Bipolar worse at night
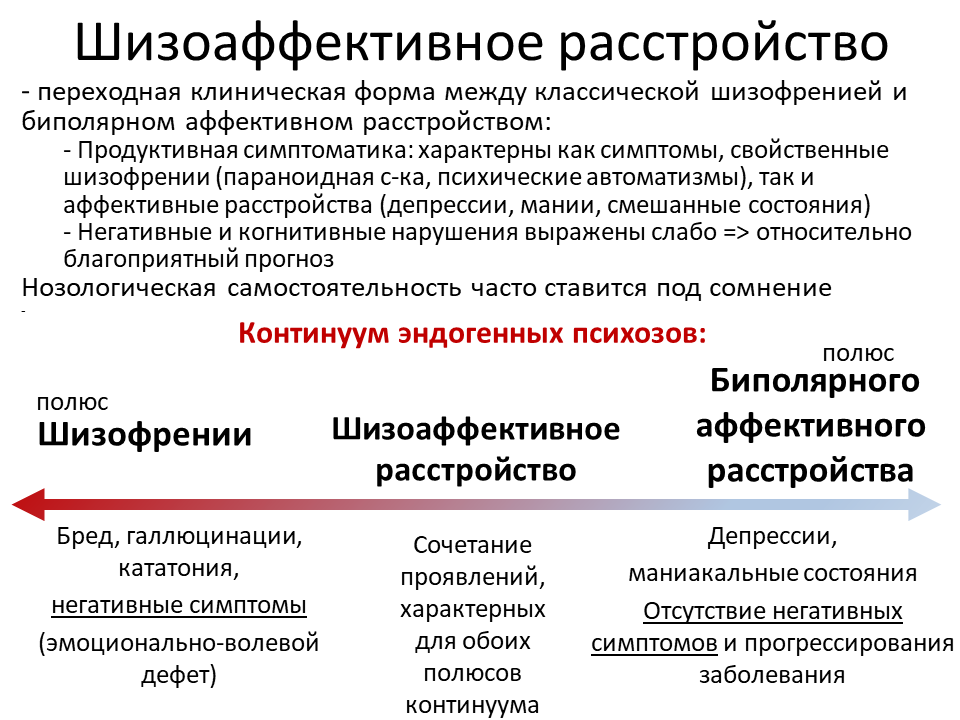
Diurnal variation in the direction of mood switches in patients with rapid-cycling bipolar disorder
Save citation to file
Format: Summary (text)PubMedPMIDAbstract (text)CSV
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Add to My Bibliography
- My Bibliography
Unable to load your delegates due to an error
Please try again
Your saved search
Name of saved search:
Search terms:
Test search terms
Email: (change)
Which day? The first SundayThe first MondayThe first TuesdayThe first WednesdayThe first ThursdayThe first FridayThe first SaturdayThe first dayThe first weekday
Which day? SundayMondayTuesdayWednesdayThursdayFridaySaturday
Report format: SummarySummary (text)AbstractAbstract (text)PubMed
Send at most: 1 item5 items10 items20 items50 items100 items200 items
Send even when there aren't any new results
Optional text in email:
Create a file for external citation management software
. 1997 Feb;58(2):79-84.
doi: 10.4088/jcp.v58n0205.
S Feldman-Naim 1 , E H Turner, E Leibenluft
Affiliations
Affiliation
- 1 Clinical Psychobiology Branch, National Institute of Mental Health, Bethesda, Md 20892-1390, USA.
- PMID: 9062377
- DOI: 10.4088/jcp.v58n0205
S Feldman-Naim et al. J Clin Psychiatry. 1997 Feb.
. 1997 Feb;58(2):79-84.
doi: 10. 4088/jcp.v58n0205.
4088/jcp.v58n0205.
Authors
S Feldman-Naim 1 , E H Turner, E Leibenluft
Affiliation
- 1 Clinical Psychobiology Branch, National Institute of Mental Health, Bethesda, Md 20892-1390, USA.
- PMID: 9062377
- DOI: 10.4088/jcp.v58n0205
Abstract
Background: We assessed diurnal variation in the direction of mood switches in a sample of outpatients with rapid-cycling bipolar disorder who were on stable medication regimens. We predicted that patients would be more likely to switch from depression into mania or hypomania during the daytime hours and from mania/hypomania into depression overnight.
Method: Fifteen patients with rapid-cycling bipolar disorder completed self-rated mood scales twice a day: once shortly after awakening and once at bedtime. Using 3 months of data for each patient, we performed categorical analyses (McNemar chi-square) to study the direction of mood switches between each day's morning and evening rating and between each evening rating and the subsequent morning rating.
Results: As predicted, switches that occurred between the morning and evening ratings were more likely to be from depression into mania/ hypomania or euthymia (64.3%) than in the opposite direction (35.6%; p < .0001). Similarly, switches that occurred between the evening rating and the next morning's ratings were more likely to be from mania/hypomania or euthymia into depression (64.8%) than in the opposite direction (35.2%; p < . 0001).
0001).
Conclusion: Extended wakefulness, exposure to light, increased activity, and/or endogenous rhythms could contribute to the elevation of mood during the course of the day. Sleep, darkness, reduced activity, and/or endogenous rhythms could contribute to the tendency to switch into depression overnight. Clinicians should attend to the time of day that clinical assessments are performed in patients with rapid-cycling bipolar disorder. Potential therapeutic implications include the use of light or activity during depression and use of induced sleep or exposure to darkness during mania/hypomania.
Similar articles
-
"Mixed hypomania" in children and adolescents: is it a pediatric bipolar phenotype with extreme diurnal variation between depression and hypomania?
Dilsaver SC, Akiskal HS.
 Dilsaver SC, et al. J Affect Disord. 2009 Jul;116(1-2):12-7. doi: 10.1016/j.jad.2008.10.016. Epub 2008 Nov 12. J Affect Disord. 2009. PMID: 19007995
Dilsaver SC, et al. J Affect Disord. 2009 Jul;116(1-2):12-7. doi: 10.1016/j.jad.2008.10.016. Epub 2008 Nov 12. J Affect Disord. 2009. PMID: 19007995 -
Risk of switch in mood polarity to hypomania or mania in patients with bipolar depression during acute and continuation trials of venlafaxine, sertraline, and bupropion as adjuncts to mood stabilizers.
Leverich GS, Altshuler LL, Frye MA, Suppes T, McElroy SL, Keck PE Jr, Kupka RW, Denicoff KD, Nolen WA, Grunze H, Martinez MI, Post RM. Leverich GS, et al. Am J Psychiatry. 2006 Feb;163(2):232-9. doi: 10.1176/appi.ajp.163.2.232. Am J Psychiatry. 2006. PMID: 16449476 Clinical Trial.
