What are symptoms of turrets
Tourette Syndrome Fact Sheet | National Institute of Neurological Disorders and Stroke
What is Tourette syndrome?
What are the signs and symptoms of Tourette syndrome?
How is TS diagnosed?
How is TS treated?
What causes TS?
What research is being done?
Where can I get more information?
What is Tourette syndrome?
Tourette syndrome (TS) is a neurological disorder characterized by sudden, repetitive, rapid, and unwanted movements or vocal sounds called tics. TS is one of a group of disorders of the developing nervous system called tic disorders.
There is no cure for TS, but treatments are available to help manage some symptoms.
Onset of Tics and Duration
Tics come and go over time, varying in type, frequency, location, and severity. The first symptoms usually occur between the ages of 5 and 10 years, generally in the head and neck area and may progress to include muscles of the trunk and arms and legs. Motor tics generally occur before the development of vocal tics and simple tics often precede complex tics.
Most people with TS experience their worst tic symptoms in their early teens, but tics typically lessen and become controlled by the late teens to early 20s. For some people, TS can be a chronic condition with symptoms that last into adulthood. Many people do not need treatment when symptoms do not interfere with daily life. Some individuals may become tic-free or no longer need medication to control their tics. In some cases, tics may worsen in adulthood. TS is not a degenerative condition (one that continues to get worse) and individuals with TS have a normal life expectancy.
top
What are the signs and symptoms of Tourette syndrome?
The motor (involving movement) or vocal (involving sound) tics of Tourette syndrome are classified as either simple or complex. They may range from very mild to severe, although most cases are mild.
Simple tics: sudden, brief, repetitive movements that involve a limited number of muscle groups. They are more common than complex tics.
Complex tics: distinct, coordinated patterns of movement involving several muscle groups.
Examples of motor tics seen in Tourette syndrome
- Simple motor tics include eye blinking and other eye movements, facial grimacing, shoulder shrugging, and head or shoulder jerking.
- Complex motor tics might include facial grimacing combined with a head twist and a shoulder shrug. Other complex motor tics may appear purposeful, including sniffing or touching objects, hopping, jumping, bending, or twisting.
Examples of vocal (phonic) tics in Tourette syndrome
- Simple vocal tics include repetitive throat clearing, sniffing, barking, or grunting sounds.
- Complex vocal tics may include repeating one’s own words or phrases, repeating others’ words or phrases (called echolalia), or more rarely, using vulgar, obscene, or swear words (called coprolalia).
Some of the most dramatic and disabling tics may include motor movements that result in self-harm such as punching oneself in the face or vocal tics such as echolalia or swearing. Some tics are preceded by an urge or sensation in the affected muscle group (called a premonitory urge). Some with TS will describe a need to complete a tic in a certain way or a certain number of times to relieve the urge or decrease the sensation.
Tic triggers
Tics are often worse with excitement or anxiety and better during calm, focused activities. Certain physical experiences can trigger or worsen tics; for example, tight collars may trigger neck tics. Hearing another person sniff or clear the throat may trigger similar sounds. Tics do not go away during light sleep but are often significantly diminished; they go away completely in deep sleep.
Although the symptoms of TS are unwanted and unintentional (called involuntary), some people can suppress or otherwise manage their tics to minimize their impact on functioning. However, people with TS often report a substantial buildup in tension when suppressing their tics to the point where they feel that the tic must be expressed (against their will). Tics in response to an environmental trigger can appear to be voluntary or purposeful but are not.
However, people with TS often report a substantial buildup in tension when suppressing their tics to the point where they feel that the tic must be expressed (against their will). Tics in response to an environmental trigger can appear to be voluntary or purposeful but are not.
Disorders Associated with TS
Many individuals with TS experience additional co-occurring neurobehavioral problems (how the brain affects emotion, behavior, and learning) that often cause more impairment than the tics themselves. Although most individuals with TS experience a significant decline in motor and vocal tics in late adolescence and early adulthood, the associated neurobehavioral conditions may continue into adulthood.
The most common co-occurring conditions include:
- Attention Deficit Hyperactivity Disorder (ADHD), including problems with concentration, hyperactivity, and impulsivity.
- Obsessive Compulsive Disorder or Behaviors (OCD/OCB): repetitive, unwanted thoughts, ideas, or sensations (obsessions) that make the person feel the need to perform behaviors repeatedly or in a certain way (compulsions).
 Repetitive behaviors can include handwashing, checking things, and cleaning, and can significantly interfere with daily life.
Repetitive behaviors can include handwashing, checking things, and cleaning, and can significantly interfere with daily life. - Anxiety (fear, unease, or apprehension about a situation or event that may have an uncertain ending).
- Learning disabilities such as problems with reading, writing, and arithmetic that are not related to intelligence.
- Behavioral or conduct issues, including socially inappropriate behaviors, aggression, or anger.
- Problems falling or staying asleep.
- Social skills deficits and social functioning difficulties, such as trouble with social skills and with maintaining social relationships.
- Sensory processing issues, such as difficulty organizing and responding to sensory information related to touch, taste, smells, sounds, or movement.
