Tms therapy ocd
Deep TMS Treatment For OCD (Obsessive-Compulsive Disorder)
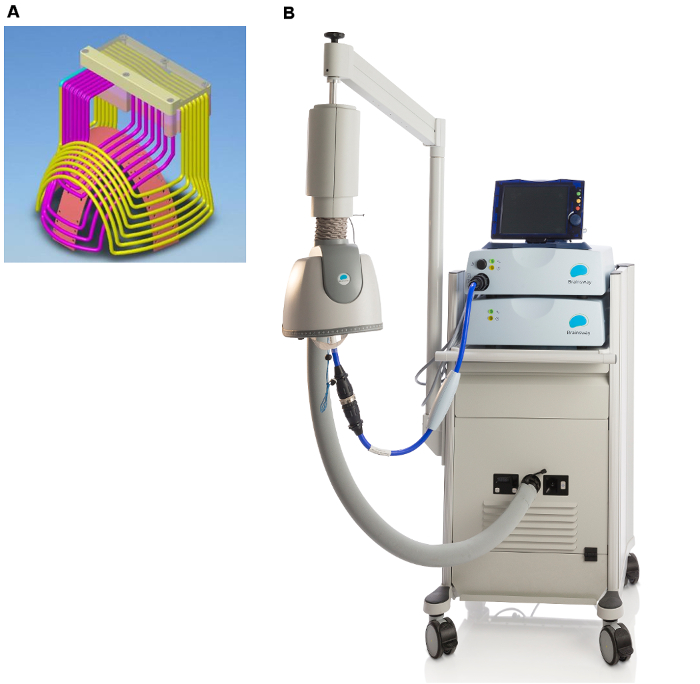
Introducing BrainsWay Deep TMS for OCD
Deep Transcranial Magnetic Stimulation, or Deep TMS™, has been shown to safely and effectively alleviate the symptoms of obsessive-compulsive disorder (OCD), particularly those patients who have not achieved sufficient improvement from traditional OCD treatment options.
The treatment utilizes a magnetic field emitted by BrainsWay’s patented H7-coil to directly reach broader and deeper brain regions than its predecessors, regulating the neural activity of brain structures associated with OCD – specifically the anterior cingulate cortex and medial prefrontal cortex.
A peer-reviewed multicenter clinical study found Deep TMS to be a highly effective OCD treatment, with more than one in three treatment-resistant OCD patients achieving “response”, greatly improving their quality of life.
As a noninvasive procedure, Deep TMS is a well-tolerated treatment that does not cause any adverse or long-lasting side effects. It does not require a significant recovery period, and the 18-min treatment can easily be integrated into each patient’s day-to-day schedule.
Obsessive-Compulsive Disorder: Key Points
Obsessive-compulsive disorder, or OCD, is a mental disorder defined as a combination of anxiety-inducing thoughts and behavior. OCD can be time-consuming, create significant distress on the individual facing it and take a toll on family, friends, and colleagues.
The condition’s two main components are ruminative thoughts (“obsessions”) and the actions meant to soothe them (“compulsions”).
Obsessive Thoughts: OCD usually arises from distressing, repetitive thinking. Common categories that fuel OCD-related anxiety include:
- Cleanliness and fear of contamination.
- Worrying about disastrous events.
- Focusing on organizing, counting, symmetry, or “just right” thinking.
- Taboo thoughts or mental rituals.

Compulsive Behavior: When battling OCD, many patients develop compulsive, ritualistic behavior as a way to suppress their stressful thought content – for example, excessive hand washing.
While these compulsive behaviors are meant to help reduce anxiety, in time they are incorporated into the individual’s obsessive OCD patterns, until they begin inducing stress themselves. This creates a cycle of thoughts and actions that exhaust the individual experiencing them, causing them a great deal of despair.
OCD Demographics: According to the DSM V, OCD occurs in 1.2% of the population. While females are found to be affected at a slightly higher rate than males, males are more likely to develop OCD during childhood.
