Ptsd abandonment triggers
Abandonment Trauma | Rosewood Centers
Speak to a Rosewood Specialist
(800) 845-2211
Speak to a Rosewood Specialist
(800) 845-2211
What is Abandonment Trauma?
From the moment a baby comes into the world, forming attachments to parents or other caregivers is critical to a child’s emotional, physical and psychological development. For an infant, having a gentle and responsive caregiver provides the nurturing a child needs to grow into a healthy adult. A cared for child develops self-esteem, feels secure in exploring the world around him or her and has a strong foundation for understanding how to build healthy relationships later in life.
But if those earliest relationships break down, the child may experience what is known as abandonment or neglect trauma. Mental health issues, substance abuse or the physical absence of parents or caregivers due to death or divorce can all contribute to abandonment trauma, also known as post-traumatic stress disorder (PTSD) of abandonment.
How Abandonment Trauma Hurts Development
Abandonment trauma leaves children feeling unsafe, unimportant and unsure of how their needs are going to be met. This can leave an imprint on an individual’s psychological well-being into adulthood, increasing the likelihood of developing substance use disorders, eating disorders, relationship difficulties and mental health disorders.
Healthy individuals rely on stable and safe relationships throughout the developmental years to show them how to grow healthy relationships throughout life. The earliest relationships teach children how to identify danger, bond with new people, identify their own needs, and how to be loved by another person.
Traumatic experiences in childhood, such as a parent who is under the influence of alcohol and drugs or has serious psychiatric issues and fails to adequately protect and care for their child, are major causes of abandonment trauma. But there can be other situations that can contribute to PTSD of abandonment as well. An elementary school student trying to reconcile why one parent now lives far away due to a divorce, or a teenager who has a parent in jail, can also experience feelings of abandonment and subsequently show signs of abandonment trauma. While not every child who goes through these experiences necessarily suffers long-term issues as a result, he or she can certainly contribute to problems later on in life, especially when combined with other forms of trauma or other issues within the family.
An elementary school student trying to reconcile why one parent now lives far away due to a divorce, or a teenager who has a parent in jail, can also experience feelings of abandonment and subsequently show signs of abandonment trauma. While not every child who goes through these experiences necessarily suffers long-term issues as a result, he or she can certainly contribute to problems later on in life, especially when combined with other forms of trauma or other issues within the family.
While it’s more common for abandonment trauma to occur during the developmental years of childhood and early adulthood, the events that trigger abandonment trauma can happen at any time in life. Adults may experience abandonment trauma as a result of an unwanted divorce or the death of a partner or spouse. The ending of these most important relationships can make the individual feel less safe, less loved, and less equipped to have healthy relationships in the future.
Causes of Abandonment Disorder
Abandonment disorder, also referred to as abandonment syndrome, is caused by an adverse experience or experiences that leave a person feeling unsafe, fearful and alone.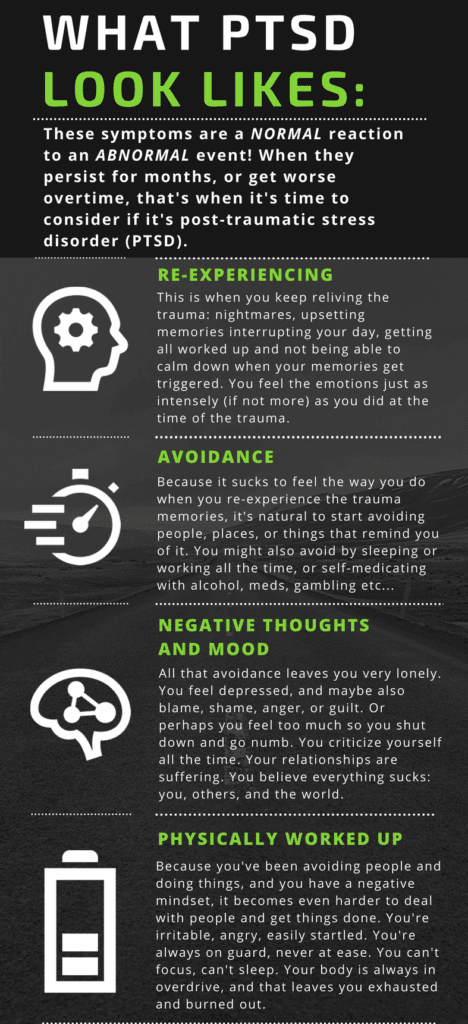 The intense emotional distress can impact a person’s health over a lifetime. PTSD of abandonment stems from losses and disconnections in early childhood, such as:
The intense emotional distress can impact a person’s health over a lifetime. PTSD of abandonment stems from losses and disconnections in early childhood, such as:
- A parent who is emotionally unavailable.
