Propranolol for panic disorder
Propranolol: medicine for heart problems, anxiety and migraine
1. About propranolol
Propranolol belongs to a group of medicines called beta blockers. It's used to treat heart problems, help with anxiety and prevent migraines.
If you have a heart problem, you can take propranolol to:
- treat high blood pressure
- treat conditions that cause an irregular heartbeat (arrhythmia), like atrial fibrillation
- help prevent future heart disease, heart attacks and strokes
- help prevent chest pain caused by angina
Propranolol can help reduce your symptoms if you have too much thyroid hormone in your body (thyrotoxicosis). You'll usually take it together with medicines to treat an overactive thyroid.
This medicine is only available on prescription. It comes as tablets, slow release capsules, or as a liquid that you swallow.
2. Key facts
- Propranolol slows down your heart rate and makes it easier for your heart to pump blood around your body.
- It's usually prescribed for high blood pressure and other heart problems, but it can also help with the physical signs of anxiety, like sweating and shaking.
- Your very first dose of propranolol may make you feel dizzy, so take it at bedtime. After that, if you do not feel dizzy, you can take it in the morning.
- The main side effects of propranolol are feeling dizzy or tired, cold hands or feet, difficulties sleeping and nightmares. These side effects are usually mild and short-lived.
3. Who can and cannot take propranolol
Most adults and children aged 12 and over can take propranolol. But it is not officially approved for treating high blood pressure in children under 12 years old.
But it is not officially approved for treating high blood pressure in children under 12 years old.
Propranolol is not suitable for everyone. To make sure it's safe for you, tell your doctor before starting to take propranolol if you:
- have ever had an allergic reaction to propranolol or any other medicine
- have low blood pressure or a slow heart rate
- have heart failure which is getting worse
- have diabetes
- have liver or kidney problems
- have severe blood circulation problems in your limbs (such as Raynaud's phenomenon), which may make your fingers and toes tingle or turn paler than usual or blue
- have metabolic acidosis, when there is too much acid in your blood
- have lung disease or asthma
- are pregnant, trying to get pregnant or breastfeeding
4.
 How and when to take propranolol
How and when to take propranolol Propranolol comes as 2 different types of medicine:
- standard release – this releases propranolol into your body quickly, so you may need to take it several times a day depending on your dose
- slow release – this releases the medicine slowly so you do not have to take it as often, once a day is usually enough
If you are taking it once a day, your doctor may advise you to take your first dose before bedtime, because it can make you feel dizzy. After the first dose, if you do not feel dizzy, take propranolol in the morning.
Important
Keep taking propranolol even if you feel well. You will still be getting the benefits of the medicine.
Dosage and strength
Propranolol tablets come in strengths of 10mg, 40mg, 80mg or 160mg. The slow release capsules are 80mg or 160mg. The liquid comes in strengths of 5mg, 10mg, 40mg or 50mg in 5ml.
The slow release capsules are 80mg or 160mg. The liquid comes in strengths of 5mg, 10mg, 40mg or 50mg in 5ml.
How much you take depends on why you need propranolol.
The usual doses for adults are:
- high blood pressure – the starting dose is usually 80mg, taken twice a day. If this dose is not working well enough to reduce your blood pressure, your doctor may increase it to a maximum of 160mg twice a day
- migraine or angina (chest pain) – 40mg, taken 2 or 3 times a day. This can be increased to 120mg to 240mg a day. Your doctor or pharmacist will explain how to split the dose over the day
- irregular heartbeat (arrhythmia) – 10mg to 40mg, taken 3 or 4 times a day
- anxiety – 40mg taken once a day which can be increased to 40mg taken 3 times a day
- too much thyroid hormone (thyrotoxicosis) – 10mg to 40mg, taken 3 or 4 times a day
Doses are usually lower for people aged over 65 or people with a kidney or liver problem.
If your child needs propranolol, your doctor will usually use your child's weight to work out the right dose.
How to take it
Propranolol does not usually upset your stomach so you can take it with or without food. It's best to do the same each day.
Swallow the tablets whole with a drink of water. If you find the tablets difficult to swallow, some brands have a score line to help you break the tablet in half. Check the information leaflet for your brand to see if you can do this.
If you're taking capsules, swallow them whole with a drink of water. Do not break, chew or crush them.
If you're taking propranolol as a liquid, it will come with a plastic syringe or spoon to help you measure out the right dose. If you do not have one, ask your pharmacist for one. Do not use a kitchen teaspoon as it will not measure the right amount of medicine.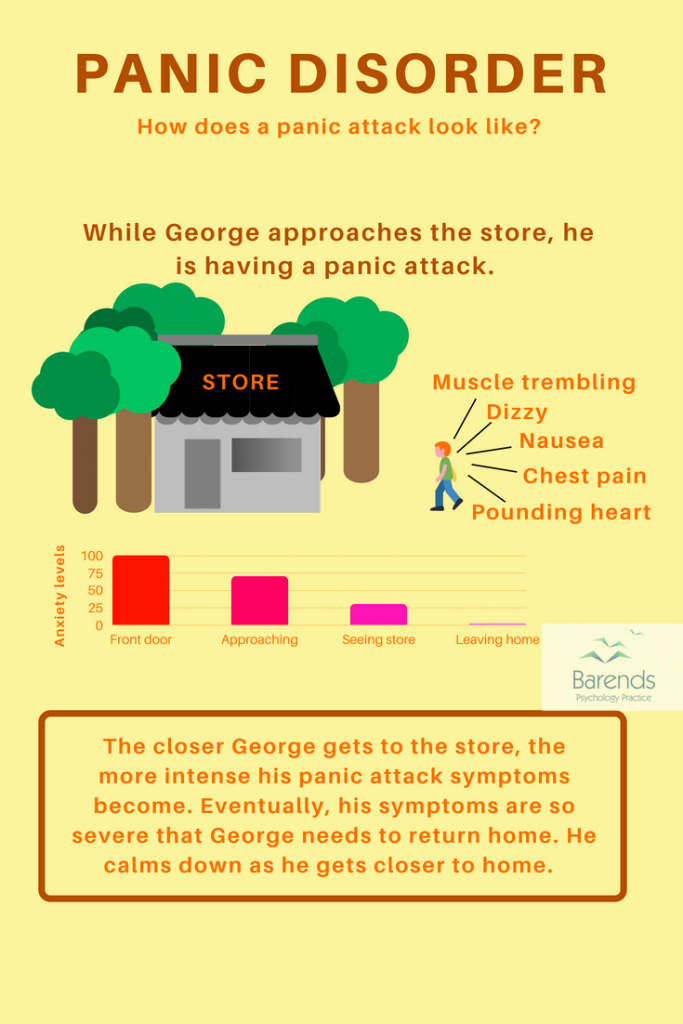
If you forget to take it
If you forget to take a dose of propranolol, take it as soon as you remember, unless it's nearly time for your next dose. In this case, just leave out the missed dose and take your next dose at the usual time.
Never take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you often forget doses, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
If you take too much
An overdose of propranolol can slow down your heart rate and make it difficult to breathe. It can also cause dizziness and trembling.
The amount of propranolol that can lead to an overdose varies from person to person.
Urgent advice: Contact 111 for advice now if:
- you take more than your prescribed dose of propranolol
Call 111 or go to 111 online
If you need to go to A&E, do not drive yourself.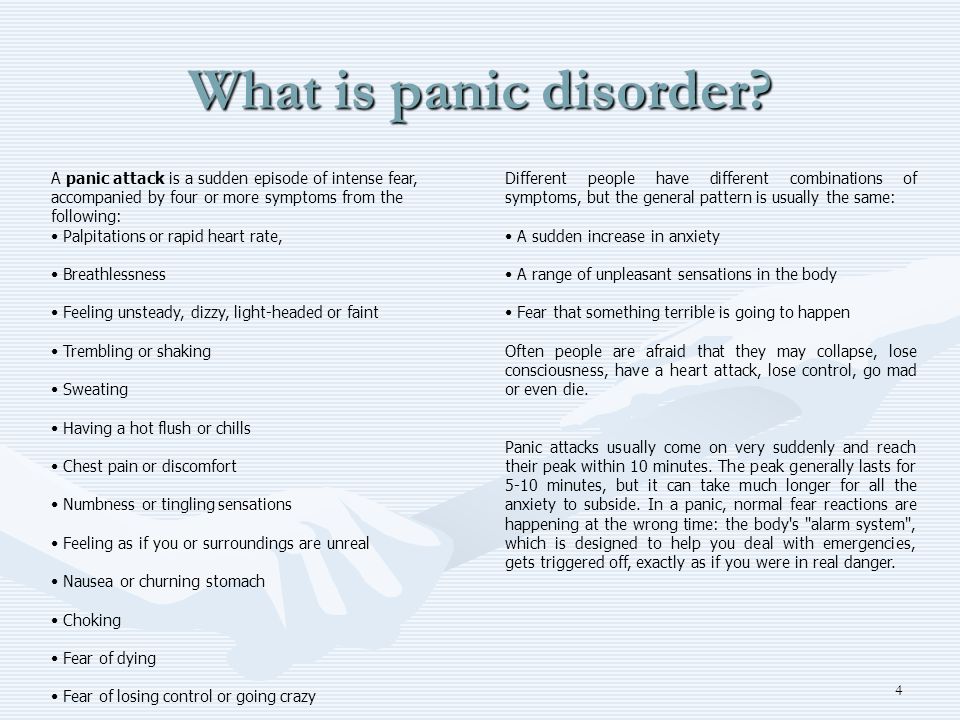 Get someone else to drive you or call for an ambulance.
Get someone else to drive you or call for an ambulance.
Take the propranolol packet or leaflet inside it plus any remaining medicine with you.
5. Side effects
Like all medicines, propranolol can cause side effects in some people, but many people have no side effects or only minor ones.
Side effects often improve as your body gets used to the medicine.
Common side effects
These common side effects happen in more than 1 in 100 people. They're usually mild and short-lived.
Talk to your doctor or pharmacist if the side effects bother you or last more than a few days:
- headaches
- feeling tired, dizzy or weak
- cold fingers or toes
- feeling or being sick (nausea or vomiting), or diarrhoea
- stomach pain
Serious side effects
It happens rarely, but some people have serious side effects when taking propranolol.
Tell a doctor or contact 111 straight away if:
- the whites of your eyes turn yellow, your skin turns yellow although this may be less obvious on brown on black skin, or you have pale poo or dark pee – these can be signs of liver problems
- you get nosebleeds that last for more than 10 minutes, unexplained bruising, or you bruise more easily than usual – these can be signs of low numbers of platelets in your blood (thrombocytopenia)
Go to 111.nhs.uk or call 111.
Immediate action required: Call 999 or go to A&E now if:
- you have shortness of breath with a cough which gets worse when you exercise (like walking up stairs), swollen ankles or legs, chest pain, or an irregular heartbeat – these are signs of heart problems
- you have shortness of breath, wheezing and tightening of your chest – these can be signs of lung problems
Serious allergic reaction
In rare cases, propranolol may cause a serious allergic reaction (anaphylaxis).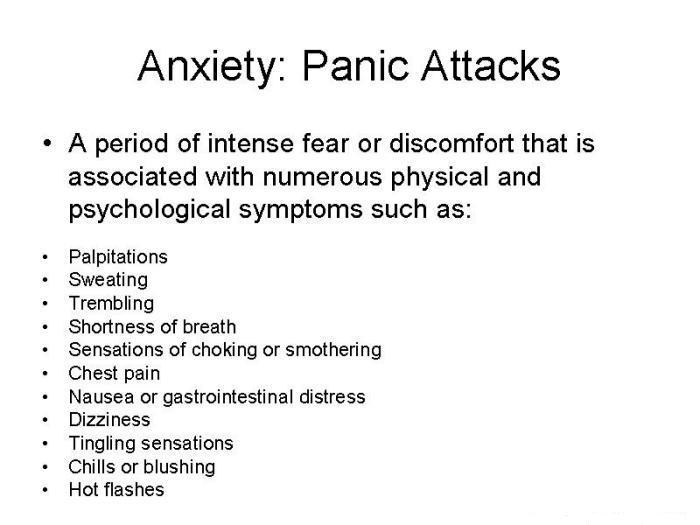
Immediate action required: Call 999 or go to A&E now if:
- you get a skin rash that may include itchy, red, swollen, blistered or peeling skin
- you're wheezing
- you get tightness in the chest or throat
- you have trouble breathing or talking
- your mouth, face, lips, tongue or throat start swelling
You could be having a serious allergic reaction and may need immediate treatment in hospital.
These are not all the side effects of propranolol. For a full list, see the leaflet inside your medicine packet.
Information:
You can report any suspected side effect using the Yellow Card safety scheme.
Visit Yellow Card for further information.
6. How to cope with side effects of propranolol
What to do about:
- headaches – make sure you rest and drink plenty of fluids.
 Try not to drink too much alcohol. Ask your pharmacist to recommend a painkiller. Talk to your doctor if the headaches last longer than a week or are severe.
Try not to drink too much alcohol. Ask your pharmacist to recommend a painkiller. Talk to your doctor if the headaches last longer than a week or are severe. - feeling tired, dizzy or weak – as your body gets used to propranolol, these side effects should wear off. If propranolol makes you feel dizzy, sit or lie down until you feel better. It's best not to drink alcohol as it will make you feel worse. Do not drive or ride a bike until you feel better.