-
Relationship between sleep and mood in patients with rapid-cycling bipolar disorder.
Leibenluft E, Albert PS, Rosenthal NE, Wehr TA.
 Leibenluft E, et al. Psychiatry Res. 1996 Jul 31;63(2-3):161-8. doi: 10.1016/0165-1781(96)02854-5. Psychiatry Res. 1996. PMID: 8878312
Leibenluft E, et al. Psychiatry Res. 1996 Jul 31;63(2-3):161-8. doi: 10.1016/0165-1781(96)02854-5. Psychiatry Res. 1996. PMID: 8878312 -
Bipolar II disorder : epidemiology, diagnosis and management.
Benazzi F. Benazzi F. CNS Drugs. 2007;21(9):727-40. doi: 10.2165/00023210-200721090-00003. CNS Drugs. 2007. PMID: 17696573 Review.
-
Rate of switch from bipolar depression into mania after morning light therapy: A historical review.
Benedetti F. Benedetti F. Psychiatry Res. 2018 Mar;261:351-356. doi: 10.1016/j.psychres.2018.01.013. Epub 2018 Jan 9. Psychiatry Res. 2018. PMID: 29348073 Review.
See all similar articles
Cited by
-
Manipulating the sleep-wake cycle and circadian rhythms to improve clinical management of major depression.

Hickie IB, Naismith SL, Robillard R, Scott EM, Hermens DF. Hickie IB, et al. BMC Med. 2013 Mar 22;11:79. doi: 10.1186/1741-7015-11-79. BMC Med. 2013. PMID: 23521808 Free PMC article.
-
P2RX7: expression responds to sleep deprivation and associates with rapid cycling in bipolar disorder type 1.
Backlund L, Lavebratt C, Frisén L, Nikamo P, Hukic Sudic D, Träskman-Bendz L, Landén M, Edman G, Vawter MP, Ösby U, Schalling M. Backlund L, et al. PLoS One. 2012;7(8):e43057. doi: 10.1371/journal.pone.0043057. Epub 2012 Aug 28. PLoS One. 2012. PMID: 22952630 Free PMC article.
-
Diurnal variation of depressive symptoms.
Wirz-Justice A. Wirz-Justice A. Dialogues Clin Neurosci. 2008;10(3):337-43.
 doi: 10.31887/DCNS.2008.10.3/awjustice. Dialogues Clin Neurosci. 2008. PMID: 18979947 Free PMC article. Review.
doi: 10.31887/DCNS.2008.10.3/awjustice. Dialogues Clin Neurosci. 2008. PMID: 18979947 Free PMC article. Review. -
Sleep functioning in relation to mood, function, and quality of life at entry to the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD).
Gruber J, Harvey AG, Wang PW, Brooks JO 3rd, Thase ME, Sachs GS, Ketter TA. Gruber J, et al. J Affect Disord. 2009 Apr;114(1-3):41-9. doi: 10.1016/j.jad.2008.06.028. Epub 2008 Aug 15. J Affect Disord. 2009. PMID: 18707765 Free PMC article.
-
Clock genes may influence bipolar disorder susceptibility and dysfunctional circadian rhythm.
Shi J, Wittke-Thompson JK, Badner JA, Hattori E, Potash JB, Willour VL, McMahon FJ, Gershon ES, Liu C. Shi J, et al.
 Am J Med Genet B Neuropsychiatr Genet. 2008 Oct 5;147B(7):1047-55. doi: 10.1002/ajmg.b.30714. Am J Med Genet B Neuropsychiatr Genet. 2008. PMID: 18228528 Free PMC article.
Am J Med Genet B Neuropsychiatr Genet. 2008 Oct 5;147B(7):1047-55. doi: 10.1002/ajmg.b.30714. Am J Med Genet B Neuropsychiatr Genet. 2008. PMID: 18228528 Free PMC article.
See all "Cited by" articles
MeSH terms
Full text links
Physicians Postgraduate Press, Inc.
Cite
Format: AMA APA MLA NLM
Add to Collections
- Create a new collection
- Add to an existing collection
Name your collection:
Name must be less than 100 characters
Choose a collection:
Unable to load your collection due to an error
Please try again
Send To
Sundown Syndrome and Bipolar Disorder: Is There a Link?
Sundown syndrome refers to a specific state of confusion and agitation that shows up sometime between late afternoon and dusk and persists into the evening.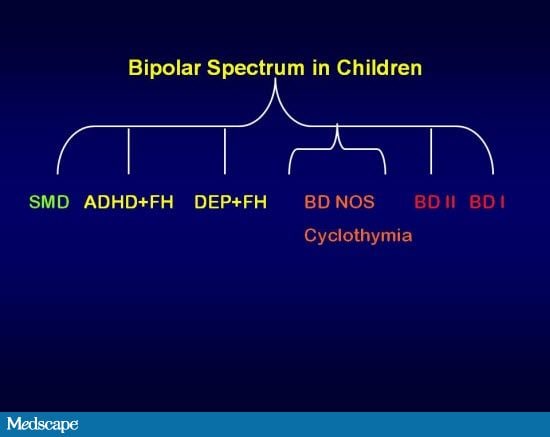 For the most part, experts associate sundown syndrome, or sundowning, with dementia.
For the most part, experts associate sundown syndrome, or sundowning, with dementia.
Scientific research has yet to identify one specific cause of sundown syndrome. One widely accepted explanation suggests the brain changes associated with Alzheimer’s disease, Lewy body dementia, and other types of dementia can affect circadian rhythms.
This disruption to the biological clock alters normal sleep-wake cycles and triggers evening confusion and distress.
To date, no research specifically links sundowning to bipolar disorder. That said, plenty of evidencedoes link bipolar disorder to circadian rhythm dysfunction and related sleep disruptions.
Without a doubt, an irregular biological clock can affect the amount of sleep you get, not to mention its quality. But can it also cause evening confusion, disorientation, and other symptoms similar to sundown syndrome?
Read on to learn more, plus get some tips to cope and get support.
