Psychology cpt billing codes
CPT Codes for Psychotherapy and Other Psychology Services
CPT codes allow mental health professionals to identify services for payment.
Current Procedural Terminology (CPT) codes are used to identify various types of psychological services, ranging from psychotherapy and group therapy to psychological testing services.
Clinicians use these codes to bill clients and file health insurance claims to private insurance providers and government insurance providers such as Medicare and Medicaid.
The codes have recently been updated to reflect changes made in the field of psychiatry.
Current Procedural Terminology (CPT codes) are used by psychologists and other mental health professionals to bill for their services to a private or government insurance provider.
The list we’ve included below isn’t a complete one, but rather a list of some of the most commonly used CPT codes in mental health and psychology services, meant to be used as a quick reference sheet.
It has been updated with the most recent and relevant code changes as of March 2022.
Billing codes generally don’t change very often, so the code you’ve been using may likely still be relevant.
Traditional face-to-face, individual psychotherapy sessions are usually billed only for 45 minutes (90834). It might be a good idea to get to know this code. You’ll likely use this one often.
Most mental health professionals use code 90791 for an intake interview and 90847 for family therapy.
In general, you’re responsible for using the most accurate and appropriate CPT billing code when billing for services that you provide, regardless of who does the actual billing on your behalf.
So it’s crucial you get to know the CPT codes.
| CPT Code | Description | Date changed |
| 90791 | Psychiatric diagnostic evaluation without medical services | |
| 90792 | Psychiatric diagnostic evaluation with medical services | |
| 90832 | Individual psychotherapy, 30 minutes | |
| +90833 | Individual psychotherapy, 30 minutes with evaluation and management service (E/M) | |
| 90834 | Individual psychotherapy, 45 minutes | |
| +90836 | Individual psychotherapy, 45 minutes with E/M | |
| 90837 | Individual psychotherapy, 60 minutes | |
| +90838 | Individual psychotherapy, 60 minutes with E/M | |
| 90845 | Psychoanalysis | |
| 90846 | Family psychotherapy without client present, 50 minutes | |
| 90847 | Family psychotherapy with client present, 50 minutes | |
| 90849 | Multiple-family group psychotherapy | |
| 90853 | Group psychotherapy (other than of a multiple-family group) | |
| Psychotherapy for Crisis | ||
| 90839 | Psychotherapy for crisis, first 60 minutes | |
| 90840 | Psychotherapy for crisis, each additional 30 minutes (list separately in addition to code for primary service) | |
| Psychological / Neuropsychological Testing | ||
| 96105 | Assessment of aphasia, per hour | |
| 96112 | Developmental test administration by physician or qualified healthcare professional, with interpretation and report, first hour | 2019 |
| +96113 | Developmental test administration by physician or qualified healthcare professional, with interpretation and report, each additional 30 minutes | 2019 |
| 96116 | Neurobehavioral status exam, first hour | 2019 |
| *96121 | Neurobehavioral status exam, additional hour | 2019 |
| 96125 | Standardized cognitive performance testing, per hour | |
| 96130 | Psychological testing and evaluation by a physician or qualified healthcare professional, first hour | 2019 |
