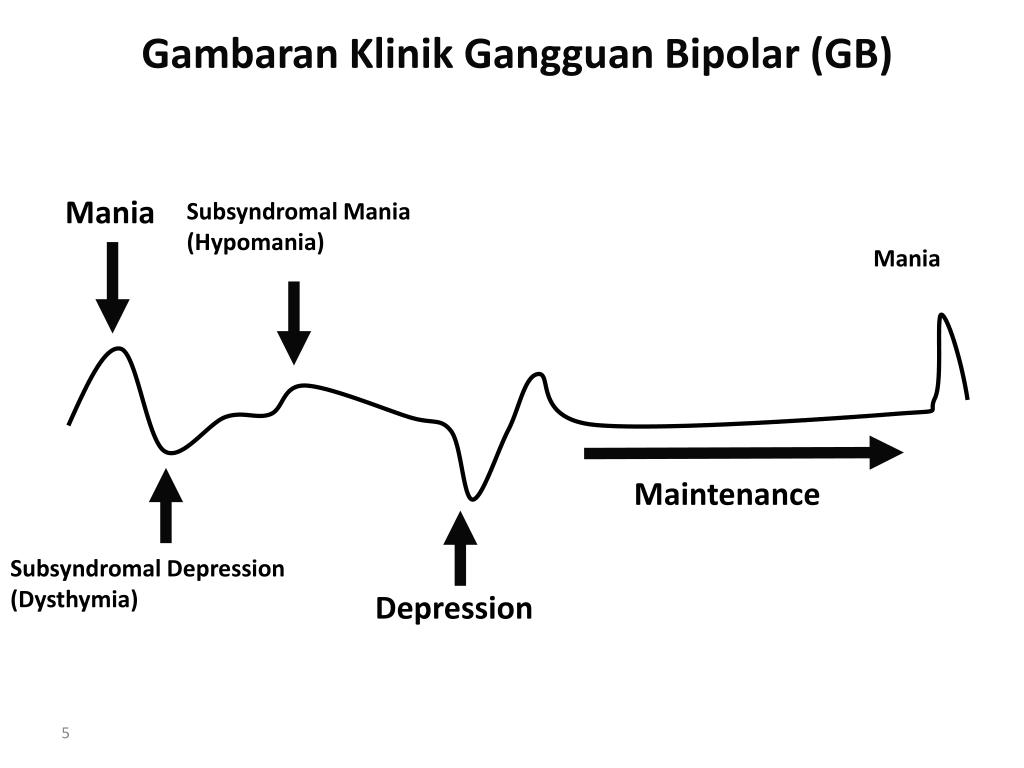
Types of hypomania
A More Nuanced View of Hypomania
Is dysphoric hypomania a phase of mania itself? Or does it represent a descent into a mixed state?
©ChristosGeorghiou/ Shutterstock
RESEARCH UPDATE
Hypomania is often characterized as a euphoric experience, a “mild version of mania.” For example, here’s WebMD:
"It’s a less severe form of mania. It actually may feel pretty good because your mood is up and you have more energy than usual, but it’s not out of control. The problem is that for someone with bipolar disorder, hypomania can evolve into mania. Or it can switch to serious depression."
Or Wikipedia; though slightly more balanced (irritability is mentioned), it describes hypomania thus:
"Characteristic behaviors are extremely energetic, talkative, and confident commonly exhibited with a flight of creative ideas."
Doesn’t that sound appealing? If hypomania was just mild mania, why wouldn’t people want to return to it? This way of thinking about hypomania reinforces some practitioners’ inclination to blame patients for being non-compliant: “they just want their highs. ”
The problem is that pure euphoric hypomanias are, in my experience, rather uncommon. True, patients don’t come in to see us to complain of euphoric hypomania. But I don’t hear about this very often during their subsequent depressions. Patients more commonly go through a phase that is initially pleasurable; but later, perhaps driven by the decreased sleep that accompanies early hypomania, the experience can change into something much more dysphoric.
For example, a blogger writes: “I start feeling burned out. While I still have a lot of energy, I don't have that ‘I love the world’ feeling . . . things don't just slide off my back. While I try not to ‘snap’ back at people, I am not always successful . . . I become far less happy, joyful, and kind. I dislike being criticized in any which way.”
