Anger disorders dsm
Got an Anger Disorder? Not According to the DSM
Source: Source: (c) creatista
Do you know anyone with an anger disorder? I am a psychologist who specializes in helping couples to face their marriage problems, fix them, and then go on to enjoy long-lasting and long-loving marriage partnerships. A huge part of how I help these couples involves teaching them more constructive ways of handling feelings of anger. Yet if I must assign my clients, for insurance purposes, a diagnosis, anger problems is not an option. The current DSM (DSM-IV) diagnostic manual does not include excessive anger as a diagnosable disorder.
Psychoanalytic therapists talk about lacunae. I’ve always liked that word. Lacunae are gaps. A lacuna (pl. lacunas or lacunae) comes from the Latin term that, when referring to manuscripts, means a missing section of text. In music a lacuna is an extended pause or silence. In psychology, superego lacunae are gaps in superego development characteristic of, for instance, children with conduct disorders who lie, steal, punch and kick with no sense of doing anything wrong.
In the current diagnostic manual, and I believe also in the proposed new version, there is a huge lacuna when it comes to labeling anger.
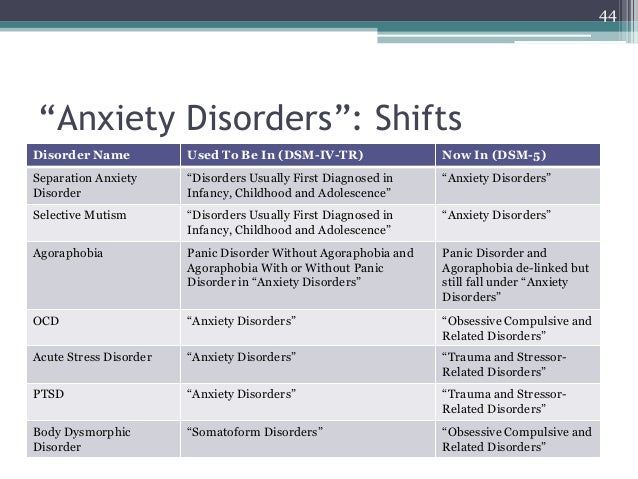
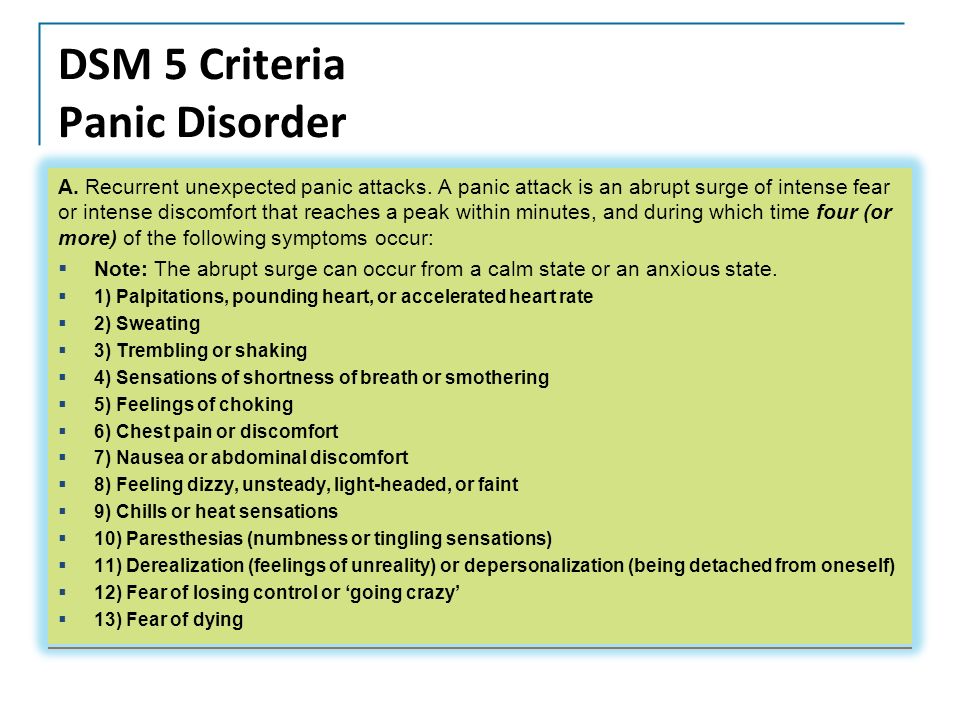
There are anxiety disorders, broken down into subcategories such as generalized anxiety disorder, phobias, panic attacks, and agoraphobia with or without panic attacks.
There are depressive disorders.
Yet there is no listing for anger disorders. The word anger does not even appear in the index!
Look at the catch-all category of Adjustment Disorders, the most commonly used category for outpatient mental health treatment:
Adjustment Disorders
- 309.9 Unspecified
- 309.24 With Anxiety
- 309.0 With Depressed Mood
- 309.3 With Disturbance of Conduct
- 309.28 With Mixed Anxiety and Depressed Mood
- 309.4 With Mixed Disturbance of Emotions and Conduct
Which diagnostic category can a therapist use for a client whose life adjustment difficulties center on excessive anger? How can a therapist diagnosis clients who react to differing viewpoints by getting mad instead of by engaging in quiet information sharing, mutual listening and creative problem-solving?
Anger falls into a hole, a gap in what the American Psychiatric Association, publisher of the DSM, recognizes as mental health problems.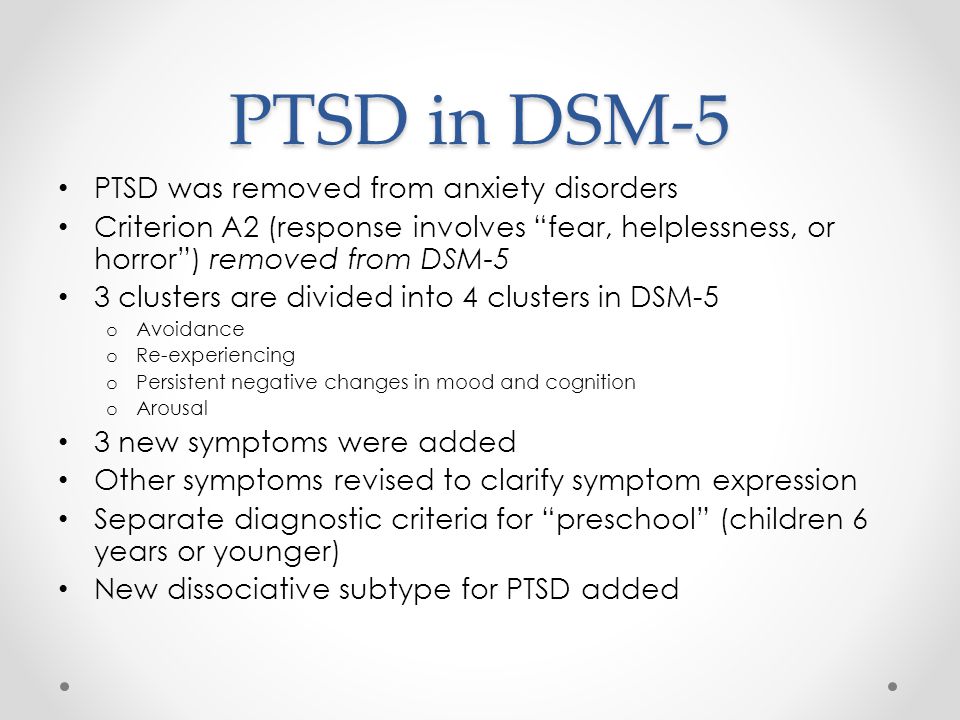
Anger is included on the symptom lists for many character disorders: psychopathy, explosive disorder, narcissism, borderline personality disorder, paranoia and more. This inclusion is good. Yet for carrying chronic underlying angry feelings that make a person unattractive to get close to, or for getting mad too often, too long, or too intensely, there is no diagnostic category
Does that mean that anger does not exist as a disturbing mental condition?
Would you consider the following scene normal emotional interacting?
Ask the person with an anger disorder if their anger is a problem. S/he is likely to tell you “I’m only mad because s/he made me mad!” That statement, in fact, may well be diagnostic of someone with an anger disorder.
Ask however any of the couples I see for marriage therapy and they will tell you how corrosive a role anger surpression and/or expression has played in the breakdown of their marriage. If they could feel angry, use that feeling as a constructive indicator to themselves of where there’s a problem, calm down, and then talk in a mutually respectful, cooperative way about the problem, they wouldn’t be coming to my office or thinking of finding a divorce lawyer.
If they could feel angry, use that feeling as a constructive indicator to themselves of where there’s a problem, calm down, and then talk in a mutually respectful, cooperative way about the problem, they wouldn’t be coming to my office or thinking of finding a divorce lawyer.
If there truly were no such thing as anger disorders, our society would not have our close-to-50% divorce rate. The world would be a better place for all of us.
Meanwhile, I just sigh. How bizarre, the DSM's blindness to the reality that excessive anger is a significant mental health problem.
------------------------------------
Denver clinical psychologist Susan Heitler, Ph.D, a graduate of Harvard and NYU, is author of Power of Two, a book, a workbook, and a website that teach the communication skills that sustain positive relationships.
Click here for a free Power of Two relationship test.
