Pre period depression
Premenstrual dysphoric disorder: MedlinePlus Medical Encyclopedia
Premenstrual dysphoric disorder (PMDD) is a condition in which a woman has severe depression symptoms, irritability, and tension before menstruation. The symptoms of PMDD are more severe than those seen with premenstrual syndrome (PMS).
PMS refers to a wide range of physical or emotional symptoms that most often occur about 5 to 11 days before a woman starts her monthly menstrual cycle. In most cases, the symptoms stop when, or shortly after, her period begins.
The causes of PMS and PMDD have not been found.
Hormone changes that occur during a woman's menstrual cycle may play a role.
PMDD affects a small number of women during the years when they are having menstrual periods.
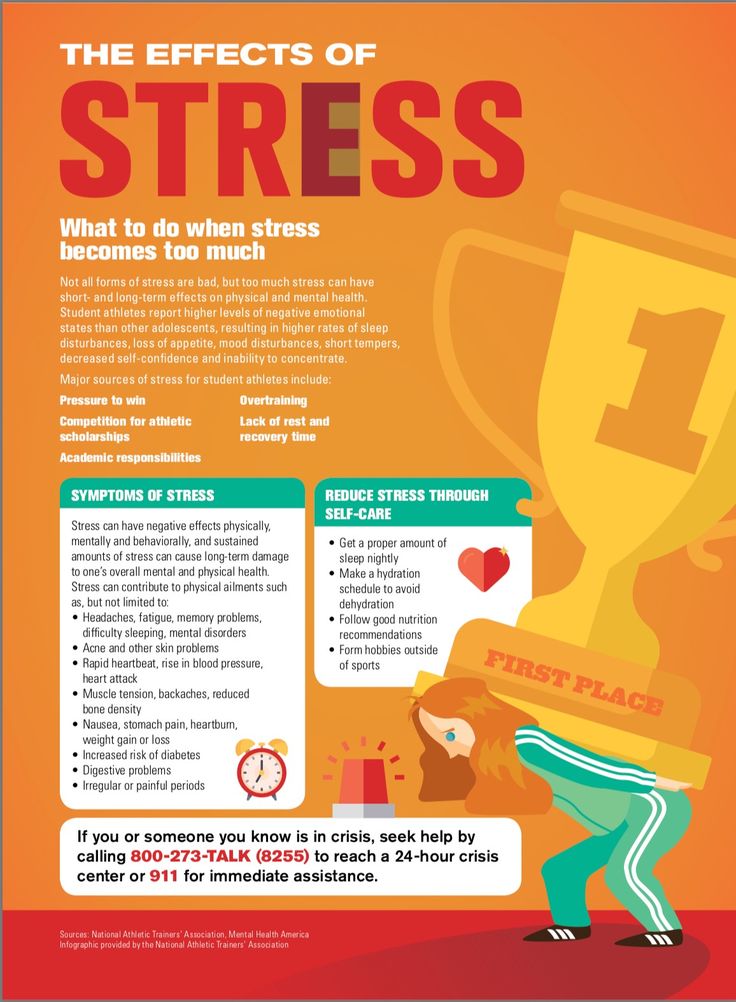
Many women with this condition have:
- Anxiety
- Severe depression
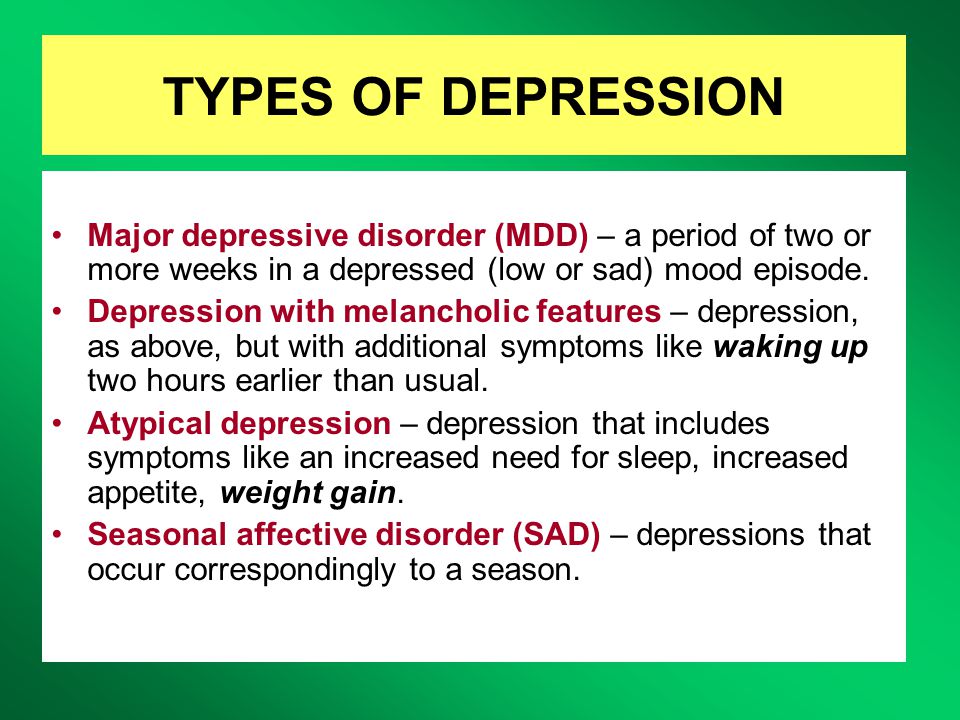
- Seasonal affective disorder (SAD)
Other factors that may play a role include:
- Alcohol or substance abuse
- Thyroid disorders
- Being overweight
- Having a mother with a history of the disorder
- Lack of exercise
The symptoms of PMDD are similar to those of PMS. However, they are very often more severe and debilitating. They also include at least one mood-related symptom. Symptoms occur during the week just before menstrual bleeding. They most often get better within a few days after the period starts.
