Flonase and ibuprofen
Alzheimer’s Disease and Intranasal Fluticasone Propionate in the FDA MedWatch Adverse Events Database
Abstract
Background:
Studies of Alzheimer’s disease suggest that neuroinflammation or deranged brain wound healing may be a cause of some cases. But a placebo controlled study showed no effect at all on Alzheimer’s disease of low dose oral prednisone after one year. Introducing the steroid directly into the hippocampus and rhinencephalon via the nose, as happens in hay fever subjects, could be more effective.
Objective:
In the present study, we analyzed FDA MedWatch data for intranasal fluticasone propionate (Flonase) to determine the frequency of Alzheimer’s disease as an adverse event reported after use of the medication.
Methods:
Machine-readable data from MedWatch, including adverse drug reaction reports from manufacturers, are part of a public database. We used the online tool eHealthMe to query the database.
Results:
By September 20, 2017, 35,221 people reported side effects to MedWatch after taking Flonase. Among them, 9 people (0.03%) had Dementia Alzheimer’s type. By October 3, 2017, 185,636 people reported side effects after taking Lipitor. Among them, 243 people (0.13%) had Dementia Alzheimer’s type. The lower incidence of Alzheimer’s dementia in the Flonase group compared to the Lipitor group was significant (p < 0.001, Fisher exact test, two tailed).
Conclusion:
Long term use of oral non-steroidal anti-inflammatory drugs (NSAIDs) is linked with reduced risk of developing Alzheimer’s disease. Data from MedWatch suggest that fluticasone propionate administered intranasally might have a similar preventive effect to ibuprofen. Perhaps combining ibuprofen and Flonase could be therapeutic. Further studies would be desirable.
Studies of Alzheimer’s disease suggest that neuroinflammation [1] or deranged brain wound healing [2] may be responsible for some cases. Injury to the brain from trauma or irradiation may initiate the process [3]. The characteristic pathologic plaques and tangles are a non-specific result of the disease process, not a cause [4].
Biochemical and neuropathological studies of brains from individuals with Alzheimer’s disease provide clear evidence for an activation of inflammatory pathways and glial inflammation [5]. If part of the neuroinflammation is autoimmune, the predominance of Alzheimer’s disease in women could be explained, since autoimmune diseases are much more common in women than men.
However, there is no beneficial effect of non-steroidal anti-inflammatory drugs (NSAIDs), such as naproxen, rofecoxib, or ibuprofen, on cognition or overall Alzheimer’s disease severity. Oral NSAIDs have no value as an Alzheimer’s disease treatment [6].
Chou et al. showed a reduction in risk of Alzheimer’s disease in rheumatoid arthritis patients on prednisone [7]; unadjusted the effect is almost significant (p = 0.1). The reduction is quite remarkable, given the tiny amounts of prednisone that reach the brain after an oral dose due to tight plasma protein binding. Balis et al. found that the cerebrospinal fluid/plasma ratio of dexamethasone is 0. 15, of prednisolone 0.079 [8]. Such minute amounts of steroid in the brain presumably have a tiny or negligible effect. Indeed, another placebo controlled study showed no effect at all on Alzheimer’s disease of low dose oral prednisone after one year [9].
15, of prednisolone 0.079 [8]. Such minute amounts of steroid in the brain presumably have a tiny or negligible effect. Indeed, another placebo controlled study showed no effect at all on Alzheimer’s disease of low dose oral prednisone after one year [9].
Introducing the steroid directly into the hippocampus and rhinencephalon via the nose, as happens in hay fever subjects, could be more effective. In the present study, we analyzed FDA MedWatch data for intranasal fluticasone propionate (Flonase) to determine the frequency of Alzheimer’s disease as an adverse event reported after use of the medication.
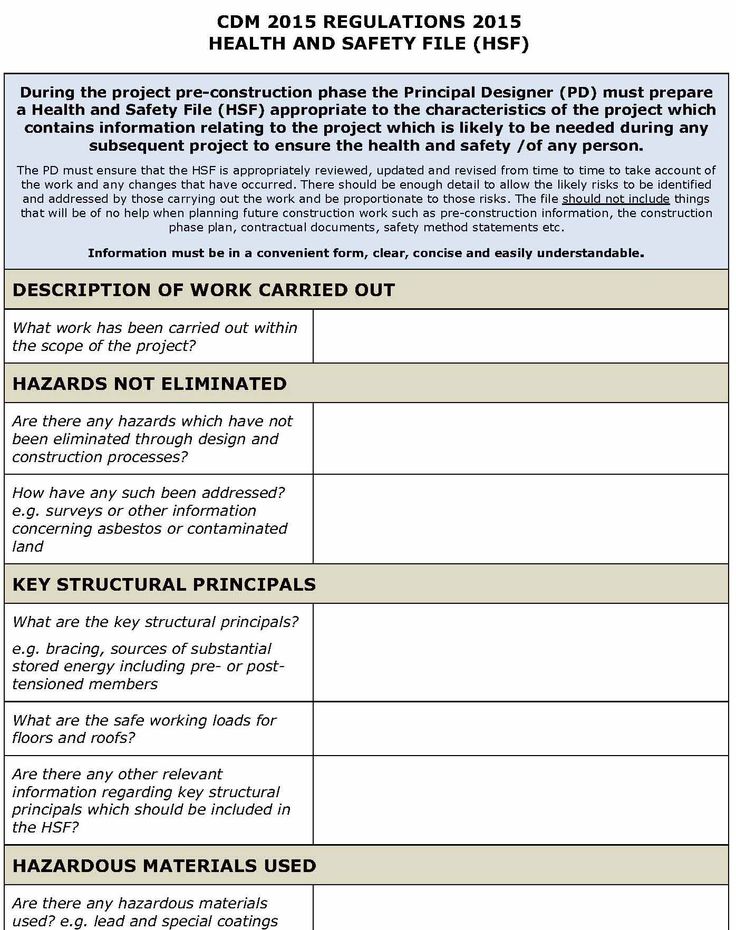
METHODS
We used data from MedWatch, the Food and Drug Administration (FDA) Safety Information and Adverse Event Reporting Program [10]. MedWatch was organized in 1993 to collect data regarding adverse events in healthcare. An adverse event is any undesirable experience associated with the use of a medical product. The MedWatch system collects reports of adverse reactions and quality problems, primarily due to drugs and medical devices, but also for other FDA-regulated products (e. g., dietary supplements, cosmetics, medical foods, and infant formulas).
g., dietary supplements, cosmetics, medical foods, and infant formulas).