Among people with dementia, sundown syndrome is fairly common, though not everyone will experience it.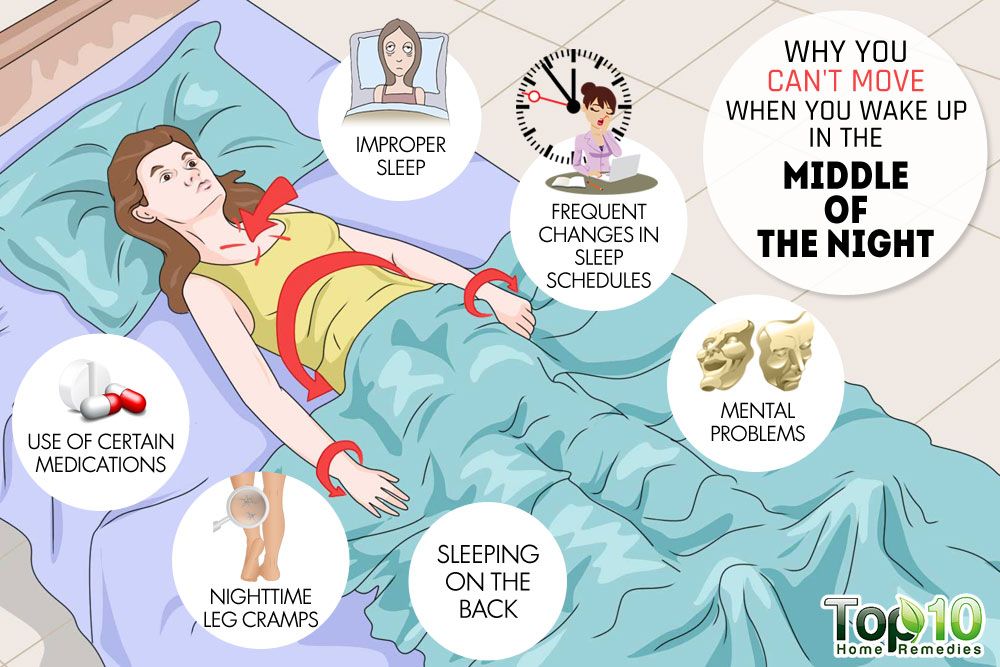
This late-day confusion can involve:
- hallucinations
- verbally and physically aggressive behavior
- anxiety or irritability
- suspiciousness or paranoia
- restlessness or pacing
- wandering
- difficulty sleeping
- lack of interest in listening to suggestions or cooperating with loved ones and other care providers
- disorientation or loss of focus
While these symptoms don’t show up at any set time — say, 4:30 p.m. — experts generally agree they appear sometime between late in the afternoon or early in the evening. In other words, when the sun goes down.
If you (or a loved one) live with bipolar disorder, many of these symptoms may sound pretty familiar. With bipolar disorder, though, symptoms can develop at any time of day. They won’t necessarily follow any set schedule.
Experts have yet to identify a bipolar-specific sundown syndrome. Still, the condition affects everyone differently, and you could absolutely notice more symptoms, or worsened symptoms, in the evening hours.
This increase in evening symptoms may happen for a few different reasons.
Body clock dysfunction
Researchers have long recognized disrupted circadian rhythms as a key characteristic of bipolar disorder.
The circadian rhythm, in basic terms, is the internal cycle that helps regulate various brain and body processes.
This cycle, which aligns with Earth’s 24-hour day, is very responsive to changes in light. That’s why you feel tired at night, when it begins to get dark, and more alert in the morning, when the sun comes up.
Yet most people with bipolar disorder experience altered sleep-wake cycles. In fact, some experts consider circadian rhythm dysfunction a key component of the condition, not to mention a major cause of sleep problems.
Sleep issues take many shapes
You might:
- have trouble falling asleep
- wake up frequently
- sleep much more than usual (more common with depression)
- need just a few hours of sleep (more common with mania or hypomania)
On the other hand, you might instead feel alert or not sleepy when evening rolls in. Or maybe you’re anxious about the amount of sleep you’re getting (or not getting).
Or maybe you’re anxious about the amount of sleep you’re getting (or not getting).
It goes without saying that you might feel somewhat cranky when you’re tired, but worried you’ll have trouble drifting off yet again.
Not getting enough sleep on a regular basis can also lead to:
- trouble focusing or thinking clearly
- irritability
- anxiety
These effects can show up throughout the day, but you could notice them more readily as the day wears on and you feel increasingly tired.
Evening chronotype
Do you consider yourself a night owl?
Some research suggests a link between “eveningness,” or evening wakefulness, and mood-related mental health conditions like bipolar disorder.
Eveningness, in short, means you favor going to bed later and sleeping in over an “early to bed, early to rise” approach.
You might burn the midnight oil because you naturally feel more energized and alert in the evening.
Still, staying up late might prove less than ideal when you still have to wake up at a specific time, since this can prevent you from getting the sleep you need. Some evidence also links eveningness to more severe symptoms of depression.
It’s worth considering, too, that you might simply be more attuned to changes in your mood and other bipolar symptoms when you feel most alert — in the late afternoon and early evening.
If everyone around you seems relaxed, calm, and ready to wind down, any irritability, anxiety, or restlessness you experience might stand out even more.
On the flip side, you might also feel restless or anxious if the approaching evening brings feelings of distress. If you dislike night, for whatever reason, this sense of disquiet could worsen your mood, especially when you can’t find relief in sleep.
Medication side effects
Bipolar medications can do a lot to improve symptoms and help reduce mood episodes.
Still, like most medications, they do carry some risk of side effects, some of which may resemble sundowning symptoms.
No clear-cut evidence links evening symptoms to bipolar medications, but a few possible links exist:
- Agomelatine, a medication that binds to melatonin receptors, may help stabilize circadian rhythms, but limited evidence suggests it might prompt symptoms of mania or hypomania in some people taking lithium for bipolar II.
- Lamotrigine (Lamictal) can help reduce mood episodes. Anxiety and sleep problems number among its commonly reported side effects, but some people also report more serious effects, including restlessness, anger and irritability, and aggressive behavior.
- Some people taking lithium, a medication commonly prescribed to treat mania, report problems with memory, concentration, and mental sharpness.
- Some atypical antipsychotics and antidepressants used to treat bipolar disorder work by blocking the neurotransmitter acetylcholine. These medications could, in some cases, lead to side effects like confusion and problems with memory, concentration, and attention.

Keep in mind, though, there’s nothing saying these symptoms always show up later in the day. But if that’s when you tend to notice them, sundowning might sound like the best way to describe your symptoms, even if that’s not what’s actually going on.