Possible Causes for OCD: OCD has been found to be associated with a number of risk factors, such as genetics, environmental factors, temperament and critical life events. Those with OCD also often battle additional mental health conditions, with three in four having a history of anxiety disorders, and nearly one in two battling depression.
Those with OCD also often battle additional mental health conditions, with three in four having a history of anxiety disorders, and nearly one in two battling depression.
Treatment Options in Your Battle Against OCD
Deep TMS: The first noninvasive device FDA-cleared to treat OCD, Deep TMS utilizes magnetic fields to safely regulate the neural activity of brain structures found to be related to OCD. A multicenter study published in 2019 by the American Journal of Psychiatry confirmed the treatment’s efficacy, concluding that focusing brain stimulation on “the medial prefrontal cortex and anterior cingulate cortex significantly improved OCD symptoms.” Deep TMS is also safe to combine with other forms of therapy, and does not cause any adverse or long-lasting side effects. It is noninvasive and can be easily incorporated into the patient’s daily schedule.
Cognitive Behavioral Therapy: CBT is a form of psychotherapy commonly used to treat OCD. The treatment focuses on the thoughts, feelings, behavior and physical reactions linked to OCD, while helping patients become less anxious in reaction to them. One subtype, Acceptance and Commitment Therapy (ACT), assists patients in developing openness and flexibility when reacting to obsessive thoughts, while committing to behavioral change.
The treatment focuses on the thoughts, feelings, behavior and physical reactions linked to OCD, while helping patients become less anxious in reaction to them. One subtype, Acceptance and Commitment Therapy (ACT), assists patients in developing openness and flexibility when reacting to obsessive thoughts, while committing to behavioral change.
Exposure and Response Prevention Therapy: ERP has also been shown to be a form of psychotherapy effective in treating OCD. ERP gradually exposes the patient to the source of their anxiety, accompanied by the support of a mental health professional, who encourages them to refrain from acting on their compulsions.
Psychopharmacology: Medication for OCD is also considered among the treatment options found helpful in reducing OCD symptoms. Several antidepressants have been FDA-approved to treat OCD, including selective serotonin reuptake inhibitors (SSRIs) and one tricyclic antidepressant (TCA). While many patients find them to be helpful, these medications can also induce possible side effects, such as weight gain and sexual dysfunction.
Lifestyle Changes to Protect Against OCD: Healthy eating, regular exercise and “sleep hygiene” (eliminating distractions when going to bed) are seen as a “winning triad” that greatly affects our ability to ward off OCD symptoms. Additional protective factors include keeping up with your regularly scheduled activities and incorporating stress management techniques such as meditation, yoga, and massage therapy into your life.
Want to learn more?
Connect with us to find out how we can help.
Fill Out the Form
Deep TMS Efficacy in Treating OCD
BrainsWay’s Deep TMS OCD treatment using the H7-coil significantly alleviates OCD symptoms, as demonstrated in a 2019 multicenter, double-blind, randomized controlled clinical study published by the American Journal of Psychiatry.
The 2019 study concluded that after six weeks of treatment, there was a statistically significant improvement in OCD symptoms for the study’s active treatment group when compared to the sham group. The study also found the improvement was maintained at least one month after the treatment’s end, at week 10.
The study also found the improvement was maintained at least one month after the treatment’s end, at week 10.
The primary measuring system used in this study was the Yale-Brown Obsessive-Compulsive Scale (Y-BOCS), the gold standard measure of OCD symptom severity. It found that 38.1% of patients in the active group achieved a full response reduction in symptom severity, compared to just 11.1% in the sham group. Additionally, 54.8% of patients in the active group achieved a partial response of reduction in symptom severity, versus just 26.7% in the sham group.
Based on a post-marketing study of over 200 patients published in the Journal of Psychiatric Research, Deep TMS has been shown to have an even greater effect in a real-life clinical practice setting. Nearly 60% of patients achieved response, defined as >30% YBOCS reduction from endpoint to baseline, after 29 sessions. >70% of patients reached first response after an average of 18.5 Deep TMS sessions or 31.6 days. >50% of patients achieved a sustained response (one-month meeting response criteria) after an average of 20 sessions or 32.1 days.
