Ocd treatment therapy
International OCD Foundation | How is OCD Treated?
Overview
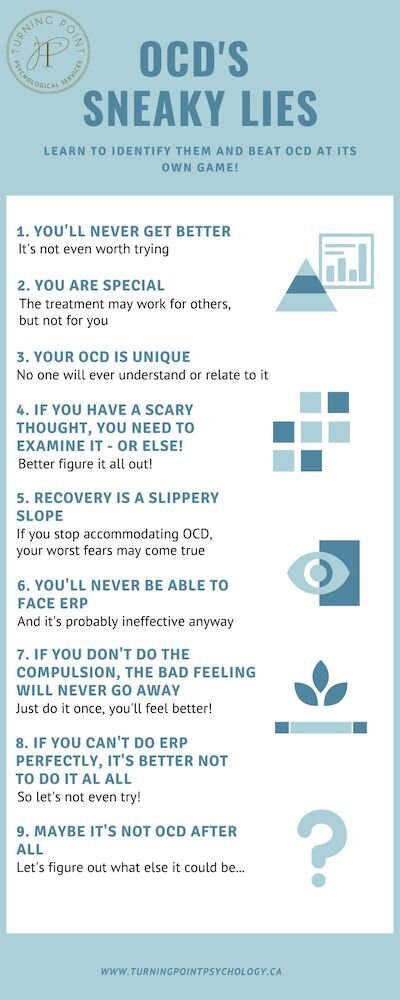
- Treatment for most OCD patients should involve Exposure and Response Prevention (ERP) and/or medication.
- The majority of people with OCD (about 7 out of 10) will benefit from either medication or ERP.
What Are the Most Effective Treaments for OCD?
The most effective treatments for OCD are Cognitive Behavior Therapy (CBT) and/or
medication. [1] More specifically, the most effective treatments are a type of CBT called Exposure and Response Prevention (ERP), which has the strongest evidence supporting its use in the treatment of OCD, and/or a class of medications called serotonin reuptake inhibitors, or SRIs.
Exposure and Response Prevention is typically done by a licensed mental health professional (such as a psychologist, social worker, or mental health counselor) in an outpatient setting. This means you visit your therapist’s office at a set appointment time once or a few times a week. Click here for help finding the right therapist for you.
Medications can only be prescribed by a licensed medical professionals (such as your physician or a psychiatrist), who would ideally work together with your therapist to develop a treatment plan. Click here to learn more about medications for OCD.
Taken together, ERP and medication are considered the “first-line” treatments for OCD. In other words, START HERE! About 70% of people will benefit from ERP and/or medication for their OCD.
What if Outpatient ERP Hasn’t Worked? Are There More Intensive Options?
Yes. If you or a loved one has tried traditional outpatient therapy and would like to try a more intensive level of care, there are options.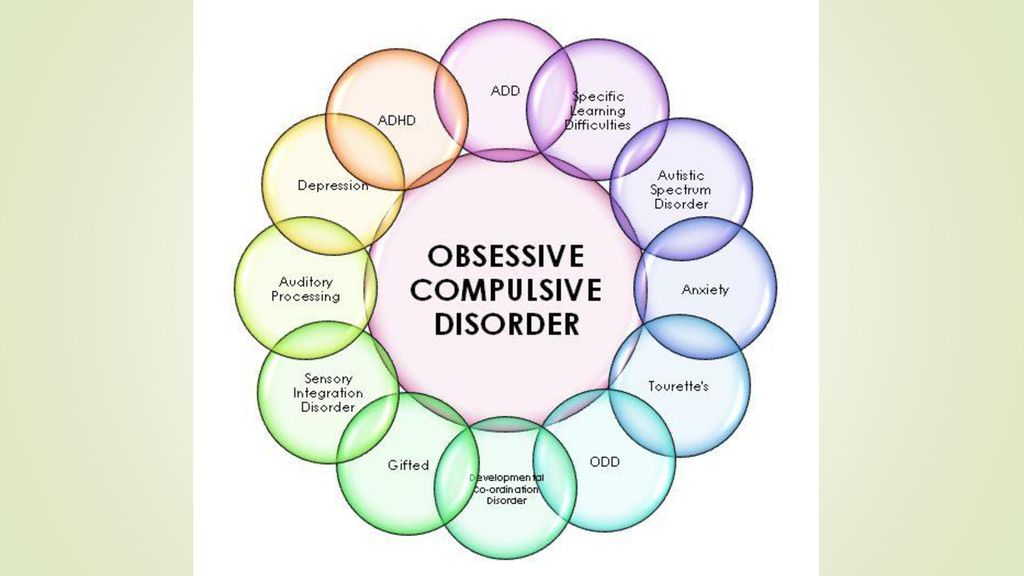 The IOCDF keeps a Resource Directory of intensive treatment centers, specialty outpatient clinics, and therapist who provide these various levels of services for OCD. The following lists therapy options from least intensive to most intensive:
The IOCDF keeps a Resource Directory of intensive treatment centers, specialty outpatient clinics, and therapist who provide these various levels of services for OCD. The following lists therapy options from least intensive to most intensive:
- Traditional Outpatient – Patients see a therapist for individual sessions as often as recommended by their therapist generally one or two times a week for 45-50 minutes. (Most Therapists in the Resource Directory as well as “Specialty Outpatient Clinics” offer this type of treatment).
- Intensive Outpatient – Patients may attend groups and one individual session per day several days per week. Clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment.
- Day Program – Patients attend treatment during the day (typically group and individual therapy) at a mental health treatment center usually from 9am – 5pm up to five days a week.
 Many clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment.
Many clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment. - Partial Hospitalization – Same as the Day Program but patients attend the treatment at a mental health hospital. Several clinics designated as “Intensive Treatment Programs” in the Resource Directory offer this level of treatment.
- Residential – Patients are treated while living voluntarily in an unlocked mental health treatment center or hospital. Clinics designated as “Residential” in the Resource Directory offer this level of treatment.
- Inpatient – This is the highest level of care for a mental health condition. Treatment is provided on a locked unit in a mental health hospital on a voluntary or sometimes involuntary basis. Patients are admitted into this level of care if they are unable to care for themselves or are a danger to themselves or others. The goals of inpatient treatment are to stabilize the patient, which generally takes several days to a week, and then transition the patient to a lower level of care.

Additional Treatment Options for OCD
Other recommendations from the APA Practice Guideline,1 cite research showing that ERP delivered in a group format, as well as ERP therapy delivered via videoconferencing (teletherapy), might be effective. Also, there is some promising new research showing that Acceptance and Commitment Therapy may be helpful for OCD. You can search for any of these treatment types in the Resource Directory.
OCD treatment can be difficult, and requires a lot of courage and determination. Having a support network to talk to during treatment can make all the difference.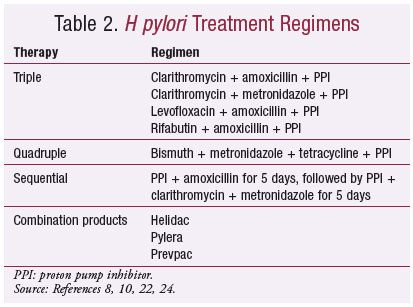 Consider accessing a support group in your area. Click here to learn more about support groups.
Consider accessing a support group in your area. Click here to learn more about support groups.
OCD can be a family affair. Read more here about the impact on families and what family members can do.
When severe OCD proves resistant to standard forms of treatment, there are other options available. However, it should be noted that all of the following procedures are still currently being researched. While there is evidence to suggest that they could potentially be helpful in reducing OCD symptoms, they are not concretely proven to do so. These should be utilized as a last resort when all of the evidence-based treatment methods for OCD (outlined above) have already been accessed:
What about PANDAS?
PANDAS (Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal infections) is a rare type of OCD that occurs in childhood following the immune system’s overreaction to an infection, such as strep throat.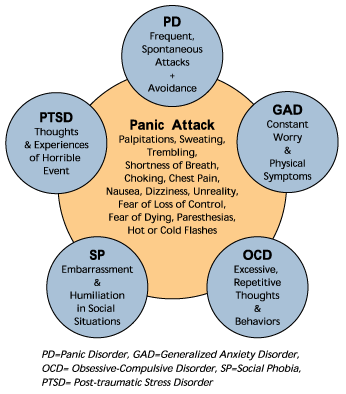 PANDAS should be managed with early antibiotic treatment for strep infections. Continued symptoms can be treated with standard OCD treatments such as exposure and response prevention (ERP) therapy and/or SRI medication*. For more information on PANDAS, including diagnosis and treatment, click here.
