Trauma focused cognitive behavioral therapy tf cbt
Find a TF-CBT Certified Therapist
Aaron Oie
1400 Madison Ave. Ste 610 Mankato, MN 56021 507-387-3777 [email protected]Abbey Guggisberg
2320 US HWY 12 Ste 2 Willmar, MN 56201 5074306442 [email protected]Abbey Scherer
Moontree Psychotherapy Center Madison, WI 53703 608-877-6553 [email protected]Abby Fedewa, LMSW
30000 Hiveley Inkster, MI 48141 734-447-4340 [email protected]Abby Middleton
7501 Penn Ave Pittsburgh, PA 15208 4123875166 [email protected]Abby Rainey
Shelterhouse Midland, MI 48642 9896981620 [email protected]Abena Brown-Elhillali
1750 East Fairmount Ave Baltimore, MD 21231 443-923-7922 [email protected]Abena Derkyi
6686 winbarr way canal winchester, OH 43110 614-625-0362 [email protected]Abigail Cohn
3505 North 124th St Brookfield, WI 53005 414-431-4444 [email protected]Abigail Gonzalez
7651 S.Abigail Kennedy [email protected]
Abigayle Koller
300 Foxcroft Ave., Suite 307 Martinsburg, WV 25401 304-596-2390 [email protected]Acacia Johnson [email protected]
Adam Benton
4004 McCain Blvd, North Little Rock, AR 72116 5018124268 [email protected]Adam Cortez [email protected]
Adam Wilcox
1331 12th Avenue Altoona, PA 16601 8142012751 [email protected]Adedayo Olowoyo [email protected]
Adi Moorman [email protected]
Adila Anwari
701 West Broad street Bethlehem, PA 18018 484-767-0035 [email protected]Adina Rosenberg
2037 Chestnut Street # 30503 Philadelphia, PA 19103 215-431-3111 [email protected]Aditi Gohil
567 Vauxhall Street Ext Waterford, CT 06385 860-800-2421 [email protected]Adrian King
111 North Hudson Altus, OK 73521 580-379-4085 [email protected]Adriana Youssef
1100 Washington Avenue South Minneapolis, MN 55414 6124326798 [email protected]Adrianna Nemeth
614 Romence Rd Portage, MI 49024 2696157637 ext 700 [email protected]Cognitive Behavioral Therapy (CBT) for Treatment of PTSD
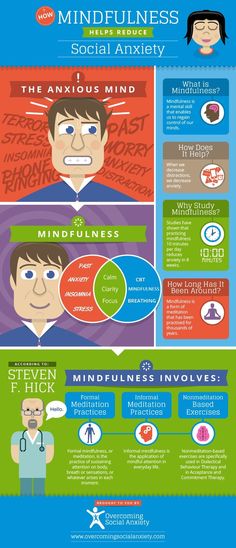
Cognitive behavioral therapy focuses on the relationship among thoughts, feelings, and behaviors; targets current problems and symptoms; and focuses on changing patterns of behaviors, thoughts and feelings that lead to difficulties in functioning.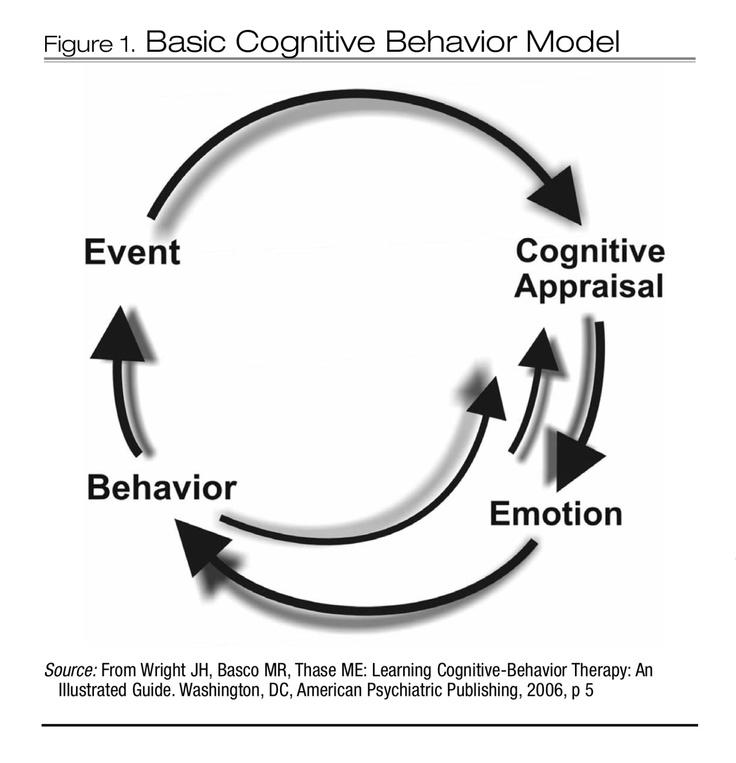
Introduction to CBT
Cognitive behavioral therapy focuses on the relationship among thoughts, feelings, and behaviors, and notes how changes in any one domain can improve functioning in the other domains. For example, altering a person’s unhelpful thinking can lead to healthier behaviors and improved emotion regulation. CBT targets current problems and symptoms and is typically delivered over 12-16 sessions in either individual or group format.
