Psychiatric diagnosis definition
Mental illness - Diagnosis and treatment
Diagnosis
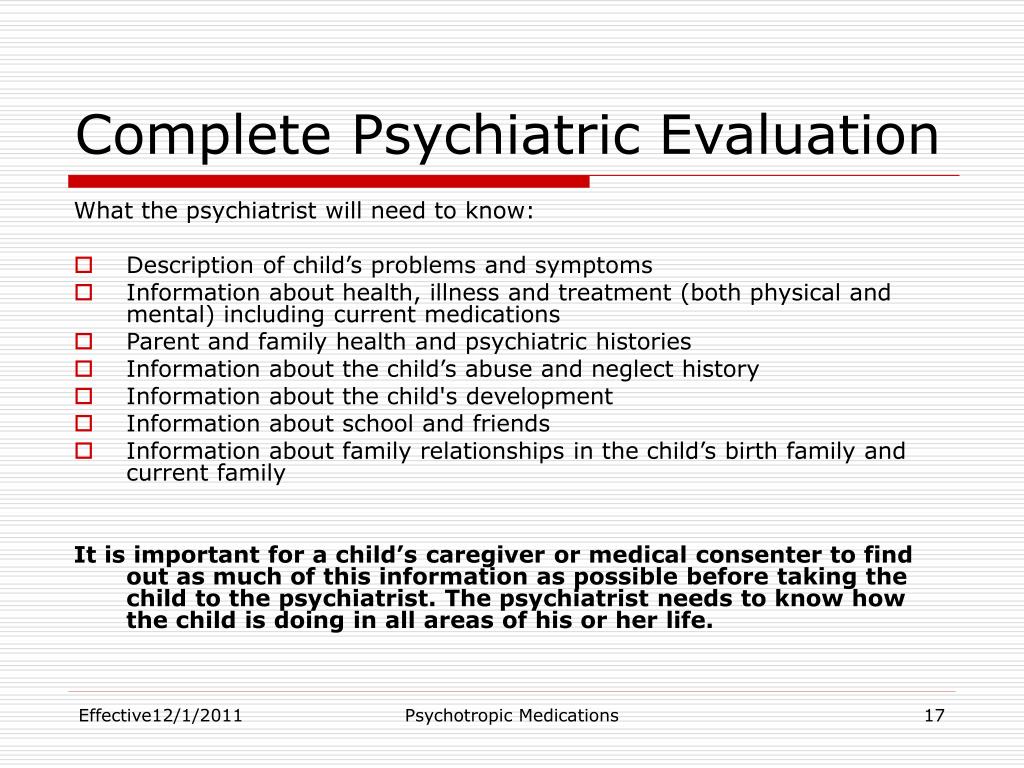
To determine a diagnosis and check for related complications, you may have:
- A physical exam. Your doctor will try to rule out physical problems that could cause your symptoms.
- Lab tests. These may include, for example, a check of your thyroid function or a screening for alcohol and drugs.
- A psychological evaluation. A doctor or mental health professional talks to you about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
Determining which mental illness you have
Sometimes it's difficult to find out which mental illness may be causing your symptoms. But taking the time and effort to get an accurate diagnosis will help determine the appropriate treatment. The more information you have, the more you will be prepared to work with your mental health professional in understanding what your symptoms may represent.
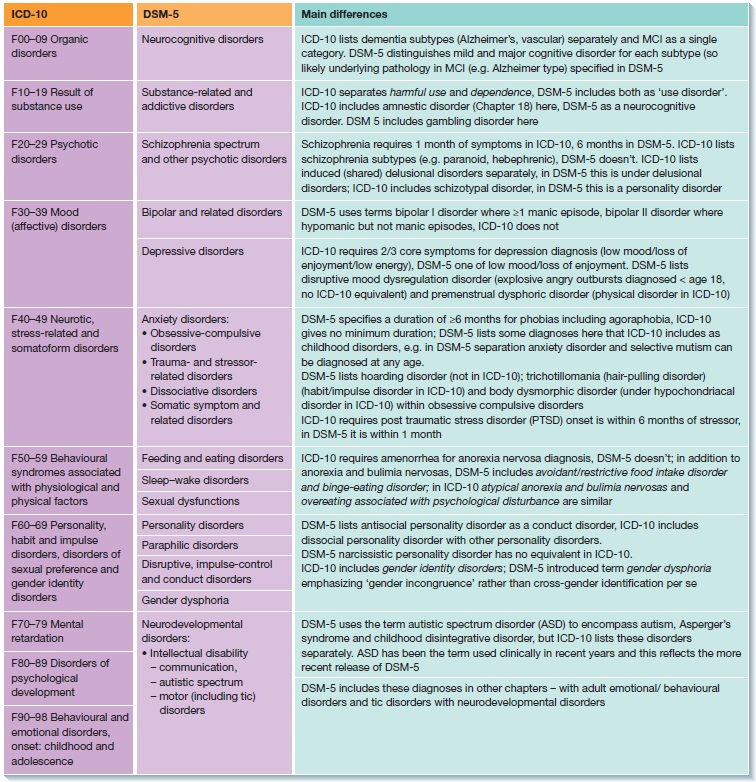
The defining symptoms for each mental illness are detailed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. This manual is used by mental health professionals to diagnose mental conditions and by insurance companies to reimburse for treatment.
Classes of mental illness
The main classes of mental illness are:
- Neurodevelopmental disorders. This class covers a wide range of problems that usually begin in infancy or childhood, often before the child begins grade school. Examples include autism spectrum disorder, attention-deficit/hyperactivity disorder (ADHD) and learning disorders.
- Schizophrenia spectrum and other psychotic disorders. Psychotic disorders cause detachment from reality — such as delusions, hallucinations, and disorganized thinking and speech. The most notable example is schizophrenia, although other classes of disorders can be associated with detachment from reality at times.

- Bipolar and related disorders. This class includes disorders with alternating episodes of mania — periods of excessive activity, energy and excitement — and depression.
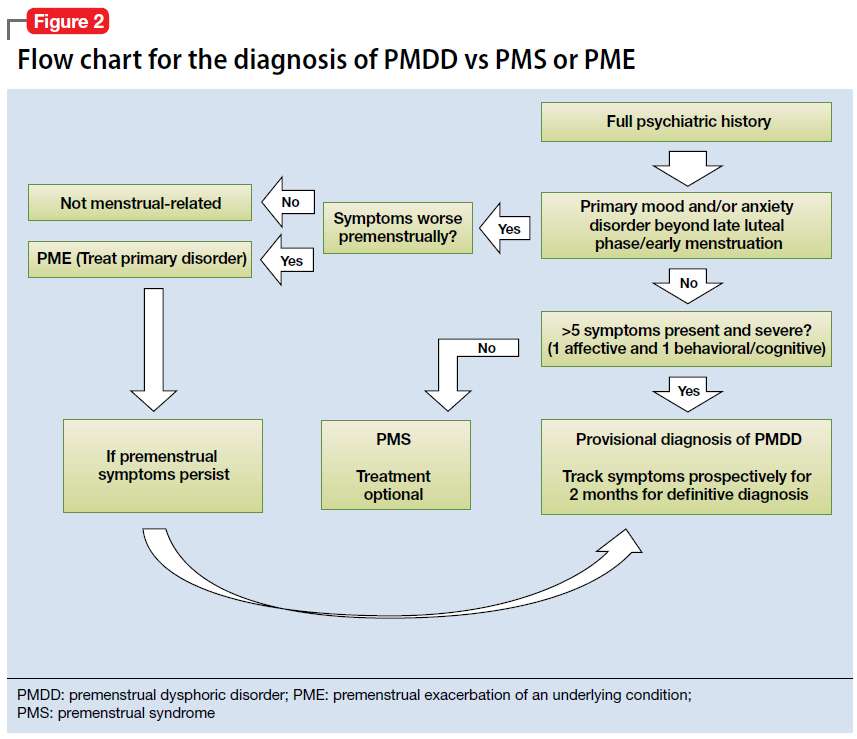
- Depressive disorders. These include disorders that affect how you feel emotionally, such as the level of sadness and happiness, and they can disrupt your ability to function. Examples include major depressive disorder and premenstrual dysphoric disorder.