| +96131 | Psychological testing and evaluation by a physician or qualified healthcare professional, each additional hour | 2019 |
| 96132 | Neuropsychological testing and evaluation by a physician or qualified healthcare professional, first hour | 2019 |
| +96133 | Neuropsychological testing and evaluation by a physician or qualified healthcare professional, each additional hour | 2019 |
| 96136 | Neuropsychological or psychological test administration and scoring by a physician or qualified healthcare professional, first hour | 2019 |
| +96137 | Neuropsychological or psychological test administration and scoring by a physician or qualified healthcare professional, each additional hour | 2019 |
| 96138 | Neuropsychological or psychological test administration and scoring by a technician, first hour | 2019 |
| +96139 | Neuropsychological or psychological test administration and scoring by a technician, each additional hour | 2019 |
| Health Behavior Assessment and Intervention | ||
| 96156 | Health behavior assessment or re-assessment | 2020 |
| 96158 | Health behavior intervention, individual, face-to-face, first 30 minutes | 2020 |
| +96159 | Health behavior intervention, individual, face-to-face, each additional 15 minutes | 2020 |
| 96164 | Health behavior intervention, group (2 or more clients), face-to-face, first 30 minutes | 2020 |
| +96165 | Health behavior intervention, group (2 or more clients), face-to-face, each additional 15 minutes | 2020 |
| 96167 | Health behavior intervention, family (with the client present), face-to-face, first 30 minutes | 2020 |
| +96168 | Health behavior intervention, family (with the client present), face-to-face, each additional 15 minutes | 2020 |
| 96170 | Health behavior intervention, family (without the client present), face-to-face, first 30 minutes | 2020 |
| +96171 | Health behavior intervention, family (without the client present), face-to-face, each additional 15 minutes | 2020 |
Recently, several CPT codes were changed to better describe various psychological, neurological, and behavioral assessments.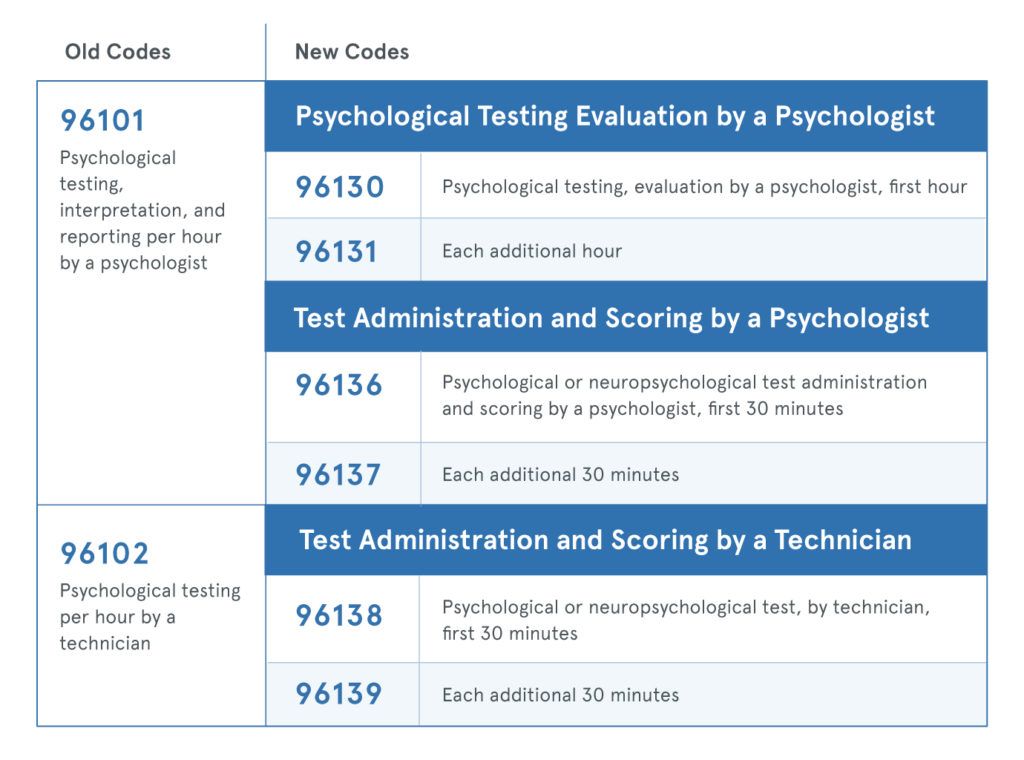
In the new codes, greater distinctions are made between whether the assessment is being given by a mental health professional, such as a psychologist or neurologist, or a technician.
Additionally, the testing services now have a stand-alone code for the primary service, as well as add-on codes for each additional service and extra time.
The primary changes in the CPT codes include:
- developmental test administration
- neurobehavioral status exam
- psychological testing and evaluation
- neuropsychological testing and evaluation
- neuropsychological or psychological test administration or scoring
- health behavior assessments and interventions
With the new codes, clinicians can better describe the exact amount of time they spend performing psychotherapy services.
These codes can also differentiate whether the test was administered by a healthcare or mental health professional or a technician.
According to the Centers for Disease Control and Prevention (CDC), U. S. adults made an average of 30 million mental health-related physician office visits from 2012 to 2014.
S. adults made an average of 30 million mental health-related physician office visits from 2012 to 2014.
In 2018, physician visits are estimated at 55.7 million.
These mental health visits cover everything from assessments and psychological testing to individual and group therapy.
