What is residual schizophrenia
What is residual schizophrenia?
Residual schizophrenia was a subtype of schizophrenia in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-4). However, healthcare professionals no longer use these subtypes in diagnosis. The DSM-5 includes several other changes in the diagnostic criteria for schizophrenia.
Healthcare professionals use the DSM-5, which the American Psychiatric Association publishes, to help them diagnose people with certain mental health conditions.
Unlike the DSM-4, the DSM-5 does not list the subtypes of schizophrenia. Due to this, residual schizophrenia is no longer a valid diagnosis.
This article discusses how the changes in the DSM-5 affect the diagnosis and treatment of schizophrenia.
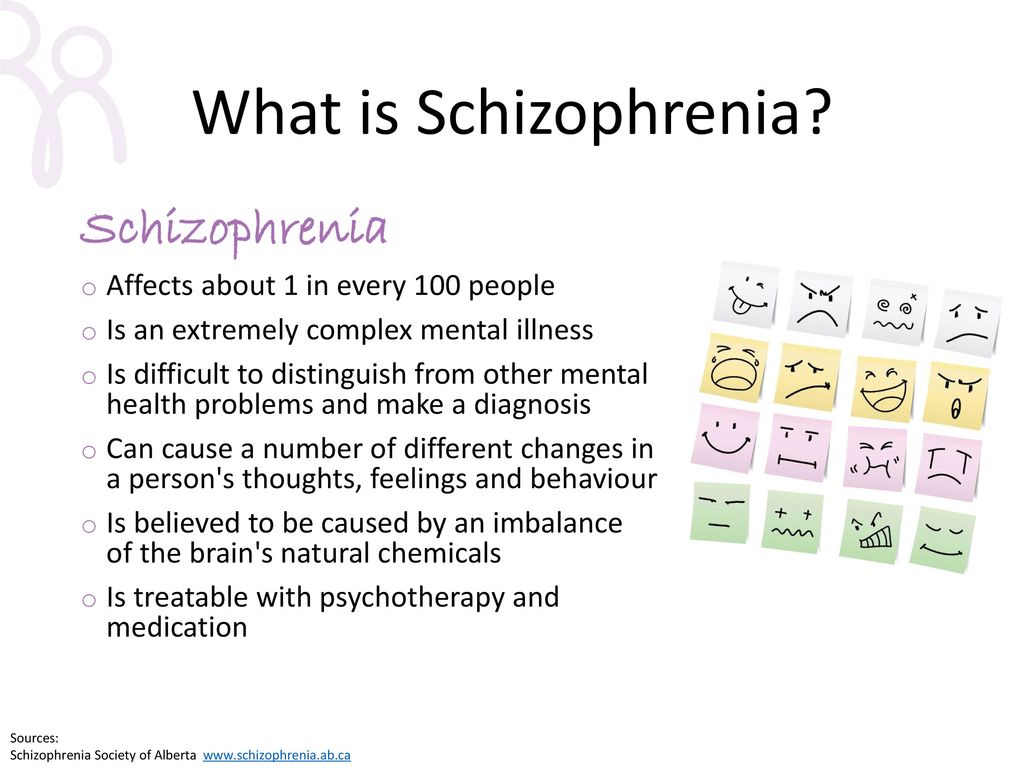
Schizophrenia is a long-term mental health condition that can cause hallucinations, delusions, and altered or disorganized thinking, among other symptoms. It may disrupt a person’s thinking, emotions, and relationships.
The symptoms can present at any time, but on average, they begin in late adolescence and early adulthood.
Learn moreRead the articles below to find out more about schizophrenia.
- Understanding the symptoms of schizophrenia
- What are the different types of schizophrenia?
- What is catatonic schizophrenia?
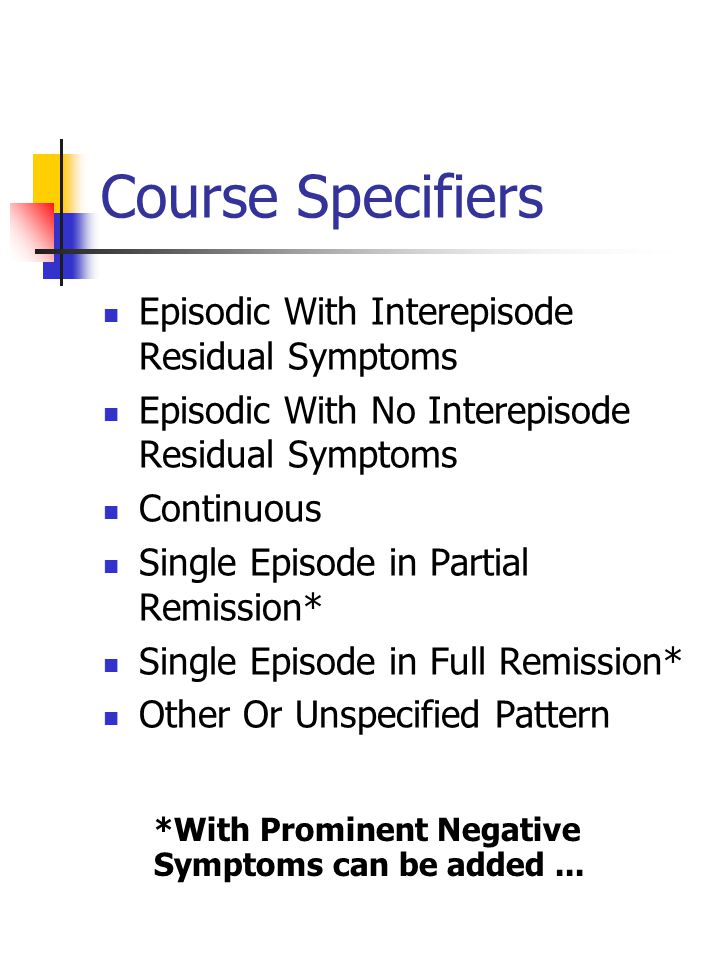
When experts updated the DSM-4 to create the DSM-5, they made several changes to the classification of schizophrenia.
Firstly, they renamed schizophrenia “schizophrenia spectrum disorder.”
Healthcare professionals see this as a more accurate term, as schizophrenia is a variable and complex condition. The symptoms of schizophrenia can vary significantly among individuals.
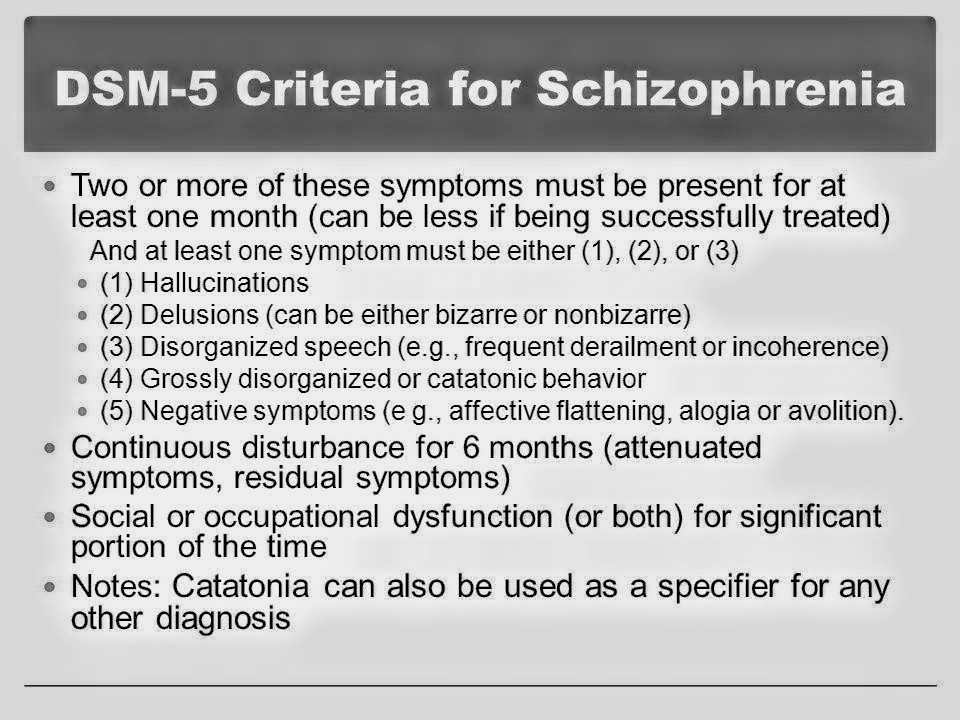
According to the DSM-5, a person must experience certain symptoms to receive a diagnosis of schizophrenia spectrum disorder. These are:
- delusions
- hallucinations
- disorganized speech
- disorganized or catatonic behavior
- negative symptoms, such as not showing feelings or having a complete lack of motivation
A person must experience at least two of these symptoms frequently over 1 month to receive a diagnosis, and one of these symptoms must be delusions, hallucinations, or disorganized speech.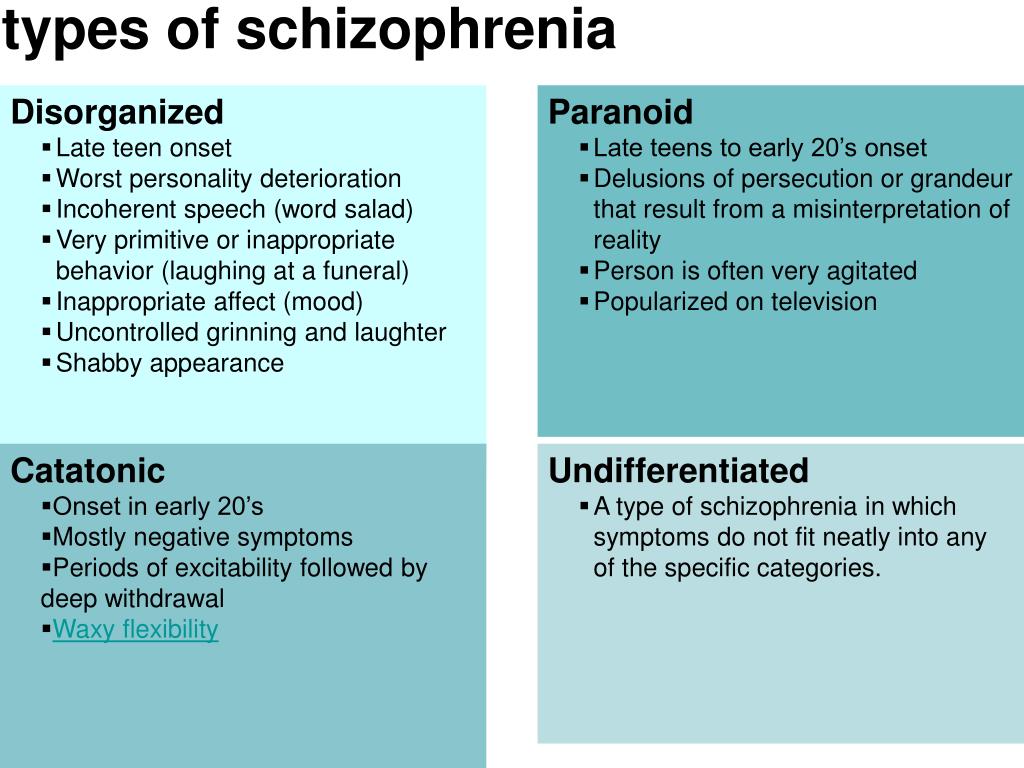
In the older DSM-4, a person could receive a diagnosis if they had one symptom and experienced one of the following:
- bizarre delusions
- auditory hallucinations of a running commentary
- two or more voices talking with each other
However, this additional method of diagnosis is not present in the more recent DSM-5.