- Anxiety disorders. Anxiety is an emotion characterized by the anticipation of future danger or misfortune, along with excessive worrying. It can include behavior aimed at avoiding situations that cause anxiety. This class includes generalized anxiety disorder, panic disorder and phobias.
- Obsessive-compulsive and related disorders. These disorders involve preoccupations or obsessions and repetitive thoughts and actions. Examples include obsessive-compulsive disorder, hoarding disorder and hair-pulling disorder (trichotillomania).
- Trauma- and stressor-related disorders. These are adjustment disorders in which a person has trouble coping during or after a stressful life event. Examples include post-traumatic stress disorder (PTSD) and acute stress disorder.
- Dissociative disorders. These are disorders in which your sense of self is disrupted, such as with dissociative identity disorder and dissociative amnesia.
- Somatic symptom and related disorders. A person with one of these disorders may have physical symptoms that cause major emotional distress and problems functioning. There may or may not be another diagnosed medical condition associated with these symptoms, but the reaction to the symptoms is not normal. The disorders include somatic symptom disorder, illness anxiety disorder and factitious disorder.
- Feeding and eating disorders. These disorders include disturbances related to eating that impact nutrition and health, such as anorexia nervosa and binge-eating disorder.

- Elimination disorders. These disorders relate to the inappropriate elimination of urine or stool by accident or on purpose. Bed-wetting (enuresis) is an example.
- Sleep-wake disorders. These are disorders of sleep severe enough to require clinical attention, such as insomnia, sleep apnea and restless legs syndrome.
- Sexual dysfunctions. These include disorders of sexual response, such as premature ejaculation and female orgasmic disorder.
- Gender dysphoria. This refers to the distress that accompanies a person's stated desire to be another gender.
- Disruptive, impulse-control and conduct disorders. These disorders include problems with emotional and behavioral self-control, such as kleptomania or intermittent explosive disorder.
- Substance-related and addictive disorders. These include problems associated with the excessive use of alcohol, caffeine, tobacco and drugs.
 This class also includes gambling disorder.
This class also includes gambling disorder. - Neurocognitive disorders. Neurocognitive disorders affect your ability to think and reason. These acquired (rather than developmental) cognitive problems include delirium, as well as neurocognitive disorders due to conditions or diseases such as traumatic brain injury or Alzheimer's disease.
- Personality disorders. A personality disorder involves a lasting pattern of emotional instability and unhealthy behavior that causes problems in your life and relationships. Examples include borderline, antisocial and narcissistic personality disorders.
- Paraphilic disorders. These disorders include sexual interest that causes personal distress or impairment or causes potential or actual harm to another person. Examples are sexual sadism disorder, voyeuristic disorder and pedophilic disorder.
- Other mental disorders. This class includes mental disorders that are due to other medical conditions or that don't meet the full criteria for one of the above disorders.
Treatment
Your treatment depends on the type of mental illness you have, its severity and what works best for you. In many cases, a combination of treatments works best.
If you have a mild mental illness with well-controlled symptoms, treatment from your primary care provider may be sufficient. However, often a team approach is appropriate to make sure all your psychiatric, medical and social needs are met. This is especially important for severe mental illnesses, such as schizophrenia.
Your treatment team
Your treatment team may include your:
- Family or primary care doctor
- Nurse practitioner
- Physician assistant
- Psychiatrist, a medical doctor who diagnoses and treats mental illnesses
- Psychotherapist, such as a psychologist or a licensed counselor
- Pharmacist
- Social worker
- Family members
Medications
Although psychiatric medications don't cure mental illness, they can often significantly improve symptoms. Psychiatric medications can also help make other treatments, such as psychotherapy, more effective. The best medications for you will depend on your particular situation and how your body responds to the medication.
Psychiatric medications can also help make other treatments, such as psychotherapy, more effective. The best medications for you will depend on your particular situation and how your body responds to the medication.
Some of the most commonly used classes of prescription psychiatric medications include:
- Antidepressants. Antidepressants are used to treat depression, anxiety and sometimes other conditions. They can help improve symptoms such as sadness, hopelessness, lack of energy, difficulty concentrating and lack of interest in activities. Antidepressants are not addictive and do not cause dependency.
- Anti-anxiety medications. These drugs are used to treat anxiety disorders, such as generalized anxiety disorder or panic disorder. They may also help reduce agitation and insomnia. Long-term anti-anxiety drugs typically are antidepressants that also work for anxiety. Fast-acting anti-anxiety drugs help with short-term relief, but they also have the potential to cause dependency, so ideally they'd be used short term.
- Mood-stabilizing medications. Mood stabilizers are most commonly used to treat bipolar disorders, which involves alternating episodes of mania and depression. Sometimes mood stabilizers are used with antidepressants to treat depression.
- Antipsychotic medications. Antipsychotic drugs are typically used to treat psychotic disorders, such as schizophrenia. Antipsychotic medications may also be used to treat bipolar disorders or used with antidepressants to treat depression.
Psychotherapy
Psychotherapy, also called talk therapy, involves talking about your condition and related issues with a mental health professional. During psychotherapy, you learn about your condition and your moods, feelings, thoughts and behavior. With the insights and knowledge you gain, you can learn coping and stress management skills.
There are many types of psychotherapy, each with its own approach to improving your mental well-being. Psychotherapy often can be successfully completed in a few months, but in some cases, long-term treatment may be needed. It can take place one-on-one, in a group or with family members.
Psychotherapy often can be successfully completed in a few months, but in some cases, long-term treatment may be needed. It can take place one-on-one, in a group or with family members.
When choosing a therapist, you should feel comfortable and be confident that he or she is capable of listening and hearing what you have to say. Also, it's important that your therapist understands the life journey that has helped shape who you are and how you live in the world.
Brain-stimulation treatments
Brain-stimulation treatments are sometimes used for depression and other mental health disorders. They're generally reserved for situations in which medications and psychotherapy haven't worked. They include electroconvulsive therapy, repetitive transcranial magnetic stimulation, deep brain stimulation and vagus nerve stimulation.
Make sure you understand all the risks and benefits of any recommended treatment.
Hospital and residential treatment programs
Sometimes mental illness becomes so severe that you need care in a psychiatric hospital. This is generally recommended when you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else.
This is generally recommended when you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else.
Options include 24-hour inpatient care, partial or day hospitalization, or residential treatment, which offers a temporary supportive place to live. Another option may be intensive outpatient treatment.
Substance misuse treatment
Problems with substance use commonly occur along with mental illness. Often it interferes with treatment and worsens mental illness. If you can't stop using drugs or alcohol on your own, you need treatment. Talk to your doctor about treatment options.