MedWatch offers a choice between a voluntary reporting form, designed primarily for health care professionals and the general public, and a mandatory adverse event reporting service (AERS) form, available to manufacturers, importers, and medical product user facilities that manage and store medical products. The latter group is required by law to submit the mandatory form immediately upon discovery of a product malfunction. Printable mail-in forms are available as an alternative to the online submission system [11].
A MedWatch report of an adverse event does not establish causation. For any given report, there is no certainty that the drug in question caused the reaction. The adverse event may have been related to the underlying disease being treated, perhaps caused by another drug being taken concurrently, or something else.
Machine-readable data from MedWatch, including adverse drug reaction reports from manufacturers, are part of a public database. We used the online tool eHealthMe to query the database [12, 13]. Data are exclusively from MedWatch, not from social media [14].
We used the online tool eHealthMe to query the database [12, 13]. Data are exclusively from MedWatch, not from social media [14].
RESULTS
By September 20, 2017, 35,221 people reported side effects to FDA after taking Flonase (intranasal fluticasone propionate). Among them, 9 people (0.03%) had Dementia Alzheimer’s type (Fig. 1).
By October 3, 2017, 185,636 people reported side effects after taking Lipitor (atorvastatin). Among them, 243 people (0.13%) had Dementia Alzheimer’s type (Fig. 1). In a large-scale randomized controlled trial evaluating statin therapy as a treatment for mild to moderate Alzheimer disease, atorvastatin was not associated with significant clinical benefit over 72 weeks [15].
Fig.1
MedWatch Alzheimer’s disease reports in patients using Flonase, Lipitor (atorvastatin), and ibuprofen by year. Number of reports is above the corresponding bar.
By October 8, 2017, 102,006 people reported side effects when taking Ibuprofen. Among them, 34 people (0.03%) had Dementia Alzheimer’s type, a proportion identical to Flonase (Fig. 1). Ibuprofen reduces the risk of Alzheimer’s disease, although, as was mentioned, it is not a treatment [16].
Among them, 34 people (0.03%) had Dementia Alzheimer’s type, a proportion identical to Flonase (Fig. 1). Ibuprofen reduces the risk of Alzheimer’s disease, although, as was mentioned, it is not a treatment [16].
The lower incidence of Alzheimer’s dementia in the Flonase group compared to the Lipitor group was significant (p < 0.001, Fisher exact test, two tailed).
80% of the people taking Flonase were over 60; 93% of the people taking Lipitor were over 60; 89% of the people taking ibuprofen were over 60 (Table 1). 89% of the patients using Flonase were female, versus 56% of the patients taking Lipitor and 82% of the patients taking ibuprofen. The most common other conditions in patients who reported Alzheimer’s disease are listed in Table 2. Drugs most often used by patients who reported Alzheimer’s disease are listed in Table 3. Additional side effects in patients who reported Alzheimer’s disease are listed in Table 4.
Table 1
Age distribution of patients using Flonase, Lipitor, or ibuprofen
| Age | Flonase | Lipitor | Ibuprofen |
| 10–19 | 0 | 0.63% | 3.70% |
| 20–29 | 0 | 0.00% | 0.00% |
| 30–39 | 0 | 0.63% | 3.70% |
| 40–49 | 0 | 0. 00% 00% | 0.00% |
| 50–59 | 20% | 5.70% | 3.70% |
| 60+ | 80% | 93.04% | 88.89% |
Table 2
Most common other conditions in patients who reported Alzheimer’s disease
| Flonase | Lipitor | Ibuprofen |
| Trigeminal Neuralgia (1 person, 11.11%) | Sleep Disorder (13 people, 5. 35%) 35%) | Rheumatoid Arthritis (7 people, 20.59%) |
| Sinus Disorder (1 person, 11.11%) | Depression (9 people, 3.70%) | Preventive Health Care (6 people, 17.65%) |
| Metastases To Spine (1 person, 11.11%) | Diabetes (8 people, 3.29%) | Osteoporosis (4 people, 11.76%) |
| High Blood Pressure (1 person, 11.11%) | Osteoporosis (7 people, 2.88%) | Multiple Myeloma (4 people, 11.76%) |
| Depression (1 person, 11.11%) | Ill-Defined Disorder (7 people, 2.88%) | Chronic Obstructive Pulmonary Disease (4 people, 11.76%) |
Table 3
Other drugs most commonly used by patients who reported Alzheimer’s disease
| Flonase | Lipitor | Ibuprofen |
| Aspirin (4 people, 44.44%) | Aricept (47 people, 19.34%) | Aspirin (14 people, 41.18%) |
| Zometa (3 people, 33.33%) | Aspirin (21 people, 8.64%) | Lorazepam (10 people, 29.41%) |
| Lasix (3 people, 33.33%) | Namenda (20 people, 8.23%) | Humira (9 people, 26.47%) |
Calcium (3 people, 33. 33%) 33%) | Plavix (14 people, 5.76%) | Norvasc (8 people, 23.53%) |
| Albuterol (3 people, 33.33%) | Nexium (13 people, 5.35%) | Cymbalta (7 people, 20.59%) |
Table 4
Other common side effects in patients who reported Alzheimer’s disease
| Flonase | Lipitor | Ibuprofen |
| Pneumonia (5 people, 55.56%) | Memory Loss (55 people, 22.63%) | Fall (9 people, 26. 47%) 47%) |
| Pain (5 people, 55.56%) | Stroke (24 people, 9.88%) | Breathing Difficulty (8 people, 23.53%) |
| Headache (5 people, 55.56%) | Depression (21 people, 8.64%) | Memory Loss (7 people, 20.59%) |
| Gastroesophageal Reflux Disease (5 people, 55.56%) | Diarrhea (20 people, 8.23%) | Drug Ineffective (7 people, 20.59%) |
| Fall (5 people, 55.56%) | Pneumonia (18 people, 7.41%) | Injury (6 people, 17.65%) |
DISCUSSION
One case control study demonstrated that hay fever and other allergies were associated with diminished risk of Alzheimer’s disease (odds ratio 0.6) [17]. Hay fever patients’ use of nasal glucocorticoids might be lessening their risk of Alzheimer’s disease and functioning as a treatment in early cases. Another analysis found no effect of hay fever [18], but subjects’ use of anti-allergy anticholinergics, such as diphenhydramine, may have confused the results by raising risk of Alzheimer’s disease [19].