- Childhood neglect due to substance abuse, such as alcoholism or drug abuse.
- Mental illness, such as depression, in a parent or caregiver.
- A serious physical illness in a parent or caregiver, leaving the person to be unable to tend to the child’s basic needs for love and attention.
- The sudden loss of a parent or caregiver who the child depended on to feel safe and loved.
- Significant family instability, such as parents who are preoccupied with a difficult divorce or a parent who is only sporadically engaged with the child.
Signs of PTSD of Abandonment
While each individual is unique and experiences trauma differently, certain symptoms may indicate an individual is living with PTSD of abandonment:
- Fear of being left behind or abandoned.

- Inability to form healthy relationships in the teenage or adult years.
- Low self-esteem and feelings of self-worth.
- Anxiety and insecurity.
- Depression.
- Feelings of helplessness, inadequacy, being “not enough.”
- “Checking out” of relationships or friendships, feeling unattached or emotionally unavailable to connect.
- Holding on to a relationship, even if it is unhealthy or abusive, so as to avoid any feelings of abandonment or loneliness.
- Episodes of self-harming behaviors.
- Fear of conflict within a relationship, or avoiding the conflict at all costs.
- Avoiding all relationships or friendships.
- An excessive and pronounced need for control, whether it be control over environment, other people, or situations.
- Self-judgment and setting unrealistic expectations, perfectionism.
- Reacting to situations on one extreme or the other, for example, reacting too much or not at all to difficult situations.

- Emotional flashbacks, leading to feelings of panic or intense emotional distress.
We are here to help you.
Call (800) 845-2211
The Link Between Trauma and Eating Disorders
Past traumatic experiences are well-known contributors to eating disorders such as anorexia and bulimia. Trauma leads to a loss of feelings of control. People may attempt to cope with the stress and anxiety stemming from trauma by withholding food, such as in anorexia, purging or binge eating. The behaviors can be a tactic people use to numb or distance themselves from disturbing memories and emotions. Some researchers have also suggested that the eating disorder is a form of self-abuse, self-blame and a reaction to shame that has resulted from the trauma. Through the eating disorder behavior, the person with the eating disorder is recreating the pain they felt as a result of the trauma, only this time the individual has control over what is happening rather than having it inflicted on them.
Anorexia is a condition in which an individual severely restricts food and calories in order to loose weight, and has difficulty maintaining a healthy body weight. When left untreated, anorexia is a long-term illness and has a high risk of death.
Bulimia is characterized by a cycle of uncontrolled food binging behaviors followed by purging, such as vomiting or using laxatives, restricting behaviors, for example, fasting, or excessive exercise.
Binge eating disorder occurs when a person eats more in a short amount of time than most people would, while also feeling unable to control the eating. These episodes are often followed by feelings of guilt, embarrassment, or self-disgust.
How Abandonment Trauma Contributes to Eating Disorders
Like other forms of trauma, post-traumatic stress of abandonment specifically can also contribute to eating disorders. Individuals who have experienced past abandonment trauma situations are more likely to have self-harming behaviors, low self-esteem and feelings of self-worth, as well as a need for a sense of control. This can be a breeding ground for eating disorders.
This can be a breeding ground for eating disorders.
For example, people who live with anorexia often suffer with anxiety issues. Strictly counting calories and maintaining a low body weight allows them to gain a sense of control over that aspect of their life. Similarly, individuals who live with bulimia or binge eating disorder often struggle with self-judgment and shame, as well as self-harm.
