Stop intrusive thoughts ocd
How to Take the Power Back from Intrusive Thought
03.22.2017
Debra Kissen, PhD, MHSA
Member Since 2010
Dr. Debra Kissen is CEO of Light On Anxiety CBT Treatment Center. Dr. Kissen specializes in Cognitive Behavioral Therapy (CBT) for anxiety and related disorders. Dr. Kissen is the author of the Panic Workbook for Teens, Rewire Your Anxious Brains for Teens: Using CBT, Neuroscience, and Mindfulness to Help You End Anxiety, Panic, and Worry (The Instant Help Solutions Series) and the soon to be released Break Free from Intrusive Thoughts: An Evidence-Based Guide for Managing Fear and Finding Peace. Dr. Kissen also has a special interest in the principles of mindfulness and their application for anxiety disorders. Dr. Kissen has presented her research on CBT and mindfulness-based treatments for anxiety and related disorders at regional and national conferences. Dr. Kissen is the Co-Chair of the Anxiety and Depression Association of America Public Education Committee.
Dr. Kissen was the recipient of the 2020 Gratitude for Giving Spirit Award and the 2018 Anxiety Depression Association of America Member of Distinction Award.
Dr. Kissen often serves as a media psychologist and is available for press inquiries and strives to further the dissemination of empirically supported treatment (EST) information by offering user friendly quotes and simple to understand, practical tips and solutions to help mental health consumers move past stress and anxiety.
Dr. Kissen and ADAA
"I was lucky enough to do my early practicums under the leadership and guidance of Dr. Karen Cassiday who is now president of ADAA. I learned from Dr. Cassiday that time spent with ADAA is one of the best professional investments that I could make. Through continuing education, professional connections and additional contact with mental health consumers, ADAA is truly my professional home. I have always had a passion for enhancing dissemination of empirically supported treatment protocols to mental health consumers.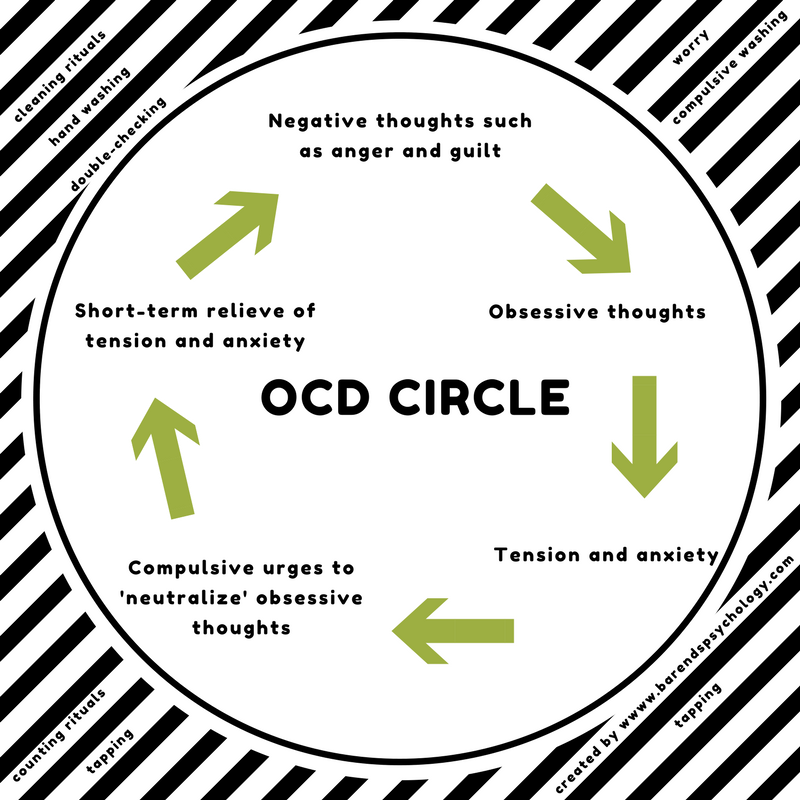 The public education committee offers a wonderful opportunity to create innovative programming to reach mental health consumers where they are, not just in the treatment room. I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
The public education committee offers a wonderful opportunity to create innovative programming to reach mental health consumers where they are, not just in the treatment room. I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
Light on Anxiety CBT Treatment Center
Boost Search Results
On
March 22, 2017
How to Take the Power Back from Intrusive Thought OCD
Step 1: See Through OCD’s Scare Tactics
OCD is the fear network of the brain sending a signal that something is wrong and needs to be done about it IMMEDIATELY. OCD only reports on feared consequences that are important to a person. For example, if somebody does not fear spilling water on the floor, OCD will not send the intrusive thought, “Oh no you spilled water. You must clean it up IMMEDIATELY”. On the other hand if someone does care about the safety of her family, OCD might say, “Oh no you left the stove on. You must go back and check IMMEDIATELY or the most important people in your life will die and it will be all your fault.” Similarly, if you care deeply about your family's well-being or your students safety, OCD may inject itself into your awareness with the thought “Oh no. What if I lose control and harm my children or students.”
You must go back and check IMMEDIATELY or the most important people in your life will die and it will be all your fault.” Similarly, if you care deeply about your family's well-being or your students safety, OCD may inject itself into your awareness with the thought “Oh no. What if I lose control and harm my children or students.”
My clients always ask me what it means about them that they could have such “horrible thoughts”. What I tell them is that somewhere within an obsession is the flip side of a core value. If OCD taunts you with images and thoughts about offending god, then religion must be important to you. If OCD reviews all the ways your family could be hurt, then your family is clearly one of your top priorities.
There is checklist of common intrusive thoughts that I find helpful to share with my patients. There are numerous thoughts on this list regarding losing control and acting out violently or sexually. Several research studies found that when this list is shown to a non-clinical sample of people, approximately 90 percent of those surveyed will agree to having experienced some of the intrusive thoughts.
When the non-clinical sample is asked how bothered they are by experiencing these intrusive thoughts, they are most often only mildly bothered by them. In contrast, when this same list is shown to individuals diagnosed with OCD, a similar percentage of the sample will agree to having experienced these intrusive thoughts but the big difference is how much distress these thoughts evoke for the OCD sample. For those meeting criteria for OCD, there will be a much higher level of emotional distress when these same intrusive thoughts surface.
What keeps OCD alive and well is not the experience of intrusive thoughts but actually one’s reaction to them. The more one dislikes experiencing intrusive thoughts and then tries to repress or fight with these thoughts, the greater the frequency of intrusive thoughts one will experience. The very act of trying to “not have” a bothersome thought guarantees its resurfacing. The only way to know if you are having or not having a thought is to think “Am I think about X” or “I better not think about X” which of course causes one to think about X.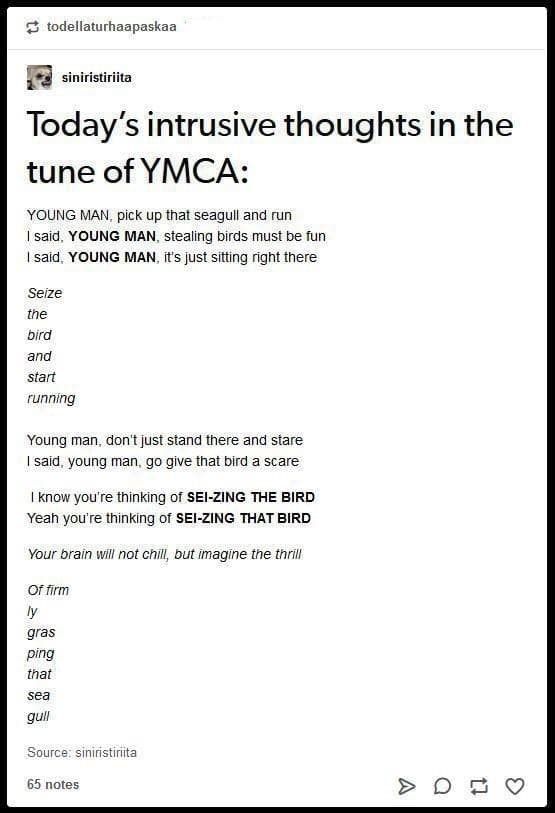
So back to the question of why do those meeting criteria for OCD have such disturbing thoughts? Because they are human and to be human means one will experience freaky, odd thoughts. The human mind is constantly spinning around trying to find interesting problems to solve, in order to keep us alive. We don’t have the speed of the jaguar or the strength of a bear but we do have an all too powerful mind that is very good at planning for future challenges but also for tying itself into a knot. Freedom from OCD is not about stopping the mind from offering up strange and occasionally disturbing thoughts but learning how to recognize spam vs. urgent mail.
