Social ocd symptoms
What are the Social Signs of Obsessive Compulsive Disorder?
How to Recognize the Social Signs of Obsessive Compulsive Disorder
Obsessive compulsive disorder (OCD) is a mental condition that is characterized by a compulsive need to perform certain routines or think certain thoughts. As a chronic condition, OCD can affect all parts of a person’s daily life. It may interfere with a person’s romantic life, friendships, and more. Understanding the social signs of obsessive compulsive disorder can make it easier to manage the condition.
What Are the Social Signs of Obsessive Compulsive Disorder?
In day to day life, OCD typically presents in the form of intrusive thoughts and repetitive rituals. Most patients have persistent thoughts that cause intense anxiety, and performing rituals can help temporarily calm these obsessive concerns.
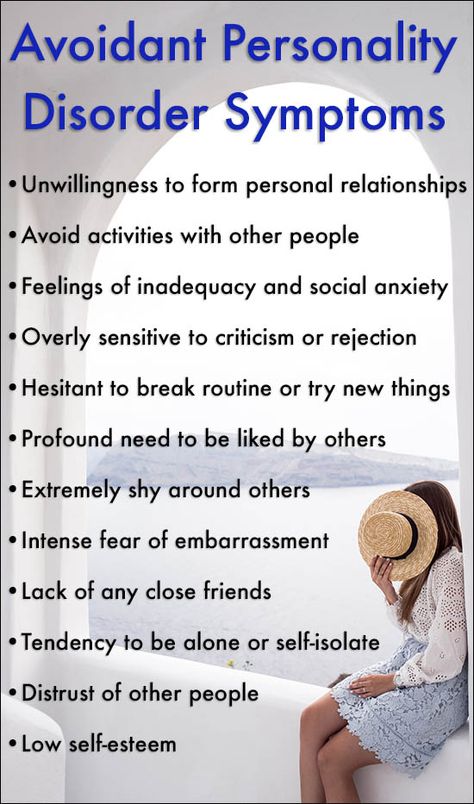
A person with OCD tends to struggle with social situations, even if they are not worried about hiding their symptoms from others. The condition is closely linked to depression and anxiety, making it hard to interact with others. In social situations, OCD may present itself through one or more of the following symptoms:
- Constant fears that people are mad at them
- Unrealistic worries about their relationships
- Feeling too tired to socialize
- Being late or not attending social gatherings for unexplained reasons
- Anger or lashing out when rituals are interrupted
- Sudden unexplained avoidance of friends or family members
- Rigid expectations for friends and family
How OCD Affects Family Life
Since most of a person’s time is spent around family members, OCD is most likely to affect these relationships. OCD rituals have a tendency to cause delays and disruptions in family life, which can lead to resentment on both sides. This is especially true if the family member has become involved in a ritual, such as the OCD person tugging their sibling’s hair a set number of times.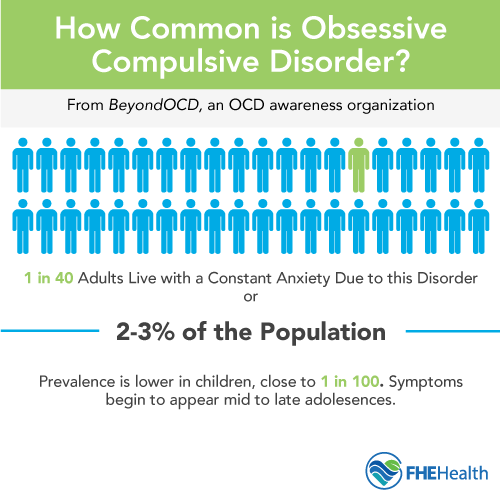 There can be a lot of social friction because a person with OCD may get mad when rituals are interrupted or become clingy and anxious due to intrusive thoughts telling them they are disliked.
There can be a lot of social friction because a person with OCD may get mad when rituals are interrupted or become clingy and anxious due to intrusive thoughts telling them they are disliked.
Maintaining positive family relationships requires both sides to be understanding. Family members need to provide an OCD person with enough time and space for their condition while avoiding enabling. At the same time, people with OCD need to work on getting OCD treatment and not pulling others into OCD rituals and anxieties. For the best outcomes, it is usually a good idea for all members of the family to attend family therapy.
How OCD Affects Friendships
Many people with OCD end up feeling socially isolated because the condition can make it so hard to make friends. The first challenge is simply getting to know people and building friendships. Having intrusive thoughts like “everyone dislikes you” or “you’re talking in a weird voice” makes it very hard to open up to others. If you are self-conscious about your OCD, it may feel easier to avoid others instead of getting into situations where you display symptoms. The symptoms of OCD can also make it hard to maintain friendships. People with OCD may be too worn out from rituals to support friends, and their rituals may leave them little time for social outings. Over time, this can cause friendships to fade.
The symptoms of OCD can also make it hard to maintain friendships. People with OCD may be too worn out from rituals to support friends, and their rituals may leave them little time for social outings. Over time, this can cause friendships to fade.
Making and keeping friends when you have OCD is very challenging, but it is also rewarding. Being able to have close social relationships can help prevent the depression that is so common in OCD. Therapy can help people with OCD manage their symptoms and get the courage to put themselves out there instead of staying isolated. Being upfront with friends about the social challenges of OCD can help them be more understanding of the fact that friendship with you may be different.
How OCD Affects Dating
OCD can also affect the search for a life partner. People with OCD may struggle with intrusive thoughts telling them “Are you sure this person is the one?” or “Should you keep dating them even though you hate it when they bite their nails?” A particularly challenging part of dating with OCD is simply the OCD stigma. Many people struggle with knowing when to disclose OCD to their partners. Mentioning it immediately can cause potential partners to focus on stereotypes instead of your actual personality. However, waiting until you get to know a person can make them feel misled. Typically, experts recommend being upfront and providing information on how your OCD affects you.
