Other name for propranolol
Propranolol: medicine for heart problems, anxiety and migraine
1. About propranolol
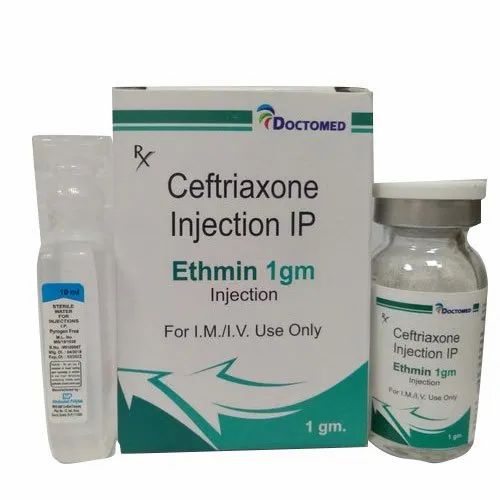
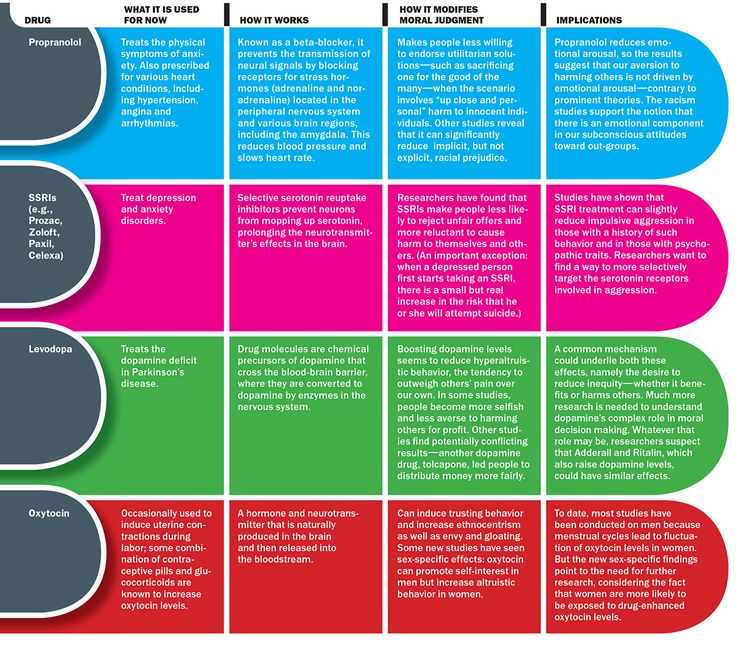
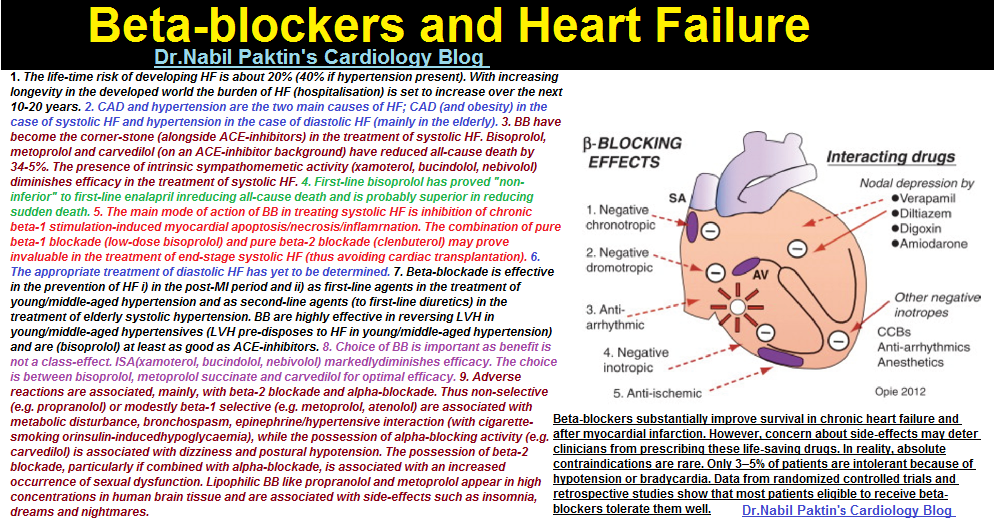
Propranolol belongs to a group of medicines called beta blockers. It's used to treat heart problems, help with anxiety and prevent migraines.
If you have a heart problem, you can take propranolol to:
- treat high blood pressure
- treat conditions that cause an irregular heartbeat (arrhythmia), like atrial fibrillation
- help prevent future heart disease, heart attacks and strokes
- help prevent chest pain caused by angina
Propranolol can help reduce your symptoms if you have too much thyroid hormone in your body (thyrotoxicosis). You'll usually take it together with medicines to treat an overactive thyroid.
This medicine is only available on prescription. It comes as tablets, slow release capsules, or as a liquid that you swallow.
2. Key facts
- Propranolol slows down your heart rate and makes it easier for your heart to pump blood around your body.
- It's usually prescribed for high blood pressure and other heart problems, but it can also help with the physical signs of anxiety, like sweating and shaking.
- Your very first dose of propranolol may make you feel dizzy, so take it at bedtime. After that, if you do not feel dizzy, you can take it in the morning.
- The main side effects of propranolol are feeling dizzy or tired, cold hands or feet, difficulties sleeping and nightmares. These side effects are usually mild and short-lived.
3. Who can and cannot take propranolol
Most adults and children aged 12 and over can take propranolol. But it is not officially approved for treating high blood pressure in children under 12 years old.
But it is not officially approved for treating high blood pressure in children under 12 years old.
Propranolol is not suitable for everyone. To make sure it's safe for you, tell your doctor before starting to take propranolol if you:
- have ever had an allergic reaction to propranolol or any other medicine
- have low blood pressure or a slow heart rate
- have heart failure which is getting worse
- have diabetes
- have liver or kidney problems
- have severe blood circulation problems in your limbs (such as Raynaud's phenomenon), which may make your fingers and toes tingle or turn paler than usual or blue
- have metabolic acidosis, when there is too much acid in your blood
- have lung disease or asthma
- are pregnant, trying to get pregnant or breastfeeding
4.
 How and when to take propranolol
How and when to take propranolol Propranolol comes as 2 different types of medicine:
- standard release – this releases propranolol into your body quickly, so you may need to take it several times a day depending on your dose
- slow release – this releases the medicine slowly so you do not have to take it as often, once a day is usually enough
If you are taking it once a day, your doctor may advise you to take your first dose before bedtime, because it can make you feel dizzy. After the first dose, if you do not feel dizzy, take propranolol in the morning.
Important: Important
Keep taking propranolol even if you feel well. You will still be getting the benefits of the medicine.
Dosage and strength
Propranolol tablets come in strengths of 10mg, 40mg, 80mg or 160mg. The slow release capsules are 80mg or 160mg. The liquid comes in strengths of 5mg, 10mg, 40mg or 50mg in 5ml.
The slow release capsules are 80mg or 160mg. The liquid comes in strengths of 5mg, 10mg, 40mg or 50mg in 5ml.
How much you take depends on why you need propranolol.
The usual doses for adults are:
- high blood pressure – the starting dose is usually 80mg, taken twice a day. If this dose is not working well enough to reduce your blood pressure, your doctor may increase it to a maximum of 160mg twice a day
- migraine or angina (chest pain) – 40mg, taken 2 or 3 times a day. This can be increased to 120mg to 240mg a day. Your doctor or pharmacist will explain how to split the dose over the day
- irregular heartbeat (arrhythmia) – 10mg to 40mg, taken 3 or 4 times a day
- anxiety – 40mg taken once a day which can be increased to 40mg taken 3 times a day
- too much thyroid hormone (thyrotoxicosis) – 10mg to 40mg, taken 3 or 4 times a day
Doses are usually lower for people aged over 65 or people with a kidney or liver problem.
If your child needs propranolol, your doctor will usually use your child's weight to work out the right dose.
How to take it
Propranolol does not usually upset your stomach so you can take it with or without food. It's best to do the same each day.
Swallow the tablets whole with a drink of water. If you find the tablets difficult to swallow, some brands have a score line to help you break the tablet in half. Check the information leaflet for your brand to see if you can do this.
If you're taking capsules, swallow them whole with a drink of water. Do not break, chew or crush them.
If you're taking propranolol as a liquid, it will come with a plastic syringe or spoon to help you measure out the right dose. If you do not have one, ask your pharmacist for one. Do not use a kitchen teaspoon as it will not measure the right amount of medicine.