>50% of patients achieved a sustained response (one-month meeting response criteria) after an average of 20 sessions or 32.1 days.
Read more about Deep TMS efficacy
Deep TMS as a Safe Treatment for OCD
As a noninvasive treatment course, Deep TMS does not necessitate anesthesia, does not cause any significant side effects, and can be incorporated into the patient’s schedule with ease.
Deep TMS has been proven to be a safe treatment option by a number of studies. A 2018 study published by Brain Stimulation Journal highlighted Deep TMS’s safety, finding it to be a safe OCD treatment: “Deep TMS stimulation over the mPFC (medial prefrontal cortex) and ACC (anterior cingulate cortex) is a safe and effective intervention for improving OCD symptoms in patients who failed to receive sufficient benefit from treatments with SRIs and CBT.”
Read more about Deep TMS safety
Review the Patient Manual
Deep TMS OCD Treatment Protocol
BrainsWay’s Deep TMS technology includes a patented H-Coil, held inside a cushioned helmet that is fitted onto the patient’s head. Once activated, the H-Coil sends a magnetic pulse that acts to regulate the brain’s neural activity.
Once activated, the H-Coil sends a magnetic pulse that acts to regulate the brain’s neural activity.
Deep TMS sessions for OCD treatment involve a brief personalized provocation, or exposure, to activate the relevant areas of the brain, followed by an 18-minute TMS treatment. A full course of BrainsWay OCD usually requires daily sessions over a six-week period.
Read more about the Deep TMS procedure
Listen to Patient Testimonials
Antonella’s Story
Here how an OCD patient’s quality of life significantly improved after BrainsWay OCD treatment by Dr. Ryan Vidrine of TMS Health Solutions.
Check out additional testimonials of patients and healthcare providers in our video gallery.
Learn More About BrainsWay’s Deep TMS Therapy for OCD
Country*United StatesCanadaMexicoUnited KingdomFranceGermanyAustriaSwitzerlandUnited Arab EmiratesAfghanistanAntigua and BarbudaAnguillaAlbaniaArmeniaAngolaAntarcticaArgentinaAustraliaArubaAland IslandsAzerbaijanBosnia and HerzegovinaBarbadosBangladeshBelgiumBurkina FasoBulgariaBahrainBurundiBeninSaint BarthélemyBermudaBrunei DarussalamBolivia, Plurinational State ofBonaire, Sint Eustatius and SabaBrazilBahamasBhutanBouvet IslandBotswanaBelarusBelizeCocos (Keeling) IslandsCongo, the Democratic Republic of theCentral African RepublicCongoCote d'IvoireCook IslandsChileCameroonChinaColombiaCosta RicaCubaCape VerdeCuraçaoChristmas IslandCyprusCzech RepublicDjiboutiDenmarkDominicaDominican RepublicAlgeriaEcuadorEstoniaEgyptWestern SaharaEritreaSpainEthiopiaFinlandFijiFalkland Islands (Malvinas)Faroe IslandsGabonGrenadaGeorgiaFrench GuianaGuernseyGhanaGibraltarGreenlandGambiaGuineaGuadeloupeEquatorial GuineaGreeceSouth Georgia and the South Sandwich IslandsGuatemalaGuinea-BissauGuyanaHeard Island and McDonald IslandsHondurasCroatiaHaitiHungaryIndonesiaIrelandIsraelIsle of ManIndiaBritish Indian Ocean TerritoryIraqIran, Islamic Republic ofIcelandItalyJerseyJamaicaJordanJapanKenyaKyrgyzstanCambodiaKiribatiComorosSaint Kitts and NevisKorea, Democratic People's Republic ofKorea, Republic ofKuwaitCayman IslandsKazakhstanLao People's Democratic RepublicLebanonSaint LuciaLiechtensteinSri LankaLiberiaLesothoLithuaniaLuxembourgLatviaLibyan Arab JamahiriyaMoroccoMonacoMoldova, Republic ofMontenegroSaint Martin (French part)MadagascarMacedonia, the former Yugoslav Republic ofMaliMyanmarMongoliaMacaoMartiniqueMauritaniaMontserratMaltaMauritiusMaldivesMalawiMalaysiaMozambiqueNamibiaNew CaledoniaNigerNorfolk IslandNigeriaNicaraguaNetherlandsNorwayNepalNauruNiueNew