Schizophrenia caused by
Causes - Schizophrenia - NHS
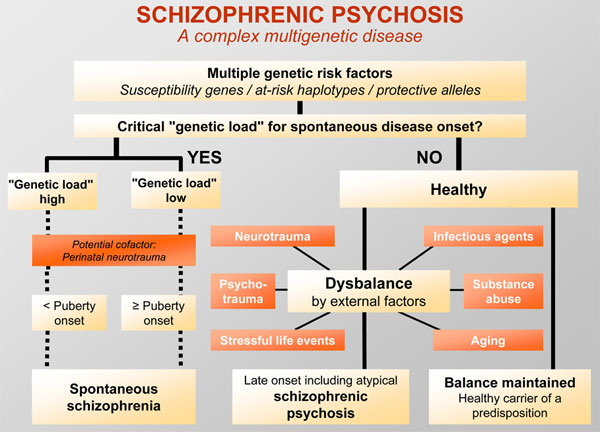
The exact causes of schizophrenia are unknown. Research suggests a combination of physical, genetic, psychological and environmental factors can make a person more likely to develop the condition.
Some people may be prone to schizophrenia, and a stressful or emotional life event might trigger a psychotic episode. However, it's not known why some people develop symptoms while others do not.
Increased risk
Genetics
Schizophrenia tends to run in families, but no single gene is thought to be responsible.
It's more likely that different combinations of genes make people more vulnerable to the condition. However, having these genes does not necessarily mean you'll develop schizophrenia.
Evidence that the disorder is partly inherited comes from studies of twins. Identical twins share the same genes.
In identical twins, if a twin develops schizophrenia, the other twin has a 1 in 2 chance of developing it, too. This is true even if they're raised separately.
In non-identical twins, who have different genetic make-ups, when a twin develops schizophrenia, the other only has a 1 in 8 chance of developing the condition.
While this is higher than in the general population, where the chance is about 1 in 100, it suggests genes are not the only factor influencing the development of schizophrenia.
Brain development
Studies of people with schizophrenia have shown there are subtle differences in the structure of their brains.
These changes are not seen in everyone with schizophrenia and can occur in people who do not have a mental illness. But they suggest schizophrenia may partly be a disorder of the brain.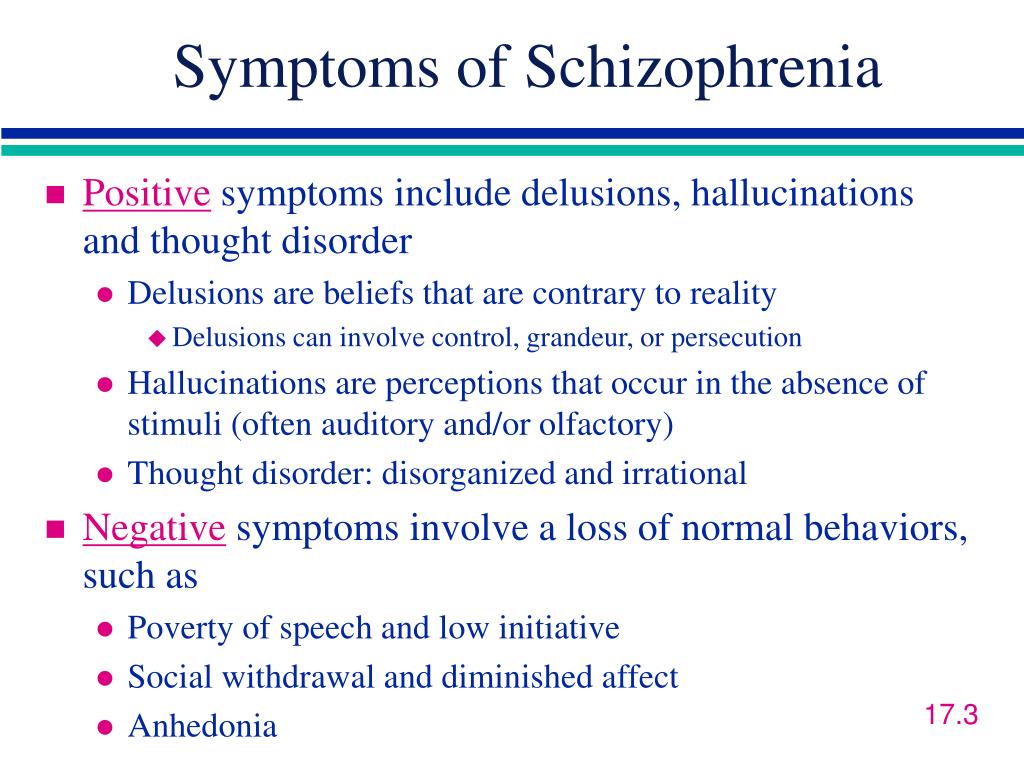
Neurotransmitters
Neurotransmitters are chemicals that carry messages between brain cells.
There's a connection between neurotransmitters and schizophrenia because drugs that alter the levels of neurotransmitters in the brain are known to relieve some of the symptoms of schizophrenia.
Research suggests schizophrenia may be caused by a change in the level of 2 neurotransmitters: dopamine and serotonin.
Some studies indicate an imbalance between the 2 may be the basis of the problem. Others have found a change in the body's sensitivity to the neurotransmitters is part of the cause of schizophrenia.
Pregnancy and birth complications
Research has shown people who develop schizophrenia are more likely to have experienced complications before and during their birth, such as:
- a low birthweight
- premature labour
- a lack of oxygen (asphyxia) during birth
It may be that these things have a subtle effect on brain development.
Triggers
Triggers are things that can cause schizophrenia to develop in people who are at risk.
These include:
Stress
The main psychological triggers of schizophrenia are stressful life events, such as:
- bereavement
- losing your job or home
- divorce
- the end of a relationship
- physical, sexual or emotional abuse
These kinds of experiences, although stressful, do not cause schizophrenia. However, they can trigger its development in someone already vulnerable to it.
Drug abuse
Drugs do not directly cause schizophrenia, but studies have shown drug misuse increases the risk of developing schizophrenia or a similar illness.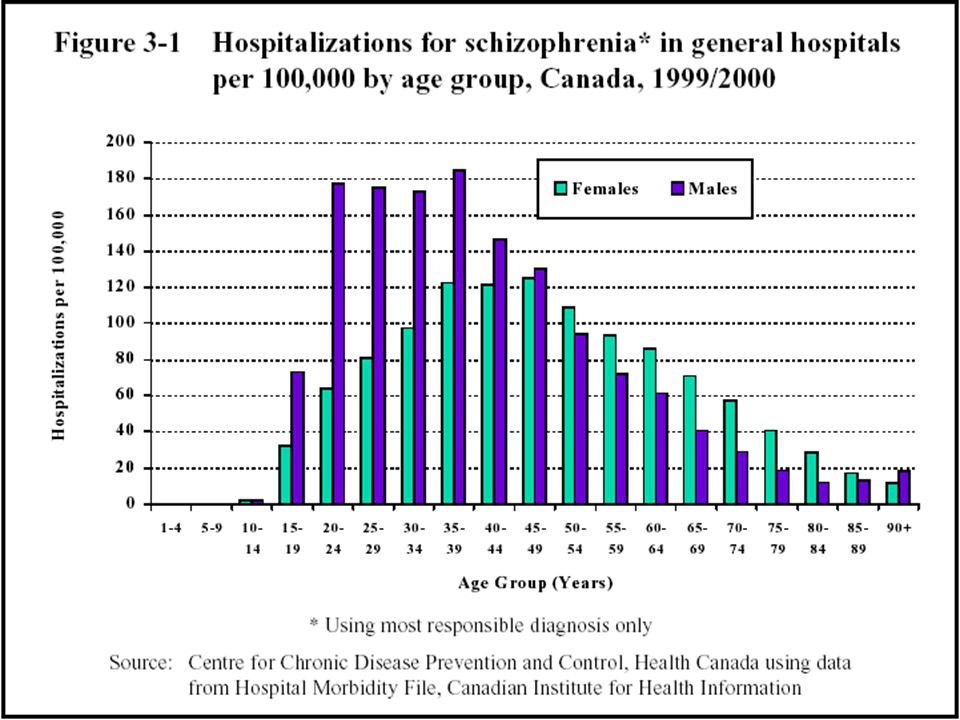
Certain drugs, particularly cannabis, cocaine, LSD or amphetamines, may trigger symptoms of schizophrenia in people who are susceptible.
