy or dialectical behavioral therapy in the treatment of eating disorders. After a person completes inpatient or intensive outpatient intervention, ongoing support in the form of group therapy is essential to support a long-recovery.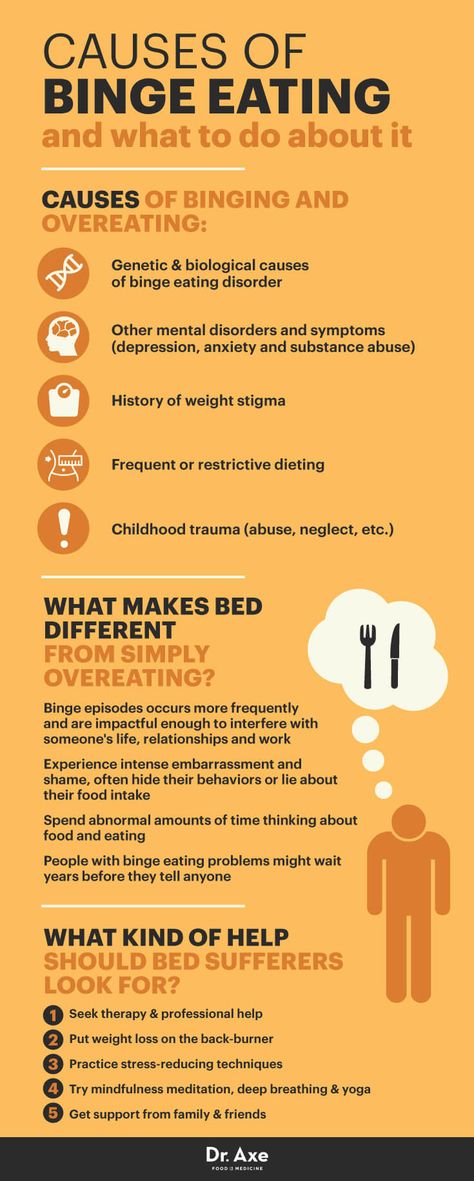 By addressing the underlying trauma and developing healthy coping mechanisms, a person with an eating disorder can overcome their obstacles and lead a healthy, happy life.
By addressing the underlying trauma and developing healthy coping mechanisms, a person with an eating disorder can overcome their obstacles and lead a healthy, happy life.
Cassandra Gibson-Judkins, LCSW
Assistant Executive Director
Cassandra Gibson-Judkins, Assistant Executive Director, is a licensed clinical social worker who has dedicated her career to providing services to children, youth and families. She has been a loyal employee at Eggleston since 1978. During her tenure at Eggleston, she has held numerous leadership positions in residential treatment, foster family, adoptions, and behavioral health program divisions. In addition, she served at the Department of Children and Family Services form 10 years, specializing in adoption services.
Eating problems
Eating behavior is the totality of our eating habits - our taste preferences, eating habits, diet, etc. Eating behavior depends on many factors - cultural, ethnic, family traditions and values, the characteristics of the upbringing and behavior of family members and the biological characteristics of the body, the standards and standards of norm and beauty that have developed in this society. These habits can change—and often change over time—but not all of these changes will be considered a painful eating disorder. The most obvious unhealthy eating behaviors include anorexia nervosa and bulimia .
These habits can change—and often change over time—but not all of these changes will be considered a painful eating disorder. The most obvious unhealthy eating behaviors include anorexia nervosa and bulimia .
Anorexia nervosa (lat. anorexia neurosa) (from other Greek ἀν- - “without-”, “non-” and ὄρεξις - “urge to eat, appetite”) - eating disorder , characterized by deliberate weight loss, caused and / or supported by the patient, in order to lose weight or to prevent weight gain. In anorexia, there is a pathological desire to lose weight, accompanied by a strong fear of obesity. The patient has a distorted perception of their physical form and there is a concern about weight gain, even if this is not actually observed. The overall prevalence of anorexia nervosa is 1.2% among women and 0.29% among men. About 90% of patients with anorexia are girls aged 12-24 years. The remaining 10% includes men and women of more mature age up to menopause.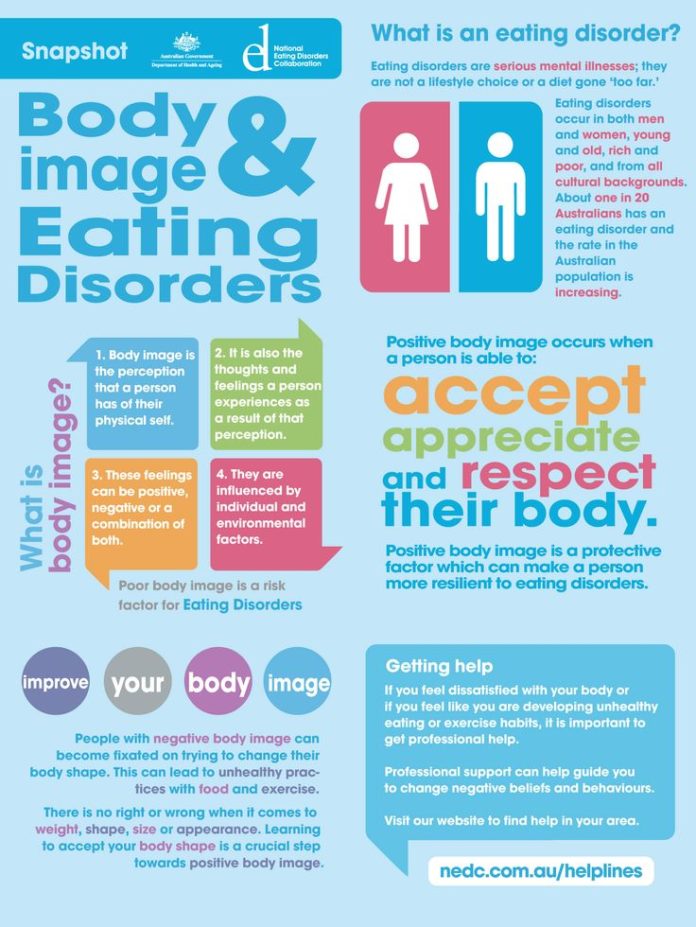
The causes of anorexia and bulimia are divided into biological, psychological (family influence and internal conflicts), and social (environmental influence: expectations, standards and standards of beauty, social stereotypes, diets). Biological factors - overweight and early onset of the first menstruation. In addition, the cause of the disease may lie in the dysfunction of neurotransmitters regulating eating behavior, such as serotonin, dopamine, norepinephrine. Family factors - More likely to develop an eating disorder in those who have relatives or loved ones suffering from anorexia nervosa, bulimia nervosa or obesity. Having a family member or relative with depression, alcohol or drug abuse or addiction, also increases the risk of an eating disorder. Personality factors - Psychological risk factors include perfectionism and obsessive personality, especially for the restrictive type of anorexia nervosa.