Pathological self soothing
Pathological Self-Soothing - When Self-Soothing Stops Serving Us — Counselling South Dublin [SouthSide] Help for Your Mental Health and Wellness
Are you overdoing the self-soothing?The need to soothe distress is paramount in human experience. When we are overwhelmed with uncomfortable feelings brought about through various life stressors, we often turn to different things, substances, experiences or people for comfort.
Some forms of self-soothing help to regulate our emotions, restoring our sense of calm and equilibrium in a healthy way. However, other forms of self-soothing behaviours are maladaptive and detrimental to our health in the long run and could propel us on to the slippery and painful downward slope towards addiction.
When a situation or problem arises which lies beyond our ability to cope with it, we sometimes ‘cope’ by diving headlong into a packet of chocolate biscuits and clearing the lot; zoning out into a zombie fog aimlessly cruising internet shopping sites, engaging in high octane risky behaviours such as extreme sports, dangerous sexual encounters, placing reckless sporting bets. We seek and extract temporary highs available from recreational drugs (and sometimes prescribed drugs).
This is a game of snakes and ladders and as you experience the temporary buzz of scaling the ladder, the snake is always waiting for you and he appears to be getting longer and longer than the ladder you temporarily climbed—you might even slide off the board entirely as life becomes much too hard.
The urge to escape discontentment with our present state
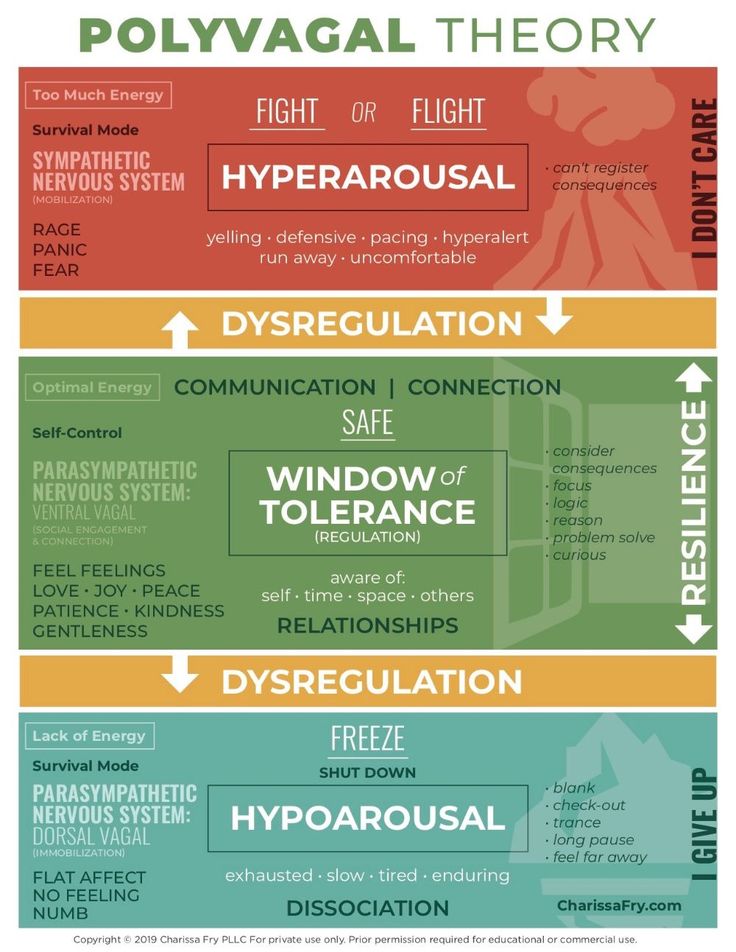
Pathological self-soothing behaviours generally have an escapist quality to them. When our discomfort becomes too much for us to handle, we can ‘escape’ or ‘flee’ from the discomfort through overindulging in food (comfort eating), alcohol and drugs (self-medication), gambling, shopping, sex addiction (acting out).
Often, these escapist behaviours are unconscious to us or barely conscious to us; it is only when we develop a more honest and deeper relationship with ourselves that we begin to recognise a destructive pattern.
Sometimes the maladaptive nature of our self-soothing behaviours are so outside our awareness that it is other people such as our loved ones who attempt to bring these problematic behaviours to our attention.
As the ‘fleeing’ nature of the self soothing behaviour is an avoidance strategy, the underlying issues do not get addressed.
Once self-soothing through ‘acting out’ or ‘self-medicating’ runs its course, we are back with a bang at the exact place where we began with the same painful feelings, but these feelings are becoming increasingly worse over time with each acting out or self-medicating cycle.
A part of consciousness can emerge within us that knows at some level that what we are doing is self-sabotaging. This conscious part can compound the pain inside our internal world by heaping more guilt and shame upon us as we see ourselves failing to address—or even discover—the underlying issues.
Something is gnawing …
When we can no longer run away from ourselves
As the amount and intensity of our maladaptive self-soothing behaviours increase over time, they begin to take a toll on our physiology, our emotions and our relationships. This is the time to reach out and seek help.
