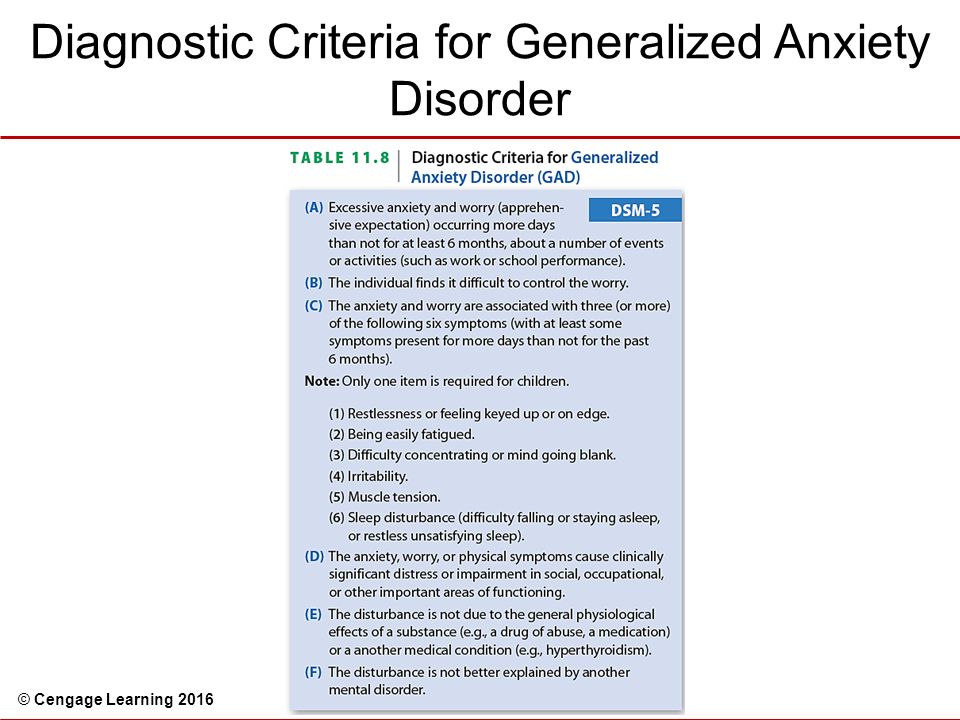
Dsm 5 anxiety diagnostic criteria
Updates to Anxiety Disorders and Phobias in the DSM-5
Anxiety disorders are common mental health disorders — the criteria for anxiety disorders have changed from the DSM-4 to the DSM-5.
Anxiety disorders are one of the most common psychiatric disorders worldwide. Phobias are categorized as anxiety disorders, with specific phobia (fear of something that poses little or no actual danger) being the most common anxiety disorder.
If you experience anxiety, it can be overwhelming and exhausting. Anxiety disorders often have high comorbidity with other mental health disorders. There are various treatments for anxiety disorders, and the treatment may look different based on the type of anxiety disorder.
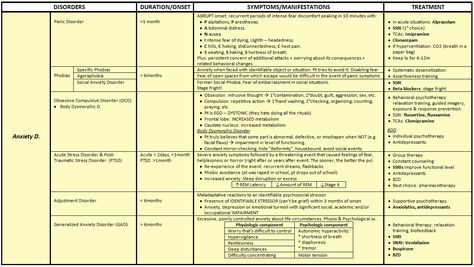
In the anxiety disorders section of the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), there are 11 anxiety disorders and a panic attack specifier that can be used for other mental health disorders. The previous version of the DSM, the DSM-4, outlined 12 categories of anxiety disorders.
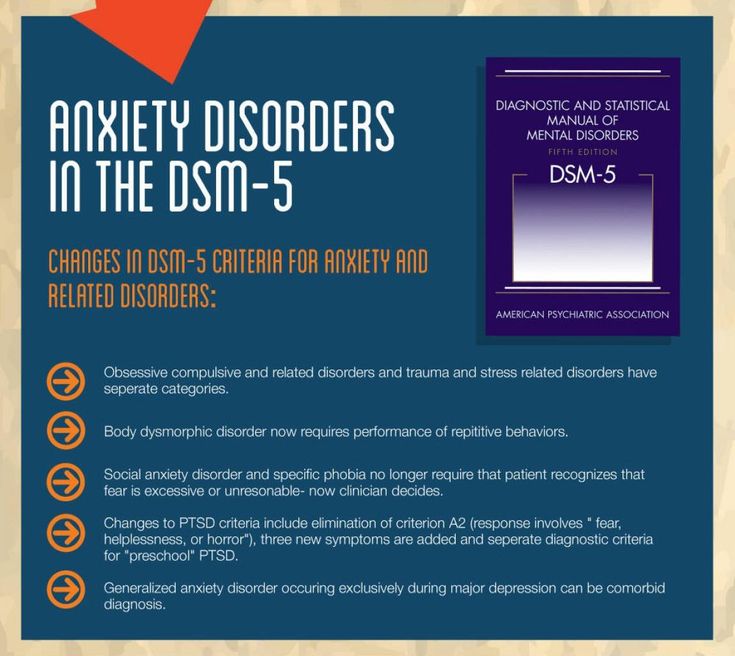
There were several changes to the DSM-5 classification of anxiety disorders. Panic disorder and agoraphobia (fear of places or situations that might cause panic) were previously linked in the DSM-4 and are now separate disorders with differing criteria.
The DSM-5 also added separation anxiety and selective mutism (inability to speak in particular social situations) in the anxiety disorders section.
