Schizophrenia effectiveness treatment
Towards a framework for treatment effectiveness in schizophrenia
1. American Psychiatric Association . Practice guideline for the treatment of patients with schizophrenia. 2nd ed. 2004. [Google Scholar]
2. Falkai P, Wobrock T, Lieberman J, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, Part 1: acute treatment of schizophrenia. World J Biol Psychiatry. 2005;6(3):132–191. [PubMed] [Google Scholar]
3. Falkai P, Wobrock T, Lieberman J, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, part 2: long-term treatment of schizophrenia. World J Biol Psychiatry. 2006;7(1):5–40. [PubMed] [Google Scholar]
4. Correll CU, Leucht S, Kane JM. Lower risk for tardive dyskinesia associated with second-generation antipsychotics: a systematic review of 1-year studies. Am J Psychiatry. 2004;161(3):414–425. [PubMed] [Google Scholar]
5. Heal DJ, Gosden J, Jackson HC, Cheetham SC, Smith SL. Metabolic consequences of antipsychotic therapy: preclinical and clinical perspectives on diabetes, diabetic ketoacidosis, and obesity. Handb Exp Pharmacol. 2012;(212):135–164. [PubMed] [Google Scholar]
6. Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373(9657):31–41. [PubMed] [Google Scholar]
7. Leucht S, Komossa K, Rummel-Kluge C, et al. A meta-analysis of head-to-head comparisons of second-generation antipsychotics in the treatment of schizophrenia. Am J Psychiatry. 2009;166(2):152–163. [PubMed] [Google Scholar]
8. Richelson E, Souder T. Binding of antipsychotic drugs to human brain receptors focus on newer generation compounds. Life Sci. 2000;68(1):29–39. [PubMed] [Google Scholar]
9. Nasrallah HA. Atypical antipsychotic-induced metabolic side effects: insights from receptor-binding profiles.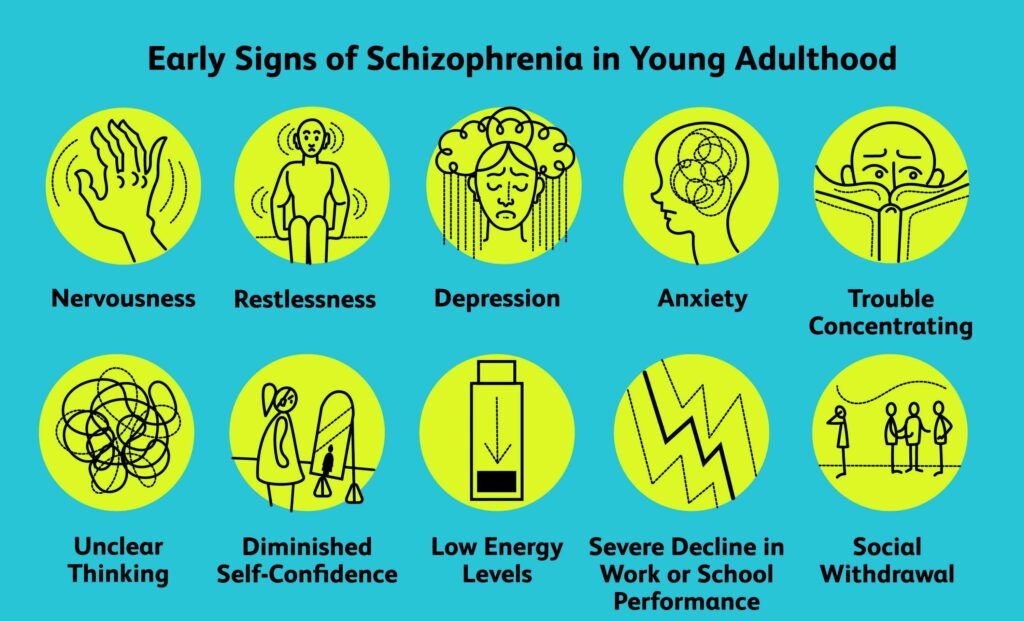 Mol Psychiatry. 2008;13(1):27–35. [PubMed] [Google Scholar]
Mol Psychiatry. 2008;13(1):27–35. [PubMed] [Google Scholar]
10. Johnsen E, Jørgensen HA. Effectiveness of second generation antipsychotics: a systematic review of randomized trials. BMC Psychiatry. 2008;8:31. [PMC free article] [PubMed] [Google Scholar]
11. Kahn RS, Fleischhacker WW, Boter H, et al. Effectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trial. Lancet. 2008;371(9618):1085–1097. [PubMed] [Google Scholar]
12. Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005;353(12):1209–1223. [PubMed] [Google Scholar]
13. Zimbroff DL. Management of acute psychosis: from emergency to stabilization. CNS Spectr. 2003;8(11 Suppl 2):10–15. [PubMed] [Google Scholar]
14. Casey DE. Long-term treatment goals: enhancing healthy outcomes. CNS Spectr. 2003;8(11 Suppl 2):26–28. [PubMed] [Google Scholar]
15. Keshavan MS, Nasrallah HA, Tandon R. Schizophrenia, “Just the Facts” 6. Moving ahead with the schizophrenia concept: from the elephant to the mouse. Schizophr Res. 2011;127(1–3):3–13. [PMC free article] [PubMed] [Google Scholar]
Keshavan MS, Nasrallah HA, Tandon R. Schizophrenia, “Just the Facts” 6. Moving ahead with the schizophrenia concept: from the elephant to the mouse. Schizophr Res. 2011;127(1–3):3–13. [PMC free article] [PubMed] [Google Scholar]
16. Stroup TS, McEvoy JP, Swartz MS, et al. The National Institute of Mental Health Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) project: schizophrenia trial design and protocol development. Schizophr Bull. 2003;29(1):15–31. [PubMed] [Google Scholar]
17. Dossenbach M, Erol A, el Mahfoud KM, et al. Effectiveness of antipsychotic treatments for schizophrenia: interim 6-month analysis from a prospective observational study (IC-SOHO) comparing olanzapine, quetiapine, risperidone, and haloperidol. J Clin Psychiatry. 2004;65(3):312–321. [PubMed] [Google Scholar]
18. Haro JM, Edgell ET, Novick D, et al. Effectiveness of antipsychotic treatment for schizophrenia: 6-month results of the Pan-European Schizophrenia Outpatient Health Outcomes (SOHO) study. Acta Psychiatr Scand. 2005;111(3):220–231. [PubMed] [Google Scholar]
Acta Psychiatr Scand. 2005;111(3):220–231. [PubMed] [Google Scholar]
19. Jones PB, Barnes TR, Davies L, et al. Randomized controlled trial of the effect on Quality of Life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1) Arch Gen Psychiatry. 2006;63(10):1079–1087. [PubMed] [Google Scholar]
20. Lewis SW, Barnes TR, Davies L, et al. Randomized controlled trial of effect of prescription of clozapine versus other second-generation antipsychotic drugs in resistant schizophrenia. Schizophr Bull. 2006;32(4):715–723. [PMC free article] [PubMed] [Google Scholar]
21. Tandon R, Marcus RN, Stock EG, et al. A prospective, multicenter, randomized, parallel-group, open-label study of aripiprazole in the management of patients with schizophrenia or schizoaffective disorder in general psychiatric practice: Broad Effectiveness Trial With Aripiprazole (BETA) Schizophr Res. 2006;84(1):77–89. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
22. McEvoy JP, Lieberman JA, Perkins DO, et al. Efficacy and tolerability of olanzapine, quetiapine, and risperidone in the treatment of early psychosis: a randomized, double-blind 52-week comparison. Am J Psychiatry. 2007;164(7):1050–1060. [PubMed] [Google Scholar]
23. Perkins DO, Gu H, Weiden PJ, McEvoy JP, Hamer RM, Lieberman JA. Predictors of treatment discontinuation and medication nonadherence in patients recovering from a first episode of schizophrenia, schizophreniform disorder, or schizoaffective disorder: a randomized, double-blind, flexible-dose, multicenter study. J Clin Psychiatry. 2008;69(1):106–113. [PubMed] [Google Scholar]
24. Nasrallah HA, Targum SD, Tandon R, McCombs JS, Ross R. Defining and measuring clinical effectiveness in the treatment of schizophrenia. Psychiatr Serv. 2005;56(3):273–282. [PubMed] [Google Scholar]