Bipolar subtype
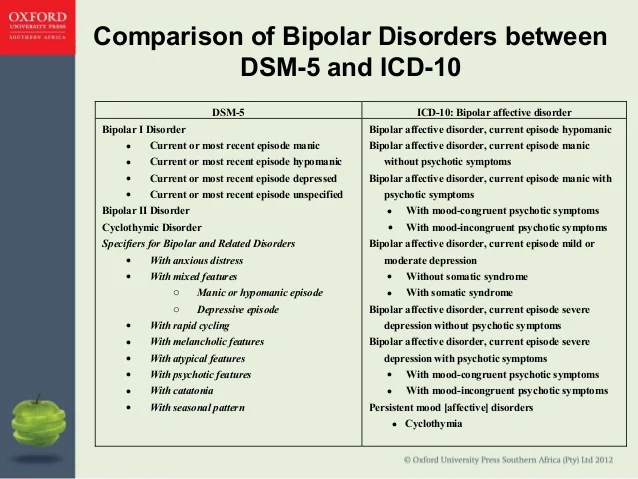
Different types of bipolar disorder exist, and these subtypes can involve different symptom patterns.
Bipolar with mixed features involves a combination of manic and depressive symptoms in the same mood episode. Mania might leave you needing little sleep and feeling more alert than usual, while depression might provoke irritability or anger, restlessness, and trouble concentrating.
If you’ve never had a mixed episode before, you might feel disoriented and confused, not to mention distressed, by the unusual symptoms.
With rapid cycling bipolar disorder, your mood could shift over the course of the day. When symptoms of depression or psychosis, including irritability, paranoia, or disorientation, come on in the evening hours, they can closely resemble sundowning symptoms.
There’s also late-onset bipolar disorder to consider. Bipolar mood symptoms often begin by early adulthood, but the condition can show up for the first time in later life. That means older adults can develop the condition alongside dementia and experience symptoms of sundowning as well as mood episodes.
Therapy, medication, or a combination of the two tend to have the most benefit for improving symptoms of bipolar disorder.
Still, plenty of lifestyle changes can make a difference, too. The tips below may be particularly helpful for symptoms that seem to worsen as night falls.
Keep a consistent schedule
Routines and activities that change from day to day can affect your circadian rhythm and lead to an irregular sleep-wake cycle.
Maintaining a consistent schedule can help regulate your internal clock and improve your sleep as well as your mood. As much as possible, try to stick to a set timeline for:
- getting up in the morning
- meals
- starting and finishing work
- physical activity
- relaxation and hobbies
- going to bed at night
Even making a few changes where possible can help.
Maybe your job requires you to work varying hours, and there’s nothing you can do about that. You could, however, try waking up and going to sleep at the same time each day, instead of sleeping in when you have later shifts.
Exercise
Regular physical activity can help restore a consistent circadian rhythm, plus:
- promote better sleep
- ease feelings of anxiety and depression, and in some cases, hypomania
- reduce stress
- improve quality of life
If you’re able to exercise, current guidelines suggest aiming for about half an hour of physical activity most days of the week.
Tip: Consider a morning or afternoon walk, bike ride, or hike to reap the added benefits of nature and natural light.
Follow natural patterns of light and dark
You can use daylight to switch back to a 24-hour sleep-wake cycle:
- Open curtains or spend a few minutes outside after you wake up to catch some sunlight.
- Try to get some time outside during the day to remind your body it’s daytime.

- Turn on lights indoors on rainy or overcast days.
- In winter, when night falls early, use indoor lighting to stay alert and awake.
- Dim lights and turn off screens when you’re ready to wind down for bed — usually about an hour or two before bedtime.
You can also try light therapy to boost natural light exposure during the winter months, or if you don’t get a lot of sunlight where you live.
Start a wind-down routine
An ideal bedtime routine typically starts long before the clock informs you it’s time to dive under the covers.
Swapping stimulating activities — think loud music, intense workouts, or flashy video games — for more soothing ones can help your brain ease into bedtime mode.
Consider these relaxing activities in the hours before bedtime:
- taking a warm bath
- trying meditation or guided imagery
- reading a book
- listening to soft music
- working on a puzzle
Picking up a few calming hobbies can help relieve stress, which could improve mood symptoms while helping you feel more ready for sleep.
Take it further: Transform your room into the perfect sleep environment.
In almost all cases, bipolar disorder requires professional treatment.
While you can take steps to reduce mood episodes and ease symptoms on your own, support from a trained mental health professional is usually key to lasting improvement.
If you believe you could have bipolar disorder, connecting with a therapist as soon as possible can put you on the path to exploring effective treatment options and getting relief. Therapists can also offer more guidance on navigating sleep problems and other nighttime distress.
Reaching out to a therapist becomes even more important if you notice unusual evening wakefulness along with fogginess and difficulty concentrating, restlessness, irritability, or any mix of mania and depression. Mixed mood episodes are serious, so it’s best to get help right away.
Already working with a therapist? Don’t hesitate to mention any changes in the pattern of mood episodes, such as symptoms that suddenly get worse at night.
Your therapist can help you identify possible causes and consider alternate approaches to treatment, if needed.
Experts still have more to learn about the causes of bipolar disorder and how it affects sleep-wake cycles.
Circadian rhythm disruptions could very well factor into symptoms that seem to get worse at night, but other factors might also play a part.
It’s always worth mentioning any new or unusual symptoms, including changes in when they appear, to your therapist or other healthcare professional.
Crystal Raypole writes for Healthline and Psych Central. Her fields of interest include Japanese translation, cooking, natural sciences, sex positivity, and mental health, along with books, books, and more books. In particular, she’s committed to helping decrease stigma around mental health issues. She lives in Washington with her son and a lovably recalcitrant cat.
7 rules for a fulfilling life with bipolar disorder
June 18, 2020 A life Speaker
Daily routine, proper nutrition and mindfulness will help to cope with mood swings.
Masha Pushkina
Founder of the Bipolar Association, author of the books Bipolar People: How Bipolar People Live and Dream About and Bipolar Disorder: A Survival Guide.
For three years I have been leading a community that brings together people with mood disorders and their loved ones. These are very different personalities - from schoolchildren to company leaders, but they all have a common problem: sharp and often unpredictable swings of emotions that affect all areas of life. Many understand that medication and psychotherapy can help curb mood swings. But not everyone is ready to admit that the results of treatment largely depend on themselves - their daily activities and lifestyle. Bad habits can trigger disease attacks and slow down treatment, while good habits help maintain balance. nine0003
1. More order, less chaos
I know very well how hard it is for a creative person to keep within limits. After all, you really want to ride on a wave of mood: either hang out all night long or work 20 hours in a row on an interesting project, or spend weeks watching TV shows without leaving your room. But a chaotic lifestyle is exactly what shatters an already unstable psyche.
But a chaotic lifestyle is exactly what shatters an already unstable psyche.