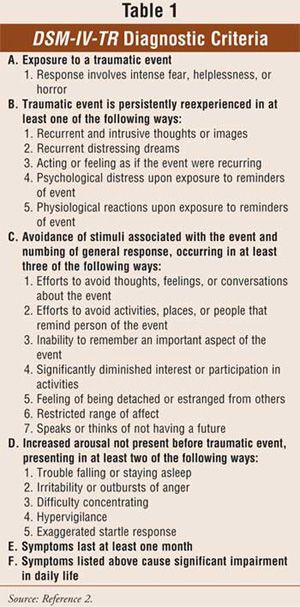
The American Psychiatric Association (APA) also removed obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD) from the anxiety disorders section in the DSM-5. OCD in the DSM-5 now falls under obsessive-compulsive and related disorders, and PTSD falls under trauma and stressor-related disorders.
Of the 11 anxiety disorders in the DSM-5, approximately 7.3% of individuals globally live with one of these disorders.
Separation anxiety disorder
Separation anxiety disorder is characterized by a persistent fear of being away from home or without an attachment figure. This usually causes the person significant distress, and they may have difficulty going to school or work due to the separation.
This usually causes the person significant distress, and they may have difficulty going to school or work due to the separation.
People with separation anxiety disorder may also be prone to nightmares or have excessive anxiety about unwelcome events happening to their attachment figure.
Separation anxiety was a new addition to the DSM-5 categorization of anxiety disorders. It was previously listed under conditions that occur in childhood. The change was due to 2016 research that supported a high prevalence of separation anxiety in adults.
Selective mutism
Selective mutism is generally seen in children. The disorder refers to the inability to speak in specific social situations. Selective mutism can last into adulthood if a child does not receive treatment. Selective mutism is different than a communication disorder.
Selective mutism typically first appears at a crucial moment in a child’s life, such as beginning preschool. For a diagnosis of selective mutism, it must be present for at least 1 month.
Selective mutism was an addition to the DSM-5. It was previously listed under disorders that occur in childhood.
Specific phobia
Specific phobia is when a person experiences extreme anxiety when they anticipate exposure or are exposed to a feared stimulus. There are generally five categories of specific phobias:
- animal type (spiders, snakes, dogs)
- natural environment type (tornadoes, heights, water, fire)
- blood injection type (Needles, medical procedures)
- situational type (flying on an airplane, enclosed spaces)
- other type (phobias that do not fit into the previous four categories)
Social anxiety disorder (social phobia)
Social anxiety disorder is characterized by extreme fear of social situations. If you experience social anxiety, you may feel an extreme fear of criticism or scrutiny by others in social interactions. This intense fear often leads to avoidance of the social situation and can cause impairments in school, work, or relationships.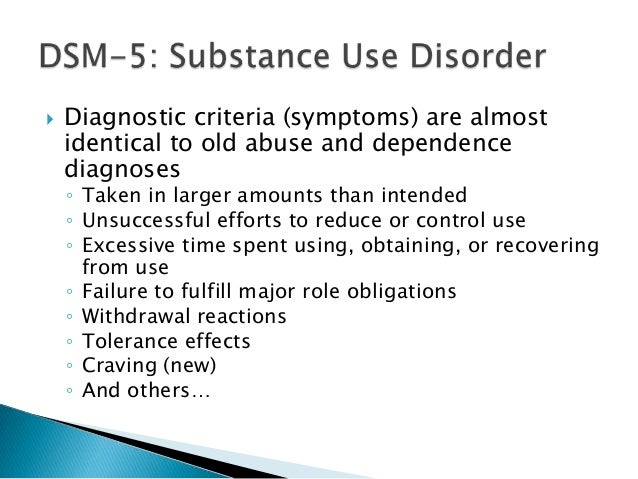
Panic disorder
Panic disorder is a common mental health condition in which a person experiences recurrent panic attacks. If you have been diagnosed with panic disorder, you may experience an extreme surge of fear and discomfort due to a perceived loss of control. There is often not a specific trigger to the panic attack.
Physical symptoms that may signal the presence of a panic attack include:
- dizziness
- nausea
- racing heart
- shaking
- trembling
- sweating
- chills
- unsteadiness
- shortness of breath
- the sensation of choking
- chest pain
- abdominal pain
- fear of losing control
- fear of dying
The APA changed panic disorder in the DSM-5 as it was previously linked with agoraphobia and is now a separate diagnosis.
Generalized anxiety disorder (GAD)
Generalized anxiety disorder is diagnosed when an individual experiences persistent worry about everyday challenges out of proportion to the perceived threat.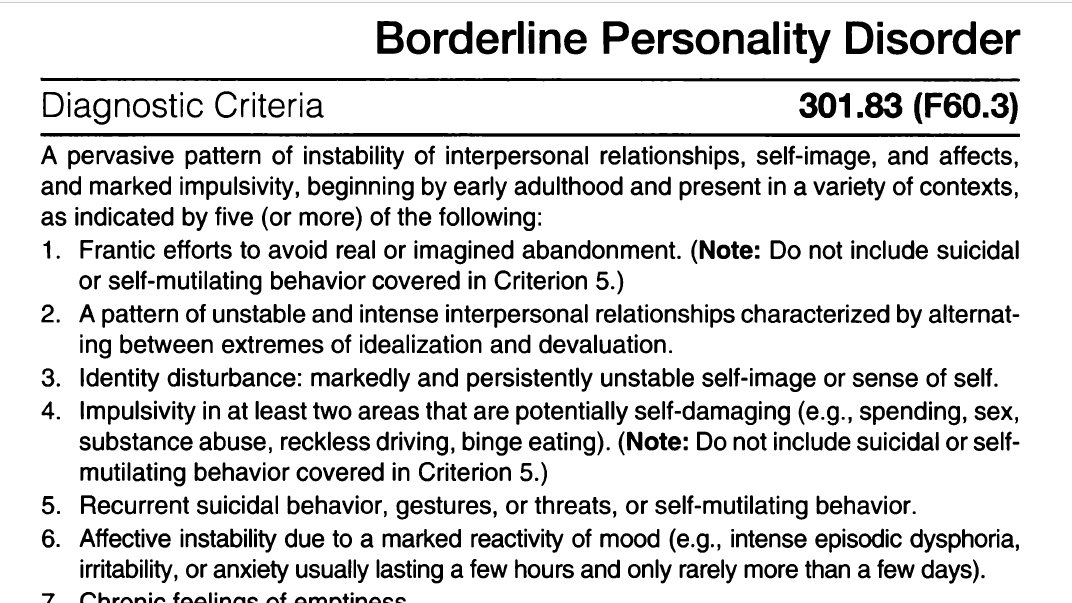 People with GAD usually experience excessive fear that can last months to years.