PANDAS should be managed with early antibiotic treatment for strep infections. Continued symptoms can be treated with standard OCD treatments such as exposure and response prevention (ERP) therapy and/or SRI medication*. For more information on PANDAS, including diagnosis and treatment, click here.
*Closely watching a child's reaction to SRIs is important as they can cause severe behavioral problems, including suicidal thoughts.
Learn More About OCD
International OCD Foundation | Medications for OCD
PLEASE NOTE: The International OCD Foundation has no conflicts of interest or financial relationships related to the content of this web page.The following information refers to OCD medications in adults. For information on medication in children, click here.
Overview
- Medication is an effective treatment for OCD.
- About 7 out of 10 people with OCD will benefit from either medication or Exposure and Response Prevention (ERP).
 For the people who benefit from medication, they usually see their OCD symptoms reduced by 40-60%.
For the people who benefit from medication, they usually see their OCD symptoms reduced by 40-60%. - For medications to work, they must be taken regularly and as directed by their doctor. About half of OCD patients stop taking their medication due to side effects or for other reasons. If you experience side effects, you should bring this up with your doctor so they can help you address them. They may be able to change your dose or find a different type of SRI that your system better tolerates.
What kinds of medications may help OCD?
The types of medication that research has shown to be most effective for OCD are a type of drug called a Serotonin Reuptake Inhibitor (SRI), which are traditionally used as an antidepressants, but also help to address OCD symptoms. (Note: Depression can sometimes result from OCD, and doctors can treat both the OCD and depression with the same medication.)
Do all antidepressants help OCD symptoms?
No! Some commonly used antidepressants have almost no effect whatsoever on OCD symptoms. Drugs, such as imipramine (Tofranil®) or amitriptyline (Elavil®), that are good antidepressants, rarely improve OCD symptoms.
Drugs, such as imipramine (Tofranil®) or amitriptyline (Elavil®), that are good antidepressants, rarely improve OCD symptoms.
Which Medications Help OCD?
The following antidepressants have been found to work well for OCD in research studies:
|
|
|
|
|
|
|
|
Have These Drugs Been Tested?
Anafranil has been around the longest and is the best-studied OCD medication. There is growing evidence that the other drugs are as effective. In addition to these carefully studied drugs, there are hundreds of case reports of other drugs being helpful. For example, duloxetine (Cymbalta®) has been reported to help OCD patients who have not responded to these other medications.
In addition to these carefully studied drugs, there are hundreds of case reports of other drugs being helpful. For example, duloxetine (Cymbalta®) has been reported to help OCD patients who have not responded to these other medications.
What Are the Usual Doses for These Drugs?
High doses are often needed for these drugs to work in most people.* Studies suggest that the following doses may be needed:
|
|
|
|
|
|
|
|
Which Drug Should Someone Try First?
Whenever any of the above drugs have been studied head to head, there seems to be no significant difference in how well they work. However, for any given patient, one drug may be very effective, and the others may not. The only way to tell which drug will be the most helpful with the least side effects is to try each drug for about 3 months. Remember! It is important not to give up after failing one or two drugs. Drugs work very differently for each person.
However, for any given patient, one drug may be very effective, and the others may not. The only way to tell which drug will be the most helpful with the least side effects is to try each drug for about 3 months. Remember! It is important not to give up after failing one or two drugs. Drugs work very differently for each person.
How Do These Medications Work?
It remains unclear as to how these particular drugs help OCD. The good news is that after decades of research, we know how to treat patients, even though we do not know exactly why our treatments work.
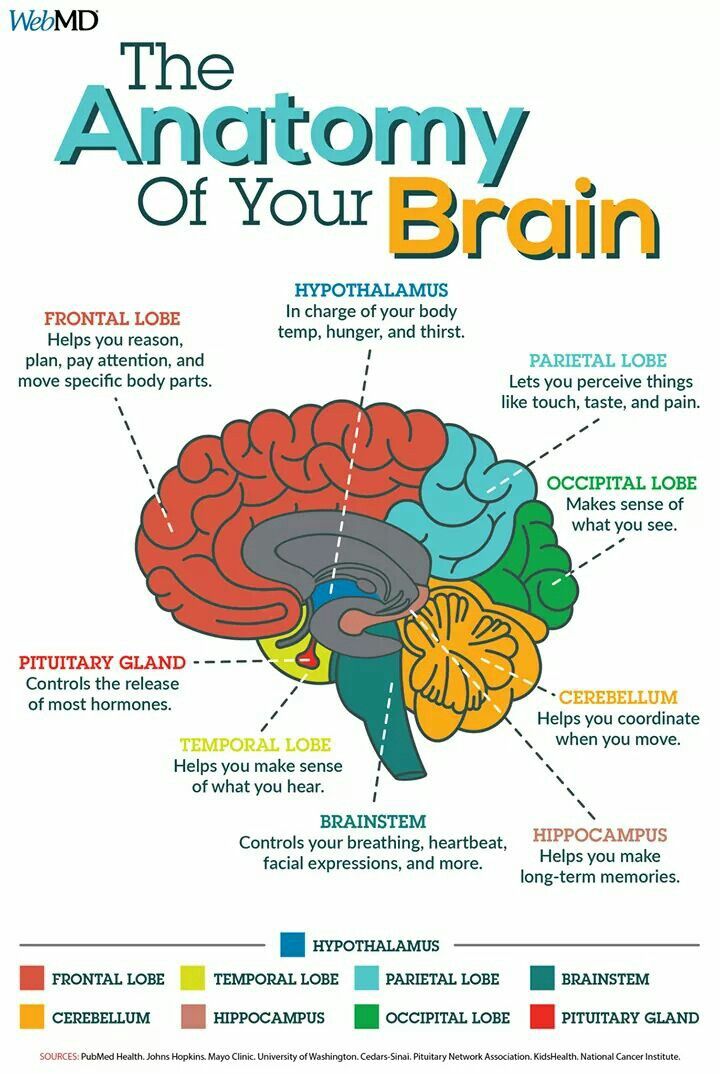
We do know that each of these medications affect a chemical in the brain called serotonin. Serotonin is used by the brain as a messenger. If your brain does not have enough serotonin, then your the nerves in your brain might not be communicating right. Adding these medications to your body can help boost your serotonin and get your brain back on track.
Are There Side Effects?- Yes.
 Most patients will experience one or more side effects from all of the medications listed above.
Most patients will experience one or more side effects from all of the medications listed above. - The patient and doctor must weigh the benefits of the drug against the side effects.
- It is important for the patient to be open about problems that may be caused by the medication. Sometimes an adjustment in dose or a switch in the time of day it is taken is all that is needed.
Who Should Not Take These Medications?
- Women who are pregnant or are breastfeeding should weigh the decision to take these drugs with their doctor. If severe OCD cannot be controlled any other way, research has indicated that these medications seem to be safe. Many pregnant women have taken them without difficulty. Some OCD patients choose to use exposure and response prevention (ERP) to minimize medication use during the first or last trimester of pregnancy. Click here to read more about the benefits and risks of using SRIs during pregancy and/or while breastfeeding.
- Very elderly patients should avoid Anafranil as the first drug tried, since it has side effects that can interfere with thinking and can cause or worsen confusion.
- Patients with heart problems should use special caution if taking Anafranil.
What if I cannot take even the smallest pill size of the medication?
Some patients are sensitive to these medications and can’t stand the effects that come with even the lowest dose. However, patients can start at very low doses (for example, 1-2 mg per day) and very slowly increase the dose. For most people, they will eventually be able to handle the medication at its normal dose.
Ask your doctor if you can try a lower dose by breaking pills in half or using a liquid form of medication to slowly increase your doses.
ALWAYS be sure to talk to your doctor before making any changes to the way you take your medications!
The following is one example as told by Dr. Michael Jenike:
“One woman, who was started on Prozac 20 mg/day, complained of bothersome side effects such as increased anxiety, shakiness, and terrible insomnia. She felt it made her OCD worse.