Click the Power of Two logo to learn the skills for a strong, emotionally healthy and loving marriage.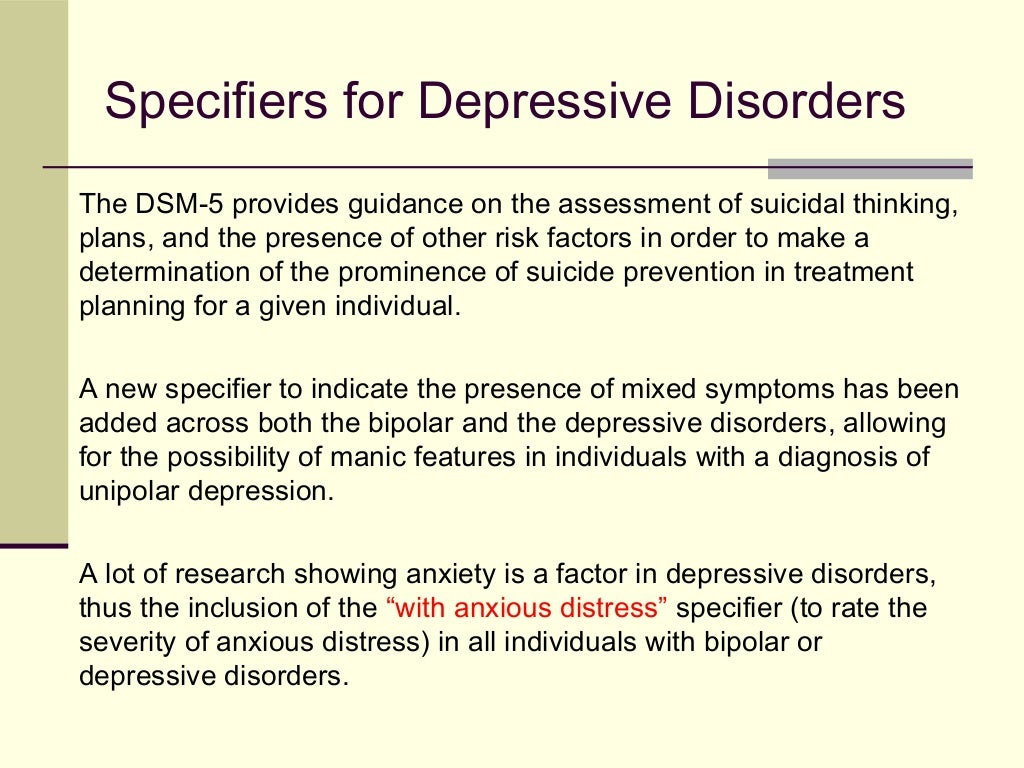
--------------------------------------
Adding the Diagnosis of Temper Dysregulation Disorder to DSM-5
These issues-among others-raise this question: Is the addition of a new diagnosis such as TDD to DSM-5 the best way to manage the issue of classification of youths with chronic, severe irritability and potential misdiagnosis of bipolar disorder?
The DSM-5 Childhood and Adolescent Disorders Work Group has proposed adding a new diagnosis called temper dysregulation disorder with dysphoria (TDD). The core features of TDD are pervasive irritable and/or sad mood and recurrent, severe anger outbursts, both of which must be consistently present for at least 1 year. The temper outbursts must be grossly out of proportion to the situation; be inconsistent with developmental level; and occur, on average, 3 or more times per week. The negative mood must be present nearly every day. The mood and temper outbursts must be present in at least 2 settings (in school, at home, or during social activities with peers) and be severe in at least 1 setting.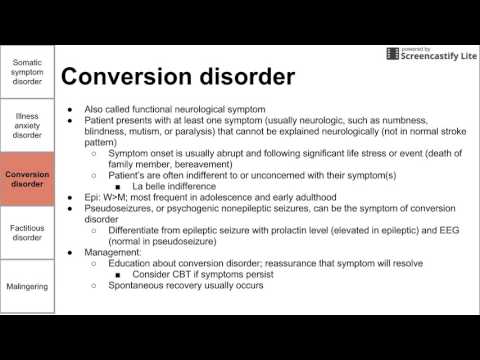 Age must be at least 6 years, and the onset must be before age 10.
Age must be at least 6 years, and the onset must be before age 10.
Information from the DSM-5 Web site indicates that the rapid increase in the frequency of the diagnosis of bipolar disorder in children and adolescents was a major driving force in the creation of TDD.1,2 TDD would provide a diagnostic “home” for youths who have chronic irritability and explosive anger outbursts, thereby reducing the chance that they might receive a diagnosis of bipolar disorder.
The DSM-5 Web site openly acknowledges the fact that research on TDD is in its early stages and that scientific support for it as a separate diagnostic entity is limited.1,2 The Web site also notes that the substantial overlap of TDD with oppositional defiant disorder (ODD) makes it unlikely that these 2 diagnoses have a distinct pathophysiology.
These issues-among others-raise this question: Is the addition of a new diagnosis such as TDD to DSM-5 the best way to manage the issue of classification of youths with chronic, severe irritability and potential misdiagnosis of bipolar disorder?
Understanding TDD
TDD would be different from most other diagnoses in DSM-5, in that all of its core diagnostic criteria are shared by other DSM disorders. There are no signs or symptoms that are unique to TDD. Criterion A, irritable and/or sad mood, is part of the diagnostic criteria for many disorders in child psychiatry: dysthymic disorder, major depressive disorder, bipolar disorder, generalized anxiety disorder, posttraumatic stress disorder, and ODD. Criterion B, severe tem-per outbursts, is a behavioral manifestation of irritable mood; these outbursts can be present in all of the preceding disorders, and temper outbursts are part of the DSM-IV criteria for ODD and for intermittent explosive disorder.
There are no signs or symptoms that are unique to TDD. Criterion A, irritable and/or sad mood, is part of the diagnostic criteria for many disorders in child psychiatry: dysthymic disorder, major depressive disorder, bipolar disorder, generalized anxiety disorder, posttraumatic stress disorder, and ODD. Criterion B, severe tem-per outbursts, is a behavioral manifestation of irritable mood; these outbursts can be present in all of the preceding disorders, and temper outbursts are part of the DSM-IV criteria for ODD and for intermittent explosive disorder.
Some would liken irritability in child psychiatry to fever in general medicine: even if it is severe and chronic, it can be a symptom of many different illnesses. Because chronic irritability is a symptom and temper outbursts are evidence of that symptom, TDD may be conflating a symptom with a syndrome.
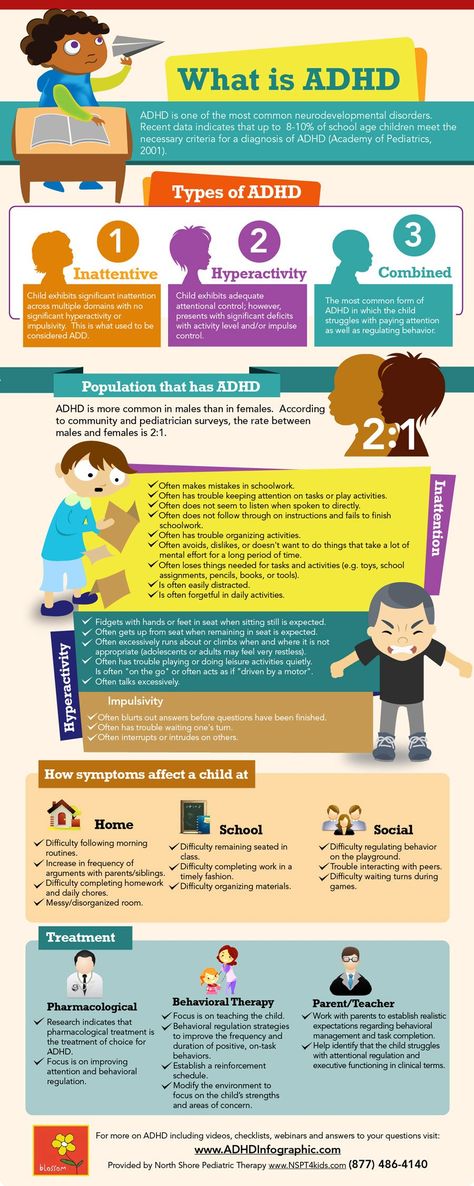
The diagnostic criteria attempt to address the lack of specificity by advising physicians not to diagnose TDD when the irritability and temper outbursts occur exclusively during the course of a mood or psychotic disorder or when the outbursts are not better accounted for by another disorder.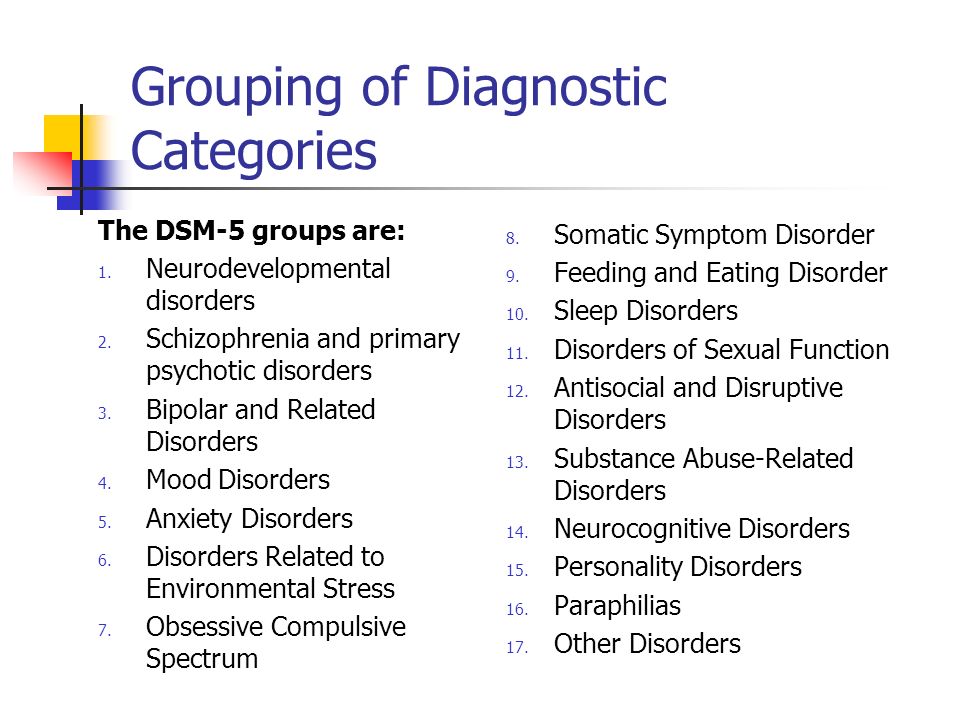 However, TDD can coexist with diagnoses such as ODD, attention-deficit/hyperactivity disorder (ADHD), conduct disorder, and substance use disorder.
However, TDD can coexist with diagnoses such as ODD, attention-deficit/hyperactivity disorder (ADHD), conduct disorder, and substance use disorder.
Episodic presentations of elevated mood and manic symptoms that last more than a day for the past year exclude a TDD diagnosis. These specifications may reduce the application of a TDD diagnosis to youths with mood, psychotic, and anxiety disorders. However, irritability is often a prodromal symptom of mood and psychotic disorders. Over the course of these disorders, irritability can be prominent even when other specific symptoms are not present. ODD and ADHD are frequently comorbid with many child psychiatric disorders. Therefore, it may be exceedingly difficult to determine whether the chronic, explosive irritability occurs “exclusively during the course of mood or psychotic disorders” or is “better accounted for by other disorders,” especially in clinical settings where there is limited time to perform comprehensive assessments.
Irritable mood and anger outbursts are common reasons for referral of youths for psychiatric assessment. However, there are usually other symptoms or psychosocial factors that accompany the chronic irritability. Consider the case vignettes of 3 different 7-year-old boys, all of whom present with severe anger outbursts and chronic irritability.
However, there are usually other symptoms or psychosocial factors that accompany the chronic irritability. Consider the case vignettes of 3 different 7-year-old boys, all of whom present with severe anger outbursts and chronic irritability.