People with GAD usually experience excessive fear that can last months to years.
GAD can cause significant problems with concentration. If you have GAD, you may experience trouble controlling your worrying and be aware that you are worrying too much.
Agoraphobia
Agoraphobia is a fear of situations or places that may cause feelings of panic, entrapment, helplessness, or embarrassment.
If you have agoraphobia, you may have difficulty leaving your house. Fears of crowds, traveling, elevators, movie theatres, malls, etc., might cause significant challenges.
People with agoraphobia may also have recurrent panic attacks, and the thought of leaving the house may cause considerable anxiety to the point of avoidance.
Agoraphobia is an addition to the DSM-5 as it was previously linked with panic disorder. Agoraphobia now has separate criteria.
Substance/medication-induced anxiety disorder
Substance/medication-induced anxiety disorder is an anxiety disorder in which anxiety or panic occurs after using alcohol, drugs, or medication. This can occur during the intoxication or withdrawal phases of using a substance or medication.
This can occur during the intoxication or withdrawal phases of using a substance or medication.
To be diagnosed with a substance/medication-induced anxiety disorder, you cannot have experienced anxiety before you started taking the substance, even if that substance made your anxiety symptoms worse.
Anxiety disorder due to another medical condition
Anxiety disorder due to a medical condition occurs when a medical condition causes extreme fear, anxiety, or panic. If you have anxiety or worry about your medical condition, this is not considered an anxiety disorder.
This diagnosis is used only if anxiety and panic symptoms are present due to your medical condition.
An example of this would be if you began to experience panic attacks due to your diagnosed thyroid disease. This is also referred to as comorbid anxiety.
Other specified anxiety disorder
Other specified anxiety disorder may be diagnosed if you have most but not all of the criteria for an anxiety disorder. For example, anxiety often causes significant distress, but a few of the symptoms to meet the full standards are not met.
For example, anxiety often causes significant distress, but a few of the symptoms to meet the full standards are not met.
Unspecified anxiety disorder
Unspecified anxiety disorder is often diagnosed if you experience anxiety or panic but don’t meet the full criteria for the symptoms of another anxiety disorder. It is often used in hospitals or other settings when there may be a lack of information to make a complete diagnosis.
The APA publishes and updates the DSM on an irregular basis. The DSM has been revised seven times since its first publication in 1952. The DSM-5 update was a lengthy process that lasted nearly a decade and was based on research, a panel of experts, and conferences to review the strength and evidence of the proposed updates.
According to the APA, changes to the DSM-5 were based on the clinical knowledge of experts in the mental health field and advances in field research.
If you have an anxiety disorder, you may experience challenges with daily living.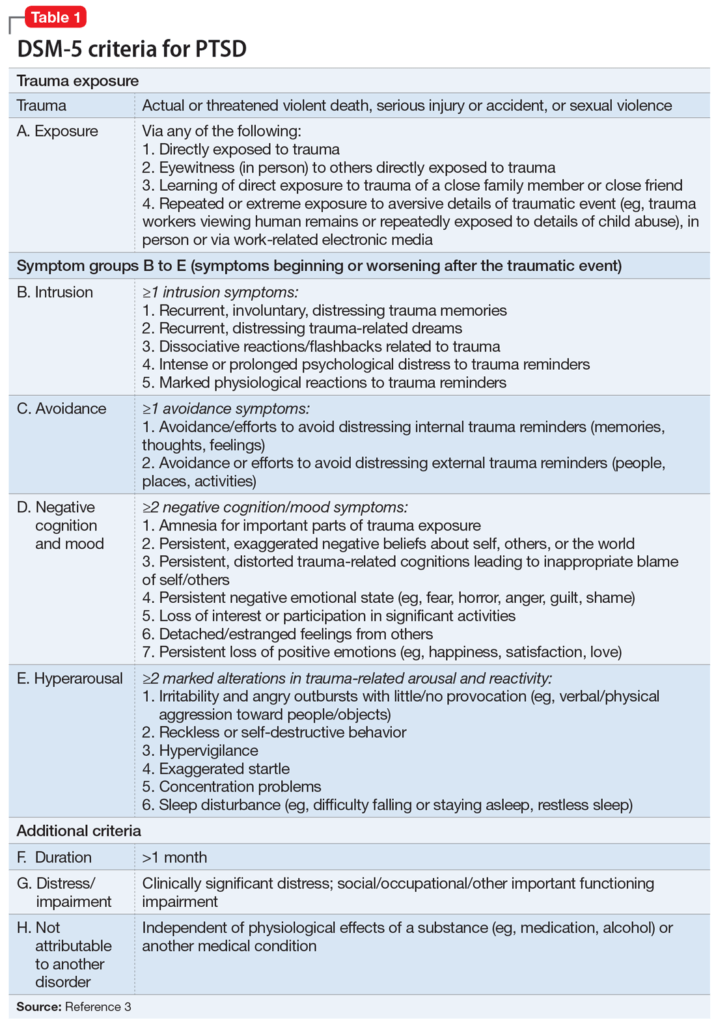 For example, work, school, and relationships may become challenging due to excessive worry or panic.
For example, work, school, and relationships may become challenging due to excessive worry or panic.
Anxiety disorders can be treated, often with psychotherapy and medication. If you have an anxiety disorder, help is available. The Anxiety and Depression Association of America also offers helpful resources and education for managing anxiety.