For another rich example, see Sarah Sullivan’s blog on dysphoric hypomania. Or for a book-length account of the complexity of mood experience-in case you don’t get to hear these details daily-check out Lost Marbles by Natasha Tracy. She describes excruciating agitation with intense, relentless suicidal ideation during nights of no sleep at all. She discovered that moderate self-harm provided some temporary relief from these states, demonstrating that cutting is not pathognomonic for borderline personality disorder, as also observed by other bloggers and researchers.1,2
She describes excruciating agitation with intense, relentless suicidal ideation during nights of no sleep at all. She discovered that moderate self-harm provided some temporary relief from these states, demonstrating that cutting is not pathognomonic for borderline personality disorder, as also observed by other bloggers and researchers.1,2
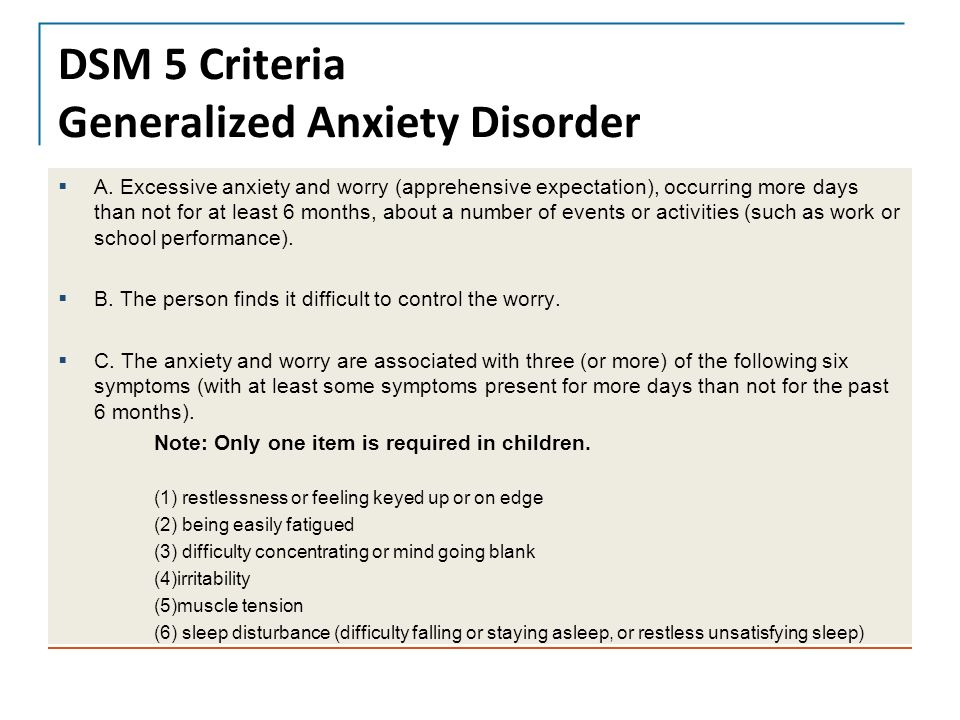
Is dysphoric hypomania a phase of mania itself? Or does it represent a descent into a mixed state? Does this even matter? Patients’ accounts of the complexity of their mood experience, such as those above, make the DSM-5–induced controversy over which symptoms to count toward a mixed state almost comical. Granted, multiple agencies want lines drawn somewhere (eg, insurance companies, the FDA, the military, the legal system). We can thank the DSM committee members for their efforts. But let’s not confuse the criteria with the complex reality of the illness.
We can thank the DSM committee members for their efforts. But let’s not confuse the criteria with the complex reality of the illness.
Take irritability. While disallowed by the DSM-5 mixed state definition, this symptom is prominent in research studies that quantify symptoms during mixed states. For example, in the BRIDGE-II-MIX study, irritability was overall the most common mixed state symptom (depending on which definition for the condition was used).3Gin Malhi and colleagues from Australia recently coined the acronym “DIP” for distractibility, irritability, and psychomotor agitation. They found these 3 symptoms, all disallowed by the DSM-5, “may be cardinal features of mixed states.”4
Take insomnia. In dysphoric hypomania, this is not the classic “decreased need for sleep.” Patients would love some lorazepam or zolpidem. Indeed, they may be perceived by physicians as “drug-seeking,” which is utterly ironic if the same physician is prescribing an antidepressant that might be inducing these mixed state symptoms. Unfortunately, I think this is extremely common, based on the primary care psychiatric consults I’m doing these days.
Defining mixed states, including dysphoric hypomania, is less tortuous if one adopts a “dimensional” (jargon term for spectrum) approach to diagnosis-as recommended by the head of the Bipolar Spectrum Division of the National Institute of Mental Health.5 (Note the title of her division.) A dimensional view of mixed states regards depression as a continuum, from not at all mixed to fully mixed.6
But researchers prefer to use cutoffs. One of the most recent analyses from the longitudinal Stanley Foundation dataset used the Young Mania Rating Scale (YMRS) and set the cutoff for mixed depression as more than 2 on the YMRS. Of all the visits with bipolar depression over a 7-year period, 43% were mixed, using that definition.7 In other words, mixed states-more broadly defined than the DSM-5 criteria-are extremely common.
Does all this terminology matter?
Mixed states are extremely puzzling to patients-and some practitioners. The very term “bipolar” promotes the opposite conception: contrary “poles,” which as such could not possibly “mix.” One patient went 24 years without recognizing her bipolarity because of this terminology; she experienced a dramatic turnaround in course and understanding with individual psychoeducation (20 minutes each therapy visit spent reading from a textbook!).
8 Our group found that antidepressant tapers were associated with resolution of suicidal ideation in a small case series of patients who likely had mixed states, but did not meet DSM-IV criteria for bipolar disorders.9
The very term “bipolar” promotes the opposite conception: contrary “poles,” which as such could not possibly “mix.” One patient went 24 years without recognizing her bipolarity because of this terminology; she experienced a dramatic turnaround in course and understanding with individual psychoeducation (20 minutes each therapy visit spent reading from a textbook!).
8 Our group found that antidepressant tapers were associated with resolution of suicidal ideation in a small case series of patients who likely had mixed states, but did not meet DSM-IV criteria for bipolar disorders.9
The bottom line
With the advent of the DSM-5, Bipolar II can finally be recognized as having mixed states (in the DSM-IV, only full mania and full depression counted). So now, dysphoric hypomania can be formally recognized. Perhaps this will help us all move beyond simplistic descriptions of hypomania that can leave patients and practitioners wondering if dysphoric, agitated states can be “bipolar. ”
”
Disclosures:
Dr. Phelps is Director of the Mood Disorders Program at Samaritan Mental Health in Corvallis, Ore. He is the Bipolar Disorder Section Editor for Psychiatric Times. Dr. Phelps stopped accepting honoraria from pharmaceutical companies in 2008 but receives honoraria from McGraw-Hill and W.W. Norton & Co. for his books on bipolar disorders.
References:
1. John H, Sharma V. Misdiagnosis of bipolar disorder as borderline personality disorder: clinical and economic consequences. World J Biol Psychiatry. 2009;10(4 Pt 2):612-615.
2. Pope CJ, Xie B, Sharma V, Campbell MK. A prospective study of thoughts of self-harm and suicidal ideation during the postpartum period in women with mood disorders. Arch Womens Ment Health. 2013;16:483-488.
