Signs of avoidance
Avoidant Personality Disorder: Symptoms, Treatments, and Complications
Written by Susan Quilty
In this Article
- Avoidant Personality Disorder Symptoms
- Social Impact of Avoidant Personality Disorder
- Avoidant Personality Disorder Treatments
- Avoidant Personality Disorder and Other Conditions
Avoidant personality disorder is characterized by feelings of extreme social inhibition, inadequacy, and sensitivity to negative criticism and rejection. Yet the symptoms involve more than simply being shy or socially awkward. Avoidant personality disorder causes significant problems that affect the ability to interact with others and maintain relationships in day-to-day life. About 1% of the general population has avoidant personality disorder.
Avoidant Personality Disorder Symptoms
Avoidant personality disorder symptoms include a variety of behaviors, such as:
- Avoiding work, social, or school activities for fear of criticism or rejection.
It may feel as if you are frequently unwelcome in social situations, even when that is not the case. This is because people with avoidant personality disorder have a low threshold for criticism and often imagine themselves to be inferior to others.
- Low self-esteem
- Self-isolation
When in social situations, a person with avoidant personality disorder may be afraid to speak up for fear of saying the wrong thing, blushing, stammering, or otherwise getting embarrassed. You may also spend a great deal of time anxiously studying those around you for signs of approval or rejection.
A person who has an avoidant personality disorder is aware of being uncomfortable in social situations and often feels socially inept. Despite this self-awareness, comments by others about your shyness or nervousness in social settings may feel like criticism or rejection. This is especially true if you are teased, even in a good-natured way, about your avoidance of social situations.
Social Impact of Avoidant Personality Disorder
Avoidant personality disorder causes a fear of rejection that often makes it difficult to connect with other people. You may be hesitant to seek out friendships, unless you are certain that the other person will like you. When you are involved in a relationship, you may be afraid to share personal information or talk about your feelings. This can make it difficult to maintain intimate relationships or close friendships.
According to the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (DSM-5), a person diagnosed with avoidant personality disorder needs to show at least four of the following criteria:
- Avoids occupational activities that involve significant interpersonal contact, because of fears of criticism, disapproval, or rejection.
- Is unwilling to get involved with people unless they are certain of being liked.
- Shows restraint within intimate relationships because of the fear of being shamed or ridiculed.

- Is preoccupied with being criticized or rejected in social situations.
- Is inhibited in new interpersonal situations because of feelings of inadequacy.
- Views self as socially inept, personally unappealing, or inferior to others.
- Is unusually reluctant to take personal risks or to engage in any new activities because they may prove embarrassing.
Avoidant behavior may commonly be seen in children or adolescents, but a diagnosis of a personality disorder cannot be made in childhood because shyness, fear of strangers, social awkwardness, or being sensitive to criticism are often a normal part of child and adolescent development.
A mental health professional can assess your symptoms, make an accurate diagnosis, and suggest the appropriate treatment options.
Avoidant Personality Disorder Treatments
As with other personality disorders, a mental health professional will design a treatment plan that is appropriate for you. Avoidant personality disorder treatments vary, but they will likely include talk therapy.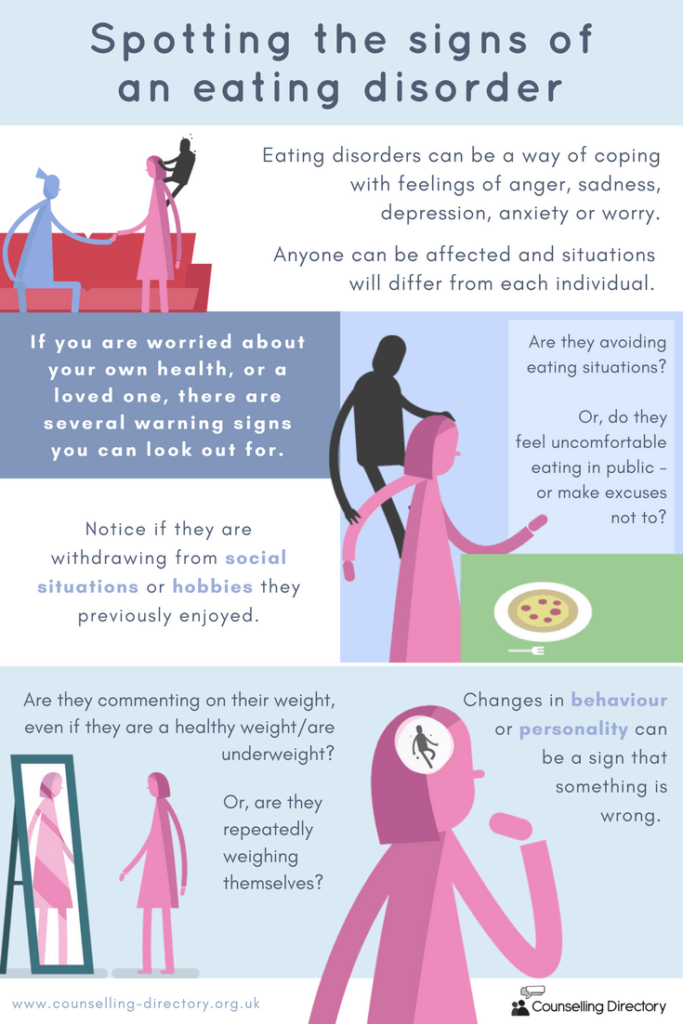 If a co-existing condition, such as depression or anxiety disorder, is also diagnosed, appropriate medications may also be used.
If a co-existing condition, such as depression or anxiety disorder, is also diagnosed, appropriate medications may also be used.
Avoidant Personality Disorder and Other Conditions
Other mental health disorders can occur along with avoidant personality disorder. Treatments in these cases will be designed to help with the symptoms of each disorder. A few of the conditions that most frequently occur with avoidant personality disorder include:
- Social phobia, in which a person experiences overwhelming anxiety and self-consciousness in common social situations.
- Dependent personality disorder, in which people rely excessively on others for advice or to make decisions for them.
- Borderline personality disorder, in which people have difficulties in many areas including social relationships, behavior, mood, and self-image.
Many avoidant personality disorder symptoms are commonly shared among these other conditions, particularly in the case of generalized social phobia. Because of this, the disorders can be easily confused. It may take some time for a mental health professional to make a clear diagnosis and choose the appropriate treatments for you.
Because of this, the disorders can be easily confused. It may take some time for a mental health professional to make a clear diagnosis and choose the appropriate treatments for you.
Mental Health: Paranoid Personality Disorder
Written by WebMD Editorial Contributors
In this Article
- What Are the Symptoms of Paranoid Personality Disorder?
- What Causes Paranoid Personality Disorder?
- How Is Paranoid Personality Disorder Diagnosed?
- How Is Paranoid Personality Disorder Treated?
- What Complications Are Associated With Paranoid Personality Disorder?
- What Is the Outlook for People With Paranoid Personality Disorder?
- Can Paranoid Personality Disorder Be Prevented?
