Paralyzing panic attack
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
causes, symptoms, diagnosis and treatment - medalvian
Skype or WhatsApp consultation available.
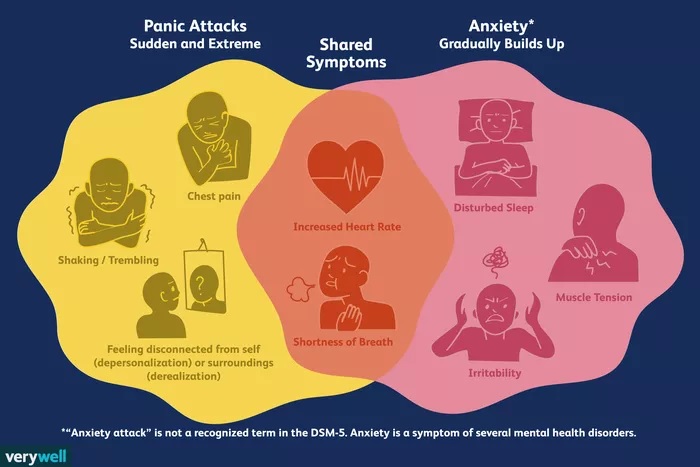
A panic attack is a sudden, uncontrollable attack of severe, “peak” anxiety that has no real and justified cause. This condition is accompanied by intense fear and bodily symptoms - palpitations, shortness of breath, heaviness and pain in the chest, excessive sweating, trembling in the body.
Such attacks can occur not only during the day, but also at night. There is no mind control in sleep - anxiety can manifest itself in threatening, frightening dreams, or it can manifest itself as a panic attack. During the day, a person keeps all emotions in himself, and at night the control weakens, and an attack occurs. Panic attacks in a dream have a certain danger to human health, do not neglect and underestimate the possible adverse effects. Quality sleep is a necessary condition for the full restoration of physical and mental strength. During an attack, there is a sharp awakening with a painful feeling of anxiety and fear, accompanied by all the same bodily symptoms: heart palpitations, shortness of breath, heaviness and pain in the chest, excessive sweating, trembling in the body. Several such nights - and this will lead to a deterioration in general well-being, irritability, decreased performance, i.e. quality of life will be lost.
During the day, a person keeps all emotions in himself, and at night the control weakens, and an attack occurs. Panic attacks in a dream have a certain danger to human health, do not neglect and underestimate the possible adverse effects. Quality sleep is a necessary condition for the full restoration of physical and mental strength. During an attack, there is a sharp awakening with a painful feeling of anxiety and fear, accompanied by all the same bodily symptoms: heart palpitations, shortness of breath, heaviness and pain in the chest, excessive sweating, trembling in the body. Several such nights - and this will lead to a deterioration in general well-being, irritability, decreased performance, i.e. quality of life will be lost.
Panic attacks during sleep cause insomnia. It seems to a person that if he does not sleep, then this will help to avoid an attack. Going to bed is delayed for various reasons. The very thought of going to bed soon causes anxiety and fear.
Such seizures can occur in children, adolescents, and adults; people who have a more sensitive emotional system are most susceptible to them. It is not always possible to immediately recognize that this condition is precisely a panic attack in a dream, but the fact that the quality of night sleep suffers is a serious argument for consulting a psychiatrist, psychotherapist.
It is not always possible to immediately recognize that this condition is precisely a panic attack in a dream, but the fact that the quality of night sleep suffers is a serious argument for consulting a psychiatrist, psychotherapist.
This condition has a close relationship with both biological and psychological causes; it is a disorder that requires professional help from a psychiatrist, psychotherapist.
Causes
Biological causes may be due to the fact that the endocrine glands begin to release a large amount of adrenaline into the blood. This hormone is normally produced in extreme situations that threaten human health or life. It is he who influences the acceleration of all physiological reactions, that is, the heartbeat quickens, the sweat glands and lungs begin to work hard. This is how the body prepares to defend or flee from a deadly threat.