Educational Settings
Although students with TS often function well in the regular classroom, ADHD, learning disabilities, obsessive-compulsive symptoms, and frequent tics can greatly interfere with academic performance or social adjustment. After a comprehensive assessment, students should be placed in an educational setting that meets their individual needs. Students may require tutoring, smaller or special classes, private study areas, exams outside the regular classroom, other individual performance accommodations, and in some cases special schools.
After a comprehensive assessment, students should be placed in an educational setting that meets their individual needs. Students may require tutoring, smaller or special classes, private study areas, exams outside the regular classroom, other individual performance accommodations, and in some cases special schools.
top
How is TS diagnosed?
To diagnose TS, a doctor looks for the following:
- Presence of both motor and vocal tics that occur several times a day, every day or intermittently for at least 1 year.
- Onset of tics before age 18.
- Tics not caused by medications, other substances, or medical conditions.
Common tics are often diagnosed by knowledgeable clinicians. However, atypical symptoms (different from classical symptoms) or atypical presentations (for example, symptoms that begin in adulthood) may require specific specialty expertise for diagnosis.
There are no blood, laboratory, or imaging tests needed for diagnosis. In rare cases, neuroimaging studies, such as magnetic resonance imaging (MRI) or computerized tomography (CT), electroencephalogram (EEG) studies, or certain blood tests may be used to rule out other conditions that might be confused with TS.
In rare cases, neuroimaging studies, such as magnetic resonance imaging (MRI) or computerized tomography (CT), electroencephalogram (EEG) studies, or certain blood tests may be used to rule out other conditions that might be confused with TS.
It may take some time to receive a formal diagnosis of TS. Families and physicians unfamiliar with the disorder might think mild and even moderate tic symptoms may be negligible or unimportant, a part of a developmental phase, or the result of another condition. For example, some parents may think that eye blinking is related to vision problems or that sniffing is related to seasonal allergies.
top
How is TS treated?
Because tic symptoms often are mild and do not cause impairment, some people with TS require no treatment. There are effective medications and other treatments for people whose symptoms interfere with daily functioning.
Medications
- Medications that block dopamine (drugs that may be used to treat psychotic and non-psychotic disorders) are the most consistently useful medications to suppress tics (for example, haloperidol and pimozide).
 These drugs may have or cause side effects and should be carefully managed by a physician or healthcare provider
These drugs may have or cause side effects and should be carefully managed by a physician or healthcare provider - Alpha-adrenergic agonists such as clonidine and guanfacine. These medications are used primarily for hypertension (high blood pressure) but are also used in the treatment of tics. These drugs may have or cause side effects and should be carefully managed by a physician or healthcare provider.
- Stimulant medications such as methylphenidate and dextroamphetamine can lessen ADHD symptoms in people with TS without causing tics to become more severe. Previously, these drugs were not recommended for children with tics or TS and those with a family history of tics. Some studies show the short-term use of these drugs can help children with TS who also have ADHD.
- Antidepressants, specifically, serotonin reuptake inhibitors (clomipramine, fluoxetine, fluvoxamine, paroxetine, and sertraline) have been proven effective in some people to control symptoms of depression, OCD, and anxiety.

Unfortunately, there is no one medication that is helpful to all people with TS, nor does any medication completely eliminate symptoms.
Other therapies and treatments can include:
- Behavioral treatments such as awareness training and competing response training can be used to reduce tics. A recent NIH-funded, multi-center randomized control trial called Cognitive Behavioral Intervention for Tics (CBIT) showed that training to voluntarily move in response to a premonitory urge can reduce tic symptoms. Other behavioral therapies, such as biofeedback or supportive therapy, have not been shown to reduce tic symptoms. However, supportive therapy can help a person with TS better cope with the disorder and deal with the secondary social and emotional problems that sometimes occur.
- Psychotherapy can help individuals cope with the disorder and deal with accompanying problems or conditions, including ADHD, depression, anxiety, and OCD.
top
What causes TS?
Most cases of TS involve the interaction of multiple gene variations and environmental factors.
Although the cause of TS is unknown, current research points to abnormalities in certain brain regions (including the basal ganglia, frontal lobes, and cortex), the circuits that connect these regions, and the neurotransmitters (dopamine, serotonin, and norepinephrine) responsible for communication between nerve cells (called neurons).
TS Inheritance
Evidence from twin and family studies suggests that TS is an inherited disorder. A small number of people with Tourette syndrome have mutations involving the SLITRK1 gene, which affects how neurons grow and connect with one another, and scientists continue to look for other genes involved with TS. Abnormalities in the NRXN1 and CNTN6 genes, which also regulate the normal formation of these nerve connections, also may play a role in TS. Although there may be a few genes with substantial effects, it is also possible that many genes with smaller effects and environmental factors may play a role in the development of TS.
It is important for families to understand that genetic tendency may not necessarily result in TS; instead, it may express itself as a milder tic disorder or as obsessive-compulsive behaviors. It is also possible that children who inherit the gene abnormality will not develop any TS symptoms.
