Symptoms of ocpd
Obsessive-compulsive personality disorder: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus.gov/ency/article/000942.htm
To use the sharing features on this page, please enable JavaScript.
Obsessive-compulsive personality disorder (OCPD) is a mental condition in which a person is preoccupied with:
- Rules
- Orderliness
- Control
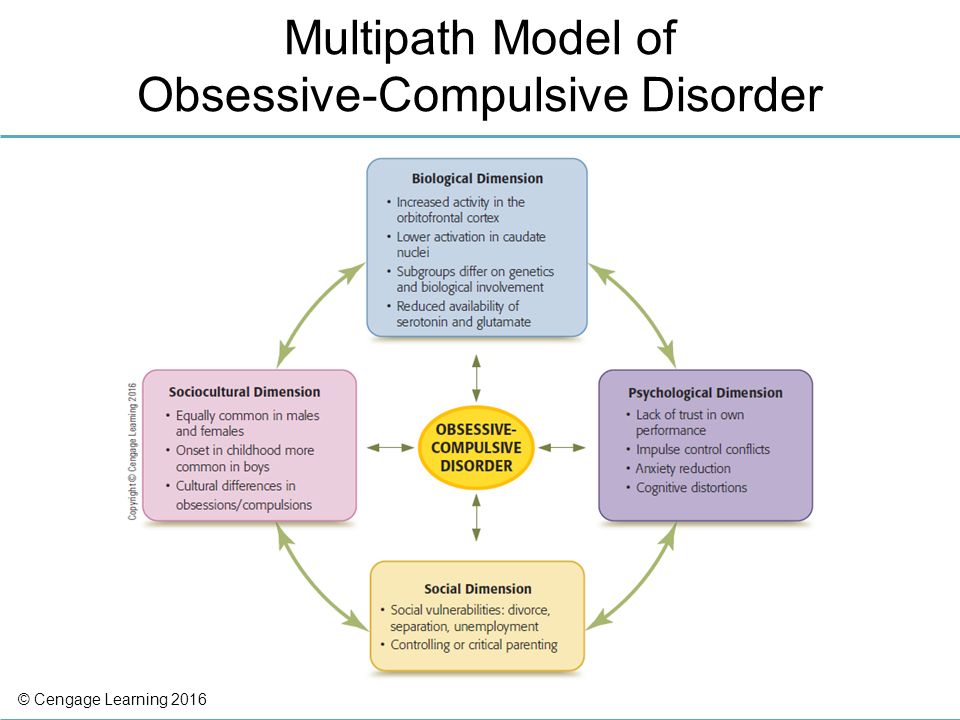
OCPD tends to occur in families, so genes may be involved. A person's childhood and environment may also play roles.
This disorder can affect both men and women. It occurs most often in men.
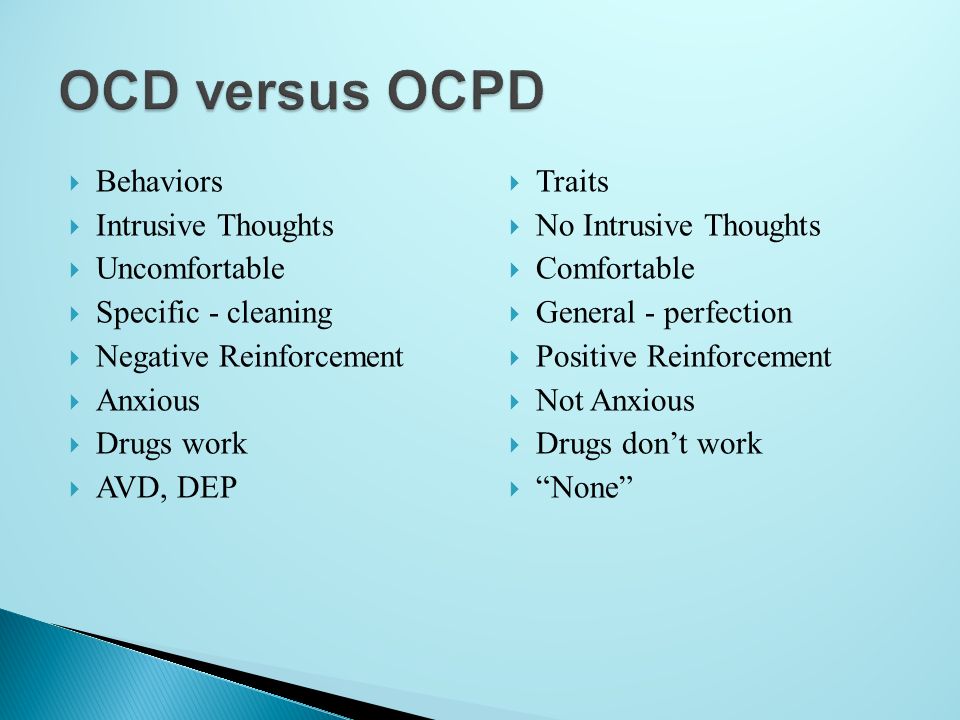
OCPD has some of the same symptoms as obsessive-compulsive disorder (OCD). People with OCD have unwanted thoughts, while people with OCPD believe that their thoughts are correct. In addition, OCD often begins in childhood while OCPD usually starts in the teen years or early 20s.
People with either OCPD or OCD are high achievers and feel a sense of urgency about their actions. They may become very upset if other people interfere with their rigid routines. They may not be able to express their anger directly. People with OCPD have feelings that they consider more appropriate, like anxiety or frustration.
A person with OCPD has symptoms of perfectionism that usually begin by early adulthood. This perfectionism may interfere with the person's ability to complete tasks because their standards are so rigid. They may withdraw emotionally when they are not able to control a situation. This can interfere with their ability to solve problems and form close relationships.
Other signs of OCPD include:
- Over-devotion to work
- Not being able to throw things away, even when the objects have no value
- Lack of flexibility
- Lack of generosity
- Not wanting to allow other people to do things
- Not willing to show affection
- Preoccupation with details, rules, and lists