Another analysis found no effect of hay fever [18], but subjects’ use of anti-allergy anticholinergics, such as diphenhydramine, may have confused the results by raising risk of Alzheimer’s disease [19].
Both pregnenolone and progesterone arrive in the brain after nasal administration [20]. Intranasal regular insulin improves cognition in Alzheimer’s disease, probably because of its brain effects [21]; and the kinetics of intranasal ACTH suggest that it gets into the brain [22]. Therefore, intranasal fluticasone probably gets into the brain via the nose, as well.
The rodent hippocampus is particularly sensitive to glucocorticoids. While glucocorticoids are essential for an effective stress response, their oversecretion was originally hypothesized to contribute to age-related hippocampal degeneration. However, conflicting findings were reported on whether prolonged exposure to elevated glucocorticoids endangered the hippocampus; and whether the primate hippocampus, where Alzheimer’s disease originates, even responds to glucocorticoids as the rodent hippocampus does [23].
Our use of adverse event drug reports has distinct problems. One problem is that the analysis does not include all those taking Flonase, ibuprofen or Lipitor who did not have any adverse reaction (including Alzheimer’s disease) to any drug they were taking. This problem might be addressed by prescription records (or company sales records) indicating how many took the drug. A big data approach could involve a large national database sample from Taiwan or South Korea, tracking medication usage and later medical diagnoses.
Another problem in our analysis is that those who reported adverse effects were likely also taking other medications, which may be associated with Alzheimer’s disease, either increasing or decreasing the risk (some because they treat a disease that is a risk factor for Alzheimer’s disease). This problem might be addressed more systematically by a big data analysis of MedWatch to seek drugs negatively associated with Alzheimer’s disease. However, it is implausible that the patterns of other medications in our analysis were the same for those taking Flonase, ibuprofen, and Lipitor.
In a previous study, Lerner et al. found that delirium is an initial symptom in about 3% of patients diagnosed with Alzheimer’s disease [24]. Medications are one of the biggest causes of delirium, especially benzodiazepines [25], which were common in patients taking atorvastatin as a concurrent medication. Dementia has been listed as a side effect of atorvastatin (and other statins), but might represent the confluence of two common disorders: hypercholesterolemia and dementia (which is not the same as Alzheimer’s disease).
It is possible that individuals already suffering some degree of dementia would be less bothered by seasonal rhinitis or have less access to over the counter drugs such as fluticasone nasal spray. These phenomena could account for part of the observed lower incidence of Dementia Alzheimer’s type reports in patients using Flonase®.
Nevertheless, long term use of oral non-steroidal anti-inflammatory drugs is linked with reduced risk of developing Alzheimer’s disease [26]. These drugs also potentially inhibit brain wound healing [2]. We posit that NSAIDS and steroids both inhibit wound healing in the brain (a well-known fact in the periphery). We further suggest that the lower incidence of AD due to NSAIDS and steroids may be through inhibiting brain wound healing. That is, there is an initial event, and the brain response is what causes the dementia which we call “Alzheimer’s disease.” NSAIDS and steroids may be preventive through a wound healing inhibition mechanism. Our hypothesis is consistent with the idea that amyloid and tau and their cascade of pathology are both a brain response linked to the genesis of the problem [4].
These drugs also potentially inhibit brain wound healing [2]. We posit that NSAIDS and steroids both inhibit wound healing in the brain (a well-known fact in the periphery). We further suggest that the lower incidence of AD due to NSAIDS and steroids may be through inhibiting brain wound healing. That is, there is an initial event, and the brain response is what causes the dementia which we call “Alzheimer’s disease.” NSAIDS and steroids may be preventive through a wound healing inhibition mechanism. Our hypothesis is consistent with the idea that amyloid and tau and their cascade of pathology are both a brain response linked to the genesis of the problem [4].
In summary, data from MedWatch presented here suggest that fluticasone propionate administered intranasally might have a similar preventive effect to ibuprofen. Glucocorticoids, moreover, inhibit wound healing. Perhaps combining ibuprofen and Flonase could be therapeutic. Further studies would be desirable.
CONFLICT OF INTEREST
The authors have no conflict of interest to report.