The more order in the life of a bipolar person, the smoother his mood. In addition, if you are used to a certain regime, it will be much easier for you to maintain it even in depression - automatically, without gigantic volitional efforts. nine0003
The most important components of the daily routine:
- Quality sleep. At least 8 hours per night, at the same time. During periods of depression, it is normal to sleep more, but for a couple of hours, not twice.
- Stable operation. Even if you are a freelancer, try to work around the same time and the same number of hours in a row. Night shifts, and even more so their alternation with day shifts, are categorically contraindicated.
- No gadgets or activity before bed. The bipolar brain can be very difficult to calm down, thoughts are spinning in it without stopping. To fall asleep normally, you need to exclude external stimulation an hour or two before bedtime.
 A common culprit for insomnia is gadgets with bright screens. nine0022
A common culprit for insomnia is gadgets with bright screens. nine0022 - Regular walks or outdoor exercise. Even if you have to literally force yourself to get out of the house, the sun and fresh air improve your mood - it's a fact!
2. The support of loved ones saves
When you either shock others with crazy ideas, or lie low, turning off your phone, it's easy to lose friends. But the support of understanding loved ones is what can save you at the most difficult moment.
First, it is an outsider's perspective: if a friend knows you well, he will notice suspicious changes and advise you to take action. Secondly, when you are understood and supported, it is easier to get through difficult times. nine0003
It is very important that during the days of deterioration there is a person who is aware of what is happening and does not blame you for it. Discuss with your loved one in advance what measures he can take if he notices something is amiss. And don't forget to thank him when you feel better.
If your relatives do not recognize and do not understand your problems, look for support elsewhere. For example, in support groups that exist both in real life and online.
3. Mindfulness is important
Many associate mindfulness with yoga and Buddhist practices. But this is a universal skill, very useful for people who are constantly captured by a storm of emotions. It is needed to notice changes in mood in time, track what could have caused them, and separate emotions from facts. nine0003
One popular technique is to keep a mood chart. Every day, you rate your mood on a 10-point scale, enter information about medications and triggers (that is, events that provoke deterioration in you).
There are many smartphone apps for developing mindfulness and other self-control skills. I can recommend Brain.fm, Daylio, Mood Tracker, Woebot, DBT.
appbox fallback https://play.google.com/store/apps/details?id=com.woebot&hl=ru&gl=ru
appbox fallback https://apps. apple.com/ru/app/1305375832
apple.com/ru/app/1305375832
appbox fallback https://play.google.com/store/apps/details?id=com.brainfm.app&hl=ru&gl=ru
Download
Price: Free
Download
Price: Free
Download
Price: Free
4. Less stress
Strong stress is one of the main enemies. The psyche of a person with bipolar disorder is much less resistant to excessive stress. Stress can trigger another mania or depression. Just take it for granted and do not demand great feats from yourself. It is possible that trials and “coming out of the comfort zone” really harden someone, but this is definitely not about people with mood swings. nine0003
But that doesn't mean that you don't need to work on your stress resistance: it can be increased within reasonable limits if you take a feasible load and give yourself time to rest and recover as soon as you feel worse.
The key principle here is self-care. It is especially important during depressive periods, when energy is at zero and any little thing can bring you to tears. The best thing to do at a time like this is to take a break and relax, reducing things to the bare minimum. This is much better than heroically dragging them to a nervous breakdown. nine0003
In hypomania, it is important to be careful not to pile on projects that will simply crush you with their weight as soon as the wave of euphoria subsides.
5. Complete meals on schedule
Rapid fluctuations in blood sugar contribute to mood swings.
So it is important to eat a normal lunch on time, and not snack on sweets and fatty fast food on the go.
In addition, it is common for people with bipolar disorder and depression to eat mountains of goodies when they are in a bad mood, or to eat at night when they cannot sleep. Over the years, this habit leads to very unpleasant consequences, from excess weight to diabetes. nine0003
nine0003
When taking medicines, you need to be especially attentive to the diet, because many of them increase appetite.
In addition to the quantity of food, its quality is also important. The Mediterranean diet is considered the most useful for nourishing the brain - more greens, fish and fruits, and less starchy, sweet and fatty. And if you do not live by the sea, nutritional supplements - omega-3 acids - can replace the lack of fish.
6. Exercise for the mind
Mental abilities are much less affected in bipolar disorder than in other mental illnesses. But people who are prone to prolonged depression almost always complain of a deterioration in attention, memory, and logical thinking. nine0003
During mood swings, the brain works "with a scratch". I want to “stupid” all day and flip through social networks. But in order not to become irrevocably stupid, it is necessary to regularly give yourself mental tasks, even small ones.
Remember the expression "cognitive rehabilitation" - this is a specially designed training of cognitive functions. And to put it in very simple words, exercises that help restore and maintain mental abilities at a good level.
And to put it in very simple words, exercises that help restore and maintain mental abilities at a good level.
Here, for example, is one of the popular programs. nine0003
Download
Price: Free
Download
Price: Free
7. No drugs
Bipolar disorder is probably the only disease that can be enjoyed, albeit with health risks. After all, the bipolar brain often captures a feeling of euphoria without any external reasons. But this means that additional doping (strong alcohol, a lot of cigarettes in a row, all kinds of prohibited substances) is doubly dangerous. From it can literally "break the roof": in people with a tendency to manic episodes, stimulant substances can cause a real psychosis. It can manifest itself in the form of hallucinations, panic attacks, memory lapses, suicidal thoughts, aggression, and a host of other unpleasant things. In addition, people with mood disorders are many times more prone to harmful addictions than healthy people. nine0003
nine0003
It is important to remember that psychotropic substances are incompatible with drug treatment, their combination can be very dangerous.
Read also 🧐
- What is bipolar affective disorder and how to live with it
- How to recognize alcoholism, depression and other mental disorders
- 12 signs of an anxiety disorder
how I live with bipolar affective disorder
This text was written by a reader in the Community. Carefully edited and formatted according to editorial standards.
Daria Borisova
found out that she suffers from bipolar disorder
Author profile
In September 2021, when I was 25, my husband and I immigrated to the United States. Six months later, I was diagnosed with bipolar affective disorder.
I suspect that the disease began to develop earlier, back in Moscow, when we were preparing to move. Then for the first time I felt bad and turned to a psychologist. In general, communication with him helped: it became easier for me. But, as time has shown, not for long.
In general, communication with him helped: it became easier for me. But, as time has shown, not for long.