Genetic studies also suggest that some forms of ADHD and OCD are genetically related to TS, but there is less evidence for a genetic relationship between TS and other neurobehavioral problems that commonly co-occur with TS.
The gender of the person also plays an important role in TS gene expression. At-risk males are more likely to have tics and at-risk females are more likely to have obsessive-compulsive symptoms.
Genetic counseling of individuals with TS should include a full review of all potentially hereditary conditions in the family.
top
What research is being done?
Within the Federal government, the National Institute of Neurological Disorders and Stroke (NINDS), a part of the National Institutes of Health (NIH), is responsible for supporting and conducting research on the brain and nervous system. NINDS and other NIH components, such as the National Institute of Mental Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Drug Abuse, and the National Institute on Deafness and Other Communication Disorders, support research of relevance to TS, either at NIH laboratories or through grants to major research institutions across the country.
NINDS and other NIH components, such as the National Institute of Mental Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, the National Institute on Drug Abuse, and the National Institute on Deafness and Other Communication Disorders, support research of relevance to TS, either at NIH laboratories or through grants to major research institutions across the country.
Another component of the Department of Health and Human Services, the Centers for Disease Control and Prevention (CDC), funds professional education programs as well as TS research.
Knowledge about TS comes from studies across numerous medical and scientific disciplines, including genetics, neuroimaging, neuropathology, clinical trials (medication and non-medication), epidemiology, neurophysiology, neuroimmunology, and descriptive/diagnostic clinical science.
Genetic studies. Currently, NIH-funded investigators are conducting a variety of large-scale genetic studies involving TS. Understanding the genetics of TS genes may strengthen clinical diagnosis, improve genetic counseling, lead toward a better understanding of its causes, and provide clues for more effective therapies.
Understanding the genetics of TS genes may strengthen clinical diagnosis, improve genetic counseling, lead toward a better understanding of its causes, and provide clues for more effective therapies.
Neurostimulation. NINDS-funded research is testing the effectiveness and safety of deep-brain stimulation (DBS) for treating tics and co-occurring conditions, such as obsessive-compulsive behaviors, in individuals with TS who do not respond well to medications and behavioral therapy. DBS uses a surgically implanted, battery-operated medical device called an implantable pulse generator (IPG)—similar to a heart pacemaker and approximately the size of a stopwatch—to deliver electrical stimulation to specific areas in the brain that control movement, which blocks the abnormal nerve signals that cause symptoms.
Neuroimaging studies. Advances in imaging technology and an increase in trained investigators have led to an increasing use of novel and powerful techniques to identify brain regions, circuitry, and neurochemical factors important in TS and related conditions, such as ADHD and OCD.
Neuropathology (the study of nervous system diseases). There has been an increase in the number and quality of donated brains from TS patients available for research purposes. This increase, coupled with advances in neuropathological techniques, has led to initial findings with implications for neuroimaging studies and animal models of TS.
Clinical trials. Several clinical trials in TS recently have been completed or currently are underway. These include studies of stimulant treatment of ADHD in TS and behavioral treatments for reducing tic severity in children and adults. Smaller trials of novel approaches to treatment such as dopamine agonists and glutamatergic medications also show promise. Neurostimulation treatments such as DBS and noninvasive transcranial magnetic stimulation in children and adults are also ongoing.
Epidemiology and clinical science. Careful epidemiological studies (those that track the pattern or incidence of a disease) now estimate the prevalence of TS to be substantially higher than previously thought, with a wider range of clinical severity. Furthermore, clinical studies are providing new findings regarding TS and co-existing conditions. These include subtyping studies of TS and OCD, an examination of the link between ADHD and learning problems in children with TS, and a new appreciation of sensory tics. One of the most important and controversial areas of TS science involves the relationship between TS and autoimmune brain injury associated with group A beta-hemolytic streptococcal infections or other infectious processes. There are many epidemiological and clinical investigations currently underway in this area.
Furthermore, clinical studies are providing new findings regarding TS and co-existing conditions. These include subtyping studies of TS and OCD, an examination of the link between ADHD and learning problems in children with TS, and a new appreciation of sensory tics. One of the most important and controversial areas of TS science involves the relationship between TS and autoimmune brain injury associated with group A beta-hemolytic streptococcal infections or other infectious processes. There are many epidemiological and clinical investigations currently underway in this area.
top
How can I help with research?
Consider joining a clinical study. Both healthy individuals and those with a disease or condition can participate in medical research studies (sometimes called clinical trials or protocols) to help researchers better understand a disease and perhaps develop new treatments. For information about clinical studies on disorders including Tourette syndrome and how to participate in one, please contact the NIH’s Patient Recruitment and Public Liaison office at 800-411-1222 or visit the Clinicaltrials. gov website at http://www.clinicaltrials.gov.
gov website at http://www.clinicaltrials.gov.
top
Where can I get more information?
For more information on neurological disorders or research programs funded by the National Institute of Neurological Disorders and Stroke, contact the Institute's Brain Resources and Information Network (BRAIN) at:
BRAIN
P.O. Box 5801
Bethesda, MD 20824
800-352-9424
Other NIH research efforts. More information about research on Tourette syndrome supported by NINDS and other NIH Institutes and Centers can be found using NIH RePORTER, a searchable database of current and past research projects supported by NIH and other federal agencies. RePORTER also includes links to publications and resources from these projects. Enter “Tourette syndrome” to start your search.