CASE VIGNETTES
Albert, Henry, and Bill separately present for assessment at a child psychiatric outpatient clinic for concerns about severe anger outbursts. Each boy has outbursts, which are described as “rages” or “meltdowns,” in which he screams, throws things, turns over chairs, breaks things, and threatens others. At times, he will punch or kick a sibling or caregiver in the midst of the outbursts and will smash things against the door if he is forced to stay in his room. The outbursts can last anywhere from 15 minutes up to 2 hours and occur several times a week. All 3 boys were described by their parents as being moody since their toddler years, but each has become much more irritable over the past year. All 3 seem angry or miserable nearly every day.
In addition, Albert’s mother reports that he has been chronically hyperactive, impulsive, and distractible for as long she can remember. He has had low frustration tolerance since his toddler years and never grew out of his “terrible twos.” He responds to limit setting by doing the opposite of what the authority figure demands. Albert is bossy with peers and will quit playing with them if they do not do what he wants to do and will get back at other children if they do anything to bother him.
Henry’s mother states that he was very shy with strangers, starting at an early age. He was also very anxious in anticipation of situations of separation from his parents and some of his “meltdowns” occurred during these times, often prompting his parents to curtail planned activities. Marital relations between his parents have been strained. Henry has frequent nightmares about his parents being harmed and often demands to sleep with them at night. Transition to first grade was very problematic, and Henry’s “explosions” often occur before school.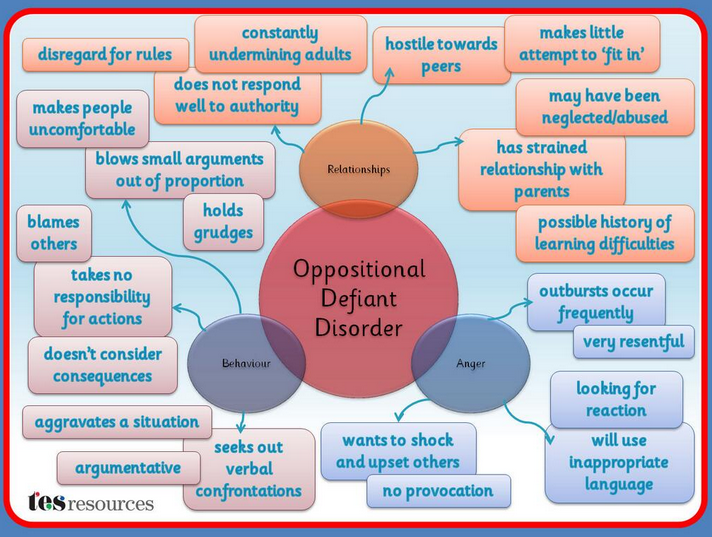 However, they can also occur at other times, especially when his parents set limits, refuse to give him something he wants, or are arguing with each other.
However, they can also occur at other times, especially when his parents set limits, refuse to give him something he wants, or are arguing with each other.
Bill’s mother has noticed that since the onset of the rages, he has times when he becomes very silly and inappropriately giddy, to the point where it annoys other children. During these episodes, Bill is hyperactive; is talkative to the point at which others cannot understand what he is saying; and engages in reckless, risk-taking behaviors with his bike and skateboard. However, if he is thwarted in his desires during these moods, it provokes a major outburst. Sometimes during these moods, Bill stays up much of the night “bouncing off the walls” and can get up for school without a problem. However, his mother says that these episodes only last a day at most and happen 2 or 3 times a month, and she cannot recall them ever occurring for days in a row. Bill’s mother is worried because the child’s father has bipolar disorder and his paternal grandmother says that Bill is “just like his dad was when he was a kid.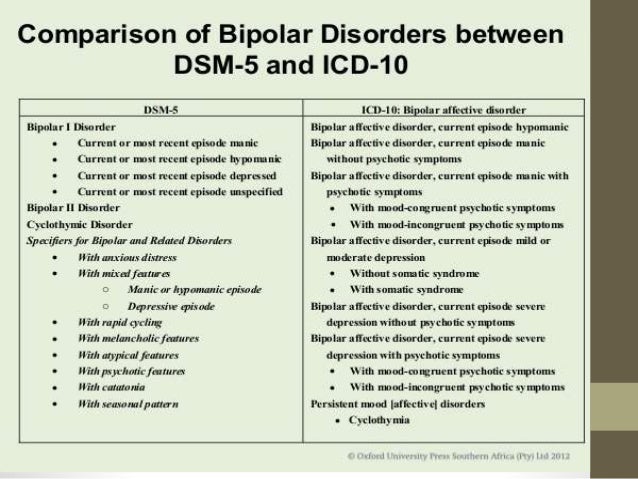 ”
”
Each of these boys could meet criteria for TDD. But do we think that these presentations are all the same syndrome that share a similar neurobiological basis, family history, and response to treatment? Does the availability of the new diagnostic label of TDD improve the diagnostic formulation and treatment plan for these children?
I suggest that the 3 boys have different syndromes, all of which include chronic irritability and explosive anger outbursts as part of the symptom presentation, and each would probably require different treatment strategies. In some ways, the TDD diagnosis can distract the clinician from focusing on the underlying problems, whether it is the likely ADHD and ODD in Albert’s case, the prominent anxiety and family dynamic issues in Henry’s case, or the possible early signs of bipolar disorder in Bill’s case. Having the information that all 3 boys could meet criteria for TDD does not help us decide what treatment to use or what the family should expect as far as future course of illness.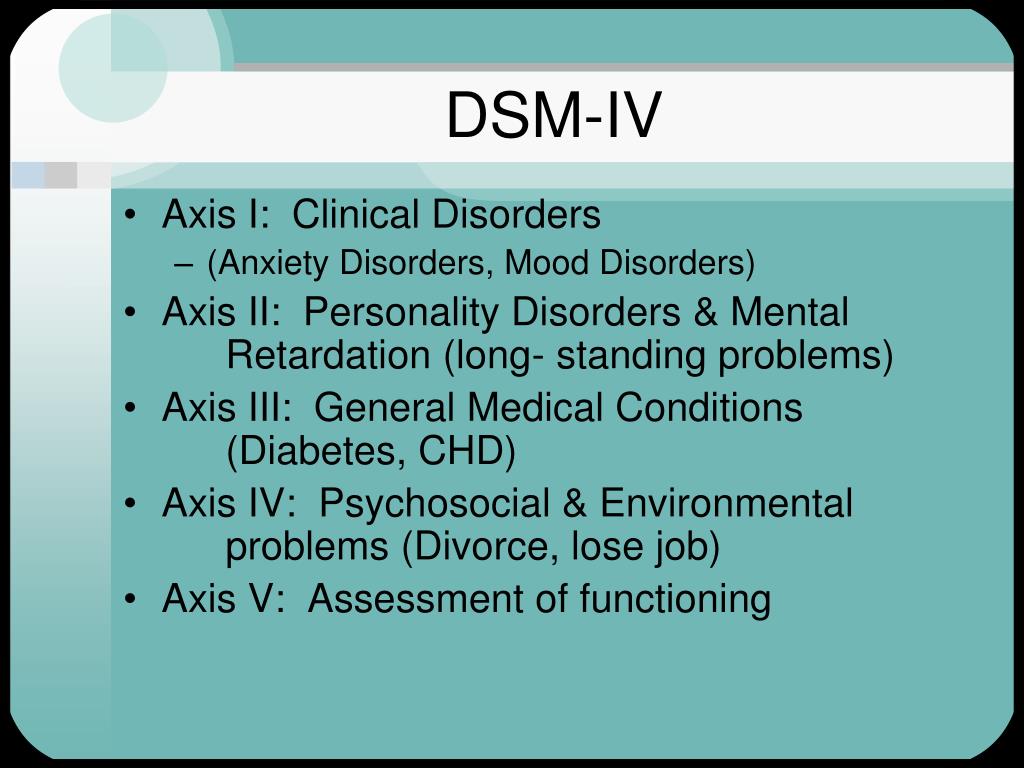
Severe mood dysregulation
The limited scientific support for TDD comes from studies of a related but more specific diagnostic phenotype, severe mood dysregulation (SMD). Symptoms of SMD are chronic, recurrent anger outbursts and irritable, sad mood that are present in TDD, but they also include hyperarousal, such as insomnia, racing thoughts, rapid speech, agitation, intrusiveness, and hyperactivity. We do not know whether data regarding the more specifically defined SMD phenotype would apply to the broader TDD diagnosis.
The Intramural Research Program of the NIMH studies examined the phenomenology and neurobiology of youths with SMD and compared them with healthy youths and youths who have bipolar I disorder. Participants were referred from across the country and were thoroughly evaluated to determine whether they met study criteria. The rates of ADHD and ODD were about 85% in the youths with SMD; the high rate of comorbidity forms the basis for the statement on the DSM-5 Web site that TDD and ODD are unlikely to have distinct pathophysiology. 1,2
1,2
The results from these groundbreaking studies strongly suggest that as a group, youths in this referred sample who meet criteria for SMD differ in significant ways from those who have clearly episodic bipolar I disorder and from healthy children. However, it is not at all clear that the results from these carefully selected research samples of youths with the SMD phenotype apply to children who meet TDD criteria in routine clinical settings. This is not a criticism of these studies; such a recruitment strategy is preferred during the early stages of innovative research. Rather, the concern is whether it is appropriate to extend these initial results to establish a new psychiatric illness with broader criteria that will be applied in very different settings.
There are no published studies that examine the prospective use of the TDD diagnostic criteria in clinical or epidemiological samples. The diagnostic criteria for SMD were applied retrospectively to the epidemiological dataset from the Great Smoky Mountains Study.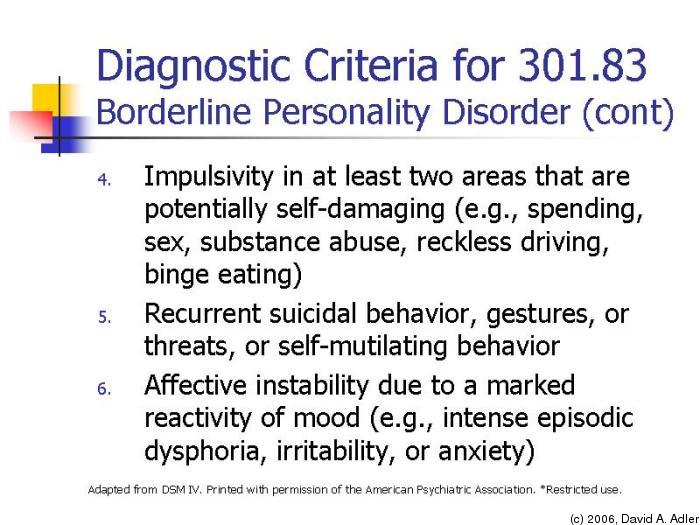 The results indicate that the SMD proxy diagnosis was common in this community sample; 3.2% of youths met the criteria for SMD.3 Because the TDD criteria are essentially a subset of the SMD criteria, it is possible that a significantly higher percentage would meet the criteria for TDD.