This treatment is strongly recommended for the treatment of PTSD.
How CBT Can Help with PTSD
Several theories specific to trauma explain how CBT can be helpful in reducing the symptoms of PTSD.
For example, emotional processing theory (Rauch & Foa, 2006) suggests that those who have experienced a traumatic event can develop associations among objectively safe reminders of the event (e.g., news stories, situations, people), meaning (e.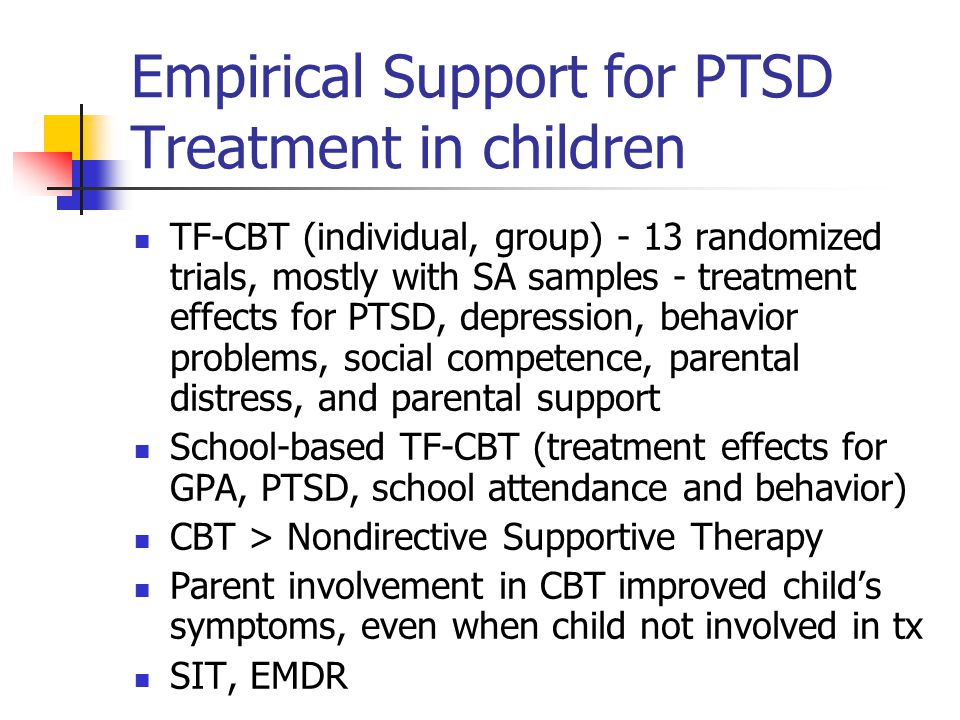 g., the world is dangerous) and responses (e.g., fear, numbing of feelings). Changing these associations that lead to unhealthy functioning is the core of emotional processing.
g., the world is dangerous) and responses (e.g., fear, numbing of feelings). Changing these associations that lead to unhealthy functioning is the core of emotional processing.
Social cognitive theory (Benight & Bandura, 2004) suggests that those who try to incorporate the experience of trauma into existing beliefs about oneself, others, and the world often wind up with unhelpful understandings of their experience and perceptions of control of self or the environment (i.e., coping self-efficacy). For instance, if someone believes that bad things happen to bad people, being raped confirms that one is bad, not that one was unjustly violated.