This is the time to reach out and seek help.
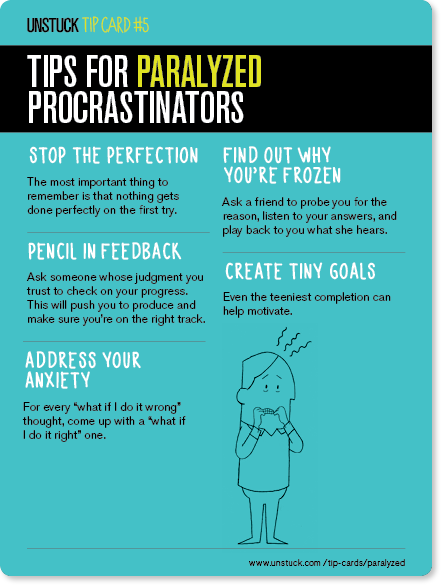
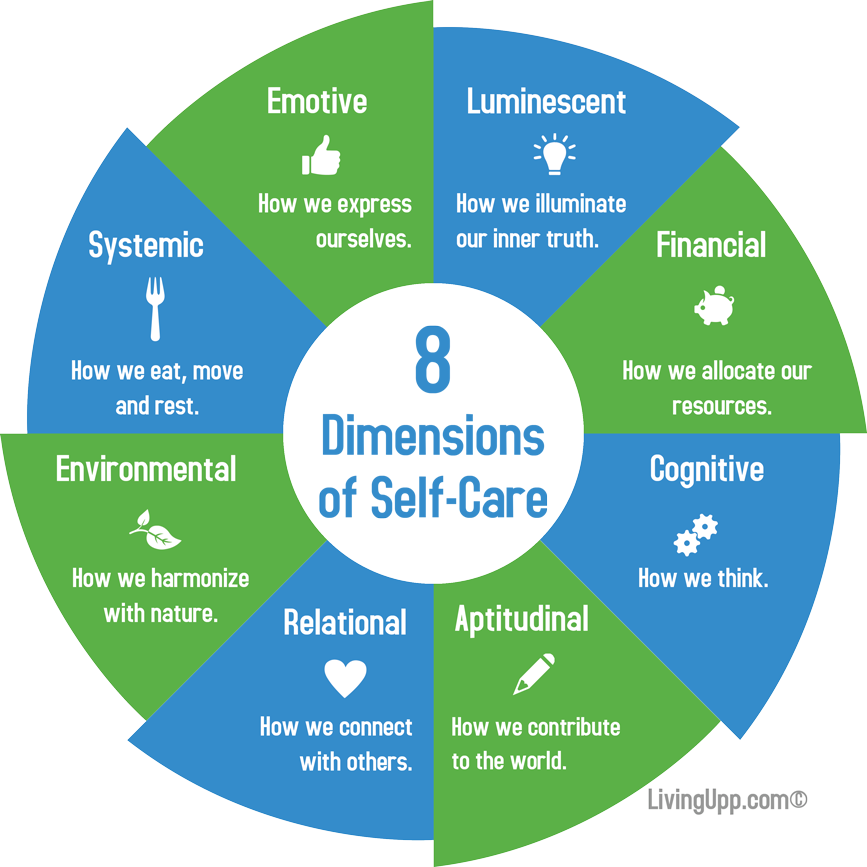
Healthy self soothing is the exact opposite of ‘fleeing’. It is a loving embrace of ‘self’ and a respectful empathy for our own vulnerabilities.
Of course, when we don't like ourselves it is very difficult to do this. Why have we come to dislike and disrespect ourselves? Many psychological theories exist which attempt to answer this question.
Part of self-development involves discovering what makes sense for us and what holds ‘meaning’ and ‘value’ for us. These are the deeper self-reflective questions, which cycles of maladaptive self-soothing keep us away from asking and exploring.
“Unhealthy self-soothing has an acting outwards energy and direction away from ‘self’. Healthy self-soothing has an exploration inwards direction towards ‘self’”
Some seemingly healthy behaviours such as attending meditation and yoga classes, gym workouts, spiritual practices can become maladaptive when we overdo them and they contribute to a decline in our relational qualities. We might find ourselves feeling superior to those who don't engage is such practices. Yoga, meditation and spirituality can become dogma.
We might find ourselves feeling superior to those who don't engage is such practices. Yoga, meditation and spirituality can become dogma.
Some spiritual seeking practices may represent a fleeing from one’s ‘self’ as a way to avoid the psychological discomfort with one’s ‘self’.
Sometimes we may experience an aura of anger from spiritual people. I know from my own experience growing up in a Catholic family, I experienced a pressure to move quickly towards forgiveness if I felt someone had wronged me. My anger towards the person was not processed and I was compelled into a rigid forgiveness space which really was not forgiveness at all—I was encouraged to ‘turn the other cheek’ when I was not ready to turn the other cheek. Taking a ‘spiritual’ position can be an unconscious way to avoid a healthy processing of anger.