ZealandOmanPanamaPeruFrench PolynesiaPapua New GuineaPhilippinesPakistanPolandSaint Pierre and MiquelonPitcairnPalestinian Territory, OccupiedPortugalParaguayQatarReunionRomaniaSerbiaRussian FederationRwandaSaudi ArabiaSolomon IslandsSeychellesSudanSwedenSingaporeSaint Helena, Ascension and Tristan da CunhaSloveniaSvalbard and Jan MayenSlovakiaSierra LeoneSan MarinoSenegalSomaliaSurinameSouth SudanSao Tome and PrincipeEl SalvadorSint Maarten (Dutch part)Syrian Arab RepublicSwazilandTurks and Caicos IslandsChadFrench Southern TerritoriesTogoThailandTajikistanTokelauTimor-LesteTurkmenistanTunisiaTongaTurkeyTrinidad and TobagoTuvaluChinese TaipeiTanzania, United Republic ofUkraineUgandaUruguayUzbekistanHoly See (Vatican City State)Saint Vincent and the GrenadinesVenezuela, Bolivarian Republic ofVirgin Islands, BritishViet NamVanuatuWallis and FutunaSamoaYemenMayotteSouth AfricaZambiaZimbabwe
null
*Are you a. ..Prescribing Healthcare ProviderNon-Prescribing Healthcare ProviderPatient / CaregiverOther
..Prescribing Healthcare ProviderNon-Prescribing Healthcare ProviderPatient / CaregiverOther
You may also be interested in…
Major Depressive Disorder (MDD)
Depression is a neuropsychiatric disorder that is expressed in emotional, physiological, and behavioral...
Understanding Deep Transcranial Magnetic Stimulation For OCD
NOV. 08, 2019
By Steven Ryan Vidrine, M.D.
Many patients struggling with Obsessive Compulsive Disorder (OCD) are familiar with the go-to treatment approaches: medication (usually SSRIs) and exposure-response prevention (ERP) therapy, which was developed specifically for the treatment of OCD. For many patients, these first-line treatments work. Unfortunately, many other patients struggle to feel better with medication or struggle to tolerate the side effects.
Additionally, ERP therapy can be difficult to find and to afford. If one is able to get a therapist specialized in OCD treatment, the therapy itself is often quite difficult and uncomfortable. The idea behind ERP is for the individual to face their fears and learn to refrain from engaging in compulsions. For many patients, there are just too many hurdles, or the process is too long and difficult. For some “treatment resistant” individuals, they do everything as recommended and are still left with significant symptoms.
The idea behind ERP is for the individual to face their fears and learn to refrain from engaging in compulsions. For many patients, there are just too many hurdles, or the process is too long and difficult. For some “treatment resistant” individuals, they do everything as recommended and are still left with significant symptoms.
For those patients, there are additional treatment options available. And we’re starting to understand how one of these treatment options, deep transcranial magnetic stimulation (dTMS), can work with therapy and medication to reduce symptoms more effectively.
What is dTMS?
At my practice, one treatment modality that we offer is non-invasive deep transcranial magnetic stimulation (dTMS). dTMS is the first new therapy in over a decade to be FDA-cleared for treating OCD. This outpatient treatment is intended for patients who have not found success with medication and therapy and are looking for another option.
dTMS works by targeting parts of the brain known to be involved in OCD with temporary magnetic fields. Patients go in for daily 20-minute sessions, Monday through Friday, for five to six weeks. And often continue to improve after the treatment period ends.
Patients go in for daily 20-minute sessions, Monday through Friday, for five to six weeks. And often continue to improve after the treatment period ends.