Understanding these theories helps the therapist more effectively use cognitive behavioral treatment strategies.
Using CBT to Treat PTSD
Therapists use a variety of techniques to aid patients in reducing symptoms and improving functioning. Therapists employing CBT may encourage patients to re-evaluate their thinking patterns and assumptions in order to identify unhelpful patterns (often termed “distortions”) in thoughts, such as overgeneralizing bad outcomes, negative thinking that diminishes positive thinking, and always expecting catastrophic outcomes, to more balanced and effective thinking patterns. These are intended to help the person reconceptualize their understanding of traumatic experiences, as well as their understanding of themselves and their ability to cope.
These are intended to help the person reconceptualize their understanding of traumatic experiences, as well as their understanding of themselves and their ability to cope.
Exposure to the trauma narrative, as well as reminders of the trauma or emotions associated with the trauma, are often used to help the patient reduce avoidance and maladaptive associations with the trauma. Note, this exposure is done in a controlled way, and planned collaboratively by the provider and patient so the patient chooses what they do. The goal is to return a sense of control, self-confidence, and predictability to the patient, and reduce escape and avoidance behaviors.
Education about how trauma can affect the person is quite common as is instruction in various methods to facilitate relaxation. Managing stress and planning for potential crises can also be important components of CBT treatment. The provider, with the patient, has some latitude in selecting which elements of cognitive behavioral therapy are likely to be most effective with any particular individual.
Case Example
Jill, a 32-year-old Afghanistan War veteran
Jill had been experiencing PTSD symptoms for more than five years. She consistently avoided thoughts and images related to witnessing her fellow service members being hit by an improvised explosive device (IED). This case example explains how Jill's therapist used a cognitive worksheet as a starting point for engaging in Socratic dialogue.
For Patients & Families
What is Cognitive Behavioral Therapy?
CBT has been demonstrated to be effective for a range of problems including depression, anxiety disorders, and posttraumatic stress disorder. In many studies, CBT has been demonstrated to be as effective as, or more effective than, other forms of psychological therapy or psychiatric medications.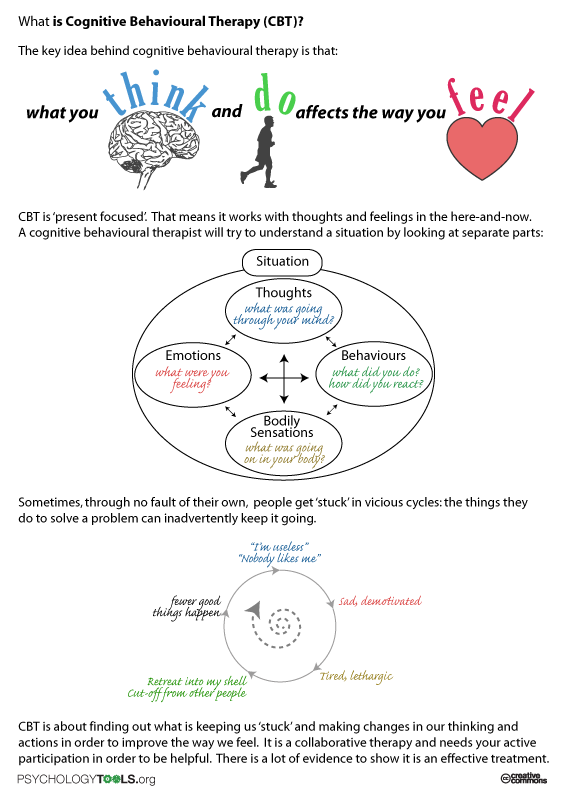
References & Resources
Journal Article
Benight, C. C., & Bandura, A. (2004). Social cognitive theory of posttraumatic recovery: The role of perceived self-efficacy. Behaviour Research and Therapy, 42(10), 1129–1148.
Book
Monson, C. M. & Shnaider, P. (2014). Treating PTSD with cognitive-behavioral therapies: Interventions that work. Washington, DC: American Psychological Association.
Book
Ehlers, A. (2013). Trauma-focused cognitive behavior therapy for posttraumatic stress disorder and acute stress disorder. In Simos, G., & Hofmann, S. G. (eds). CBT for anxiety disorders: A practitioner book (pp. 161-190). New York, NY: Wiley.
