Sensitive to chewing sounds
Misophonia: Triggers & Management
People who suffer from misophonia do, in fact, have real physiological effects when they are exposed to the provoking sounds.
Misophonia is a condition in which a person is overly sensitive to sounds. Usually the trigger sounds are noises made by other people, such as chewing or tapping a pen. People who suffer from misophonia become disturbed or aggravated when they hear the sounds. Some misophonics avoid the irritating sounds by physically leaving the room, while others may display angry outbursts.
Sounds that trigger misophonia
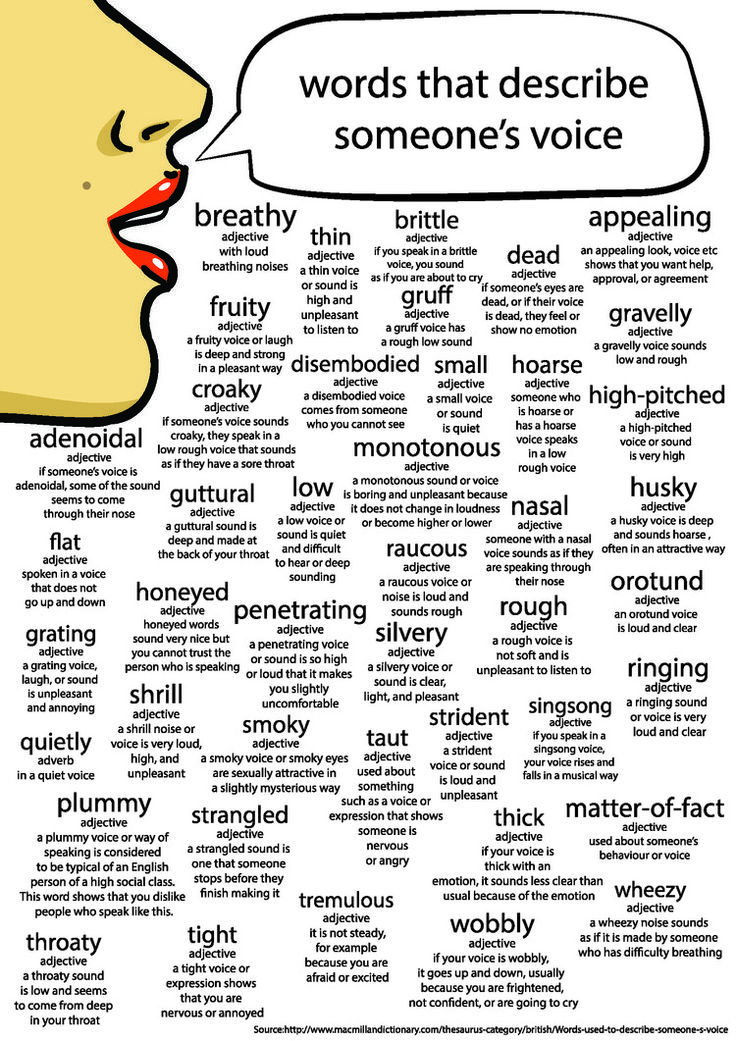
A number of sounds can elicit the agitation characteristic of misophonia. Chewing noises are probably the most common trigger, but other sounds such as slurping, crunching, mouth noises, tongue clicking, sniffling, tapping, joint cracking, nail clipping, and the infamous nails on the chalkboard are all auditory stimuli that incite misophonia.
Most of the sounds that trigger misophonia are produced by the human body, but some misophonics become annoyed by the sounds of inanimate objects, such as clicking of a remote control or the whirring of a motor, although the degree of irritation is not usually as severe. Interestingly, people who suffer from misophonia do not experience irritation when they produce the same exact noises themselves.
Physical response to trigger sounds
It turns out that people who suffer from misophonia do, in fact, have real physiological effects when they are exposed to the provoking sounds. The few studies of the physiology of this condition demonstrate that physical responses include measurable autonomic responses that are not seen in a control group.
Comorbid conditions
There are degrees of severity misophonia, and it can be heightened in times of stress. Comorbid conditions include obsessive-compulsive disorder and generalized anxiety disorder, but interestingly, there is not an association with attention deficit hyperactivity disorder.
