What effect can prolonged stress have on your immune system
How Does Stress Affect the Immune System?
Stress can take a toll on your mental health, especially if it’s chronic. But can it affect your immune response? Learn how stress levels affect your immune system and what you can do to keep your stress levels in check.
web on
Stress and the immune system have a complex relationship. Your immune system knows when you’re stressed about work, family, finances or current events. The body’s natural defender is sensitive to psychological stress, especially if it’s chronic.
Stress and Immune System Function
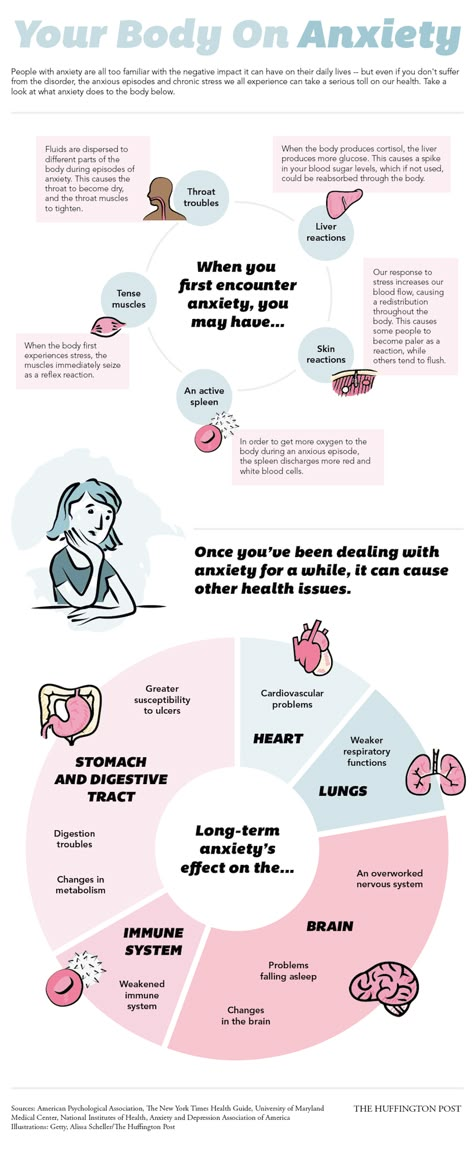
Stress can reduce the number of natural killer cells or lymphocytes in the body, which are needed to fight viruses, according to the American Psychological Association.
A review of studies in Current Opinion in Psychology found that stress can cause the immune system to produce an inflammatory response, which can be temporarily beneficial for fighting germs. However, if inflammation is persistent and widespread, it can contribute to chronic diseases, including the buildup of plaque on your arterial walls. This is just one of the many factors at play in the complex relationship between stress and your heart.
Chronic stress can produce higher-than-normal levels of the hormone
cortisol. This can hamper the body’s anti-inflammatory response and cause continual infections, according to recent immunology research studies.
If you’re dealing with stress you can’t seem to shake, take time to identify the sources and find ways to avoid or cope with them. You’ll be doing your immune system— and health—a favor.
Helpful Ways to Fight Stress
Here are four ways to battle stress for better mental well-being and a healthier body.
Make Time for Relationships
During stressful times, you may feel the urge to step back and avoid socializing. However, this is the time reaching out to the people you love means the most. It is especially important to stay connected during the pandemic.
It is especially important to stay connected during the pandemic.
Your social support system can help you cope with life problems by improving your self-esteem. Take some time for a video-chat date with a friend, attend an online gathering or give a family member a call.
Silence Negative Self-Talk
Choose to look at stressful situations in a positive light. Replace negative thoughts, such as “Nothing is going how I planned,” with positive thoughts, such as “It’s fine that things went differently than planned. I can handle it.” Finding the right therapist can help you cope during difficult times and teach you helpful techniques for combatting negative thoughts.
Sing it Out
No matter if you can carry a tune or not, some studies have linked singing and listening to music to lower levels of cortisol, the “stress hormone,” and decreased feelings of stress.
Go for a Walk
Never underestimate the power of a stroll through nature. Research shows that a 90-minute walk outdoors can reduce activity in the brain linked to repetitive negative thoughts. It is also a great way to sneak some physical activity into your day!
It is also a great way to sneak some physical activity into your day!
Listen to a Podcast
Everyday Habits for Stress Reduction
Stress reduction can be a learned behavior—and an everyday habit that helps you lead a more joyful life. By practicing mindfulness-based stress reduction, regularly, you can make time to live more freely in the moment, focus on the present and give yourself the “mindspace”—or the breathing room—to positively affect your feelings, thoughts and behaviors. Join integrative health professional Ginny Jump, CRNP, for inspiration, advice and an uncommonly relaxing discussion about stress. Listen to the podcast.