Participating in your own care
Working together, you and your primary care provider or mental health professional can decide which treatment may be best, depending on your symptoms and their severity, your personal preferences, medication side effects, and other factors. In some cases, a mental illness may be so severe that a doctor or loved one may need to guide your care until you're well enough to participate in decision-making.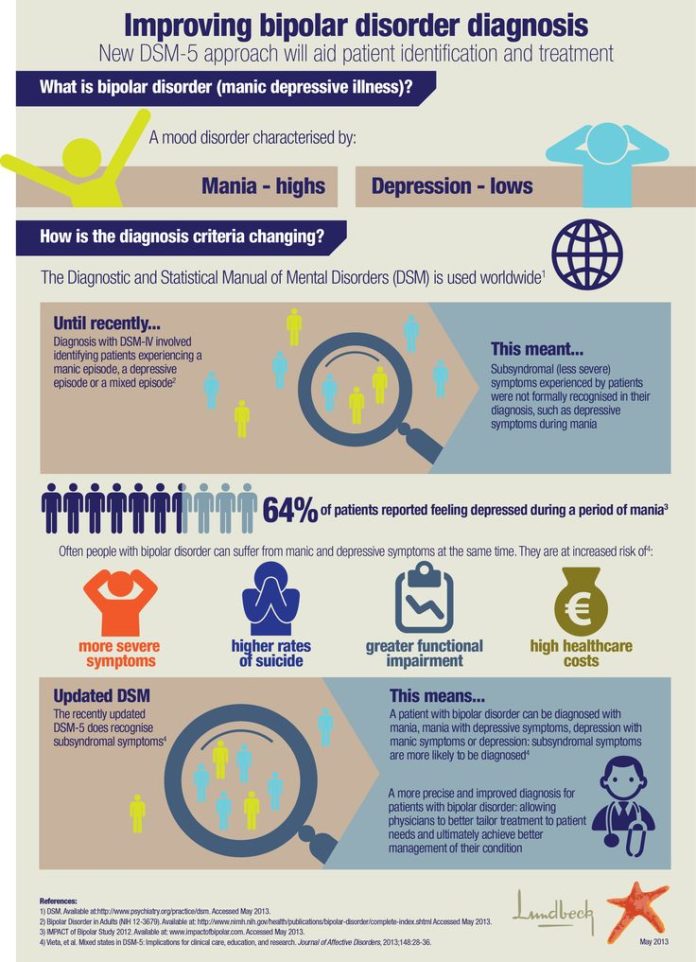
More Information
- Mental health providers: Tips on finding one
- Deep brain stimulation
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.
To provide you with the most relevant and helpful information, and understand which
information is beneficial, we may combine your email and website usage information with
other information we have about you. If you are a Mayo Clinic patient, this could
include protected health information. If we combine this information with your protected
health information, we will treat all of that information as protected health
information and will only use or disclose that information as set forth in our notice of
privacy practices.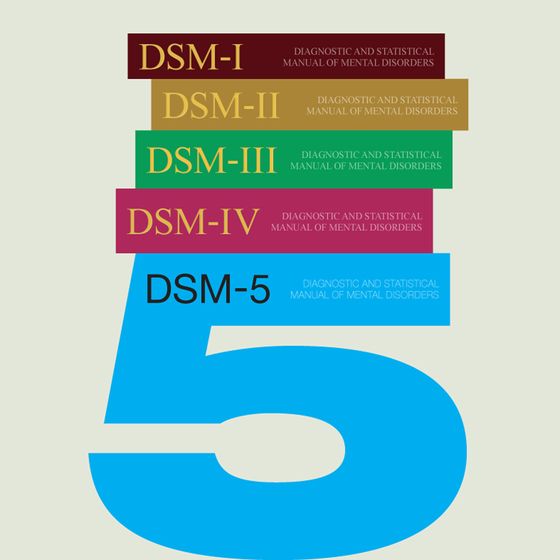 You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
You may opt-out of email communications at any time by clicking on
the unsubscribe link in the e-mail.
Lifestyle and home remedies
In most cases, a mental illness won't get better if you try to treat it on your own without professional care. But you can do some things for yourself that will build on your treatment plan:
- Stick to your treatment plan. Don't skip therapy sessions. Even if you're feeling better, don't skip your medications. If you stop, symptoms may come back. And you could have withdrawal-like symptoms if you stop a medication too suddenly. If you have bothersome drug side effects or other problems with treatment, talk to your doctor before making changes.
- Avoid alcohol and drug use. Using alcohol or recreational drugs can make it difficult to treat a mental illness. If you're addicted, quitting can be a real challenge. If you can't quit on your own, see your doctor or find a support group to help you.
- Stay active. Exercise can help you manage symptoms of depression, stress and anxiety. Physical activity can also counteract the effects of some psychiatric medications that may cause weight gain. Consider walking, swimming, gardening or any form of physical activity that you enjoy. Even light physical activity can make a difference.
- Make healthy choices. Maintaining a regular schedule that includes sufficient sleep, healthy eating and regular physical activity are important to your mental health.
- Don't make important decisions when your symptoms are severe. Avoid decision-making when you're in the depth of mental illness symptoms, since you may not be thinking clearly.
- Determine priorities. You may reduce the impact of your mental illness by managing time and energy. Cut back on obligations when necessary and set reasonable goals. Give yourself permission to do less when symptoms are worse.
 You may find it helpful to make a list of daily tasks or use a planner to structure your time and stay organized.
You may find it helpful to make a list of daily tasks or use a planner to structure your time and stay organized. - Learn to adopt a positive attitude. Focusing on the positive things in your life can make your life better and may even improve your health. Try to accept changes when they occur, and keep problems in perspective. Stress management techniques, including relaxation methods, may help.
Coping and support
Coping with a mental illness is challenging. Talk to your doctor or therapist about improving your coping skills, and consider these tips:
- Learn about your mental illness. Your doctor or therapist can provide you with information or may recommend classes, books or websites. Include your family, too — this can help the people who care about you understand what you're going through and learn how they can help.
- Join a support group. Connecting with others facing similar challenges may help you cope.
 Support groups for mental illness are available in many communities and online. One good place to start is the National Alliance on Mental Illness.
Support groups for mental illness are available in many communities and online. One good place to start is the National Alliance on Mental Illness. - Stay connected with friends and family. Try to participate in social activities, and get together with family or friends regularly. Ask for help when you need it, and be upfront with your loved ones about how you're doing.
- Keep a journal. Or jot down brief thoughts or record symptoms on a smartphone app. Keeping track of your personal life and sharing information with your therapist can help you identify what triggers or improves your symptoms. It's also a healthy way to explore and express pain, anger, fear and other emotions.
Preparing for your appointment
Whether you schedule an appointment with your primary care provider to talk about mental health concerns or you're referred to a mental health professional, such as a psychiatrist or psychologist, take steps to prepare for your appointment.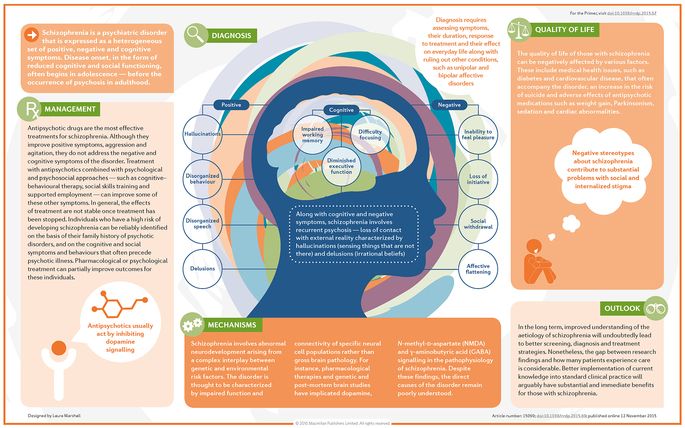
If possible, take a family member or friend along. Someone who has known you for a long time may be able to share important information, with your permission.
What you can do
Before your appointment, make a list of:
- Any symptoms you or people close to you have noticed, and for how long
- Key personal information, including traumatic events in your past and any current, major stressors
- Your medical information, including other physical or mental health conditions
- Any medications, vitamins, herbal products or other supplements you take, and their dosages
- Questions to ask your doctor or mental health professional
Questions to ask may include:
- What type of mental illness might I have?
- Why can't I get over mental illness on my own?
- How do you treat my type of mental illness?
- Will talk therapy help?
- Are there medications that might help?
- How long will treatment take?
- What can I do to help myself?
- Do you have any brochures or other printed material that I can have?