Information also is available from the following
Child Neurology Foundation (link is external)
201 Chicago Avenue, Suite 200
Minneapolis, MN 55415
info@childneurologyfoundation. org (link sends e-mail) (link sends e-mail)
org (link sends e-mail) (link sends e-mail)
Tel: 612-928-6325
Tourette Association of America
42-40 Bell Boulevard, Suite 205
Bayside, NY 11361-2820
[email protected]
Tel: 718-224-2999; 888-486-8738
U.S. Centers for Disease Control and Prevention (CDC)
Information and statistics on Tourette Syndrome
800-232-4636
MedlinePlus
National Library of Medicine
National Institutes of Health
"Tourette Syndrome Fact Sheet", NINDS, Publication date April 2021
NIH Publication No. 21-NS-2163
Back to Tourette Syndrome Information Page
See a list of all NINDS disorders
Publicaciones en Español
Síndrome de Tourette
Prepared by:
Office of Communications and Public Liaison
National Institute of Neurological Disorders and Stroke
National Institutes of Health
Bethesda, MD 20892
NINDS health-related material is provided for information purposes only and does not necessarily represent endorsement by or an official position of the National Institute of Neurological Disorders and Stroke or any other Federal agency. Advice on the treatment or care of an individual patient should be obtained through consultation with a physician who has examined that patient or is familiar with that patient's medical history.
Advice on the treatment or care of an individual patient should be obtained through consultation with a physician who has examined that patient or is familiar with that patient's medical history.
All NINDS-prepared information is in the public domain and may be freely copied. Credit to the NINDS or the NIH is appreciated.
Tourette's syndrome - NHS
Tourette's syndrome is a condition that causes a person to make involuntary sounds and movements called tics.
It usually starts during childhood, but the tics and other symptoms usually improve after several years and sometimes go away completely.
There's no cure for Tourette's syndrome, but treatment can help manage symptoms.
People with Tourette's syndrome may also have obsessive compulsive disorder (OCD), attention deficit hyperactivity disorder (ADHD) or learning difficulties.
Symptoms of Tourette's syndrome
Tics are the main symptom of Tourette's syndrome. They usually appear in childhood between the ages of 2 and 14 (around 6 years is the average).
They usually appear in childhood between the ages of 2 and 14 (around 6 years is the average).
People with Tourette's syndrome have a combination of physical and vocal tics.
Examples of physical tics include:
- blinking
- eye rolling
- grimacing
- shoulder shrugging
- jerking of the head or limbs
- jumping
- twirling
- touching objects and other people
Examples of vocal tics include:
- grunting
- throat clearing
- whistling
- coughing
- tongue clicking
- animal sounds
- saying random words and phrases
- repeating a sound, word or phrase
- swearing
Swearing is rare and only affects about 1 in 10 people with Tourette's syndrome.
Tics are not usually harmful to a person's overall health, but physical tics, such as jerking of the head, can be painful.
Tics can be worse on some days than others.
They may be worse during periods of:
- stress
- anxiety
- tiredness
People with Tourette's syndrome can have mood and behavioural problems, such as:
- attention deficit hyperactivity disorder (ADHD)
- obsessive compulsive disorder (OCD)
- depression or anxiety
Children with Tourette's syndrome may also be at risk of bullying because their tics might single them out.
Premonitory sensations
Most people with Tourette's syndrome experience a strong urge before a tic, which has been compared to the feeling you get before needing to itch or sneeze.
These feelings are known as premonitory sensations. Premonitory sensations are only relieved after the tic has been carried out.
Examples of premonitory sensations include:
- a burning feeling in the eyes before blinking
- a dry or sore throat before grunting
- an itchy joint or muscle before jerking
Controlling tics
Some people can control their tics for a short while in certain social situations, like in a classroom. It requires concentration, but gets easier with practise.
Controlling tics can be tiring. A person may have a sudden release of tics after a day trying to control them, like after returning home from school.
Tics may be less noticeable during activities involving a high level of concentration, such as reading an interesting book or playing sports.
When to get medical advice
You should contact a GP if you or your child start having tics.
Many children have tics for several months before growing out of them, so a tic does not necessarily mean your child has Tourette's syndrome.
Diagnosing Tourette's syndrome
There's no single test for Tourette's syndrome. Tests and scans, such as an MRI scan, may be used to rule out other conditions.
You can be diagnosed with Tourette's syndrome if you've had several tics for at least a year.
Getting a firm diagnosis can help you and others understand your condition better, and give you access to the right kind of treatment and support.
To get a diagnosis, a GP may refer you to different specialists, such as a neurologist (a brain and nervous system specialist).
Treating Tourette's syndrome
There's no cure for Tourette's syndrome and most children with tics do not need treatment for them.
Treatment may sometimes be recommended to help you control your tics.