PTSD from abandonment trauma can leave people feeling anxious and worried about their own physical and emotional safety. Children worried about how their basic needs will be met may suffer from anxiety and have a pronounced need for control over what’s happening around them.
Abandonment trauma may also cause people to enter into or stay in unhealthy or abusive relationships, which in turn can lead to additional trauma that feeds eating disorders.
It’s important to recognize that there is rarely just one factor contributing to an eating disorder. It’s often a culmination of experiences, combined with other genetic, environmental and psychological factors, that tips a person into eating disorder behaviors.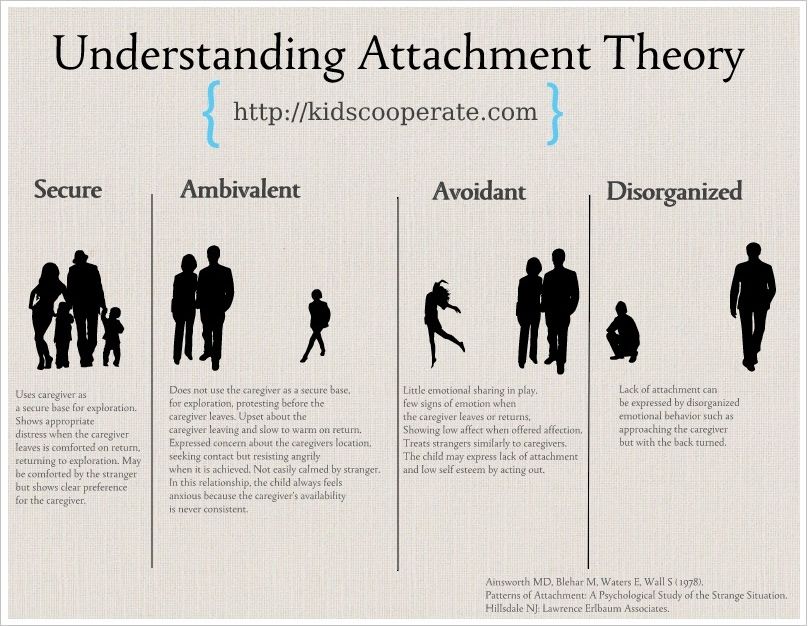
PTSD of Abandonment is Linked To:
- Anxiety
- Borderline personality disorders
- Depression
- Eating disorders
- Other mood disorders
Treating Abandonment Disorder
The symptoms of PTSD of abandonment may be mild or severe. When it comes to diagnosing and treating eating disorders, the treatment team at Rosewood Centers for Eating Disorders works with the individual to uncover the root of the eating disorder behavior. Along the way, it is common for the health team to find issues with anxiety, obsessions or compulsions, a desire to control, and past traumas.
In most cases, the abandonment situation has occurred long before the eating disorder begins. It may take time for individuals to make the connection that the past trauma is a contributor to the eating disorder because one coping mechanism can be to block out or minimize the experience. The abandonment may have also happened when the individual was too young to remember the details.
When the underlying trauma is identified, and unhealthy coping skills are addressed through a multidisciplinary approach, the individual can not only conquer their eating disorder, but can also learn how to foster healthy relationships in their future. Through therapy, counseling and trauma treatment techniques such as EMDR, individuals can recover from abandonment. This includes coming to terms with the abandonment and addressing co-occurring disorders that may have emanated from it. Recovery from abandonment trauma also means learning ways to avoid self-sabotage in relationships that may occur as a result of their anxiety, a difficulty trusting and a tendency to isolate or withdraw from others.
Goals of treatment include helping people develop the self-esteem and sense of self-worth that they may have lost due to trauma of abandonment. Treatment can help people identify the source of their need for control. In group and individual therapy, individuals learn to identify what makes a healthy relationship and develop an understanding of how they deserve to be treated by those they interact with, and those they love. Techniques such as cognitive behavioral therapy and dialectical behavior therapy help individuals learn ways of coping with anxiety, stress and interpersonal conflict without resorting to eating disorder behaviors. In treatment, people also receive medications and help in managing co-occurring disorders such as depression, bipolar disorder, borderline personality disorder and other conditions that can fuel the eating disorder.