Journal Article
Rauch, S., & Foa, E. (2006). Emotional processing theory (EPT) and exposure therapy for PTSD. Journal of Contemporary Psychotherapy, 36(2), 61-65. doi: 10.1007/s10879-006-9008-y
Book
Grey, N. (Ed.) (2009). A casebook of cognitive therapy for traumatic stress reactions. Hove, UK: Routledge.
(Ed.) (2009). A casebook of cognitive therapy for traumatic stress reactions. Hove, UK: Routledge.
Updated July 31, 2017
Date created: March 2017
COGNITIVE-BEHAVIORAL PSYCHOTHERAPY IN THE STRUCTURE OF THE PSYCHOLOGICAL SERVICE OF A MODERN PRESCHOOL EDUCATIONAL INSTITUTION | Consultation on the topic:
COGNITIVE-BEHAVIORAL PSYCHOTHERAPY IN THE STRUCTURE OF THE PSYCHOLOGICAL SERVICE OF A MODERN PRESCHOOL EDUCATIONAL INSTITUTION
Т.А. Kudash,
Head of GBOU School No. 1349, structural unit No. 1 (Moscow), [email protected]
A.I. Melekhin,
Clinical psychologist, certified cognitive-behavioral psychotherapist School No. 1349, structural subdivision No. 1 (Moscow), [email protected]
O.V. Melekhina,
Teacher-defectologist GBOU School No. 1349, structural unit No. 1 (Moscow)
1 (Moscow)
trauma. For example, sexual abuse, domestic violence, physical abuse. Children who have a traumatic grief reaction after the loss of a loved one (parents, brother, sister).
Preschool children often cannot fully understand what happened, they begin to blame themselves, they develop strong negative emotions, which can often be combined with sleep disorders, eating disorders, irritable bowel syndrome, accompanied by mutism, stuttering and other psychogenic problems character. Parents try not to talk about the trauma with both the child and specialists. The child himself has distorted thoughts and feelings about the traumatic experience. Behavioral and emotional problems appear: renunciation, avoidance of communication with adults and peers, interest in play activities and activities decreases, the child often begins to get colds.
In this regard, the question arises: how can the possibilities of the psychological and pedagogical service of a preschool educational institution help a child with psychological trauma?
What is Cognitive Behavioral Therapy?
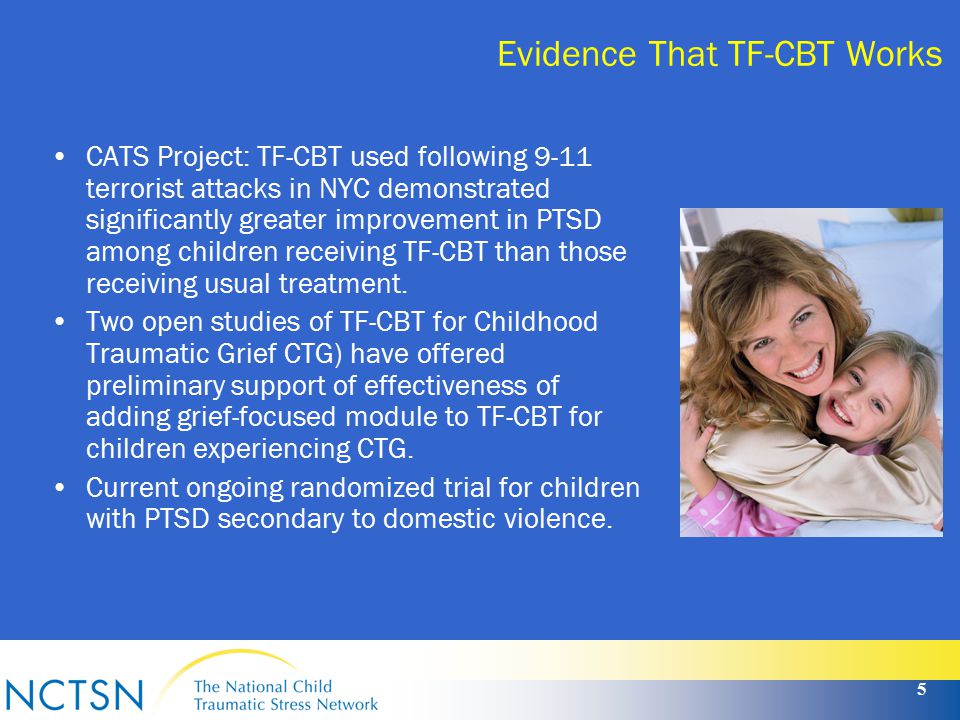