25. Kinon BJ, Chen L, Ascher-Svanum H, et al. Challenging the assumption that improvement in functional outcomes is delayed relative to improvement in symptoms in the treatment of schizophrenia. Schizophr Res. 2010;118(1–3):176–182. [PubMed] [Google Scholar]
Schizophr Res. 2010;118(1–3):176–182. [PubMed] [Google Scholar]
26. Stauffer VL, Case M, Kinon BJ, et al. Early response to antipsychotic therapy as a clinical marker of subsequent response in the treatment of patients with first-episode psychosis. Psychiatry Res. 2011;187(1–2):42–48. [PubMed] [Google Scholar]
27. Giegling I, Porcelli S, Balzarro B, et al. Antipsychotic response in the first week predicts later efficacy. Neuropsychobiology. 2012;66(2):100–105. [PubMed] [Google Scholar]
28. Ascher-Svanum H, Zhu B, Faries DE, Lacro JP, Dolder CR, Peng X. Adherence and persistence to typical and atypical antipsychotics in the naturalistic treatment of patients with schizophrenia. Patient Prefer Adherence. 2008;2:67–77. [PMC free article] [PubMed] [Google Scholar]
29. Liu-Seifert H, Adams DH, Kinon BJ. Discontinuation of treatment of schizophrenic patients is driven by poor symptom response: a pooled post-hoc analysis of four atypical antipsychotic drugs. BMC Med. 2005;3:21.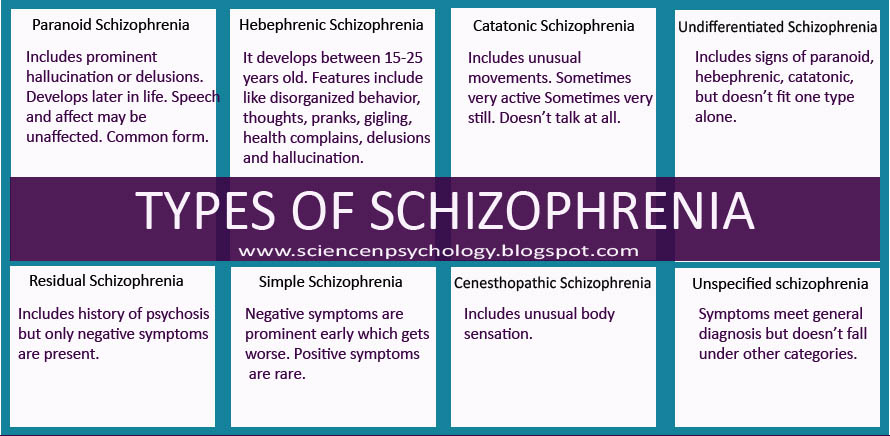 [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
30. Andreasen NC, Carpenter WT, Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441–449. [PubMed] [Google Scholar]
31. Emsley R, Oosthuizen P, Koen L, Niehaus DJ, Medori R, Rabinowitz J. Remission in patients with first-episode schizophrenia receiving assured antipsychotic medication: a study with risperidone long-acting injection. Int Clin Psychopharmacol. 2008;23(6):325–331. [PubMed] [Google Scholar]
32. Lauriello J, Lambert T, Anderson S, Lin D, Taylor CC, McDonnell D. An 8-week, double-blind, randomized, placebo-controlled study of olanzapine long-acting injection in acutely ill patients with schizophrenia. J Clin Psychiatry. 2008;69:790–799. [PubMed] [Google Scholar]
33. Kane JM, Sanchez R, Perry PP, et al. Aripiprazole intramuscular depot as maintenance treatment in patients with schizophrenia: a 52-week, multicenter, randomized, double-blind, placebo-controlled study.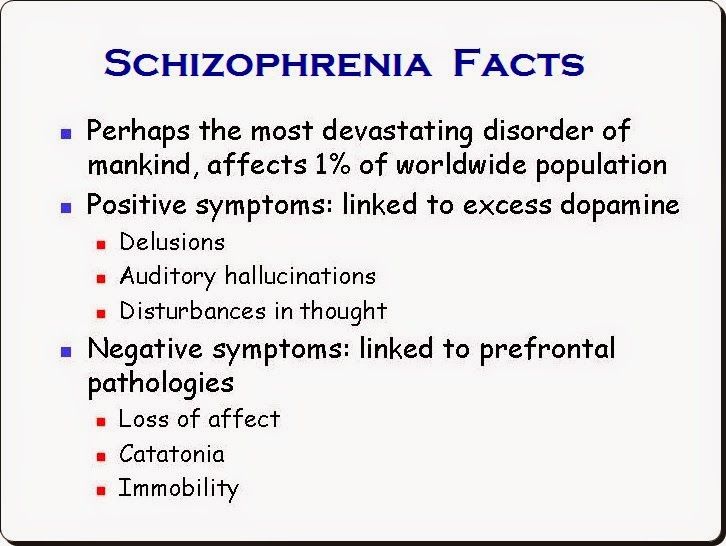 J Clin Psychiatry. 2012;73:617–624. [PubMed] [Google Scholar]
J Clin Psychiatry. 2012;73:617–624. [PubMed] [Google Scholar]
34. Potkin SG, Weiden PJ, Loebel AD, Warrington LE, Watsky EJ, Siu CO. Remission in schizophrenia: 196-week, double-blind treatment with ziprasidone vs haloperidol. Int J Neuropsychopharmacol. 2009;12(9):1233–1248. [PubMed] [Google Scholar]
35. Gorwood P, Peuskens J, European Group On Functional Outcomes, Remission in Schizophrenia Setting new standards in schizophrenia outcomes: Symptomatic remission 3 years before versus after the andreasen criteria. Eur Psychiatry. 2012;27(3):170–175. [PubMed] [Google Scholar]
36. Lambert M, Karow A, Leucht S, Schimmelmann BG, Naber D. Remission in schizophrenia: validity, frequency, predictors, and patients’ perspective 5 years later. Dialogues Clin Neurosci. 2010;12(3):393–407. [PMC free article] [PubMed] [Google Scholar]
37. AlAqeel B, Margolese HC. Remission in schizophrenia: critical and systematic review. Harv Rev Psychiatry. 2012;20:281–297. [PubMed] [Google Scholar]
38. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. [PMC free article] [PubMed] [Google Scholar]
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. [PMC free article] [PubMed] [Google Scholar]
39. Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol. 1967;6(4):278–296. [PubMed] [Google Scholar]
40. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. [PubMed] [Google Scholar]
41. Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: the Calgary Depression Scale. Br J Psychiatry Suppl. 1993;(22):39–44. [PubMed] [Google Scholar]
42. Hofer A, Rettenbacher MA, Edlinger M, et al. Outcomes in schizophrenia outpatients treated with amisulpride or olanzapine. Pharmacopsychiatry. 2007;40(1):1–8. [PubMed] [Google Scholar]
43. Kahn RS, Schulz SC, Palazov VD, et al. Efficacy and tolerability of once-daily extended release quetiapine fumarate in acute schizophrenia: a randomized, double-blind, placebo-controlled study.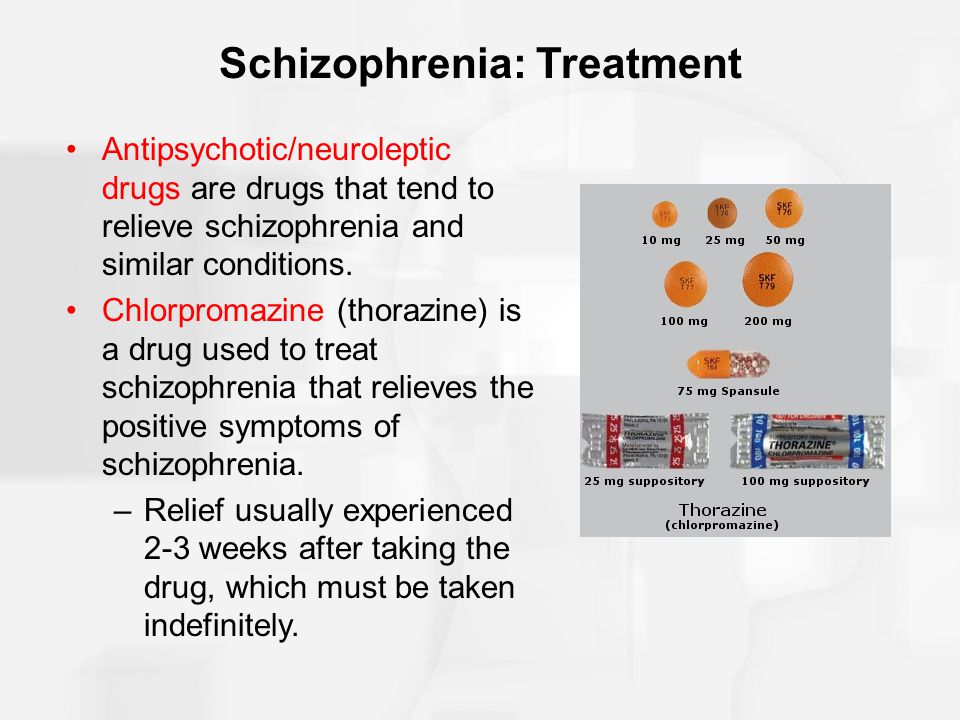 J Clin Psychiatry. 2007;68(6):832–842. [PubMed] [Google Scholar]
J Clin Psychiatry. 2007;68(6):832–842. [PubMed] [Google Scholar]
44. Meltzer HY, Bobo WV, Nuamah IF, et al. Efficacy and tolerability of oral paliperidone extended-release tablets in the treatment of acute schizophrenia: pooled data from three 6-week, placebo-controlled studies. J Clin Psychiatry. 2008;69(5):817–829. [PubMed] [Google Scholar]
45. Keefe RS, Bilder RM, Davis SM, et al. Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Arch Gen Psychiatry. 2007;64(6):633–647. [PubMed] [Google Scholar]
46. Keefe RS, Poe M, Walker TM, Kang JW, Harvey PD. The Schizophrenia Cognition Rating Scale: an interview-based assessment and its relationship to cognition, real-world functioning, and functional capacity. Am J Psychiatry. 2006;163(3):426–432. [PubMed] [Google Scholar]
47. Galderisi S, Davidson M, Kahn RS, et al. Correlates of cognitive impairment in first episode schizophrenia: the EUFEST study. Schizophr Res.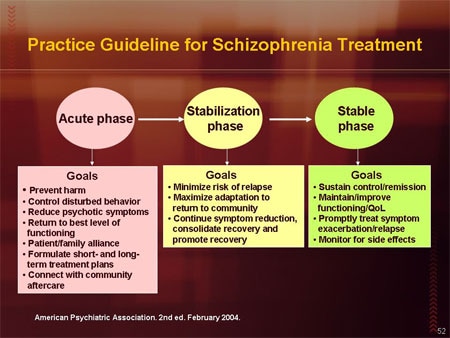 2009;115(2–3):104–114. [PubMed] [Google Scholar]
2009;115(2–3):104–114. [PubMed] [Google Scholar]
48. Mausbach BT, Depp CA, Bowie CR, et al. Sensitivity and specificity of the UCSD Performance-based Skills Assessment (UPSA-B) for identifying functional milestones in schizophrenia. Schizophr Res. 2011;132(2–3):165–170. [PMC free article] [PubMed] [Google Scholar]