Here is a list of common PMDD symptoms:
- Lack of interest in daily activities and relationships
- Fatigue or low energy
- Sadness or hopelessness, possibly thoughts of suicide
- Anxiety
- Out of control feeling
- Food cravings or binge eating
- Mood swings with bouts of crying
- Panic attacks
- Irritability or anger that affects other people
- Bloating, breast tenderness, headaches, and joint or muscle pain
- Problems sleeping
- Trouble concentrating
No physical exam or lab tests can diagnose PMDD. A complete history, physical exam (including a pelvic exam), thyroid testing, and psychiatric evaluation should be done to rule out other conditions.
Keeping a calendar or diary of symptoms can help women identify the most troublesome symptoms and the times when they are likely to occur. This information may help your health care provider diagnose PMDD and determine the best treatment.
This information may help your health care provider diagnose PMDD and determine the best treatment.
A healthy lifestyle is the first step to managing PMDD.
- Eat healthy foods with whole grains, vegetables, fruit, and little or no salt, sugar, alcohol, and caffeine.
- Get regular aerobic exercise throughout the month to reduce the severity of PMS symptoms.
- If you have problems sleeping, try changing your sleep habits before taking medicines for insomnia.
Keep a diary or calendar to record:
- The type of symptoms you are having
- How severe they are
- How long they last
Antidepressants may be helpful.
The first option is most often an antidepressant known as a selective serotonin-reuptake inhibitor (SSRI). You can take SSRIs in the second part of your cycle up until your period starts. You may also take it the whole month. Ask your provider.
Cognitive behavioral therapy (CBT) may be used either with or instead of antidepressants. During CBT, you have about 10 visits with a mental health professional over several weeks.
During CBT, you have about 10 visits with a mental health professional over several weeks.
Other treatments that may help include:
- Birth control pills typically help reduce PMS symptoms. Continuous dosing types are most effective, especially those that contain a hormone called drospirenone. With continuous dosing, you may not get a monthly period.
- Diuretics may be useful for women who have significant short-term weight gain from fluid retention.
- Other medicines (such as Depo-Lupron) suppress the ovaries and ovulation.
- Pain relievers such as aspirin or ibuprofen may be prescribed for headache, backache, menstrual cramps, and breast tenderness.
Most studies have shown that nutritional supplements, such as vitamin B6, calcium, and magnesium are not helpful in relieving symptoms.
After proper diagnosis and treatment, most women with PMDD find that their symptoms go away or drop to tolerable levels.
PMDD symptoms may be severe enough to interfere with a woman's daily life. Women with depression may have worse symptoms during the second half of their cycle and may need changes in their medicine.
Women with depression may have worse symptoms during the second half of their cycle and may need changes in their medicine.
Some women with PMDD have suicidal thoughts. Suicide in women with depression is more likely to occur during the second half of their menstrual cycle.
PMDD may be associated with eating disorders and smoking.
Call 911 or the local emergency number, or a local crisis line right away if you are having thoughts of suicide.
Call your provider if:
- Symptoms DO NOT improve with self-treatment
- Symptoms interfere with your daily life
PMDD; Severe PMS; Menstrual disorder - dysphoric
- Depression and the menstrual cycle
Gambone JC. Menstrual cycle-influenced disorders. In: Hacker NF, Gambone JC, Hobel CJ, eds. Hacker & Moore's Essentials of Obstetrics and Gynecology. 6th ed. Philadelphia, PA: Elsevier; 2016:chap 36.
Mendiratta V, Lentz GM. Primary and secondary dysmenorrhea, premenstrual syndrome, and premenstrual dysphoric disorder: etiology, diagnosis, management. In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 37.