If you forget to take it
If you forget to take a dose of propranolol, take it as soon as you remember, unless it's nearly time for your next dose. In this case, just leave out the missed dose and take your next dose at the usual time.
Never take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you often forget doses, it may help to set an alarm to remind you. You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
If you take too much
An overdose of propranolol can slow down your heart rate and make it difficult to breathe. It can also cause dizziness and trembling.
The amount of propranolol that can lead to an overdose varies from person to person.
Urgent advice: Contact 111 for advice now if:
- you take more than your prescribed dose of propranolol
Call 111 or go to 111 online
If you need to go to A&E, do not drive yourself. Get someone else to drive you or call for an ambulance.
Get someone else to drive you or call for an ambulance.
Take the propranolol packet or leaflet inside it plus any remaining medicine with you.
5. Side effects
Like all medicines, propranolol can cause side effects in some people, but many people have no side effects or only minor ones.
Side effects often improve as your body gets used to the medicine.
Common side effects
These common side effects happen in more than 1 in 100 people. They're usually mild and short-lived.
Talk to your doctor or pharmacist if the side effects bother you or last more than a few days:
- headaches
- feeling tired, dizzy or weak
- cold fingers or toes
- feeling or being sick (nausea or vomiting), or diarrhoea
- stomach pain
Serious side effects
It happens rarely, but some people have serious side effects when taking propranolol.
Tell a doctor or contact 111 straight away if:
- the whites of your eyes turn yellow, your skin turns yellow although this may be less obvious on brown on black skin, or you have pale poo or dark pee – these can be signs of liver problems
- you get nosebleeds that last for more than 10 minutes, unexplained bruising, or you bruise more easily than usual – these can be signs of low numbers of platelets in your blood (thrombocytopenia)
Go to 111.nhs.uk or call 111.
Immediate action required: Call 999 or go to A&E now if:
- you have shortness of breath with a cough which gets worse when you exercise (like walking up stairs), swollen ankles or legs, chest pain, or an irregular heartbeat – these are signs of heart problems
- you have shortness of breath, wheezing and tightening of your chest – these can be signs of lung problems
Serious allergic reaction
In rare cases, propranolol may cause a serious allergic reaction (anaphylaxis).
Immediate action required: Call 999 or go to A&E now if:
- you get a skin rash that may include itchy, red, swollen, blistered or peeling skin
- you're wheezing
- you get tightness in the chest or throat
- you have trouble breathing or talking
- your mouth, face, lips, tongue or throat start swelling
You could be having a serious allergic reaction and may need immediate treatment in hospital.
These are not all the side effects of propranolol. For a full list, see the leaflet inside your medicine packet.
Information:
You can report any suspected side effect using the Yellow Card safety scheme.
Visit Yellow Card for further information.
6. How to cope with side effects of propranolol
What to do about:
- headaches – make sure you rest and drink plenty of fluids.
 Try not to drink too much alcohol. Ask your pharmacist to recommend a painkiller. Talk to your doctor if the headaches last longer than a week or are severe.
Try not to drink too much alcohol. Ask your pharmacist to recommend a painkiller. Talk to your doctor if the headaches last longer than a week or are severe. - feeling tired, dizzy or weak – as your body gets used to propranolol, these side effects should wear off. If propranolol makes you feel dizzy, sit or lie down until you feel better. It's best not to drink alcohol as it will make you feel worse. Do not drive or ride a bike until you feel better.
- cold fingers or toes – put your hands or feet under warm running water, massage them and wiggle your fingers and toes. Do not smoke or have drinks with caffeine in, as this can make your blood vessels narrower and further restrict blood flow to your hands and feet. Try wearing mittens (they're warmer than gloves) and warm socks. Do not wear tight watches or bracelets.
- feeling or being sick or diarrhoea – stick to simple meals and do not eat rich or spicy food.
 It might help to take your propranolol after a meal or snack. Drink lots of fluids, such as water or squash, to avoid dehydration. Take small, frequent sips if you're being sick. Signs of dehydration include peeing less than usual or having dark, strong-smelling pee. Do not take any other medicines to treat diarrhoea and vomiting without speaking to a pharmacist or doctor. If you take contraceptive pills and you're being sick or have severe diarrhoea, your contraception may not protect you from pregnancy. Check the pill packet for advice.
It might help to take your propranolol after a meal or snack. Drink lots of fluids, such as water or squash, to avoid dehydration. Take small, frequent sips if you're being sick. Signs of dehydration include peeing less than usual or having dark, strong-smelling pee. Do not take any other medicines to treat diarrhoea and vomiting without speaking to a pharmacist or doctor. If you take contraceptive pills and you're being sick or have severe diarrhoea, your contraception may not protect you from pregnancy. Check the pill packet for advice. - stomach pain – try to rest and relax. It can help to eat and drink slowly and have smaller and more frequent meals. Putting a heat pad or covered hot water bottle on your tummy may also help. If you are in a lot of pain, speak to your pharmacist or doctor.
7. Pregnancy and breastfeeding
Propranolol and pregnancy
Propranolol is not thought to be harmful during pregnancy, but it may affect your baby's growth in later pregnancy. Discuss taking propranolol with your doctor or midwife as you may need extra scans to check your baby's growth.
Discuss taking propranolol with your doctor or midwife as you may need extra scans to check your baby's growth.
If you're trying to get pregnant or you're already pregnant, talk to your doctor about the benefits and possible harms of taking propranolol. There may be other medicines that are better to use during pregnancy.
Propranolol and breastfeeding
If your doctor or health visitor says that your baby is healthy, it's OK to take propranolol while breastfeeding.
Propranolol passes into breast milk in tiny amounts. It has not been known to cause any side effects in breastfed babies.
It's important to treat your high blood pressure to keep you well. Breastfeeding will also benefit both you and your baby.
If you notice that your baby is not feeding as well as usual, or seems unusually sleepy, or if you have any other concerns about your baby, then talk to your doctor or health visitor.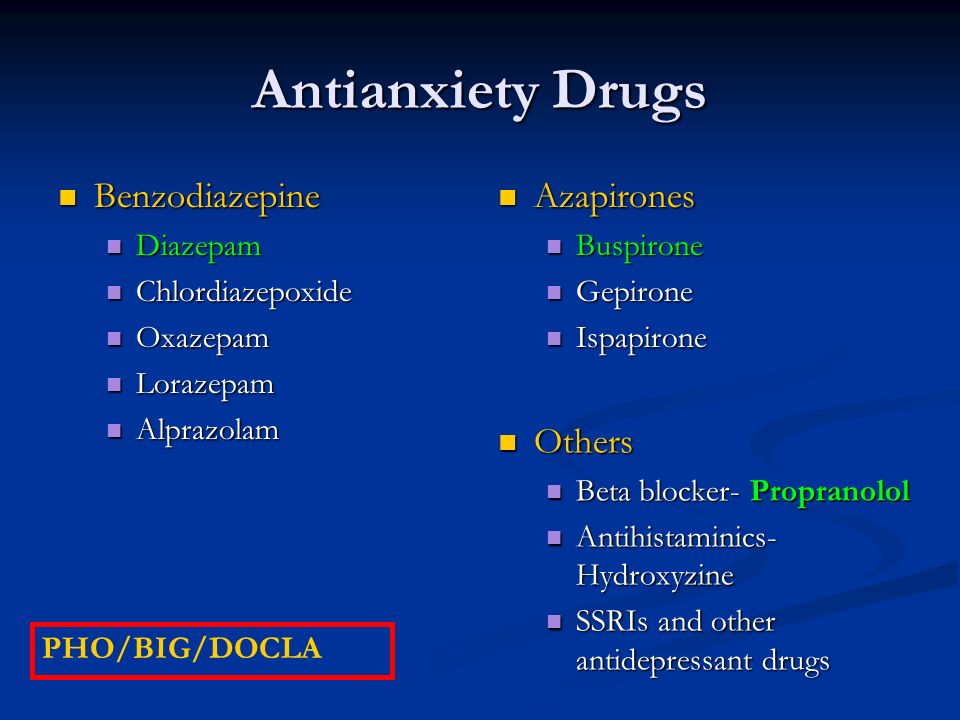
Non-urgent advice: Tell your doctor if you're:
- trying to get pregnant
- pregnant
- breastfeeding
For more information about how propranolol can affect you and your baby during pregnancy, visit the Best Use of Medicines in Pregnancy (BUMPS) website.