Each visit and procedure requires a unique CPT code. It’s crucial for mental health professionals to stay current on CPT code updates.
CPT Codes for Psychotherapy and Other Psychology Services
CPT codes allow mental health professionals to identify services for payment.
Current Procedural Terminology (CPT) codes are used to identify various types of psychological services, ranging from psychotherapy and group therapy to psychological testing services.
Clinicians use these codes to bill clients and file health insurance claims to private insurance providers and government insurance providers such as Medicare and Medicaid.
The codes have recently been updated to reflect changes made in the field of psychiatry.
Current Procedural Terminology (CPT codes) are used by psychologists and other mental health professionals to bill for their services to a private or government insurance provider.
The list we’ve included below isn’t a complete one, but rather a list of some of the most commonly used CPT codes in mental health and psychology services, meant to be used as a quick reference sheet.
It has been updated with the most recent and relevant code changes as of March 2022.
Billing codes generally don’t change very often, so the code you’ve been using may likely still be relevant.
Traditional face-to-face, individual psychotherapy sessions are usually billed only for 45 minutes (90834). It might be a good idea to get to know this code. You’ll likely use this one often.
Most mental health professionals use code 90791 for an intake interview and 90847 for family therapy.
In general, you’re responsible for using the most accurate and appropriate CPT billing code when billing for services that you provide, regardless of who does the actual billing on your behalf.
So it’s crucial you get to know the CPT codes.
| CPT Code | Description | Date changed |
| 90791 | Psychiatric diagnostic evaluation without medical services | |
| 90792 | Psychiatric diagnostic evaluation with medical services | |
| 90832 | Individual psychotherapy, 30 minutes | |
| +90833 | Individual psychotherapy, 30 minutes with evaluation and management service (E/M) | |
| 90834 | Individual psychotherapy, 45 minutes | |
| +90836 | Individual psychotherapy, 45 minutes with E/M | |
| 90837 | Individual psychotherapy, 60 minutes | |
| +90838 | Individual psychotherapy, 60 minutes with E/M | |
| 90845 | Psychoanalysis | |
| 90846 | Family psychotherapy without client present, 50 minutes | |
| 90847 | Family psychotherapy with client present, 50 minutes | |
| 90849 | Multiple-family group psychotherapy | |
| 90853 | Group psychotherapy (other than of a multiple-family group) | |
| Psychotherapy for Crisis | ||
| 90839 | Psychotherapy for crisis, first 60 minutes | |
| 90840 | Psychotherapy for crisis, each additional 30 minutes (list separately in addition to code for primary service) | |
| Psychological / Neuropsychological Testing | ||
| 96105 | Assessment of aphasia, per hour | |
| 96112 | Developmental test administration by physician or qualified healthcare professional, with interpretation and report, first hour | 2019 |
| +96113 | Developmental test administration by physician or qualified healthcare professional, with interpretation and report, each additional 30 minutes | 2019 |
| 96116 | Neurobehavioral status exam, first hour | 2019 |
| *96121 | Neurobehavioral status exam, additional hour | 2019 |
| 96125 | Standardized cognitive performance testing, per hour | |
| 96130 | Psychological testing and evaluation by a physician or qualified healthcare professional, first hour | 2019 |
| +96131 | Psychological testing and evaluation by a physician or qualified healthcare professional, each additional hour | 2019 |
| 96132 | Neuropsychological testing and evaluation by a physician or qualified healthcare professional, first hour | 2019 |
| +96133 | Neuropsychological testing and evaluation by a physician or qualified healthcare professional, each additional hour | 2019 |
| 96136 | Neuropsychological or psychological test administration and scoring by a physician or qualified healthcare professional, first hour | 2019 |
| +96137 | Neuropsychological or psychological test administration and scoring by a physician or qualified healthcare professional, each additional hour | 2019 |
| 96138 | Neuropsychological or psychological test administration and scoring by a technician, first hour | 2019 |
| +96139 | Neuropsychological or psychological test administration and scoring by a technician, each additional hour | 2019 |
| Health Behavior Assessment and Intervention | ||
| 96156 | Health behavior assessment or re-assessment | 2020 |
| 96158 | Health behavior intervention, individual, face-to-face, first 30 minutes | 2020 |
| +96159 | Health behavior intervention, individual, face-to-face, each additional 15 minutes | 2020 |
| 96164 | Health behavior intervention, group (2 or more clients), face-to-face, first 30 minutes | 2020 |
| +96165 | Health behavior intervention, group (2 or more clients), face-to-face, each additional 15 minutes | 2020 |
| 96167 | Health behavior intervention, family (with the client present), face-to-face, first 30 minutes | 2020 |
| +96168 | Health behavior intervention, family (with the client present), face-to-face, each additional 15 minutes | 2020 |
| 96170 | Health behavior intervention, family (without the client present), face-to-face, first 30 minutes | 2020 |
| +96171 | Health behavior intervention, family (without the client present), face-to-face, each additional 15 minutes | 2020 |
Recently, several CPT codes were changed to better describe various psychological, neurological, and behavioral assessments.
