Obesity and mental health uk
The Relationship Between Mental Health and Obesity
This month we spoke to Arti Dhokia, Advanced Mental Health and Gastroenterology Dietitian at Priory Hospital Woodbourne, about the relationship between mental health and obesity. Arti specialises in eating disorders, spotting the early signs of disordered eating, weight gain/loss management, and has a particular interest in obesity management.
We explore the links between ‘food and mood’, what the signs and symptoms of poor nutrition are and how it is linked to mental health recovery, the effects that mental health medication can have on weight, and what particular foods can help to improve wellbeing.
Why is this so important?
Despite there being a number of demographic variables that could affect the direction and/or strength of this link, including socioeconomic status, level of education, age, gender and ethnicity, a 2010 systematic review highlighted a two-way association between depression and obesity.
The review found that people who were obese had a 55% increased risk of developing depression over time, whereas people experiencing depression had a 58% increased risk of becoming obese.
It is estimated that the NHS spent £6.1 billion on overweight and obesity-related ill-health from 2014 to 2015. Failing to address the challenge posed by the obesity epidemic will place an even greater burden on NHS resources. This emphasises the importance of spotting the early signs of disordered eating as well as carefully considering the influence of mental health on obesity.
The relationship between mental health and obesity is complex
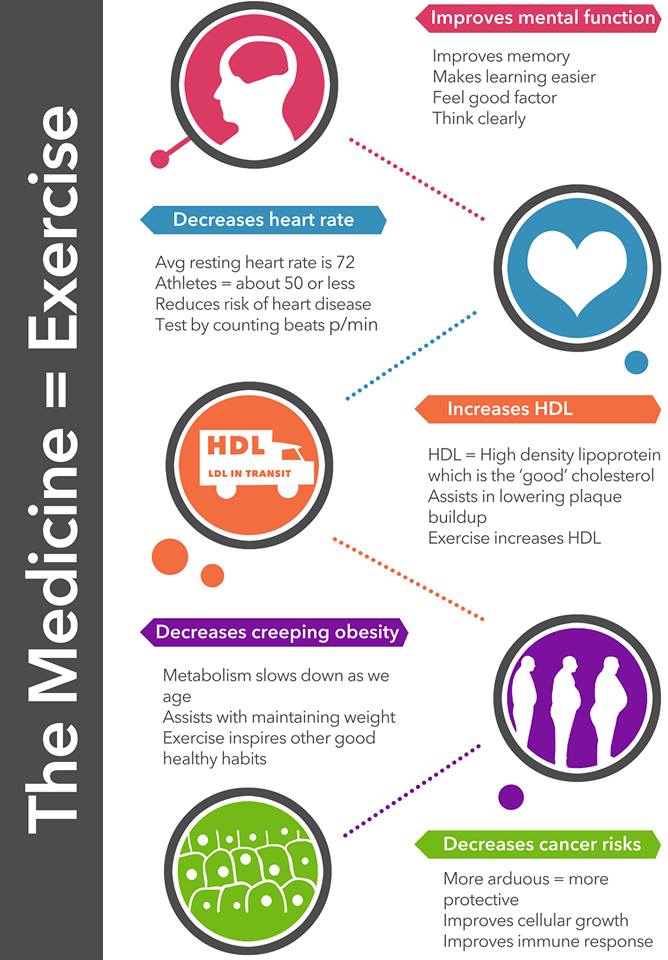
It has become increasingly clear that obesity may also be a side effect of medications used to manage mental health issues. Increased appetite or overwhelming lethargy can both contribute to undesired weight gain and the associated long-term consequences.
Moreover, the development of co-morbid conditions such as diabetes or joint pain can significantly reduce quality of life. As medication is often an essential element of treatment, diet and lifestyle changes should be first-line interventions for managing weight.
As medication is often an essential element of treatment, diet and lifestyle changes should be first-line interventions for managing weight.
General healthy eating guidelines, although indispensable, may alone not be effective in precipitating change in this patient group. Additional education is often required, to enable patients to develop a greater understanding of the relationship between food and mood, in order to make small but meaningful changes.
For example, serotonin is made from the amino acid tryptophan, which is better absorbed with carbohydrate-rich foods, which goes some way to explain ‘carbohydrate cravings’ and the excessive consumption of sweet and comforting carbohydrate foods, to boost mood. However, evidence to show that an increase in carbohydrate consumption can improve mood in the long-term, is currently lacking. The short-term reward associated with these foods can contribute to excess weight gain, and consolidate habitual behaviours that patients may struggle to change if no intervention is offered.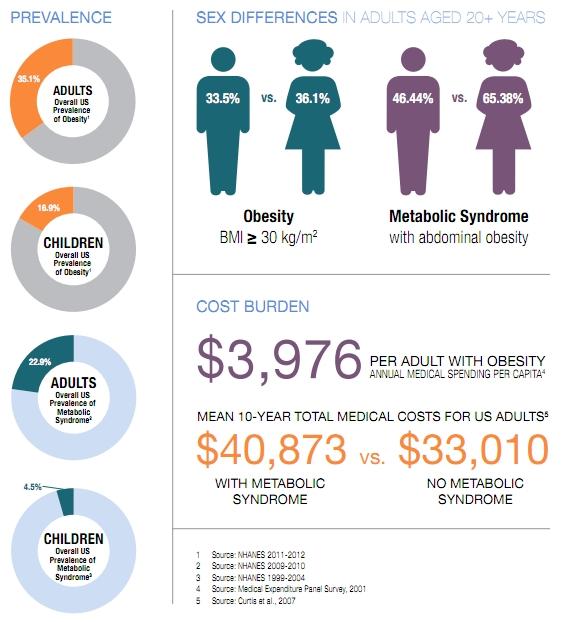
Improvements in both dietary intake and one’s relationship with food will likely result in reduced weight gain and improved mental health, which in turn is likely to improve compliance with medication.
Signs and symptoms of poor nutrition, and how it is linked to mental health recovery
The association between poor nutrition and anxiety disorders is well documented and there are many signs and symptoms a GP can look out for when making as assessment as to whether a patient may have disordered eating:
- Loose or tight clothes, belts, jewellery
- Being tired and less energetic
- Not being as capable at performing activities of daily living
- Being less physically active e.g. not being able to walk as far or as quickly as before
- Changes in mood, such as becoming depressed and lethargic
- Getting ill often, and taking a long time to recover
- Delayed wound healing
- Poor concentration
It is important to remember that weight loss or weight gain can be due to many different reasons – weight monitoring in patients is very important, and unintended weight loss should be a red flag.
What can be done in a GP consultation?