Of course this also depends on how we define spiritualism. Is spiritualism a journey towards ‘self’, in the manner of unearthing our true or real ‘self’ by discovering a divine spiritual kernel within us, or is it a movement away from ‘self’—transcending our ‘self’ where we may see our ordinary or real ‘self’ as flawed, tainted and representative of original sin and egocentricity.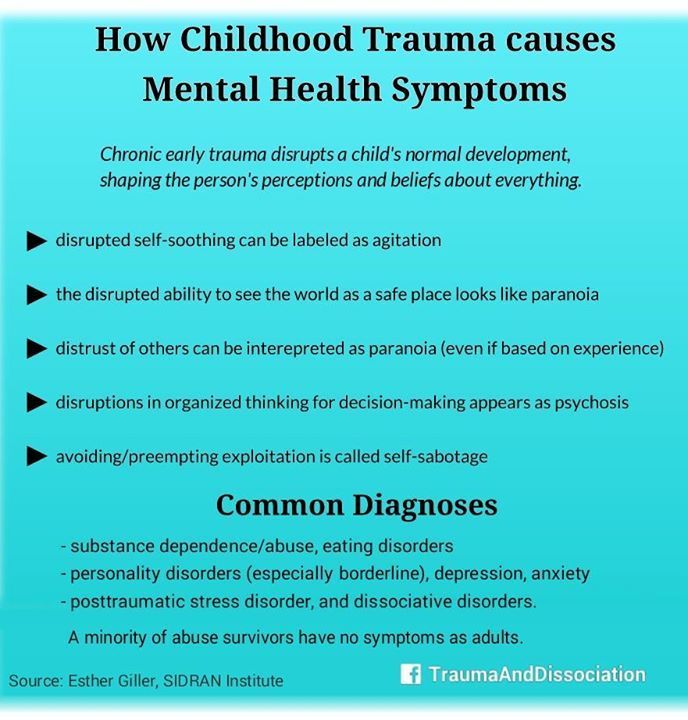
All this falls into the realm of meaning and values, prisms through which we ultimately judge our own attempts at self soothing and self development.
This is not to say spiritualism, yoga and meditation do not hold incredible soothing and healing value for us. They do. We just need to be mindful of not taking things to extremes.
Dialoguing with ‘self’
That is why an intervention such as counselling or psychotherapy can help to open up this internal dialogue and change the fundamental relationship with ourselves. We can develop our meta-observer or ‘beholding eye’ by exercising our self-awareness muscles.
In psychotherapy, we get to ‘process’ our painful feelings (rather than flee from them), extrapolate vital messages from them, come to make sense of them and ultimately heal them.
People usually get to this point when they realise running away from painful feelings no longer works for them.
Check out 5 Helpful Self Soothing Techniques
Also, if one of the intense feelings you are trying to soothe is anger, check out 11 self-exploration questions about your anger.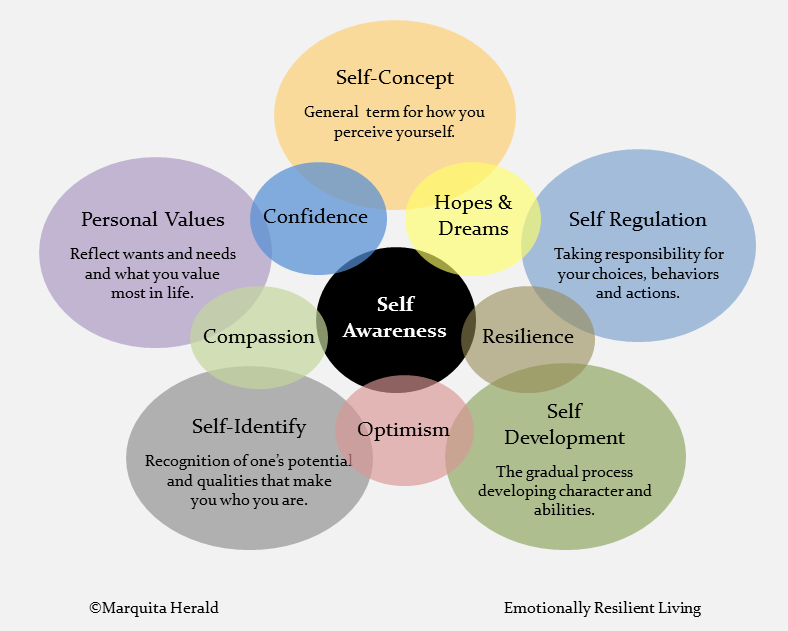
Self-Soothing in Children and Adolescents.