REFERENCES
[1] | McManus RM , Heneka MT (2017) Role of neuroinflammation in neurodegeneration: New insights. Alzheimers Res Ther 9, 14. |
[2] | Lehrer S , Rheinstein PH (2016) A derangement of the brain wound healing process may cause some cases of Alzheimer’s disease. Discov Med 22, 43–46. |
[3] | Lehrer S , Rheinstein PH , Rosenzweig KE (2017) Association of radon background and total background ionizing radiation with Alzheimer’s disease deaths in U.S. states. J Alzheimers Dis 59, 737–741. |
[4] | Castellani RJ , Perry G (2014) The complexities of the pathology-pathogenesis relationship in Alzheimer disease. Biochem Pharmacol 88, 671–676. |
[5] | D’Andrea MR , Cole GM , Ard MD (2004) The microglial phagocytic role with specific plaque types in the Alzheimer disease brain. Neurobiol Aging 25, 675–683. |
[6] | Miguel-Alvarez M , Santos-Lozano A , Sanchis-Gomar F , Fiuza-Luces C , Pareja-Galeano H , Garatachea N , Lucia A (2015) Non-steroidal anti-inflammatory drugs as a treatment for Alzheimer’s disease: A systematic review and meta-analysis of treatment effect. Drugs Aging 32, 139–147. |
[7] | Chou RC , Kane M , Ghimire S , Gautam S , Gui J (2016) Treatment for rheumatoid arthritis and risk of Alzheimer’s disease: A nested case-control analysis. CNS Drugs 30, 1111–1120. |
[8] | Balis FM , Lester CM , Chrousos GP , Heideman RL , Poplack DG (1987) Differences in cerebrospinal fluid penetration of corticosteroids: Possible relationship to the prevention of meningeal leukemia. J Clin Oncol 5, 202–207. |
[9] | Aisen PS , Davis KL , Berg JD , Schafer K , Campbell K , Thomas RG , Weiner MF , Farlow MR , Sano M , Grundman M , Thal LJ (2000) A randomized controlled trial of prednisone in Alzheimer’s disease. |
[10] | Kessler DA (1993) Introducing MEDWatch. A new approach to reporting medication and device adverse effects and product problems. JAMA 269, 2765–2768. |
[11] | Craigle V (2007) MedWatch: The FDA safety information and adverse event reporting program. J Med Libr Assoc 95, 224. |
[12] | US Department of Health and Human Services eHealthMe study from FDA and social media reports [electronic source]. http://www.ehealthme.com/print/ds15829624 |
[13] | Salihoglu M , Turhan V , Onem Y , Ulcay A , Uzun G , Ay H (2013) Sudden hearing loss in a patient receiving piperacillin/tazobactam and daptomycin for diabetic foot infection. Scand J Infect Dis 45, 239–240. |
[14] | Coloma PM , Becker B , Sturkenboom MC , van Mulligen EM , Kors JA (2015) Evaluating social media networks in medicines safety surveillance: Two case studies. |
[15] | Feldman HH , Doody RS , Kivipelto M , Sparks DL , Waters DD , Jones RW , Schwam E , Schindler R , Hey-Hadavi J , DeMicco DA , Breazna A (2010) Randomized controlled trial of atorvastatin in mild to moderate Alzheimer disease: LEADe. Neurology 74, 956–964. |
[16] | Vlad SC , Miller DR , Kowall NW , Felson DT (2008) Protective effects of NSAIDs on the development of Alzheimer disease. Neurology 70, 1672–1677. |
[17] | Shalat SL , Seltzer B , Pidcock C , Baker EL Jr (1987) Risk factors for Alzheimer’s disease: A case-control study. Neurology 37, 1630–1633. |
[18] | Breteler MM , van Duijn CM , Chandra V , Fratiglioni L , Graves AB , Heyman A , Jorm AF , Kokmen E , Kondo K , Mortimer JA , et al. (1991) Medical history and the risk of Alzheimer’s disease: A collaborative re-analysis of case-control studies. |
[19] | Risacher SL , McDonald BC , Tallman EF , West JD , Farlow MR , Unverzagt FW , Gao S , Boustani M , Crane PK , Petersen RC , Jack CR Jr , Jagust WJ , Aisen PS , Weiner MW , Saykin AJ , Alzheimer’s Disease Neuroimaging Initiative (2016) Association between anticholinergic medication use and cognition, brain metabolism, and brain atrophy in cognitively normal older adults. JAMA Neurol 73, 721–732. |
[20] | Ducharme N , Banks WA , Morley JE , Robinson SM , Niehoff ML , Mattern C , Farr SA (2010) Brain distribution and behavioral effects of progesterone and pregnenolone after intranasal or intravenous administration. Eur J Pharmacol 641, 128–134. |
[21] | Craft S , Claxton A , Baker LD , Hanson AJ , Cholerton B , Trittschuh EH , Dahl D , Caulder E , Neth B , Montine TJ , Jung Y , Maldjian J , Whitlow C , Friedman S (2017) Effects of regular and long-acting insulin on cognition and Alzheimer’s disease biomarkers: A pilot clinical trial. |
[22] | Lehrer S , Rheinstein P (2015) Two compartment model of MSH/ACTH may be a surrogate for intranasal insulin central nervous system kinetic. https://www.j-alz.com/content/two-compartment-model-mshacth-may-be-surrogate-intranasal-insulin-central-nervous-system |
[23] | Conrad CD (2008) Chronic stress-induced hippocampal vulnerability: The glucocorticoid vulnerability hypothesis. Rev Neurosci 19, 395–411. |
[24] | Lerner AJ , Hedera P , Koss E , Stuckey J , Friedland RP (1997) Delirium in Alzheimer disease. Alzheimer Dis Assoc Disord 11, 16–20. |
[25] | Clegg A , Young JB (2011) Which medications to avoid in people at risk of delirium: A systematic review. Age Ageing 40, 23–29. |
[26] | Wyss-Coray T , Rogers J (2012) Inflammation in Alzheimer disease-a brief review of the basic science and clinical literature. |
Fluticasone and ibuprofen do not add to the effect of salmeterol on organic dust-induced airway inflammation and bronchial hyper-responsiveness
Randomized Controlled Trial
. 2008 Jul;264(1):83-94.
doi: 10.1111/j.1365-2796.2008.01928.x. Epub 2008 Feb 21.