Residential treatment for eating disorders of course also targets eating and food-related behaviors specifically. Meal plans, nutritional counseling, individual and group therapy, and experiential therapies such as cooking classes and restaurant outings provide opportunities to put the skills learned in treatment to use in the real word.
This comprehensive approach to trauma and eating disorders treatment lays the groundwork for long-term recovery. Our trauma-informed, experienced and highly credentialed clinical staff is here to help individuals heal from the damaging experiences of their past and move toward a healthier, more peaceful future.
Rosewood Eating Disorder
Treatment Centers & Locations
Get help now
(800) 845-2211
Insurance TypeEmployer ProvidedGovernment Provided (Medicare/Medicaid)Self ProvidedNoneRelationship to Patient--None--BrotherClinical ProfessionalDaughterFatherFriendGirl/boyfriendGrandparentHusbandMotherOtherPartnerSelfSisterSonSponsorWife
In-Network With Most Insurance Plans
Blue Cross Blue Shield
Beacon Health Options
First Health Network
Magellan
MultiPlan
Kaiser
United Healthcare
Accreditations & Memberships
Joint Commission Gold Seal of Approval
Residential Eating Disorders Consortium
National Eating Disorders Association
Eating Disorders Coalition
The Alliance for Eating Disorder Awareness
International Association of Eating Disorders Professionals
Follow Us
Facebook Twitter Youtube Linkedin Instagram
Facebook Twitter Linkedin Instagram
© Rosewood Centers for Eating Disorders
© 2020 Monte Nido & Affiliates
All rights reserved
We save lives while providing the opportunity for people to realize their healthy selves.
Post Traumatic Stress Disorder of Abandonment: 36 Characteristics | by Susan Anderson | Abandonment Recovery
The intense emotional crisis of abandonment can create a trauma severe enough to leave an emotional imprint on individuals’ psychobiological functioning, affecting their future choices and responses to rejection, loss, or disconnection. Following an abandonment experience in childhood or adulthood, some people develop a sequela of post-traumatic symptoms which share sufficient features with post-traumatic stress disorder to be considered a subtype of this diagnostic category.
As with other types of post-trauma, the symptoms of post-traumatic stress disorder of abandonment range from mild to severe. PTSD of abandonment is a psychobiological condition in which earlier separation traumas interfere with current life. An earmark of this interference is intrusive anxiety which often manifests as a pervasive feeling of insecurity — a primary source of self-sabotage in our primary relationships and in achieving long-range goals. Another earmark is a tendency to compulsively reenact our abandonment scenarios through repetitive patterns, i.e., abandoholism — being attracted to the unavailable.
Another factor of abandonment post-trauma is for victims to be plagued with diminished self-esteem and heightened vulnerability within social contexts (including the workplace) which intensifies their need to buttress their flagging ego strength with defense mechanisms which can be automatically discharged and whose intention is to protect the narcissistically injured self from further rejection, criticism, or abandonment. These habituated defenses are often maladaptive to their purpose in that they can create emotional tension and jeopardize emotional connections.
Victims of abandonment trauma can have emotional flashbacks that flood us with feelings ranging from mild anxiety to intense panic in response to triggers that we may or may not be conscious of. Once our abandonment fear is triggered, it can lead to what Daniel Goleman calls emotional hijacking. During an emotional hijacking, the emotional brain has taken over, leaving its victims feeling a complete loss of control over their own lives, at least momentarily. If emotional hijacking occurs frequently enough, its chronic emotional excesses can lead to self-depreciation and isolation within relationships, as well as give rise to secondary conditions such as chronic depression, anxiety, obsessive thinking, negative narcissism, and addiction.
Post Traumatic Stress Disorder (PTSD) is a so-called “disease” of the amygdala — the emotional center of the brain responsible for initiating the Fight Flee Freeze response. In PTSD, the amygdala is set on overdrive to keep us in a perpetual state of hyper-vigilance — action-ready to declare a state of emergency should it perceive any threat even vaguely reminiscent of the original trauma. The amygdala, acting as the brain’s warning system, is constantly working to protect (overprotect) us from any possibility of further injury. In the post-trauma sequelae related specifically to abandonment, the amygdala scans the environment for potential threats to our attachments or to our sense of self-worth.