Anxiety disorders are common mental health disorders, but you don’t have to face them alone.
Social anxiety disorder (social phobia) - Diagnosis and treatment
Diagnosis
Your health care provider will want to determine whether other conditions may be causing your anxiety or if you have social anxiety disorder along with another physical or mental health disorder.
Your health care provider may determine a diagnosis based on:
- Physical exam to help assess whether any medical condition or medication may trigger symptoms of anxiety
- Discussion of your symptoms, how often they occur and in what situations
- Review of a list of situations to see if they make you anxious
- Self-report questionnaires about symptoms of social anxiety
- Criteria listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association
DSM-5 criteria for social anxiety disorder include:
- Persistent, intense fear or anxiety about specific social situations because you believe you may be judged negatively, embarrassed or humiliated
- Avoidance of anxiety-producing social situations or enduring them with intense fear or anxiety
- Excessive anxiety that's out of proportion to the situation
- Anxiety or distress that interferes with your daily living
- Fear or anxiety that is not better explained by a medical condition, medication or substance abuse
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your social anxiety disorder (social phobia)-related health concerns Start Here
Treatment
Treatment depends on how much social anxiety disorder affects your ability to function in daily life. The most common treatment for social anxiety disorder includes psychotherapy (also called psychological counseling or talk therapy) or medications or both.
The most common treatment for social anxiety disorder includes psychotherapy (also called psychological counseling or talk therapy) or medications or both.
Psychotherapy
Psychotherapy improves symptoms in most people with social anxiety disorder. In therapy, you learn how to recognize and change negative thoughts about yourself and develop skills to help you gain confidence in social situations.
Cognitive behavioral therapy (CBT) is the most effective type of psychotherapy for anxiety, and it can be equally effective when conducted individually or in groups.
In exposure-based CBT, you gradually work up to facing the situations you fear most. This can improve your coping skills and help you develop the confidence to deal with anxiety-inducing situations. You may also participate in skills training or role-playing to practice your social skills and gain comfort and confidence relating to others. Practicing exposures to social situations is particularly helpful to challenge your worries.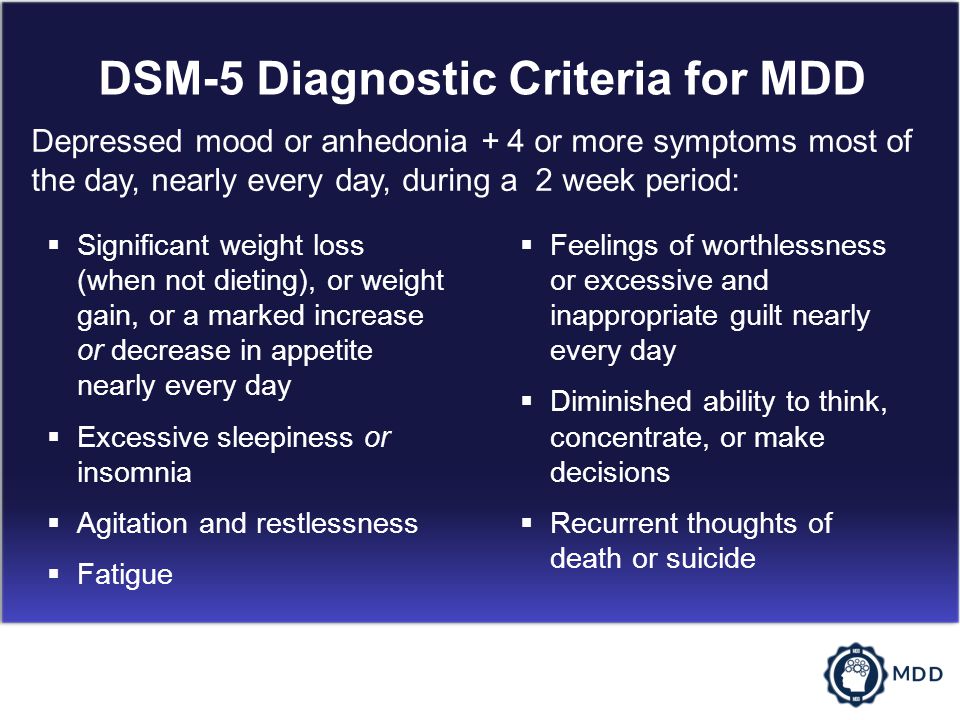
First choices in medications
Though several types of medications are available, selective serotonin reuptake inhibitors (SSRIs) are often the first type of drug tried for persistent symptoms of social anxiety. Your health care provider may prescribe paroxetine (Paxil) or sertraline (Zoloft).
The serotonin and norepinephrine reuptake inhibitor (SNRI) venlafaxine (Effexor XR) also may be an option for social anxiety disorder.
To reduce the risk of side effects, your health care provider may start you at a low dose of medication and gradually increase your prescription to a full dose. It may take several weeks to several months of treatment for your symptoms to noticeably improve.
Other medications
Your health care provider may also prescribe other medications for symptoms of social anxiety, such as:
- Other antidepressants. You may have to try several different antidepressants to find the one that's most effective for you with the fewest side effects.
- Anti-anxiety medications. Benzodiazepines (ben-zoe-die-AZ-uh-peens) may reduce your level of anxiety. Although they often work quickly, they can be habit-forming and sedating, so they're typically prescribed for only short-term use.
- Beta blockers. These medications work by blocking the stimulating effect of epinephrine (adrenaline). They may reduce heart rate, blood pressure, pounding of the heart, and shaking voice and limbs. Because of that, they may work best when used infrequently to control symptoms for a particular situation, such as giving a speech. They're not recommended for general treatment of social anxiety disorder.
