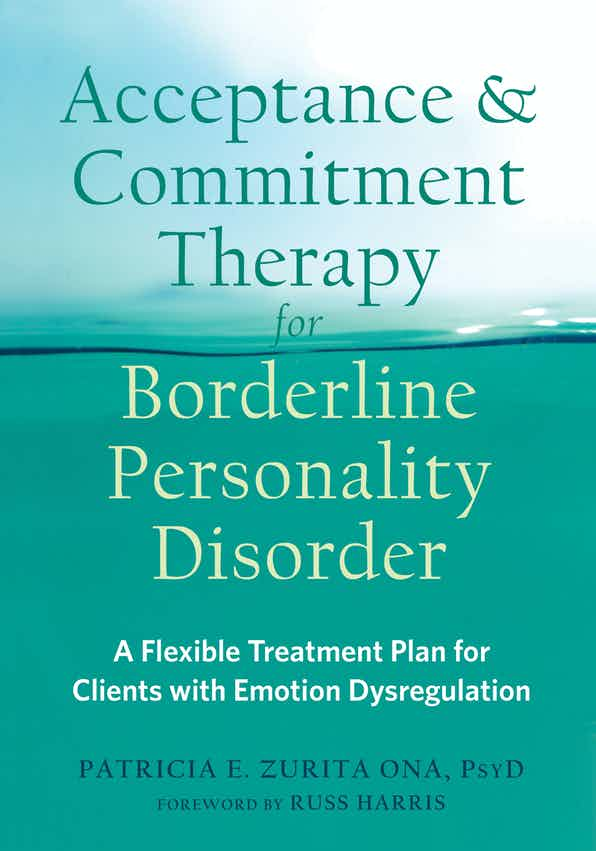
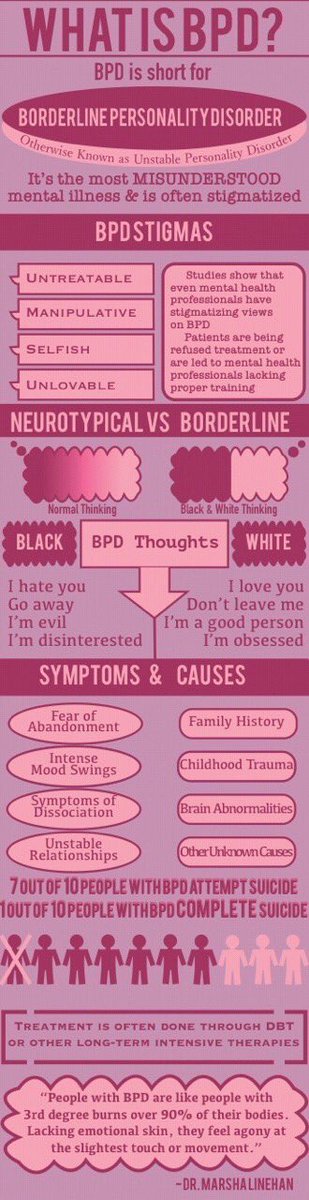
Therapy for borderline personality
Borderline personality disorder - Diagnosis and treatment
Diagnosis
Personality disorders, including borderline personality disorder, are diagnosed based on a:
- Detailed interview with your doctor or mental health provider
- Psychological evaluation that may include completing questionnaires
- Medical history and exam
- Discussion of your signs and symptoms
A diagnosis of borderline personality disorder is usually made in adults, not in children or teenagers. That's because what appear to be signs and symptoms of borderline personality disorder may go away as children get older and become more mature.
Treatment
Borderline personality disorder is mainly treated using psychotherapy, but medication may be added. Your doctor also may recommend hospitalization if your safety is at risk.
Treatment can help you learn skills to manage and cope with your condition. It's also necessary to get treated for any other mental health disorders that often occur along with borderline personality disorder, such as depression or substance misuse. With treatment, you can feel better about yourself and live a more stable, rewarding life.
Psychotherapy
Psychotherapy — also called talk therapy — is a fundamental treatment approach for borderline personality disorder. Your therapist may adapt the type of therapy to best meet your needs. The goals of psychotherapy are to help you:
- Focus on your current ability to function
- Learn to manage emotions that feel uncomfortable
- Reduce your impulsiveness by helping you observe feelings rather than acting on them
- Work on improving relationships by being aware of your feelings and those of others
- Learn about borderline personality disorder
Types of psychotherapy that have been found to be effective include:
- Dialectical behavior therapy (DBT). DBT includes group and individual therapy designed specifically to treat borderline personality disorder. DBT uses a skills-based approach to teach you how to manage your emotions, tolerate distress and improve relationships.

- Schema-focused therapy. Schema-focused therapy can be done individually or in a group. It can help you identify unmet needs that have led to negative life patterns, which at some time may have been helpful for survival, but as an adult are hurtful in many areas of your life. Therapy focuses on helping you get your needs met in a healthy manner to promote positive life patterns.
- Mentalization-based therapy (MBT). MBT is a type of talk therapy that helps you identify your own thoughts and feelings at any given moment and create an alternate perspective on the situation. MBT emphasizes thinking before reacting.
- Systems training for emotional predictability and problem-solving (STEPPS). STEPPS is a 20-week treatment that involves working in groups that incorporate your family members, caregivers, friends or significant others into treatment. STEPPS is used in addition to other types of psychotherapy.
-
Transference-focused psychotherapy (TFP).
 Also called psychodynamic psychotherapy, TFP aims to help you understand your emotions and interpersonal difficulties through the developing relationship between you and your therapist. You then apply these insights to ongoing situations.
Also called psychodynamic psychotherapy, TFP aims to help you understand your emotions and interpersonal difficulties through the developing relationship between you and your therapist. You then apply these insights to ongoing situations. - Good psychiatric management. This treatment approach relies on case management, anchoring treatment in an expectation of work or school participation. It focuses on making sense of emotionally difficult moments by considering the interpersonal context for feelings. It may integrate medications, groups, family education and individual therapy.
Medications
Although no drugs have been approved by the Food and Drug Administration specifically for the treatment of borderline personality disorder, certain medications may help with symptoms or co-occurring problems such as depression, impulsiveness, aggression or anxiety. Medications may include antidepressants, antipsychotics or mood-stabilizing drugs.
Talk to your doctor about the benefits and side effects of medications.
Hospitalization
At times, you may need more-intense treatment in a psychiatric hospital or clinic. Hospitalization may also keep you safe from self-injury or address suicidal thoughts or behaviors.
Recovery takes time
Learning to manage your emotions, thoughts and behaviors takes time. Most people improve considerably, but you may always struggle with some symptoms of borderline personality disorder. You may experience times when your symptoms are better or worse. But treatment can improve your ability to function and help you feel better about yourself.
You have the best chance for success when you consult a mental health provider who has experience treating borderline personality disorder.