3. Perugi G, Angst J, Azorin JM, et al; BRIDGE-II-Mix Study Group. Mixed features in patients with a major depressive episode: the BRIDGE-II-MIX study. J Clin Psychiatry. 2015;76:e351-e358.
2015;76:e351-e358.
4. Malhi GS, Fritz K, Allwang C, et al. Are manic symptoms that ‘dip’ into depression the essence of mixed features. J Affect Disord. 2016;192:104-108.
5. Leibenluft E. Categories and dimensions, brain and behavior: the yins and yangs of psychopathology. JAMA Psychiatry. 2014;71:15-17.
6. Phelps J. A Spectrum Approach to Mood Disorders: Not Fully Bipolar But Not Unipolar – Practical Management. New York: W.W. Norton & Company; 2016.
7. Miller S, Suppes T, Mintz J, et al. Mixed depression in bipolar disorder: prevalence rate and clinical correlates during naturalistic follow-up in the Stanley Bipolar Network. Am J Psychiatry. 2016;173:1015-1023.
8. Saito-Tanji Y, Tsujimoto E, Taketani R, et al. Effectiveness of simple individual psychoeducation for bipolar II disorder. Case Rep Psychiatry. 2016;2016:6062801.
9. Phelps J, Manipod V. Treating anxiety by discontinuing antidepressants: a case series. Med Hypotheses. 2012;79:338-341.
Med Hypotheses. 2012;79:338-341.
Symptoms, Treatments, and Tips for Managing
Hypomania — periods of intense energetic, happy, or irritated moods — is a part of life for many people with bipolar disorder.
Hypomanic episodes are a type of mood episode in bipolar disorder. Depending on the type of bipolar disorder you have, mood episodes might include highs (mania or hypomania) and/or lows (depression).
Hypomania is a milder form of mania. Although hypomania has a less severe impact than mania, it can still be disruptive and come with its own set of challenges.
While mood episodes can significantly impact your life, the right treatments and coping methods can reduce their impact and improve your overall well-being.
An episode of hypomania is a period of at least 4 days in a row when you have lots of extra energy, and you may feel very happy — or very irritable — for most of the day.
Sometimes, you might enjoy the feelings that come with hypomania. At other times, you might feel like they’re uncomfortable or distressing.
At other times, you might feel like they’re uncomfortable or distressing.
Either way, you’ll typically be able to carry on with your usual daily activities. But, you might also end up making decisions or doing things you wouldn’t normally, and that might have harmful consequences.
A diagnosis of bipolar II disorder requires that you have at least one hypomanic episode, before or after a major depressive episode.
Some people with bipolar I disorder also have hypomania. Hypomania or similar symptoms might occur in seasonal affective disorder or schizoaffective disorder, as well.
During a hypomanic episode, you might feel happy, euphoric, excited, agitated, overly energized, or easily distracted.
These are significant changes to your typical mood and behavior, so people who know you may notice the difference in you.
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), an episode of hypomania involves at least 3 of the following behavior changes:
- elevated self-esteem, high self-confidence, or feelings of grandiosity
- less need for sleep, such as feeling rested after only 3 hours of sleep
- feeling more talkative than usual or feeling a pressure to keep talking
- racing thoughts or quickly-changing ideas
- feeling easily distracted
- doing many activities at once, such as work tasks, organizing social events, or seemingly purposeless movements
- engaging in activities that may lead to harmful consequences, such as excessive spending, dangerous driving, or risky financial investments
By definition, the symptoms of hypomania aren’t severe enough to significantly affect your daily life or require hospitalization.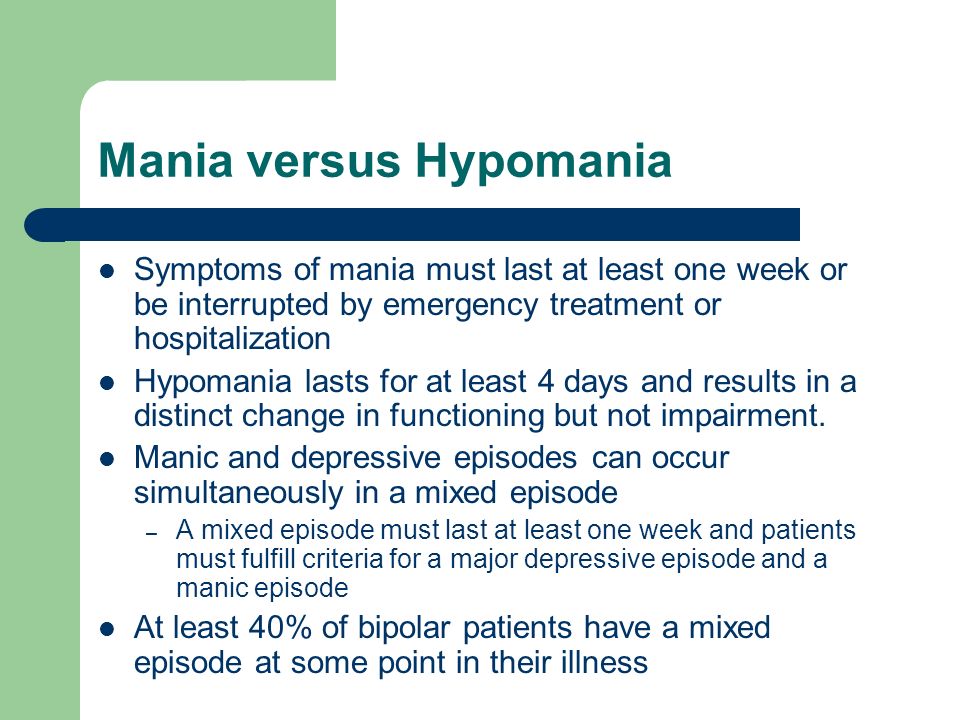 If symptoms are severe, it’s more likely that it’s mania.