She had horrible side effects from even 12.5 mg of Anafranil, and later with low dosages of Paxil and Zoloft. She requested to start 1-2 mg/day of liquid Prozac, because she heard it was good from other patients that she met from a computer bulletin board. She felt no side effects, and over a period of a few weeks, she got up to 20 mg/day without the previous side effects that she had felt on this dose in the past. Under the supervision of her doctor, she continued to increase the Prozac to 60 mg/day over a couple more months. Her OCD gradually improved quite dramatically.”
Should I Take These Medications Only When I Am Feeling Stressed?
No. This is a common mistake. These medications are meant to be taken every day to keep your serotonin at a constant level. They are not taken like typical anti-anxiety meds, when you feel upset or anxious. It is best not to miss doses if possible. However, if you do miss a dose here or there, it is unlikely that any bad effect on OCD will occur.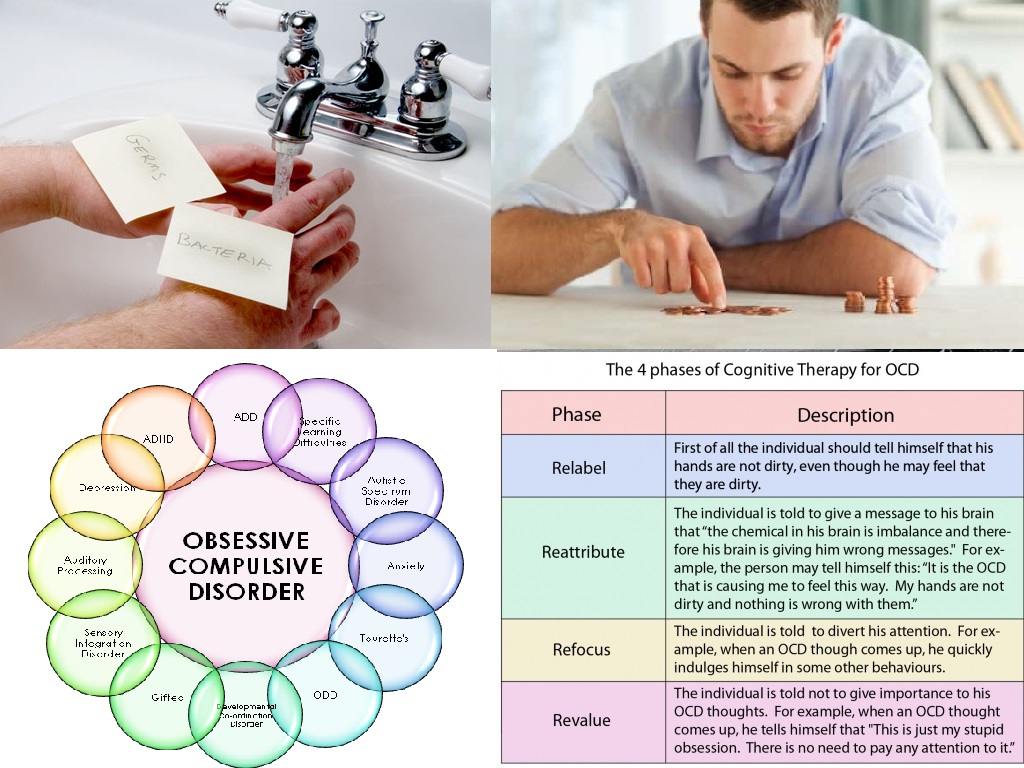 In fact, sometimes your doctor might tell you to skip doses to help manage troublesome side effects, like sexual problems.
In fact, sometimes your doctor might tell you to skip doses to help manage troublesome side effects, like sexual problems.
What Kind of Doctor Should I Look For to Prescribe These Medications?
Although any licensed physician can legally prescribe these drugs, it is probably best to deal directly with a board-certified psychiatrist who understands OCD. It is important to find a psychiatrist who has special knowledge about the use of drugs to treat mental health disorders. Click here to find a psychiatrist in your area. (Look for therapists with an MD or DO after their name.)
What If I am Afraid to Take My Medication Because I Have an Obsessional Fear About Drugs?
Usually with help from a doctor that you trust, your fears can be overcome. If you have fears about taking medication, ERP can be started first and part of the therapy can focus on these fears of medications.
How Long Does it Take for These Medications to Work?
It is important not to give up on a medication until you have been taking it as prescribed for 10 to 12 weeks. Many patients feel no positive effects for the first few weeks of treatment but then improve greatly.
Many patients feel no positive effects for the first few weeks of treatment but then improve greatly.
Will I Have to Take Medications Forever?
No one knows how long patients should take these medications once they have been effective. Some patients are able to stop their medications after a 6 to 12-month treatment period. It does appear that over half of OCD patients (and maybe many more) will need to be on at least a low dose of medication for years, perhaps even for life. It seems likely that the risk of relapse is lower if patients learn to use behavior therapy techniques while they are doing well on medications. And if medication is tapered slowly (even over several months), the ERP treatment may enable patients to control any symptoms that return when they stop taking the medication.
After medications are stopped, symptoms do not return immediately; they may start to return within a few weeks to a few months. If OCD symptoms return after a medication is stopped, most patients will have a good response if the medication is restarted.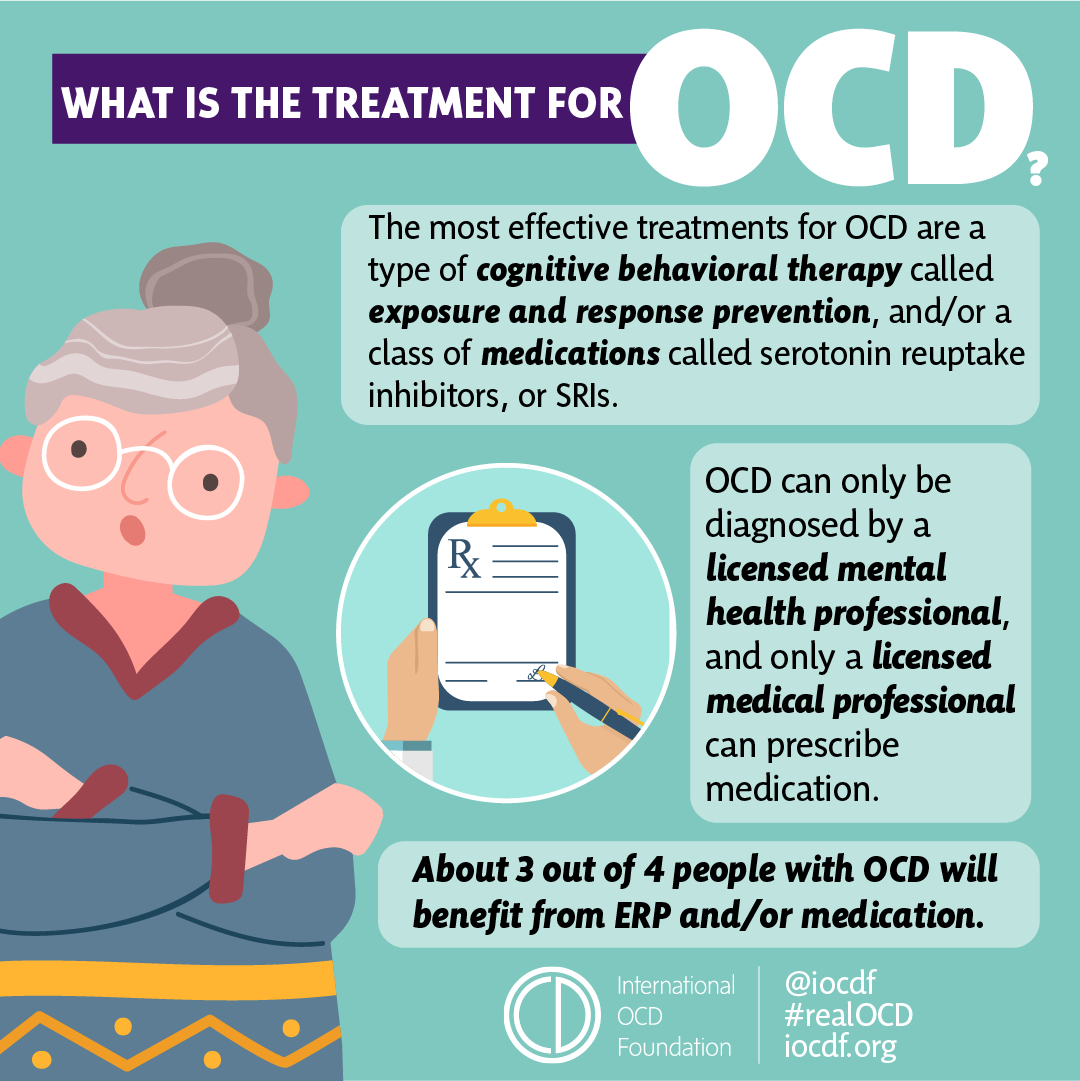
Can I Drink Alcohol While on These Medications?