More Information
- Psychotherapy
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Coping and support
Symptoms associated with borderline personality disorder can be stressful and challenging for you and those around you.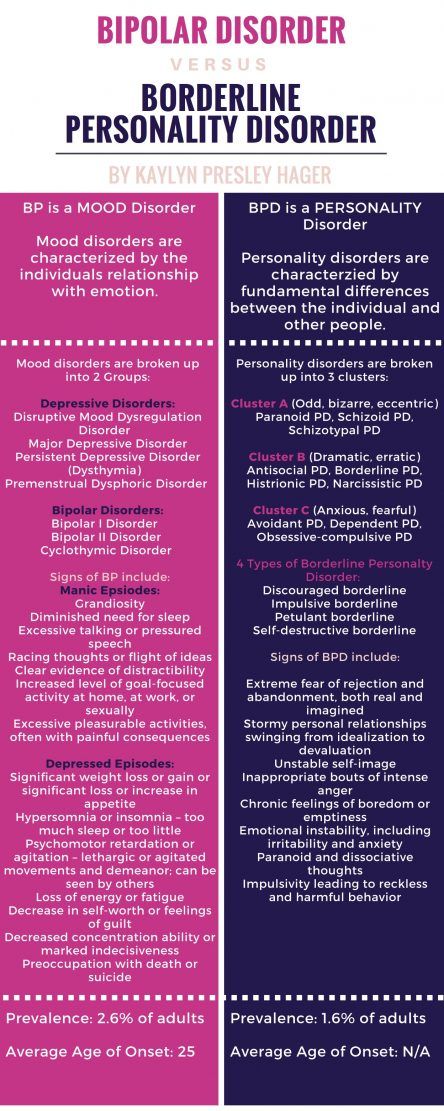 You may be aware that your emotions, thoughts and behaviors are self-destructive or damaging, yet you feel unable to manage them.
You may be aware that your emotions, thoughts and behaviors are self-destructive or damaging, yet you feel unable to manage them.
In addition to getting professional treatment, you can help manage and cope with your condition if you:
- Learn about the disorder so that you understand its causes and treatments
- Learn to recognize what may trigger angry outbursts or impulsive behavior
- Seek professional help and stick to your treatment plan — attend all therapy sessions and take medications as directed
- Work with your mental health provider to develop a plan for what to do the next time a crisis occurs
- Get treatment for related problems, such as substance misuse
- Consider involving people close to you in your treatment to help them understand and support you
- Manage intense emotions by practicing coping skills, such as the use of breathing techniques and mindfulness meditation
- Set limits and boundaries for yourself and others by learning how to appropriately express emotions in a manner that doesn't push others away or trigger abandonment or instability
- Don't make assumptions about what people are feeling or thinking about you
- Reach out to others with the disorder to share insights and experiences
- Build a support system of people who can understand and respect you
- Keep up a healthy lifestyle, such as eating a healthy diet, being physically active and engaging in social activities
- Don't blame yourself for the disorder, but recognize your responsibility to get it treated
Preparing for your appointment
You may start by seeing your primary care doctor. After an initial appointment, your doctor may refer you to a mental health provider, such as a psychologist or psychiatrist. Here's some information to help you prepare for your appointment.
After an initial appointment, your doctor may refer you to a mental health provider, such as a psychologist or psychiatrist. Here's some information to help you prepare for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you or people close to you have noticed, and for how long
- Key personal information, including traumatic events in your past and any current major stressors
- Your medical information, including other physical or mental health conditions
- All medications you take, including prescription and over-the-counter medications, vitamins and other supplements, and the doses
- Questions you want to ask your doctor so that you can make the most of your appointment
Take a family member or friend along, if possible. Someone who has known you for a long time may be able to share important information with the doctor or mental health provider, with your permission.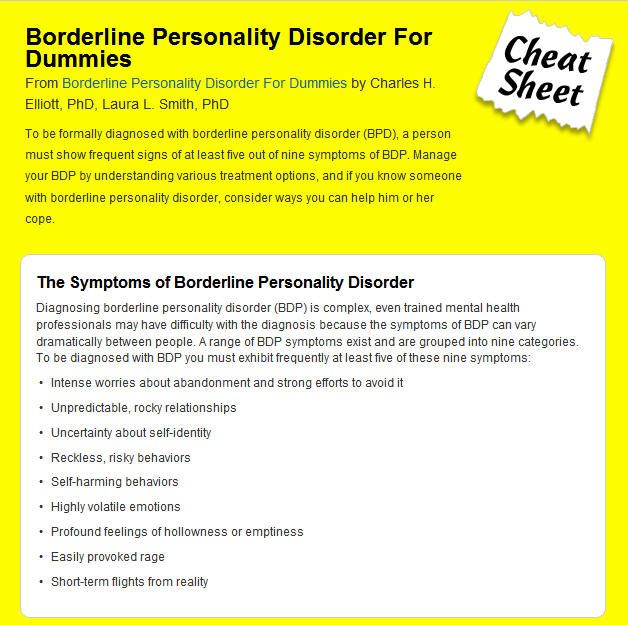
Basic questions to ask your doctor or a mental health provider include:
- What's likely causing my symptoms or condition?
- Are there any other possible causes?
- What treatments are most likely to be effective for me?
- How much can I expect my symptoms to improve with treatment?
- How often will I need therapy sessions and for how long?
- Are there medications that can help?
- What are the possible side effects of the medication you may prescribe?
- Do I need to take any precautions or follow any restrictions?
- I have these other health conditions. How can I best manage them together?
- How can my family or close friends help me in my treatment?
- Do you have any printed material that I can take? What websites do you recommend?
Don't hesitate to ask questions during your appointment.
What to expect from your doctor
A doctor or mental health provider is likely to ask you a number of questions. Be ready to answer them to save time for topics you want to focus on. Possible questions include:
Be ready to answer them to save time for topics you want to focus on. Possible questions include:
- What are your symptoms? When did you first notice them?
- How are these symptoms affecting your life, including your personal relationships and work?
- How often during the course of a normal day do you experience a mood swing?
- How often have you felt betrayed, victimized or abandoned? Why do you think that happened?
- How well do you manage anger?
- How well do you manage being alone?
- How would you describe your sense of self-worth?
- Have you ever felt you were bad, or even evil?
- Have you had any problems with self-destructive or risky behavior?
- Have you ever thought of or tried to harm yourself or attempted suicide?
- Do you use alcohol or recreational drugs or misuse prescription drugs? If so, how often?
- How would you describe your childhood, including your relationship with your parents or caregivers?
- Were you physically or sexually abused or were you neglected as a child?
- Have any of your close relatives or caregivers been diagnosed with a mental health problem, such as a personality disorder?
- Have you been treated for any other mental health problems? If yes, what diagnoses were made, and what treatments were most effective?
- Are you currently being treated for any other medical conditions?
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
TREATING BPD | National Education Alliance for Borderline Personality Disorder
Treatments for Borderline Personality Disorder
Current research shows that treatment can decrease the symptoms and suffering of people with BPD.
Talk therapy is usually the first choice of treatment (unlike some other illnesses where medication is often first.) Generally, treatment involves one to two sessions a week with a mental health counselor. For therapy to be effective, people must feel comfortable with and trust their therapist.
Some BPD symptoms are easier to treat than others. Fears that others might leave, intense, unstable relationships or feelings of emptiness are often hardest to change. Research shows that treatment is more effective in decreasing anger, suicide attempts and self- harm, as well as helping to improve over-all functioning and social adjustment
People whose symptoms improve may still have issues related to co-occurring disorders, such as depression, substance abuse, eating disorders, or post-traumatic stress disorder. However, research suggests that full-blown BPD symptoms rarely coming back after remission.