I must give a disclaimer here that OCD loves taking anything that is reassuring and turning it into a compulsion. So, if you are reading this blog for the hundredth time and desperately trying to figure out if this sounds like you and if your “awful thoughts” are OCD or if in fact you are an awful person, then STOP reading this blog.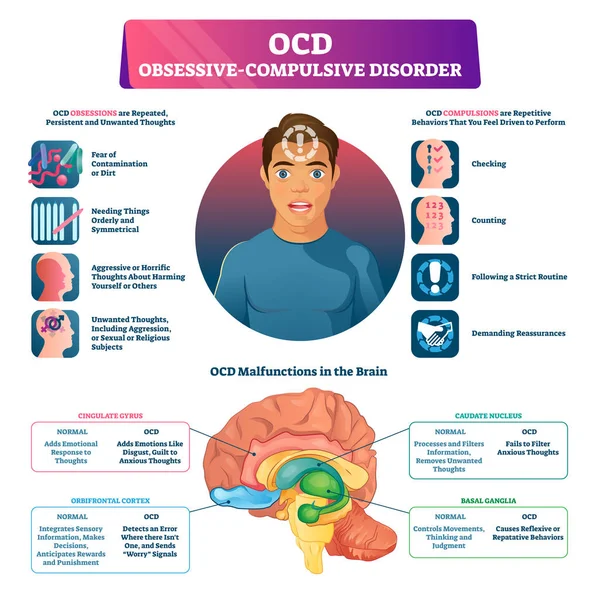 As I am sure your experience has shown you obtaining short-term anxiety relief through a compulsion comes at a cost in the form of greater overall anxiety. Instead, strive for long-term freedom from OCD by teaching your mind to not take itself so seriously.
As I am sure your experience has shown you obtaining short-term anxiety relief through a compulsion comes at a cost in the form of greater overall anxiety. Instead, strive for long-term freedom from OCD by teaching your mind to not take itself so seriously.
Step 2: Exposure and Response Prevention (ERP)
There is no way past OCD except through it. As described in step one, the more one avoids an intrusive thought, the more one will experience the feared, bothersome, super annoying thought. Therefore, we need to flip the equation on its head and practice bringing on the thought while disengaging from any compulsions that have been utilized to obtain short-term anxiety relief. Common compulsions engaged in, when struggling with intrusive thought OCD are reassurance seeking, information seeking/googling to determine if there is something wrong with self, mental reviewing and avoidance. The best way to organize exposure tasks is by creating an exposure hierarchy that outlines baby steps that you can take to slowly but surely prove to OCD who is in charge (hint…YOU).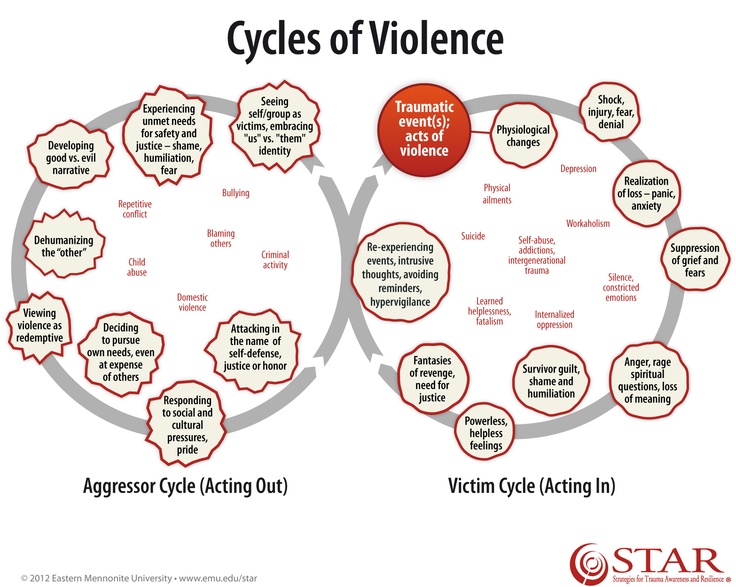
Step 3: Get Support
“Support” may sound superfluous but without it your Intrusive Thought OCD fighting plan will most likely be a bust. It is near impossible to do this work alone. It is not that you are not smart enough or determined enough or brave enough to beat OCD. The reason you need external support is because there is nothing more powerful in taking the wind out of OCD’s sails than voicing intrusive thoughts out loud, to a compassionate, informed coach. The same intrusive thoughts that feel so real, all powerful and self-defining when swirling around in your head will disintegrate when said out loud. When your intrusive thoughts are released into the world and your supportive coach looks back at you, and still sees the YOU they believe in and hears your intrusive thought as “blah blah blah” and possibly laughable, your brain will be one step closer to understanding that these thoughts are spam mail and nothing more.
In terms of finding a supportive OCD coach, you can contact a therapist that is well trained in CBT for OCD but if this is price prohibitive or if there is not access in your local community to OCD experts, there are other options. You can purchase a CBT for OCD workbook and go chapter by chapter through it with any licensed therapist in your community. You can schedule an appointment with one of ADAA’s OCD specialists who offer tele-mental health services. And it is perfectly acceptable to purchase a CBT for OCD workbook and go through the material together with a friend or family member.
You can purchase a CBT for OCD workbook and go chapter by chapter through it with any licensed therapist in your community. You can schedule an appointment with one of ADAA’s OCD specialists who offer tele-mental health services. And it is perfectly acceptable to purchase a CBT for OCD workbook and go through the material together with a friend or family member.
So you now know the three basic steps necessary to kick intrusive thought OCD to the curb. And remember, we are all so much more than our thoughts. Our lives are defined by the actions that we choose to take, not by the electrical storm of thoughts that flicker through our minds.
Dr. Kissen and Dr. Ashley D. Kendall, PhD presented a live webinar on this topic on March 12, 2018 at 1:00 pm ET.
This webinar shares tips and tools to:
- Identify if you may be dealing with harm OCD
- Make sense of why harm OCD picks such painful themes and content
- Take the power away from harm OCD
- Re-engage in your life now that you are giving less of your attention and energy to harm OCD
Watch here.
Debra Kissen, PhD, MHSA
Member Since 2010
Dr. Debra Kissen is CEO of Light On Anxiety CBT Treatment Center. Dr. Kissen specializes in Cognitive Behavioral Therapy (CBT) for anxiety and related disorders. Dr. Kissen is the author of the Panic Workbook for Teens, Rewire Your Anxious Brains for Teens: Using CBT, Neuroscience, and Mindfulness to Help You End Anxiety, Panic, and Worry (The Instant Help Solutions Series) and the soon to be released Break Free from Intrusive Thoughts: An Evidence-Based Guide for Managing Fear and Finding Peace. Dr. Kissen also has a special interest in the principles of mindfulness and their application for anxiety disorders. Dr. Kissen has presented her research on CBT and mindfulness-based treatments for anxiety and related disorders at regional and national conferences. Dr. Kissen is the Co-Chair of the Anxiety and Depression Association of America Public Education Committee. Dr. Kissen was the recipient of the 2020 Gratitude for Giving Spirit Award and the 2018 Anxiety Depression Association of America Member of Distinction Award.
Dr. Kissen often serves as a media psychologist and is available for press inquiries and strives to further the dissemination of empirically supported treatment (EST) information by offering user friendly quotes and simple to understand, practical tips and solutions to help mental health consumers move past stress and anxiety.
Dr. Kissen and ADAA
"I was lucky enough to do my early practicums under the leadership and guidance of Dr. Karen Cassiday who is now president of ADAA. I learned from Dr. Cassiday that time spent with ADAA is one of the best professional investments that I could make. Through continuing education, professional connections and additional contact with mental health consumers, ADAA is truly my professional home. I have always had a passion for enhancing dissemination of empirically supported treatment protocols to mental health consumers. The public education committee offers a wonderful opportunity to create innovative programming to reach mental health consumers where they are, not just in the treatment room. I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
I hope the future of mental health care delivery will allow for many more opportunities to expand access to mental health care through public education initiatives such as those spearheaded at ADAA."
Light on Anxiety CBT Treatment Center
Obsessive-Compulsive Disorder (OCD)
ADAA Blog Content and Blog Comments Policy
ADAA Blog Content and Blog Comments Policy
ADAA provides this Website blogs for the benefit of its members and the public. The content, view and opinions published in Blogs written by our personnel or contributors – or from links or posts on the Website from other sources - belong solely to their respective authors and do not necessarily reflect the views of ADAA, its members, management or employees. Any comments or opinions expressed are those of their respective contributors only. Please remember that the open and real-time nature of the comments posted to these venues makes it is impossible for ADAA to confirm the validity of any content posted, and though we reserve the right to review and edit or delete any such comment, we do not guarantee that we will monitor or review it. As such, we are not responsible for any messages posted or the consequences of following any advice offered within such posts. If you find any posts in these posts/comments to be offensive, inaccurate or objectionable, please contact us via email at [email protected] and reference the relevant content. If we determine that removal of a post or posts is necessary, we will make reasonable efforts to do so in a timely manner.