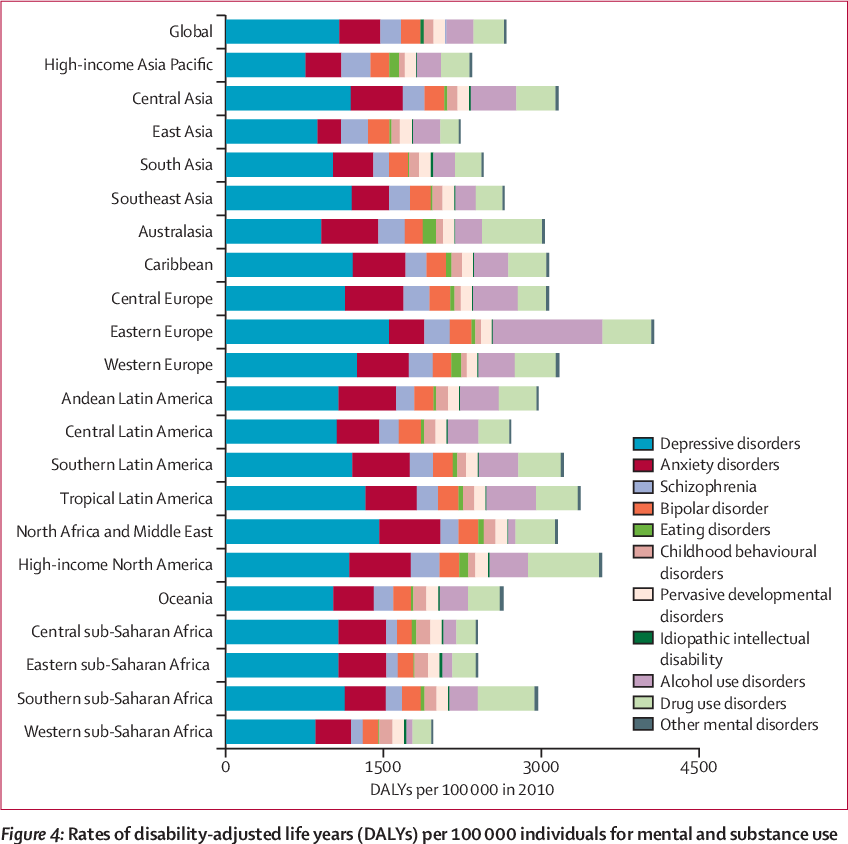 Low self-esteem and frustration tolerance, feelings of inferiority, insecurity and inadequacy are risk factors. Cultural factors - these include: living in an industrialized country and an emphasis on harmony (thinness) as an important and significant sign of female beauty. Stressful events, such as the death of a close relative or friend, or sexual or physical abuse, can also be risk factors for developing an eating disorder. The self-esteem of an anorexic patient depends on the figure and weight, and the weight is not assessed objectively, the perception of the norm is reduced inadequately. Losing weight is regarded as an achievement, weight gain is regarded as insufficient self-control. Such views persist even in the last stage (“my height is 170, weight 39kilogram, I want to weigh 30”).
Low self-esteem and frustration tolerance, feelings of inferiority, insecurity and inadequacy are risk factors. Cultural factors - these include: living in an industrialized country and an emphasis on harmony (thinness) as an important and significant sign of female beauty. Stressful events, such as the death of a close relative or friend, or sexual or physical abuse, can also be risk factors for developing an eating disorder. The self-esteem of an anorexic patient depends on the figure and weight, and the weight is not assessed objectively, the perception of the norm is reduced inadequately. Losing weight is regarded as an achievement, weight gain is regarded as insufficient self-control. Such views persist even in the last stage (“my height is 170, weight 39kilogram, I want to weigh 30”).
Stages of anorexia
- Dysmorphomanic — thoughts about one's own inferiority and inferiority predominate, due to imaginary fullness.
 Characterized by a depressed mood, anxiety, prolonged examination of oneself in the mirror. During this period, there are the first attempts to limit oneself in food, the search for the ideal diet.
Characterized by a depressed mood, anxiety, prolonged examination of oneself in the mirror. During this period, there are the first attempts to limit oneself in food, the search for the ideal diet. - Anorectic - occurs against the background of persistent starvation. A weight loss of 20-30% is achieved, which is accompanied by euphoria and a tightening of the diet, "to lose even more weight." At the same time, the patient actively convinces himself and those around him that he has no appetite and exhausts himself with great physical exertion. Due to a distorted perception of his body, the patient underestimates the degree of weight loss. The volume of fluid circulating in the body decreases, which causes hypotension and bradycardia. This condition can be accompanied by chilliness, dry skin, and even alopecia (baldness). Another clinical sign is the cessation of the menstrual cycle in women and a decrease in libido and spermatogenesis in men. Adrenal function is also impaired, up to adrenal insufficiency.