K Strandberg 1 , A Ek, L Palmberg, K Larsson
Affiliations
Affiliation
- 1 Lung and Allergy Research, The National Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden. [email protected]
- PMID: 18298484
- DOI: 10.
 1111/j.1365-2796.2008.01928.x
1111/j.1365-2796.2008.01928.x
Free article
Randomized Controlled Trial
K Strandberg et al. J Intern Med. 2008 Jul.
Free article
. 2008 Jul;264(1):83-94.
doi: 10.1111/j.1365-2796.2008.01928.x. Epub 2008 Feb 21.
Authors
K Strandberg 1 , A Ek, L Palmberg, K Larsson
Affiliation
- 1 Lung and Allergy Research, The National Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden. karin.strandberg@ki.
 se
se
- PMID: 18298484
- DOI: 10.1111/j.1365-2796.2008.01928.x
Abstract
Background: Exposure in a pig house causes airway inflammation and bronchial hyper-responsiveness which are not influenced by anti-asthma drugs, including a beta(2)-agonist (salmeterol).
Objectives: We hypothesized that a glucocorticoid or a cyclo-oxygenase-inhibitor synergistically interacts with salmeterol offering a protection against dust-induced increased bronchial responsiveness and airway inflammation. As data did not confirm previous results a retrospective analysis of pooled data on dust-induced bronchial hyper-responsiveness from four other studies was performed.
Design: Fluticasone or ibuprofen was administered for 1 week and salmeterol or placebo was inhaled 1 h prior to a 3-h exposure in a pig barn in a double-blind, placebo-controlled, cross-over design (2-3 weeks apart) in 12 healthy subjects. Lung function, bronchial responsiveness to methacholine and inflammatory markers were evaluated before and after exposure. Pre- and postexposure bronchial responsiveness in nontreated subjects was retrospectively evaluated from four previous studies.
Subjects: Twelve healthy, nonatopic nonsmokers.
Results: Salmeterol partially protected against bronchial hyper-responsiveness but did not influence inflammatory markers. Fluticasone and ibuprofen did not add to these effects. The retrospective analysis showed that PD(20)FEV(1) after exposure in a pig barn is almost totally independent of pre-exposure PD(20)FEV(1)-level; all subjects end up at the same low postexposure PD(20)FEV(1).
Conclusion: Contradictory to our previous results, salmeterol offered partial protection against enhanced bronchial responsiveness induced by exposure in a pig barn. This effect was not modified by fluticasone or ibuprofen. Our data clearly demonstrate that interventions altering bronchial responsiveness must be compared between groups with similar prechallenge bronchial responsiveness or in a cross-over design.
Similar articles
-
Salmeterol does not alter increased bronchial responsiveness caused by organic dust exposure.
Ek A, Palmberg L, Sundblad BM, Larsson K. Ek A, et al. Chest. 2005 Oct;128(4):3038-47. doi: 10.1378/chest.128.4.3038. Chest. 2005. PMID: 16236984
-
The effect of reducing the fine-particle mass of salmeterol from metered-dose inhalers on bronchodilatation and bronchoprotection against methacholine challenge: a randomized, placebo-controlled, double-blind, crossover study.

Langley SJ, Allen D, McDonnell B, Wheeler N, Sharma RK, Sykes A, Woodcock A. Langley SJ, et al. Clin Ther. 2005 Jul;27(7):1004-12. doi: 10.1016/j.clinthera.2005.07.006. Clin Ther. 2005. PMID: 16154479 Clinical Trial.
-
Effect of regular salmeterol treatment on albuterol-induced bronchoprotection in mild asthma.
Yates DH, Worsdell M, Barnes PJ. Yates DH, et al. Am J Respir Crit Care Med. 1997 Sep;156(3 Pt 1):988-91. doi: 10.1164/ajrccm.156.3.9610051. Am J Respir Crit Care Med. 1997. PMID: 9310023 Clinical Trial.
-
[Bronchodilator effect of salmeterol and inhibition of bronchial hyperreactivity].
Boulet LP. Boulet LP. Rev Mal Respir. 1992;9 Suppl 1:R11-3. Rev Mal Respir.
 1992. PMID: 1350363 Review. French.
1992. PMID: 1350363 Review. French. -
[Budesonide/formoterol maintenance and reliever therapy. A new treatment approach for adult patients with asthma].
Korn S, Vogelmeier C, Buhl R. Korn S, et al. Med Klin (Munich). 2008 May 15;103(5):299-310. doi: 10.1007/s00063-008-1050-y. Med Klin (Munich). 2008. PMID: 18484216 Review. German.
See all similar articles
Cited by
-
Cholinergic mechanisms in an organic dust model simulating an acute exacerbation in patients with COPD.
Palmberg L, Sundblad BM, Ji J, Karén J, Larsson K. Palmberg L, et al. Int J Chron Obstruct Pulmon Dis. 2018 Nov 1;13:3611-3624. doi: 10.2147/COPD.S171495. eCollection 2018. Int J Chron Obstruct Pulmon Dis.
 2018. PMID: 30464444 Free PMC article.
2018. PMID: 30464444 Free PMC article. -
Acute effects of acrolein in human volunteers during controlled exposure.
Dwivedi AM, Johanson G, Lorentzen JC, Palmberg L, Sjögren B, Ernstgård L. Dwivedi AM, et al. Inhal Toxicol. 2015;27(14):810-21. doi: 10.3109/08958378.2015.1115567. Epub 2015 Dec 4. Inhal Toxicol. 2015. PMID: 26635308 Free PMC article. Clinical Trial.