Many people struggle with knowing when to disclose OCD to their partners. Mentioning it immediately can cause potential partners to focus on stereotypes instead of your actual personality. However, waiting until you get to know a person can make them feel misled. Typically, experts recommend being upfront and providing information on how your OCD affects you.
If you do find someone to date, close romantic relationships are affected by OCD in several unique ways. People with OCD tend to have high levels of insecurity, so they need a partner who can provide frequent affection and affirmation. Depression and anxiety can affect arousal levels, making your sex life less frequent. To maintain a romantic relationship, most OCD people need a lot of support and assistance. Both personal OCD treatment and couples therapy can help with some of the challenges. Educating your partner on your OCD symptoms can help them interact with you in a more positive way.
Using TMS Treatment for OCD
If you have OCD, you do not have to let inconvenient symptoms and social OCD stigma keep you from building rewarding relationships. Transcranial magnetic stimulation (TMS) may be able to provide relief. This non-invasive, pain-free treatment involves using magnetic fields to stimulate the brain. Repeated treatments can help activate areas of the brain and improve overall functioning. An analysis of multiple studies involving TMS on OCD patients concluded that it was a safe and highly effective treatment. Especially when the TMS targeted the orbitofrontal cortex and supplementary motor area, it helped to reduce overall OCD-related symptoms.
Transcranial magnetic stimulation (TMS) may be able to provide relief. This non-invasive, pain-free treatment involves using magnetic fields to stimulate the brain. Repeated treatments can help activate areas of the brain and improve overall functioning. An analysis of multiple studies involving TMS on OCD patients concluded that it was a safe and highly effective treatment. Especially when the TMS targeted the orbitofrontal cortex and supplementary motor area, it helped to reduce overall OCD-related symptoms.
Getting relief from OCD symptoms can make it easier to focus on your relationships and social life. At Pulse TMS we can help you manage your OCD through the use of TMS treatment. Give us a call today to learn more about our services.
When Symptoms of OCD and Social Anxiety Overlap
Social OCD refers to experiencing obsessions and compulsions around the fear of being rejected, judged, or humiliated by others. It may also refer to overlapping symptoms of OCD and social anxiety.
Obsessive-compulsive disorder (OCD) is a mental health condition characterized by two primary symptoms: persistent intrusive thoughts (obsessions) and repetitive behaviors or rituals (compulsions).
Social OCD isn’t an established clinical term or a formal diagnosis. It may refer to overlapping symptoms of OCD and social anxiety.
Social anxiety is one of many anxiety disorders characterized by fear or panic of social interactions and of being criticized and rejected socially.
For people with social OCD, obsessions may be about social interactions or social performance. When this is the case, you may experience uncontrollable thoughts and intrusive images about people making fun of you, rejecting you even without knowing you, or humiliating you.
When this fear of social humiliation and rejection is a persistent symptom and impacts your daily routine, a mental health professional may diagnose both OCD and social anxiety.
Both social anxiety disorder and obsessive-compulsive disorder are chronic conditions that may involve debilitating symptoms.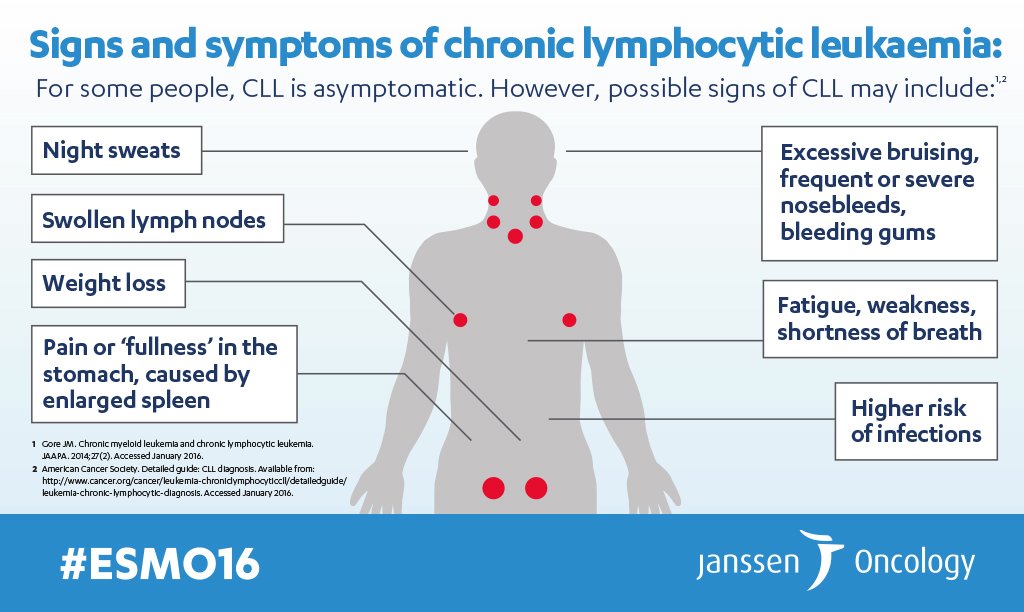 They’re two separate diagnoses.
They’re two separate diagnoses.
It’s possible for symptoms of OCD and social anxiety to occur together, though. This would mean that you live with two separate conditions. In fact, research suggests that social anxiety disorder is the most frequently co-occurring disorder for those with OCD.
But it’s also possible for someone with OCD to experience obsessions about social rejection for a period of time without receiving a social anxiety diagnosis.
To receive both diagnoses, you would need to meet the diagnostic criteria for both conditions. Diagnostic criteria are established by the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text revision (DSM-5-TR), a reference handbook used by most U.S. mental health professionals.
Diagnostic criteria for OCDAccording to the DSM-5-TR, two main criteria must be met for you to receive an OCD diagnosis:
- You experience repetitive and persistent obsessions and compulsions.
