What causes out of body feeling
Out-of-Body Experience: What’s Really Happening
An out-of-body experience is often described as feeling like you’ve left your physical body. There are many potential causes, including several medical conditions and experiences.
An out-of-body experience (OBE) is a sensation of your consciousness leaving your body. These episodes are often reported by people who’ve had a near-death experience. Some might also describe an OBE as a dissociative episode.
People typically experience their sense of self inside their physical body. You most likely view the world around you from this vantage point. But during an OBE, you may feel as if you’re outside yourself, looking at your body from another perspective.
What really goes on during an OBE? Does your consciousness actually leave your body? Experts aren’t totally sure, but they have a few hunches, which we’ll get into later.
It’s hard to nail down what an OBE feels like, exactly.
According to accounts from people who’ve experienced them, they generally involve:
- a feeling of floating outside your body
- an altered perception of the world, such as looking down from a height
- the feeling that you’re looking down at yourself from above
- a sense that what’s happening is very real
OBEs typically happen without warning and usually don’t last for very long.
If you have a neurological condition, such as epilepsy, you may be more likely to experience OBEs.They may also happen more frequently. But for many people, an OBE will happen very rarely, maybe only once in a lifetime if at all.
Some estimates suggest around 5 percent of people have experienced the sensations associated with an OBE, though some suggest this number may be higher.
There’s some debate over whether the sensations and perceptions associated with OBEs happen physically or as a sort of hallucinatory experience.
A recent 2022 review tried to explore this by evaluating a variety of studies and case reports evaluating consciousness, cognitive awareness, and recall in people who survived cardiac arrest.
They noted that some people report experiencing a separation from their body during resuscitation and some even reported an awareness of events they wouldn’t have seen from their actual perspective.
In addition, one study included in the review noted that two participants reported having both visual and auditory experiences while in cardiac arrest.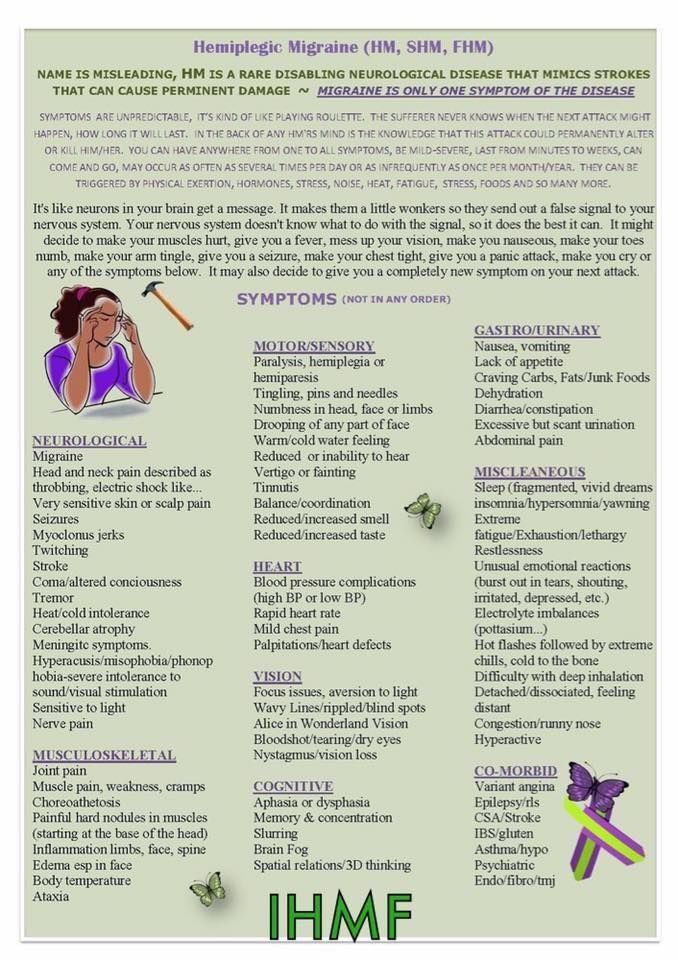 Only one was well enough to follow up, but he gave an accurate, detailed description of what took place for about three minutes of his resuscitation from cardiac arrest.
Only one was well enough to follow up, but he gave an accurate, detailed description of what took place for about three minutes of his resuscitation from cardiac arrest.
Still, there’s no scientific evidence to support the idea that a person’s consciousness can actually travel outside the body.
Veridical perception
Veridical perception is a controversial concept. It refers to the idea that you can leave your body during an OBE, allowing you to witness something that you may not have otherwise.
Some anecdotal reports of this phenomena exist, with a few people even providing specific, accurate details about events that have happened during surgical procedures or while clinically dead.
Many people use these stories as evidence to support the existence of life after death.
However, the idea of veridicial perception is still limited to anecdotal claims and there is no research available to support it.