- Weight monitoring in patients taking mental health medication is essential – intervention should ideally begin as soon as weight increases are noted
- Ask questions around changes in appetite
- Have discussions around the relationship between food consumption and mood. This can help to start discussions around food choices and comfort eating
- Attempt to gain input from family and carers, if they are attending the GP consultation with the patient. This is invaluable as it is well documented that patients ‘under-report’, when asked what they are eating
Educating patients on good nutrition and mental wellbeing
Diet is a low risk, cost-effective and modifiable risk factor when considering mental health recovery. GPs should be encouraged and supported to test people for nutritional deficiencies if they suspect that their mental health problems could be linked to poor diet, and to prescribe supplements if there is a deficiency.
Carbohydrate
The ability to concentrate comes from the adequate supply of energy to the brain; up to 25% of our total glucose intake is used by the brain. It is thought that a low carbohydrate diet can lead to low mood. With the rise in popularity of ketogenic diets (high protein/high fat), it is important that patients suffering or recovering from mental health issues are aware of the role of carbohydrates in brain function and absorption of tryptophan for serotonin production.
These patients may be particularly susceptible to the enticement of fad dieting, as they may have gained weight from mental health medication and have reduced self-esteem as a result.
Iron
Low levels of iron and the resulting reduction in oxyhaemoglobin can lead to patients feeling tired, weak and lethargic. This is likely to significantly impact on an individual’s self-efficacy and mood. The risk of anaemia is reduced with adequate intakes of iron, particularly from red meat, poultry and fish. Vegetarian sources are found in beans, pulses and fortified breakfast cereals.
Vegetarian sources are found in beans, pulses and fortified breakfast cereals.
It may be helpful to ask about an anaemic patient’s consumption of tea, as tannin in tea reduces iron absorption. Avoiding tea with meals can be helpful, and drinking orange juice with iron containing foods even more so, as this will help to increase absorption.
B vitamins
Deficiencies in B vitamins can increase the feeling of tiredness, and cause patients to feel depressed and irritable. Fortified foods include wholegrain cereals and animal protein foods such as meat, fish, eggs and dairy.
B vitamin deficiency is common amongst vegans. The Vegan Society states that the ‘Veganuary’ campaign, where people eat vegan for the month of January, grew by 183% in 2018, with a whopping 168,500 participants. With veganism becoming a rising trend, it is imperative that the risk of B vitamin deficiency and supplementation is discussed for those with at risk or with a history of mental health disorders.
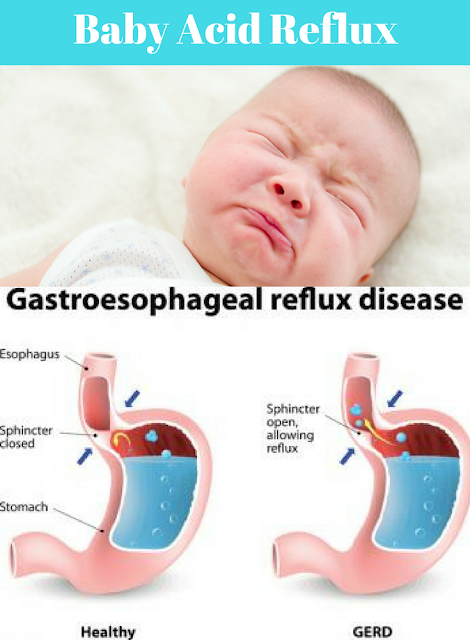
IBS, probiotics and FODMAP
Irritable bowel syndrome (IBS) is associated with higher levels of mood disorders, anxiety, and other psychiatric conditions. IBS reportedly affects up to 23% of people around the world, and although IBS is not fully understood, symptoms appear to result from a disturbance in the brain-gut axis—the line of communication that exists between the brain and the gastrointestinal tract—and may be underpinned by disruptions in the microbiome-immune interface.
The current state of the gut microbiome can be preserved by improving dietary fibre and diversity of foods to promote microbial diversity.
The gold standard for IBS management is the Low FODMAP diet for IBS, which reduces fermentation in the bowel, and allows the gut respite from ongoing fermentation by omitting long chain carbohydrates from the diet, delivered under the supervision of a specialist dietitian. With a 71% success rate of satisfactory symptom reduction at one year (as reported by Kings College London), the FODMAP diet has provided a much needed framework for IBS treatment in primary care.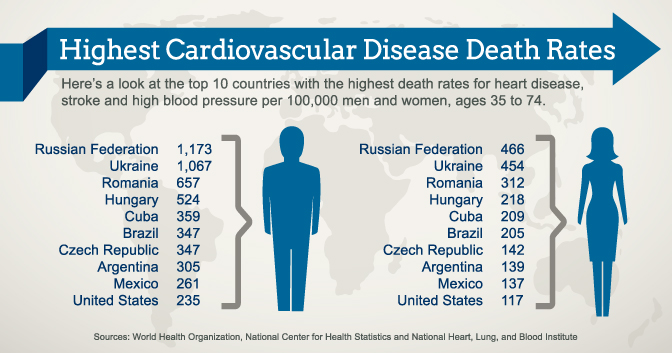
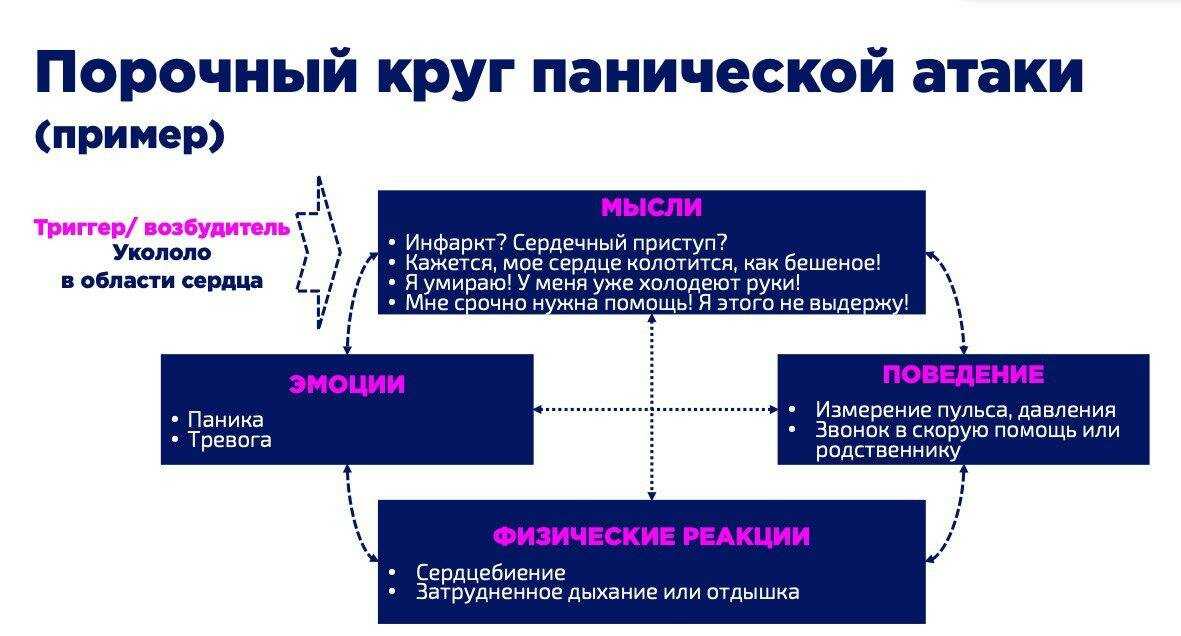
The influence of cognitive behavioural therapy (CBT)
Dietary management of IBS can improve symptoms significantly, however this is most effective when placed alongside psychological therapies such as CBT. This treatment allows the patient to understand root causes of disordered eating and teaches them how to cope better with anxiety and depression, which may lead to over-eating.
