What is sleep paralysis a sign of
Sleep Paralysis - Causes, Symptoms, Treatment, and Prevention
Written by Beth Roybal
Medically Reviewed by Jennifer Robinson, MD on November 17, 2022
Is Sleep Paralysis a Symptom of a Serious Problem?
Sleep researchers conclude that, in most cases, sleep paralysis is simply a sign that your body is not moving smoothly through the stages of sleep. Rarely is sleep paralysis linked to deep underlying psychiatric problems.
Over the centuries, symptoms of sleep paralysis have been described in many ways and often attributed to an "evil" presence: unseen night demons in ancient times, the old hag in Shakespeare's Romeo and Juliet, and alien abductors. Almost every culture throughout history has had stories of shadowy evil creatures that terrify helpless humans at night. People have long sought explanations for this mysterious sleep-time paralysis and the accompanying feelings of terror.
What Is Sleep Paralysis?
Sleep paralysis is a feeling of being conscious but unable to move. It occurs when a person passes between stages of wakefulness and sleep. During these transitions, you may be unable to move or speak for a few seconds up to a few minutes. Some people may also feel pressure or a sense of choking. Sleep paralysis may accompany other sleep disorders such as narcolepsy. Narcolepsy is an overpowering need to sleep caused by a problem with the brain's ability to regulate sleep.
When Does Sleep Paralysis Usually Occur?
Sleep paralysis usually occurs at one of two times. If it occurs while you are falling asleep, it's called hypnagogic or predormital sleep paralysis. If it happens as you are waking up, it's called hypnopompic or postdormital sleep paralysis.
What Happens With Hypnagogic Sleep Paralysis?
As you fall asleep, your body slowly relaxes. Usually you become less aware, so you do not notice the change. However, if you remain or become aware while falling asleep, you may notice that you cannot move or speak.
What Happens With Hypnopompic Sleep Paralysis?
During sleep, your body alternates between REM (rapid eye movement) and NREM (non-rapid eye movement) sleep. One cycle of REM and NREM sleep lasts about 90 minutes. NREM sleep occurs first and takes up to 75% of your overall sleep time. During NREM sleep, your body relaxes and restores itself. At the end of NREM, your sleep shifts to REM. Your eyes move quickly and dreams occur, but the rest of your body remains very relaxed. Your muscles are "turned off" during REM sleep. If you become aware before the REM cycle has finished, you may notice that you cannot move or speak.
One cycle of REM and NREM sleep lasts about 90 minutes. NREM sleep occurs first and takes up to 75% of your overall sleep time. During NREM sleep, your body relaxes and restores itself. At the end of NREM, your sleep shifts to REM. Your eyes move quickly and dreams occur, but the rest of your body remains very relaxed. Your muscles are "turned off" during REM sleep. If you become aware before the REM cycle has finished, you may notice that you cannot move or speak.
Who Develops Sleep Paralysis?
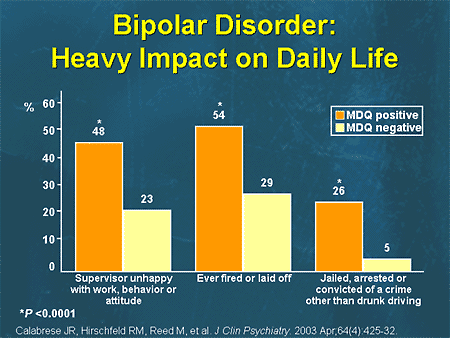
Up to as many as four out of every 10 people may have sleep paralysis. This common condition is often first noticed in the teen years. But men and women of any age can have it. Sleep paralysis may run in families. Other factors that may be linked to sleep paralysis include:
- Lack of sleep
- Sleep schedule that changes
- Mental conditions such as stress or bipolar disorder
- Sleeping on the back
- Other sleep problems such as narcolepsy or nighttime leg cramps
- Use of certain medications, such as those for ADHD
- Substance abuse
How Is Sleep Paralysis Diagnosed?