One older 2014 study investigating the validity of veridical perception in people who had survived cardiac arrest found that neither of the two individuals who reported awareness during resuscitation were able to identify specific items that were only viewable from above.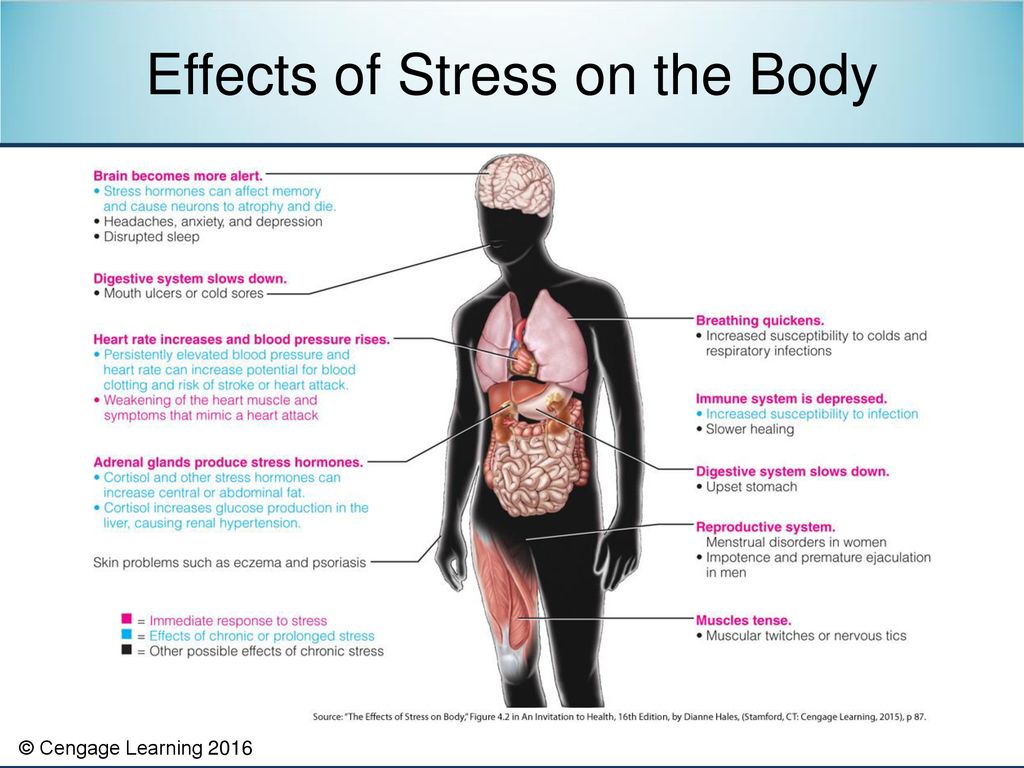
No one’s sure about the exact causes of OBEs, but experts have identified several possible explanations.
Stress or trauma
A frightening, dangerous, or difficult situation can provoke a fear response, which might cause you to dissociate from the situation and feel as if you’re an onlooker. This may make you feel as though you are watching the events from somewhere outside your body.
According to 2017 research reviewing the experience of women in labor, OBEs during childbirth aren’t unusual.
The study didn’t specifically link OBEs to post-traumatic stress disorder, but the authors did point out that women who had OBEs had either gone through trauma during labor or another situation not related to childbirth.
This suggests that OBEs could occur as a way to cope with trauma, but more research is needed on this potential link.
Medical conditions
Experts have linked several medical and mental health conditions to OBEs, including:
- epilepsy
- migraine
- cardiac arrest
- brain injuries
- depression
- anxiety
- Guillain-Barré syndrome
Dissociative disorders, particularly depersonalization-derealization disorder, can involve frequent feelings or episodes where you seem to be observing yourself from outside your body.
Sleep paralysis has also been noted as a possible cause of OBEs. It refers to a temporary state of waking paralysis that occurs during REM sleep and often involves hallucinations.
Research suggests many people who have OBEs with a near-death experience also often experience sleep paralysis.
In addition, a review of literature from 2020 suggests that sleep-wake disturbances may contribute to dissociative symptoms. This can include a feeling of leaving your body.
Medication and drugs
Some people report having an OBE while under the influence of anesthesia.
Other substances, including cannabis, ketamine, or hallucinogenic drugs such as LSD, can cause this sensation.
Near-death experiences
OBEs can occur during near-death experiences, often alongside other phenomena like flashbacks of previous memories or seeing a light at the end of a tunnel.
Though it’s not clear exactly why this happens, it’s believed to be caused by disruptions in certain areas of the brain involved with processing sensory information. A 2021 review suggests that these experiences may be more likely to occur during life threatening situations, which can include:
A 2021 review suggests that these experiences may be more likely to occur during life threatening situations, which can include:
- cardiac arrest
- traumatic injury
- brain hemorrhage
- drowning
- suffocation
Strong G-forces
Pilots and astronauts sometimes experience OBEs when strong gravitational forces, or G-forces, are encountered. This is because it causes blood to pool in the lower body, which can lead to loss of conscious and may induce an OBE.
Extreme G-forces can also cause spatial disorientation, peripheral vision loss, and disconnection between cognition and the ability to act.
Paranormal
Though not backed by research, some people believe that OBEs can occur when your soul or spirit leaves your body.
One form is known as “traveling clairvoyance,” which some mediums claim allows your soul to visit distant locations in order to gain information.
Others believe that certain meditative practices can help you reach a state of consciousness that transcends the body and mind, leading to an OBE.
Some people also experiment with astral projection, which is a spiritual practice that involves making an intentional effort to send your consciousness from your body toward a spiritual plane or dimension.
However, research as not been able to show that these practices cause OBEs.
Other experiences
OBEs might be able to be induced, intentionally or accidentally, by:
- brain stimulation
- sleep deprivation
- sensory deprivation
- hypnosis or meditative trance
However, additional research is still needed to support this.
Existing research hasn’t connected experiencing spontaneous OBEs to any serious health risks. In some cases, you might feel a bit dizzy or disoriented after.
However, OBEs and dissociation in general can cause lingering feelings of emotional distress.
You might feel confused over what happened or wonder if you have a brain issue or mental health condition. You might also not like the sensation of an OBE and worry about it happening again.
Some people also claim that it’s possible for your consciousness to remain trapped outside of your body following an OBE, but there’s no evidence to support this.
Simply having an OBE doesn’t necessarily mean you need to see a healthcare professional. You may have this experience once just before drifting off to sleep, for example, and never again. If you don’t have any other symptoms, you probably don’t have any reason for concern.
If you feel uneasy about what happened, even if you don’t have any physical or psychological conditions, there’s no harm in mentioning the experience to a doctor. They may be able to help by ruling out serious conditions or offering some reassurance.