- These obsessions and compulsions take considerable time from your daily routine (more than 1 hour per day) or they cause you significant distress that translates into impairment or inability to function.
According to the DSM-5-TR, the criteria to receive a social anxiety diagnosis are:
- Significant fear about social events where you may be exposed to other people’s judgment and criticism.
- Persistent fear that others may recognize social anxiety symptoms in you that may lead you to be humiliated or embarrassed in public. It may also be fear that you won’t know how to act and offend others.
- Consistent fear about the same social situations.
- Tendency to avoid social situations or experience impairing levels of fear when exposed to those.
- Your fear of these social interactions isn’t proportionate to the threat you face.
- These symptoms last for at least 6 months but typically more than that.
- Your fear of social situations impairs the way you function at work, school, and in relationships.
- These symptoms cannot be explained by an injury, disease, or substance use.
- These symptoms cannot be explained by any other anxiety disorder or mental health condition.
- If you live with any injury, disease, or condition, your fear is unrelated to those or impairing.
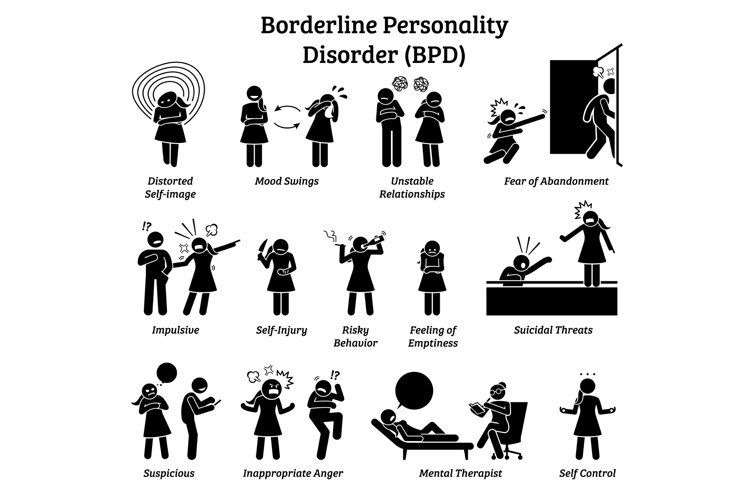
A person with both OCD and social anxiety may be more likely to experience obsessions with social themes. This may lead to symptoms commonly seen in people with “responsibility OCD,” also known as “social scrupulosity OCD.”
Responsibility OCD involves feeling an extreme fear of harming someone else’s feelings. For instance, you might worry excessively that you’ll say something in front of your friends that may remind them of a traumatic experience they lived. You experience intrusive images and thoughts about saying what you fear. This may lead you to repeatedly shrug your shoulders when you’re in front of your friends.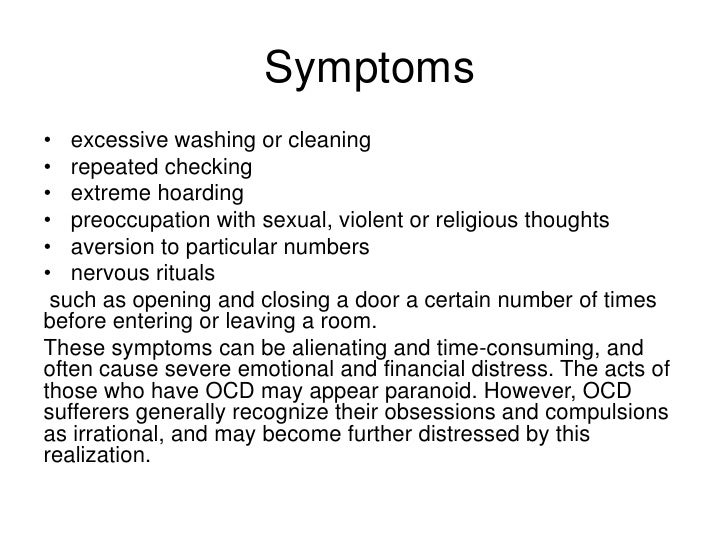
Social scrupulosity is a theme in OCD and doesn’t mean you also live with social anxiety, unless you meet all the criteria for this condition.
OCD is not a social disorder nor is it a social disability.
Even though OCD symptoms can be debilitating and highly distressing, many people with the disorder can navigate different aspects of life, including employment, romantic relationships, and social interactions.
OCD doesn’t cause social anxiety disorder, and social anxiety doesn’t cause OCD. However, it’s possible that one may be a contributing factor to the other in some instances. In fact, they often co-occur.
In one study, social anxiety disorder was seen in about 20% of participants with OCD. Those with both OCD and social anxiety disorder were more likely to experience severe depression symptoms and insecure attachment styles.
Both OCD and social anxiety disorder can be managed with the support of a mental health professional.
Cognitive behavioral therapy (CBT) is one of the most effective treatments for both conditions.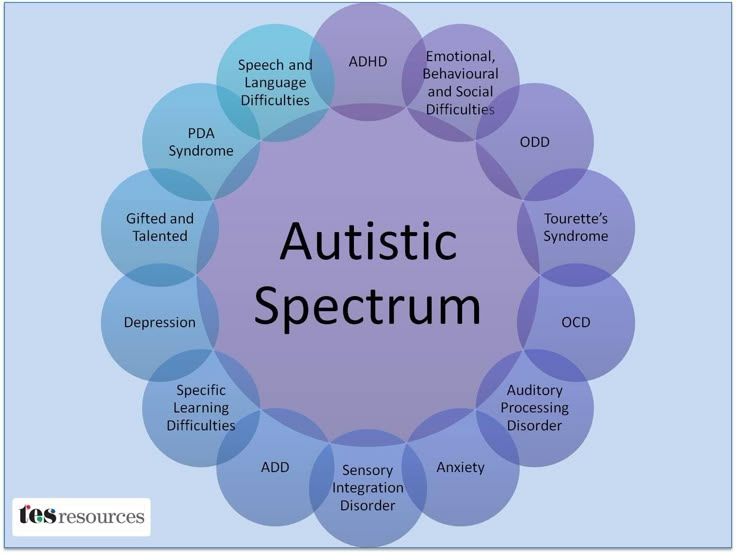
CBT for the management of social anxiety disorder may include techniques like exposure therapy, which involves gradually exposing you to your social fears until your anxiety is reduced or gone.