 Due to the active decay of tissues, appetite is additionally suppressed by intoxication of the body.
Due to the active decay of tissues, appetite is additionally suppressed by intoxication of the body. - Cachectic — period of irreversible dystrophy of internal organs. Comes in 1.5-2 years. During this period, weight loss reaches 50 percent or more of its mass. In this case, protein-free edema occurs, the water-electrolyte balance is disturbed, and the level of potassium in the body sharply decreases. This step is usually irreversible. Dystrophic changes lead to irreversible inhibition of the functions of all systems and organs and death.
Bulimia Nervosa (from other Greek βοῦς, bus - "bull" and other Greek λῑμός, limos - "hunger") (literally bullish hunger, kinorexia) - an eating disorder characterized by a sharp increase in appetite (wolfish appetite), usually coming in the form of an attack and accompanied by a feeling of excruciating hunger, general weakness, sometimes pain in the epigastric region. This violation of eating behavior is manifested mainly by recurring bouts of gluttony, food "spree".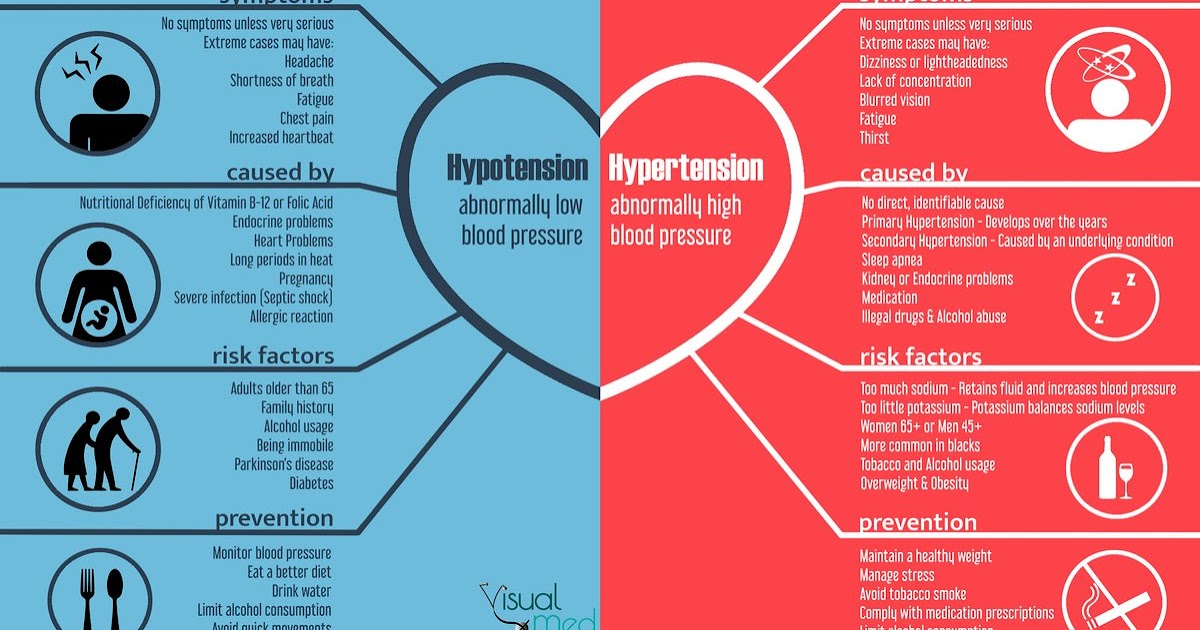 To avoid obesity, most patients with bulimia at the end of the "revelry" resort to one or another method of cleansing the stomach and intestines, artificially inducing vomiting in themselves or taking laxatives and diuretics. Others use excessive exercise or intermittent fasting. Like those with anorexia nervosa, most bulimics are young women, usually in their late teens and early 30s. Bulimics often look normal and healthy on the outside, but are usually overly demanding of themselves and others, prone to loneliness and depression. They tend to raise standards and lower self-esteem. Their life is almost entirely focused on food, their own figure and the need to hide their "mania" from others. Even when working or attending school, they usually shun society. Bulimia can be indicated by depression, poor sleep, talk of suicide, excessive fear of gaining weight, and frantic grocery shopping. Typically, bulimics have "bouts" about 11 times a week, but the frequency of such attacks varies from 1-2 per week to 4-5 per day.