There are several treatments that are most often used to manage BPD
Dialectical behavior therapy (DBT) focuses on the concept of mindfulness, or paying attention to the present emotion. DBT teaches skills to control intense emotions, reduce self-destructive behavior, manage distress, and improve relationships. It seeks a balance between accepting and changing behaviors. This proactive, problem-solving approach was designed specifically to treat BPD. Treatment includes individual therapy sessions, skills training in a group setting, and phone coaching as needed. DBT is the most studied treatment for BPD and the one shown to be most effective.
DBT teaches skills to control intense emotions, reduce self-destructive behavior, manage distress, and improve relationships. It seeks a balance between accepting and changing behaviors. This proactive, problem-solving approach was designed specifically to treat BPD. Treatment includes individual therapy sessions, skills training in a group setting, and phone coaching as needed. DBT is the most studied treatment for BPD and the one shown to be most effective.
Mentalization-based therapy (MBT) is a talk therapy that helps people identify and understand what others might be thinking and feeling.
Transference-focused therapy (TFP) is designed to help patients understand their emotions and interpersonal problems through the relationship between the patient and therapist. Patients then apply the insights they learn to other situations.
Good Psychiatric Management: GPM provides mental health professionals an easy-to-adopt “tool box” for patients with severe personality disorders.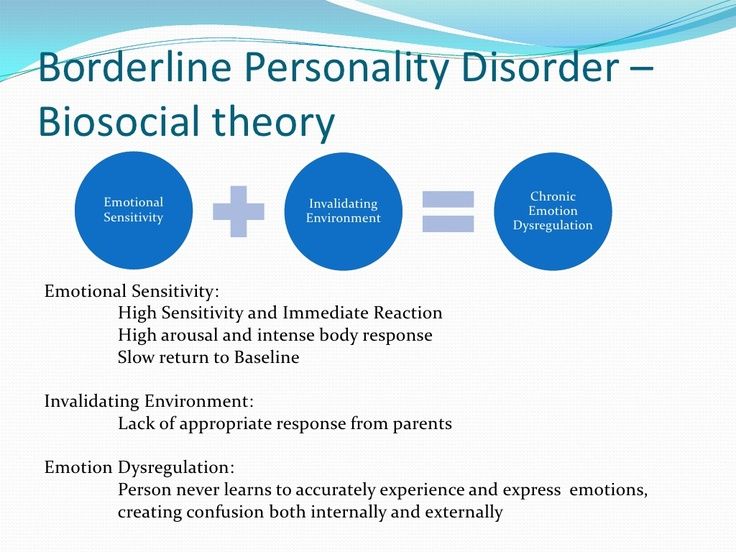
Medications cannot cure BPD but can help treat other conditions that often accompany BPD such as depression, impulsivity, and anxiety. Often patients are treated with several medications, but there is little evidence that this approach is necessary or effective. People with BPD are encouraged to talk with their prescribing doctor about what to expect from each medication and its side effects. 1
Self-Care activities include: regular exercise, good sleep habits, a nutritious diet, taking medications as prescribed, and healthy stress management. Good self-care can help to reduce common symptoms of BPD such as mood changes, impulsive behavior, and irritability.
1. Zanarini MC, Frankenburg FR. omega-3 Fatty acid treatment of women with borderline personality disorder: a double-blind, placebo-controlled pilot study. Am J Psychiatry. 2003 Jan;160(1):167–9.
What to do with BPD? Advice for “border guards”
Medical issues
Text: Masha Pushkina,
Ekaterina Tarasova
Illustrations: Alena Belyakova
November 09, 2017
Borderline personality disorder (BPD) is a mental illness associated with instability in interpersonal relationships and self-image, emotional instability and impulsivity. We have already talked about how people with BPD live, and today we will figure out what types of therapy are effective for borderline disorder and what experts advise border guards and their loved ones.
We have already talked about how people with BPD live, and today we will figure out what types of therapy are effective for borderline disorder and what experts advise border guards and their loved ones.
Anastasia Umanskaya, Gestalt psychotherapist: “Long-term psychotherapy is the main treatment for borderline personality disorder. And the most efficient. Therapy helps a person learn the skills to cope with strong emotions and maintain long-term relationships. The effectiveness of dialectical-behavioral psychotherapy has been studied the most. In addition to it, psychotherapy based on mentalization, psychotherapy focused on transference, psychodynamic therapy are effective in the treatment of BPD. The therapist draws up a treatment plan taking into account the characteristics of the character, personality and living conditions of the patient and includes individual therapy and group sessions.
BPD Therapy
The service market offers many types of therapeutic treatment, in which an ignorant patient can become confused. We have compiled the main types of therapies with proven effectiveness.
We have compiled the main types of therapies with proven effectiveness.
Dialectical Behavior Therapy (DBT)
A type of behavioral therapy developed specifically for people with BPD by American psychologist Marsha Linehan, author of Cognitive Behavioral Therapy for Borderline Personality Disorder. Within its framework, the patient is invited to realize that there are different points of view on the situation, which he perceives as “unbearable” and “hopeless”, so that he can eventually choose a more adequate behavior. The main point in this therapy is the need to accept patients as they are, while at the same time trying to teach them to change. During the DBT process, the therapist teaches the patient the necessary skills for emotional regulation, interpersonal effectiveness, stress coping skills, general mental engagement, and self-control. The emphasis in DBT is on acknowledging the person's emotional responses so that the person suffering from BPD feels supported. The duration of such therapy is usually from twenty-four to forty-eight weeks.
The duration of such therapy is usually from twenty-four to forty-eight weeks.
Dmitry Pushkarev, psychotherapist , develops DBT in Russia: “Every person, finding himself in a crisis situation, is looking for ways to cope with it. But they can be destructive: alcohol, aggression, suicide. Accordingly, the task of therapy is to teach the patient practical skills that will help to get out of the crisis. These are techniques of awareness, control of emotions, accepting a situation or finding a way out of it. DBT is a direction of therapy that has become very widespread in recent years. Initially, the technique was developed for people with chronic suicidal behavior - for those who repeat attempts to kill themselves and injure themselves even after treatment in a hospital (it is important to remember that young men and women often end up in Russian hospitals with a third or fourth suicide attempt). Today, DBT is used in the treatment of severe patients, including those with serious mental disorders - with borderline personality disorder or depression.
Russian experts have founded the first Dialectical Behavior Therapy Society to spread this practice. Here, psychotherapists can learn DBT, and patients can undergo group and personal trainings.”
Mentalization Based Therapy (MBT)
Aimed at stabilizing the sense of self and helping the patient manage emotions in relationships. Mentalization is the process by which one person forms an idea of the behavior, thoughts, words, and reactions of other people. This process allows you to explain the behavior of others and requires an analysis of the circumstances of the actions. People suffering from BPD most often misinterpret the actions and actions of other people, putting their own subjective meaning into everything, which is why they do not accurately understand the states of others. In the process of therapy, the patient learns to accurately perceive the motives of the actions of other people. The therapist explains that any situation can be perceived from different angles, teaches you to ask clarifying questions about what a person might think, feel and do in the context of interaction with a person suffering from BPD. The task of therapy is to form the ability to reflect and teach the patient other skills of interpersonal interaction.
The task of therapy is to form the ability to reflect and teach the patient other skills of interpersonal interaction.
Transfer Focused Therapy (TFP)
TFP is a psychodynamic psychotherapy with step by step instructions. It was developed specifically for the treatment of borderline pathology and is based on the idea that the patient experiences external reality through his split inner world - and therefore sees others in black and white (idealization or devaluation). The task of the therapist is to help the patient become aware of this distortion and learn to perceive both the negative and positive traits of people at the same time.