People with PTSD of abandonment can have heightened emotional responses to abandonment triggers that are often considered insignificant by others. For instance, depending on circumstances, when we feel slighted, criticized, or excluded, it can instigate an emotional hijacking and interfere in, and even jeopardize our personal or professional life.
Below, I’ll identify some of the other issues related to post-traumatic stress disorder of abandonment:
This list is meant to be descriptive, rather than exhaustive of the many issues related to the abandonment syndrome.
- An intense fear of abandonment that interferes in forming primary relationships in adulthood.
- Intrusive insecurity that interferes in your social life and goal achievement.
- Anxiety with authority figures.
- A tendency toward self-defeating behavior patterns that sabotage your love life, goals, or career.
- A tendency to repeatedly subject yourself to people or experiences that lead to another loss, another rejection, and other trauma.
- An intrusive reawakening of old losses; echoes of old feelings of vulnerability and fear which interfere in current experience.
- Heightened memories of traumatic separations and other events.
- Conversely, partial or complete memory blocks of childhood traumas.
- Low self-esteem, low sense of entitlement, performance anxiety.
- Feelings of emotional detachment, i.e. feeling numb to past losses.
- Conversely, difficulty letting go of the painful feelings of old rejections and losses.
- Difficulty letting go, even when we know the relationship cannot meet our basic needs
- Episodes of self-neglectful or self-destructive behavior.
- Difficulty withstanding (and overreacting to) the customary emotional ups and downs of your adult relationships.
- Difficulty working through the ordinary levels of conflict and disappointment within your adult relationships.
- Extreme sensitivity to perceived rejections, exclusions or criticisms.
- The emotional pendulum swing between fear of engulfment and fear of abandonment; you can alternate between ‘feeling the walls close in’ if someone gets too close and feeling insecure, love-starved — on a precipice of abandonment — if you are not sure of the person’s love.
- Difficulty feeling the affection and other physical comforts offered by a willing partner — “keeping them out” or “pushing them away; evidence of emotional anorexia or emotional bulimia.
- The tendency to ‘get turned off’ and ‘lose the connection’ by involuntarily shutting down romantically and/or sexually on a willing partner.
- Conversely, the tendency to feel hopelessly hooked on a partner who is emotionally distancing.
- The tendency to have emotional hangovers ‘the morning after’ you have had contact with an ex or someone over whom you have felt pain.
- Difficulty naming your feelings or sorting through an emotional fog.
- - a tendency to avoid close relationships altogether to avoid the risk of abandonment.
- Conversely, a tendency to rush into relationships and clamp-on too quickly.
- Difficulty letting go because you have attached with emotional epoxy, even when you know your partner is no longer able to fulfill your needs, or even when you know your partner is not good for you.
- An excessive need for control, whether it’s about the need to control the other’s behavior and thoughts, or about being excessively self-controlled; a need to have everything perfect and done your way.
- Conversely, a tendency to create chaos by avoiding responsibility, procrastinating, giving up control to others, and feeling out of control.
- A heightened sense of responsibility to others, rescuing, attending to people’s needs, even when they have not voiced them.
- The tendency to have unrealistic expectations and heightened reactivity toward others such that it creates conflict and burns bridges to your social connections.
- People-pleasing — excessive need for acceptance or approval.
- Self-judgment; unrealistic expectations toward yourself.
- The fear response to people’s anger, which unwittingly sets you up to being “controlled” by them.
- Co-dependency issues in which you give too much of yourself to others and feel you don’t get enough back.
- The tendency to act impulsively without being able to put the brakes on, even when you are aware of the negative consequences.
- The tendency toward unpredictable outbursts of anger.
- Conversely, the tendency to under-react to anger out of fear of breaking the connection and also out of your extreme aversion to ‘not being liked’.
The impact of abandonment trauma can be mitigated by abandonment recovery — a program of therapy techniques designed to help you overcome abandonment and its aftermath of self-sabotaging patterns.
© Susan Anderson November 12 2013, updated and revised Sept 28 2016
Originally published at https://www.abandonment.net.