As such, we are not responsible for any messages posted or the consequences of following any advice offered within such posts. If you find any posts in these posts/comments to be offensive, inaccurate or objectionable, please contact us via email at [email protected] and reference the relevant content. If we determine that removal of a post or posts is necessary, we will make reasonable efforts to do so in a timely manner.
ADAA expressly disclaims responsibility for and liabilities resulting from, any information or communications from and between users of ADAA’s blog post commenting features. Users acknowledge and agree that they may be individually liable for anything they communicate using ADAA’s blogs, including but not limited to defamatory, discriminatory, false or unauthorized information. Users are cautioned that they are responsible for complying with the requirements of applicable copyright and trademark laws and regulations. By submitting a response, comment or content, you agree that such submission is non-confidential for all purposes. Any submission to this Website will be deemed and remain the property of ADAA.
Any submission to this Website will be deemed and remain the property of ADAA.
The ADAA blogs are forums for individuals to share their opinions, experiences and thoughts related to mental illness. ADAA wants to ensure the integrity of this service and therefore, use of this service is limited to participants who agree to adhere to the following guidelines:
1. Refrain from transmitting any message, information, data, or text that is unlawful, threatening, abusive, harassing, defamatory, vulgar, obscene, that may be invasive of another 's privacy, hateful, or bashing communications - especially those aimed at gender, race, color, sexual orientation, national origin, religious views or disability.
Please note that there is a review process whereby all comments posted to blog posts and webinars are reviewed by ADAA staff to determine appropriateness before comments are posted. ADAA reserves the right to remove or edit a post containing offensive material as defined by ADAA.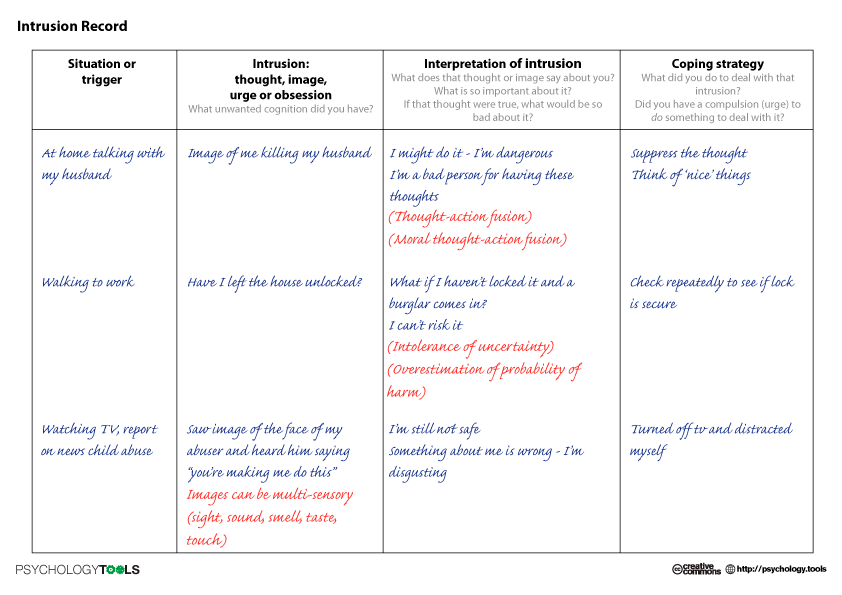
ADAA reserves the right to remove or edit posts that contain explicit, obscene, offensive, or vulgar language. Similarly, posts that contain any graphic files will be removed immediately upon notice.
2. Refrain from posting or transmitting any unsolicited, promotional materials, "junk mail," "spam," "chain mail," "pyramid schemes" or any other form of solicitation. ADAA reserves the right to delete these posts immediately upon notice.
3. ADAA invites and encourages a healthy exchange of opinions. If you disagree with a participant 's post or opinion and wish to challenge it, do so with respect. The real objective of the ADAA blog post commenting function is to promote discussion and understanding, not to convince others that your opinion is "right." Name calling, insults, and personal attacks are not appropriate and will not be tolerated. ADAA will remove these posts immediately upon notice.
4. ADAA promotes privacy and encourages participants to keep personal information such as address and telephone number from being posted. Similarly, do not ask for personal information from other participants. Any comments that ask for telephone, address, e-mail, surveys and research studies will not be approved for posting.
Similarly, do not ask for personal information from other participants. Any comments that ask for telephone, address, e-mail, surveys and research studies will not be approved for posting.
5. Participants should be aware that the opinions, beliefs and statements on blog posts do not necessarily represent the opinions and beliefs of ADAA. Participants also agree that ADAA is not to be held liable for any loss or injury caused, in whole or in part, by sponsorship of blog post commenting. Participants also agree that ADAA reserves the right to report any suspicions of harm to self or others as evidenced by participant posts.
RESOURCES AND NEWS
Evidence-based Tips & Strategies from our Member Experts
RELATED ARTICLES
Block reference
Why We Get Them and How to Stop Them
Intrusive thoughts are unexpected images or thoughts that seem to pop into your head. They’re often strange or distressing. But these thoughts happen to almost everyone from time to time.
Intrusive thoughts seem to come out of nowhere. These thoughts and images are unwanted and often unpleasant. The content can sometimes be aggressive or sexual, or you could suddenly think about a mistake or a worry.
You might feel distressed when this happens, but having an intrusive thought once in a while is a typical part of life.
In most cases, intrusive thoughts do not have any particular meaning. As long as you recognize that these are only thoughts, and you have no desire to act on them, intrusive thoughts are not harmful.
However, if they’re happening often, causing significant concern, or interfering with your daily activities, it’s a good idea to talk with a doctor.
Read on to learn more about why intrusive thoughts happen and how you can manage them.
There are several different types of intrusive thoughts. Some people may have intrusive thoughts about:
- germs, infections, or other kinds of contamination
- violent acts, aggression, or causing harm to other people
- doubts about doing tasks wrong or leaving tasks unfinished
- religion, blasphemy, or being an immoral person
- sexual acts or situations
- acting out or saying the wrong thing in public
It’s also possible to have other types of intrusive thoughts that do not fit into these categories.
Sometimes, people who experience intrusive thoughts become worried about what they mean. This can lead to someone trying to control or stop the thoughts. People may also feel ashamed and want to keep them secret from others.
Keep in mind that the image or thought might be disturbing, but it does not usually have a particular meaning. If you have no desire or intention to act on the thought, and you can easily move on with your day, then it’s probably nothing to worry about.
Thoughts of hurting yourself or others are a reason to reach out for help. If you’re thinking about hurting yourself or someone else, get emergency care right away. Go to the nearest emergency room or contact your local emergency services.
It’s common to have an intrusive thought every once in a while. In fact, it happens to almost everyone. A 2014 study found that about 94 percent of participants had at least one intrusive thought in the 3 months prior to the study.
In the 2014 study, “doubting” intrusions — or worries about doing tasks correctly — were the most common. Intrusive thoughts of a sexual or religious nature were the least likely to be reported.
Intrusive thoughts of a sexual or religious nature were the least likely to be reported.
Although intrusive thoughts are usually nothing to worry about, sometimes they can start to interfere with your daily life.
People who feel fear or guilt about their intrusive thoughts, or feel like they need to take action to control the thoughts, may be experiencing something more serious. If that’s the case, it’s a good idea to talk with a doctor.
Intrusive thoughts may not have a cause. They can just happen randomly. Some thoughts wander into your brain. Then just as quickly, they exit, leaving no lasting impression.
Less commonly, intrusive thoughts are related to an underlying mental health condition, like obsessive-compulsive disorder (OCD) or post-traumatic stress disorder (PTSD). These thoughts could also be a symptom of another health issue, such as:
- brain injury
- dementia
- Parkinson’s disease
Signs that there might be an underlying cause include intrusive thoughts that:
- last longer than a brief moment
- continue to pop back into your head
- cause distress over time
- make you feel like you need to control your thoughts
Changes to mental health are nothing to take lightly. Early symptoms of some conditions may also include:
Early symptoms of some conditions may also include:
- changes in thought patterns
- obsessive thoughts
- thoughts of disturbing imagery
These thoughts are nothing to be ashamed of, but they are a reason to seek a diagnosis and treatment so that you can start to feel better.