Phrases every border guard should learn:
How do I feel now?
What do you mean?
What exactly do you want from me?
Is this reality or my fantasy?
I need time to answer you.
I am worthy of love and respect. But close people deserve a respectful attitude.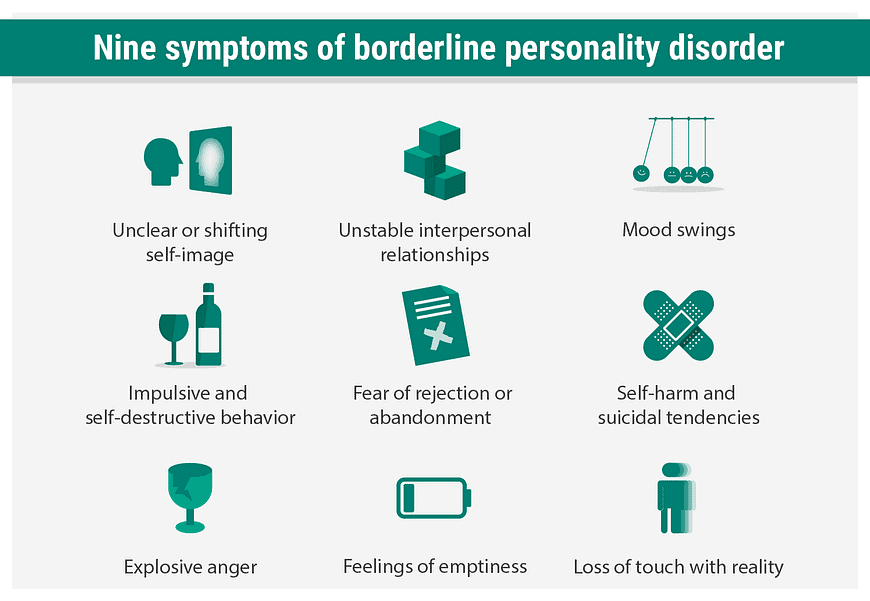
It will pass soon, we must wait a little.
Cognitive behavioral therapy
A type of psychotherapy that aims to change the way you think, with the result that you change your mood and behavior, is one of the first to be proven effective. Based on the notion that negative actions or feelings are the result of current distorted observations and thoughts, and not unconscious problems from the past.
Together with the therapist, the patient works to identify specific patterns of negative thoughts and behavioral responses to difficult and stressful situations. Treatment involves developing more balanced and constructive ways to respond to stress. The therapist teaches the patient constructive forms of behavior, correcting dysfunctional thoughts and patterns of behavior. The result can be achieved in ten to twenty sessions.
Schema Therapy
Schema (or schematic) therapy was developed by the American psychologist Jeffrey Young based on cognitive behavioral therapy, psychoanalysis, object relations theory, attachment theory and gestalt therapy. Schema uses various therapeutic techniques: interpersonal skills, one-on-one dialogues, group discussions. The name of Young's therapy emphasizes the idea that the "borderline" is acting according to a pattern formed in childhood. Such a schema is formed under the influence of traumatic events or maltreatment in childhood and is activated in adulthood under the influence of similar circumstances, provoking a certain perception of the world and reactions to it. The goal of schema therapy is to help the patient become aware of their schemas and the source of the emotions that arise when these schemas are activated, to experience these emotions and find ways to respond to events differently, destroying old patterns of behavior.
Schema uses various therapeutic techniques: interpersonal skills, one-on-one dialogues, group discussions. The name of Young's therapy emphasizes the idea that the "borderline" is acting according to a pattern formed in childhood. Such a schema is formed under the influence of traumatic events or maltreatment in childhood and is activated in adulthood under the influence of similar circumstances, provoking a certain perception of the world and reactions to it. The goal of schema therapy is to help the patient become aware of their schemas and the source of the emotions that arise when these schemas are activated, to experience these emotions and find ways to respond to events differently, destroying old patterns of behavior.
Alexander Erichev, a researcher at the Bekhterev Research Institute, presented a new direction for Russia in cognitive behavioral therapy. In Russia, this direction is just beginning its journey, so there are only a few certified specialists who can be contacted.
Self-help
Anastasia Umanskaya, Gestalt psychotherapist: “For a person suffering from borderline personality disorder, a sense of security is extremely important. This means minimizing stress in your personal life and at work so that responsibilities in business and at home are clearly defined, without ambiguities and generalizations. Stress will destabilize him.
It is important for a person with BPD to be aware of their own impulses and moods. Psychotherapy will help to distinguish between real needs and painful impulses caused by the imagination. A simple yet powerful way to become more self-aware is to ask yourself, “How do I feel?” several times a day.
It is important to inhibit impulsive behavior. “Measure twice, cut once” is the motto for a person with BPD who wants to improve their quality of life.
It is necessary to master self-soothing techniques. It can be meditation, breathing techniques, yoga classes, soothing music, aromatic bath. Breathing techniques will help you pause to respond to the stimulus more slowly and less impulsively.
It is important to learn how to express both positive and negative emotions in an ecological way. If the former are welcome in our society, then it is more difficult with negative emotions. But if you just suppress them, they accumulate, and sooner or later an emotional outburst will follow. Therefore, one should learn to express them, but in a form acceptable to others.
It is helpful to remind yourself that you are worthy of love and respect. As an exercise, often remember your merits, achievements and reasons for pride. Set realistic goals for yourself. Many small achievements will support you much better than one big and difficult achievement.
It is important not to succumb to criticism within yourself and scold yourself as little as possible. Remind yourself that even the most difficult period is temporary and will end sooner or later.
A healthy lifestyle is always useful.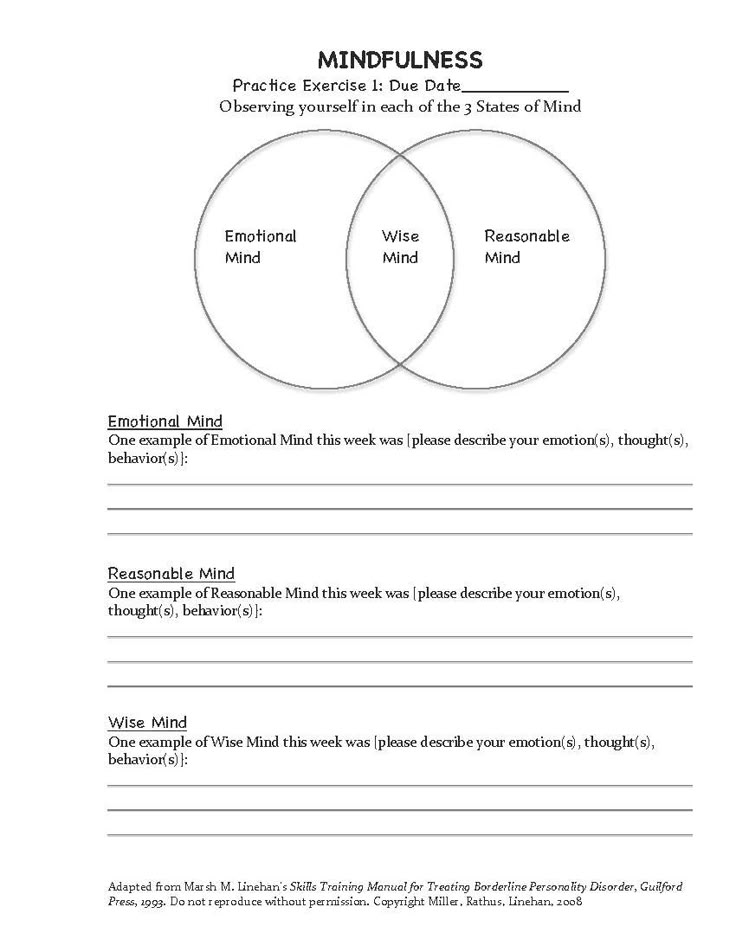 Sports activities help relieve excessive anxiety and anxiety. Physical exercise releases endorphins, the happy hormone. And what seems absolutely terrible to you, perhaps after a run, will no longer be so scary. But you need to know the measure in sports, so as not to get the opposite effect of overload and stress.