In the new codes, greater distinctions are made between whether the assessment is being given by a mental health professional, such as a psychologist or neurologist, or a technician.
Additionally, the testing services now have a stand-alone code for the primary service, as well as add-on codes for each additional service and extra time.
The primary changes in the CPT codes include:
- developmental test administration
- neurobehavioral status exam
- psychological testing and evaluation
- neuropsychological testing and evaluation
- neuropsychological or psychological test administration or scoring
- health behavior assessments and interventions
With the new codes, clinicians can better describe the exact amount of time they spend performing psychotherapy services.
These codes can also differentiate whether the test was administered by a healthcare or mental health professional or a technician.
According to the Centers for Disease Control and Prevention (CDC), U. S. adults made an average of 30 million mental health-related physician office visits from 2012 to 2014.
S. adults made an average of 30 million mental health-related physician office visits from 2012 to 2014.
In 2018, physician visits are estimated at 55.7 million.
These mental health visits cover everything from assessments and psychological testing to individual and group therapy.
Each visit and procedure requires a unique CPT code. It’s crucial for mental health professionals to stay current on CPT code updates.
End of 50 minute hour? World of Psychology
On January 1, 2013, new coding procedures will go into effect for mental health services. Our Current Procedural Terminology (CPT) codes are used to bill insurers for services, and the psychiatry coding has not changed since 1998. Existing codes are self-explanatory. For example, psychiatrists are often discharged with the CPT code "90807", which is a 45-50 minute drug-managed outpatient psychotherapy session. Everyone knows what that means.
Psychiatry has changed since 1998, and the current codes do not sense the complexity or variety of what psychiatrists do now. In addition to the basic CPT codes, there are more specific Evaluation and Management (E/M) codes that require certain elements of the exam and documentation, but many psychiatrists, myself included, have practiced without ever using these E/M codes.
In addition to the basic CPT codes, there are more specific Evaluation and Management (E/M) codes that require certain elements of the exam and documentation, but many psychiatrists, myself included, have practiced without ever using these E/M codes.
New CPT codes include a level of sophistication that mental health clinicians and their support staff are only just now beginning to learn. The new codes were announced by the American Medical Association in mid-September and which new codes psychiatric professionals should use is not entirely clear; it requires training. A two-hour webinar was held at the National Council for Community Behavioral Health and demonstrated 99 slides to start the learning process. Their webinar reached maximum capacity and potential registrants were turned away. The American Psychiatric Association held a meeting in mid-November to train district leaders on how to do coding, and in my state the Maryland Psychiatric Society will begin offering workshops in December.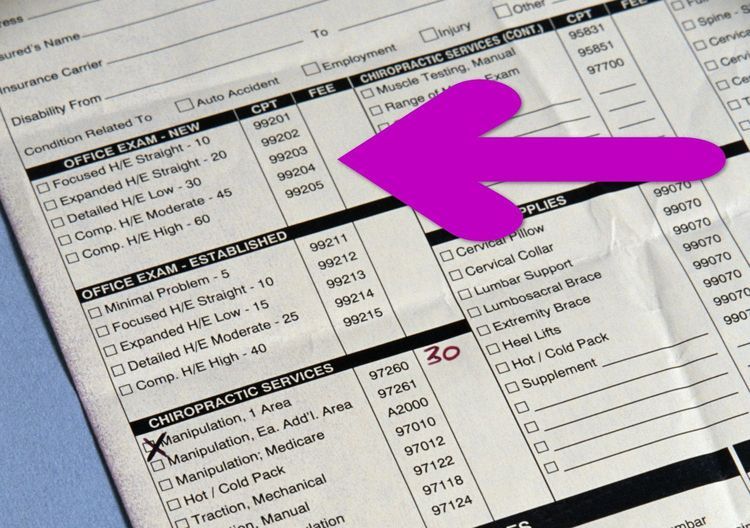
New codes, like the old ones, allow you to pay for psychotherapy depending on the time, but in increments of 30, 45 and 60 minutes. Presumably longer sessions will result in higher reimbursement, but under the new rules, a 50-minute session - or any psychotherapy session that takes 38-52 minutes - will be coded as 45 minutes. The code for a 60 minute session will require the session to be at least 53 minutes long.