Intrusive thoughts are not always the result of an underlying condition. Anyone can experience them.
But there are several conditions that include intrusive thoughts as a symptom. They include:
OCD
In OCD, intrusive thoughts cause serious distress. A person with OCD often makes significant efforts to try to suppress or stop their unwanted thoughts (obsessions). This usually involves repeating particular behaviors or habits over and over.
The behaviors and habits, known as compulsions, can interfere with a person’s quality of life. But it’s possible for OCD to improve significantly with treatment.
PTSD
People living with PTSD may have intrusive thoughts related to a traumatic event they’ve experienced. These thoughts or memories can bring forth other symptoms of PTSD, such as insomnia or an unpleasant state of overalertness.
These thoughts or memories can bring forth other symptoms of PTSD, such as insomnia or an unpleasant state of overalertness.
PTSD can interfere with a person’s daily functioning. However, with trauma-focused treatment, it’s possible to get relief from symptoms.
Eating disorders
People with an eating disorder may experience intrusive thoughts about their body, losing weight, or what they eat. This can include guilt, shame, or fear related to food or body image. These intrusions can cause serious distress.
Eating disorders can also cause significant changes in behaviors related to food and eating.
It’s important to talk with a doctor if you have eating disorder symptoms. With treatment, it can be possible to avoid serious complications.
Intrusive thoughts are powerful because they seem to “stick” in your mind. They’re upsetting because they feel so foreign.
The best way to manage intrusive thoughts is to reduce your sensitivity to the thought and its contents.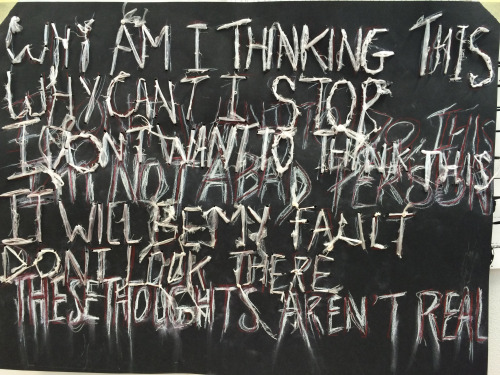 The following strategies may help.
The following strategies may help.
Ways to manage intrusive thoughts
- Cognitive behavioral therapy (CBT). In CBT, you’ll work with a therapist to learn ways of thinking that can help you become less sensitive to the intrusive thoughts. In a controlled setting, your therapist may also expose you to triggers for your intrusive thoughts so you can learn to react to them differently.
- Medication. Sometimes, medications are used to treat conditions like OCD and PTSD. Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to treat these mental health conditions.
- Self-care. A good step toward treating intrusive thoughts is recognizing what they are: just thoughts. You can learn to label them when they happen and recognize that thoughts are not the same as intent or behavior. This may help reduce the frequency or intensity of unwanted thoughts.
The first step toward a diagnosis is talking with a doctor.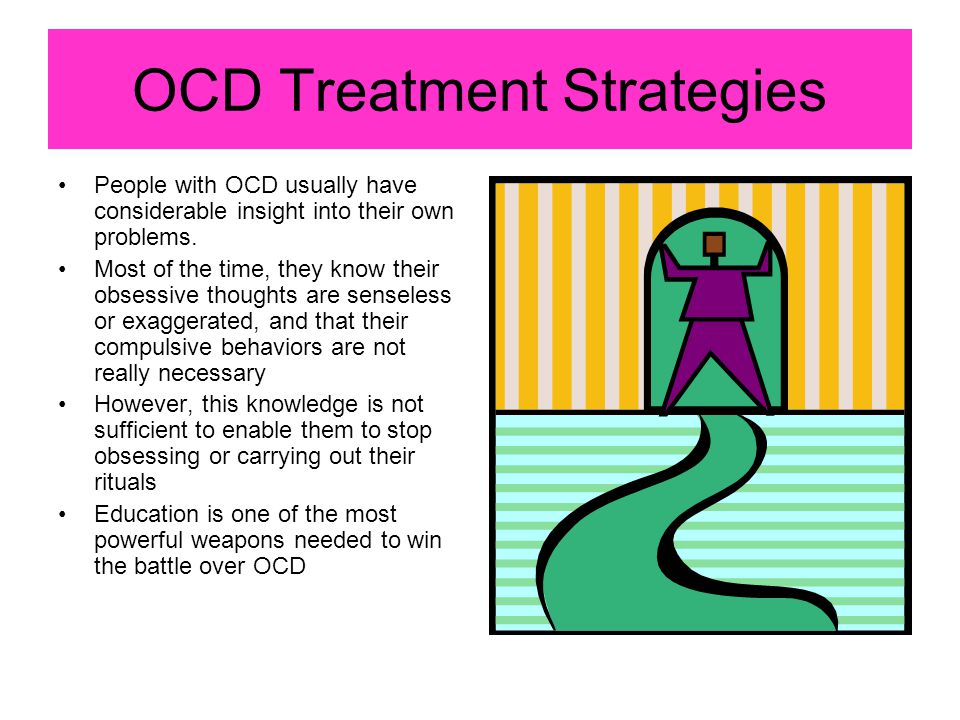 They’ll review your symptoms and medical history. They may conduct a physical exam and, in some cases, use questionnaires or tests to find out more about your symptoms.
They’ll review your symptoms and medical history. They may conduct a physical exam and, in some cases, use questionnaires or tests to find out more about your symptoms.
If they find no physical issue that could be leading to intrusive thoughts, they may refer you to a licensed psychologist or psychiatrist. These individuals are trained to recognize the signs and symptoms of possible causes for intrusive thoughts, including OCD and PTSD.
A psychologist or psychiatrist can work with you to identify the thoughts when they occur and how you respond to them. This will help them come to a diagnosis and decide whether there’s another possible cause.
Intrusive thoughts can feel distressing, but if one pops up once in a while, it’s probably nothing to be concerned about. In many cases, they are not caused by anything in particular. By recognizing that it’s only a thought, you can help yourself move past it.
When intrusive thoughts are related to an underlying condition, like OCD or PTSD, getting started with a diagnosis and treatment may take some time.
But sticking to your treatment plan can help ease symptoms and make the thoughts less frequent. Options like medication and CBT can help you cope with the thoughts when they do happen.
If your intrusive thoughts are interfering with your day-to-day life, talk with a doctor about your experiences. Getting treatment can help make intrusive thoughts more manageable.
7 ways to cope with bad thoughts
Unpleasant thoughts are sometimes more terrible than the events that caused them - it is extremely difficult to get rid of them. Some people spend several hours a day on them! What can be opposed to bad thoughts?
It turns out that there are a number of methods that will help block the appearance of bad thoughts or cope with them if they have already come. Most of these methods are offered by the American psychologist Danielle Wegner, who has devoted decades of her life to the problem. nine0003
1. SWITCH
Don't try not to think of a white monkey - think of a black one. Or better yet, a purple flamingo. Try to switch your mind to some other subject that you also like to think about very much, but which at the same time has positive connotations. Get yourself a few “continued” thoughts that raise more and more questions and the need for answers to them - which means they are drawn into a completely different stream of thoughts. Is it true that Brad Pitt has silicone muscles? I read about it somewhere. But if so, how does he use them? After all, silicone is not able to contract like real muscles - or is there some way to make it do this? And there is also a conspiracy theory according to which our Earth is really flat, and only a cabal of evil scientists has been convincing us for several centuries that it is spherical. Wait, what about satellite images and records from space? And they are falsified by the same scientists. But what about the poles? There is only one pole - the North one, it is in the center of the Earth, which is flat as a disk, and along the edges of the disk there are glaciers that scientists pass off as Antarctica.