If you find yourself unable to move or speak for a few seconds or minutes when falling asleep or waking up, then it is likely you have isolated recurrent sleep paralysis.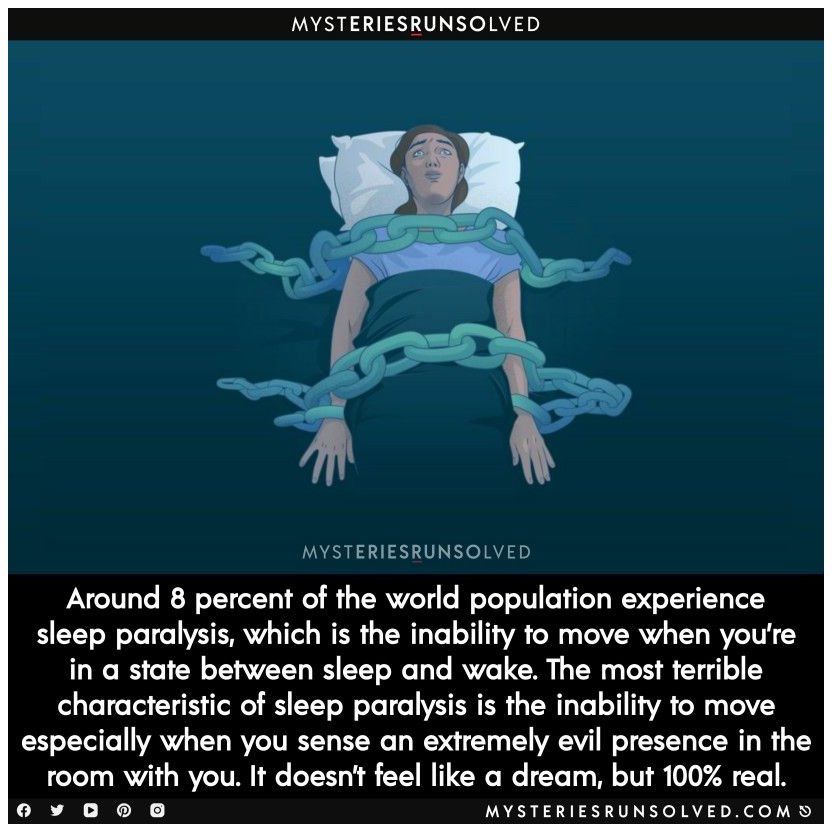 Often there is no need to treat this condition.
Often there is no need to treat this condition.
Check with your doctor if you have any of these concerns:
- You feel anxious about your symptoms
- Your symptoms leave you very tired during the day
- Your symptoms keep you up during the night
Your doctor may want to gather more information about your sleep health by doing any of the following:
- Ask you to describe your symptoms and keep a sleep diary for a few weeks
- Discuss your health history, including any known sleep disorders or any family history of sleep disorders
- Refer you to a sleep specialist for further evaluation
- Conduct overnight sleep studies or daytime nap studies to make sure you do not have another sleep disorder
How Is Sleep Paralysis Treated?
Most people need no treatment for sleep paralysis. Treating any underlying conditions such as narcolepsy may help if you are anxious or unable to sleep well. These treatments may include the following:
- Improving sleep habits -- such as making sure you get six to eight hours of sleep each night
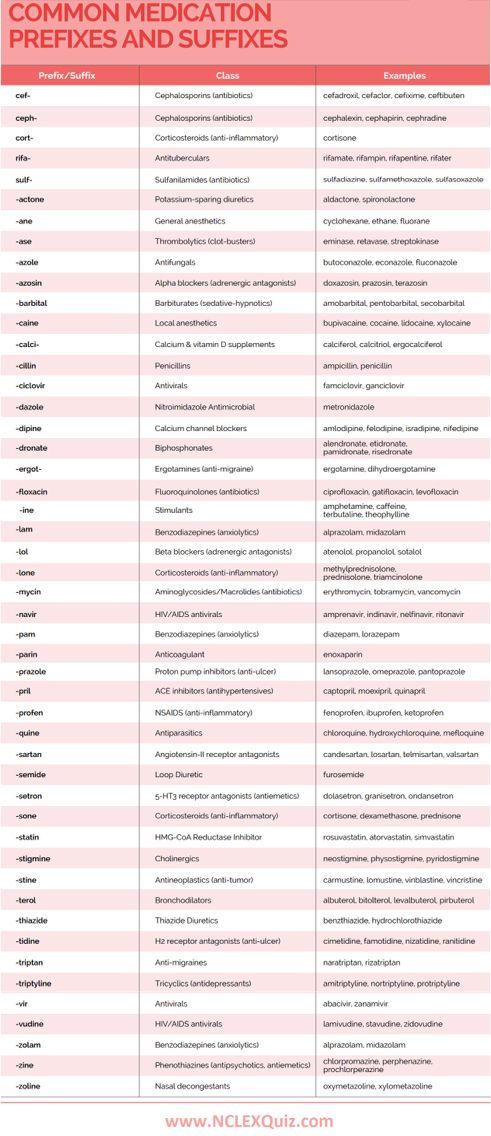
- Using antidepressant medication if it is prescribed to help regulate sleep cycles
- Treating any mental health problems that may contribute to sleep paralysis
- Treating any other sleep disorders, such as narcolepsy or leg cramps
What Can I Do About Sleep Paralysis?