Managing misophonia
Most people who experience misophonia have enough insight to understand that their level of agitation is not reasonable or fair and would like to reduce the symptoms. A few common methods of self-treatment include simply leaving the room, wearing headphones, or finding a way to drown out the noise. Self-distraction is a more advanced and difficult technique of managing symptoms and it is easier to practice distraction in times when personal stress level is low and when the noises themselves are less agitating. Some misophonia sufferers cope with the feelings of turmoil by mimicking the annoying sounds, which seems to disempower the sounds while also possibly allowing an acceptable ‘venting’ of some of the illogical rage.
A few common methods of self-treatment include simply leaving the room, wearing headphones, or finding a way to drown out the noise. Self-distraction is a more advanced and difficult technique of managing symptoms and it is easier to practice distraction in times when personal stress level is low and when the noises themselves are less agitating. Some misophonia sufferers cope with the feelings of turmoil by mimicking the annoying sounds, which seems to disempower the sounds while also possibly allowing an acceptable ‘venting’ of some of the illogical rage.
There have not been studies looking at therapeutic treatment for misophonia and at this time there is no standard pharmacological approach. It appears to be a disorder that is likely to be self-diagnosed. In some instances, friends or family members who are repeatedly the targets of anger may identify the problem. But, it is possible that some sufferers could lack the conscientiousness to insightfully self diagnose themselves or that some misophonia sufferers could become violent, believing that the perpetrator of the noise is to blame.
Have you ever had to deal with misophonia in the clinical setting? How would you advise patients and their loved ones to cope with this disorder?
Reference: Edelstein M, et al. Misphonia: physiological investigations and case descriptions. Front Hum Neurosci. 2013 Jun 25;7:296.
What Is Misophonia?
Written by WebMD Editorial Contributors
In this Article
- What Happens?
- How Do You Get It?
- How Do You Treat It?
Do certain daily sounds trigger an over-the-top emotional reaction, but yet don’t seem to bother anyone else?
This is the case with misophonia -- a strong dislike or hatred of specific sounds.
What Happens?
Misophonia is a disorder in which certain sounds trigger emotional or physiological responses that some might perceive as unreasonable given the circumstance. Those who have misophonia might describe it as when a sound “drives you crazy.” Their reactions can range from anger and annoyance to panic and the need to flee. The disorder is sometimes called selective sound sensitivity syndrome.
The disorder is sometimes called selective sound sensitivity syndrome.
Individuals with misophonia often report they are triggered by oral sounds -- the noise someone makes when they eat, breathe, or even chew. Other adverse sounds include. keyboard or finger tapping or the sound of windshield wipers. Sometimes a small repetitive motion is the cause -- someone fidgets, jostles you, or wiggles their foot.
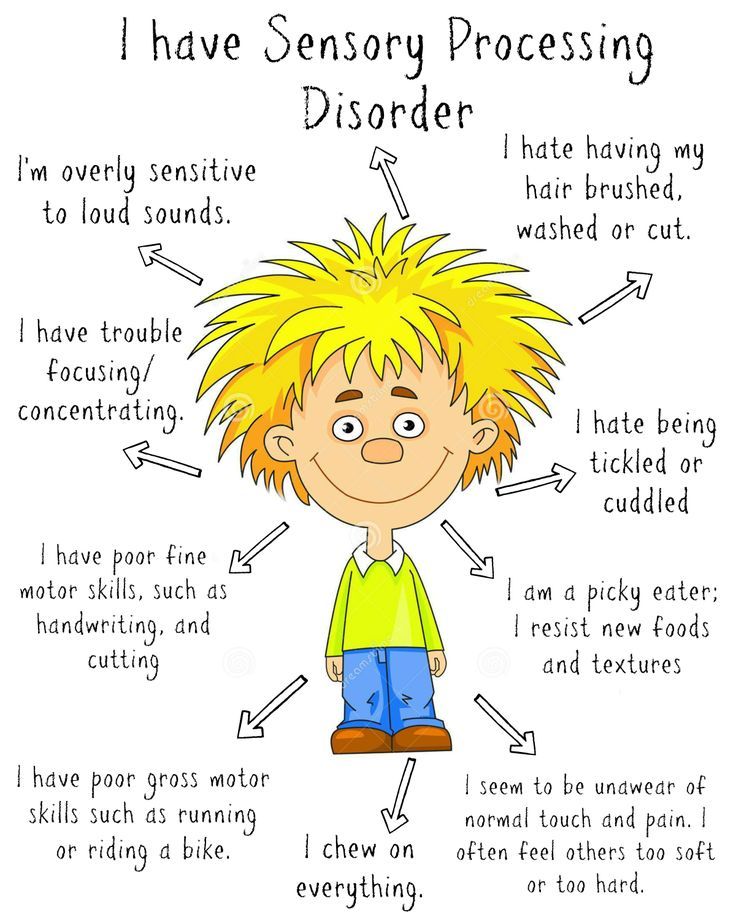
Similarly, people with misophonia also say they often react to the visual stimuli that accompanies sounds, and may also respond intensely to repetitive motions. Researchers believe that those with misophonia may already have issues with how their brains filter sounds and that one of the features of “misophonic sounds” may be their repetitive noise. That repetition then exacerbates the other auditory processing problems.