8. Cautions with other medicines
There are some medicines that may affect the way propranolol works.
Tell your doctor if you're taking:
- other medicines for high blood pressure. The combination with propranolol can sometimes lower your blood pressure too much. This may make you feel dizzy or faint. If this keeps happening to you, your doctor may change your dose
- other medicines for an irregular heartbeat such as amiodarone or flecainide
- other medicines which can lower your blood pressure.
 These include some antidepressants, nitrates (for chest pain), baclofen (a muscle relaxant), medicines for an enlarged prostate gland like tamsulosin, or Parkinson's disease medicines such as levodopa
These include some antidepressants, nitrates (for chest pain), baclofen (a muscle relaxant), medicines for an enlarged prostate gland like tamsulosin, or Parkinson's disease medicines such as levodopa - asthma or chronic obstructive pulmonary disease (COPD) medicines
- diabetes medicines, particularly insulin – propranolol may make it more difficult to recognise the warning signs of low blood sugar. Speak to your doctor if you have low blood sugar levels without getting any of the usual warning signs. Check your blood sugar after exercise, and follow usual advice about checking it before driving, cycling or operating machinery
- medicines to treat nose or sinus congestion, or other cold remedies (including those you can buy in the pharmacy)
- medicines for allergies, such as ephedrine, noradrenaline or adrenaline
- non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, diclofenac or naproxen.
 These medicines may increase your blood pressure, so it's best to keep them to a minimum
These medicines may increase your blood pressure, so it's best to keep them to a minimum
Mixing propranolol with herbal remedies or supplements
There's very little information about taking herbal remedies and supplements with propranolol. They are not tested in the same way as pharmacy and prescription medicines.
Medicine safety
Tell your doctor or pharmacist if you're taking any other medicines, including herbal medicines, vitamins or supplements.
9. Common questions about propranolol
How does propranolol work?Propranolol is a type of medicine called a beta blocker.
Like other beta blockers, propranolol works by changing the way your body responds to some nerve impulses, including in the heart. It slows down your heart rate and makes it easier for your heart to pump blood around your body.
It works differently if you're using it for anxiety. When you are anxious, your brain makes chemical messengers called adrenaline and noradrenaline. These make your heart rate faster and make you sweat or shake. Propranolol helps block the effects of these chemical messengers. This reduces the physical signs of anxiety.
It's not fully understood how propranolol prevents migraines. It may work by relaxing the blood vessels involved, or by reducing activity in the visual cortex. This is the part of the brain where migraines are believed to start.
How long does propranolol take to work?Propranolol usually starts to work in a few hours.
For heart conditions or high blood pressure, propranolol can take up to a week to reach its full effect. You may not feel any different but that does not mean it is not working. It's important to keep taking your medicine.
For migraines, it can take several weeks for propranolol to start making a real difference, so keep taking it.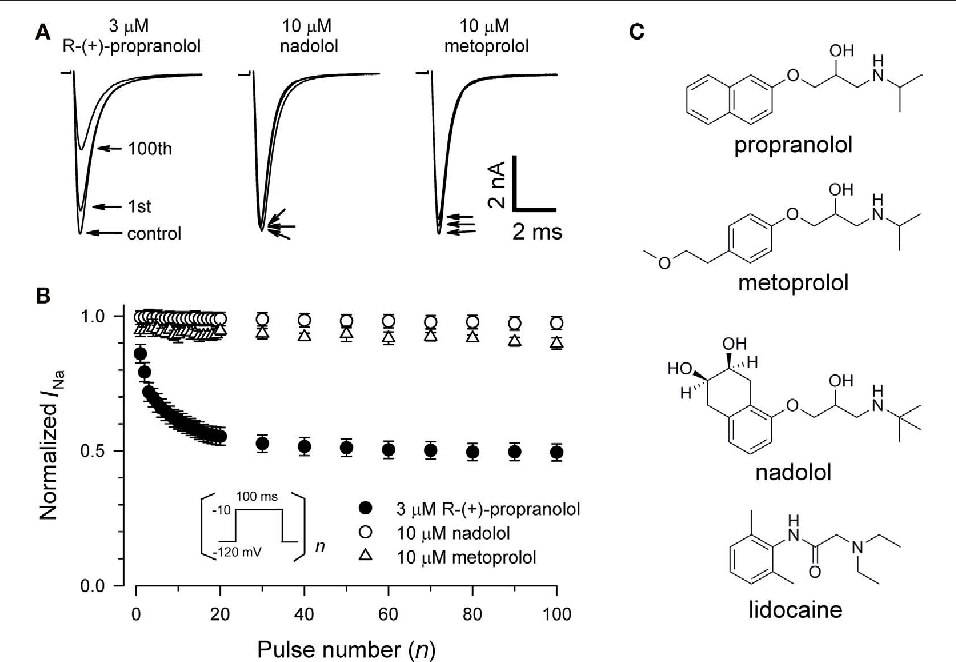
This depends on why you're taking propranolol.
For heart conditions or high blood pressure, treatment is usually long term and may be for the rest of your life.
For anxiety, you'll usually take propranolol for a short amount of time, to help with your physical symptoms. Speak to your doctor about the risks and benefits of taking it for more than a few months. This will depend on your symptoms, whether it's a one-off or a recurring problem, how well propranolol works for you and whether you get side effects.
For migraines, treatment can last for several months or years, depending on how bad your symptoms are.
Can I take propranolol for a long time?Propranolol is generally safe to take for a long time.
If you're taking it for a heart condition, or to prevent migraines, it works best when you take it long term.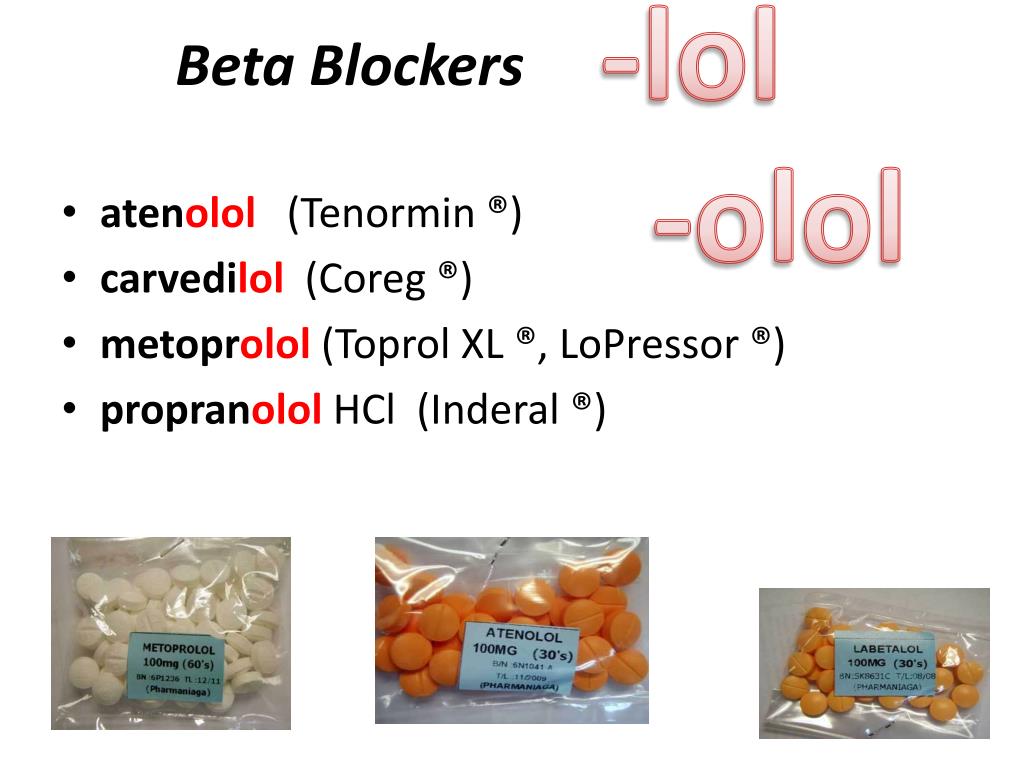
If you're taking it for anxiety, there do not seem to be any lasting harmful effects if you take it for several months or years. But it's best to take propranolol only for as long as you need it.
You'll need to have your blood pressure checked regularly if you're taking propranolol for a long time for migraines or anxiety.
What will happen if I stop taking it?Talk to your doctor if you want to stop taking propranolol. If you're bothered by side effects, your doctor may be able to prescribe a different medicine instead.