Using amphetamines or cocaine can lead to psychosis, and can cause a relapse in people recovering from an earlier episode.
Research has shown that teenagers and young adults who use cannabis regularly are more likely to develop schizophrenia in later adulthood.
Want to know more?
- Mind: How can recreational drugs affect mental health?
- Mind: What causes schizophrenia?
Page last reviewed: 11 November 2019
Next review due: 11 November 2022
Schizophrenia - Symptoms and causes
Overview
Schizophrenia is a serious mental disorder in which people interpret reality abnormally. Schizophrenia may result in some combination of hallucinations, delusions, and extremely disordered thinking and behavior that impairs daily functioning, and can be disabling.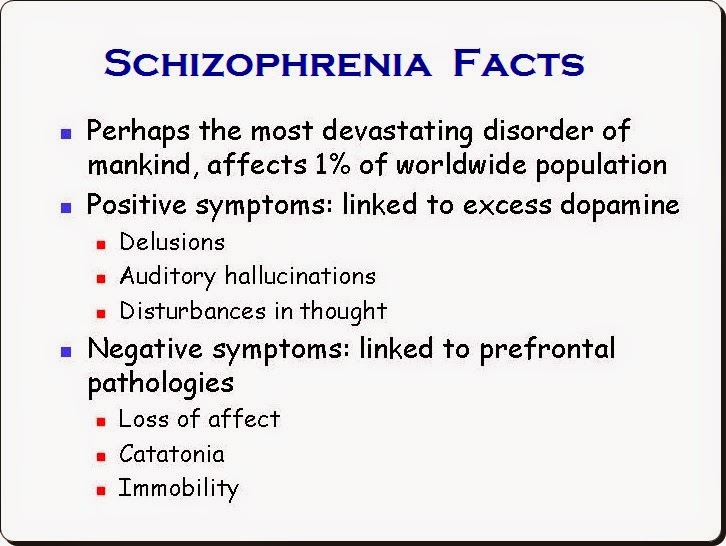
People with schizophrenia require lifelong treatment. Early treatment may help get symptoms under control before serious complications develop and may help improve the long-term outlook.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
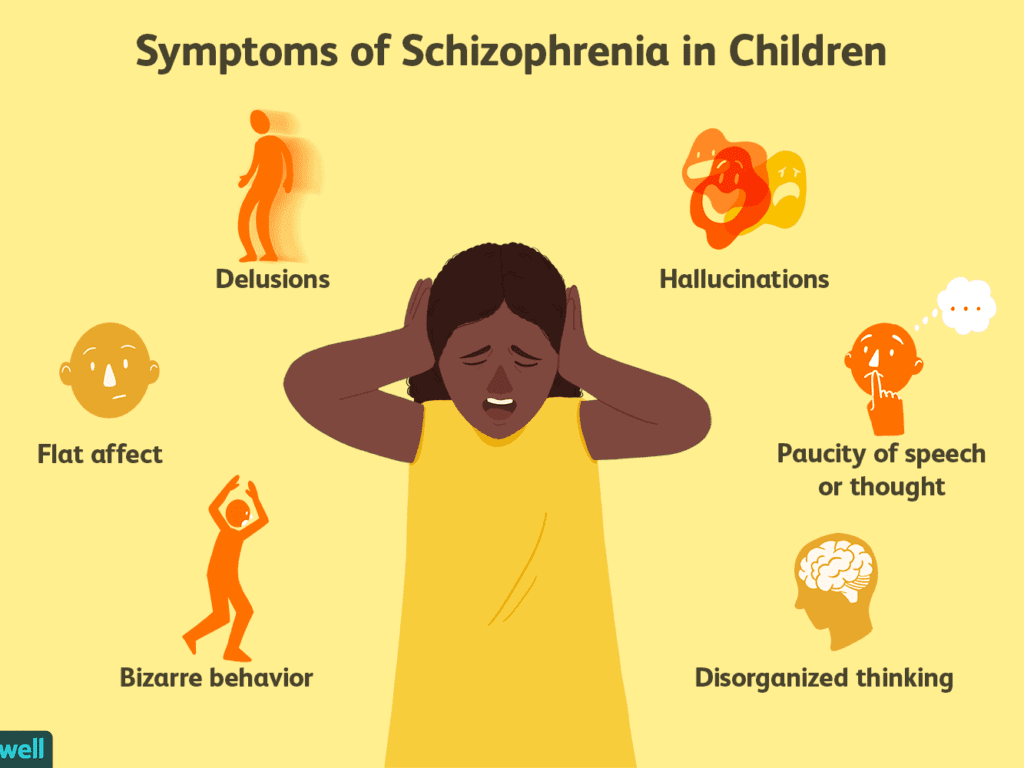
Schizophrenia involves a range of problems with thinking (cognition), behavior and emotions. Signs and symptoms may vary, but usually involve delusions, hallucinations or disorganized speech, and reflect an impaired ability to function. Symptoms may include:
- Delusions. These are false beliefs that are not based in reality. For example, you think that you're being harmed or harassed; certain gestures or comments are directed at you; you have exceptional ability or fame; another person is in love with you; or a major catastrophe is about to occur. Delusions occur in most people with schizophrenia.
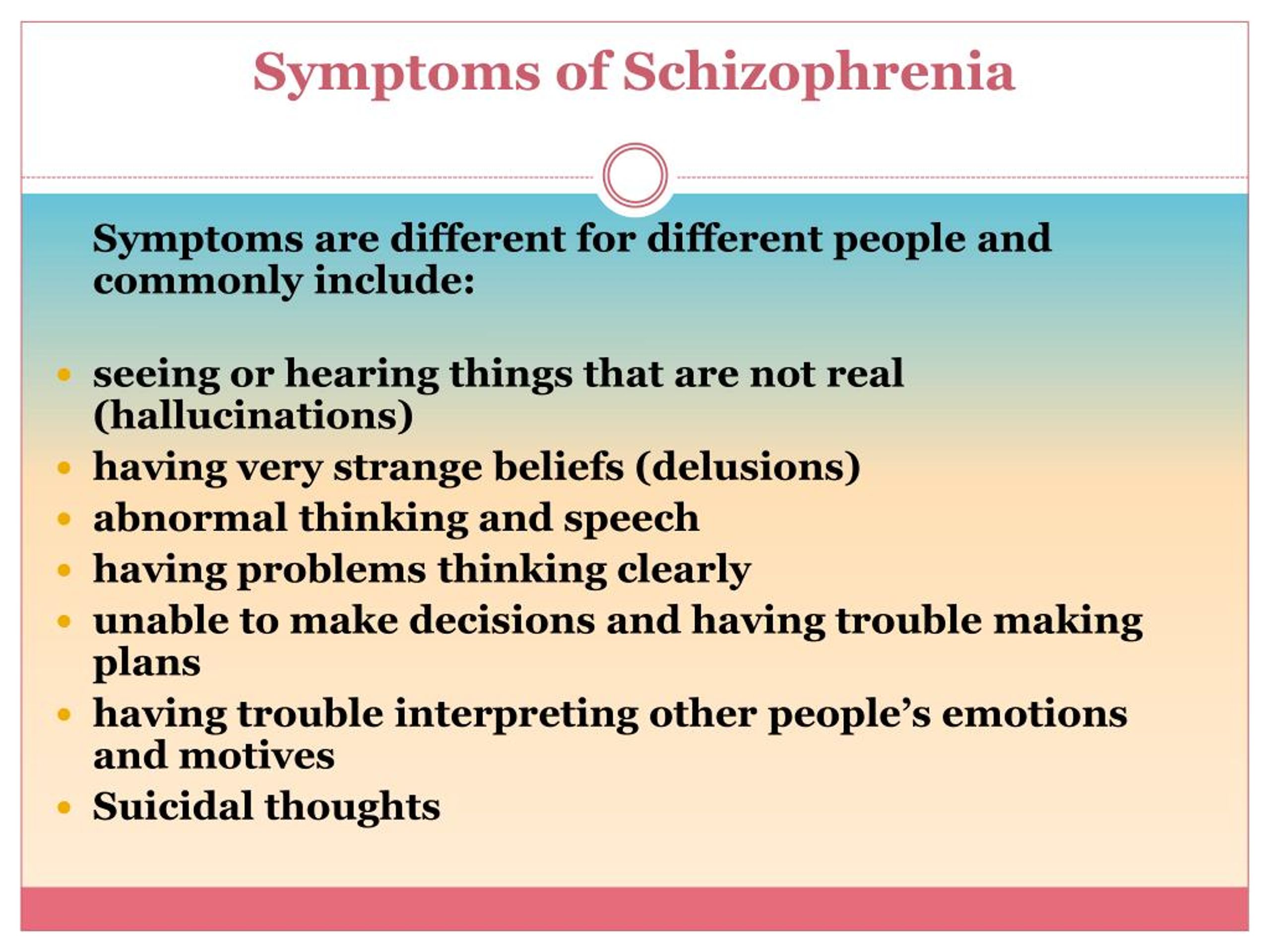
- Hallucinations. These usually involve seeing or hearing things that don't exist. Yet for the person with schizophrenia, they have the full force and impact of a normal experience. Hallucinations can be in any of the senses, but hearing voices is the most common hallucination.