Many patients drink alcohol while on these medications and handle it well, but be sure to ask your doctor or pharmacist if it is safe. It is important to keep in mind that alcohol may have a greater effect on individuals who are taking these medications; one drink could affect an individual as if it were two drinks. Also, alcohol may limit some of the medications’ benefits, so it may be wise to try not to drink alcohol during the first couple of months after starting any new medication.
Do I Need Other Treatments Too?
Most psychiatrists and therapists believe that combining a type of Cognitive Behavior Therapy (CBT), specifically Exposure and Response Prevention (ERP), and medication is the most effective approach.
What if I Can’t Afford My Medication?
Drug companies give doctors free samples of some medications. Doctors give these samples to patients who cannot afford the cost of the medications.
Most drug companies also have programs that help patients get these and other medications free or at a reduced cost. For more information, visit: www.pparx.org or call 1-888-477-2669.
By Michael Jenike, MD
Chair, International OCD Foundation’s Scientific Advisory Board
Harvard Medical School
* The FDA has issued some warnings on the use of this medication in higher doses. Please check with your physician.
Obsessive Compulsive Disorder Treatment
Great Thought is an obsessive compulsive disorder treatment program. We will relieve you of obsessive thoughts, movements and rituals. Let's get back to life!
Symptoms of obsessive-compulsive disorder
- Frightening images and drives
- Compulsive acts (rituals)
- Intrusive check of one's own actions
- Fear of trouble, pollution or infection
- Inexplicable desire to count something
- Excessive organization and pedantry
- Perfectionism in relationships, work and even leisure
- "Stuck", "looping" on one's thoughts
You feel that over time your mood becomes worse: apathy, depression, obsessions increase, and rituals begin to fill all your free time or harm your physical health.
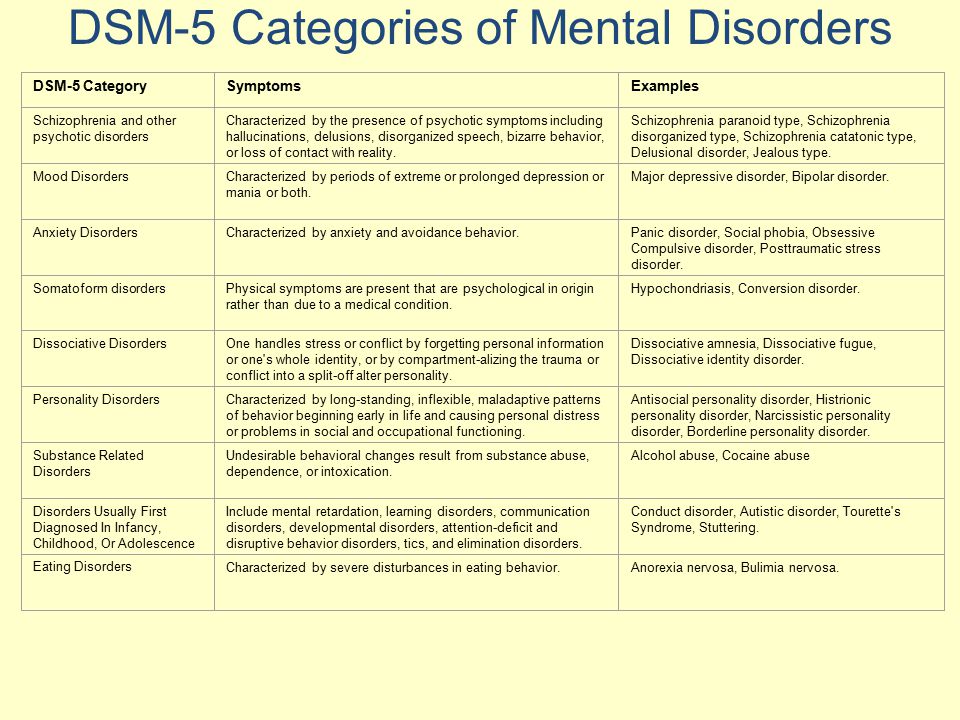
You may have had more than one meeting with psychologists, psychotherapists and psychiatrists. You are not given the "scary" psychiatric diagnoses of Schizophrenia or Bipolar Disorder, but are prescribed medication and psychotherapy nonetheless. However, such treatment cannot be called effective - the symptoms persist and only aggressive pharmacotherapy temporarily reduces anxiety. nine0003
What is obsessive-compulsive disorder?
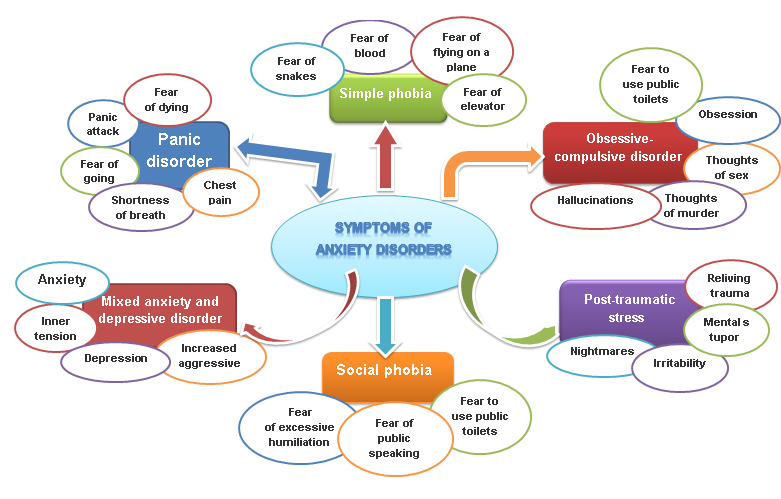
Obsessive-compulsive disorder is a syndrome characterized by the presence of obsessive thoughts (obsessions) to which a person reacts with certain actions (compulsions). The causes of the disorder are rarely superficial. The syndrome is also accompanied by the development of obsessive memories and various pathological phobias. May be chronic, episodic or progressive.
Obsession - obsessive thought, persistent desire for something, uncontrollable and accompanied by anxiety and intense anxiety. In an attempt to cope with such thoughts, a person resorts to committing compulsions. nine0003
nine0003
Compulsion - an irresistible need to perform certain actions (rituals), which can be assessed by the person himself as irrational or meaningless, and the internal need to perform them is forced and is the result of obsessive ideas.
Common examples of OCD manifestations
- An exaggerated sense of danger. Fear of the materiality of thoughts:
- "now I will lose control and hurt my loved ones"
- "something terrible is about to happen, I can feel it"
- "I shouldn't think like that, all this will come true because of me"
- Pathological fear of pollution. Thirst for Purity
- Excessive perfectionism, exaggerated responsibility - "everything must be done perfectly", "everything depends on me, mistakes are unacceptable"
How does this painful algorithm work?
Most people have unwanted or obsessive thoughts quite often, but all sufferers of the disorder greatly exaggerate their importance. Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer. nine0003
Fear of one's own thoughts leads to attempts to neutralize the negative feelings that arise from obsessions, for example by avoiding thought-provoking situations or by engaging in "rituals" of excessive self-cleansing or prayer. nine0003
As we noted earlier, repetitive avoidance behavior can "get stuck", "loop", that is, have a tendency to repeat. The cause of obsessive-compulsive disorder is the interpretation of intrusive thoughts as catastrophic and true.