Stopping propranolol suddenly may make your health problem worse. In addition, if you stop suddenly after taking it for a long time, you may get extra side effects as a reaction to stopping it. These include an irregular heart rate, sweating and shaking.
If you stop taking propranolol, it will take about 1 to 2 days for it to be completely out of your body but the side effects can last for up to 1 week.
Propranolol works as well as other beta blockers for reducing blood pressure. The main difference between propranolol and other beta blockers is that it does not just affect your heart. It can affect other parts of your body too, such as your lungs.
There are lots of other medicines to lower your blood pressure and treat chest pain. They work in a different way to beta blockers and include:
- ACE inhibitors like ramipril and lisinopril
- angiotensin receptor blockers like candesartan
- calcium channel blockers like amlodipine
- medicines that make you pee more (diuretics) like furosemide
Beta blockers are not usually the first choice for high blood pressure. The medicine your doctor prescribes depends on your age and ethnicity.
If you're under 55 and not of African Caribbean or black African origin, you'll usually be offered an ACE inhibitor or an angiotensin receptor blocker.
If you're 55 or older, or you're any age and of African Caribbean or black African origin, you'll usually be offered a calcium channel blocker.
Sometimes you may have to try other blood pressure-lowering medicines if you get side effects. Many people need to take a combination of different medicines to lower their blood pressure.
How does it compare with other medicines for preventing migraine?Atenolol, metoprolol, timolol and nadolol are all beta blockers and they work well in preventing migraines. However, most doctors prescribe propranolol.
There are some other medicines that are known to prevent migraines but they are not officially approved in the UK. They include amitriptyline, sodium valproate and gabapentin and they may have different side effects.
Topiramate can also be used to prevent migraines. It works just as well as propranolol. However, topiramate has not been officially approved for migraine for children under the age of 16.
Ask your doctor or pharmacist which medicine is best for you.
How does it compare with other medicines for anxiety?Propranolol treats the physical symptoms of anxiety – for example, it stops your heart beating too fast. You'll usually only take propranolol for a short time.
The physical symptoms of anxiety are caused by chemical imbalances in the brain. Your doctor may prescribe an antidepressant like sertraline to treat these imbalances. You usually take antidepressants long term.
Many doctors prefer medicine-free treatments for anxiety. These include talking therapies like cognitive behavioural therapy. If you're having talking therapy, your doctor may prescribe propranolol at the same time. This will help you with your physical symptoms.
This will help you with your physical symptoms.
Tell your doctor that you're taking propranolol if you're going to be put to sleep using general anaesthetic, or you're having any kind of major operation.
Your doctor may advise you to stop taking propranolol before surgery. This is because propranolol can lower your blood pressure too much when it's combined with some anaesthetics.
Can I drink alcohol with it?Drinking alcohol can increase the blood pressure-lowering effect of propranolol, which can make you feel dizzy or lightheaded.
During the first few days of taking propranolol or after an increase in your dose, it's best to stop drinking alcohol until you see how the medicine affects you.
If you find propranolol makes you feel dizzy it's best to stop drinking alcohol.
Apart from being careful with alcohol, you can eat and drink normally while taking propranolol.
Eating a healthy, balanced diet can help if you have high blood pressure or another heart condition.
Will it make me put on weight?Some people on propranolol say they put on weight, especially in the first few months of taking it. This is not known to be a common side effect of taking propranolol, and there is not enough information to say for sure why some people put on weight.
It could, for example, be because propranolol can make you feel tired which could make you less active. It could also affect the way your body uses energy.
If you're worried about putting on weight with propranolol, speak to your doctor.
Will it affect my contraception?Propranolol will not stop your contraception working.
However, some types of hormonal methods of contraception, like the combined pill and contraceptive patch, are not usually recommended if you're taking propranolol or other medicines for high blood pressure. This is because some hormonal contraceptives can raise your blood pressure and stop propranolol working properly.
Talk to your doctor if you're taking a hormonal contraceptive.
If propranolol makes you sick (vomit) or have severe diarrhoea for more than 24 hours, your contraceptive pills may not protect you from pregnancy. Look on the pill packet to find out what to do.
Read more about what to do if you're on the pill and you're being sick or have diarrhoea.
Will it affect my fertility?There is no evidence that propranolol affects fertility in men or women.
If you're trying to get pregnant, or you're having problems getting pregnant while on propranolol, speak to your doctor.
Some people on propranolol say their sex drive goes down and some men find they cannot get an erection. However, this is not a common side effect and there is not enough evidence to say for sure that propranolol is causing it.
If you're having problems with your sex life, talk to your doctor.
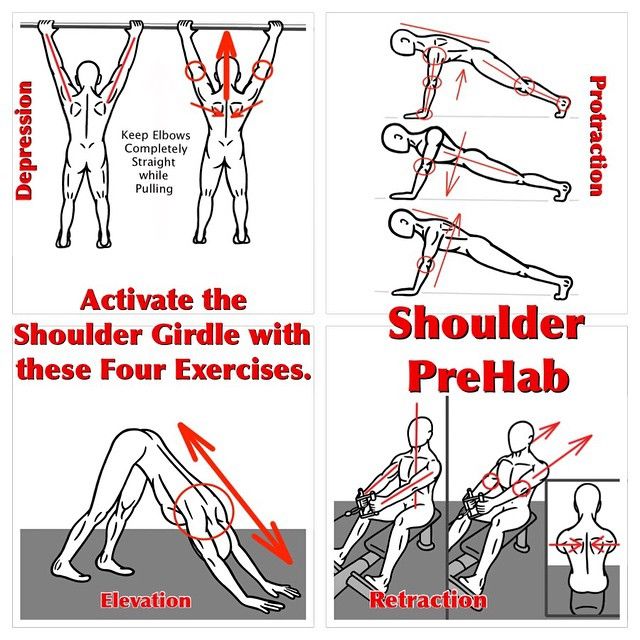
Do I need to avoid playing sports?You do not need to stop playing sports if you take propranolol. But do not push yourself too much.
Regular exercise is good for you because it lowers blood pressure by keeping your heart and blood vessels in good condition.
Be aware, though, that in some sports propranolol is not allowed if you're competing at a high level.
Can I drive or ride a bike?Propranolol can make some people feel dizzy, especially when they first start taking it or after taking a bigger dose. If this happens to you, do not drive a car, ride a bike, or use tools or machinery.
If this happens to you, do not drive a car, ride a bike, or use tools or machinery.
It's an offence to drive a car if your ability to drive safely is affected. It's your responsibility to decide if it's safe to drive. If you're in any doubt, do not drive.
Talk to your doctor or pharmacist if you're unsure whether it's safe for you to drive while taking propranolol. GOV.UK has more information on the law on drugs and driving.
Can lifestyle changes help?If you have heart problems, you can boost the health of your heart by making some key lifestyle changes. These changes will also help if you have high blood pressure.
- Quit smoking – smoking increases your heart rate and blood pressure. Quitting smoking brings down your blood pressure and relieves heart failure symptoms. Try to avoid second-hand smoke too.
- Cut down on alcohol – drinking alcohol while you're taking propranolol can make you feel dizzy or light headed.
 Also drinking too much alcohol raises blood pressure over time and makes heart failure worse. It's best to keep to the recommended limit of no more than 14 units of alcohol a week. A standard glass of wine (175ml) is 2 units. A pint of lager or beer is usually 2 to 3 units of alcohol.
Also drinking too much alcohol raises blood pressure over time and makes heart failure worse. It's best to keep to the recommended limit of no more than 14 units of alcohol a week. A standard glass of wine (175ml) is 2 units. A pint of lager or beer is usually 2 to 3 units of alcohol. - Exercise – regular exercise lowers blood pressure by keeping your heart and blood vessels in good condition. It does not need to be too energetic, walking every day will help.
- Eat well – aim to eat a diet that includes plenty of fruit and vegetables, wholegrains, fat-free or low-fat dairy products and lean proteins. It's a good idea to follow these tips for a lower salt diet too. Eating too much salt is the biggest cause of high blood pressure. The more salt you eat, the higher your blood pressure will be. Aim for no more than 6g of salt a day.
- Deal with stress – when you're anxious or upset, your heart beats faster, you breathe more heavily and your blood pressure often goes up.
 This can make heart failure worse too. Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help avoid stress.
This can make heart failure worse too. Find ways to reduce stress in your life. To give your heart a rest, try napping or putting your feet up when possible. Spend time with friends and family to be social and help avoid stress.