Treatment is usually available on the NHS and can involve:
- behavioural therapy
- medicine
Behavioural therapy
Behavioural therapy is usually provided by a psychologist or a specially trained therapist.
2 types of behavioural therapy have been shown to reduce tics:
- habit reversal training – this approach involves working out the feelings that trigger tics; the next stage is to find an alternative, less noticeable way of relieving the urge to tic
- exposure with response prevention (ERP) – this method trains you to better control your urge to tic; techniques are used to recreate the urge to tic to train you to tolerate the feeling, without doing the tic, until the urge passes
Medicine
Some people's tics are helped with medicines, but this is usually only recommended if the tics are more severe or affecting daily activities.
Medicines for Tourette's syndrome can have side effects and they will not work for everyone.
Causes of Tourette's syndrome
The cause of Tourette's syndrome is unknown. It's thought to be linked to a part of the brain that helps regulate body movements.
For unknown reasons, boys are more likely to be affected by Tourette's syndrome than girls.
Further help and support
For more information about treatment and support, contact the charity Tourettes Action.
Video: Tourette's syndrome
In this video, a neurologist talks about Tourette's syndrome and what treatment and support is available.
Media last reviewed: 1 February 2021
Media review due: 1 February 2024
Page last reviewed: 04 January 2021
Next review due: 04 January 2024
Dr. Mazda K. Turel - popular neurosurgeon: Book appointment, reviews
Dr. Mazda K. Turel - popular neurosurgeon: Book appointment, reviews | Medidgens
Mazda K. Turel - popular neurosurgeon: Book appointment, reviews | Medidgens Get the best quote
- Announcement
- DRISTRY
- procedure
- Frequently asked questions
Biography
Conditions treated by Mazda K. Turele
Neurosurgery - this is a medical specialist who diagnoses and treats the conditions influenced to the nervous system, including the brain, peripheral nerves, spinal cord and spine. Neurosurgeons offer patients both non-surgical and surgical treatment. Here is a list of some of the conditions that Dr. Mazda K. Turel treats:
TURLETOMS, and symptoms, and symptoms, and symptoms, and symptoms, and symptoms, and symptoms that are the same.

If your body exhibits any of the following symptoms, see a neurosurgeon who can help diagnose the underlying conditions. Some conditions may be mild, while others may require immediate attention. Timely correct diagnosis can prevent serious diseases. nine0003
- Fatigue
- Prominent scalp veins
- Drowsiness
- Memory problems
- Seizures
- Nausea or vomiting
- Moderate to severe pain in the lower back, buttocks and legs.
- Limited range of motion
- Unusually large head size
- Numbness or weakness in the lower back, buttocks, legs, or feet
- Stiffness in the lower back
- Muscle spasms during activity or at rest
- Inability to maintain normal posture due to stiffness and/or pain
- Pain aggravated by movement; loss of movement
- Headaches that may be severe and worse with physical activity or in the early morning.
- Eye downward deviation or sunset sign
- Rapidly increasing head circumference
- Trouble sleeping
- "Tingling" in legs, toes or feet
- Bulging and tight fontanel or soft spot
Neurological symptoms are usually caused by a disorder that affects the nervous system and can vary greatly because the nervous system controls many different bodily functions.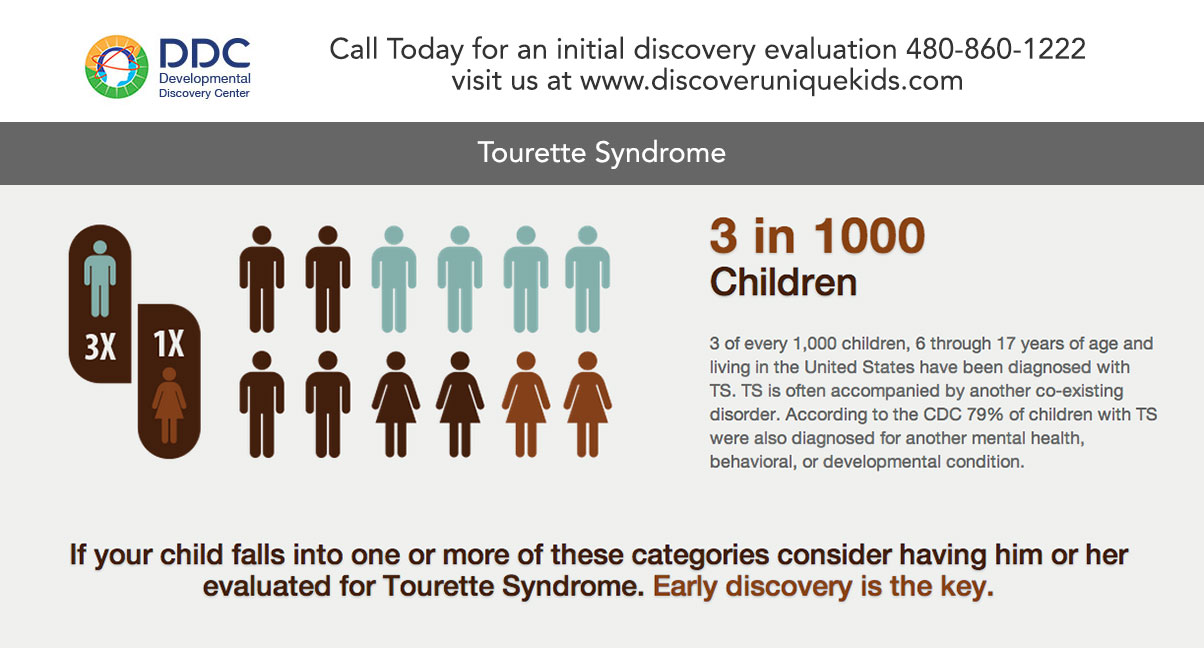 Symptoms can be any form of pain and can include muscle function, special feelings, sleep, awareness, and mental activity.