Self-Soothing in Children and Adolescents. Is it More Than Just “a Habit” or “Unwanted Behaviour”?
by Kaelan Jones, Provisional Psychologist - BPsych (Hons) MProfPsyc
January 2020
“Self-soothing” refers to any behaviour an individual uses to regulate their emotional state by themselves. Self-soothing behaviours are often developed in the early years of life, are repetitive/habitual in nature, and are often viewed by a child or adolescent as calming or comforting. Self-soothing behaviours are identifiable across the lifespan. It is not uncommon for adults to continue to engage in the self-soothing behaviours they developed during childhood, however, many of these behaviours do diminish with time and self-awareness. Although self-soothing is a life skill that can be very important for emotional wellbeing, some self-soothing behaviours that a child or adolescent might be engaging in may be considered socially inappropriate for their age or self-injurious
- Thumb-sucking
- Fingernail biting
- Cuticle picking
- Sucking on clothing or other objects
- Rocking
- Knuckle cracking
- Pulling hair, eyebrows, or eyelashes
- Hair twirling
- Picking nose or skin
- Head banging
- Biting the ends of pencils or other objects
- Masturbation
- Alcohol/drug experimentation
- Self-harm (e.
 g. cutting):
g. cutting):
Common reasons for why a child or adolescent might be engaging in self-soothing behaviours
- Trouble coping with or understanding their emotions
- Stress, which can be brought on by change (e.g. parental separation, school transition) or challenges (e.g. peer conflict, study/exams)
- Current or previous exposure to trauma
- Attachment issues – children with inconsistent care during their early years of life (e.g. the first three years) learn to rely on themselves for care
- Sensory seeking
- Tic Disorder – Tics are brief, sudden, repetitive, and stereotyped movements or sounds, and are not uncommon amongst school-aged children. On average, Tics generally become apparent at 6 to 7 years of age, peak around 10 to 12 years of age. The behaviour could be due to a Tic Disorder, and if persisting for more than 12 months, it is recommended that the behaviour be looked at by a professional.
- Try to ignore the behaviour.
 Whilst the behaviour might be irritating or considered inappropriate, generally the behaviour will disappear over time as the child gets older and comes to understand and cope with their emotions. Sometimes, when attention is given to the behaviour, particularly negative attention such as punishment or ridicule, the tension that the behaviour relieves will likely increase, and in turn increase the behaviour without conscious awareness. Therefore, paying attention to the behaviour can reinforce the behaviour.
Whilst the behaviour might be irritating or considered inappropriate, generally the behaviour will disappear over time as the child gets older and comes to understand and cope with their emotions. Sometimes, when attention is given to the behaviour, particularly negative attention such as punishment or ridicule, the tension that the behaviour relieves will likely increase, and in turn increase the behaviour without conscious awareness. Therefore, paying attention to the behaviour can reinforce the behaviour. - Observe the behaviour to better understand its purpose. For instance, when are they engaging in the self-soothing behaviour? Is the behaviour occurring when they are bored, tired, anxious, or hungry etc.? Once the triggers of the self-soothing behaviour are identified, we can try to remove or lessen the impact of the trigger.
- Approach your child with understanding and without judgement of their behaviour.
- Be physically and emotionally present with your child.
 Assist them to identify and verbalise their feelings, and together work out what they need in terms of support.
Assist them to identify and verbalise their feelings, and together work out what they need in terms of support. - Positive reinforcement is recognised as a successful way to produce a change in or prevent a behaviour. When you notice that your child is not engaging in the behaviour for extended periods of time, a small reward can be given. You can also reward the new behaviour that you want to see adopted by your child. For younger children, star charts can be helpful. For older children, daily monitoring of behaviours with a behavioural diary can be helpful.
- Role model effective, appropriate, and non-injurious self-soothing behaviours for your child or adolescent. How you cope with stressors will influence how your child learns to cope with stressors. When you feel overwhelmed you can say something like “I have so much to get done today that I don’t know how I am going to do it all! I think I am going to need a minute to do my deep breathing, and then I will feel better.
 ” This will demonstrate to your child that you have acknowledged your stress by putting it into words and have responded to it in an effective way.
” This will demonstrate to your child that you have acknowledged your stress by putting it into words and have responded to it in an effective way. - Redirect your child to a more appropriate behaviour each time they engage in the inappropriate one. For example, if they are nose picking, redirect them towards playing with a fidget object, or if they are self-harming redirect them to flicking an elastic band against their wrist.