If you get severe headaches, there are steps you can take to help prevent migraines. This includes working out what things trigger an attack so you can avoid them.
Beta blockers - NHS
Beta blockers work mainly by slowing down the heart. They do this by blocking the action of hormones like adrenaline.
Beta blockers usually come as tablets.
They are prescription-only medicines, which means they can only be prescribed by a GP or another suitably qualified healthcare professional.
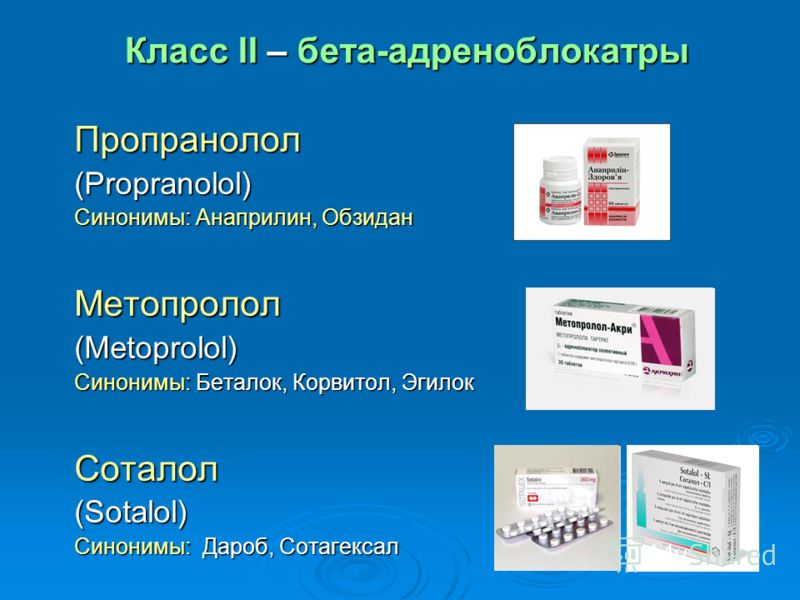
Commonly used beta blockers include:
- atenolol (also called Tenormin)
- bisoprolol (also called Cardicor or Emcor)
- carvedilol
- labetalol (also called Trandate)
- metoprolol (also called Betaloc or Lopresor)
- propranolol (also called Inderal or Angilol)
- sotalol
Uses for beta blockers
Beta blockers may be used to treat:
- angina – chest pain caused by narrowing of the arteries supplying the heart
- heart failure – failure of the heart to pump enough blood around the body
- atrial fibrillation – irregular heartbeat
- heart attack – an emergency where the blood supply to the heart is suddenly blocked
- high blood pressure – when other medicines have been tried, or in addition to other medicines
Less commonly, beta blockers are used to prevent migraine or treat:
- an overactive thyroid (hyperthyroidism)
- anxiety
- tremor
- glaucoma – as eyedrops
There are several types of beta blocker, and each one has its own characteristics. The type prescribed for you will depend on your health condition.
The type prescribed for you will depend on your health condition.
Who can take beta blockers
Beta blockers are not suitable for everyone. To make sure they are safe for you, tell your doctor before starting a beta blocker if you have:
- had an allergic reaction to a beta blocker or any other medicine in the past
- low blood pressure or a slow heart rate
- serious blood circulation problems in your limbs (such as Raynaud's phenomenon, which may make your fingers and toes tingle or turn pale or blue)
- metabolic acidosis – when there's too much acid in your blood
- lung disease or asthma
Tell your doctor if you're trying to get pregnant, are already pregnant or breastfeeding.
It's important not to stop taking beta blockers without seeking your doctor's advice. In some cases suddenly stopping the medicine may make your health condition worse.
In some cases suddenly stopping the medicine may make your health condition worse.
Cautions with other medicines
There are some medicines that may interfere with the way that beta blockers, including beta blocker eyedrops, work.
Tell your doctor if you're taking:
- other medicines for high blood pressure. The combination with beta blockers can sometimes lower your blood pressure too much. This may make you feel dizzy or faint
- other medicines for an irregular heartbeat such as amiodarone or flecainide
- other medicines that can lower your blood pressure. These include some antidepressants, nitrates (for chest pain), baclofen (a muscle relaxant), medicines for an enlarged prostate gland like tamsulosin, or Parkinson's disease medicines such as levodopa
- medicines for asthma or chronic obstructive pulmonary disease (COPD)
- medicines for diabetes, particularly insulin – beta blockers may make it more difficult to recognise the warning signs of low blood sugar
- medicines to treat nose or sinus congestion, or other cold remedies (including those you can buy in the pharmacy)
- medicines for allergies, such as ephedrine, noradrenaline or adrenaline
- non-steroidal anti-inflammatory medicines (NSAIDs), such as ibuprofen.
 These medicines may increase your blood pressure, so it's best to keep them to a minimum
These medicines may increase your blood pressure, so it's best to keep them to a minimum
Side effects of beta blockers
Most people taking beta blockers have either no or very mild side effects that become less troublesome with time.
Contact your GP if you're having symptoms that bother you or last more than a few days.
Side effects commonly reported by people taking beta blockers include:
- feeling tired, dizzy or lightheaded (these can be signs of a slow heart rate)
- cold fingers or toes (beta blockers may affect the blood supply to your hands and feet)
- difficulties sleeping or nightmares
- feeling sick
It happens rarely, but some people have serious side effects when taking beta blockers.
Tell a doctor straight away if you have:
- shortness of breath with a cough that gets worse when you exercise (like walking up stairs), swollen ankles or legs, chest pain, or an irregular heartbeat – these are signs of heart problems
- shortness of breath, wheezing and tightening of your chest – these can be signs of lung problems
- yellow skin or the whites of your eyes turn yellow – these can be signs of liver problems
These are not all the side effects of beta blockers. For a full list, see the leaflet inside your medicine packet.
For a full list, see the leaflet inside your medicine packet.
You can report suspected side effects using the Yellow Card Scheme.
For more information on the side effects of beta blockers, read about the specific medicine you take in our Medicines A to Z.
Missed or extra doses
Most beta blockers are taken once a day, apart from certain beta blockers that are used during pregnancy and Sotalol, which is given 2 or 3 times a day.
What if I forget to take it?
If you forget to take a dose of your beta blocker, take it as soon as you remember, unless it is nearly time for your next dose. In this case, just leave out the missed dose and take your next dose as normal.
Never take 2 doses at the same time. Never take an extra dose to make up for a forgotten one.
If you often forget doses, it may help to set an alarm to remind you.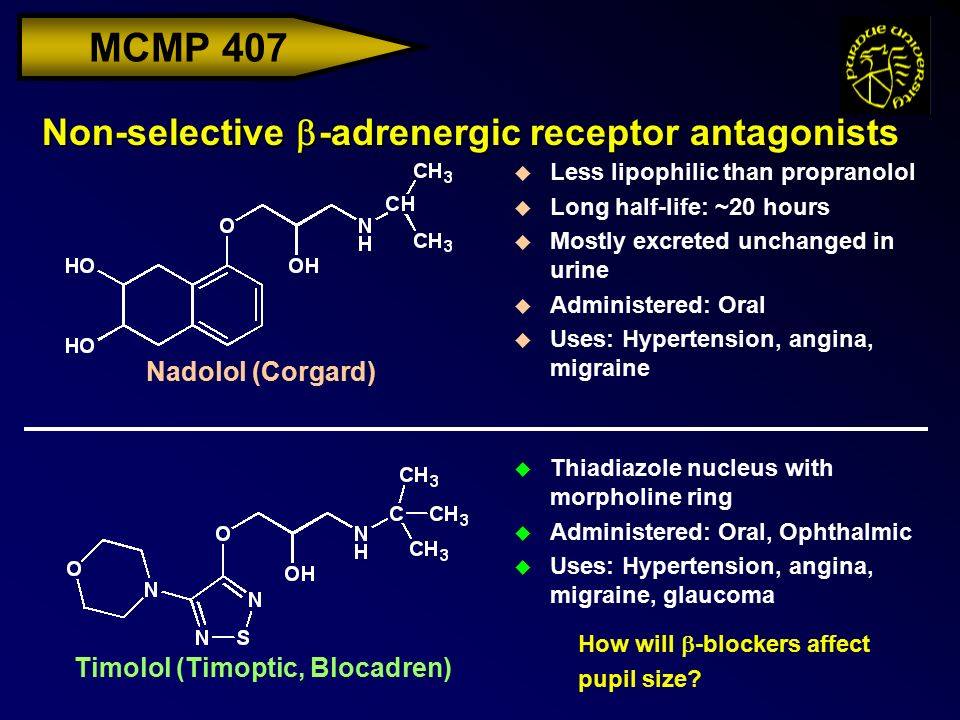 You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
You could also ask your pharmacist for advice on other ways to help you remember to take your medicine.