- What websites do you recommend?
Don't hesitate to ask any other questions during your appointment.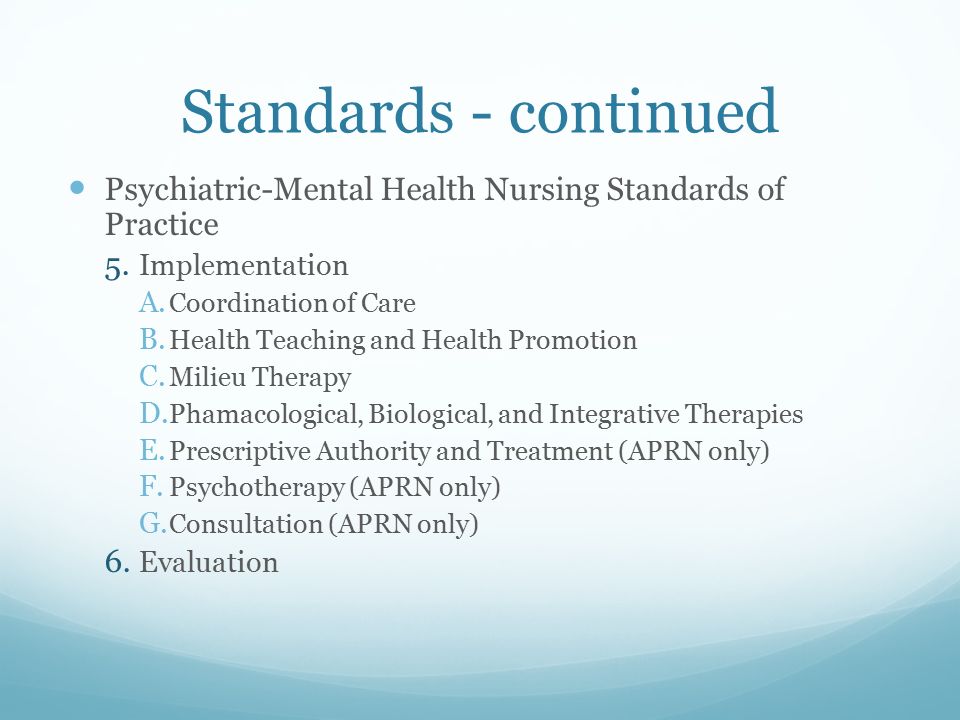
What to expect from your doctor
During your appointment, your doctor or mental health professional is likely to ask you questions about your mood, thoughts and behavior, such as:
- When did you first notice symptoms?
- How is your daily life affected by your symptoms?
- What treatment, if any, have you had for mental illness?
- What have you tried on your own to feel better or control your symptoms?
- What things make you feel worse?
- Have family members or friends commented on your mood or behavior?
- Do you have blood relatives with a mental illness?
- What do you hope to gain from treatment?
- What medications or over-the-counter herbs and supplements do you take?
- Do you drink alcohol or use recreational drugs?
Your doctor or mental health professional will ask additional questions based on your responses, symptoms and needs. Preparing and anticipating questions will help you make the most of your time with the doctor.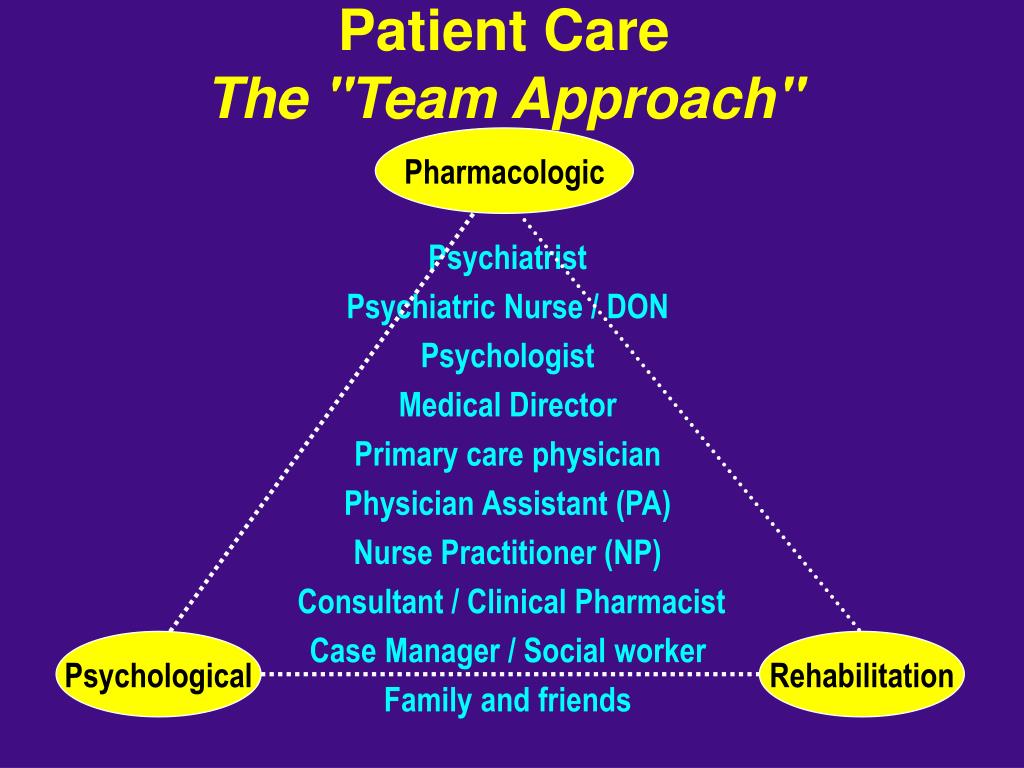
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
What Are Psychiatric Disorders? - San Diego
Your mental health affects every facet of your life: your relationships, your career, your self-esteem, and your ability to communicate effectively and contribute to your community. If your mental health is suffering, then other parts of your life will inevitably suffer, too.
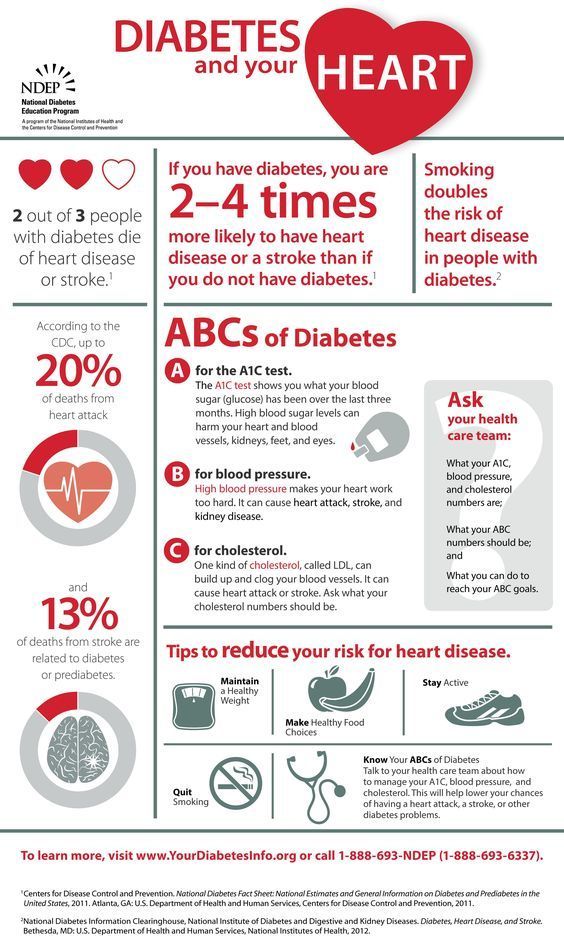
Despite the severe impact poor mental health can have on day-to-day living, so many people fail to seek treatment for their psychiatric disorders. According to a report from Mental Health America, over 40 million Americans are living with mental illness, yet more than half of them are not receiving proper treatment.