The results indicate that the SMD proxy diagnosis was common in this community sample; 3.2% of youths met the criteria for SMD.3 Because the TDD criteria are essentially a subset of the SMD criteria, it is possible that a significantly higher percentage would meet the criteria for TDD.
Psychiatry has been heavily criticized for “overdiagnosing” kids and “pathologizing” normal behavior. It is therefore of concern that establishing TDD could label a sizable percentage of youths with a new diagnosis. The Great Smoky Mountains Study also illustrates how diagnostic criteria can function quite differently in research settings than in the general clinical or epidemiological settings. The rates of ADHD and ODD in the youths with SMD in the Great Smoky Mountains Study sample were about 25%, more than 3-fold lower than rates in the youths with SMD in the neurobiological studies. Clearly, there were significant differences in the psychopathology of the youths identified as having SMD in the epidemiological sample versus those recruited for the NIMH studies.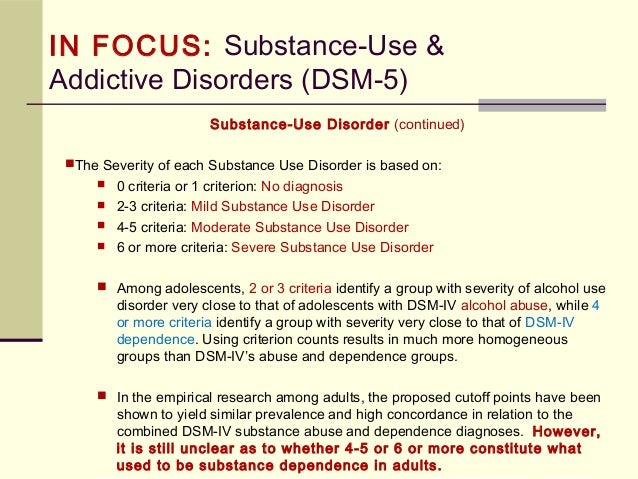
Overdiagnosis vs misdiagnosis of bipolar disorder in children
It seems clear that TDD does not have a sufficient level of research support to justify creating a new psychiatric diagnosis. Then why has it been proposed? The primary reason put forth on the DSM-5 Web site is the need to stem the tide of the perceived substantial overdiagnosis of bipolar disorder in children.1,2 Regardless of where one stands on the issue of the extent of misdiagnosis of bipolar disorder, it is clear that the use of bipolar disorder as a diagnosis on third-party payer claims for pediatric psychiatric services has increased substantially over the past decade.4,5 In addition, it has been my experience and that of others who specialize in the assessment of children with severe mood disorders, that there are some children with chronic, explosive irritability referred with a bipolar diagnosis who clearly do not have bipolar disorder.
It does not seem likely that building a new diagnostic “home” for these children without a solid scientific foundation will properly address the issue of misdiagnosis.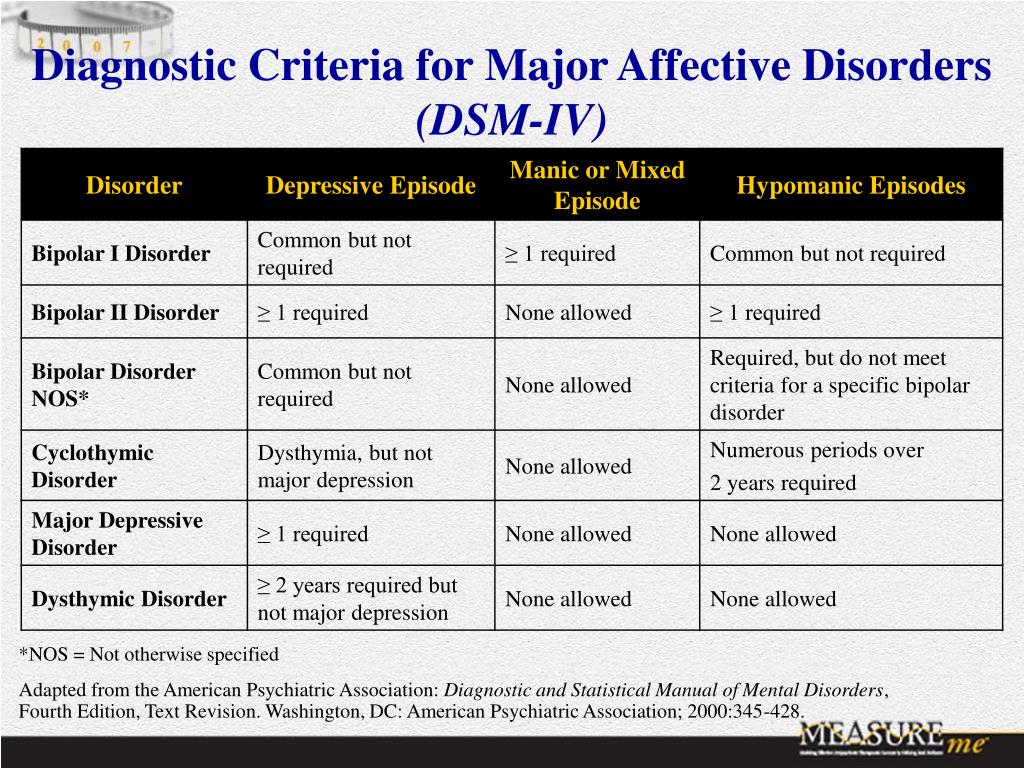 Many of these children have diagnosable DSM-IV disorders with scientifically supported treatments. There are no established treatments for TDD. Shifting the focus away from identifiable conditions and the psychosocial factors that may contribute to them is counterproductive-whether the diagnostic distraction is bipolar disorder or TDD. Granted, many children and adolescents have received proper treatment for whatever other DSM-IV disorders have been identified and whose psychosocial issues have been addressed to the best extent possible, yet they still exhibit chronic, explosive irritability. However, additional research is needed to better understand the phenomenology, pathophysiology, and treatment responsiveness of these children. Giving them a specific DSM-5 diagnosis such as TDD implies that we actually know what is going on. It would be better to acknowledge that given the current state of the science, we do not know enough to specify a diagnosis and instead indicate that they have a mood disorder not otherwise specified.
Many of these children have diagnosable DSM-IV disorders with scientifically supported treatments. There are no established treatments for TDD. Shifting the focus away from identifiable conditions and the psychosocial factors that may contribute to them is counterproductive-whether the diagnostic distraction is bipolar disorder or TDD. Granted, many children and adolescents have received proper treatment for whatever other DSM-IV disorders have been identified and whose psychosocial issues have been addressed to the best extent possible, yet they still exhibit chronic, explosive irritability. However, additional research is needed to better understand the phenomenology, pathophysiology, and treatment responsiveness of these children. Giving them a specific DSM-5 diagnosis such as TDD implies that we actually know what is going on. It would be better to acknowledge that given the current state of the science, we do not know enough to specify a diagnosis and instead indicate that they have a mood disorder not otherwise specified.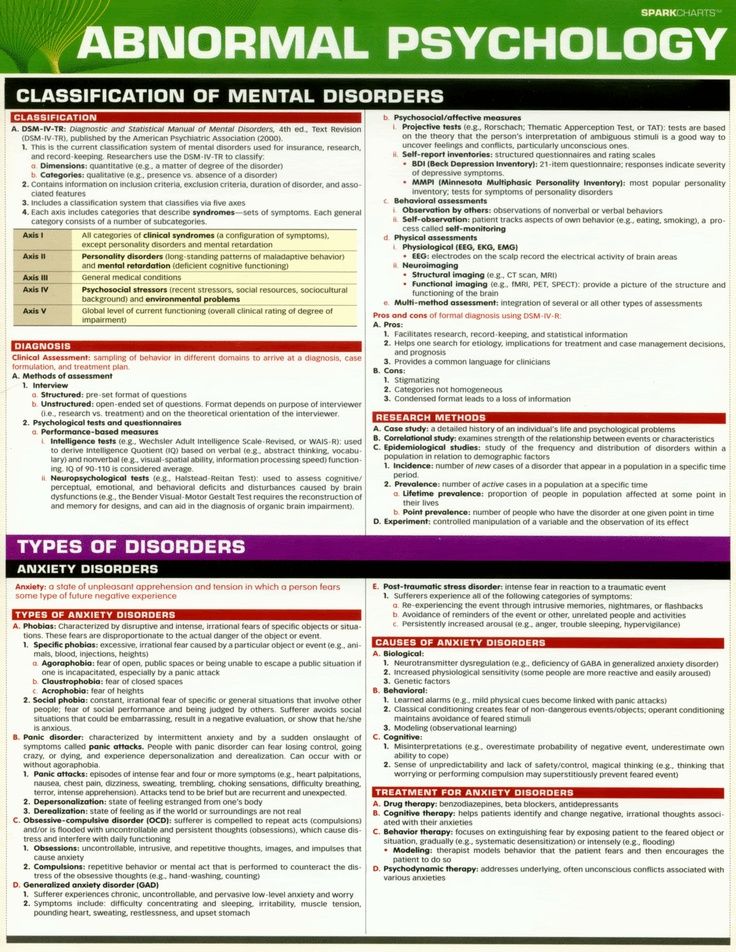
Alternative options
Because it is quite possible that there are subsets of children and adolescents with chronic irritability and explosive outbursts who have a phenotype that could merit the construction of a new diagnosis in the future, what are the options for DSM-5 other than establishing a stand-alone TDD diagnosis? One possibility would be to use TDD as a course specifier for other diagnoses in children, in particular ADHD and disruptive behavior, mood, autism spectrum, and anxiety disorders. Another option would be to place TDD or SMD in the Appendix as a diagnosis for future study. Either of these options could facilitate research on the nature of chronic, explosive irritability in youths.