In: Lobo RA, Gershenson DM, Lentz GM, Valea FA, eds. Comprehensive Gynecology. 7th ed. Philadelphia, PA: Elsevier; 2017:chap 37.
Novac A. Depressive, bipolar, and related mood disorders. In: Kellerman RD, Rakel DP, eds. Conn's Current Therapy 2021. Philadelphia, PA: Elsevier; 2021:795-806.
Updated by: LaQuita Martinez, MD, Department of Obstetrics and Gynecology, Emory Johns Creek Hospital, Alpharetta, GA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Premenstrual dysphoric disorder (PMDD) | Office on Women's Health
Premenstrual dysphoric disorder (PMDD) is a health problem that is similar to premenstrual syndrome (PMS) but is more serious. PMDD causes severe irritability, depression, or anxiety in the week or two before your period starts. Symptoms usually go away two to three days after your period starts. You may need medicine or other treatment to help with your symptoms.
What is PMDD?
PMDD is a condition similar to PMS that also happens in the week or two before your period starts as hormone levels begin to fall after ovulation. PMDD causes more severe symptoms than PMS, including severe depression, irritability, and tension.
Who gets PMDD?
PMDD affects up to 5% of women of childbearing age.1 Many women with PMDD may also have anxiety or depression.2
What are the symptoms of PMDD?
Symptoms of PMDD include:3
- Lasting irritability or anger that may affect other people
- Feelings of sadness or despair, or even thoughts of suicide
- Feelings of tension or anxiety
- Panic attacks
- Mood swings or crying often
- Lack of interest in daily activities and relationships
- Trouble thinking or focusing
- Tiredness or low energy
- Food cravings or binge eating
- Trouble sleeping
- Feeling out of control
- Physical symptoms, such as cramps, bloating, breast tenderness, headaches, and joint or muscle pain
What causes PMDD?
Researchers do not know for sure what causes PMDD or PMS. Hormonal changes throughout the menstrual cycle may play a role. A brain chemical called serotonin may also play a role in PMDD. Serotonin levels change throughout the menstrual cycle. Some women may be more sensitive to these changes.
Hormonal changes throughout the menstrual cycle may play a role. A brain chemical called serotonin may also play a role in PMDD. Serotonin levels change throughout the menstrual cycle. Some women may be more sensitive to these changes.
How is PMDD diagnosed?
Your doctor will talk to you about your health history and do a physical examination. You will need to keep a calendar or diary of your symptoms to help your doctor diagnose PMDD.
You must have five or more PMDD symptoms, including one mood-related symptom, to be diagnosed with PMDD.
How is PMDD treated?
Treatments for PMDD include:
- Antidepressants called selective serotonin reuptake inhibitors (SSRIs). SSRIs change serotonin levels in the brain. The Food and Drug Administration (FDA) approved three SSRIs to treat PMDD:4
- Sertraline
- Fluoxetine
- Paroxetine HCI
- Birth control pills. The FDA has approved a birth control pill containing drospirenone (droh-SPIR-uh-nohn) and ethinyl estradiol (ETH-uh-nil es-truh-DEYE-ohl), to treat PMDD.
- Over-the-counter pain relievers may help relieve physical symptoms, such as cramps, joint pain, headaches, backaches, and breast tenderness. These include:
- Ibuprofen
- Naproxen
- Aspirin
- Stress management, such as relaxation techniques and spending time on activities you enjoy5
Making healthy changes, such as eating a healthy combination of foods across the food groups, cutting back on salty and sugary foods, and getting more physical activity, may also help relieve some PMDD symptoms. But PMDD can be serious enough that some women should go to a doctor or nurse to discuss treatment options. And, if you are thinking of hurting yourself or others, call 911 right away.
Sources
- Potter, J., Bouyer, J., Trussell, J., Moreau, C. (2009). Premenstrual Syndrome Prevalence and Fluctuation over Time: Results from a French Population-Based Survey: Journal of Women’s Health; 18(1): 31–39.
- Pearlstein, T.
 , Steiner, M. (2008). Premenstrual dysphoric disorder: burden of illness and treatment update. Journal of Psychiatry & Neuroscience; 33(4): 291–301.
, Steiner, M. (2008). Premenstrual dysphoric disorder: burden of illness and treatment update. Journal of Psychiatry & Neuroscience; 33(4): 291–301. - American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: The American Psychiatric Association.
- The Medical Letter. (2003). Which SSRI? Med Lett Drugs Ther; 45(1170):93-5.
- Goodale, I.L., Domar, A.D., Benson, H. (1990). Alleviation of premenstrual syndrome symptoms with the relaxation response. Obstet Gynecol; 75(4):649-55.
All material contained on these pages are free of copyright restrictions and maybe copied, reproduced, or duplicated without permission of the Office on Women’s Health in the U.S. Department of Health and Human Services. Citation of the source is appreciated.