To avoid obesity, most patients with bulimia at the end of the "revelry" resort to one or another method of cleansing the stomach and intestines, artificially inducing vomiting in themselves or taking laxatives and diuretics. Others use excessive exercise or intermittent fasting. Like those with anorexia nervosa, most bulimics are young women, usually in their late teens and early 30s. Bulimics often look normal and healthy on the outside, but are usually overly demanding of themselves and others, prone to loneliness and depression. They tend to raise standards and lower self-esteem. Their life is almost entirely focused on food, their own figure and the need to hide their "mania" from others. Even when working or attending school, they usually shun society. Bulimia can be indicated by depression, poor sleep, talk of suicide, excessive fear of gaining weight, and frantic grocery shopping. Typically, bulimics have "bouts" about 11 times a week, but the frequency of such attacks varies from 1-2 per week to 4-5 per day.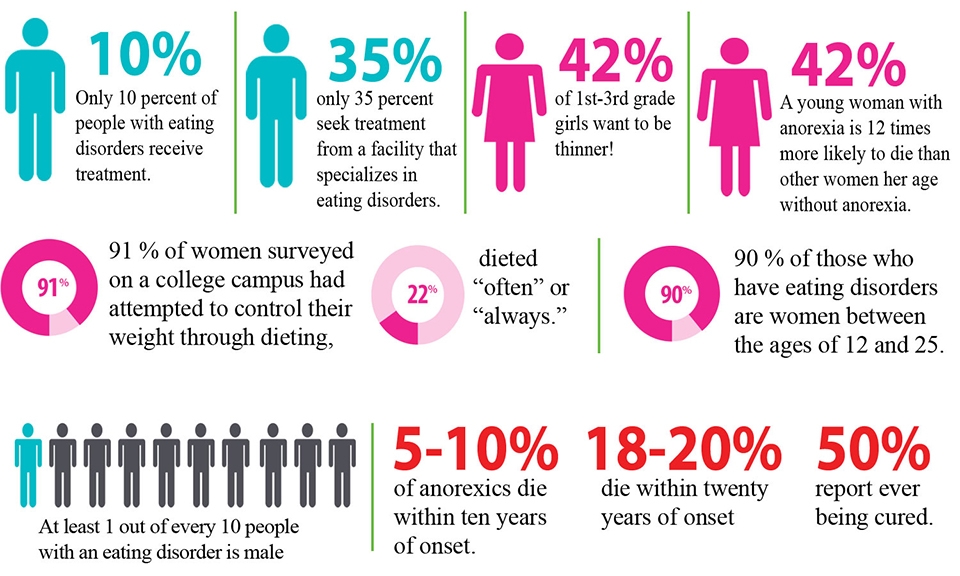 Bulimia can have severe health consequences. Frequent vomiting causes irritation of the pharynx and esophagus, as well as destruction of tooth enamel by acid from the stomach. Sometimes there is a cessation of menstruation. The most serious effects are associated with dehydration and loss of electrolytes (sodium and potassium) due to vomiting and diarrhea caused by laxatives.
Bulimia can have severe health consequences. Frequent vomiting causes irritation of the pharynx and esophagus, as well as destruction of tooth enamel by acid from the stomach. Sometimes there is a cessation of menstruation. The most serious effects are associated with dehydration and loss of electrolytes (sodium and potassium) due to vomiting and diarrhea caused by laxatives.
The treatment of anorexia and bulimia requires the combined efforts of doctors from different specialties. Integral components of treatment are alimentary rehabilitation and measures aimed at restoring body weight. Nutritional rehabilitation programs typically use emotional care and support, as well as a variety of behavioral psychotherapy techniques that involve a combination of reinforcing stimuli that integrates exercise, a strict exercise regimen and rest, in addition, prioritizing target body weight, desirable behaviors and informative feedback. The nutritional management of patients with anorexia nervosa is an important part of their treatment. In chronic starvation, the need for energy is reduced. Therefore, weight gain can be promoted by initially providing a relatively low caloric intake and then gradually increasing it. There are several schemes for increasing nutrition, the observance of which guarantees the absence of side effects and complications in the form of edema, impaired mineral metabolism, and damage to the digestive organs. Supportive psychotropic drugs are often used in the treatment of anorexia and bulimia, in particular antidepressants and atypical antipsychotics . Plays an important role, individual psychotherapy ; it should be carried out by a specialist who inspires confidence in the patient. We all come from childhood. In people with eating problems, the upbringing and family situation is often quite typical. Lack of parental attention and approval, or a “contrast shower” due to sudden changes in parental mood, love and affection, forms a “complex” and attitude in the child: I must earn love! Serving her, the child becomes a perfectionist, demanding first of all to himself: everything must be perfect, from grades at school to appearance, figures .
The nutritional management of patients with anorexia nervosa is an important part of their treatment. In chronic starvation, the need for energy is reduced. Therefore, weight gain can be promoted by initially providing a relatively low caloric intake and then gradually increasing it. There are several schemes for increasing nutrition, the observance of which guarantees the absence of side effects and complications in the form of edema, impaired mineral metabolism, and damage to the digestive organs. Supportive psychotropic drugs are often used in the treatment of anorexia and bulimia, in particular antidepressants and atypical antipsychotics . Plays an important role, individual psychotherapy ; it should be carried out by a specialist who inspires confidence in the patient. We all come from childhood. In people with eating problems, the upbringing and family situation is often quite typical. Lack of parental attention and approval, or a “contrast shower” due to sudden changes in parental mood, love and affection, forms a “complex” and attitude in the child: I must earn love! Serving her, the child becomes a perfectionist, demanding first of all to himself: everything must be perfect, from grades at school to appearance, figures . .. Often parents believe that instead of praise it is better to spur their daughter to success by comparisons. "Katya studies better! And Masha is so neat!" the child hears. Mothers, speaking in this way, believe that they come from the best of intentions and will benefit their child by this, they want to give an incentive for great accomplishments and improvement of their child. So, with mother's milk, the stereotype is sown that one should strive to be the first, the very best. The most interesting, smart, beautiful! The most neat, elegant and well-dressed! Unable to distinguish between emotional hunger and physiological hunger, a person easily switches from psychological problems to bodily ones, jams experiences in the literal and figurative sense of the word. Instead of friends, rest and entertainment - the first, second, third and compote. The lack of human communication, love and support is filled with cakes, pastries, favorite dishes and just what turns up under a hot hand and an irritated stomach.