There's no need to fear nighttime demons or alien abductors. If you have occasional sleep paralysis, you can take steps at home to control this disorder. Start by making sure you get enough sleep. Do what you can to relieve stress in your life -- especially just before bedtime. Try new sleeping positions if you sleep on your back. And be sure to see your doctor if sleep paralysis routinely prevents you from getting a good night's sleep.
If you have occasional sleep paralysis, you can take steps at home to control this disorder. Start by making sure you get enough sleep. Do what you can to relieve stress in your life -- especially just before bedtime. Try new sleeping positions if you sleep on your back. And be sure to see your doctor if sleep paralysis routinely prevents you from getting a good night's sleep.
Sleep paralysis - NHS
Sleep paralysis is when you cannot move or speak as you are waking up or falling asleep. It can be scary but it's harmless and most people will only get it once or twice in their life.
What happens during sleep paralysis
During sleep paralysis you may feel:
- awake but cannot move, speak or open your eyes
- like someone is in your room
- like something is pushing you down
- frightened
These feelings can last up to several minutes.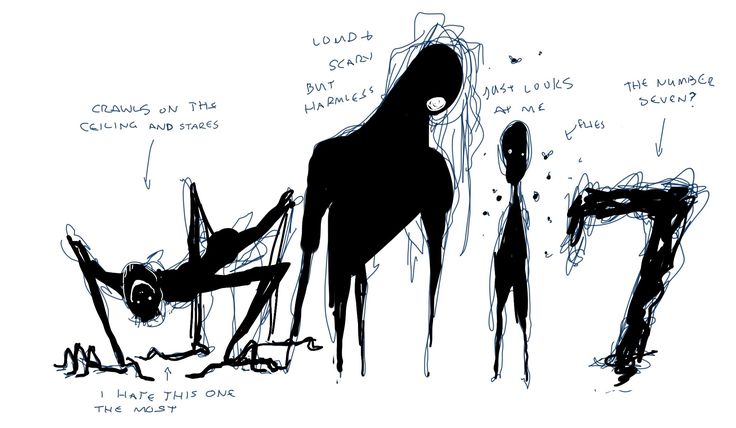
Causes of sleep paralysis
Sleep paralysis happens when you cannot move your muscles as you are waking up or falling asleep. This is because you are in sleep mode but your brain is active.
It's not clear why sleep paralysis can happen but it has been linked with:
- insomnia
- disrupted sleeping patterns – for example, because of shift work or jet lag
- narcolepsy – a long-term condition that causes a person to suddenly fall asleep
- post-traumatic stress disorder (PTSD)
- generalised anxiety disorder
- panic disorder
- a family history of sleep paralysis
Things you can do to help prevent sleep paralysis
You may be able to prevent sleep paralysis by changing your sleeping habits.
Do
-
try to regularly get 7 to 9 hours of sleep a day
-
go to bed at roughly the same time each night and get up at the same time each morning
-
get regular exercise, but not in the 4 hours before going to bed
Don’t
-
do not eat a big meal, smoke, or drink alcohol or caffeine shortly before going to bed
-
do not sleep on your back – this can make sleep paralysis more likely to happen
Non-urgent advice: See a GP if:
You often have sleep paralysis and you feel:
- very anxious or scared to go to sleep
- tired all the time due to lack of sleep
Treating sleep paralysis
A GP may be able to treat an underlying condition that could be triggering sleep paralysis such as insomnia or post-traumatic stress disorder.