Page last updated: February 22, 2021
Premenstrual Dysphoric Disorder - Phoenix Center
What is Premenstrual Dysphoric Disorder?
Premenstrual dysphoric disorder is a hormone-based cyclical mood disorder commonly considered to be a severe form of premenstrual syndrome (PMS). While up to 85% of women experience PMS, only about 5% of women are diagnosed with premenstrual dysphoric disorder, according to psychiatric studies. Premenstrual dysphoric disorder can occur at any time during a woman's reproductive years, although the median age of onset is 26 years.
While up to 85% of women experience PMS, only about 5% of women are diagnosed with premenstrual dysphoric disorder, according to psychiatric studies. Premenstrual dysphoric disorder can occur at any time during a woman's reproductive years, although the median age of onset is 26 years.
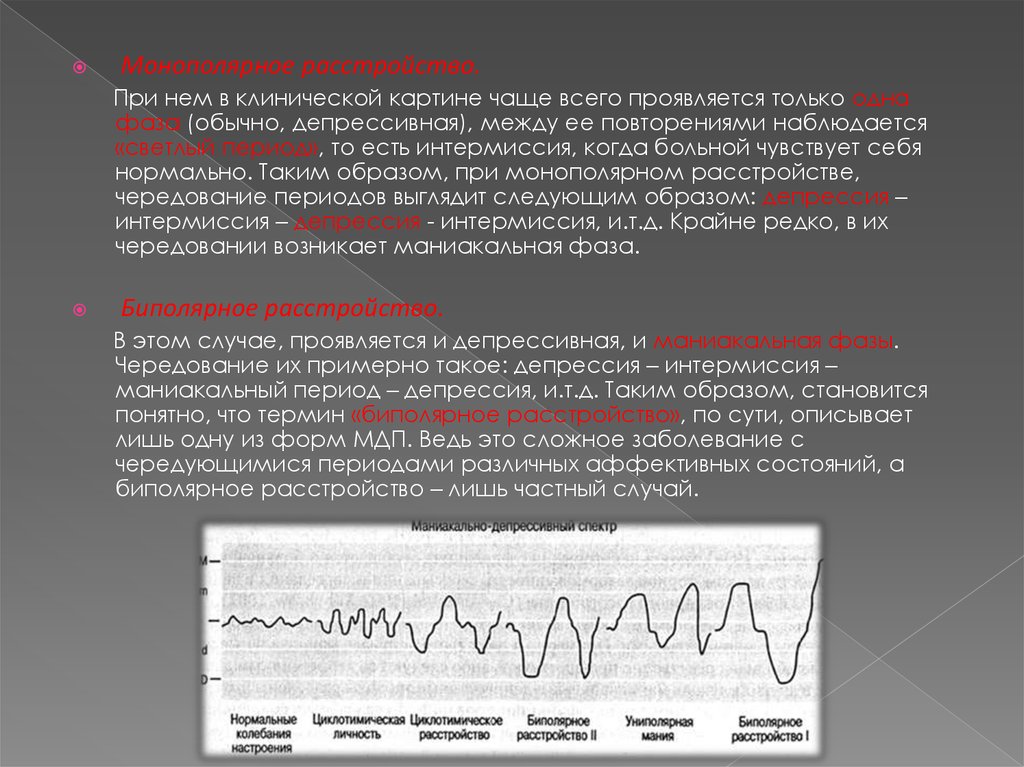
As with PMS, PMDD symptoms begin in the late luteal phase of the menstrual cycle (after ovulation) and end shortly after the onset of menstruation. Although most women experience PMS from time to time in the days leading up to their period, the symptoms do not cause any clinically significant distress or affect their ability to continue their daily activities. However, for women with PMDD, more severe PMS-related problems, especially psychological ones, interfere with daily life. Such psychological symptoms include depression and suicidal thoughts, anxiety, irritability and tension. These symptoms do not necessarily occur every cycle, but they are present in most cycles. Some months may be worse than others.
PMDD can begin any time after a woman's first menstrual period, although many people report worsening symptoms as they approach menopause. There are no symptoms after menopause and during pregnancy, although it is important to note that women with PMDD are at high risk of experiencing postpartum depression after childbirth.
Causes
Researchers are still working to determine the exact cause of PMDD, although it has been suggested that women with the disorder are more sensitive to the normal fluctuations in estrogen and progesterone that cause premenstrual symptoms.
Risk factors:
- Environment: Stress, history of interpersonal trauma, and seasonal changes are all environmental factors that may be associated with the presence of premenstrual dysphoric disorder.
- Genetic: Although the heritability of premenstrual dysphoric disorder is unknown, it is believed that premenstrual symptoms are typically 50% heritable.
- Menstrual cycle modifiers: Women who use oral contraceptives may have fewer premenstrual complaints than women who do not use oral contraceptives.