The disorder appears to range from mild to severe. Individuals report a range of physiologic and emotional responses, with accompanying cognitions. If you have a mild reaction, you might feel:
- Anxious
- Uncomfortable
- The urge to flee
- Disgust
If your response is more severe, the sound in question might cause:
- Rage
- Anger
- Hatred
- Panic
- Fear
- Emotional distress
The disorder can put a cramp in your social life. Those with the misophonia have been known to develop anticipatory anxiety when going into situations where trigger sounds may be present. You might avoid restaurants or eat separately from your spouse, family, or roommates.
Those with the misophonia have been known to develop anticipatory anxiety when going into situations where trigger sounds may be present. You might avoid restaurants or eat separately from your spouse, family, or roommates.
Over time, you may also respond to visual triggers, too. Seeing something that you know may create the offending sound may elicit a response.
How Do You Get It?
The age of the onset of this lifelong condition is not known but some people report symptoms between the ages of 9 and 13. Misophonia is more common with girls and comes on quickly, although it doesn’t appear to be related to any one event.
Doctors aren’t sure what causes misophonia, but it’s not a problem with your ears. They think it’s part mental, part physical. It could be related to how sound affects your brain and triggers automatic responses in your body.
Because your ears are normal and your hearing is OK, the doctor may have trouble with a diagnosis. Misophonia is sometimes mistaken for anxiety or bipolar or obsessive-compulsive disorder. Some doctors think it should be classified as a new disorder.
Some doctors think it should be classified as a new disorder.
Often doctors are unaware of the condition, and there is no consensus in regard to classification. Misophonia appears to occur on its own and also along with other health, developmental and psychiatric problems.
A breakthrough study recently found that misophonia is a brain-based disorder. Researchers point to a disruption in the connectivity in parts of the brain that process both sound stimulation and the fight/flight response. It also involves parts of the brain that code the importance of sounds.
How Do You Treat It?
The condition does affect daily life, but you can learn to manage it.
Treatment often involves a multidisciplinary approach combining sound therapy by audiologists and supportive counseling in which coping strategies are emphasized.
You might try a device like a hearing aid that creates a sound in your ear similar to a waterfall. The noise distracts you from triggers and reduces reactions.
Other treatments include talk therapy.
Your lifestyle also plays a role. Get regular exercise, plenty of sleep, and manage your stress. You can also wear ear plugs and headsets to tune out sounds. Set up quiet areas or safe spots in your home where no one will make the noises that bother you.
And find support. The Misophonia Association is based in Oregon and California, and holds a yearly convention for suffers. The International Misophonia Research Network Misophonia-Research.com is a resource for doctors and researchers interested in learning more about misophonia. Misophonia International.com offers free resources, such as handouts for parents, and webinars in association with Duke University for those in the U.S., Canada and U.K.
Finally for those in the U.K. who are looking for support and research reports, try www.allergictosound.com
You can also find online and social media groups where people share coping strategies.
causes, symptoms, prevention and treatment
Types of bruxism
There are three forms of bruxism:
-
Noisy bruxism or grinding.
 Grinding of the teeth occurs when the chewing muscles and lower jaw move. The long course of the disease is dangerous pathological abrasion of teeth.
Grinding of the teeth occurs when the chewing muscles and lower jaw move. The long course of the disease is dangerous pathological abrasion of teeth. -
Silent bruxism or clenching of teeth. A typical symptom is a tightly clenched jaw without extraneous sounds. To a lesser extent provokes a decrease in enamel. More often leads to the formation of cracks in the tooth enamel. nine0003
-
mixed form. Combines the features of the two forms described above.
Depending on the time of occurrence of dental grinding, bruxism is divided into daytime, nighttime and combined (episodes are repeated regardless of the time of day).
Causes of bruxism
In infants, bruxism is regarded as a variant of the norm. In this way, the child tries to reduce the intensity of the discomfort associated with the eruption of milk teeth. nine0003
Help! The prevalence of bruxism in children under 7 years of age is 50-80%. The second peak of the disease occurs at the age of 13–18 years.