-
MyD88 in lung resident cells governs airway inflammatory and pulmonary function responses to organic dust treatment.
Poole JA, Wyatt TA, Romberger DJ, Staab E, Simet S, Reynolds SJ, Sisson JH, Kielian T. Poole JA, et al. Respir Res. 2015 Sep 16;16(1):111. doi: 10.1186/s12931-015-0272-9. Respir Res. 2015. PMID: 26376975 Free PMC article.

-
Compartment differences of inflammatory activity in chronic obstructive pulmonary disease.
Ji J, von Schéele I, Bergström J, Billing B, Dahlén B, Lantz AS, Larsson K, Palmberg L. Ji J, et al. Respir Res. 2014 Aug 26;15(1):104. doi: 10.1186/s12931-014-0104-3. Respir Res. 2014. PMID: 25155252 Free PMC article.
-
cAMP-dependent protein kinase activation decreases cytokine release in bronchial epithelial cells.
Wyatt TA, Poole JA, Nordgren TM, DeVasure JM, Heires AJ, Bailey KL, Romberger DJ. Wyatt TA, et al. Am J Physiol Lung Cell Mol Physiol. 2014 Oct 15;307(8):L643-51. doi: 10.1152/ajplung.00373.2013. Epub 2014 Aug 22. Am J Physiol Lung Cell Mol Physiol. 2014. PMID: 25150062 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Treatment and prevention of acute sinusitis
In most cases, acute sinusitis does not require treatment, as it is caused by a viral infection (runny nose). As a rule, self-medication is sufficient for a speedy recovery and smoothing out the symptoms.
As a rule, self-medication is sufficient for a speedy recovery and smoothing out the symptoms.
Treatment to relieve symptoms
Your doctor may recommend medication to relieve the symptoms of sinusitis. For example, drugs such as:
- Nasal saline spray to be injected into the nose several times a day to clear the nasal passages. nine0018
- Nasal corticosteroids. Corticosteroid nasal sprays can prevent or reduce inflammation. Examples of drugs: fluticasone (Flonase), mometasone (Nasonex), budesonide (Rinocort Aqua), triamcinolone (Nasacort AQ), beclomethasone (Beconase AQ).
- Decongestants. These preparations are available over the counter without a prescription and include drops, tablets and nasal sprays. These drugs are used for several days, otherwise they can increase nasal congestion. nine0018
- Over-the-counter pain relievers include aspirin, acetaminophen (Tylenol and others) and ibuprofen (Advil, Motrin and others).
 Children should not be given aspirin.
Children should not be given aspirin.
Antibiotics
- Antibiotics are not usually needed to treat acute sinusitis.
- Antibiotics cannot treat acute sinusitis caused by a viral or fungal infection.
- Most cases of acute bacterial sinusitis can be treated without antibiotics. nine0018
- Antibiotics are generally used to treat severe, recurrent, or prolonged cases of bacterial infection.
- Antibiotics for acute sinusitis caused by a bacterial infection: amoxicillin, clarithromycin, etc. If the prescribed drug does not help against the infection, or the sinusitis recurs, the doctor may prescribe a different antibiotic.
- If your doctor has prescribed antibiotics for you, you need to complete the full course of treatment. This means that you need to take them for 10 to 14 days, even if the condition has already improved. If antibiotics are stopped early, symptoms may return. nine0018
Antifungals
In rare cases, acute sinusitis is caused by a fungal infection. Then intravenous drugs such as amphotericin B or voriconazole must be used. The dose of the drug, as well as how long you need to take it, depends on the severity of the infection and how quickly the symptoms of the disease are weakened.
Then intravenous drugs such as amphotericin B or voriconazole must be used. The dose of the drug, as well as how long you need to take it, depends on the severity of the infection and how quickly the symptoms of the disease are weakened.
Immunotherapy
If your sinusitis is accompanied by allergies, your doctor may prescribe allergen-specific immunotherapy, which will reduce your body's response to allergens and help improve the condition. nine0003
Home treatment tips
The following tips will help you relieve your sinusitis symptoms:
- Stay in bed or at home. This will help your body fight infection and get better sooner.
- Drink plenty of fluids, such as water or juice. This will make the mucus thinner, which will help it drain. Avoid drinks containing caffeine or alcohol as they dehydrate the body. In addition, alcohol can worsen swollen sinuses and nose.
 nine0018
nine0018 - Steam your nose. Breathe the steam over a bowl of hot water, covering your head with a towel, keeping your face directly above the steam. Or take a hot shower (if you don't have a fever), breathing warm, moist air. This will help relieve pain and help the mucus pass.
- Apply warm compresses to the face. To relieve facial pain, cover your nose, cheeks, and eyes with a towel soaked in warm water.
- Flush nasal passages. Use a specially designed spray bottle (eg Sinus Rinse) to rinse your nasal passages. nine0018
- Sleep with your head elevated. This will help improve passage from the sinuses and reduce nasal congestion.
Prevention of acute sinusitis
To reduce the risk of acute sinusitis:
- Avoid upper respiratory infections. Minimize contact with people who have a cold. Wash your hands frequently with soap, especially before eating. nine0018
- Track your allergies.
 Monitor allergy symptoms by visiting your doctor.
Monitor allergy symptoms by visiting your doctor. - Avoid smoky areas and places with polluted air. Tobacco smoke and other pollutants can cause irritation and inflammation in the nasal passages and lungs.
