Ptsd social anxiety
The Connection I Psych Central
PTSD and social anxiety are sometimes connected, but with the right support, you can manage the symptoms of both.
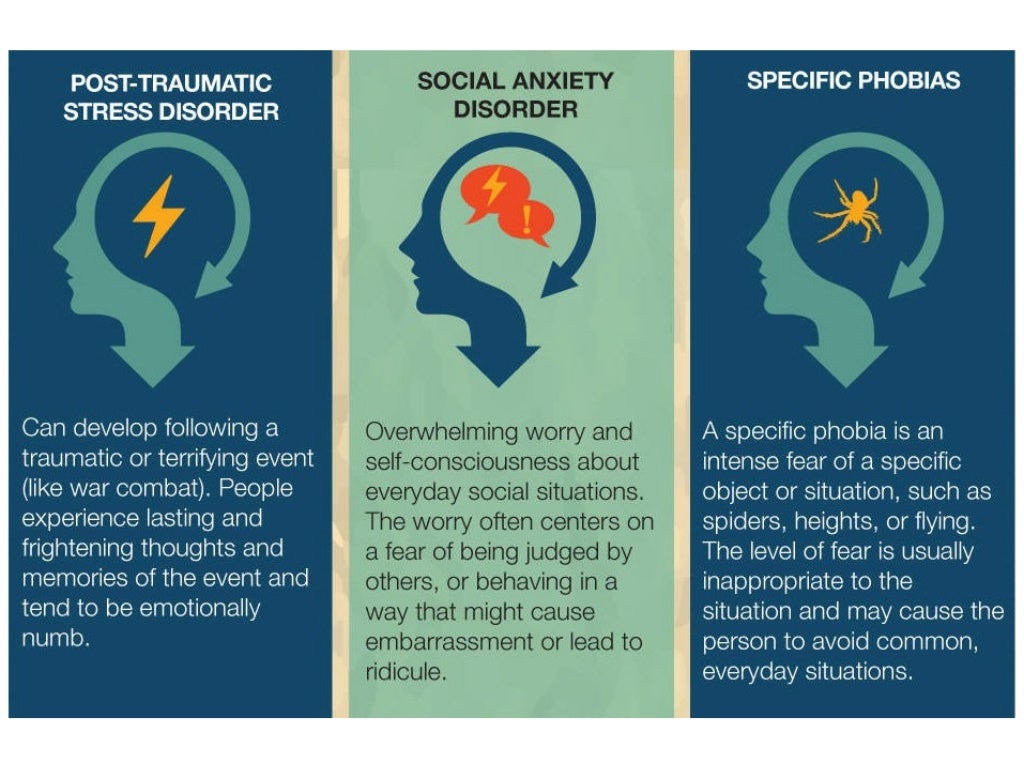
If you’ve experienced trauma that’s led to post-traumatic stress disorder (PTSD), you may already have anxiety. If you also live with social anxiety disorder, this may increase the number of situations that cause you stress.
Anxiety and the aftereffects of trauma are often connected but there are treatments and tips to manage both.
There are a few ways that social anxiety disorder and post-traumatic stress disorder (PTSD) are connected.
People with PTSD might:
- feel different because of PTSD, so they avoid social situations
- experience socially isolating shame or guilt stemming from PTSD
- live with depression from PTSD, which makes it difficult to maintain a social life
People with social anxiety may have a higher chance of experiencing PTSD because of social trauma, which according to research from 2020, can involve fear of humiliation and rejection in social situations.
Social trauma: Is it real?
There is an ongoing debate about what constitutes a social trauma and whether it meets the criteria for PTSD as outlined by the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text-revision (DSM-R-TR).
The criteria for PTSD include having experienced a trauma that poses a threat of death, injury, or sexual violence. Some may argue that a fear of rejection or humiliation doesn’t carry the same threat.
While it’s clear that these types of experiences may be more likely to lead to symptoms of PTSD, it’s crucial to consider that it’s not the event itself but a person’s perception of the event that can lead to a sense of constant threat.
It’s crucial for mental health professionals to consider a different approach to understanding what makes an experience traumatic and what may lead to symptoms of PTSD.
Taking into account each person’s unique experience can help understand the different types of threats that may play a role in PTSD, including social traumas.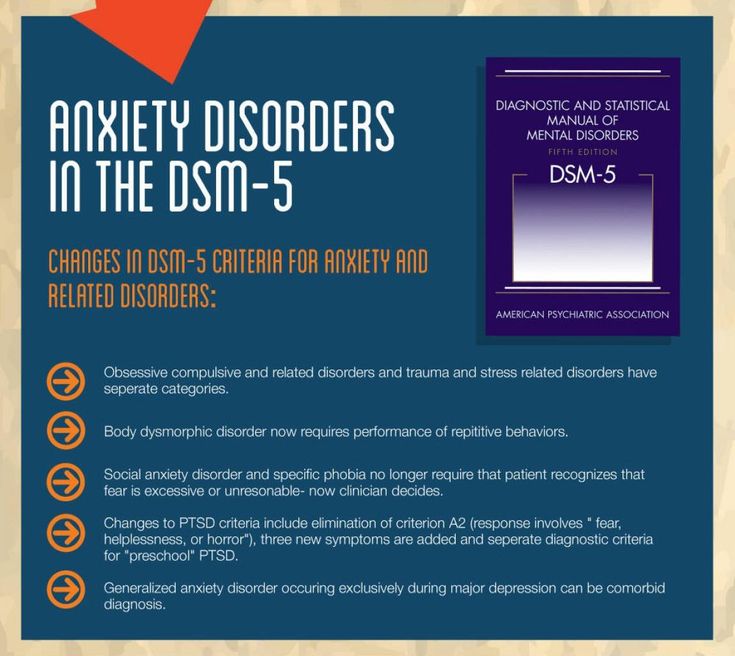
If you’re experiencing symptoms of PTSD because of a social trauma, know that whatever you’re feeling is real and valid.
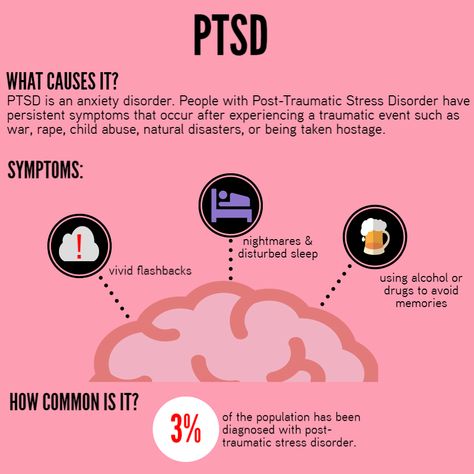
Anyone can experience PTSD. It can occur if your nervous system doesn’t fully reset after trauma.
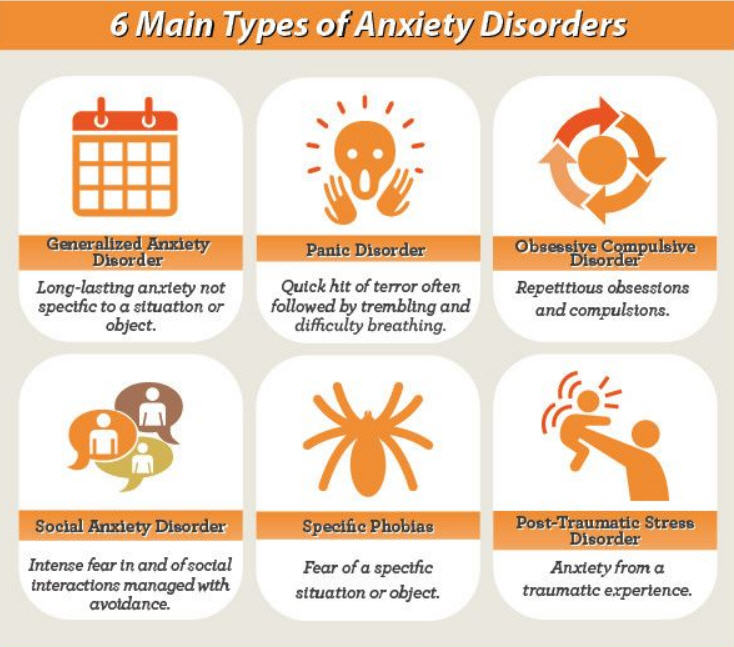
The effects of PTSD fall into four categories:
- Intrusion. Flashbacks, memories, and dreams are examples of these involuntary experiences.
- Avoidance. You may not want to think or talk about the trauma you’ve experienced and may avoid places, people, and other reminders.
- Mood and cognition changes. Distorted thoughts are an example, including wrongly blaming yourself for the trauma.
- Reactivity changes. You might feel irritable or behave recklessly.
The types of traumas that can cause PTSD includes:
- a serious accident
- the threat of death
- significant injury
- sexual violence
- a natural disaster
- war, combat, or terrorism
PTSD can also result from repeated exposure to the trauma of others, as experienced by a police officer or first responder.
According to the American Psychiatric Association (APA), PTSD affects around 3.5% of adults in the United States each year.
Social anxiety disorder affects an estimated 12.1% of adults in the United States, according to the National Institute of Mental Health.