If this does not help they might refer you to a doctor who specialises in sleep conditions.
Treatment from a specialist
You might be given medicine usually used to treat depression. Taking this type of medicine at a lower dose can also help with sleep paralysis.
You might also be referred for cognitive behavioural therapy (CBT).
Page last reviewed: 07 February 2023
Next review due: 07 February 2026
Sleep paralysis. What is Sleep Paralysis?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Sleep paralysis is a violation of the process of awakening or falling asleep, characterized by total muscular atony against the background of waking consciousness. In most patients, it develops at the moment of awakening, accompanied by a temporary impossibility of voluntary movements, a feeling of fear, threatening hallucinations. Diagnosed clinically. Additionally, a consultation with a neurologist, a psychiatrist, and a comprehensive polysomnographic study are required. Treatment consists in the normalization of lifestyle, adherence to sleep, the exclusion of overload, the use of various methods that allow you to relax, calm down before going to bed.
In most patients, it develops at the moment of awakening, accompanied by a temporary impossibility of voluntary movements, a feeling of fear, threatening hallucinations. Diagnosed clinically. Additionally, a consultation with a neurologist, a psychiatrist, and a comprehensive polysomnographic study are required. Treatment consists in the normalization of lifestyle, adherence to sleep, the exclusion of overload, the use of various methods that allow you to relax, calm down before going to bed.
ICD-10
G47.8 G83.8
- Causes
- Pathogenesis
- Classification
- Sleep paralysis symptoms
- Diagnostics
- Sleep paralysis treatment
- Prognosis and prevention
- Prices for treatment
General
For centuries, people have associated sleep paralysis with the machinations of demons, sorcerers, evil spirits. With the advent of somnographic research methods, it was possible to find a scientific explanation for this phenomenon. Within the framework of modern neurology, sleep paralysis belongs to the group of parasomnias, including nightmares, somnambulism, sleep intoxication, bruxism, nocturnal enuresis, and sleep-related eating disorders. Statistics show that 6-7% of the population has experienced sleep paralysis during their lifetime. Among patients with narcolepsy, paralytic parasomnia occurs in 45-50% of cases. The age of those suffering from this phenomenon varies between 12-30 years.
Within the framework of modern neurology, sleep paralysis belongs to the group of parasomnias, including nightmares, somnambulism, sleep intoxication, bruxism, nocturnal enuresis, and sleep-related eating disorders. Statistics show that 6-7% of the population has experienced sleep paralysis during their lifetime. Among patients with narcolepsy, paralytic parasomnia occurs in 45-50% of cases. The age of those suffering from this phenomenon varies between 12-30 years.
sleep paralysis
Causes
The pathological condition is based on a disorder in the sequence of onset of falling asleep or awakening of consciousness and the atony of skeletal muscles that characterizes the REM sleep phase. The reasons for the development are not exactly established. Predisposing factors are:
- Sleep disorders. The presence of insomnia, narcolepsy increases the likelihood of other pathological changes in the course and sequence of sleep phases.
 Chronic sleep deprivation, constant regime changes, frequent change of time zones have a similar effect.
Chronic sleep deprivation, constant regime changes, frequent change of time zones have a similar effect. - Psycho-emotional overload. Acute and chronic stress can cause dysregulation of sleep-wake cycles. Patients with paralytic parasomnia note an increase in episodes of paralysis against the background of mental overstrain.
- CNS toxicity. With drug addiction, substance abuse, alcoholism, nicotine addiction, long-term use of certain pharmaceuticals (tranquilizers, antidepressants), substances entering the body have a harmful effect on the brain. The result may be a malfunction in the functioning of systems that regulate sleep and wakefulness.
- Sleep on the back. Paralytic parasomnia occurs predominantly in patients sleeping in the supine position. Sleep on the side proceeds without episodes of paralysis. The reason for this pattern is unclear.
- Hereditary determinism. The genetic basis of the disease has not yet been studied, but cases of its occurrence within the same family are known.