The British Society of Gastroenterology recommends psychological therapy alongside FODMAP diet as first-line treatment when the patient has a history of anxiety, panic attacks, or depression.
Obesity in secure mental health units: A call to action
https://ukhsa.blog.gov.uk/2017/02/15/obesity-in-secure-mental-health-units-a-call-to-action/
Obesity rates among the general population are increasing, rising from 15% in 1993 to 26% in 2014.
However, for those with severe mental health problems, the rate of obesity is even higher due to the effects of medication, poor diet, alcohol misuse and less active lifestyles.
In addition, life expectancy of people living with serious mental illness is 15–20 years less than the general population and the need for parity of esteem between mental and physical health is a current priority.
As part of our role to provide advice to the NHS on specialised mental health services, PHE has published a review of evidence on obesity in adult mental health secure units and what the implications are for practice.
The impact of obesity for those in secure mental health servicesCurrently, around 6,000 people in the UK are detained in three high, 65 medium and 150 low secure mental health units due to their assessed risk to others or custodial sentences.
In these units, residents are not free to enter or leave at will.
A key finding of the review was that not only is obesity and overweight more prevalent in the population detained within mental health secure units (with rates of up to 80% reported) than in the general population (around 60%), patients appear to be more at risk of weight gain when detained.
Factors influencing this include a combination of medication side effects, condition-related reduction in motivation for self-care, and environmental influences.
In mental health secure units, we also found evidence that there is a high risk of weight gain following admission, stemming from the combined effects of incarceration, ease of access to high calorific food, and the potential lack of access to recommended levels of physical activity.
The picture above highlights some of the risk factors we identified in the literature and the interaction between them
What interventions work in tackling obesity in secure mental health units?A small body of exploratory research identified as part of the review highlighted that in order to address obesity and achieve parity of esteem between mental and physical health in secure mental health units, a number of elements must be in place.
These include access to evidence based health promotion approaches and the associated training and equipment required, a range of dietary and physical activity strategies to reduce the obesogenic environment and changes in policy at ward level that address staff and patient behaviour change.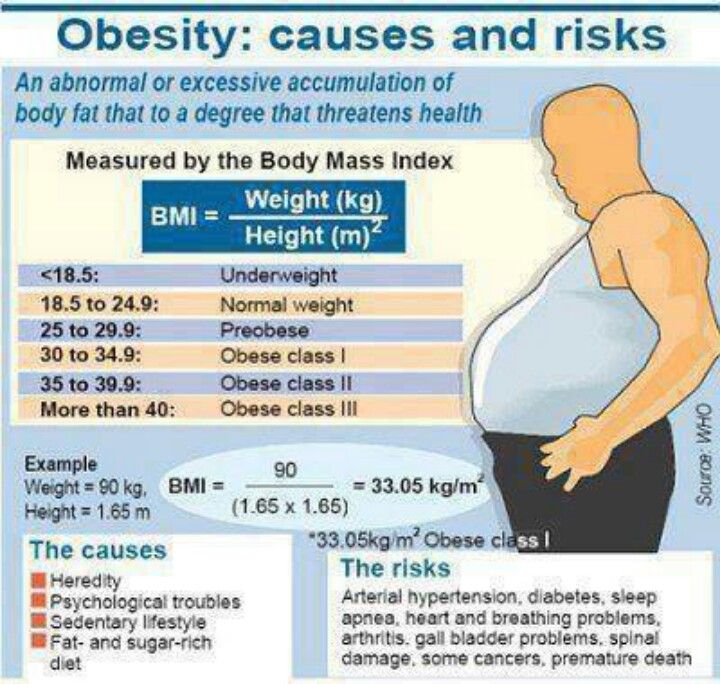
Interventions require attention to national guidance, such as NICE guidelines and policies, alignment with quality assessment and robust evaluation.
However, there is strong evidence of the need to tackle obesity on the ground in secure settings, for example the rates of obesity are high and can worsen over time with standard care.
Evidence suggests that small sequential steps are currently being made to change culture, policies, and staff and patient behaviours. However, there is much more to be explored in terms of tackling the problem.
Interventions need to be evaluated in larger-scale studies to assess how effective and applicable different approaches might be for specific populations, in particular those detained in secure units.
Our review conclusions recommend a focus on the following factors to reduce obesity and improve health and wellbeing:
- Implementing policies that increase access to healthier food choices and physical activities
- Encouraging staff to role model healthy behaviours
- Gradually changing ward or unit policy and culture to encourage healthy lifestyle choices
- Providing activities that are enjoyable and social.
These changes can also impact positively on feelings of confidence and wellbeing and help ease mental health problems.
A partnership approachAs well as reviewing published evidence we have engaged with service users, clinicians, commissioners and academics in the fields of mental health and obesity in the development of this review.
Our conversations highlighted that secure mental health services need guidance to assist decision making around some of the factors identified in our report, with food policies as well as access to NICE recommended levels of physical activity highlighted as key areas where support could be developed further.
While we know food policies in particular can be challenging to implement for a variety of reasons, the amount of calories that residents access over and above the daily recommendations for maintaining a healthy BMI can be detrimental to physical health in the long term.
We have identified this as an area that we will continue to explore along with our partner organisations including NHS England, the CQC, and of course service users and clinical experts going forwards.
The review has been undertaken in collaboration with PHE Yorkshire and Humber and the University of Sheffield, supported by a Medical Research Council grant.
Interested in receiving more blogs like this? Please sign up for updates via email or follow us on Twitter.
90,000 Fighting obesity in the UK reaches a new level. News. Channel OneIt has become unfashionable in the UK to fight overweight. There is a new trend - the struggle for the rights of those who have this extra weight. Supporters of this movement assure: it helps to preserve mental health! And doctors object: the obesity of the nation is gaining alarming proportions.