Paranoid personality disorder (PPD) is one of a group of conditions called "Cluster A" personality disorders which involve odd or eccentric ways of thinking. People with PPD also suffer from paranoia, an unrelenting mistrust and suspicion of others, even when there is no reason to be suspicious.
This disorder usually begins by early adulthood and appears to be more common in men than in women.
What Are the Symptoms of Paranoid Personality Disorder?
People with PPD are always on guard, believing that others are constantly trying to demean, harm, or threaten them. These generally unfounded beliefs, as well as their habits of blame and distrust, might interfere with their ability to form close relationships. People with this disorder:
- Doubt the commitment, loyalty, or trustworthiness of others, believing others are using or deceiving them
- Are reluctant to confide in others or reveal personal information due to a fear that the information will be used against them
- Are unforgiving and hold grudges
- Are hypersensitive and take criticism poorly
- Read hidden meanings in the innocent remarks or casual looks of others
- Perceive attacks on their character that are not apparent to others; they generally react with anger and are quick to retaliate
- Have recurrent suspicions, without reason, that their spouses or lovers are being unfaithful
- Are generally cold and distant in their relationships with others, and might become controlling and jealous
- Cannot see their role in problems or conflicts and believe they are always right
- Have difficulty relaxing
- Are hostile, stubborn, and argumentative
What Causes Paranoid Personality Disorder?
The exact cause of PPD is not known, but it likely involves a combination of biological and psychological factors.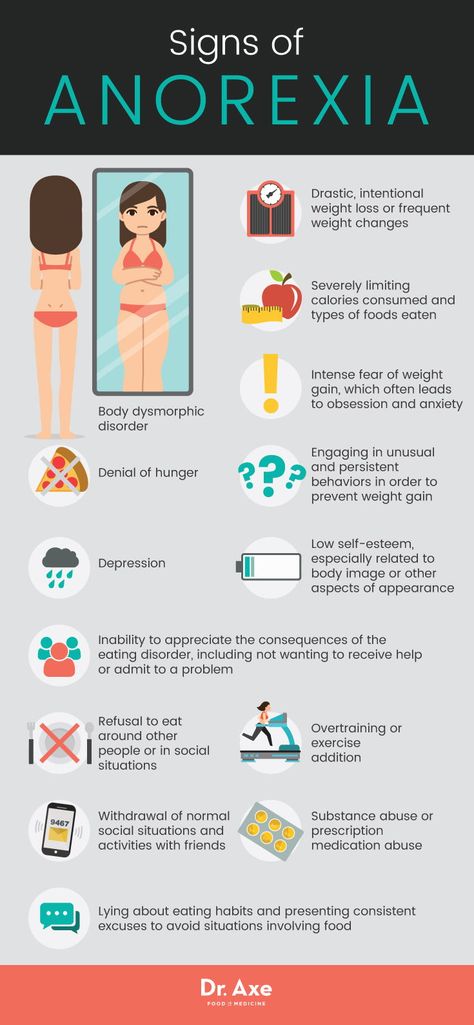 The fact that PPD is more common in people who have close relatives with schizophrenia suggests a genetic link between the two disorders. Early childhood experiences, including physical or emotional trauma, are also suspected to play a role in the development of PPD.
The fact that PPD is more common in people who have close relatives with schizophrenia suggests a genetic link between the two disorders. Early childhood experiences, including physical or emotional trauma, are also suspected to play a role in the development of PPD.
How Is Paranoid Personality Disorder Diagnosed?
If physical symptoms are present, the doctor will begin an evaluation by performing a complete medical and psychiatric history and, if indicated, a physical exam. Although there are no laboratory tests to specifically diagnose personality disorders, the doctor might use various diagnostic tests to rule out physical illness as the cause of the symptoms.
If the doctor finds no physical reason for the symptoms, they might refer the person to a psychiatrist or psychologist, health care professionals who are specially trained to diagnose and treat mental illnesses. Psychiatrists and psychologists use specially designed interview and assessment tools to evaluate a person for a personality disorder.
How Is Paranoid Personality Disorder Treated?
People with PPD often do not seek treatment on their own because they do not see themselves as having a problem. When treatment is sought, psychotherapy (a form of counseling) is the treatment of choice for PPD. Treatment likely will focus on increasing general coping skills, as well as on improving social interaction, communication, and self-esteem.
Because trust is an important factor of psychotherapy, treatment is challenging since people with PPD have such distrust of others. As a result, many people with PPD do not follow their treatment plan.
Medication generally is not a major focus of treatment for PPD. However, medications, such as anti-anxiety, antidepressant or antipsychotic drugs, might be prescribed if the person's symptoms are extreme, or if they also suffer from an associated psychological problem, such as anxiety or depression.
What Complications Are Associated With Paranoid Personality Disorder?
The thinking and behaviors associated with PPD can interfere with a person's ability to maintain relationships, as well as their ability to function socially and in work situations. In many cases, people with PPD become involved in legal battles, suing people or companies they believe are "out to get them."
In many cases, people with PPD become involved in legal battles, suing people or companies they believe are "out to get them."
What Is the Outlook for People With Paranoid Personality Disorder?
The outlook for people with PPD varies. It is a chronic disorder, which means it tends to last throughout a person's life. Although some people can function fairly well with PPD and are able to marry and hold jobs, others are completely disabled by the disorder. Because people with PPD tend to resist treatment, the outcome often is poor.
Can Paranoid Personality Disorder Be Prevented?
Although prevention of PDD might not be possible, treatment can sometimes allow a person who is prone to this condition to learn more productive ways of dealing with situations.
Avoidance behavior (psychological mechanisms and psychopathological features). Part 1: Anxiety Disorders - Psychiatry and Psychopharmacotherapy. P.B. Gannushkina №03 2016
Avoidance behavior is one of the main forms of defensive behavior in patients with mental disorders. The clinical signs characterizing phobic and delusional avoidance are considered. Features of avoidance behavior in obsessive-phobic disorders are determined by the psychopathological structure, content and severity of obsessive disorders.
The clinical signs characterizing phobic and delusional avoidance are considered. Features of avoidance behavior in obsessive-phobic disorders are determined by the psychopathological structure, content and severity of obsessive disorders.
Key words: avoidance behavior, anxiety, obsessions, phobic avoidance, delusional avoidance.
For citation: V.I. Krylov, V.A. Korkina Avoidance behavior (psychological mechanisms and psychopathological features). Part 1: anxiety disorders. Psychiatry and psychopharmacotherapy. 2016; 18(3):4–8.
I.M.Pavlov First Saint Petersburg State Medical University of the Ministry of Health of the Russian Federation. 197022, Russian Federation, Saint Petersburg, ul. L'va Tolstogo, d. 6/8
Avoidance behavior is one of the main forms of protective behavior in patients with mental disorders. We consider the clinical signs that characterize phobic avoidance and delusional avoidance. Features avoidance behavior in obsessive – phobic disorders are defined psychopathological structure, content and severity compulsive disorders.
Key words: avoidance behavior, anxiety, obsessions, phobic avoidance, avoidance delusional.