If symptoms are severe, it’s more likely that it’s mania.
It is possible to have symptoms of hypomania from taking certain drugs, such as cocaine, or from psychiatric medications, like when starting a new course of antidepressants.
But your doctor likely won’t diagnose hypomania unless the symptoms continue beyond the effects of the drug being in your system.
To diagnose mania or hypomania, your doctor will also rule out other medical conditions that could cause similar symptoms — like hyperthyroidism or diabetes.
And finally, if you have repeated periods of hypomania and depression symptoms — but not enough to reach the criteria for a full episode, your doctor may diagnose cyclothymic disorder.
The symptoms of hypomania and mania are the same. The differences lie in how severe they are and the duration.
In hypomania, your symptoms aren’t severe enough to significantly disrupt your social or work life. They’re also not severe enough that you need hospital care.
There are also no features of psychosis in a hypomanic episode. For instance, you wouldn’t experience hallucinations or delusions, which can be present in a manic episode.
For diagnosing the two episodes, hypomania must last for at least 4 days in a row, while mania must occur for at least 1 week or any duration if hospitalization is required.
Just one episode of mania is enough for diagnosing bipolar I — even if you haven’t experienced an episode of depression.
And while the impacts of hypomania are less severe than those of mania, the DSM-5 states that bipolar II isn’t considered a “milder version” of bipolar I.
This is because the intense mood changes that come with untreated bipolar II usually lead to serious issues in social and work life, and episodes of depression may be longer and more severe.
Treatments for bipolar disorder aim to help you maintain stable moods and keep your symptoms managed. This usually involves a combo of medication and therapy.
Psychotherapy, aka talk therapy, can help you identify and change your troubling emotions, thoughts, and behaviors. Some therapy options for bipolar disorder can include:
- interpersonal and social rhythm therapy (IPSRT)
- psychoeducation
- cognitive behavioral therapy (CBT)
- family focused therapy
- dialectical behavioral therapy (DBT)
Medications for bipolar disorder often include:
- mood stabilizers
- atypical antipsychotics
- antidepressants to help with symptoms of depression
- medications to help with sleep or anxiety
According to the National Institute of Mental Health, regular exercise can help reduce depression and anxiety symptoms, while promoting better sleep. Being able to get quality sleep can significantly boost your mental health.
Need more info? Here’s a list of treatments for bipolar disorder.
Every person’s experience will be different, so of course your coping methods will be different, too.
But with some trial and error, you can find the best ways to cope with episodes of hypomania (and any other symptoms you have).
An important first step is to work out your personal triggers that you’re having or about to have a hypomanic episode. Knowing your triggers can help you feel empowered and more in control.
Tracking your moods — such as through apps or journals — can help you keep track of and notice changes to your moods. You can also check out the Depression and Bipolar Support Alliance (DBSA)’s free wellness tracker that you can print out and stick on your wall or keep in a folder.
You may also find it helpful to ask a loved one or two to let you know when they notice some signs, because you might not always be aware that it’s happening.
Here are some tips for preventing episodes of mania and hypomania:
- When you notice your triggers, reach out. Accepting help from others takes practice, but if you think you’re about to experience a mood episode, it can really help to reach out to your treatment team, along with family and friends.
 Noticing your symptoms early and getting help can prevent an episode from worsening.
Noticing your symptoms early and getting help can prevent an episode from worsening. - Avoid substance use. Alcohol and drug use can interfere with medications and your moods.
- Be patient — with yourself and your treatment. Learning the best ways to cope and finding the right meds for you can take time. Be patient and gentle with yourself.
- Take it one step at a time. Small steps can help things feel more manageable. Think: Setting up a sleep routine, talking with a friend for support, or reaching out to a doctor or therapist.
- Join a support group. Not everyone you know will understand your symptoms or condition, and while you can try to explain it, joining a support group of like-minded people can be a breath of healing air.
- Relieve your stress. Try using stress management techniques to relieve stress, which can exacerbate mood symptoms. Try a new exercise or a daily walk, meditation, or deep breathing.
- Set up a crisis plan. By putting together an emergency action plan, you can get the help you need — fast. Put together a list of resources and people you can call in a moment of crisis.
- Aim for better sleep. Sleep is often found lacking in people with bipolar disorder, and less sleep can mean more stress. So aim for good sleep hygiene. Sleep at the same time every night and maintain good sleep habits like avoiding screens an hour before bed.
Even if you feel good during a hypomanic episode, it’s important to stick with your treatment plan. In the long term, treatments help stabilize your mood and ultimately reduce the impact of depressive episodes, too.
For more support with managing bipolar disorder, check out the DBSA and International Bipolar Foundation.
Bipolar Disorder | Symptoms, complications, diagnosis and treatment
Bipolar disorder, formerly called manic depression, is a mental health condition that causes extreme mood swings that include emotional highs (mania or hypomania) and lows (depression). Episodes of mood swings may occur infrequently or several times a year.
Episodes of mood swings may occur infrequently or several times a year.
When you become depressed, you may feel sad or hopeless and lose interest or pleasure in most activities. When the mood shifts to mania or hypomania (less extreme than mania), you may feel euphoric, full of energy or unusually irritable. These mood swings can affect sleep, energy, alertness, judgment, behavior, and the ability to think clearly.
Although bipolar disorder is a lifelong condition, you can manage your mood swings and other symptoms by following a treatment plan. In most cases, bipolar disorder is treated with medication and psychological counseling (psychotherapy).
Symptoms
There are several types of bipolar and related disorders. These may include mania, hypomania, and depression. The symptoms can lead to unpredictable changes in mood and behavior, leading to significant stress and difficulty in life.
- Bipolar disorder I.
 You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis).