But why does this hormone begin to be released during sleep, when a person is safe and not in danger? The answer to this question is not completely clear yet.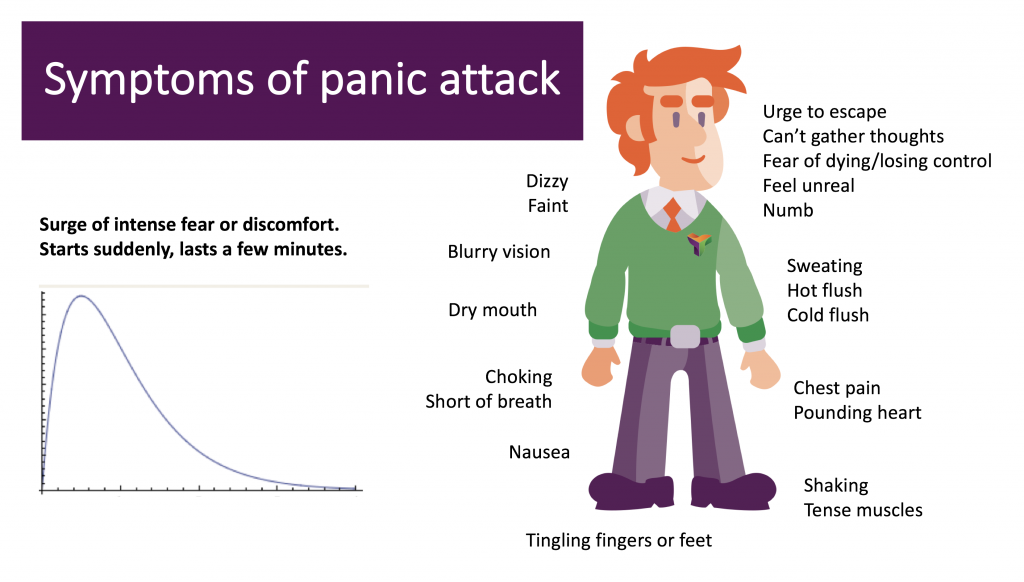 Most likely, there are individual psychological reasons here - for example, increased personal anxiety as a character trait: most often seizures occur in suspicious, emotionally vulnerable and anxious people. It is they who are most prone to self-flagellation and long experiences of life events; and / or negative experience of relationships in the past, in which a person acquired such qualities as distrust, suspicion, lack of internal, psychological permission to relax (“you cannot lose control for a minute, you cannot relax - otherwise something irreparable will happen”).
Most likely, there are individual psychological reasons here - for example, increased personal anxiety as a character trait: most often seizures occur in suspicious, emotionally vulnerable and anxious people. It is they who are most prone to self-flagellation and long experiences of life events; and / or negative experience of relationships in the past, in which a person acquired such qualities as distrust, suspicion, lack of internal, psychological permission to relax (“you cannot lose control for a minute, you cannot relax - otherwise something irreparable will happen”).
Provoking factors for panic attacks at night during sleep are:
- Chronic alcohol consumption or excessive consumption of alcoholic beverages before bedtime.
- Severe stress.
- Childhood psychological trauma.
- Hormonal disorders.
- Exhaustion of the nervous system due to constant experiences, stress.
- Hereditary predisposition to anxiety disorders.
- Traumatic brain injury.
- Labor activity that is associated with constant emotional stress or risk to life.
According to statistics, about 50% of people diagnosed with neurosis or vegetative-vascular dystonia suffered from nighttime panic attacks.
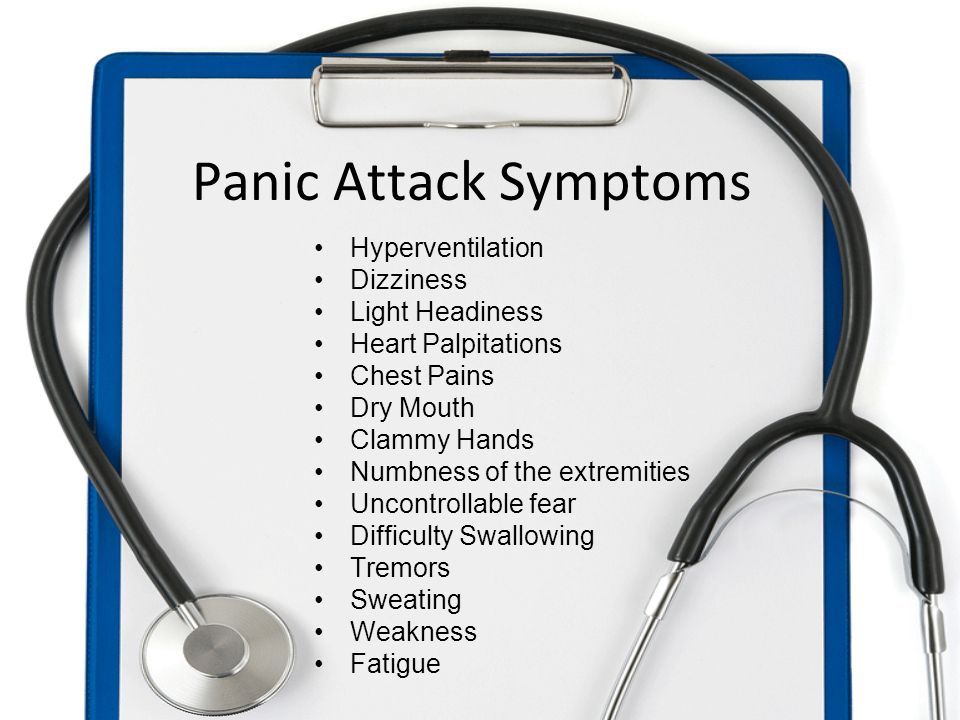
Symptoms
Panic attacks occur during deep sleep, between 2 and 4 am. In rare cases, this condition occurs immediately after falling asleep.