ᐈ PTSD Diagnosis ~【Post Traumatic Stress Disorder】
Post-traumatic stress disorder, or PTSD, is a severe mental condition that progresses as a result of a single or recurring event that has a negative impact on a person's mental health. Symptoms of PTSD can appear immediately or several months after the injury.
The likelihood of developing post-traumatic stress disorder is the same for patients of different age groups. The main risk factor is the severity of the injury, the initial state of the psyche, psychological and biological predisposition.
Vidkriti Zgornuti
Classification
In the modern classification, 4 types of post-traumatic syndrome are distinguished:
Acute.
Appears in the first days after a stressful situation. Symptoms appear very brightly within 2-3 months.
Chronic.
Characterized by a gradual increase in signs of pathology, exhaustion of the nervous system, changes in character and interests.
Deformation.
Manifested in patients with a long-term chronic mental disorder. Progress leads to the formation of phobias, neuroses, feelings of anxiety.
Delayed.
The clinical picture becomes apparent 3-6 months after the injury. Various external stimuli can provoke the progress of PTSD.
There are also 3 stages of PTSD: acute, chronic and delayed.
In the first case, this is the period of the beginning of an extreme situation. The state is saved until it ends. Characterized by excessive anxiety for one's own life, lethargy, confusion.
A chronic condition occurs after the trigger has been removed if the patient feels restless. It is possible that the clouding of the mind persists, the person does not understand what happened. Often there are changes in speech and motor functions.
In some cases, with PTSD, the stages of such a plan are not observed, a delayed form appears, that is, the characteristic symptoms appear after a few months, and before that the patient feels normal.
This medical problem also varies in severity. With a mild course of post-traumatic syndrome, the patient's state of health remains unchanged, the ability to work professionally and the ability to communicate with other individuals is preserved. With a severe degree of damage, chronic mental disorders are diagnosed, schizophrenia is possible. With prolonged progress, PTSD leads to malfunctions of the brain, affects the functioning of the endocrine and nervous systems.
Post-traumatic syndromes are characterized by diverse signs, depending on which division into clinical types is provided: When detecting post-traumatic stress disorder, the main task of a specialist is to correctly differentiate the diagnosis by establishing the type and type. Vidkriti Zgornuti The main factor that provokes post-traumatic stress disorder is a tragic event, a traumatic situation. A psychologically healthy person can face PTSD, but the course of the disease will be easier for him than for a person with a shaken psyche. In all cases, the syndrome has an undulating course, often leading to a permanent change in personality. Vidkriti Zgornuti The list of symptoms of PTSD includes the following changes: Vidkriti Zgornuti According to statistics, the disease in children is detected no more often than in adults, but experts in the field of psychotherapy assure that the disorder in children progresses faster. Pathology is diagnosed by a child psychiatrist. The doctor determines what traumatic event occurred and what changes in the nervous system it provoked. During the diagnosis, the patient's reaction to the impact of stimuli is assessed, the presence of memories reproduced in a dream, during a game or in stories is clarified. A consultation with a child psychologist will allow you to establish the type of disorder, determine the scheme of influence and establish a prognosis for recovery. Treatment of PTSD in children is a long-term work with a child psychologist or psychotherapist. Complex therapy requires the combined use of several techniques. The patient is shown cognitive-behavioral correction, psychotherapy and drug treatment aimed at stabilizing the work of the central nervous system. Vidkriti Zgornuti The diagnosis of PTSD should not be ignored. Over time, the problem can worsen and lead to irreversible complications. Only acute disorders can be corrected, after the transition to a chronic form, therapy is complicated, a pathological change in personality is observed. A person manifests pronounced narcissistic qualities, the development of alcoholism and drug addiction is not excluded. Together, these factors are unfavorable signs, and therefore aggravate the prognosis for recovery. Vidkriti Zgornuti Post-traumatic stress disorder is established on the basis of the patient's complaints about psychological trauma, tragic events in the past. Diagnosis of PTSD is provided with the help of special questionnaires confirming the presence of