Trauma-focused Cognitive Behavioral Therapy (CBT) is the gold standard in psychotherapeutic work with children of middle and older preschool age all over the world.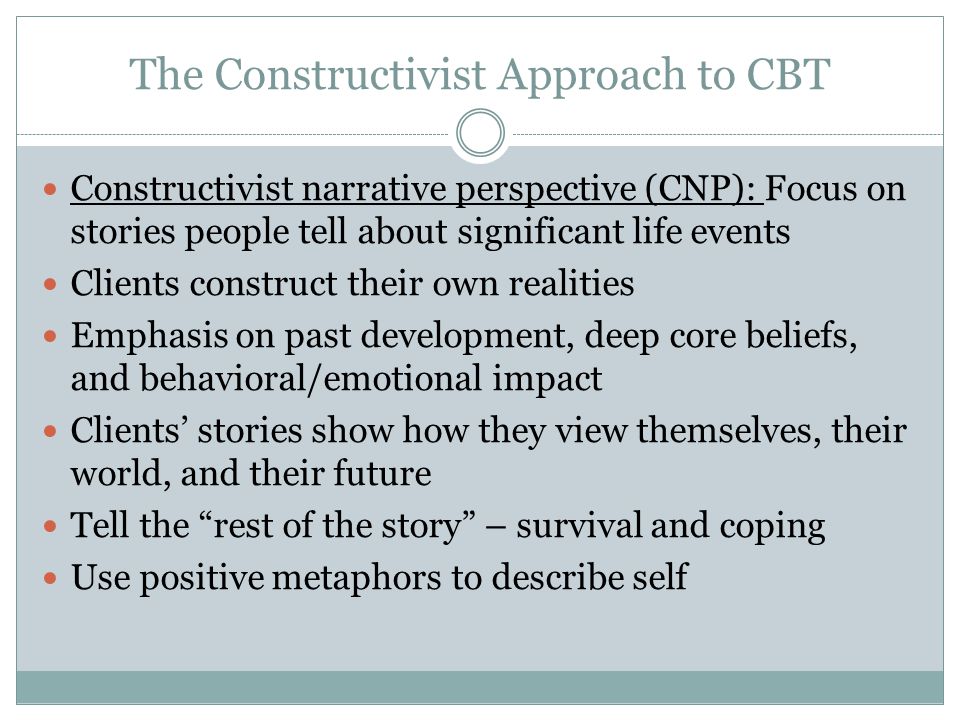 This directive direction of psycho-corrective work has proven itself all over the world and allows you to overcome the consequences of various psychological traumas, behavioral and emotional problems.
This directive direction of psycho-corrective work has proven itself all over the world and allows you to overcome the consequences of various psychological traumas, behavioral and emotional problems.
Initially, this line of psychotherapy was developed for the treatment of monophobia, anxiety, depressive episodes in adults (Wolpe, 1969; Beck, 1976). It was further used in the treatment of adults who were victims of rape and developed symptoms of post-traumatic stress disorder (Foa, Rothbaum, Riggs, Murdock, 1991). More recently, this area of psychotherapy has been applied and adapted to children of preschool, primary school age and adolescents with emotional and behavioral problems. For example, fears, excessive anxiety, eating disorders, sleep disorders (Beidel and Turner, 1998).
Cognitive Behavioral Therapy is not only well established for dealing with trauma problems, but also for overcoming learning difficulties in children (Patterson, 2005; Forehand & Kotchick, 2002). It is especially worth noting the separate application of this direction in helping parents in solving behavioral problems with their children.
It is especially worth noting the separate application of this direction in helping parents in solving behavioral problems with their children.
Cognitive behavioral psychotherapy is a short-term psychocorrectional work that includes 12-18 sessions from 20-30 minutes to 50-90 minutes depending on the age characteristics of the child, the need for psychotherapeutic assistance, the degree of the psychological state of the child.
Goals of cognitive-behavioral psychotherapy
- Reduction of negative emotional and behavioral reactions that may be reactive as a result of psychological trauma.
- Provide support and teach skills to effectively cope with emotional distress, depressive episodes in parents.
- Train parents on how to best respond to their children's problems and support their children.