You have had at least one manic episode, which may be preceded or accompanied by hypomanic or major depressive episodes. In some cases, mania can cause a break with reality (psychosis). - Bipolar disorder II. You have had at least one major depressive episode and at least one hypomanic episode, but never had a manic episode.
- Cyclothymic disorder. You have had at least two years - or one year in children and adolescents - many periods of hypomanic symptoms and periods of depressive symptoms (though less severe than major depression).
- Other types. These include, for example, bipolar and related disorders caused by certain drugs or alcohol, or due to health conditions such as Cushing's disease, multiple sclerosis, or stroke.
Bipolar II is not a milder form of Bipolar I but is a separate diagnosis. Although bipolar I manic episodes can be severe and dangerous, people with bipolar II can be depressed for longer periods of time, which can cause significant impairment.
Although bipolar disorder can occur at any age, it is usually diagnosed in adolescence or early twenties. Symptoms can vary from person to person, and symptoms can change over time.
Mania and hypomania
Mania and hypomania are two different types of episodes, but they share the same symptoms. Mania is more pronounced than hypomania and causes more noticeable problems at work, school, and social activities, as well as relationship difficulties. Mania can also cause a break with reality (psychosis) and require hospitalization.
Both a manic episode and a hypomanic episode include three or more of these symptoms:
- Abnormally optimistic or nervous
- Increased activity, energy or excitement
- Exaggerated sense of well-being and self-confidence (euphoria)
- Reduced need for sleep
- Unusual talkativeness
- Distractibility
- Poor decision-making - for example, in speculation, in sexual encounters or in irrational investments
Major depressive episode
Major depressive episode includes symptoms that are severe enough to cause noticeable difficulty in daily activities such as work, school, social activities, or relationships. Episode includes five or more of these symptoms:
Episode includes five or more of these symptoms:
- Depressed mood, such as feeling sad, empty, hopeless, or tearful (in children and adolescents, depressed mood may manifest as irritability)
- Marked loss of interest or feeling of displeasure in all (or nearly all) activities
- Significant weight loss with no diet, weight gain, or decreased or increased appetite (in children, failure to gain weight as expected may be a sign of depression)
- Either insomnia or sleeping too much
- Either anxiety or slow behavior
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Decreased ability to think or concentrate, or indecisiveness
- Thinking, planning or attempting suicide
Other features of bipolar disorder
Signs and symptoms of bipolar I and bipolar II disorder may include other signs such as anxiety disorder, melancholia, psychosis, or others. The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
The timing of symptoms may include diagnostic markers such as mixed or fast cycling. In addition, bipolar symptoms may occur during pregnancy or with the change of seasons.
When to see a doctor
Despite extreme moods, people with bipolar disorder often do not realize how much their emotional instability disrupts their lives and the lives of their loved ones and do not receive the necessary treatment.
And if you are like people with bipolar disorder, you can enjoy feelings of euphoria and be more productive. However, this euphoria is always accompanied by an emotional disaster that can leave you depressed and possibly in financial, legal, or other bad relationships.
If you have symptoms of depression or mania, see your doctor or mental health professional. Bipolar disorder does not improve on its own. Getting mental health treatment with a history of bipolar disorder can help control your symptoms.
Bipolar affective disorder (BAD), its signs, types and methods of treatment
Manifestations of various emotions, a change in a person's mood, manifestations of both sadness and joy are normal and depend on many factors - from temperament and character to ongoing events that influence from the outside. However, when these changes are excessive, often unexpected and for no apparent reason, emotions get out of control, or a person remains in a radically positive or negative mood for a long time, it is very likely that bipolar disorder can be diagnosed. This disease was first described at the end of 19century, the famous German psychiatrist Emil Kripelin, calling it manic-depressive psychosis. Many world famous personalities such as Vincent van Gogh, Isaac Newton, Ludwig van Beethoven, Abraham Lincoln suffered from this disease. The pronounced form of this disease, which in the international classification of diseases is called bipolar affective disorder (BAD), is detected in 3% of the world's population.
However, when these changes are excessive, often unexpected and for no apparent reason, emotions get out of control, or a person remains in a radically positive or negative mood for a long time, it is very likely that bipolar disorder can be diagnosed. This disease was first described at the end of 19century, the famous German psychiatrist Emil Kripelin, calling it manic-depressive psychosis. Many world famous personalities such as Vincent van Gogh, Isaac Newton, Ludwig van Beethoven, Abraham Lincoln suffered from this disease. The pronounced form of this disease, which in the international classification of diseases is called bipolar affective disorder (BAD), is detected in 3% of the world's population.
CONTENT OF THE ARTICLE
- 1. Bipolar Personality Disorder - Overview
- 2. Symptoms and signs
- 3. Types of Bipolar Disorder
- 4. Phases of Bipolar Disorder
- 5. Bipolar disorder in women
- 6. Treatment of Bipolar Personality Disorder
It is not uncommon for women to be treated with a combination of drug therapy and cognitive behavioral or interpersonal therapy with a psychotherapist.
Bipolar personality disorder - general information
According to statistics, bipolar disorder affects people from 14 to 44 years old. Unlike adults, children and adolescents experience more frequent mood swings from mania to depression, sometimes several times a day. 90% of young people make their debut precisely from the phase of depression or melancholy. Another feature of bipolar disorder is that, due to the low level of diagnosis, the patient can live with this disease for 5-10 years without knowing the cause of the painful symptoms.
Most often, bipolar disorder is diagnosed in people whose immediate family members have had a similar problem. The causes of this disease are unknown, but stress, overstrain, and various diseases can provoke the manifestation of its symptoms. However, having fenced off a person from the influence of these factors, it is impossible to get rid of the problem, you need to seek help from a psychotherapist.