.. Often parents believe that instead of praise it is better to spur their daughter to success by comparisons. "Katya studies better! And Masha is so neat!" the child hears. Mothers, speaking in this way, believe that they come from the best of intentions and will benefit their child by this, they want to give an incentive for great accomplishments and improvement of their child. So, with mother's milk, the stereotype is sown that one should strive to be the first, the very best. The most interesting, smart, beautiful! The most neat, elegant and well-dressed! Unable to distinguish between emotional hunger and physiological hunger, a person easily switches from psychological problems to bodily ones, jams experiences in the literal and figurative sense of the word. Instead of friends, rest and entertainment - the first, second, third and compote. The lack of human communication, love and support is filled with cakes, pastries, favorite dishes and just what turns up under a hot hand and an irritated stomach.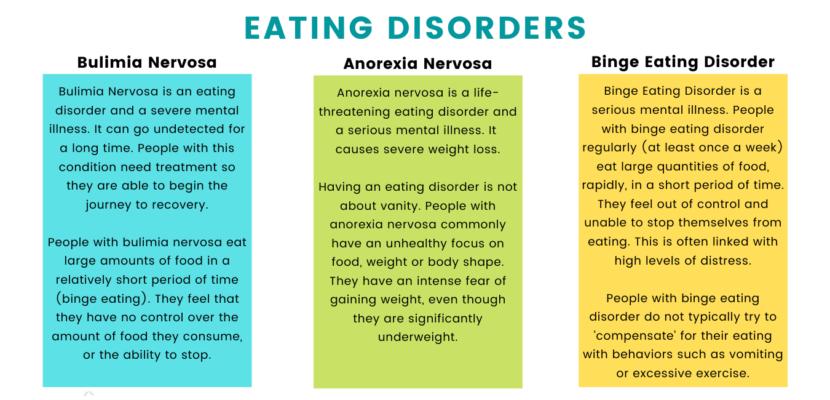 Family and friends usually do not understand the essence of the problem and experiences of a person with an eating disorder. They say: "Pull yourself together! Eat like all normal people!". This does not give the desired effect. Moreover, it drives a person with a problem of eating behavior even more into a psychological impasse and nervous tension. Great successes in the treatment of eating disorders are demonstrated by cognitive-behavioral psychotherapy and family therapy. Pharmacotherapy is at best an adjunct to other types of psychotherapy. Psychotherapy is aimed at correcting distorted cognitive formations in the form of perceiving oneself as fat, determining one's own value solely depending on the image of one's own body and a deep sense of inefficiency and inferiority. One of the elements of cognitive therapy is cognitive restructuring . In this approach, patients must find specific negative thoughts, list the evidence for those thoughts and list the evidence that refutes those thoughts, draw a valid conclusion, and use it to guide their own behavior.
Family and friends usually do not understand the essence of the problem and experiences of a person with an eating disorder. They say: "Pull yourself together! Eat like all normal people!". This does not give the desired effect. Moreover, it drives a person with a problem of eating behavior even more into a psychological impasse and nervous tension. Great successes in the treatment of eating disorders are demonstrated by cognitive-behavioral psychotherapy and family therapy. Pharmacotherapy is at best an adjunct to other types of psychotherapy. Psychotherapy is aimed at correcting distorted cognitive formations in the form of perceiving oneself as fat, determining one's own value solely depending on the image of one's own body and a deep sense of inefficiency and inferiority. One of the elements of cognitive therapy is cognitive restructuring . In this approach, patients must find specific negative thoughts, list the evidence for those thoughts and list the evidence that refutes those thoughts, draw a valid conclusion, and use it to guide their own behavior. Another element of cognitive therapy is focused problem solving . In this procedure, the patient identifies a specific problem, develops different solutions, considers the likely effectiveness and feasibility of each solution to the problem, chooses the best one, determines the steps to implement this solution, implements it, and then evaluates the entire process of solving the problem based on the result. Another essential element of cognitive therapy is monitoring: the patient should make daily records of food intake, including the type of food eaten, the time of the meal, and a description of the environment in which the meal was taken. Family therapy is especially effective in children and those under 18 years of age. It is aimed at correcting disturbed relationships in the family, leading to the development of an eating disorder in a child.
Another element of cognitive therapy is focused problem solving . In this procedure, the patient identifies a specific problem, develops different solutions, considers the likely effectiveness and feasibility of each solution to the problem, chooses the best one, determines the steps to implement this solution, implements it, and then evaluates the entire process of solving the problem based on the result. Another essential element of cognitive therapy is monitoring: the patient should make daily records of food intake, including the type of food eaten, the time of the meal, and a description of the environment in which the meal was taken. Family therapy is especially effective in children and those under 18 years of age. It is aimed at correcting disturbed relationships in the family, leading to the development of an eating disorder in a child.
Eating disorders, anorexia, bulimia, binge eating, eating disorders, treatment | Psychological center PsyQ.
 ru
ru Eating disorders
Eating disorders affect people who focus on food and their weight.
Any person pays attention to food intake. In addition, everyone has periods when he eats either less or more than usual. However, most people return to a normal diet. If it doesn't, it's most likely an eating disorder.
Eating disorders details
Eating disorders are serious behavioral and mental problems.
Eating disorders are:
- Anorexia nervosa, in which you lose weight but do not eat enough because you think you are overweight.
- Bulimia, when periods of overeating are followed by periods of cleansing and refusal of food, sometimes with the help of artificially induced vomiting or laxatives
- Overeating, when nutrition is completely out of control
Women are more likely than men to have eating disorders. As a rule, they appear in adolescence and often coexist with depression and anxiety disorders.
Eating disorders can lead to heart and kidney disease and even death. Timely treatment is very important. Treatment for eating disorders includes monitoring, psychotherapy, nutritional counseling, and sometimes medication.
Timely treatment is very important. Treatment for eating disorders includes monitoring, psychotherapy, nutritional counseling, and sometimes medication.
Will you pay more attention to nutrition?
Your problems may be related to an eating disorder.
Eating disorders, clinical picture
Eating disorders are characterized by extremes. They are present when a person has severe eating disorders, such as excessive reduction in food intake, severe overeating, or feelings of extreme displeasure or concern about their weight or body.
A person with an eating disorder may start to eat only slightly more or less than usual, but at some point the desire to eat less or more gets out of hand. Eating disorders are very complex, and despite scientific research, their biological, behavioral, and social underpinnings are still not easy to understand.