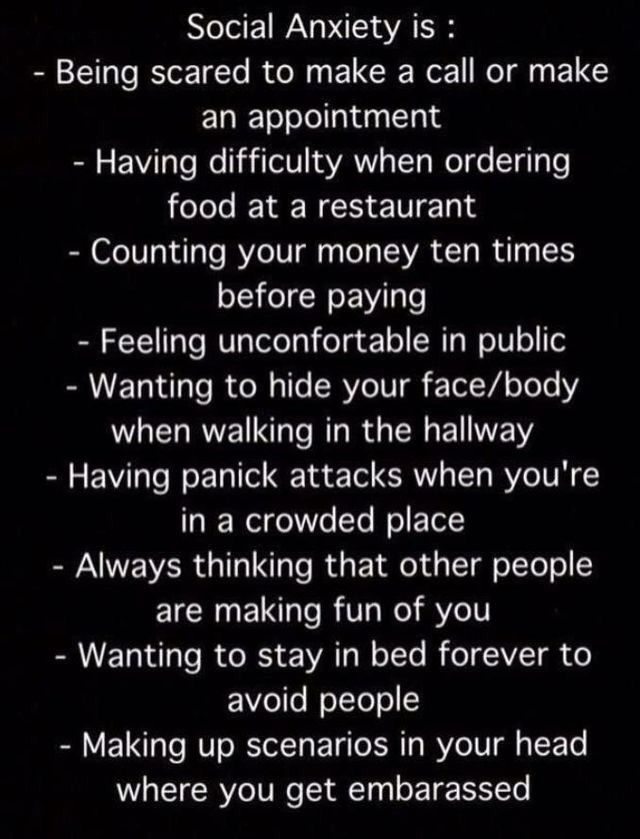
People with social anxiety disorder experience stress in social situations, including a fear of being judged or humiliated.
Social anxiety can cause physical symptoms such as a racing heart and interfere with your ability to speak or interact with others. Some people with social anxiety disorder may have trouble going to work or school.
According to research from 2019, an estimated 3.2% to 16% of people living with social anxiety disorder also experience PTSD. If a person’s primary diagnosis is PTSD, the co-occurrence of social anxiety disorder increases to about 43%.
A 2020 study found that social anxiety disorder, formerly known as social phobia, was second only to depressive disorders as the most common co-occurring diagnosis with PTSD.
People living with PTSD can feel a high amount of social stress, and certain social situations might trigger PTSD. You might find yourself in a continuous state of hypervigilance because your sympathetic (fight, flight, or freeze response) nervous system expects more threatening situations.
This can make social situations anxiety provoking.
If you have a primary diagnosis of social anxiety disorder, you may experience social trauma differently than other people. You may develop PTSD because of social trauma.
Ordinarily, the criteria for a PTSD diagnosis include having experienced a trauma that poses the threat of death, injury, or sexual violence. But people with social anxiety disorder may have a lower threshold for trauma when it’s social in nature.
For people with pre-existing social anxiety, this type of experience can be particularly upsetting.
A 2020 study involving people living with social anxiety disorder, obsessive-compulsive disorder (OCD), and a control group with no psychiatric diagnoses found that one-third of those with social anxiety disorder met the criteria for PTSD because of social trauma.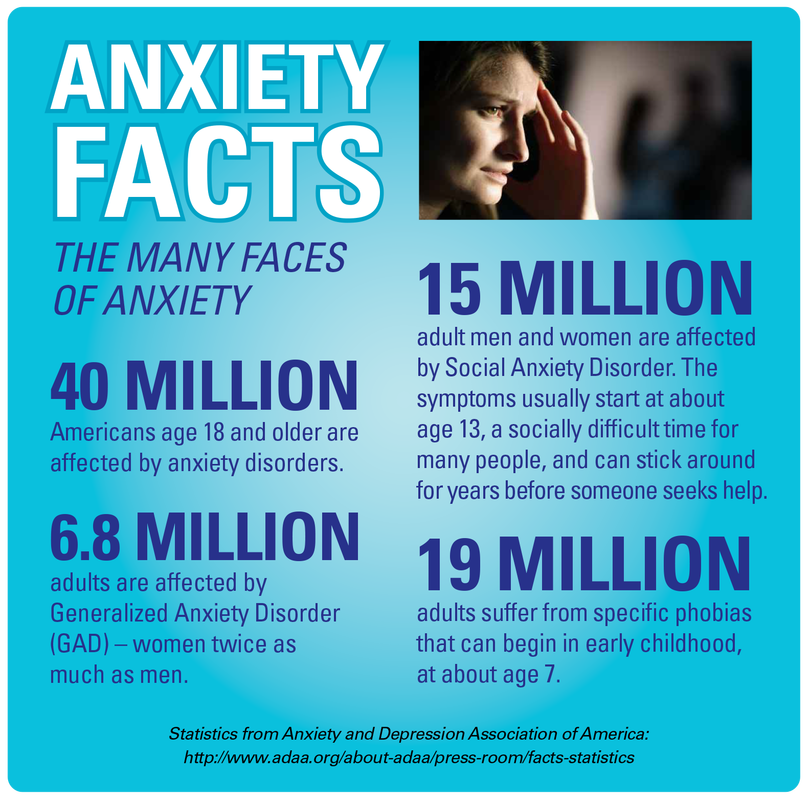
None of the people with OCD or the control group experienced clinically significant PTSD traits from their social trauma.
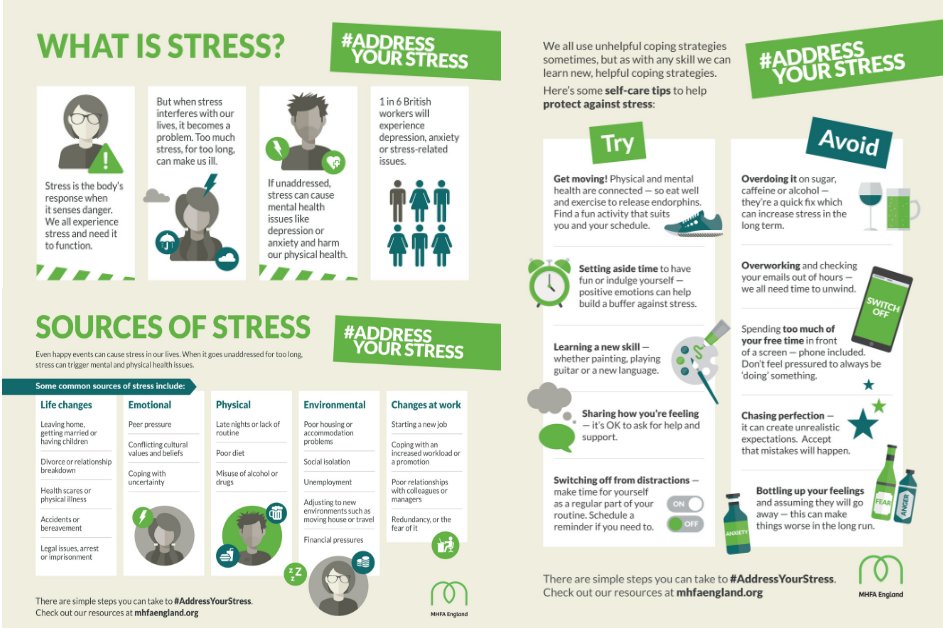
There are other strategies you can try to help manage your symptoms.
In the moment
Both PTSD and social anxiety can undermine your feeling of being in control. It can help to have ways of quickly regaining your sense of security.
- Name your feeling. If you’re caught off guard by an anxiety or PTSD response such as dizziness or an upset stomach, naming it as a trigger reaction can help the unpleasant feeling pass more easily.
- Breathe. Focusing on slowing and deepening your breathing is an effective anxiety-management tool.
- Connect to your surroundings. Turning your attention to sensory input can be calming. Try naming and counting a few things you can hear, see, smell, feel, and taste.
- Distract yourself. Using humor, calming music, or a simple activity can take your mind off your anxious feelings.
It also helps to know your triggers, so you can manage how often you encounter them.
Lifestyle
Another way to manage PTSD and social anxiety is to assess and adjust your lifestyle. It’s OK to focus on one area at a time as you build new habits such as:
- regular exercise
- improved nutrition
- restorative sleep
- enjoyable leisure activities
- positive social contact
Mindfulness
If you haven’t yet tried it, consider exploring a mindfulness practice. There’s evidence pointing to its effectiveness for both PTSD and anxiety.
A 2022 review found that mindfulness reduced PTSD symptoms. For social anxiety disorder, a 2021 review found that mindfulness-based interventions helped to reduce symptoms, and the effects lasted for 12 months.
Both PTSD and social anxiety can make it difficult to interact with other people in certain situations. You may have a harder time at work or school, or even during shorter public encounters such as a trip to the grocery store.
But there are treatment options that can help manage your symptoms.
Keep in mind that if a therapy or medication isn’t working for you, there are other options. Communicating regularly with a healthcare or mental health professional can help, particularly if you want to change your treatment direction.
If you’re unsure where to start, you can check out Psych Central’s hub on finding mental health support.
The Connection I Psych Central
PTSD and social anxiety are sometimes connected, but with the right support, you can manage the symptoms of both.
If you’ve experienced trauma that’s led to post-traumatic stress disorder (PTSD), you may already have anxiety. If you also live with social anxiety disorder, this may increase the number of situations that cause you stress.
Anxiety and the aftereffects of trauma are often connected but there are treatments and tips to manage both.
There are a few ways that social anxiety disorder and post-traumatic stress disorder (PTSD) are connected.
People with PTSD might:
- feel different because of PTSD, so they avoid social situations
- experience socially isolating shame or guilt stemming from PTSD
- live with depression from PTSD, which makes it difficult to maintain a social life
People with social anxiety may have a higher chance of experiencing PTSD because of social trauma, which according to research from 2020, can involve fear of humiliation and rejection in social situations.
Social trauma: Is it real?
There is an ongoing debate about what constitutes a social trauma and whether it meets the criteria for PTSD as outlined by the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, text-revision (DSM-R-TR).
The criteria for PTSD include having experienced a trauma that poses a threat of death, injury, or sexual violence. Some may argue that a fear of rejection or humiliation doesn’t carry the same threat.