OCPD is diagnosed based on a psychological evaluation. The health care provider will consider how long and how severe the person's symptoms are.
The health care provider will consider how long and how severe the person's symptoms are.
Medicines may help reduce anxiety and depression from OCPD. Talk therapy is thought to be the most effective treatment for OCPD. In some cases, medicines combined with talk therapy is more effective than either treatment alone.
Outlook for OCPD tends to be better than that for other personality disorders. The rigidness and control of OCPD may prevent many of the complications, such as substance use, which are common in other personality disorders.
The social isolation and difficulty handling anger that are common with OCPD may lead to depression and anxiety later in life.
Complications may include:
- Anxiety
- Depression
- Difficulty moving forward in career situations
- Relationship difficulties
See your provider or mental health professional if you or someone you know has symptoms of OCPD.
Personality disorder - obsessive-compulsive; OCPD
American Psychiatric Association. Obsessive-compulsive personality disorder. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013:678-682.
Obsessive-compulsive personality disorder. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013:678-682.
Blais MA, Smallwood P, Groves JE, Rivas-Vazquez RA, Hopwood CJ. Personality and personality disorders. In: Stern TA, Fava M, Wilens TE, Rosenbaum JF, eds. Massachusetts General Hospital Comprehensive Clinical Psychiatry. 2nd ed. Philadelphia, PA: Elsevier; 2016:chap 39.
Gordon OM, Salkovskis PM, Oldfield VB, Carter N. The association between obsessive compulsive disorder and obsessive compulsive personality disorder: prevalence and clinical presentation. Br J Clin Psychol. 2013;52(3):300-315. PMID: 23865406 pubmed.ncbi.nlm.nih.gov/23865406/.