More to Read
- How to Reduce the Stress in Your Life
- Guided Meditation: A Daily Exercise to Reduce the Stress, Anxiety, and Depression in Your Life
- Parenting and Mental Health: Building Your Toolkit
Still feeling stressed?
Discover some other scientifically-backed stress relief methods.
Subscribe to Our Emails
First Name*Last Name*
Email*
Mailing Zip/Postal Code*
Birthdate*
Home Phone*
Listen to Our Newest Podcasts
About Us
The University of Maryland Medical System (UMMS) is a university-based regional health care system focused on serving the health care needs of Maryland.
We bring innovation, discovery and research to the care we provide all while educating the state’s future physicians and health care professionals through our partnership with the University of Maryland School of Medicine and the UM Schools of Nursing, Pharmacy, Social Work and Dentistry in Baltimore.
Learn more.
Medical Disclaimer
The content provided in this blog has been reviewed by University of Maryland Medical System providers or affiliates who are subject matter experts.
The content is for informational purposes only and is not intended as medical advice, or as a substitute for the medical advice of a trained healthcare provider.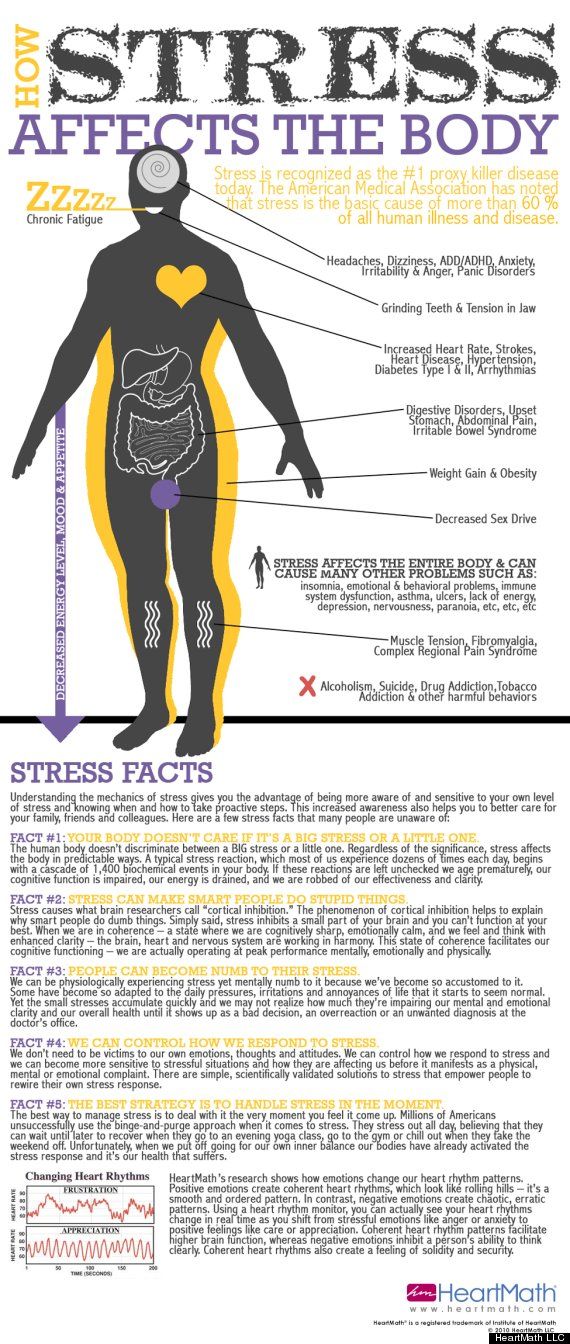
Always seek out the advice of a qualified medical provider with any questions you may have regarding a medical condition or treatment and before undertaking a new health care regimen.
Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Find a provider at umms.org/doctor.
What Happens When Your Immune System Gets Stressed Out? – Cleveland Clinic
For most of us, stress is just a part of life. It can last for a few hours — like the time leading up to a final exam — or for years — like when you’re taking care of an ailing loved one.
Stress is sometimes a motivator that helps you rise to the occasion. At other times, it’s simply overwhelming. Whatever the case, if it’s chronic, it can take a toll on your immune system.
Clinical immunologist Leonard Calabrese, DO, offers insights on how stress impacts your immunity and what you can do to minimize the effect.