Research could potentially provide a solid scientific basis to justify a new diagnosis with more specific criteria. The concern about misdiagnosis of bipolar disorder in children could be addressed directly in the bipolar disorder section, by specifications in the diagnostic criteria, and/or clarifications in the accompanying text.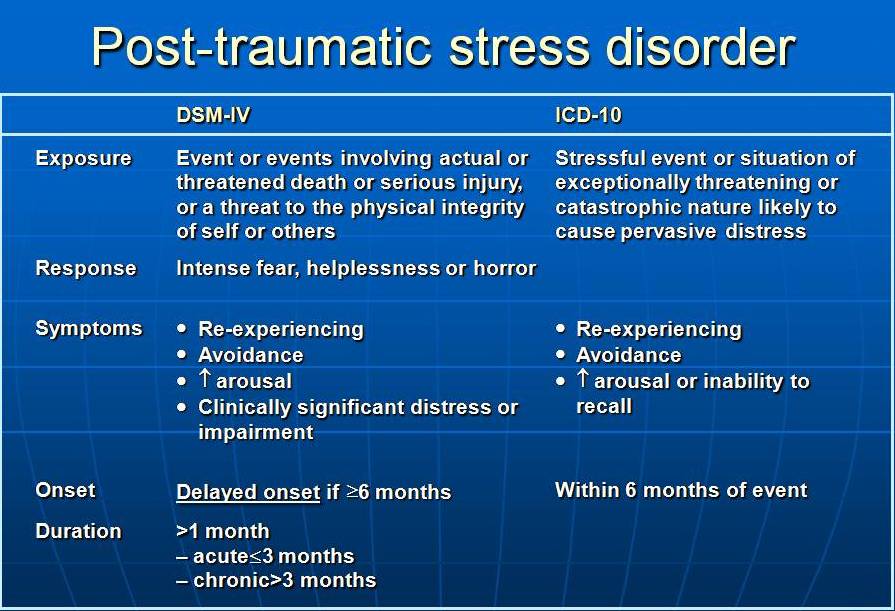 Such changes could facilitate additional education about the difficulties of diagnosing bipolar disorder in youths as well as how to classify youths with chronic, explosive irritability.
Such changes could facilitate additional education about the difficulties of diagnosing bipolar disorder in youths as well as how to classify youths with chronic, explosive irritability.
Conclusion
The members of the DSM-5 work groups have an extremely difficult responsibility to balance the potential risks and benefits of changes to DSM. However, in the case of youths with chronic, explosive irritability, I think it is premature to create a new psychiatric diagnosis. TDD does not have sufficient scientific support at this time, and we do not have evidence as to how it will function in clinical and epidemiological settings.
The criteria as currently constructed will likely identify a very heterogeneous group of children and adolescents with widely divergent developmental outcomes and treatment needs. These issues, plus the similarity of the TDD name to “temper tantrums,” have the potential to undermine how the public perceives child psychiatry. The negative consequences of establishing TDD outweigh the potential advantages, especially when there are reasonable alternatives to address the clinical concerns and research needs identified by the DSM-5 work groups.
References:
References
1. DSM-5 Childhood and Adolescent Disorders Work Group. Justification for Temper Dysregulation Disorder with Dysphoria; 2010. http://www.dsm5.org/Proposed%20Revision%20Attachments/Justification%20for%20Temper%20Dysregulation%20Disorder%20with%20Dysphoria.pdf. Accessed July 11, 2010.
2. American Psychiatric Association. Issues Perti-nent to a Developmental Approach to Bipolar Disorder in DSM-5. 2010. http://www.dsm5.org/Proposed%20Revision%20Attachments/APA%20Developmental%20Approaches%20to%20Bipolar%20Disorder.pdf. Accessed July 1, 2010.
3. Brotman MA, Schmajuk M, Rich BA, et al. Prevalence, clinical correlates, and longitudinal course of severe mood dysregulation in children. Biol Psychiatry. 2006;60:991-997.
4. Moreno C, Laje G, Blanco C, et al. National trends in the outpatient diagnosis and treatment of bipolar disorder in youth. Arch Gen Psychiatry.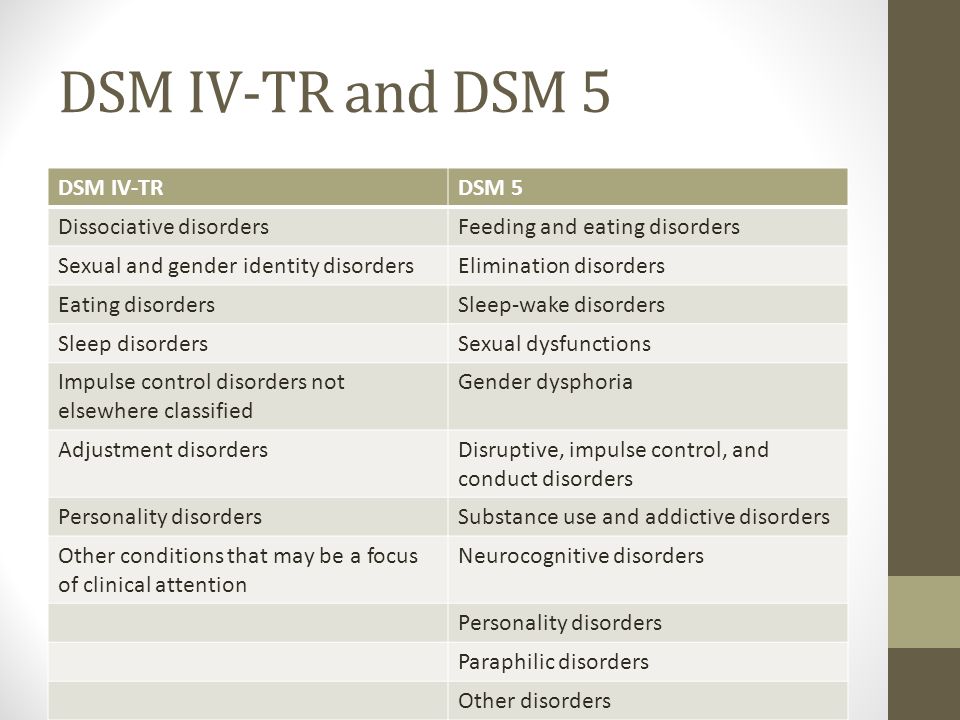 2007;64:1032-1039.
2007;64:1032-1039.
5. Blader JC, Carlson GA. Increased rates of bipolar disorder diagnoses among U.S. child, adolescent, and adult inpatients, 1996-2004. Biol Psychiatry. 2007;62:107-114.
Anger attacks and "anger disorders": clinical relevance, problem of classification, comorbidity and therapy (literature review) | Simutkin
1. Abramova AA Aggressiveness in depressive disorders: author. dis. … cand. psychol. Sciences. - Moscow. - 2005. - 23s.
2. Vaksman A.V. Hostility and aggressiveness in the structure of depression (patterns of formation, prognostic significance, therapy and social and psychological adaptation): author's abstract. dis. … cand. honey. Sciences. - Moscow. - 2005. - 26 p.
3. Izard K.E. Psychology of emotions / Perev. from English. - St. Petersburg: Publishing House "Peter". - 2000. - 464 p.
4. Mazo GE, Ganzenko MA Depression in women during the menopausal transition // Psychiatry and psychopharmacotherapy.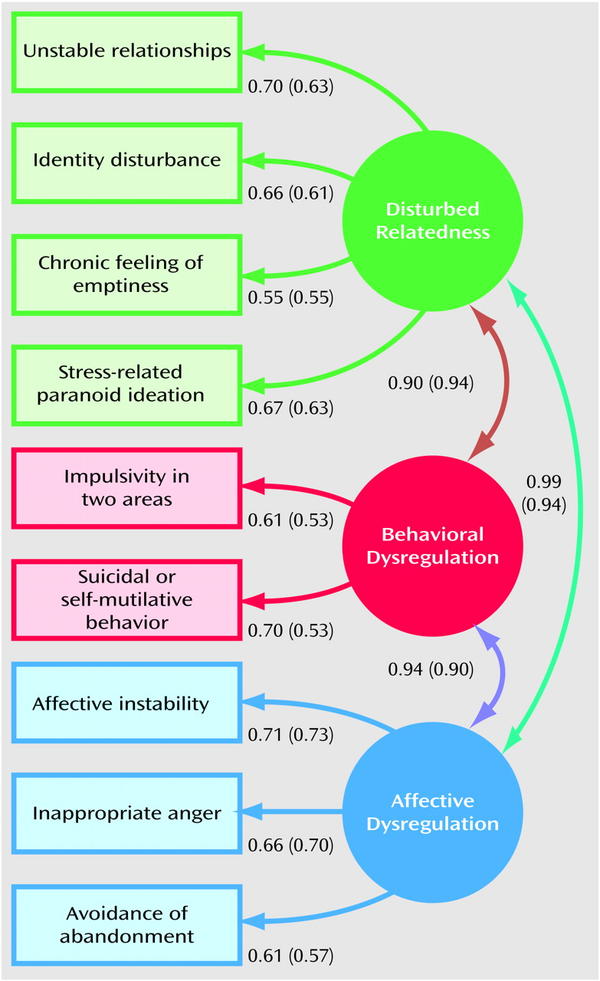 - 2016. - V. 18, No. 6. - P. 30–36.
- 2016. - V. 18, No. 6. - P. 30–36.
5. Simutkin G.G., Yakovleva A.L., Bokhan N.A. The problem of comorbidity of affective disorders and personality disorders (a review of foreign literature) // Social and Clinical Psychiatry. - 2014. - Volume 24, No. 2. — P.91–97.
6. Freud Z. Sadness and melancholy // Psyche: structure and functioning. - M .: Academic project, - 2007. - S. 208-223.
7. American Psychiatric Association: Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association. — 2013.
8. Benazzi F. Major depressive disorder with anger: a bipolar spectrum disorder? // Psychother. Psychosom. - 2003. - Vol.72. - P. 300-306. DOI: 10.1159/000073026
9. Besharat M, Nia M, Farahani H. Anger and major depressive disorder: The mediating role of emotion regulation and anger rumination.- Asian J Psychiatr. - 2013. - Vol.6. - P.35-41. DOI:10.1016/j.ajp.2012.07.013.