Pathogenesis
Physiological sleep begins with a slow phase (FMS), which is replaced by a fast one (FBS). The latter is characterized by a pronounced decrease in the tone of skeletal muscles, excluding the respiratory ones. The rhythm of breathing quickens, the breath becomes shorter. Brain activity rises to the level of wakefulness. With paralytic parasomnia, the sequence of processes is disrupted, the person's consciousness wakes up before muscle tone is restored, there is a feeling of immobility - sleep paralysis. The appearance of paralysis is also possible at the moment of falling asleep, when the phase of REM sleep occurs, and consciousness is still in the waking state.
Since in the FBS there is a reflex setting of breathing to frequent short breaths, attempts by the awakened person to take a deep breath fail, which causes a feeling of compression in the chest. The inability to move is perceived by the brain as a life-threatening situation, a large number of neurotransmitters are released, provoking feelings of fear, panic, hallucinations. The vestibular apparatus is active, but due to the lack of movements it does not receive information from the periphery, which causes unusual sensations of flying in the air.
The vestibular apparatus is active, but due to the lack of movements it does not receive information from the periphery, which causes unusual sensations of flying in the air.
Classification
Parasomnia occurs at the moment of transition from a sleepy state to wakefulness and vice versa. The classification is based on the belonging of seizures to the period of falling asleep or awakening. In accordance with this criterion, sleep paralysis is divided into:
- Hypnopompic - observed during waking up. Occurs rarely. It arises as a result of the onset of FBS until the consciousness is completely immersed in a sleepy state. Patients experience a feeling of immobility prior to falling asleep.
- Hypnagogic - appears when going to sleep. observed in the vast majority of cases. Caused by the preservation of all the physiological features of the FBS with the awakening of consciousness that has already begun. Accompanied by a vivid clinical picture, severe emotional experiences.

Sleep paralysis symptoms
The pathological condition is similar to gross paresis in stroke. The patient is unable to perform voluntary motor acts. The feeling of immobility is excruciating, accompanied by panic fear, visual and auditory hallucinations. The patient sees dark figures, nightmares, hears threats, noise, steps, a specific squeak, feels the presence of hostile creatures. There is a violation of orientation in space, there is an illusion of flight, circling, hovering in the air, being in a moving elevator.
There may be a feeling of false movements - the illusion of turning over on one side when realizing the lack of motor ability. Complaints of a feeling of chest compression, suffocation, inability to breathe are typical. Sleep paralysis has a paroxysmal course. A paralytic episode lasts from a few seconds to 2-3 minutes; there are no neurological symptoms in the post-attack period. The frequency of seizures ranges from one episode to two or three paroxysms per night. Attacks do not pose a threat to life, are not accompanied by real asphyxia and other complications.
Attacks do not pose a threat to life, are not accompanied by real asphyxia and other complications.
Diagnostics
Characteristic symptoms allow you to establish sleep paralysis based on the clinical picture. The examination is carried out with the recurrence of paralytic episodes, aimed at excluding neurological and psychiatric pathology. The list of diagnostic procedures includes:
- Neurologist examination. Neurological status without features. Signs of emotional lability, asthenia against the background of overwork, existing background sleep disorders can be detected.
- Polysomnography. In the presence of video surveillance, it is possible to fix a paralytic episode: the patient is motionless, eyes are open, the face expresses fear, cardiorespiratory monitoring registers changes typical for FBS (tachycardia, tachypnea with a decrease in inspiratory volume). Electroencephalography makes it possible to differentiate sleep paralysis from nocturnal epileptic paroxysms.

- MSLT test. Multiple latency testing is done when narcolepsy is suspected. The diagnosis confirms the reduction of latency, the presence of more than 2 episodes of falling asleep.
- Psychiatric consultation. It is carried out by the method of conversation, observation, psychological testing. Needed to rule out comorbid psychiatric disorders.
Differential diagnosis is carried out with other somnological disorders, mental illness, epilepsy. Narcolepsy is accompanied by paroxysms of hypnolepsy - irresistible daytime hypersomnia. Somnambulism is the reverse state of sleep paralysis, occurs against the background of the absence of muscle hypotension in FBS. In the course of a somnological study, sleep apnea syndrome is excluded according to respiratory monitoring data, epilepsy - according to EEG results.