“Eliminating or modifying these factors in one’s life is vital to protect and augment the immune response,” he says. “It’s necessary to buffer the inevitability of the aging process.”
“It’s necessary to buffer the inevitability of the aging process.”
What impact does stress have on you?
Stress occurs when life events surpass your abilities to cope. It causes your body to produce greater levels of the stress hormone cortisol.
Advertising Policy
In short spurts, cortisol can boost your immunity by limiting inflammation. But over time, your body can get used to having too much cortisol in your blood. And this opens the door for more inflammation, Dr. Calabrese says.
In addition, stress decreases the body’s lymphocytes — the white blood cells that help fight off infection. The lower your lymphocyte level, the more at risk you are for viruses, including the common cold and cold sores.
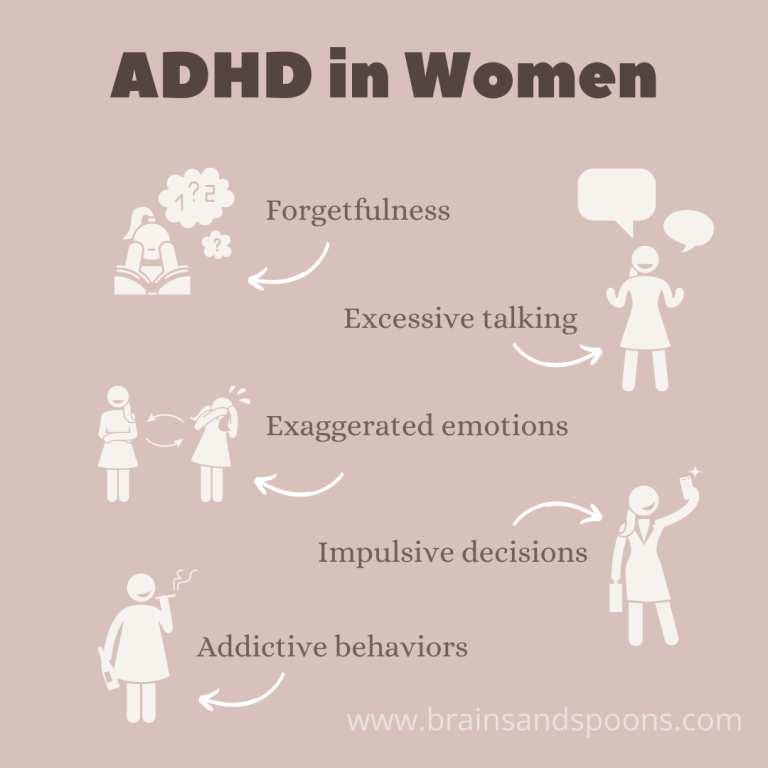
High stress levels also can cause depression and anxiety, again leading to higher levels of inflammation. In the long-term, sustained, high levels of inflammation point to an overworked, over-tired immune system that can’t properly protect you.
Conditions that stress causes
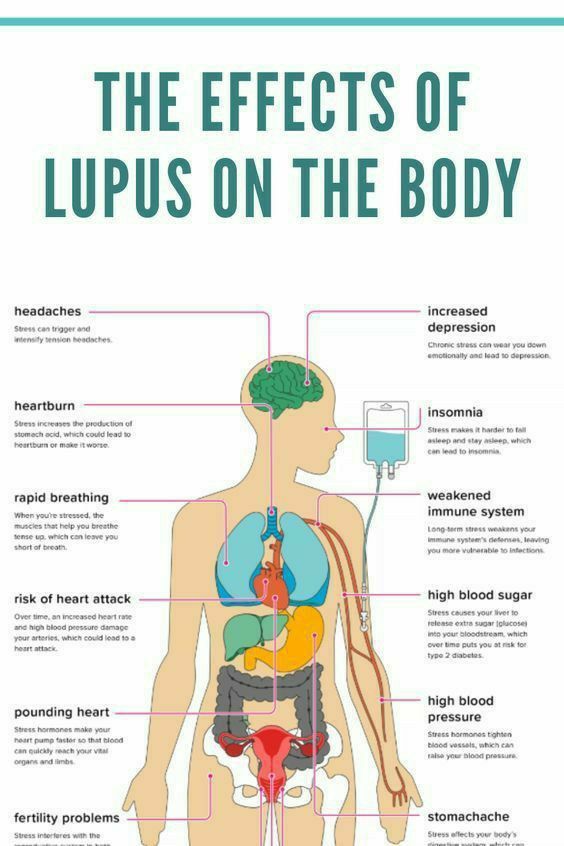
If you don’t control high stress levels, chronic inflammation can accompany it and can contribute to the development and progression of many diseases of the immune system such as:
Advertising Policy
- Arthritis
- Fibromyalgia
- Lupus
- Psoriasis
- Inflammatory bowel disease
Under sustained, long-term stress, you also can develop cardiovascular problems, including a fast heart rate and heart disease, as well as gastric ulcers.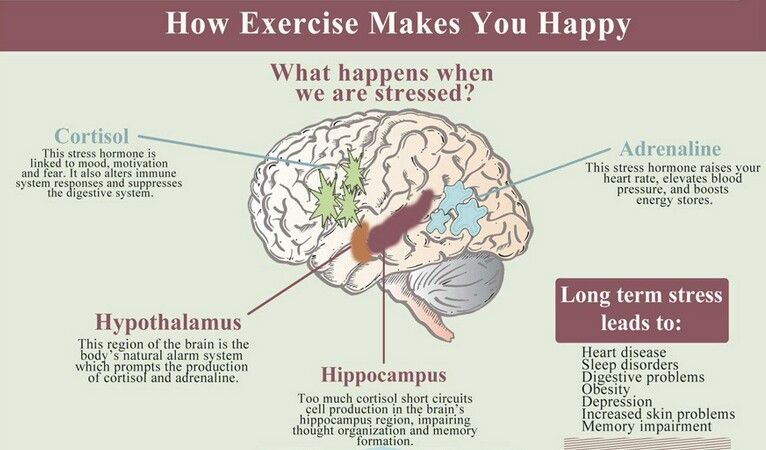 You’ll also be at greater risk for type 2 diabetes, various cancers and mental decline.