10. Dougherty D, Rauch S, Deckersbach T et al.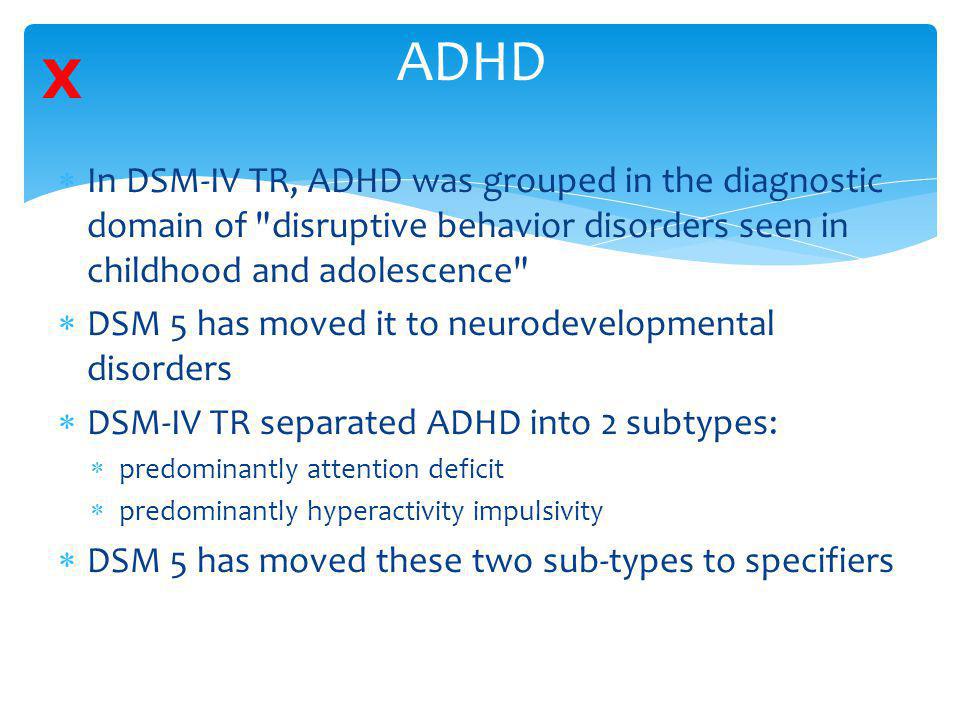 Ventromedial Prefrontal Cortex and Amygdala Dysfunction During an AngerInduction Positron Emission Tomography Study in Patients With Major DepressiveDisorder With Anger Attacks. — Arch Gen Psychiatry. - 2004. - Vol.61. — P.795. DOI:10.1001/archpsyc.61.8.795.
Ventromedial Prefrontal Cortex and Amygdala Dysfunction During an AngerInduction Positron Emission Tomography Study in Patients With Major DepressiveDisorder With Anger Attacks. — Arch Gen Psychiatry. - 2004. - Vol.61. — P.795. DOI:10.1001/archpsyc.61.8.795.
11. Dutton D, Karakanta C. Depression as a risk marker for aggression: A critical review. Aggressive Violent Behav. - 2013. - Vol.18. - P.310-319. DOI:10.1016/j.avb.2012.12.002.
12. Farabaugh A, Sonawalla S, Johnson DP et al. Early improvements in anxiety, depression, and anger/hostility symptoms and response to antidepressant treatment. — Ann Clin Psychiatry. - 2010. - Vol.22. - P.166-171.
13. Farnam A, MehrAra A, Dadashzadeh H, Chalabianlou G, Safikhanlou S. Studying the Effect of Sertraline in Reducing Aggressive Behavior in Patients with Major Depression. - Adv Pharm Bull. - 2017. - vol.7. - P.275-279. DOI:10.15171/apb.2017.033.
14. Fava M, Alpert J, Nierenberg A et al. Fluoxetine Treatment of Anger Attacks: A Replication Study.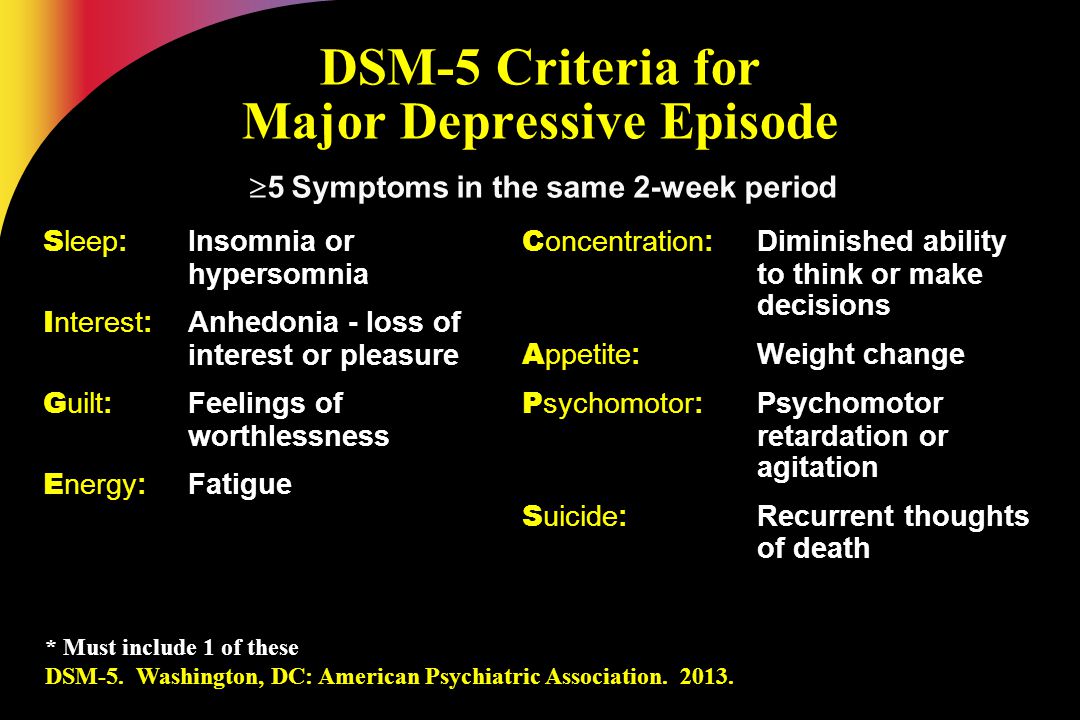 Annals of Clinical Psychiatry. - 1996.-Vol.8. — P.7-10. DOI:10.3109/10401239609149084.
Annals of Clinical Psychiatry. - 1996.-Vol.8. — P.7-10. DOI:10.3109/10401239609149084.
15. "Anger attacks": possible variants of panic and major depressive disorders. — American Journal of Psychiatry. - 1990. - Vol.147. - P.867-870. DOI:10.1176/ajp.147.7.867.
16. Fava M, Anderson K, Rosenbaum J. Are Thymoleptic-Responsive “Anger Attacks” a Discrete Clinical Syndrome? — Psychosomatics. - 1993. - Vol.34. - P.350-355. DOI:10.1016/s0033-3182(93)71869-1.
17. Fava M, Hwang I, Rush A, Sampson N, Walters E, Kessler R. The importance of irritability as a symptom of major depressive disorder: results from the National Comorbidity Survey Replication. — Mol Psychiatry. — 2009. — Vol.15. - P.856-867. DOI:10.1038/mp.2009.20.
18. Fava M, Ménard F, Davidsen C, Baker R. Adjunctive Brexpiprazole in Patients With Major Depressive Disorder and Irritability. — J Clin Psychiatry. - 2016. - Vol.77. - P.1695-1701. DOI:10.4088/jcp.15m10470.
19. Fava M, Nierenberg AA, Quitkin FM et al.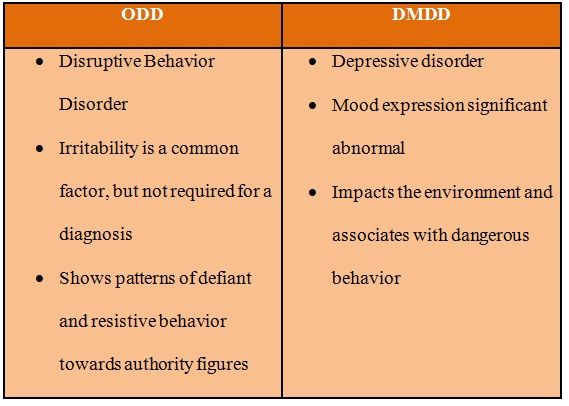 A preliminary study on the efficacy of sertraline and imipramine on anger attacks in atypical depression and dystymia - Psychopharmacol Bull. - 1997. - Vol.33. - P.101-113.
A preliminary study on the efficacy of sertraline and imipramine on anger attacks in atypical depression and dystymia - Psychopharmacol Bull. - 1997. - Vol.33. - P.101-113.
20. Fava M, Rappe S, West J, Herzog D. Anger attacks in eating disorders. — Psychiatry Res. - 1995. - Vol.56. - P.205-212. DOI:10.1016/0165-1781(95)02577-j.
21. Fava M, Rosenbaum J. Anger attacks in depression. Depress Anxiety. - 1998. - Vol.8. — P.59-63. DOI:10.1002/(sici)1520-6394(1998)8:1+<59::aid-da9>3.3.co;2-p.
22. Fava M, Rosenbaum JF. Anger attacks in patients with depression. — J Clin Psychiatry. - 1999. - Vol.60. - P.21-24.
23. Anger attacks in unipolar depression, Part 1: Clinical correlates and response to fluoxetine treatment. — American Journal of Psychiatry. - 1993.-Vol.150. — P.1158-1163. DOI:10.1176/ajp.150.8.1158.
24. Fava M, Rosenbaum JF, McCarthy M, Pava J, Steingard R, Bless E. Anger attacks in depressed outpatients and their response to fluoxetine. - Psychopharmacol Bull.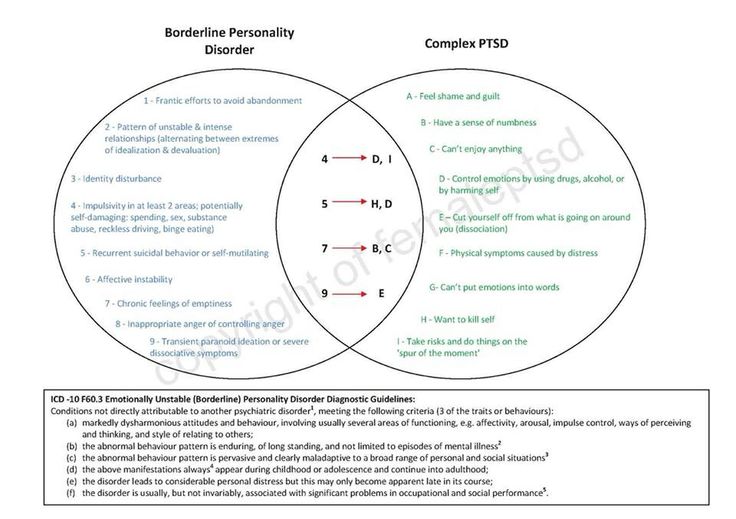 - 1991. - Vol.27. - P.275-279.
- 1991. - Vol.27. - P.275-279.
25. Fava M, Vuolo R, Wright E, Nierenberg A, Alpert J, Rosenbaum J. Fenfluramine challenge in unipolar depression with and without anger attacks. — Psychiatry Res. - 2000. - Vol.94. — P.9-18. DOI:10.1016/s0165-1781(00)00120-7.
26. Goldman L, Haaga D. Depression and the Experience and Expression of Anger in Marital and Other Relationships. — J Nerv Ment Dis. - 1995. - Vol.183. - P.505-509. DOI:10.1097/00005053-199508000-00002.