Sleep paralysis treatment
In most cases, therapy includes a conversation with the patient about the causes of paralytic episodes, measures to normalize the daily routine, psychological relaxation before bedtime. Drug treatment is prescribed in the presence of neurotic disorders and mental illness. To prevent the occurrence of new episodes of paralysis, the following recommendations can be observed:
Drug treatment is prescribed in the presence of neurotic disorders and mental illness. To prevent the occurrence of new episodes of paralysis, the following recommendations can be observed:
- Work mode optimization. It is necessary to avoid physical and mental overload, find time for rest. General strengthening physical exercises, walks in the fresh air are useful.
- Sleep mode normalization. Going to bed and waking up should be at the same time every day. The recommended duration of sleep is 8-9 hours.
- Relaxation before sleep. Aroma and herbal baths, sedative massage, soothing herbal preparations, calm music have a relaxing effect. Before going to bed, it is necessary to give up watching TV, mental stress, working at a computer, as they activate the activity of the brain.
- Wake on demand. Studies have shown the occurrence of paralytic parasomnia only with independent awakening. To prevent seizures, you should wake up on an alarm clock, ask loved ones to wake you up in the morning.
An important point is the patient's awareness of the mechanism of occurrence of parasomnic paroxysms. The help of a psychologist is possible. Psychological consultations include the development of methods for reducing emotional experiences, an accelerated exit from an attack. Training in relaxation techniques is recommended, which the patient subsequently uses independently.
Prognosis and prevention
Sleep paralysis is characterized by a benign course, spontaneous disappearance of symptoms against the background of lifestyle changes. Relapse of the disease, increased frequency of seizures provoke stressful situations, non-compliance with the regime, overload. Prevention is aimed at eliminating trigger factors: stress, excessive stress, sleep deprivation, constant changes in regimen. The main points of primary and secondary prevention are a healthy lifestyle, a calm and benevolent acceptance of any life situations, a reasonable professional and educational workload, and timely treatment of existing somnological disorders.
You can share your medical history, what helped you in the treatment of sleep paralysis.
Sources
- Sleep paralysis or old witch syndrome/ Dursunova AI// International Journal of Experimental Education. - 2014 - No. 6.
- The phenomenon of lucid dreams/ Kotlyarov EE, Vetvitskaya SM// International Student Scientific Bulletin. - 2017 - No. 6.
- Introspective analysis of the manifestations of sleep paralysis/ Zhilov DA, Nalivaiko TV// Topical issues of modern psychology and pedagogy. Collection of reports of the XVI International scientific conference. - 2014.
- Introspective analysis of the manifestations of sleep paralysis/ Zhilov D.A., Nalivaiko T.V.// Topical issues of modern psychology and pedagogy. Collection of reports of the XVI International scientific conference. - 2014.
- This article was prepared based on the materials of the site: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment.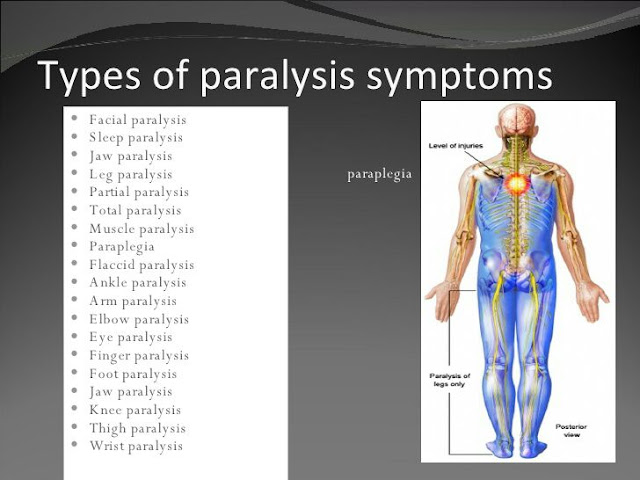 In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Sleep paralysis: causes, symptoms, treatment
Summary. Knowledge of the mechanisms of the development of the disease can help to overcome it
Sleep paralysis (sleep stupor) - a condition characterized by temporary paralysis with preserved consciousness; usually occurs when falling asleep or at the moment of awakening. This pathology is often accompanied by complex hallucinations and intense fear. The phenomenon of sleep paralysis occurs in 5-40% of people aged 12-30 years, most common among people with narcolepsy. Sleep stupor is considered to be physically harmless, but misunderstanding of the essence with its regular experience is a significant psychological trauma.