criteria similar to the disease. Self-testing for PTSD is not always accurate because some factors may be hidden. Vidkriti Zgornuti The treatment of PTSD is determined individually, taking into account the characteristics of the patient, the type of pathology and the presence or absence of concomitant disorders. The most effective are cognitive behavioral therapy and hypnotherapy. According to the indications, psychotherapy is combined with medication. Treatment of PTSD often requires the use of adrenergic blockers, antidepressants, tranquilizers, neuroleptics. As auxiliary methods, therapeutic massage is used. Vidkriti Zgornuti A rehabilitation doctor or psychotherapist can help prevent the development of serious problems. The doctor should explain to the patient that an acute reaction to stress is normal for the human body. Another prevention of PTSD is to avoid possible stress and maintain mental balance. Vidkriti Zgornuti The article is for informational purposes only. Please remember: self-medication can harm your health. Vidkriti Zgornuti Vidkriti Zgornuti The author of the article: Elena Tarasenko Psychotherapist, psychiatrist If a problem is found, the patient should contact a psychiatrist. Specialists of the MEDICOM clinic working with the latest techniques will help you to undergo high-quality diagnostics and treatment of PTSD in Kyiv. You can seek help and take a test for PTSD at the clinic's subdivisions located in Obolon and Pechersk. Mental health requires careful attention, so it is better to turn to professionals! show more
The main causes of PTSD
The causes of PTSD include:
There is a reassessment of one's own ideals, one's importance in life, a change in old ideas.
Clinical symptoms of PTSD
PTSD in children: features
Children are a risk group due to an increased predisposition to post-traumatic stress syndrome, impressionability and sensitivity. The reasons for the development of the problem in children are psychological trauma, unfavorable social conditions and individual developmental characteristics.
Complications
Diagnostics
Often the psychiatrist recommends an additional consultation in the presence of relatives or people from close circle. This allows you to differentiate the diagnosis and exclude the presence of other, symptomatically similar diseases.
Treatment
Prevention of PTSD
The main task is to start the impact immediately after the injury, to work out the event in a quality manner in order to prevent the problem from becoming chronic. Also, to prevent the development of post-traumatic stress disorder will help:
Sources
Which doctor treats PTSD?
If signs of PTSD are found in a child, consultation with a child psychiatrist or psychologist is necessary. The consequences of PTSD can be irreversible, so it is very important to undergo a full examination, determine the type of pathology, establish the cause and work out a treatment regimen.
Certificates
Reviews
10/23/2021 18:14
Alexander
To the author. Definitely, PTSD is really serious. Skoda, which doctors know, do not outperform neither sick nor relatives. I broke my ankle for 3 years: 4 operations, then 3 fates in the police, fear that I would become disabled, depression, and the pressure of my relatives simply made me crazy. I don’t show how self-tapping can come in. Obov'yazkovo idit to the psychologist.
11.09.2021 20:40
Galina Andriivna Sinyavska
She licked on the wet bed near the kitchen. I had a compression fracture of the ridge, I wanted to die. I had to visit a psychologist. Without її help, I would not have run into it. The psychologist gave a reason to overcome fears and come to the solution of the problem.
07/30/2021 10:47
Valentina
Thank you majesty, that important article was written with grace. I learned a lot of new things. At once, I’ll lie on the knight with a fracture, I’ll be respectful to the new. I would not have thought before that about the mental state of a person after a serious injury, you also need to be turbulent.
15.06.2021 18:26
Vitaly
Thank you for the information and help. Kulik Maria Sergeevna is a very good specialist. So far, we have come to the consultation without the child, in order to reconnoiter the situation, so to speak. The doctor was very friendly, asked a lot of questions, then gave recommendations on how to behave with our son after being beaten by classmates at school. He is very closed, and we are slowly slipping into despair. Now the only hope is for Maria Sergeevna.
05/22/2021 11:55
Olga
I thank Kulik Mariya Sergievna for help. We have fired houses, it became late at night. Thank you to relatives from Kiev, who gave them a seat. Alesina became unrecognizable. The axis of infection from Sergiyk seems to be a psychologist, who at night finds uncontrollable panic on him, and it is unrealistic to calm down. Already after the third session, I remembered the progress.