These subtypes featured in the DSM-4, allowing doctors to diagnose people with different forms of schizophrenia.
The DSM-5 does not include these subtypes, so healthcare professionals no longer use them to classify schizophrenia.
Residual type
The DSM-4 advises a diagnosis of residual schizophrenia when a person has had at least one schizophrenic episode but is no longer experiencing positive symptoms.
Positive symptoms are symptoms that cause a change in thoughts and behavior, such as:
- delusions
- hallucinations
- disorganized speech or behavior
A person with residual schizophrenia will still have negative symptoms.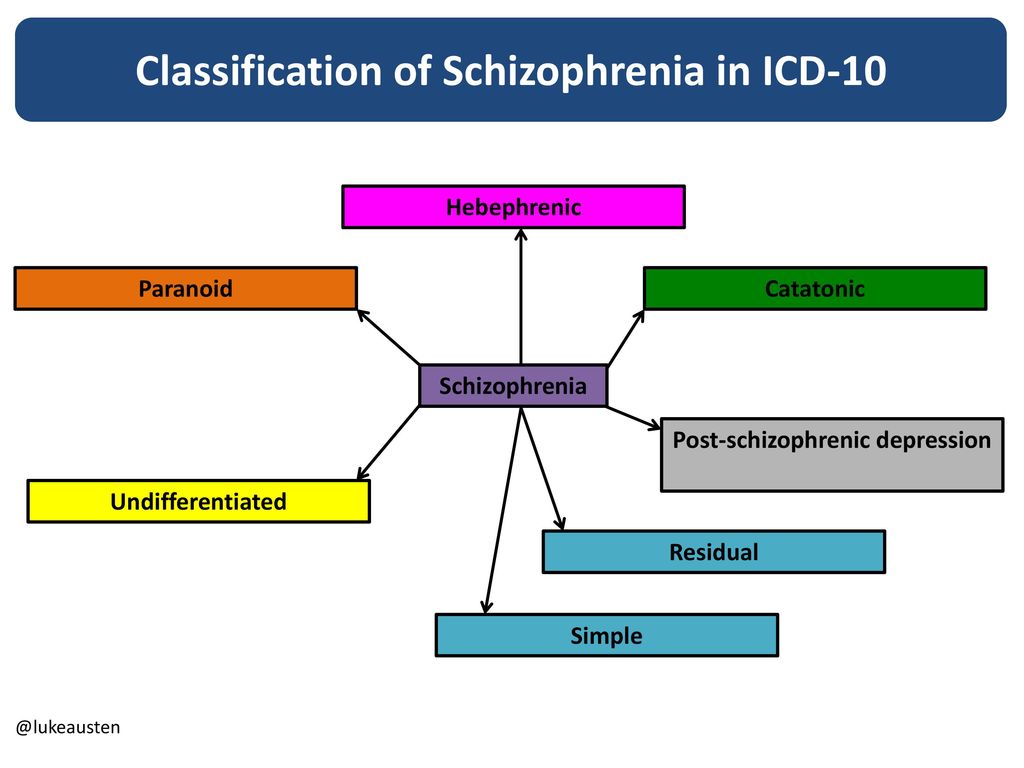 These are symptoms that cause people to withdraw and feel emotionless or flat.
These are symptoms that cause people to withdraw and feel emotionless or flat.
They include:
- flat affect, or not showing emotion
- alogia, or restricted quantity of speech
- avolition, or a total lack of motivation
Catatonic type
In the DSM-4, the criteria for a catatonic schizophrenia diagnosis state that a person must be experiencing at least two of these symptoms:
- lack of movement, being near-unconscious, or holding a rigid posture
- excessive motor activity that seems to have no purpose
- refusal to speak or follow instructions
- placing themselves in inappropriate positions, repeatedly doing purposeless movements, or making exaggerated movements or grimaces
- repeating what other people say or mimicking their movements
Disorganized type
The DSM-4 lists disorganized schizophrenia as a subtype that involves all of the following symptoms:
- disorganized speech
- disorganized behavior
- expressing no emotions or inappropriate ones
Paranoid type
According to the DSM-4, a person likely has paranoid schizophrenia if they exhibit one or more delusions or auditory hallucinations that happen regularly.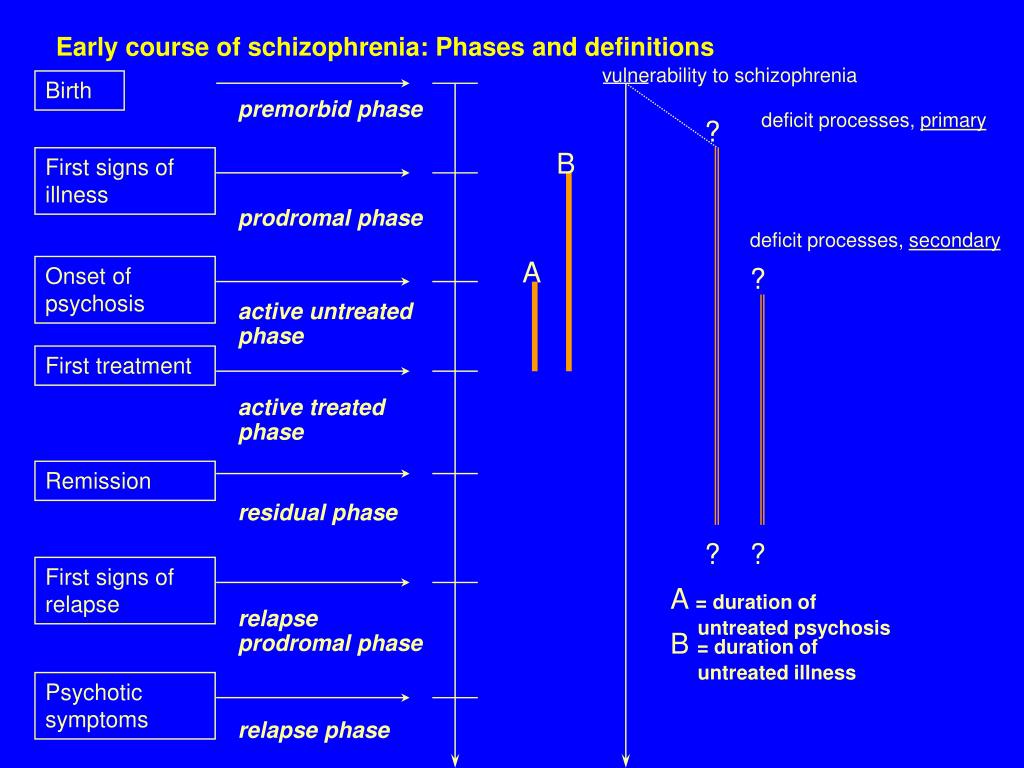
However, the person must have no experience of disorganized speech or behavior, catatonic behavior, or inappropriate or lack of emotions.
Undifferentiated type
In the DSM-4, a person who has undifferentiated schizophrenia meets the criteria for having schizophrenia, but their symptoms do not fit into any of the other subtypes.