For citation: Krylov V.I., Korkina V.A. Avoidance behavior (psychological mechanisms and psychopathological features). Part 1: anxiety
The issue of diagnostic assessment and qualification of behavioral phenomena is one of the most urgent problems of clinical and theoretical psychiatry, attracting the attention of leading experts [1, 2]. In some cases, behavioral disorders become a manifestation of deviant deviant behavior and cannot be qualified as a sign of a disease; in others, behavioral disorders are symptoms of a disease.
In the main modern classifications used in psychiatry, most diagnostic categories include a combination of psychopathological and behavioral features. The criterion for diagnosing a manic state is not only a painfully elevated mood, traditionally considered as a pathology of emotions, but also such a behavioral sign as revelry, which cannot be unambiguously attributed to the pathology of a certain mental process. Diagnostic criteria for the main forms of eating disorders - anorexia nervosa and bulimia nervosa include both psychopathological (obsessive fear of gaining weight) and behavioral (avoidance of fatty foods, recurrent episodes of overeating) signs.
Diagnostic criteria for the main forms of eating disorders - anorexia nervosa and bulimia nervosa include both psychopathological (obsessive fear of gaining weight) and behavioral (avoidance of fatty foods, recurrent episodes of overeating) signs.
The absence of a general definition of the term “behavioral disorder” makes it difficult to distinguish between pathological variants of behavioral phenomena and extreme variants of deviant behavior.
Behavioral disorders observed in clinical practice reflect different levels of mental disorder. It is relevant to study the correlation of various variants of behavioral disorders with certain registers of mental damage. Of practical and theoretical interest is the consideration of the issue of qualification of behavioral signs from the standpoint of the traditional division of symptoms into positive and negative disorders.
There are different approaches to the identification and systematics of behavioral phenomena in the literature. The abundance of terms used to qualify behavioral phenomena is not only associated with a variety of forms of behavior, but is also partly determined by the fact that representatives of various scientific disciplines – physiology, sociology, criminology, psychology, medicine – are studying deviations and behavioral disorders.
The abundance of terms used to qualify behavioral phenomena is not only associated with a variety of forms of behavior, but is also partly determined by the fact that representatives of various scientific disciplines – physiology, sociology, criminology, psychology, medicine – are studying deviations and behavioral disorders.
Deviations in behavior can be determined by various psychological mechanisms. Depending on the psychological mechanisms underlying behavioral deviations, compensatory, hypercompensatory, manipulative, provocative behavior is distinguished. The same group, with a certain degree of conditionality, can include attitudinal behavior aimed at hiding from others the true motives of actions and actions.
A number of terms are used to refer to the clinical behavior of patients with various mental disorders. To characterize the behavior of narcissistic personalities (hysterical neurosis and hysterical psychopathy in the traditional sense), the terms “demonstrative”, “theatrical”, “masked behavior” are used. When describing the behavior of individuals with schizophrenia spectrum disorders, the term "autistic behavior" is widely used.
When describing the behavior of individuals with schizophrenia spectrum disorders, the term "autistic behavior" is widely used.
When qualifying various variants of defensive behavior that allow to temporarily reduce the severity of emotional stress, avoiding, controlling and ritual behavior are distinguished.
In a separate group, behavioral phenomena associated with drives are distinguished. The concept of “eating disorders” unites a group of disorders that are quite heterogeneous in clinical and pathogenetic terms, to some extent associated with food craving. The term “gender-role behavior disorders” unites a group of disorders, no less heterogeneous in terms of clinical manifestations and mechanisms of development, associated with deviations and disorders of sexual desire.
In addictology, to characterize the behavior of patients with psychoactive substance abuse and non-chemical forms of addiction, terms similar in meaning, but not identical, "addicted", "addictive", "gambling behavior" are used.
The concepts of auto-aggressive and self-destructive behavior have become quite widespread in the literature. At the same time, there is no consensus on the issue of the relationship between the concepts of auto-aggressive and auto-destructive behavior. The first point of view considers self-destructive behavior as a particular variant, a variety of self-aggressive. In this case, self-destructive behavior includes activities with a high risk of physical damage. The second point of view involves the assignment to self-destructive behavior of actions and deeds that cause not only physical, but also moral harm to the body. Self-destructive behavior is opposed to constructive behavior, in which actions and deeds provide personal growth.
In behaviorism, behavior is considered as a set of motor and related verbal and emotional reactions to the impact of environmental stimuli. The key position of behaviorism is the postulate that it is possible to study mental activity only through the interpretation of objectively observed acts of behavior. Behavior is interpreted as a reaction to external aversive stimuli, through which a person adapts to the environment. Aversive stimuli are events or bodily physiological sensations that have an unpleasant, painful connotation. Aversive stimuli are perceived by the subject as punishment. In response to the possible impact of the stimulus, reactions of passive or active avoidance or prevention of the stimulus are possible.
Behavior is interpreted as a reaction to external aversive stimuli, through which a person adapts to the environment. Aversive stimuli are events or bodily physiological sensations that have an unpleasant, painful connotation. Aversive stimuli are perceived by the subject as punishment. In response to the possible impact of the stimulus, reactions of passive or active avoidance or prevention of the stimulus are possible.
In the case of negative reinforcement, the behavioral response is formed and maintained by withdrawing the stimulus. With positive reinforcement, a behavioral response is shaped and maintained by providing an alternative to an external stimulus.
Avoidance behavior (AE) is a system of measures that prevent contact with objects that cause the appearance or increase of anxiety. Avoidance is understood as any behavioral act that allows you to avoid unpleasant and dangerous situations, events, incentives. PI can be of a conscious purposeful or little conscious nature.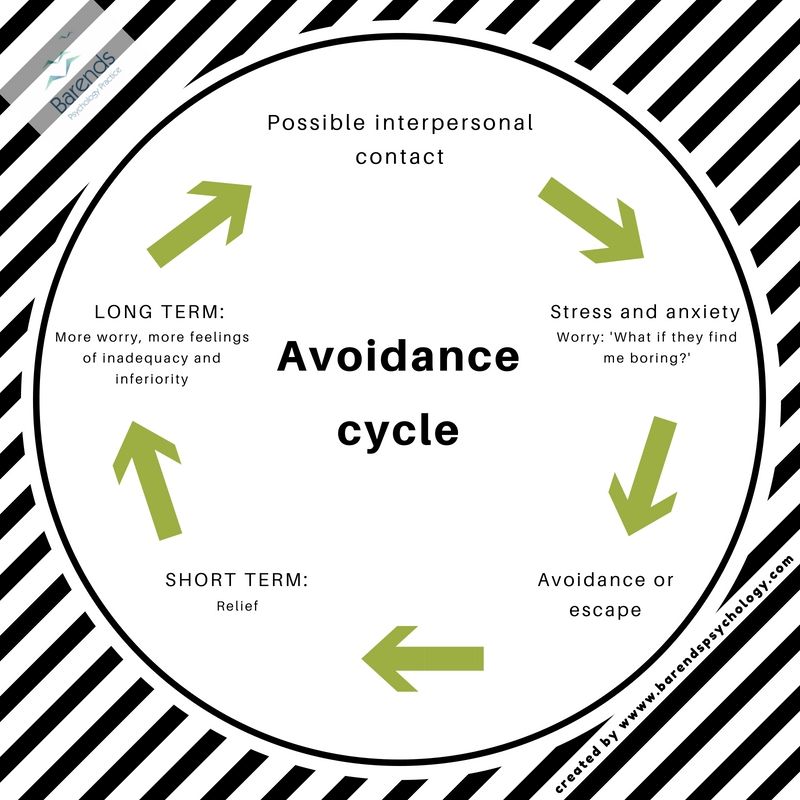
The conditioned avoidance reflex is formed on the basis of the classical combination of the conditioned and unconditioned stimulus. At stage I, a neutral event acquires the character of a trigger factor due to the fact that it is combined in time with a stimulus that, by its nature, causes anxiety. Due to this, objects, situations that were previously neutral in their content, as well as thoughts and images, by the mechanism of a conditioned reflex, cause emotional stress. At stage II, an avoidance reaction is formed, which reduces emotional stress.