- cold fingers or toes – put your hands or feet under warm running water, massage them and wiggle your fingers and toes. Do not smoke or have drinks with caffeine in, as this can make your blood vessels narrower and further restrict blood flow to your hands and feet. Try wearing mittens (they're warmer than gloves) and warm socks. Do not wear tight watches or bracelets.
- feeling or being sick or diarrhoea – stick to simple meals and do not eat rich or spicy food.
 It might help to take your propranolol after a meal or snack. Drink lots of fluids, such as water or squash, to avoid dehydration. Take small, frequent sips if you're being sick. Signs of dehydration include peeing less than usual or having dark, strong-smelling pee. Do not take any other medicines to treat diarrhoea and vomiting without speaking to a pharmacist or doctor. If you take contraceptive pills and you're being sick or have severe diarrhoea, your contraception may not protect you from pregnancy. Check the pill packet for advice.
It might help to take your propranolol after a meal or snack. Drink lots of fluids, such as water or squash, to avoid dehydration. Take small, frequent sips if you're being sick. Signs of dehydration include peeing less than usual or having dark, strong-smelling pee. Do not take any other medicines to treat diarrhoea and vomiting without speaking to a pharmacist or doctor. If you take contraceptive pills and you're being sick or have severe diarrhoea, your contraception may not protect you from pregnancy. Check the pill packet for advice. - stomach pain – try to rest and relax. It can help to eat and drink slowly and have smaller and more frequent meals. Putting a heat pad or covered hot water bottle on your tummy may also help. If you are in a lot of pain, speak to your pharmacist or doctor.
7. Pregnancy and breastfeeding
Propranolol and pregnancy
Propranolol is not thought to be harmful during pregnancy, but it may affect your baby's growth in later pregnancy. Discuss taking propranolol with your doctor or midwife as you may need extra scans to check your baby's growth.
Discuss taking propranolol with your doctor or midwife as you may need extra scans to check your baby's growth.
If you're trying to get pregnant or you're already pregnant, talk to your doctor about the benefits and possible harms of taking propranolol. There may be other medicines that are better to use during pregnancy.
Propranolol and breastfeeding
If your doctor or health visitor says that your baby is healthy, it's OK to take propranolol while breastfeeding.
Propranolol passes into breast milk in tiny amounts. It has not been known to cause any side effects in breastfed babies.
It's important to treat your high blood pressure to keep you well. Breastfeeding will also benefit both you and your baby.
If you notice that your baby is not feeding as well as usual, or seems unusually sleepy, or if you have any other concerns about your baby, then talk to your doctor or health visitor.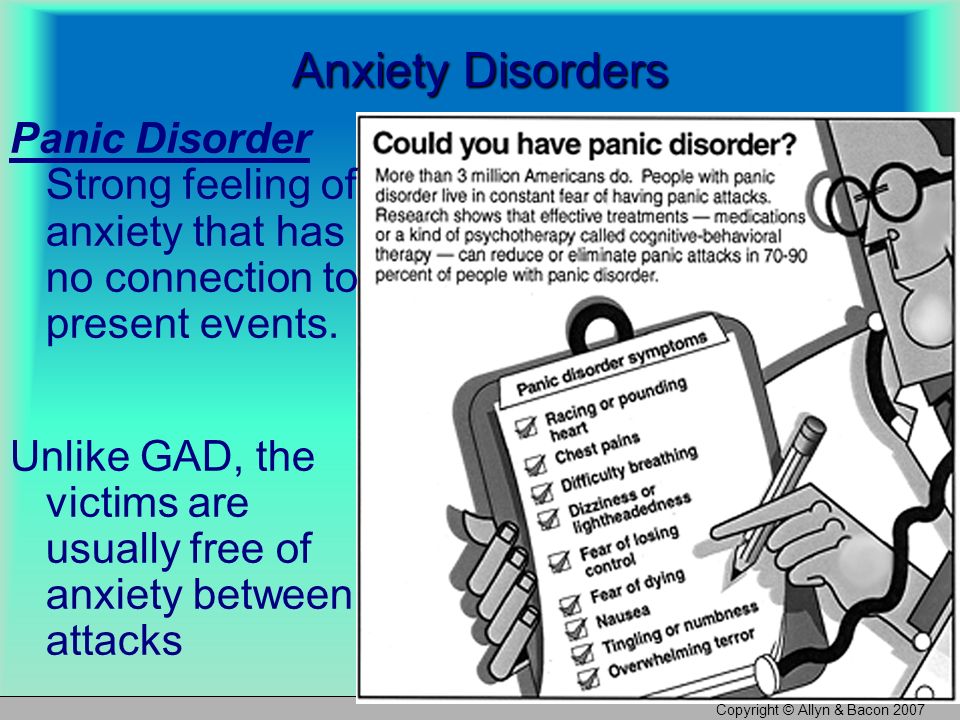
Non-urgent advice: Tell your doctor if you're:
- trying to get pregnant
- pregnant
- breastfeeding
For more information about how propranolol can affect you and your baby during pregnancy, visit the Best Use of Medicines in Pregnancy (BUMPS) website.
8. Cautions with other medicines
There are some medicines that may affect the way propranolol works.
Tell your doctor if you're taking:
- other medicines for high blood pressure. The combination with propranolol can sometimes lower your blood pressure too much. This may make you feel dizzy or faint. If this keeps happening to you, your doctor may change your dose
- other medicines for an irregular heartbeat such as amiodarone or flecainide
- other medicines which can lower your blood pressure.
 These include some antidepressants, nitrates (for chest pain), baclofen (a muscle relaxant), medicines for an enlarged prostate gland like tamsulosin, or Parkinson's disease medicines such as levodopa
These include some antidepressants, nitrates (for chest pain), baclofen (a muscle relaxant), medicines for an enlarged prostate gland like tamsulosin, or Parkinson's disease medicines such as levodopa - asthma or chronic obstructive pulmonary disease (COPD) medicines
- diabetes medicines, particularly insulin – propranolol may make it more difficult to recognise the warning signs of low blood sugar. Speak to your doctor if you have low blood sugar levels without getting any of the usual warning signs. Check your blood sugar after exercise, and follow usual advice about checking it before driving, cycling or operating machinery
- medicines to treat nose or sinus congestion, or other cold remedies (including those you can buy in the pharmacy)
- medicines for allergies, such as ephedrine, noradrenaline or adrenaline
- non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, diclofenac or naproxen.
 These medicines may increase your blood pressure, so it's best to keep them to a minimum
These medicines may increase your blood pressure, so it's best to keep them to a minimum
Mixing propranolol with herbal remedies or supplements
There's very little information about taking herbal remedies and supplements with propranolol. They are not tested in the same way as pharmacy and prescription medicines.
Important: Medicine safety
Tell your doctor or pharmacist if you're taking any other medicines, including herbal medicines, vitamins or supplements.
9. Common questions about propranolol
How does propranolol work?Propranolol is a type of medicine called a beta blocker.
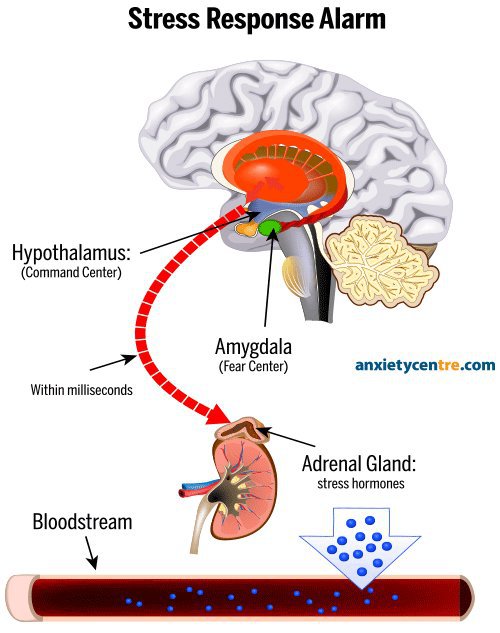
Like other beta blockers, propranolol works by changing the way your body responds to some nerve impulses, including in the heart. It slows down your heart rate and makes it easier for your heart to pump blood around your body.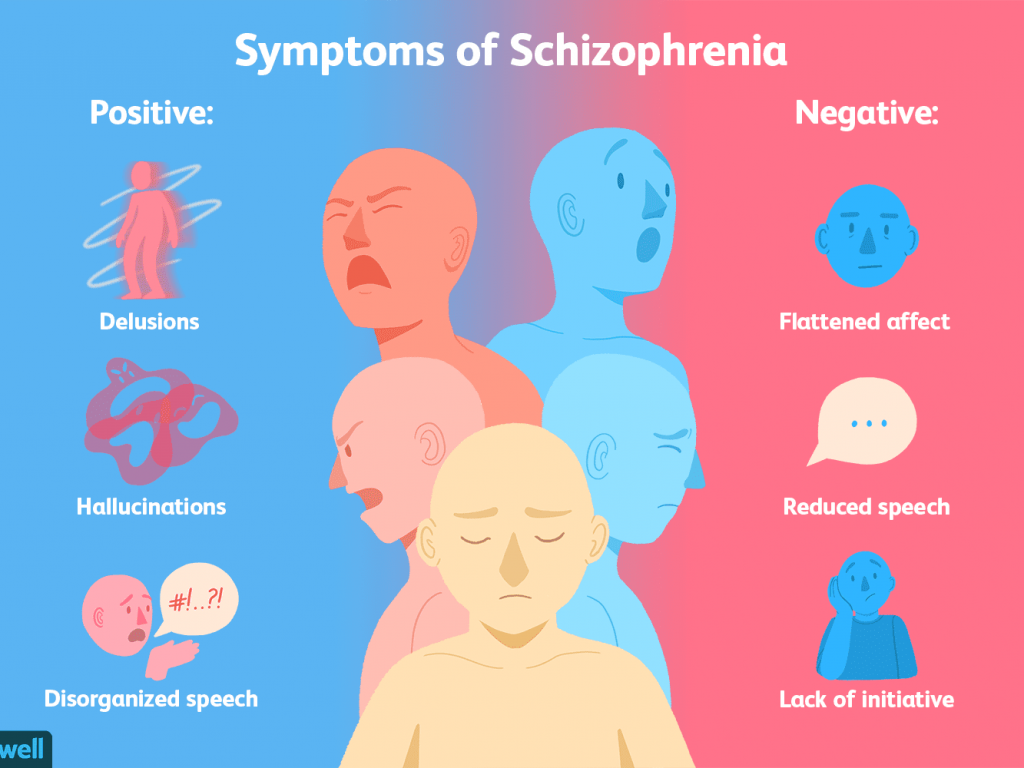
It works differently if you're using it for anxiety. When you are anxious, your brain makes chemical messengers called adrenaline and noradrenaline. These make your heart rate faster and make you sweat or shake. Propranolol helps block the effects of these chemical messengers. This reduces the physical signs of anxiety.
It's not fully understood how propranolol prevents migraines. It may work by relaxing the blood vessels involved, or by reducing activity in the visual cortex. This is the part of the brain where migraines are believed to start.
How long does propranolol take to work?Propranolol usually starts to work in a few hours.
For heart conditions or high blood pressure, propranolol can take up to a week to reach its full effect. You may not feel any different but that does not mean it is not working. It's important to keep taking your medicine.
For migraines, it can take several weeks for propranolol to start making a real difference, so keep taking it.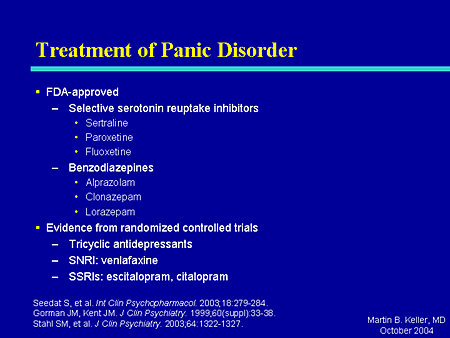
This depends on why you're taking propranolol.
For heart conditions or high blood pressure, treatment is usually long term and may be for the rest of your life.
For anxiety, you'll usually take propranolol for a short amount of time, to help with your physical symptoms. Speak to your doctor about the risks and benefits of taking it for more than a few months. This will depend on your symptoms, whether it's a one-off or a recurring problem, how well propranolol works for you and whether you get side effects.
For migraines, treatment can last for several months or years, depending on how bad your symptoms are.
Can I take propranolol for a long time?Propranolol is generally safe to take for a long time.
If you're taking it for a heart condition, or to prevent migraines, it works best when you take it long term.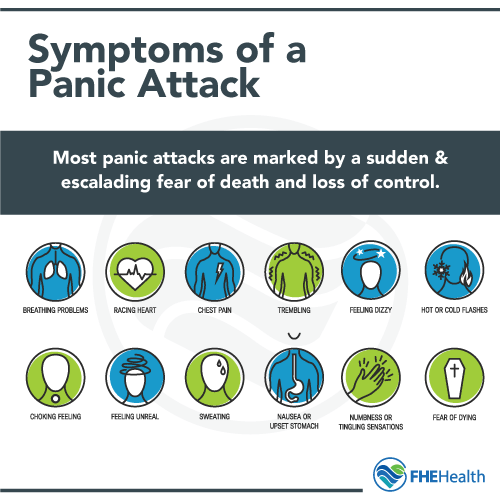
If you're taking it for anxiety, there do not seem to be any lasting harmful effects if you take it for several months or years. But it's best to take propranolol only for as long as you need it.
You'll need to have your blood pressure checked regularly if you're taking propranolol for a long time for migraines or anxiety.