While it’s clear that these types of experiences may be more likely to lead to symptoms of PTSD, it’s crucial to consider that it’s not the event itself but a person’s perception of the event that can lead to a sense of constant threat.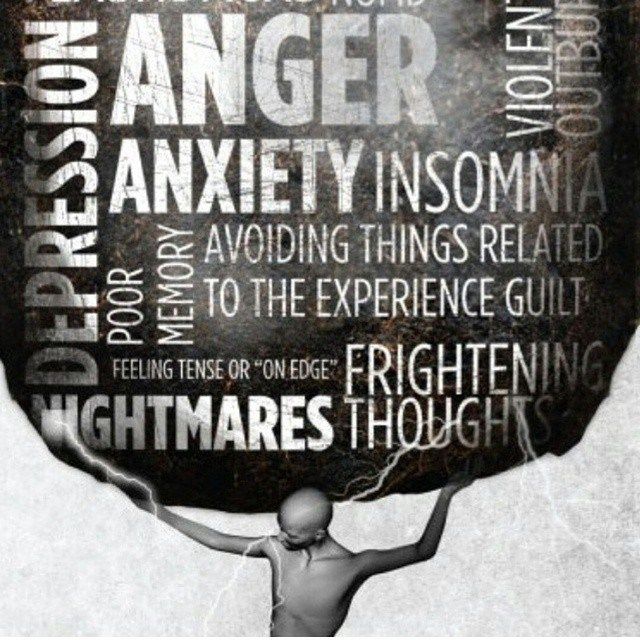
It’s crucial for mental health professionals to consider a different approach to understanding what makes an experience traumatic and what may lead to symptoms of PTSD.
Taking into account each person’s unique experience can help understand the different types of threats that may play a role in PTSD, including social traumas.
If you’re experiencing symptoms of PTSD because of a social trauma, know that whatever you’re feeling is real and valid.
Anyone can experience PTSD. It can occur if your nervous system doesn’t fully reset after trauma.
The effects of PTSD fall into four categories:
- Intrusion. Flashbacks, memories, and dreams are examples of these involuntary experiences.
- Avoidance. You may not want to think or talk about the trauma you’ve experienced and may avoid places, people, and other reminders.
- Mood and cognition changes. Distorted thoughts are an example, including wrongly blaming yourself for the trauma.
- Reactivity changes. You might feel irritable or behave recklessly.
The types of traumas that can cause PTSD includes:
- a serious accident
- the threat of death
- significant injury
- sexual violence
- a natural disaster
- war, combat, or terrorism
PTSD can also result from repeated exposure to the trauma of others, as experienced by a police officer or first responder.
According to the American Psychiatric Association (APA), PTSD affects around 3.5% of adults in the United States each year.
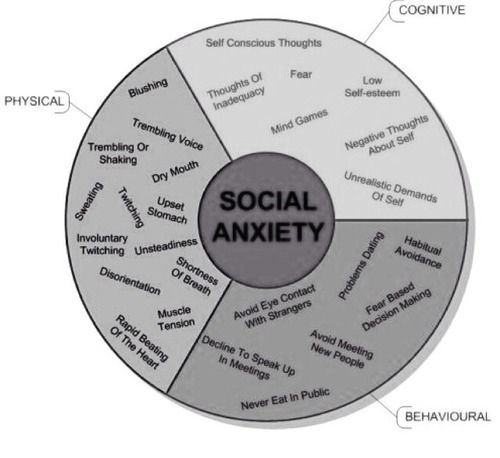
Social anxiety disorder affects an estimated 12.1% of adults in the United States, according to the National Institute of Mental Health.
People with social anxiety disorder experience stress in social situations, including a fear of being judged or humiliated.
Social anxiety can cause physical symptoms such as a racing heart and interfere with your ability to speak or interact with others.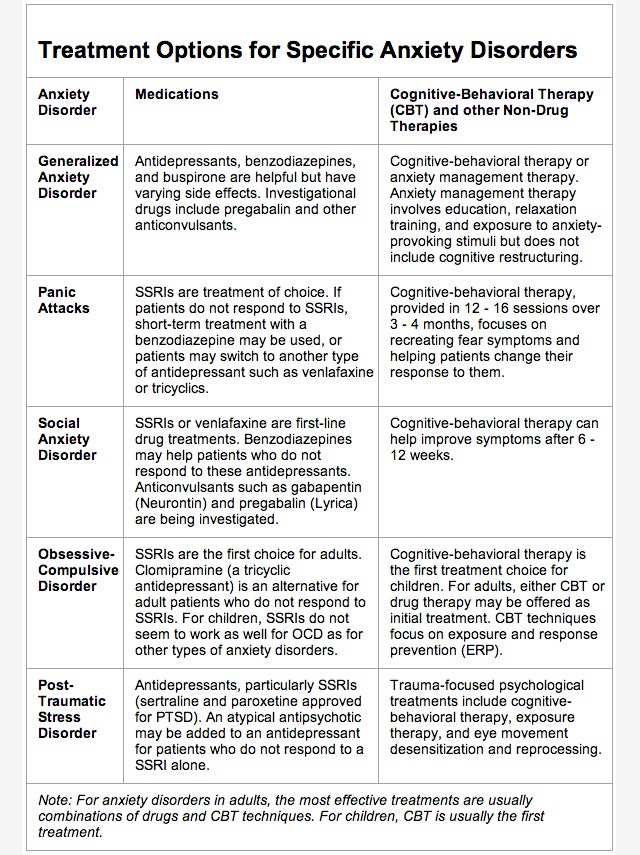 Some people with social anxiety disorder may have trouble going to work or school.
Some people with social anxiety disorder may have trouble going to work or school.
According to research from 2019, an estimated 3.2% to 16% of people living with social anxiety disorder also experience PTSD. If a person’s primary diagnosis is PTSD, the co-occurrence of social anxiety disorder increases to about 43%.
A 2020 study found that social anxiety disorder, formerly known as social phobia, was second only to depressive disorders as the most common co-occurring diagnosis with PTSD.
People living with PTSD can feel a high amount of social stress, and certain social situations might trigger PTSD. You might find yourself in a continuous state of hypervigilance because your sympathetic (fight, flight, or freeze response) nervous system expects more threatening situations.
This can make social situations anxiety provoking.
If you have a primary diagnosis of social anxiety disorder, you may experience social trauma differently than other people. You may develop PTSD because of social trauma.
Ordinarily, the criteria for a PTSD diagnosis include having experienced a trauma that poses the threat of death, injury, or sexual violence. But people with social anxiety disorder may have a lower threshold for trauma when it’s social in nature.
For people with pre-existing social anxiety, this type of experience can be particularly upsetting.
A 2020 study involving people living with social anxiety disorder, obsessive-compulsive disorder (OCD), and a control group with no psychiatric diagnoses found that one-third of those with social anxiety disorder met the criteria for PTSD because of social trauma.
None of the people with OCD or the control group experienced clinically significant PTSD traits from their social trauma.
There are other strategies you can try to help manage your symptoms.
In the moment
Both PTSD and social anxiety can undermine your feeling of being in control. It can help to have ways of quickly regaining your sense of security.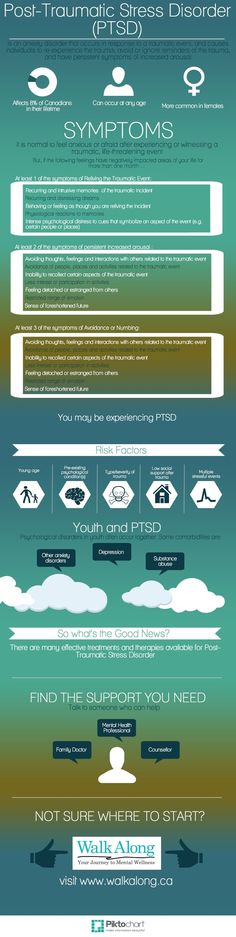
- Name your feeling. If you’re caught off guard by an anxiety or PTSD response such as dizziness or an upset stomach, naming it as a trigger reaction can help the unpleasant feeling pass more easily.
- Breathe. Focusing on slowing and deepening your breathing is an effective anxiety-management tool.
- Connect to your surroundings. Turning your attention to sensory input can be calming. Try naming and counting a few things you can hear, see, smell, feel, and taste.
- Distract yourself. Using humor, calming music, or a simple activity can take your mind off your anxious feelings.
It also helps to know your triggers, so you can manage how often you encounter them.
Lifestyle
Another way to manage PTSD and social anxiety is to assess and adjust your lifestyle. It’s OK to focus on one area at a time as you build new habits such as:
- regular exercise
- improved nutrition
- restorative sleep
- enjoyable leisure activities
- positive social contact
Mindfulness
If you haven’t yet tried it, consider exploring a mindfulness practice. There’s evidence pointing to its effectiveness for both PTSD and anxiety.
There’s evidence pointing to its effectiveness for both PTSD and anxiety.
A 2022 review found that mindfulness reduced PTSD symptoms. For social anxiety disorder, a 2021 review found that mindfulness-based interventions helped to reduce symptoms, and the effects lasted for 12 months.
Both PTSD and social anxiety can make it difficult to interact with other people in certain situations. You may have a harder time at work or school, or even during shorter public encounters such as a trip to the grocery store.
But there are treatment options that can help manage your symptoms.
Keep in mind that if a therapy or medication isn’t working for you, there are other options. Communicating regularly with a healthcare or mental health professional can help, particularly if you want to change your treatment direction.
If you’re unsure where to start, you can check out Psych Central’s hub on finding mental health support.
Some features of post-traumatic stress disorder in modern conditions //Psychological newspaper
The events of the last 3 years in the history of Russia have greatly increased the demand for practical psychology and psychotherapy. The pandemic and the special military operation to protect the DPR and LPR have in many cases caused post-traumatic stress disorder.