You’ll also be at greater risk for type 2 diabetes, various cancers and mental decline.
How can you better manage your stress levels?
Stress reduction strategies not only give your mind a break, but they can also relieve the pressure on your immune system. You can take steps to reduce short-term and long-term stress, Dr. Calabrese says. Two tactics are most effective:
- Meditation (also called mindfulness): Meditate for 10 minutes to 15 minutes three or four times weekly to lower your stress. It reduces your cortisol levels and reduces inflammation. Research also shows it helps prevent the breakdown of your chromosomes that leads to cancer and premature aging.
- Yoga: Practicing yoga also lowers stress hormone levels and calms your nervous system to reduce inflammation. Deep breathing helps boost your resistance to infection. Inverted poses in yoga help circulate fluid through your lymphatic system, filtering out toxins.
Stress in acute situations, however, can be healthful and protective, so it’s not all bad for us.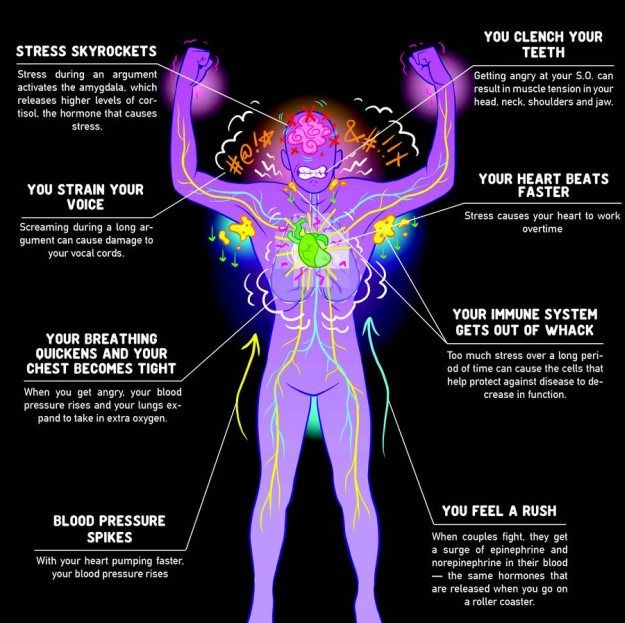 Remember: it’s chronic stress that we seek to control.
Remember: it’s chronic stress that we seek to control.
The influence of stress, mental tension on the human immune system
Why do some people remain healthy even in old age, while others at the same age develop chronic diseases and even die relatively young? Although this is due to individual genetic factors, researchers at the University of Southern California have shown that it can also be due to individual stress levels.