If you periodically experience over the years:
- Constant or fluctuating anxiety
- The need to perform certain ritualized actions nine0007 A persistent decline in the quality of life due to the need to avoid certain thoughts and actions, places and events
And you are also persecuted:
- Significant problems in studies and career
- Failure to establish a serious relationship
- Constant criticism and pressure from relatives
- Many senseless activities
- Excessive involvement in computer games and the Internet, alcohol
- Loneliness and isolation
We strongly recommend that you do not delay seeking help and that you complete a remedial program.
Consultations and psychotherapeutic sessions according to the program are held several times a week, until the relief of severe symptoms, then the frequency of meetings with specialists is reduced to 2–3 per month. Count on the fact that in the end we will deal with your problem together.
Treatment of obsessive-compulsive disorder in Neuro-Psi
Every day, the specialists of the NEURO-PSI clinic analyze the world practice in the field of psychiatry and psychotherapy. The goal is the impartial selection and implementation of those methods of treatment and psychological assistance, the effectiveness of which has been convincingly proven in independent studies.
We are guided by the principles of evidence-based medicine and use as a basic method of treatment a psychotherapeutic paradigm, the effectiveness of which has been widely recognized by the professional community. nine0003
1. What is the essence of the obsessive-compulsive disorder treatment program
Since obsessive thoughts, rituals and conditions are only symptoms of mental dysfunction, the root cause must be treated in order to achieve a stable result. A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
A comprehensive work is carried out with the client, taking into account the main factors that create well-being.
The main emphasis is on teaching the client how to properly respond to his thoughts, emotions, inner feelings and interpretation of external events. nine0003
All types of psychotherapeutic and drug treatments serve the same goal: to achieve the best result in the shortest possible time. At the same time, by coordinating the efforts of specialists in various fields, the most complete coverage of all types of mental illnesses, disorders and disorders is possible.
2. What treatments are used
- Priority:
- Cognitive-Behavioral Therapy. nine0007 Schema Therapy.
- Reality Therapy.
- Choice Theory.
- Rational pharmacotherapy.
- Jacobson progressive muscle relaxation.
 nine0007 Traditional and modern gymnastic systems, relaxation techniques.
nine0007 Traditional and modern gymnastic systems, relaxation techniques.
- Work with bad habits.
- Diet correction.
- Professional and social adaptation.
3. How is the treatment under the program
Each treatment program at the NEURO-PSI clinic consists of four stages:
- diagnostics,
- work with disease symptoms,
- work with the causes of the disease,
- consolidation of the achieved results.
Work efficiency is increased by dividing the treatment process into a predetermined number of sessions, at convenient times and without hospitalization. This means that each program is adapted to the problem that the client has addressed. nine0003
The program method of treatment is predictable, time-limited, productive, and, most importantly, understandable for the client.
Of course, the treatment takes place in a comfortable mode without interruption from work, study or family. Specialists of various profiles will work with you (team method). This is necessary to minimize the risk of diagnostic errors that could lead to the adoption of a suboptimal treatment plan.
Improvements in well-being and mood (healing) occur in stages: after the decrease in emotional problems, bodily symptoms decrease. Working with the causes (etiology) of obsessive-compulsive disorder helps to avoid relapses in the future. nine0003
4. What are the results and prognosis?
Upon completion of the program, you get rid of obsessive thoughts and rituals, fear of pollution, unmotivated fears, panic attacks and multiple vegetative symptoms (sudden jumps in blood pressure, heart palpitations, dizziness, nausea).
According to statistics, the effectiveness of the methods used approaches 100% if all recommendations of specialists are followed.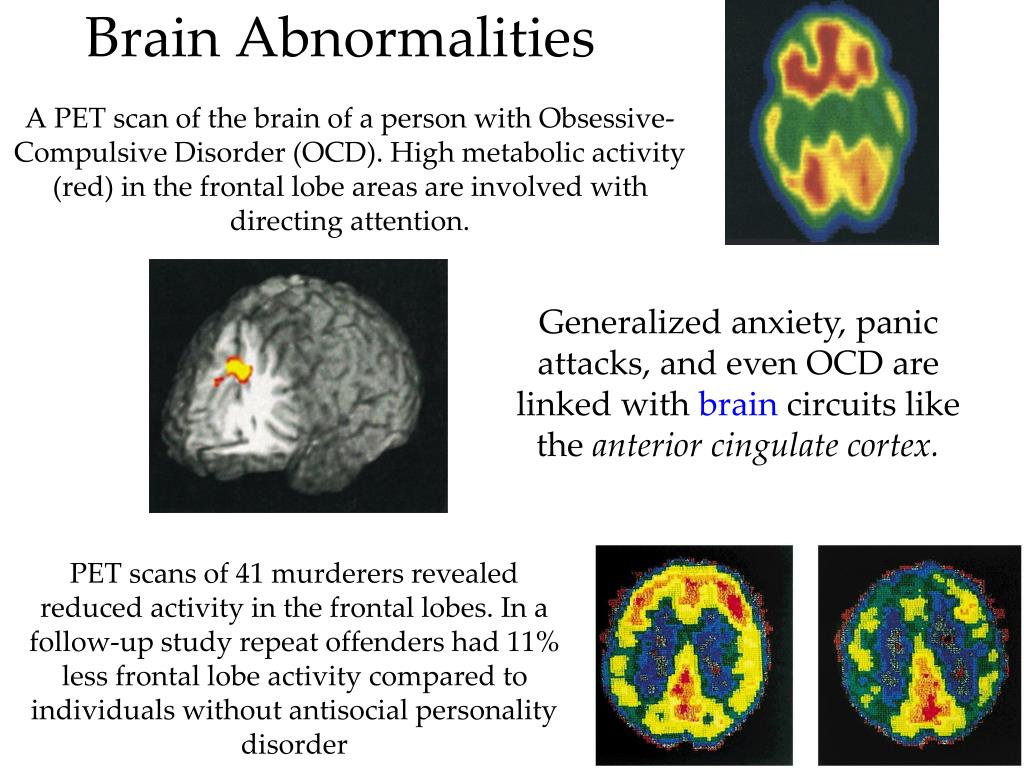
Skills you acquire during the program:
- self-control and self-regulation
- constructive analysis of the state of the body
- understanding one's own mental and emotional sphere
- ability to control one's attention
- ability to act consciously in stressful situations
Significantly improves the emotional and physical condition, gains self-confidence, in the future. Emotional stress is removed, sleep and appetite are restored. The efficiency is greatly increased. nine0003
5. Where to start taking the course
In order for you to know the treatment plan, we recommend signing up for a diagnostic (first) consultation.
Obsessive-compulsive disorder
A prominent role among mental illnesses is played by syndromes (complexes of symptoms), united in the group of obsessive-compulsive disorder (OCD), which received its name from the Latin terms obsessio and compulsio.
Obsession (lat. obsessio - taxation, siege, blockade). nine0003
obsessio - taxation, siege, blockade). nine0003
Compulsions (lat. compello - I force). 1. Obsessive drives, a kind of obsessive phenomena (obsessions). Characterized by irresistible attraction that arises contrary to the mind, will, feelings. Often they are unacceptable to the patient, contrary to his moral and ethical properties. Unlike impulsive drives, compulsions are not realized. These drives are recognized by the patient as wrong and painfully experienced by them, especially since their very appearance, due to its incomprehensibility, often gives rise to a feeling of fear in the patient 2. The term compulsions is also used in a broader sense to refer to any obsessions in the motor sphere, including obsessive rituals. nine0003
In domestic psychiatry, obsessive states were understood as psychopathological phenomena, characterized by the fact that phenomena of a certain content repeatedly appear in the mind of the patient, accompanied by a painful feeling of coercion [Zinoviev PM, 193I]. For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account.