Sleep paralysis is mentioned in different cultures. Among the Slavic peoples, it is associated with mara (kikimora), a nightlight (demon), which jumps on its chest in the middle of the night to warn of good or bad.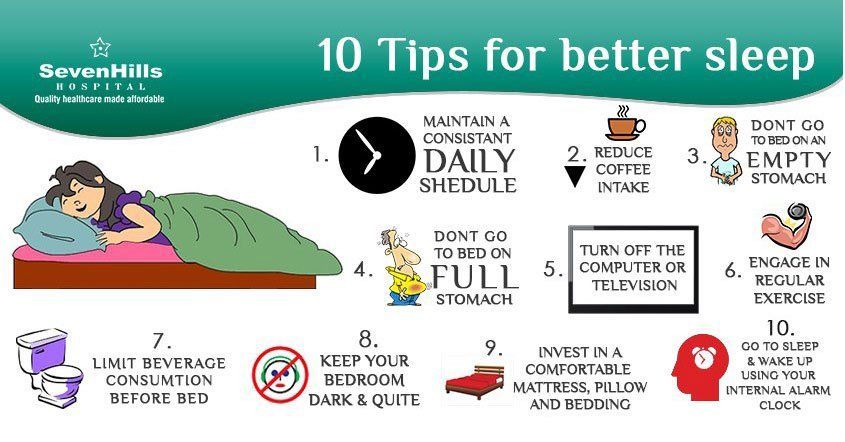 In Mexico they say “the corpse climbed on me”, in Newfoundland (Canada) they call this state “the old witch”, in the Muslim tradition, sleep paralysis is attributed to the tricks of genies.
In Mexico they say “the corpse climbed on me”, in Newfoundland (Canada) they call this state “the old witch”, in the Muslim tradition, sleep paralysis is attributed to the tricks of genies.
This pathology was the basis of the series of works of the Swiss-English artist Henry Fuseli "Nightmare". In four paintings, the artist depicted a sleeping woman with an incubus (in medieval legends, a dissolute demon) on her chest, the embodiment of unconscious fears.
Signs and symptoms of sleep paralysis:
- inability to move, lasting from a few seconds to a few minutes;
- preservation of consciousness;
- inability to speak;
- hallucinations and frightening sensations;
- chest pressure, bed moving, doors opening;
- inability to separate reality from fiction;
- feeling of impending death;
- intense perspiration;
- headache and muscle pain;
- paranoia.

Sleep paralysis usually occurs when a person sleeps on their back. The predisposing factors of the pathology are excessive tension, overexcitation, jet lag after a long flight, changes in sleep patterns, and associated panic disorders. This pathology can be a symptom of other diseases: depression, migraine, narcolepsy, obstructive sleep apnea syndrome, arterial hypertension and anxiety disorders.
The hypnotic episodes characteristic of sleep paralysis are of 3 types:
- sensations of the presence of an "intruder": opening doors, shuffling feet, a person in the shadows, a humanoid, a foreigner, etc.;
- incubus: feeling of pressure on the chest, difficulty in breathing, suffocation, sexual violence;
- vestibulo-motor hallucinations: sensation of falling, swimming, flying, hovering over one's body.
Sleep paralysis is based on desynchronization of brain and muscle activity during REM sleep. So, during this period, the parts of the brain responsible for identifying situations that threaten a person are in a state of increased sensitivity, perceiving everyday sounds and other stimuli, usually ignored by the brain, as a potential danger.
Since sleep paralysis often occurs against the background of uncontrolled chronic stress and sleep disturbances, the correction of this condition is primarily associated with the elimination of these factors.
Doctors advise:
- even on weekends and holidays, adhere to the same sleep-wake schedule;
- create favorable conditions for sleep: a comfortable mattress, bedding and underwear, as well as a clean, dark, cool bedroom;
- reduce the brightness of the lighting in the evening hours, as well as provide a dim night light;
- intensive daylight;
- avoid naps after 3 pm, limit nap duration to ≤90 min;
- do not eat 2 hours before bedtime, refrain from evening alcohol and caffeine;
- daily exercise, but no later than 2 hours before bedtime;
- create a ritual with soothing activities before bed, such as listening to soothing music, reading, etc.;
- Avoid email at least 1 hour before bedtime.

Learn more