Specifics of cognitive-behavioral psychotherapy of children
All work with a child of preschool age is adapted to the age-psychological characteristics of the child.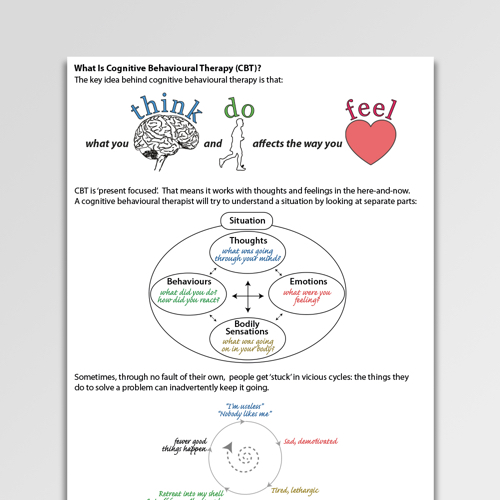
Visual diagrams, toys are used (bibabo toys are especially useful), an interactive drawing board, a tablet computer with the installed program (Triangle of Life) are actively used. Classes are held individually. They include classes with a child and a parent (guardian), or a joint lesson with a child and a parent together. Each session is designed to build a therapeutic relationship, as well as psychoeducation, teaching skills to effectively cope with stress, organizing a safe environment for resolving and processing traumatic experiences.
Joint "child-parent sessions" are aimed at helping parents and children in practice use the techniques they have learned to reduce stress, anxiety, and fears. They are also aimed at promoting effective parent-child communication for discussion, experiencing the trauma.
Cognitive-behavioral psychotherapy of psychological trauma includes three areas of work:
- Cognitive psychotherapy - aimed at changing behavior.
 Work with negative automatic thoughts, images, convictions, beliefs.
Work with negative automatic thoughts, images, convictions, beliefs. - Behavioral psychotherapy - aimed at changing habitual non-adaptive responses (anger, fear, anxiety). Identification of situations, incentives that cause these responses.
- Family therapy - aimed at studying the patterns of interaction between family members and helps to identify and solve problems.
The work of an educator, clinical psychologist, defectologist is based on building a safe environment in which a child can verbally (story) or non-verbally (drawing, role-play, etc.) talk about his traumatic experience. Work with beliefs, negative (destructive) emotions of the child using behavioral and cognitive techniques.
To start working with psychological trauma, on the one hand, it is important to create a safe environment for interaction between a specialist and a child, and on the other hand, to teach a child a “set of tools”, strategies for managing anxiety and stress. For example, the technique of controlled breathing, progressive muscle relaxation, etc.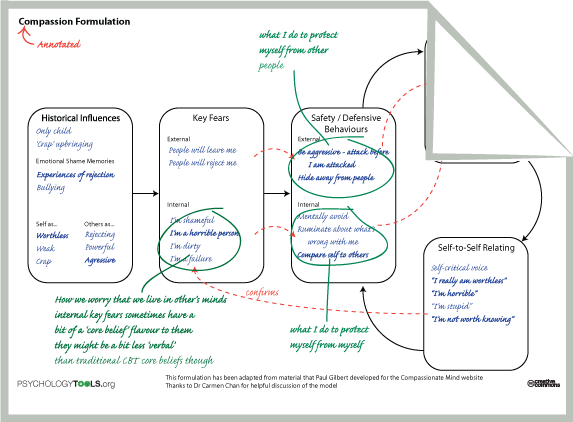 All these techniques are not only mastered by imitating a specialist, but also played together by the child in a role-playing game so that he knows in what situations it is better to use these techniques. Homework is required. For example, do the exercise once a day. You can also additionally ask the child to show this exercise to their parents. In parenting sessions, the child's parent is taught these techniques and asked to do them with the child every day for a set amount of time.
All these techniques are not only mastered by imitating a specialist, but also played together by the child in a role-playing game so that he knows in what situations it is better to use these techniques. Homework is required. For example, do the exercise once a day. You can also additionally ask the child to show this exercise to their parents. In parenting sessions, the child's parent is taught these techniques and asked to do them with the child every day for a set amount of time.