The second peak of the disease occurs at the age of 13–18 years.
At any other age, the manifestation of teeth grinding is based on a combination of several causes:
-
hereditary predisposition. The chance of bruxism in a child is 50% higher if first-line relatives suffered from this disease. nine0003
-
dental factors. Episodes of involuntary teeth grinding provoke congenital and acquired disorders in the structure and functioning of the dental system. Due to the deformation and trauma of the teeth, malocclusion, developmental anomalies, the jaws do not completely close, and in order to ensure the coordinated operation of the chewing apparatus, the muscles come into tone, the muscle fibers involuntarily contract. Poor-quality dental treatment, incorrectly selected prostheses and braces, arthritis and arthrosis of the temporomandibular joint initiate bruxism. nine0003
-
Diseases of the nervous system. Teeth grinding can occur as a result of birth or traumatic brain injury, damage to the central nervous system during fetal development or during childbirth (perinatal encephalopathy).

-
Pathology of ENT organs. At risk are patients who have permanently disturbed nasal breathing due to adenoids, deviated nasal septum, chronic rhinitis. nine0003
-
Disorders of the psyche and behavior. Stress, neurosis, anxiety and constant experiences provoke an involuntary spasm of the masticatory muscles and gnashing of teeth. Bruxism occurs in people who constantly experience psycho-emotional overstrain, have a negative emotional mood.
-
neurological and movement disorders. A favorable condition for the manifestation of bruxism is considered deviations in the activity of the central and peripheral nervous system. The course of bruxism is often accompanied by sleep disturbance: nightmares, snoring, short-term respiratory arrest (apnea), enuresis. Tonic spasm of masticatory muscles (trismus) and bruxism occur due to damage to the motor neurons of the trigeminal nerve. Teeth grinding is one of the symptoms of neurological complications associated with the use of neuroleptic drugs (antipsychotics).
 nine0003
nine0003
Other causes of bruxism are not widely recognized, but they do exist. These include: reflux esophagitis (reflux of gastric contents into the esophagus), helminthic invasions, osteochondrosis of the cervical spine. In the occurrence of bruxism, bad habits are of some importance: smoking, alcohol addiction, coffee and chewing gum abuse, and malnutrition.
Call now
+7 (495) 186-01-41
Sign up
Symptoms of bruxism
Episodes of bruxism are accompanied by grinding and tapping of teeth. The attack lasts from a few seconds to several minutes. During the night can be repeated many times. Usually a similar symptom is observed by parents or spouses, since a person does not control his condition during sleep. After multiple nocturnal episodes of bruxism, the next morning the patient feels facial muscle and jaw pain, dizziness, headache, lack of sleep. nine0003
nine0003
Daytime bruxism is characterized by uncontrollable clenching of the teeth. Usually, a spasm of the masticatory muscles provokes some kind of stressful situation or event that requires prolonged concentration: playing on a computer, doing homework.
Help! If teeth grinding occurs during sleep, then this is bruxism. If the episodes recur during the daytime, this condition is regarded as bruxiomania. nine0003
With a combination of daytime and nighttime bruxism, the patient has concomitant symptoms:
-
instability in behavior
-
headache and dizziness,
-
problems with sleep and falling asleep,
-
pain and ringing in the ears
- nine0002 daytime sleepiness,
-
biting a pencil and pen,
-
frequent use of chewing gum,
-
discomfort when closing teeth,
-
waking up exhausted.
With a long course of bruxism, a pathological decrease in the enamel of individual or all teeth develops, chips and cracks in the enamel, fillings and dentures are formed, the sensitivity of the teeth to cold, hot, salty, sweet is exacerbated. nine0003
Injury to the periodontal tissues provokes inflammation of the periodontium (tissues surrounding the tooth), followed by mobility and premature loss of the tooth. Gingivitis, stomatitis, and fibroma of the oral cavity are the result of constant traumatization of the oral mucosa.