Sports activities help relieve excessive anxiety and anxiety. Physical exercise releases endorphins, the happy hormone. And what seems absolutely terrible to you, perhaps after a run, will no longer be so scary. But you need to know the measure in sports, so as not to get the opposite effect of overload and stress.
It is important to keep a regular schedule. Mood instability and self-doubt create inner chaos. And the schedule of food, sleep, exercise will make the world more stable and predictable.”
In case of severe mental pain, it is necessary to distract yourself, switch your attention to watching a movie, socializing, shopping - that is, to do everything to change painful emotions with the help of events. Sometimes you need to give yourself a break or take a little vacation.
If you are in a serious crisis, have suicidal thoughts, you can put your hands down and wash yourself with cold water, and then try to focus on what you see: describe objects and their shape to switch focus. Then - perform breathing exercises: inhale for three counts and exhale for five counts. After a couple of minutes of such breathing, you need to try to approach the problem again and try to think in a constructive way. Start analyzing your behavior: understand what event provoked pain and destructive behavior, what emotions and thoughts arose. Try to imagine what the consequences of your different behaviors in this situation will be.
Then - perform breathing exercises: inhale for three counts and exhale for five counts. After a couple of minutes of such breathing, you need to try to approach the problem again and try to think in a constructive way. Start analyzing your behavior: understand what event provoked pain and destructive behavior, what emotions and thoughts arose. Try to imagine what the consequences of your different behaviors in this situation will be.
It is worth learning to tell yourself:
Stop! Step back. Inhale-exhale.
What happened is not yet a catastrophe: it's just a specific situation.
I can do it! I can handle! I will survive! I can!
I am not you. I have my own interests, needs, values.
This person is not only bad and not only good, he can be different, and I can be different.
I can take it!
I accept myself.
I will take care of myself, I will do something nice for myself.
My life is worth living!
"Pill against borderline"
There is no consensus on the medical treatment of BPD.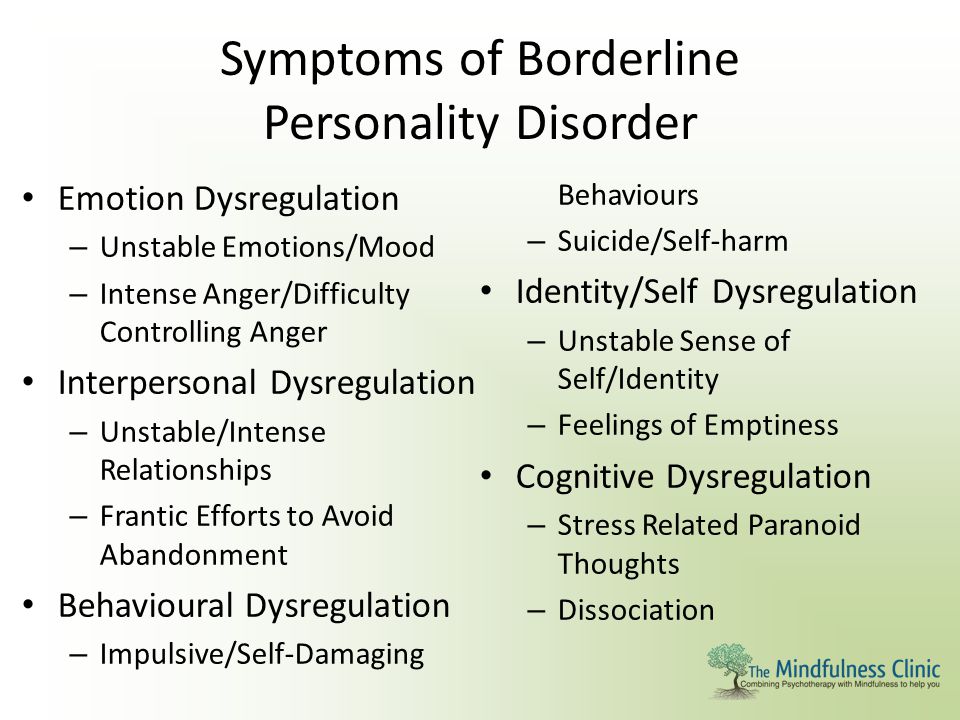 There are no “BPD pills” (like lithium for bipolar disorder or antidepressants for depression, for example). But BPD rarely comes alone. There is evidence that in 85% of cases, patients also have other disorders. Most often, these are different types of anxiety disorders, including post-traumatic (probably severe trauma and "starts" the development of BPD), panic attacks, addictions, anorexia and bulimia, obsessive-compulsive disorder, dissociative disorder.
There are no “BPD pills” (like lithium for bipolar disorder or antidepressants for depression, for example). But BPD rarely comes alone. There is evidence that in 85% of cases, patients also have other disorders. Most often, these are different types of anxiety disorders, including post-traumatic (probably severe trauma and "starts" the development of BPD), panic attacks, addictions, anorexia and bulimia, obsessive-compulsive disorder, dissociative disorder.
Anxiety, depression, irritability, attacks of aggression and suspicion, mood swings and short-term psychotic episodes can be treated with traditional medicines, so that part of the unpleasant symptoms can be eliminated relatively quickly.
BPD patients often end up in a psychiatric hospital, usually after a suicide attempt. There they are treated primarily with medication to help them survive the most difficult period. A patient on medication should strictly follow the doctor's recommendations: do not prescribe or cancel drugs on their own and do not change the dosage without consulting a doctor.
Blogger Ksenia Ivanenko: “The easiest way to get psychiatric help is to contact the PND or outpatient departments at hospitals (when anyone in need can sign up for a consultation with a doctor of their choice). You can also consult a psychiatrist privately. For free hospitalization in most state psychiatric hospitals, you must first contact the PND, get a referral, come to the hospital for a commission, go through it, wait for the doctors' decision. You can go to a public hospital on a paid basis, but even in this case, there may be queues and you have to wait until a place appears in the right department.”
How to understand that you need the help of a psychiatrist and other methods you can not cope with BPD?
Anna Ushkalova, psychiatrist: If you often feel uncontrollable anxiety, excitement, your emotional state is constantly deteriorating, the desire to harm yourself increases, suicidal thoughts appear, something strange seems or sees you, be sure to contact a psychiatrist.
How effective are medications in treating BPD?
A.U.: Although psychotherapy is the mainstay of treatment for BPD, medications can significantly improve well-being. They reduce the severity of emotional fluctuations, depression, manifestations of impulsivity, aggression and auto-aggression.