What will happen if I stop taking it?Talk to your doctor if you want to stop taking propranolol. If you're bothered by side effects, your doctor may be able to prescribe a different medicine instead.
Stopping propranolol suddenly may make your health problem worse. In addition, if you stop suddenly after taking it for a long time, you may get extra side effects as a reaction to stopping it. These include an irregular heart rate, sweating and shaking.
If you stop taking propranolol, it will take about 1 to 2 days for it to be completely out of your body but the side effects can last for up to 1 week.
Propranolol works as well as other beta blockers for reducing blood pressure. The main difference between propranolol and other beta blockers is that it does not just affect your heart. It can affect other parts of your body too, such as your lungs.
There are lots of other medicines to lower your blood pressure and treat chest pain. They work in a different way to beta blockers and include:
- ACE inhibitors like ramipril and lisinopril
- angiotensin receptor blockers like candesartan
- calcium channel blockers like amlodipine
- medicines that make you pee more (diuretics) like furosemide
Beta blockers are not usually the first choice for high blood pressure. The medicine your doctor prescribes depends on your age and ethnicity.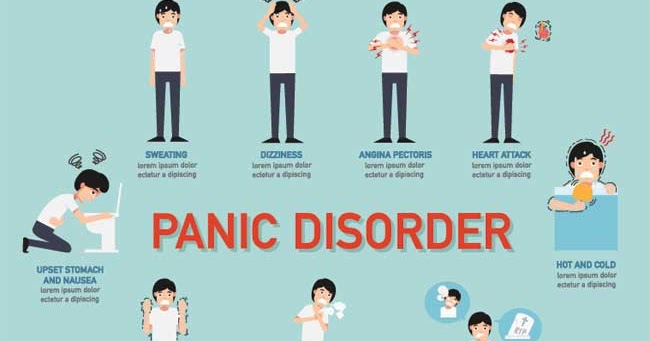
If you're under 55 and not of African Caribbean or black African origin, you'll usually be offered an ACE inhibitor or an angiotensin receptor blocker.
If you're 55 or older, or you're any age and of African Caribbean or black African origin, you'll usually be offered a calcium channel blocker.
Sometimes you may have to try other blood pressure-lowering medicines if you get side effects. Many people need to take a combination of different medicines to lower their blood pressure.
How does it compare with other medicines for preventing migraine?Atenolol, metoprolol, timolol and nadolol are all beta blockers and they work well in preventing migraines. However, most doctors prescribe propranolol.
There are some other medicines that are known to prevent migraines but they are not officially approved in the UK. They include amitriptyline, sodium valproate and gabapentin and they may have different side effects.
Topiramate can also be used to prevent migraines. It works just as well as propranolol. However, topiramate has not been officially approved for migraine for children under the age of 16.
Ask your doctor or pharmacist which medicine is best for you.
How does it compare with other medicines for anxiety?Propranolol treats the physical symptoms of anxiety – for example, it stops your heart beating too fast. You'll usually only take propranolol for a short time.
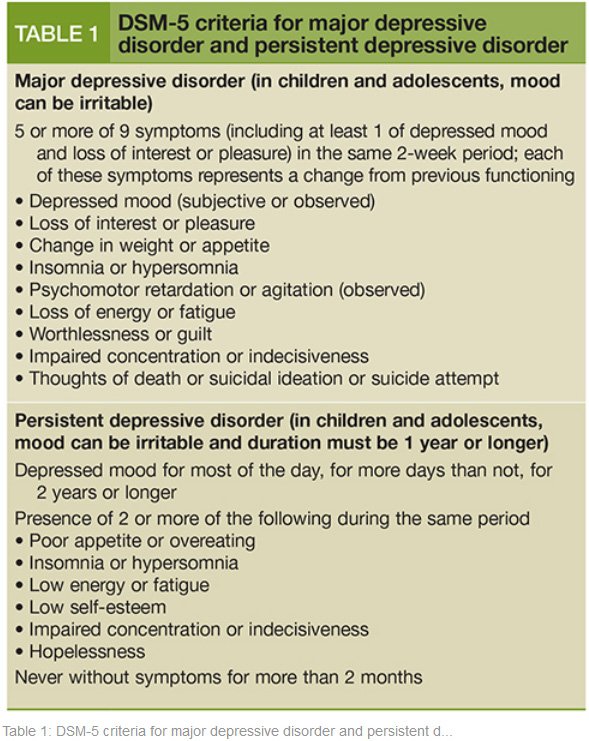
The physical symptoms of anxiety are caused by chemical imbalances in the brain. Your doctor may prescribe an antidepressant like sertraline to treat these imbalances. You usually take antidepressants long term.
Many doctors prefer medicine-free treatments for anxiety. These include talking therapies like cognitive behavioural therapy. If you're having talking therapy, your doctor may prescribe propranolol at the same time.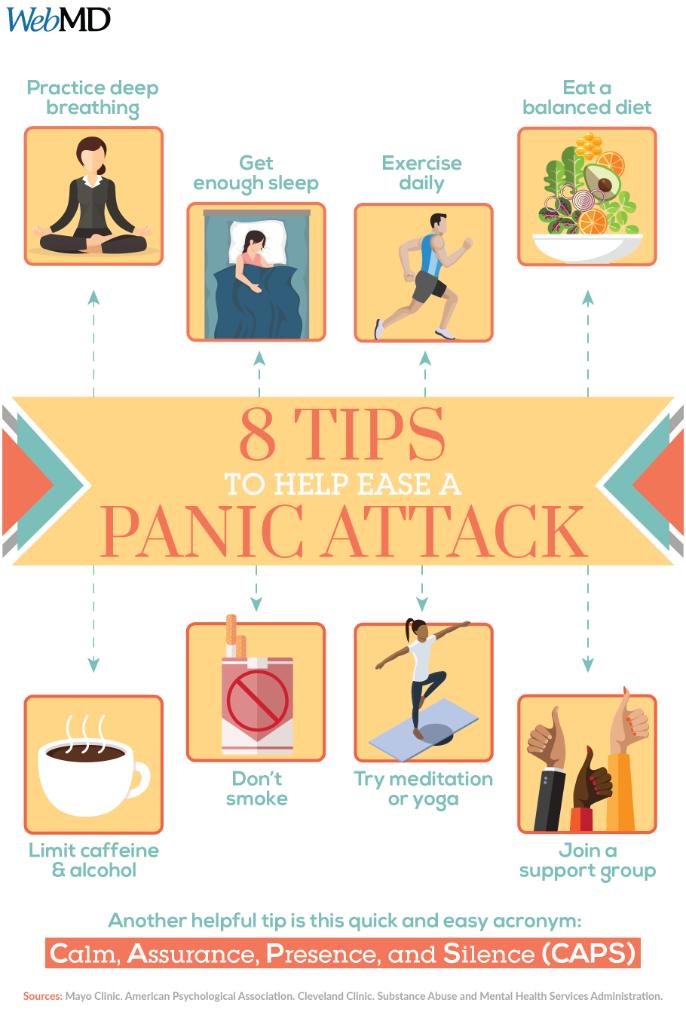 This will help you with your physical symptoms.
This will help you with your physical symptoms.
Tell your doctor that you're taking propranolol if you're going to be put to sleep using general anaesthetic, or you're having any kind of major operation.
Your doctor may advise you to stop taking propranolol before surgery. This is because propranolol can lower your blood pressure too much when it's combined with some anaesthetics.
Can I drink alcohol with it?Drinking alcohol can increase the blood pressure-lowering effect of propranolol, which can make you feel dizzy or lightheaded.
During the first few days of taking propranolol or after an increase in your dose, it's best to stop drinking alcohol until you see how the medicine affects you.
If you find propranolol makes you feel dizzy it's best to stop drinking alcohol.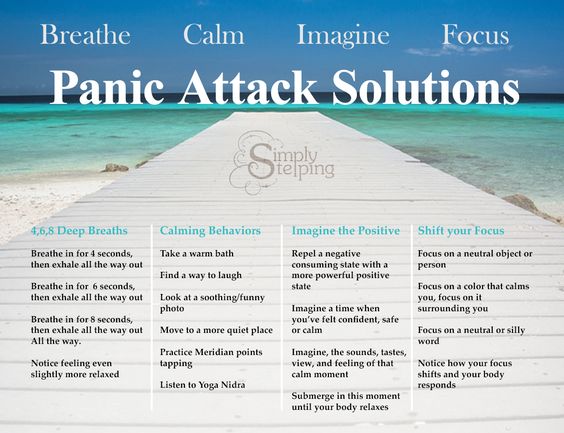
Apart from being careful with alcohol, you can eat and drink normally while taking propranolol.
Eating a healthy, balanced diet can help if you have high blood pressure or another heart condition.
Will it make me put on weight?Some people on propranolol say they put on weight, especially in the first few months of taking it. This is not known to be a common side effect of taking propranolol, and there is not enough information to say for sure why some people put on weight.
It could, for example, be because propranolol can make you feel tired which could make you less active. It could also affect the way your body uses energy.
If you're worried about putting on weight with propranolol, speak to your doctor.
Will it affect my contraception?Propranolol will not stop your contraception working.
However, some types of hormonal methods of contraception, like the combined pill and contraceptive patch, are not usually recommended if you're taking propranolol or other medicines for high blood pressure. This is because some hormonal contraceptives can raise your blood pressure and stop propranolol working properly.
Talk to your doctor if you're taking a hormonal contraceptive.
If propranolol makes you sick (vomit) or have severe diarrhoea for more than 24 hours, your contraceptive pills may not protect you from pregnancy. Look on the pill packet to find out what to do.
Read more about what to do if you're on the pill and you're being sick or have diarrhoea.
Will it affect my fertility?There is no evidence that propranolol affects fertility in men or women.
If you're trying to get pregnant, or you're having problems getting pregnant while on propranolol, speak to your doctor.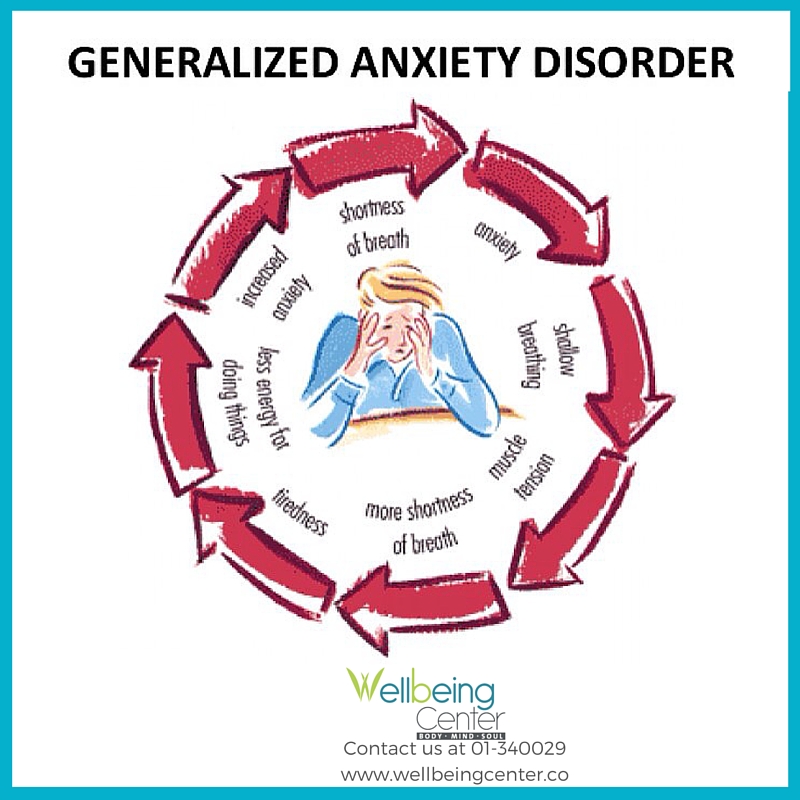
Some people on propranolol say their sex drive goes down and some men find they cannot get an erection. However, this is not a common side effect and there is not enough evidence to say for sure that propranolol is causing it.
If you're having problems with your sex life, talk to your doctor.
Do I need to avoid playing sports?You do not need to stop playing sports if you take propranolol. But do not push yourself too much.
Regular exercise is good for you because it lowers blood pressure by keeping your heart and blood vessels in good condition.
Be aware, though, that in some sports propranolol is not allowed if you're competing at a high level.
Can I drive or ride a bike?Propranolol can make some people feel dizzy, especially when they first start taking it or after taking a bigger dose.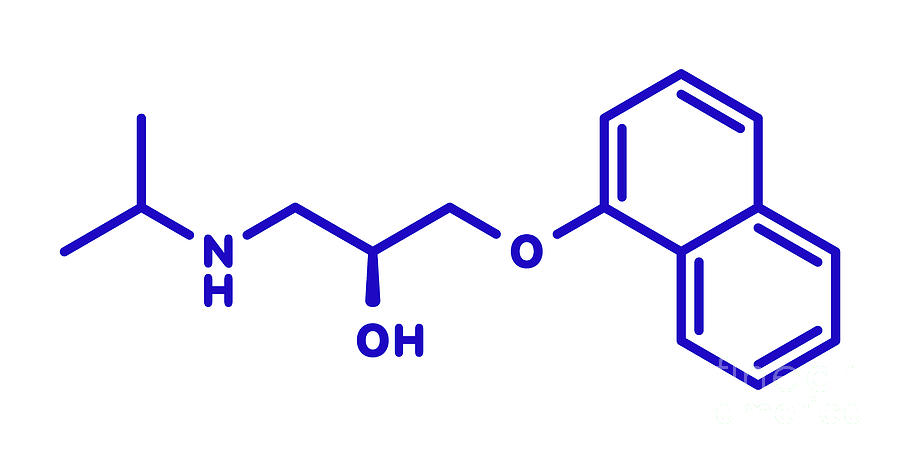 If this happens to you, do not drive a car, ride a bike, or use tools or machinery.