- The Psychology of Torture
- Alternative Therapies Mental Health Improvement
- Therapy with a Real Trauma Doctor: Part One
- Sorry Wounded Healers
- Positive Psychology in Martial Arts
medications, E/M codes will be required for each appointment, and the code for pharmacological management will be cancelled. Time spent on medication and education should not be included in total psychotherapy time if the psychiatrist is doing both, so two codes would be used for the same visit and services offered in the same appointment should be different. You have it, right? The E/M codes will allow for five different levels of difficulty and will require the psychiatrist to provide specific documentation regarding history, expertise, and medical decision making. After analyzing all of this, I still haven't figured out the E/M codes and don't know what codes to use for my typical 50 minute psychotherapy session, which I think will now be 53 minutes, or maybe 38 minutes, which might be billed for 45 minutes – plus an added indefinite period of time required to complete the E/M medication related service once the level of difficulty has been determined. There will also be codes for crisis management and difficult family situations. Simply put, there will now be approximately 17 different ways to code a 50-minute drug management psychotherapy session, depending on what is said in the session, and each combination will give a different pay. There doesn't seem to be a code for the time spent figuring out the correct code for each session, or any concern that these issues might distract physicians from the concerns of patient care.
You have it, right? The E/M codes will allow for five different levels of difficulty and will require the psychiatrist to provide specific documentation regarding history, expertise, and medical decision making. After analyzing all of this, I still haven't figured out the E/M codes and don't know what codes to use for my typical 50 minute psychotherapy session, which I think will now be 53 minutes, or maybe 38 minutes, which might be billed for 45 minutes – plus an added indefinite period of time required to complete the E/M medication related service once the level of difficulty has been determined. There will also be codes for crisis management and difficult family situations. Simply put, there will now be approximately 17 different ways to code a 50-minute drug management psychotherapy session, depending on what is said in the session, and each combination will give a different pay. There doesn't seem to be a code for the time spent figuring out the correct code for each session, or any concern that these issues might distract physicians from the concerns of patient care.
So what does this mean for mentally healthy practitioners and for patients who are receiving treatment? I think these changes will eventually become easy enough for those who offer only psychotherapy or only treatment. For psychiatrists, there is hope that coding will better understand what we are really doing and allow us to appreciate the complexity that distinguishes psychiatry from other mental health specialties. The fear is that these changes will create a lot of confusion, especially in the first place, and they promise to increase the paperwork burden and worry about inadvertently fraudulent claims.
Six weeks before implementation, tens of thousands of individual clinicians, administrators and institutions still need to be trained and then fine-tuned in the way they practice, document and pay.
I suspect that we are in a transitional phase and that appointments will be sent with incorrect reject-only codes. Eventually, kinks will be developed, but the new system promises to be more cumbersome.