It’s also a good idea to talk with a healthcare professional if you’re having any sleep issues, including insomnia or symptoms of sleep paralysis, such as hallucinations.
Recognize an emergency
Seek immediate help if you’ve had an OBE and are experiencing:
- severe head pain
- flashing lights in your vision
- seizures
- loss of consciousness
- low mood or changes in mood
- thoughts of suicide
Whether your consciousness can truly leave your physical body hasn’t been scientifically proven.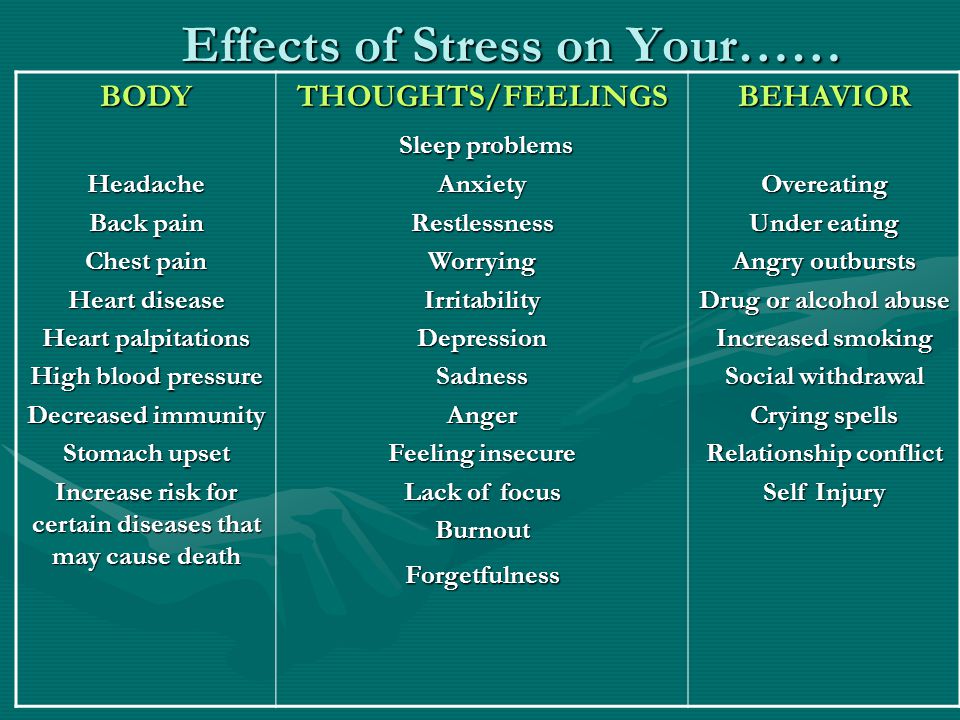 But for centuries, many people have reported experiencing sensations of their consciousness leaving their body.
But for centuries, many people have reported experiencing sensations of their consciousness leaving their body.
OBEs appear to be more common with some conditions, including certain dissociative disorders and epilepsy. Many people also report having an OBE during a near-death experience, including during cardiac arrest or brain injury.
Out-of-Body Experience: What’s Really Happening
An out-of-body experience is often described as feeling like you’ve left your physical body. There are many potential causes, including several medical conditions and experiences.
An out-of-body experience (OBE) is a sensation of your consciousness leaving your body. These episodes are often reported by people who’ve had a near-death experience. Some might also describe an OBE as a dissociative episode.
People typically experience their sense of self inside their physical body. You most likely view the world around you from this vantage point. But during an OBE, you may feel as if you’re outside yourself, looking at your body from another perspective.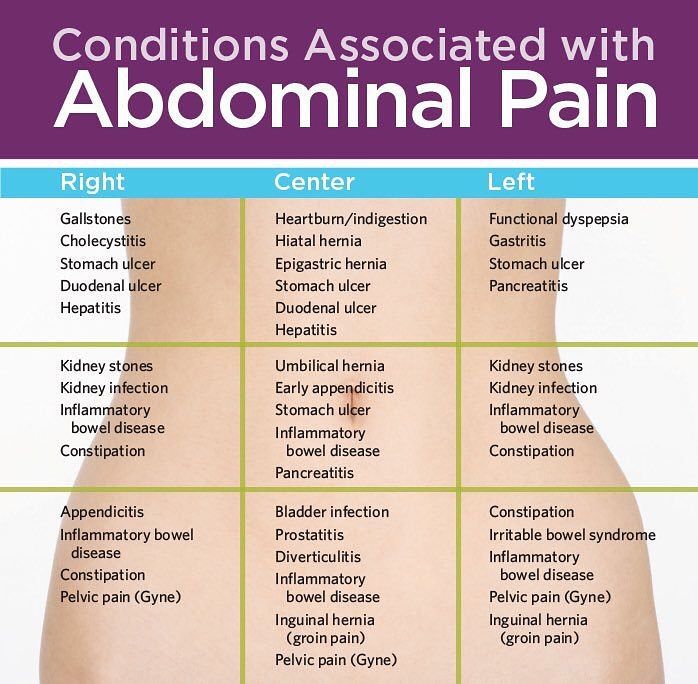
What really goes on during an OBE? Does your consciousness actually leave your body? Experts aren’t totally sure, but they have a few hunches, which we’ll get into later.
It’s hard to nail down what an OBE feels like, exactly.
According to accounts from people who’ve experienced them, they generally involve:
- a feeling of floating outside your body
- an altered perception of the world, such as looking down from a height
- the feeling that you’re looking down at yourself from above
- a sense that what’s happening is very real
OBEs typically happen without warning and usually don’t last for very long.