- Use humidifiers. If the air in your home is dry, such as an air heater, using humidifiers can help prevent sinusitis. Keep the appliance clean and free of mold. nine0018
You can get more detailed information about the treatment and prevention of acute sinusitis from the otolaryngologists of the Health 365 clinic in Yekaterinburg.
otorhinolaryngology (ENT)
otolaryngologist
ENT for children
ENT patients over 70
Reception with endoscopy
Diagnostics
Operations in the hospital
Diagnosis and treatment , sphenoiditis) in Yekaterinburg in children and adults:
- st. Forge, 83
- st. Bazhova, 68
- st. Bazhova, 137
- st. Soyuznaya, 2
- st.
 Stepan Razin, 122
Stepan Razin, 122 - st. Krestinsky, 2
Clinic "Health 365" - a network of multidisciplinary clinics of an expert class
Making an appointment with a doctor:
+7 (343) 270-17-17
Commercial and administrative issues:
+7 (343) 270 -20
Email:
[email protected]
Flonase vs. Nasacort: Differences, Similarities, and Which is Best for You - Drug Vs. Friend
Home >> Drug Vs. Friend >> Flonase vs Nasacort: Differences, Similarities & Which is Best for You
Drug Vs. Friend
Drug Overview and Key Differences | Conditions of treatment | Efficiency | Insurance coverage and cost comparison | Side effects | Drug Interactions | Warnings | FAQ
Runny nose, itching, watery eyes - seasonal allergy season. If you suffer from seasonal or persistent allergies, you don't sneeze alone. More than 50 million Americans suffer from allergies every year.
Flonase (fluticasone propionate or fluticasone) and Nazacort (triamcinolone acetonide or triamcinolone) are two popular medications used to relieve allergies. They belong to a class of drugs called glucocorticoids, better known as steroids. Nasal steroids reduce swelling and nasal congestion, improving symptoms. Although both drugs are known as steroids, they do have some notable differences, which we will discuss below. nine0003
What are the main differences between Flonase and Nasacort?
Flonase (fluticasone) and nasacort (triamcinolone) are nasal corticosteroids used to treat: allergy. A few years ago, both drugs were only available with a prescription, but are now available over the counter (OTC). Both drugs are available in adult and pediatric forms.
Flonase is still available as a prescription drug, as is its generic, fluticasone. Flonaz is also available as Sensimist, an adult and children's formulation that creates a more gentle mist. Both drugs can be used in children and adults, but Nazacort can be used in children 2 years of age and older, and Flonase can be used in children 4 years of age and older. nine0205
Flonaz is also available as Sensimist, an adult and children's formulation that creates a more gentle mist. Both drugs can be used in children and adults, but Nazacort can be used in children 2 years of age and older, and Flonase can be used in children 4 years of age and older. nine0205
Baby Nasal Spray
Gentle Spray
Baby Gentle Spray
Baby Nasal Spray
 Once symptoms subside, reduce spray to 1 spray per nostril per day.
Once symptoms subside, reduce spray to 1 spray per nostril per day. Children aged 2 to 6 years: 1 spray in each nostril daily.
Children 6 to 12 years of age: 1 spray per nostril per day (may temporarily increase to 2 sprays per nostril per day and decrease again after symptoms subside)
*Consult your doctor if your child needs to use more than 2 months per year
*consult your doctor if your child needs to use more than 2 months a year
Conditions treated with Flonase and Nasacort
Flonase and Nasacort are used to treat nasal allergy symptoms . Both drugs can be used for seasonal or year-round allergy symptoms. Flonaz and nazacort can also be used. off label for some conditions such as nasal polyps and chronic or viral rhinosinusitis (or bacterial rhinosinusitis in addition to antibiotics). nine0003
Both drugs can be used for seasonal or year-round allergy symptoms. Flonaz and nazacort can also be used. off label for some conditions such as nasal polyps and chronic or viral rhinosinusitis (or bacterial rhinosinusitis in addition to antibiotics). nine0003
| Condition | Flonase | Nasakort | ||
| Treatment of nasal seasonal or year -old non -allergic rhinitis | Yes (dated 4 years) Yes, yes (from 4 years) yes (from 4 years) Yes (from 4 years) older) | |||
| Relief of hay fever/other upper respiratory allergies | yes | yes | ||
| Treatment of nasal polyps | Not for the purpose of | not for the purpose of | ||
| Acute bacterial rhinosinusitis in combination with antibiotics | not for the purpose of | not for the appointment of | ||
| non -purpose | non | Relief of symptoms of viral rhinosinusitis | Off label | Off label |
Is Flonaz or Nazacort more effective? nine0187
A recent study After 28 days of treatment, flonase and nasacort were found to be equally effective in treating nasal allergy symptoms and both were well tolerated. Another study showed that flonase and nazacort were equally safe, effective, and well tolerated.
Another study showed that flonase and nazacort were equally safe, effective, and well tolerated.
The most effective medicine for you should be determined by you and your doctor, who may take into account your condition(s), medical history, and other medicines you are taking. nine0003
Coverage and Cost Comparison of Flonase and Nasacort
Flonase is usually covered by insurance and Medicare Part D in the generic form of fluticasone, but the over-the-counter version is usually not covered. Medicare Part D copay for generic fluticasone is $0 to $20. Flonase can cost over $50, but can be purchased for as little as $12-$29 with a SingleCare Pharmacy Coupon.