Faster doesn't mean better! Fitness instructor Carly Wilkinson is now always positive! For the peace of mind of the students, she would never say in class: let's burn calories, reduce the waist and work off yesterday's pizza. These expressions are prohibited. nine0003
“I don't think if you're healthy you're thin. It's not the same thing. You can be very thin, but not healthy. In my classes I give the opportunity to enjoy any results. I want the students to say, “Yes! I did it, I'm proud of myself! That is, the emphasis is on the capabilities of the body, and not on how you are reflected in the mirror, ”says fitness instructor Carly Wilkinson.
You can be very thin, but not healthy. In my classes I give the opportunity to enjoy any results. I want the students to say, “Yes! I did it, I'm proud of myself! That is, the emphasis is on the capabilities of the body, and not on how you are reflected in the mirror, ”says fitness instructor Carly Wilkinson.
The reflection in the mirror doesn't matter to Abby Jessop either. It was she who suggested getting rid of words that could offend overweight people. And the Union of Students of the University of Bristol supported the idea. And now there, too, about calories, either good or nothing. Otherwise, students will strive to become thin, which will lead to eating disorders such as anorexia, Jessop wrote in her article: “This rhetoric is harmful both for people with eating disorders and for those at risk. It conveys the toxic ideals of diet culture. It is clear that the preservation of such a culture is deeply damaging to the well-being of the people, and the fight against this language and misinformation in universities should be a priority.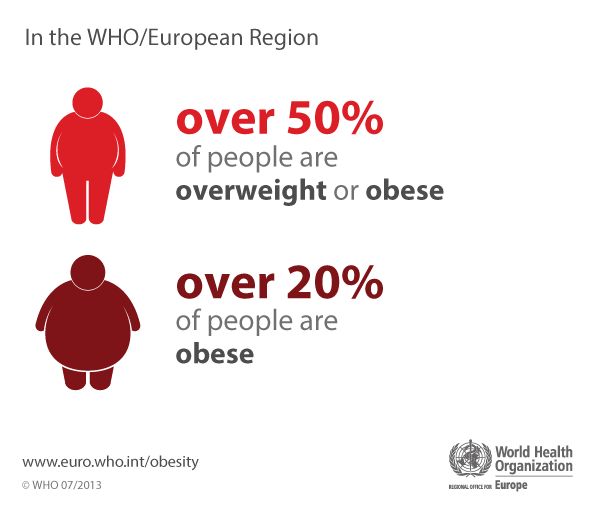 ” nine0003
” nine0003
We don't need such fitness! Or worth a try? The idea split Britain. For the ban, followers of the now fashionable concept of body positivity. They are already teaching parents how to teach their children.
“My parents advised me on diets. And they, as we know, do not work and are absolutely toxic. My advice to parents: keep diets as far away from your children as possible,” says Hanni Ross.
This is bad advice! Proven by Jen Atkin. She is also Miss Britain 2020. Jen won this title thanks to hard training. In two years, Jen lost almost 50 kilograms. nine0003
“I think that banning these expressions is a crazy idea. It's just completely demotivating. In my opinion, people should stop eating a lot and start taking their health seriously. And these phrases like “lose excess weight” only help to think about it, their ban will do even more harm than good, ”says Jen Atkin.
In each of us, regardless of weight and build, there are two people: one is an athlete, he always wants to be better, faster, stronger, and the other who likes to stay at home, watch TV, play and chew something. And this slacker in Britain is increasingly winning. As a result, obesity has already become one of the main problems here. nine0003
And this slacker in Britain is increasingly winning. As a result, obesity has already become one of the main problems here. nine0003
6 out of 10 Britons are overweight. Therefore, the authorities have developed a national program to combat obesity. The kingdom banned fast food ads on TV until 9 p.m. and forced restaurants to remove two-for-one deals on junk food. But this is not enough for experts.
“If we are to tackle obesity in Britain, we must call a spade a spade and be frank with children. They eat 2-3 times more sugar than they should. The main thing to do is to set clear limits on portions and calories for fast food and limit the content of fat, salt, sugar in it, ”said Tam Fry, representative of the National Obesity Forum. nine0003
Now obesity is doubly dangerous. Being overweight increases the risk of complications with coronavirus. The Prime Minister of Britain knows this from his own experience, therefore, after recovering from COVID-19, Boris Johnson began to lose weight. The Prime Minister is working out with personal fitness instructor Harry Jameson. What words the coach motivates the prime minister is unknown, but on his Instagram, Harry often writes that he himself burned as many calories as he could. In response, subscribers only smile and give him likes. nine0003
The Prime Minister is working out with personal fitness instructor Harry Jameson. What words the coach motivates the prime minister is unknown, but on his Instagram, Harry often writes that he himself burned as many calories as he could. In response, subscribers only smile and give him likes. nine0003
Yoair Blog - Anthropology world blog post.
Message Views: 12,437
Obesity is one of the leading risk factors for premature death, causing 4.7 million (8%) deaths worldwide in 2017. In many societies it is considered an individual problem. However, some view obesity as a social problem rather than an individual one. The UK has one of the highest rates of obesity in Europe (Littleford, 2022). In fact, the UK government considers obesity "one of the biggest health crises facing the country" (gov.uk). Public Health England (PHE) is spearheading the government's new Better Health campaign. The goal of the campaign is to encourage people to lead a healthier lifestyle and lose weight if necessary.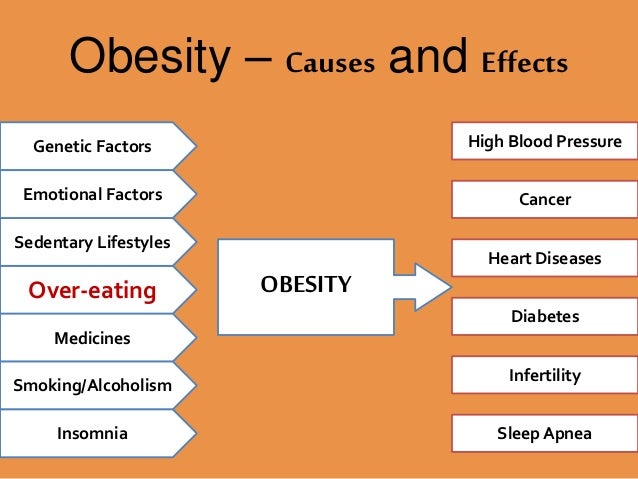 This article will examine the problem of obesity and its impact on British society. nine0003
This article will examine the problem of obesity and its impact on British society. nine0003
What is obesity?