In sleep panic attacks, symptoms include the following:
- abrupt sudden awakening from a feeling of anxiety and intense fear;
- lack of air;
- difficult shortness of breath;
- increased sweating;
- tachycardia;
- increased blood pressure;
- sensation of paralysis or stiffness of the body;
- dizziness;
- chest pain;
- chills, numbness of extremities.
In time, a night attack lasts from 10-20 minutes. Due to paralyzing horror, a person is unable to call for help. Sometimes awakening comes from one's own cry. The darkness in which a person finds himself only aggravates his condition. Therefore, in panic attacks at night during sleep, the symptoms are more pronounced than in daytime attacks.
Sometimes awakening comes from one's own cry. The darkness in which a person finds himself only aggravates his condition. Therefore, in panic attacks at night during sleep, the symptoms are more pronounced than in daytime attacks.
In the first 5-10 minutes after a sudden awakening, there is confusion and disorientation in space. Then comes awareness of the situation. A person tries to calm his pulse, and calm down. Feelings of anxiety and fear can be disturbing for several days, intensifying in the evening. This is due to the fear of falling asleep and again falling into an insurmountable nightmare.
Panic attacks during sleep are also symptomatic of intrusive thoughts (so-called obsessions). There is a fear of serious illness, death, heart attack in a dream. Without proper treatment, seizures can become more frequent and occur every night.
Help with panic attacks
A person suffering from panic attacks at night cannot correctly assess his condition. Often, waking up with a feeling of fear and anxiety is perceived as an ordinary nightmare, so they are in no hurry to seek help.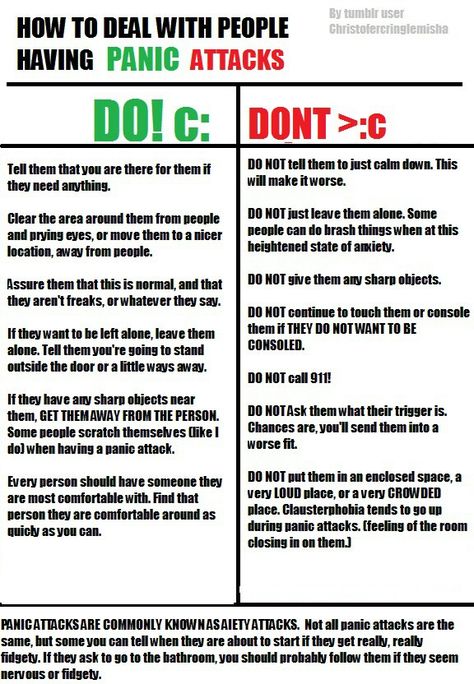 But such episodes are becoming more frequent, and the state of health is worse. When panic attacks occur in a dream, treatment should only be prescribed by a psychiatrist or psychotherapist. At the initial consultation, the doctor collects an anamnesis. Only sincere answers and a confidential conversation with a doctor will help to correctly diagnose and select the optimal therapy. The main goal of conversations with a doctor is to learn to quickly recognize your panic attack and, over time, learn to cope with it, learn to help yourself, gain personal experience of successfully overcoming, coping, and thereby minimize the risk of its reappearance.