The DSM-5 saw the removal of the different schizophrenia subtypes. There were several reasons for their removal, including:
- they did not allow for the variable nature of schizophrenia
- healthcare professionals only used some of the subtypes clinically
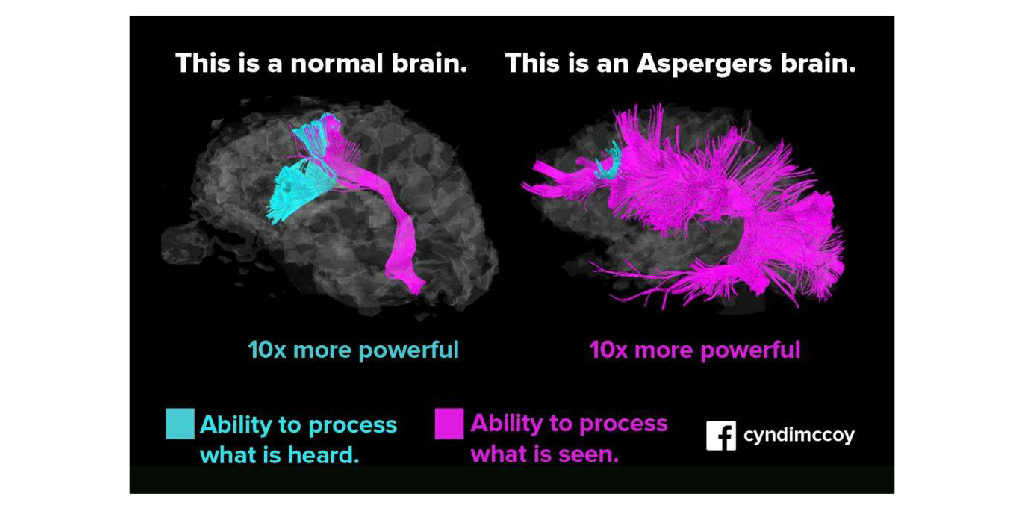
- there were no significant differences in brain function between subtypes
- the subtypes did not predict the course of the condition
- some people did not fit into a subtype based on their symptoms
- scientific reports were no longer using them
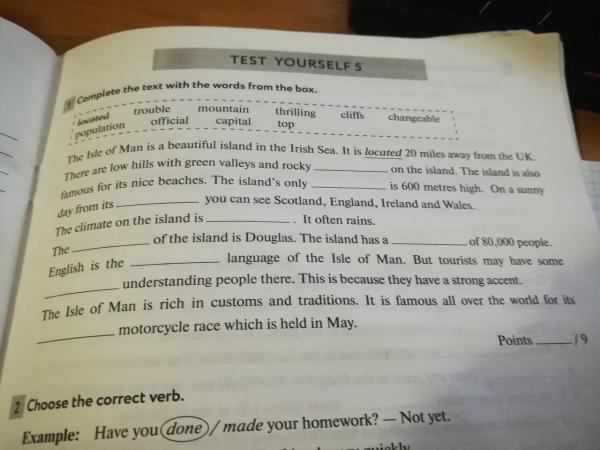
Experts also made several changes to the diagnostic criteria for schizophrenia when they updated the DSM-4 to create the DSM-5.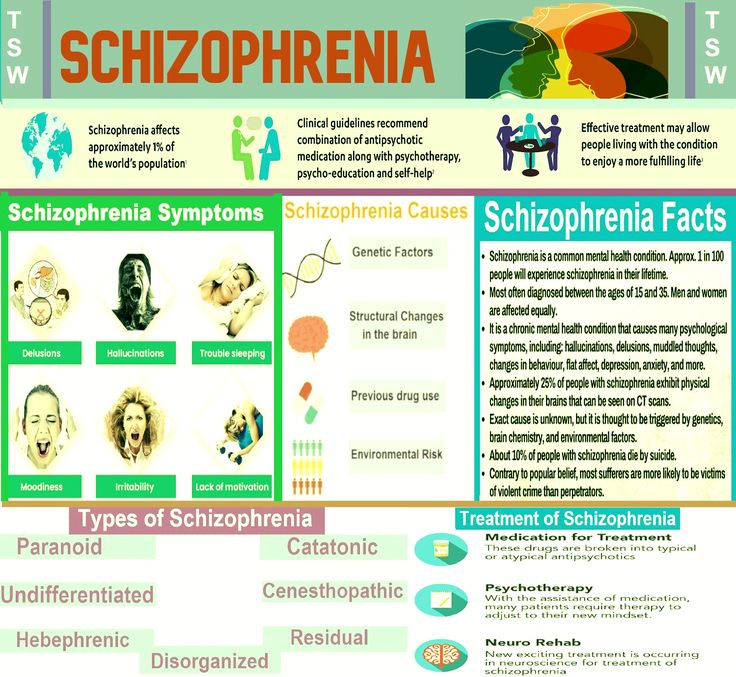
This table shows the major changes in more detail:
Research from 2014 found that more than 99.5% of people whom healthcare professionals diagnosed with schizophrenia using earlier versions of the DSM still met the criteria for it using the DSM-5.
The authors state that the removal of the subtypes was justified, as they did not help predict a person’s response to treatment. They also note that the addition of a symptom severity scale may help healthcare professionals choose the best course of treatment for an individual.
Residual schizophrenia is a subtype of schizophrenia. However, according to the DSM-5, it is no longer a valid diagnosis.
Experts made changes to the criteria for a schizophrenia diagnosis to help healthcare professionals make more accurate diagnoses.
These changes have not affected the number of people who receive a diagnosis of schizophrenia.
Additionally, these changes may lead to improvements in the treatment of schizophrenia symptoms.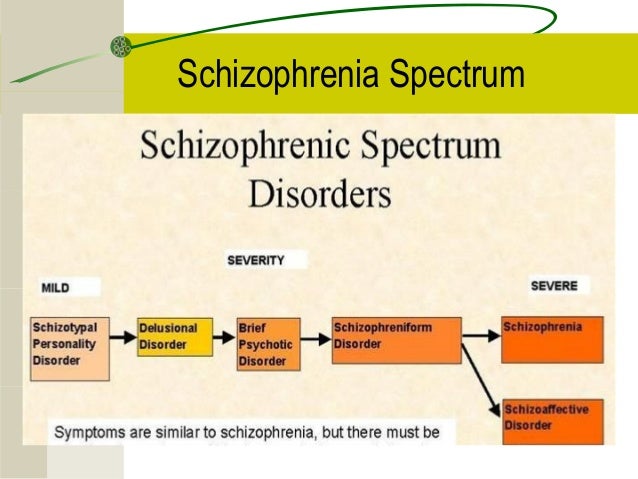
What is residual schizophrenia?
Residual schizophrenia was a subtype of schizophrenia in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-4). However, healthcare professionals no longer use these subtypes in diagnosis. The DSM-5 includes several other changes in the diagnostic criteria for schizophrenia.
Healthcare professionals use the DSM-5, which the American Psychiatric Association publishes, to help them diagnose people with certain mental health conditions.
Unlike the DSM-4, the DSM-5 does not list the subtypes of schizophrenia. Due to this, residual schizophrenia is no longer a valid diagnosis.
This article discusses how the changes in the DSM-5 affect the diagnosis and treatment of schizophrenia.
Schizophrenia is a long-term mental health condition that can cause hallucinations, delusions, and altered or disorganized thinking, among other symptoms. It may disrupt a person’s thinking, emotions, and relationships.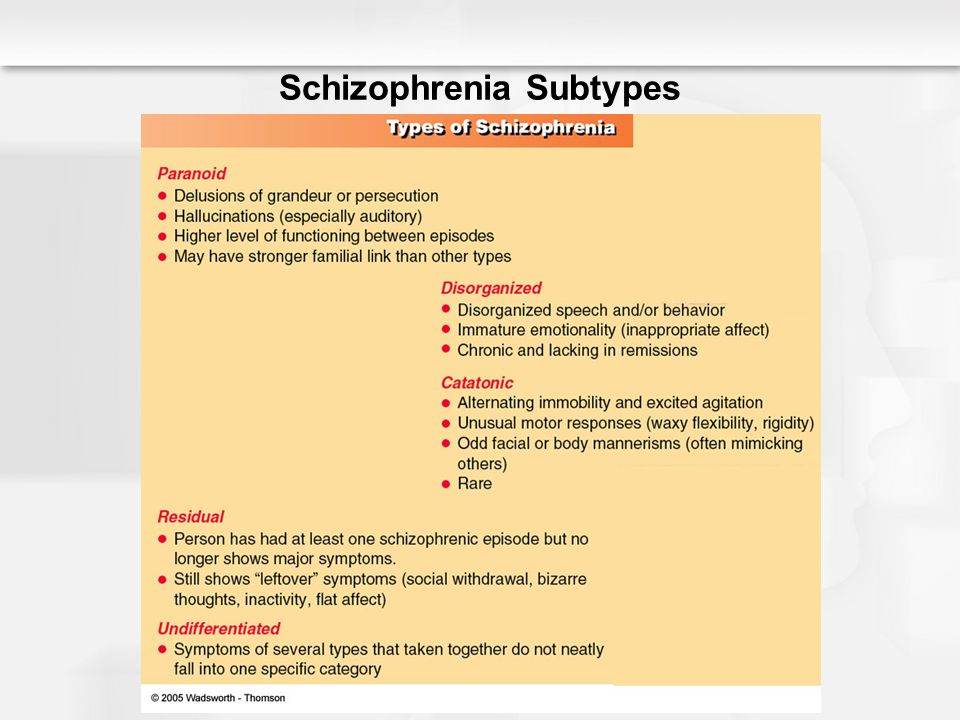
The symptoms can present at any time, but on average, they begin in late adolescence and early adulthood.
Learn moreRead the articles below to find out more about schizophrenia.
- Understanding the symptoms of schizophrenia
- What are the different types of schizophrenia?
- What is catatonic schizophrenia?
When experts updated the DSM-4 to create the DSM-5, they made several changes to the classification of schizophrenia.
Firstly, they renamed schizophrenia “schizophrenia spectrum disorder.”
Healthcare professionals see this as a more accurate term, as schizophrenia is a variable and complex condition. The symptoms of schizophrenia can vary significantly among individuals.