- Encourage your child to engage in activities that allow for sensory stimulation and the release of any tension or nervous energy (e.g. team sports, jumping, running, boxing)
If the current self-soothing behaviour that the child or adolescent is engaging in is causing serious injury (e.g. cutting wrists, head banging), is socially inappropriate for the context (e.g. masturbation, picking nose), or is detrimental to their physical and/or mental health (e.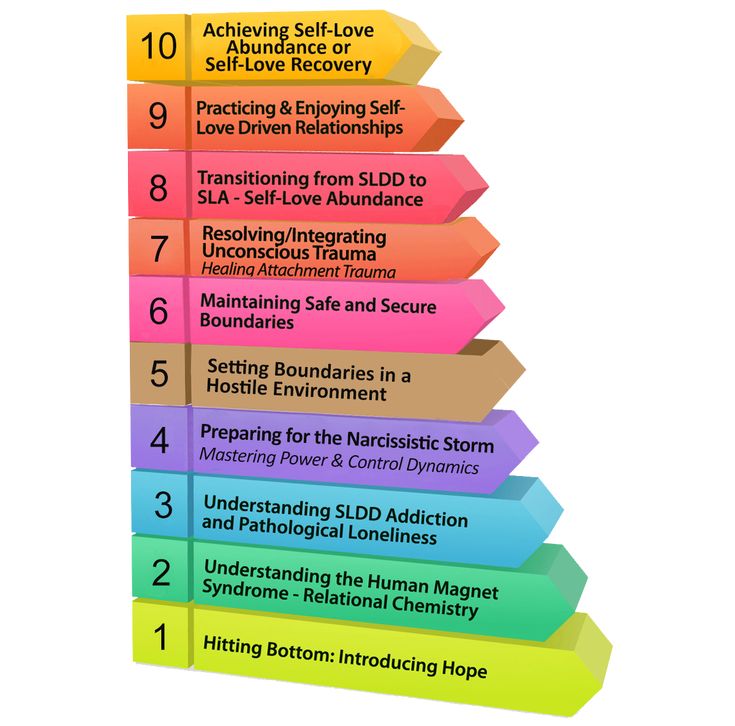 g. excessive alcohol and other drug use), then ideally we want to replace the behaviour with something that is less injurious, socially appropriate, and positive for their overall health. When the current self-soothing behaviours are causing significant harm to the child or adolescent, they should not be ignored. To introduce a replacement self-soothing behaviour, invite your child or adolescent to sit down with you to discuss your concerns about their current behaviour without judgement, punishment, or ridicule. Suggest a range of replacement behaviours to trial, and let them know that they have your support as they trial new behaviours to find something that is right for them (e.g. offering to do a daily walk with them or offering to take them out shopping to find a fidget object).
g. excessive alcohol and other drug use), then ideally we want to replace the behaviour with something that is less injurious, socially appropriate, and positive for their overall health. When the current self-soothing behaviours are causing significant harm to the child or adolescent, they should not be ignored. To introduce a replacement self-soothing behaviour, invite your child or adolescent to sit down with you to discuss your concerns about their current behaviour without judgement, punishment, or ridicule. Suggest a range of replacement behaviours to trial, and let them know that they have your support as they trial new behaviours to find something that is right for them (e.g. offering to do a daily walk with them or offering to take them out shopping to find a fidget object).
- Squeezing a stress ball
- Cuddling a soft toy
- Playing with a pet
- Fidget objects – e.
 g. rings, bracelets, spinners
g. rings, bracelets, spinners - Flicking elastic band against wrist
- Listening to music
- Going for a walk
- Having a warm bubble bath
- Hitting a punching bag
- Talking about feelings
- Mindfulness/meditation – refer to the following apps and podcasts:
Headspace: https://www.headspace.com/headspace-meditation-app
Peace Out: https://bedtime.fm/peaceout
Smiling Mind: https://www.smilingmind.com.au/
Sources
https://lifelinechild.org/self-soothing/
https://blogs.psychcentral.com/childhood-neglect/2018/05/how-to-learn-the-skill-for-a-lifetime-self-soothing/
https://www.healthychildren.org/English/family-life/family-dynamics/communication-discipline/Pages/Common-Childhood-Habits.aspx
https://childrensmd.org/uncategorized/kids-tics-whats-normal-see-specialist/
Back to Resources
What is pathological demand avoidance?
05/14/19
Description of the characteristics of a possible profile for autism, which some experts propose to consider separately
Source: PDA Society
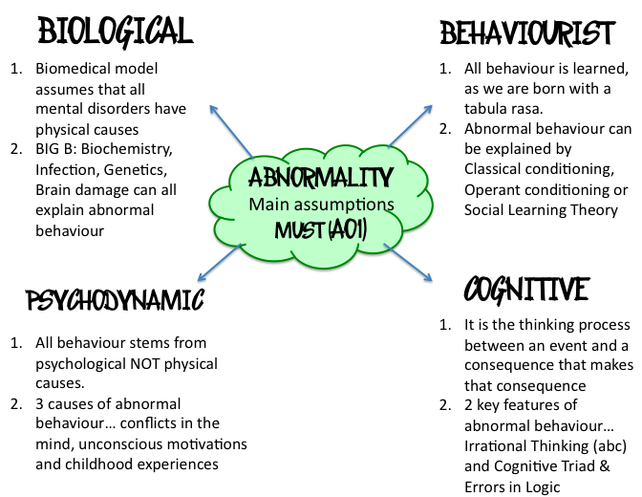
Pathological avoidance of requirements (PIT) is not a separate diagnosis, but a separate diagnosis, but specific behavioral profile that occurs in autism. People with a PIT profile have difficulties that are common to other people on the autism spectrum and fall into three areas:
- Difficulties with social communication.
- Difficulties with social interaction.
- Restricted and repetitive patterns of behavior (including sensory seeking behavior and sensory avoidance behavior).