The pandemic and the special military operation to protect the DPR and LPR have in many cases caused post-traumatic stress disorder.
In Russia, the phenomenon of military neurosis (the modern name of post-traumatic stress disorder - PTSD) has been known since at least the Russo-Japanese War (1904-1905), when more than 3,000 soldiers passed through the Harbin hospital, who did not have physical injuries, but who were clearly mentally ill. Somewhat later, in 1914, Russian psychiatrist N.N. Bazhenov described "horror affects" in the victims of the earthquake in Messina in 1908 (Italy), which included shock reactions (stunning, indifference to one's own life and the lives of loved ones, etc.). After the end of the Second World War, in the article "Psychogenies of Wartime" (1948), a domestic psychiatrist E.K. Krasnushkin wrote: “The mental impact on a person during the war acquires an unusual severity for peaceful conditions ... the psychogenic factor in a large group of diseases became the leading one and was the cause of the disease .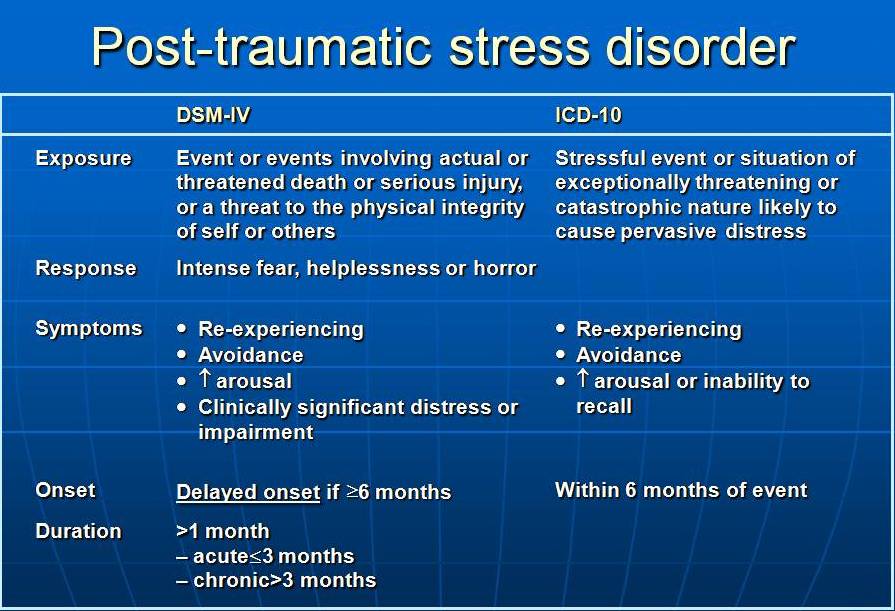 .. psychotrauma leads to organic changes in the body” (quoted from [3]).
.. psychotrauma leads to organic changes in the body” (quoted from [3]).
In the USSR in the 1980s, a significant number of various psycho-traumatic events occurred, including man-made ones (the accident at the Chernobyl nuclear power plant, 1986; the railway accident near Ufa, 1989), natural (the Spitak earthquake, 1988), military (the Afghan war, 1979-1989) and interethnic-conflict nature (Armenian-Azerbaijani clashes in Nagorno-Karabakh, 1988; Fergana pogroms, 1989). This stimulated the development of the problems of post-stress disorders in our country, including their medical and biological components, clinics and methods of treatment, as well as psychological and psychiatric correlates of PTSD. Psychological studies of that time were focused on studying the consequences of hostilities on the “Afghan” military personnel who took part in them, the psychophysiological and psychological characteristics of the victims of natural and environmental disasters. nine0003
The catastrophic socio-economic and political consequences of Gorbachev's "perestroika" for the country gave scientists and practitioners a lot of material to work with (including aviation, natural disasters and events involving the use of weapons, such as the constitutional crisis of 1993 and two wars in Chechnya). There is a laboratory at the Institute of Psychology of the Russian Academy of Sciences that studies the psychological characteristics of stress (its current name is the laboratory for the psychology of the development of the subject in normal and post-traumatic states), and many studies of this kind have been and are being conducted in it. Psychological studies of this period were associated with the study of socio-psychological work with participants in extreme events, psychocorrection and psychotherapy of post-stress disorders, personality traits in extreme conditions. nine0003
There is a laboratory at the Institute of Psychology of the Russian Academy of Sciences that studies the psychological characteristics of stress (its current name is the laboratory for the psychology of the development of the subject in normal and post-traumatic states), and many studies of this kind have been and are being conducted in it. Psychological studies of this period were associated with the study of socio-psychological work with participants in extreme events, psychocorrection and psychotherapy of post-stress disorders, personality traits in extreme conditions. nine0003
A new wave of PTSD research is linked to the COVID-19 pandemic and patients who have ended up in intensive care. As studies show, they developed severe post-traumatic stress disorder, which is usually fixed after participating in hostilities (Boiko O.M., Medvedeva T.I., Enikolopov S.N., Vorontsova O.Yu., Kazmina O.Yu. ., 2020; Kozlov V.V., 2021, 2022; Vasil'eva A.V., 2020; Tkhostov A.Sh., Rasskazova E. I., 2020; Sorokin M.Yu., Kasyanov E.D., Rukavishnikov G .V., Makarevich O.V., Neznanov N.G., Lutova N.B., Mazo G.E., 2020 and others). nine0003
I., 2020; Sorokin M.Yu., Kasyanov E.D., Rukavishnikov G .V., Makarevich O.V., Neznanov N.G., Lutova N.B., Mazo G.E., 2020 and others). nine0003
As far as we can imagine, in the recent history of the psychology of PTSD, studies carried out during special military operations in conflict zones will play a role.
Usually, PTSD occurs during events that have a super-powerful negative destructive effect on the mental state of the individual. Sometimes PTSD occurs in cases where the situation in itself is not extraordinary, but for various subjective reasons it can be a serious psychological trauma for a particular person, that is, the cause of PTSD in many respects relates to the individual psychological characteristics of the individual and special sensitivity to certain qualities of life situations. nine0019 The main determinant of the event's trauma is the feeling-experience of one's own helplessness and worthlessness, that a person cannot cope with the situation, cannot overcome the challenge of a life situation, is not able to effectively and adequately respond to what is happening.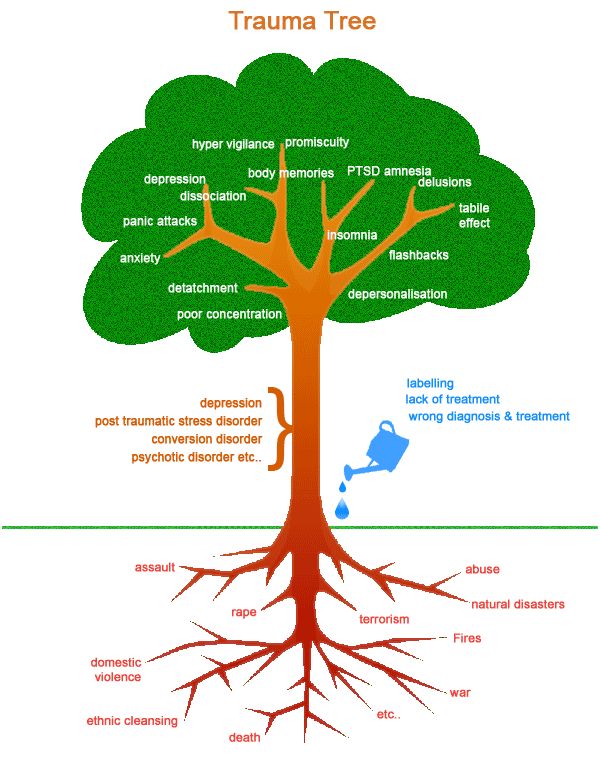
As our research shows, PTSD is always associated with an individual inability to integrate the intensity or content of an acute crisis situation. At the same time, the external characteristics of the crisis may differ from each other, trigger mechanisms may have a different character, and reactions to crisis situations will be specific to each person. Therefore, to understand the crisis, it is important to know the psychological mechanisms of its occurrence, its inner essence [6]. nine0003
PTSD is considered mainly from the point of view of the destructive impact on a person, as a negative disintegration of the personality. In integrative psychology since the 1990s, stress, PTSD, psychological trauma, and crises are considered from the point of view of a person's positive integration of the resource components of the experience of experiencing difficult events and upheavals. In our opinion, extreme events can initiate personal growth, self-knowledge, self-regulation, spiritual self-improvement, improvement of behavioral strategies, social maturity and responsibility, awakening the essential powers of a person and true existential meanings and values. nine0003
nine0003
In the shock crisis of PTSD, a sudden cataclysm in the social environment (unexpected death of a spouse or violence, loss of integral status or significant social status) can cause a strong emotional reaction that suppresses the adaptive mechanisms of the individual. The same kind of effect can be achieved in the material "I" - a sudden incurable disease or suspicion of it, clinical death or the threat of death, the presence of an objective danger to life and health, the loss of a significant fragment of a bodily structure or function, a personally significant material value - bankruptcy, natural disaster, robbery. Psycho-spiritual experiences of shock intensity are possible, which completely devalue the material and social "I", the basic values and meanings of life. Since the event occurs suddenly, unexpectedly, and the person usually does not have time to prepare for a terrible blow, he can fall into an emotional shock and experience the entire phenomenology of PTSD due to the extraordinary nature of the conditions. nine0003
nine0003
PTSD is an extreme challenge for the individual, associated with an extraordinary abrupt departure from the norm of habitual actions and operations and the experience of shock.