With the current trend towards an increase in the number of older people in the world, it is important to understand the differences in health status associated with aging. It is possible that age-related changes in the immune system are the main contributor to the increased morbidity and mortality in the elderly. The immune system naturally weakens with age as disease- and infection-fighting white blood cells wear out and fewer new cells are produced to replace them. Stressful situations throughout life, such as chronic overwork at work, domestic and family conflicts, discrimination lead to even faster aging of the immune system.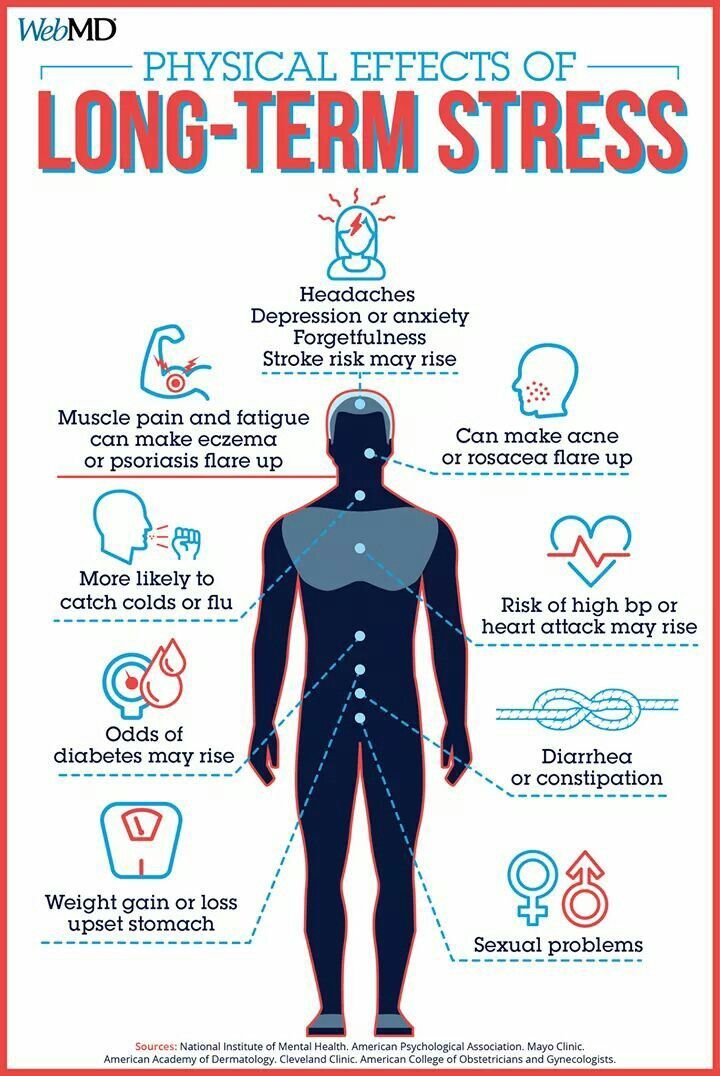 An aging immune system, in turn, increases the risk of cancer, heart disease, infectious diseases, organ failure, and premature death. When a person's immune system is weakened, the effectiveness of vaccinations decreases, and individual organ systems age faster. nine0003
An aging immune system, in turn, increases the risk of cancer, heart disease, infectious diseases, organ failure, and premature death. When a person's immune system is weakened, the effectiveness of vaccinations decreases, and individual organ systems age faster. nine0003
The work of Eric Klopak, a researcher at the Leonard Davis School of Gerontology, and colleagues made it possible to elucidate the immunological mechanisms involved in accelerated aging under the influence of socioeconomic factors and lifestyle. The study also identified important avenues that can be helpful in addressing inequalities in aging and preventing excessive losses during epidemics and pandemics, including COVID-19. The researchers studied a sample of more than 5,700 Americans with an average age of 68. They assessed five stressors thought to affect health: chronic stress, stressful life events, everyday discrimination, lifelong discrimination, and life trauma. The results of the study showed that psychosocial stress is the most important factor contributing to the potentiation of immune aging, which manifests itself in the form of a decrease in the subpopulation of naive and an increase in the pool of terminally differentiated T-lymphocytes, which are indicators of biological age. nine0003
nine0003
Mental stress can seriously affect physical health