According to the DSM-5, a person must experience certain symptoms to receive a diagnosis of schizophrenia spectrum disorder. These are:
- delusions
- hallucinations
- disorganized speech
- disorganized or catatonic behavior
- negative symptoms, such as not showing feelings or having a complete lack of motivation
A person must experience at least two of these symptoms frequently over 1 month to receive a diagnosis, and one of these symptoms must be delusions, hallucinations, or disorganized speech.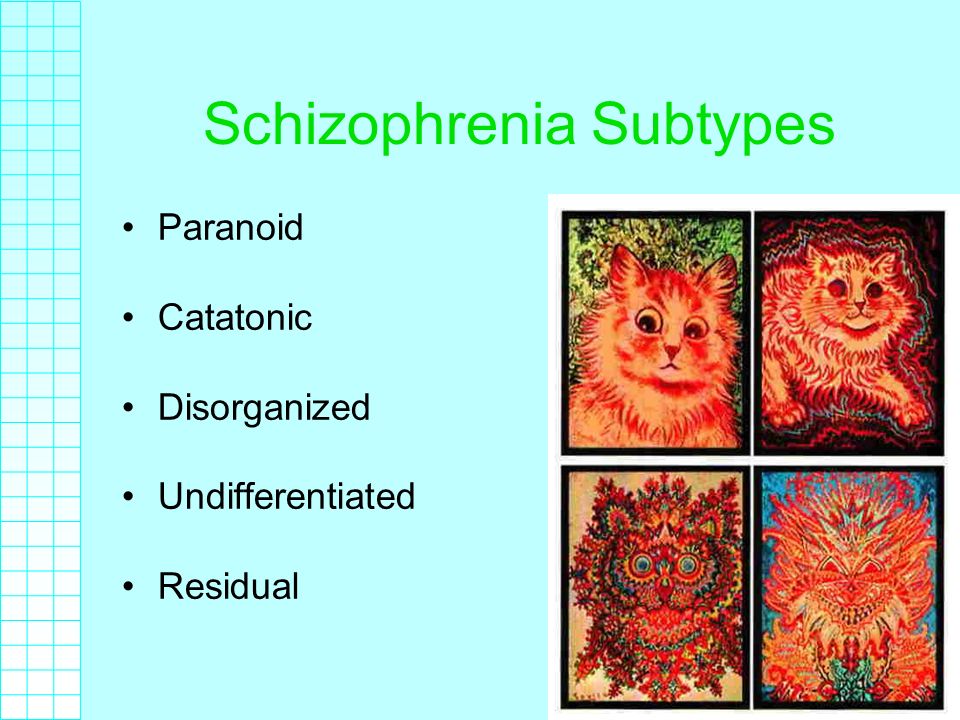
In the older DSM-4, a person could receive a diagnosis if they had one symptom and experienced one of the following:
- bizarre delusions
- auditory hallucinations of a running commentary
- two or more voices talking with each other
However, this additional method of diagnosis is not present in the more recent DSM-5.
These subtypes featured in the DSM-4, allowing doctors to diagnose people with different forms of schizophrenia.
The DSM-5 does not include these subtypes, so healthcare professionals no longer use them to classify schizophrenia.
Residual type
The DSM-4 advises a diagnosis of residual schizophrenia when a person has had at least one schizophrenic episode but is no longer experiencing positive symptoms.
Positive symptoms are symptoms that cause a change in thoughts and behavior, such as:
- delusions
- hallucinations
- disorganized speech or behavior
A person with residual schizophrenia will still have negative symptoms.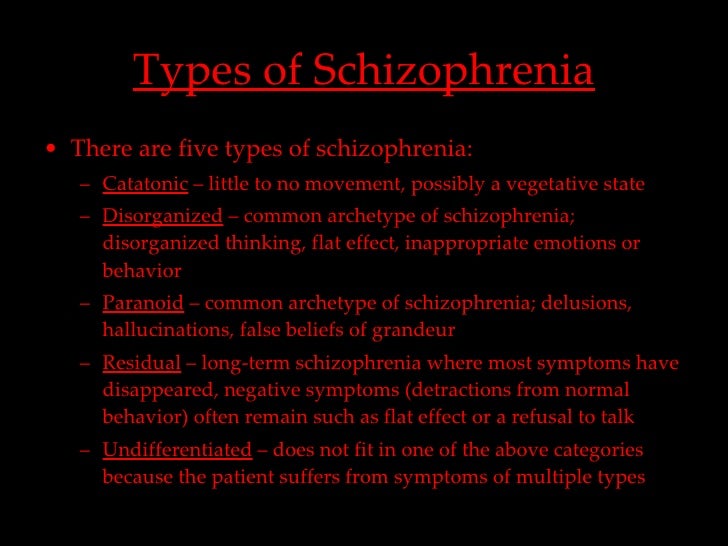 These are symptoms that cause people to withdraw and feel emotionless or flat.
These are symptoms that cause people to withdraw and feel emotionless or flat.
They include:
- flat affect, or not showing emotion
- alogia, or restricted quantity of speech
- avolition, or a total lack of motivation
Catatonic type
In the DSM-4, the criteria for a catatonic schizophrenia diagnosis state that a person must be experiencing at least two of these symptoms:
- lack of movement, being near-unconscious, or holding a rigid posture
- excessive motor activity that seems to have no purpose
- refusal to speak or follow instructions
- placing themselves in inappropriate positions, repeatedly doing purposeless movements, or making exaggerated movements or grimaces
- repeating what other people say or mimicking their movements
Disorganized type
The DSM-4 lists disorganized schizophrenia as a subtype that involves all of the following symptoms:
- disorganized speech
- disorganized behavior
- expressing no emotions or inappropriate ones
Paranoid type
According to the DSM-4, a person likely has paranoid schizophrenia if they exhibit one or more delusions or auditory hallucinations that happen regularly.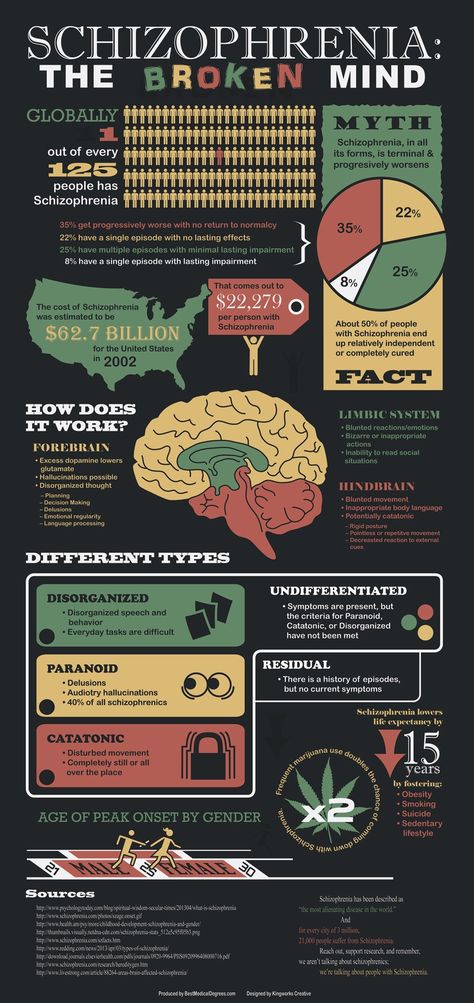
However, the person must have no experience of disorganized speech or behavior, catatonic behavior, or inappropriate or lack of emotions.
Undifferentiated type
In the DSM-4, a person who has undifferentiated schizophrenia meets the criteria for having schizophrenia, but their symptoms do not fit into any of the other subtypes.
The DSM-5 saw the removal of the different schizophrenia subtypes. There were several reasons for their removal, including:
- they did not allow for the variable nature of schizophrenia
- healthcare professionals only used some of the subtypes clinically
- there were no significant differences in brain function between subtypes
- the subtypes did not predict the course of the condition
- some people did not fit into a subtype based on their symptoms
- scientific reports were no longer using them
Experts also made several changes to the diagnostic criteria for schizophrenia when they updated the DSM-4 to create the DSM-5.
This table shows the major changes in more detail:
Research from 2014 found that more than 99.5% of people whom healthcare professionals diagnosed with schizophrenia using earlier versions of the DSM still met the criteria for it using the DSM-5.
The authors state that the removal of the subtypes was justified, as they did not help predict a person’s response to treatment. They also note that the addition of a symptom severity scale may help healthcare professionals choose the best course of treatment for an individual.
Residual schizophrenia is a subtype of schizophrenia. However, according to the DSM-5, it is no longer a valid diagnosis.
Experts made changes to the criteria for a schizophrenia diagnosis to help healthcare professionals make more accurate diagnoses.
These changes have not affected the number of people who receive a diagnosis of schizophrenia.
Additionally, these changes may lead to improvements in the treatment of schizophrenia symptoms.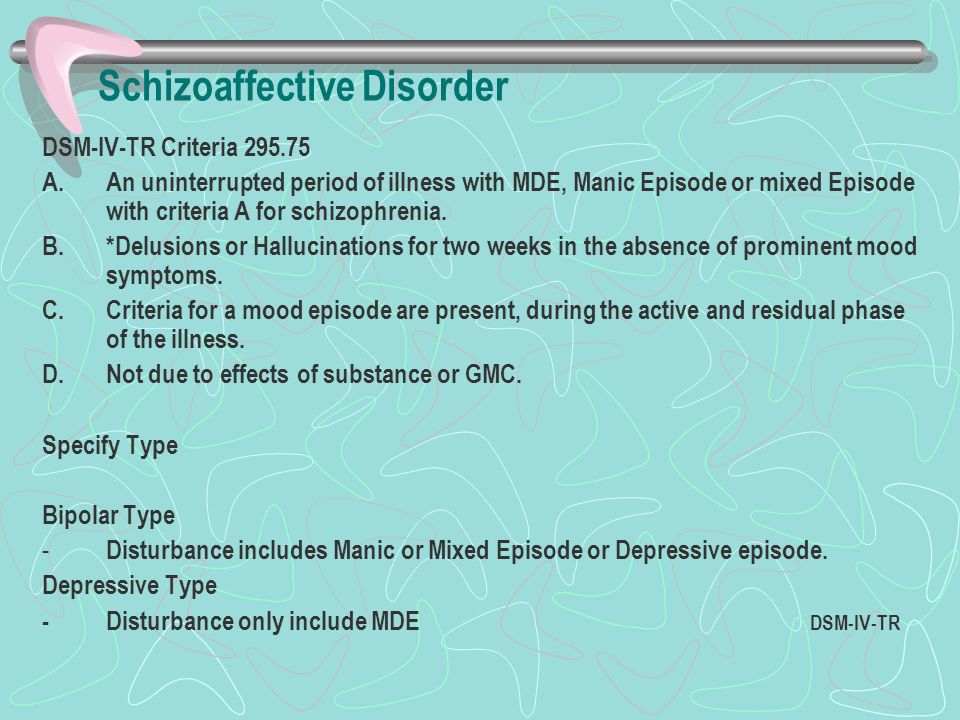
Residual schizophrenia
With residual type of schizophrenia (residual schizophrenia) (F20.5) noted:
- Absence of marked delusions, hallucinations, incoherent thinking, or significantly disorganized behavior;
- Identified stable symptoms of the disease, characteristic of schizophrenia.