Emotions play a regulatory role in the organization of purposeful behavior. Behavioral avoidance is reinforced through the ability to reduce emotional discomfort. Thus, emotions determine the formation of behavior aimed at satisfying the basic need for security. Behavioral responses that have been useful in a similar situation in the past are recorded.
The typology of PI, based on the physiological approach, suggests the allocation of active and passive avoidance variants [3].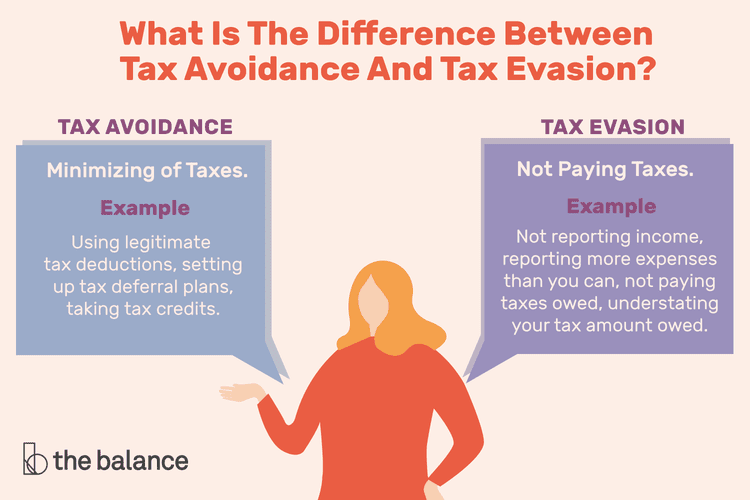 Passive avoidance is a system of behavior aimed at preventing contact with stimuli that provoke emotional stress. At its core, passive avoidance is a direct analogue of the flight response. The protective value of passive avoidance lies in the rejection of certain forms of behavior, which allows you to avoid encountering situations that cause emotional stress [3]. An example of passive avoidance is the desire of patients with agoraphobia (AF) to avoid getting into a situation of difficult assistance.
Passive avoidance is a system of behavior aimed at preventing contact with stimuli that provoke emotional stress. At its core, passive avoidance is a direct analogue of the flight response. The protective value of passive avoidance lies in the rejection of certain forms of behavior, which allows you to avoid encountering situations that cause emotional stress [3]. An example of passive avoidance is the desire of patients with agoraphobia (AF) to avoid getting into a situation of difficult assistance.
Active avoidance is a system of actions aimed at eliminating the consequences of possible contact with a stimulus that provokes emotional stress. At its core, active avoidance is a compromise between fight and flight responses. The protective value of active avoidance lies in the development of new forms of behavior that reduce anxiety. An example of active avoidance is frequent repeated handwashing in compulsions of contamination and contamination.
It is believed that passive avoidance is more characteristic of patients with obsessive fears (phobias), while active avoidance is more common in patients with ideational obsessions (obsessions).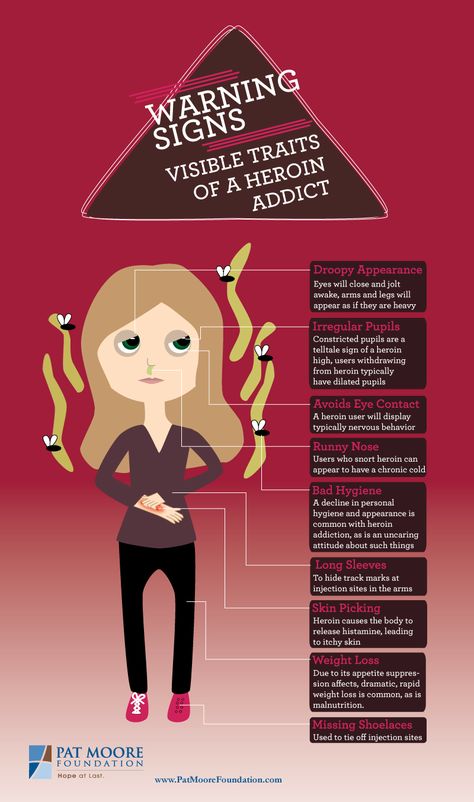
A protective stereotype of behavior is fixed because of its effectiveness. Both passive and active avoidance can reduce the level of emotional stress.
PI is characterized by a variety of manifestations. PI can take different forms - avoidance of a collision with threatening objects and situations, suppression or distraction from fears, doubts, memories, painful bodily sensations.
In behavioral psychology, the terms "avoidance" and "escape" are used to refer to PIs. The term "avoidance" (leaving for a safe space) is used to describe the passive version of the PI. The term "escape" (action to prevent the application of the stimulus) is used to refer to the active PI variant.
The PN typology, developed on the basis of the psychological approach, provides for the identification of emotional and cognitive avoidance along with PN [4]. Emotional avoidance is understood as behavior aimed at getting rid of unwanted internal experiences and those external influences that cause them, a tendency to abandon certain personally significant emotions, ideas, memories, sensations [2, 5].
There are two relatively independent components in emotional avoidance. The emotional component itself expresses rejection, a negative assessment of certain external and internal stimuli and the experiences associated with them. The behavioral component is the actions taken to eliminate threatening stimuli and experiences. Emotional avoidance is maintained and fixed through negative reinforcement.
Cognitive avoidance is based on the processing of information with the analysis of the situation to prevent undesirable developments [6, 7]. The conditionality of dividing integral mental activity into separate processes, functions, and states makes it difficult to unambiguously distinguish between emotional and cognitive avoidance. In this regard, it is hardly possible to single out discriminating features that make it possible to clearly distinguish between emotional and cognitive avoidance. Any variant of avoiding behavior is not possible without the participation of both emotions and thinking.
PI in many cases has a protective compensatory character. In particular, the PI of patients with severe somatic diseases that pose an immediate threat to life, such as attacks of angina pectoris, bronchial asthma, and paroxysmal cardiac arrhythmias, has a protective, psychologically motivated character. Avoiding situations of difficult medical care, physical and emotional overload in these cases is absolutely justified and justified.