CBT for the management of OCD typically involves exposure and response prevention (ERP) therapy. ERP also gradually exposes you to your fears while helping you not to engage in a compulsion to relieve the anxiety they cause you. In time, you learn that you don’t need to engage in compulsions to decrease anxiety.
In some cases, medication may also be used to treat OCD and social anxiety.
Social anxiety disorder and OCD are two separate mental health diagnoses. In some instances, someone can live with both conditions.
It’s also possible for someone with OCD to have obsessions around a fear of social interactions without meeting the criteria for social anxiety.
Only a mental health professional can provide an accurate diagnosis and a management plan for both conditions.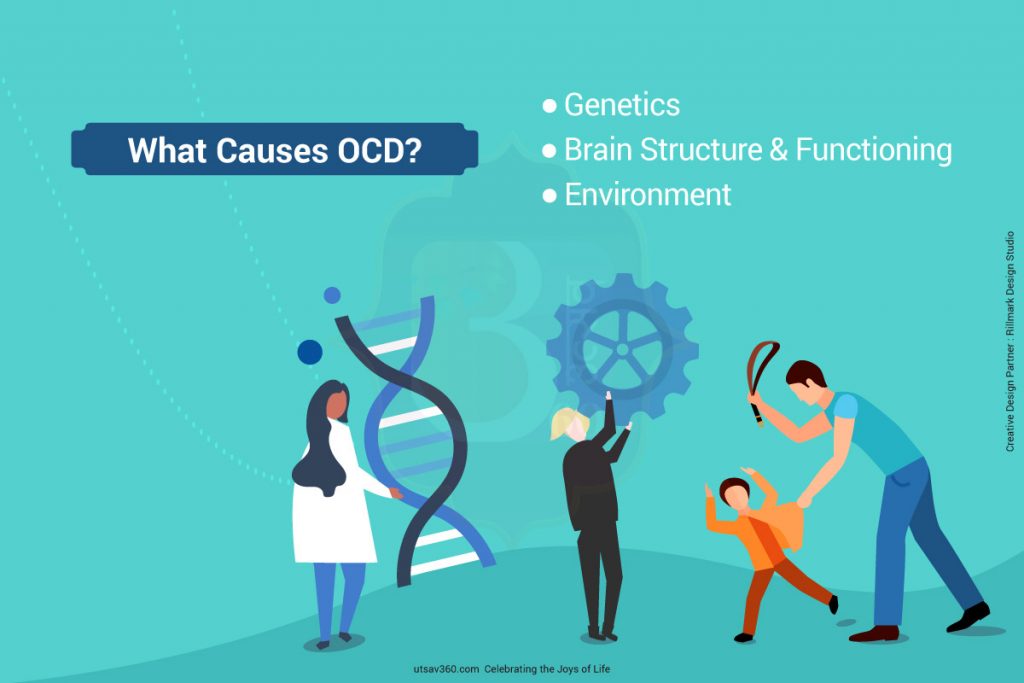
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
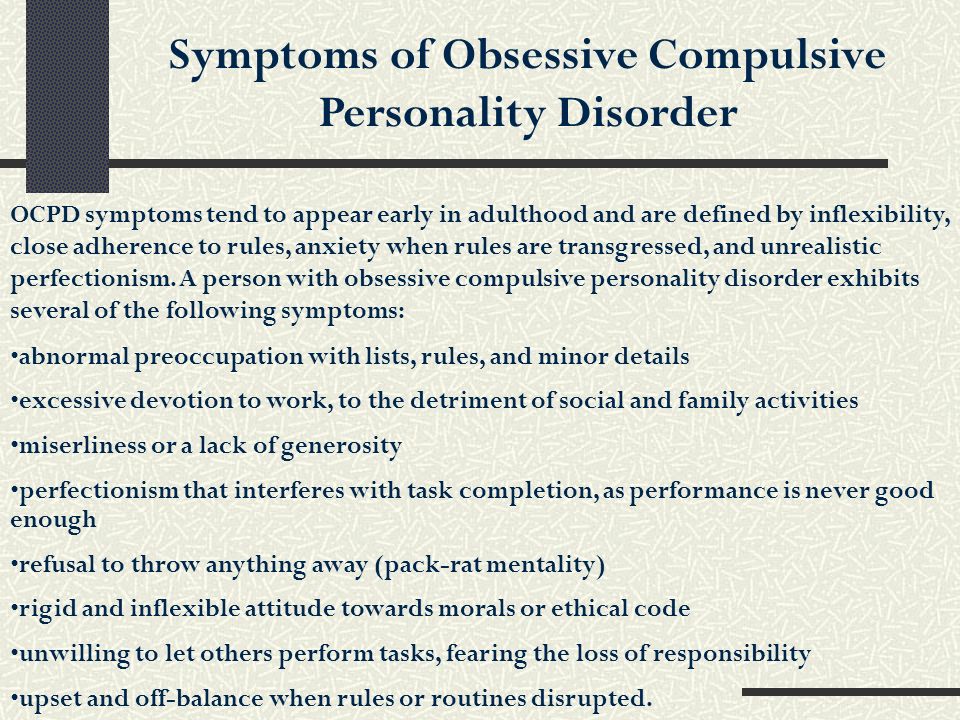
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety.
What is obsessive-compulsive disorder?
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions.