According to the National Health Service (NHS), the term "obese" describes a person who is very overweight and has a lot of body fat. According to the NHS, the easiest and most common way to check if someone is at a healthy weight for their height is to calculate their body mass index (BMI). The formula for BMI = kg / m 2 , where kg is the weight of a person in kilograms, and m 2 is their height in meters squared. Result from 30 to 39.9 means the person is obese, and 40 or higher means the person is severely obese.
However, the NHS emphasizes that BMI is not used to diagnose obesity because heavily muscled people can have a high BMI without much fat. The NHS website also suggests that for most people, BMI is a useful indicator of whether someone's weight is healthy.
Another, more reliable way to measure excess fat is waist size, which can be used as an additional measure for overweight people.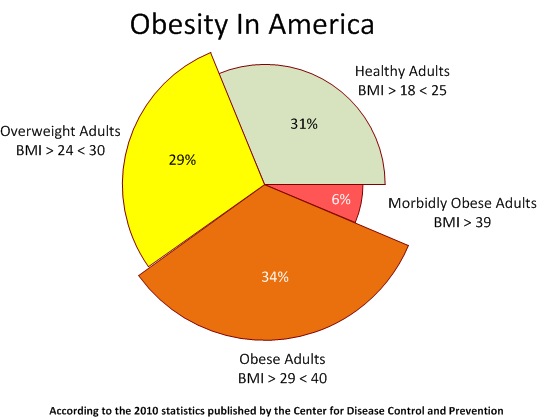 Men waist size 94 cm or more, for women, the waist size is 80 cm or more.
Men waist size 94 cm or more, for women, the waist size is 80 cm or more.
Causes of obesity
In addition to the most obvious causes such as genetics, medical causes, calories, poor diet and lack of physical activity, there are several other factors that can have a significant impact on whether a person becomes obese or not . According to the report Fighting Obesity: The Role of the National Health Service in a System-wide Approach (2021), four factors interact to shape health. These are socioeconomic factors, unhealthy behaviors, the physical environment along with social relationships, and finally , treatment and support provided by the health and care system (Holmes, 2021). nine0003
Environment
The environment in which people live can be a serious problem for a healthy diet. This is because people who are surrounded by foods that are high in sugar, salt, or fat will choose these types of foods by default. Unfortunately, fast food establishments are more prevalent in disadvantaged areas, meaning that people from disadvantaged backgrounds are more likely to have unhealthy diets and in turn become more obese than people from less disadvantaged areas (Holmes, 2021). . nine0003
. nine0003
Economic
In addition to environmental factors affecting diet, there will be an economic factor related to food prices. For many people, healthy choices are simply more expensive. In fact, only half of UK households can meet the costs outlined in the government's Eatwell Guide (Holmes, 2021).
Psychosocial factor
However, environmental and economic factors are not only related to income and choice. As noted in the report, poverty is driven by various psychosocial factors. For example, people living in conditions of deprivation experience high levels of stress that leave them lacking the mental energy to devote time to food preparation, food preparation, or the opportunity to make healthy choices (Holmes, 2021). nine0003
Why is obesity a problem?
Obesity is considered a common problem in the United Kingdom. It is estimated that it affects about 1 in every 4 adults and 1 in every 5 children between the ages of 10 and 11. This means that 25% of adults in the UK are obese.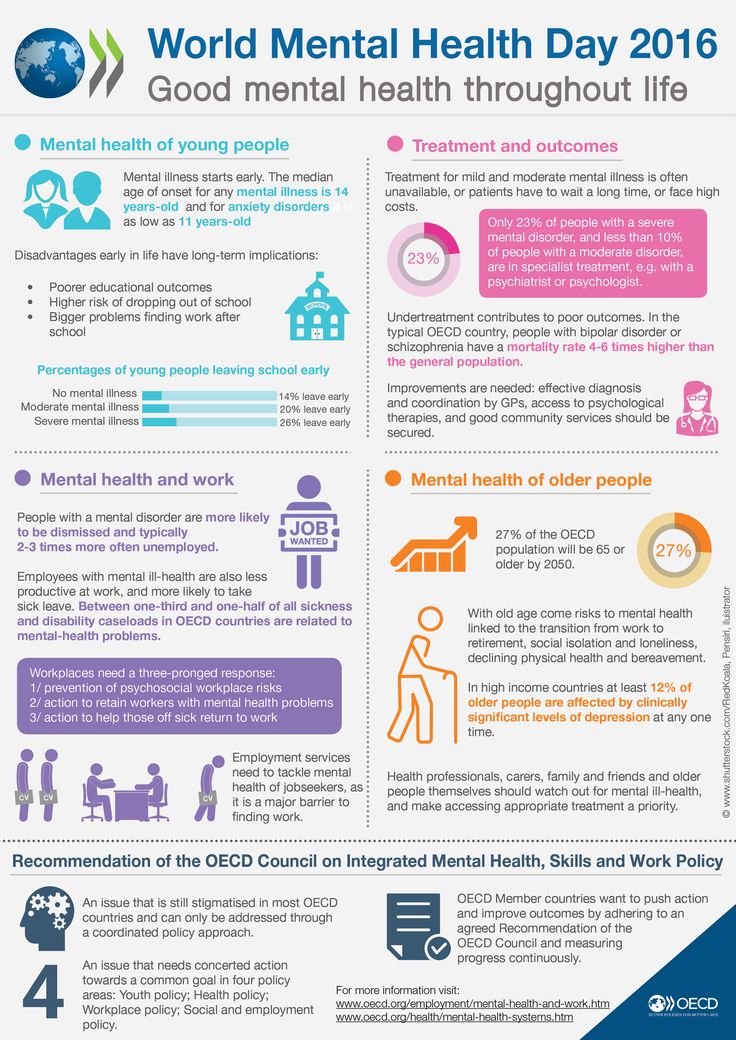 In addition, an additional 62% of UK adults are overweight (Littleford, 2022). Globally, adult obesity is more common than malnutrition. At least one third of the world's adult population is overweight or obese (Seidell and Halberstadt, 2015). The rise in obesity worldwide is leading to serious health problems and reduced quality of life. The United Kingdom has 7 million cases of diabetes, 6.5 million cases of heart disease and stroke, and 500,000 obesity-related cancers (Littleford, 2022). According to obesity research, there is evidence that obesity may be associated with a range of physical and psychosocial health problems. nine0003 UK Weight Statistics (2022) (healthexpress.co.uk)
In addition, an additional 62% of UK adults are overweight (Littleford, 2022). Globally, adult obesity is more common than malnutrition. At least one third of the world's adult population is overweight or obese (Seidell and Halberstadt, 2015). The rise in obesity worldwide is leading to serious health problems and reduced quality of life. The United Kingdom has 7 million cases of diabetes, 6.5 million cases of heart disease and stroke, and 500,000 obesity-related cancers (Littleford, 2022). According to obesity research, there is evidence that obesity may be associated with a range of physical and psychosocial health problems. nine0003 UK Weight Statistics (2022) (healthexpress.co.uk)
Obesity and increased risk of disease
Combating obesity is important because it can lead to a number of serious diseases. The main conditions associated with being overweight are:
- High blood pressure and high cholesterol
- Ischemic heart disease
- blow
- Enter 2 diabetes
- Certain cancers (eg, breast, colon, kidney, and bowel cancers)
- Diseases of the gallbladder and stones in the gallbladder
- Osteoarthritis (joint condition affecting the knees, hips or back)
- Gout (disease affecting the joints caused by excess uric acid in the blood)
- Asthma and sleep apnea (a breathing condition in which a person snores heavily and briefly stops breathing during sleep)
- Complications of pregnancy
Although not everyone who is obese has these problems, being overweight or obese increases the risk of these conditions (Ratini, 2020). nine0003
nine0003
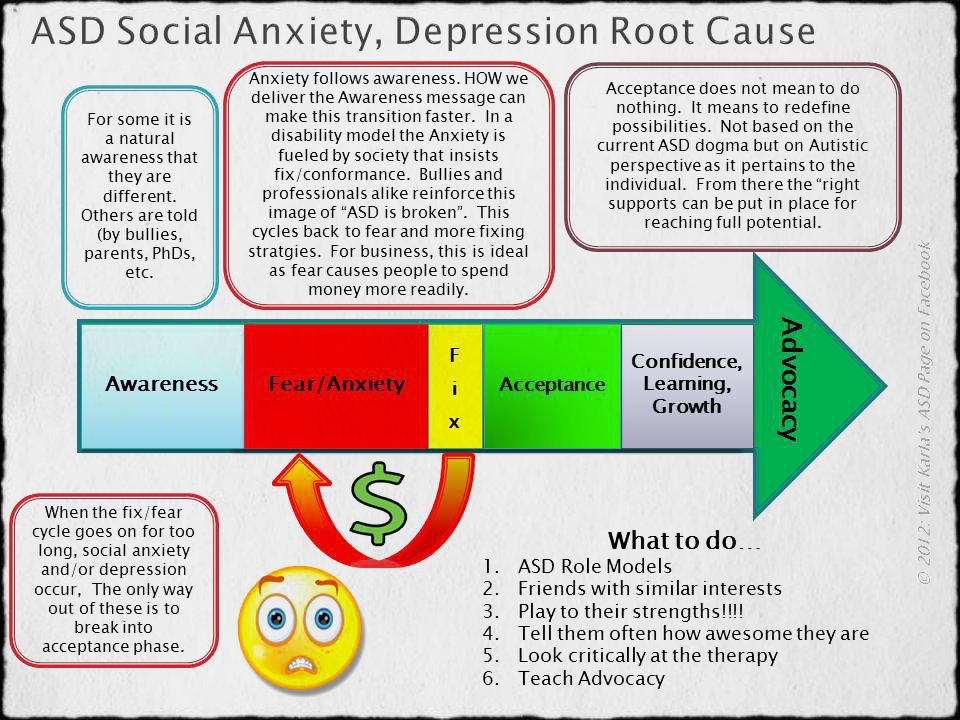
Effects of obesity on mental and emotional health
In addition to all the physical problems associated with obesity, researchers have found an association between obesity and psychosocial health problems. Being overweight affects the quality of life. Many obese people are physically unable to do what they love, such as travel. This can lead to various negative outcomes such as isolation, loneliness and even depression (Vafiadis, 2021). nine0003
discrimination
Another major problem for those struggling with weight issues is discrimination. Despite the fact that as obesity increases, so does our tolerance for it. This means that being overweight or obese has become more acceptable. Significant discrimination against people with obesity still exists in many societies. Society often creates negative stereotypes and attitudes that associate obesity with unattractiveness, laziness and indiscipline. These attitudes and attitudes can be present at work, at school, among peers, in the family, and even in medical settings. Discrimination has a significant impact on people's mental health and can lead to low self-esteem, depression and anxiety (Vafiadis, 2021). nine0003 Obesity among young people is one of the main causes of ridicule and bullying (today.uconn.edu)
Discrimination has a significant impact on people's mental health and can lead to low self-esteem, depression and anxiety (Vafiadis, 2021). nine0003 Obesity among young people is one of the main causes of ridicule and bullying (today.uconn.edu)
Anxiety
Finally, obesity can cause chronic pain as well as increase inflammation. This can lower people's immunity and may be one of the contributing factors to depression and anxiety (Vafiadis, 2021). Thus, obesity represents a public health crisis that has a negative impact on affected people. This reduces life expectancy by an average of 3–10 years (NHS). But this problem has a negative impact not only on the individual, but also on society as a whole. This is because it significantly increases the national health budget (Seidell and Halberstadt, 2015). nine0003
Economic costs of obesity
Adult obesity rates are on the rise in the UK. Over the past 25 years, the number of obese people in the UK has nearly quadrupled.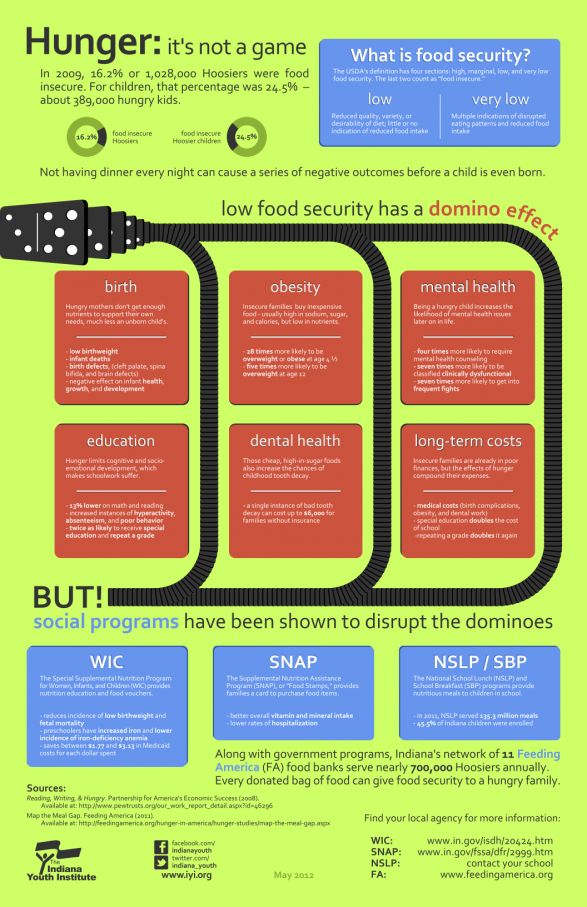 As the number of people who are overweight, obese or morbidly obese increases, the costs of treating diseases caused by obesity also increase. It has been estimated that the total cost of obesity to health services worldwide is US$990 billion per year (that's 13% of health care spending). The highest costs are in the Eastern Mediterranean and Americas regions. By 2025, the global prevalence of obesity is estimated to reach 18% in men and over 21% in women (World Obesity, 2020). nine0003
As the number of people who are overweight, obese or morbidly obese increases, the costs of treating diseases caused by obesity also increase. It has been estimated that the total cost of obesity to health services worldwide is US$990 billion per year (that's 13% of health care spending). The highest costs are in the Eastern Mediterranean and Americas regions. By 2025, the global prevalence of obesity is estimated to reach 18% in men and over 21% in women (World Obesity, 2020). nine0003
In the United Kingdom, between 2014 and 2015, the NHS spent £6.1 billion on obesity-related illnesses. According to a report by the Royal Foundation titled Fighting obesity: the role of the National Health Service in a system-wide approach, it is projected to rise to £9.7bn per year by 2050 (Holmes, 2021). Obesity is considered the biggest burden for the UK National Health Service. In the UK, the annual cost of bariatric surgery (weight loss) is in excess of £4.5 billion. In 2019In 2020, there were more than 8,000 hospitalizations of women and more than 3,500 hospitalizations of men in England alone, where obesity was the primary or secondary diagnosis. This is 17% more than in 2018-19 (NHS Digital, 2021).