But such episodes are becoming more frequent, and the state of health is worse. When panic attacks occur in a dream, treatment should only be prescribed by a psychiatrist or psychotherapist. At the initial consultation, the doctor collects an anamnesis. Only sincere answers and a confidential conversation with a doctor will help to correctly diagnose and select the optimal therapy. The main goal of conversations with a doctor is to learn to quickly recognize your panic attack and, over time, learn to cope with it, learn to help yourself, gain personal experience of successfully overcoming, coping, and thereby minimize the risk of its reappearance.
Sleep panic attack symptoms and treatment are interdependent. With a high level of anxiety, as well as with severe or frequent attacks, a course of anti-anxiety (anxiolytic) drugs gives a good effect. Medications are selected individually, and only with the consent of the patient.
If you have a panic attack in your sleep, how to deal with it without pills?
At the beginning of the disease, relaxation and muscle relaxation techniques help to quickly calm down and bring the nervous system back to normal. This is taught in psychotherapy sessions. Breathing techniques, therapeutic hypnosis, cognitive-behavioral psychotherapy are also effectively used.
This is taught in psychotherapy sessions. Breathing techniques, therapeutic hypnosis, cognitive-behavioral psychotherapy are also effectively used.
Individual and then group psychotherapy is an important step in the treatment of panic attacks. A person needs to understand, understand what his individual causes of anxiety attacks in the daytime are made up of. Learn to respond appropriately to various stressful situations. Find your individual regimen, which is a healthy lifestyle, clearly follow the recommendations of the attending physician. Only in this case the prognosis will be favorable.
Coping with a panic attack at work
How to deal with a panic attack at work | Big Ideas PsychologyArticle published in Harvard Business Review Russia Ruth White Photo: aluxum/Getty Images
You are at work and suddenly you are terrified. Your heart is pounding, your hands are trembling, your head is spinning, you are sweating, you are out of breath.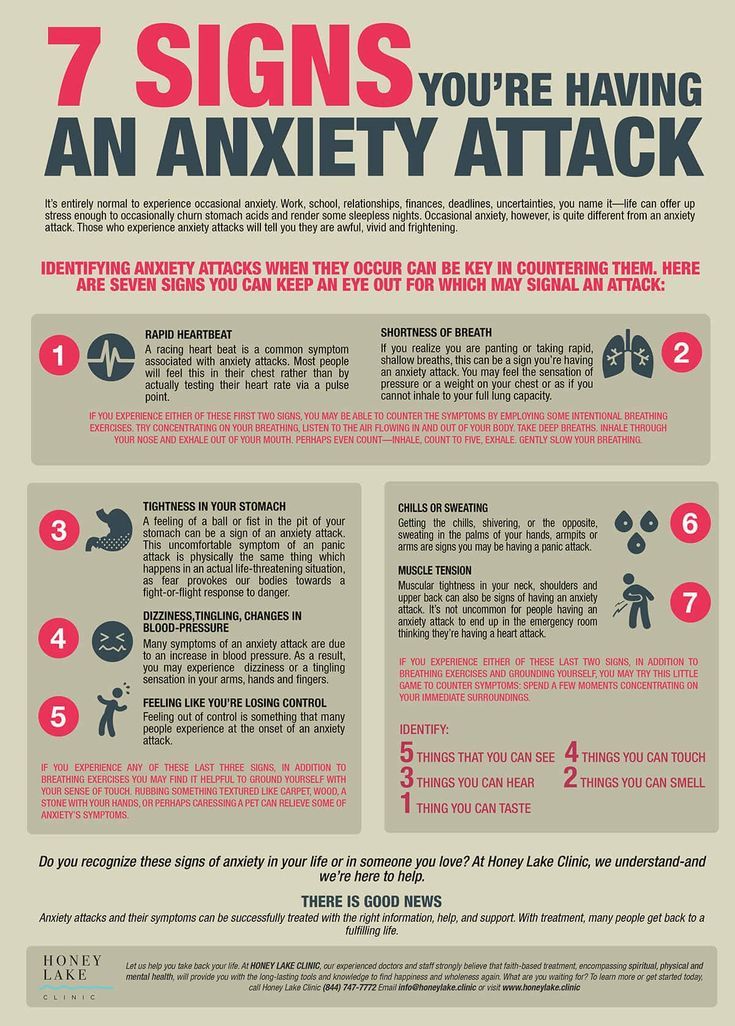 You think you're having a heart attack and you're dying. You are about to call an ambulance when you start to let go. You've had a panic attack.