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
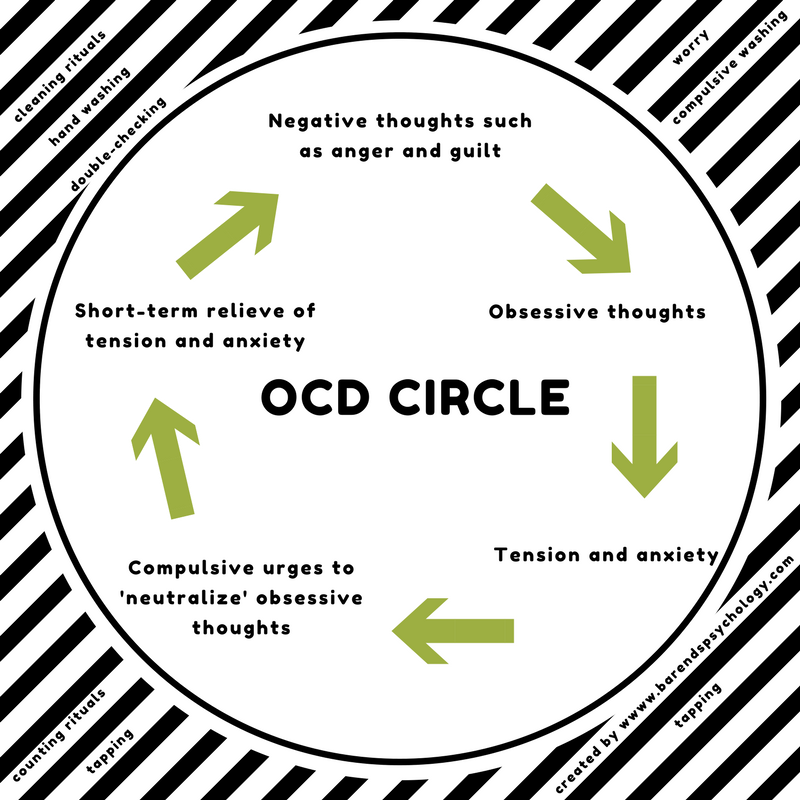
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer.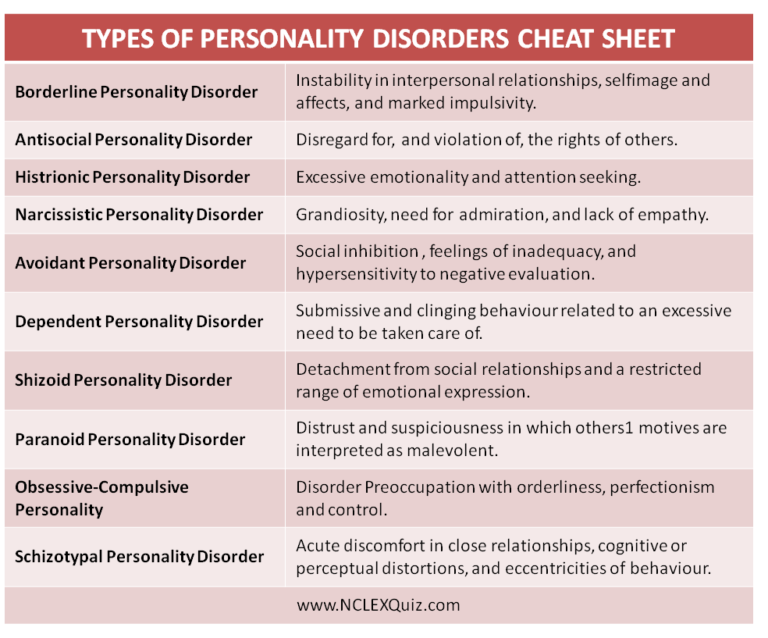
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions
- A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community.
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result.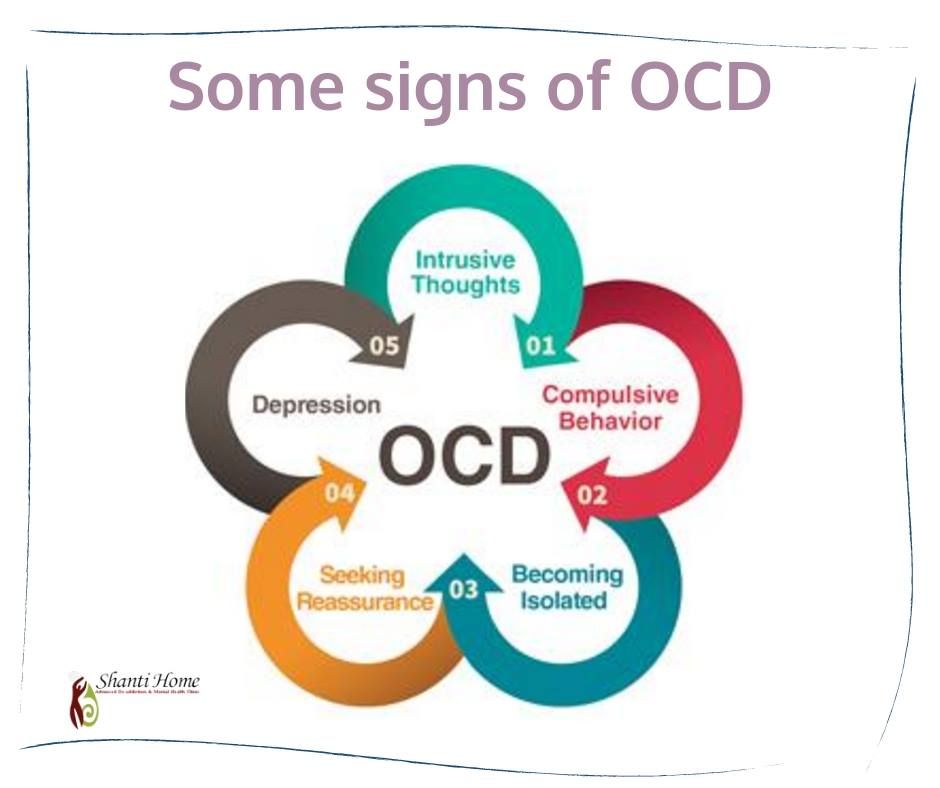 A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events.