One way that dTMS for OCD differs from depression treatment is that the treatment is most effective when paired with a brief “provocation” or “exposure” personally designed for the patient based on their OCD fears. The belief is that by activating the OCD circuitry at the time of stimulation, we can better target their specific symptoms and better help their brain recalibrate its response.
A trial, that led to the FDA clearance of the treatment, has shown that dTMS can be highly effective in reducing OCD symptom severity. The treatment is non-invasive, and the only common side effects are mild scalp discomfort and minor headaches that usually go away after the first couple weeks of treatment.
How Can dTMS Be Used with Therapy?
While the clinical trial data is promising, the dTMS approach has only been FDA approved for the treatment of OCD since August 2018. So many psychiatrists and patients still have questions about how it works and how it might be used in addition to other treatment approaches.
So many psychiatrists and patients still have questions about how it works and how it might be used in addition to other treatment approaches.
As one of the first psychiatrists to begin using the device in routine clinical practice, I’ve treated several OCD patients since the treatment was approved. The severity of these cases has ranged from moderate (significant impact on function but still maintaining expected work/social activities) to severe (on disability, requiring residential treatment or hospitalization). I have seen this treatment fail for some and work wonders for others.
In my experience, dTMS reduces symptom severity seemingly through increasing patients’ ability to resist compulsions and engage more effectively with ERP therapy, even when overall obsessions may not have drastically changed. I have worked with several patients who tried medications and ERP with OCD specialists several times in the past, and didn’t see improvements. But once they paired their treatment with dTMS, they were able to progress and feel better at much a greater rate. Patients often describe feeling that they have more control over the behaviors they choose, that obsessions are quieter or easier to ignore, and that they feel they can fight the obsessions and compulsions more successfully.
Patients often describe feeling that they have more control over the behaviors they choose, that obsessions are quieter or easier to ignore, and that they feel they can fight the obsessions and compulsions more successfully.
As a clinician who believes in ERP as the cornerstone of OCD treatment, this anecdotal evidence is an opportunity to take what we already know to work in most cases, and boost its effects with dTMS. I’m excited about this new treatment option for patients, and as a provider, I have enjoyed being able to have another tool to use against OCD. I encourage you to ask your psychiatrist about dTMS if you feel like it might be the right approach for you.
Dr. Vidrine is a Board-Certified Psychiatrist who specializes in treating patients with OCD, Body Dysmorphia, Anxiety Disorders, and Treatment-Resistant Depression. He is a member of TMS Health Solutions, a practice which specializes in caring for the 40% of patients who don’t respond to medication and providing innovative and effective therapies.
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
We’re always accepting submissions to the NAMI Blog! We feature the latest research, stories of recovery, ways to end stigma and strategies for living well with mental illness. Most importantly: We feature your voices.
Check out our Submission Guidelines for more information.