For N.s. characteristic involuntary, even against the will, the emergence of obsessions with clear consciousness. Although the obsessions are alien, extraneous in relation to the patient's psyche, the patient is not able to get rid of them. They are closely related to the emotional sphere, accompanied by depressive reactions, anxiety. Being symptomatic, according to S.L. Sukhanov [1912], "parasitic", they do not affect the course of intellectual activity in general, remain alien to thinking, do not lead to a decrease in its level, although they worsen the efficiency and productivity of the patient's mental activity. Throughout the course of the disease, a critical attitude is maintained towards obsessions. N.s. conditionally divided into obsessions in the intellectual-affective (phobia) and motor (compulsions) spheres, but most often several of their types are combined in the structure of the disease of obsessions. The isolation of obsessions that are abstract, affectively indifferent, indifferent in their content, for example, arrhythmomania, is rarely justified; An analysis of the psychogenesis of a neurosis often makes it possible to see a pronounced affective (depressive) background at the basis of the obsessive account.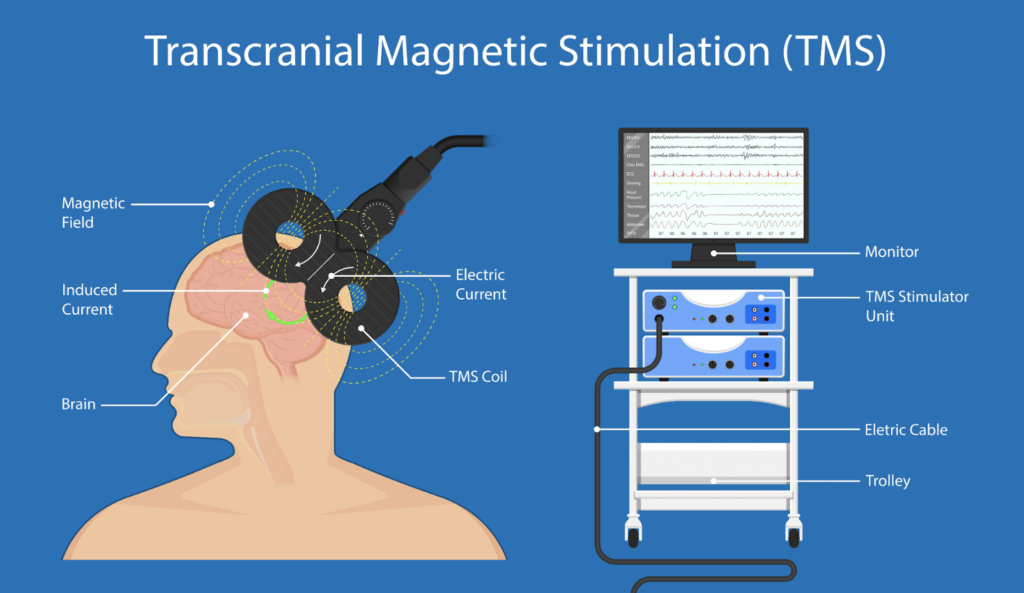 Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A.
Along with elementary obsessions, the connection of which with psychogeny is obvious, there are “cryptogenic” ones, when the cause of painful experiences is hidden [Svyadoshch L.M., 1959]. N.s. are observed mainly in individuals with a psychasthenic character. This is where apprehensions are especially characteristic. In addition, N.S. occur within the framework of neurosis-like states with sluggish schizophrenia, endogenous depressions, epilepsy, the consequences of a traumatic brain injury, somatic diseases, mainly hypochondria-phobic or nosophobic syndrome. Some researchers distinguish the so-called. "Neurosis of obsessive states", which is characterized by the predominance of obsessive states in the clinical picture - memories that reproduce a psychogenic traumatic situation, thoughts, fears, actions. In genesis play a role: mental trauma; conditioned reflex stimuli that have become pathogenic due to their coincidence with others that previously caused a feeling of fear; situations that have become psychogenic due to the confrontation of opposing tendencies [Svyadoshch A. M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
M., 1982]. It should be noted that these same authors emphasize that N.s.c. occurs with various character traits, but most often in psychasthenic personalities.
Currently, almost all obsessive-compulsive disorders are united in the International Classification of Diseases under the concept of "obsessive-compulsive disorder".
OKR concepts have undergone a fundamental reassessment over the past 15 years. During this time, the clinical and epidemiological significance of OCD has been completely revised. If it was previously thought that this is a rare condition observed in a small number of people, now it is known that OCD is common and causes a high percentage of morbidity, which requires the urgent attention of psychiatrists around the world. Parallel to this, our understanding of the etiology of OCD has broadened: the vaguely formulated psychoanalytic definition of the past two decades has been replaced by a neurochemical paradigm that explores the neurotransmitter disorders that underlie OCD. And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide. nine0003
And most importantly, pharmacological interventions specifically targeting serotonergic neurotransmission have revolutionized the prospects for recovery for millions of OCD patients worldwide. nine0003
The discovery that intense serotonin reuptake inhibition (SSRI) was the key to effective treatment for OCD was the first step in a revolution and spurred clinical research that showed the efficacy of such selective inhibitors.
As described in ICD-10, the main features of OCD are repetitive intrusive (obsessive) thoughts and compulsive actions (rituals).
In a broad sense, the core of OCD is the syndrome of obsession, which is a condition with a predominance in the clinical picture of feelings, thoughts, fears, memories that arise in addition to the desire of patients, but with awareness of their pain and a critical attitude towards them. Despite the understanding of the unnaturalness, illogicality of obsessions and states, patients are powerless in their attempts to overcome them. Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety. nine0003
Obsessional impulses or ideas are recognized as alien to the personality, but as if coming from within. Obsessions can be the performance of rituals designed to alleviate anxiety, such as washing hands to combat "pollution" and to prevent "infection". Attempts to drive away unwelcome thoughts or urges can lead to severe internal struggle, accompanied by intense anxiety. nine0003
Obsessions in the ICD-10 are included in the group of neurotic disorders.
The prevalence of OCD in the population is quite high. According to some data, it is determined by an indicator of 1.5% (meaning "fresh" cases of diseases) or 2-3%, if episodes of exacerbations observed throughout life are taken into account. Those suffering from obsessive-compulsive disorder make up 1% of all patients receiving treatment in psychiatric institutions. It is believed that men and women are affected approximately equally. nine0003
CLINICAL PICTURE
The problem of obsessive-compulsive disorders attracted the attention of clinicians already at the beginning of the 17th century. They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years.
They were first described by Platter in 1617. In 1621 E. Barton described an obsessive fear of death. Mentions of obsessions are found in the writings of F. Pinel (1829). I. Balinsky proposed the term "obsessive ideas", which took root in Russian psychiatric literature. In 1871, Westphal coined the term "agoraphobia" to refer to the fear of being in public places. M. Legrand de Sol [1875], analyzing the features of the dynamics of OCD in the form of "insanity of doubt with delusions of touch, points to a gradually becoming more complicated clinical picture - obsessive doubts are replaced by ridiculous fears of" touch "to surrounding objects, motor rituals join, the fulfillment of which is subject to the whole life sick. However, only at the turn of the XIX-XX centuries. researchers were able to more or less clearly describe the clinical picture and give syndromic characteristics of obsessive-compulsive disorders. The onset of the disease usually occurs in adolescence and adolescence. The maximum of clinically defined manifestations of obsessive-compulsive disorder is observed in the age range of 10-25 years. nine0003
nine0003
Main clinical manifestations of OCD:
Obsessional thoughts - painful, arising against the will, but recognized by the patient as their own, ideas, beliefs, images, which in a stereotyped form forcibly invade the patient's consciousness and which he tries to resist in some way. It is this combination of an inner sense of compulsive urge and efforts to resist it that characterizes obsessional symptoms, but of the two, the degree of effort exerted is the more variable. Obsessive thoughts may take the form of single words, phrases, or lines of poetry; they are usually unpleasant to the patient and may be obscene, blasphemous, or even shocking. nine0003
Obsessional imagery is vivid scenes, often violent or disgusting, including, for example, sexual perversion.
Obsessional impulses are urges to do things that are usually destructive, dangerous or shameful; for example, jumping into the road in front of a moving car, injuring a child, or shouting obscene words while in society.
Obsessional rituals include both mental activities (eg, counting repeatedly in a particular way, or repeating certain words) and repetitive but meaningless acts (eg, washing hands twenty or more times a day). Some of them have an understandable connection with the obsessive thoughts that preceded them, for example, repeated washing of hands - with thoughts of infection. Other rituals (for example, regularly laying out clothes in some complex system before putting them on) do not have such a connection. Some patients feel an irresistible urge to repeat such actions a certain number of times; if that fails, they are forced to start all over again. Patients are invariably aware that their rituals are illogical and usually try to hide them. Some fear that such symptoms are a sign of the onset of insanity. Both obsessive thoughts and rituals inevitably lead to problems in daily activities. nine0003
Obsessive rumination (“mental chewing gum”) is an internal debate in which the arguments for and against even the simplest everyday actions are endlessly revised. Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”. nine0003
Some obsessive doubts relate to actions that may have been incorrectly performed or not completed, such as turning off the gas stove faucet or locking the door; others concern actions that could harm other people (for example, the possibility of driving past a cyclist in a car, knocking him down). Sometimes doubts are associated with a possible violation of religious prescriptions and rituals - “remorse of conscience”. nine0003
Compulsive actions - repetitive stereotypical actions, sometimes acquiring the character of protective rituals. The latter are aimed at preventing any objectively unlikely events that are dangerous for the patient or his relatives.