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy.
- Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Psychopharmacotherapy (if indicated)
- Biofeedback Therapy
- Rational psychocorrection of stress
- Jacobson progressive muscle relaxation.
- Traditional and modern gymnastic systems, relaxation techniques.
- Breathing techniques .
- Stress exposure.
- Self-control training.
- Jacobson progressive muscle relaxation.
- Lifestyle modification
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed.
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.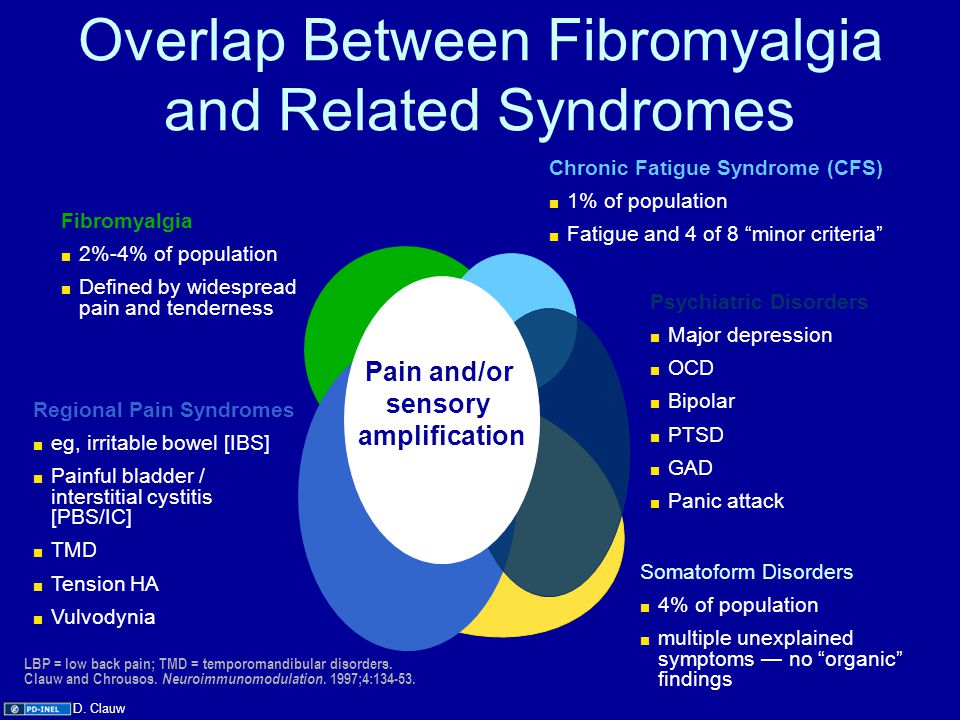
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future.
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future.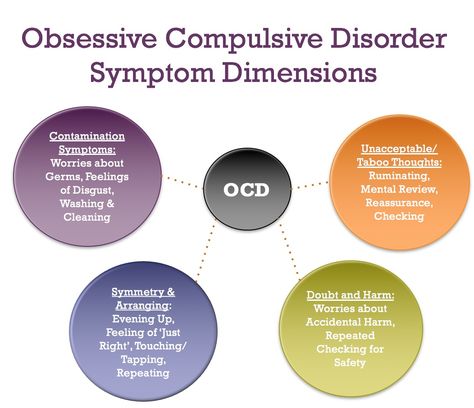 Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased.
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
Obsessive-compulsive disorder (OCD) - causes, symptoms, signs, examples, diagnosis (test), treatment
Signs of obsessive-compulsive disorder (OCD) do not depend on the will of the person, as they relate to mental illness. There are two main features:
- obsessions - obsessive thoughts, ideas, images;
- compulsions are repetitive actions or rituals.
The second name of the disease is obsessive-compulsive disorder. The content of thoughts and images is perceived by the patient as alien, their pain is recognized, but it is not possible to get rid of them on their own.
Features of obsessive-compulsive disorder
Obsessive-compulsive personality disorder was described in the first half of the 19th century by the French psychiatrist Esquirol, and was called the "disease of doubt. " Subsequently, scientists identified the main difference between the disease - the patient's perception of the alienation of the experienced. All other mental illnesses absorb the personality, changing it beyond recognition. A mentally ill person becomes completely different than before the illness. In OCD, the core of the personality remains intact, but the accompanying rituals and experiences are overwhelming, making life difficult. However, there have been cases where a major psychiatric illness (schizophrenia, bipolar disorder) began as OCD.
" Subsequently, scientists identified the main difference between the disease - the patient's perception of the alienation of the experienced. All other mental illnesses absorb the personality, changing it beyond recognition. A mentally ill person becomes completely different than before the illness. In OCD, the core of the personality remains intact, but the accompanying rituals and experiences are overwhelming, making life difficult. However, there have been cases where a major psychiatric illness (schizophrenia, bipolar disorder) began as OCD.
The morbid state must be distinguished from the natural fear necessary for survival. The fear of depth, the desire to move away from a moving train or a landslide, the desire to hide in an explosion are just reasonable behavior, although tinged with intense fear.