Updated by: Fred K. Berger, MD, addiction and forensic psychiatrist, Scripps Memorial Hospital, La Jolla, CA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Obsessive-Compulsive Personality Disorder (OCPD) - Psychiatric Disorders
By
Mark Zimmerman
, MD, Rhode Island Hospital
Medically Reviewed May 2021 | Modified Sep 2022
View Patient Education
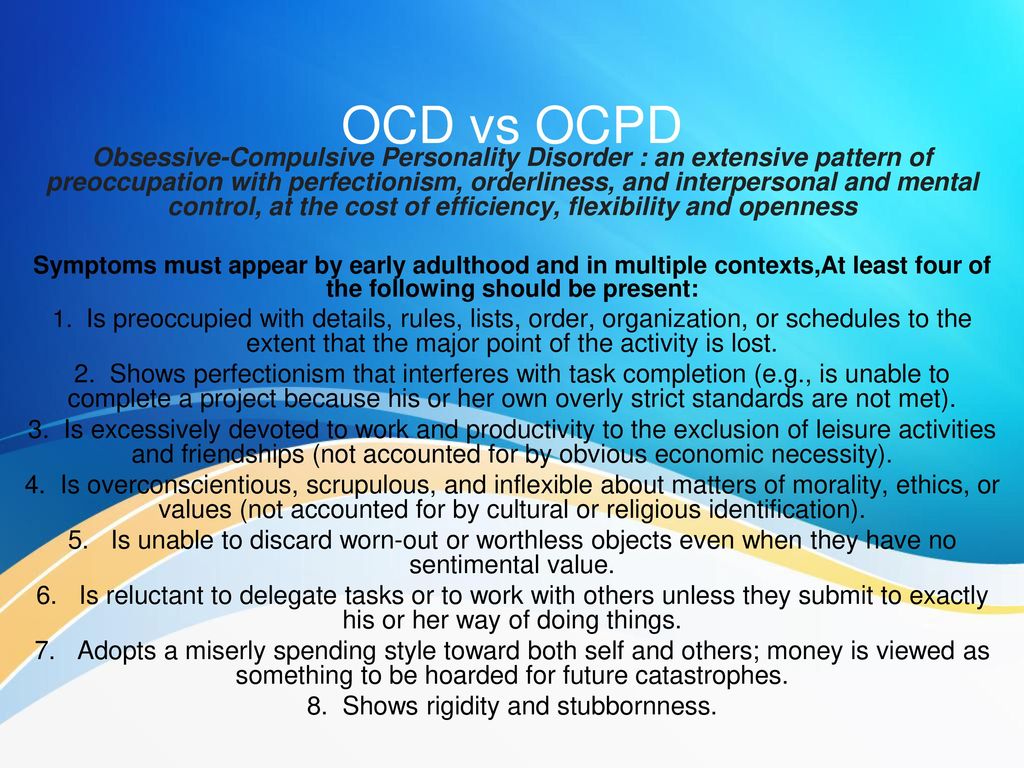
Obsessive-compulsive personality disorder is characterized by a pervasive preoccupation with orderliness, perfectionism, and control (with no room for flexibility) that ultimately slows or interferes with completing a task. Diagnosis is by clinical criteria. Treatment is with psychodynamic psychotherapy, cognitive-behavioral therapy, and selective serotonin reuptake inhibitors (SSRIs).
(See also Overview of Personality Disorders Overview of Personality Disorders Personality disorders in general are pervasive, enduring patterns of thinking, perceiving, reacting, and relating that cause significant distress or functional impairment. Personality disorders... read more .)
Personality disorders... read more .)
Because patients with obsessive-compulsive personality disorder need to be in control, they tend to be solitary in their endeavors and to mistrust the help of others.
About 2.1 to 7.9% of the general population are estimated to have obsessive-compulsive personality disorder; it is more common among men.
Familial traits of compulsivity, restricted range of emotion, and perfectionism are thought to contribute to this disorder.