Or better yet, a purple flamingo. Try to switch your mind to some other subject that you also like to think about very much, but which at the same time has positive connotations. Get yourself a few “continued” thoughts that raise more and more questions and the need for answers to them - which means they are drawn into a completely different stream of thoughts. Is it true that Brad Pitt has silicone muscles? I read about it somewhere. But if so, how does he use them? After all, silicone is not able to contract like real muscles - or is there some way to make it do this? And there is also a conspiracy theory according to which our Earth is really flat, and only a cabal of evil scientists has been convincing us for several centuries that it is spherical. Wait, what about satellite images and records from space? And they are falsified by the same scientists. But what about the poles? There is only one pole - the North one, it is in the center of the Earth, which is flat as a disk, and along the edges of the disk there are glaciers that scientists pass off as Antarctica.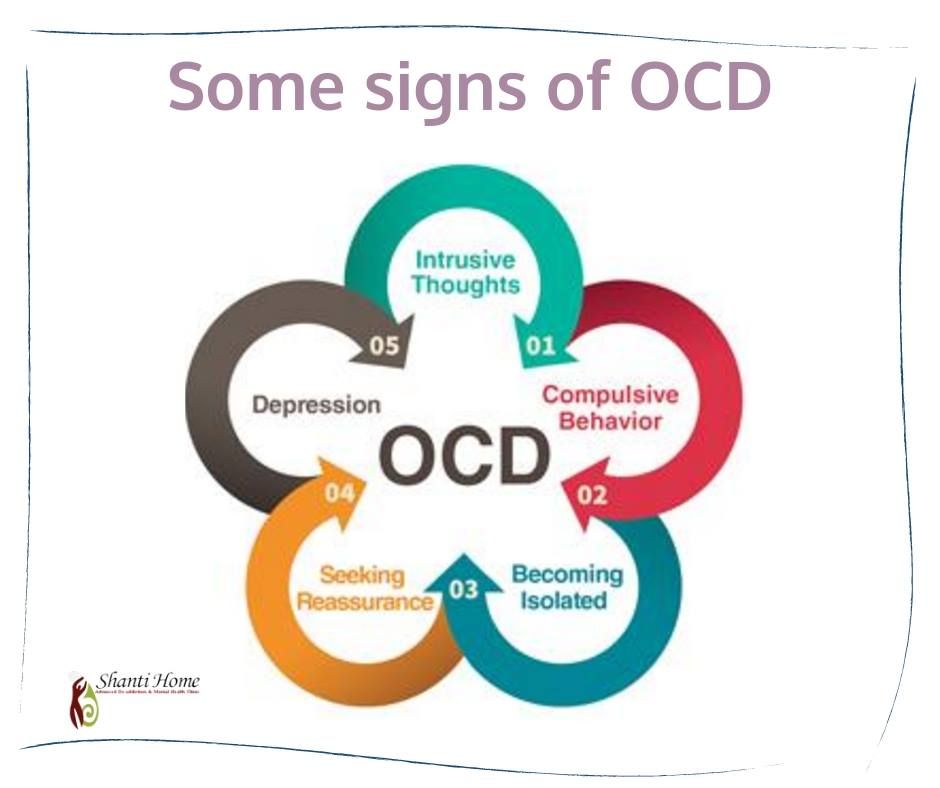 And so on - soon the seething stream of this nonsense will take you in a completely new direction. nine0003
And so on - soon the seething stream of this nonsense will take you in a completely new direction. nine0003
2. AVOID STRESS
Some people find that a strong impression will help them cope with intrusive thoughts, such as a scandal with their neighbors or running naked through a winter city at night. However, studies show that the more you shake up your emotions, the weaker it is before the “alien invasion” of uninvited thoughts. On the contrary, try to calm down and rest - the more strength you have and the better your brain is, the more chances you have to repel an attack. nine0003
3. STOP THE BAD THOUGHTS
Deal with the obsessive thought - you will definitely pay attention to it, but only later. Include in your daily schedule "half an hour for painful thoughts" - but not before bedtime, but, for example, at the height of the working day. Thinking about what is bothering you during your lunch break will quickly take your mind off your problems and plunge back into work. Sooner or later, the subconscious mind will get used to the fact that obsessive thoughts have their own time with strictly defined limits, and will stop pestering you at other hours. Now you can think about how to exterminate annoying thoughts at this time. nine0003
Sooner or later, the subconscious mind will get used to the fact that obsessive thoughts have their own time with strictly defined limits, and will stop pestering you at other hours. Now you can think about how to exterminate annoying thoughts at this time. nine0003
4. FOCUS ON THE OBSESSION
Once upon a time, a patient came to the great physician Abu Ali ibn Sina, who complained that his eyelid was twitching. Ibn Sina prescribed him an extremely dubious remedy: every hour to begin to blink on purpose with an obstinate eyelid. The patient chuckled, but promised to strictly follow the prescribed. A few days later he came to thank the doctor. Like the remedy prescribed by Ibn Sina, this method works on the principle of "on the contrary": when an obsessive thought comes to you, try to force yourself to think it over from all sides, turn it this way and that, make yourself afraid that it will slip away from you - and you will soon feel that her grip is weakening and she herself would be glad to escape from you. nine0003
nine0003
5. RECOGNIZE THE INEVITABILITY OF A BAD THOUGHT
Another way, somewhat similar to the previous one, is to replace the fear of the appearance of an unkillable thought with complete indifference to it. Learn to think of it as something external: for example, if it is the thought that a loved one left you, get used to the idea that this thought has nothing to do with him (or her), but exists on its own: here now I will go to bed, and my number one Thought will come to me again. Accustom yourself to the fact that this thought does not develop and does not tell you anything new - it just comes and goes, as twelve o'clock at night or winter come and go. And very soon you will feel that she is really leaving *. nine0003
6. MEDITATE
Meditation is a great way to organize your mind, bringing your thoughts under control. Practice it daily, trying to achieve a state of complete thoughtlessness. It is not easy, but if you learn how to do it, you will be able to induce this state at will, including it at the time of the day when you are most prone to bad thoughts, or in the situation when you become most defenseless against them. If a bad thought is not positively reinforced in the form of your willingness to devote your brain resources to it, it begins to wane—and soon fades away. nine0003
If a bad thought is not positively reinforced in the form of your willingness to devote your brain resources to it, it begins to wane—and soon fades away. nine0003
7. THINK ABOUT YOUR GOALS
How is bad thought different from gas? Gas, as we know from a physics textbook, occupies the entire volume provided, and a bad thought is not yet provided ... It teaches us to concentrate on it, forgetting that there is so much good in the world that it is much more pleasant to think about. Obsessive thoughts are especially fond of people who have neither a major lifelong goal nor an interesting hobby. Take yourself out of the state of sad thoughts, thinking about the path to success, about what will bring you satisfaction. If you make an effort, you will gradually be able to accustom yourself to positive dreams. nine0003
How do I deal with obsessive thoughts and rituals? Rubric: Psychologists do not give advice
What are obsessive thoughts and actions? Why, in moments of drastic change and stress, do many seek rituals that reduce anxiety? How can I help a loved one who has OCD-like symptoms? We discuss the topic of obsessive thoughts and actions, as well as the diagnosis and treatment of OCD with psychotherapists Treatfield.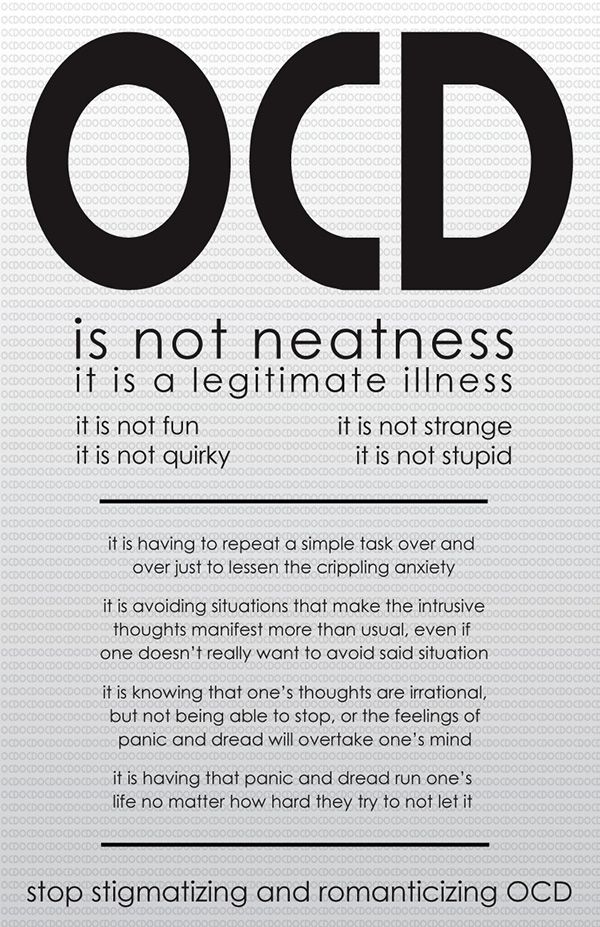
What are obsessive thoughts and actions? How do they arise and why do they sometimes almost disappear, and then suddenly intensify? Why obsessive rituals aren't always OCD? How to distinguish OCD from obsession? nine0058