49. Nuechterlein KH, Green MF, Kern RS, et al. The MATRICS Consensus Cognitive Battery, part 1: test selection, reliability, and validity. Am J Psychiatry. 2008;165(2):203–213. [PubMed] [Google Scholar]
50. Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The Brief Assessment of Cognition in Schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. 2004;68(2–3):283–297. [PubMed] [Google Scholar]
51. Rummel-Kluge C, Kissling W. Psychoeducation for patients with schizophrenia and their families. Expert Rev Neurother. 2008;8(7):1067–1077. [PubMed] [Google Scholar]
52. Larsen DL, Attkisson CC, Hargreaves WA, Nguyen TD.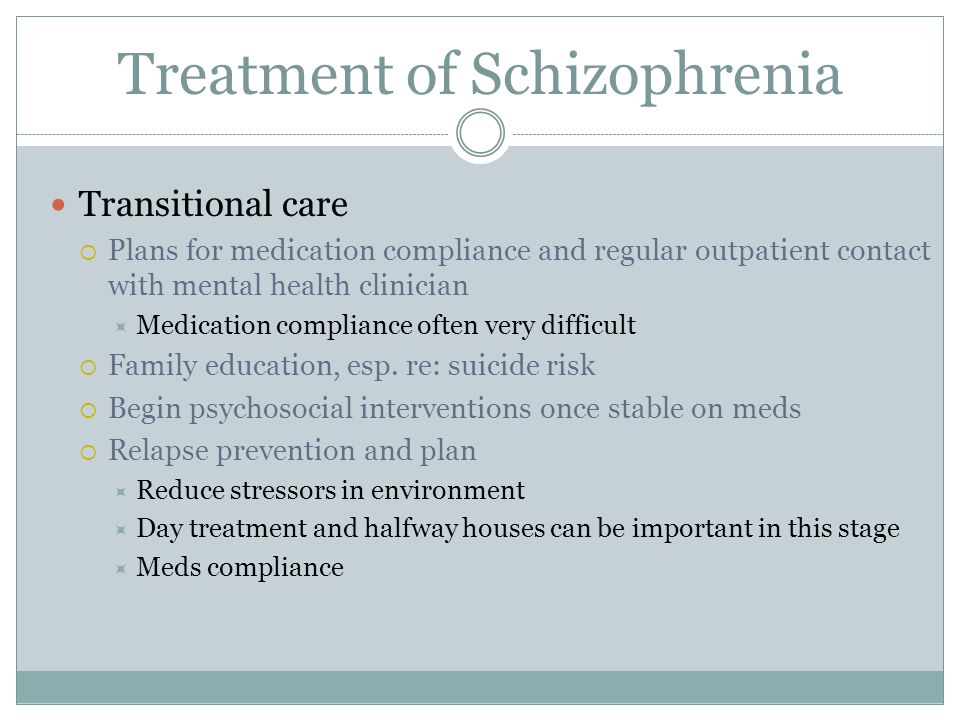 Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. [PubMed] [Google Scholar]
Assessment of client/patient satisfaction: development of a general scale. Eval Program Plann. 1979;2(3):197–207. [PubMed] [Google Scholar]
53. Ruggeri M, Lasalvia A, Dall’Agnola R, et al. Development, internal consistency and reliability of the Verona Service Satisfaction Scale – European Version. EPSILON Study 7. European Psychiatric Services: Inputs Linked to Outcome Domains and Needs. Br J Psychiatry Suppl. 2000;(39):s41–s48. [PubMed] [Google Scholar]
54. Richardson M, Katsakou C, Torres-Gonzalez F, Onchev G, Kallert T, Priebe S. Factorial validity and measurement equivalence of the Client Assessment of Treatment Scale for psychiatric inpatient care – a study in three European countries. Psychiatry Res. 2011;188(1):156–160. [PubMed] [Google Scholar]
55. Endicott J, Nee J, Harrison W, Blumenthal R. Quality of Life Enjoyment and Satisfaction Questionnaire: a new measure. Psychopharmacol Bull. 1993;29(2):321–326. [PubMed] [Google Scholar]
56. Atkinson MJ, Sinha A, Hass SL, et al. Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes. 2004;2:12. [PMC free article] [PubMed] [Google Scholar]
Validation of a general measure of treatment satisfaction, the Treatment Satisfaction Questionnaire for Medication (TSQM), using a national panel study of chronic disease. Health Qual Life Outcomes. 2004;2:12. [PMC free article] [PubMed] [Google Scholar]
57. Gharabawi GM, Greenspan A, Rupnow MF, et al. Reduction in psychotic symptoms as a predictor of patient satisfaction with antipsychotic medication in schizophrenia: data from a randomized double-blind trial. BMC Psychiatry. 2006;6:45. [PMC free article] [PubMed] [Google Scholar]
58. Vernon MK, Revicki DA, Awad AG, et al. Psychometric evaluation of the Medication Satisfaction Questionnaire (MSQ) to assess satisfaction with antipsychotic medication among schizophrenia patients. Schizophr Res. 2010;118(1–3):271–278. [PubMed] [Google Scholar]
59. Juckel G, Morosini PL. The new approach: psychosocial functioning as a necessary outcome criterion for therapeutic success in schizophrenia. Curr Opin Psychiatry. 2008;21(6):630–639.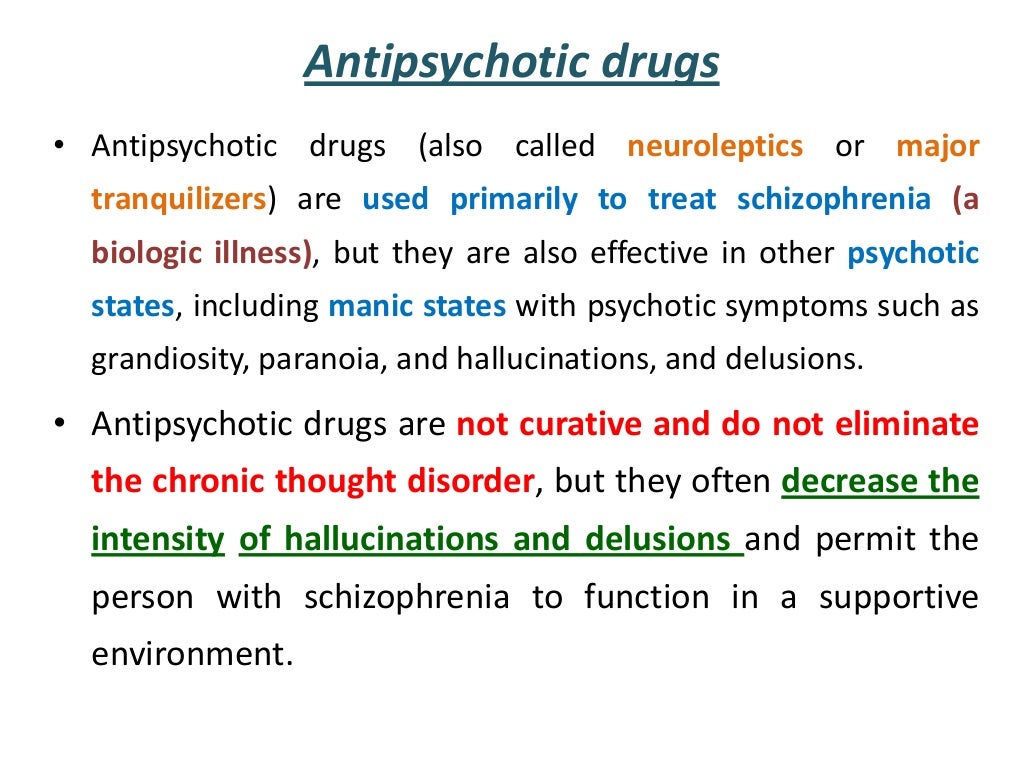 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
60. Galderisi S, Mucci A, Bitter I, et al. Persistent negative symptoms in first episode patients with schizophrenia: results from the European First Episode Schizophrenia Trial. Eur Neuropsychopharmacol. 2013;23:196–204. [PubMed] [Google Scholar]
61. Morgan C, Burns T, Fitzpatrick R, Pinfold V, Priebe S. Social exclusion and mental health: conceptual and methodological review. Br J Psychiatry. 2007;191:477–483. [PubMed] [Google Scholar]
62. Patrick DL, Burns T, Morosini P, Gagnon DD, Rothman M, Adriaenssen I. Measuring social functioning with the personal and social performance scale in patients with acute symptoms of schizophrenia: interpretation of results of a pooled analysis of three Phase III trials of paliperidone extended-release tablets. Clin Ther. 2010;32(2):275–292. [PubMed] [Google Scholar]
63. Mosolov SN, Potapov AV, Ushakov UV. Remission in schizophrenia: results of cross-sectional with 6-month follow-up period and 1-year observational therapeutic studies in an outpatient population.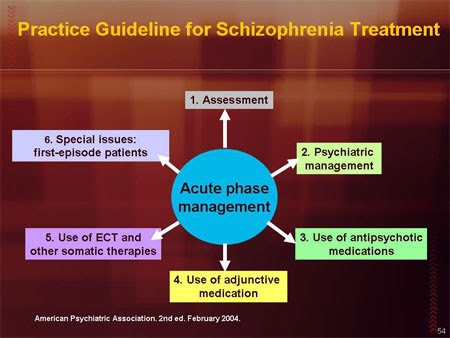 Ann Gen Psychiatry. 2012;11:1. [PMC free article] [PubMed] [Google Scholar]
Ann Gen Psychiatry. 2012;11:1. [PMC free article] [PubMed] [Google Scholar]
64. Mosolov SN, Potapov AV, Ushakov UV, Shararenko AA, Kostyukova AB. Design and validation of standardized clinical and functional remission criteria in schizophrenia. Neuropsychiatr Dis Treat. 2014;10:167–181. [PMC free article] [PubMed] [Google Scholar]
65. Karow A, Naber D, Lambert M, Moritz S, EGOFORS initiative Remission as perceived by people with schizophrenia, family members and psychiatrists. Eur Psychiatry. 2012;27(6):426–431. [PubMed] [Google Scholar]
66. Morosini PL, Magliano L, Brambilla L, Ugolini S, Pioli R. Development, reliability and acceptability of a new version of the DSM-IV Social and Occupational Functioning Assessment Scale (SOFAS) to assess routine social functioning. Acta Psychiatr Scand. 2000;101(4):323–329. [PubMed] [Google Scholar]
67. Nafees B, van Hanswijck de Jonge P, Stull D, et al. Reliability and validity of the Personal and Social Performance scale in patients with schizophrenia.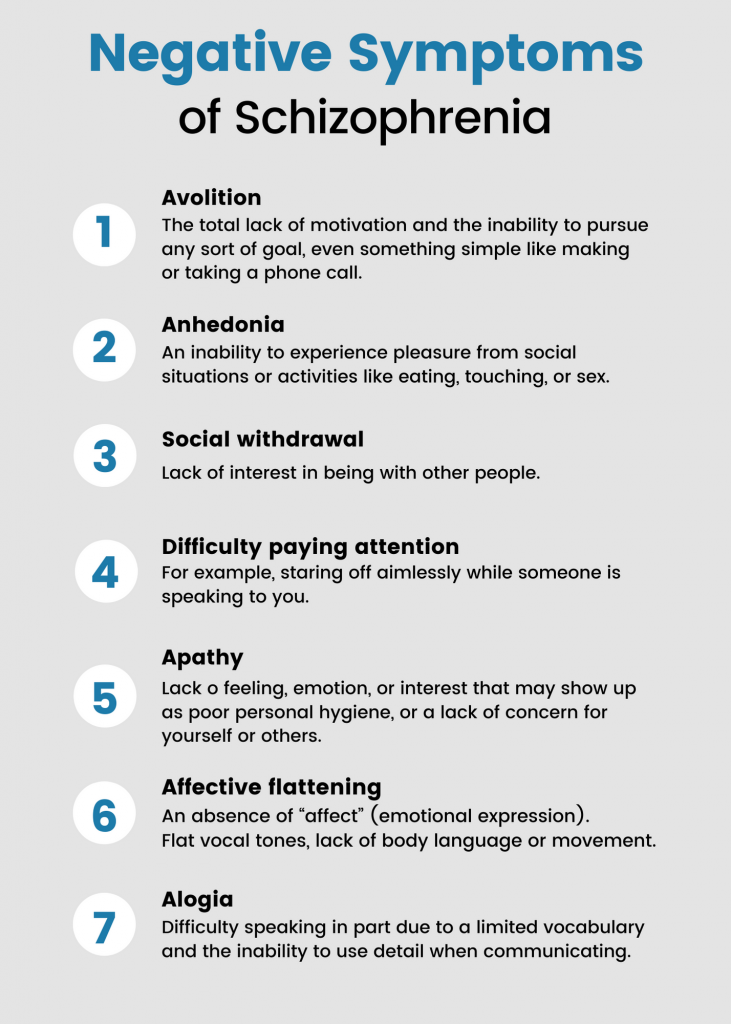 Schizophr Res. 2012;140(1–3):71–76. [PubMed] [Google Scholar]
Schizophr Res. 2012;140(1–3):71–76. [PubMed] [Google Scholar]
68. Brissos S, Palhava F, Marques JG, et al. The Portuguese version of the Personal and Social Performance Scale (PSP): reliability, validity, and relationship with cognitive measures in hospitalized and community schizophrenia patients. Soc Psychiatry Psychiatr Epidemiol. 2012;47(7):1077–1086. [PubMed] [Google Scholar]
69. Tianmei S, Liang S, Yun’ai S, et al. The Chinese version of the Personal and Social Performance Scale (PSP): validity and reliability. Psychiatry Res. 2011;185(1–2):275–279. [PubMed] [Google Scholar]