- Disorganized thinking (speech). Disorganized thinking is inferred from disorganized speech. Effective communication can be impaired, and answers to questions may be partially or completely unrelated. Rarely, speech may include putting together meaningless words that can't be understood, sometimes known as word salad.
- Extremely disorganized or abnormal motor behavior. This may show in a number of ways, from childlike silliness to unpredictable agitation. Behavior isn't focused on a goal, so it's hard to do tasks. Behavior can include resistance to instructions, inappropriate or bizarre posture, a complete lack of response, or useless and excessive movement.
- Negative symptoms. This refers to reduced or lack of ability to function normally. For example, the person may neglect personal hygiene or appear to lack emotion (doesn't make eye contact, doesn't change facial expressions or speaks in a monotone). Also, the person may lose interest in everyday activities, socially withdraw or lack the ability to experience pleasure.
Symptoms can vary in type and severity over time, with periods of worsening and remission of symptoms. Some symptoms may always be present.
In men, schizophrenia symptoms typically start in the early to mid-20s. In women, symptoms typically begin in the late 20s. It's uncommon for children to be diagnosed with schizophrenia and rare for those older than age 45.
Symptoms in teenagers
Schizophrenia symptoms in teenagers are similar to those in adults, but the condition may be more difficult to recognize. This may be in part because some of the early symptoms of schizophrenia in teenagers are common for typical development during teen years, such as:
- Withdrawal from friends and family
- A drop in performance at school
- Trouble sleeping
- Irritability or depressed mood
- Lack of motivation
Also, recreational substance use, such as marijuana, methamphetamines or LSD, can sometimes cause similar signs and symptoms.
Compared with schizophrenia symptoms in adults, teens may be:
- Less likely to have delusions
- More likely to have visual hallucinations
When to see a doctor
People with schizophrenia often lack awareness that their difficulties stem from a mental disorder that requires medical attention. So it often falls to family or friends to get them help.
Helping someone who may have schizophrenia
If you think someone you know may have symptoms of schizophrenia, talk to him or her about your concerns. Although you can't force someone to seek professional help, you can offer encouragement and support and help your loved one find a qualified doctor or mental health professional.
If your loved one poses a danger to self or others or can't provide his or her own food, clothing, or shelter, you may need to call 911 or other emergency responders for help so that your loved one can be evaluated by a mental health professional.
In some cases, emergency hospitalization may be needed.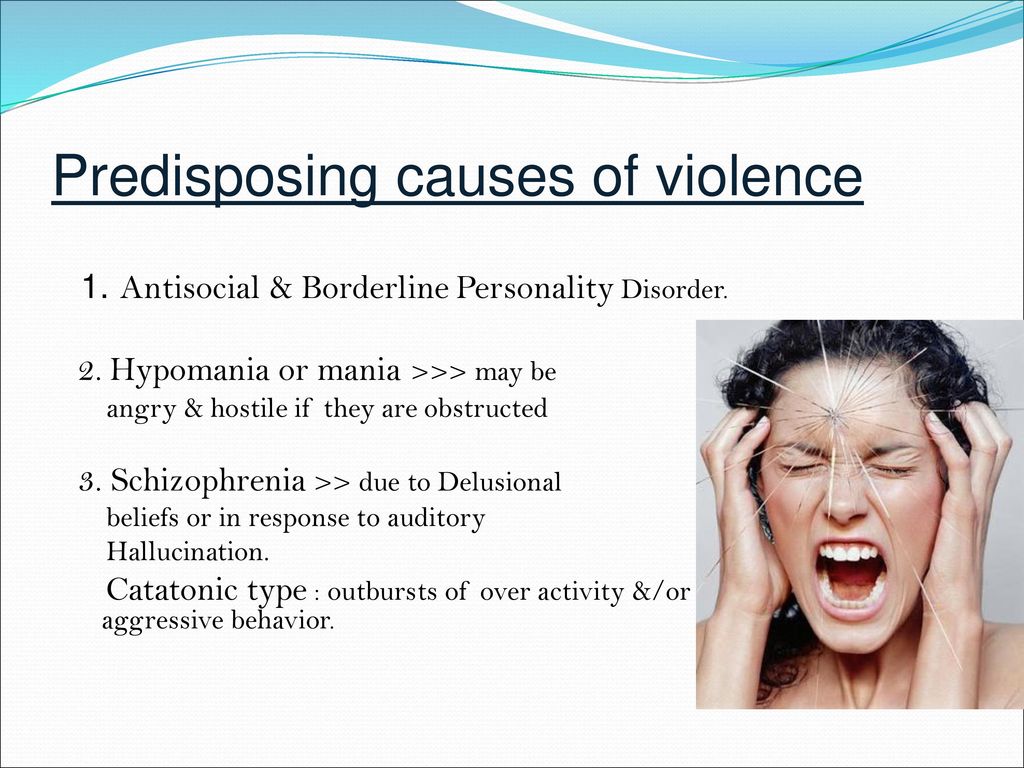 Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Laws on involuntary commitment for mental health treatment vary by state. You can contact community mental health agencies or police departments in your area for details.
Suicidal thoughts and behavior
Suicidal thoughts and behavior are common among people with schizophrenia. If you have a loved one who is in danger of attempting suicide or has made a suicide attempt, make sure someone stays with that person. Call 911 or your local emergency number immediately. Or, if you think you can do so safely, take the person to the nearest hospital emergency room.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
It's not known what causes schizophrenia, but researchers believe that a combination of genetics, brain chemistry and environment contributes to development of the disorder.
Problems with certain naturally occurring brain chemicals, including neurotransmitters called dopamine and glutamate, may contribute to schizophrenia. Neuroimaging studies show differences in the brain structure and central nervous system of people with schizophrenia. While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
While researchers aren't certain about the significance of these changes, they indicate that schizophrenia is a brain disease.
Risk factors
Although the precise cause of schizophrenia isn't known, certain factors seem to increase the risk of developing or triggering schizophrenia, including:
- Having a family history of schizophrenia
- Some pregnancy and birth complications, such as malnutrition or exposure to toxins or viruses that may impact brain development
- Taking mind-altering (psychoactive or psychotropic) drugs during teen years and young adulthood
Complications
Left untreated, schizophrenia can result in severe problems that affect every area of life. Complications that schizophrenia may cause or be associated with include:
- Suicide, suicide attempts and thoughts of suicide
- Anxiety disorders and obsessive-compulsive disorder (OCD)
- Depression
- Abuse of alcohol or other drugs, including nicotine
- Inability to work or attend school
- Financial problems and homelessness
- Social isolation
- Health and medical problems
- Being victimized
- Aggressive behavior, although it's uncommon
Prevention
There's no sure way to prevent schizophrenia, but sticking with the treatment plan can help prevent relapses or worsening of symptoms. In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
In addition, researchers hope that learning more about risk factors for schizophrenia may lead to earlier diagnosis and treatment.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Schizophrenia and psychosis due to drug use
From October 1, 2020 to Petersburg started the month of anti-drug events dedicated to International Day Against Drug Abuse and Drug Abuse illegal traffic.
Events traditionally held in April have been rescheduled for October.