Symptoms
To be diagnosed with PMDD, a woman must have experienced symptoms for most of the previous year's menstrual cycles, and these symptoms must have had an adverse effect on work or social functioning.
While the main symptoms are related to mood and anxiety, behavioral and physical symptoms usually also occur.
In most cases, at least five of the following symptoms should be present in the week before menstruation, begin to improve within a few days of onset, and become minimal the next week:
- Mood swings
- Irritability, anger or increased interpersonal conflicts
- Depressed mood, feelings of hopelessness or self-deprecating thoughts
- Anxiety, tension and/or feeling on edge
- Decreased interest in normal activities
- Difficulty concentrating
- Severe lack of energy
- Changes in appetite
- Hypersomnia or insomnia
- Feeling overwhelmed or out of control
- Physical symptoms such as sore or swollen breasts, joint or muscle pain, a feeling of bloating or weight gain.
Diagnosis
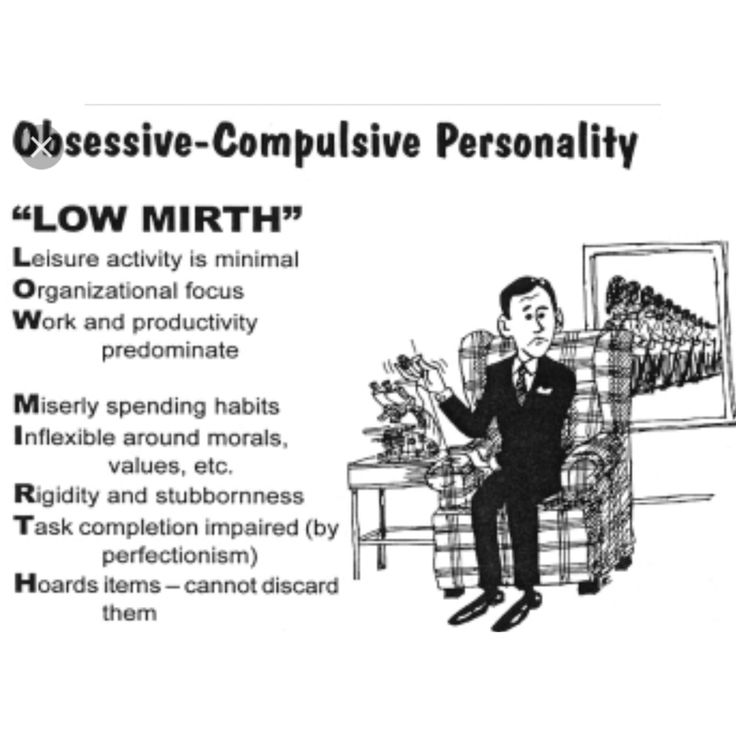
The clinician must determine that the patient's symptoms are not simply an exacerbation of another disorder, such as depression or panic disorder, and cannot be attributed to the effects of substance abuse.
What is the difference between PMS and PMDD?
PMS is less severe than PMDD because it usually does not interfere with daily functioning and the symptoms are less severe. A diagnosis of PMDD requires the presence of at least five symptoms.
Furthermore, although women may experience some mood swings in the days leading up to their period, psychological symptoms of PMDD such as severe depression, anxiety, and suicidal thoughts are not associated with PMS.
Comorbidity
Although a woman will not be diagnosed with PMDD if she experiences worsening symptoms of another psychiatric disorder only during menstruation, PMDD may be considered in addition to a diagnosis of another psychiatric disorder if the person has symptoms that are markedly different from those seen that are observed as part of an ongoing disorder.
Treatment
Women with PMDD may be prescribed a group of antidepressants called selective serotonin reuptake inhibitors (SSRIs). Doctor-approved sertraline, fluoxetine, or paroxetine hydrochloride may be prescribed to relieve symptoms.
In addition, over-the-counter pain relievers can help with breast tenderness, muscle aches and pains, cramps, and headaches. Your doctor may suggest that you try ibuprofen, naproxen, or aspirin to relieve these physical symptoms.
Psychotherapy
Living with severe depression and anxiety doesn't have to be something you have to deal with alone. Cognitive behavioral therapy (CBT) is a structured, action-oriented type of psychological treatment that focuses on the interaction between thoughts, feelings, and behaviors. CBT has been proven to be an effective treatment for mood and anxiety disorders, and to help people better manage physical symptoms such as pain.