What is bipolar affective disorder
Medical edition
on guard of health
Bipolar affective disorder, or BAD, is a mental illness that is manifested by sharp mood swings: from excessively elevated, that is, episodes of mania, to excessively depressed, episodes of depression.
Bipolar disorder differs from ordinary mood swings in the duration of the changes. If a healthy person feels melancholy or inner uplift for several hours, then in a patient with BAD episodes last from several weeks to 3-6 months. nine0003
In addition, with BAD, the ups and downs in mood are brighter, they interfere with a normal life and work. During manias, a person sleeps little, talks a lot, and jumps from one idea to another. May buy things that he cannot afford, take risks, engage in promiscuity, be obsessive and aggressive. A milder version of mania is hypomania. In this case, the symptoms are not so bright, so loved ones may not even notice the changes.
In this case, the symptoms are not so bright, so loved ones may not even notice the changes.
During episodes of depression, a person, depending on the severity, may feel increased sleepiness or, conversely, insomnia, feel guilty, helpless and irritated. Some people have thoughts of suicide. nine0003
It happens that the symptoms of mania and depression are combined in one phase: the patient simultaneously feels a surge of energy and is in a depressed state. Such episodes of BAD are called mixed.
The number of episodes and their order cannot be predicted. In the intervals between exacerbations of the disease, a person usually feels normal.
The exact causes of bipolar disorder are unknown. It is believed that the disease develops due to an imbalance in the brain of neurotransmitters: serotonin, norepinephrine and dopamine. These substances are responsible for the "communication" of nerve cells with each other. The risk of getting sick is higher in those whose relatives already suffer from BAD. The average age of onset is 25 years. Although it also occurs in children and adolescents. nine0003
The average age of onset is 25 years. Although it also occurs in children and adolescents. nine0003
There is no cure for bipolar disorder, but with the right therapy it is possible to achieve a long-term remission - a state in which the symptoms of the disorder do not appear.
Patients are usually recommended drug therapy in combination with psychotherapy: normotimic drugs that stabilize mood, antidepressants that help cope with depression, neuroleptics that relieve excessive arousal. Medicines and their dosage are selected by a psychiatrist individually.
Patients receiving care continue to lead normal and productive lives. Without treatment, the disorder worsens: episodes of depression and mania become more frequent and become more severe over time. nine0003
Why I went to see a psychologist
In Russia, I worked as a pediatric dentist. After the move, my husband and I set out to earn our living illegally for about a year, and then we had to get a work permit. I planned to enter a local university in order to confirm my qualifications and continue my medical practice in the United States.
I planned to enter a local university in order to confirm my qualifications and continue my medical practice in the United States.
To prepare for emigration, I watched videos on YouTube. In them, people who moved to the United States shared the problems they faced after moving. A lot of their stories scared me. For example, they said that illegal workers can be thrown away with pay, that a decrease in social status is difficult to survive psychologically, and many families cannot withstand difficulties after moving and break up. Therefore, six months before the trip, I decided to turn to a psychologist to help me mentally prepare for the upcoming changes. nine0003
/psychotherapy/
How psychotherapy works
Around the same time, my workload increased at the clinic where I worked. Due to stress, sleep was disturbed: I slept 12, and sometimes 15 hours a day. During periods when she was especially worried, rashes appeared on her body. I was sure that all these problems were “from nerves”, so I hoped that a psychologist would also help with them. I did not turn to other specialists.
I was sure that all these problems were “from nerves”, so I hoped that a psychologist would also help with them. I did not turn to other specialists.
I found a psychologist on the recommendation of a friend. At the first appointment, he simply listened to my complaints without offering any tests. The specialist explained the deterioration in my well-being by the desire to get away from reality - he advised me to move more, go out more often and have fun. One session with him cost 5500 R. In total, we had 10 of them.
As a result of the consultations, I got what I wanted: I felt more confident before the trip, I began to worry less. My rashes are gone. Only sleep did not improve: on weekends I slept both at night and during the day.
Now I think that the episode in Moscow was a mild form of depression. And the stress from the move led to the fact that the disorder worsened.
See a doctor
We do not make recommendations in this article. Please consult with your doctor before deciding on treatment. The responsibility for your health rests solely with you. nine0003
The responsibility for your health rests solely with you. nine0003
How I felt worse
In the USA, the most difficult thing for me was the lack of a legal job: I had to give up my specialty and do manual labor. It seemed that seven years of study at a Russian university had been flushed down the toilet and hopelessly lost. Nevertheless, the first two months after the move, I felt fine, and later I again felt an irresistible craving for bed.
The condition worsened gradually. At first, I tried to lie down in any free time, especially on the way to work in the car, and later I slept for days on end. nine0003
/mental-stat/
How many Russians suffer from mental illness
The world was gradually turning gray, a feeling of emptiness grew inside, my appetite disappeared, I ate only out of inertia. At the same time, the sight of food was disgusting. I stopped taking care of myself, rarely washed my hair, did not do makeup. In shopping malls, I was scared by loud noises and bright lights.
I often didn't know where I was. I could wander around the parking lot for hours, forgetting where I parked.
The new symptoms were much worse than those I experienced in Moscow. If then I would rate the severity of my condition as a three on a ten-point scale, then this time it was a full nine.
In addition, I had suicidal thoughts. Only a complete lack of strength and, oddly enough, thoughts about our cat kept me from attempting suicide. For some reason, it seemed to me that no one but me could take care of him.
My treatment
AntidepressantsAs soon as the first symptoms of the disease appeared, I complained about them in correspondence with a good friend in Moscow. She offered the help of her friend, a psychiatrist and psychotherapist rolled into one, who was ready to consult me online.
At first I had doubts: I was afraid that the specialist would discuss my well-being with a friend. But then I realized that a professional would not do this, and agreed.
/list/psihiatr/
12 important questions for psychiatrist Kirill Sychev
The first consultation took place on the 20th of November. The doctor treated me very carefully: she asked me about the problems and everything that preceded them. We even dug into my past and discussed childhood traumas. As a result, she diagnosed me with a "depressive episode" and prescribed antidepressants from the group of selective serotonin reuptake inhibitors - escitalopram.
In addition, the psychiatrist recommended not to work at night, to adhere to a certain daily routine and not to take alcohol, as it is incompatible with antidepressants. nine0003
There were difficulties in getting the medicine. A doctor from Russia inspired me with confidence, so I did not look for another specialist in the USA. Moreover, I did not have medical insurance, and local friends scared me that going to a psychiatrist privately was expensive. I had to ask my friends to buy an antidepressant in Moscow and send it to the USA by Russian Post. I paid 7,000 R for the first batch of the drug, and the shipment cost 3,500 R.