The goal is to expand the forms of participation of the population in prevention of non-medical consumption and drug trafficking drugs and psychotropic substances, as well as the formation of public opinion, motivating for a healthy lifestyle and the resistance of adolescents and youth to drug pressure.
Within the framework of the month of anti-drug activities from 1 to 31 October in St. Petersburg GBUZ "Psychoneurological Dispensary No. 1 planned a set of anti-drug outreach activities, which will be implemented in cooperation with the administration of Vasileostrovsky district, subordinate institutions of education, healthcare, social defense and local governments.
1 planned a set of anti-drug outreach activities, which will be implemented in cooperation with the administration of Vasileostrovsky district, subordinate institutions of education, healthcare, social defense and local governments.
Activities will be carried out subject to current restrictions, related to the spread of a new coronavirus infection, and in compliance with all safety standards.
Is it possible to develop schizophrenia as a result of addiction?
Drug addiction, like Alcoholism today is one of the main social problems of society. Any addiction is a disease, no matter what substance it is caused by, the most important thing is that people suffer at the same time, their environment, their families are in dysfunctional connections. Children from these families do not receive proper education. Today this is a big scourge for Russia.
Is it possible to develop schizophrenia "from drug addiction"? It is difficult to answer the question unambiguously, each case considered by psychiatrists individually.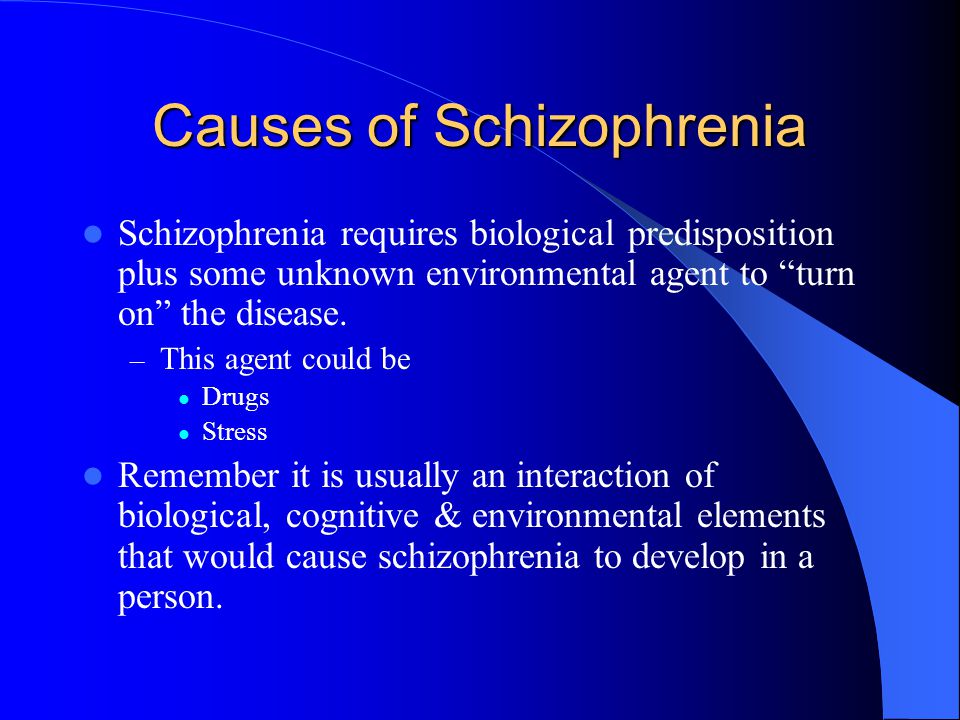 The brain is a fine structure, it is the balance of a large the amount of neurotransmitters. When you interfere with this structure, the consequences may be the most unpredictable.
The brain is a fine structure, it is the balance of a large the amount of neurotransmitters. When you interfere with this structure, the consequences may be the most unpredictable.
Drugs, especially synthetic production, have a strongly negative effect on the nervous human system. Such drugs can not only destroy brain cells, but and cause mental disorders. Schizophrenia and drug addiction are linked in complex ways. relationships, so, after taking drugs, it is possible to develop symptoms similar to those of schizophrenia (perceptual disturbances, hallucinatory states). At the same time, anyone who decides to “try” the drug must understand that that even a single use can lead to dire consequences for psyche. Is it worth experimenting with with your psyche?
Drugs with psychedelic effect (LSD, spices, amphetamines, etc.) can easily provoke the debut of schizophrenia in a healthy person, if his genes already predisposition to this disease. Scientists have proven that the amphetamines against the background of schizophrenia leads to an aggravation of the clinical picture and significant deterioration in the patient's condition. If the diagnosis has already been made, but the patient continues to use psychoactive substances, the prognosis is extremely adverse. The processes of destruction of brain cells, as well as degradation personality under the influence of drugs occur much faster. high risk the onset of psychosis, which are much more severe than outside the reception narcotic substances.
If the diagnosis has already been made, but the patient continues to use psychoactive substances, the prognosis is extremely adverse. The processes of destruction of brain cells, as well as degradation personality under the influence of drugs occur much faster. high risk the onset of psychosis, which are much more severe than outside the reception narcotic substances.
Many schizophrenics are under the influence of drugs become socially dangerous. They can kill or cripple others without feeling any remorse (even after coming out of a state of narcotic intoxication). Another danger is the possibility of suicide of the patient, who in such a state can imagine numerous dangers, enemies or vice versa - instead of a balcony of the 15th floor a person can see a green lawn and strive to get into it.
The development of schizophrenia can provoke strong psychoactive substances used in large quantities that have a strong hallucinogenic effect. One of the studies confirms the fact of the development of acute psychoses against the background of cannabis use.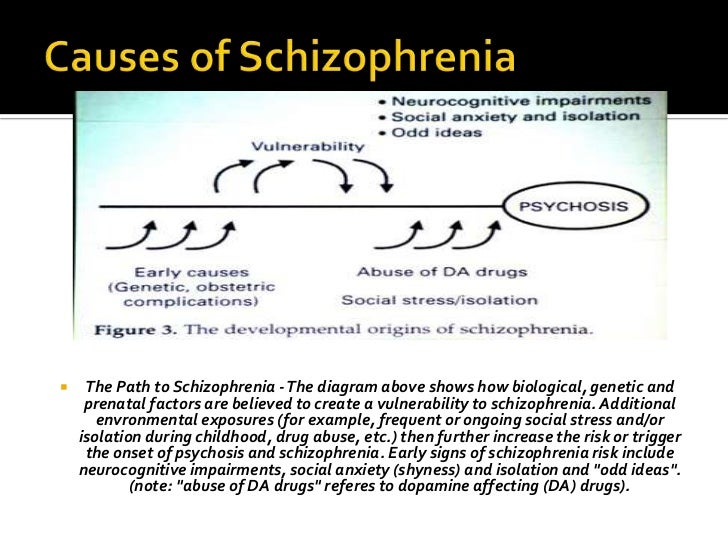
Psychoses against the backdrop of addiction. Synthetic drugs cause mental disorders that are extremely difficult to treat. Long-term use of synthetic drugs causes severe anxiety, panic attacks and depression. Substance use causes irritability, sleep and appetite disorders, behavioral and sexual violations.
Drugs lead to affective disorders that can "flow" under the guise of dysthymia, depression, bipolar disorder.
Also among drug addicts many patients suffering from paranoid schizophrenia, which is observed in lovers of synthetic analogues of cocaine: amphetamine, pervitin, methamphetamine. Symptoms manifest as delusional, auditory, visual, and tactile hallucinations. Patients with these disorders have aggressive behavior, they are often involved in criminal situations.