PTSD is always a significant loss when an extreme life situation destroys significant elements of the personality structure and functionality.
- The state of shock develops immediately after PTSD and lasts from several days to a month, coexisting with signs of the next stage - experiences. A person is not aware of the loss, is not able to comprehend what happened, what is happening is perceived as in a fog or in a dream. Then comes disbelief that this could happen. Psychological defenses are repression and denial. Their involvement is natural and beneficial as it helps the person gradually come to terms with what has happened. Towards the end of the shock stage after psychic anesthesia, suffering begins, indicating the beginning of the experience, that is, the “work of grief”.
 The coming completion is indicated by elements of understanding and recognition of the loss, as well as the circumstances under which it occurred. nine0038
The coming completion is indicated by elements of understanding and recognition of the loss, as well as the circumstances under which it occurred. nine0038 - In the state of experiencing , which is the most intense in the process of grief, the understanding and recognition of the loss reaches the degree of clarity of the fact. Ritual acts and other specific events play an important role in this. Suffering usually reaches its greatest strength and is distinguished by a variety of manifestations. Awareness leads a person to the gaping emptiness that arose after the loss, and the need to get used to it. Attempts to fill it are expressed in repeated returns and stories about the circumstances of the loss. Then the person goes further and further, there are diverse memories of the loss, of the past. They not only contribute to the understanding of the loss, but also lead to idealization and identification with the departed through the involvement of repression mechanisms. However, passing into the past characterizes the beginning of acceptance and integration of the experience of loss.
 nine0038
nine0038 - Loss acceptance status (integration) . The "work of grief" at this time consists in overcoming mental suffering, ideas of self-blame, preoccupation with the image of loss and identification with it in order to return to reality. Acceptance of loss does not exclude the possibility that pangs of conscience and guilt can be long lasting. Gradually disappears hostile attitude towards others. Memories of the past are preserved, which significantly reduce emotional stress. The development of their new place in the world begins, and the energy switches to relationships and activities that are not related to loss. nine0038
In real life, the dynamics of the stages of grief are not linear, they are more like overlapping cycles.
Shock, experience, and acceptance do not follow strictly one after the other, although the sequence itself is typical and therefore predictable. Their manifestations often overlap. Since grief is an individual process, the characteristics of the stages can coexist in various combinations, creating unique opportunities for positive change.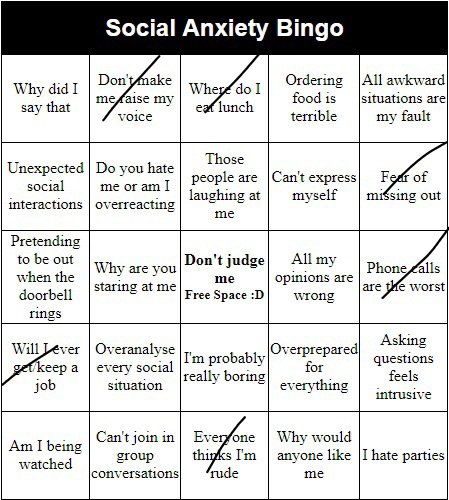 nine0003
nine0003
There are only 4 exits from the shock zone of PTSD.
1. Positive integration of with the transition to a new qualitative level of integrity of consciousness and personality, when there is a significant decrease in anxiety, depressive symptoms, anger or shame about what happened. The crisis state is an initiation into the nuclear semantic structure, leading to the introjection of new life values into the consciousness of the individual and, thus, becomes a real transformation of the individual. The crisis state is a test for compliance with the new situation in the material, social, spiritual "I", for compliance with new social requirements. A psychologically critical state requires the concentration of all forces together to solve the problems that are set before the individual. Positive integration occurs when a person has the strength and skills to organize activity to overcome the test, and also when he can and knows how to gather them into one whole at the moment against the background of social support. Positive integration requires skills of awareness, self-control, self-regulation. A person suffering from PTSD should gradually begin to use various conscious and subconscious coping strategies to reduce the intensity of post-traumatic symptoms. Of all these strategies, only problem-solving behavior is constructive and adaptive to positively integrate the experience of PTSD, which is always deprivation, frustration. PTSD is always a challenge for the individual. It is a test of rootedness, introjection of some important attitudes and values of the individual. nine0003
Positive integration requires skills of awareness, self-control, self-regulation. A person suffering from PTSD should gradually begin to use various conscious and subconscious coping strategies to reduce the intensity of post-traumatic symptoms. Of all these strategies, only problem-solving behavior is constructive and adaptive to positively integrate the experience of PTSD, which is always deprivation, frustration. PTSD is always a challenge for the individual. It is a test of rootedness, introjection of some important attitudes and values of the individual. nine0003
With the positive integration of the experience of PTSD, a person returns to trust in the world and people, self-confidence, optimism and a surge of energy, the ability to build projects for the future, interest in previous hobbies, work, interpersonal relationships. Memories of the event become significantly less traumatic and no longer cause intense fear, they are integrated into the life experience of the individual and are perceived as part of the past and a lesson, without interfering with enjoyment of life.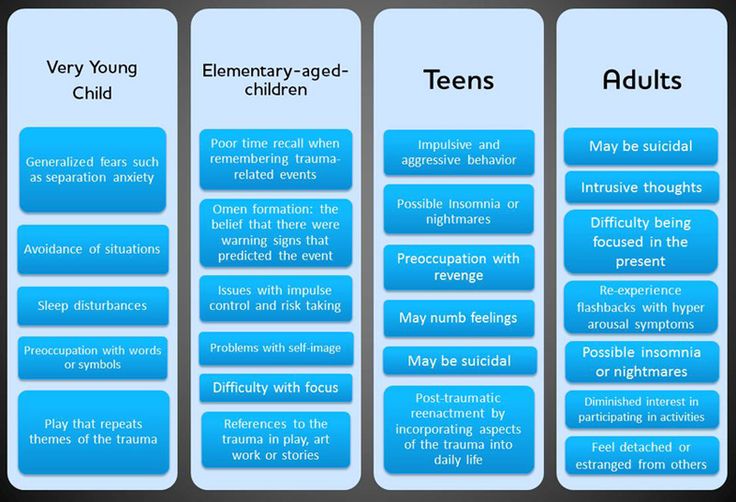
With negative disintegration, there is a decrease in intolerable tension due to neurotic or psychopathic patterns of behavior.
Anxious type of PTSD is characterized by symptoms of anxiety, irritability, internal tension, obsessive anxious thoughts about the traumatic situation and one's condition, sleep disorders (difficulty falling asleep). The patient often fears trauma-related nightmares and for this reason deliberately delays the onset of sleep. In the evening and at night, there may be feelings of lack of air, palpitations, sweating, chills, or hot flashes. Such patients strive for communication and some kind of purposeful activity, since they get relief from activity. nine0003
The asthenic type of PTSD is characterized by passivity, indifference to previously interested in life events, indifference to other people and to professional activities. The experience of loss of a sense of pleasure from life is characteristic. The mind is dominated by thoughts of one's own failure. Unlike the anxious type, in these cases, memories of a traumatic event are devoid of brightness, detail, and emotional coloring. There may be resentment and irritability. There is hypersomnia with the inability to get out of bed, painful drowsiness (sometimes throughout the day). nine0003
The mind is dominated by thoughts of one's own failure. Unlike the anxious type, in these cases, memories of a traumatic event are devoid of brightness, detail, and emotional coloring. There may be resentment and irritability. There is hypersomnia with the inability to get out of bed, painful drowsiness (sometimes throughout the day). nine0003