There are two main types of eating disorders - anorexia and bulimia. Most diseases are similar to anorexia or bulimia, but with slightly different characteristics. Overeating has received a lot of attention from scientific researchers and the media recently, but it is also a type of eating disorder.
Overeating has received a lot of attention from scientific researchers and the media recently, but it is also a type of eating disorder.
Eating disorders often appear during adolescence or early adulthood, but some studies indicate that they may develop during childhood or vice versa later in adulthood. Women and girls are much more likely than men to suffer from eating disorders. Men and boys are estimated to make up 5 to 15 percent of patients with anorexia or bulimia and about 35 percent of people suffering from binge eating. Eating disorders are a real, treatable disease with complex psychological and biological causes. They often coexist with other psychiatric disorders such as depression, substance abuse, or anxiety disorders. People with eating disorders can also suffer from numerous physiological complications, such as heart disease or kidney failure, which can lead to death.
Eating disorders are treatable
Psychological treatments are effective for most eating disorders.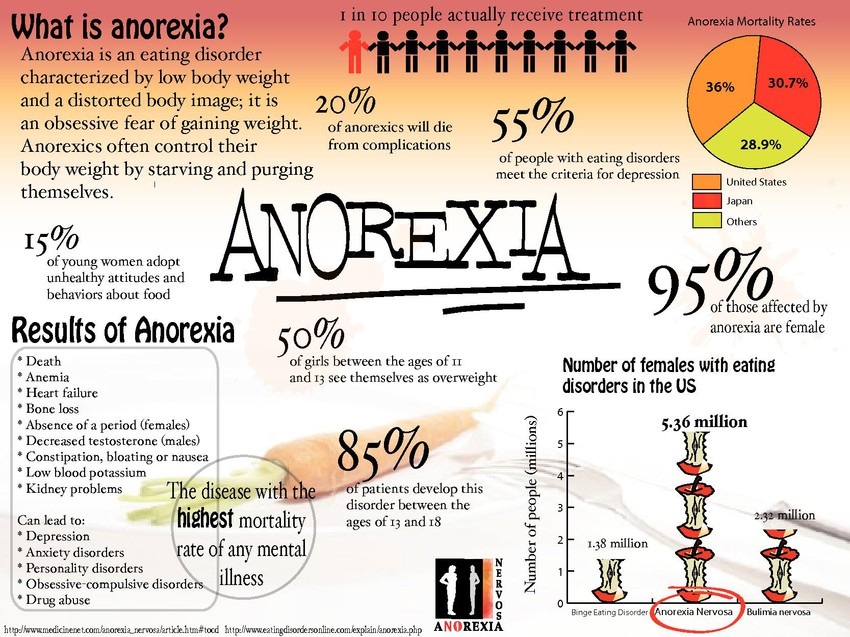 However, in more complex and chronic cases, treatment may include medical intervention and monitoring, medications, and nutritional counseling. Some patients must be hospitalized for treatment of malnutrition or excess weight.
However, in more complex and chronic cases, treatment may include medical intervention and monitoring, medications, and nutritional counseling. Some patients must be hospitalized for treatment of malnutrition or excess weight.
Anorexia
Anorexia nervosa is characterized by emaciation, a persistent desire to be thin and an unwillingness to maintain a normal or healthy weight, body image distortion and a strong fear of gaining weight, absence of menses in girls and women, and extremely disturbing eating behavior. Some people with anorexia try to lose weight by following an overly restrictive diet, others lose weight by artificially inducing vomiting, abusing laxatives or enemas.
Many people with anorexia believe that they are overweight, even if they are starving or clearly malnourished. The person becomes obsessed with nutrition and weight control. A person with anorexia usually weighs all foods, counts calories, and eats only very small amounts and only certain foods. Some people with anorexia re-establish a normal diet after a single course of treatment, while others experience relapses. People with chronic anorexia suffer more severely. Over the years, while they battle the disease, their physical health gradually deteriorates.
Some people with anorexia re-establish a normal diet after a single course of treatment, while others experience relapses. People with chronic anorexia suffer more severely. Over the years, while they battle the disease, their physical health gradually deteriorates.
According to some studies, people with anorexia are 10 times more likely to die as a result of a common illness compared to people without disabilities. The most common causes that lead to death are cardiac arrest, and an imbalance of electrolytes and fluids in the body. There is also a serious risk of suicide.
A significant number of people with anorexia also have mental and physiological illnesses such as depression, anxiety, compulsive behavior, substance abuse, cardiovascular and neurological disorders, and physical developmental disorders.
Other symptoms may develop over time, including:
- thinning of the bones (osteopenia and osteoporosis)
- brittle nails and hair
- dry and yellowing of the skin
- growth of body hair
- mild anemia, muscle weakness
- severe constipation
- low blood pressure, decreased breathing and heart rate
- drop in body temperature, resulting in a person who is cold all the time
- lethargy
Treatment of anorexia has three components of success:
- restoring normal weight
- treating psychological causes of eating disorders
- correcting behaviors and/or thoughts that lead to eating problems and preventing relapse mood, may help in the treatment of patients with anorexia by reversing the depressed mood and anxiety symptoms that often accompany anorexia. Recent studies, however, show that antidepressants do not help in some patients' fight against possible relapses of anorexia. In addition, the effectiveness of drugs during the critical first phase of recovery in patients of normal weight is questionable. In general, the question of whether drugs can help patients beat anorexia remains open, but research in this area continues.
Recent studies, however, show that antidepressants do not help in some patients' fight against possible relapses of anorexia. In addition, the effectiveness of drugs during the critical first phase of recovery in patients of normal weight is questionable. In general, the question of whether drugs can help patients beat anorexia remains open, but research in this area continues.