Stick with it
Don't give up if treatment doesn't work quickly. You can continue to make strides in psychotherapy over several weeks or months. Learning new skills to help manage your anxiety takes time. And finding the right medication for your situation can take some trial and error.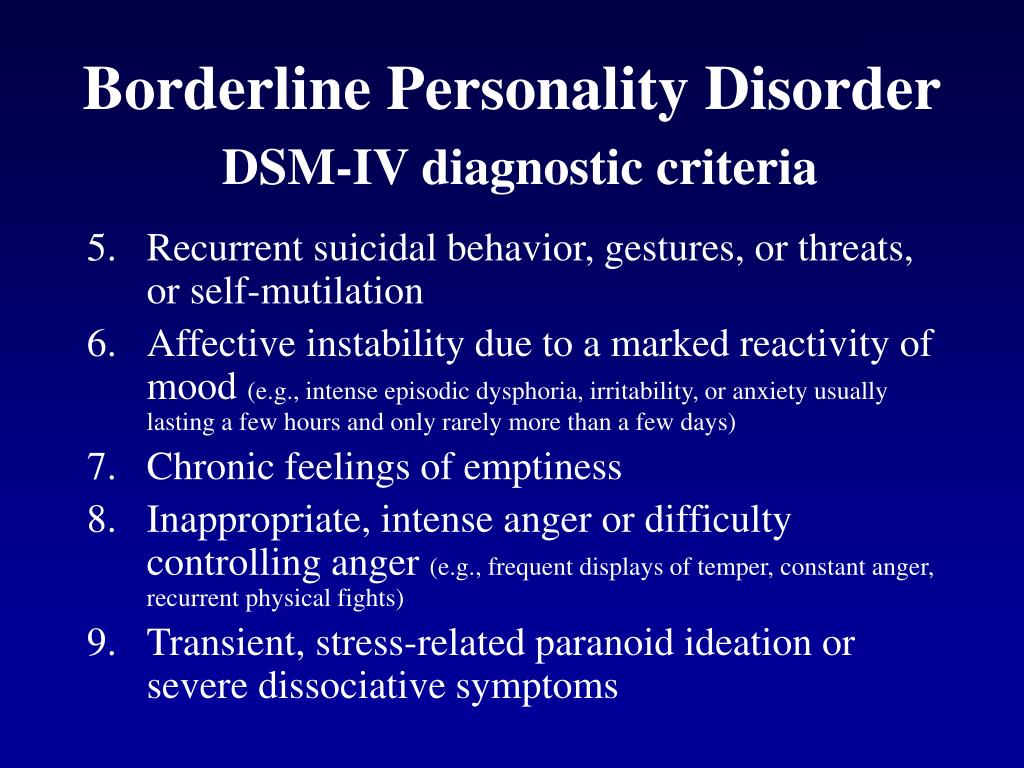
For some people, the symptoms of social anxiety disorder may fade over time, and medication can be discontinued. Others may need to take medication for years to prevent a relapse.
To make the most of treatment, keep your medical or therapy appointments, challenge yourself by setting goals to approach social situations that cause you anxiety, take medications as directed, and talk to your health care provider about any changes in your condition.
Alternative medicine
Several herbal remedies have been studied as treatments for anxiety, but results are mixed. Before taking any herbal remedies or supplements, talk with your health care team to make sure they're safe and won't interact with any medications you take.
More Information
- Social anxiety disorder (social phobia) care at Mayo Clinic
- Cognitive behavioral therapy
- Psychotherapy
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.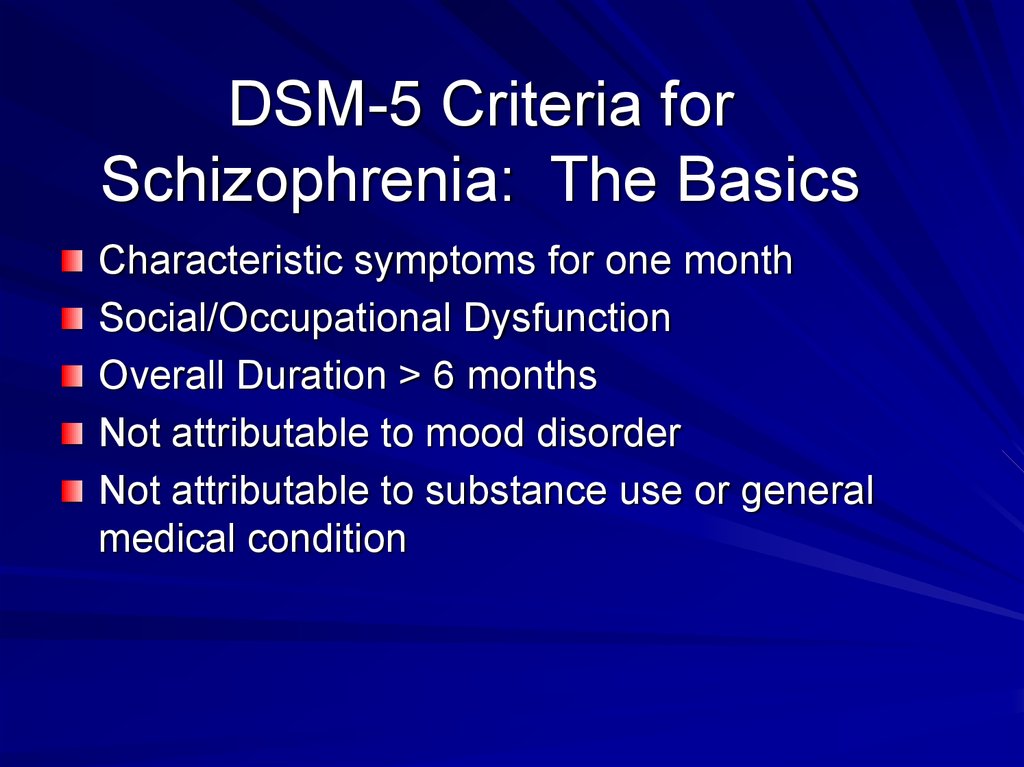 Click here for an email preview.
Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Lifestyle and home remedies
Although social anxiety disorder generally requires help from a medical expert or qualified psychotherapist, you can try some of these techniques to handle situations that are likely to trigger symptoms:
- Learn stress-reduction skills.
- Get physical exercise or be physically active on a regular basis.
- Get enough sleep.
- Eat a healthy, well-balanced diet.
- Avoid alcohol.
- Limit or avoid caffeine.
- Participate in social situations by reaching out to people with whom you feel comfortable.
Practice in small steps
First, consider your fears to identify what situations cause the most anxiety. Then gradually practice these activities until they cause you less anxiety. Begin with small steps by setting daily or weekly goals in situations that aren't overwhelming. The more you practice, the less anxious you'll feel.
Consider practicing these situations:
- Eat with a close relative, friend or acquaintance in a public setting.
- Purposefully make eye contact and return greetings from others, or be the first to say hello.
- Give someone a compliment.
- Ask a retail clerk to help you find an item.
- Get directions from a stranger.
- Show an interest in others — ask about their homes, children, grandchildren, hobbies or travels, for instance.
- Call a friend to make plans.
Prepare for social situations
At first, being social when you're feeling anxious is challenging. As difficult or painful as it may seem initially, don't avoid situations that trigger your symptoms. By regularly facing these kinds of situations, you'll continue to build and reinforce your coping skills.
These strategies can help you begin to face situations that make you nervous:
- Prepare for conversation, for example, by reading about current events to identify interesting stories you can talk about.
- Focus on personal qualities you like about yourself.
- Practice relaxation exercises.
- Learn stress management techniques.
- Set realistic social goals.
- Pay attention to how often the embarrassing situations you're afraid of actually take place.
 You may notice that the scenarios you fear usually don't come to pass.
You may notice that the scenarios you fear usually don't come to pass. - When embarrassing situations do happen, remind yourself that your feelings will pass and you can handle them until they do. Most people around you either don't notice or don't care as much as you think, or they're more forgiving than you assume.
Avoid using alcohol to calm your nerves. It may seem like it helps temporarily, but in the long term it can make you feel even more anxious.
Coping and support
These coping methods may help ease your anxiety:
- Routinely reach out to friends and family members.
- Join a local or reputable internet-based support group.
- Join a group that offers opportunities to improve communication and public speaking skills, such as Toastmasters International.
- Do pleasurable or relaxing activities, such as hobbies, when you feel anxious.
Over time, these coping methods can help control your symptoms and prevent a relapse. Remind yourself that you can get through anxious moments, that your anxiety is short-lived and that the negative consequences you worry about so much rarely come to pass.
Remind yourself that you can get through anxious moments, that your anxiety is short-lived and that the negative consequences you worry about so much rarely come to pass.
Preparing for your appointment
You may see your primary care provider, or your provider may refer you to a mental health professional. Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Situations you've been avoiding, especially those that are important to your functioning
- Any symptoms you've been experiencing, and for how long, including any symptoms that may seem unrelated to the reason for your appointment
- Key personal information, especially any significant events or changes in your life shortly before your symptoms appeared
- Medical information, including other physical or mental health conditions with which you've been diagnosed
- Any medications, vitamins, herbs or other supplements you're taking, including dosages
- Questions to ask your health care provider or a mental health professional
You may want to ask a trusted family member or friend to go with you to your appointment, if possible, to help you remember key information.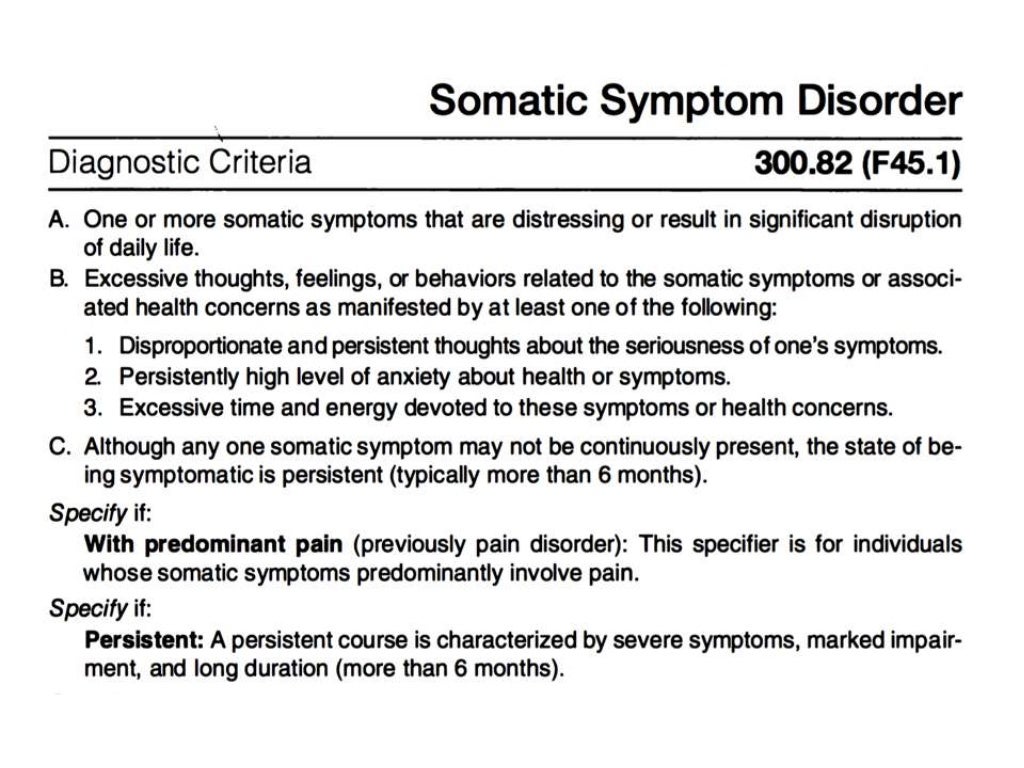
Some questions to ask your health care provider may include:
- What do you believe is causing my symptoms?