What if I take too much?
An overdose of beta blockers can slow down your heart rate and make it difficult to breathe. It can also cause dizziness and trembling.
The amount of beta blocker that can lead to an overdose varies from person to person.
Call your doctor or go to A&E straight away if you take too much of your beta blocker.
Page last reviewed: 16 July 2019
Next review due: 16 July 2022
List of medicines with PROPRANOLOL - the active substance PROPRANOLOL in the drug guide Vidal
International name INN: Rec.INN
Single component preparations
trade names of preparations containing only the active substance PROPRANOLOL
| Anaprilin | Tab. | ATOLL (Russia) Produced by: OZONE (Russia) | ||
| Anaprilin | Tab. | BIOSYNTHESIS PAO (Russia) Group: BIOTEK MFPDC (Russia) | ||
| Anaprilin | Tab. | SYNTHESIS (Russia) | ||
| Anaprilin | Tab. 10 mg: 50 pcs. reg. No.: LS-002039 dated 30.08.11 | TATHIMPHARMPREPARATIONS (Russia) | ||
| Anaprilin | Tab. | AVEXIMA (Russia) Produced by: IRBITSK HFZ (Russia) | ||
| Anaprilin | Tab. | PHARMACEUTICAL COMPANY HEALTH (Ukraine) | ||
| Anaprilin | Tab. 40 mg: 10, 15, 20, 30 or 50 pcs. reg. No.: LS-002339 dated 05.07.10 | PHARMSTANDARD-LEKSREDSTVA (Russia) | ||
| Anaprilin | Tab. | ATOLL (Russia) Produced by: OZONE (Russia) | ||
| Anaprilin | Tab. | URALBIOPHARM (Russia) | ||
| Anaprilin | Tab. 40 mg: 50 or 100 pcs. reg. No.: P N003239/01 dated 03.12.08 | SYNTHESIS (Russia) | ||
| Anaprilin | Tab. | TATHIMPHARMPREPARATIONS (Russia) | ||
| Anaprilin | Tab. 40 mg: 50 pcs. reg. No.: LSR-005891/08 from 23.07.08 | AVEXIMA (Russia) Produced by: IRBITSK HFZ (Russia) | ||
| Anaprilin | Tab. | PHARMACEUTICAL COMPANY HEALTH (Ukraine) | ||
| Anaprilin Medisorb | Tab. 40 mg: 7, 10, 14, 20, 21, 28, 30, 35, 40, 42, 50, 56, 70, 100 or 140 pcs. reg. No.: P N003958/01 dated 12.03.10 Re-registration date: 05/23/18 | MEDISORB (Russia) | ||
| Anaprilin Reneval | Tab. | UPDATE (Russia) | ||
| Anaprilin Reneval | Tab. 40 mg: 50 or 100 pcs. reg. No.: LS-002037 dated 29.08.11 | UPDATE (Russia) | ||
| Hemangiol ® | Oral solution 3. | PIERRE FABRE MEDICAMENT (France) Produced by: Pierre Fabre Medicine Production (France) | ||
Descriptions of drugs with invalid reg. beats or not supplied to the Russian market
| Obzidan | Tab. | ACTAVIS GROUP hf. (Iceland) Produced by: SCHWARZ PHARMA (Germany) |
Arpimed
If any of the above factors are present, or if you are unsure about their absence, you must inform your doctor who will be able to advise you in this situation.
Warnings and precautions
Talk to your doctor or pharmacist before taking Capotril.
If you are taking any of the following medicines to treat high blood pressure:
- angiotensin II receptor blockers (ARBs) (also known as sartans - eg valsartan, telmisartan, irbesartan), particularly in the presence of diabetes mellitus complicated by kidney problems,
- aliskiren.
The attending physician may evaluate the patient's kidney function, blood pressure, electrolytes (eg potassium) levels at regular intervals.
You should also read the information in the subheading “ Do not take Capotrile »
Tell your doctor:
- if you are pregnant or planning to become pregnant. Capotrile is not recommended for use in the early stages of pregnancy, and should not be taken if the patient is more than 3 months pregnant as it may cause serious harm to the unborn child (see Pregnancy section),
- about the presence of kidney disease,
- about the presence of liver disease,
- if you are on dialysis,
- about the presence of cardiovascular diseases, in particular those associated with the pathology of the heart valves,
- about the presence of diabetes,
- if you have recently experienced excessive vomiting or diarrhea,
- if you are receiving immunosuppressive therapy.

- If you suffer from collagen vascular diseases such as rheumatoid arthritis, systemic lupus erythematosus or scleroderma.
- If you have an infection accompanied by a sore throat or fever, which may be due to a change in the number of white blood cells, then it is necessary to monitor this process by your doctor with a blood test.
- If you are about to have a dental or major surgery involving the use of an anesthetic.
- If you are considering desensitizing therapy for wasp or bee stings, tell the doctor who will be treating you that you are taking Capotril.
- If you are planning to have a blood decholesterolization procedure (LDL apheresis), you must tell your doctor that you are taking Capotril.
Tell your doctor that you are taking Capotrile before having any blood or urine tests because taking Capotrile may affect the results of some tests.
Children and adolescents
The safety and efficacy of Capotril in children have not been established.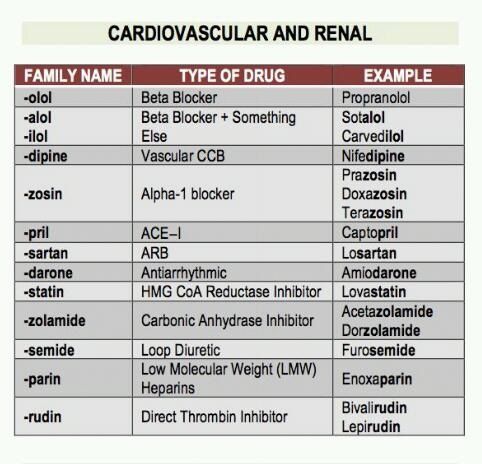
Other medicines and Capotrile
Tell your doctor or pharmacist if you have recently taken or are taking any other medicines. It is especially important to tell your doctor if you are taking any of the following medicines:
- non-steroidal anti-inflammatory painkillers - NSAIDs (e.g. indomethacin, ibuprofen),
- immunosuppressants (e.g. azathioprine and cyclophosphamide),
- dietary supplements containing potassium , salt substitutes containing potassium, or any other drug that may increase body potassium (eg, amiloride, spironolactone, triamterene),
- diuretics ,
- drugs for treatment gout (e.g. allopurinol, probenecid),
- medicines to treat diabetes (e.g. insulin)
- medicines that cause dilation of blood vessels (e.g. minoxidil, clonidine),
- medicines to treat psychiatric disorders including manic depression and depression (eg lithium or amitriptyline),
- medicines to treat high blood pressure (e.
 g. beta-blockers such as propranolol, atenolol or calcium channel blockers such as amlodipine, nifedipine),
g. beta-blockers such as propranolol, atenolol or calcium channel blockers such as amlodipine, nifedipine), - medicines for use during and after a heart attack .
- medicines to treat irregular heartbeats (eg, procainamide).
The physician may need to change the dose and/or take other precautions if the patient is taking an angiotensin II receptor blocker (ARB) or aliskiren (see also information under the subheadings "Do not take Capotril" and "Warnings and precautions").
Capotrile with food and drink
Capotrile can be taken with or without food.
A moderate amount of alcohol will not affect the effect of Capotril, however, it is necessary to consult with the attending physician whether the patient is allowed to drink alcohol.
Pregnancy and breast-feeding
If you are pregnant or breastfeeding, or planning to become pregnant, ask your doctor or pharmacist for advice before taking Capotril.
Pregnancy
You must tell your doctor if you are pregnant or if you are pregnant. The attending physician usually advises the patient to stop taking Capotril before planning or immediately in the event of pregnancy and recommends taking another medicine with identical indications instead of Capotril. Capotrile is not recommended in early pregnancy, and is not approved for use after 3 months of pregnancy, as this can cause serious harm to the unborn child.
Breastfeeding
Tell your doctor if you are breastfeeding or planning to do so soon. Breastfeeding of newborns (in the first few weeks after birth), and especially premature babies, is not recommended while taking Capotril.