In addition, a major difficulty for people with pathological demand avoidance is “the anxiety-induced need to control and avoid the demands and expectations of others” (Understanding PDA in Children. Christie, Duncan, Fidler & Healy, 2011). Moreover, a 2016 study from the University of Newcastle, UK, suggests that this extreme degree of anxiety in people with PIT is exacerbated by uncertainty intolerance.
At the same time, it is autism that causes the development of an extreme degree of avoidance of demands and the need for control. It is important to note that “demand avoidance” is considered a possible sign and symptom of autism according to the UK National Institute for Care and Quality guidelines. Thus, it can be said that “demand avoidance” is, in principle, a possible symptom of autism.
However, for people with a PIT profile, demand avoidance is different from what other people on the autism spectrum experience. In their case, avoidance reaches an extreme degree and has signs of obsession. This extreme degree of avoidance includes not only avoidance of unpleasant, difficult, or anxiety-producing tasks, but extends to the most basic requirements of everyday life. It is difficult for a person with PIT to follow even his own expectations, very often he avoids doing even what he really wants to do.
Autism is multidimensional, with many different traits and characteristics, and each person will have their own experience of autism. Autism affects everyone differently and to varying degrees. Some people on the autism spectrum have one or more of the traits associated with PIT. However, if all or most of the characteristics of PIT are very frequent and intense, along with other symptoms of autism, then it is important to include the profile of PIT in the overall diagnosis, or note that autism spectrum disorder in this case is characterized by "extreme demand avoidance. " This is because people with PIT need very specific support and it is important to understand their needs well.
Different terms can be used in terms of terminology - PIT, autism spectrum disorder with extreme demand avoidance, or ASD with PIT profile. Different terms may reflect both the individual characteristics of the child and the preferences of the specialist in terms of terminology. Any term is appropriate as long as it includes a detailed description of the child's individual profile and facilitates a better selection of support and assistance strategies.
PIT is a lifelong form of disability, as is the case with other autism profiles. People with PIT need different levels of support at different stages of life, depending on the extent to which the condition affects them. There is limited evidence that early diagnosis and improved care in childhood increase the likelihood that they will become more competent and independent in the future.
How do people with PIT feel?
Before we take a closer look at the characteristics and key features of the profile of PIT in ASD, it will be useful to understand how people with PIT perceive it themselves and how it affects them. The key to successfully supporting a person with PIT is acknowledging, empathizing with, and understanding the difficulties and heightened vulnerabilities that may be hidden behind what appears to be stubbornness or aggressiveness.
"It makes me feel afraid when people look at me, but I don't know why."
“I feel like there are two versions of me inside. They are constantly fighting each other. One me wants to do business, but the other me constantly stops itself. It seems to me that inside I am torn apart, as if there is a monster inside me that is killing me, and this monster is myself!”
“I feel very sad that sometimes I get so angry that I might hit someone. Everything inside me shrinks and I can't hear anything. Then I don’t even remember what I did.”
“I'm like a poorly designed robot that keeps breaking down. There have been a few moments in my life when I have sunk into dark depression, self-blame and self-hatred.”
"Even though I act like I'm angry, I'm actually terrified. "
First of all, it is important to recognize and remember that we are talking about people with “invisible disabilities”. They are simply trying to find their place in a world that causes them confusion and great fear, but, nevertheless, they strive to live in this world on an equal footing with everyone.
What are the main characteristics of pathological demand avoidance?
Resistance and avoidance of the most common demands of life. For example: get out of bed, join a family activity, put on a new piece of clothing. Avoidance can take place even when the person himself wants to do it, for example, we are talking about going to the cinema to see a new film, which the person has been looking forward to for several days. In cases where the initial avoidance strategies described below fail, a rapid escalation of behavior can occur, some individuals may resort to extreme avoidance measures - yelling, swearing, fighting, destroying things. Other people with PIT may withdraw into themselves, remain silent, or run away. This is a nervous breakdown that can be seen as a form of panic attack.
Use of social avoidance strategies. For example, switching attention: “Oh, I like your earrings, where did you get them?” Excuses: "I can't walk, my legs hurt." Postponements: "I'll do it in ten minutes." Dive into fantasy: "I'm a cat, cats don't wear clothes." Shouting someone else's request: "I can't hear you, I sing - la-la-la."
Superficially the individual appears to be sociable. For example, people with PIT, unlike other people on the autism spectrum, may maintain more socially appropriate eye contact. Their conversational skills may seem much better than other people with autism, but it turns out that they do not understand social nuances well. For example, they do not understand the difference between themselves and a person in authority, they find it difficult to change their behavior depending on the needs of other people, and they do not always understand how or why their behavior affects the emotional state of others, which negatively affects their relationship. .
Extreme mood swings and impulsivity. For example, they may have difficulty regulating their emotions and have difficulty controlling their reactions to situations and people. A person can be joyful and sociable now and very angry and sad in just a couple of seconds, and, for outside observers, these changes look inexplicable. Often these mood swings are associated with other people's expectations and pressure due to some kind of requirements.