70. Apiquian R, Elena UR, Herrera-Estrella M, et al. Validity of the Spanish version of the Personal and Social Performance scale in schizophrenia. Schizophr Res. 2009;112(1–3):181–186. [PubMed] [Google Scholar]
71. Nasrallah H, Morosini P, Gagnon DD. Reliability, validity and ability to detect change of the Personal and Social Performance scale in patients with stable schizophrenia. Psychiatry Res.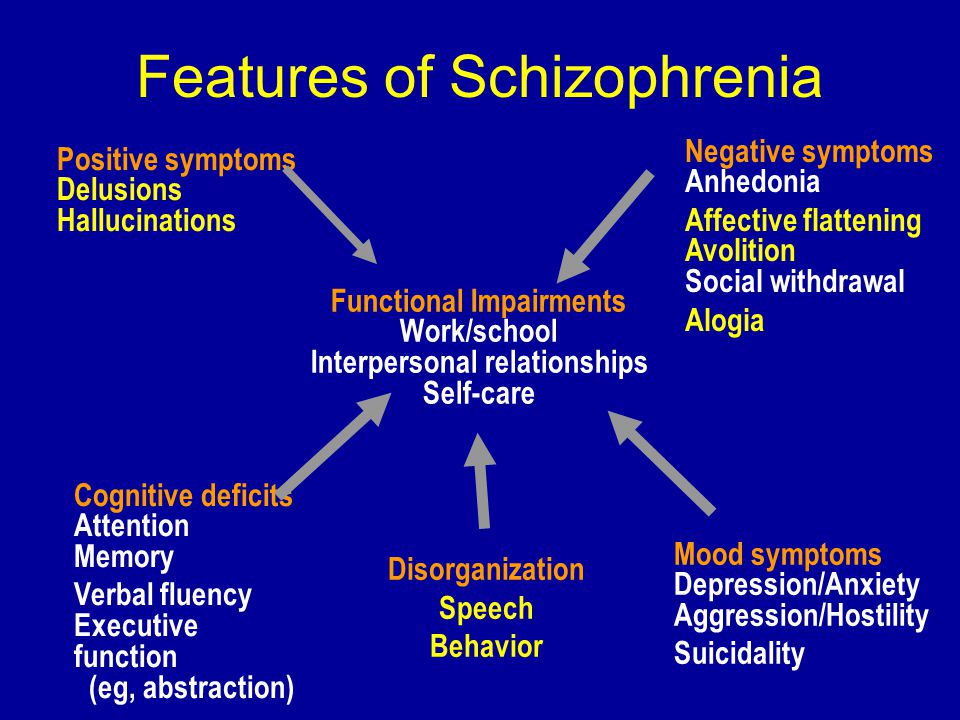 2008;161(2):213–224. [PubMed] [Google Scholar]
2008;161(2):213–224. [PubMed] [Google Scholar]
72. Patrick DL, Burns T, Morosini P, et al. Reliability, validity and ability to detect change of the clinician-rated Personal and Social Performance scale in patients with acute symptoms of schizophrenia. Curr Med Res Opin. 2009;25(2):325–338. [PubMed] [Google Scholar]
73. Figueira ML, Brissos S. Measuring psychosocial outcomes in schizophrenia patients. Curr Opin Psychiatry. 2011;24:91–99. [PubMed] [Google Scholar]
74. Mendes Menzes AK, Macedo G, Mattos P, Reis de Sá Júnior A, Louza MR. Personal and Social Performance (PSP) scale for patients with schizophrenia: translation to Portuguese, cross-cultural adaption and interrater reliability. J Bras Psiquiatr. 2012;61:176–180. [Google Scholar]
75. Juckel G, Schaub D, Fuchs N, et al. Validation of the Personal and Social Performance (PSP) Scale in a German sample of acutely ill patients with schizophrenia. Schizophr Res. 2008;104(1–3):287–293. [PubMed] [Google Scholar]
76. Srisurapont M, Arunpongpaisal S, Chuntaruchikapong S, et al. Cross-cultural validation and inter-rater reliability of the Personal and Social Performance Scale, Thai Version. J Med Assoc Thai. 2008;91:1603–1608. [PubMed] [Google Scholar]
Srisurapont M, Arunpongpaisal S, Chuntaruchikapong S, et al. Cross-cultural validation and inter-rater reliability of the Personal and Social Performance Scale, Thai Version. J Med Assoc Thai. 2008;91:1603–1608. [PubMed] [Google Scholar]
77. Burns T, Patrick D. Social functioning as an outcome measure in schizophrenia studies. Acta Psychiatr Scand. 2007;116(6):403–418. [PubMed] [Google Scholar]
78. Schaub D, Brüne M, Bierhoff HW, Juckel G. Comparison of self- and clinician’s ratings of Personal and Social Performance in patients with schizophrenia: the role of insight. Psychopathology. 2012;45(2):109–116. [PubMed] [Google Scholar]
79. Schaub D, Brüne M, Jaspen E, Pajonk FG, Bierhoff HW, Juckel G. The illness and everyday living: close interplay of psychopathological syndromes and psychosocial functioning in chronic schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2011;261(2):85–93. [PubMed] [Google Scholar]
80. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia.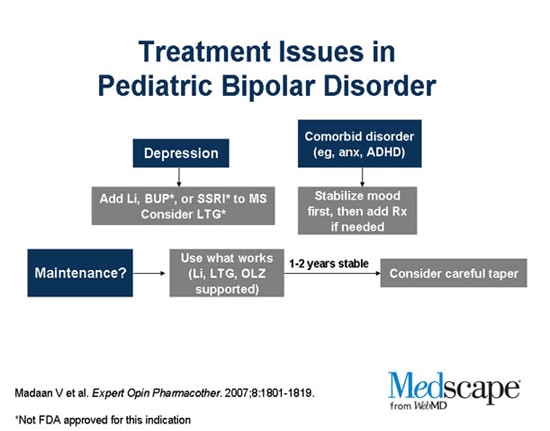 Schizophr Bull. 1987;13(2):261–276. [PubMed] [Google Scholar]
Schizophr Bull. 1987;13(2):261–276. [PubMed] [Google Scholar]
Schizophrenia - Diagnosis and treatment
Diagnosis
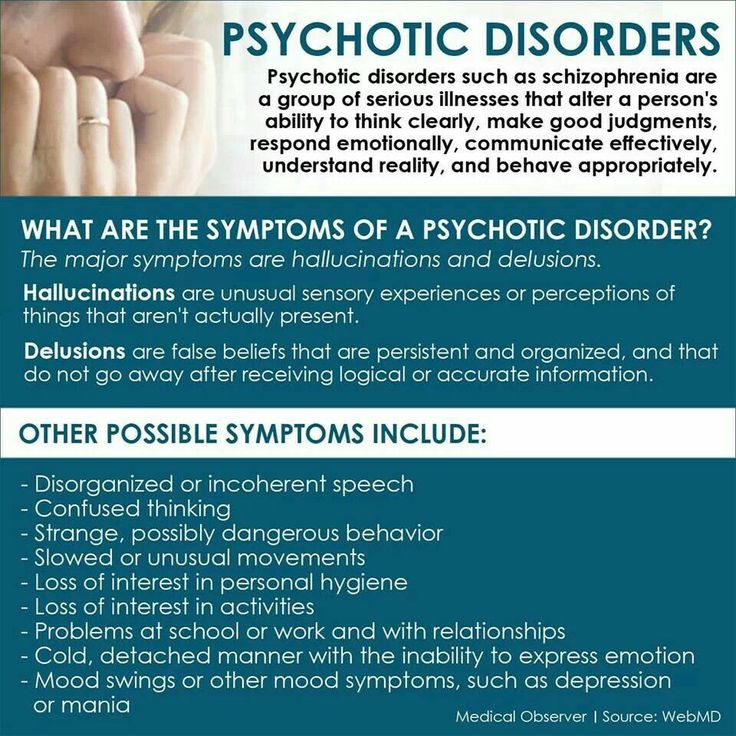
Diagnosis of schizophrenia involves ruling out other mental health disorders and determining that symptoms are not due to substance abuse, medication or a medical condition. Determining a diagnosis of schizophrenia may include:
- Physical exam. This may be done to help rule out other problems that could be causing symptoms and to check for any related complications.
- Tests and screenings. These may include tests that help rule out conditions with similar symptoms, and screening for alcohol and drugs. The doctor may also request imaging studies, such as an MRI or CT scan.
- Psychiatric evaluation. A doctor or mental health professional checks mental status by observing appearance and demeanor and asking about thoughts, moods, delusions, hallucinations, substance use, and potential for violence or suicide.
 This also includes a discussion of family and personal history.
This also includes a discussion of family and personal history. - Diagnostic criteria for schizophrenia. A doctor or mental health professional may use the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
More Information
- CT scan
- MRI
Treatment
Schizophrenia requires lifelong treatment, even when symptoms have subsided. Treatment with medications and psychosocial therapy can help manage the condition. In some cases, hospitalization may be needed.
A psychiatrist experienced in treating schizophrenia usually guides treatment. The treatment team also may include a psychologist, social worker, psychiatric nurse and possibly a case manager to coordinate care. The full-team approach may be available in clinics with expertise in schizophrenia treatment.
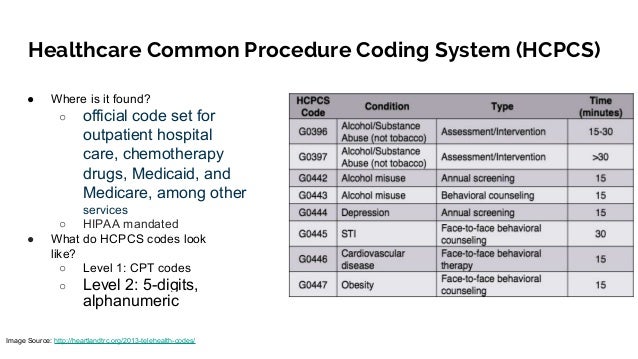
Medications
Medications are the cornerstone of schizophrenia treatment, and antipsychotic medications are the most commonly prescribed drugs. They're thought to control symptoms by affecting the brain neurotransmitter dopamine.
They're thought to control symptoms by affecting the brain neurotransmitter dopamine.
The goal of treatment with antipsychotic medications is to effectively manage signs and symptoms at the lowest possible dose. The psychiatrist may try different drugs, different doses or combinations over time to achieve the desired result. Other medications also may help, such as antidepressants or anti-anxiety drugs. It can take several weeks to notice an improvement in symptoms.
Because medications for schizophrenia can cause serious side effects, people with schizophrenia may be reluctant to take them. Willingness to cooperate with treatment may affect drug choice. For example, someone who is resistant to taking medication consistently may need to be given injections instead of taking a pill.
Ask your doctor about the benefits and side effects of any medication that's prescribed.