This is 17% more than in 2018-19 (NHS Digital, 2021).
Obesity and children
In the United Kingdom, one in five children in the year of admission (i.e. ages 1-5) is obese. More than a third of children aged 4 years (5-6 years) are overweight or obese. Like adults, children living in poorer areas are twice as likely to be obese. nine0003
According to the data, 26% of children aged 10-11 living in disadvantaged areas are obese, while among 12-10-year-olds living in the least disadvantaged areas, only 11% are obese. Similarly, 13% of children aged 4-5 years from disadvantaged areas are obese, while only 5% of children aged 4-5 years from the least disadvantaged areas are obese (Littleford, 2022).
Obesity affects the body image of children and has negative physical and psychological consequences similar to those experienced by obese adults. Many children in the UK have problems with self-confidence and their bodies; 46% of 15-year-old girls consider themselves "too fat" compared to 23% of boys. These children are also more likely to report being bullied because of their weight (Littleford, 2022). The discrimination and stigma that leads to bullying has a significant negative impact on children's mental health and can cause low self-esteem, anxiety and depression. nine0003
These children are also more likely to report being bullied because of their weight (Littleford, 2022). The discrimination and stigma that leads to bullying has a significant negative impact on children's mental health and can cause low self-esteem, anxiety and depression. nine0003
Government strategies to combat and prevent obesity in the UK
Over the past seven years, there have been six policy changes to reduce and prevent obesity. In 2016, Childhood Obesity: An Action Plan aimed to "significantly reduce the rate of childhood obesity over the next ten years". The policy also introduced proposals to reduce the sugar content of soft drinks, which went into effect two years later in 2018 (Holmes, 2021). nine0003
In 2018, the Childhood Obesity Action Plan Chapter 2 contains a commitment to halve childhood obesity by 2030 and close the apparent obesity gap between children from the most and least disadvantaged areas (Holmes, 2021).
Next year, 2019, Childhood Obesity: Action Plan Chapter 3 Part Improving Our Health: Prevention in the 2020s aims to halve the prevalence of childhood obesity and consult on food labeling options products, as well as reduce the sugar content in food. dairy drinks (Holmes, 2021). nine0003
dairy drinks (Holmes, 2021). nine0003
Government Strategies to Prevent Obesity in the 2020s
Most recently, in 2020, a new government plan called "Fighting Obesity: Empowering Adults and Children to Lead Healthier Lives" was adopted. The policy encourages people to lose weight and commits to improving the quality of food labeling by requiring restaurants to introduce calorie labeling on menus. In addition to this, the policy aims to change the way food is marketed. This will be based on a ban on television advertising of junk food (foods high in fat, sugar or salt) after 9p.m. when children are most likely to see them (Gov.uk).
Another government action was taken in 2021 with the theme “Integration and Innovation: Working Together to Improve Health and Social Protection for All”. This policy highlights proposals, including the introduction of a calorie labeling law and a ban on advertising. In addition, it explains how the NHS should focus more on prevention and provides guidance on how this should be done in the future (Holmes, 2021).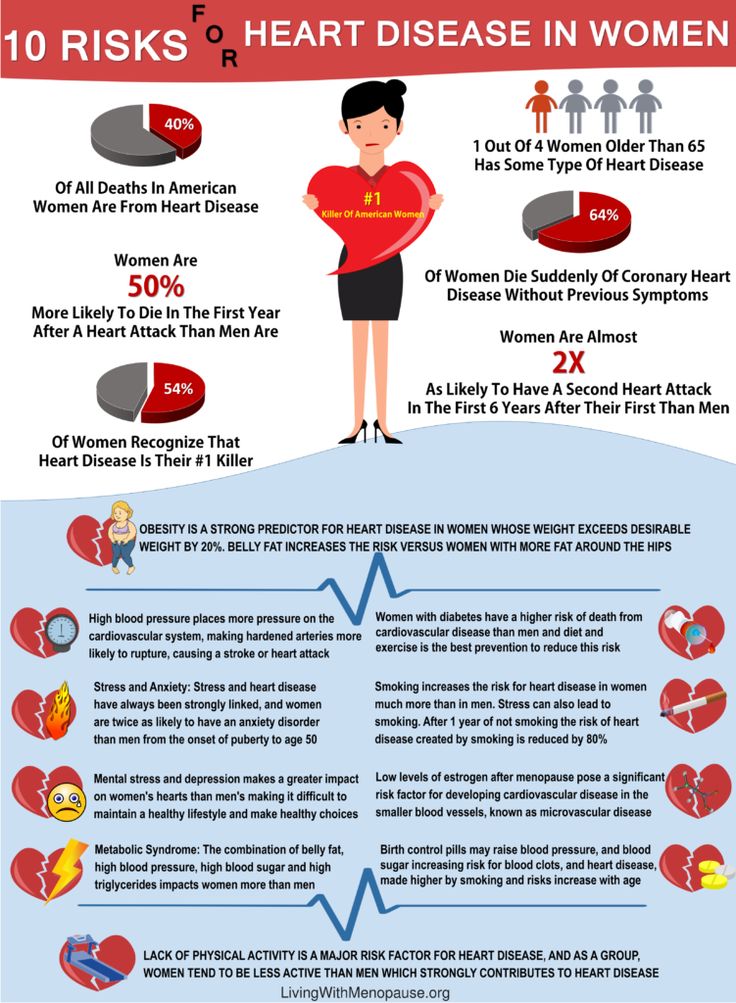 nine0003
nine0003