Dysphoric PTSD is characterized by the constant presence of discontent, irritation (up to outbursts of rage) against the background of a depressed and gloomy mood. The imagination is dominated by images of punishment of offenders and scenes of aggression with one's own participation in the role of the aggressor. Often patients are unable to control themselves and subsequently regret their aggressive reactions. Sometimes this forces them to minimize their contact with others. Outwardly, patients look gloomy, their behavior is distinguished by isolation, isolation, and reticence. Usually they do not seek help and come to the attention of specialists due to behavioral disorders that their environment draws attention to.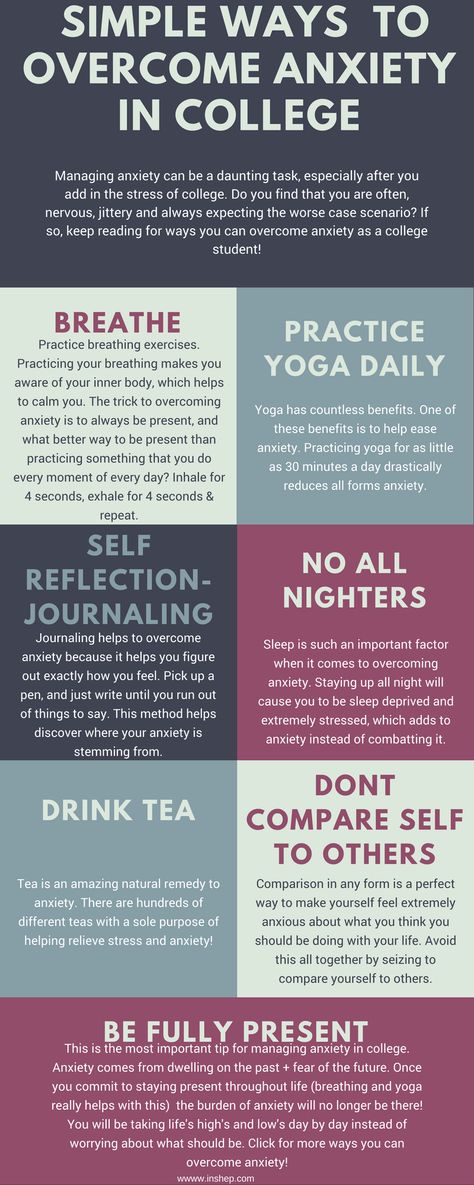 nine0003
nine0003
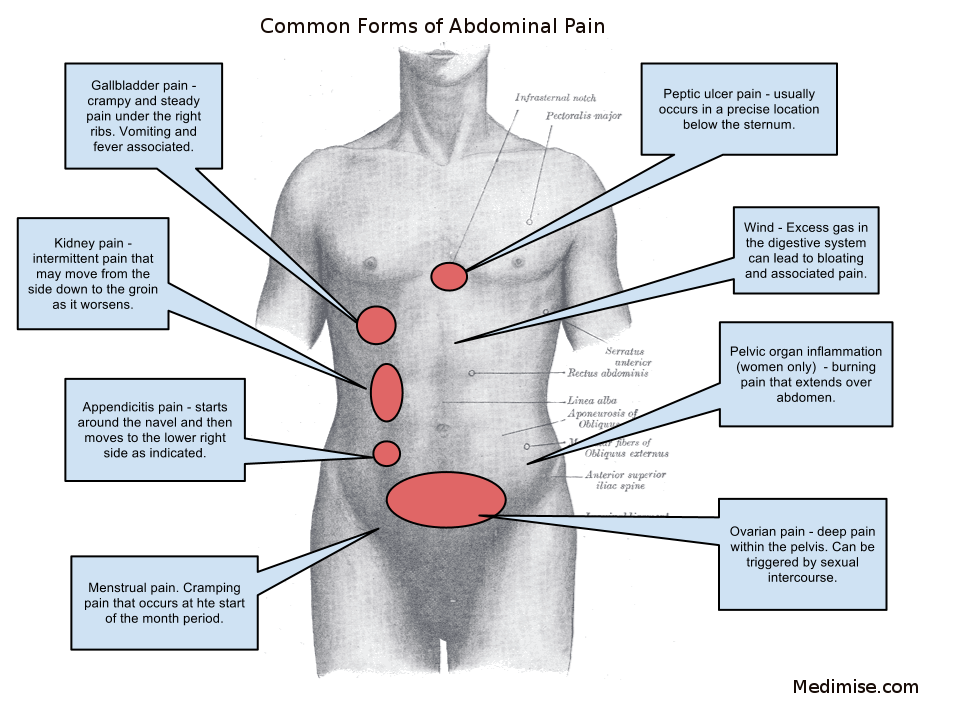
The somatoform type of PTSD is characterized by an abundance of somatoform disorders, while unpleasant sensations are localized mainly in the region of the heart (54%), gastrointestinal tract (36%) and head (20%), which is combined with psychovegetative paroxysms. Avoidance behavior is common in the context of panic attacks. The patient is primarily concerned with unpleasant bodily sensations. There is an anxious expectation of the onset of symptoms. This anxiety may be stronger than the fear of the traumatic event. nine0003
The hysterical type of PTSD manifests itself in the form of demonstrative behavior, the desire to attract attention, increased suggestibility and autosuggestibility.
The depressive type is characterized by low mood and pessimism.
In addition to the above types, there are variants of PTSD called "dissociative", "hypochondriac" and "mixed" [2].
The person may become withdrawn, secretive, suspicious, or depressed. A disturbed perception of an event can lead to undeserved reproaches by others for their failures. In some cases, tension reduction occurs by taking alcohol or medications. There may be suicide attempts or aggressive behavior. Negative psychopathological disintegration as an outcome of the PTSD crisis is completely optional, but sometimes happens due to the acuteness of individual problems and the lack of necessary social support. nine0003
A disturbed perception of an event can lead to undeserved reproaches by others for their failures. In some cases, tension reduction occurs by taking alcohol or medications. There may be suicide attempts or aggressive behavior. Negative psychopathological disintegration as an outcome of the PTSD crisis is completely optional, but sometimes happens due to the acuteness of individual problems and the lack of necessary social support. nine0003
3. Negative personality disintegration: social deviations.
Social deviations are a consequence of the PTSD crisis as a way of adaptation and rehabilitation to a new personality with acquired symptoms. At the same time, all the consequences of PTSD, except for mild forms, lead to social deviations. In socio-psychological terms, the consequences of PTSD cause phenomena that pose a real threat to the survival of the individual in a given social community, disruption of compliance with social and moral norms and cultural values, disruption of self-development and self-realization in the society to which a person belongs. From the point of view of clinical psychology, PTSD causes a deviation from the norms of interpersonal interactions accepted in a given society: actions, deeds, statements made both within the framework of mental health and in various forms of neuropsychiatric pathology, especially at the borderline level. nine0003
From the point of view of clinical psychology, PTSD causes a deviation from the norms of interpersonal interactions accepted in a given society: actions, deeds, statements made both within the framework of mental health and in various forms of neuropsychiatric pathology, especially at the borderline level. nine0003
In the context of deviant behavior, of particular interest are scientific works that examine PTSD experienced by police officers (participants in counter-terrorist operations), and studies devoted to the peculiarities of their transfer when returning from "hot spots" patterns of "unreacted aggression" to the practice of everyday service [4] .
Deviant behavior of a person as a result of PTSD does not correspond to generally accepted or officially established social norms and causes a negative assessment from other people (social sanctions). Deviant behavior, although it causes real damage to the personality itself, to the people around it, is associated with the general orientation of the personality to relieve the neuropsychic stress of PTSD. It is accompanied by the phenomena of social disadaptation and has a pronounced individual psychological originality. nine0003
It is accompanied by the phenomena of social disadaptation and has a pronounced individual psychological originality. nine0003
Of the whole huge list of deviant behavior, hooliganism, recklessness on the roads, criminality, alcoholism, drug addiction, substance abuse, gambling, terrorism, extremism, vandalism, self-harm are the main ones as a result of PTSD. At the same time, the basic motive of the individual is the desire to reduce the intensity of post-traumatic symptoms.
The consequence of PTSD is often irritability, outbursts of anger, fatigue and loss of interest in communication and various activities, social phobia and distrust of people. This leads to social exclusion and marginalization - to a break in relations with relatives and friends, to the breakup of the family, to the inability to make family and friends, problems in the professional sphere. nine0003
Aggression and antisocial behavior as a deviation in PTSD can be determined by playing the role of the aggressor by the victim of violence.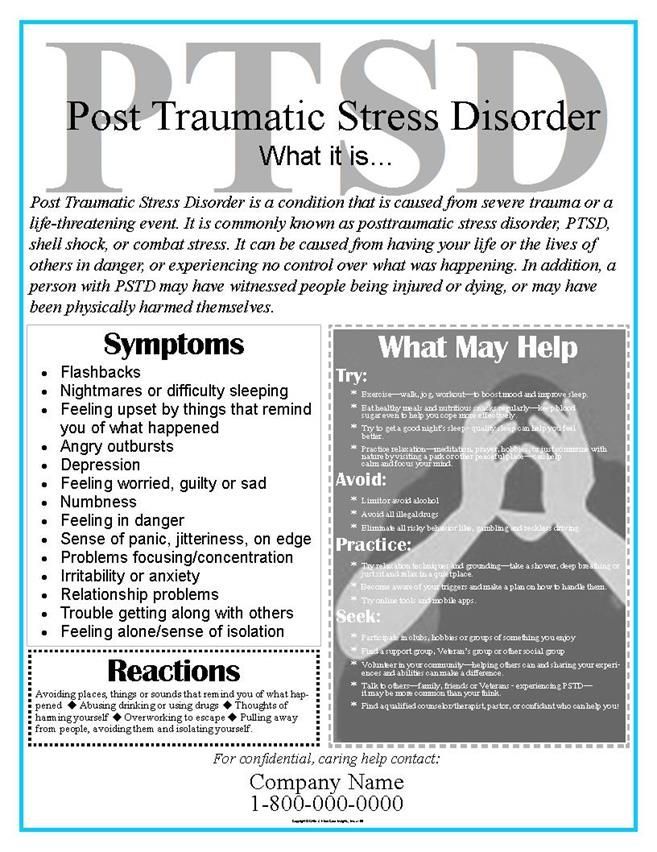 In this case, crime, terrorism, extremism, vandalism can become a consequence and a symptom.
In this case, crime, terrorism, extremism, vandalism can become a consequence and a symptom.
PTSD is always an intense and extreme experience that is associated with peak states of consciousness, the emotional experience of glee, a surge of energy, the extraordinaryness of fear, curiosity, terror, and drive. Physiologically, this phenomenon is due to the fact that at the time of injury, the brain releases endorphins - substances that reduce the feeling of pain and fear and even create a feeling of special pleasure and pleasure of a euphoric nature. A certain phenomenon of passionate attachment and a thirst for intense experience arises in a person, a desire to be in a situation of extreme danger, which temporarily brings him out of a state of fading in everyday reality and allows him to feel again at the peak of experiences. nine0003
Alcohol abuse is a consequence of PTSD. This dependence occurs in 52% of men and 28% of women suffering from PTSD. Among the deviations, alcoholism is the main cause of the marginalization of the individual (unemployment, poverty, homelessness, committing criminal behavior, hooliganism, etc. ). This is due, on the one hand, to the cultural prevalence of the phenomenon of alcohol consumption itself, and on the other hand, to social justification and tacit empathic support for the motive of coping with the symptoms of PTSD with the help of alcohol consumption by a person. nine0003
). This is due, on the one hand, to the cultural prevalence of the phenomenon of alcohol consumption itself, and on the other hand, to social justification and tacit empathic support for the motive of coping with the symptoms of PTSD with the help of alcohol consumption by a person. nine0003
Without a doubt, the deviations of substance abuse and drug addiction in PTSD do not find support in the social environment and are prosecuted as criminal behavior, at the same time, many people use the strategy of substance use as a way to reduce the intensity of post-traumatic symptoms.