Bipolar disorder is a disease that cannot be completely cured.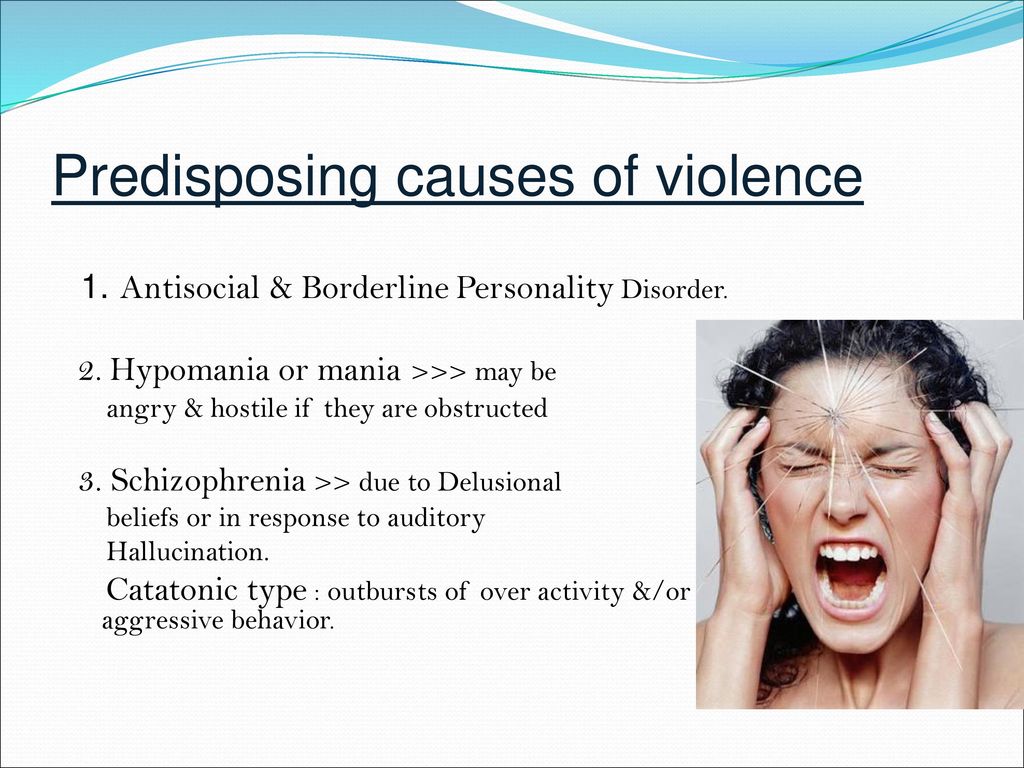 But with properly selected medication and psychotherapy, the quality of life is significantly improved and the periods between phases are lengthened. The person remains socialized and able to work.
But with properly selected medication and psychotherapy, the quality of life is significantly improved and the periods between phases are lengthened. The person remains socialized and able to work.
Symptoms and signs
From the name it is clear that we are talking about two different poles of affective manifestations, that is, mood manifestations. One of these conditions is depression. Depression in bipolar disorder is pronounced, with vivid symptoms. It can last up to a year and is manifested not only by low mood, lack of ability to enjoy and interest in ongoing events, but also by psychosis, when ideas of self-accusation arise, the patient feels inferior, unnecessary, poisoning the life of others. There are also nihilistic thoughts about suffering from some kind of severe illness, despite medical evidence to the contrary. There may be delusional thoughts, as well as suicidal thoughts and even attempts.
The other pole of bipolar disorder is a hypomanic state or hypomania, the characteristic features of which are an increased euphoric emotional background, the patient is constantly on the move, hyperactive, and is distinguished by very fast, associative speech.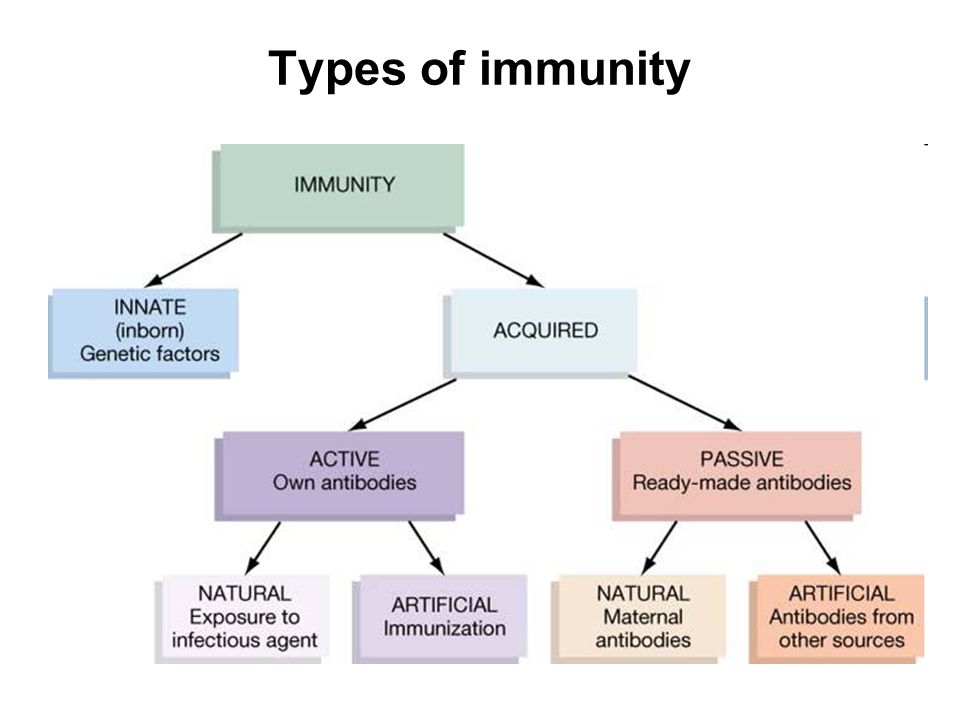 The patient is constantly cheerful, often hypersexual, almost always awake or sleeping 2-3 hours a day.