Avoidance acquires a pathological character in cases where the severity of avoiding behavior does not correspond to a real threat, or it persists for a long time after the real danger has passed. The constant and unreasonable desire to avoid confrontation with anxiety-provoking stimuli is combined with a disproportionate, excessive anxious reaction to real sources of danger, thoughts and images associated with the threat.
PI is an objective clinical indicator that reflects the severity of the condition. The severity of avoidance varies widely. Depending on the severity of defensive behavior, selective and absolute avoidance are distinguished. With selective avoidance, patients tend to avoid encountering a limited, strictly defined number of objects and situations. In the case of absolute avoidance, the desire to avoid contact with external stimuli acquires an undifferentiated character. Patients try to avoid contact with almost all objects and situations that are to some extent thematically related to the content of painful experiences.
Depending on the severity of defensive behavior, selective and absolute avoidance are distinguished. With selective avoidance, patients tend to avoid encountering a limited, strictly defined number of objects and situations. In the case of absolute avoidance, the desire to avoid contact with external stimuli acquires an undifferentiated character. Patients try to avoid contact with almost all objects and situations that are to some extent thematically related to the content of painful experiences.
In psychology, avoidance is referred to as archaic coping strategies closely associated with negative emotionality and low self-esteem [8, 9]. The coping strategy of avoidance provides a reduction in the experience of threat in individuals with a high level of anxiety. In a stressful situation, patients experience a feeling of confusion and helplessness, in this regard, they tend to evade, avoid difficult conflict situations [9].
Avoidance is a behavioral strategy aimed at limiting contacts with the surrounding reality and avoiding solving emerging problems. The choice of a strategy of coping behavior in a given situation is largely determined by the characteristics of the individual. Avoidance is the main strategy of defensive behavior of persons with sensitive character accentuation. The underdevelopment of communication skills, the lack of experience in active problem solving determines the constant appeal of people with a sensitive warehouse to avoidance. Persons with sensitive accentuation are afraid of being rejected, of failing. At the same time, they are convinced that they must avoid difficult, problematic situations at all costs. Due to fear of failure, they avoid new responsibilities, promotions, "tend to keep to themselves and not attract attention." Any failure, problem in interpersonal relationships is perceived by them as a disaster.
The choice of a strategy of coping behavior in a given situation is largely determined by the characteristics of the individual. Avoidance is the main strategy of defensive behavior of persons with sensitive character accentuation. The underdevelopment of communication skills, the lack of experience in active problem solving determines the constant appeal of people with a sensitive warehouse to avoidance. Persons with sensitive accentuation are afraid of being rejected, of failing. At the same time, they are convinced that they must avoid difficult, problematic situations at all costs. Due to fear of failure, they avoid new responsibilities, promotions, "tend to keep to themselves and not attract attention." Any failure, problem in interpersonal relationships is perceived by them as a disaster.
Abrupt changes in an established life stereotype become traumatic for an anancaste person. The manifestation of avoidance among anancasters is the rejection of the new, opposition to attempts at change and modernization.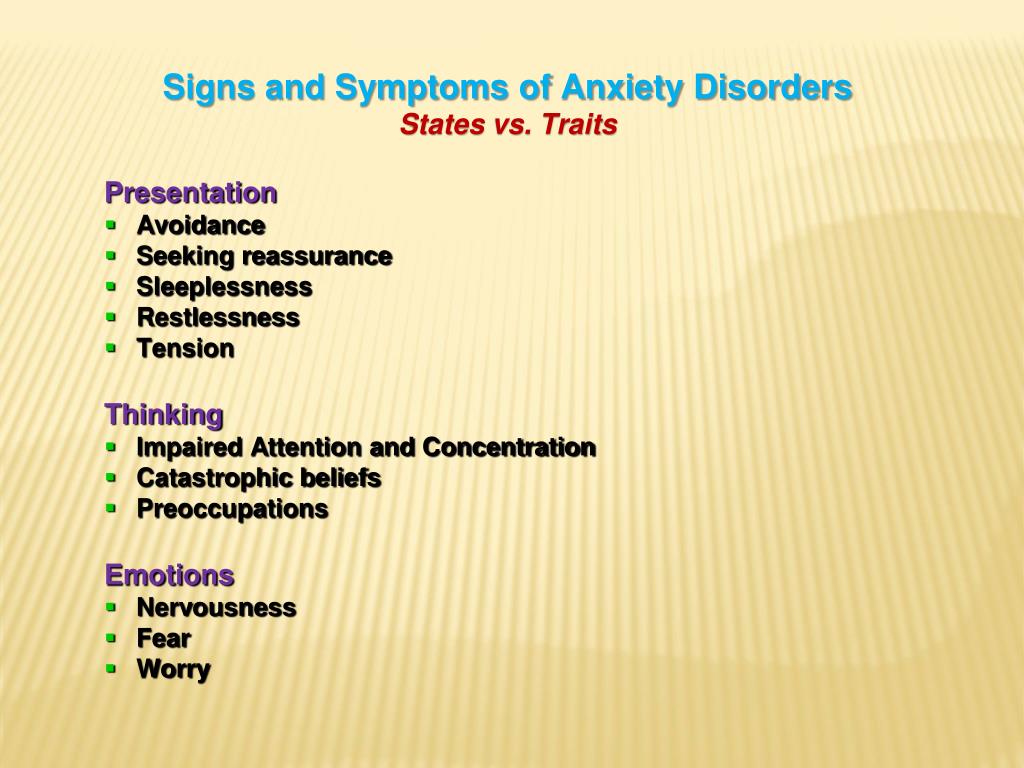
For hysterical individuals, situations that do not allow satisfying the need for increased attention, recognition of others become psycho-traumatic. Persons with hysteroid accentuation of character are not capable of systematic, painstaking work, they avoid situations in which they find themselves on the sidelines.
The tendency for avoidant behavior in schizoid persons is associated with the lack of need for communication as such, lack of empathy. The unusual and even paradoxical nature of emotional response determines the extreme selectivity in communication, the desire to evade deep emotional contacts.
Among the various clinical variants of personality disorders identified in the International Classification of Diseases, 10th revision, anxiety (avoidant) disorder (AD) occupies a special position. The main feature of avoidant disorder is hypersensitivity to potential rejection. Formalized operational diagnosis of avoidant personality disorder requires the presence of at least 4 of 6 criteria, 3 of which reflect PI:
a) avoidance of social or work activities, including interpersonal contacts, due to fear of criticism, disapproval, rejection;
b) unwillingness to enter into relationships with people, not being sure of their attractiveness;
c) limited lifestyle due to the need for physical security.
PI is typical for different variants of TR. The motivational component of anxious affect determines the desire to avoid objects and situations that pose a real or imagined threat.
Compulsive disorders are characterized by avoidance of the so-called risk situations that cause the actualization of obsession. The constancy and invariance of the plot of painful experiences is a characteristic feature of phobias - obsessive fears. This is one of the main differences between phobias and other disorders of the anxiety spectrum, in which the content of the cognitive component of anxiety is variable. Encountering a phobic stimulus causes an increase in anxiety. In this regard, the avoidance of phobic stimuli is the main form of defensive behavior of patients with obsessive fears.