If you have a neurological condition, such as epilepsy, you may be more likely to experience OBEs.They may also happen more frequently. But for many people, an OBE will happen very rarely, maybe only once in a lifetime if at all.
Some estimates suggest around 5 percent of people have experienced the sensations associated with an OBE, though some suggest this number may be higher.
There’s some debate over whether the sensations and perceptions associated with OBEs happen physically or as a sort of hallucinatory experience.
A recent 2022 review tried to explore this by evaluating a variety of studies and case reports evaluating consciousness, cognitive awareness, and recall in people who survived cardiac arrest.
They noted that some people report experiencing a separation from their body during resuscitation and some even reported an awareness of events they wouldn’t have seen from their actual perspective.
In addition, one study included in the review noted that two participants reported having both visual and auditory experiences while in cardiac arrest. Only one was well enough to follow up, but he gave an accurate, detailed description of what took place for about three minutes of his resuscitation from cardiac arrest.
Still, there’s no scientific evidence to support the idea that a person’s consciousness can actually travel outside the body.
Veridical perception
Veridical perception is a controversial concept. It refers to the idea that you can leave your body during an OBE, allowing you to witness something that you may not have otherwise.
Some anecdotal reports of this phenomena exist, with a few people even providing specific, accurate details about events that have happened during surgical procedures or while clinically dead.
Many people use these stories as evidence to support the existence of life after death.
However, the idea of veridicial perception is still limited to anecdotal claims and there is no research available to support it.
One older 2014 study investigating the validity of veridical perception in people who had survived cardiac arrest found that neither of the two individuals who reported awareness during resuscitation were able to identify specific items that were only viewable from above.
No one’s sure about the exact causes of OBEs, but experts have identified several possible explanations.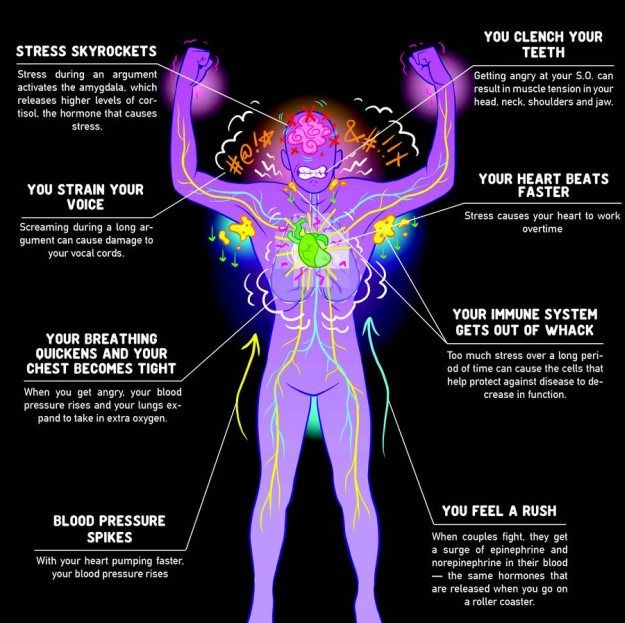
Stress or trauma
A frightening, dangerous, or difficult situation can provoke a fear response, which might cause you to dissociate from the situation and feel as if you’re an onlooker. This may make you feel as though you are watching the events from somewhere outside your body.
According to 2017 research reviewing the experience of women in labor, OBEs during childbirth aren’t unusual.
The study didn’t specifically link OBEs to post-traumatic stress disorder, but the authors did point out that women who had OBEs had either gone through trauma during labor or another situation not related to childbirth.
This suggests that OBEs could occur as a way to cope with trauma, but more research is needed on this potential link.
Medical conditions
Experts have linked several medical and mental health conditions to OBEs, including:
- epilepsy
- migraine
- cardiac arrest
- brain injuries
- depression
- anxiety
- Guillain-Barré syndrome
Dissociative disorders, particularly depersonalization-derealization disorder, can involve frequent feelings or episodes where you seem to be observing yourself from outside your body.
Sleep paralysis has also been noted as a possible cause of OBEs. It refers to a temporary state of waking paralysis that occurs during REM sleep and often involves hallucinations.
Research suggests many people who have OBEs with a near-death experience also often experience sleep paralysis.
In addition, a review of literature from 2020 suggests that sleep-wake disturbances may contribute to dissociative symptoms. This can include a feeling of leaving your body.
Medication and drugs
Some people report having an OBE while under the influence of anesthesia.
Other substances, including cannabis, ketamine, or hallucinogenic drugs such as LSD, can cause this sensation.
Near-death experiences
OBEs can occur during near-death experiences, often alongside other phenomena like flashbacks of previous memories or seeing a light at the end of a tunnel.
Though it’s not clear exactly why this happens, it’s believed to be caused by disruptions in certain areas of the brain involved with processing sensory information. A 2021 review suggests that these experiences may be more likely to occur during life threatening situations, which can include:
A 2021 review suggests that these experiences may be more likely to occur during life threatening situations, which can include:
- cardiac arrest
- traumatic injury
- brain hemorrhage
- drowning
- suffocation
Strong G-forces
Pilots and astronauts sometimes experience OBEs when strong gravitational forces, or G-forces, are encountered. This is because it causes blood to pool in the lower body, which can lead to loss of conscious and may induce an OBE.
Extreme G-forces can also cause spatial disorientation, peripheral vision loss, and disconnection between cognition and the ability to act.
Paranormal
Though not backed by research, some people believe that OBEs can occur when your soul or spirit leaves your body.
One form is known as “traveling clairvoyance,” which some mediums claim allows your soul to visit distant locations in order to gain information.
Others believe that certain meditative practices can help you reach a state of consciousness that transcends the body and mind, leading to an OBE.
Some people also experiment with astral projection, which is a spiritual practice that involves making an intentional effort to send your consciousness from your body toward a spiritual plane or dimension.