If this happens to you, do not drive a car, ride a bike, or use tools or machinery.
It's an offence to drive a car if your ability to drive safely is affected. It's your responsibility to decide if it's safe to drive. If you're in any doubt, do not drive.
Talk to your doctor or pharmacist if you're unsure whether it's safe for you to drive while taking propranolol. GOV.UK has more information on the law on drugs and driving.
Can lifestyle changes help?If you have heart problems, you can boost the health of your heart by making some key lifestyle changes. These changes will also help if you have high blood pressure.
- Quit smoking – smoking increases your heart rate and blood pressure. Quitting smoking brings down your blood pressure and relieves heart failure symptoms. Try to avoid second-hand smoke too.
- Cut down on alcohol – drinking alcohol while you're taking propranolol can make you feel dizzy or light headed.
 Also drinking too much alcohol raises blood pressure over time and makes heart failure worse. It's best to keep to the recommended limit of no more than 14 units of alcohol a week. A standard glass of wine (175ml) is 2 units. A pint of lager or beer is usually 2 to 3 units of alcohol.
Also drinking too much alcohol raises blood pressure over time and makes heart failure worse. It's best to keep to the recommended limit of no more than 14 units of alcohol a week. A standard glass of wine (175ml) is 2 units. A pint of lager or beer is usually 2 to 3 units of alcohol. - Exercise – regular exercise lowers blood pressure by keeping your heart and blood vessels in good condition. It does not need to be too energetic, walking every day will help.
- Eat well – aim to eat a diet that includes plenty of fruit and vegetables, wholegrains, fat-free or low-fat dairy products and lean proteins. It's a good idea to follow these tips for a lower salt diet too. Eating too much salt is the biggest cause of high blood pressure. The more salt you eat, the higher your blood pressure will be. Aim for no more than 6g of salt a day.
- Deal with stress – when you're anxious or upset, your heart beats faster, you breathe more heavily and your blood pressure often goes up.
 This can make heart failure worse too. Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help avoid stress.
This can make heart failure worse too. Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help avoid stress.
If you get severe headaches, there are steps you can take to help prevent migraines. This includes working out what things trigger an attack so you can avoid them.
Propranolol for the treatment of anxiety disorders: Systematic review and meta-analysis
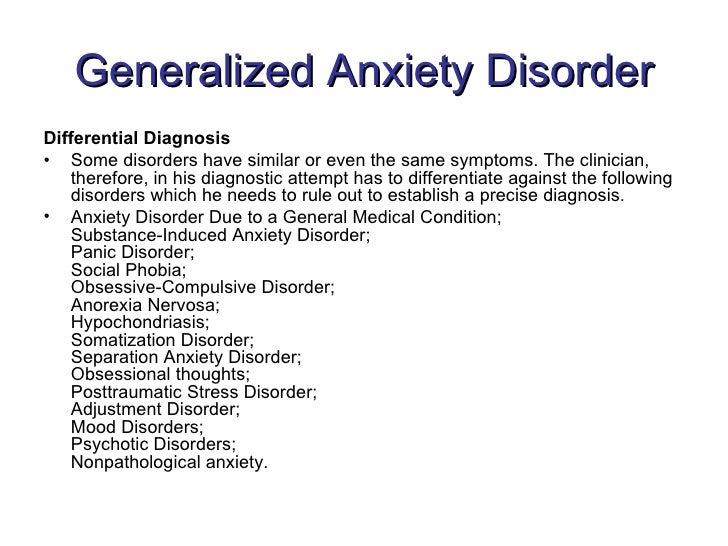
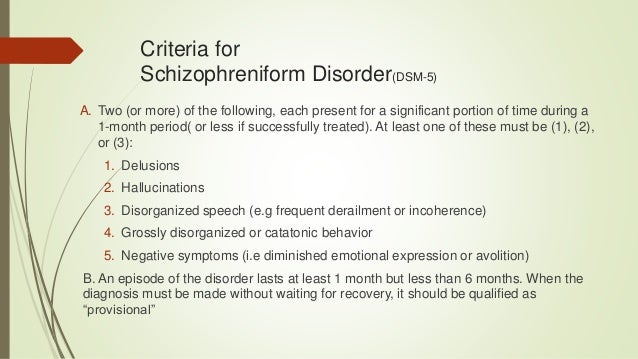
American Psychiatric Association (2013) Diagnostic and Statistical Manual of Mental Disorders, 5th Edition Washington, DC: American Psychiatric Association. [Google Scholar]
Baldwin DS, Anderson IM, Nutt DJ, et al. (2014) Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: A revision of the 2005 guidelines from the British Association for Psychopharmacology. J Psychopharmacol 28: 403–439.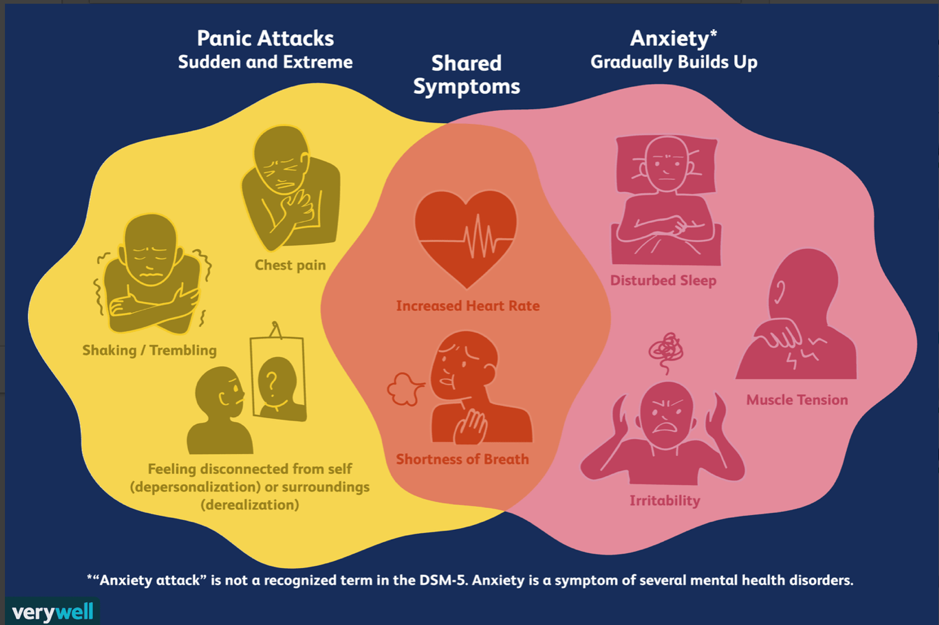 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
Balon R, Yeragani VK, Pohl R, et al. (1990) Somatic and psychological symptoms during isoproterenol-induced panic attacks. Psychiatry Res 32: 103–112. [PubMed] [Google Scholar]
Becker AL. (1976) Oxprenolol and propranolol in anxiety states. A double-blind comparative study. S Afr Med J 50: 627–629. [PubMed] [Google Scholar]
Black JW, Crowther AF, Shanks RG, et al. (1964) A new adrenergic betareceptor antagonist. Lancet 1: 1080–1081. [PubMed] [Google Scholar]
Brantigan CO, Brantigan TA, Joseph N. (1982) Effect of beta blockade and beta stimulation on stage fright. Am J Med 72: 88–94. [PubMed] [Google Scholar]
Brewer C. (1972) Beneficial effect of beta-adrenergic blockade on ‘exam nerves’. Lancet 2: 435. [PubMed] [Google Scholar]
Brunet A, Orr SP, Tremblay J, et al. (2008) Effect of post-retrieval propranolol on psychophysiologic responding during subsequent script-driven traumatic imagery in post-traumatic stress disorder. J Psychiatr Res 42: 503–506. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
Clark DB, Agras WS. (1991) The assessment and treatment of performance anxiety in musicians. Am J Psychiatry 148: 598–605. [PubMed] [Google Scholar]
Clark DM. (1986) A cognitive approach to panic. Behav Res Ther 24: 461–470. [PubMed] [Google Scholar]
Debiec J, Ledoux JE. (2004) Disruption of reconsolidation but not consolidation of auditory fear conditioning by noradrenergic blockade in the amygdala. Neuroscience 129: 267–272. [PubMed] [Google Scholar]
Drew PJ, Barnes JN, Evans SJ. (1985) The effect of acute beta-adrenoceptor blockade on examination performance. Br J Clin Pharmacol 19: 783–786. [PMC free article] [PubMed] [Google Scholar]
Dyck JB, Chung F. (1991) A comparison of propranolol and diazepam for preoperative anxiolysis. Can J Anaesth 38: 704–709. [PubMed] [Google Scholar]
Elman MJ, Sugar J, Fiscella R, et al. (1998) The effect of propranolol versus placebo on resident surgical performance. Trans Am Ophthalmol Soc 96: 283–291; discussion 291–294.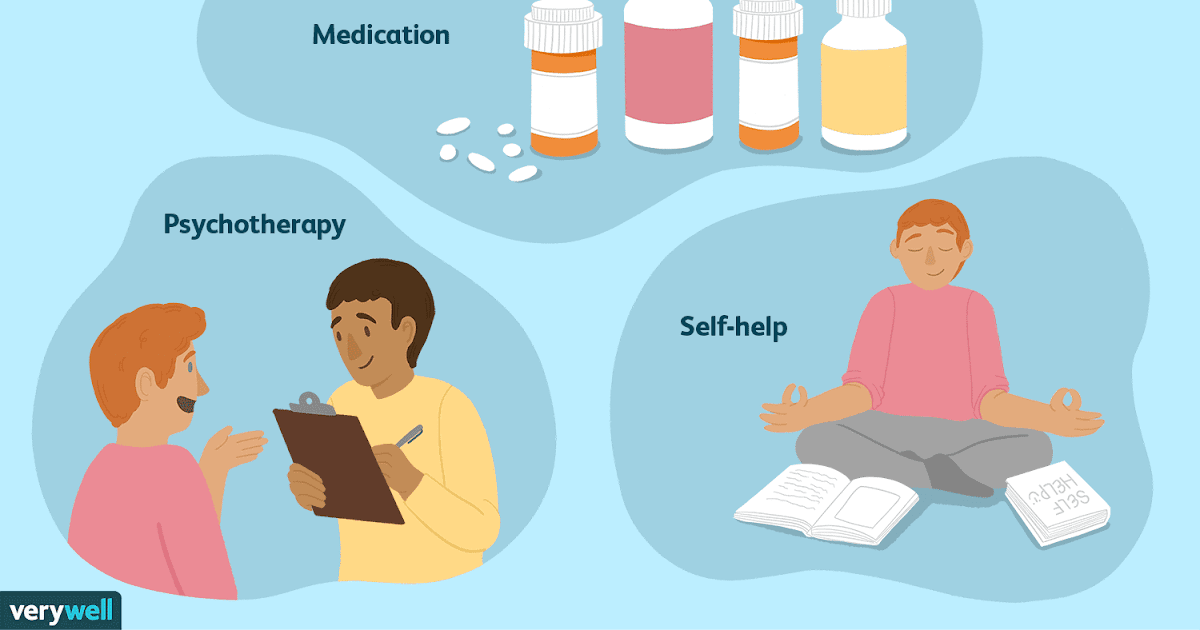 [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
Fagerström KO, Hugdahl K, Lundström N. (1985) Effect of beta-receptor blockade on anxiety with reference to the three-systems model of phobic behavior. Neuropsychobiology 13: 187–193. [PubMed] [Google Scholar]
Falloon IR, Lloyd GG, Harpin RE. (1981) The treatment of social phobia. Real-life rehearsal with nonprofessional therapists. J Nerv Mental Dis 169: 180–184. [PubMed] [Google Scholar]
Finnie PSB, Nader K. (2012) The role of metaplasticity mechanisms in regulating memory destabilization and reconsolidation. Neurosci Biobehav Rev 36: 1667–1707. [PubMed] [Google Scholar]
Fleminger S, Greenwood RJ, Oliver DL. (2006) Pharmacological management for agitation and aggression in people with acquired brain injury. Cochrane Database Syst Rev 4: CD003299. [PubMed] [Google Scholar]
Freemantle N, Cleland J, Young P, et al. (1999) beta Blockade after myocardial infarction: Systematic review and meta regression analysis. BMJ 318: 1730–1737. [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
Fuster V, Rydén LE, Cannom DS, et al. (2006) ACC/AHA/ESC 2006 Guidelines for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice. Circulation 114: e257–e354. [PubMed] [Google Scholar]
Gardner D. (2010) A pill to block out the bad memories: Experts make breakthrough to help people forget traumatic past events. Daily Mail, 23rd November Available at: http://www.dailymail.co.uk/health/article-1332181/Experts-make-breakthrough-help-people-forget-traumatic-past-events.html#ixzz2yqLLsBQ7 (accessed 8 July 2015).