Residual schizophrenia
- Weak severity, but persistence of positive symptoms
- Tendency to overvalued formations
- Signs of neurocognitive deficit
- Change in outlook after the first episode of the manifestation of the disease
- Asociality
This category includes cases in which at least one episode of schizophrenia was observed (affective-delusional, catatonic-delusional).
Residual schizophrenia is relatively rare compared to its other forms, only in 2.9% of cases among all patients of a psychoneurological dispensary with a diagnosis of "residual remission" (Smulevich A.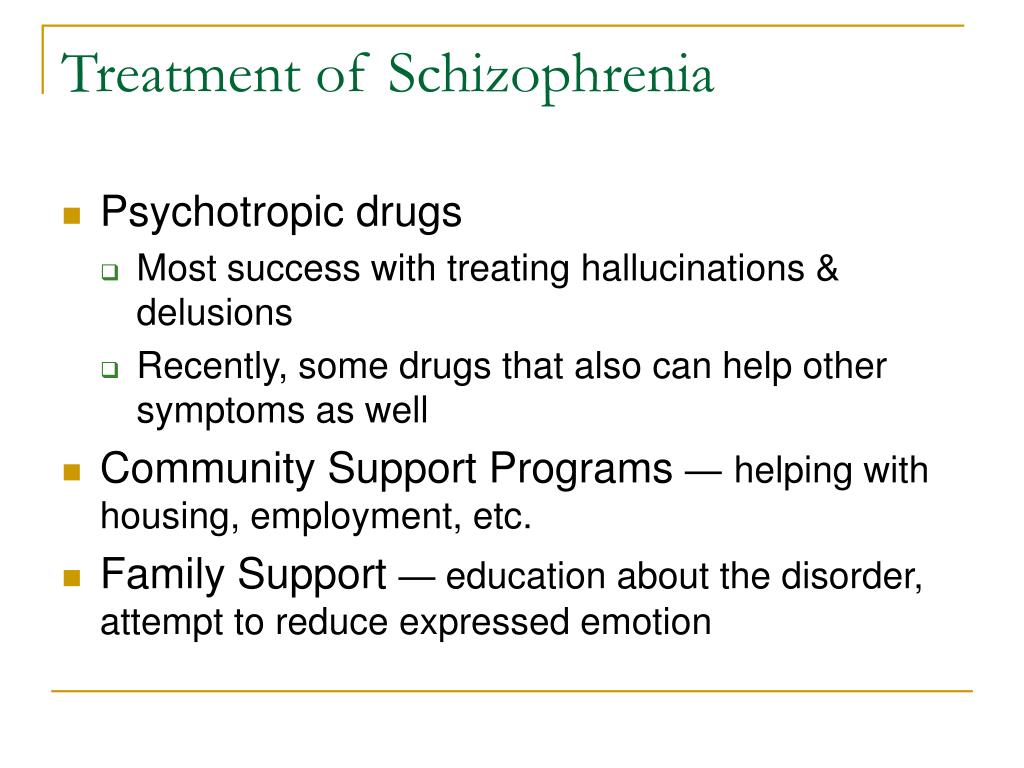 B. et al., 2006).
B. et al., 2006).
There are no pronounced symptoms of psychosis in the clinical picture of residual schizophrenia. Illusions and hallucinations, delusions and catatonic disorders can be minor, rudimentary and not accompanied by vivid affective experiences.
Typical is stable emotional flattening (flat or inadequate affect), social isolation.
The patient is distinguished by eccentric behavior: vagrancy, garbage collection, talking to himself in the presence of strangers, insufficient attention to personal hygiene.
Noteworthy is the compensatory psychological processing by the patient of his experiences.
Noticeably illogical and unclear thinking, reflecting a violation of the associative process, the patient's speech is overloaded with complex expressions or, on the contrary, poor.
The strange beliefs of the patient are noteworthy, which influence his behavior and most often do not coincide with the norms of society. Often there are various superstitions, beliefs in telepathy, overvalued ideas regarding any people or events.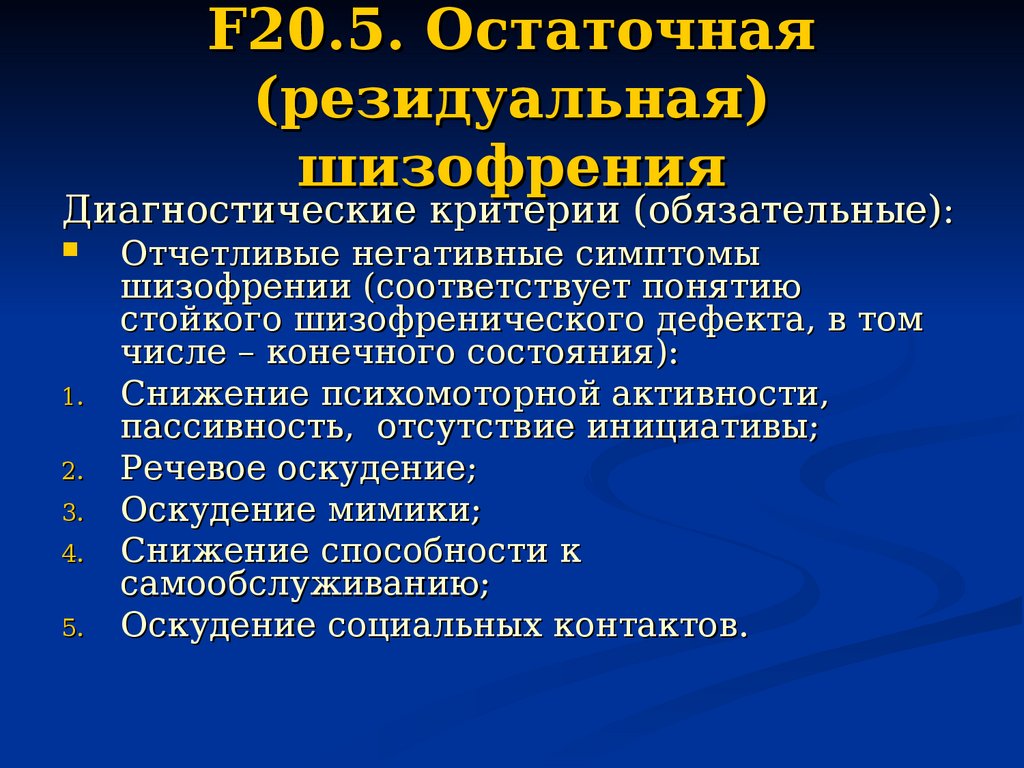
Within the framework of residual schizophrenia, one can speak of a “new” (Mayer-Gross W., 1920) or “second” (Vie J., 1939) life of a patient after an acute psychotic episode. Here there is a cardinal change in worldview, accompanied by a change in lifestyle after the experienced psychosis.
Personality changes are characterized by "acquired" schizoidization, mental weakness, manifested by passivity, increased fatigue, vulnerability, and a sense of insecurity.
The development of a personality according to the “new life” type is characterized by the appearance in adulthood of hobbies that are completely inconsistent with the previous interests, often acquiring the character of professional activity (healers, psychics, etc.) and leading to the rejection of the former way of life. Such personality development occurs as part of the stabilization of a pathological process that does not require active pharmacotherapy and is comparable to syndromic remission in schizophrenia (Andreasen N.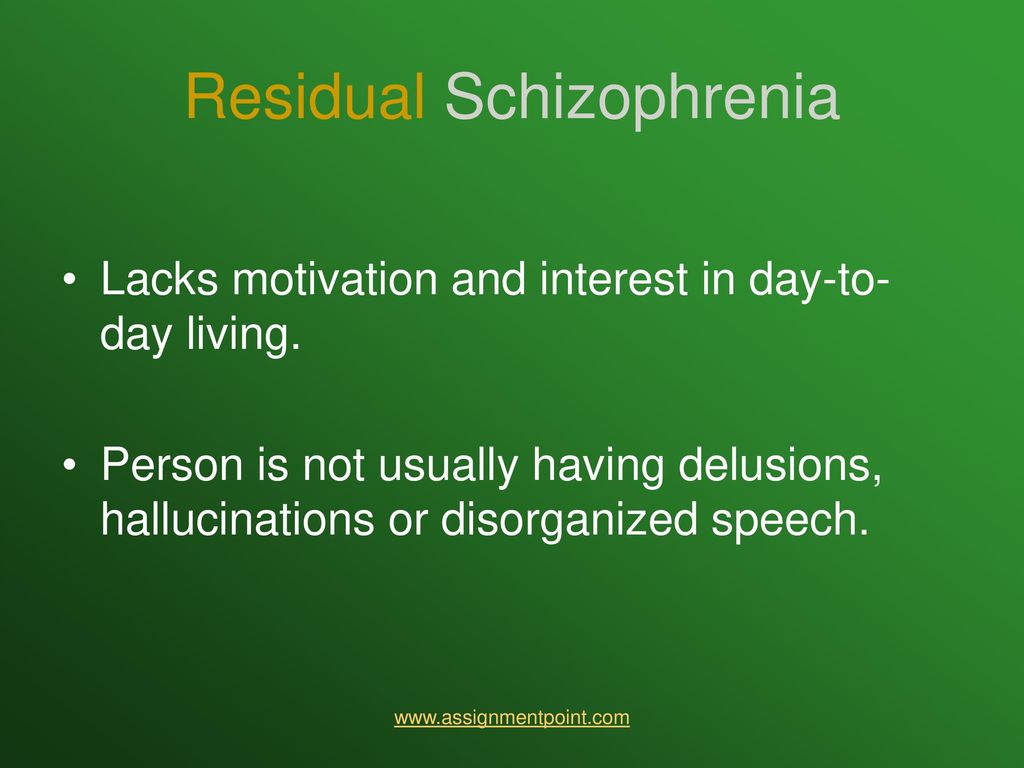 et al., 2005).
et al., 2005).
According to L.K. Pavlova and N.A. Ilyina (2007), the “soil” for a “new life” can be persistent long-term hypomania replacing post-attack depression, as well as personality changes of the Verschrobene type: strange behavior with signs of “regressive syntonicity”; a decrease in intelligence and the level of professional adaptation with the formation of pragmatism and practical social attitudes; amplification of the premorbid tendency to overvalued formations.