If used in an older child, the physician should report the benefits and risks of using Capotril during breastfeeding compared to other treatments.
Talk to your doctor or pharmacist before taking any medicine.
When planning a surgical intervention
Before surgery and anesthesia (even for dental procedures), it is necessary to inform the attending physician or dentist about the current use of Capotrile, as a sudden drop in blood pressure is possible.
Driving and operating machinery
Capotrile may affect the ability to drive vehicles, usually when the drug is first taken, or when the dose of the drug is changed by a doctor. If dizziness occurs when taking Capotrila tablets, you should not drive vehicles and operate mechanisms.
Capotrile contains lactose
Capotrile contains lactose, which is a disaccharide. If you have an intolerance to some sugars, call your doctor before taking this drug.
How to take Capotrile
Take Capotrile exactly as directed by your doctor or pharmacist.
Tablets are taken orally with a glass of water.
Recommended doses:
For the treatment of high blood pressure
The usual starting dose is 12. 5 - 25 mg twice a day. The attending physician may gradually increase the dose to 100 - 150 mg per day. You may need to take other blood pressure medications at the same time.
5 - 25 mg twice a day. The attending physician may gradually increase the dose to 100 - 150 mg per day. You may need to take other blood pressure medications at the same time.
Elderly patients and those with kidney problems should start at a lower starting dose.
In heart failure
The usual starting dose is 6.25-12.5 mg two or three times a day. Your doctor may gradually increase the dose up to 150 mg per day.
After a heart attack
The usual starting dose is 6.25 mg, which will then be increased by the attending physician to 150 mg per day.
For the treatment of patients with diabetes and kidney disease
The usual dose is 75 - 100 mg per day.
Elderly patients (over 65):
Your doctor may prescribe you a lower dose of the drug. If you have impaired kidney function, your doctor may gradually increase your dose until your blood pressure is adequately controlled.
The doctor can then adjust the dosage according to individual needs.
For children
The initial dose is 0.3 mg/kg of body weight, which can be gradually increased by the attending physician.
For children with kidney disease, premature babies, newborns and infants
The initial dose should be 0.15 mg/kg of body weight.
Different doctors sometimes prescribe different doses for the above groups of patients, therefore, in each individual case, a doctor should be consulted. If necessary, for a dosage of 12.5 mg, the tablet can be divided in half.
Occasionally, patients may experience dizziness after taking the first one or two doses of Capotril. In this case, you should lie down until these symptoms disappear.
Take Capotrile at about the same time each morning. Capotrile can be taken before, during or after meals.
Even if you feel well, continue taking Capotrile until your doctor decides otherwise.
When taking Capotril at a dose higher than recommended
If you or someone else has taken too many pills, you should go to the nearest emergency room of the treatment center or tell your doctor immediately. The packaging and all remaining tablets should be taken with you.
If you forget to take Capotrile
Do not worry if you miss another dose of the drug. You just have to keep taking your usual dose as prescribed.
Do not take a double dose to make up for a missed dose. If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
If you stop taking Capotril tablets
Do not stop taking this drug without telling your doctor.
If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
Possible side effects
Like all medicines, Capotril can cause side effects, although not everyone gets them. If any of the following adverse reactions develop, you should stop taking Capotril and consult a doctor immediately:
If any of the following adverse reactions develop, you should stop taking Capotril and consult a doctor immediately:
- swelling of the hands, face, lips or tongue,
- shortness of breath,
- sudden, unexpected rash or burning, redness or peeling of the skin,
- sore throat or fever,
- severe dizziness or fainting,
- severe abdominal pain,
- unnaturally rapid or irregular pulse,
- yellowing of the skin and/or eyes (jaundice). Dizziness
- Dry mouth
- Itching
- Insomnia
- Rash Diarrhea or constipation
- Hair loss
- Dry, irritating cough
- Taste disorders
- Dyspeptic disorders, nausea, vomiting, abdominal pain
- Respiratory failure
- Gastric ulcers
Infrequent side effects (more than 1/1000 but less than 1/100 (more than 0.1%, but less than 1%) )
- Frequent, irregular, severe heartbeat
- Fatigue
- Chest pain
- General malaise
- Low blood pressure
- Paleness
- Decreased blood flow to the arms and legs (eg, Raynaud's syndrome)
- Edema of the eyes and lips (angioedema)
- Hot flashes
- Loss of appetite
- Headache
- Numbness or tingling
Rare side effects (more than 1/10000 but less than 1/1000 (more than 0. 01% but less than 0.1%))
01% but less than 0.1%))
- Oral manifestations
- Renal dysfunction or renal insufficiency
- Changes in urinary frequency
- Kidney disease or failure
Very rare side effects ( less than 1/10000 (less than 0.01%) )
- DISEPTION OF FURGE AND EMPLICTION OF PRODUCTION OF PRODUCTION AND ENTICT
- Liver injury and inflammation or jaundice
- Confusion, depression, loss of consciousness
- Minor stroke
- Muscle pain
- Blurred vision
- Joint pain
- Heart problems including heart attack and chest infections
- Wheezing or labored breathing
- Inflammation of the pancreas
- Rash or skin reactions
- Runny nose
- Swelling of the mammary glands in men
- Swelling of the tongue
- High temperature
- Impotence
- Skin photosensitivity
- Stevens-Johnson syndrome (severe disease with blisters on the skin, mouth, eyes and genitals)
- Changes in the levels of various substances in the blood or lymphatic system (eg potassium, sugars)
If any of these side effects become serious, or if you experience any side effects not listed in this package leaflet, tell your doctor or pharmacist immediately. It will be very helpful if the patient pays attention to what he experienced, when it started and how long it lasted.
It will be very helpful if the patient pays attention to what he experienced, when it started and how long it lasted.
Additional information
What Capotrile 25 mg tablets contains
other ingredients: hydrogenated castor oil, ethylcellulose, sodium starch glycolate, magnesium stearate, purified talc, lactose monohydrate, microcrystalline cellulose.
How and how long to store Capotril tablets
Keep out of the reach of children, at a temperature not exceeding 25 0 C, in original packaging.
Shelf life - 3 years. Do not use after the expiration date stated on the package. The expiry date is the last day of the month indicated on the drug packaging.
Do not dispose of drugs down the drain (water supply). Ask your pharmacist how to dispose of drugs you no longer need. These measures will help protect the environment.
What can a capitril of 25 mg tablets look, which is packaging
Capotril 25 mg tablet
Round with a flat end surface of a white or almost white table with a specific smell, with a risk of risk.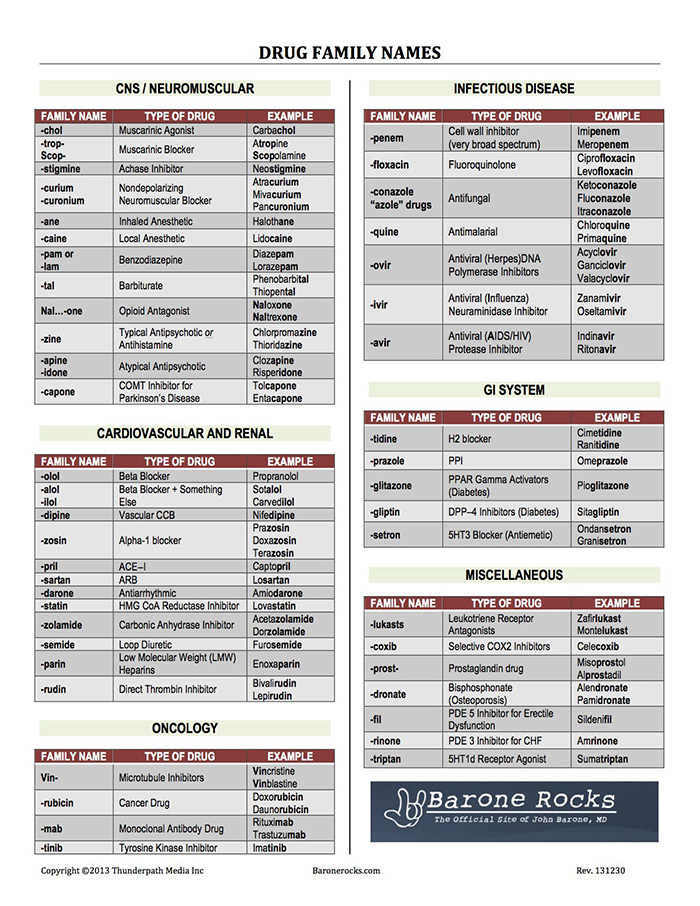
 10 mg: 10, 20, 25, 30, 40, 50, 60, 70, 75, 80, 90, 100, 120, 125, 150, 175, 180, 200, 210, 225, 240, 250, 270, 300 , 350, 400, 450 or 500 pcs.