Working with parents in cognitive-behavioral psychotherapy
As mentioned above, psychocorrectional work is built not only with the child, but also with parents who cannot cope with the fact that their child is in a situation of psychological trauma. Parents often experience "parental distress" i.e. excessive neuropsychic stress accompanied by the development of functional disorders from various organ systems. This state is accompanied by catastrophic, dichotomous (black and white) negative thoughts that increase tension)
Specialists work with negative thoughts that are of an anxious and ruminating nature; they are based on the themes of self-accusation, catastrophization, obligation (“I should”, “who if not me”), anxiety (“what if”, “what if”). Teaches parents how to cope with their maladaptive state.
Teaches parents how to cope with their maladaptive state.
One of the parents is also asked to monitor the emotional state of their child during the course of psycho-correctional work. To fix on a certain analog scale (0-10 points) the level of anxiety, aggressiveness, tension, isolation and show the dynamics to specialists.
Psychoeducation
Before involving parents in psychotherapy, it is necessary to conduct psychoeducation, which includes:
- Discussion of the results of a psychological (neuropsychological) examination (cognitive, emotional and volitional spheres) of a child with the selection of therapy targets and the construction of recommendations.
- Substantiation and review of psycho-correctional work (psychotherapy). Providing an algorithm, clear steps. For example, first the child is taught the skills of coping with discomfort, tension. Talking about a traumatic event with a child will be in specially organized forms, slowly, with a greater degree of support from a specialist.
- Talk about childhood psychological trauma, symptoms. Emphasize early initiation of psychotherapy to prevent long-term problems in the child.
- The importance of talking directly to the child about the trauma in order to help them begin to deal with their feelings about what happened.
- Help the parent understand their role in the child's psychotherapy. It is important to convey to the parent that this treatment model emphasizes the importance of teamwork. Any initiative of the parent, questions, suggestions are welcome at all stages of psychotherapy.
- Development of a child safety plan (personal safety skills for parent and child).
Basic strategies used in CBT
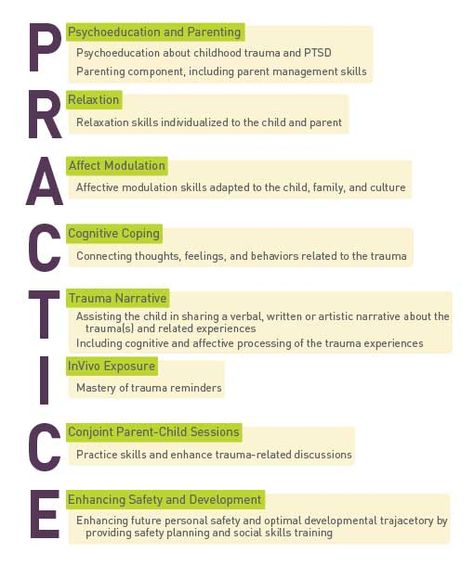
Basic techniques used in CBT can be abbreviated as practice (“PRACTICE”)
- P – Psychoeducation and recognition skills training. Discussion with parents, caregivers about child abuse. Typical emotional and behavioral reactions as a result of psychological trauma.
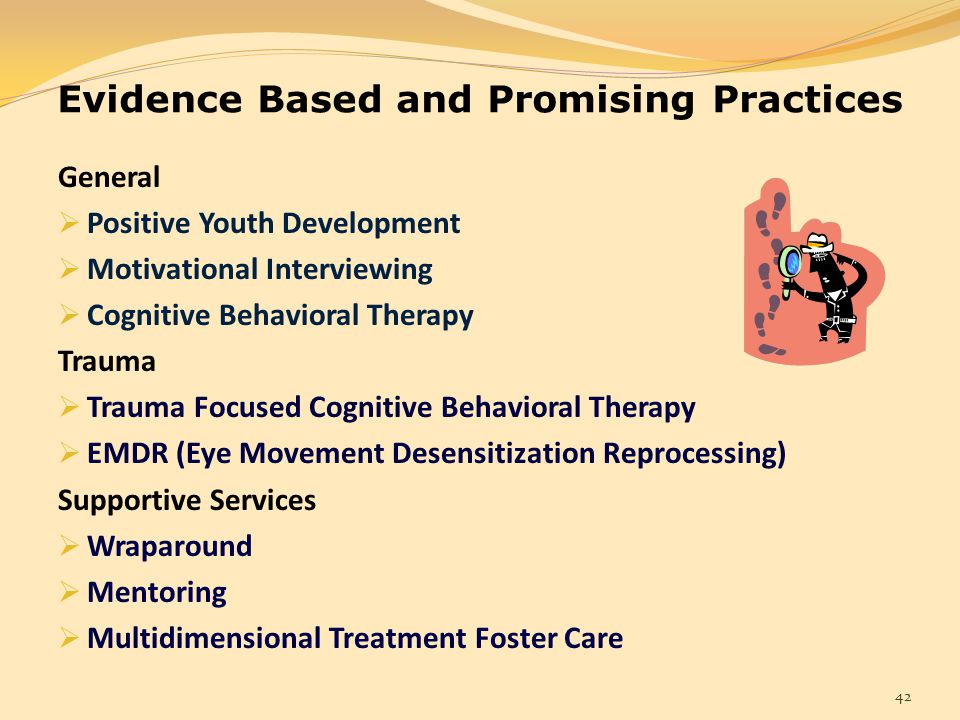 Teaching parents effective behavior management strategies and effective communication with a traumatized child.