While the stigma associated with psychiatric disorders is real, it’s important to understand that mental illness is a common and highly treatable health condition. Since education is the first step toward erasing stigma, let’s explore exactly what a psychiatric disorder is, and how it can be overcome so you can live your life to the fullest.
A Broad Definition of Psychiatric Disorders
The American Psychiatric Association defines a mental health disorder as a medical problem, “involving:
- Significant changes in thinking, emotion, and/or behavior, and
- Distress and/or problems functioning in social, work, or family activities.”
This is a rather broad definition, essentially boiling psychiatric disorders down to problems that people experience with their minds and their moods. However, there are a number of specific diagnoses categorized under the larger umbrella of mental illness.
Different Types of Psychiatric Disorders
According to Mental Health America, there are over 200 classified types of psychiatric disorders, but some of the most frequently diagnosed ones are:
- Bipolar disorder
- Schizophrenia
- Borderline personality disorder
- Depression
- Generalized anxiety disorder
- Addictive disorders, including drug abuse, alcohol abuse, and behavioral addictions
These diagnoses aren’t mutually inclusive; it’s possible to be diagnosed with one or more simultaneously.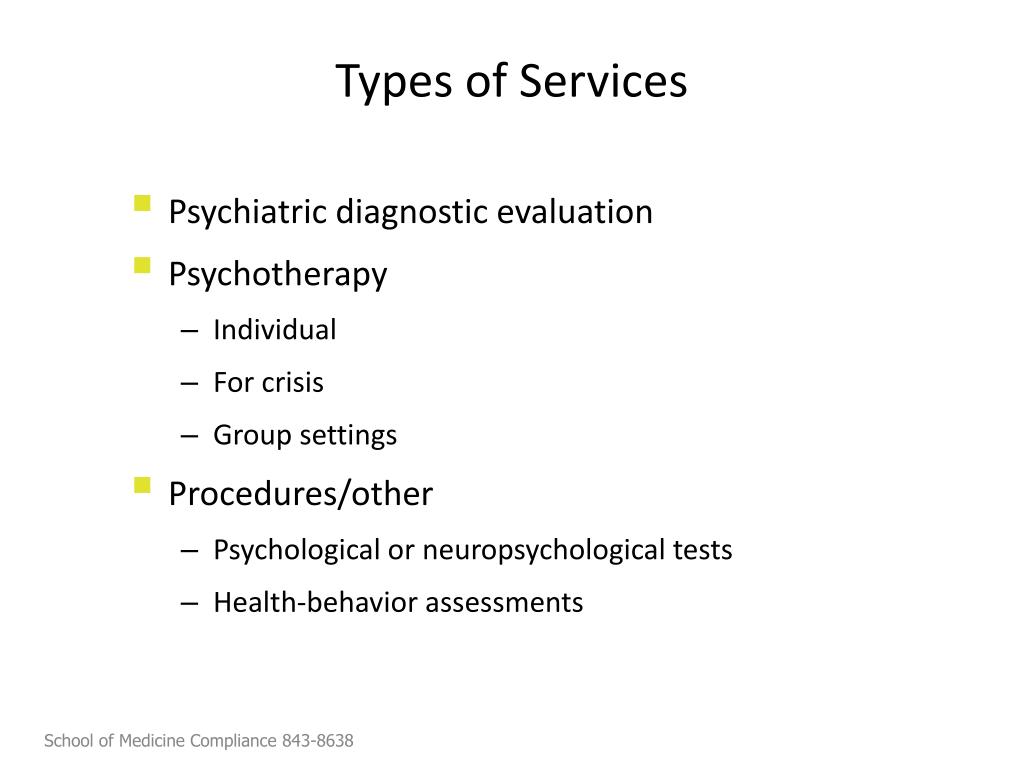 For example, addictive disorders often co-occur with another mental health disorder, such as depression or bipolar disorder.
For example, addictive disorders often co-occur with another mental health disorder, such as depression or bipolar disorder.
Common Symptoms of Psychiatric Disorders
Identifying mental illness can be challenging since it usually presents itself differently in different individuals. However, there are a few common warning signs to look out for.
- Extreme sadness
- Excessive worry
- Severe changes in mood
- Difficulty discerning reality from delusion
- Isolation and avoidance of friends or social activities
- Sudden changes in sleeping habits, eating habits, or sex drive
- Alcohol or drug abuse
- Suicidal thoughts
If you are experiencing any of these symptoms, it’s crucial to seek out help.
Treatment for Psychiatric Disorders
Treatment plans for psychiatric disorders vary depending on the exact diagnosis and the specific needs of the individual patient. Most reputable mental health hospitals will include some combination of the following in their course of treatment:
- Psychotherapy
Counseling sessions may take place either one-on-one or in a group setting with a licensed and trained mental health care professional. The goal of these sessions is to identify troublesome thoughts and behaviors, then develop strategies and coping mechanisms for handling them.
The goal of these sessions is to identify troublesome thoughts and behaviors, then develop strategies and coping mechanisms for handling them.
- Medication
Because psychiatric disorders are afflictions of the brain, many conditions may benefit from medication to relieve severe symptoms and help return thoughts and emotions to a manageable state.
- Aftercare
If you’re in residential treatment or a psychiatric hospital, an aftercare plan provides you with a road map for staying healthy when you’re back in the real world.
Alvarado Parkway Institute Can Help You Overcome Mental Illness
For over 35 years, Alvarado Parkway Institute has been a trusted name in California psych care. We understand the stigma and challenges associated with mental illness, and we are dedicated to helping our patients get the help they need to live healthy, fulfilling lives. With both inpatient and outpatient mental health services, we develop customized treatment plans, complete with aftercare programs to ensure patient success over the long term.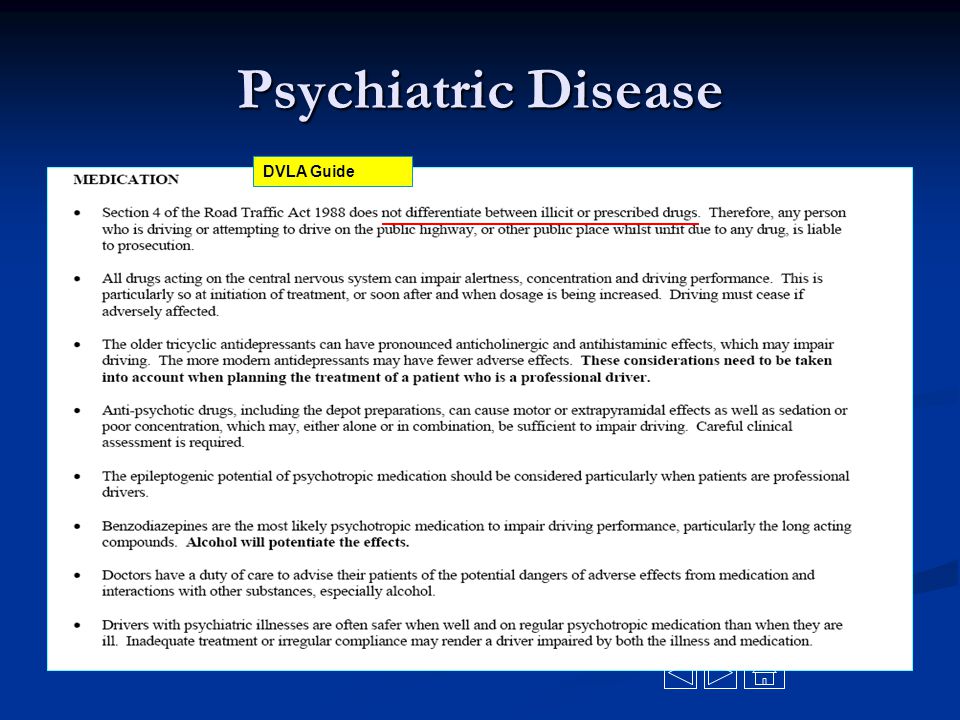
Call us at (619) 667-6125 and get on the road to wellness today.