Surgery
When medical treatment fails, surgical removal of the ovaries, known as oophorectomy, may be considered.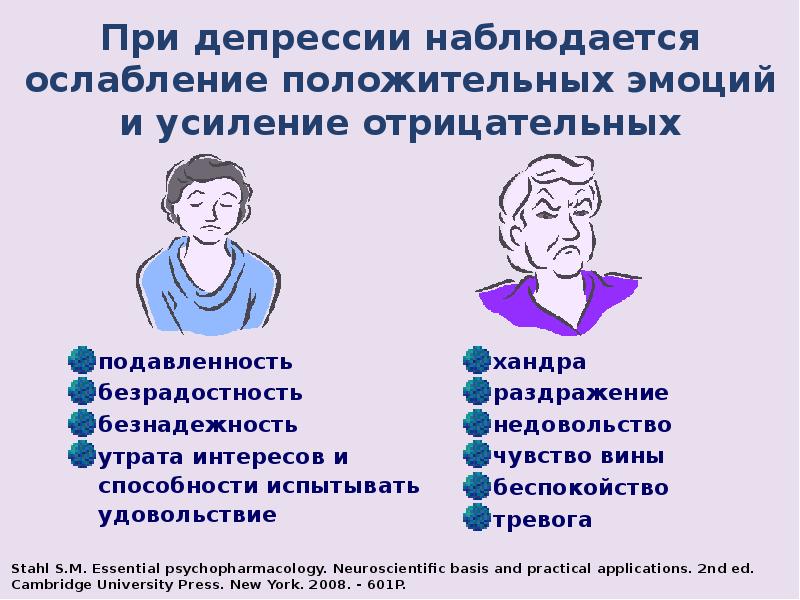 While spaying has been shown to relieve symptoms of PMDD, it also causes women to stop ovulating and enter menopause, which is also associated with various symptoms. Opting for surgery to remove the ovaries is a difficult and serious decision that will likely be the last resort for treating PMDD.
While spaying has been shown to relieve symptoms of PMDD, it also causes women to stop ovulating and enter menopause, which is also associated with various symptoms. Opting for surgery to remove the ovaries is a difficult and serious decision that will likely be the last resort for treating PMDD.
Alternative treatments
If medication or surgery is not an effective treatment, you can try natural remedies to relieve symptoms. Research shows that meditation can reduce anxiety, depression, and pain, all common symptoms of PMDD. To relieve menstrual cramps, take a warm bath and use only proven products that do not cause discomfort.
Premenstrual syndrome. What is Premenstrual Syndrome?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Premenstrual syndrome is a cyclically recurring symptom complex observed in the second half of the menstrual cycle (3-12 days before menstruation). It has an individual course, may be characterized by headache, severe irritability or depression, tearfulness, nausea, vomiting, skin itching, swelling, pain in the abdomen and in the heart, palpitations, etc. Edema, skin rashes, flatulence, painful engorgement of the mammary glands. In severe cases, neurosis may develop.
- Causes of premenstrual syndrome
- Symptoms of premenstrual syndrome
- Diagnosis of premenstrual syndrome
- Treatment of premenstrual syndrome
- Prices for treatment
General
Premenstrual syndrome, or PMS, are called vegetative-vascular, neuropsychic and metabolic-endocrine disorders that occur during the menstrual cycle (more often in the second phase). Synonyms for this condition, found in the literature, are the concepts of "premenstrual illness", "premenstrual tension syndrome", "cyclic illness". Every second woman over the age of 30 is familiar with premenstrual syndrome firsthand, in women under 30 this condition is somewhat less common - in 20% of cases. In addition, manifestations of premenstrual syndrome are usually companions of emotionally unstable, thin, asthenic body types of women, who are more often involved in the intellectual field of activity.
Every second woman over the age of 30 is familiar with premenstrual syndrome firsthand, in women under 30 this condition is somewhat less common - in 20% of cases. In addition, manifestations of premenstrual syndrome are usually companions of emotionally unstable, thin, asthenic body types of women, who are more often involved in the intellectual field of activity.
Premenstrual syndrome
Causes of premenstrual syndrome
Until now, gynecology as a science cannot unambiguously say what factors and causes underlie the development of premenstrual syndrome. It is believed that previous stresses, neuroinfections, surgical termination of pregnancy (abortion), injuries and operations, as well as various gynecological and general somatic diseases that create a background for the manifestations of premenstrual syndrome, contribute to the onset and more severe course of PMS.
The most common is the opinion that the causes that determine the development of premenstrual syndrome are hormonal fluctuations that occur in the female body during the menstrual cycle. These observations underlie the hormonal theories of the origin of premenstrual syndrome.
These observations underlie the hormonal theories of the origin of premenstrual syndrome.
One of the theories considers as a fundamental cause of premenstrual syndrome - a change in the ratio of the hormones progesterone and estrogen in the second half of the menstrual cycle. Excess estrogen production leads to fluid retention in tissues, edema, swelling of the mammary glands, and cardiovascular disorders. The effect of estrogens on brain structures causes neuro-emotional disorders - depression or aggression, irritability, tearfulness, etc. Another hormonal theory links premenstrual syndrome with hypersecretion of the hormone prolactin, which causes water and sodium retention, changes in the mammary glands.