Second-generation antipsychotics
These newer, second-generation medications are generally preferred because they pose a lower risk of serious side effects than do first-generation antipsychotics. Second-generation antipsychotics include:
Second-generation antipsychotics include:
- Aripiprazole (Abilify)
- Asenapine (Saphris)
- Brexpiprazole (Rexulti)
- Cariprazine (Vraylar)
- Clozapine (Clozaril, Versacloz)
- Iloperidone (Fanapt)
- Lurasidone (Latuda)
- Olanzapine (Zyprexa)
- Paliperidone (Invega)
- Quetiapine (Seroquel)
- Risperidone (Risperdal)
- Ziprasidone (Geodon)
First-generation antipsychotics
These first-generation antipsychotics have frequent and potentially significant neurological side effects, including the possibility of developing a movement disorder (tardive dyskinesia) that may or may not be reversible. First-generation antipsychotics include:
- Chlorpromazine
- Fluphenazine
- Haloperidol
- Perphenazine
These antipsychotics are often cheaper than second-generation antipsychotics, especially the generic versions, which can be an important consideration when long-term treatment is necessary.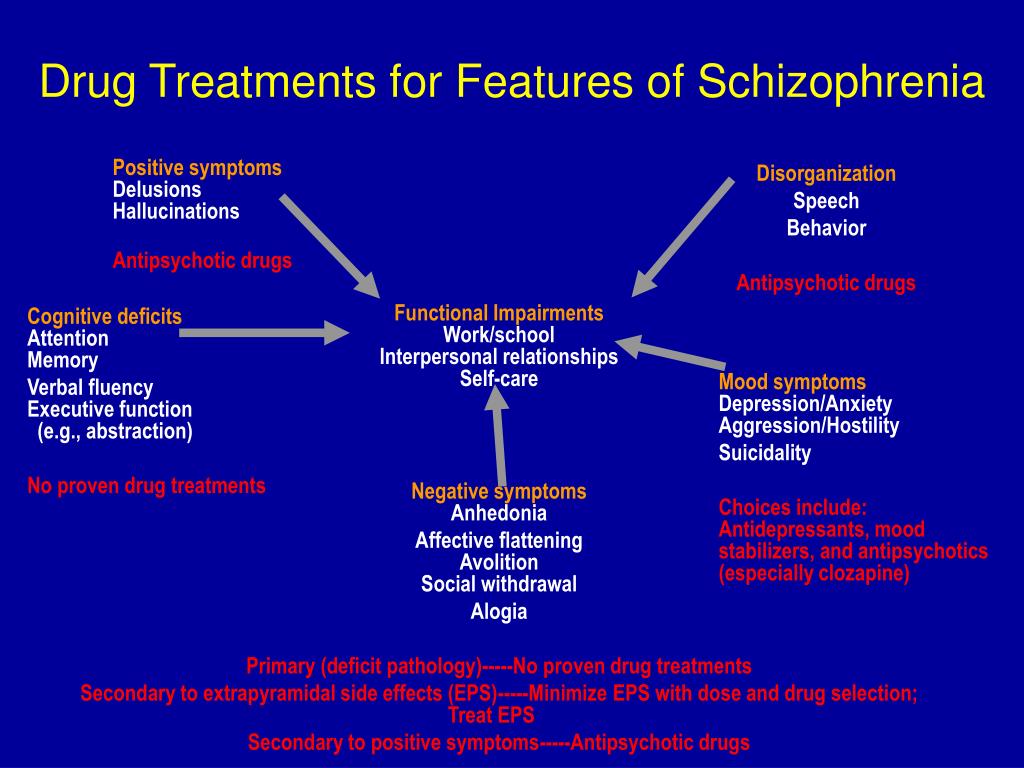
Long-acting injectable antipsychotics
Some antipsychotics may be given as an intramuscular or subcutaneous injection. They are usually given every two to four weeks, depending on the medication. Ask your doctor about more information on injectable medications. This may be an option if someone has a preference for fewer pills and may help with adherence.
Common medications that are available as an injection include:
- Aripiprazole (Abilify Maintena, Aristada)
- Fluphenazine decanoate
- Haloperidol decanoate
- Paliperidone (Invega Sustenna, Invega Trinza)
- Risperidone (Risperdal Consta, Perseris)
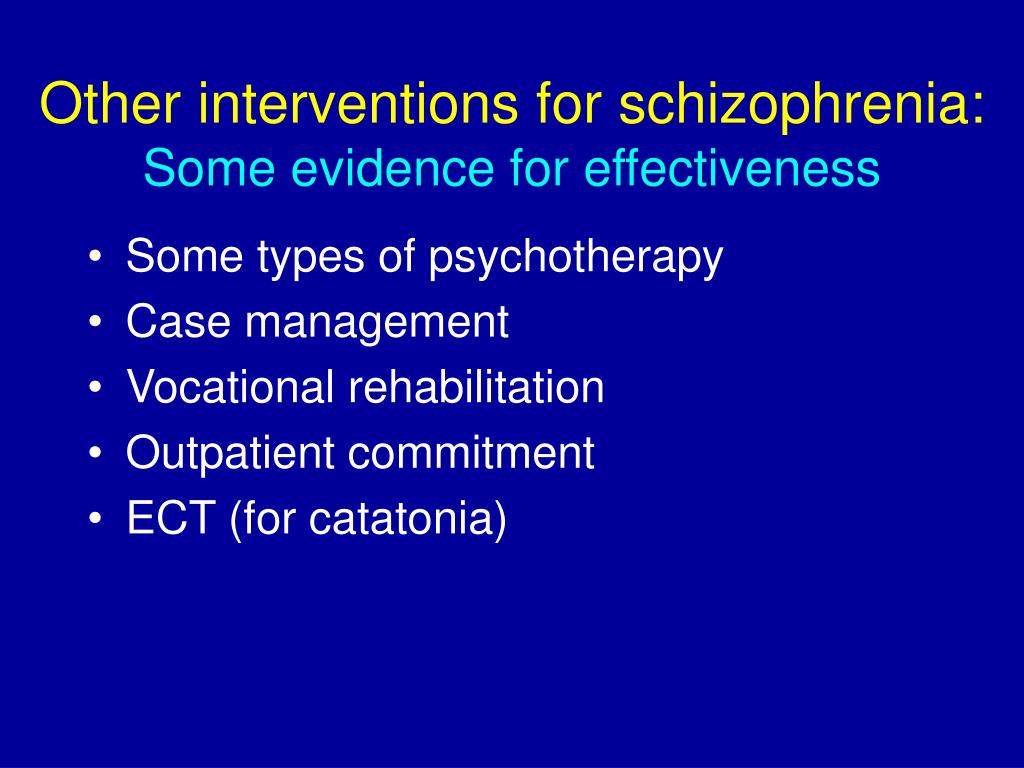
Psychosocial interventions
Once psychosis recedes, in addition to continuing on medication, psychological and social (psychosocial) interventions are important. These may include:
- Individual therapy. Psychotherapy may help to normalize thought patterns. Also, learning to cope with stress and identify early warning signs of relapse can help people with schizophrenia manage their illness.
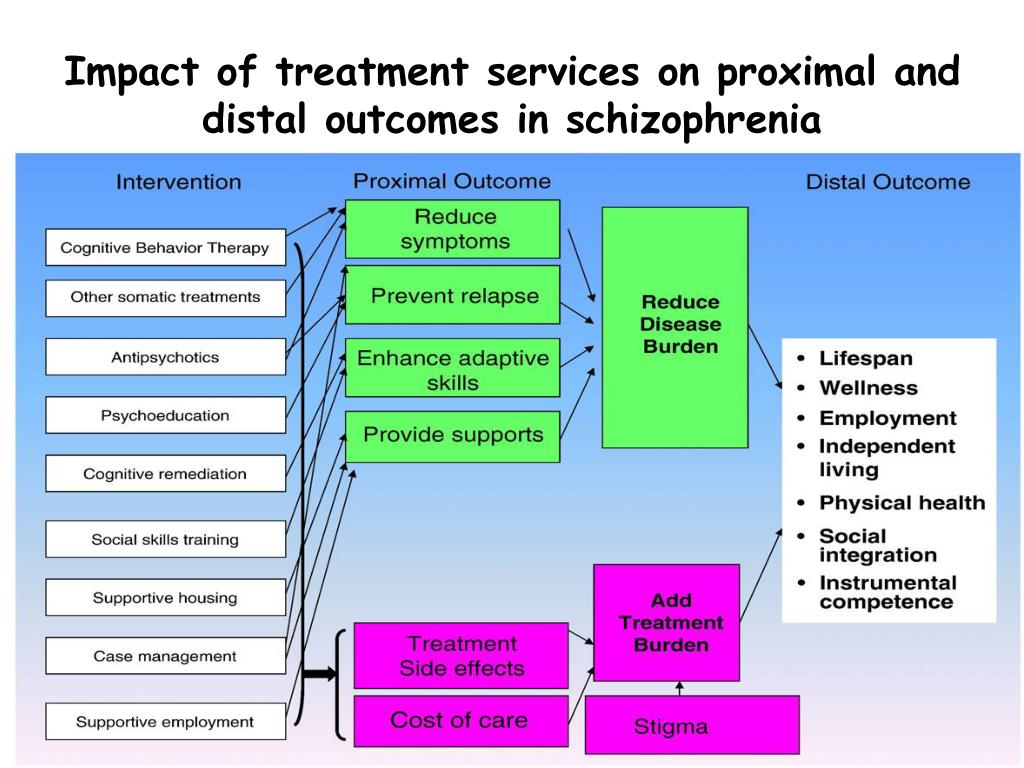
- Social skills training. This focuses on improving communication and social interactions and improving the ability to participate in daily activities.
- Family therapy. This provides support and education to families dealing with schizophrenia.
- Vocational rehabilitation and supported employment. This focuses on helping people with schizophrenia prepare for, find and keep jobs.
Most individuals with schizophrenia require some form of daily living support. Many communities have programs to help people with schizophrenia with jobs, housing, self-help groups and crisis situations. A case manager or someone on the treatment team can help find resources. With appropriate treatment, most people with schizophrenia can manage their illness.
Hospitalization
During crisis periods or times of severe symptoms, hospitalization may be necessary to ensure safety, proper nutrition, adequate sleep and basic hygiene.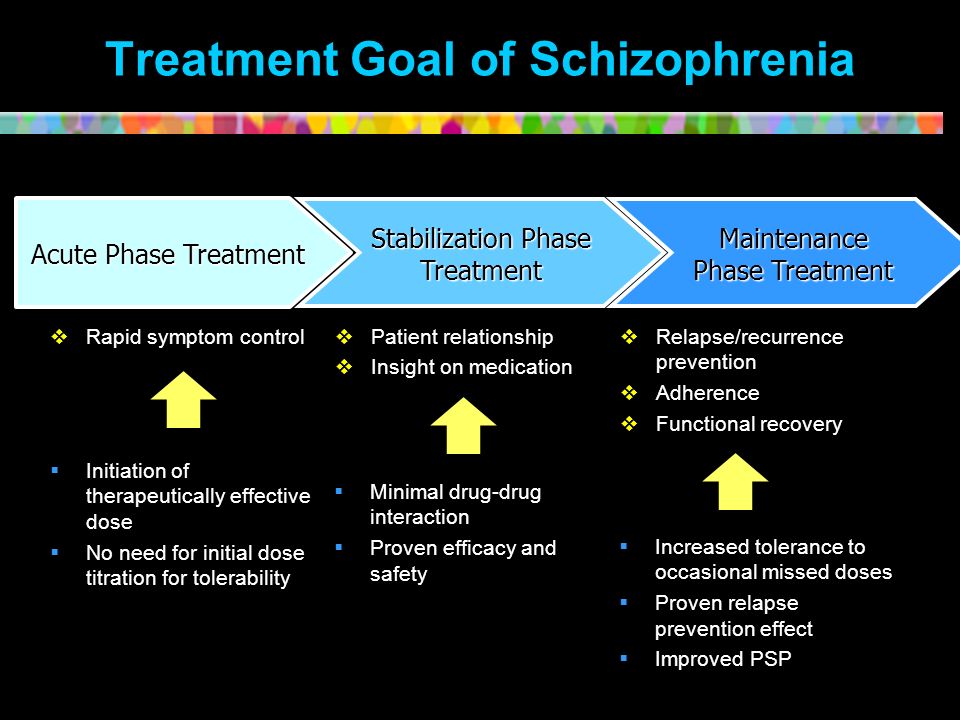
Electroconvulsive therapy
For adults with schizophrenia who do not respond to drug therapy, electroconvulsive therapy (ECT) may be considered. ECT may be helpful for someone who also has depression.