For a physician who participates in health insurance networks, payments may increase, and for those who do not participate, these changes may allow their patients to receive better reimbursement for out-of-network services. So far, though, that doesn't look good, at least not for Medicare providers and recipients. The 2013 Medicare fee schedule, released last week, shows that reimbursement for psychiatric assessments through medical services - those done by psychiatrists - will be lower than reimbursement for psychiatric assessments by social workers and psychologists. And timed psychotherapy provided by psychiatrists who also provide E/M services will be reimbursed at a lower rate than psychotherapy provided by those who do not deal with medical issues. This does not make sense and seems to contradict the premise that the creation of a comprehensive service coding system would promote understanding of the complexity of the medical aspects of treating mental disorders, parity of treatment, and reducing the stigma to see a psychiatrist.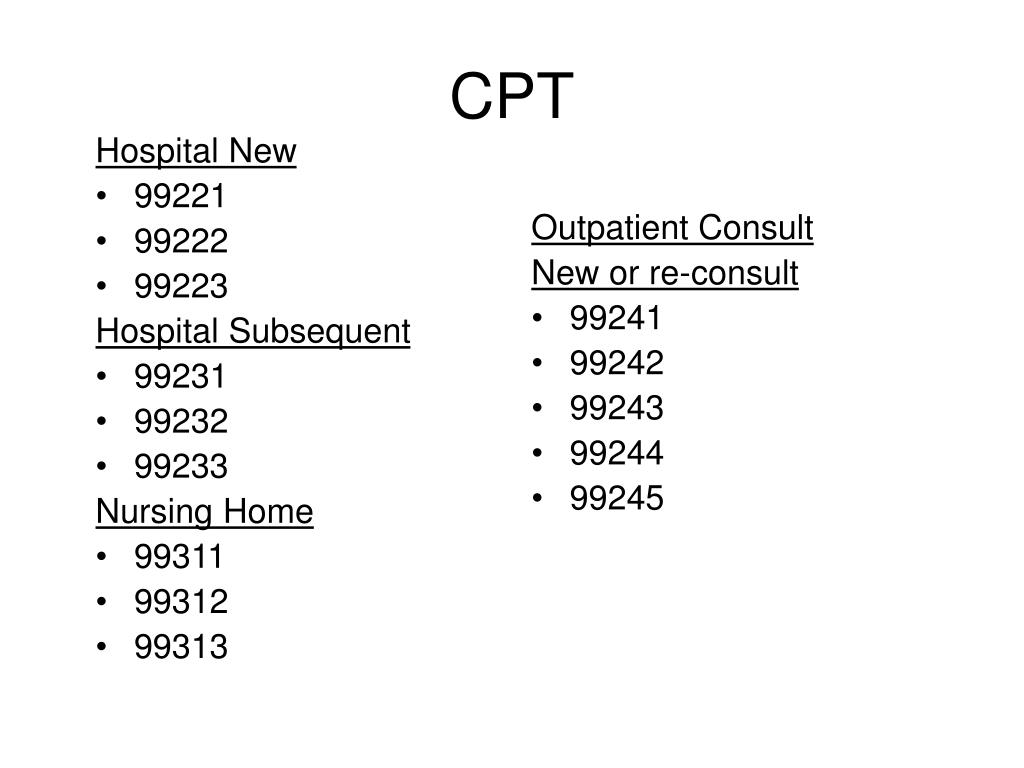
I talked about this a little more with pros and cons on KevinMD, here .
You now have 38 minutes.
Dina Miller, MD, is a psychiatrist in Baltimore. She co-authored Shrink Rap: Three Psychiatrists Explain Their Work
Partner Center Billing Overview
- Article
- Reading takes 5 minutes
Associated Roles : Admin Agent | billing administrator | global administrator | technical support agent | sales agent
This article provides basic billing and billing information for CSP partners in Partner Center, including:
- Account search
- Invoicing to customers
- Accounts
- Price lists
- Terms of payment
- Taxes and VAT
- Adjustments/credits/cancellations
- Credit notes
- Next steps
Find an account
To find an account in Partner Center, follow these steps.
-
Sign in to Partner Center and select Billing .
-
Download the latest invoice or previous invoices in section Billing log .
Customer billing
Microsoft does not impose any requirements or conditions on your billing management practices.
Review the reconciliation files to determine customer transactions. Use the customer name and other relevant fields to identify transactions.
Billing types
Partner Center billing types:
- License-based billing
- Billing based on usage
- One-time billing
Invoice currency
Billing based on licenses and usage . Products are billed in the currency of the country or region where you are located. Billing is the same regardless of the location of the customer you sold products to.
One time billing . You are billed in the partner's location currency, regardless of the location of the customer you sold products to. For more information, see New Commerce Model in CSP - Azure Billing.
For more information, see New Commerce Model in CSP - Azure Billing.
Invoices
An invoice is a summary of all charges for the current billing period.
The summary includes costs for the program, all products, and all clients.
For examples of monthly and yearly billing scenarios, see Common Billing Scenarios.
-
Billing based on usage and licenses:
-
The invoice will be available within two days after the selected UTC billing date.