It should be noted that the strategy of alcohol and substance use in PTSD is very destructive for the individual, and at the same time, the addiction syndrome develops much faster, and rehabilitation takes much longer and is much more difficult in the form of various deviations, addictions, affective, cognitive impairments. nine0003
4. Negative personality disintegration: death.
Death in PTSD has many faces. We can, as the extreme limit of the negative disintegration of personality, consider death as:
We can, as the extreme limit of the negative disintegration of personality, consider death as:
- social death;
- psychological death of a person;
- physical death.
Social death we consider as the destruction of the main statuses and roles of the individual, the isolation of the individual in the social day and the impossibility and impotence of reverse recovery. nine0003
The psychological death of a person is the most severe variant of the disintegration of a person, when he is completely unable to function normally. With psychological death, the state of the individual looks like a chronic mental pathology, often diagnosed with schizophrenia, which, as you know, was originally designated dementia precox (from Latin dēmentia praecox - “dementia praecox”). The diagnosis does not mean that the person "died" forever, since with appropriate treatment, patients can be healed. nine0003
Physical death. PTSD increases the risk of suicide, which rises to 38%. The risk is compounded by the fact that 20 to 25% of suicides are committed under the influence of alcohol or drugs, which for many people with PTSD are ways to cope with his symptoms. According to the 2018 WHO Global Report on Alcohol Consumption and Health, there is a 7-fold increased risk of attempting suicide immediately after drinking alcohol. Of course, among the consequences of PTSD there is pseudo-suicide, which is committed in a state of depression or passion and is not so much an attempt to take one's own life as a "cry for help", an attempt to attract the attention of others to oneself and one's problems. Hidden suicide (life-threatening and life-shortening behavior) manifests itself not only in alcoholism, drug addiction, substance abuse, refusal of medical care for serious illnesses and other types of self-destructive behavior, but also in deliberate disregard for traffic rules, recklessness, non-compliance with safety regulations , propensity for extreme sports without proper training and equipment, neglect of danger in various life situations.
PTSD increases the risk of suicide, which rises to 38%. The risk is compounded by the fact that 20 to 25% of suicides are committed under the influence of alcohol or drugs, which for many people with PTSD are ways to cope with his symptoms. According to the 2018 WHO Global Report on Alcohol Consumption and Health, there is a 7-fold increased risk of attempting suicide immediately after drinking alcohol. Of course, among the consequences of PTSD there is pseudo-suicide, which is committed in a state of depression or passion and is not so much an attempt to take one's own life as a "cry for help", an attempt to attract the attention of others to oneself and one's problems. Hidden suicide (life-threatening and life-shortening behavior) manifests itself not only in alcoholism, drug addiction, substance abuse, refusal of medical care for serious illnesses and other types of self-destructive behavior, but also in deliberate disregard for traffic rules, recklessness, non-compliance with safety regulations , propensity for extreme sports without proper training and equipment, neglect of danger in various life situations. nine0003
nine0003
Pandemic and PTSD.
Our research, which we conducted during 2020–2022, showed that the majority of respondents (from 57 to 72%) are dominated by negative negative emotions: anxiety, fear, irritation, anger, fatigue, annoyance, lack of will, distrust, despondency, violence, alienation, etc. [1, 5]. In our opinion, it was the negative emotional cluster that created the psychological prerequisites for the fact that 30% of people who ended up in intensive care during the COVID-19 pandemic, subsequently observed symptoms of post-traumatic stress disorder. With PTSD, clinical symptoms such as unmotivated vigilance, explosive reactions, memory impairment and general anxiety, insomnia and suicidal thoughts are possible. It should be noted that PTSD occurs not only in people who got into an extremely difficult psychotraumatic situation, extraordinary stress during intensive care, but also in medical workers who were constantly in contact with patients, providing them with assistance.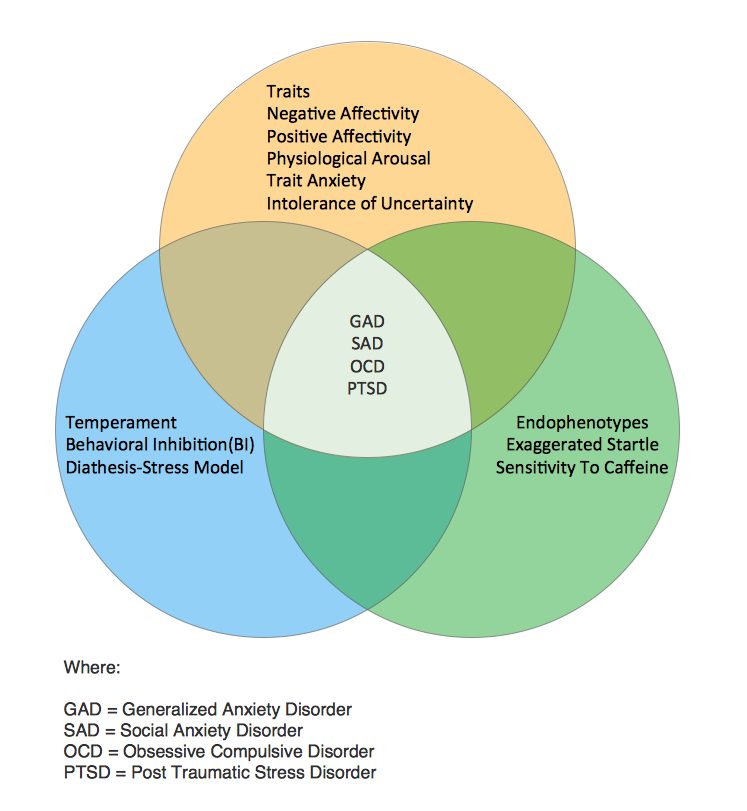 Data on the incidence of moderate depression, anxiety disorders, and post-traumatic stress disorder were taken from 65 studies, including 97,333 healthcare professionals from 21 countries. The prevalence of depression was 21.7% (95% CI, 18.3%–25.2%), anxiety disorder 22.1% (95% CI, 18.2%–26.3%), and post-traumatic stress disorder 21. 5% (95% CI, 10.5%–34.9%). The prevalence of anxiety disorders and depression was higher in studies performed in the Middle East (34.6% compared to 28.9%) [7].
Data on the incidence of moderate depression, anxiety disorders, and post-traumatic stress disorder were taken from 65 studies, including 97,333 healthcare professionals from 21 countries. The prevalence of depression was 21.7% (95% CI, 18.3%–25.2%), anxiety disorder 22.1% (95% CI, 18.2%–26.3%), and post-traumatic stress disorder 21. 5% (95% CI, 10.5%–34.9%). The prevalence of anxiety disorders and depression was higher in studies performed in the Middle East (34.6% compared to 28.9%) [7].
- The impact of the COVID-19 epidemic on mental health and psychosocial support for the elderly / Yu. A. Bubeev, V. V. Kozlov, L. D. Syrkin [et al.] // Advances in Gerontology, 2020. V. 33. No. 6 . pp. 1043–1049.
- Dzeruzhinskaya N. A., Syropyatov O. G. Post-traumatic stress disorder. A guide for self-study. Kyiv: Ukrainian Military Medical Academy, 2014.
- Kadyrov R.V. Post-traumatic stress disorder (PTSD): state of the problem, psychodiagnostics and psychological assistance.
 Moscow: Yurayt, 2020. 644 p.
Moscow: Yurayt, 2020. 644 p. - Kitaev-Smyk L. A. Stress of war. Front-line observations of a psychologist. Moscow: Russian Institute of Cultural Studies, 2001. 80 p. nine0038
- Kozlov V.V. Psychology of a pandemic. 2nd edition, expanded and supplemented. Yaroslavl: RPF "Titul", 2022. 126 p.
- Kozlov, VV Psychology of crisis. Saratov: Higher education, 2014. 386 p.
- Yufei Li, Scherer N., Lambert F., Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PLOS ONE, 2021; 16(3). pp. 12–20. nine0038
Source: Kozlov V.V. Some features of post-traumatic stress disorder in modern conditions // Yaroslavl Psychological Bulletin. 2022. No. 2 (53). pp. 45-50.
Photo: website of the Eurasian Humanitarian Institute
What is PTSD and how to get rid of it
April 14 Likbez Health
It is possible to maintain a healthy mind even after a disaster. nine0003
nine0003
What is PTSD
Post Traumatic Stress Disorder, or PTSD for short, is a mental condition that interferes with the lives of some victims or bystanders of horrific events: combat, catastrophes, accidents, physical or sexual abuse. Initially, the diagnosis was made to those who had been in the war, but PTSD can develop in anyone.
Most people feel anxious, sad, angry or irritated after a traumatic event. They have insomnia and constant fatigue. This is a normal reaction to a threat to life and health, a feeling of helplessness and loss of control over what is happening. But after a month, these manifestations, as a rule, weaken and people return to normal life. nine0003
If the symptoms do not go away, the person continues to be tormented by memories and nightmares, we can talk about the development of post-traumatic stress disorder. According to WHO, 9% of those who have experienced something terrible need treatment for it. At the same time, women suffer from PTSD 2.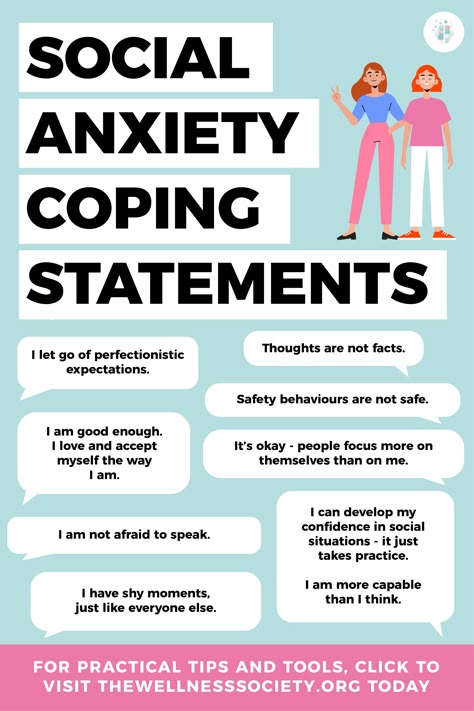 5 times more often than men, although men face more dangerous situations.