In the development of premenstrual syndrome, a certain role of prostaglandins, hormone-like substances produced in body tissues and involved in the regulation of many physiological processes, has also been proven. An excess of prostaglandins causes migraine-like headaches, digestive disorders, and vegetative-vascular reactions.
Other numerous theories consider water-salt metabolism disorders (water intoxication theory), deficiency of vitamins (vitamin A, B6) and trace elements (calcium, magnesium, zinc), genetic factor, hypothalamic disorders as the causes of premenstrual syndrome. A number of researchers believe that premenstrual syndrome is caused by a whole range of reasons that are individual in each clinical case. Therefore, the diagnosis of premenstrual syndrome has its own specifics and certain difficulties.
Symptoms of premenstrual syndrome
Based on the leading symptoms that accompany premenstrual syndrome, the following forms of disorders are distinguished: neuropsychic, cephalgic, edematous, crisis, atypical. Often, these forms of premenstrual syndrome do not exist in isolation, so treatment for PMS is usually symptomatic.
The neuropsychic form of premenstrual syndrome is characterized by disturbances in the emotional and nervous spheres: insomnia, weakness, mood instability, irritability, tearfulness, aggression, fatigue, unreasonable longing, depression (up to suicidal thoughts), an unreasonable sense of fear, sexual disturbances, auditory and olfactory disorders , dizziness. Against the background of neuropsychiatric disorders, there are also disturbances in appetite, flatulence (bloating), soreness and engorgement of the mammary glands.
Against the background of neuropsychiatric disorders, there are also disturbances in appetite, flatulence (bloating), soreness and engorgement of the mammary glands.
In the clinical picture of the cephalgic form of premenstrual syndrome, the leading ones are vegetative-vascular and neurological symptoms: migraine-like headache attacks, diarrhea, palpitations, pain in the heart area, hypersensitivity to smells and sounds, nervousness, insomnia. Characteristic is a headache, throbbing in the temples, accompanied by swelling of the eyelids, nausea and vomiting. The cephalgic form of premenstrual syndrome often develops in women with a burdened history who have suffered traumatic brain injuries, neuroinfections, and severe stress. Of the comorbidities, these women usually suffer from cardiovascular pathology, hypertension, and gastrointestinal diseases.
With the edematous form of premenstrual syndrome, interstitial fluid retention and associated swelling of the face and extremities, weight gain, thirst, and reduced urination become the leading manifestation. In addition, there are engorgement of the mammary glands, itching of the skin, indigestion (flatulence, constipation, diarrhea), headaches and joint pain, etc.
In addition, there are engorgement of the mammary glands, itching of the skin, indigestion (flatulence, constipation, diarrhea), headaches and joint pain, etc.
The course of the crisis form of premenstrual syndrome is manifested by sympathetic-adrenal crises, characterized by attacks of rising blood pressure, tachycardia, heart pain without ECG deviations, panic fear. The end of the crisis, as a rule, accompanies profuse urination. Often attacks are provoked by stress and overwork. The crisis form of premenstrual syndrome can develop from untreated cephalgic, neuropsychic or edematous forms and usually manifests itself after 40 years. The background for the course of the crisis form of premenstrual syndrome are diseases of the heart, blood vessels, kidneys, digestive tract.
Cyclic manifestations of atypical forms of premenstrual syndrome include: an increase in body temperature (in the second phase of the cycle up to 37.5 ° C), hypersomnia (drowsiness), ophthalmoplegic migraine (headaches with oculomotor disorders), allergic reactions (ulcerative stomatitis and ulcerative gingivitis, asthmatic syndrome, indomitable vomiting, iridocyclitis, Quincke's edema, etc. ).
).
When determining the severity of the course of premenstrual syndrome, they proceed from the number of symptomatic manifestations, highlighting the mild and severe forms of premenstrual syndrome. A mild form of premenstrual syndrome is manifested by 3-4 characteristic symptoms that appear 2-10 days before the onset of menstruation, or by the presence of 1-2 significantly pronounced symptoms. In a severe form of premenstrual syndrome, the number of symptoms increases to 5-12, they appear 3-14 days before the onset of menstruation. At the same time, all or several of the symptoms are pronounced significantly.
In addition, an indicator of a severe form of the course of premenstrual syndrome is always a disability, regardless of the severity and number of other manifestations. A decrease in working capacity is usually noted in the neuropsychic form of premenstrual syndrome.
It is customary to distinguish three stages in the development of premenstrual syndrome:
Diagnosis of premenstrual syndrome
The main diagnostic criterion for premenstrual syndrome is the cyclicity, the periodic nature of complaints arising on the eve of menstruation and their disappearance after menstruation.
The diagnosis of "premenstrual syndrome" can be made on the basis of the following signs:
- A state of aggression or depression.
- Emotional imbalance: mood swings, tearfulness, irritability, conflict.
- Bad mood, feeling of melancholy and hopelessness.