Lifelong exposure to stressful situations is a significant risk factor for poor health, increased risk of early development of age-related diseases and premature death. Models that study the mechanisms that drive these effects focus on the consequences of reactivation and long-term activation of the sympathoadrenal and hypothalamic-pituitary-adrenal systems, which leads to "wear and tear" of the body at the biological level. It is assumed that biological wear and tear manifests itself at the cellular level, manifesting itself in the form of accumulation of DNA damage, increased inflammation, and shortening of telomeres. Critically short telomere lengths in immune cells and cellular stress (such as DNA damage) can lead cells into a non-replicating state called cellular senescence. In addition to localized tissue-specific aging, age-related changes in immune function contribute to systemic aging, organ failure, and premature mortality, making immune aging a critical factor in premature aging and mortality.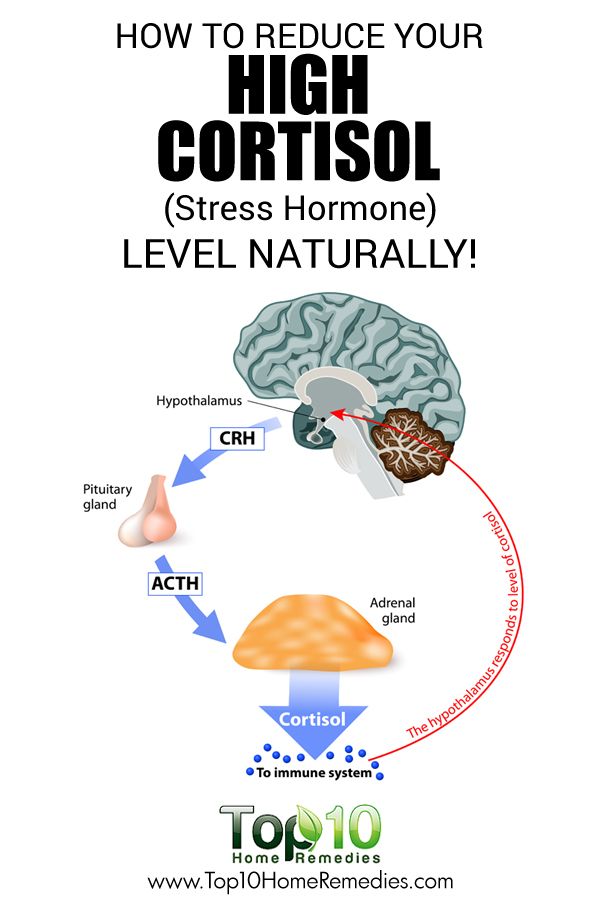 nine0003
nine0003
Immune aging, including a decrease in the number of undifferentiated (naive) and an increase in terminally differentiated immune T cells, plays a role in immune health and tissue-specific aging and may contribute to an increased risk of poor health among those experiencing severe and/or persistent psychosocial stress. Previous studies have been limited to assessing the contribution of life stress to accelerated immune aging and to the contribution of factors such as lifestyle and cytomegalovirus (CMV) infection. In a new study, the relationship of social stress (namely, everyday discrimination, lifelong discrimination, life stressful events, life trauma and chronic stress) with cellular markers of immune aging was assessed by flow cytometry. nine0003
Immunologically, biological age is determined by the composition of the immune cell population. At the same time, the aging immune system is characterized by a reduced pool of naive B and T cells, an increased pool of terminally differentiated T cells, and an increased pool of CD8 + cells compared to CD4 +.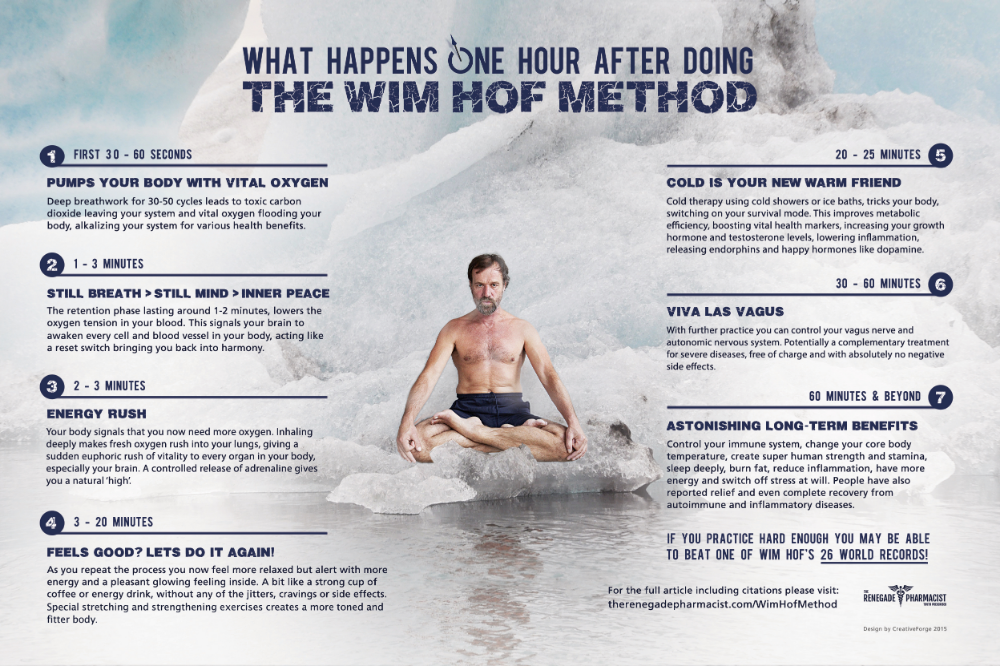 Social stress can alter the immune system in several ways, including increasing inflammatory signaling and decreasing antiviral responses.