The plot of ideational obsessions (obsessions), obsessive doubts, memories, ideas can change very quickly. In this regard, PI is not so effective in obsessions [8]. Moreover, with abstract obsessions (obsessive philosophizing, obsessive counting), the probability of actualization of painful experiences depends little on external situational factors.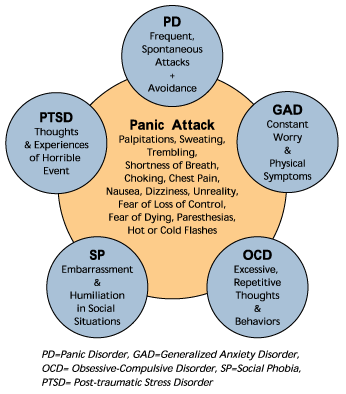 With abstract obsessions, PI, as a rule, is impossible.
With abstract obsessions, PI, as a rule, is impossible.
The phenomenon of avoidance is considered as one of the main factors determining the occurrence and persistence of obsessive disorders. Avoidance of potential danger, often exaggerated or imagined, reduces the level of anxiety and fabricated fear of potential sources of danger. Protective actions in the form of avoiding danger, on the one hand, temporarily weaken the feeling of anxiety, but on the other hand, through the mechanism of negative reinforcement, they contribute to the fixation of obsessions.
Social phobias (SF). Patients with SF use various forms of active avoidance and PI to reduce anxiety levels. The severity of PI varies widely - from the refusal of optional meetings and contacts (selective avoidance) to the complete refusal of any social contacts (absolute avoidance).
Avoidance of eye contact during communication is a special form of active PI inherent in patients with social fears [10, 11]. As a rule, in order to hide the experienced emotions, patients avert their eyes to the side, fix their eyes on foreign objects. Refusal of direct eye contact with the interlocutor allows patients to prevent the appearance of painful erroneous judgments about a possible negative assessment of their personal qualities, intelligence, behavior by others.
As a rule, in order to hide the experienced emotions, patients avert their eyes to the side, fix their eyes on foreign objects. Refusal of direct eye contact with the interlocutor allows patients to prevent the appearance of painful erroneous judgments about a possible negative assessment of their personal qualities, intelligence, behavior by others.
Fear of being the center of attention determines the desire to avoid any form of communication. Patients refuse to meet with friends and acquaintances, they specifically select work that involves a minimum of contacts.
In SF, avoidance behavior is a link between anxiety and depressive disorders [12]. The lack of social support and forced isolation are considered as two main psychological factors that determine the development of depressive symptoms. The reduction of PI in psychotherapeutic and drug treatment is accompanied by a decrease in the level of depressive symptoms.
Panic disorder and AF. In AF, the dominant emotional experience of patients is the fear of falling into a "trap", i.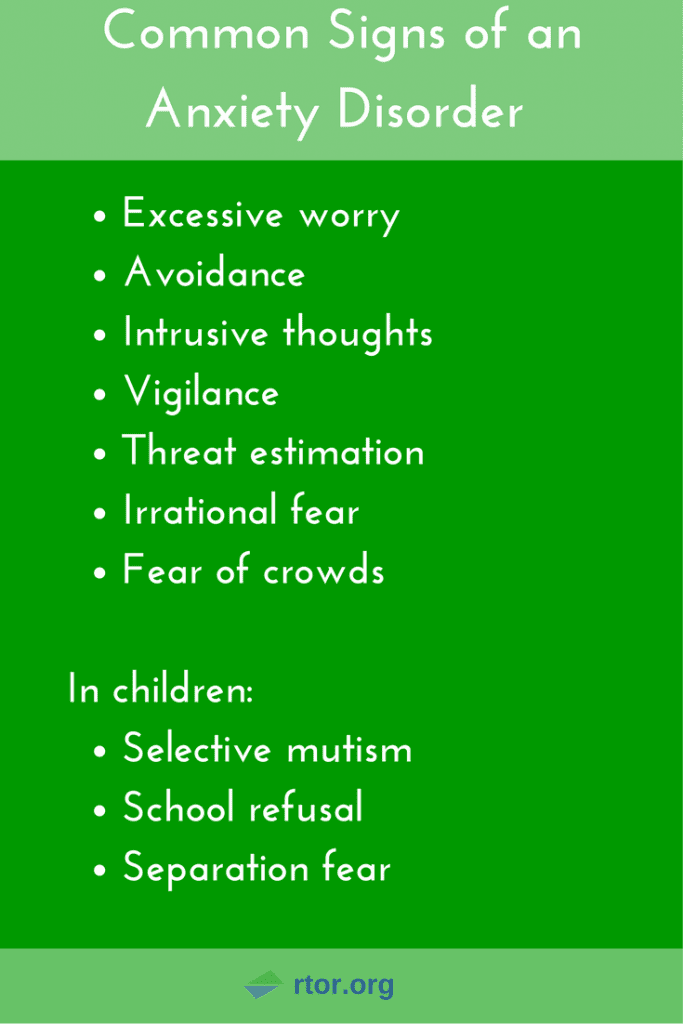 e. a situation in which there is no access to "safety signals". The PI is based on the desire to gain access to a safe place, which is such a "safety signal".
e. a situation in which there is no access to "safety signals". The PI is based on the desire to gain access to a safe place, which is such a "safety signal".
In some cases, patients avoid strictly defined situations: traveling by public transport during rush hour, visiting entertainment centers, hypermarkets. Critical attitude to behavior, the ability to overcome fear are preserved.
In other cases, PI becomes undifferentiated. There is no dependence between the severity of avoidance and the probability of getting into a “dangerous” situation. Patients avoid any situation of difficult assistance. The critical attitude to behavior is lost.
PI is considered as the most unfavorable prognostic symptom of AF. The most widespread and recognized among specialists is the systematics of defensive behavior of the passive type with the allocation of situational, interoceptive avoidance options, as well as avoidance based on experience [12, 13].
Situational avoidance is aimed at avoiding external objects and situations that cause anxiety and actualization of obsessions.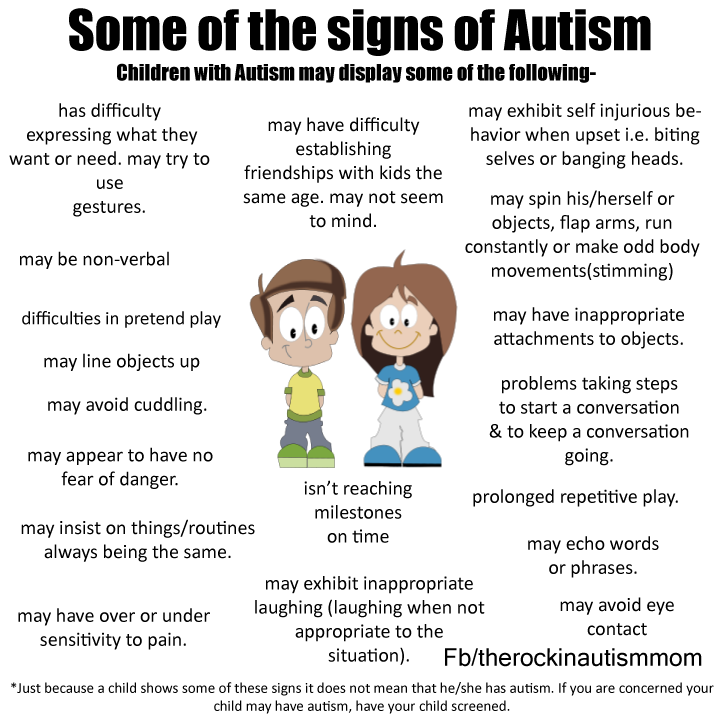 First of all, patients avoid situations in which it may be difficult to provide emergency care - they refuse to visit stadiums, travel by public transport, and travel out of town. At its core, situational avoidance is a special form of so-called spatial defense.