LEARN MORE
High-frequency transcranial magnetic stimulation (TMS) as a new approach in the treatment of obsessive-compulsive disorder (OCD)
High-frequency transcranial magnetic stimulation (TMS) as a new approach in the treatment of obsessive-compulsive disorder (OCD)
04/17/2019 21:31
Hospital, Recreation
New research proves that high-frequency deep transcranial magnetic stimulation (dTMS), targeting areas of the brain involved in obsessive-compulsive disorder (OCD), is a promising, state-of-the-art treatment for OCD.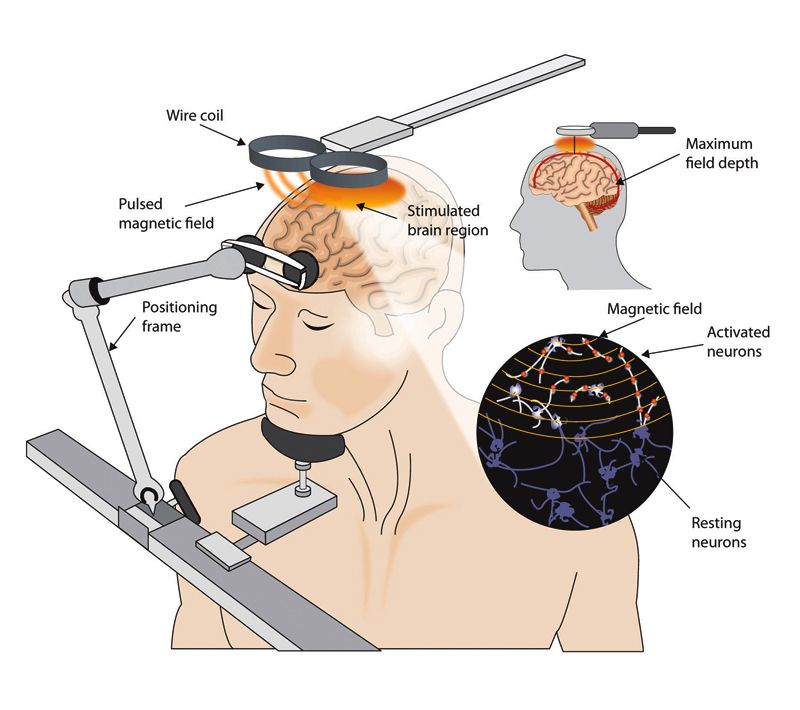 It is a severe, often disabling disorder that, in half of the cases, does not respond adequately to currently approved therapies (Aron Tendler, MD, chief medical officer of Brainsway, told Medscape Medical News).
It is a severe, often disabling disorder that, in half of the cases, does not respond adequately to currently approved therapies (Aron Tendler, MD, chief medical officer of Brainsway, told Medscape Medical News).
A new study looked at the issue of the greatest effectiveness of two frequency characteristics of magnetic stimulation: low frequency, with a frequency of 1 pulse per second, and high frequency, with a frequency of 20 pulses per second. Special magnetic coils have been created, magnetic impulses from which can penetrate into deeper layers of brain structures than is required for the treatment of depression.
The study included 40 patients with OCD who did not respond to drug therapy. Each patient underwent the dTMS treatment five times a week, with a session duration of approximately 18 minutes, for five weeks.
After this period, patients receiving the 20 Hz pacing protocol experienced a 27% decrease in the intensity of symptoms of OCD on the Yale-Brown Scale (YBOCS) compared to baseline, and patients receiving the 1 Hz pacing protocol had a decrease points was 12%. Control patients who received a "sham" procedure (no stimulation) showed a 6% decrease in YBOCS.
Control patients who received a "sham" procedure (no stimulation) showed a 6% decrease in YBOCS.
The statistical difference between the HF protocol and the control group was significant.
In parallel, an electroencephalographic examination (EEG) was performed. His data indicated increased activity in the anterior cingulate cortex in the high frequency protocol group.
Eric Hollander, MD, professor of clinical psychiatry and behavioral sciences at the Albert Einstein College of Medicine in New York, said that treatment-resistant OCD is a common and disabling disorder and that many patients fail to respond to conventional therapies . The scientist also noted the importance of the new dTMS magnetic coils, which are able to penetrate deep brain structures and, in particular, have a stimulating effect on the anterior cingulate gyrus. The induction of neuroplasticity in this area of the brain is of interest because it is the one that is activated when patients get stuck reacting to conflicting information, an action that can play an important role in the clinical picture of OCD.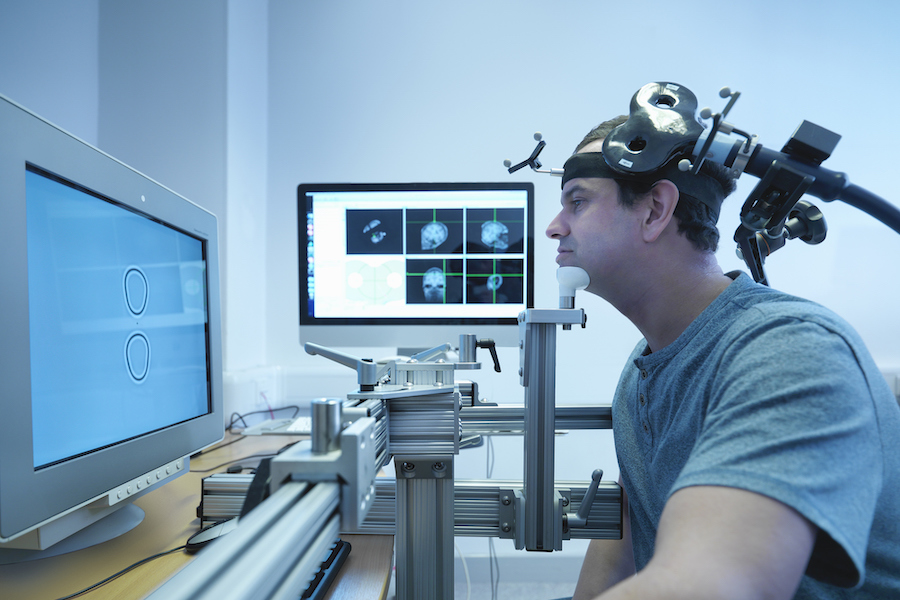 Surprisingly, the high-frequency stimulation was found to be more effective than the low-frequency one. The authors of the study suggested that high-frequency stimulation allows the frontal lobes to better control the hyperactivity of the striatum (Corp. Striatum), which "controls" obsessive thoughts and compulsive behavior.