On Wednesday, April 6, 2022, new rules requiring calorie information to be displayed on menus and food labels came into effect after parliament approved changes in 2021. As a result, large businesses with more than 250 employees are now required by law to display calorie information - packaged food and soft drinks. Businesses include cafes, restaurants, and takeaways. Health Secretary Maggie Trope said: “It is very important that we all have access to the information we need to maintain a healthy weight, and that starts with knowing how many calories our food is. We are used to knowing this when we shop at the supermarket, but this is not the case when we eat out or buy takeaway food.” (Government.uk)
Better Health Anti-Obesity Campaign
The Better Health campaign was launched in 2020 to support people in the UK to take action and improve their health. The goal of the campaign is to improve people's well-being through simple steps towards a positive and healthy lifestyle.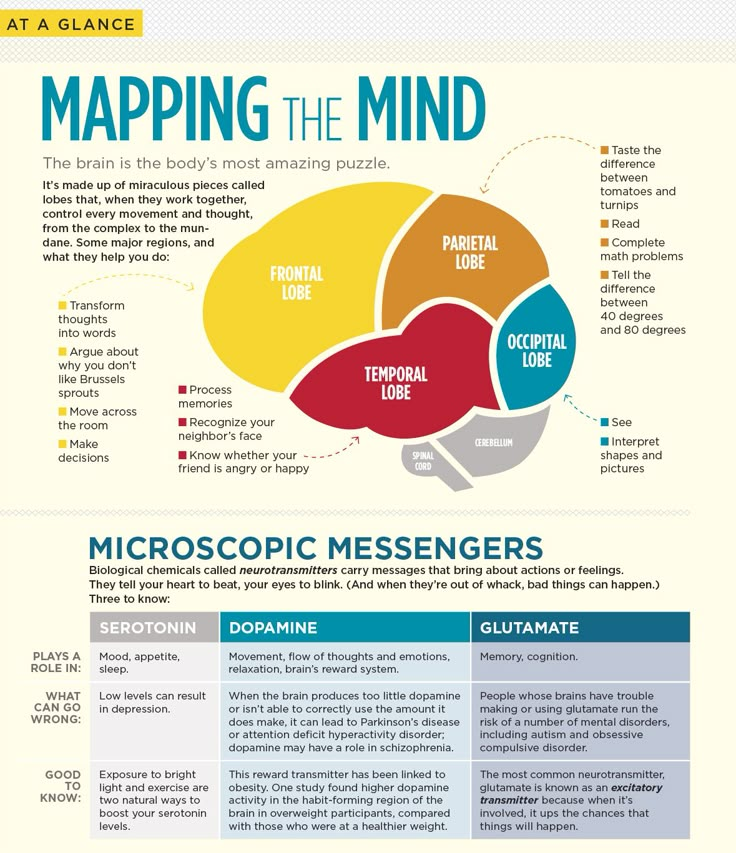 According to Talbot and Branley-Bell (2021), public reaction to the Better Health campaign has been mixed. Many people support the ideas behind the campaign, while others criticize the lack of focus on mental health and "superficial" solutions to obesity, which can do more harm than good to those suffering from eating disorders. nine0003
According to Talbot and Branley-Bell (2021), public reaction to the Better Health campaign has been mixed. Many people support the ideas behind the campaign, while others criticize the lack of focus on mental health and "superficial" solutions to obesity, which can do more harm than good to those suffering from eating disorders. nine0003
Government approaches to combating obesity are important in improving access to information. However, addressing the various complex factors that influence obesity, such as environmental risk factors, requires a much broader approach, according to a report from the Royal Foundation. For example, using taxation and facilitating healthy lifestyle choices for those who live in the most disadvantaged areas of the UK (Holmes, 2021).
The cultural significance of obesity in anthropology
Obesity is a problem studied by various disciplines. An anthropological approach to obesity focuses on the complex evolutionary background and differences in the prevalence of obesity across cultures.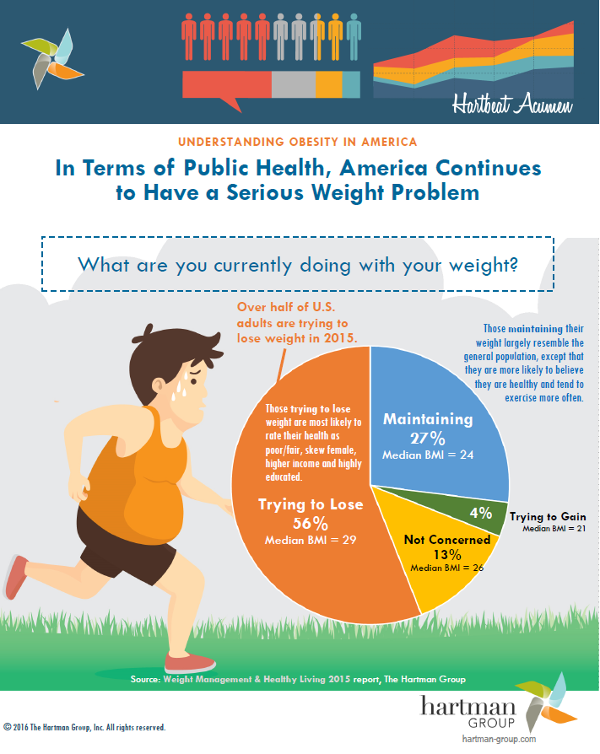 Similarly, attitudes towards obesity and perceptions of body image vary across cultures. There are cultural norms, values, and beliefs specific to certain cultures and societies that surround the look. Thus, in some cultures, obesity is seen as a sign of affluence due to the predominance of other social problems such as poverty and food insecurity. Thus, obesity is culturally significant because it affects culture, and vice versa. nine0003
Similarly, attitudes towards obesity and perceptions of body image vary across cultures. There are cultural norms, values, and beliefs specific to certain cultures and societies that surround the look. Thus, in some cultures, obesity is seen as a sign of affluence due to the predominance of other social problems such as poverty and food insecurity. Thus, obesity is culturally significant because it affects culture, and vice versa. nine0003
Links:
Gov.uk (2020) “ New obesity strategy unveiled as country urged to lose weight to beat coronavirus (COVID-19) and protect NHS.” Available: gov.uk
Government.uk (2022) "New calorie labeling rules come into effect to improve nation's health." Available: gov.uk
Holmes, J. (2021) Fighting obesity: The role of the NHS in a system-wide approach. Available: kingsfund.org.uk
Littleford, R. (2022) " Obesity Statistics: Facts and Figures in the UK". Available: HealthExpress.