Various forms of psychotherapy, including individual, group and family therapy, can help address the psychological causes of illness. Some studies show that in the treatment of adolescent anorexia, family therapy in which parents take responsibility for nutrition is the most effective way to help a young person with anorexia to normalize weight, nutrition and improve mood.
It should be noted that an integrated approach to the treatment of anorexia, involving medical care and supportive psychotherapy, is the most effective. However, the result of treatment directly depends on the patient's interest in correcting the current situation.
Bulimia
Bulimia is characterized by periodic episodes of eating unusually large amounts of food, and a feeling of lack of control over the eating process. Binging episodes are followed by another type of behavior that compensates for overeating, such as purging (eg, induced vomiting, overuse of laxatives or diuretics), strict fasting, and/or inadequate exercise.
Unlike anorexia, people with bulimia usually have a normal weight for their age and height. But, like people with anorexia, they fear gaining weight, desperately want to lose weight, and are dissatisfied with body size and shape. Usually, episodes of bulimia (compulsive eating) occur secretly, as they are often accompanied by feelings of disgust and shame. Cycles of compulsive eating and purging usually repeat several times a week. Similar to anorexia, people with bulimia often have psychiatric disorders such as depression, anxiety, and/or substance abuse.
There are also physiological disorders caused by purging episodes, such as electrolyte imbalances, gastrointestinal disorders, and dental disorders.
Other symptoms of bulimia:
- chronic inflammation and sore throat
- swelling of glands in the neck and throat
- destruction of tooth enamel due to exposure to gastric juices and increased tooth sensitivity
- gastroenterological disorders
- irritation and upset of the intestines from the abuse of laxatives
- Kidney problems due to diuretic abuse
- Severe dehydration
As with anorexia, treatment for bulimia is often complex and depends on the individual's needs.
To reduce or stop binge eating and purging episodes, the patient may receive nutritional counseling, psychotherapy (such as psychoanalysis), and medication. Some antidepressants, such as fluoxetine (Prozac), which is the only drug approved to treat bulimia, may help patients who also suffer from depression and/or anxiety. Addressing the associated psychological problems, in turn, helps reduce the frequency of binge eating and purging, and reduces the chance of relapse.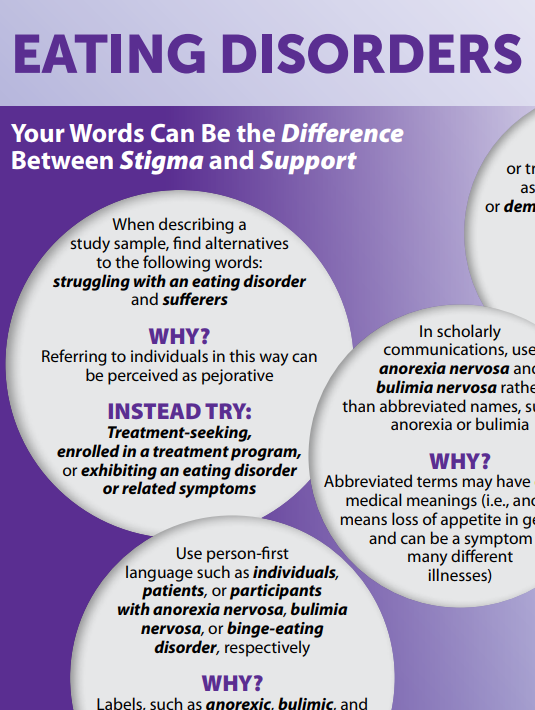 Therapy can be either individually oriented or in a group.
Therapy can be either individually oriented or in a group.
Binge eating or compulsive overeating
Binge eating or compulsive overeating is also an eating disorder and is characterized by recurrent episodes of binge eating during which the person feels a loss of control over himself and the process of eating. Unlike bulimia, binge eating episodes are not followed by purging episodes, such as inadequate exercise or fasting. As a result, people suffering from compulsive overeating are often overweight or obese. They also experience guilt and/or shame, which can lead to more binge eating.
Obese people with compulsive overeating often have comorbid psychiatric disorders such as anxiety, depression, and personality disorders. In addition, there is no doubt a direct link between obesity, cardiovascular disease and hypertension.
Treatment options for binge eating or compulsive eating are similar to those used to treat bulimia. Fluoxetine and other antidepressants may reduce the frequency of binge eating and help relieve depression in some patients.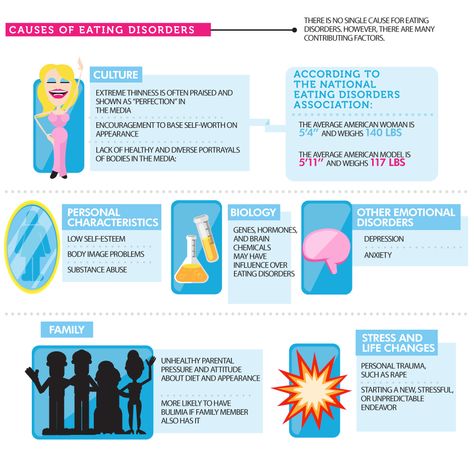
Individual psychotherapy, especially psychoanalysis, is used effectively to treat the underlying psychological problems associated with overeating, and group therapy is also used.
Antidepressant Warning
Despite the relative safety and popularity of antidepressants, a number of studies show that they can cause unpredictable reactions in some people, especially adolescents and young adults. In 2004, a thorough review of published and unpublished clinical trials of antidepressants was conducted in the United States, in which nearly 4,400 children and adolescents took part. The review found that 4% of those taking antidepressants had suicidal thoughts or attempts (although there were no reported cases of suicide), compared with 2% of people in the placebo control group.
Possible side effects while taking antidepressants:
Worsening of depressive symptoms, suicidal thoughts or behavior, unusual behavioral changes such as insomnia, agitation, or withdrawal from normal social situations.