Is hospitalization necessary and in what cases?
A.U.: The need for hospitalization arises in case of suicidal intent, life-threatening or health-threatening behavior. Hospitalization may also be indicated for psychotic symptoms.
It must be remembered that drugs will not help in solving the specific problems of "border guards", such as violation of self-identification, emotional chaos, fear of loneliness, weak self-control. Psychotherapy has proved its effectiveness here.
What to do if a person close to you is a “border guard”?
Anastasia Umanskaya: “People with BPD are usually described as 'difficult', 'manipulative', 'demanding' and 'requiring too much attention'.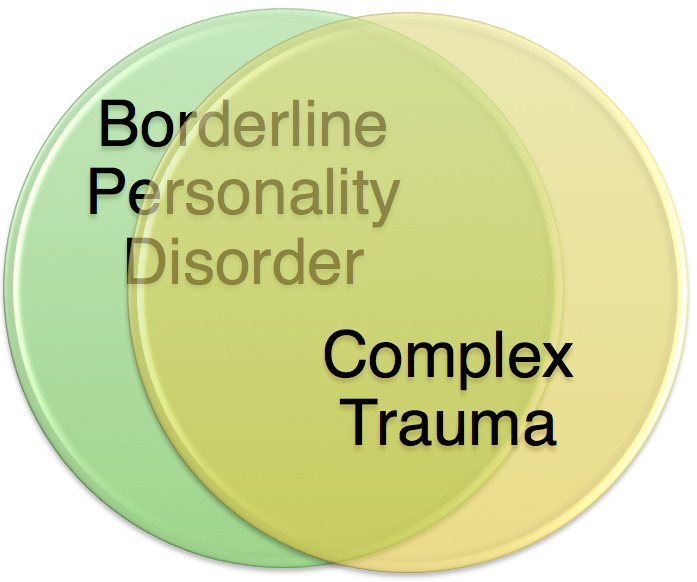 They get angry at their relatives and move away from them, they do not know how to manage destructive emotions and withstand difficulties. So the family of a person with BPD often feels emotional stress and even hostility.
They get angry at their relatives and move away from them, they do not know how to manage destructive emotions and withstand difficulties. So the family of a person with BPD often feels emotional stress and even hostility.
In romantic relationships, people with BPD also tend to create chaos, stress, and conflict. Often they are chronically dissatisfied with their partner. Such features can undermine relationships with family members, friends, colleagues.
Despite all this, constructive relationships are possible. They are more likely with a stable partner who is able to withstand the emotional outbursts of the "border guard" and peacefully respond to them without breaking off the relationship. And it’s good if he has patience and the ability to soften mood swings.
1. If your partner suffers from borderline disorder, it is important that you create a safe environment at home with clear boundaries of what is and is not acceptable and an understandable distance between you. Your loved one is very important clarity, consistency and predictability of your behavior.
Your loved one is very important clarity, consistency and predictability of your behavior.
2. Be aware of the cycles of devaluation-idealization: adoration can quickly turn into hatred, and vice versa, so do not take emotional outbursts as true attitude towards you.
3. Always take seriously the BPD sufferer's threats to harm or commit suicide. This is not manipulation, he really can do this.
4. It is important not to discount the feelings of a person with BPD, even if those close to them do not understand at all what is happening. The feelings that he experiences are the most real, and it is important for him that they be recognized.
5. Don't forget to take care of yourself: get enough sleep, eat on time, rest. Organize support for yourself and don't focus on a partner who can take all of your time. Communicate with friends who understand you, relax alone. Maybe see a therapist."
With adequate treatment, the prognosis for the "border guard" looks quite optimistic: there are chances of a complete cure (as doctors say, "achieve a long-term remission").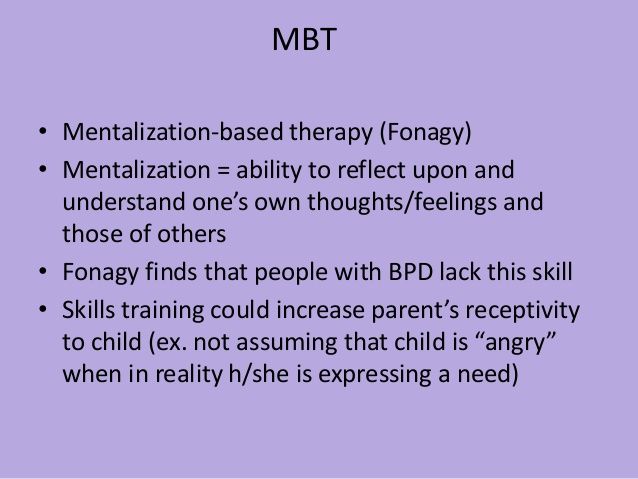
Studies show that after six years of therapy, seventy percent of patients have eliminated their main symptoms. After two years of treatment, remission occurred in a third of patients, after four years - in almost half. Only in six percent of patients the disease returned again after remission.
Useful resources about BPD
In 2017, the first Russian Resource Center was opened - an information portal for people suffering from borderline personality disorder, created on the basis of the experience of colleagues from the USA and Australia.
At the Center for Cognitive Behavioral Therapy, you can sign up for practical training on coping with stress and controlling emotions.
Russia's first community of dialectical behavior therapy (DBT).
Psychology Today Magazine: Borderline Personality Disorder
The largest English-language resource on BPD
BPD section at mind. org.uk
org.uk
A book about BPD written in plain language: I. Yu. Mlodik “House of Cards. Psychotherapeutic assistance to clients with borderline disorder”
Social networks:
Borderline personality disorder. Resource Center
VKontakte / Facebook
Psychotherapy for borderline personality disorders
VKontakte I / Vkontakte II
Research and articles about BPD
Facebook I / Facebook II
Patient communication groups
VKontakte / Facebook
+ Stories of people with BPD
Read also
On the verge: how to live with borderline personality disorder
Masha Pushkina, Ekaterina Tarasova, Alena Belyakova
What is borderline personality disorder, what are its causes, how to live with BPD and how to build a relationship with a “border guard”
Text
Masha Pushkina
Moscow
Text
Ekaterina Tarasova
Nizhny Novgorod
Illustrations
Alena Belyakova
Moscow
Add a comment
comments powered by HyperComments
{{{description}}}}
diagnostics and therapy //Psychological newspaper
The first of a series of VEIP open webinars dedicated to working with borderline patients, "Clinic, diagnosis, etiology and pathogenesis of borderline personality disorder" . Host: Olga Gamayunova.
Host: Olga Gamayunova.
“Borderline patients are considered very difficult to work with. I want to talk about the specifics that cause very intense countertransference experiences in therapists (not only psychoanalysts). And these experiences can be very difficult to cope with, and this is just one of our main tasks - to cope with them and help our patients cope with feelings. With the most powerful, most intense affects. In the case of borderline patients, this comes to the fore.