Social stress can alter the immune system in several ways, including increasing inflammatory signaling and decreasing antiviral responses.
It turned out that the effect of stress factors is directly related to changes in the composition of subpopulations of T-lymphocytes, which are markers of biological age. Researchers have found that different types of stress affect the ratio of old, weakened (terminally differentiated) T cells, which are less active in the immune system, to newly formed (naive) T cells, which can help boost immunity. For example, under chronic stress and complex psychological trauma, there was a decrease in the proportion of CD4 + naive T-lymphocytes (immune cells that have not yet encountered the antigen). Prolonged discrimination and chronic life stress led to an increase in the subpopulation of terminally differentiated CD4+ cells. Also reliable markers of chronic stress were a decrease in naive CD8 + lymphocytes and an increase in the number of weakened terminally differentiated CD8 + cells. A decrease in the ratio of CD4 + to CD8 + lymphocytes was also characteristic. Lifestyle factors and seropositivity for cytomegalovirus infection partially attenuated these effects. All these effects did not depend on passport age, gender, and racial or ethnic origin. nine0003
A decrease in the ratio of CD4 + to CD8 + lymphocytes was also characteristic. Lifestyle factors and seropositivity for cytomegalovirus infection partially attenuated these effects. All these effects did not depend on passport age, gender, and racial or ethnic origin. nine0003
Findings
This study demonstrates the important role of psychosocial stress in accelerating immune aging, highlighting the key contribution of behavior and mental self-regulation to health. These results raise the possibility that interventions aimed at reducing stress or increasing psychological resilience can potentially help reduce the phenomena of T-cell immunological aging. Timely vaccination against cytomegalovirus infection can also play a role. nine0002 You must have heard the phrase: "all diseases are from nerves." Indeed, high psycho-emotional stresses undermine the body's defenses. How and why does stress affect a person's immunity?
Against the background of intense stress, immunity decreases. This happens for the following reasons:
This happens for the following reasons:
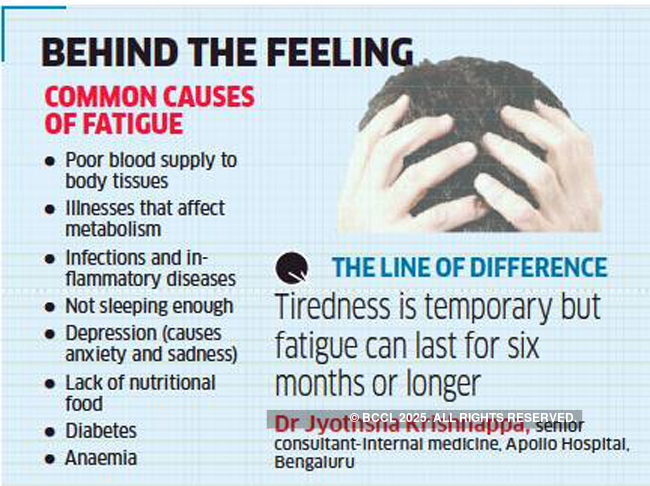
- Strong emotions release cortisol, which is called the stress hormone, into the bloodstream. High concentrations of this hormone depress the immune system. If the stress passes quickly, the body easily recovers from the release of cortisol. But if the stress is chronic, recovery does not occur, that is, the level of cortisol is always higher than normal. This condition provokes the development of an inflammatory reaction, which "distracts" the immune system from fighting viruses and bacteria. In addition, prolonged stress contributes to the disruption of the work of T-lymphocytes. And these cells are needed by the body to neutralize foreign microorganisms. nine0057
- Strong experiences suppress immune responses, which reduces the number of cells that produce antibodies. Antibodies are the “weapon” of the body with which it destroys bacteria and viruses. That is why people living in a state of stress are more likely to get ARVI.