Regular the use of the mixture in demand today, acute hallucinations are added to delusional ideas, impaired thinking, gross changes are clearly visible personality. Spice addicts, usually after a certain amount of time end up in a psychiatric ward, because they become dangerous for a healthy society.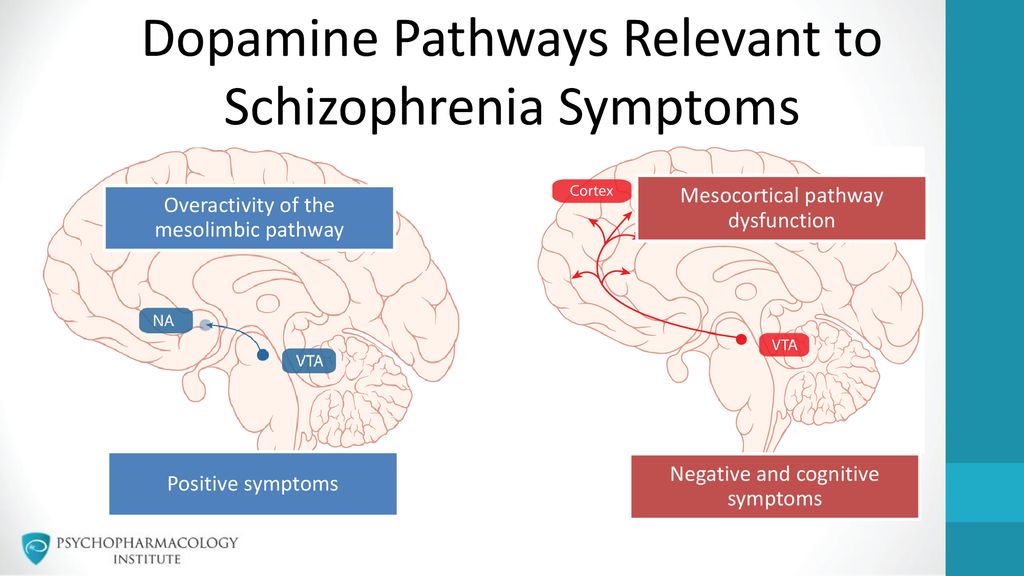 Then doctors may suspect the progression of schizophrenia, creeping unnoticed under the influence of synthetic cannabinoids, to to which the prohibited drug belongs.
Then doctors may suspect the progression of schizophrenia, creeping unnoticed under the influence of synthetic cannabinoids, to to which the prohibited drug belongs.
In addition to being provokes a significant decrease in the cortical content of dopamine, at the same time by increasing its content in the midbrain, the drug leads to extremely rapid development of a debilitating mental disorder. If a person is prone to the emergence of a mental disorder, indulging in drugs, he reaches the fact that the hidden illness is transformed into schizophrenia with all the consequences consequences. Progressing by leaps and bounds, it completely cuts off person from normal life.
Mental drug treatment . Therapy drug-induced psychosis significantly complicated, synthetic psychoactive substances strongly bind to brain receptors and accumulate in body tissues. This condition is treated primarily in a psychiatric hospital, psycho-neurological dispensary by qualified specialists - narcologist, psychiatrist, psychotherapist.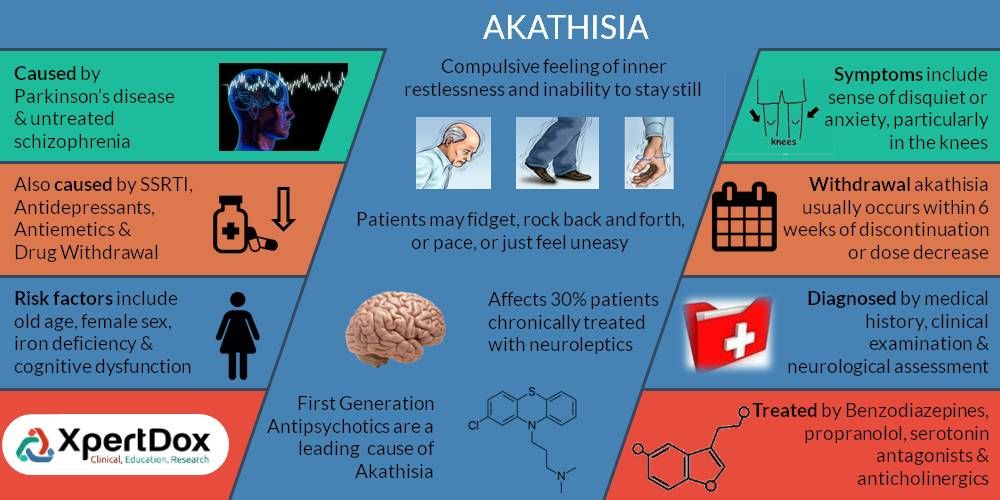
We are still not completely understand how to treat it. You need to select a drug regimen. Often this is the selection of drugs in order to a little bit to restore the psyche. Often the process takes several years (!!!) Treatment drug addiction is a complex process that requires a lot of effort and takes a lot of time.
The best way to fight long-term psychotherapy can be with harmful dependence. As in healthy and in sick people, the cause of cravings for alcohol and drugs is most often an increased level of anxiety, which helps to remove work with a competent a psychotherapist who knows how to interact with mentally ill patients, knows the peculiarities of their thinking and ways of influencing specific altered consciousness of a patient with schizophrenia.
Conclusion: Mandatory a condition for successful therapy is compliance with the rehabilitation period, which can last from 6 months to several years. The most difficult is search for an incentive to continue life without drugs.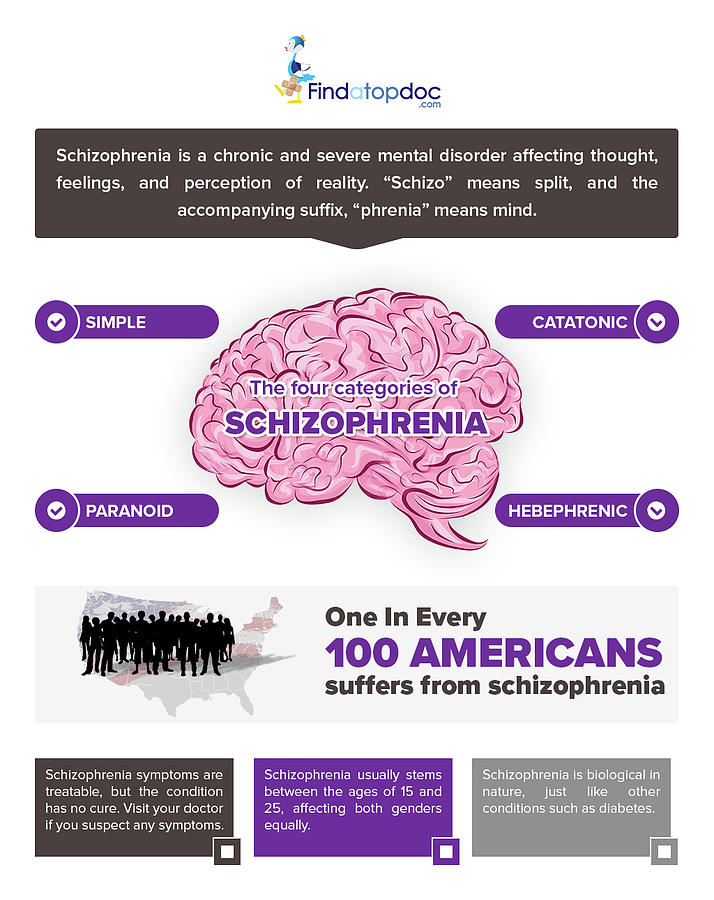 In this case, it is required help of professional psychotherapists, psychologists and support of relatives. Any pathological addiction schizophrenia is dangerous for the patient and can aggravate the course of the disease. Unfortunately, science does not know of a "magic pill" that can instantly rid the patient of drug addiction. Long-term work with specialists, trust doctor and careful intake of prescribed medications will help the patient cope with dangerous habits for him, and with the underlying disease, in order to return again to a normal (or almost normal) life in society.
In this case, it is required help of professional psychotherapists, psychologists and support of relatives. Any pathological addiction schizophrenia is dangerous for the patient and can aggravate the course of the disease. Unfortunately, science does not know of a "magic pill" that can instantly rid the patient of drug addiction. Long-term work with specialists, trust doctor and careful intake of prescribed medications will help the patient cope with dangerous habits for him, and with the underlying disease, in order to return again to a normal (or almost normal) life in society.
SPb GBUZ "Psycho-neurological dispensary No. 1" social work specialist Vysotskaya V.P. Depression in schizophrenia: diagnosis and therapy
Perhaps the only issue on which a certain consensus has been reached is that depression is an integral part of schizophrenia and it can develop in any form and at any stage of the course of the disease [20].
 Although there are indications of a “mitigating” effect of depression on the manifestations of schizophrenia [2, 26], most researchers consider the presence of depression as an unfavorable prognostic factor that reduces the quality of life of patients, aggravates their psychosocial functioning disorders and increases the risk of suicide [28].