Diagnosis and diagnosis in psychiatry — Center "Phoenix"
The variety of clinical manifestations of mental illness sometimes creates significant difficulties in determining the nosological affiliation of one or another psychopathological symptomatology ...
Methodology and research
symptoms (signs) of the disease. It is with the definition of individual signs of the disease that psychiatric diagnostics . At the same time, the relationship of this symptom to a particular syndrome and to the nosological form of the disease is identified.
So let's start with the concept of symptoms. Symptoms (The definition of signs of a mental disorder in our case corresponds to the international standard for the study of major mental illnesses adopted by the World Health Organization (WHO).), according to Jackson's well-known concept, are divided into negative and positive. The former include symptoms of the loss of certain functions of mental activity (exhaustion of mental activity, psychopathization of the personality, a decrease in energy potential, dementia). Positive, or productive, symptoms are the result of painful excitation of functional systems (illusions, hallucinations, delusional and obsessive ideas, manic and depressive states, etc.). Negative symptoms (minus symptoms) are nosologically more specific than productive ones (plus symptoms). At the same time, it is inert, invariant and relatively resistant to therapy. Negative and positive violations, despite the fact that they differ from each other, are closely interconnected. The clear severity of negative symptoms entails the rudimentary manifestations of positive ones. The slow, chronic course of the disease is accompanied by the prevalence of negative symptoms, the acute development of psychosis is accompanied by pronounced productive disorders. Productive symptoms are especially clearly manifested in psychoses associated with a disorder of consciousness (amental, delirious, oneiric, etc.
The former include symptoms of the loss of certain functions of mental activity (exhaustion of mental activity, psychopathization of the personality, a decrease in energy potential, dementia). Positive, or productive, symptoms are the result of painful excitation of functional systems (illusions, hallucinations, delusional and obsessive ideas, manic and depressive states, etc.). Negative symptoms (minus symptoms) are nosologically more specific than productive ones (plus symptoms). At the same time, it is inert, invariant and relatively resistant to therapy. Negative and positive violations, despite the fact that they differ from each other, are closely interconnected. The clear severity of negative symptoms entails the rudimentary manifestations of positive ones. The slow, chronic course of the disease is accompanied by the prevalence of negative symptoms, the acute development of psychosis is accompanied by pronounced productive disorders. Productive symptoms are especially clearly manifested in psychoses associated with a disorder of consciousness (amental, delirious, oneiric, etc. ), as well as in other conditions accompanied by psychomotor agitation (catatonic, hebephrenic, etc.) and acute hallucinatory-delusional symptoms.
), as well as in other conditions accompanied by psychomotor agitation (catatonic, hebephrenic, etc.) and acute hallucinatory-delusional symptoms.
The concept of "negative" and "positive" disorders, although they are among the cardinal in general psychopathology, is not always interpreted unambiguously. In particular, negative disorders are considered to be persistent, irreversible, and positive ones are considered temporary, dynamic, transient expressions of a mental defect. However, clinical studies in recent years have shown that with intensive antipsychotic treatment, reversibility and compensation of negative disorders is possible. Therefore, it should be considered that negative symptoms are associated not so much with the loss of mental functions, but with the temporary cessation of the functioning of individual systems.
Psychopathological symptoms similar in external manifestations may have a different diagnostic solution. For example, zoopsy occurs in patients with delirium tremens. As a rule, they see animals, insects reduced in size, somewhat elongated, black-headed. This indicates that these disorders belong specifically to alcoholic psychosis. At the same time, the brightness, colorfulness of hallucinatory phenomena with scenes of religious content or violent events indicates the possible presence of epileptic disease in patients. A similar comparison can be made with respect to auditory hallucinations in alcoholic and syphilitic hallucinosis, hallucinatory-paranoid schizophrenia; or violations of thinking in the form of its fragmentation (in schizophrenia) or incoherence (in an amental state).
As a rule, they see animals, insects reduced in size, somewhat elongated, black-headed. This indicates that these disorders belong specifically to alcoholic psychosis. At the same time, the brightness, colorfulness of hallucinatory phenomena with scenes of religious content or violent events indicates the possible presence of epileptic disease in patients. A similar comparison can be made with respect to auditory hallucinations in alcoholic and syphilitic hallucinosis, hallucinatory-paranoid schizophrenia; or violations of thinking in the form of its fragmentation (in schizophrenia) or incoherence (in an amental state).
However, individual symptoms do not provide sufficient information for a psychiatric diagnosis. Only the analysis of a number of signs of the disease, similar to each other in the clinical picture, that is, the allocation of disease syndromes, makes it possible to determine the clinical boundaries of a particular process. Syndromic diagnosis is more accurate than symptomatic.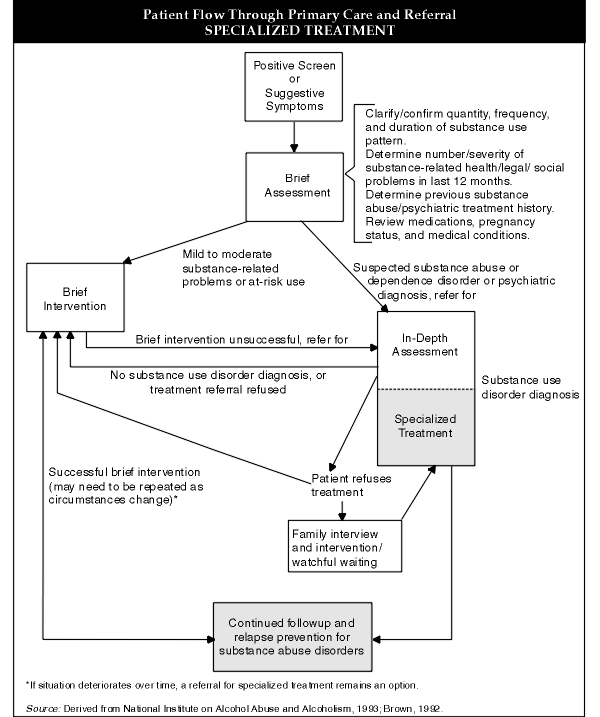 The syndrome reflects the activity of an entire functional system and, as a rule, is closely related to other syndromes.
The syndrome reflects the activity of an entire functional system and, as a rule, is closely related to other syndromes.
Regulation diagnosis is the final stage of psychiatric diagnosis , which is carried out on the basis of a comprehensive analysis of psychopathological symptoms, individual personality traits, objective and subjective anamnesis data, disease dynamics and the results of paraclinical studies. However, for an accurate diagnosis of mental illness, it is not enough just to state pathological changes. To do this, it is necessary to study the etiology and pathogenesis of the disease.
The variety of clinical manifestations of various mental illnesses often creates exceptional difficulties in determining the nosological affiliation of one or another psychopathological symptomatology. In this case, the doctor uses the most important method for diagnosing mental illness - method of clinical observation . The doctor must see the patient, listen, examine him.
The doctor must see the patient, listen, examine him.
Unfortunately, in psychiatry, in contrast to other medical fields, there are fewer opportunities for the use of instrumental techniques that make it possible to directly study the organ affected by the pathological process - the brain. Therefore, in psychiatry, the main method of research is the clinical and psychopathological method. It made it possible to substantiate the nosolic specificity of schizophrenia, borderline neuropsychiatric disorders, a group of exogenous and coarse-organic psychoses, and also to create a modern classification of mental illnesses.