I suppose that today we will talk about borderline patients as a nosological category, we will try to understand how ideas about these patients appeared, starting with Z. Freud, and what we have today. Let's talk about the clinical picture, that is, about what we observe in the office when the patient comes, what we hear in his stories, what we must be attentive to in order to understand whether the patient is borderline in front of us, neurotic or psychotic, how we conduct differential diagnosis.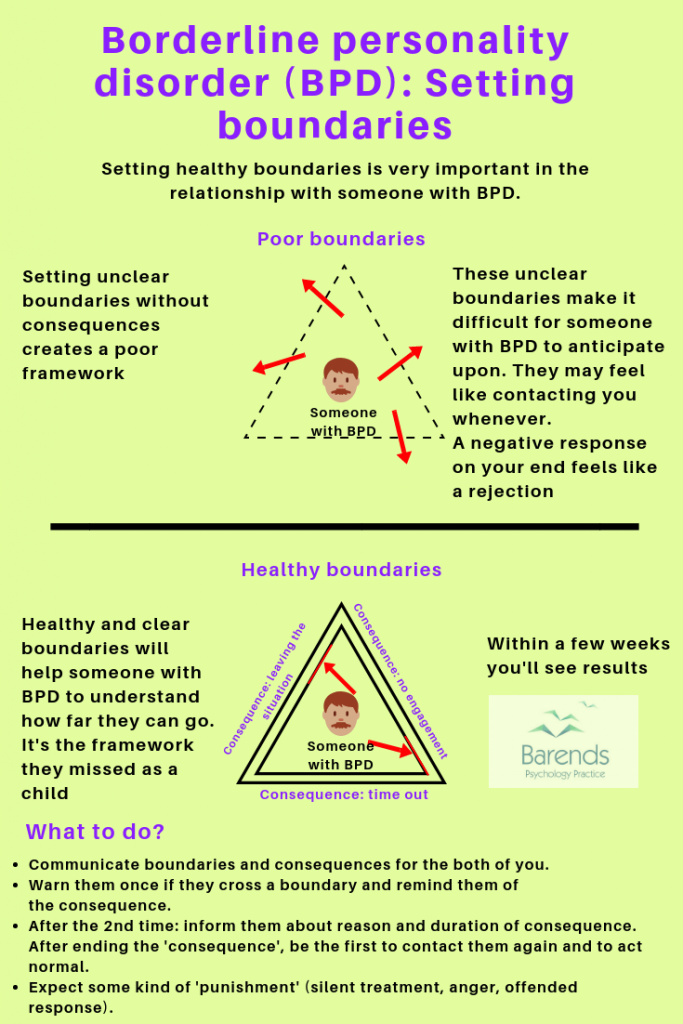 You and I already know that on the basis of our conclusion about the psychoanalytic diagnosis, we are building a further work strategy. We work with neurotics in such a classical psychoanalytic manner, in the form of interpretive psychoanalytic therapy, with borderline patients - in expressive therapy, with psychotic patients - in the format of supportive therapy. They are quite different from each other and an important professional task is to determine at the first meetings which form of psychotherapy suits this particular person the most and can help the most.
You and I already know that on the basis of our conclusion about the psychoanalytic diagnosis, we are building a further work strategy. We work with neurotics in such a classical psychoanalytic manner, in the form of interpretive psychoanalytic therapy, with borderline patients - in expressive therapy, with psychotic patients - in the format of supportive therapy. They are quite different from each other and an important professional task is to determine at the first meetings which form of psychotherapy suits this particular person the most and can help the most.
Next time I would like us to talk about the two main forms of psychoanalytic work with borderline patients that exist today, namely, the transference-oriented therapy proposed by Otto Kernberg, and the second form, relatively recently available to Russian analysts - psychoanalytic psychotherapy based on mentalization (developed by Peter Fonagy).
I would like to devote the third webinar to the views of analytical psychologists, that is, Jungian analysts, on the borderline personality. This view, in my opinion, is extremely interesting, very extraordinary and at the same time opens up additional possibilities. It may not be suitable for someone, but for someone it will turn out to be the very therapeutic professional Grail that will allow you to be as effective as possible in working with these difficult patients.
This view, in my opinion, is extremely interesting, very extraordinary and at the same time opens up additional possibilities. It may not be suitable for someone, but for someone it will turn out to be the very therapeutic professional Grail that will allow you to be as effective as possible in working with these difficult patients.
And I would like to devote the fourth webinar to the views of French analysts on the border structure, namely, the views of Andre Green. Unfortunately, in Russian there is an official translation of only one chapter from his book "Private Madness". The chapter is published in the collection "Lessons of French Psychoanalysis" and is called "Dead Mother". Unfortunately, the remaining chapters have not yet been translated into Russian, so I believe that for those who do not yet read fluently in English and French, Green's concepts in my presentation could be interesting and useful ...
Today we will talk about who we plan to work with and what our therapeutic goals are.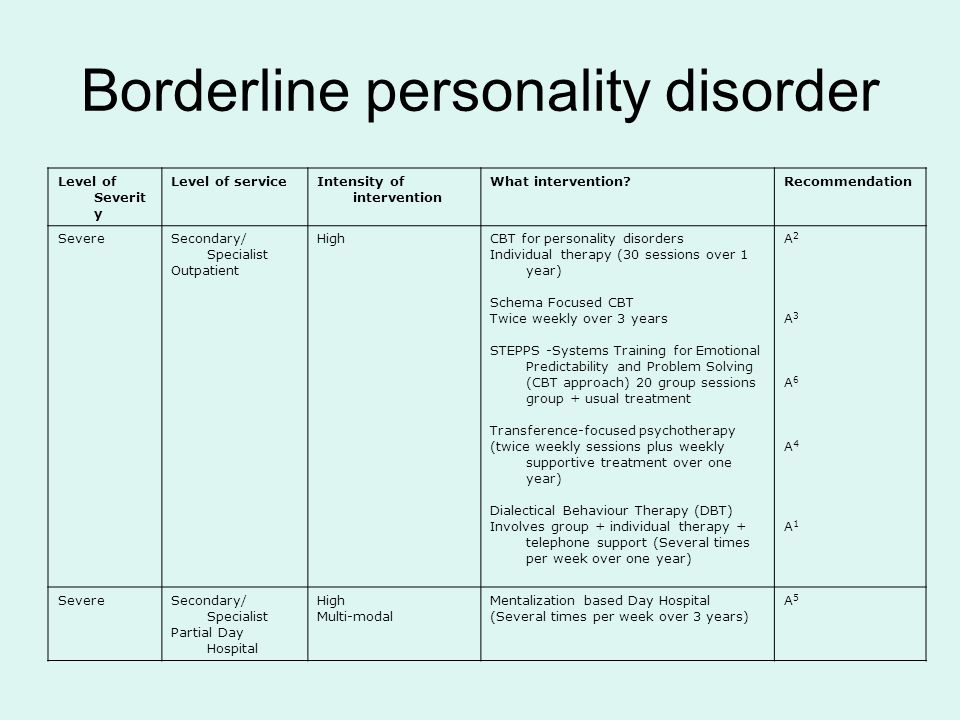 I would like to start with a statement by the ancient Jewish philosopher Hillel. He said: “If I am not for myself, then who is for me? And if I am only for myself, then who am I? If we try to develop this maxim, we can come up with very interesting ideas about what mental health is. We know that there is no such category in classical psychoanalysis. Freud said that we strive for it as some kind of ideal, but still remain neurotic. Modern psychoanalysts see it somewhat differently. Mental health is, first of all, the ability to give yourself what you need. With this ability, all the people who come to us have great difficulties. In borderline patients, the ability to give to oneself what is needed, to satisfy one's own needs and desires, is practically absent. The borderline patient is in dire need of someone who would perform these functions for him. The neurotic patient is somewhat capable of this, but is usually limited in this ability, and Freud, in his later writings, gave us the reason why a person who realizes in the process of psychoanalysis that his restrictions on self-satisfaction are, in fact, illusory, not corresponding to reality, yet continues to impose these restrictions on itself.