Obsessive-compulsive disorder in women and men occurs with the same frequency of 2 to 5%. Some authors argue that women are more likely to get sick. Statistics are kept only in developed countries where medical care is available.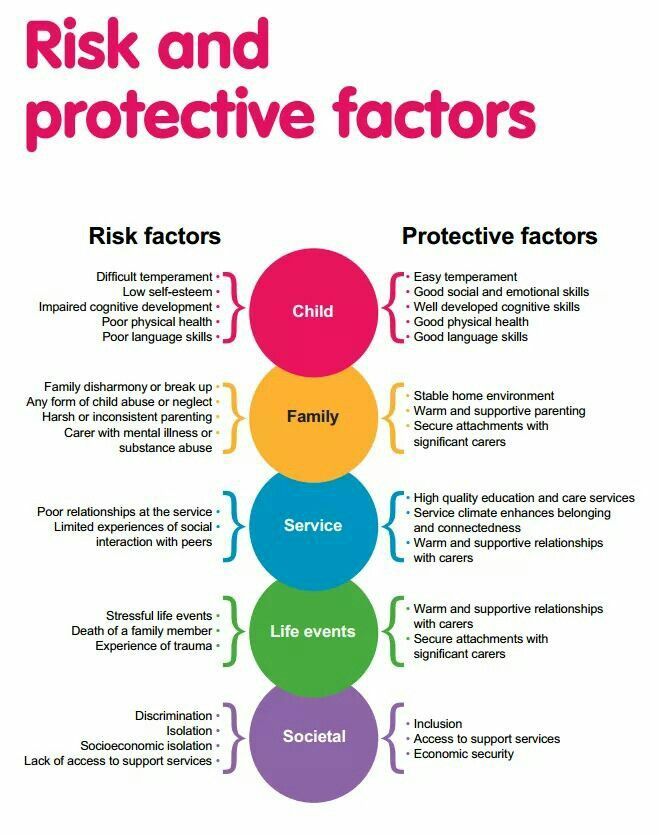 It is not known if the disease occurs elsewhere.
It is not known if the disease occurs elsewhere.
Causes of obsessive-compulsive disorder
There is no final coherent theory regarding the reasons yet. The following variants are discussed:
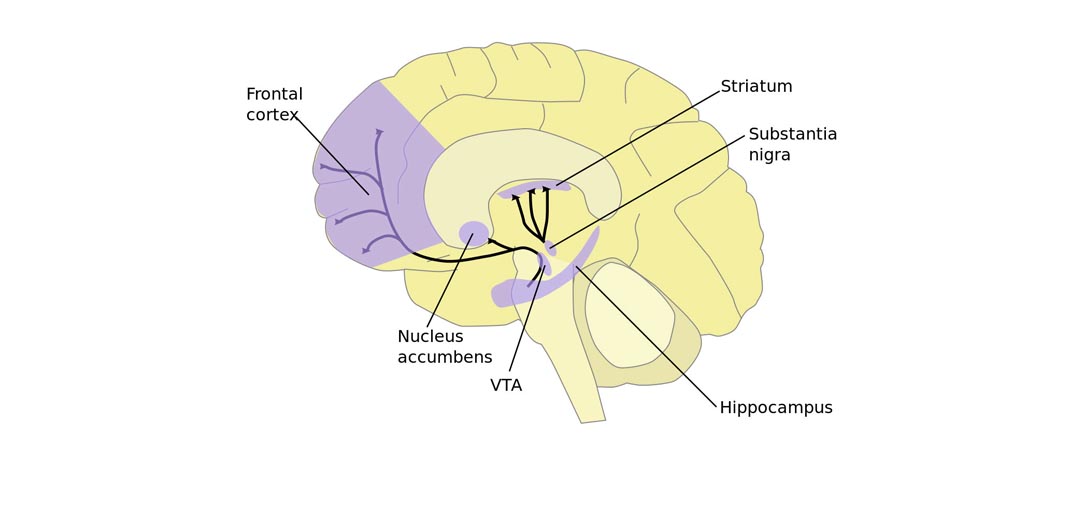
- hereditary predisposition – violations of the synthesis of neurotransmitters (chemical substances involved in the transmission of nerve impulses) are always of a genetic nature;
- increased activity of some parts of the brain, namely in the limbic system - the dentate gyrus, the prefrontal part of the cerebral cortex;
- a decrease in the concentration of substances responsible for emotions (serotonin, dopamine) in the thalamus, cortical circuit;
- deviations in the work of brain receptors;
- anomalies in the development of certain zones, in particular the cerebellum and the inferior frontal gyrus;
- congenital or acquired disorders of nerve impulse transmission.
Changes in the work of the cortex and limbic system occur both for genetic reasons and under the influence of adverse external factors.
Provoking factors are:
- immune system malfunctions;
- stress, especially chronic;
- physiological fluctuations in hormonal status in women during pregnancy, childbirth and lactation, as well as during the menstrual cycle;
- encephalopathies of various origins, especially vascular ones;
- trauma and surgery on the brain;
- personal life problems, especially loneliness;
- alcoholism and drug use;
- infectious diseases - hepatitis, herpetic lesions, HIV;
- severe somatic pathology - a chronic increase in thyroid function, inflammation of the kidneys, pancreas, liver, stomach.
Obsessive-compulsive disorder in children develops between the ages of 3 and 12 years, it practically does not occur in babies. The closer to adolescence, the higher the incidence. The biological prerequisites are:
- brain damage occurring in the prenatal period and in early childhood;
- violations of the transmission of a nerve impulse, including changes in the number of neurotransmitters;
- mutation in the gene responsible for the production of serotonin;
- streptococcal infection in the first year of life.
Psychologists have a slightly different view of the nature of the disorder. The main hypothesis is considered to be psychoanalytic, namely the conflict of internal sexual aggression and parental prohibition on such relationships. It is also noted that OCD is more often formed in people with anancastic (stuck) personality traits. One of the undoubted reasons is a difficult, destructive family environment with constant scandals. The death of a mother in early childhood and the loss of a father after the age of 3 years have an extremely unfavorable effect on health. Too strict upbringing, lack of affection and understanding, excessive parental requirements have a negative impact on children.