More Information
- Family therapy
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.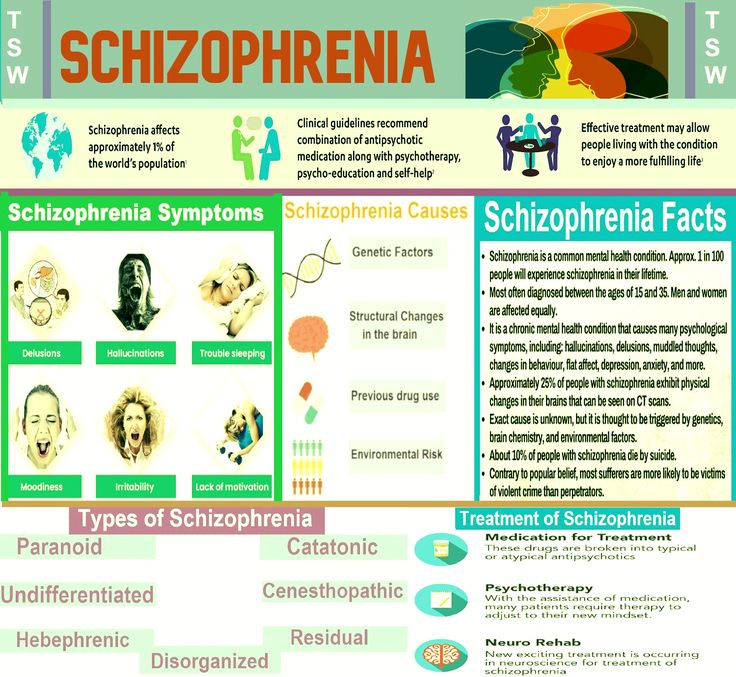 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Coping and support
Coping with a mental disorder as serious as schizophrenia can be challenging, both for the person with the condition and for friends and family. Here are some ways to cope:
- Learn about schizophrenia. Education about the disorder can help the person with schizophrenia understand the importance of sticking to the treatment plan. Education can help friends and family understand the disorder and be more compassionate with the person who has it.
- Stay focused on goals. Managing schizophrenia is an ongoing process. Keeping treatment goals in mind can help the person with schizophrenia stay motivated. Help your loved one remember to take responsibility for managing the disorder and working toward goals.
- Avoid alcohol and drug use. Using alcohol, nicotine or recreational drugs can make it difficult to treat schizophrenia.
 If your loved one is addicted, quitting can be a real challenge. Get advice from the health care team on how best to approach this issue.
If your loved one is addicted, quitting can be a real challenge. Get advice from the health care team on how best to approach this issue. - Ask about social services assistance. These services may be able to assist with affordable housing, transportation and other daily activities.
- Learn relaxation and stress management. The person with schizophrenia and loved ones may benefit from stress-reduction techniques such as meditation, yoga or tai chi.
- Join a support group. Support groups for people with schizophrenia can help them reach out to others facing similar challenges. Support groups may also help family and friends cope.
Preparing for your appointment
If you're seeking help for someone with schizophrenia, you may start by seeing his or her family doctor or health care professional. However, in some cases when you call to set up an appointment, you may be referred immediately to a psychiatrist.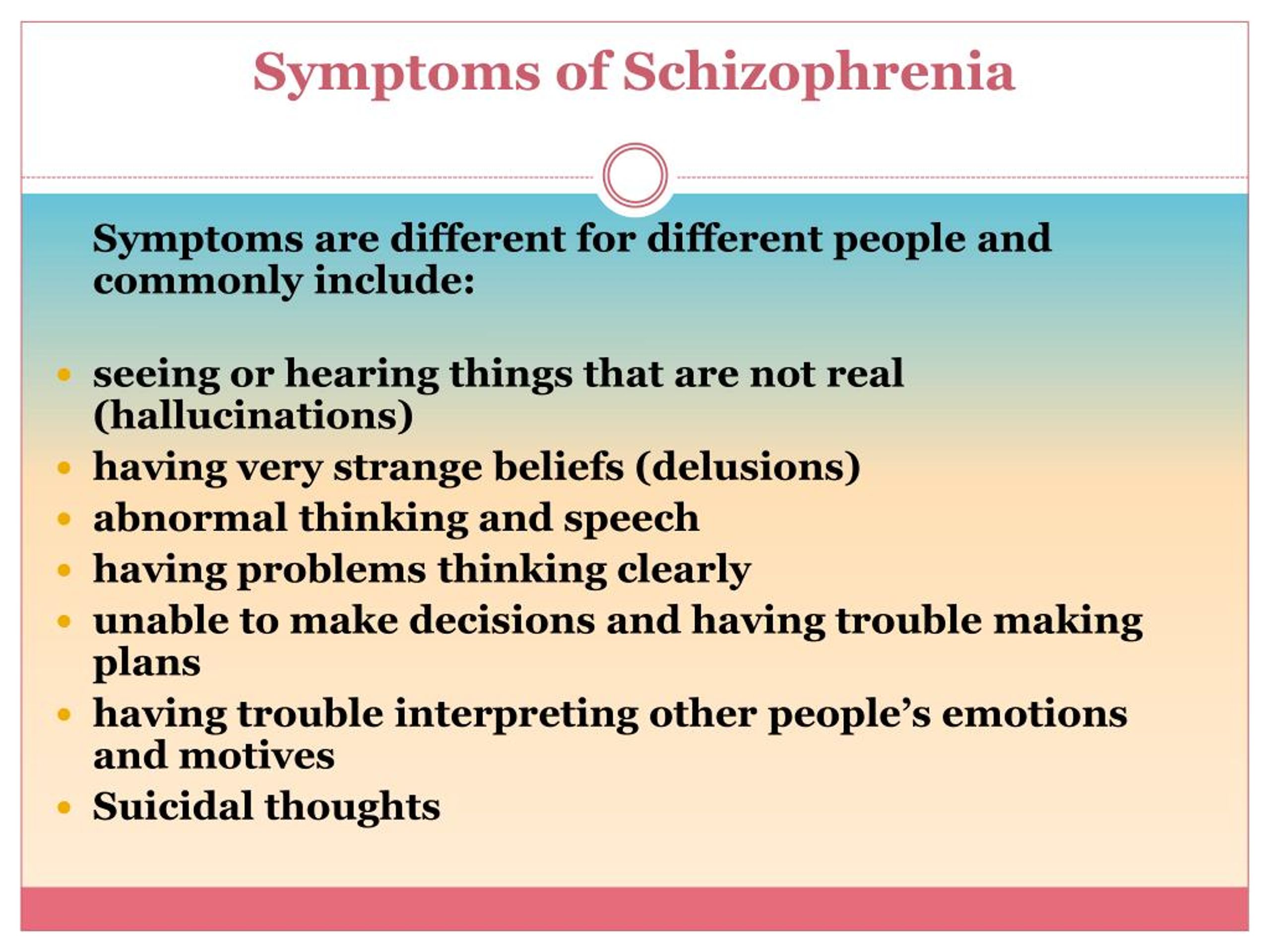
What you can do
To prepare for the appointment, make a list of:
- Any symptoms your loved one is experiencing, including any that may seem unrelated to the reason for the appointment
- Key personal information, including any major stresses or recent life changes
- Medications, vitamins, herbs and other supplements that he or she is taking, including the dosages
- Questions to ask the doctor
Go with your loved one to the appointment. Getting the information firsthand will help you know what you're facing and what you need to do for your loved one.
For schizophrenia, some basic questions to ask the doctor include:
- What's likely causing the symptoms or condition?
- What are other possible causes for the symptoms or condition?
- What kinds of tests are needed?
- Is this condition likely temporary or lifelong?
- What's the best treatment?
- What are the alternatives to the primary approach you're suggesting?
- How can I be most helpful and supportive?
- Do you have any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask any other questions during your appointment.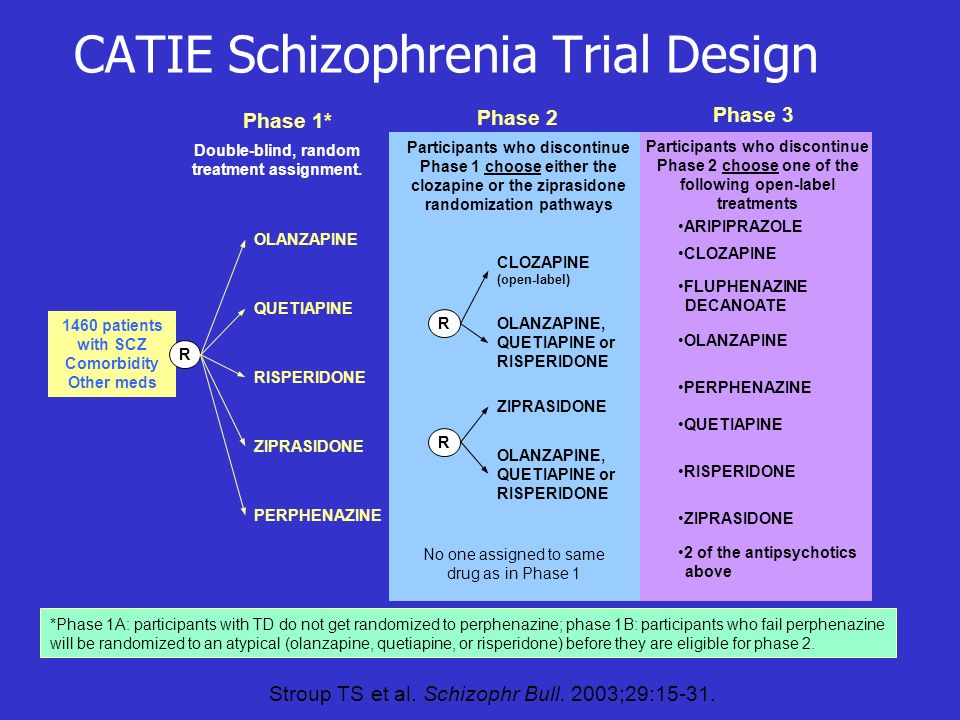
What to expect from your doctor
The doctor is likely to ask you a number of questions. Anticipating some of these questions can help make the discussion productive. Questions may include:
- What are your loved one's symptoms, and when did you first notice them?
- Has anyone else in your family been diagnosed with schizophrenia?
- Have symptoms been continuous or occasional?
- Has your loved one talked about suicide?
- How well does your loved one function in daily life — is he or she eating regularly, going to work or school, bathing regularly?
- Has your loved one been diagnosed with any other medical conditions?
- What medications is your loved one currently taking?