Complications of bruxism
Long-term undesirable consequences include dysfunction of the TMJ. This is a violation of the temporomandibular joint. The condition is accompanied by pain in the temples, neck, head, inability to open the mouth wide, clicks in the joint when yawning and chewing. The disease without treatment is dangerous by the development of arthrosis and immobilization of the temporomandibular joint.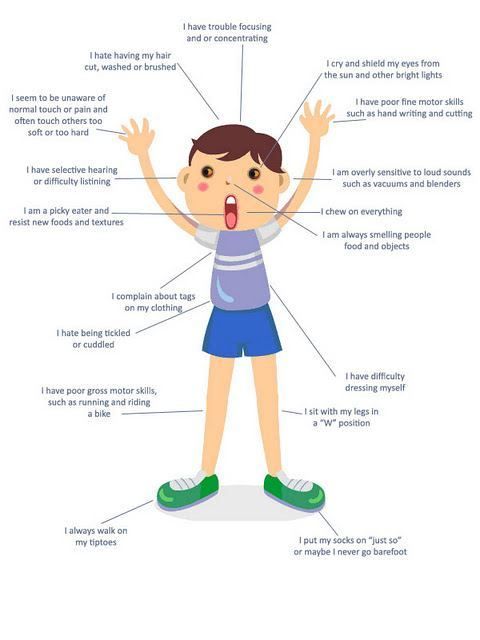 nine0003
nine0003
Chronic nocturnal bruxism is complicated by pain in the muscles of the back and neck, migraine, dizziness. Almost 80% of patients experience toothache, 65% have injuries to the tongue, lips and inner surface of the cheeks.
Bruxism diagnostics
Bruxism is confirmed by the dentist on the basis of dental examination data, complaints of the patient or his relatives about the grinding of teeth. When examining the oral cavity, the doctor detects characteristic changes: a wedge-shaped defect, malocclusion, trauma to the tongue and mucous membranes of the cheeks, lips, violation of the integrity of the enamel or dental structures. On palpation, there is tension in the muscles of the face, pain in the area of the temporomandibular joint. nine0133
For an objective assessment of bruxism, brux checkers are used. These are special caps made on the basis of a cast and model of the patient's jaw in order to determine unwanted occlusal contacts of the teeth of the upper and lower jaws. After wearing the mouth guard at night, it is transferred to the laboratory for analysis and determination of which teeth are under increased stress.
After wearing the mouth guard at night, it is transferred to the laboratory for analysis and determination of which teeth are under increased stress.
Polysomnography is used to diagnose bruxism. Before going to bed, special sensors are applied to the patient's body, which record any movements, brain activity, mobility of the temporomandibular joint. In patients with bruxism, the pathological activity of the masticatory muscles is determined. nine0003
To identify the true cause of teeth grinding, specialists of a different profile are often involved - a neurologist, otolaryngologist, gastroenterologist, psychologist.
Treatment of bruxism
Usually in young children, bruxism does not require special treatment, as it resolves on its own by the age of 7 years. To get rid of a pathological habit for adults, they use an integrated approach with the appointment of conservative therapy, dental treatment, psycho- and physiotherapy. nine0003
General recommendations for all groups of patients are fortified nutrition, moderate physical activity, alternating work and rest. It is also important to limit coffee and caffeinated drinks, alcohol, tobacco, and, if possible, eliminate stress and anxiety.
It is also important to limit coffee and caffeinated drinks, alcohol, tobacco, and, if possible, eliminate stress and anxiety.
Conservative therapy
With bruxism aggravated by neurological disorders, anticonvulsant and nootropic drugs, neurovitamins of group B, and brain metabolites are prescribed. The course of treatment is long, from 2 to 4 months under the supervision of a neurologist. nine0003
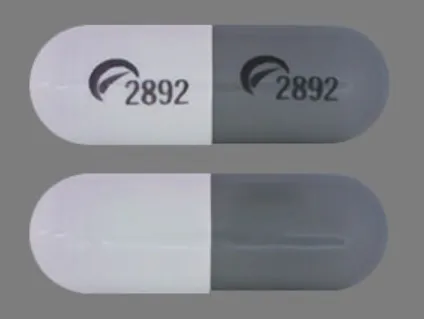
To reduce the activity of the muscles of the masticatory muscles, calcium and magnesium preparations are used, to normalize the quality of sleep and eliminate anxiety, light sedatives and hypnotics are used. Treatment is supplemented with multivitamin complexes to reduce recovery time, strengthen immunity.
Dental treatment
At the first stage, caries and periodontal inflammation, if any, are treated. Further, according to an individual cast, a protective cap is made of soft plastic and rubber. A cap is put on the upper teeth to prevent their friction against the lower teeth, to prevent the destruction of the enamel. nine0133
nine0133
After eliminating the causes and manifestations of bruxism, dentists are involved in the restoration of wedge-shaped defects, the installation of fillings, the manufacture of crowns, prostheses or veneers.