Surprisingly, the high-frequency stimulation was found to be more effective than the low-frequency one. The authors of the study suggested that high-frequency stimulation allows the frontal lobes to better control the hyperactivity of the striatum (Corp. Striatum), which "controls" obsessive thoughts and compulsive behavior.
Anxiety and Depression Association of America (ADAA) Conference 2016: Abstract 122, presented April 1, 2016.
Fill out the form and we will contact you within 24 hours.
| Share
On August 17, Brainway received FDA (Food and Drug Administration) approval to market “Brainsway,” a transcranial magnetic stimulation (TMS) system for the treatment of obsessive-compulsive disorder (OCD) . Obsessive-compulsive disorder is a common chronic disorder in which the patient suffers from involuntary obsessive or frightening thoughts and behaviors with recurring obsessive seizures and phobias. Typically, OCD is treated with psychotherapy, with or without medication. According to the National Institute of Psychiatry in the United States, in 2017, about 1% of the American adult population suffered from OCD. Despite a good therapeutic response in many patients, some of them continue to experience symptoms of the disease. Transcranial magnetic stimulation is a procedure that uses magnetic fields to stimulate nerve cells in the brain. In 2008, TMS was approved for the treatment of major depressive episode, and in 2013 TMS was expanded to treat headaches in certain types of migraine. Current data were obtained from a randomized, multicenter study of 100 patients, 49 of whom were treated with the Brainsway device and 51 were treated with a simulator device. Patients receiving OCD drug therapy at the time of the study continued the course without changing dosages. The Yale-Brown Obsessive-Compulsive Rating Scale resulted in 38 percent positive responses to Brainsway therapy and 11 percent of patients responding positively to the simulant device. The most common side effect recorded was headaches (37.5% of patients in the Brainsway group and 35.3% of patients in the placebo group). No serious side effects have been reported from the use of Brainsway. Other mild to moderate transient reactions included local pain on use or discomfort, jaw, facial, muscle, neck pain, and spasms and convulsions. Brainsway medical equipment is contraindicated in patients with metal implants or stimulating devices near or in the head area, including cochlear implants, vagus nerve stimulators, implanted aneurysm clips, deep brain stimulators, stents, etc. |
 According to the American Agency for Quality Control of Therapy, TMS has shown its potential in helping patients suffering from depression and headaches during clinical trials. This registration will provide another therapeutic option for OCD patients who have not responded to conventional treatment.
According to the American Agency for Quality Control of Therapy, TMS has shown its potential in helping patients suffering from depression and headaches during clinical trials. This registration will provide another therapeutic option for OCD patients who have not responded to conventional treatment.