27. Hollander E, Tracy K, Swann A et al. Divalproex in the Treatment of Impulsive Aggression: Efficacy in Cluster B Personality Disorders. — Neuropsychopharmacology. - 2003. - Vol.28. - P.1186-1197. DOI:10.1038/sj.npp.1300153.
28. Huband N, Ferriter M, Nathan R, Jones H. Antiepileptics for aggression and associated impulsivity. Cochrane Database of Systematic Reviews. — 2010. DOI:10.1002/14651858.cd003499.pub3.
29. Iosifescu D, Renshaw P, Dougherty D et al. Major Depressive Disorder With Anger Attacks and Subcortical MRI White Matter Hyperintensities. — J Nerv Ment Dis. - 2007. - Vol.195. - P.175-178. DOI:10.1097/01.nmd.0000253820.69362.87.
— J Nerv Ment Dis. - 2007. - Vol.195. - P.175-178. DOI:10.1097/01.nmd.0000253820.69362.87.
30. Jakupcak M, Tull M. Effects of Trauma Exposure on Anger, Aggression, and Violence in a Nonclinical Sample of Men. Violence Vict. - 2005. - Vol.20. - P. 589-598. DOI:10.1891/vivi.2005.20.5.589.
31. Joe S, Lee J, Kim S, Won S, Lim J, Ha K. Posttraumatic Embitterment Disorder and Hwabyung in the General Korean Population. — Psychiatry Investig. - 2017. - Vol.14. — P.392. DOI:10.4306/pi.2017.14.4.392.
32. Jones R, Arlidge J, Gillham R, Reagu S, van den Bree M, Taylor P. Efficacy of mood stabilisers in the treatment of impulsive or repetitive aggression: systematic review and meta-analysis. — British Journal of Psychiatry. - 201. - Vol.1198. - P.93-98. DOI:10.1192/bjp.bp.110.083030.
33. Judd L, Schettler P, Coryell W, Akiskal H, Fiedorowicz J. Overt Irritability/Anger in Unipolar Major Depressive Episodes. — JAMA Psychiatry. - 2013. - Vol.70. — P.1171. DOI:10.1001/jamapsychiatry. 2013.1957.
2013.1957.
34. Kennedy H. Anger and Irritability. — British Journal of Psychiatry. - 1992. - Vol.161. - P.145-153. DOI:10.1192/bjp.161.2.145.
35. Kessler R, Coccaro E, Fava M, Jaeger S, Jin R, Walters E. The Prevalence and Correlates of DSM-IV Intermittent Explosive Disorder in the National Comorbidity Survey Replication. — Arch Gen Psychiatry. - 2006. - Vol.63. — P.669. DOI:10.1001/archpsyc.63.6.669.
36. Kovess-Masfety V, Alonso J, Angermeyer M et al. Irritable mood in adult major depressive disorder: results from the world mental health surveys. — Depress Anxiety. - 2013. - Vol.30. — P.395-406. DOI:10.1002/da.22033.
37. Lee J, Wachholtz A, Choi K. A Review of the Korean Cultural Syndrome Hwa-Byung: Suggestions for Theory and Intervention. — Journal of Asia Pacific Counseling. - 2014. - Vol.4. - P.49-64. DOI:10.18401/2014.4.1.4.
38. Linden M. Posttraumatic Embitterment Disorder. — Psychother Psychosom. - 2003. - Vol.72. — P.195-202. DOI:10.1159/000070783.
39. Linden M, Baumann K, Rotter M, Schippan B. Diagnostic criteria and the standardized diagnostic interview for posttraumatic embitterment disorder (PTED). — Int J Psychiatry Clin Pract. - 2008. - Vol.12. — P.93-96. DOI:10.1080/13651500701580478.
40. Maeda K, Sugino H, Akazawa H et al. Brexpiprazole I: In Vitro and In Vivo Characterization of a Novel Serotonin-Dopamine Activity Modulator. — Journal of Pharmacology and Experimental Therapeutics. - 2014. - Vol.350. - P.589-604. DOI:10.1124/jpet.114.213793.
41. Mammen O, Pilkonis P, Chengappa K, Kupfer D. Anger Attacks in Bipolar Depression. — J Clin Psychiatry. - 2004. - Vol.65. - P.627-633. DOI:10.4088/jcp.v65n0506.
42. McGlashan T, Grilo C, Sanislow C et al. TwoYear Prevalence and Stability of Individual DSM-IV Criteria for Schizotypal, Borderline, Avoidant, and Obsessive-Compulsive Personality Disorders: Toward a Hybrid Model of Axis II Disorders. — American Journal of Psychiatry. - 2005. - Vol.162. — P.883-889. DOI:10.1176/appi.ajp.162.5.883.
— P.883-889. DOI:10.1176/appi.ajp.162.5.883.
43. Meshkat D, Kutzelnigg A, Kasper S Winkler D. Ärgerattacken bei Depressionen: Geschlechtsspezifische Aspekte. — Journal für Neurologie Neurochirurgie und Psychiatrie. - 2010. - Vol.11. — P.22-25.
44. Min S. Clinical Correlates of Hwa-Byung and a Proposal for a New Anger Disorder. — Psychiatry Investig. - 2008. - Vol.5. — P.125. DOI:10.4306/pi.2008.5.3.125.
45. Min S, Suh S, Song K. Symptoms to Use for Diagnostic Criteria of Hwa-Byung, an Anger Syndrome. — Psychiatry Investig. — 2009. — Vol.6. — P.7. DOI:10.4306/pi.2009.6.1.7.
46. Morand P, Thomas G, Bungener C, Ferreri M, Jouvent R. Fava's Anger Attacks Questionnaire: evaluation of the French version in depressed patients. — European Psychiatry. - 1998. - Vol.13. - P.41-45. DOI:10.1016/s0924-9338(97)86750-8.
47. Painuly N, Sharan P, Mattoo S. Antecedents, concomitants and consequences of anger attacks in depression. — Psychiatry Res. - 2007. -Vol.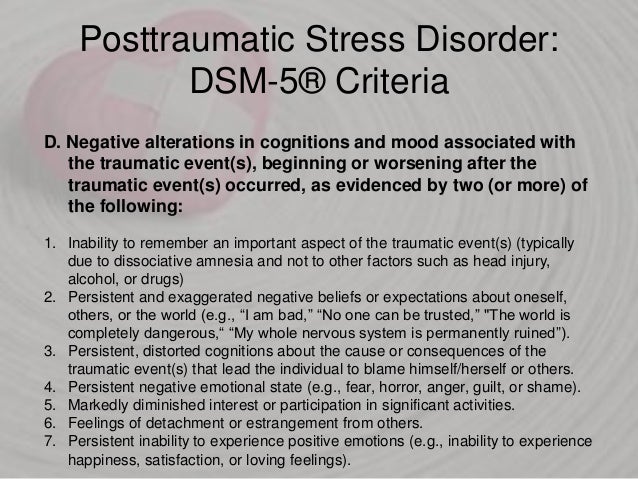 153. - P.39-45. DOI:10.1016/j.psychres.2006.03.001.
153. - P.39-45. DOI:10.1016/j.psychres.2006.03.001.
48. Painuly N, Grover S, Gupta N, Mattoo S. Prevalence of anger attacks in depressive and anxiety disorders: Implications for their construct? — Psychiatry Clin Neurosci. - 2011. - Vol.65. - P.165-174. DOI:10.1111/j.1440-1819.2010.02177.x.
49. Painuly NP, Grover S, Mattoo SK, Gupta N. Anger attacks in obsessive compulsive disorder. - Ind Psychiatry J. - 2011. - Vol.20. - P.115-119. DOI:10.4103/0972-6748.102501.
50. Pasquini M, Picardi A, Speca A et al. Clinical Practice and Epidemiology in Mental Health. - 2007. - Vol.3. — P.3. DOI:10.1186/1745-0179-3-3.
51. Perlis R, Fava M, Trivedi M et al. Irritability is associated with anxiety and greater severity, but not bipolar spectrum features, in major depressive disorder. - Acta Psychiatr Scand. - 2009. - Vol.119. - P.282-289. DOI:10.1111/j.1600-0447.2008.01298.x.
52. Perlis R, Smoller J, Fava M, Rosenbaum J, Nierenberg A, Sachs G. The prevalence and clinical correlates of anger attacks during depressive episodes in bipolar disorder.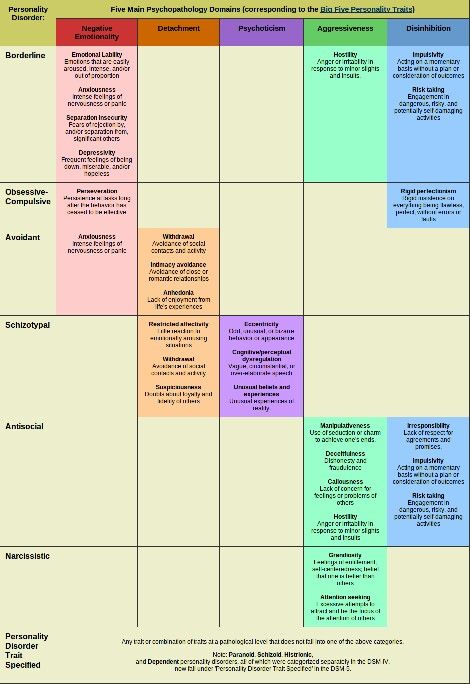 — J Affect Discord. - 2004. - Vol.79. — P.291-295. DOI:10.1016/s0165-0327(02)00451-2.
— J Affect Discord. - 2004. - Vol.79. — P.291-295. DOI:10.1016/s0165-0327(02)00451-2.
53. Rosenbaum JF, Fava M, Pava JA et al. Anger attacks in unipolar depression, Part 2: Neuroendocrine correlates and changes following fluoxetine treatment. — American Journal of Psychiatry. - 1993. - Vol.150. - P.1164-1168. DOI:10.1176/ajp.150.8.1164.
54. Rutz W, von Knorring L, Pihlgren H, Rihmer Z, Wålinder J. Prevention of male suicides: lessons from Gotland study. — The Lancet. - 1995. - Vol.345. — P.524. DOI:10.1016/s0140-6736(95)90622-3.
55. Saini M. A Meta-analysis of the Psychological Treatment of Anger: Developing Guidelines for Evidence-Based Practice. — J Am Acad Psychiatry Law. - 2009. - Vol.37. - P.473-488.
56. Sayar K, Guzelhan Y, Solmaz M et al. Annals of Clinical Psychiatry. - 2000. - Vol.12. - P.213-218. DOI:10.1023/a:1009082409702.