- Are there any other possible causes?
- How will you determine my diagnosis?
- Should I see a mental health specialist?
- Is my condition likely temporary or chronic?
- Are effective treatments available for this condition?
- With treatment, could I eventually be comfortable in the situations that make me so anxious now?
- Am I at increased risk of other mental health problems?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your health care provider
Your health care provider or a mental health professional will likely ask you a number of questions. Be ready to answer them to reserve time to go over any points you want to focus on.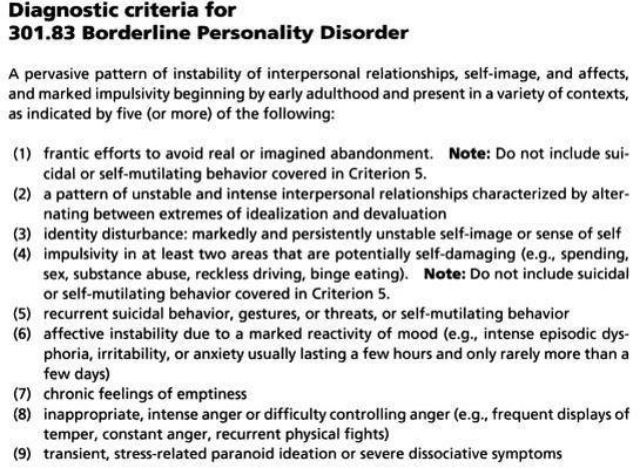 Your health care provider may ask:
Your health care provider may ask:
- Does fear of embarrassment cause you to avoid doing certain activities or speaking to people?
- Do you avoid activities in which you're the center of attention?
- Would you say that being embarrassed or looking stupid is among your worst fears?
- When did you first notice these symptoms?
- When are your symptoms most likely to occur?
- Does anything seem to make your symptoms better or worse?
- How are your symptoms affecting your life, including work and personal relationships?
- Do you ever have symptoms when you're not being observed by others?
- Have any of your close relatives had similar symptoms?
- Have you been diagnosed with any medical conditions?
- Have you been treated for mental health symptoms or mental illness in the past? If yes, what type of therapy was most beneficial?
- Have you ever thought about harming yourself or others?
- Do you drink alcohol or use recreational drugs? If so, how often?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Not Found (#404)
hide menu
Issues of the current year
-
1
-
1-2 (138)
1
Issue 1 content, 2023
-
Anxiety at the hour of war: encouragement of summer people for crisis conditions
-
Possibility of correction of dysfunction of the brain of a degenerative and vascular character
-
Geriatric syndromes in clinical practice
L.
 M.Yona, G. M. Khristoforova, O. G. Garkavenko
M.Yona, G. M. Khristoforova, O. G. Garkavenko -
Management of patients with dementia aggravated by behavioral and psychological symptoms
-
Depression and pain syndrome in patients with frail age and concomitant pathologies
-
Potential for pharmacotherapy in patients with dementia
M.V. Polyvoda
-
Multidisciplinary study in epileptology
-
Effectiveness of antidepressants in treatment of pain
-
Sleep well in a frail age: focus on Parkinson's disease
-
Possibility of correction of sleep disorders in the case of a frail age in the minds of stress
-
Prolonged grief reaction: nature, risk factors, diagnostics and cognitive-behavioral therapy
Paul Bulin
1-2 (138)
Other projects of the publishing house "Health of Ukraine"
Specialization medical portal
Child doctor
Medical aspects of women's health
Clinical Immunology, Allergology, Infectology
Rational pharmacotherapy
Borderline Personality Disorder signs and symptoms • Psychologist Yaroslav Isaikin
According to the Diagnostic and Statistical Manual of Mental Disorders
According to the DSM-V, signs of borderline personality disorder include marked instability in interpersonal relationships, self-image, emotional instability, and marked impulsivity.
All signs of the disorder begin at a young age and appear in a variety of situations.
Diagnosis requires five (or more) of the following in addition to the general criteria for a personality disorder:
- A tendency to exert excessive effort to avoid a real or imagined fate being abandoned . Note: Do not include suicidal behavior and acts of self-harm described in Criterion 5.
- Tendency to engage in intense, tense and unstable relationships characterized by alternation of extremes - idealization and depreciation.
- Identity disorder: noticeable and persistent instability of the image or feeling of the self.
- Impulsivity in at least two areas that involve self-harm (eg, spending money, sexual behavior, substance abuse, traffic violations, habitual overeating). Note: Do not include suicidal behavior and acts of self-harm described in Criterion 5.
- Recurrent suicidal behavior, hints or threats of suicide, acts of self-harm .

- Affective instability, very changeable mood (for example, periods of intense dysphoria, irritability or anxiety, usually lasting for several hours and only occasionally for several days or more).
- Constantly experienced feeling of emptiness .
- Inappropriate manifestations of intense anger or difficulty controlling anger (eg, frequent irritability, persistent anger, repeated fights).
- Transient stress-induced paranoid ideas or severe dissociative symptoms
Behavioral patterns in Borderline Personality Disorder (Marsha M. Linehan)
- Emotional vulnerability and a sense of their own emotional vulnerability. May include a tendency to blame the social environment for unrealistic expectations and demands.
- Self-invalidation - tendency to ignore or deny, not to recognize one's own emotional reactions, thoughts, ideas and behavior.
 Unrealistically high standards and expectations are being set. May include intense shame, self-hatred, and self-directed anger.