Comorbidities may be present. Patients often also have a depressive disorder Depressive Disorders Depressive disorders are characterized by sadness severe enough or persistent enough to interfere with function and often by decreased interest or pleasure in activities. Exact cause is unknown... read more (major depressive disorder or persistent depressive disorder) or an alcohol use disorder Alcohol Toxicity and Withdrawal Alcohol (ethanol) is a central nervous system depressant. Large amounts consumed rapidly can cause respiratory depression, coma, and death. Large amounts chronically consumed damage the liver... read more .
Large amounts consumed rapidly can cause respiratory depression, coma, and death. Large amounts chronically consumed damage the liver... read more .
Symptoms of obsessive-compulsive personality disorder may lessen even over a time period as short as 1 year, but their persistence (ie, remission and relapse rates) during the long term are less clear.
In patients with obsessive-compulsive personality disorder, preoccupation with order, perfectionism, and control of themselves and situations interferes with flexibility, effectiveness, and openness. Rigid and stubborn in their activities, these patients insist that everything be done in specific ways.
To maintain a sense of control, patients focus on rules, minute details, procedures, schedules, and lists. As a result, the main point of a project or activity is lost. These patients repeatedly check for mistakes and pay extraordinary attention to detail. They do not make good use of their time, often leaving the most important tasks until the end. Their preoccupation with the details and making sure everything is perfect can endlessly delay completion. They are unaware of how their behavior affects their coworkers. When focused on one task, these patients may neglect all other aspects of their life.
Their preoccupation with the details and making sure everything is perfect can endlessly delay completion. They are unaware of how their behavior affects their coworkers. When focused on one task, these patients may neglect all other aspects of their life.
Because these patients want everything done in a specific way, they have difficulty delegating tasks and working with others. When working with others, they may make detailed lists about how a task should be done and become upset if a coworker suggests an alternative way. They may reject help even when they are behind schedule.
Patients with obsessive-compulsive personality disorder are excessively dedicated to work and productivity; their dedication is not motivated by financial necessity. As a result, leisure activities and relationships are neglected. They may think they have no time to relax or go out with friends; they may postpone a vacation so long that it does not happen, or they may feel they must take work with them so that they do not waste time. Time spent with friends, when it occurs, tends to be in a formally organized activity (eg, a sport). Hobbies and recreational activities are considered important tasks requiring organization and hard work to master; the goal is perfection.
Time spent with friends, when it occurs, tends to be in a formally organized activity (eg, a sport). Hobbies and recreational activities are considered important tasks requiring organization and hard work to master; the goal is perfection.
These patients plan ahead in great detail and do not wish to consider changes. Their relentless rigidity may frustrate coworkers and friends.
Expression of affection is also tightly controlled. These patients may relate to others in a formal, stiff, or serious way. Often, they speak only after they think of the perfect thing to say. They may focus on logic and intellect and be intolerant of emotional or expressive behavior.
These patients may be overzealous, picky, and rigid about issues of morality, ethics, and values. They apply rigid moral principles to themselves and to others and are harshly self-critical. They are rigidly deferential to authorities and insist on exact compliance to rules, with no exceptions for extenuating circumstances.
For a diagnosis of obsessive-compulsive personality disorder, patients must have
This pattern is shown by the presence of ≥ 4 of the following:
Preoccupation with details, rules, schedules, organization, and lists
A striving to do something perfectly that interferes with completion of the task
Excessive devotion to work and productivity (not due to financial necessity), resulting in neglect of leisure activities and friends
Excessive conscientiousness, fastidiousness, and inflexibility regarding ethical and moral issues and values
Unwillingness to throw out worn-out or worthless objects, even those with no sentimental value
Reluctance to delegate or work with other people unless those people agree to do things exactly as the patients want
A miserly approach to spending for themselves and others because they see money as something to be saved for future disasters
Rigidity and stubbornness
Also, symptoms must have begun by early adulthood.