Psychologist answers Lesia Loriashvili
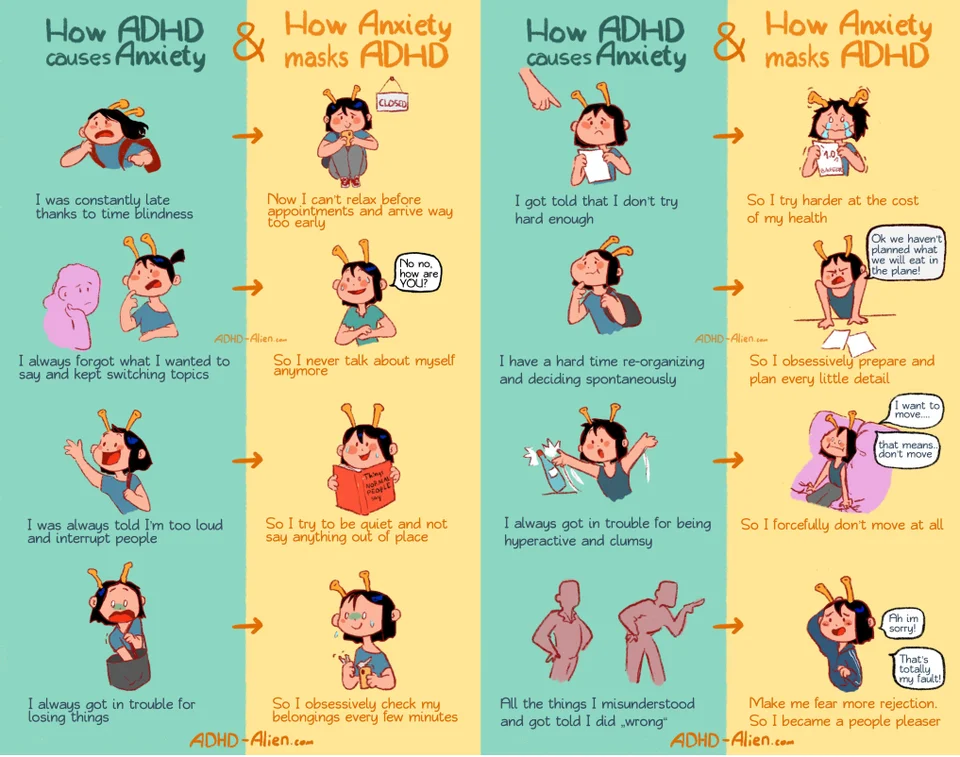
There are two types of obsessions: obsessions and compulsions. Obsessions are recurring thoughts, urges, or images. Compulsions are actions, repetitive behavior. They "force" a person to think or act in a certain way and significantly impair functioning. If this activity is also subject to a rigid organizational structure, this is called compulsive rituals.
Obsessions are characterized by absurdity, strangeness, pathology: obsessive thoughts have nothing to do with a person's will. These ideas provoke constant intellectual activity, and quite intense and exhausting. This is a very hard mental work that requires effort and gives rise to a special asthenic state - that is, a person is extremely tired. nine0003
nine0003
Let's try to draw parallels with actual situations. Many people think: “I’ll sit in quarantine, rest, I’ll have holidays,” but no! In practice, we are seeing even more fatigue from internal anxieties and external news that come from all messengers. There is an obsessive attempt to get rid of the flow of disturbing information or obsessive absorption of news. That's how easy it is to be in the place of a person with OCD symptoms now!
Compulsive actions are experienced even more painfully than thoughts, because these actions can contradict the ideals and moral ideas of a person. In fear of getting infected, I will not shake hands and hug when meeting a friend, I will not offer to visit. In a pandemic situation, when anxiety is running high, it may seem that people around are suffering from OCD, but obsessive thoughts and actions in such situations save us from experiencing the uncontrollability and unpredictability of the situation. For example, the desire to accumulate stocks of food or antiseptics in ordinary life would look pathological. The ritual in the form of wiping purchases and door handles with alcohol or hanging outerwear on the balcony, washing clothes after each exit to the street, could well be considered painful six months ago, but not now, when the threat is real and close. nine0003
The ritual in the form of wiping purchases and door handles with alcohol or hanging outerwear on the balcony, washing clothes after each exit to the street, could well be considered painful six months ago, but not now, when the threat is real and close. nine0003
See also: 5 Questions about OCD and Obsessions
These intrusive and inappropriate thoughts and actions that are hard to let go, that bring suffering, take a lot of time or interfere with daily activities have visited everyone at least once in a lifetime. “How much can I do in self-isolation!” But a month has passed, and I continue to look at the graphs of the extensive growth of cases of COVID-19. Such behavior can be perceived by the person himself as a serious problem, already the hands are red and the skin is cracking from endless washing of hands, but WHO recommends. And it turns out that obsessive-compulsive behavior in the current situation is the fight against a real threat. nine0003
This is exactly how you can distinguish an OCD symptom from an adequate defensive response in a worldwide pandemic. The ability to assess one's condition, testing reality is the main criterion for adequacy. I can stop when I go too far: for example, I put on a mask in public places, but then take it off and breathe in the fresh air in nature when there are no people around.
The ability to assess one's condition, testing reality is the main criterion for adequacy. I can stop when I go too far: for example, I put on a mask in public places, but then take it off and breathe in the fresh air in nature when there are no people around.
Being critical of obsessive thoughts and actions can be frightening (“I don't recognize myself!”). This is perceived as an invasion: “I don’t tend to do this, can’t I control myself ?!” There may be a terrible sense of shame that will prevent you from asking for help and support. But in a pandemic situation, we are closer than ever to understanding people with mental difficulties. nine0003
Obsessions are often triggered by stressors and loss of control. Every third person has now lost his job or is on forced leave. The only thing you can control in a quarantine situation is not to leave the house, but social isolation can be experienced even harder.
People with OCD often find themselves in isolation because they cannot build relationships: the partner cannot stand constant attempts to control or endure endless rituals.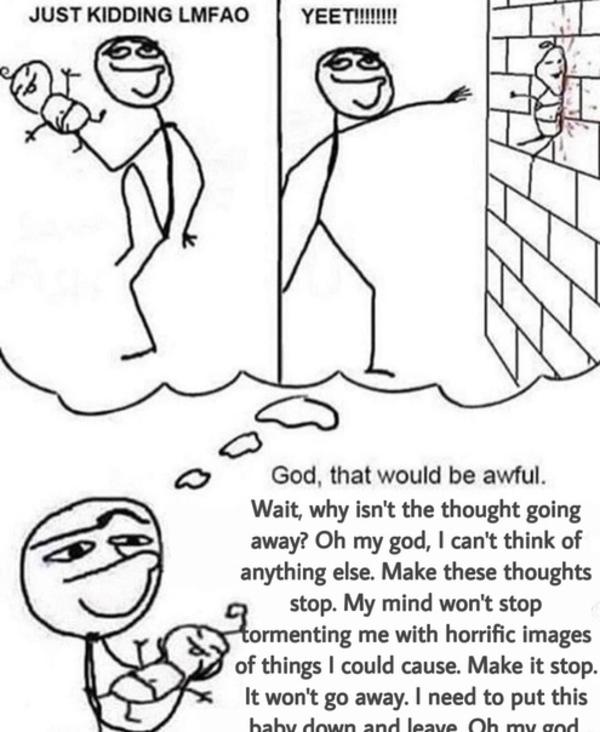 Interestingly, right now we are all, to one degree or another, in isolation and experiencing the same level of anxiety that people with OCD experience in everyday life. We feel besieged inside apartments and houses, we are attacked by news of the threat and death. This is exactly how a person suffering from obsessions feels. Powerlessness is a key feeling that everyone has to face in trying to control reality. Even the most developed countries could not resist the spread of the disease. Awareness of powerlessness is the best way to experience strength. There is no cure for the new virus, but there are those simple efforts that anyone can make: self-isolate, take precautions, keep your distance, and help the older generation. nine0003
Interestingly, right now we are all, to one degree or another, in isolation and experiencing the same level of anxiety that people with OCD experience in everyday life. We feel besieged inside apartments and houses, we are attacked by news of the threat and death. This is exactly how a person suffering from obsessions feels. Powerlessness is a key feeling that everyone has to face in trying to control reality. Even the most developed countries could not resist the spread of the disease. Awareness of powerlessness is the best way to experience strength. There is no cure for the new virus, but there are those simple efforts that anyone can make: self-isolate, take precautions, keep your distance, and help the older generation. nine0003
Relief can come from being able to express feelings associated with painful experiences, especially the normal frustration, anger, anger, and grief that accompany OCD and many people in an epidemic emergency.