I would like to start with a statement by the ancient Jewish philosopher Hillel. He said: “If I am not for myself, then who is for me? And if I am only for myself, then who am I? If we try to develop this maxim, we can come up with very interesting ideas about what mental health is. We know that there is no such category in classical psychoanalysis. Freud said that we strive for it as some kind of ideal, but still remain neurotic. Modern psychoanalysts see it somewhat differently. Mental health is, first of all, the ability to give yourself what you need. With this ability, all the people who come to us have great difficulties. In borderline patients, the ability to give to oneself what is needed, to satisfy one's own needs and desires, is practically absent. The borderline patient is in dire need of someone who would perform these functions for him. The neurotic patient is somewhat capable of this, but is usually limited in this ability, and Freud, in his later writings, gave us the reason why a person who realizes in the process of psychoanalysis that his restrictions on self-satisfaction are, in fact, illusory, not corresponding to reality, yet continues to impose these restrictions on itself. It seems that there is such a phenomenon as an unconscious feeling of guilt for one's own life, for one's desires, for getting pleasure. Neurotic patients, as a result of this feeling of guilt, which finds its expression in neurotic conflict, are limited in this ability to give themselves what they need. But still, they can do it to some extent. Borderline patients are practically unable to do this for themselves.
It seems that there is such a phenomenon as an unconscious feeling of guilt for one's own life, for one's desires, for getting pleasure. Neurotic patients, as a result of this feeling of guilt, which finds its expression in neurotic conflict, are limited in this ability to give themselves what they need. But still, they can do it to some extent. Borderline patients are practically unable to do this for themselves.
The second point that follows from this maxim about mental health is the ability to give others what they need. In neurotic patients, the ability to give to others is expressed, rather, excessively - they are able to give something to others to the detriment of themselves. One of the focuses of our work is to harmonize this imbalance so that a person can give to others without hurting himself. It is also very difficult for borderline patients with this ability - they practically cannot give anything to others, because they have their own most intense deficit. Mental health is also the ability to take from others what you need and what they give, or finding others who will give you what you need. In neurotic patients this search is usually limited. They believe that they should take everything that is offered to them, even if they do not need something, or are not ready to take anything at all. And this distortion is often based on an unconscious sense of guilt - neurotic patients believe that they infringe, deprive, harm other people if they ask or take something from them. Relatively recently, it was a behavioral norm when a mother told her child: “Good girls don’t take sweets, even if they really want to and they are offered sweets.” And this impossibility to take, because you are either ashamed or feel guilty, just limits the neurotic patient in getting what he needs from the world.
In neurotic patients this search is usually limited. They believe that they should take everything that is offered to them, even if they do not need something, or are not ready to take anything at all. And this distortion is often based on an unconscious sense of guilt - neurotic patients believe that they infringe, deprive, harm other people if they ask or take something from them. Relatively recently, it was a behavioral norm when a mother told her child: “Good girls don’t take sweets, even if they really want to and they are offered sweets.” And this impossibility to take, because you are either ashamed or feel guilty, just limits the neurotic patient in getting what he needs from the world.
The borderline patient also has this incapacity, but the reasons for it are different. In borderline patients (according to M. Klein and her followers) there is an archaic greed. Borderline patients really want to take, they really want to take everything, but at the same time it turns out to be very problematic to take, because this is given at an unconscious level is perceived as something bad - something that poisons, leads to death or plunges into such dependence on others that leads to absorption by another man, to the loss of himself.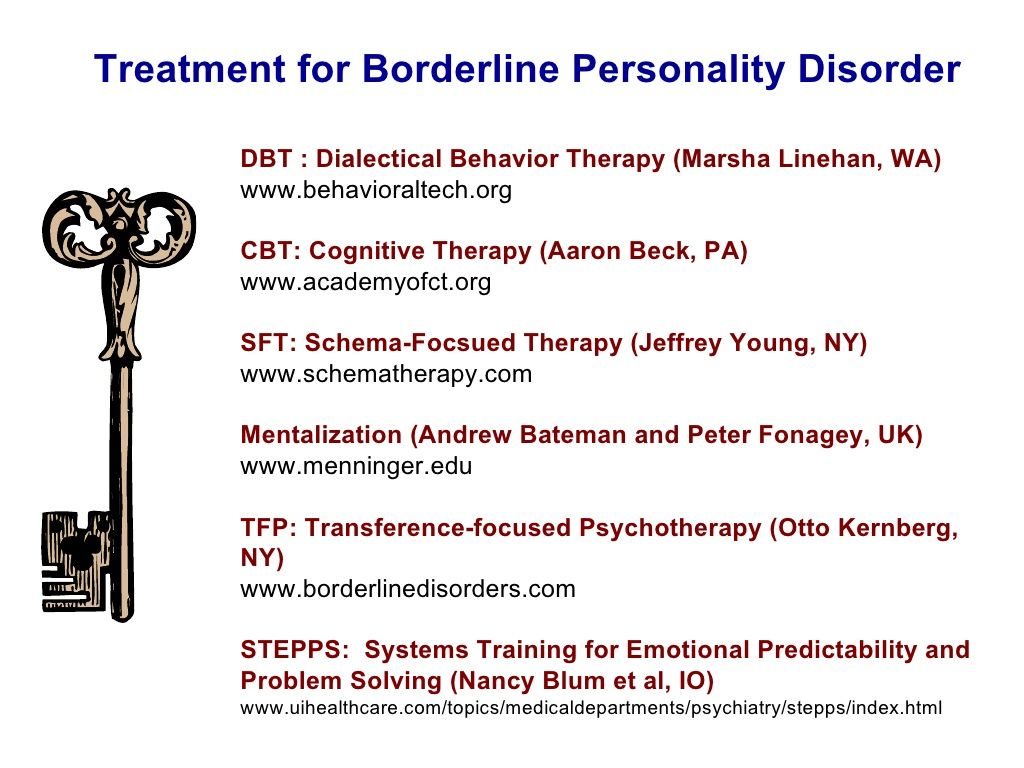 What the world offers them turns out to be either not right, or not then, or not in the amount they need, or too little, or too much. And all this, of course, significantly complicates the work of the analyst, since in a certain sense psychotherapy is analogous to feeding. We give something to our patients, interpretations, for example, understanding, processed affects, and it is extremely difficult for borderline patients to accept this from us. Intense experiences arise both in them, and in the countertransference in response, very strong experiences arise in us ... ”:
What the world offers them turns out to be either not right, or not then, or not in the amount they need, or too little, or too much. And all this, of course, significantly complicates the work of the analyst, since in a certain sense psychotherapy is analogous to feeding. We give something to our patients, interpretations, for example, understanding, processed affects, and it is extremely difficult for borderline patients to accept this from us. Intense experiences arise both in them, and in the countertransference in response, very strong experiences arise in us ... ”:
A series of open webinars on the borderline personality on the channel of the East European Institute of Psychoanalysis: March 23 "Clinic, diagnosis, etiology and pathogenesis of borderline personality disorder", March 28 "Psychoanalytic therapy of the borderline personality: transfer-oriented therapy (O.