- Reduced immunity due to stress is also observed against the background of a decrease in the number of natural killers (NK-lymphocytes). These cells of the immune system are the first line of defense against cancer. nine0057
- Under stress, the processes of interaction between the nervous and immune systems are disrupted. This is manifested, in particular, by the development of chronic fatigue syndrome. In this state, a person quickly gets tired, constantly feels weak. The immune system is in a passive state and reacts more slowly to threats.
- With strong and constant experiences, macrophages at some point can release a large number of cytokines - signaling molecules that are responsible for the formation of an inflammatory response. If there are too many cytokines, a cytokine storm occurs. In a cytokine storm, the tissues of the focus of inflammation are quickly destroyed, affecting neighboring tissues. This process can capture the whole organ. A cytokine storm is a dangerous reaction of the body, it can even lead to death.
 nine0057
nine0057
Please note that not all stress weakens the immune system. If the stressful situation does not last long (for example, you are late for work), then it will not lead to negative consequences. But if there is a long, intense stressful effect, it depresses the immune system. This condition should not be taken lightly, attributing it only to a bad mood or fatigue.
Many are wondering, how to strengthen the immune system in a situation of chronic stress.
To begin with, it should be noted that the restoration of the nervous system and the strengthening of immunity is not a matter of one day or even one week. Therefore, if you realize that you have been living in stress for some time, first of all try to protect yourself from meeting viruses and bacteria. In this case, we are not talking about masks, but Breathe Oil ® . It destroys viruses and bacteria in the inhaled air and therefore reduces the risk of infection by 3 times.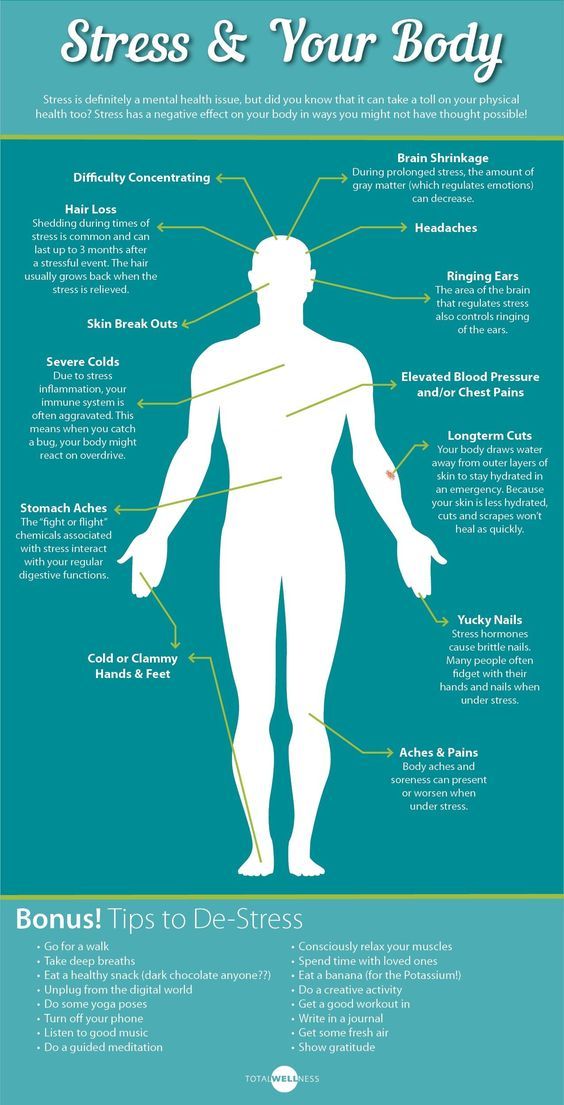 This is especially true during flu and SARS season. Use Breathe Oil ® at home, on public transport, at work. Moreover, it has no restrictions on the frequency and duration of use.
This is especially true during flu and SARS season. Use Breathe Oil ® at home, on public transport, at work. Moreover, it has no restrictions on the frequency and duration of use.
And already against the background of the use of Dyshi Oil ® , you can strengthen the immune system.
It is very important to get rid of the source of strong feelings. Can't do it yourself? Seek advice from a qualified psychologist or psychotherapist. You should not be shy about visiting a specialist, because mental health needs the same care as physical health. The doctor will not give you advice on how to live on, but can recommend ways to get rid of psychological pressure, help you look at the situation from a different angle. nine0003
To restore immunity after stress, doctors advise more rest. This requires a full sleep (at least 7-8 hours) and positive emotions. When a person does what he loves, meets friends, the hormone oxytocin is released in his body (it is called the hormone of happiness).