Giles J. (2005) Beta-blockers tackle memories of horror. Nature 436: 448–449. [PubMed] [Google Scholar]
Grosz HJ. (1972) Narcotic withdrawal symptoms in heroin users treated with propranolol. Lancet 2: 564–566. [PubMed] [Google Scholar]
Hamilton M.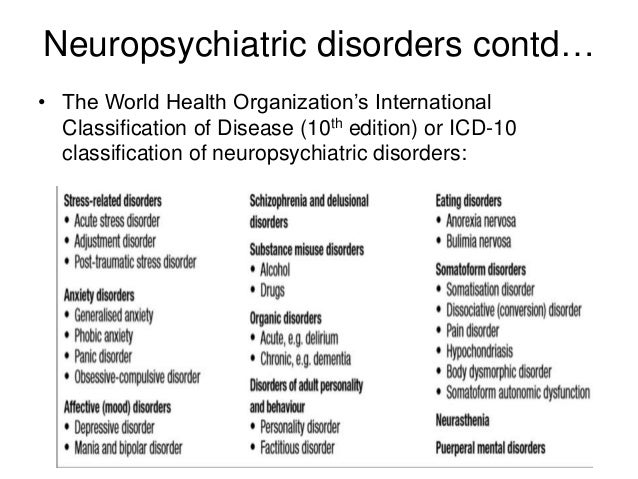 (1959) The assessment of anxiety states by rating. Br J Med Psychol 32: 50–55. [PubMed] [Google Scholar]
(1959) The assessment of anxiety states by rating. Br J Med Psychol 32: 50–55. [PubMed] [Google Scholar]
Higgins J, Altman D, Sterne J. (2011a) Chapter 8: Assessing risk of bias in included studies. In: Higgins J, Green S. (eds), Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0., The Cochrane Collaboration. Available at: http://www.cochrane-handbook.org/ (accessed 9 July 2015).
Higgins J, Deeks J, Altman D. (2011b) Chapter 16: Special topics in statistics. In: Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. Available at: http://www.cochrane-handbook.org/ (accessed 9 July 2015).
Jakobsson J, Rane K, Ryberg G. (1995) Oral premedication one hour before minor gynaecological surgery – does it have any effect? A comparison between ketobemidone, lorazepam, propranolol and placebo. Acta Anaesthesiol Scand 39: 359–363. [PubMed] [Google Scholar]
Johansen JP, Cain CK, Ostroff LE, et al. (2011) Molecular mechanisms of fear learning and memory.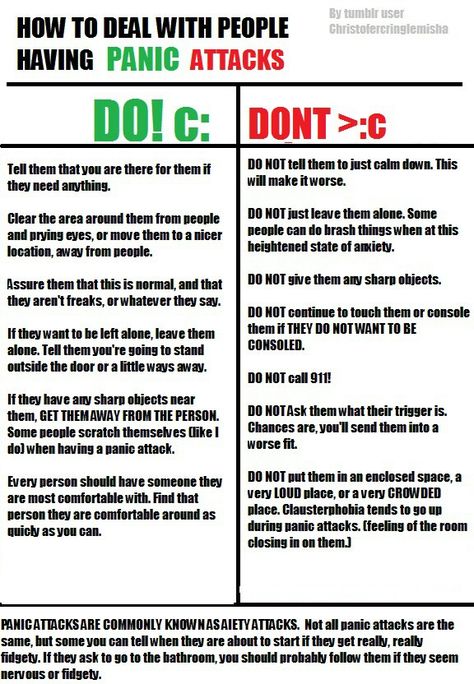 Cell 147: 509–524. [PMC free article] [PubMed] [Google Scholar]
Cell 147: 509–524. [PMC free article] [PubMed] [Google Scholar]
Kathol RG, Noyes R, Slymen DJ, et al. (1980) Propranolol in chronic anxiety disorders. A controlled study. Arch Gen Psychiatry 37: 1361–1365. [PubMed] [Google Scholar]
Kindt M, Soeter M, Vervliet B. (2009) Beyond extinction: Erasing human fear responses and preventing the return of fear. Nat Neurosci 12: 256–258. [PubMed] [Google Scholar]
Lehrer J. (2012) The forgetting pill erases painful memories forever. Wired, 17th February Available at: http://www.wired.com/2012/02/ff_forgettingpill/all/ (accessed 8 July 2015).
Liu HH, Milgrom P, Fiset L. (1991) Effect of a beta-adrenergic blocking agent on dental anxiety. J Dent Res 70: 1306–1308. [PubMed] [Google Scholar]
Lonergan MH, Olivera-Figueroa LA, Pitman RK, et al. (2013) Propranolol’s effects on the consolidation and reconsolidation of long-term emotional memory in healthy participants: A meta-analysis. J Psychiatry Neurosci 38: 222–231. [PMC free article] [PubMed] [Google Scholar]
McGaugh JL. (2000) Memory – a century of consolidation. Science 287: 248–251. [PubMed] [Google Scholar]
(2000) Memory – a century of consolidation. Science 287: 248–251. [PubMed] [Google Scholar]
Mealy K, Ngeh N, Gillen P, et al. (1996) Propranolol reduces the anxiety associated with day case surgery. Eur J Surg 162: 11–14. [PubMed] [Google Scholar]
Meibach RC, Dunner D, Wilson LG, et al. (1987) Comparative efficacy of propranolol, chlordiazepoxide, and placebo in the treatment of anxiety: A double-blind trial. J Clin Psychiatry 48: 355–358. [PubMed] [Google Scholar]
Merlo E, Milton AL, Goozee ZY, et al. (2014) Reconsolidation and extinction are dissociable and mutually exclusive processes: Behavioral and molecular evidence. J Neurosci 34: 2422–2431. [PMC free article] [PubMed] [Google Scholar]
Merlo E, Milton AL, Everitt BJ. (2015) Enhancing cognition by affecting memory reconsolidation. Curr Opin Behav Sci 4: 41–47. [Google Scholar]
Michelson D, Allgulander C, Dantendorfer K, et al. (2001) Efficacy of usual antidepressant dosing regimens of fluoxetine in panic disorder: Randomised, placebo-controlled trial. Br J Psychiatry 179: 514–518. [PubMed] [Google Scholar]
Br J Psychiatry 179: 514–518. [PubMed] [Google Scholar]
Mitte K. (2005) A meta-analysis of the efficacy of psycho- and pharmacotherapy in panic disorder with and without agoraphobia. J Affect Disord 88: 27–45. [PubMed] [Google Scholar]
Moher D, Liberati A, Tetzlaff J, et al. (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6: e1000097. [PMC free article] [PubMed] [Google Scholar]
Munjack DJ, Crocker B, Cabe D, et al. (1989) Alprazolam, propranolol, and placebo in the treatment of panic disorder and agoraphobia with panic attacks. J Clin Psychopharmacol 9: 22–27. [PubMed] [Google Scholar]
Munjack DJ, Rebal R, Shaner R, et al. (1985) Imipramine versus propranolol for the treatment of panic attacks: A pilot study. Compr Psychiatry 26: 80–89. [PubMed] [Google Scholar]
Nader K, Schafe GE, Le Doux JE. (2000) Fear memories require protein synthesis in the amygdala for reconsolidation after retrieval. Nature 406: 722–726. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
Noyes R, Anderson DJ, Clancy J, et al. (1984) Diazepam and propranolol in panic disorder and agoraphobia. Arch Gen Psychiatry 41: 287–292. [PubMed] [Google Scholar]
Oehrberg S, Christiansen PE, Behnke K, et al. (1995) Paroxetine in the treatment of panic disorder. A randomised, double-blind, placebo-controlled study. Br J Psychiatry 167: 374–379. [PubMed] [Google Scholar]
Otto MW, Tuby KS, Gould RA, et al. (2001) An effect-size analysis of the relative efficacy and tolerability of serotonin selective reuptake inhibitors for panic disorder. Am J Psychiatry 158: 1989–1992. [PubMed] [Google Scholar]
Ratey JJ, Bemporad J, Sorgi P, et al. (1987) Open trial effects of beta-blockers on speech and social behaviors in 8 autistic adults. J Autism Dev Disord 17: 439–446. [PubMed] [Google Scholar]
Ravaris CL, Friedman MJ, Hauri PJ, et al. (1991) A controlled study of alprazolam and propranolol in panic-disordered and agoraphobic outpatients. J Clin Psychopharmacol 11: 344–350.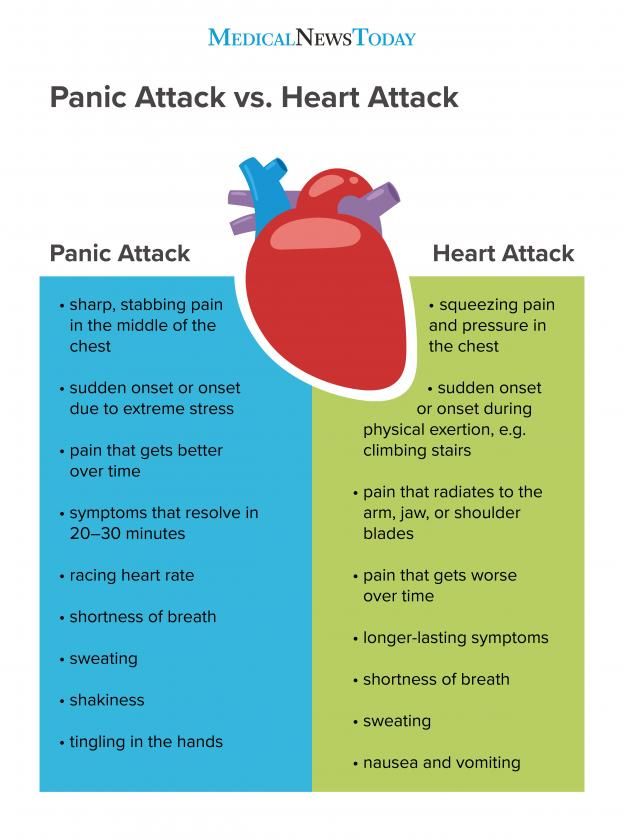 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
Roy-Byrne P, Stein M, Hermann R. (2013) Pharmacotherapy for panic disorder.In: Post T. (ed.) UpToDate®. Waltham, MA: UpToDate® Available at: http://www.uptodate.com/contents/pharmacotherapy-for-panic-disorder (accessed 9 July 2015). [Google Scholar]
Roy-Byrne PP, Craske MG, Stein MB. (2006) Panic disorder. Lancet 368: 1023–1032. [PubMed] [Google Scholar]
Sandoz (2012) 1.3.1.1. Summary of product characteristics: Paroxetine Sandoz® 10/20/30 tablets RVG 33722–3–26613. Almere. [Google Scholar]
Schmidt FL, Oh I-S, Hayes TL. (2009) Fixed- versus random-effects models in meta-analysis: Model properties and an empirical comparison of differences in results. Br J Math Stat Psychol 62: 97–128. [PubMed] [Google Scholar]
Sevenster D, Beckers T, Kindt M. (2013) Prediction error governs pharmacologically induced amnesia for learned fear. Science 339: 830–833. [PubMed] [Google Scholar]
Soeter M, Kindt M. (2010) Dissociating response systems: Erasing fear from memory. Neurobiol Learn Mem 94: 30–41. [PubMed] [Google Scholar]
Neurobiol Learn Mem 94: 30–41. [PubMed] [Google Scholar]
Stone W, Gleser G, Gottschalk L. (1973) Anxiety and beta-adrenergic blockade. Arch Gen Psychiatry 29: 620–622. [PubMed] [Google Scholar]
Turner P, Granville-Grossman KL. (1965) Effect of adrenergic receptor blockade of the tachycardia of thyrotoxicosis and anxiety state. Lancet 2: 1316–1318. [PubMed] [Google Scholar]
Webb AJS, Fischer U, Mehta Z, et al. (2010) Effects of antihypertensive-drug class on interindividual variation in blood pressure and risk of stroke: A systematic review and meta-analysis. Lancet 375: 906–915. [PubMed] [Google Scholar]
Wheatley D. (1969) Comparative effects of propranolol and chlordiazepoxide in anxiety states. Br J Psychiatry 115: 1411–1412. [PubMed] [Google Scholar]
Wilkinson G, Balestrieri M, Ruggeri M, et al. (1991) Meta-analysis of double-blind placebo-controlled trials of antidepressants and benzodiazepines for patients with panic disorders. Psychol Med 21: 991–998. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
Yorkston NJ, Zaki SA, Malik MK, et al. (1974) Propranolol in the control of schizophrenic symptoms. BMJ 4: 633–635. [PMC free article] [PubMed] [Google Scholar]
FGBNU NTsPZ. ‹‹Panic disorder (clinic, diagnosis, therapy)››
Isolation of PD was significant not only according to clinical criteria, but also according to the characteristics of the patients' response to therapy, which include:
-
High efficacy of antidepressants;
-
Insufficient effect of the use of traditional benzodiazepine tranquilizers;
-
Insufficient effectiveness of psychotherapy. nine0003
Russian psychiatrists still practice the use of traditional benzodiazepines (diazepam, chlordiazepoxide, phenazepam) in PR, less often - small doses of antidepressants (amitriptyline, azaphen) and small antipsychotics (teralen, sonapax), or a combination of these groups of drugs often does not lead to to a lasting and pronounced effect.
It is now established that PR responds well to pharmacotherapy. Panic disorder treatment can be divided into 3 main steps:
-
Stopping PN up to the establishment of remission (4-6 weeks - 2-3 months)
-
Stabilizing (further treatment) therapy to consolidate the results, restore the level of social adaptation, overcome agoraphobic manifestations (anticipation anxiety, avoidant behavior) and early relapses (4-6 months). At this stage, it is necessary to conduct adequate psychotherapy.