Symptoms can be any form of pain and can include muscle function, special feelings, sleep, awareness, and mental activity.
Opening hours Mazda K Turel
Mazda K Turel doctor's hours of operation are Monday to Saturday from 11 am to 5 pm. The doctor has Sunday off. Although the doctor is mostly available during business hours, you should check with the doctor about their availability and then visit their clinic/hospital. nine0003
Popular procedures performed by Dr. Mazda K. Turel
Popular procedures performed by the doctor Mazda K Turel are listed below:
- Deep stimulation of the brain
- Disc replacement (neck / lumber)
- 9000
- Craniotomy
- spondyx
- Kyphoplasty
- Brain Tumor Treatment
- Laminectomy
- Scoliosis Surgery
Dr. Mazda K. Turel is a renowned neurosurgeon known for his patient-centered approach and high success rate. The physician fully evaluates the patient's condition before performing any procedure to understand the risk associated with the procedure. With vast experience in handling even the most complex cases with high precision and accuracy, the doctor follows medical protocols to ensure the safety of the patient. Also, the doctor is aware of the latest techniques. nine0003
With vast experience in handling even the most complex cases with high precision and accuracy, the doctor follows medical protocols to ensure the safety of the patient. Also, the doctor is aware of the latest techniques. nine0003
Qualification
- MBBS
- M.CH
Cast experience
- Senior resident of the University of Rasha, Chicago, USA
- Senior Oddinator - Western Hospital of Toronto, Canada,
- Associate Professor - Christian medical college, Christian medical college, Christian medical college, Christmas Medical Medical Vellore,
Telemedicine Physicians
Dr. Manoj Khanal
Neurologist
New Delhi, India
 Dandy
Dandy Share your experience about Mazda
Write review 9000
Frequent Mazda K. Turret is a specialized neuro -child and one of the most pre -sedentary .
No, this doctor does not offer telemedicine through MediGence.
Dr. Mazda K Turel is one of the most sought after specialists in India with over 9 years of experienceyears.
Frequently asked questions related to the neurosurgeon
Neurosurgeons perform surgical treatment of diseases of the brain and spine. They are considered one of the very experienced and trained professionals in the field of medicine and consult with other doctors on various issues. Neurosurgeons treat people with a range of neurological problems such as low back pain, brain tumors, carpal tunnel syndrome, and diseases of the peripheral nervous system. Neurosurgeons mainly see patients in their clinics, as well as public and private hospitals. Sometimes they have to work with other specialists and medical experts to get their opinion on diagnosis and surgical procedures. They also evaluate diagnostic tests to know the exact underlying conditions and proceed with treatment accordingly. nine0003
Neurosurgeons mainly see patients in their clinics, as well as public and private hospitals. Sometimes they have to work with other specialists and medical experts to get their opinion on diagnosis and surgical procedures. They also evaluate diagnostic tests to know the exact underlying conditions and proceed with treatment accordingly. nine0003
Diagnostic tests are an important tool for determining the condition from which the patient is suffering. So, the neurosurgeon will ask you to do some tests to find out the cause of the symptoms, which will later help to find the condition the patient is suffering from. Based on the diagnosis, the doctor can initiate appropriate treatment. For a complete assessment of your condition, you will need a neurological examination, which may include the following:
- Blood tests
- MRI of the brain
- Myelogram
- Luminical puncture
- CT brain
- Study of nervous conductivity velocity / Electromiography
- Neurological exam
- X -ray
- 9000 9000 MRI spine
for diagnosing neurological states one or more of the following tests:
- Cerebral angiogram
- Myelogram CT
- Computer tomography
- Luminical puncture
- MRI
- X -ray pictures
- Electromycephalogram
- Electromiogram
- Spinal puncture KT
You need to visit the neurosurgery when any of the following features appear: 9000
Neurosurgeons perform complex brain surgeries. In addition, they deal with the entire nervous system and treat all parts of the body affected by nervous diseases. Usually, the neurosurgeon diagnoses the patient's symptoms and draws up a minimally invasive treatment plan.
In addition, they deal with the entire nervous system and treat all parts of the body affected by nervous diseases. Usually, the neurosurgeon diagnoses the patient's symptoms and draws up a minimally invasive treatment plan.