First of all, patients avoid situations in which it may be difficult to provide emergency care - they refuse to visit stadiums, travel by public transport, and travel out of town. At its core, situational avoidance is a special form of so-called spatial defense.
Interoceptive avoidance involves limiting or even completely avoiding various types of physical activity (brisk walking, running, lifting weights) and the use of substances (alcohol, caffeine, nicotine) that can cause autonomic shifts that resemble the clinical manifestations of panic attacks (PA).
Finally, experiential avoidance aims to facilitate coping with phobic stimuli through the use of so-called "safety cues" to reduce anxiety. The constant wearing of a mobile phone for an emergency call can help reduce the anxiety of waiting for a repetition of PA. To reduce anxiety, various mental techniques can be used, for example, distraction when counting various objects and objects that are in the field of view.
Protective behavior has its own characteristics depending on the predominance of certain vegetative disorders in the PA structure. Patients with cardiophobia and strokeophobia, which are based on PA with a predominance of cardiovascular disorders, try, if possible, to avoid exposure to factors that can adversely affect the state of coronary and cerebral blood flow. In the case of a predominance of respiratory disorders in the PA structure and the associated fear of suffocation, patients tend to avoid stuffy, poorly ventilated rooms, use a special ventilation regimen, and perform special breathing exercises.
Obsessions of an extracorporeal threat. PI in mysophobia is based on the presence of a stable relationship between the emotion of disgust and anxiety [14]. Disgust motivates avoidance of objects and situations, contact with which is characterized by an increased risk of contamination and infection with bacteria, viruses, and helminths. Protective behavior in mysophobia consists of active (frequent washing of hands, treatment of objects with antiseptics) and passive (putting on protective clothing, gloves) avoiding actions [14].
Contrasting obsessions (CI) are characterized by the involuntary appearance in the mind of thoughts, inclinations, images, feelings that are opposite to the moral and ethical attitudes and views of the patient. Experiences of auto- and hetero-aggressive content - suicidal and homocidophobia - can be attributed to the most common CIs.
PI is aimed at avoiding situations that increase the likelihood of the implementation of aggressive impulses. Protective behavior of patients has its own characteristics depending on the direction of painful experiences. Patients with homocidophobia avoid visiting crowded places, try not to leave the house if possible. In the case of suicidophobia, patients do not approach open windows, try not to go out onto the balcony, and when traveling on the subway, stay away from the edge of the platform.
The main content of fear is usually accompanied by a fear of objects that can be used to realize a painful impulse. The most common fear of sharp objects - knives, razors, scissors.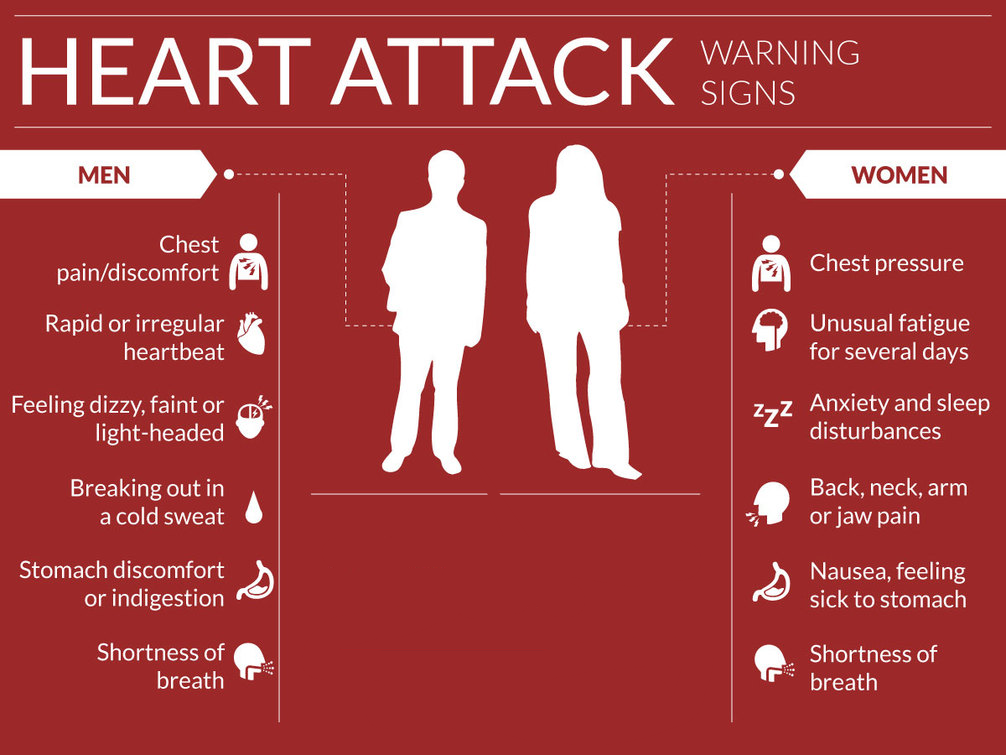 With a preventive protective purpose, patients withdraw from circulation all piercing and cutting objects.
With a preventive protective purpose, patients withdraw from circulation all piercing and cutting objects.
Many patients with CI tend to avoid any physical contact with others (touching, shaking hands, hugs) as much as possible, which increases the likelihood of the implementation of aggressive urges. Fearing the commission of violent acts, patients limit or even completely refuse intimate relationships with sexual partners.
Patients with a retrospective direction of the anxiety vector carefully follow the criminal chronicle, media reports concerning violent actions, repeatedly return to those places where, in their opinion, aggressive actions may have been committed.
Contrasting desires can acquire an imperative character. In this case, in order to overcome the urge, patients are forced to perform substitution actions, which are a special form of active PI. To overcome the urge to aggression, reduce emotional damage, patients are forced to perform auto-aggressive actions in the form of injections, cuts.
Isolated (simple) phobias (IF). The main clinical manifestation of IF is an obsessive fear of any specific objects and situations: elevator rides, air travel, heights, natural phenomena, animals or insects. With simple phobias, in the vast majority of cases, there is no tendency to generalize obsessions with the formation of secondary fears. In this regard, the PI is selective. Strictly defined situations that cause the actualization of fear are avoided.