At the same time, biological research methods are also widely used in psychiatry. They are aimed primarily at establishing the causes and pathogenesis of mental illness. True, without the clinical identification of psychopathological conditions, it is impossible to correlate the results of biological studies with data relating to the prognosis and outcome of mental illness, as well as therapy, prevention and social rehabilitation. Nevertheless, the data of modern neurophysiology, biochemistry, genetics, and psychology provide valuable information for the correct diagnosis of mental illness.
Nevertheless, the data of modern neurophysiology, biochemistry, genetics, and psychology provide valuable information for the correct diagnosis of mental illness.
When making a clinical diagnosis of a mental illness, the clinician should take into account that it could change the patient's personality, and in determining its cause, the subjective anamnesis may not correspond to the data of an objective study. The factor that caused the disease in the future may not have any effect on its course, and it will develop according to its pathogenetic laws.
It should be said that the psychiatrist in his daily practical work constantly has to deal not only with various pathological phenomena of mental activity, but also with deviations of the patient's somatic functions, as well as with the complex interweaving of his interpersonal relationships.
Patients with a somato-neurological profile usually report more complaints to the doctor than mentally ill patients. The latter often do not complain at all and do not consider themselves sick for a long time.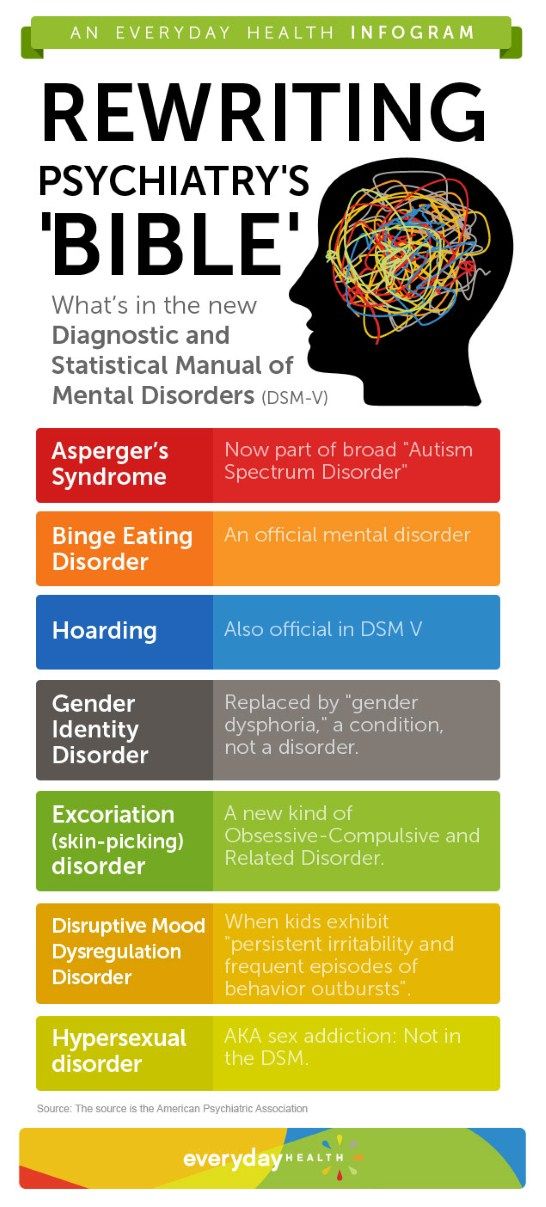 A mentally ill person often lacks the feeling of discomfort inherent in a somatically ill person. Mental illness can be asymptomatic for a long time or manifest itself with only one or two signs, which is fraught with a late diagnosis.
A mentally ill person often lacks the feeling of discomfort inherent in a somatically ill person. Mental illness can be asymptomatic for a long time or manifest itself with only one or two signs, which is fraught with a late diagnosis.
Psychiatric diagnostics is aimed at determining not only the nosological affiliation, stage of development and type of course of the disease, but also its prognosis in relation to life, recovery, and ability to work.
However, it should be remembered that the specificity of the clinical manifestations of various mental illnesses, in particular exogenous and endogenous psychoses, is very relative. Psychopathological symptoms can undergo a wide variety of changes depending on the premorbid properties of the personality, its constitutional features, and the nature of the impact of psychotraumatic situations. The most difficult to identify borderline neuropsychiatric disorders. They can develop not only as a reaction to a difficult situation, but also endogenously, they can be congenital and acquired. Here, the most difficult issue of psychiatric diagnosis is especially acute - the definition of norm and pathology. Signs of the endogenous course of the pathological process can also carry exogenous diseases - organic, reactive, various symptomatic psychoses.
Here, the most difficult issue of psychiatric diagnosis is especially acute - the definition of norm and pathology. Signs of the endogenous course of the pathological process can also carry exogenous diseases - organic, reactive, various symptomatic psychoses.
At the same time, the relativity of the specificity of mental disorders does not exclude the possibility of nosological diagnosis of diseases. The study in the aggregate of all signs expressing the unity of etiology and pathogenesis allows the clinician to determine the nosological independence of a particular disease. At the same time, both information about the patient himself and objective data about his relatives and social environment play a significant role. Of great difficulty is the solution of issues related to systematics in psychiatry. The classifications of mental illnesses that exist both in our country and abroad are to a certain extent conditional, since there is no consensus among psychiatrists from different countries in identifying individual psychopathological signs and in understanding the causes and mechanisms of development of many mental disorders.
The 10th revision of the International Classification of Diseases (ICD-10) is currently being adapted (In the United States, a national classification was introduced, which formed the basis of the ICD-10. The classification was first adopted by the American Psychiatric Association in 1952 and since then repeatedly DSM-III-R has been in force since 1987, and its 4th revision is currently being developed and used.). The classification of mental illness in the 10th revision has undergone significant changes compared to previous classifications. First of all, the number of diseases according to the nosological principles of division traditional in clinical psychiatry has been reduced and preference has been given to syndromic rubrics. The boundaries of schizophrenia are narrowed, the division of diseases into psychoses and neuroses is excluded, some new headings are introduced using original terminology that was not previously used. For example, throughout the classification, the term "disorder" is introduced instead of the terms "illness, illness". According to the authors of the classification, the term "disorder" is more accurate, since it refers to a more specific group of symptoms than is the case when using the concept of "disease".
According to the authors of the classification, the term "disorder" is more accurate, since it refers to a more specific group of symptoms than is the case when using the concept of "disease".
Source: New Psychiatry #1, 2010
Psychiatric Diagnosis - Reflections of a Psychoanalyst
“Aaah!!! The psychiatrist diagnosed me!!! - thoughts of a psychoanalyst.
“The psychologist referred her to a psychiatrist. The psychiatrist made the diagnosis. But she's not crazy!