- State of anxiety and fear.
- Decreased emotional tone and interest in current events.
- Increased fatigue and weakness.
- Decreased attention, memory impairment.
- Change in appetite and taste preferences, signs of bulimia, weight gain.
- Insomnia or drowsiness.
- Painful tension of the mammary glands, swelling
- Head, muscle or joint pain.
- Deterioration of the course of chronic extragenital pathology.
The manifestation of five of the above signs with the obligatory presence of at least one of the first four allows us to speak with confidence about premenstrual syndrome. An important link in the diagnosis is the patient's keeping a diary of self-observation, in which she must note all violations in her state of health for 2-3 cycles.
A study in the blood of hormones (estradiol, progesterone and prolactin) allows you to establish the form of premenstrual syndrome. It is known that the edematous form is accompanied by a decrease in the level of progesterone in the second half of the menstrual cycle. Cephalgic, neuropsychic and crisis forms of premenstrual syndrome are characterized by an increase in the level of prolactin in the blood. The appointment of additional diagnostic methods is dictated by the form of premenstrual syndrome and leading complaints.
A pronounced manifestation of cerebral symptoms (headaches, fainting, dizziness) is an indication for an MRI or CT scan of the brain to exclude its focal lesions. Indicative for neuropsychic, edematous, cephalgic and crisis forms of the premenstrual cycle are the results of the EEG. In the diagnosis of the edematous form of premenstrual syndrome, the measurement of daily diuresis, accounting for the amount of fluid drunk, and conducting tests to study the excretory function of the kidneys (for example, Zimnitsky's test, Reberg's test) play an important role. With painful engorgement of the mammary glands, an ultrasound of the mammary glands or mammography is necessary to exclude organic pathology.
Indicative for neuropsychic, edematous, cephalgic and crisis forms of the premenstrual cycle are the results of the EEG. In the diagnosis of the edematous form of premenstrual syndrome, the measurement of daily diuresis, accounting for the amount of fluid drunk, and conducting tests to study the excretory function of the kidneys (for example, Zimnitsky's test, Reberg's test) play an important role. With painful engorgement of the mammary glands, an ultrasound of the mammary glands or mammography is necessary to exclude organic pathology.
An examination of women suffering from one form or another of premenstrual syndrome is carried out with the participation of doctors of various specialties: a neurologist, therapist, cardiologist, endocrinologist, psychiatrist, etc. Assigned symptomatic treatment, as a rule, leads to an improvement in well-being in the second half of the menstrual cycle.
Treatment of premenstrual syndrome
In the treatment of premenstrual syndrome, drug and non-drug methods are used.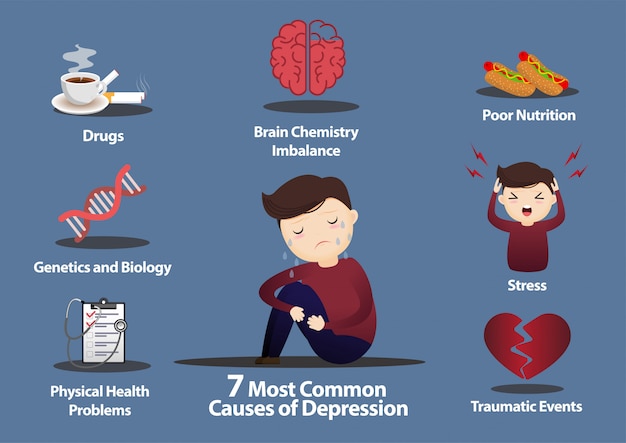 Non-drug therapy includes psychotherapeutic treatment, compliance with the regime of work and good rest, physiotherapy exercises, physiotherapy. An important point is the observance of a balanced diet with the use of a sufficient amount of vegetable and animal protein, vegetable fiber, vitamins. In the second half of the menstrual cycle, you should limit the intake of carbohydrates, animal fats, sugar, salt, caffeine, chocolate, and alcoholic beverages.
Non-drug therapy includes psychotherapeutic treatment, compliance with the regime of work and good rest, physiotherapy exercises, physiotherapy. An important point is the observance of a balanced diet with the use of a sufficient amount of vegetable and animal protein, vegetable fiber, vitamins. In the second half of the menstrual cycle, you should limit the intake of carbohydrates, animal fats, sugar, salt, caffeine, chocolate, and alcoholic beverages.
Drug treatment is prescribed by a specialist doctor, taking into account the leading manifestations of premenstrual syndrome. Since neuropsychic manifestations are expressed in all forms of premenstrual syndrome, almost all patients are shown taking sedative (sedative) drugs a few days before the expected onset of symptoms. Symptomatic treatment of premenstrual syndrome involves the use of painkillers, diuretics, antiallergic drugs.
The leading place in the medical treatment of premenstrual syndrome is occupied by specific hormonal therapy with progesterone analogues.