-
Prophylactic (long-term) therapy aimed at preventing the development of relapses and maintaining a stable remission (up to 1 year or more)
Currently, the following anti-panic (used to block PN) drugs are distinguished: tricyclic antidepressants, selective serotonergic drugs, MAO inhibitors, etc. atypical (or high potency) benzodiazepines (alprazolam and clonazepam).
A) Tricyclic antidepressants (TAD).
The most commonly used tricyclic antidepressants are clomipramine (anafranil), imipramine (melipramine), demipramine (petilil, pertofran), nortriptyline, and amitriptyline. The effectiveness of the tetracyclic antidepressant maprotiline (Ludiomil) and the atypical TAD tianeptine (Coaxil, Stablon) similar in action to TAD is described. Clomipramine (anafranil) is the most commonly used and most effective TAD in the treatment of PR. nine0003
TAD treatment is initiated at low doses (12.5–25 mg/day) and then gradually increased to a tolerable level (average 12.5–25 mg over 3–5 days). The average effective daily dose is usually 150-200 mg / day, rarely reaches 300 mg. The anti-panic effect of TAD is also “delayed” like the thymoanaleptic, but comes on somewhat faster - the latent period is usually about two weeks. TAD has an effect in PR mainly due to the effect on the thymic and especially on the phobic component, less affecting the expectation anxiety and somatovegetative manifestations. In the case of a good reaction, a decrease in the frequency of PR occurs rather quickly, anxiety of expectation and phobias are reduced, and mood is evened out. However, in half of the patients, from the first days of TAD use, an increase in anxiety and vegetative symptoms occurs, which increases the occurrence of PP, therefore, with an inadequate increase in dosages, the patient's condition either does not improve at all, or the initial improvement will be lost after a few weeks. Patients may reach a “tolerance plateau” two or three times before the final dose is selected. To avoid premature discontinuation of the drug, any benzodiazepine drugs (diazepam 5-10 mg / day, phenazepam 0.5-1 mg / day), as well as α-blockers (anaprilin 20-40 mg / day), can be added to TAD, which allows to reduce the severity of exacerbation of PR and wait for a somewhat delayed effect of the antidepressant. TAD treatment is continued for 4-6 months, and if the condition is stable, a gradual reduction in dose levels is started, which usually lasts 1-2 months.
In the case of a good reaction, a decrease in the frequency of PR occurs rather quickly, anxiety of expectation and phobias are reduced, and mood is evened out. However, in half of the patients, from the first days of TAD use, an increase in anxiety and vegetative symptoms occurs, which increases the occurrence of PP, therefore, with an inadequate increase in dosages, the patient's condition either does not improve at all, or the initial improvement will be lost after a few weeks. Patients may reach a “tolerance plateau” two or three times before the final dose is selected. To avoid premature discontinuation of the drug, any benzodiazepine drugs (diazepam 5-10 mg / day, phenazepam 0.5-1 mg / day), as well as α-blockers (anaprilin 20-40 mg / day), can be added to TAD, which allows to reduce the severity of exacerbation of PR and wait for a somewhat delayed effect of the antidepressant. TAD treatment is continued for 4-6 months, and if the condition is stable, a gradual reduction in dose levels is started, which usually lasts 1-2 months. In the future, decide on a longer prophylactic therapy. Thus, the main disadvantages of TAD are the delayed effect and pronounced side effects, especially those associated with hyperstimulation of the autonomic nervous system: palpitations, tremor, hyperhidrosis, dizziness, anticholinergic effects, paradoxical increase in blood pressure, sexual dysfunction, weight gain. These effects are especially pronounced in amitriptyline, which significantly limits its use in this group of patients. Efficacy was noted in some patients with PR of the atypical TAD tianeptine (coaxil) at a dose of 37.5 mg/day. Decrease or blockade of PP, reduction or decrease in the intensity of agoraphobia are observed by 5-6 weeks of treatment. A good effect is noted in patients with "atypical" PP and signs of "secondary" depression, comorbid PD. nine0003
In the future, decide on a longer prophylactic therapy. Thus, the main disadvantages of TAD are the delayed effect and pronounced side effects, especially those associated with hyperstimulation of the autonomic nervous system: palpitations, tremor, hyperhidrosis, dizziness, anticholinergic effects, paradoxical increase in blood pressure, sexual dysfunction, weight gain. These effects are especially pronounced in amitriptyline, which significantly limits its use in this group of patients. Efficacy was noted in some patients with PR of the atypical TAD tianeptine (coaxil) at a dose of 37.5 mg/day. Decrease or blockade of PP, reduction or decrease in the intensity of agoraphobia are observed by 5-6 weeks of treatment. A good effect is noted in patients with "atypical" PP and signs of "secondary" depression, comorbid PD. nine0003
B) selective serotonin reuptake inhibitors (SSRIs).
In addition to TAD, selective serotonin reuptake inhibitors are effective in the treatment of PR: fluoxetine (Prozac, Portal, Prodep), fluvoxamine (fevarin, floxifral. Luvox), sertraline (Zoloft), paroxetine (Paxil), citalopram (Cipramil). The main disadvantage of this group is the occurrence during the first 2-3 weeks of treatment of hyperstimulation (irritability, insomnia, nervousness) and increased anxiety and panic symptoms (probably due to excessive stimulation of serotonin autoreceptors). The technique of application does not differ from the treatment of depression, but the initial doses are usually minimal (5 mg fluoxetine, 50 mg fluvoxamine, 25 mg sertraline). Within 2 weeks, the dose is brought to an average, and then, if necessary, it is increased or remains the same. Subsequently, even with prolonged therapy, the dose does not change. For long-term (maintenance) treatment, drugs are much more convenient than TAD due to the lack of anticholinergic and adrenergic effects and possible single dose during the day. nine0003
Luvox), sertraline (Zoloft), paroxetine (Paxil), citalopram (Cipramil). The main disadvantage of this group is the occurrence during the first 2-3 weeks of treatment of hyperstimulation (irritability, insomnia, nervousness) and increased anxiety and panic symptoms (probably due to excessive stimulation of serotonin autoreceptors). The technique of application does not differ from the treatment of depression, but the initial doses are usually minimal (5 mg fluoxetine, 50 mg fluvoxamine, 25 mg sertraline). Within 2 weeks, the dose is brought to an average, and then, if necessary, it is increased or remains the same. Subsequently, even with prolonged therapy, the dose does not change. For long-term (maintenance) treatment, drugs are much more convenient than TAD due to the lack of anticholinergic and adrenergic effects and possible single dose during the day. nine0003
B) monoamine oxidase inhibitors (MAOIs).
In Russia in recent years, only the so-called. reversible MAOIs (moclobemide (Aurorix) and pyrazidol).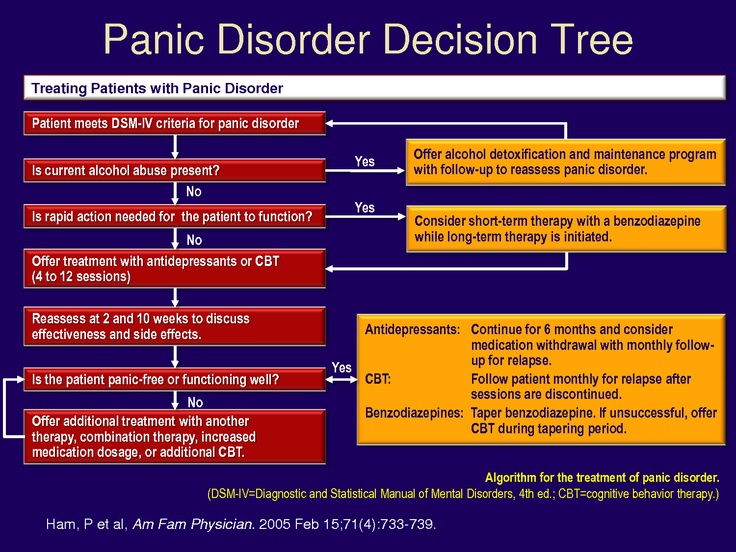 They are usually used in cases of intolerance to the above drugs - studies on their use are insufficient. In general, they seem to be inferior in effectiveness to the above drugs, but are much better tolerated. Moclobemide is particularly effective in the combination of PP with social phobia. Treatment begins with 25-50 mg / day with a gradual increase in dose of 50 mg / day. The effective daily dose is usually 450-600 mg/day. nine0003
They are usually used in cases of intolerance to the above drugs - studies on their use are insufficient. In general, they seem to be inferior in effectiveness to the above drugs, but are much better tolerated. Moclobemide is particularly effective in the combination of PP with social phobia. Treatment begins with 25-50 mg / day with a gradual increase in dose of 50 mg / day. The effective daily dose is usually 450-600 mg/day. nine0003
D) Atypical (high potency) benzodizepines (ABZD).
An important group for the treatment of PR are atypical benzodiazepines: alprazolam (Xanax, Cassadan) and clonazepam (Antelepsin, Rivotril). Features of ABZD is their high affinity for benzodiazepine receptors (3 times higher than that of typical BZD). Unlike antidepressants, which reduce PN and agoraphobia, but have little effect on the anxiety of expecting an attack, alprozalam not only suppresses the anticipation and avoidance component (agoraphobic), but also stops the psychopathological and somatovegetative manifestations of the attack itself (panic component) and prevents the development of PN. In addition, it practically does not cause side effects up to a dose of 4-6 mg / day, i.e. it has a very good tolerance. The drug does not cause exacerbation of anxiety like antidepressants, the anti-panic effect develops without a "latent period". In addition, alprazolam has a distinct antidepressant (thymoanaleptic) effect, which develops 2-3 weeks after the start of therapy. The disadvantage is the possibility of developing dependence (substance abuse) and "withdrawal syndrome", as well as the need for 3-4 times a day due to a short half-life (the prolonged form of Xanax retard is free from this disadvantage). Rarely, compared with other BZD, weakness, lethargy, drowsiness, fatigue, ataxia are noted. The likelihood of developing dependence limits the possibility of long-term (more than 4-6 weeks) taking the drug, however, if antidepressants are intolerant, alprazolam must be prescribed for a long time, followed by an extremely slow dose reduction. Initial doses of alprazolam 0.25-0.
In addition, it practically does not cause side effects up to a dose of 4-6 mg / day, i.e. it has a very good tolerance. The drug does not cause exacerbation of anxiety like antidepressants, the anti-panic effect develops without a "latent period". In addition, alprazolam has a distinct antidepressant (thymoanaleptic) effect, which develops 2-3 weeks after the start of therapy. The disadvantage is the possibility of developing dependence (substance abuse) and "withdrawal syndrome", as well as the need for 3-4 times a day due to a short half-life (the prolonged form of Xanax retard is free from this disadvantage). Rarely, compared with other BZD, weakness, lethargy, drowsiness, fatigue, ataxia are noted. The likelihood of developing dependence limits the possibility of long-term (more than 4-6 weeks) taking the drug, however, if antidepressants are intolerant, alprazolam must be prescribed for a long time, followed by an extremely slow dose reduction. Initial doses of alprazolam 0.25-0. 5 mg/day with an increase of 0.25-0.5 mg every 3 days until complete blockade of the occurrence of PP. Preservation of PP, their recurrence indicates an insufficient dose of the drug, and side effects (sedation, lethargy, drowsiness) indicate the need to reduce the dose. Average doses are 4-6 mg/day, treatment is continued for 4-6 months after which, with good adaptation of patients, the dose is reduced at an average rate of 0.5 mg per week in order to avoid withdrawal syndrome. nine0003
5 mg/day with an increase of 0.25-0.5 mg every 3 days until complete blockade of the occurrence of PP. Preservation of PP, their recurrence indicates an insufficient dose of the drug, and side effects (sedation, lethargy, drowsiness) indicate the need to reduce the dose. Average doses are 4-6 mg/day, treatment is continued for 4-6 months after which, with good adaptation of patients, the dose is reduced at an average rate of 0.5 mg per week in order to avoid withdrawal syndrome. nine0003
Clonazepam (antelepsin, rivotril) also has a pronounced anti-panic effect at a dose of 2-6 mg/day, however, it has more pronounced side effects (drowsiness, lethargy, ataxia, depressogenicity), which limits its use. At the same time, due to the longer half-life, a milder “withdrawal syndrome” is noted, there is no need for a three-time mandatory appointment, and it is easier to reduce the dose. The initial dose is usually 0.5 mg 2 times a day, with a gradual increase to 2-6 mg / day. nine0003
In long-term treatment with BDD, the safety, efficacy, and indications for therapy should be periodically assessed. It is recommended to answer the following questions at certain intervals (2-4 months):
It is recommended to answer the following questions at certain intervals (2-4 months):
-
Do existing disorders justify continued therapy? Did the patient feel much better after BZD therapy?
-
Does the duration of use remain within the prescribed range, has the patient avoided other unprescribed medications? nine0003
-
Does the patient show signs of intoxication or confusion associated with the use of BZD or their combination with other drugs?