Tourelles Bridge - frwiki.wiki
Pont de Tourelles is an old French bridge crossing the Loire at Orléans.
Summary
- 1 Geography
- 2 History
- 2.1 From the 12th - to the 15th - centuries: gradually fortified bridge [ 1 ]
- 2.2 1429: Siege of Orleans [ 2 ]
- 2.3 From the 15th - to the 17th - centuries: the influence of the weather
- 2.4 1628: first bars in basket handles [ 1 ]
- 2.5 1745: bridge critical [ 1 ]
- 2.6 1760: demolition [ 1 ]
- 3 Description
- 4 Notes and references
- 5 See also
- 5.
 1 Related articles
1 Related articles - 5.2 External link
- 5.3 Bibliography
- 5.
Geography
Location of the bridge over the Loire
The Pont de Tourelles connects the two banks of the Loire, from the fortress of Chatelet on the right bank to the fort of Tourelles on the left bank. It is erected a hundred meters upstream from the site of the current George-V bridge in the city of Orléans, then located in the province of Orléanais in the Kingdom of France. nine0003
History
XII - to XV - gradually strengthened bridge
The construction of the bridge takes 20 years, between 1120 and 1140.
The Tourelle Bridge has experienced many vicissitudes due to bad weather - floods and ice breaking, but also as a result of the battles and sieges that it has witnessed. The damage done to it over the centuries naturally leads to repairs and, in many cases, structural changes. nine0003
nine0003
Since its foundation, the bridge has 21 arches, including 14 between the turrets and the Saint-Antoine turret and seven between this arch and the Chatelet.
After the defeat faced by the English troops at the Battle of Agincourt during the Hundred Years' War, the Orléans decided to strengthen the defenses of their city and from 1417 built boulevards on the hill of Saint-Antoine, a great bastille built in timber.
1429: Siege of Orléans
Plan of the Tourelles Bridge - Eugene Viollet-le-Duc
When the English laid siege to Orleans, they, moving along the left bank of the Loire, presented themselves, coming from the natural region of Sologne, opposite the Boulevard de Tourelles (see map opposite, at A ). Then this boulevard is just a product of earth and wood. At , they capture it, and the inhabitants of Orléans leave the Fort de Tourelles (at B ) to retire to the Bastille Saint-Antoine (at F ) located on the island, after having received precautionary measures by cutting the arch (at I ) of this part of the bridge. The British, for their part, cut the arch (at K ). Orléans hastily found a wooden boulevard on Belle Croix (at C ). It is in this narrow space that the most notable military exploits take place. The Bastille Saint-Antoine (at F ) is preceded by a chapel (at D ) placed under the name of this saint, and a chaplain (at E ) intended to receive pilgrims and backward travelers. B H is the city gate and at G is the lock.
The British, for their part, cut the arch (at K ). Orléans hastily found a wooden boulevard on Belle Croix (at C ). It is in this narrow space that the most notable military exploits take place. The Bastille Saint-Antoine (at F ) is preceded by a chapel (at D ) placed under the name of this saint, and a chaplain (at E ) intended to receive pilgrims and backward travelers. B H is the city gate and at G is the lock.
The second drawbridge is practiced in front of the city gate H . A perspective view by the French architect Eugène Viollet-le-Duc shows the entrance to the Pont d'Orléans, with its boulevard on the left bank, from the Solon side, after repairs carried out after the 1428 siege.
In 1591 and 1592 we rebuilt this boulevard (at A ) with casemates in the shape of a double-pincer ravelin, at a time when the Porte de Tourelles still existed. nine0003
Belle-Croix, located at C on the forepeak of one of the bridge piers, is a bronze monument consisting of a crucifix mounted on a plinth decorated with a bas-relief representing the Blessed Virgin, Saint Peter, Saint Paul, Saint Jacques, Saint-Étienne and the Bishops of Orléans Saint-Aignan and Saint-Evert. In the Middle Ages it was common practice to place a cross in the middle of bridges. In front of the Boulevard de Tourelles is the monastery of the Augustins, which the inhabitants of Orléans destroyed when the English arrived to clear the area around the castle. However, this monastery itself is surrounded by a fence and a moat and can serve as an advanced defense. Therefore, we drive up only in front of the entrance to the Orleans bridge, as well as in front of the entrance to the Calendra bridge in Cahors, on the side. nine0003
In the Middle Ages it was common practice to place a cross in the middle of bridges. In front of the Boulevard de Tourelles is the monastery of the Augustins, which the inhabitants of Orléans destroyed when the English arrived to clear the area around the castle. However, this monastery itself is surrounded by a fence and a moat and can serve as an advanced defense. Therefore, we drive up only in front of the entrance to the Orleans bridge, as well as in front of the entrance to the Calendra bridge in Cahors, on the side. nine0003
XV - to XVII - : influence of weather
Drawing of the Tourelles bridge - Eugene Viollet-le-Duc
The bridge must have been badly damaged during these difficult months: in particular, four arches were broken. In addition, after the departure of the enemy, we thought about restoring it, as well as the boulevard and Fort de Tourelles, also tested. They started by building a temporary footbridge to restore the passage.