In addition to the above, in a number of obsessive-compulsive disorders, a number of well-defined symptom complexes stand out, and among them are obsessive doubts, contrasting obsessions, obsessive fears - phobias (from the Greek. phobos).
nine0002 Obsessive thoughts and compulsive rituals may intensify in certain situations; for example, obsessive thoughts about harming other people often become more persistent in the kitchen or some other place where knives are kept. Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently. nine0003
Since patients often avoid such situations, there may be a superficial resemblance to the characteristic avoidance pattern found in phobic anxiety disorder. Anxiety is an important component of obsessive-compulsive disorders. Some rituals reduce anxiety, while after others it increases. Obsessions often develop as part of depression. In some patients, this appears to be a psychologically understandable reaction to obsessive-compulsive symptoms, but in other patients, recurrent episodes of depressive mood occur independently. nine0003 Obsessions (obsessions) are divided into figurative or sensual, accompanied by the development of affect (often painful) and obsessions of affectively neutral content.
Sensual obsessions include obsessive doubts, memories, ideas, drives, actions, fears, an obsessive feeling of antipathy, an obsessive fear of habitual actions.
Obsessive doubts - intrusively arising contrary to logic and reason, uncertainty about the correctness of committed and committed actions. The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession. nine0003
The content of doubts is different: obsessive everyday fears (whether the door is locked, whether windows or water taps are closed tightly enough, whether gas and electricity are turned off), doubts related to official activities (whether this or that document is written correctly, whether the addresses on business papers are mixed up , whether inaccurate figures are indicated, whether orders are correctly formulated or executed), etc. Despite repeated verification of the committed action, doubts, as a rule, do not disappear, causing psychological discomfort in the person suffering from this kind of obsession. nine0003
Obsessive memories include persistent, irresistible painful memories of any sad, unpleasant or shameful events for the patient, accompanied by a sense of shame, remorse. They dominate the mind of the patient, despite the efforts and efforts not to think about them.
Obsessive impulses - urges to commit one or another tough or extremely dangerous action, accompanied by a feeling of horror, fear, confusion with the inability to get rid of it. The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented. nine0003
The patient is seized, for example, by the desire to throw himself under a passing train or push a loved one under it, to kill his wife or child in an extremely cruel way. At the same time, patients are painfully afraid that this or that action will be implemented. nine0003
Manifestations of obsessive ideas can be different. In some cases, this is a vivid "vision" of the results of obsessive drives, when patients imagine the result of a cruel act committed. In other cases, obsessive ideas, often referred to as mastering, appear in the form of implausible, sometimes absurd situations that patients take for real. An example of obsessive ideas is the patient's conviction that the buried relative was alive, and the patient painfully imagines and experiences the suffering of the deceased in the grave. At the height of obsessive ideas, the consciousness of their absurdity, implausibility disappears and, on the contrary, confidence in their reality appears. As a result, obsessions acquire the character of overvalued formations (dominant ideas that do not correspond to their true meaning), and sometimes delusions.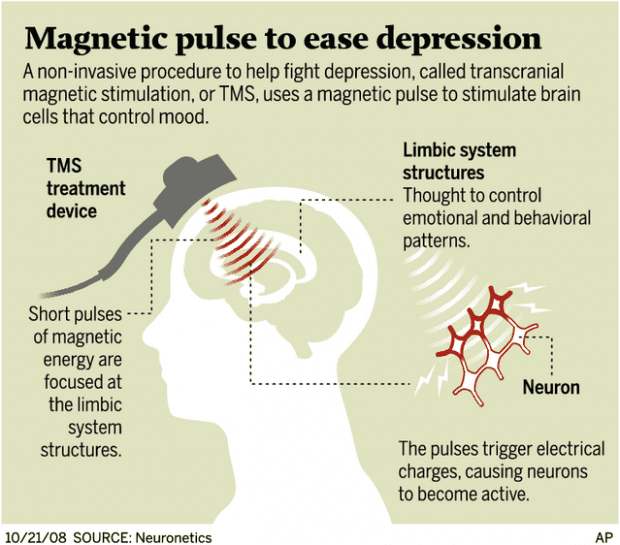 nine0003
nine0003
An obsessive feeling of antipathy (as well as obsessive blasphemous and blasphemous thoughts) - unjustified, driven away by the patient from himself antipathy towards a certain, often close person, cynical, unworthy thoughts and ideas in relation to respected people, in religious persons - in relation to saints or ministers churches.
Obsessive acts are acts done against the wishes of the sick, despite efforts made to restrain them. Some of the obsessive actions burden the patients until they are realized, others are not noticed by the patients themselves. Obsessive actions are painful for patients, especially in those cases when they become the object of attention of others. nine0003
Obsessive fears, or phobias, include an obsessive and senseless fear of heights, large streets, open or confined spaces, large crowds of people, the fear of sudden death, the fear of falling ill with one or another incurable disease. Some patients may develop a wide variety of phobias, sometimes acquiring the character of fear of everything (panphobia). And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
And finally, an obsessive fear of the emergence of fears (phobophobia) is possible.
Hypochondriacal phobias (nosophobia) - an obsessive fear of some serious illness. Most often, cardio-, stroke-, syphilo- and AIDS phobias are observed, as well as the fear of the development of malignant tumors. At the peak of anxiety, patients sometimes lose their critical attitude to their condition - they turn to doctors of the appropriate profile, require examination and treatment. The implementation of hypochondriacal phobias occurs both in connection with psycho- and somatogenic (general non-mental illnesses) provocations, and spontaneously. As a rule, hypochondriacal neurosis develops as a result, accompanied by frequent visits to doctors and unreasonable medication. nine0003
Specific (isolated) phobias - obsessive fears limited to a strictly defined situation - fear of heights, nausea, thunderstorms, pets, treatment at the dentist, etc. Since contact with situations that cause fear is accompanied by intense anxiety, the patients tend to avoid them.
Obsessive fears are often accompanied by the development of rituals - actions that have the meaning of "magic" spells that are performed, despite the critical attitude of the patient to obsession, in order to protect against one or another imaginary misfortune: before starting any important business, the patient must perform some that specific action to eliminate the possibility of failure. Rituals can, for example, be expressed in snapping fingers, playing a melody to the patient or repeating certain phrases, etc. In these cases, even relatives are not aware of the existence of such disorders. Rituals, combined with obsessions, are a fairly stable system that usually exists for many years and even decades. nine0003
Obsessions of affectively neutral content - obsessive sophistication, obsessive counting, recalling neutral events, terms, formulations, etc. Despite their neutral content, they burden the patient, interfere with his intellectual activity.
Contrasting obsessions ("aggressive obsessions") - blasphemous, blasphemous thoughts, fear of harming oneself and others. Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.