Obsessive-compulsive personality disorder should be distinguished from the following disorders:
Obsessive-compulsive disorder (OCD) Obsessive-Compulsive Disorder (OCD) Obsessive-compulsive disorder (OCD) is characterized by recurrent, persistent, unwanted, and intrusive thoughts, urges, or images (obsessions) and/or by repetitive behaviors or mental acts that... read more : Patients with OCD have true obsessions (repetitive, unwanted, intrusive thoughts that cause marked anxiety) and compulsions (ritualistic behaviors that they feel they must do to reduce their anxiety-related obsessions). Patients with OCD are often distressed by their lack of control over compulsive drives; in patients with obsessive-compulsive personality disorder, the need for control is driven by their preoccupation with order so their behavior, values, and feelings are acceptable and consistent with their sense of self.
Avoidant personality disorder Avoidant Personality Disorder (AVPD) Avoidant personality disorder is characterized by the avoidance of social situations or interactions that involve risk of rejection, criticism, or humiliation.
 Diagnosis is by clinical criteria... read more : Both avoidant and obsessive-compulsive personality disorders are characterized by social isolation; however, in patients with obsessive-compulsive personality disorder, isolation results from giving priority to work and productivity rather than relationships, and these patients mistrust others only because of their potential to intrude on the patients' perfectionism.
Diagnosis is by clinical criteria... read more : Both avoidant and obsessive-compulsive personality disorders are characterized by social isolation; however, in patients with obsessive-compulsive personality disorder, isolation results from giving priority to work and productivity rather than relationships, and these patients mistrust others only because of their potential to intrude on the patients' perfectionism.Schizoid personality disorder Schizoid Personality Disorder (ScPD) Schizoid personality disorder is characterized by a pervasive pattern of detachment from and general disinterest in social relationships and a limited range of emotions in interpersonal relationships... read more : Both schizoid and obsessive-compulsive personality disorders are characterized by a seeming formality in interpersonal relationships and by detachment. However, the motives are different: a basic incapability for intimacy in patients with schizoid personality disorder vs discomfort with emotions and dedication to work in patients with obsessive-compulsive personality disorder.
Psychodynamic psychotherapy
Cognitive-behavioral therapy
Selective serotonin reuptake inhibitors (SSRIs)
General treatment Treatment Personality disorders in general are pervasive, enduring patterns of thinking, perceiving, reacting, and relating that cause significant distress or functional impairment. Personality disorders... read more of obsessive-compulsive personality disorder is similar to that for all personality disorders.
Information about treatment for obsessive-compulsive personality disorder is sparse. Also, treatment is complicated by the patient's rigidity, obstinacy, and need for control, which can be frustrating for therapists.
Psychodynamic therapy and cognitive-behavioral therapy can help patients with obsessive-compulsive personality disorder. Sometimes during therapy, the patient's interesting, detailed, intellectualized conversation may seem psychologically oriented, but it is void of affect and does not lead to change.
SSRIs Selective Serotonin Reuptake Inhibitors (SSRIs) Several drug classes and drugs can be used to treat depression: Selective serotonin reuptake inhibitors (SSRIs) Serotonin modulators (5-HT2 blockers) Serotonin-norepinephrine reuptake inhibitors... read more may be useful.