A review of pediatric research conducted between 1988 and 2006 found that the benefits of antidepressants are likely to outweigh the risks for children and adolescents with severe depression and anxiety disorders.
Eating disorders in men and boys
Although eating disorders primarily affect women and girls, men and boys are also at risk. One in four diagnosed teenage cases of anorexia occurs in boys. Eating disorders affect women and men in much the same way.
Just like women who suffer from eating disorders, men have impaired body image and often suffer from muscle dysmorphia. This same type of disorder, but characterized by a greater preoccupation with the body, often leads to excessive muscle building. Some boys with an eating disorder want to lose weight, while others want to gain it. Boys who think they are too thin are at a higher risk of using steroids or other dangerous muscle-building drugs.
Boys with eating disorders have the same set of emotional, physical, and behavioral signs and symptoms as girls, but for various reasons, are less likely to be correctly diagnosed as eating disorders are stereotyped as purely female problems.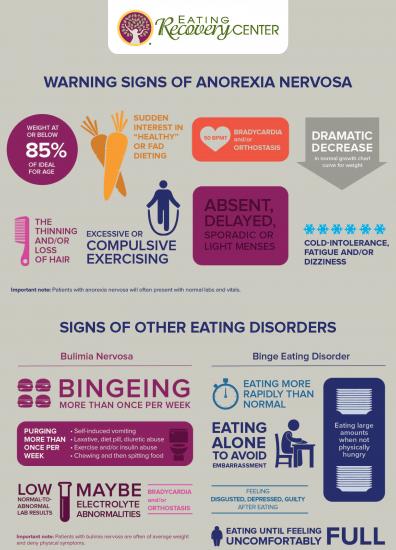
Modern Eating Disorder Research
Researchers are currently working to identify the underlying processes involved in eating disorders that should help guide optimal treatment. For example, what is anorexia: the result of a violation of body image, self-esteem problems, obsessive thoughts, obsessive behavior, or a combination of all of these processes? Is it possible to predict, by identifying something as a risk factor, when a sharp decrease in body weight will occur, and therefore try to avoid it?
These and other questions may be answered in the near future. Scientists, psychologists and doctors study how medical diseases, biological causes, behavioral issues, along with genetic factors influence the manifestation and development of the disease. They are looking for risk factors, trying to identify biological and psychological markers and develop tools focused on specific ways to normalize and control eating behavior.
Eat right (articles)
Will anorexia become the main male disease of the 21st century?
It would seem that anorexia (complete or partial refusal to eat) so common in our time is characteristic only of girls, but most experts are sure that in the 21st century, cases of bulimia and anorexia among men will only increase .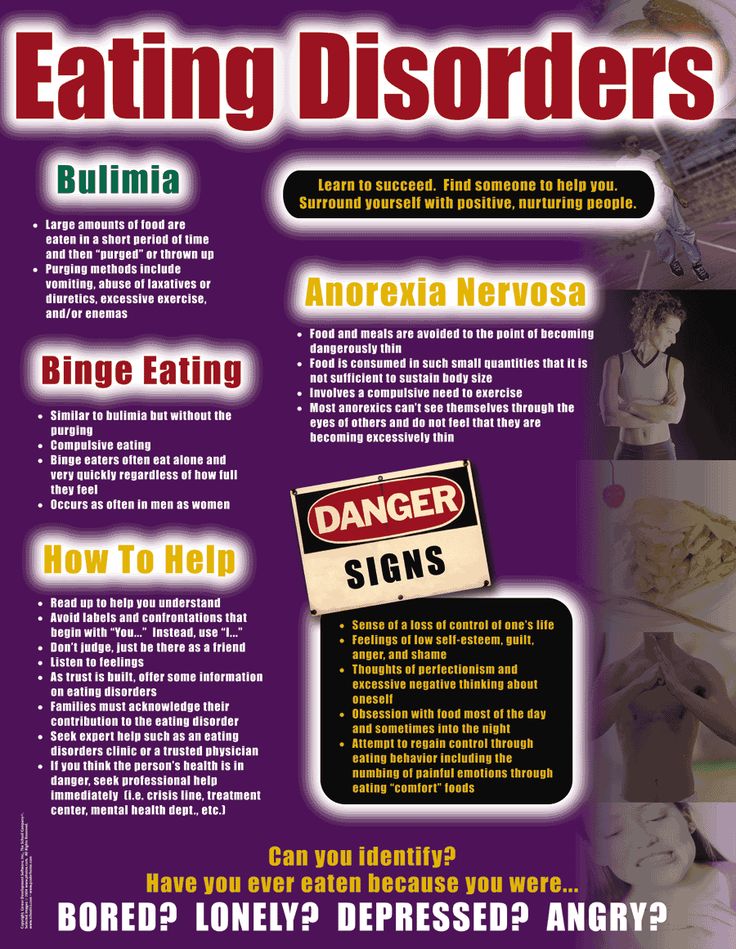 ..
..
Psychological causes overeating
The first signs of overeating should not be neglected. As long as they are small, you can easily fix the situation. Over time it will get harder. The need for food will begin to arise automatically, overeating will become habitual. This is how psychological dependence is developed ...
Nutritional epidemiology
The discipline of nutritional epidemiology uses epidemiological approaches to establish the relationship between nutrition and the occurrence of certain diseases. Until recently, many nutritionists and epidemiologists believed that the difficulties in assessing people's nutrition ...
Types of eating behavior
There are three main types of eating disorders: external eating behavior, emotiogenic eating behavior, restrictive eating behavior ...
Obesity will be treated like a drug addiction
Is it possible to make sure that sweet tooth does not want a cake, and fast food lovers are not drawn to a fragrant hamburger? People get fat, harm their health, but they can’t help themselves.