The doctor or mental health professional will ask additional questions based on responses, symptoms and needs.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Breakthrough in the treatment of schizophrenia: Janssen's new drug Trevicta is registered in Russia
Breakthrough in the treatment of schizophrenia: New drug Trevicta by Janssen is registered in Russia
Janssen, Johnson & Johnson Pharmaceutical Division ”, announces the registration in Russia of a new drug “Trevicta” (long-acting paliperidone palmitate) with a regimen of administration once every three months) for the maintenance treatment of patients with schizophrenia, which can significantly increase the interval between antipsychotic injections and use the drug 4 times a year, instead of monthly administration, as in the current use of injectable prolonged forms.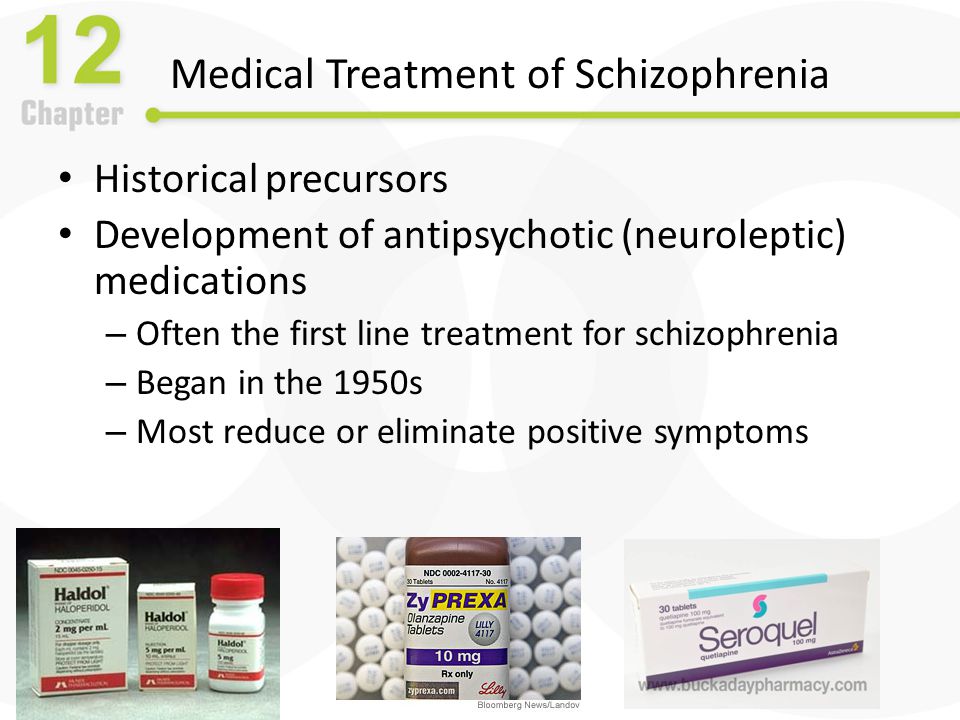 nine0003
nine0003
Trevicta is currently the antipsychotic with the longest dosing interval between two uses among all antipsychotics registered in Russia[1], which ensures the maintenance of the optimal concentration of the drug in the blood of patients and, accordingly, the lowest frequency of its use. Trevicta is prescribed only to those patients whose condition was stable during previous therapy with Xeplion (paliperidone palmitate, used to treat schizophrenia once a month). The 3-monthly paliperidone palmitate dosage form may be a valuable treatment option for patients with schizophrenia because the extended half-life of paliperidone may reduce the risk of relapse for an extended period after the last injection. The results of a placebo-controlled study of the drug "Trevikta" showed that about 95% of patients were stabilized for more than 1 year on therapy, and the median time to relapse was 274 days.
Ekaterina Pogodina, Executive Director of Janssen in Russia, said: “Schizophrenia and the expansion of Russian patients' access to modern therapy for this disease, in our opinion, require more attention from both the state and society today.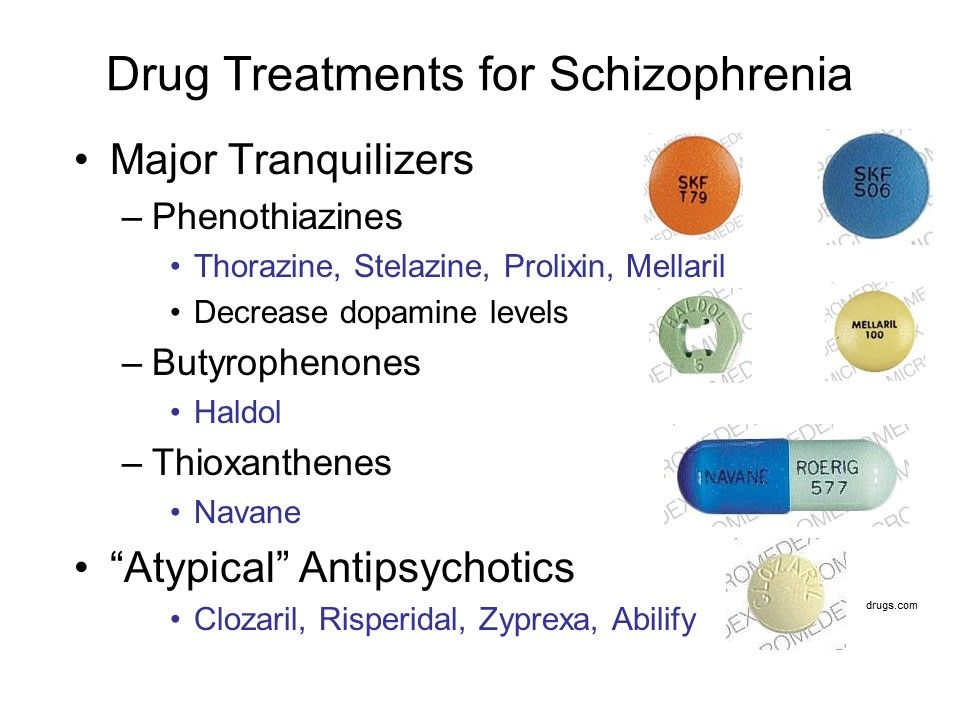 The medical aspect is also extremely relevant - ensuring adherence to treatment, maintaining a stable condition of the patient and the absence of relapses. Today, thanks to the registration of the innovative drug Trevicta, Russian healthcare has taken a big step towards solving the problem of socialization and adaptation of patients with this disease.” nine0003
The medical aspect is also extremely relevant - ensuring adherence to treatment, maintaining a stable condition of the patient and the absence of relapses. Today, thanks to the registration of the innovative drug Trevicta, Russian healthcare has taken a big step towards solving the problem of socialization and adaptation of patients with this disease.” nine0003
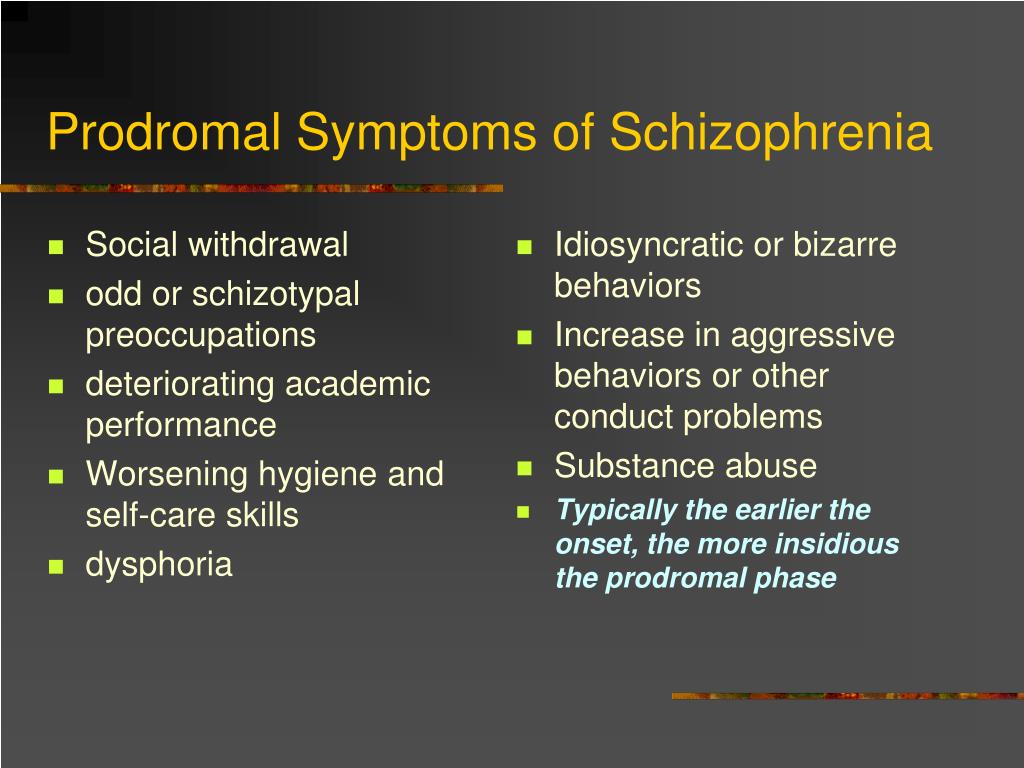
President of the Russian Society of Psychiatrists, Director of the St. Petersburg Research Psychoneurological Institute. V.M. Bekhtereva, MD, prof. Nikolai Grigoryevich Neznanov said: “The first 5 years of schizophrenia are a critical period in relation to the clinical and social consequences of the disease, and it is extremely important at this stage to provide intensive biopsychosocial assistance to patients aimed at improving the long-term prognosis. The level of relapses in such patients is very high due to poor compliance with the therapy regimen, and one of the conditions for a favorable prognosis of the disease is the quality of remission, which is associated both with the control of productive symptoms and, to a greater extent, with the effectiveness of the impact of therapy on negative, cognitive and affective disease symptoms.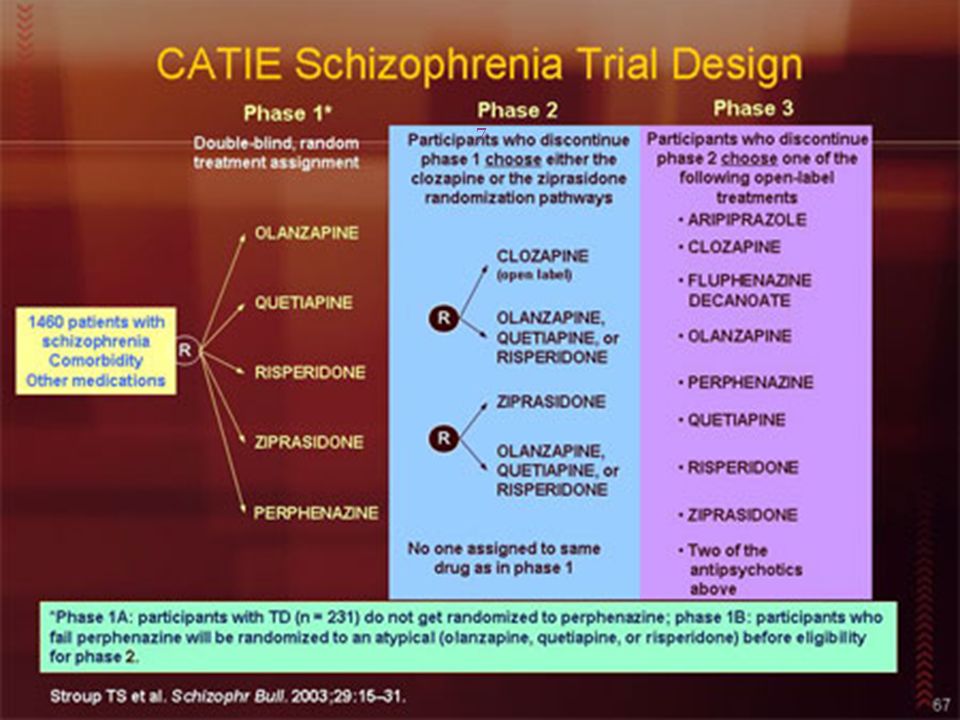 An important factor in providing maintenance therapy is the adherence of patients to treatment, which largely depends on the combination of the effectiveness and tolerability of psychopharmacotherapy. In this regard, injectable long-acting atypical antipsychotics meet all modern requirements and approaches to the treatment of patients with schizophrenia.” nine0003
An important factor in providing maintenance therapy is the adherence of patients to treatment, which largely depends on the combination of the effectiveness and tolerability of psychopharmacotherapy. In this regard, injectable long-acting atypical antipsychotics meet all modern requirements and approaches to the treatment of patients with schizophrenia.” nine0003
Schizophrenia is a serious mental illness that leads to significant clinical and socioeconomic consequences: poor adherence to therapy increases the risk of negative outcomes of the disease, including relapses, readmissions, suicides, and, accordingly, increases the socioeconomic burden of the disease. In addition, schizophrenia is characterized by frequent hospitalizations (rehospitalization rate was 40%) and high patient disability (66% of the total number of patients with schizophrenia with disabilities) in the Russian Federation according to the latest data. More than 60% of the burden of schizophrenia in the Russian Federation is made up of indirect costs, including: GDP losses, payments due to temporary disability, monthly cash payments, disability pensions.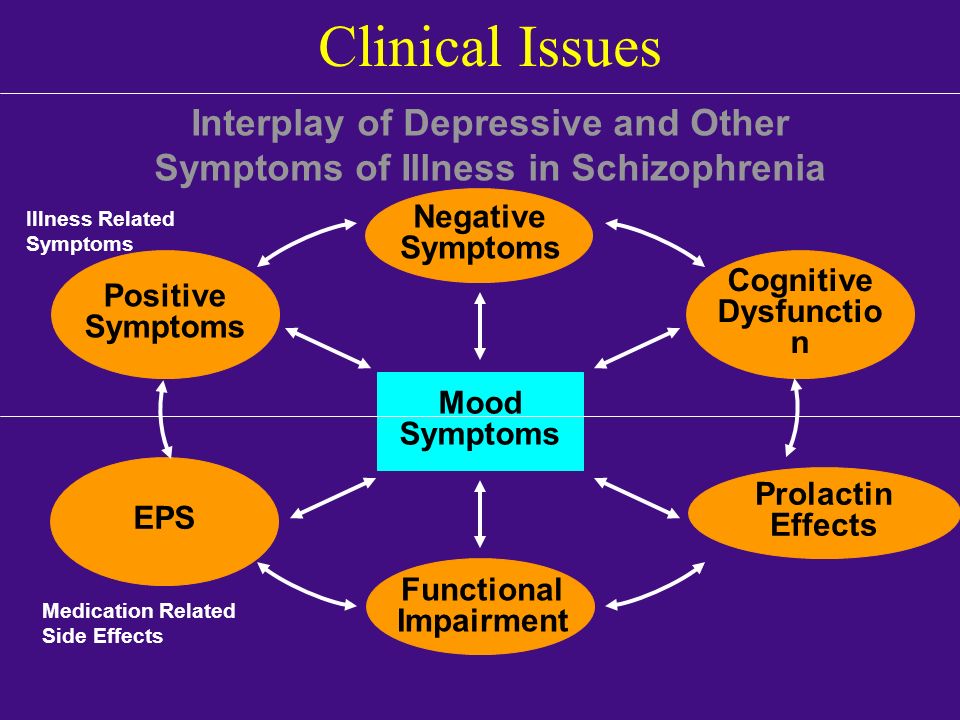 nine0003