Teaching parents effective behavior management strategies and effective communication with a traumatized child. - R - Relaxation methods. Training in conscious breathing techniques, controlled breathing, progressive muscle relaxation, relaxation using visual images.
- A - Affective (emotional) expression and regulation of this expression. Help the child and parents manage their emotional reactions, increase the efficiency of identifying negative emotions, expressing them less maladaptive. Participation in calming activities.
- K - Cognitive model "Negative automatic thought - emotions - behavior". In practice, help to understand the relationship between these three components. The study and correction of negative automatic thoughts, beliefs, beliefs leading to maladaptive reactions.
- T - Narrative (story) about the trauma and processing of this information. A gradual presentation of events, clarifying inaccurate, negative automatic thoughts about the event.

- I - Control of emotional reactions in natural conditions. When reminded in the environment of the child about the injury, use stress coping techniques.
- K - Joint parent-child sessions to improve communication and create opportunities for therapeutic discussion of trauma.
- A - Increased personal safety, teaching safety skills, interpersonal communication, coping strategies, and trauma memories.
Conclusion
Based on a large number of studies, this area of psychotherapy is effective in psychocorrective work with children who have experienced psychological trauma and who have emotional and behavioral difficulties. However, in our country, specialists in the field of child psychotherapy, psychocorrection are not familiar with this short-term, directive direction of work with children and parents who have suffered psychological trauma. There are no Russian-language sources, retraining programs for specialists to familiarize themselves with this area of child psychotherapy.
The use of cognitive-behavioral psychotherapy can improve the results in providing psychological assistance to children of different ages.
New York Best Practice | Beacon Health Parameters
New York Best Practices | Beacon Health Options [Jump to content] Mobile site search Search fieldNew York has selected recognized best practices as best practice. Beacon has adopted these recommendations for use with Medicaid. Providers can get more information from the links below.
- Substance Abuse and Mental Health Services Administration (SAMHSA). Evidence-Based Comprehensive Treatment Package (EBP) - Published January 2010, revised 2019
- Substance Abuse and Mental Health Administration (SAMHSA). Supported set of Evidence-Based Employment Practices (EBP) - Published February 2010, revised 2019
- Substance Abuse and Mental Health Administration (SAMHSA). Evidence-Based Practices (EBP) for Assertive Community Treatment (ACT) - Published October 2008, revised 2019
- Treatment Innovation.
 Seeking Safety - Published 2002, revised 2019
Seeking Safety - Published 2002, revised 2019
- Project of the National Institute on Alcohol Abuse and Alcoholism (NIAA). MATCH Project Monograph Series Volume 1 Twelve Step Facilitation Therapy Guide – NIH Publication No. 94-3722, revised 2019.
- National Childhood Traumatic Stress Network. TF-CBT: Trauma Focused Cognitive Behavioral Therapy - Published April 2012, revised 2018
- Childhood Trauma Stress National Network (NCTSN). Parent-Child Psychotherapy - Published 2012, revised 2018
- MCT services. Multisystem Therapy - Review 2018.
- American Psychological Association. Functional Family Therapy for Adolescent Behavior Problems - Copyright 2013, revised 2018
- DBT-Linehan Certification Board. Dialectical Behavior Therapy - Copyright 2014, revised 2018
- MDFT International. Multidimensional Family Therapy - Reviewed 2018
- TFC Consultants, Inc.
Learn more