However, research as not been able to show that these practices cause OBEs.
Other experiences
OBEs might be able to be induced, intentionally or accidentally, by:
- brain stimulation
- sleep deprivation
- sensory deprivation
- hypnosis or meditative trance
However, additional research is still needed to support this.
Existing research hasn’t connected experiencing spontaneous OBEs to any serious health risks. In some cases, you might feel a bit dizzy or disoriented after.
However, OBEs and dissociation in general can cause lingering feelings of emotional distress.
You might feel confused over what happened or wonder if you have a brain issue or mental health condition. You might also not like the sensation of an OBE and worry about it happening again.
Some people also claim that it’s possible for your consciousness to remain trapped outside of your body following an OBE, but there’s no evidence to support this.
Simply having an OBE doesn’t necessarily mean you need to see a healthcare professional. You may have this experience once just before drifting off to sleep, for example, and never again. If you don’t have any other symptoms, you probably don’t have any reason for concern.
If you feel uneasy about what happened, even if you don’t have any physical or psychological conditions, there’s no harm in mentioning the experience to a doctor. They may be able to help by ruling out serious conditions or offering some reassurance.
It’s also a good idea to talk with a healthcare professional if you’re having any sleep issues, including insomnia or symptoms of sleep paralysis, such as hallucinations.
Recognize an emergency
Seek immediate help if you’ve had an OBE and are experiencing:
- severe head pain
- flashing lights in your vision
- seizures
- loss of consciousness
- low mood or changes in mood
- thoughts of suicide
Whether your consciousness can truly leave your physical body hasn’t been scientifically proven. But for centuries, many people have reported experiencing sensations of their consciousness leaving their body.
But for centuries, many people have reported experiencing sensations of their consciousness leaving their body.
OBEs appear to be more common with some conditions, including certain dissociative disorders and epilepsy. Many people also report having an OBE during a near-death experience, including during cardiac arrest or brain injury.
Depersonalization: a syndrome that interferes with feeling - BBC News
Image caption,Sarah says that because of her illness, familiar places seem like decorations
People with depersonalization syndrome see the world as unreal, two-dimensional, as if in a fog. Every hundredth suffers from this disorder, but despite this, British doctors are not taught to work with such patients, experts say. nine0018
"The connections you think are valuable lose their original meaning. You know you love your family. But the thing is, you're more aware of it than you feel it," says Sarah on Victoria Derbyshire's BBC program.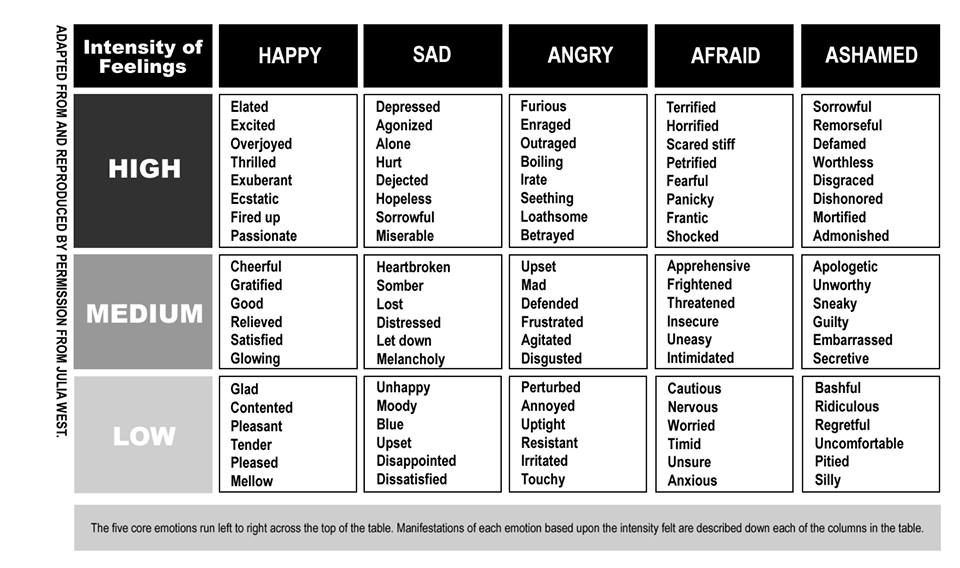 -bc.
-bc.
Sarah is an actress, she constantly tries on different images and reproduces other people's emotions. But in reality, for most of her conscious life, she is emotionally paralyzed and unable to experience any feelings.
The reason for this is a little-studied mental disorder called depersonalization. nine0011
Sarah had the syndrome three times. The first time it happened was when she was preparing for her final exams.
The main sign of depersonalization is the feeling that a person loses physical connection with the world around him and his own body.
It is believed that this is how a defense mechanism manifests when, during stress or a serious shock, consciousness is disconnected from reality. Some drugs, such as marijuana, can cause the same effect.
- Depression: a breakthrough in understanding the nature of the disease and its
- What your selfies say about you
- Google helps users recognize depression
Skip the Podcast and continue reading.
Podcast
What was that?
We quickly, simply and clearly explain what happened, why it's important and what's next.
episodes
End of Story Podcast
For people with depersonalization syndrome, the world can change in a second.
"It was an unexpected switch. Everything around seemed alien and even intimidating. Suddenly, the apartment and other places where you used to be become a film set for you, and all your things become scenery," says Sarah. nine0011
Other patients report feeling that they are outside their body, that it does not belong to them, and that the world around them seems two-dimensional and flat.
This happened to Sarah during the second episode.
"I was reading, I had a book in my hands. And suddenly my hands began to look like a picture on which two hands were drawn. There was a feeling that the real world and my perception of it did not coincide."
There was a feeling that the real world and my perception of it did not coincide."