Role play and pretense are comfortable, sometimes to the point where the line between reality and pretense blurs. For example, a person may start behaving like a character or a real person with authority in a role-playing game and forget himself to such an extent that he begins to consider himself to be this person.
Often we are talking about roles in which it is necessary to give instructions to other people and control the situation, for example, the child plays the role of a teacher with peers. Role playing can be used as a strategy to avoid other people's demands, such as "I can't lift this, I'm a tractor, the tractor has no handles." In other cases, it may be the role of an obedient child, which allows you not to attract unwanted attention. Immersion in a fantasy world can also be a way of self-defense - it's a place to go when real life gets too complicated and difficult to handle.
"Obsessive" behavior, often social in nature. People with PIT often become obsessed with some people, both real and fictional, and this can be both intense love and intense hatred, which makes relationships very difficult. Newson notes that the avoidance of demands itself has signs of obsession. The "pathological" nature of the avoidance of demands means that it is almost always a compulsion, with role play being the second significant compulsion, and the compulsions appear to be more socially oriented in PIT than in autism/Asperger's syndrome. (E Newson, K Le Maréchal, C David, Pathological demand avoidance syndrome: a necessary distinction within the pervasive developmental disorders, 2003).
PIT profile manifestations
People with PIT appear to be more competent in social communication and interaction skills than other people on the autism spectrum. However, their understanding of social interaction and communication tends to be very superficial and lack deep understanding. These people can copy and replicate the social interactions of the people around them in order to better "fit" into the social situation. They may also have well-developed oral speech, but for some people with PIT, it hides very serious difficulties in understanding and understanding other people's speech. These features mean that the difficulties of people with PIT in these areas may not be noticeable at first.
People with PIT may be controlling and dominant in situations where they are anxious and unable to control their environment. However, when they are calm and secure, they can be charming, outgoing, chatty and warm. These dramatic differences in behavior can be confusing for both parents and professionals.
People with PIT may have a variety of positive qualities and abilities that can be directed towards their primary interest, reducing anxiety, and having positive experiences with other people. Very often they are creative, passionate, purposeful individuals with a developed imagination and sense of humor.
The behavior of a person with PIT can vary greatly with different people and situations. For example, a child with PIT may be extremely anxious at home, but very lethargic and passive at school (a learned coping strategy for "camouflage"). However, this often leads to more difficult and problematic behavior at home, where the child feels safe and releases the anxiety he has been suppressing during the day. In such situations, parents may feel inadequate and remain isolated.
For other children, the demands of school lead to severe "nervous breakdowns" in the school setting, and this is often associated with educational problems when the child is expelled from school or sought to be transferred to another class at an early age. Some children experience such strong anxiety at school that they begin to categorically refuse to attend it.
Sensory difficulties
As with other cases of ASD, people with PIT often experience increased or decreased sensory sensitivity, which can be visual, olfactory, gustatory, tactile, auditory, vestibular, or proprioceptive.
Difficult and problematic behavior
A significant proportion of people with PIT experience very serious problems in controlling and regulating their emotions. In childhood, this can lead to aggressive outbursts, as well as other, not so unacceptable avoidance strategies - distractions, excuses, withdrawal, and so on. It is very important to understand that these emotional outbursts are an expression of extreme anxiety, which can quickly turn into a nervous breakdown. It is more of a "panic attack" and the approach to these breakdowns should be appropriate - it should include emotional support, training in self-soothing strategies and de-escalation techniques.
Some children become more aware of their feelings, understand social situations and regulate their emotions as they get older. This can lead to a reduction in the most problematic behaviors in adolescence and adulthood.
Mental health disorders
Mental disorders become a major problem for some children with PIT as they grow older, perhaps because they become more aware of their difficulties and how they affect their lives. These disorders include depression, low self-esteem, self-injurious behavior, eating disorders, self-isolation, obsessive-compulsive disorder (OCD), and other anxiety disorders.
For people with PIT who develop additional psychiatric disorders, it is important to seek professional help, ideally from a specialist who has experience in treating patients with an ASD profile of PIT.
What is the opinion of experts about pathological avoidance of demands?
PIT is not currently included in any official diagnostic manual (DSM-5 or ICD-10). The opinions of different experts on how valid it is to distinguish such a profile in ASD do not coincide.
The PIT profile was first described by Professor Elizabeth Newson in the early 1980s. Since then, various experienced and respected experts in the field of autism have shown interest in PIT. This growing interest and ongoing research is helping to better understand PIT and develop better ways to support and intervene.
“This is a serious coping problem that needs to be acknowledged. That problem is lack of ability, not stubbornness. This problem cannot be solved by "saying what to do" or with the help of some kind of sanctions, - Professor Elizabeth Newson, psychologist.
“PID is most simply understood as an anxiety-based need for control that leads to avoidance of other people's demands and expectations.” - Dr. Phil Christie, Consultant Child Psychologist.
“PIT is a very real clinical problem…intervention and therapy are currently based entirely on guesswork, clinical experience, trial and error. From a therapeutic point of view, this is one of the most complex combinations of problems in child and adolescent psychiatry. Strategies that have been developed for ASD, OCD and ADHD are often ineffective.” – Prof. Christopher Gillberg, Professor of Child and Adolescent Psychiatry at the University of Gothenburg and Emeritus Professor at University College London, UK.