Nasacort is only available without a prescription and is generally not covered by insurance (some state Medicaid plans may pay for generic drug) or Medicare Part D. Nasacort usually retails for over $20, but you can get it at a participating pharmacy for as little as for $13.50. with a SingleCare coupon. nine0003
nine0003
| Flonase | Nasacort | |
| Usually covered? | OTC: No Rx: Yes | No |
| Usually covered by Medicare? | OTC: No Rx: Yes | No |
| Standard Dosage | 1 Unit | 1 Unit |
| Typical Medicare Supplement | 0–20 dollars | No data |
| Cost Singlecare | 12–29 dollars | 13.50 US dollars and higher than |
General side effects Flonase against NASACORT
9000 9000 9000 are well -transferred. The most common symptoms of Flonase are headache, nausea/vomiting, asthma symptoms, and cough. The most common side effects of Nazacort are headache, asthma symptoms, and cough. Other side effects listed for both drugs occurred at about the same frequency as placebo (inactive drugs), such as nosebleeds and sore throats. nine0003
nine0003 This is not a complete list of side effects; Other side effects may occur. Check with your healthcare provider for a complete list of side effects.
| Flonase | Nasacort | |||
| Frequency | Applicable? | Frequency | ||
| Headache | yes | 6.6-16.1% | Yes | 5.5% |
| Nausea / vomiting | yes2.6–4.8% | - | ||
| ASTMA symptoms | yes | yes 3,13-7 , 2% | yes | 2.5% |
| Cough | yes | 3.6–3.8% | > 2% |
Source: Dailymed (Flona) FDA Label (Nasacort)
Flonase-Nasacort Drug Interaction
Flonase is processed by the enzyme cytochrome P 450 3A4, also known as CYP3A4. Some medications inhibit this enzyme and slow down its processing of flonase, leading to accumulation of flonase and increased side effects of steroids. Therefore, these strong inhibitors should not be taken with flonase. Nasacort does not have any drug interaction information. Other interactions are possible; consult your doctor for medical advice. nine0187
Therefore, these strong inhibitors should not be taken with flonase. Nasacort does not have any drug interaction information. Other interactions are possible; consult your doctor for medical advice. nine0187
- Possible local effects such as nosebleeds, nasal ulceration, local infection with Candida (yeast), perforation of the nasal septum and impaired wound healing.
- Steroids may cause glaucoma or cataracts. You should be closely monitored if you have any visual changes or if you have a history of increased intraocular pressure, glaucoma and/or cataracts. If you are using Flonase or Nasacort for a long time, or if you have any eye symptoms, you should consult your ophthalmologist regularly. nine0018
- If you experience a hypersensitivity reaction (skin symptoms, difficulty breathing, swelling of the face), stop taking Flonase or Nasacort and seek emergency medical attention.
- Because steroids suppress the immune system, you are more likely to get infections when using a steroid nasal spray.

- Children may experience reduced growth rate; growth should be closely monitored. The lowest possible dose should be used for the shortest possible time. nine0018
- Rarely, adrenal suppression may occur and the nasal steroid should be tapered off gradually until stopped (not stopped abruptly).
- Because there is not enough data on nasal steroids in pregnancy, you should consult your doctor before taking Flonase or Nasacort if you are pregnant. If you are already taking Flonase or Nasacort and find you are pregnant, seek the advice of your doctor.
Flonase and Nasacort FAQ
What is flonaz?
Flonase is a nasal steroid that helps relieve allergy symptoms. The active substance is fluticasone propionate. It is available over-the-counter as a brand and generic, and by prescription as a generic. It can be used in adults and children aged 4 years and older.
What is Nasacort?
Nazacort is a nasal steroid used to relieve allergy symptoms. The active ingredient in Nazacort is triamcinolone. It is available over-the-counter in both brand and generic forms. Nazacort can be used in both adults and children over the age of 2 years. nine0003
The active ingredient in Nazacort is triamcinolone. It is available over-the-counter in both brand and generic forms. Nazacort can be used in both adults and children over the age of 2 years. nine0003
Are Flonas and Nazacort the same thing?
Flonase and Nasacort are very similar and have the same uses and warnings. However, they do have some notable differences, such as active ingredient, drug interactions, and price, as noted above. Other Medications The category of nasal steroids you may have heard of includes Rinocort (budesonide), QNasl (beclomethasone), and Nasonex (mometasone). Fluticasone is also available as a combination drug in the form of the brand-name Dimista, which contains azelastine along with fluticasone. nine0003
Which is better: Flonaz or Nazacort?
Studies have shown that both drugs are very well tolerated and effective in relieving symptoms. It may take a bit of trial and error to figure out if Flonase or Nasacort is right for you.
Can I use Flonase or Nasacort during pregnancy?
There is not enough data, so it is best to discuss allergy symptoms with your doctor and find out what he suggests. It may be safe to take flonase or nascort during pregnancy if necessary, but this varies from case to case, so it is safest to ask your doctor. nine0003
It may be safe to take flonase or nascort during pregnancy if necessary, but this varies from case to case, so it is safest to ask your doctor. nine0003
Can I use Flonase or Nasacort with alcohol?
Flonaz or Nazacort are safe to use with alcohol. However, if you are taking other medicines for allergy symptoms, check with your doctor or pharmacist to see if these medicines are compatible with alcohol.
What is the most effective allergy nasal spray?
There are many allergy nasal sprays, and some of them work in different ways. While drugs such as flonase and nazacort are steroids, some allergy nasal sprays contain other ingredients, such as azelastine, which is an antihistamine and works differently than a steroid. Many people like Afrin nasal spray; however, you must be very careful when using this medicine for only 3 days or less, otherwise it may cause rebound congestion. The most effective allergy spray is the one that works best for you, and trial and error may be required to determine which allergy spray works best.

 Alzheimer’s Disease Cooperative Study. Neurology 54, 588–593.
Alzheimer’s Disease Cooperative Study. Neurology 54, 588–593. Drug Saf 38, 921–930.
Drug Saf 38, 921–930. EURODEM Risk Factors Research Group. Int J Epidemiol 20(Suppl 2), S36–S42.
EURODEM Risk Factors Research Group. Int J Epidemiol 20(Suppl 2), S36–S42. J Alzheimers Dis 57, 1325–1334.
J Alzheimers Dis 57, 1325–1334. Cold Spring Harb Perspect Med 2, a006346.
Cold Spring Harb Perspect Med 2, a006346.