Sarah's disorder is not uncommon. Three independent studies have proven that it occurs in one person out of a hundred. nine0011
Experts say the disorder has long been recognized as a medical condition. It is as common as obsessive-compulsive disorder or schizophrenia.
Some untreated patients may suffer lifelong depersonalization symptoms. And yet, not all doctors know what it is.
A doctor who recently graduated and suffers from this disorder himself stated that depersonalization was not taught in medical school or in continuing education courses for therapists. nine0011
He admitted that he misdiagnosed his patients at least twice. According to him, he will be very surprised if it turns out that at least one of his colleagues has heard about this syndrome.
Sarah says that in her life she encountered at least 20 professionals who had no idea what she was talking about. Among them are consultants, therapists, district psychiatrists and doctors.
Among them are consultants, therapists, district psychiatrists and doctors.
The Royal College of General Practitioners (RCGP) in London said that mental health was a key element of an expanded curriculum for physicians. nine0011
The institute added that the study of more complex psychological problems is still in development.
The Royal College of Psychiatry stressed the need to ensure that these disorders are properly understood.
Image caption,Dr Elaine Hunter runs the only referral center in the UK that treats patients with depersonalization
Poor diagnosis is only part of the problem, access to treatment is another complication. nine0011
There is only one specialist clinic in the UK. Its resources are limited, it can only accept 80 patients a year. Despite the fact that 650 thousand people can potentially suffer from this disease.
To access this health center free of charge, a referral from a local doctor is required. And even if the patient is diagnosed with depersonalization, treatment will have to wait several months or longer.
And even if the patient is diagnosed with depersonalization, treatment will have to wait several months or longer.
After a year of waiting in line, Sarah decided that the only way out was to pay for the treatment herself. nine0011
"I used to have panic attacks all the time. It's really scary. I knew it was a crisis," she says.
A specialist center for patients with depersonalization syndrome operates at the Maudsley Hospital in south London. However, there are restrictions for patients under 18 years of age; the center only treats adults.
Often the disease occurs in adolescence. Dr. Elaine Hunter, who heads the center, is concerned that she has to withhold care for children and adolescents. nine0011
"Sometimes 15-year-old patients come to us deeply depressed and frightened, but we have nothing to offer them," she says.
One of the adult patients of the center developed the syndrome at the age of 13.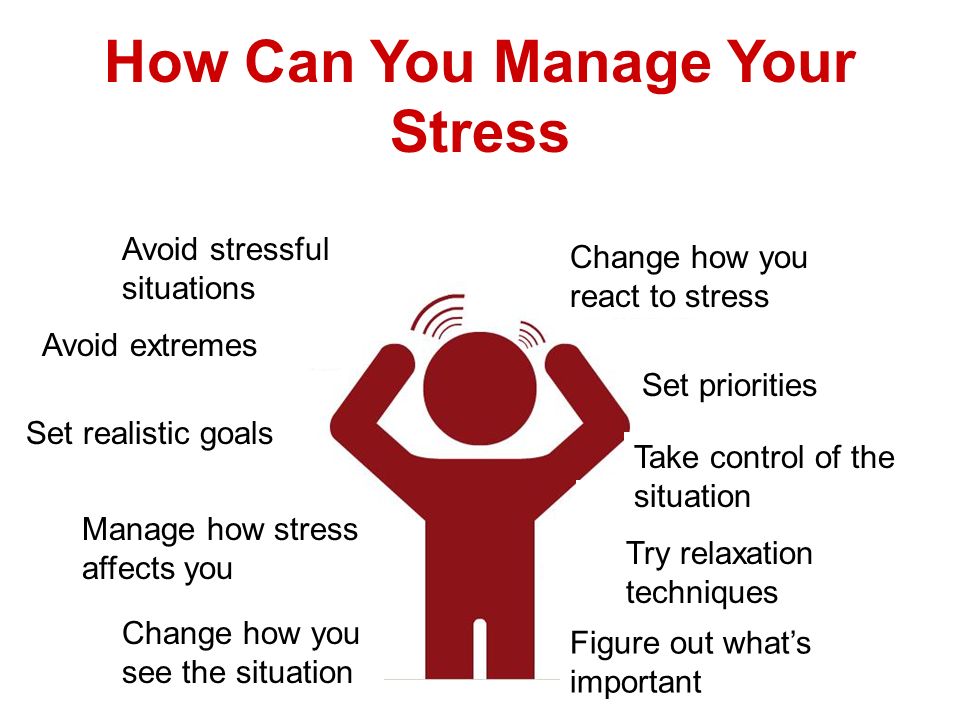 For two years she could not leave the house, she experienced ten panic attacks a day caused by the disorder.
For two years she could not leave the house, she experienced ten panic attacks a day caused by the disorder.
At the beginning of the treatment, she did not even recognize her own parents.
Dr. Hunter hopes that over time, the right treatment will be available to underage patients. nine0011
She believes that treatment should be organized in every district. Physicians in local centers for psychological assistance should undergo special training, then disseminate information among other specialists.