The course of residual schizophrenia is usually chronic.
Personality changes are especially noticeable during the period of exacerbation of somatic diseases or stay in psychotraumatic situations.
According to ICD-10, the group of schizophrenia spectrum disorders also includes schizotypal disorder (F21), temporary acute psychotic disorder (F23), schizoaffective disorder (F25), other inorganic psychotic disorders (F28) and some other psychotic conditions that manifest themselves with some symptoms schizophrenia.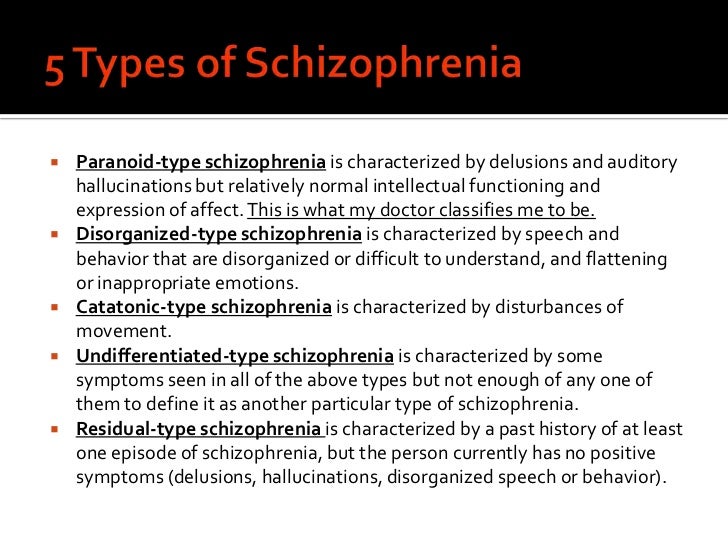
Back to Contents
Residual schizophrenia: signs, treatment - Encyclopedia Ochkov.net
Schizophrenia is an unpredictable mental illness that can occur in different forms. Some patients have only one or two seizures in their entire lives, while others lose touch with reality in a matter of months. Some types of pathology develop rapidly, and some of them progress over the years. Residual schizophrenia belongs to the second type. It is characterized by a long period of negative phase. In the article we will consider what are its features.
In this article
- General data
- Residual schizophrenia
- Causes
- Symptoms
- Diagnosis and treatment
- Forecast
General data
Schizophrenia is a polymorphic endogenous disease that affects the human mental apparatus. Polymorphism says that it occurs in different forms. The reason for its origin is the internal state of the psyche, so we are talking about endogenous nature.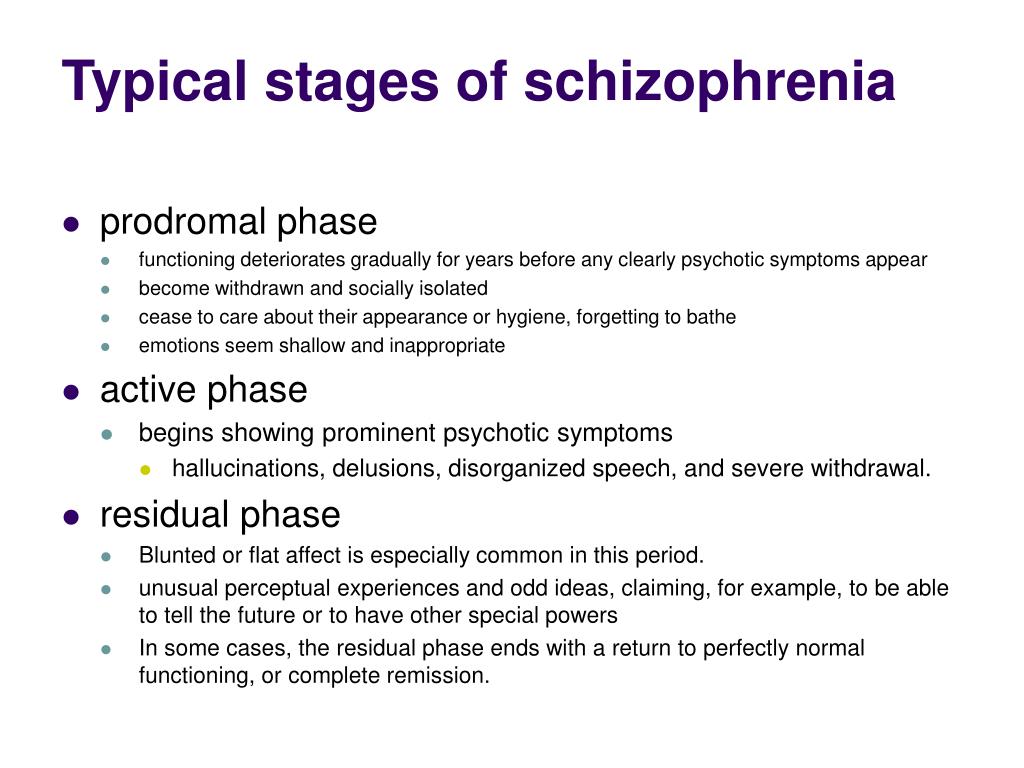 As for the direct impact on a person, schizophrenia affects the brain, and more precisely, thinking and emotional reactions.
As for the direct impact on a person, schizophrenia affects the brain, and more precisely, thinking and emotional reactions.
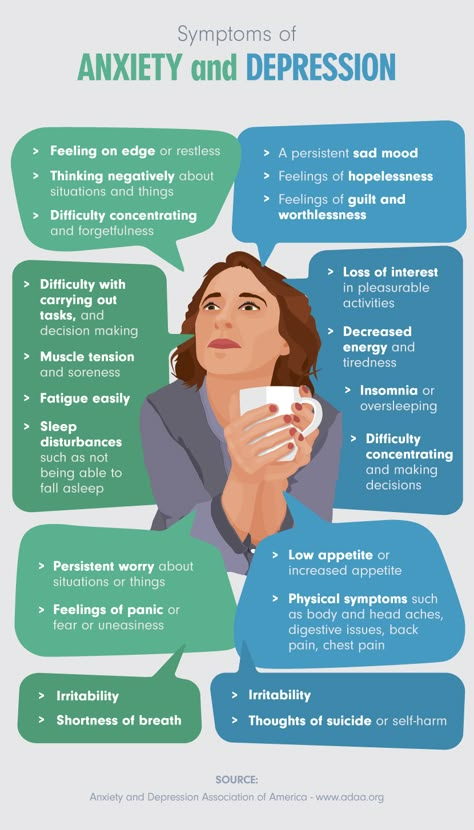
This psychopathology is detected in approximately 1% of people. The peak incidence occurs at 20-28 years of age in men, and at 26-32 years of age in women. However, schizophrenia is also diagnosed in children, as well as in the elderly. At the same time, it is often combined with anxiety disorders, depression, alcoholism and drug addiction, so it is not always possible to identify the disease at an early stage.
Many people think that schizophrenia is a split personality disorder. Others believe that it is always accompanied by hallucinations. In fact, "split personality" is too simple a wording for such a complex disease. With schizophrenic disorders, there is a disintegration of personal qualities and a person's loss of connection with reality.
If we talk about hallucinations, then they do not occur with every type of pathology.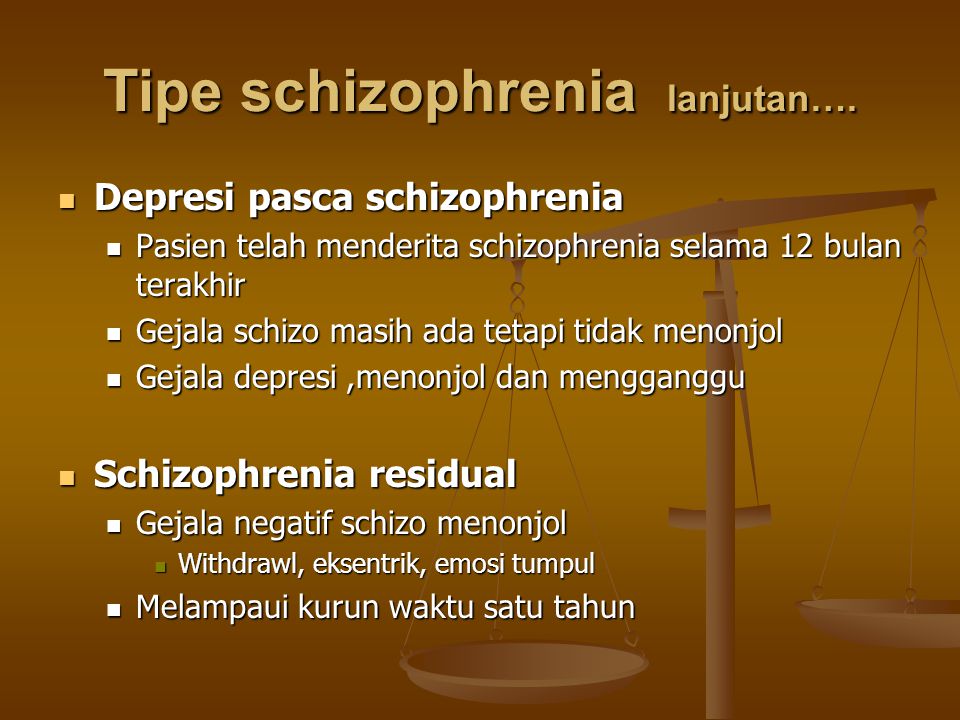 Moreover, the presence of this symptom may not indicate a disease of the schizophrenia spectrum. Residual schizophrenia refers to those forms in which hallucinations are extremely rare.
Moreover, the presence of this symptom may not indicate a disease of the schizophrenia spectrum. Residual schizophrenia refers to those forms in which hallucinations are extremely rare.
Residual schizophrenia
Residual schizophrenia is also called residual. It is registered after exacerbations (attacks) and is characterized by stable remission without pronounced signs of psychosis. Although it may be asymptomatic, it is also impossible to say that a person is completely healthy in this condition.
The patient does not have hallucinations or delusions, but his behavior is very passive and uninitiated. The patient may say that he is all right. However, relatives, as a rule, are concerned about his behavior and are very worried. They have cause for concern, since the disease can worsen at any time, despite the fact that sometimes a person stays in this state for years without any signs of psychosis.