Unrealistically high standards and expectations are being set. May include intense shame, self-hatred, and self-directed anger. - Ongoing crisis – model of frequent stressful, negative environmental events, breakdowns and obstacles, some of which arise as a result of an individual's dysfunctional lifestyle, inadequate social environment or random circumstances.
- Repressed feelings - A tendency to suppress and over-control negative emotional reactions - especially those associated with grief and loss, including sadness, anger, guilt, shame, anxiety and panic.
- Active passivity - a tendency to a passive style of solving interpersonal problems, including the inability to actively overcome the difficulties of life, often in combination with vigorous attempts to involve members of one's environment in solving one's own problems; learned helplessness is the lack of motivation for an individual to respond by action in situations where there is a real opportunity to improve the situation.
- Perceived competence - the tendency of an individual to appear more competent than he actually is; usually explained by the inability to generalize the characteristics of mood, situation and time; also the inability to demonstrate adequate non-verbal signals of emotional distress.
Take the BPD likelihood test
Clinical Rating Scale for Borderline Personality Disorder (Dmitry Romanov)
Allows the diagnosis of BPD based on signs that are easily identifiable through an appropriate question asked to the patient by a doctor (features 2-13) and also based on the assessment of the patient's behavior during the interview (sign 15). Confident diagnosis of BPD is carried out when registering a total score of 12 points or more.
1. Female
Most studies indicate that BPD is more common in females. Recent studies of BPD demonstrate the predominance of females compared to males by almost 2 times (Wang L. , Ross C. A., Zhang T., Dai Y., Xiao, Z., 2012). In addition, women with BPD seek specialized help more often than men, which, in particular, is due to gender differences in social rules of behavior.
, Ross C. A., Zhang T., Dai Y., Xiao, Z., 2012). In addition, women with BPD seek specialized help more often than men, which, in particular, is due to gender differences in social rules of behavior.
2. Presence of a situation of violence in childhood and adolescence
Often referred to as anamnestic sign associated by researchers with such pathogenetic links in BPD as stress-induced pathology of the pituitary-hypothalamus-adrenal axis (Goldberg D., 2010)
one and parents, etc.)
A frequently observed anamnestic sign of BPD is associated with the subsequent formation of gender identity disorders in patients (Kernberg O., 1975)
4. Hostility towards one of the parents
5. Early separation (for example, early marriage, leaving the parental home after reaching the age of majority)
6. Intention to change partners due to the existing defect of formation, they are incapable of complete separation and often experience hostile feelings towards the parent, with whom separation problems are associated, as well as towards the marriage partner.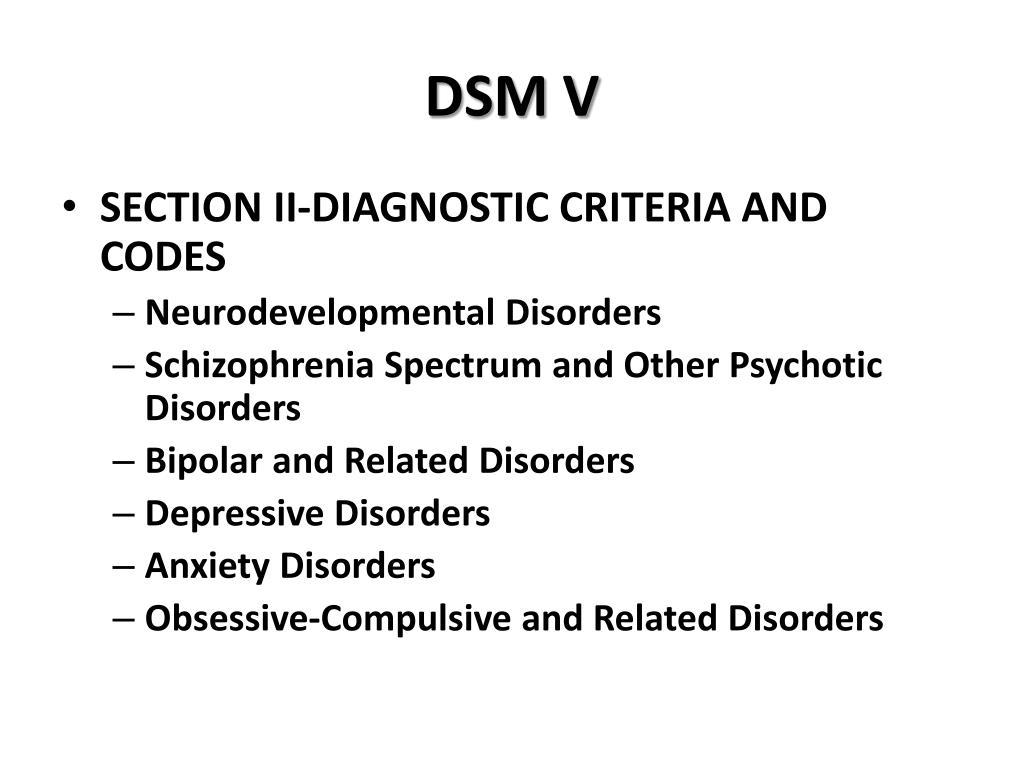 Patients are characterized by an overvalued desire to free themselves from the control of significant persons (McWilliams N., 1994)
Patients are characterized by an overvalued desire to free themselves from the control of significant persons (McWilliams N., 1994)
7. A history of self-harm/suicide
Almost all researchers call this diagnostic feature as an obligate criterion for BPD (Lainen M., 2008). Clinical diagnostic criterion DSM-V
8. History of at least one episode of brutal aggressive behavior (attack, destruction of things)
Behavioral equivalent of the DSM diagnostic criterion 5
consequences
An extremely high association of BPD and substance use disorders has been shown, reaching 73% (B. Grant et al., 2008)
Often noted by investigators BPD
11. More than one marriage (including common-law marriage)
Associated with the inability of patients with BPD to establish long-term relationships based on trust (see related DSM diagnostic criterion 5)
12.