You think you're having a heart attack and you're dying. You are about to call an ambulance when you start to let go. You've had a panic attack.
What is a panic attack?
The American Psychological Association (APA) describes a panic attack as "a sudden, unexpected, unexplained attack of intense fear." The feelings and physical sensations you experience (such as shortness of breath and tightness in your chest) are very real and can be very frightening. Panic attacks do not die, but depending on the severity and frequency, they can have a significant impact on quality of life. Panic attacks are often triggered by stressful situations, and the symptoms lessen when the stress ends. Factors that can act as triggers at work include public speaking, conflict, an important meeting, a major change such as a promotion or a big project, a work-related event, a meeting with a major client or colleagues.
According to the APA, a panic attack has the following symptoms:
● Rapid heartbeat
● Lack of air
● Almost paralyzing fear
● Lightheadedness, dizziness or nausea
● Trembling, sweating
● Choking or chest pain
● Sudden sensation of heat or cold
● Tingling in fingers and toes
● Fear of death
Panic attacks are isolated events, many experience them only once or twice in a lifetime. If you experience them more frequently, the APA advises seeing a mental health professional for diagnosis and treatment, as you may have panic disorder. Panic disorder is a condition in which people experience frequent, debilitating fear and anxiety for no apparent reason. It may be accompanied by fear of a new attack, anxiety about the problems and consequences associated with it, and changes in behavior. A persistent fear of future panic attacks is the main symptom of panic disorder. A person may begin to avoid situations that caused them to have panic attacks, and this can become a real problem at work. According to the APA, approximately 1.3% of the US population suffers from panic disorder. It is usually diagnosed in adolescence or early adulthood, and although its causes remain unclear, panic attacks can occur in connection with major life changes and stressful social or economic events, such as a pandemic or market crash. Heredity also plays a role: if one of the relatives suffers from panic disorder, the likelihood of panic attacks increases.
If you experience them more frequently, the APA advises seeing a mental health professional for diagnosis and treatment, as you may have panic disorder. Panic disorder is a condition in which people experience frequent, debilitating fear and anxiety for no apparent reason. It may be accompanied by fear of a new attack, anxiety about the problems and consequences associated with it, and changes in behavior. A persistent fear of future panic attacks is the main symptom of panic disorder. A person may begin to avoid situations that caused them to have panic attacks, and this can become a real problem at work. According to the APA, approximately 1.3% of the US population suffers from panic disorder. It is usually diagnosed in adolescence or early adulthood, and although its causes remain unclear, panic attacks can occur in connection with major life changes and stressful social or economic events, such as a pandemic or market crash. Heredity also plays a role: if one of the relatives suffers from panic disorder, the likelihood of panic attacks increases.
If you have occasional or frequent panic attacks, know that they are treatable and the sooner you see a specialist, the better. Even if it's your first or second panic attack, it's important to see a doctor right away, as its symptoms are similar to those of other serious health problems, such as a heart attack.
Coping with a panic attack at work
Work is often stressful, so it is not surprising that many people experience panic attacks at work. The stress in such a situation only intensifies: being out of the house, you cannot lie on the sofa or curl up on the bed.
If you feel a panic attack coming, find a quiet, private place where you can wait it out. If this happens at a meeting or other important moment, try to calmly leave the room to pour yourself water or go to the bathroom. If you are worried that your absence will cause anxiety, text a colleague that you are not feeling well and will return when you feel better. Once in a quiet place, follow the following strategy to manage your symptoms.
1. Breathe deeply and slowly . Try to control your breathing (https://hbr-russia.ru/karera/lichnye-kachestva-i-navyki/841697/): close your eyes (this way you will reduce exposure to irritants) and take deep breaths and slow exhalations through your mouth. Breathe in to a count of four, hold your breath for a second, and then breathe out to a count of four as well. This will slow down your heart rate and help you get rid of the nausea. In addition, you will feel in control and thus reduce fear. If you can't control your breathing, sit down and lower your head to your knees, or exhale into a paper bag if you have one.
recommended reading
Data: why it's important to work for the future
Introverted Science
Robert Kaplan
"It Didn't Work": Why Training Doesn't Always Solve Company Problems
Sue Bingham
Putting a Manager in Context
About the Author
Ruth C.