Although there are indications of a “mitigating” effect of depression on the manifestations of schizophrenia [2, 26], most researchers consider the presence of depression as an unfavorable prognostic factor that reduces the quality of life of patients, aggravates their psychosocial functioning disorders and increases the risk of suicide [28]. The incidence of depressive symptoms in schizophrenia ranges from 7 to 70% [31]. Such a wide range of indicators may be due to the examination of patients at different stages of the disease, as well as the lack of generally accepted methodological approaches not only to assessing individual depressive symptoms, but also the full-blown depressive syndrome. The results of a study by J. Sands and M. Harrow [29], who observed 70 patients with schizophrenia for 7.5 years, showed that in 24% of cases there were no depressive symptoms, 26% had individual depressive symptoms, and 14% had subsyndromal depression. and 36% had depression meeting clinical criteria for major depressive disorder [29].
Modern classifications of ICD-10 and DSM-IV when registering depression in patients with schizophrenia (in particular, post-seizure depression) suggest using the same diagnostic landmarks as for a depressive episode within an affective disorder. This approach significantly reduces the detection of depressive disorders in patients with schizophrenia. Probably, it is necessary to develop guidelines that would reflect the phenomenological specificity of depression in schizophrenia to a greater extent.
There are different concepts in the literature regarding the development of depression in schizophrenia.
According to the personality-reactive hypotheses, the formation of depression is mainly associated with the psychological reaction of the individual to the fact of the existence of a mental disorder and the social maladaptation caused by it [18]. However, within the framework of these hypotheses, there is another view: it is the presence of depression in patients with schizophrenia that causes psychological discomfort and contributes to the growth of social decompensation [33].
The pharmacogenic concept emphasizes the role of antipsychotic therapy in the formation of depression. In the literature [16, 36], the hypothesis of pseudoparkinsonian depression is widely discussed, suggesting its connection with extrapyramidal syndrome (EPS). At the same time, they do not exclude [19] the direct effect of antipsychotic drugs on dopamine transmission. The antidopamine activity of antipsychotics leads to the development of not only EPS, but also hyperprolactinemia. The latter attracts attention due to the fact that there are data in the literature [3, 8, 22, 34] on the development of affective disorders with elevated prolactin levels both in patients with endocrine disorders and in mentally ill patients. However, in our opinion, in this case, the fact that an increase in prolactin may be related to thyroid hormones, which play a significant role in the development of affective pathology, is also underestimated. It can be added to the above that when using atypical antipsychotics, which significantly less contribute to the development of neurological side effects, depressive symptoms develop during therapy in 10-13% of cases [4, 5]. Therefore, ideas about the relationship of depression with antipsychotic therapy require further development.
There is also a hypothesis that depression is an integral, core component of schizophrenia (at least one of the variants of this disease), along with negative and positive symptom complexes [5, 20]. This point of view is supported by data on the existence of depressive vulnerability in a number of patients with schizophrenia [5].
Among other things, in patients with schizophrenia, depression can be caused by a somatic disease, taking certain drugs (β-blockers, calcium channel blockers, hypnotics, indomethacin, corticosteroids), drug and drug dependence, alcoholism.
Thus, one can speak of primary depression in schizophrenia and secondary, or symptomatic, depressive states. In clinical practice, there are, apparently, depressive states, in the formation of which several (more than one) factors take part. And if a number of secondary depressions can be diagnosed in a timely manner, then in some cases it is sometimes difficult to determine the role of one or another mechanism in the formation of primary depression1. It is all the more difficult to objectively assess the contribution to the formation of depression of reactive mechanisms, which are most often present in varying degrees in patients with a chronic disease.
Diagnostic uncertainty entails therapeutic uncertainty in relation to approaches to the treatment of patients with depression in the structure of a schizophrenic attack. The most controversial issue concerns the advisability of using antidepressants in this category of patients. The main concerns are related to the risk of exacerbation of psychotic symptoms when prescribing antidepressants, as well as the possible increase in side effects due to drug interactions. So, there is data [9], that with the simultaneous appointment of antipsychotics and antidepressants in ¼ of cases, the latter have to be canceled 1-2 weeks after the start of therapy due to an increase in psychotic symptoms. It should be noted, however, that recommendations for limiting the use of antidepressants in schizophrenia are based on only a few clinical studies that have studied the combined use of conventional antipsychotics and tricyclic antidepressants, i. e. their evidence base is insufficient.
These studies are analyzed most fully in one of the meta-reviews [23], which considers the results of 11 placebo-controlled studies. His results have been contradictory. Five studies provided evidence in favor of the combined use of antidepressants with antipsychotics compared with antipsychotics alone, in six others - the opposite results. Additionally, it was noted that in one study the combination of an antidepressant and an antipsychotic was less effective than monotherapy, and in another study, an exacerbation of psychotic symptoms with an increase in the severity of thinking disorders was noted during treatment with antidepressants. There is also a study [30], which indicates that the addition of imipramine to antipsychotic therapy reduces the severity of depressive symptoms without causing an exacerbation of psychosis and significant side effects.
In recent years, a number of publications have appeared that confirm that the introduction of antidepressants into antipsychotic therapy not only does not cause exacerbation of psychotic manifestations, but, on the contrary, has additional advantages.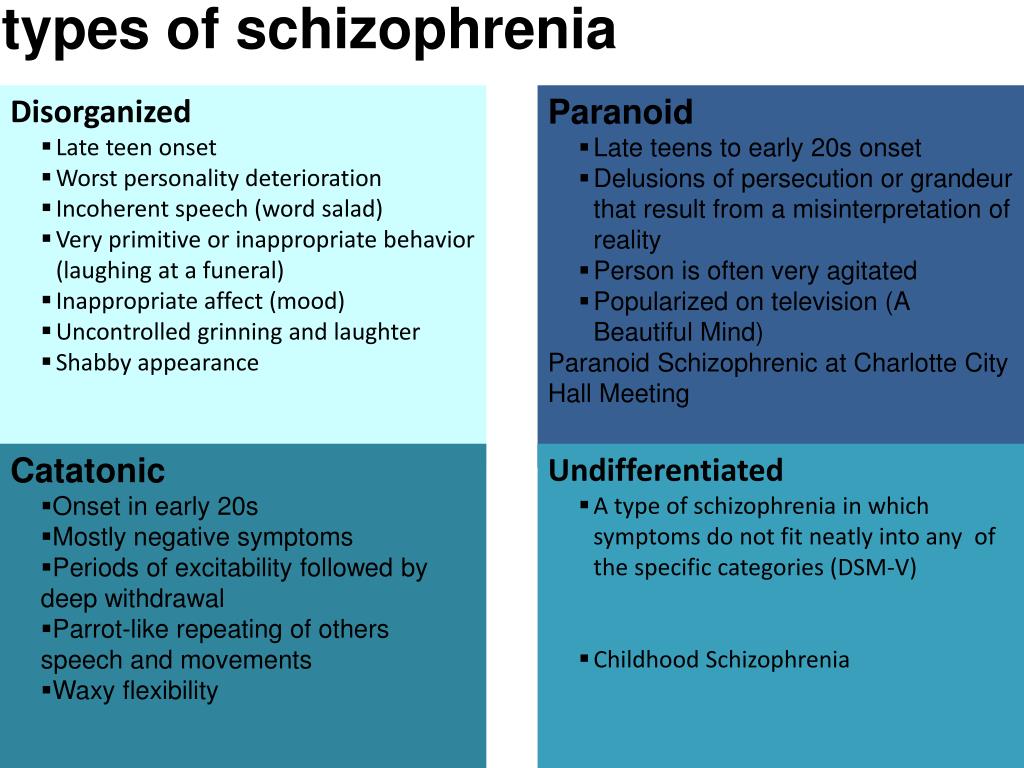 Thus, in a double-blind, placebo-controlled study [21], data were obtained on an increase in the antipsychotic effect of traditional antipsychotics when mirtazapine was added in cases where there was resistance to therapy. In the available literature, we did not find definite data on the effect of mirtazapine on depressive symptoms in patients with schizophrenia when combined with antipsychotics, but some studies [11, 32] indicate its effect on cognitive impairment that may be associated with depression.