I paid 7,000 R for the first batch of the drug, and the shipment cost 3,500 R.
What will happen to drugs in Russia: we analyze 5 groups of psychiatric drugs
An antidepressant that I bought in MoscowI waited for the medicine for about a month. All the while, my condition continued to deteriorate. On New Year's Eve, I could no longer get out of bed and just wanted to die. To reassure my friends and husband, I promised them that I would wait for treatment and not do anything to myself.
The doctor supported me: we did psychotherapy via video link. Used cognitive-behavioral therapy of the third wave. This technique teaches you to accept your feelings, work through negative experiences, take responsibility and not run away from problems. nine0003
Sometimes the doctor gave me interesting tasks, such as brushing my teeth consciously. Every day for three minutes I had to concentrate only on brushing my teeth, paying attention to what my tongue, gums and teeth felt.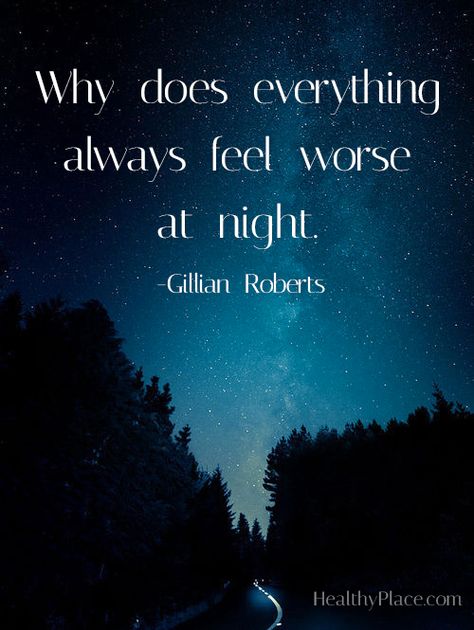 The task was difficult, but it helped to "ground" and not be carried away by thoughts into the clouds.
The task was difficult, but it helped to "ground" and not be carried away by thoughts into the clouds.
One session with a psychiatrist cost $40 (2537 R), in total I went through six of them.
In January 2022, I started taking escitalopram, the improvements were not immediate. On the recommendation of the doctor, I gradually increased the dosage, and at some point I noticed that I felt better. And after another couple of weeks, I felt not just good, but great. nine0003
It felt like I was moved to a rainbow with unicorns. I stopped sleeping at night, joked and laughed a lot, sometimes just lying on the floor laughing. I was infuriated that others did not share my fun and did everything too slowly.
/list/antidepressant-facts/
10 facts to know before taking antidepressants
Thoughts were spinning in my head like a carousel that I couldn't stop.
Feeling better, I ordered a second batch of an antidepressant from Moscow. I scored 14,000 R. I did not pay for the shipment, because the drug was transferred to the USA with a friend. nine0003
I scored 14,000 R. I did not pay for the shipment, because the drug was transferred to the USA with a friend. nine0003
I liked the state of euphoria, but it alerted the psychiatrist. She explained that antidepressants provoked a pathologically elevated mood - hypomania. And this is a sign of bipolar affective disorder, or BAD. So I heard my diagnosis for the first time.
The doctor insisted that I stop taking the antidepressant - but not immediately, but gradually reducing its dose. Otherwise, due to the abrupt withdrawal of the drug, depression could return with renewed vigor. I was also prescribed a normothymic - valproic acid. The doctor warned that drug therapy should not be abandoned, but continued with a new drug, otherwise hypomania could develop into mania - excessive activity, which is often dangerous. nine0003
I again had to wait for a drug from Russia and wonder how many more nights I would go without sleep.
My treatment
Antipsychotics In the meantime, the symptoms continued to worsen. I behaved like an electric broom: I rubbed the apartment to a shine and was in constant motion. The doctor was forced to interrupt our psychotherapy because I could not calmly sit through the session: I looked at her and laughed for no reason. It's embarrassing to even think about it now.
I behaved like an electric broom: I rubbed the apartment to a shine and was in constant motion. The doctor was forced to interrupt our psychotherapy because I could not calmly sit through the session: I looked at her and laughed for no reason. It's embarrassing to even think about it now.
In addition, I had auditory hallucinations. For the first time, I heard a male voice that asked me to do something with the papers. At first it seemed that my husband was talking to me, at that moment he was nearby. But when I looked at him, I realized that in fact he was silent. And other people were too far away for me to hear them so clearly. So I realized that it was a hallucination. nine0003
I felt as if I had been stunned, got into my head and said something loudly in the back of my head.
There were three auditory hallucinations in total. After the first one, I immediately wrote to the psychiatrist. She reassured me, said that this happens with BAD. The second and third hallucinations frightened me less: I understood that this was a manifestation of the disease and that it would pass with time.
The second and third hallucinations frightened me less: I understood that this was a manifestation of the disease and that it would pass with time.
But I couldn't wait any longer for the normotimic from Russia - I decided to buy it in the USA. To get a prescription, one had to contact a local psychiatrist. I found the doctor again through friends. It was important for me that he spoke Russian. I know English well, but I was afraid that due to the difference in mentality, the American doctor would misunderstand something and misinterpret my complaints. nine0003
How much does medicine cost in countries popular among Russians
Psychiatric services turned out to be not as expensive as friends said. For the first appointment, I paid 300 $ (19,032 R) - by local standards, this is an acceptable price.
The consultation lasted 40 minutes. The doctor listened to me carefully, asked questions and talked to my psychiatrist from Russia via video link. In the course of the conversation, it turned out that there was a paranoid component in my disorder - the idea of persecution: it seemed to me that those around me only did what they were discussing. On the street, I even often turned off the sound in my headphones to check if this was the case. I myself considered this behavior normal, so I didn’t tell the doctor about it before. nine0003
On the street, I even often turned off the sound in my headphones to check if this was the case. I myself considered this behavior normal, so I didn’t tell the doctor about it before. nine0003
The specialists agreed that it would be better to start my treatment with the atypical neuroleptic quetiapine. This drug was supposed to remove excessive excitement. Since I didn't have health insurance to cover my treatment, the doctor prescribed a cheaper generic.