NOTE: This is the Professional Version. CONSUMERS: View Consumer VersionCopyright © 2022 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Test your knowledge
Take a Quiz!Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.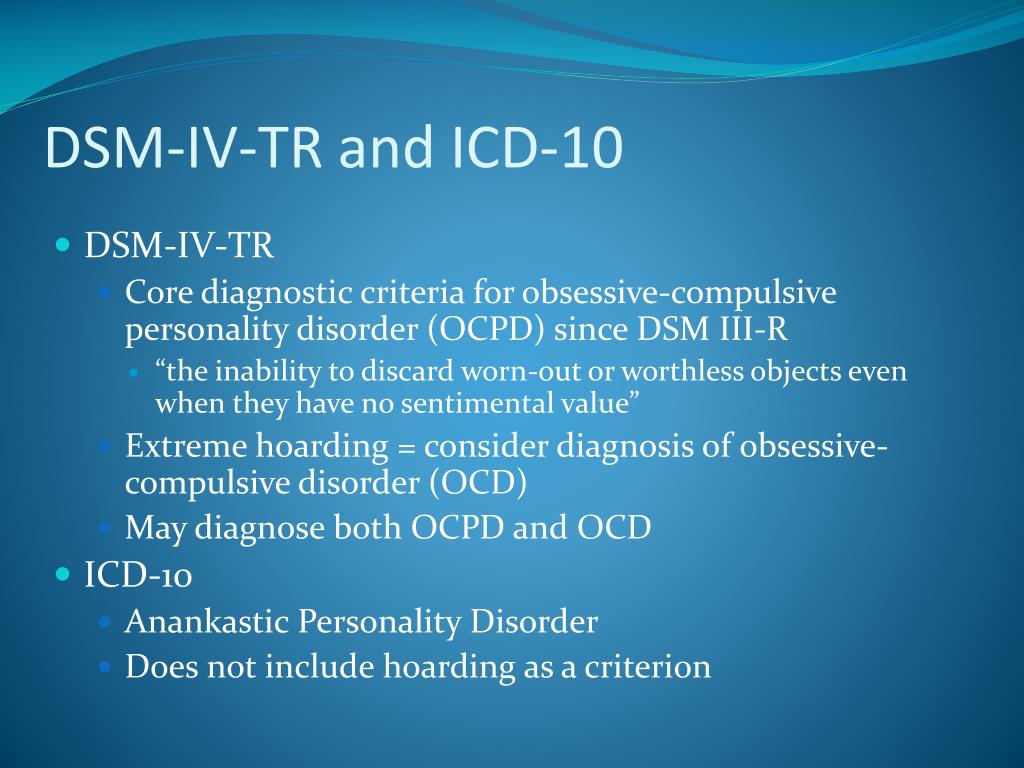
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
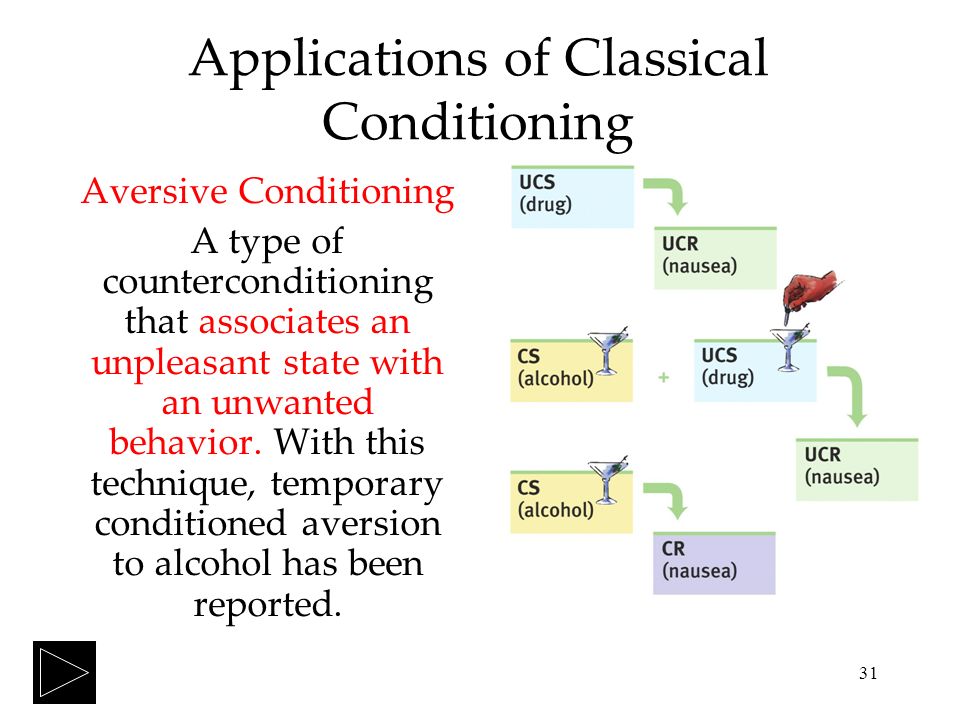
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.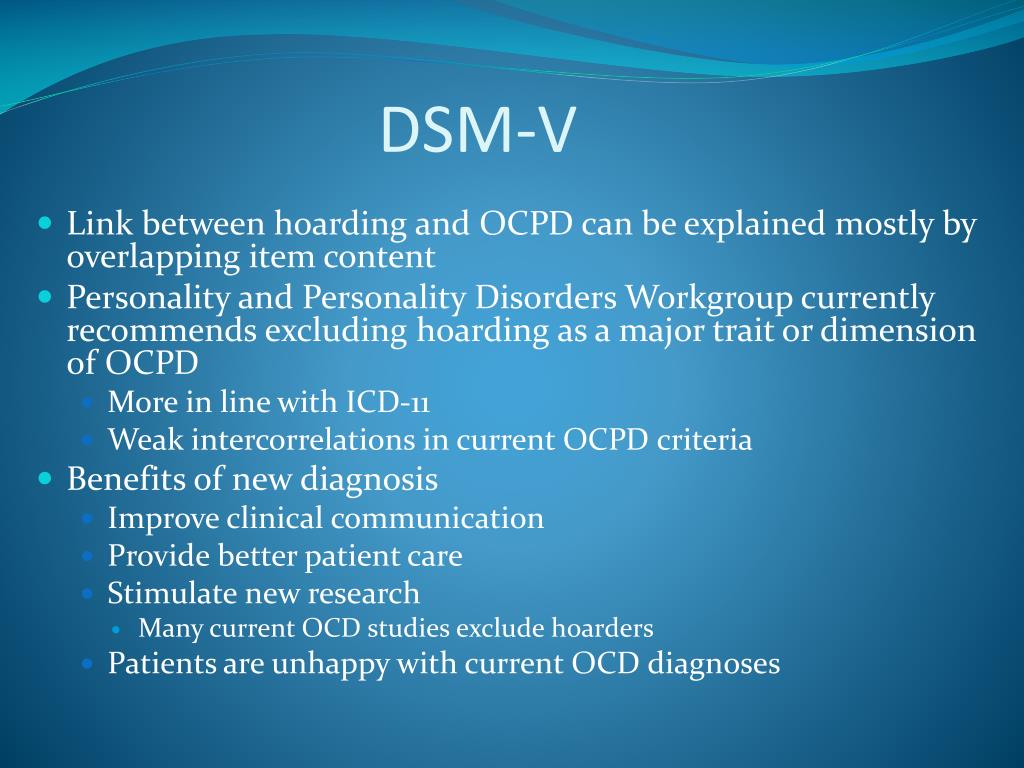
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or contamination
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- Persistent decline in quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, specialists of the Neuro-Psi clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result.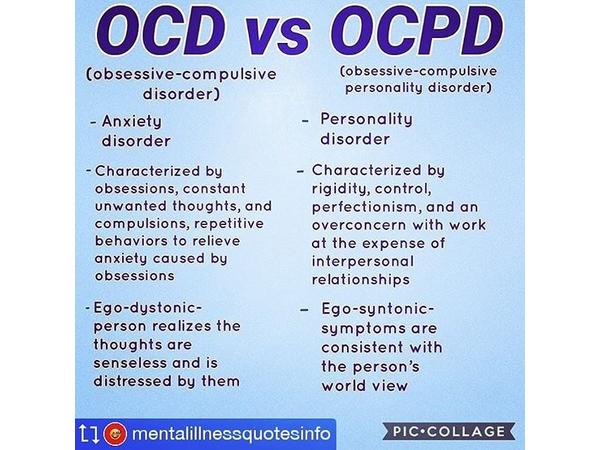 A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future.