For example, if you have a billing date of September 12, invoice generation starts at 12:00 UTC on September 13 and ends at 12:00 UTC on September 14.
-
-
One time and recurring billing:
- The billing period is compared with the calendar month.
- Account and reconciliation files are available no later than the eighth of each month.
- For more information, see Azure plan billing.
- Any product purchased next to
"New Commerce Experience"must be listed on this invoice.
Price lists
Price lists are updated monthly.
Preview price lists are available one month in advance.
To view the latest Cloud Solution Provider programs and offerings:
The following price lists are available on page Price lists :
-
Prices based on the license are guaranteed for the duration of the subscription, typically 12 months from the date of purchase.
-
Usage-based prices may change on a monthly basis.
-
Prices for products, services and software subscriptions are guaranteed for the duration of the subscription. However, prices may change upon renewal.
Adjustments and credits arrears appear on the next billing invoice after the credit or adjustment is applied.
Terms of payment
Terms of payment — exactly 60 days.
Invoices must be paid by the invoice due date (60 days after the invoice date) or your account will expire, which may affect your CSP enrollment.
You can restore suspended accounts to full functionality by paying overdue invoices.
After you provide corrected billing information, your payment will appear in the Billing workspace in Partner Center within five business days.
Taxes and VAT
You are taxed based on your data, not customer information, because the billing relationship is with you and Microsoft.
You can submit your tax identification code during account setup or by contacting support later. You will see any changes reflected in the next billing cycle.
For tax deduction and sales tax exemption, you must submit tax documentation by contacting support. Changes and related refunds will be reflected in the next billing cycle. See information about submitting income tax.
For Value Added Tax (VAT) exemption , you must submit your VAT identification number (verified by Microsoft) via a support ticket.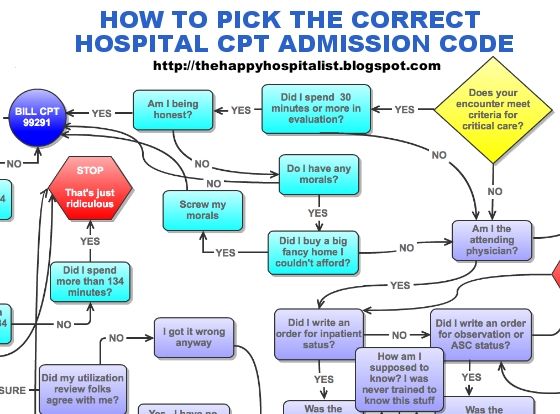 If a VAT ID is submitted (via a support request) after the account is set up, your pre-request invoices will not include the VAT ID in the invoice PDF. You will see the changes in your next billing cycle.
If a VAT ID is submitted (via a support request) after the account is set up, your pre-request invoices will not include the VAT ID in the invoice PDF. You will see the changes in your next billing cycle.
For more information about taxes, contact your local tax office or tax advisor.
Adjustments/Credits/Cancellations
License Cancellation Credits are prorated for unused days for mid-cycle cancellations (and reductions in licenses) according to the following formula:
[ROUND((ROUND(Unit Price * Quantity / Number of days in prorated Month, 2) * Number of prorated days) / Quantity, 2) * Quantity]
Billing rules
There are two types of billing frequency: annual and monthly.
Rates for capped services are subject to change during the billing cycle.
Annual billing rules
-
Subscriptions are valid for a year and automatically renew.
-
Billing occurs as 12 monthly payments or an annual invoice for an annual subscription.
-
Billing in advance for the next billing period for license-based services based on the number of licenses at the end of the previous billing period.
-
You are billed for any changes in the number of licenses (prorated calculation based on license days). The following formula is used to calculate pro rata:
[ROUND((ROUND(Unit Price * Quantity / Number of days in prorated Month, 2) * Number of prorated days) / Quantity, 2) * Quantity] -
Payment is for licenses sold, not prepared.
Monthly billing rules
-
Subscriptions are valid from month to month and automatically renew at the new rates for metered services. You are billed each month for the previous month's usage.
-
Rate cap services are subject to change during the billing cycle.
-
The invoice you receive only contains expenses that accrue during this month.
Credit Notes
You may need to request a credit or re-invoice for the following reasons:
-
You need to make changes to your address or purchase order.
Learn more