Residual schizophrenia is rare - only 2.
6% of patients.
Treatment is carried out not only during attacks, but also during remission. The further development of pathology depends on its quality.
Causes
Nothing is known for sure about the causes of any schizophrenia. Scientists have not yet been able to describe the mechanism for the development of pathology. It has only been established that its focus is in the brain, but what exactly causes it to occur and how it progresses remains a mystery.
Physicians have at their disposal a group of factors that can hypothetically provoke schizophrenia:
- Genetic predisposition. The likelihood of developing psychopathology increases if it was detected in relatives. The closer the relationship, the higher the risk. A child with two schizophrenic parents has less than a 50% chance of avoiding the disease.
- Anomalies of the brain. MRI shows that in schizophrenic disorders there is an increase in the ventricles, atrophy of the hippocampus, temporal lobes and other areas.
- Problems arising from the bearing of the fetus. We are talking about injuries, infections, unhealthy lifestyle of the mother, complicated childbirth and birth trauma.
- Social conditions. In families where there are alcoholics, drug addicts, psychopaths and other antisocial personalities, children can develop schizophrenia, psychopathy, schizoaffective disorder and other diseases. He definitely cannot avoid psychological trauma.
- Education. As a rule, schizophrenics appear in families with despotic parents or, on the contrary, in conditions of permissiveness. Also, the likelihood of developing psychopathologies increases if no one takes care of the child at all and no one loves him.
- Dependencies. Alcohol, drug addiction and smoking are not the direct culprits of schizophrenia, but they can serve as an impetus for its development. If a person began to use psychoactive substances in childhood, then the risks increase markedly.
Injuries, acute or chronic stress, prolonged depression, etc.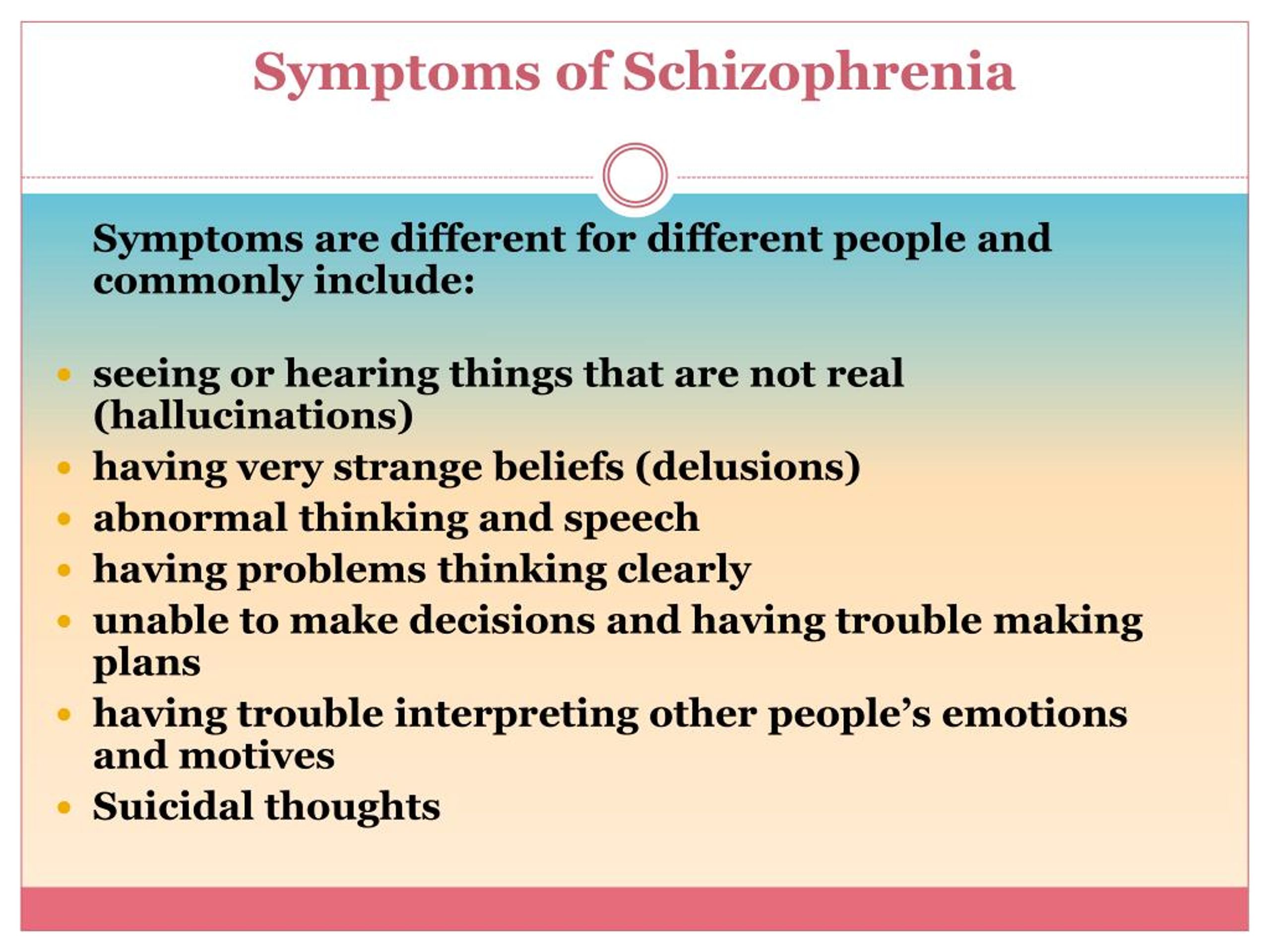 can also lead to schizophrenia or its exacerbation. The patient's medical history is carefully studied, but it is far from always possible to draw a direct link between a particular event and an attack of psychopathology.
can also lead to schizophrenia or its exacerbation. The patient's medical history is carefully studied, but it is far from always possible to draw a direct link between a particular event and an attack of psychopathology.
Symptoms
Any form of schizophrenic disorder has two sets of symptoms - positive and negative. The former are called so not because “they are good, but because they are the result of the activity of the psyche. Typical signs of productive symptoms are hallucinations and delusions.
In such a state of psychosis, the patient may be inadequate. Moreover, in most cases, he does not realize that he is sick, even if he sees grandiose and fantastic hallucinations.
The nature of hallucinations is individual. Some hear voices, while other patients see or touch objects that do not exist in reality.
With residual schizophrenia, there are usually no such symptoms.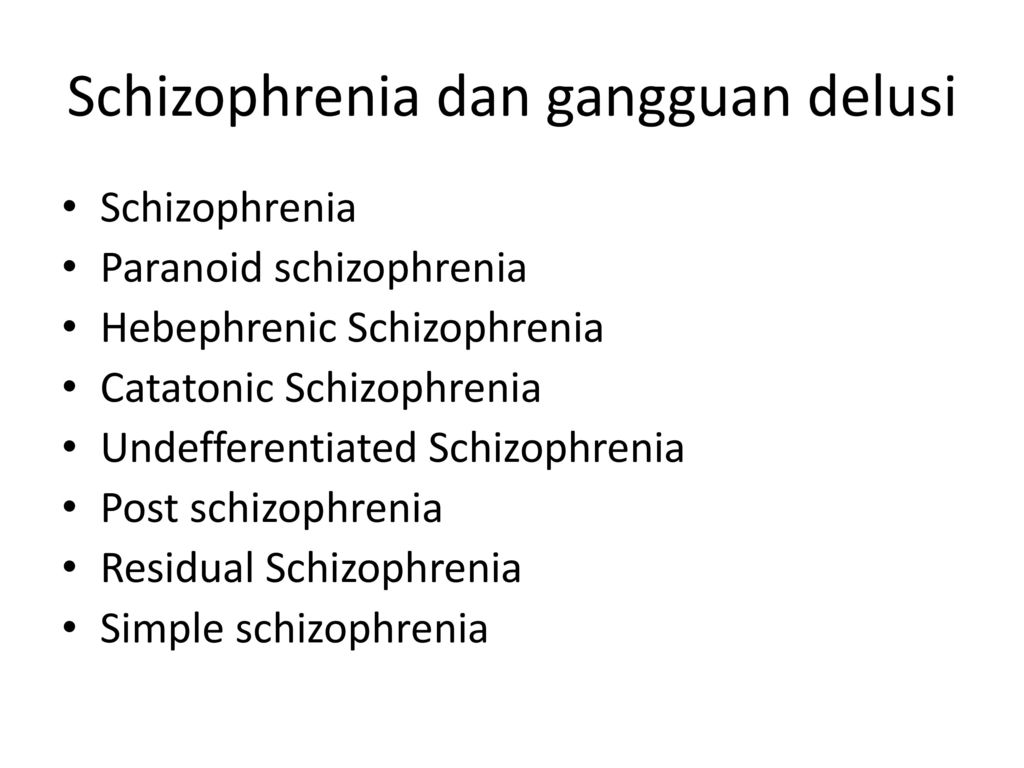 The patient is in a negative phase, which is revealed when the mental apparatus is passive. The main manifestations of residual schizophrenic disorder are:
The patient is in a negative phase, which is revealed when the mental apparatus is passive. The main manifestations of residual schizophrenic disorder are:
- No signs of psychosis for 1 year or more. This period is considered as a remission.
- Decreased motivation. A person wants nothing and strives for nothing. He is not even interested in activities that used to bring pleasure.
- Emotionlessness. The patient may not respond to others and circumstances, including dramatic and difficult situations.
- Fatigue, weakness, both physical and moral, prostration. The patient will only take up something, as soon as he gets tired. The performance is almost nil.
- Closure. With residual schizophrenia, a person does not want to communicate with anyone, he strives for loneliness, his speech is empty and meaningless. He often tries not to speak at all.
- Poor hygiene. Over time, the patient ceases to take care of himself - to wash, shave and wash clothes.