Any “no” answer is an indication that treatment should be stopped. Attempts to gradually reduce the dose are recommended every 4 months. In some patients, the drug can be completely canceled, in others an exacerbation occurs, requiring the resumption of treatment. Intermittent breaks in treatment may help to identify patients with persistent anxiety but good BZD effect: they are especially indicated for long-term therapy.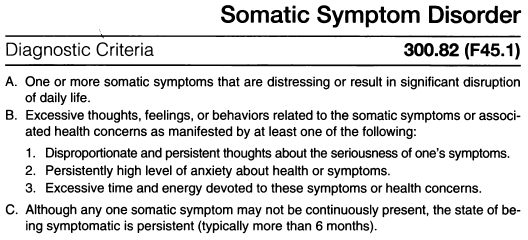 The FDA Commission (USA) in its recommendations indicates that the use of BZD for more than 4 months has not been studied. In addition, patients with personality disorders and substance abuse (including alcohol abuse) should not be treated long-term with BDD, even if they have a history. nine0003
The FDA Commission (USA) in its recommendations indicates that the use of BZD for more than 4 months has not been studied. In addition, patients with personality disorders and substance abuse (including alcohol abuse) should not be treated long-term with BDD, even if they have a history. nine0003
Traditional BZD in an isolated form are currently rarely used in PD, prescribed only as "correctors" of antidepressants in the initial phase of treatment or even anticipating the appointment of the latter ("premedication").
E) Criteria for choosing drugs.
Therapy with TAD and especially with clomipramine is clearly effective in patients with rapid onset of depression with endogeneity traits, with a high proportion of maniophobia and depersonalization-derealization disorders in the structure of PP. In patients with late addition of depression to PR, its atypical, erased character, high proportion of pseudosomatic (somatovegetative) and conversion disorders, rare agoraphobia, the effectiveness of TAD is usually low.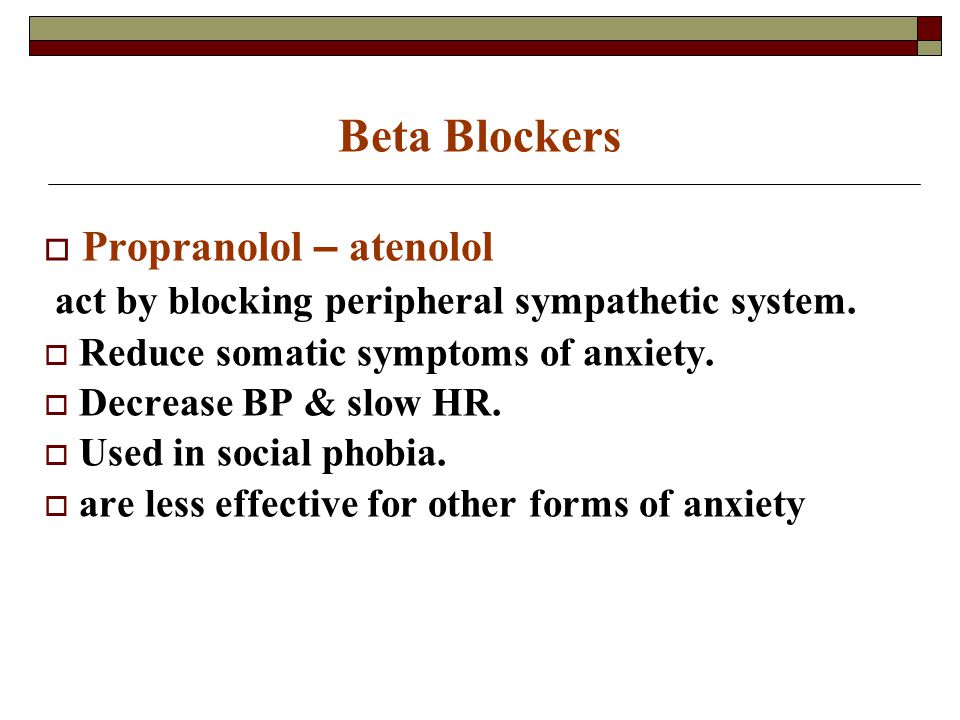 This subtype of PR is closer to the diagnosis of hypochondriacal development or "somatoform disorder" according to ICD-10. Thus, the more pronounced the mental component of anxiety and the more phobic experiences are presented, the greater the effect of TAD can be expected and the less exacerbation of PR during treatment. nine0003
This subtype of PR is closer to the diagnosis of hypochondriacal development or "somatoform disorder" according to ICD-10. Thus, the more pronounced the mental component of anxiety and the more phobic experiences are presented, the greater the effect of TAD can be expected and the less exacerbation of PR during treatment. nine0003
With a stronger representation of the somatovegetative components of the PR (compared to the "mental"), the effectiveness of TAs is less, they are worse tolerated and more often cause exacerbation of the PR. In these cases, it is necessary to decide whether to replace the TAD with an ABSA or an MAOI.
The ideal target for ABZD are predominantly somatovegetative PP without distinct agoraphobia; with severe phobic symptoms, their use does not lead to a clear effect, stopping only the anxiety of expectation and PP. A high incidence of PP and alexithymia (i.e., the inability of patients to adequately express their experiences or talk about them) are also predictors of the low effectiveness of ABZD.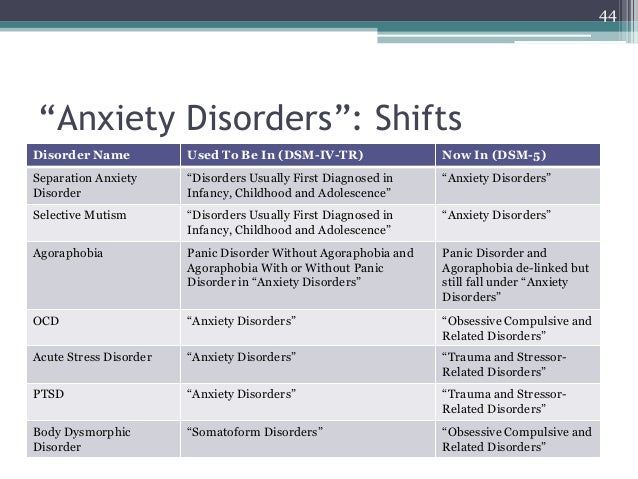 nine0003
nine0003
Thus, if we proceed from traditional nosological ideas about the place of PD as a syndrome in the structure of a particular disease, then when choosing therapy, the following should be taken into account: psychopathological phenomena (fear of going crazy, depression, depersonalization, anxiety,) “large” TADs (clomipramine, impramine, amitriptyline) are most effective. Their significance will increase even more as the PR picture approaches the melancholic raptus. Clomipramine, SSRIs, MAOIs are also the drug of choice for severe agoraphobia or the presence of other concomitant phobias or obsessions that may not be thematically related to agoraphobia, i.e. with a large proportion of ideational obsessions within the framework of sluggish schizophrenia, cyclothymia. TIR. nine0003
In case of PR within the framework of neurosis, the value of clomipramine and SSRIs is high in case of obsessive-compulsive disorder, but decreases in asthenic neurosis and hysteria, where ABZD or MAOI are more effective.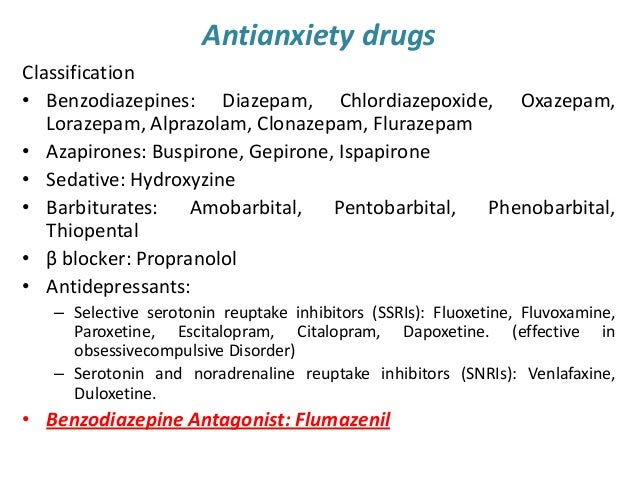
It should be noted that in the treatment of patients with PD, it is often necessary to combine basic "anti-panic" drugs with drugs that allow influencing psychopathic (most often hysterical) and overvalued (hypochondriac) disorders. In such situations, drugs from the group of neuroleptics are added to the basic drugs: thioridazine (sonapax), alimemazine (teralen), periciazine (neuleptil), sulpiride (eglonil), chrolprothixen. In addition, when diagnosing a schizophrenic process, it is necessary to add antipsychotics to the “syndromal” therapy, which have an anti-negative effect and affect the overall progression of the disease (trifluoperazine (triftazin, stelazin), clozapine (azaleptin, leponex), risperidone (rispolept), etc.). nine0003
E) PR psychotherapy.
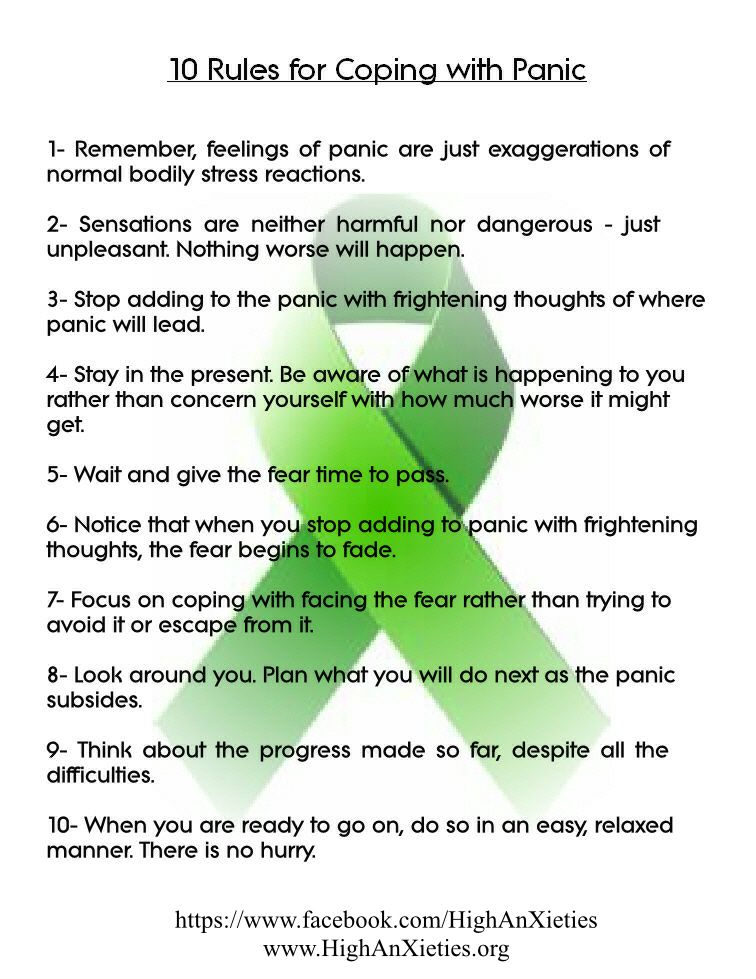
Effective treatment of PD requires (especially in cases complicated by agoraphobia) the use of psychotherapeutic techniques. The latter usually begin to be used at the stage of stabilizing (further treatment) psychopharmacotherapy and continue for some time after stopping the medication (largely facilitating the latter).
Behavioral and, more rarely, cognitive psychotherapy are most effective in PR. They allow you to reduce the level of anxiety in phobic situations and reduce the fear of waiting for an attack. nine0003
Cognitive psychotherapy is aimed at correcting fixed erroneous ideas of patients, according to which they give exaggerated reactions to non-life-threatening somatic sensations.
Systematic desensitization is the leading method of behavioral therapy (BT). immersion in a phobia situation (imaginary or real). The patient and therapist make a scale of scenes associated with the onset of symptoms, ranking them in ascending order from least to most distressing. Applying the techniques of progressive muscle relaxation, the patient learns to relax, imagining more and more painful scenes. Then the sessions are transferred from the office to a real life setting, to situations that cause anxiety. In other behavioral techniques, the patient is directly immersed in an anxiety-provoking situation: after several weeks, during which the patient is no longer disturbed by PP, the doctor encourages him to deliberately encounter phobic stimuli.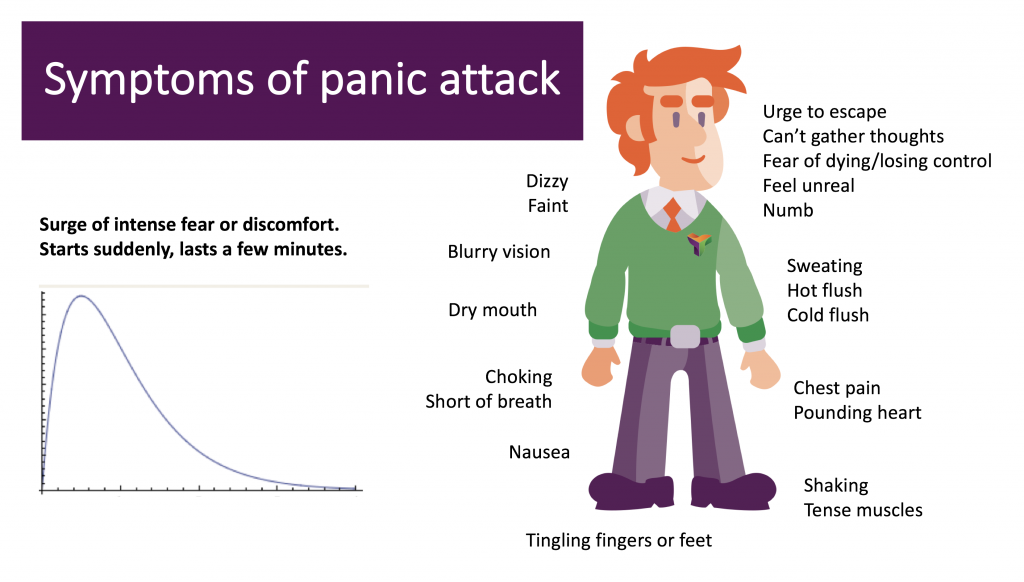 After a little training, many patients begin to feel free in previously avoided situations. A more formal PT may, however, be needed for prolonged and severe phobias. There are many techniques for their treatment, the common thing for which is a collision with a phobic stimulus in real life. Most important for therapeutic success is the duration of exposure: sessions lasting 2-3 hours are preferable to those lasting less than an hour. Another important condition is the frequent repetition of sessions, the prevention of the execution of the usual avoidance reaction for the patient and, if possible, the reproduction in sessions of circumstances close to real life. The effect of PT is significantly increased when it is carried out in groups, when patients, after training with imaginary situations, first, accompanied by a therapist, make joint trips, finding themselves in real phobogenic situations. An important modification of the method is the involvement of an instructed relative of the patient as a behavioral co-therapist.