Image caption,Sarah Ashley couldn't eat or sleep until she was treated by Dr. Hunter
Hunter developed Cognitive Behavioral Therapy (CBT) specifically for patients with depersonalization. She believes that she will be easily mastered by doctors who already have experience in talking therapy. nine0011
Sarah Ashley, a patient of Dr. Hunter, says she was initially skeptical about the technique, but after a while she felt a huge difference.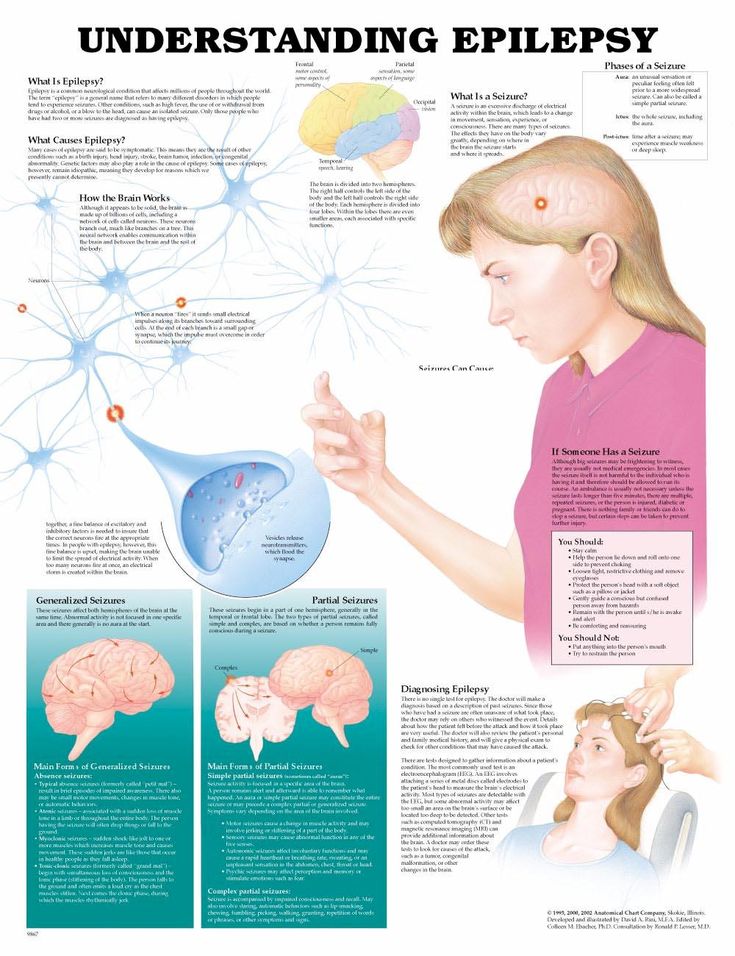
"[Before CBT] I looked at my own hands or other body parts and felt like they weren't mine. I looked at myself in the mirror and didn't realize it was me," explains Sarah.
"I couldn't eat or sleep, and due to stress I lost 42 kg. Now I still have some symptoms, but I can get over them quickly," she continues. nine0011
Treatment is available but difficult to obtain.
As Dr. Hunter says, we need to correct the situation in which patients are forced to look up information about their disorder on the Internet, and then explain to the doctor what it is about. Instead of, on the contrary, the doctor told the patient about his illness.
why a person breaks away from reality
The rhythmic activity of one of the layers of neurons causes dissociation - a change in state associated with a feeling of isolation from the surrounding world. It occurs in people with mental disorders, during anesthesia, or under the influence of certain drugs.
 T&P translated an article from the scientific media Nature, which talks about the results of a Stanford University study on dissociation. nine0125
T&P translated an article from the scientific media Nature, which talks about the results of a Stanford University study on dissociation. nine0125 How dissociation happens
Dissociation is usually described as a "feeling out of touch with reality" or an "out of body" experience. This altered state occurs in people who suffer from mental disorders resulting from severe trauma. Anesthetics can also cause dissociation. The neurological basis of dissociation remained a mystery, but a group of scientists from Stanford University was able to describe the brain rhythm by which changes occur.
The authors looked at neuronal activity in the brains of mice using a technique called "calcium imaging." They studied changes in these brain rhythms in response to a range of drugs that have sedative, anesthetic, or hallucinogenic properties, including those that cause dissociation (ketamine, phencyclidine (PCP) and dizocilpine (MK801).
Only the dissociative drugs caused fluctuations in neuronal activity in an area of the brain called the "retrosplenal cortex. " It is important for cognitive functions, including episodic memory and navigation. The oscillations occurred at a low frequency, on the order of 1–3 hertz. In contrast, non-dissociative drugs such as the anesthetic propofol and lysergic acid diethylamide (LSD) did not induce rhythmic retrosplenial activity.
" It is important for cognitive functions, including episodic memory and navigation. The oscillations occurred at a low frequency, on the order of 1–3 hertz. In contrast, non-dissociative drugs such as the anesthetic propofol and lysergic acid diethylamide (LSD) did not induce rhythmic retrosplenial activity.