The prescription was electronic, the doctor sent it to the pharmacy, from where they later called me and sent an SMS that the order was ready for delivery. I drove up in a car to a special window, like in Makavto, gave my last name, date of birth, and received the drug. A jar of pills for 30 days cost $45 (2855 R). nine0003 There are two drugs in the photo: quetiapine and valproic acid, which I was prescribed later. In American pharmacies, the prescribed amount of medicine is dispensed in jars, and not in factory packaging. Instructions are attached to the jars
Instructions are attached to the jars
Why I refused treatment, but returned to it again
The psychiatrist promised that the side effects from the antipsychotic would not be severe and I would not have problems driving a car. I specifically clarified this nuance during the consultation, because at that time I worked in delivery. nine0003
As it turned out, the doctor made a mistake. The new drug made me so sleepy that I didn't dare to drive. In addition, my head began to spin. It felt like the ground was moving underfoot in layers, like during an earthquake. Paranoid thoughts intensified: when I went into a cafe to pick up a delivery order, it seemed to me that everyone turned around and discussed how drunk I was - that's exactly how I felt at that moment. I was also worried about nausea, bloating and stomatitis. nine0003
I went to the American psychiatrist again to complain about the side effects and find another medication. The doctor said that since I'm visiting him for the second time in a month, the consultation will cost $100 (6344 R). At the same time, for the next ones, I will again have to pay $300 (19,032 R).
At the same time, for the next ones, I will again have to pay $300 (19,032 R).
/bipolyarnoe-rasstroystvo/
How much does the treatment of bipolar affective disorder cost?03 P) for a jar. By that time, I was very tired of the side effects of quetiapine. And in the instructions for the normothymic, so many new side effects were listed that I got scared and did not take it.
I decided to give up all medications and "treat" with an exclusively healthy lifestyle. I did not discuss my intentions with the American psychiatrist. And the Russian, with whom we continued to correspond, was simply put before the fact. The doctor could not dissuade me from this step, because she was on vacation and she did not have access to the Internet. nine0003
During the same period, I started reading the book by Masha Pushkina and Evgeny Kasyanov "Bipolar Disorder: A Survival Guide for Those Who Often Don't See the White Line". I devoured it in just one day.
The authors provided strong evidence in favor of drug therapy for bipolar disorder. I realized that I got excited about refusing the medicines, and again contacted the doctor from Russia, apologized and asked her to help me resume treatment.
The book described the experiences of people who have traveled the same path as me. After reading it, I felt that I was not alone and cheered up. The price of the electronic version on Litres: 299 RMy treatment
NormotimicsMy "rebellion" lasted only a few days, so I did not have time to feel worse. When I started taking valproic acid, I experienced relief: it did not cause any side effects, but it evened out my mood. Gradually, we even increased the dosage.
Until I entered the intermission - the period between exacerbations of the disease, when a person feels normal. But bright glimpses in my state happen more and more often.
Valproic acid helps keep your mood in the normal range without going into plus or minus. nine0003
nine0003
For some time, with a Russian psychiatrist, we selected the minimum dose of antipsychotic to improve sleep. But now we plan to finish taking the drug: it has already coped with its task. In addition, there is a suspicion that because of him I gained about eight extra pounds in two months of treatment. This also became a reason for cancellation.
/list/psychoterapevt/
10 important questions for psychotherapist Sergey Divisenko
In a few months we will resume psychotherapy. So far, we communicate with the Russian doctor only via WhatsApp: several times a week, she finds out how I feel and, if necessary, adjusts the doses of the drugs. When I need to clarify something about an illness, side effects of drugs, I ask for a consultation for 30-40 minutes. I pay for every $20 (1269R). During the entire observation period, I took two or three repeated consultations with the doctor.
How bipolar disorder affected my life
The illness affected my work and studies. All this time I had several jobs, one of which was delivery. At some point, it was hard for me to drive because of drowsiness, so I only helped my husband: I took orders, and we delivered them together.
All this time I had several jobs, one of which was delivery. At some point, it was hard for me to drive because of drowsiness, so I only helped my husband: I took orders, and we delivered them together.
My husband is my main support and support. It helps me fight the disease and track changes. My friends also support me. I am grateful to them for not turning away from me when they found out about the diagnosis. Some relatives decided that I invented my illness and was actually healthy. I think that the reason for this is the stigmatization of mental disorders. It is unpleasant for people to realize that their loved one is mentally ill. In general, I can understand them: while I myself am in the stage of accepting this fact. nine0003
/shizofreniya/
How much does it cost to support a relative with a mental disorder? Previously, I planned to receive letters of recommendation and collect a package of documents by September 2022. And now I've relaxed and I'm going with the flow - I'll pass the exams when I'm ready. So far, I have purchased a program for preparing for tests and I am going through it in a comfortable mode so as not to overload myself. I assist a dentist in the dental office, and my hands shake from time to time, although not much. I assume that this is a side effect of the normotimic - at least the doctor warned about this. Perhaps, because of him, I feel tired, which also affects the work. nine0003
So far, I have purchased a program for preparing for tests and I am going through it in a comfortable mode so as not to overload myself. I assist a dentist in the dental office, and my hands shake from time to time, although not much. I assume that this is a side effect of the normotimic - at least the doctor warned about this. Perhaps, because of him, I feel tired, which also affects the work. nine0003
Bipolar disorder has definitely changed my lifestyle. I gave up working at night, stopped drinking alcohol, started playing sports, and keep a daily routine. I do not take stimulants: coffee and energy drinks. Eat healthy food whenever possible.
I have become more responsible towards myself. Now I know that in any situation, I will first of all think about my health.
Expenses
Almost five months have passed since my first visit to a psychiatrist. During this period, I spent money on medicines, psychotherapy sessions, consultations of Russian and American doctors. In Moscow, she paid for the services of a psychologist. nine0003
In Moscow, she paid for the services of a psychologist. nine0003
In the US, I was given prescriptions that allow me to buy medicines at the pharmacy three times. Then you will need to contact an American psychiatrist again to get new appointments. His tricks will cost $300 (R19,032). For new sessions of psychotherapy with a Russian doctor, I will pay $40 (2537 R).
At the moment I have spent 79,500 R and $815 on treatment
| Expenses | Spending |
|---|---|
| Psychologist sessions in Moscow | 55 000 R |
| Drugs bought in Russia | 24 500 R |
| American psychiatric consultations | $400 (25,736 R) |
| Psychotherapy sessions | $240 (R15,225) |
| Russian psychiatric consultations | $100 (R6344) |
| Drugs purchased in the US | $75 (R4758) |
Expenditures
expenses
Psychologist sessions in Moscow
55 000 R
Preparations purchased in Russia
24 500 R
Consultations of the American Psychiatrist
400 $ (25 736 r)
Sesses of Psychotherapy
240 $ (15,225 r)
Consultations of the Russian psychiatrist
$ (6344 r)
Preparations purchased in the USA
[[75usd: 47 Russia inspired58]]
History of the disease.