After a little training, many patients begin to feel free in previously avoided situations. A more formal PT may, however, be needed for prolonged and severe phobias. There are many techniques for their treatment, the common thing for which is a collision with a phobic stimulus in real life. Most important for therapeutic success is the duration of exposure: sessions lasting 2-3 hours are preferable to those lasting less than an hour. Another important condition is the frequent repetition of sessions, the prevention of the execution of the usual avoidance reaction for the patient and, if possible, the reproduction in sessions of circumstances close to real life. The effect of PT is significantly increased when it is carried out in groups, when patients, after training with imaginary situations, first, accompanied by a therapist, make joint trips, finding themselves in real phobogenic situations. An important modification of the method is the involvement of an instructed relative of the patient as a behavioral co-therapist.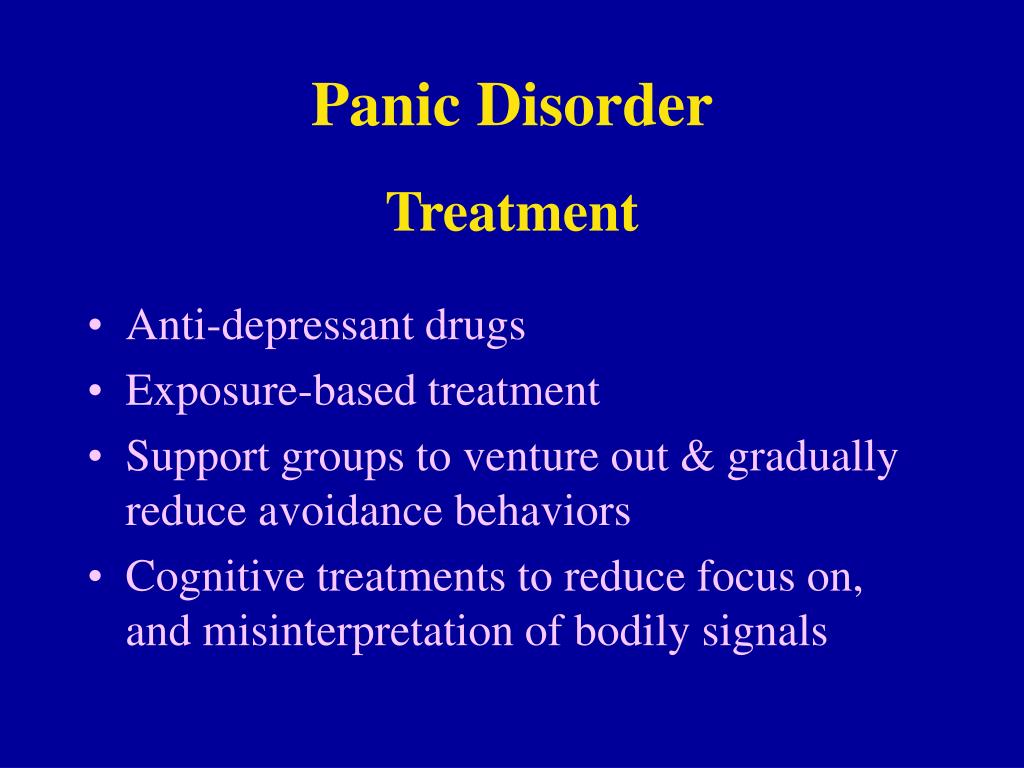 nine0003
nine0003
Underestimation of the need for APT leads to rapid recurrence of PN after discontinuation of psychopharmacotherapy and persistence of agoraphobic avoidance. On the other hand, there are patients who recover on the background of purely pharmacological treatment, and some patients, despite taking medication, remain too "scared" to even start participating in PT.
The effectiveness of other psychotherapeutic methods in PD is low and differs little from placebo (in particular, the use of psychodynamic therapy itself gives a positive effect only in 13% of cases). nine0003 90,000 anaprin during panic attacks to remove an attack
Content
- 1 Anaupoline mechanism
- 2 Method of use of anaplin with a panic attack
- 3 Contraindications for the use of anapolin
- 4 Addiction to anaprin
Anapolin very good a good drug for boring panic attack and is most commonly used by an ambulance on panic attack calls. In addition, it is inexpensive and sold without a prescription.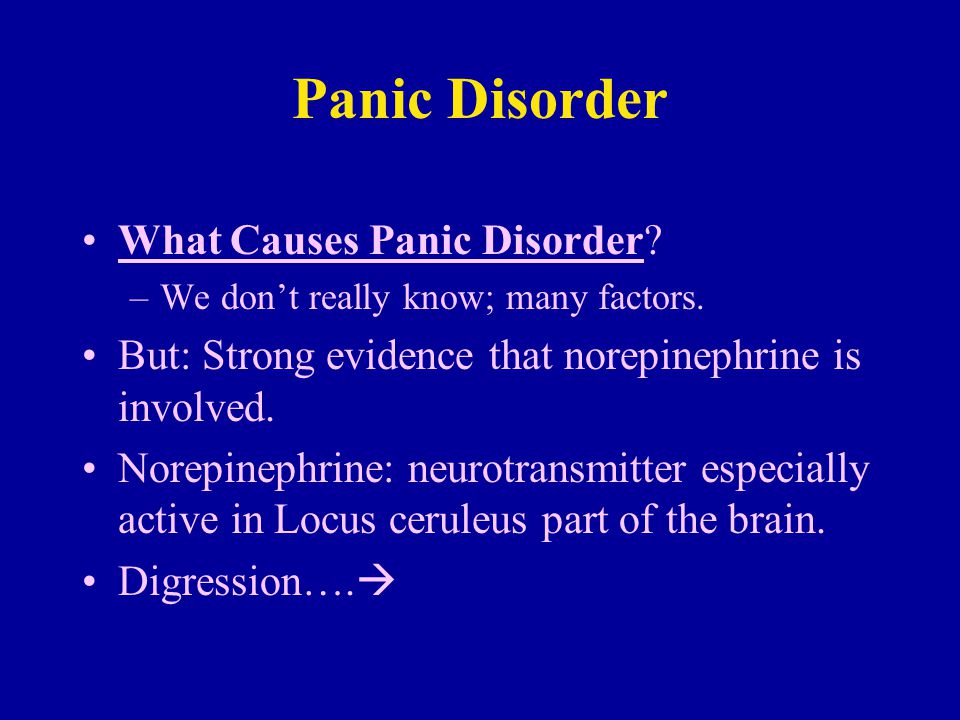 Therefore, a person suffering from panic attacks often has anaprilin in his first aid kit. nine0003
Therefore, a person suffering from panic attacks often has anaprilin in his first aid kit. nine0003
The active substance is propranolol. Analogs: Propranolol, Propamine, Stobetin and other drugs. Look carefully at the dosage of the active substance in tablets, in this article we are talking about 10 mg tablets.
The mechanism of action of anaprilin
In a panic attack, there is a sharp release of adrenaline, so the heart begins to beat rapidly, blood pressure increases, breathing quickens. Anaprilin is a beta-blocker that blocks the nerve endings that absorb adrenaline. Thus, adrenaline still continues to be released, but the nervous system does not react to it. The pulse normalizes, the pressure returns to normal, overexcitation is removed. Therefore, anaprilin quite quickly stops a panic attack. nine0003
How to use Inderal in a panic attack
Use Inderal only if you feel the onset of a panic attack. You should not drink anaprilin all the time, because it quickly develops addiction, so if there is no panic attack, then you do not need to drink anaprilin.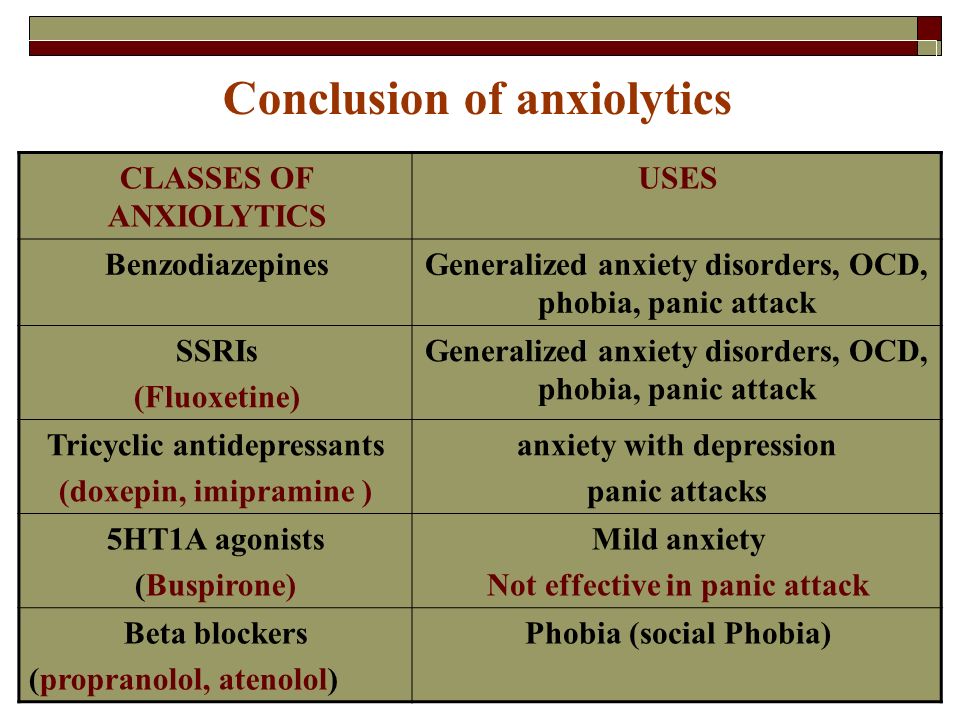
To reduce side effects on the gastrointestinal tract, it is better not to drink anaprilin tablets, but to dissolve them in the mouth under the tongue. You need to chew the tablet a little and hold it in your mouth. The drug should act within 5 minutes, then the tablet can be spit out. The action of the drug can be understood by reducing the pulse and excitement. If one tablet is not enough, take another one. With a strong attack of a panic attack, you can take two tablets of anaprilin at once (if the tablets are 10 mg each). As a rule, when anaprilin is absorbed in the mouth, numbness of the tongue appears, but after a while it passes. nine0003
If you need a longer action, for example, during a trip or flight, take 1 tablet of anaprilin inside with plenty of water. The action will begin in 15-20 minutes and last up to 5-6 hours.
Contraindications for the use of Inderal
Inderal reduces blood pressure and heart rate, so it should not be used when the pulse is below 60 beats.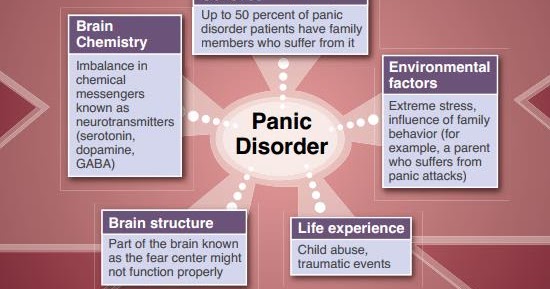 In general, if your standard pressure is low or your pulse is low, then you should be very careful about taking anaprilin. Of course, during a panic attack, there is no low pulse, but in some people, anxiety attacks are manifested in a hypotonic type, i.e. with a general decrease in body tone, with a decrease in pressure, it is better for such people to refrain from taking anaprilin. nine0003
In general, if your standard pressure is low or your pulse is low, then you should be very careful about taking anaprilin. Of course, during a panic attack, there is no low pulse, but in some people, anxiety attacks are manifested in a hypotonic type, i.e. with a general decrease in body tone, with a decrease in pressure, it is better for such people to refrain from taking anaprilin. nine0003
Also contraindicated are heart failure and bronchial problems such as bronchitis or bronchial asthma. With caution in diabetes, because. anaprilin lowers blood sugar. Often, when taking anaprilin, the concentration decreases and the reaction slows down, which must be taken into account when driving a car.
Anaprilin addiction
Anaprilin interferes with the body's hormonal system, and such interference almost always causes rapid addiction. The body tries to increase the production of adrenaline so that it finally works, and the number of adrenoreceptors also increases. Therefore, with a long-term course of taking anaprilin, there is a need to increase the dosage of the drug in order to achieve a positive effect.