Misdiagnosis
The recognition of PIT as a profile on the autism spectrum is relatively recent. The superficial sociability and often highly developed imagination of children with a PIT profile can be misleading to specialists, which may leave the child with ASD undiagnosed.
For this reason, people with PIT are particularly vulnerable to misdiagnosis when their features are attributed to various disorders they do not have, or they may go undiagnosed. External manifestations of other disorders may resemble PIT on the surface, but have completely different causes. Such disorders include oppositional defiant disorder, conduct disorder, reactive attachment disorder, and attention deficit hyperactivity disorder.
“It is important to recognize that these are children with hidden disabilities who often seem completely 'normal' to other people. Very often, the difficulties of an individual with PIT are mistakenly attributed to improper and inconsistent parenting, and as a result, parents feel that they are unfairly judged, not listened to and isolated. Parents of children with PIT themselves need a lot of support, as their children often have very severe behavioral problems.” - Dr. Judy Eaton, Consultant Clinical Psychologist.
Misdiagnosis and erroneous assumptions about the causes of a person's difficulty with PIT can lead to misunderstanding and suggesting inappropriate interventions. Very often, this only complicates and aggravates the situation and makes the life of the whole family more and more difficult. These cases highlight the importance of timely identification of such a complex ASD profile.
What causes PIT?
The causes of PIT, like other forms of autism, are still being studied. Many experts believe that this combination of strengths and challenges has many different causes. There is evidence that various environmental factors affecting brain development during pregnancy can lead to autism. There is also a lot of evidence that various genetic factors can cause autism.
However, we can say with certainty that PIT is not the result of upbringing or any social circumstances. The parents of the child are not to blame for such difficulties.
Who gets PIT?
In contrast to autism in general, the PIT profile is equally common in girls and boys. So far, no factors associated with a higher prevalence of PIT have been identified. These data may emerge as PIT is more commonly diagnosed concomitantly with ASD. PIT occurs in people of all nationalities and socioeconomic groups.
We hope that the information on our website will be useful or interesting for you. You can support people with autism in Russia and contribute to the work of the Foundation by clicking on the "Help" button.
Diagnostics and tests, Psychiatry, Comorbidities
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
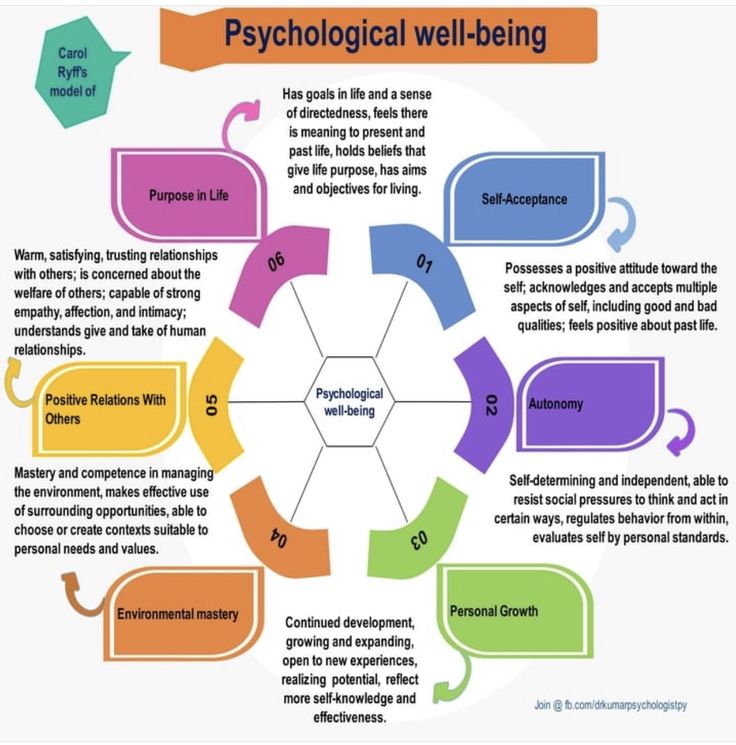
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
Now officially: BPD is a diagnosis
Borderline personality disorder is one of ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.
People with BPD are reverse solipsists: they are convinced of the inviolability of the world around them, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases. It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
Diagnosis is not a sentence, the boundary between the norm and pathology is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
Borderline personality disorder may be accompanied by alcohol, drug, gambling and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Mind, a British mental health resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone. You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
- Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control. In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
- Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.
“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books. If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with interruption of communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires the cause to be identified. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations.
For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
- Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of. At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.
Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills. Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT). Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking.
- Mentalization (MBT). It helps to explain to oneself the behavior of other people, logically argue their motives and work to improve interpersonal interaction.
- Transference Psychotherapy (TFP) teaches to perceive positive and negative qualities simultaneously, to get out of the "deification/devaluation" paradigm.