Thus, in a double-blind, placebo-controlled study [21], data were obtained on an increase in the antipsychotic effect of traditional antipsychotics when mirtazapine was added in cases where there was resistance to therapy. In the available literature, we did not find definite data on the effect of mirtazapine on depressive symptoms in patients with schizophrenia when combined with antipsychotics, but some studies [11, 32] indicate its effect on cognitive impairment that may be associated with depression.
In accordance with the topic of this review, the effect on depression in schizophrenia of modern antidepressants - selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine, which are known to have a more favorable efficacy and safety profile compared to tricyclic antidepressants, requires special consideration.
Existing concerns about the use of SSRIs in combination with atypical antipsychotics due to pharmacokinetic interactions and the risk of increased side effects seem to us somewhat exaggerated.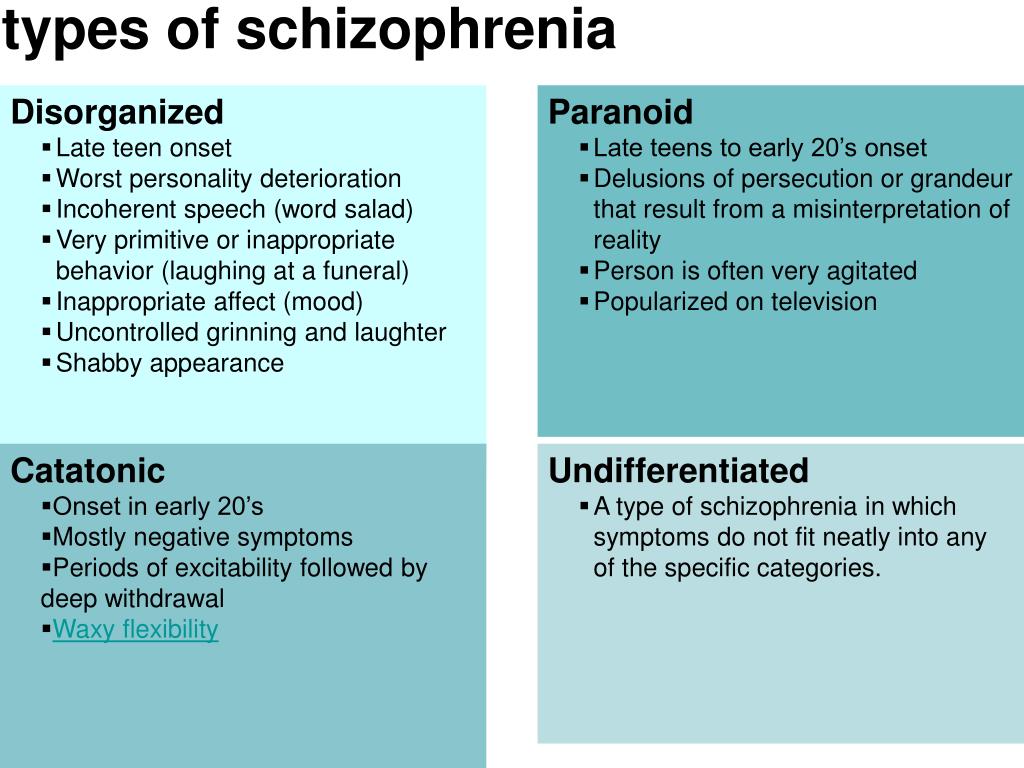 First, individual SSRIs differ in their ability to inhibit the cytochrome P450 system (fluoxetine, paroxetine are strong inhibitors, fluvoxamine has a less pronounced inhibitory ability, sertraline and citalopram have practically no effect on the microsomal enzyme system) [1]. Secondly, pharmacokinetic studies show that all SSRIs in therapeutic dosages do not cause clinically significant changes in plasma concentrations of antipsychotics and their combined use is acceptable [15, 27]. Moreover, from the standpoint of evidence-based medicine, this combination is one of the methods of choice in the treatment of psychotic and treatment-resistant depression. None of the studies with the combined use of antidepressants and antipsychotics showed a higher incidence of exacerbation of psychotic symptoms, and there is evidence of the effective use of antidepressants of the SSRI group in the treatment of an acute attack of schizophrenia.
First, individual SSRIs differ in their ability to inhibit the cytochrome P450 system (fluoxetine, paroxetine are strong inhibitors, fluvoxamine has a less pronounced inhibitory ability, sertraline and citalopram have practically no effect on the microsomal enzyme system) [1]. Secondly, pharmacokinetic studies show that all SSRIs in therapeutic dosages do not cause clinically significant changes in plasma concentrations of antipsychotics and their combined use is acceptable [15, 27]. Moreover, from the standpoint of evidence-based medicine, this combination is one of the methods of choice in the treatment of psychotic and treatment-resistant depression. None of the studies with the combined use of antidepressants and antipsychotics showed a higher incidence of exacerbation of psychotic symptoms, and there is evidence of the effective use of antidepressants of the SSRI group in the treatment of an acute attack of schizophrenia.
As an example of the above [17], a placebo-controlled study of the efficacy and safety of the combined use of fluvoxamine and olanzapine in the treatment of an acute attack of schizophrenia can be given.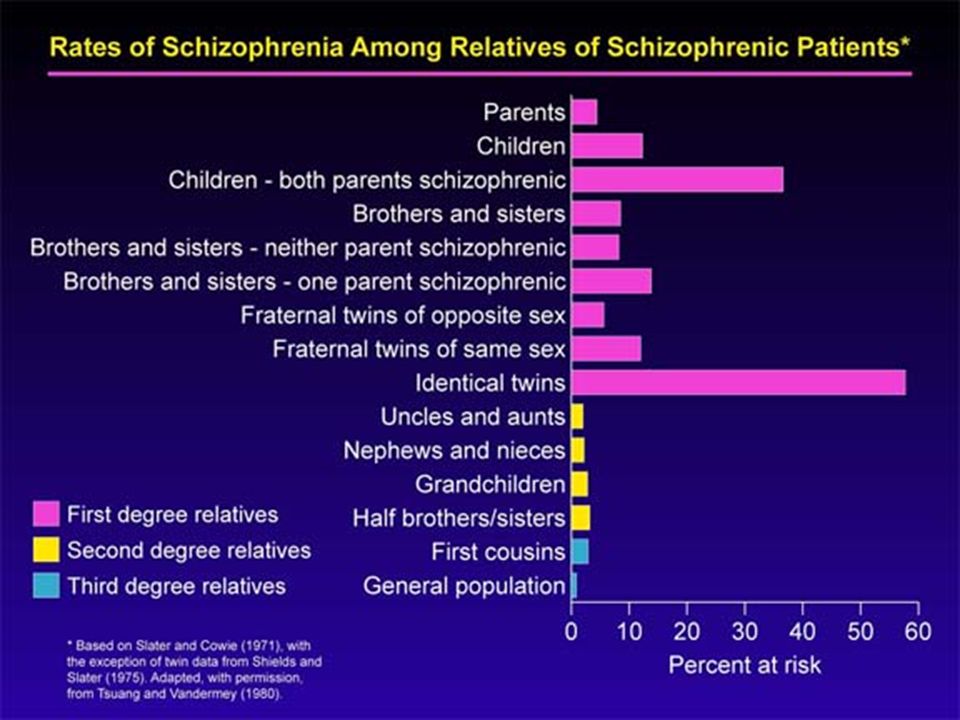 The study included 20 patients, the duration of therapy was 6 weeks. It was found that in the group of patients treated with olanzapine and fluvoxamine, there was a more pronounced reduction in the total score on the BPRS scale compared with the group treated with olanzapine and placebo. There were no differences in the incidence of side effects between the groups. This suggests that the combined use of SSRI antidepressants and antipsychotics is acceptable in terms of efficacy and safety.
The study included 20 patients, the duration of therapy was 6 weeks. It was found that in the group of patients treated with olanzapine and fluvoxamine, there was a more pronounced reduction in the total score on the BPRS scale compared with the group treated with olanzapine and placebo. There were no differences in the incidence of side effects between the groups. This suggests that the combined use of SSRI antidepressants and antipsychotics is acceptable in terms of efficacy and safety.