What should I do if I am attacked by obsessive thoughts and fantasies that bad things might happen in the future? How to weaken them, if the fight against them only strengthens them? What should I do if I began to check the gas or iron many times, and the obsessive rituals that have appeared bother me? nine0058
Psychologist answers Maria Lemeshchuk
Each of us is familiar with this emotional state, which carries a lot of excitement, anxiety and fear - and the reason for this is not stress or a real problem, but thoughts related to the future.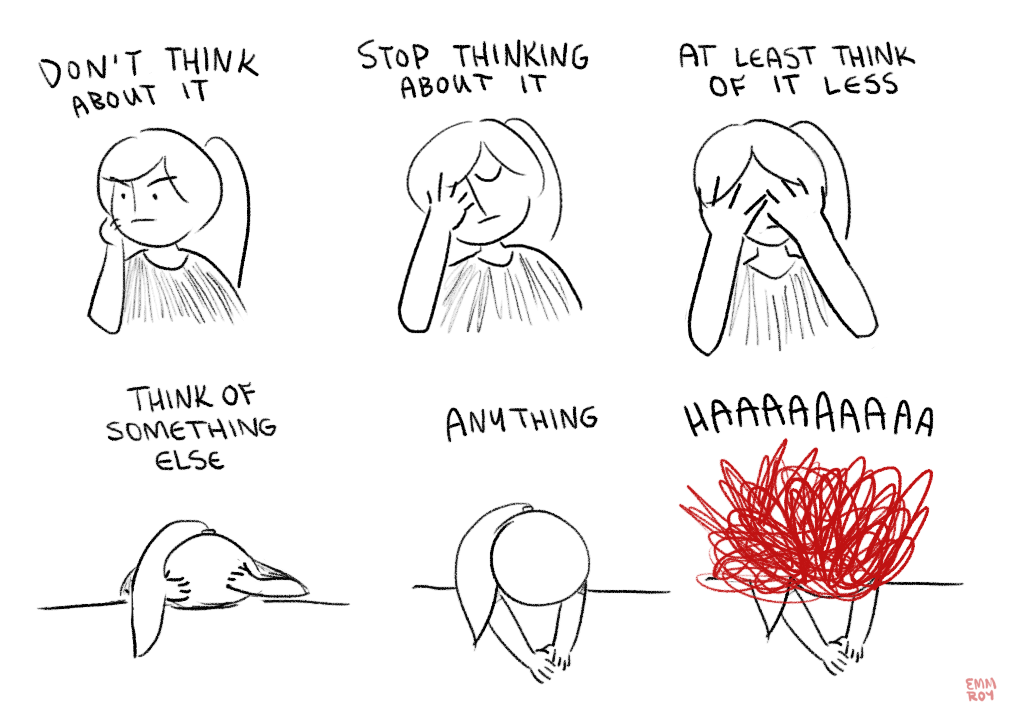 This is typical for many, since the future for us is significant, but unknown. And where there is uncertainty, there is anxiety. It's okay to occasionally catch yourself with these thoughts and stop them, but if they get too much, they become elusive and uncontrollable, spoil your mood and force you to make adjustments to your behavior, then you need to pay special attention to working with them. nine0003
This is typical for many, since the future for us is significant, but unknown. And where there is uncertainty, there is anxiety. It's okay to occasionally catch yourself with these thoughts and stop them, but if they get too much, they become elusive and uncontrollable, spoil your mood and force you to make adjustments to your behavior, then you need to pay special attention to working with them. nine0003
Usually obsessive thoughts can be recognized by the following criteria: they are forward-looking, there are many of them, they are hard to stop and they cause a lot of anxiety. When we try to calm ourselves, it helps for a short period, but then there are even more thoughts. If we increase control, plan a lot, or avoid - this also gives fleeting confidence, but it quickly passes. These strategies should not be used. In order to cope with obsessive thoughts about the future, first of all, we need to accept the fact that experiences are an integral part of our life. And experiences are different - useful and not. Useful experiences are necessary for us to mobilize, to change the strategy of action. We can influence the situation connected with them by action. Thoughts arise in close conjunction with the actual event. And if you notice such experiences, you don’t need to do anything with them, we need them, we translate them into action (for example, when we worry that we are late for work, we can call a taxi). nine0003
Useful experiences are necessary for us to mobilize, to change the strategy of action. We can influence the situation connected with them by action. Thoughts arise in close conjunction with the actual event. And if you notice such experiences, you don’t need to do anything with them, we need them, we translate them into action (for example, when we worry that we are late for work, we can call a taxi). nine0003
Experiences can be considered unhelpful if the probability that they will come true is very small, that is, the problem is not real, but possible. Such thoughts do not lead to actions, they are uncontrollable and long-lasting (for example, we worry that we will be late for a new job, which we leave in a month). Therefore, the first step in the work is to understand whether we have a real problem or a hypothetical one, whether we can influence it or not. Unhelpful experiences do not need to be corrected, we must let go of them because they are unrealistic. Don't push away, but watch them come and let go. nine0003
nine0003
It is important to develop resistance to the unknown, not to look for 100% certainty in anything. To do this, you can consciously face something new every day, try something new and still withstand a little anxiety. So we can "harden" our body - and anxious thoughts about the future will not seem so insurmountable.
We also advise you to look: Where to start to get rid of bad thoughts?
What to do if obsessive rituals (such as checking the gas and iron) disturb you? First of all, it is worth distinguishing and seeing anxiety with its consequences - thoughts and behavior. It is important to understand what thoughts are causing the gas or iron check. We need to check these thoughts for realism. If the thought arises that “because of me, my house will burn down,” you need to understand whether it is really worth checking the iron many times in order to avoid this. Thoughts do not equate to reality: we may be afraid of a fire, but these thoughts will not start a fire.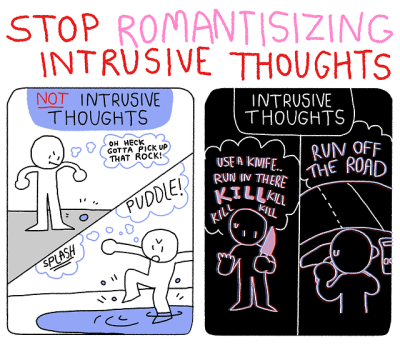 Therefore, it is important to understand whether it is worth neutralizing thoughts that are not reality with your behavior. nine0003
Therefore, it is important to understand whether it is worth neutralizing thoughts that are not reality with your behavior. nine0003
When the work on the thoughts has been done, we move on to the exposure - we gradually change the behavior in the direction of reducing the number of checks. For example, if today I checked the iron seven times, then tomorrow I can only six. So, step by step, we change behavioral patterns, while working through the thoughts that arise. At the beginning of work, if it is difficult to reduce checks, you can take a picture of the turned off iron on your phone and control only the number of views.
Dealing with neutralizing behavior can be a long process that requires patience and understanding of the difficulties of dealing with anxiety and its consequences. Understanding the nature of anxiety and obsessive actions, working on them, give good results and significantly improve the quality of human life. nine0003
How to deal with a loved one who is anxious and compulsive? Checks if the door is closed and if the gas is turned off, for example.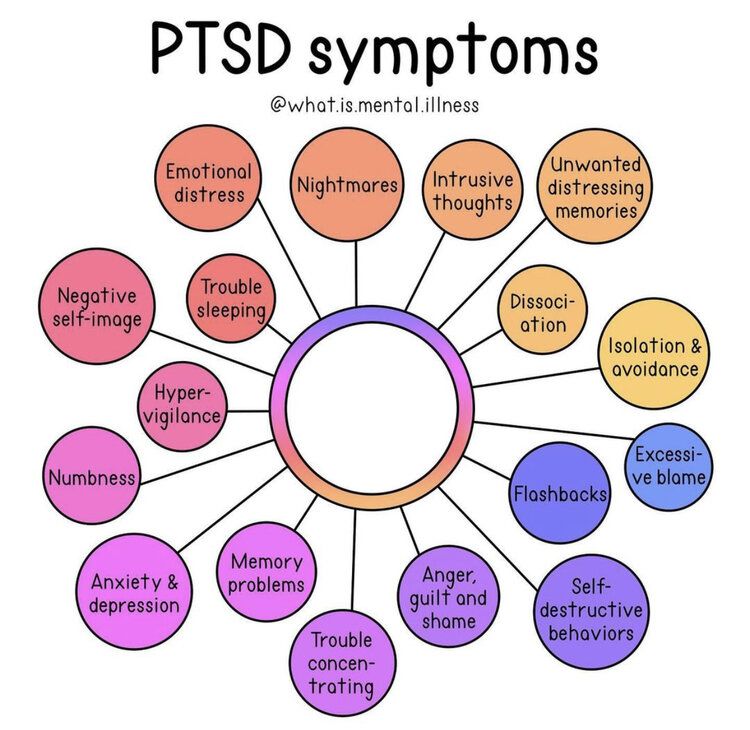 Or is captured by obsessive thoughts about the same thing and constantly talks about it. Can you help and support? How not to worsen the situation?