10 mg: 10, 20, 25, 30, 40, 50, 60, 70, 75, 80, 90, 100, 120, 125, 150, 175, 180, 200, 210, 225, 240, 250, 270, 300 , 350, 400, 450 or 500 pcs. 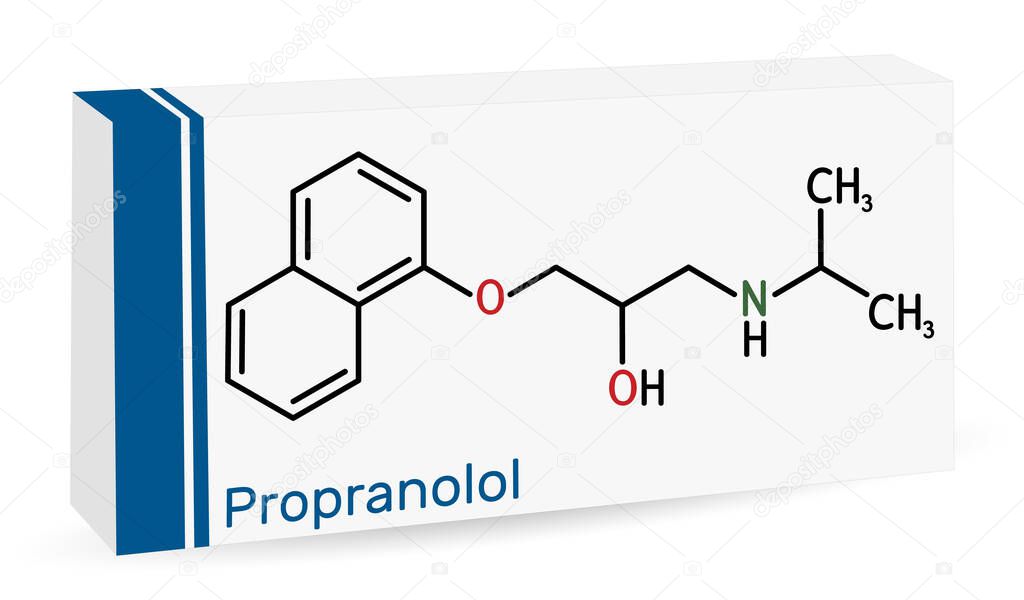 10 mg: 50 or 100 pcs.
10 mg: 50 or 100 pcs.  10 mg: 50 or 100 pcs.
10 mg: 50 or 100 pcs.  10 mg: 50 pcs.
10 mg: 50 pcs.  10 mg: 50 pcs.
10 mg: 50 pcs.  40 mg: 10, 20, 25, 30, 40, 50, 60, 70, 75, 80, 90, 100, 120, 125, 150, 175, 180, 200, 210, 225, 240, 250, 270, 300 , 350, 400, 450 or 500 pcs.
40 mg: 10, 20, 25, 30, 40, 50, 60, 70, 75, 80, 90, 100, 120, 125, 150, 175, 180, 200, 210, 225, 240, 250, 270, 300 , 350, 400, 450 or 500 pcs.  40 mg: 10, 20, 30, 40, 50, 60 or 100 pcs.
40 mg: 10, 20, 30, 40, 50, 60 or 100 pcs. 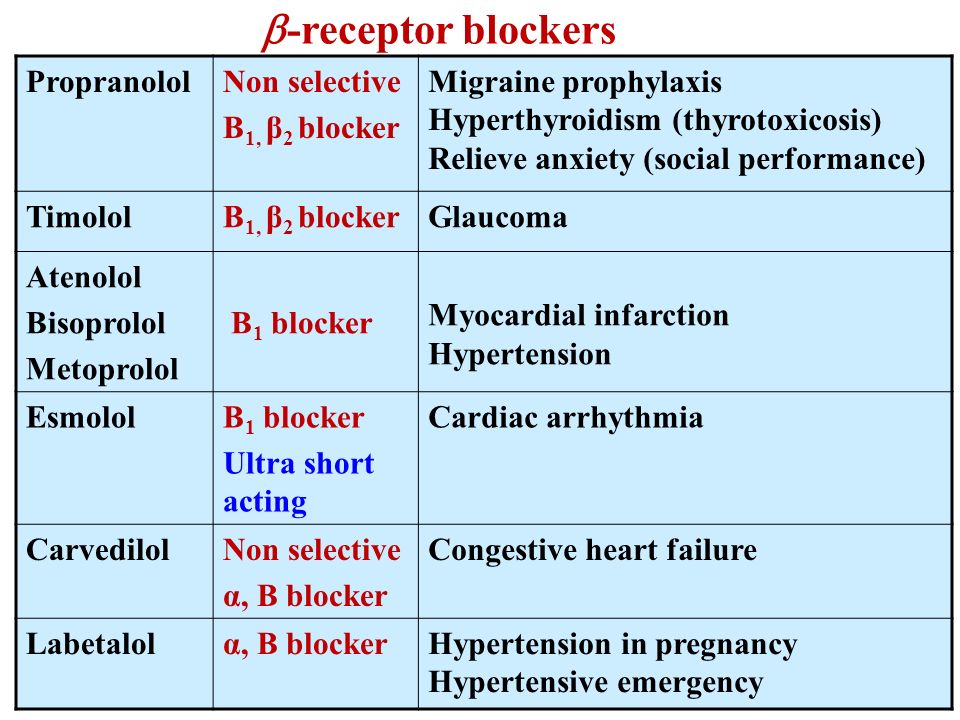 40 mg: 50 pcs.
40 mg: 50 pcs. 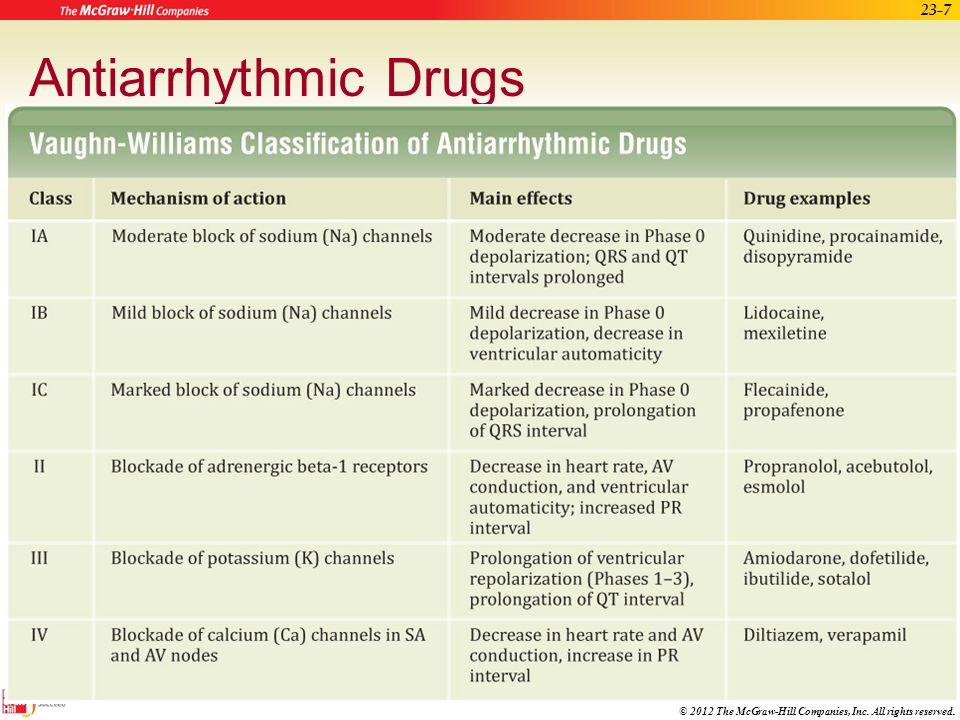 40 mg: 50 pcs.
40 mg: 50 pcs.  10 mg: 50 or 100 pcs.
10 mg: 50 or 100 pcs.  75 mg/1 ml: vial. 120 ml 1 pc. in set with dosing syringe
75 mg/1 ml: vial. 120 ml 1 pc. in set with dosing syringe  40 mg: 60 pcs.
40 mg: 60 pcs.