5 times more often than men, although men face more dangerous situations.
PTSD cannot be left untreated. The disorder spoils personal, social, work relationships, interferes with daily tasks.
Why PTSD occurs
It is not known exactly why a stress disorder develops in certain people. But there are factors that increase the risks:
- The nature of the injury. The stronger and longer the stress, the higher the likelihood of PTSD.
- Previously experienced psychological trauma. For example, childhood abuse.
- Heredity. Those with relatives who have had anxiety disorders or depression are more at risk.
- Work or hobbies associated with constant stress or danger to life. nine0038
- Presence of other mental disorders.
- Temperament and how the brain regulates hormones and other chemicals that are released in response to stress.
- Lack of support from loved ones after an injury.
- Frequent use of alcohol and other psychoactive substances.
How PTSD manifests itself
Symptoms of PTSD are more often detected within a month after the event, but sometimes they are not noticed until several years later. This can happen against the background of new stress or an accidental reminder of the experience. nine0003
Symptoms can be divided into four main groups.
Obsessive memories and dreams
- A person cannot forget and constantly replays what happened in his head.
- He has nightmares, which makes him afraid to go to bed.
- Any reminder of an event causes strong emotions or physical manifestations. For example, after a car accident, the victim reacts to a car signal with shaking in the hands or a sharp attack of fear.
Avoidance
- The victim is constantly trying to forget about the experience, it takes a lot of strength and energy.
- He diligently avoids places or people that can remind him of something terrible. For example, after the death of a loved one, a person may refuse to meet with other relatives so as not to talk about the deceased.
- Gives up favorite activities if they are somehow related to what happened. A girl who survived an attack in the stairwell may refuse to train after work because she is afraid to return home in the evening. nine0038
Changes in mood and thinking
- Negative thoughts about oneself, other people or the world appear.
- Haunted by a feeling of hopelessness. There are no goals in life and the desire to change something.
- There are memory problems. Sometimes it is not possible to remember important details of the traumatic event.
- It becomes difficult to communicate with loved ones, maintain relationships.
- Loss of interest in hobbies or meeting friends.
- The victim is not able to rejoice or grieve, only detachedly observes life from the outside. nine0038
Changes in physical and emotional reactions
- A person constantly feels a threat to life and seeks to protect himself by any means.
- Often feels guilty or ashamed.
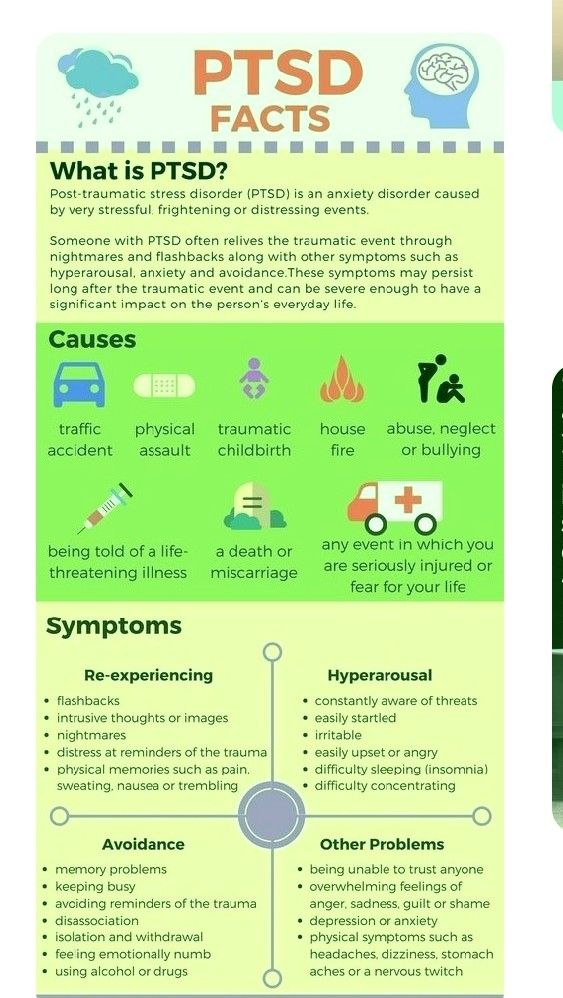 Thinking about how it could have been avoided.
Thinking about how it could have been avoided. - Loss of concentration, difficulty working or just reading a book.
- The victim may be short-tempered and aggressive.
- Sleep problems appear.
- Man unconsciously strives for self-destruction. For example, he drinks a lot or ignores traffic rules. nine0038
Symptoms may increase or decrease, appearing only with new stress or a reminder of a terrible event. The victim himself may not associate problems with sleep or concentration with the trauma experienced, especially if a lot of time has passed. But at the same time, constant stress interferes with a normal life.
What to do if you have thoughts of suicide
In this case, you should immediately seek help:
- 5 989-50-50) or the Independent Psychiatric Association (+ 7 495 625-06-20). They work around the clock.
- Write to a psychologist on the website of the Ministry of Emergency Situations - this is possible without registration.

- Contact your loved ones for support.
How is PTSD treated? The best place to start is to see a therapist. He will check if there are any physical diseases that can cause changes in the psyche. To do this, the doctor will conduct an examination and prescribe the necessary examinations. This could be a chest x-ray, blood tests, or a CT scan of the brain. nine0003
If everything is in order with the body, the therapist will refer you for a consultation with a specialized specialist. He will determine whether medication is needed or psychotherapy will be enough.
Before meeting with a psychotherapist, prepare a list of symptoms, behavioral changes, or lifestyle changes. At the appointment, ask the specialist about the experience of working with post-traumatic stress syndrome and the number of patients who have overcome it. It is important to ask all the exciting questions at once, because the success of treatment largely depends on the trusting relationship between the patient and the psychotherapist. nine0003
nine0003
What psychotherapy can be like
According to experts, only psychotherapy can get rid of PTSD. Medicines can only relieve acute manifestations and temporarily improve the quality of life.
Several methods are used to treat PTSD:
- Cognitive therapy . The doctor will analyze the thinking errors and stereotypes that prevent you from returning to normal life after an injury. For example, the thought "I'm bad because they did this to me" will gradually turn into "They did this to me, but that doesn't make me bad." The patient will keep a diary and describe in it his condition and reactions to different situations. Gradually, a person will learn to solve problems that were previously beyond his power. nine0038
- Behavioral or exposure therapy . The meaning of the method is to return to a traumatic situation under the control of a psychotherapist. The patient is immersed in the past with the help of video, sounds or verbal description, but the specialist teaches to cope without panic and horror.
 Over time, memories cease to frighten, it becomes possible to live on without looking back at the trauma.
Over time, memories cease to frighten, it becomes possible to live on without looking back at the trauma. - EMDR, or EMDR - eye movement desensitization and processing. This method was developed specifically for the treatment of post-traumatic disorders. It is believed that the brain cannot cope with the processing of a stressful event and therefore memories do not go away. In an EMDR session, the patient briefly focuses on the past and at the same time on eye movements or other stimuli: pats, sounds. This synchronizes the activity of both hemispheres and helps the brain process painful memories. If the injury was mild, four or five sessions may be enough. nine0038
What drugs can be prescribed by a doctor
Medications are prescribed at the same time as psychotherapy, if you need to remove the most striking manifestations of the disorder and improve the quality of life before psychotherapy works.
Several groups of drugs are used:
- Antidepressants .
 May reduce symptoms of anxiety and depression, improve sleep, memory and concentration.
May reduce symptoms of anxiety and depression, improve sleep, memory and concentration. - Mood Stabilizers . They are used to reduce impulsivity, anger attacks and to reduce irritability. nine0038
- Antipsychotics . They are prescribed if the shock was too severe and memories and emotions interfere with life.
- Benzodiazepines . Used to reduce severe anxiety and improve sleep. But now they are rarely appointed.
What else can you do
Taking care of yourself helps you get back to normal life faster and easier. It costs:
- Follow the treatment plan, even if it seems that psychotherapy and medication do not help. It takes time to get easier. nine0038
- Find an opportunity for good rest and sports or walks. Physical activity and healthy sleep relax and help to recover.
- Diverse and tasty food. The lack of useful elements can worsen the mental state.
- Reduce or eliminate possible sources of stress.
 New causes for concern lengthen the treatment.
New causes for concern lengthen the treatment. - Avoid coffee, alcohol and cigarettes. They can increase anxiety.
- Connect with loved ones and meet friends who can support and listen. nine0038
- Find interesting hobbies that will distract from experiences and memories.
How successful is the treatment of PTSD
Everything is individual. The result will depend on the severity of the symptoms, as well as the efforts of the patient and the support of loved ones.
But if you follow all the doctor's recommendations, sooner or later you can be cured and return to normal life.
Moreover, new preparations and methods are constantly appearing. For example, the US Food and Drug Administration recently approved an app to interrupt nightmares. nine0003
How to help a loved one with PTSD
If a relative or friend has PTSD, the most important thing is to help them seek professional help. After all, the victim may inadequately perceive the situation and believe that everything will pass by itself.