Generalized TR (GTR). The symptomatology of GAD is represented by diffuse anxiety of indefinite or polythematic content, relatively constant over time. The course of the disease, as a rule, has a fluctuating character with exacerbations caused by psycho- and somatogenic factors.
"Avoidance through anxiety" in the GAD model is considered by T.Borkovec as the main behavioral mechanism that allows to reduce the level of emotional problems [6]. Anxiety in T.Borkovec's model performs two main functions. First, “consider and prepare” yourself for different options for an undesirable development of events. Secondly, to reduce the severity of the vegetative component of the emotional reaction to the fear-inducing image. It is important to note that in GAD, PI is directed not only to stimuli that are actually associated with danger, but also to any objects and situations that have an associative connection with them.
First, “consider and prepare” yourself for different options for an undesirable development of events. Secondly, to reduce the severity of the vegetative component of the emotional reaction to the fear-inducing image. It is important to note that in GAD, PI is directed not only to stimuli that are actually associated with danger, but also to any objects and situations that have an associative connection with them.
A common feature of phobic and delusional avoidance is the irrational, unreasonable nature of behavior. In both cases, the perceived (with phobic avoidance) and real (with delusional avoidance) threat are centered on the patient's personality.
Phobic avoidance is aimed at avoiding a possible, potential threat. Characteristic is the relative constancy of avoided objects and situations. The rationale for defensive behavior may be missing. Quite often, patients cannot name possible negative consequences with avoided objects and situations.
In most cases, a critical attitude towards PN is preserved. Under certain conditions, thanks to the help and support of others, patients can overcome fear, refuse to avoid avoiding phobic objects and situations.
Under certain conditions, thanks to the help and support of others, patients can overcome fear, refuse to avoid avoiding phobic objects and situations.
PI is most typical for patients with delusional ideas of persecutory content. According to the patient, avoidance is determined by the threat that really exists at the moment. All experiences and behavior are related to the current situation. Characteristic is the variability of avoided objects and situations. In acute sensual delirium, avoidance is of an undifferentiated nature; random, sometimes even unfamiliar faces that are currently in sight are considered as a source of danger. In chronic interpretive delirium, the number of persecutors and ill-wishers includes a very specific circle of people who, according to the patient, use different methods of causing physical, material or moral damage.
No critical attitude to painful experiences and behavior. PI, as the emotional saturation increases and the plot of delusional ideas changes, can be replaced by verbal or physical aggression - "he avoids, he defends himself, he attacks.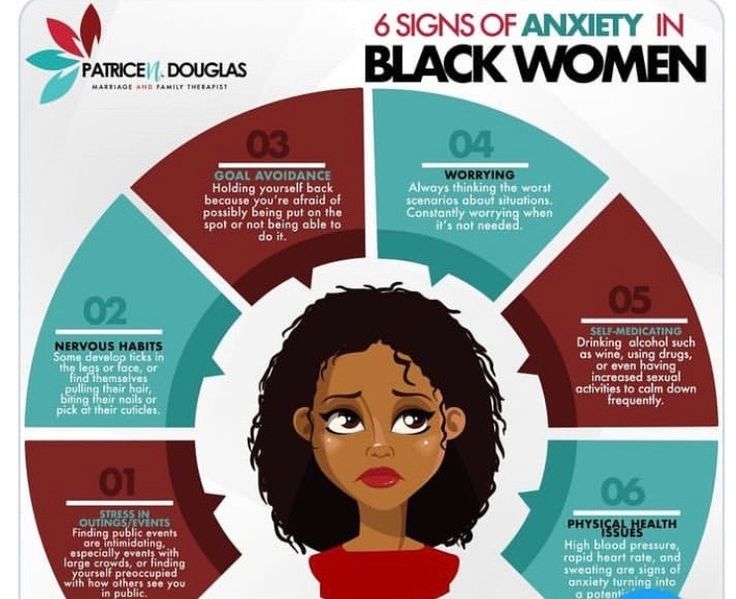 "
"
Intimacy avoidance: the syndrome of the 21st century
Psychology, Psychology of relationships, Self-development
Contents
- 1 Intimacy avoidance syndrome
- 2 Intimacy fear symptoms
- 3 Is it possible to overcome intimacy avoidance syndrome?
People seek intimacy with their own kind. Everyone needs someone who can be trusted and tell everything that has accumulated in the soul, boldly open up without fear of condemnation ... This seems to be an axiom. But in fact, many are afraid of intimacy, like fire. Why is this happening, is there really a problem and can it be dealt with?
Intimacy avoidance syndrome
Psychologists believe that intimacy avoidance is a real syndrome, a scourge for people of the 21st century. We stopped reaching out to each other, we are afraid to open up, showing ourselves not from the best side, we start only superficial relationships. Sometimes people avoid intimacy not only with friends and friends, but also with their spouses.
Why is this happening? There are several reasons:
- Features of society. We transfer communication to the virtual world, gradually narrowing personal contacts. On the Internet, it is easier to hide your true face and present yourself as who you want to appear to be. This is starting to extend to real relationships as well. People hide behind masks, just as they hide behind avatars on the net, without showing their true "I".
- Fear of judgment. We are afraid of ridicule and condemnation, so many choose superficial contacts as a defense, replacing true intimacy.
- Presence of a traumatic experience. Sometimes, having opened up to someone, we receive indifference or complete misunderstanding in response. The more such experiences in the past, the scarier it is to open yourself up in the future. Gradually, a person completely closes himself from the world, demonstrating only a certain chosen social role.
The importance of the right environment: find out here how to choose who to communicate with.
Symptoms of fear of intimacy
The fact that a person strives to avoid intimacy in relationships is indicated by the following signs:
- he prefers not to tell about himself even to people with whom he has a long-term relationship;
- panics at the thought that someone will learn confidential information about him;
- feels that he is wearing a "mask" and is afraid that someone will guess about it;
- easily breaks up with people and lets them go, not trying to improve relations after a conflict situation;
- can say that he doesn't have any really close friends.
When trying to build relationships with people, it's helpful to know what types of people there are and why each type needs a different approach. Who are introvert, extrovert and ambivert, read here .
Is it possible to overcome intimacy avoidance syndrome?
What to do if you find signs of avoidance of close relationships? First of all, to understand the reasons for the appearance of this psychological "syndrome". If it’s about trauma and rejection, you should contact a psychologist. It will help to process the traumatic experience, removing the emotional tension that has become an obstacle to the formation of close relationships.
If it’s about trauma and rejection, you should contact a psychologist. It will help to process the traumatic experience, removing the emotional tension that has become an obstacle to the formation of close relationships.
Find out here what to do if your privacy is violated.
If the reason is fear of judgment from another person, it is worth thinking about what trust is. When we trust someone, we always take a risk. And you can either take this risk, realizing that no one can guarantee that they will not deceive your expectations, or you can continue to live in your “case”. Hiding is safer, but it makes life gray and boring. Get in the habit of gradually getting to know people before showing them your true experiences. The more you yourself know about a friend, the easier it is to assess whether you can trust him, whether it makes sense to deepen relationships. Learn 5 Signs envious person who expose his nature.