An excerpt from one supervision
The term "mental disorder" most often means that the patient has some unpleasant experience for him for a sufficiently long amount of time. Diagnosis criteria - a list of necessary symptoms and their duration - are indicated in the international classifications of psychiatric syndromes. These criteria vary quite a lot from classification to classification. And I must say that symptoms that are similar in external manifestations do not always have the same causes.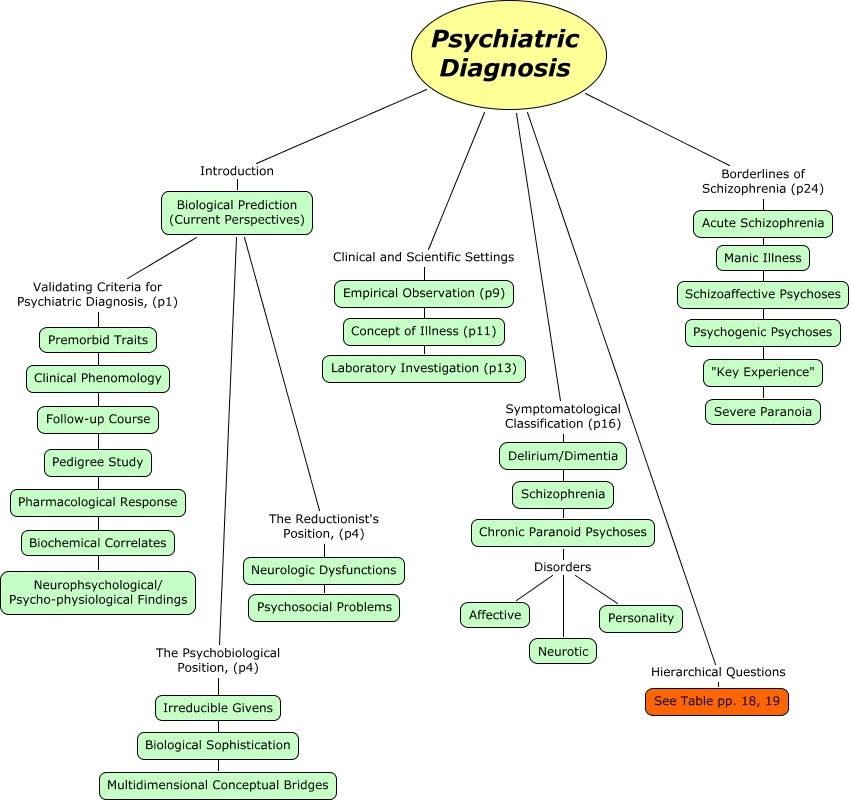
Over the years of the existence of psychiatry, doctors and researchers have listened to millions of complaints and traced millions of human destinies. And since psychiatry is a science, its followers designate a variety of normal and abnormal mental phenomena. Most often, as a diagnosis, you get the formulation of your own complaints in the language of modern psychiatry. And this does not mean that you are not normal. Life itself is the final judge for both you and psychiatrists: the main criterion for a person to have a mental disorder according to WHO requirements is social maladaptation. We are not far removed from Freud, who said that mental health is "the ability to love and work."
In their judgment of your psyche, psychiatrists are often deliberately superficial, because they judge you by external success: do you have a family, work, do you understand how to behave in society. Health is inseparable from the ability to establish human relationships (G.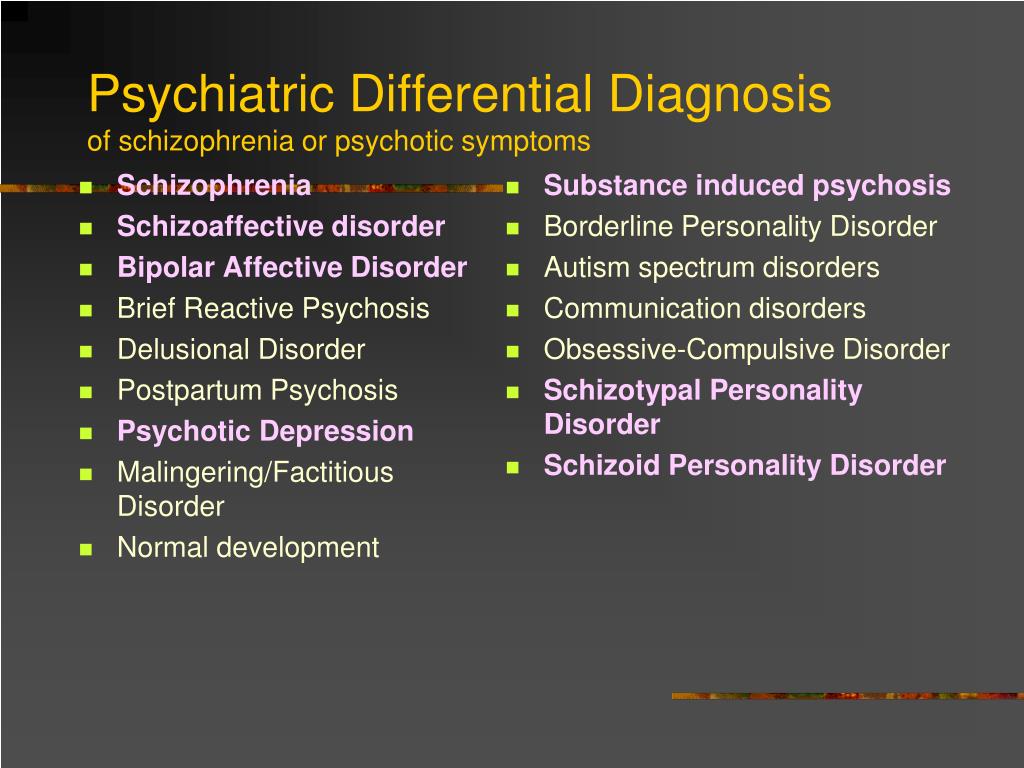 Ammon), and normal relationships with friends and relatives are your “alibi”.
Ammon), and normal relationships with friends and relatives are your “alibi”.
But sometimes life fails. Maybe you have a family and a job, but you are unhappy... And if you are lonely and not in demand with a sincere inner desire for relationships with other people and for self-realization?
And here the field of psychoanalysis begins, because psychoanalysis is about the inner.
1. Your psychiatric diagnosis is not your illness, but the illness of people in your early environment.
Society has changed a lot over the past century. Large families of traditional society have been replaced by nuclear families, society forces young mothers to go to work, and the lack of outdoor games deprives children of the opportunity to gain communication skills in a peer group. Under these conditions, it is very difficult for a child to grow up healthy: the mass disease of the Victorian era - neurosis - was replaced by more severe forms of mental pathology - borderline personality disorder, schizoid disorder, narcissism.
But many are still lucky, and they do not have gross character disorders. That is, since childhood, they have a certain mental integrity that allows these people to fully think and feel (it was in this original OKness of all people that Bern was convinced).
However, an unfavorable early environment (for example, depression, neurosis, or a personality disorder in your mother) can lead to the fact that the psyche, under the influence of real experience (and psychological messages from relatives), makes decisions about how you will interact with the world in the future.
Eric Berne called it prescriptions:
2. Your diagnosis most likely indicates that you are a sensitive, talented, sympathetic person. Mental illnesses often occur in people of creative professions, and just creative ones. This is due to the fact that many early decisions and personal adaptations occur precisely in children who are particularly sensitive to social interactions. Allis Miller, in The Tragedy of the Gifted Child, writes that dumb and under-receptive children will simply ignore the problems of social interaction with parents, and indeed parents.
Mental illnesses often occur in people of creative professions, and just creative ones. This is due to the fact that many early decisions and personal adaptations occur precisely in children who are particularly sensitive to social interactions. Allis Miller, in The Tragedy of the Gifted Child, writes that dumb and under-receptive children will simply ignore the problems of social interaction with parents, and indeed parents.
3. You are more mentally healthy than many people around you. Because you came to a psychotherapist.
Because you are reflecting on your life, trying to understand what is happening in life, and looking for the cause of your unhappiness in yourself, that is, you strive to take responsibility for your life on yourself, and do not blame your failures on other people or circumstances.
4. Maybe you just got unlucky. You have had too many traumas and too much pain in your life. Even the strongest (capable of both loving and working) people suffer for years from the consequences of life's catastrophes.
Even the strongest (capable of both loving and working) people suffer for years from the consequences of life's catastrophes.
| And time - it does not heal. It does not darn wounds, it simply closes them on top with a gauze bandage of new impressions, new sensations, life experience. And sometimes, clinging to something, this bandage flies off, and fresh air enters the wound, giving it new pain... and new life... Time is a bad doctor. It makes us forget about the pain of old wounds, inflicting more and more ... And so we crawl through life, like its wounded soldiers ... And every year the number of poorly applied bandages grows in my soul ... " Eric Maria Remarque |
Psychic trauma can only be healed through psychotherapy.
Mental health is not the absence of symptoms. This is an opportunity to follow the principle of reality (Z.