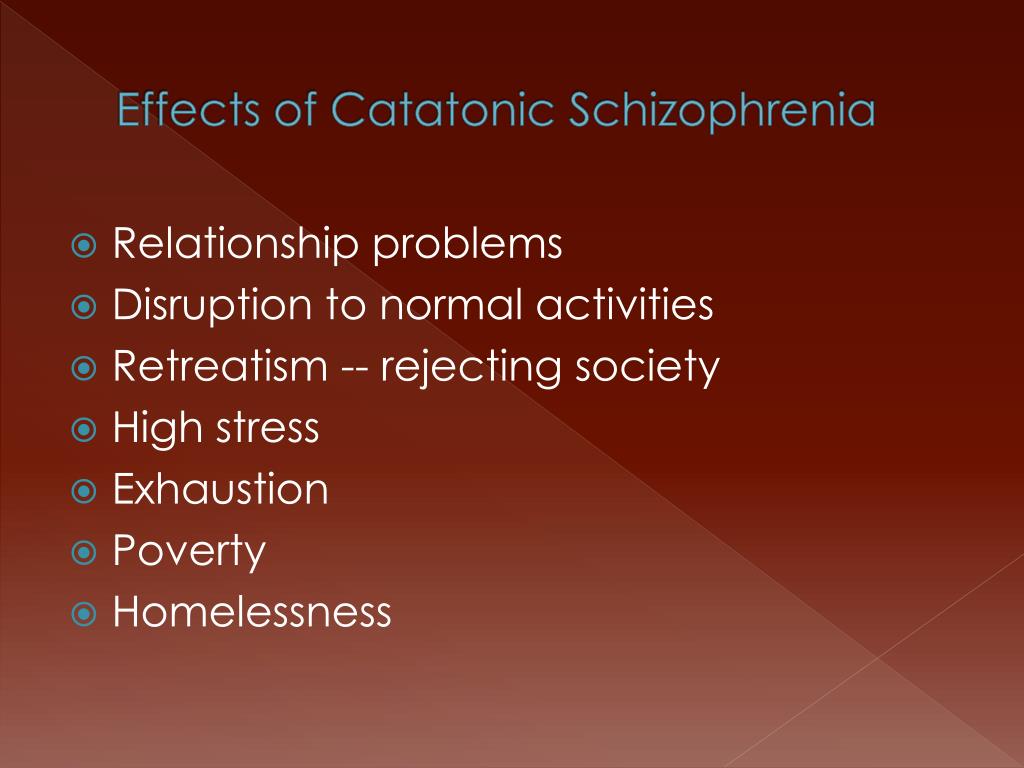 Outwardly, he looks untidy, but he does not care.
Outwardly, he looks untidy, but he does not care. - Strange behavior. The patient may talk loudly to himself in the presence of others, wander, pick up garbage and bring it home (pathological hoarding).
- Superstition. It is possible to believe both in the supernatural and in perfect absurdities, super-ideas, telepathy, etc.
To make a diagnosis of residual schizophrenia, four of the following must be observed. This requires the absence of organic brain damage, dementia and chronic depression, which are also characterized by negative symptoms.
Delusions, illusions, catatonia and hallucinations may occur in residual schizophrenia, but they are mild and do not cause vivid emotional experiences.
A person can be in remission for more than a year, but exacerbation is possible at any time.
Then positive symptoms will appear, and probably even more intensely than during the last attack.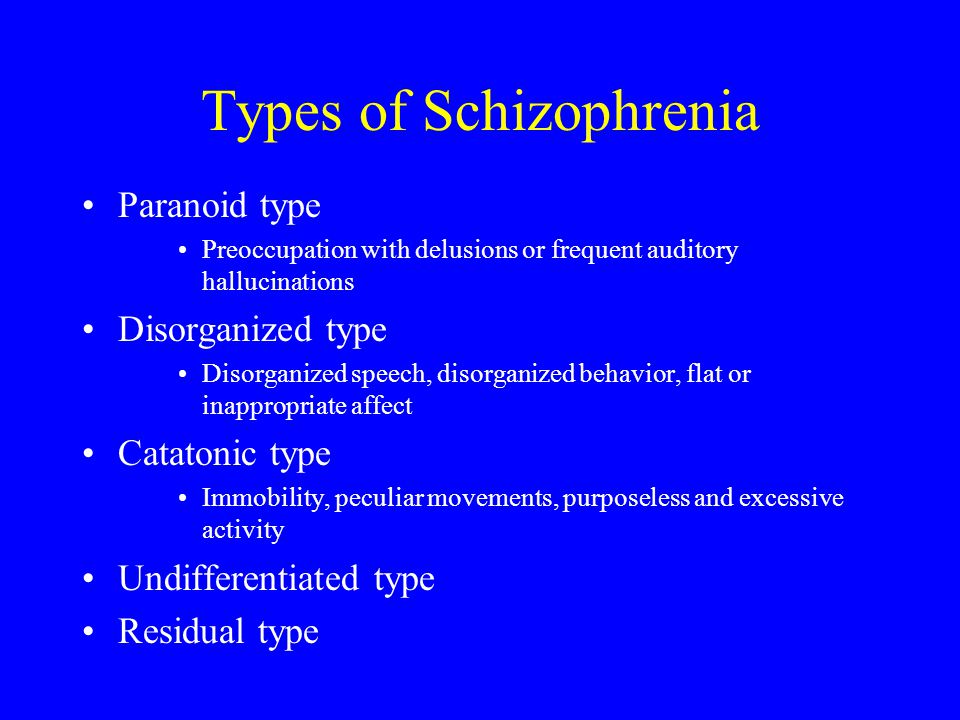 But it depends on how well the patient follows the doctor's recommendations, as well as on the timeliness of therapy when the condition worsens.
But it depends on how well the patient follows the doctor's recommendations, as well as on the timeliness of therapy when the condition worsens.
Diagnosis and treatment
Diagnosis in schizophrenia, like treatment, is not interrupted even during remission. The patient must periodically visit a psychiatrist and undergo certain studies. Thanks to this, you can notice signs of exacerbation at the initial stage. The same applies to therapy. In fact, after a diagnosis of schizophrenia is made, a person becomes a patient for the rest of his life, regardless of how often seizures occur and whether they happen, in principle.
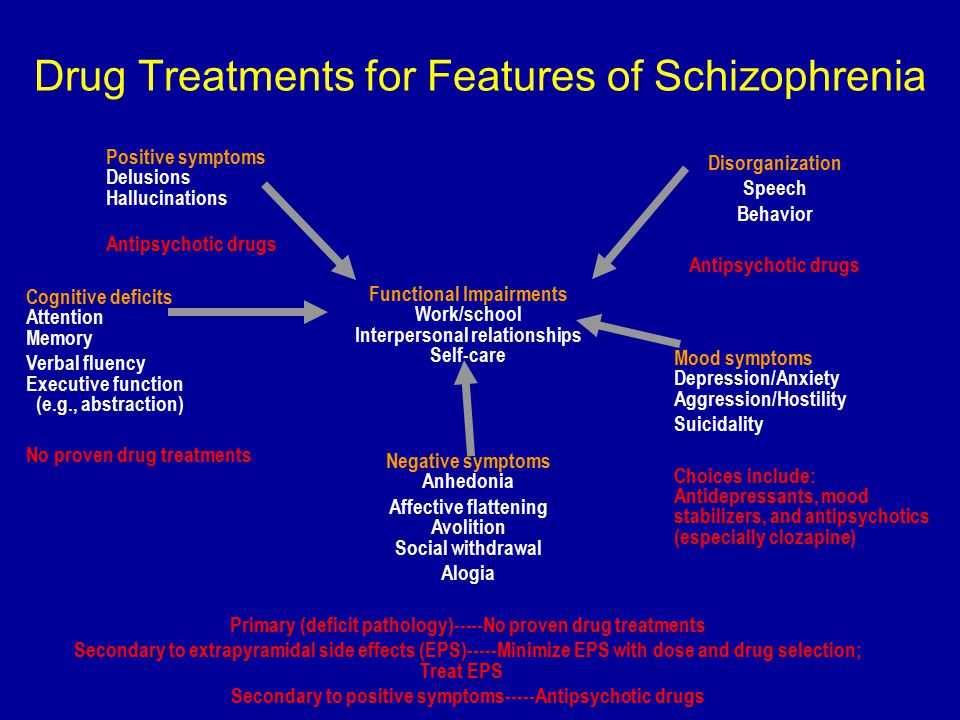
Treatment methods for exacerbation and remission are somewhat different. The following medications and techniques are used for residual schizophrenia:
- Taking antipsychotic drugs. Their task is to restore dopamine activity, which falters in schizophrenic diseases. With negative symptoms, the production of dopamine is insufficient, so the person is passive.
- Taking antidepressants. With their help, it turns out to activate the psyche by stimulating the production of serotonin.
- Hospitalization. In remission, the patient is usually at home. He might even get a job. But sometimes doctors advise you to temporarily go to the hospital and undergo an additional examination, especially at the risk of developing an exacerbation.
- Psychotherapeutic sessions. They are individual and group. Considered one of the most effective treatments for schizophrenia during remission. The patient can talk to the doctor, as well as listen to other patients with similar diseases. It helps improve mood and increase motivation.
- Work with relatives. Relatives of a schizophrenic consult a psychiatrist about the rules for communicating with their relatives, who are in the grip of schizophrenia. They must learn to communicate with him and quickly identify the symptoms of an attack.
- Training. In some cases, the patient is trained in professional skills so that he can work.
 Locking yourself in is much more dangerous. It is much more productive for the patient to work. At the same time, monotonous and manual labor is preferable.
Locking yourself in is much more dangerous. It is much more productive for the patient to work. At the same time, monotonous and manual labor is preferable.
In general, treatment for residual schizophrenia is aimed at social adaptation of the patient and reducing the negative impact of the pathology on the psyche.
Forecast
Predicting the development of schizophrenia is quite difficult. It is incurable, and therefore a person is constantly at risk. He has the opportunity to prolong remission, but only with an integrated approach to his health, not only mental, but also physical.
The earlier schizophrenia manifests itself, the more devastating its consequences.
It is recommended to go in for sports (except extreme ones), eat right, walk in the fresh air every day, take vitamins and communicate with other people.