05/01/2021 12:21
Mikhailo Valentinovich
Thank you for the information. Children are especially susceptible to mental trauma at a time. Recently, my team died of cancer, I can’t know the language of the child, although earlier we were closer. At the nearest future, I will turn to her for help to a psychologist.
04/11/2021 13:32
Leonid
I like a good article and service, I often look in when something hurts for information on symptoms and diseases. But I'm interested in PTSD. How did we experience stress in our childhood without psychologists and corrective methods? Like normal grew.
12/16/2020 18:16
Grigory Titov
Very good service, they cover a lot of relevant topics, and most importantly, they immediately write which specialist you can contact for help. We went to MEDIKOM to Maria Sergeevna, a cool psychologist. The child stuttered and was very complex about this. But with the joint efforts of a speech therapist and a psychologist, the situation was corrected. Nikita is now studying, and successfully, in the 8th grade. He became very cheerful and sociable.
Show 3 more
Total 8 reviews
leave feedback
How I live with PTSD: a first-person story
“Sometimes I think I hear his voice in the crowd, and my heart starts pounding, I fall into a stupor . ..” PTSD is post-traumatic stress disorder, it is also called Vietnamese or Afghan syndrome is a severe mental illness that affects a person who has experienced a traumatic situation: military operations, physical trauma or sexual violence. Anabella has been suffering from PTSD for several years and has agreed to tell VOICE her story.
Website editor
Tags:
consequences of injury
Psychological trauma
Personal Stories
“It's still hard for me to talk about it, but I was raped five years ago and it broke me. I justified my rapist for a long time and blamed myself for what happened: they say, I allowed him myself, I didn’t resist “worthily”, I was afraid that he would have a knife and he would kill me ...
I was attacked by a close friend who I trusted. Once he admitted that he was in love with me, and I refused him. After that, our relationship deteriorated: he began to persecute me and one day, taking advantage of the opportunity, dragged me into a car and raped me.
Gradually I sank deeper and deeper into guilt. I felt like I hadn't done enough, that I had somehow caused this situation myself. And then there were flashbacks and severe panic attacks.”
Flashbacks are sudden, usually intense, re-experiences of a past experience or elements of it. They can be so intense that the person "re-experiences" the traumatic event.
“Fortunately, I forgot most of what happened to me - my brain just erased it from my memory, and I am very grateful to him for this. I remember that day in fragments, and these fragments are constantly “flashing” in my head, and this can happen at any time. For example, when I linger on someone else's hands, I remember how my hands tried to open the window of his car.
ADVERTISING - CONTINUED BELOW
Sometimes it seems to me that I hear his voice in the crowd, and my heart starts pounding, I fall into a stupor. It’s like a cold wave runs through my whole body, my legs get heavy so that I can’t move... But in general, anything can be a trigger: a sharp movement in my direction, an aggressive anti-hero in a movie, the make of the car in which I was raped, jokes about violence, references to cheating, but most often these are other people's stories, similar to mine ... "
A trigger is an event that triggers a seizure in a PTSD patient. Most often, the trigger is part of a traumatic experience: sounds, a “picture” ... Patients with PTSD usually avoid meeting the trigger with all their might, trying to avoid a new attack.
“Ever since this happened, any touch causes me physical pain - burning, as if the skin was burned in the sun. I don't like being touched by strangers.
If panic attacks happen to people, I try to just find a quiet place and wait it out. Once I had such a severe panic attack that I thought, "This is the end." I was out of breath, asked my mother to call an ambulance, and while she called, I told her how to do resuscitation if my heart stopped. Mom was very scared then.
And because of the constant feeling of guilt, I punished myself - physically. Most of all, I was worried that another man touched me when I had a boyfriend, it was like I cheated on him.
Self-harm - intentional damage to one's body without suicidal intent. Self-harm occurs as a symptom of many mental disorders, including PTSD. The most common form of self-harm is cutting and scratching the skin with sharp objects.
“Many people think that self-harm is only cuts, but in fact it is any harm to oneself. For example, I was starving, did not allow myself to drink and sometimes sleep, forced myself to remember what had happened again and again.