The authors studied active cells in more detail using a high-resolution approach called two-photon imaging. This analysis showed that the oscillations were limited to the cells of the fifth layer of the retrosplenial cortex. The authors then recorded neural activity in many areas of the brain. Normally, other parts of the cortex and subcortex are functionally linked to neuronal activity in the retrosplenial cortex, but ketamine caused the connection to break so that many of these brain regions no longer interacted with the retrosplenal cortex. nine0011
The investigators then asked if retrosplenial rhythm induction could cause dissociation. They used mice whose layer five cells had been modified to simultaneously express two light-sensitive ion channel proteins.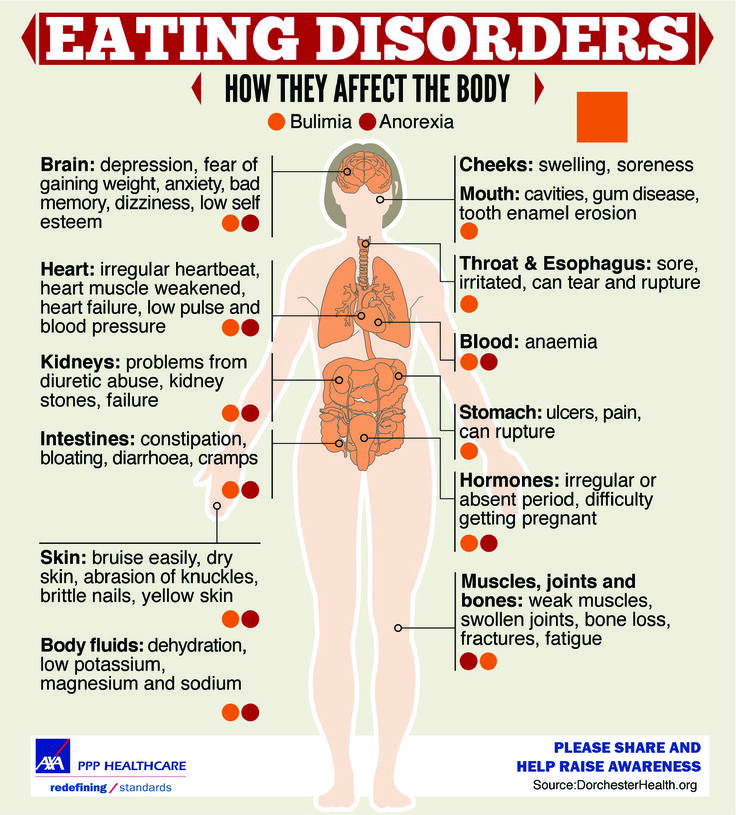 The first, the rhodopsin-2 channel, causes neurons to fire in response to blue light. The second, eNpHR3.0, causes neurons to “stop” on yellow light. Illumination of cells with alternating blue and yellow light to induce an artificial 2 Hz rhythm provoked a behavior indicating a dissociated state, similar to that induced by ketamine. For example, animals did not try to run away when hung by their tails, but usually responded to pain. nine0011
The first, the rhodopsin-2 channel, causes neurons to fire in response to blue light. The second, eNpHR3.0, causes neurons to “stop” on yellow light. Illumination of cells with alternating blue and yellow light to induce an artificial 2 Hz rhythm provoked a behavior indicating a dissociated state, similar to that induced by ketamine. For example, animals did not try to run away when hung by their tails, but usually responded to pain. nine0011
Blunted responses to threats suggest dissociation from the environment
The authors then deleted two genes that code for ion channel proteins in the retrosplenial cortex. The researchers found that the ketamine-induced rhythm was reduced in mice lacking either gene. However, only one channel was needed to induce dissociation.
Do the results of the experiment apply to humans
Researchers have recorded electrical activity in several areas of the brain of a person with epilepsy. He had previously had electrodes implanted in his skull to measure seizure activity.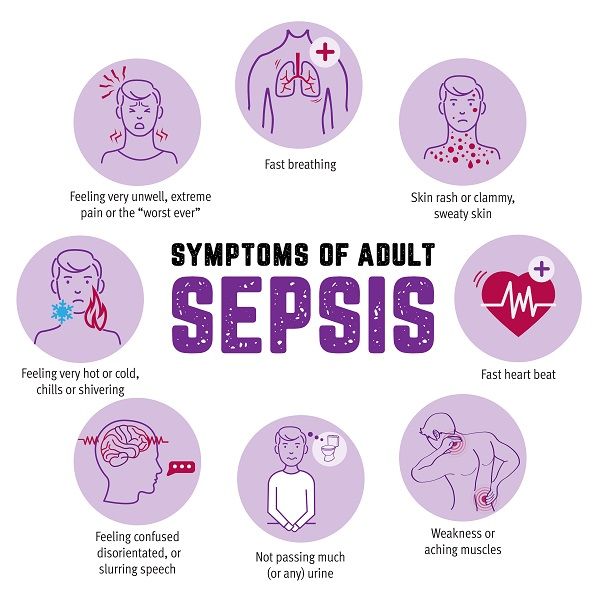 Before the onset of seizures, the person was in a state of dissociation. It correlates with a 3 Hz rhythm in the deep posteromedial cortex, a region of the human brain similar to the retrosplenial cortex in mice. When the team electrically stimulated this cortex during a brain mapping procedure, the person experienced dissociation again. nine0011
Before the onset of seizures, the person was in a state of dissociation. It correlates with a 3 Hz rhythm in the deep posteromedial cortex, a region of the human brain similar to the retrosplenial cortex in mice. When the team electrically stimulated this cortex during a brain mapping procedure, the person experienced dissociation again. nine0011
It is too early to draw final conclusions on one person. However, this study provides strong evidence that low-frequency rhythm in the deep posteromedial cortex is an evolutionarily conserved mechanism that underlies dissociation.
The success of the study is based on the reversible dissociative effects of ketamine. In subanesthetic doses, this drug causes dissociation and analgesia, and also has antidepressant and anti-suicidal properties. At these doses, electroencephalograms (EEGs that measure the activity of neurons on the surface of the brain) show that ketamine significantly suppresses the 8–12 Hz oscillations3. At higher doses that cause unconsciousness, the EEG reveals a rhythm in the frontal lobe of the human brain, alternating between low (1–4 Hz) and high (27–40 Hz) frequencies. Given that these changes occur in large areas of the brain surface, only a small layer of deep cells is responsible for dissociation. nine0011
Given that these changes occur in large areas of the brain surface, only a small layer of deep cells is responsible for dissociation. nine0011
Rapid technological progress leads to the emergence of more and more sophisticated methods for controlling neural circuits with precision and high temporal resolution. These advances make it possible to explore the nature of consciousness itself. They also help in the field of anesthesiology, allowing researchers to better understand how anesthetics cause unconsciousness, how these mechanisms intersect with natural sleep, and how people regain consciousness after anesthesia.
Research on consciousness and anesthesia also overlaps because anesthetics are a powerful and reliable tool for detecting reversible states of altered consciousness. Understanding the neural mechanisms of these altered states could lead to new approaches to consciousness modulation and pain control without the unwanted side effects that lead to changes in heart rate and blood pressure, respiratory arrest, and nausea.