The patient is constantly cheerful, often hypersexual, almost always awake or sleeping 2-3 hours a day.
Hypomania is often followed by a manic bipolar state with psychotic manifestations. The patient develops convictions in his own greatness, he believes that he is capable of anything, feels that he has a special calling in this world or that he is a descendant of great people. In extended manic episodes of mania with psychotic manifestations, anger, irritability, and direct aggression often occur. This condition leads the patient into extremely unpleasant and sometimes dangerous situations.
In addition to the typical symptoms of the disease, there are a large number of comorbid mental disorders. Comorbid mental disorders are those that accompany the underlying disease. The most common disorder of this kind is anxiety, which is manifested, among other things, by nonspecific autonomic symptoms, including sweating, palpitations, tremors of the limbs, various disorders of the gastrointestinal tract, dizziness, headaches, suffocation, and many others.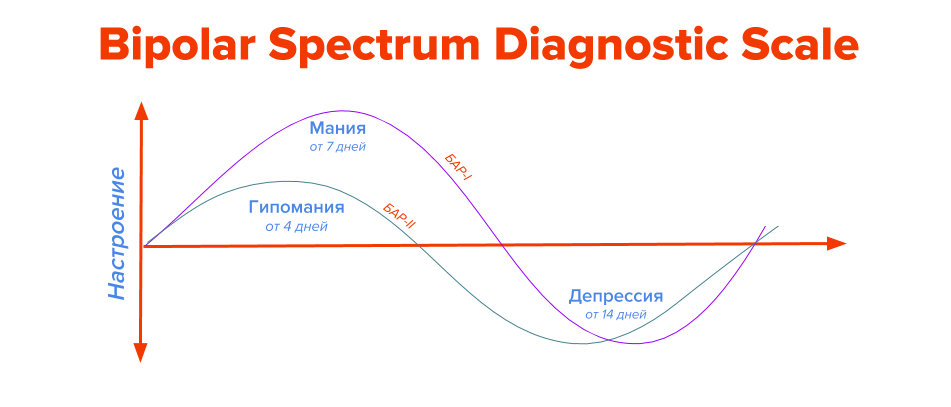 In the case when these symptoms occur suddenly, mainly in public places, they are called panic attacks.
In the case when these symptoms occur suddenly, mainly in public places, they are called panic attacks.
Types of bipolar disorder
Bipolar disorder can be of Ι and ΙΙ types.
Bipolar I disorder is a condition in which the patient has persistent manias, i.e. overexcitation, enthusiastic inappropriate behavior, manic psychosis, as well as severe depressions. Symptoms of this type are more severe, so hospitalization is indicated in most cases.
Bipolar I disorder is characterized by short periods of hypomania followed by periods of deep depression. Hypomania is a pre-manic state with less active manifestations. Hypomania lasts a very short period of time - from several days to several hours, so sometimes patients do not even notice them and do not inform the doctor about it. Only careful, painstaking work with the patient makes it possible to identify hypomania, make the correct diagnosis and prescribe treatment.
Phases of bipolar disorder
There are several phases of bipolar personality disorder:
- Depressive (unipolar depression).
 People experience a depressed mood, despair and despondency, complain of a lack of energy and mental concentration, they can either eat too much or too little and sleep.
People experience a depressed mood, despair and despondency, complain of a lack of energy and mental concentration, they can either eat too much or too little and sleep.
Depersonalization and derealization may occur at the peak of bipolar depressive disorder. The boundaries of their own "I" and the world around them become blurred, patients experience difficulties in perceiving what is happening. Familiar places seem new, the colors of the surrounding world change, the patient constantly experiences a feeling of "déjà vu". Sounds become muffled, even if someone is talking very close, it seems to the patient that the voice is coming from afar.
- Manic (hypomanic). In this state, patients are full of energy, overly happy or optimistic, euphoric, and have extremely high self-esteem. At first glance, these are positive signs, but when a person experiences large-scale manic episodes, these symptoms and such an emotional state can reach dangerous extremes.
 A patient in this phase may indiscriminately spend huge amounts of money or behave carelessly, not realizing the full danger. In conversation, people may choke on words, speak at a high speed, or jump from one thought to another. These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
A patient in this phase may indiscriminately spend huge amounts of money or behave carelessly, not realizing the full danger. In conversation, people may choke on words, speak at a high speed, or jump from one thought to another. These episodes may also be accompanied by delusions of grandeur or the adoption of serious decisions without thinking about the further consequences.
In the development of the manic phase, the following stages of development can be distinguished:
- Hypomania - increased excitement, emotional upsurge.
- Mania - all signs are more pronounced, aggression, irritability, irascibility and rage are possible.
- Phase peak. The patient constantly experiences nervous excitement, he cannot relax. All his emotions are "heated" to the limit, coordination of movements is disturbed, thoughts are illogical and abrupt, in speech he constantly jumps from one sentence to another.
- Relief of symptoms. The patient gradually calms down.
 Movement disorders are on the decline. The speed of thinking and increased emotional mood remain unchanged.
Movement disorders are on the decline. The speed of thinking and increased emotional mood remain unchanged. - Return to normal.
- Mixed. Sometimes people have complaints that are characteristic of both depression and mania at the same time. They may also experience frequent phasing—4 or more episodes in one year.
In the intervals between depressive and manic phases in bipolar disorder, there is a light period during which the general background of mood becomes relatively stable, the person continues to adequately respond to certain events, the emotional sphere is under his control. This is the main criterion for remission of bipolar disease.