Russian physiologist Pavlov believed that the disease develops in people of the thinking type with sluggish (inert) processes of excitation-inhibition.
Symptoms of obsessive-compulsive disorder
Obsessive fears or phobias have many varieties, each of which has its own name:
- cancerophobia - fear of getting cancer;
- claustrophobia - closed space;
- agoraphobia - open areas;
- thanatophobia - death;
- arachnophobia - spiders;
- nosophobia - infection.
Fear has an irrational nature, no beliefs, arguments and evidence have any effect on the patient. To protect against imaginary danger, the patient creates his own rituals or repetitive actions that he performs in strict sequence.
A classic example of obsessive-compulsive disorder: a patient with nosophobia cannot touch anything before washing his hands with hot water and soap three times. In some patients, the fear of infection is so strong that it forces them to wash the floors several times a day with an undiluted disinfectant solution. The fact that there is nothing to breathe in the room and the skin on the hands cracks to blood does not matter to the patient. In such a neglected case, we are no longer talking about any social adaptation, the patient simply cannot leave the house to get to work or walk to the store.
Diagnosis of obsessive-compulsive disorder
Establishing a diagnosis is the task of a psychiatrist, to whom, unfortunately, the patient does not always get right away.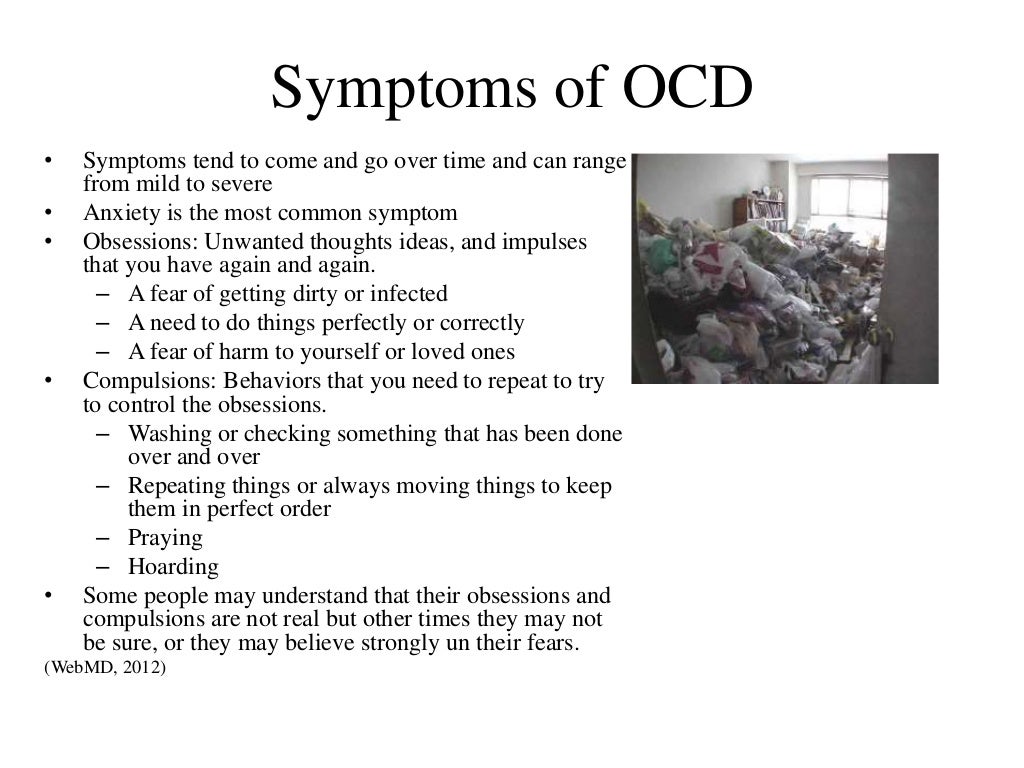 Often, a patient, who is certainly convinced that he has a somatic disease, undergoes a series of various examinations and treatments that do not bring results. Internists (doctors in internal medicine) refer to a psychiatrist after the failure of their own attempts.
Often, a patient, who is certainly convinced that he has a somatic disease, undergoes a series of various examinations and treatments that do not bring results. Internists (doctors in internal medicine) refer to a psychiatrist after the failure of their own attempts.
It is essential for the diagnosis that the obsessive thoughts or actions take up at least one hour a day. There is a "gold standard" psychological examination for obsessive-compulsive disorder - the Yale Brown test. This is a 10 section questionnaire. Each section has 5 answer options, you need to choose one, the answer is estimated in points. The scores are added up and scored on a scale from 0 to 40, with the highest score indicating extreme OCD. The questionnaire is freely available, you can complete it yourself.
The result of a neurological examination gives non-specific data characteristic of many nervous disorders: trembling of closed eyelids and outstretched arms, increased tendon reflexes, signs of autonomic imbalance. If the organic nature of the disease is suspected, neuroimaging methods (CT, MRI, and the like) are used.
If the organic nature of the disease is suspected, neuroimaging methods (CT, MRI, and the like) are used.
Treatment of obsessive-compulsive disorder
Therapy is selected strictly individually, it takes time. Usually combine several methods: both drug and non-drug.
For obsessive-compulsive disorder, psychotropic drugs from the following groups are used:
- third-generation antidepressants;
- tranquilizers;
- atypical neuroleptics.
Psychotropic drugs do not act immediately, it is possible to increase the dose with an interval of 7-14 days. The selection and combination of drugs is a delicate matter, there can be no general recommendations. However, the earlier a person sees a doctor, the less time is required to select a treatment.
Of the psychotherapeutic methods, the following types of therapy have proven themselves well:
- cognitive-behavioral;
- exposure method - collision and working out of a disturbing situation;
- stopping thought - learning to stop the influx of specific obsessions;
- hypnosis;
- auto-training;
- games and fairy tale therapy in children.

Learn more