57. Siever L. Neurobiology of Aggression and Violence. — American Journal of Psychiatry. - 2008. - Vol.165. - P.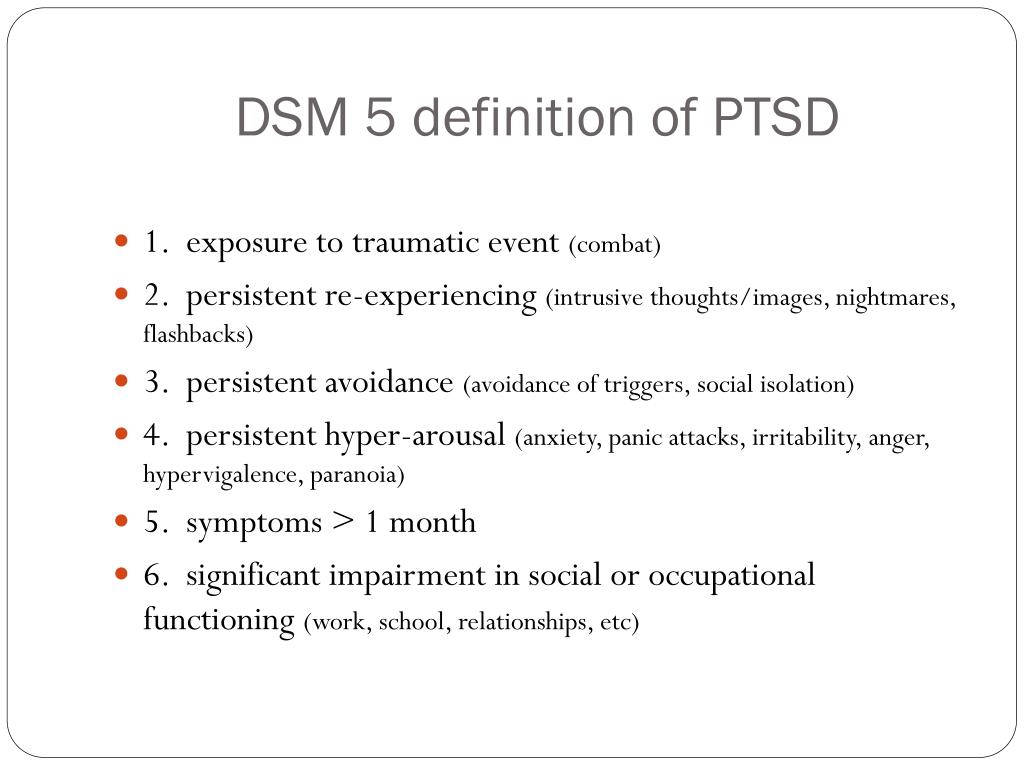 429-442. DOI:10.1176/appi.ajp.2008.07111774.
429-442. DOI:10.1176/appi.ajp.2008.07111774.
58. Van Praag H. Anxiety/aggression-driven depression. Progress in Neuro-Psychopharmacology and Biological Psychiatry. - 2001. - Vol.25. - P.893-924. DOI:10.1016/s0278-5846(01)00151-8.
59. Van Praag H. Faulty cortisol/serotonin interplay. Psychopathological and biological characterization of a new, hypothetical depression subtype (SeCA depression). — Psychiatry Res. - 1996. - 65. - P.143-157. DOI:10.1016/s0165-1781(96)02923-x.
60. Vidal-Ribas P, Brotman M, Valdivieso I, Leibenluft E, Stringaris A. The Status of Irritability in Psychiatry: A Conceptual and Quantitative Review. — Journal of the American Academy of Child & Adolescent Psychiatry. - 2016. - Vol.55. - P.556-570. DOI:10.1016/j.jaac.2016.04.014.
61. Weissman M, Klerman G, Paykel E. Clinical Evaluation of Hostility in Depression. — American Journal of Psychiatry. - 1971. - Vol.128. — P.261-266. DOI:10.1176/ajp.128.3.261.
62. Winkler D, Pjrek E, Kasper S.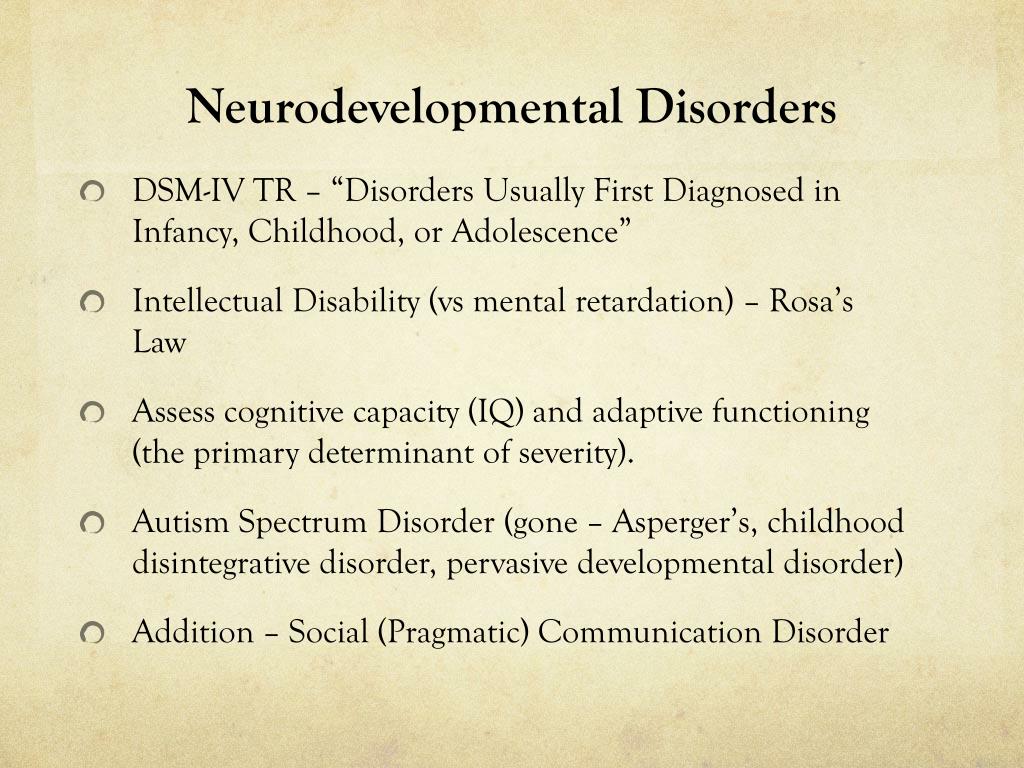 Anger Attacks in Depression - Evidence for a Male Depressive Syndrome. — Psychother Psychosom. - 2005. - Vol.74. - P.303-307. DOI:10.1159/000086321.
Anger Attacks in Depression - Evidence for a Male Depressive Syndrome. — Psychother Psychosom. - 2005. - Vol.74. - P.303-307. DOI:10.1159/000086321.
63. Winkler D, Pjrek E, Kindler J, Heiden A, Kasper S. Validation of a Simplified Definition of Anger Attacks. — Psychother Psychosom. - 2006. - Vol.75. — P.103-106. DOI:10.1159/000090894.
64. Winkler D, Pjrek E, Konstantinidis A et al. Anger attacks in seasonal affective disorder. — Int J Neuropsychopharmacol. - 2005. - Vol.9. –P.215. DOI:10.1017/s1461145705005602.
65. Yoon S, Jeon S, Ko Y et al. Adjunctive Brexpiprazole as a Novel Effective Strategy for Treating Major Depressive Disorder. — J Clin Psychopharmacol. - 2017. - Vol.37. - P.46-53. DOI:10.1097/jcp.0000000000000622.
66. Zaidi U. Gender Difference in Perceived Social Support and Clinical Anger in Depressed Patients. — IOSR Journal of Humanities and Social Science. - 2014. - Vol.19. - P.79-84. DOI:10.9790/0837-191217984.
Borderline personality disorder
The clinical category "borderline personality disorder" is attracting the growing attention of researchers and public health officials around the world.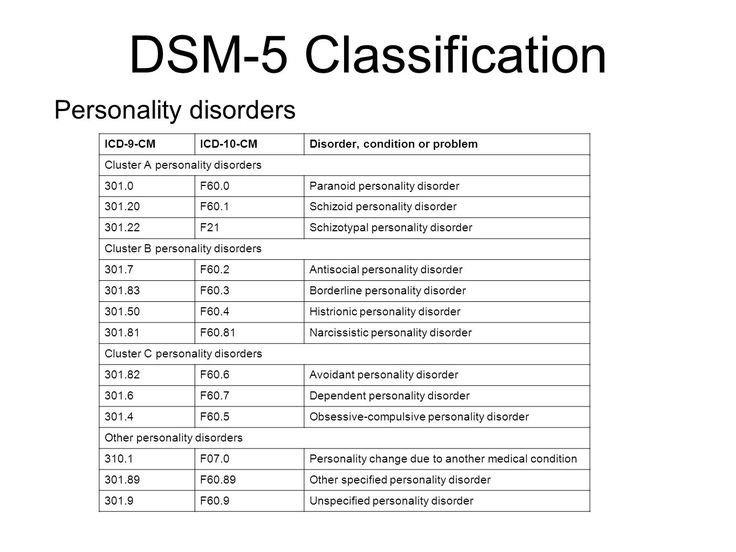
ICD-10. ICD-10 classifies borderline personality disorder as a subset of emotionally unstable personality disorder.
The characteristics of BPD are more clearly defined in the American DSM-5 classification of mental disorders, and therefore the bulk of the world literature on this disorder is based on the DSM-V definition of BPD:
DSM - V . According to the DSM-V, features of borderline personality disorder include marked instability in interpersonal relationships, self-image, emotional instability, and marked impulsivity. All signs of the disorder occur at a young age and manifest themselves in various situations. Diagnosis requires the presence, in addition to the general criteria for a personality disorder, five (or more) of the following:
- Tendency to make excessive efforts to avoid the real or imagined fate of being abandoned. Note: Do not include suicidal behavior and acts of self-harm described in Criterion 5.
- Tendency to engage in intense, tense, and unstable relationships characterized by alternating extremes of idealization and devaluation.
- Identity disorder: marked and persistent instability of the image or feeling of the Self.
- Impulsivity in at least two areas that involve self-harm (eg, spending money, sexual behavior, substance abuse, traffic violations, habitual overeating). Note: Do not include suicidal behavior and acts of self-harm described in Criterion 5.
- Recurrent suicidal behavior, hints or threats of suicide, acts of self-harm.
- Affective instability, very changeable mood (for example, periods of intense dysphoria, irritability or anxiety, usually lasting for several hours and only occasionally for several days or more).
- Constantly experienced feeling of emptiness.
- Inappropriate manifestations of intense anger or difficulty in controlling anger (eg, frequent irritability, persistent anger, repeated fights).