Bipolar disorder in women
According to statistics, bipolar Ι disorder occurs with the same frequency in men and women, and type ΙΙ disease is more often diagnosed in women. It is also known that the female course of the disease is characterized by rapid cycles and mixed episodes.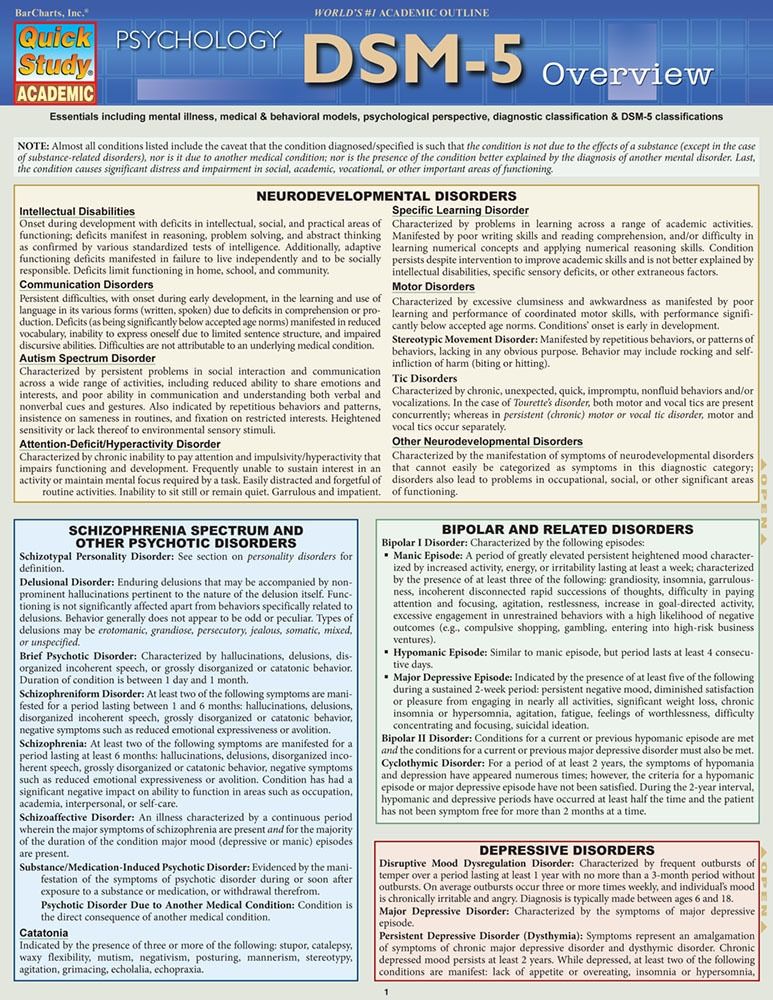 Comorbidities often include eating disorders, borderline personality disorder, alcohol or drug addiction, and psychotropic drug abuse. Women are more susceptible to such somatic diseases as migraine (intense headaches), thyroid pathologies, diabetes, and obesity.
Comorbidities often include eating disorders, borderline personality disorder, alcohol or drug addiction, and psychotropic drug abuse. Women are more susceptible to such somatic diseases as migraine (intense headaches), thyroid pathologies, diabetes, and obesity.
For women, a special technique is being developed to alleviate this disorder, since from adolescence to menopause there are specific changes in hormonal levels that must be taken into account. In addition, psychotropic substances, which are supposed to stabilize the condition, can adversely affect the intrauterine development of the fetus if the woman is in position. It is noted that in the first trimester of pregnancy this disorder is milder, but after childbirth they often have to deal with postpartum depression. Thus, at each stage of the development of the female body, a competent doctor must review and adjust the treatment regimen. Often in the treatment of women, a complex method is used that combines drug therapy and cognitive-behavioral or interpersonal therapy with a psychotherapist. This approach gives the fastest results.
This approach gives the fastest results.
Treatment for bipolar disorder
Attempts to get rid of bipolar disorder on your own do not bring the desired result and, ultimately, lead to an aggravation of the situation, including the development of drug or alcohol dependence. In the diagnosis of the disease, keeping a mood diary can help, where the patient records all his thoughts, emotions, feelings, changes in mood. Such records will help the doctor to assess the mental state in detail and make the correct diagnosis. If you suspect bipolar disorder, you should consult a doctor, and the sooner a person realizes that he has a disease and comes to the clinic for help, the sooner professional help will be provided to him and painful symptoms will be replaced by a stable condition. It is impossible to get rid of the disease on your own, since a person cannot fully adequately assess not only his actions, but also the alternation of the phases of the disease.
Bipolar disorder is one of the few mental disorders in which medication is indicated in 100% of cases, and psychotherapy is an auxiliary tool. This disease is incurable, but its diagnosis and treatment is extremely important. Treatment can reduce the number of episodes, their severity and intensity, as well as prevent negative life events, help prevent relationship breakups, job loss, and even suicidal attempts. Thus, the quality of life of a patient with bipolar disorder who is undergoing treatment will be several times higher than that of a person who neglects treatment. If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
This disease is incurable, but its diagnosis and treatment is extremely important. Treatment can reduce the number of episodes, their severity and intensity, as well as prevent negative life events, help prevent relationship breakups, job loss, and even suicidal attempts. Thus, the quality of life of a patient with bipolar disorder who is undergoing treatment will be several times higher than that of a person who neglects treatment. If the patient loses touch with reality and harms himself and others, he is subject to hospitalization, outpatient treatment in this case is not permissible.
If you have a disease, it is recommended to exclude coffee, strong tea, alcoholic and energy drinks from your diet in order not to provoke an overexcited state. If possible, you should stop smoking and in no case should you take even soft drugs. It is also very important to establish a sleep pattern, sleep at least 8 hours a day and try to go to bed at about the same time. You should learn to recognize mood swings and notice the early manifestations of new episodes.