nine0003
According to the Moscow Research Institute (NII) of Psychiatry, at the end of 2014 in the Russian Federation alone, the total number of registered patients with schizophrenia was 372.1 per 100,000 population (in total - 544,192 people)[2].
[1] State Register of Medicines // http://www.grls.rosminzdrav.ru/Default.aspx
[2] Gurovich I.Ya., Shmukler A.B., Golland V.B. and others. Psychiatric service in Russia in 2006-2011. Dynamics of indicators and analysis of development processes: monograph. Moscow:, 2012. 600 p. (updated data for 2012-2014)
Contact for inquiries from the media:
Alexey Shavenzov / [email protected]
+7 495 755 8357 (ext. 2078)
Data from a new study in the treatment of schizophrenia Medvestnik
•
New study data in...
New data on the use of cariprazine in the treatment of negative symptoms of schizophrenia were presented at the 28th Annual Meeting of the European Psychiatric Association (EPA), held online July 4-7, 2020.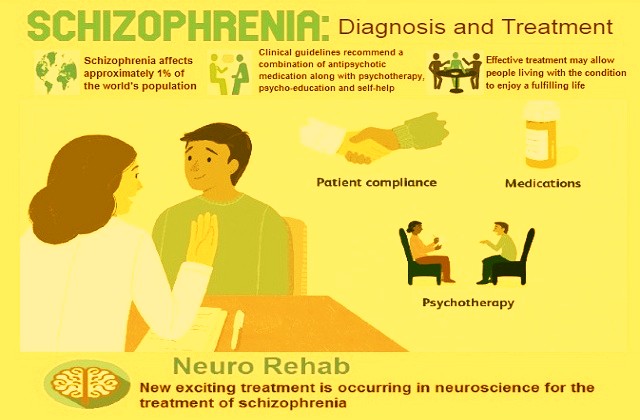 nine0003
nine0003
In an observational study conducted in outpatient psychiatric hospitals, the positive effect of the drug on the negative symptoms of schizophrenia in those patients for whom previous therapy was ineffective was confirmed, as well as a favorable safety profile of the drug. The study also showed that the effect of cariprazine on changes in heart rate and QT interval is minimal, comparable to placebo. In addition, a retrospective analysis of the use of cariprazine and risperidone showed that only cariprazine had a positive effect on negative symptoms in patients during an exacerbation of the disease. nine0003
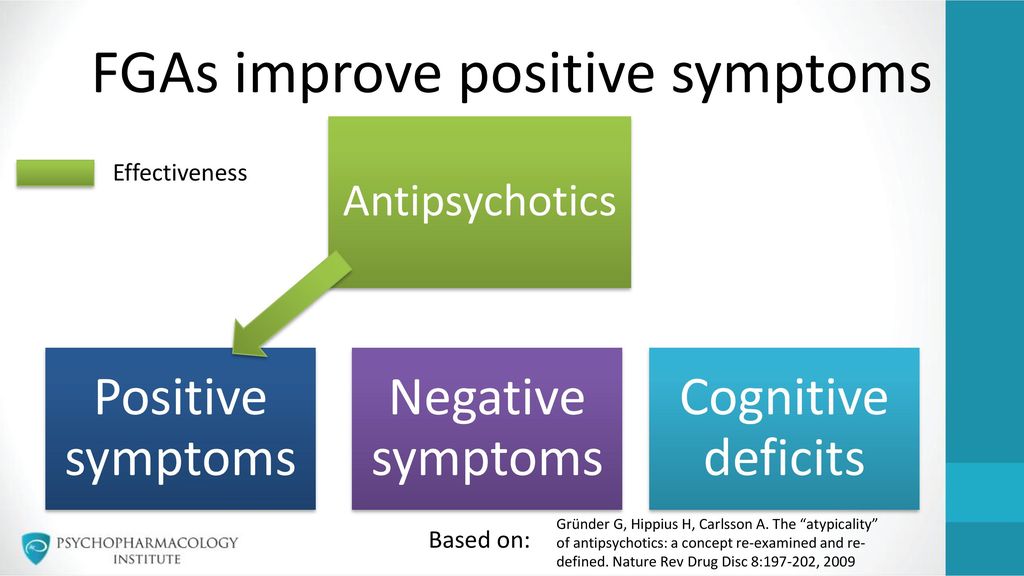
Schizophrenia is a chronic mental illness characterized by positive and negative symptoms, behavioral disorders and cognitive impairment. In the world, this disease affects about 1% of the population; 5 million people in the European Union struggle with schizophrenia. Negative symptoms of the disease appear in almost 60% of patients and have a significant impact on their daily life.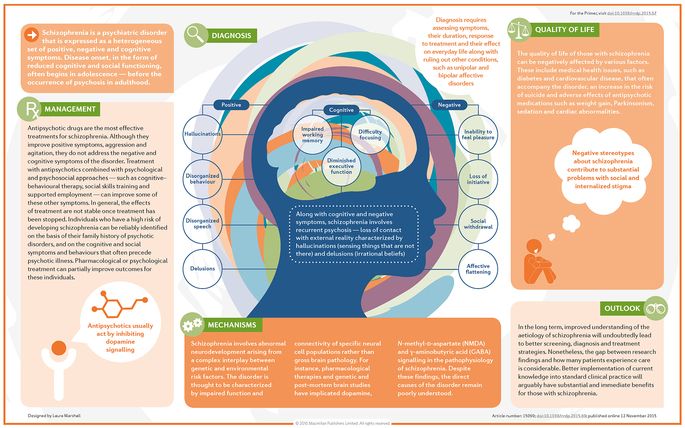 Antipsychotics have been proven to be effective in treating the positive symptoms of the disease, but treating the negative symptoms of schizophrenia remains a huge challenge for modern medicine. nine0003
Antipsychotics have been proven to be effective in treating the positive symptoms of the disease, but treating the negative symptoms of schizophrenia remains a huge challenge for modern medicine. nine0003
In double-blind studies, cariprazine has already proven effective in treating all symptoms of schizophrenia , however, it was important to obtain real clinical practice data in order to evaluate the effect of the drug on patients in their daily life. In Latvia, the manufacturer of cariprazine conducted a 16-week observational study involving 116 outpatients. The results showed that the drug had a positive effect on the relief of negative symptoms of schizophrenia in those patients who had not previously received the desired response to therapy. Also, when switching to treatment with cariprazine, the severity of the existing side effects of the previous therapy gradually decreased and no changes in weight were observed, which indicates a high safety profile of the drug. It is important to note that most physicians were extremely satisfied with the efficacy and good tolerability of cariprazine. nine0003
It is important to note that most physicians were extremely satisfied with the efficacy and good tolerability of cariprazine. nine0003
The following data were also presented at the EPA conference:
- Long-term antipsychotic treatment is indicated for all patients with schizophrenia. Drugs can be very effective but have side effects such as cardiac complications. In this connection, a retrospective analysis of the effect of cariprazine on the cardiovascular system was carried out, which showed that the effect of the drug on the parameters of the heart is generally comparable to placebo. Changes in heart rate and QT interval were minimal, the incidence of adverse events associated with the cardiovascular system, as well as associated cases of discontinuation of treatment, were extremely rare. nine0049
- In a retrospective analysis of the use of cariprazine and risperidone in the treatment of acute and primary negative symptoms of schizophrenia, both drugs showed the same effectiveness in controlling the general symptoms of exacerbation of schizophrenia.