However, most recommendations for the management of patients with schizophrenia, while allowing for the possibility of prescribing antidepressants in the development of depression, note that this approach cannot be considered as the first choice therapy, especially in cases of combination with productive symptoms [14, 25, 35 ], because there is currently no evidence base confirming the expediency of such tactics [24]. A review by The Cochrane Collaboration [37] emphasizes that although the combination of antipsychotics and antidepressants may be effective in the treatment of depressive and negative manifestations of schizophrenia, a small number of studies can neither reliably confirm nor refute this position. Moreover, the published results have significant limitations. First of all, this refers to the assessment of the depressive component. As already mentioned, the diagnostic criteria for depression offered by official classifications are very vague. Many studies use the Hamilton Depression Scale (HAM-D) to assess the level of depression, although it has been proven [7] that it has little specificity for detecting and assessing depression in patients with schizophrenia, since its indicators correlate with a negative symptom complex. In addition, attention is not always paid to at what stage of the disease an antidepressant is prescribed. And quite rarely, the psychopathological structure of depression is analyzed in detail, which can significantly affect both the course of the disease and the therapeutic prognosis [5, 10]. Thus, for a more informed decision on the advisability of using antidepressants in this aspect, additional studies, methodically clearly planned on the principles of evidence-based medicine, are needed.
Moreover, the published results have significant limitations. First of all, this refers to the assessment of the depressive component. As already mentioned, the diagnostic criteria for depression offered by official classifications are very vague. Many studies use the Hamilton Depression Scale (HAM-D) to assess the level of depression, although it has been proven [7] that it has little specificity for detecting and assessing depression in patients with schizophrenia, since its indicators correlate with a negative symptom complex. In addition, attention is not always paid to at what stage of the disease an antidepressant is prescribed. And quite rarely, the psychopathological structure of depression is analyzed in detail, which can significantly affect both the course of the disease and the therapeutic prognosis [5, 10]. Thus, for a more informed decision on the advisability of using antidepressants in this aspect, additional studies, methodically clearly planned on the principles of evidence-based medicine, are needed.
Of great interest is the point of view of practitioners on the problem under discussion, since the combination of antidepressants and antipsychotics is a fairly common variant of pharmacotherapy in psychiatric practice - in 41.5% of all courses of psychopharmacotherapy. It was found [1] that in paroxysmal schizophrenia, combined treatment with antidepressants and antipsychotics is prescribed in 50.6% of all courses of treatment, monotherapy with antipsychotics - in 41.4% and antidepressants - in 2.3%. It also turned out [9] that 70-80% of inpatients and 30-40% of outpatients with schizophrenia receive antidepressants, while antidepressants are widely prescribed for an acute attack of the disease. In this regard, the data of D. Addington et al. are also of interest. [12], who interviewed more than 3,000 psychiatrists from the US, Canada, Australia, and Europe. Their results showed that antidepressants in combination with antipsychotics are prescribed by 33% of inpatients and 36% of outpatients with schizophrenia.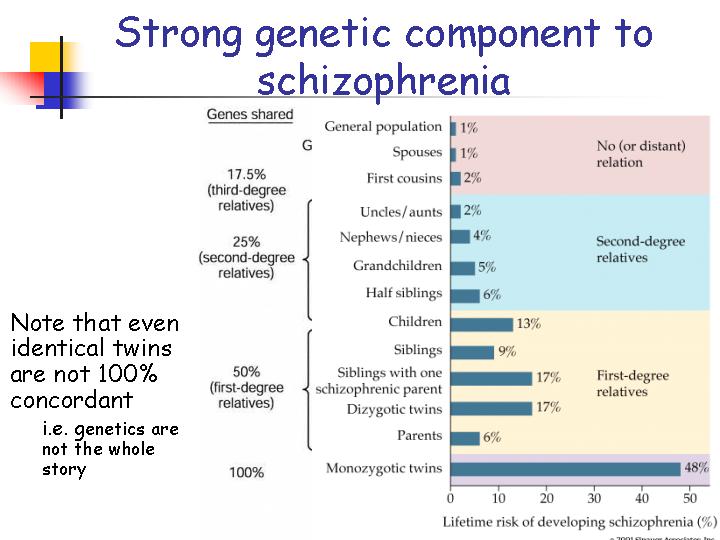 At the same time, the addition of antidepressants as the method of first choice is considered by 58% of doctors in the treatment of depression in the structure of an acute attack, 54% - postpsychotic depression and 73% - depression in patients with stable chronic schizophrenia. According to the majority of interviewed physicians, the main clinical symptoms that necessitate the prescription of antidepressants are suicidal thoughts, a sharply lowered mood, a feeling of hopelessness, anhedonia, sleep disturbances, especially early awakenings, and ideas of guilt. At the same time, 33% of respondents indicated that they rarely or never use antidepressants in patients with schizophrenia because of the risk of increased severity of productive symptoms. In 2009A similar survey was conducted by G.E. Mazo and S.E. Gorbachev [6]. According to a survey of 591 physicians, nearly half (47%) of all patients with schizophrenia are prescribed combination therapy with an antipsychotic and an antidepressant.
At the same time, the addition of antidepressants as the method of first choice is considered by 58% of doctors in the treatment of depression in the structure of an acute attack, 54% - postpsychotic depression and 73% - depression in patients with stable chronic schizophrenia. According to the majority of interviewed physicians, the main clinical symptoms that necessitate the prescription of antidepressants are suicidal thoughts, a sharply lowered mood, a feeling of hopelessness, anhedonia, sleep disturbances, especially early awakenings, and ideas of guilt. At the same time, 33% of respondents indicated that they rarely or never use antidepressants in patients with schizophrenia because of the risk of increased severity of productive symptoms. In 2009A similar survey was conducted by G.E. Mazo and S.E. Gorbachev [6]. According to a survey of 591 physicians, nearly half (47%) of all patients with schizophrenia are prescribed combination therapy with an antipsychotic and an antidepressant. The absolute majority (98%) of respondents indicated that the development of depressive disorders is an indication for changing therapy, and 73% of respondents consider it acceptable to use antidepressants in the acute period of an attack of schizophrenia. Suicidal ideation has been identified as the main indication for prescribing antidepressants (90%), depressed mood (86%), melancholy (83%), anxiety (70%), anhedonia to a lesser extent (50%), early awakenings (41%). The main factors limiting the use of antidepressants in patients with schizophrenia, 56% of respondents indicated the risk of pharmacokinetic interactions, 47% - the possibility of exacerbation of psychotic symptoms, 24% - the risk of suicidal tendencies. At the same time, 20% of respondents did not find significant restrictions on the use of antidepressants. A detailed assessment of the risk of exacerbation of acute psychotic symptoms as a result of the prescription of antidepressants was also carried out. Only 2% rate this risk as high, 34% as medium.
The absolute majority (98%) of respondents indicated that the development of depressive disorders is an indication for changing therapy, and 73% of respondents consider it acceptable to use antidepressants in the acute period of an attack of schizophrenia. Suicidal ideation has been identified as the main indication for prescribing antidepressants (90%), depressed mood (86%), melancholy (83%), anxiety (70%), anhedonia to a lesser extent (50%), early awakenings (41%). The main factors limiting the use of antidepressants in patients with schizophrenia, 56% of respondents indicated the risk of pharmacokinetic interactions, 47% - the possibility of exacerbation of psychotic symptoms, 24% - the risk of suicidal tendencies. At the same time, 20% of respondents did not find significant restrictions on the use of antidepressants. A detailed assessment of the risk of exacerbation of acute psychotic symptoms as a result of the prescription of antidepressants was also carried out. Only 2% rate this risk as high, 34% as medium. More than half (55%) consider the likelihood of such an exacerbation insignificant, and 9% - do not believe at all that the appointment of antidepressants can lead to an exacerbation of psychosis.
More than half (55%) consider the likelihood of such an exacerbation insignificant, and 9% - do not believe at all that the appointment of antidepressants can lead to an exacerbation of psychosis.
It can be seen from the data presented in the review that the discussion in the scientific community, the ambiguity and inconsistency of many provisions regarding depression in schizophrenia reflect the picture that has developed in practical public health. Despite the fact that much attention has been paid in the scientific literature to justify the limitations of the use of antidepressants in patients with schizophrenia, for practitioners, the addition of antidepressants to antipsychotics in the treatment of patients with schizophrenia with depression has become almost the main strategy of therapy. Moreover, this approach is used by most doctors, regardless of the standards of therapy existing in different countries. And although the choice of practitioners cannot be assessed from the standpoint of evidence-based medicine, it is confirmed by daily clinical observations.