Psychotherapy
Psychological methods of influence come to the fore if the cause of bruxism is unfavorable psychological factors and events. Psychotherapy helps to identify and understand conflicts, change attitudes towards a stress factor, develop skills to cope with the difficulties of life more effectively and environmentally for the body. For this, methods of relaxation and self-control, trainings, art therapy, dance and movement therapy are used. nine0003
Physiotherapy
To enhance the functional activity of the muscles of the jaw, neck and collar zone, sessions of electrical stimulation of the muscles of the masticatory muscles are prescribed (exposure to direct and alternating current pulses). In some cases, manual therapy, massage, acupuncture, magnetotherapy, warm compresses on the jaw area show a good effect.
Prevention of bruxism
Prevention of bruxism is not specific, and involves maintaining a healthy lifestyle, getting rid of bad habits, learning self-control and forming the right life position. nine0003
Timely treatment of diseases of the nervous system minimizes the risk of bruxism. It is necessary to monitor your psycho-emotional state or the child, and, if necessary, seek psychological help.
An important link in the prevention of bruxism is a regular preventive examination 1-2 times a year at the dentist. Timely diagnosis of pathologies and the choice of adequate treatment can permanently get rid of this pathological habit. nine0003
Call now
+7 (495) 186-01-41
Make an appointment
Previous article
Next article
Hyperosmia - symptoms and causes
- Advantages nine0010
- Doctors
- Contacts
- Licenses
Benefits
-
The latest, constantly updated equipment
- nine0002 Interest-free installment plan for all services
-
Online ENT consultations
-
Departure of an ENT doctor at home
-
Friendly and qualified staff
- nine0002 24/7 ENT help
Hyperosmia is an increased sensitivity to odors. This condition can lead to discomfort and cause disruption of the usual rhythm of life. First of all, susceptibility to perfumes, household chemicals, and scented candles increases.
This condition can lead to discomfort and cause disruption of the usual rhythm of life. First of all, susceptibility to perfumes, household chemicals, and scented candles increases.
Causes and accompanying symptoms of hyperosmia can be varied. An otolaryngologist will help you understand the situation and suggest the most rational options for coping with the existing problem. The main thing is to see a doctor in time. nine0003
Causes of hyperosmia
There are several factors that determine the increased sensitivity to odors. These may be:
- Genetic predisposition - some people do have a more acute sense of smell than others. This pattern is often seen in perfumers.
- Pregnancy. The hormonal changes that occur during gestation, especially in the first trimester, can lead to the fact that a woman's sense of smell is aggravated. Pronounced aromas can even cause nausea and vomiting due to overexcitation of the corresponding centers of the medulla oblongata.
 nine0010
nine0010 - Autoimmune pathologies. Quite often, adrenal insufficiency and systemic lupus erythematosus lead to an aggravation of the sense of smell.
- Borreliosis. Approximately every second person who has been bitten by a Borrelia-infected tick has increased susceptibility to odors.
- Type 1 diabetes mellitus. In the absence of adequate compensation for carbohydrate disorders, the activity of nerve receptors changes.
- Brain lesions. A similar situation can be observed in Alzheimer's disease, Parkinson's pathology, epilepsy, multiple sclerosis. nine0010
- Pathological processes of the nasal mucosa and paranasal sinuses. This is hyperosmia in the focus of inflammation, in the area of polypoid growths, etc.
- Long-term use of vasoconstrictor drugs. These drugs can excite or depress the olfactory receptors.
- Hypovitaminosis. Especially often hyperosmia develops against the background of cyanocobalamin deficiency.
- Migraine. This disease is accompanied by headache, which is often combined with nausea and vomiting.
 nine0010
nine0010
Recently, doctors have to deal with hyperosmia in the coronavirus. Of course, this infection is more characterized by a decrease in smell, but some patients also have an increased susceptibility to smells.
Symptoms of hyperosmia
Symptoms associated with hyperosmia are determined by the nature of the pathological process. Taking into account the underlying disease, the following manifestations may occur:
- skin rashes;
- runny nose, cough, fever, soreness of the nasal mucosa; nine0010
- hand tremors, headaches, dizziness, decreased memory and concentration;
- increased sensitivity of taste buds and a burning sensation of the tongue.
Treatment of hyperosmia
Hyperosmia in men and women is treated according to the underlying etiological factor. So, in case of inflammatory lesions of the nasal mucosa and paranasal sinuses, corticosteroids, immunomodulators and antibiotics are prescribed when the conditionally pathogenic flora is activated.