They started by building a temporary footbridge to restore the passage.
Ice Decay from 1434 - 1435 caused severe damage to the bridge section between the islet and the Shuttle; Only the second arch from him could be preserved of the seven he had. The remaining six were replaced by four new, more significant ones. From that moment on the bridge, there were 19arches. This was the case until the period between 1555 and 1630. Then and until his death in XVIII - m century, it is represented by more than 18 arches, whose thirteen towers and between the island and five between it and the Chatelet.
1628: first bows in basket handles
The first vaults were semicircular or pointed arches. It was not until 1628 that the first replacement of the semi-circular arch by a three-point arch took place, when, after a severe flood that put the whole structure to the severe test, it was necessary to restore the arch of the caboose adjacent to La Motte. -Antoine, on the north side. nine0003
-Antoine, on the north side. nine0003
In subsequent periods, the bridge continued to deteriorate, mainly due to floods and icing that shook the supports. This was especially true in 1732. With signs of fatigue recurring more and more, the Orléans, who were not resigned to letting their old bridge die, have ramped up repairs, consolidations and partial renovations.
1745: critical condition of the bridge
In 1745 the situation between the Chatelet and the hospital was so unsettling that engineers had to be called in from Paris. nine0003
Robert Pitrou, then Inspector General of Pont et Chaussé, was charged in 1746 with removing the danger posed by the great arch known as the Virgin and its neighbour, on the side of the city. But six years later, in 1751, when the construction of the Royal Bridge began, alarming symptoms appeared on the two supported vaults; the authorities decided to demolish two arches and replace them with a wooden footbridge.
1760: demolition
For nine years, while the construction of the Royal Bridge lasted, the old medieval bridge, out of breath, continued to provide a link between the two banks. But in July 1760, after the opening of the new building for traffic, it began to be demolished, starting with the buildings located on the outskirts of the city and on the island. The demolition of the Turel fortress began in December. To clear the Loire, the island was cleared in 1760 and 1761, which was completed in 1762. Only the Chatelet was still standing. He had only a few years to live. nine0003
But in July 1760, after the opening of the new building for traffic, it began to be demolished, starting with the buildings located on the outskirts of the city and on the island. The demolition of the Turel fortress began in December. To clear the Loire, the island was cleared in 1760 and 1761, which was completed in 1762. Only the Chatelet was still standing. He had only a few years to live. nine0003
The demolition of the bridge was carried out under a special tender for £10,000, materials were left to the contractor. The poles were blackened to the depths of oak, they were beautiful ebony, they were used to make measuring boards, rulers and walking sticks in great demand.
Description
Plan of the city of Orleans. By Alphonse Gatineau, printer, 1836, detail: Pont Royal and old Pont de Tourelles (destroyed).
The length of the bridge was 331 meters, and the width varied from 9,75 m to 10. 40 m , which made its carriageway one of the widest among the carriageways of medieval bridges.
40 m , which made its carriageway one of the widest among the carriageways of medieval bridges.
It was divided along its length by an island formed by the union of two clods, the motte Saint-Antoine upstream and the motte des Chalands-percés or Poissonniers downstream.
From the very beginning of the bridge on the Motte Saint-Antoine, a hospital, an orphanage Saint-Antoine and a chapel, the Saint-Antoine chapel, were built at the same time.
Early XV - th century, on a covered veranda, passing along the floor, in the transverse direction, establishes a connection between the two buildings.
From the beginning of XIV - th centuries, several fishermen's houses appeared on the fish embankment.
Notes and links
- ↑ a b c d e f Collective 1993, p.
 ?
? - ↑ Dictionary of French Architecture from XI - th to XVI - . Volume 2, Boutiss.
See also
Related articles
- List of bridges over the Loire
- List of bridges in the Loire
External link
- Personal website on the history of Orleans
Bibliography
- Alexandre Collin, Le Pont des Tourelles in Orléans (1120-1760): a study of bridges in the Middle Ages , Orléans, H. Herluison, ( read online ) .
- Royal Bridge Collective : George V Bridge at Orléans; its construction, its history , Orleans, Society of Friends of the Museums of Orleans, , 221 p. ( ISBN 2-9503926-3-6, EAN 9782950392633) .
| Bridges by type and length | |
|---|---|
| Structures | Suspension bridge · Cable-stayed bridge · Arch bridge · String bridge · Cantilever bridge · Truss bridge · Floating bridge · Movable bridge · Drawbridge · Drawbridge · Submersible bridge · Swing bridge · Conveyor bridge · Bailey bridge · Timber bridge · Populated bridge · covered bridge crutches bridge vierendeel bridge nine0705 |
| Materials | Metal bridge Reinforced concrete bridge Prestressed concrete bridge Timber bridge Masonry bridge Steel concrete composite bridge |
| Modes of transport | Gateway · Monkey Bridge · Railway Bridge · Highway Bridge · Canal Bridge · Air Bridge · Interrupted Bridge · Tarpaulin Bridge |
| Large axles | The longest bridges · Suspension bridges · Cable-stayed bridges · Arched bridges · Cantilever bridges. |