Or is captured by obsessive thoughts about the same thing and constantly talks about it. Can you help and support? How not to worsen the situation?
Psychologist advises Svetlana Ridzel
If your loved one has OCD, this can negatively affect your relationship. For example, your partner may require you to wash dishes with excessive (for your taste) thoroughness, refuse some household duties or travel together, or constantly need support and reassurance. As in the opposite direction, family conflicts can exacerbate anxiety and, accordingly, the intensity of obsessive thoughts and compulsions. nine0003
How can you help a loved one with OCD? First of all, it is important to find and study reliable information about the disorder, for example, on specialized sites (iocdf.org, English) or from specialists in the treatment of OCD. Knowing about the characteristics of obsessive-compulsive disorder and the factors that can exacerbate OCD can help you deal with your loved one's symptoms with greater understanding and empathy.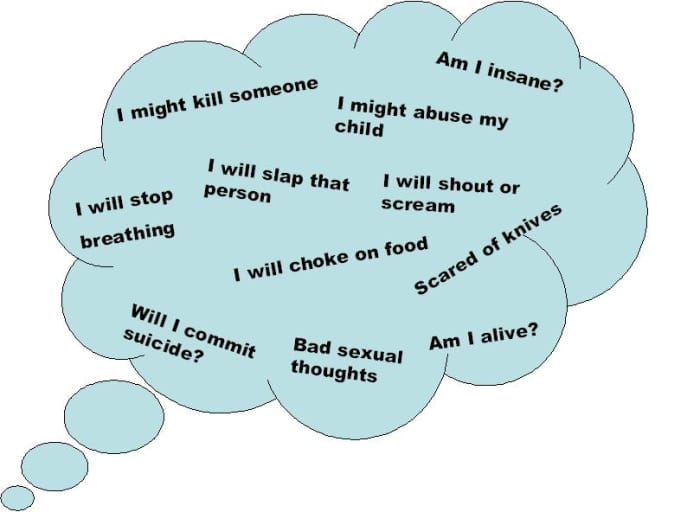
If obsessive thoughts and compulsions take a long time and seriously impair the life of your loved one, but he does not seek help, it may be worth helping him find a specialist and support him in the process of treatment. nine0003
It is important to understand that out of a sense of love and care, the family often engages in rituals or supports the avoidance: doing something for the person or agreeing to change the daily routine and/or habits. This is called "adapting to the symptom" and makes OCD more durable, as it can reduce a person's motivation for therapy. And here the help of a psychotherapist is already needed in order to develop new forms of expression of love and care within the family together with the couple or family, which would not support the symptoms. nine0003
Moreover, there are approaches in which the family becomes a kind of "co-therapist" or "coach" for a person with OCD - in sessions, family members jointly plan exposures (meeting with a trigger while simultaneously refusing rituals that reduce anxiety), develop plan how to share emotions and express support, but not get involved and rush to reduce his anxiety.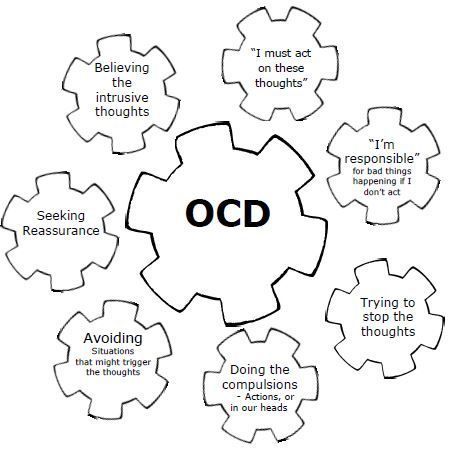 This is often difficult, as our natural response is to protect a loved one from unpleasant experiences, but a short-term reduction in anxiety does a disservice in the long run. Namely, it does not help your loved one develop a new, more adaptive attitude towards anxiety and faith in their ability to cope. nine0003
This is often difficult, as our natural response is to protect a loved one from unpleasant experiences, but a short-term reduction in anxiety does a disservice in the long run. Namely, it does not help your loved one develop a new, more adaptive attitude towards anxiety and faith in their ability to cope. nine0003
How can psychotherapy help me with obsessive thoughts and actions/rituals? How does work with such a request begin and how is it built further? Are there any chances to get rid of obsession and repetitive actions?
Psychologist answers Evgenia Chernega
Advise The average time for people with obsessive thoughts and actions to seek help is 7.5 years after the onset of symptoms. OCD is one of the most difficult types of anxiety disorders to deal with. It can significantly affect the quality of life and, developing, over time, even disable a person. However, people are often embarrassed and want to hide it, although now there are already effective methods of helping. The American Psychological Association (APA, 2007) protocol suggests cognitive behavioral therapy (CBT) and pharmacotherapy with serotonin reuptake inhibitors as two first choice interventions with empirically proven efficacy. The protocol suggests initiating treatment with CBT in all cases except when there is no access to CBT, when the patient has a past history of successful treatment with the drug of choice, or when the patient himself prefers pharmacotherapy. nine0003
The American Psychological Association (APA, 2007) protocol suggests cognitive behavioral therapy (CBT) and pharmacotherapy with serotonin reuptake inhibitors as two first choice interventions with empirically proven efficacy. The protocol suggests initiating treatment with CBT in all cases except when there is no access to CBT, when the patient has a past history of successful treatment with the drug of choice, or when the patient himself prefers pharmacotherapy. nine0003
CBT deals with behavior and thinking. Dealing with such a request in CBT begins with building trust, a sense of security, and a lack of judgment. This is important so that the person can describe their symptoms without fear or shame. The examination phase can take a long time, because each person with OCD has their own unique OCD, their own obsessions and compulsions. After establishing the main diagnosis and examining comorbid disorders (often depression, generalized anxiety disorder, impulsive disorder coexist with OCD), a decision is made whether psychotherapy is sufficient or pharmacotherapy is also needed. In the latter case, a team of psychotherapist and psychiatrist works with the client, with psychotherapy playing a leading role. During the exploration phase, the therapist helps to assess the types of obsessions, the meaning given to obsessive thoughts, their triggers, ways of avoiding them, the impact of childhood experiences, and biological factors. We explore the last episode in detail, and also look for other possible obsessions and compulsions - as a rule, there are many and they are different. Also, at the beginning of work, the client must fill out standardized scales for measuring intensity, and together we develop individual monitoring forms - the client will fill them out both during therapy and at the end to determine the effectiveness of therapy. nine0003
In the latter case, a team of psychotherapist and psychiatrist works with the client, with psychotherapy playing a leading role. During the exploration phase, the therapist helps to assess the types of obsessions, the meaning given to obsessive thoughts, their triggers, ways of avoiding them, the impact of childhood experiences, and biological factors. We explore the last episode in detail, and also look for other possible obsessions and compulsions - as a rule, there are many and they are different. Also, at the beginning of work, the client must fill out standardized scales for measuring intensity, and together we develop individual monitoring forms - the client will fill them out both during therapy and at the end to determine the effectiveness of therapy. nine0003
Next comes psychoeducation - the client learns about what OCD is, how the disorder develops, what features of thinking can influence its dynamics. For example, there are six main types of cognitive distortions that contribute to the development and maintenance of problems: perfectionism, hyperresponsibility, confusion of thoughts and actions, uncertainty intolerance, belief in controllability of thoughts, anxiety and threat intolerance. Magical thinking is also a frequent companion of OCD.
Magical thinking is also a frequent companion of OCD.
The next step is to deal with these thought pitfalls and evaluative thoughts using cognitive techniques and behavioral experiments to change the value assigned. After all, the problem is not that some thoughts come to mind. There are a billion neurons in the brain, and it is his job to generate thoughts. The thoughts that a person with OCD suffers from come into the mind of most people, but the difference between a person with OCD is that he attaches special importance to these thoughts where another thinks: “Well, that’s what comes to mind” - and moves on . At the same stage, the client learns to respond to intrusive thoughts in a new way - to let them go instead of thinking. nine0003
At the next stage, exposure occurs with anticipation of the reaction along the hierarchy of obsessions. A person trains to withstand anxiety and tension and not relieve them in the usual way - washing hands or checking switches. This is the most difficult stage of therapy, during which new neural connections are formed that allow a person to act as he wants, and not as impulses force him to.