Psychopathological formations of this group refer mainly to figurative obsessions with pronounced affective saturation and ideas that take possession of the consciousness of patients. They are distinguished by a sense of alienation, the absolute lack of motivation of the content, as well as a close combination with obsessive drives and actions. Patients with contrasting obsessions and complain of an irresistible desire to add endings to the replicas they have just heard, giving an unpleasant or threatening meaning to what has been said, to repeat after those around them, but with a touch of irony or malice, phrases of religious content, to shout out cynical words that contradict their own attitudes and generally accepted morality. , they may experience fear of losing control of themselves and possibly committing dangerous or ridiculous actions, injuring themselves or their loved ones. In the latter cases, obsessions are often combined with object phobias (fear of sharp objects - knives, forks, axes, etc.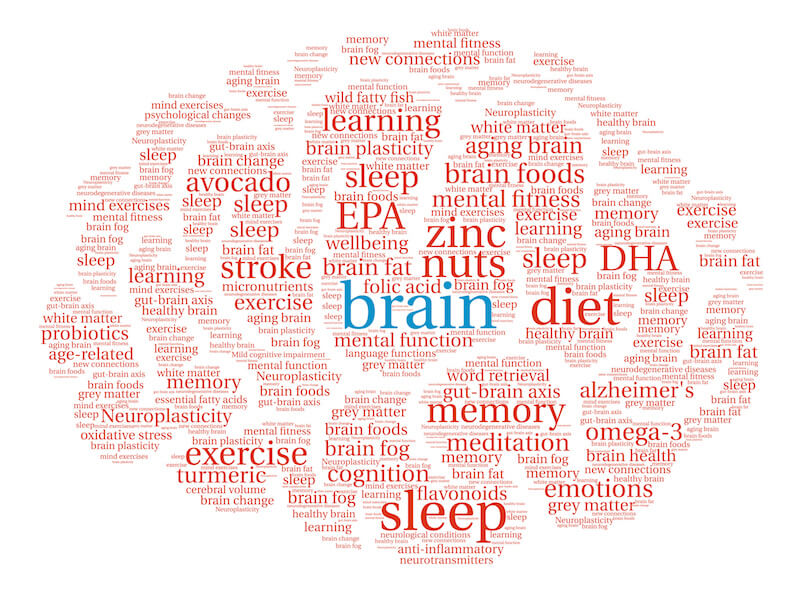 ). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals). nine0003
). The contrasting group also partially includes obsessions of sexual content (obsessions of the type of forbidden ideas about perverted sexual acts, the objects of which are children, representatives of the same sex, animals). nine0003
Obsessions of pollution (mysophobia). This group of obsessions includes both the fear of pollution (earth, dust, urine, feces and other impurities), as well as the fear of penetration into the body of harmful and toxic substances (cement, fertilizers, toxic waste), small objects (glass fragments, needles, specific types of dust), microorganisms. In some cases, the fear of contamination can be limited, remain at the preclinical level for many years, manifesting itself only in some features of personal hygiene (frequent change of linen, repeated washing of hands) or in housekeeping (thorough handling of food, daily washing of floors). , "taboo" on pets). This kind of monophobia does not significantly affect the quality of life and is evaluated by others as habits (exaggerated cleanliness, excessive disgust). Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.
Clinically manifested variants of mysophobia belong to the group of severe obsessions. In these cases, gradually becoming more complex protective rituals come to the fore: avoiding sources of pollution and touching "unclean" objects, processing things that could get dirty, a certain sequence in the use of detergents and towels, which allows you to maintain "sterility" in the bathroom. Stay outside the apartment is also furnished with a series of protective measures: going out into the street in special clothing that covers the body as much as possible, special processing of wearable items upon returning home. In the later stages of the disease, patients, avoiding pollution, not only do not go out, but do not even leave their own room. In order to avoid contacts and contacts that are dangerous in terms of contamination, patients do not allow even their closest relatives to come near them. Mysophobia is also related to the fear of contracting a disease, which does not belong to the categories of hypochondriacal phobias, since it is not determined by fears that a person suffering from OCD has a particular disease.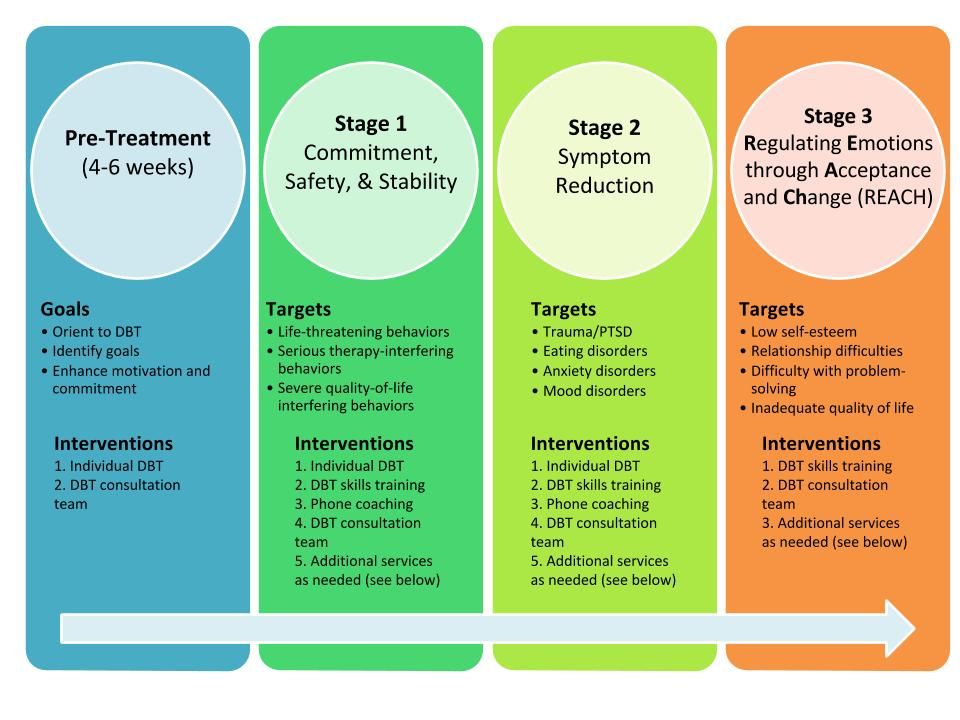 In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions. nine0003
In the foreground is the fear of a threat from the outside: the fear of pathogenic bacteria entering the body. Hence the development of appropriate protective actions. nine0003
A special place in the series of obsessions is occupied by obsessive actions in the form of isolated, monosymptomatic movement disorders. Among them, especially in childhood, tics predominate, which, unlike organically conditioned involuntary movements, are much more complex motor acts that have lost their original meaning. Tics sometimes give the impression of exaggerated physiological movements. This is a kind of caricature of certain motor acts, natural gestures. Patients suffering from tics can shake their heads (as if checking whether the hat fits well), make hand movements (as if discarding interfering hair), blink their eyes (as if getting rid of a mote). Along with obsessive tics, pathological habitual actions (lip biting, gnashing of teeth, spitting, etc.) are often observed, which differ from obsessive actions proper in the absence of a subjectively painful sense of persistence and experience them as alien, painful.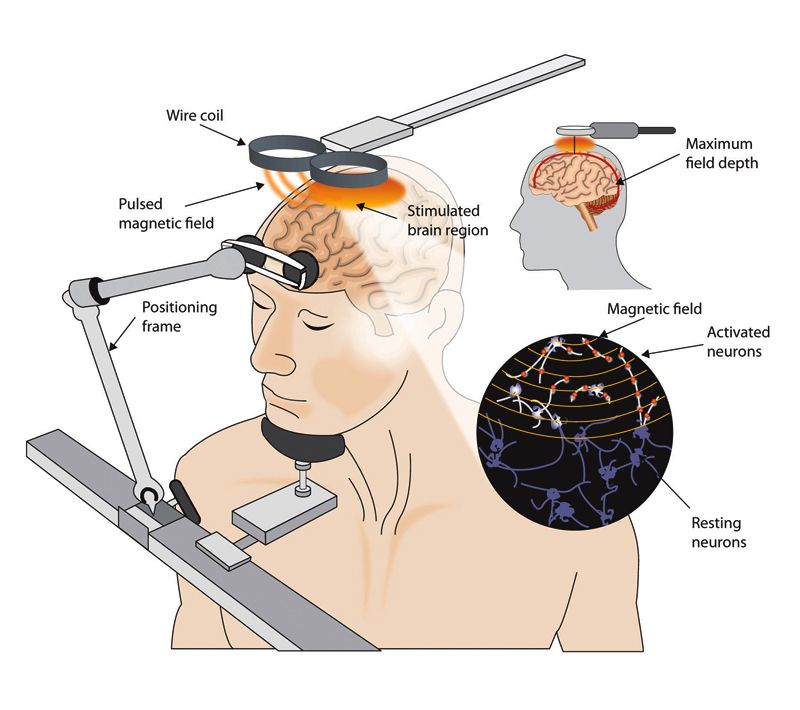 Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations. nine0003
Neurotic states characterized only by obsessive tics usually have a favorable prognosis. Appearing most often in preschool and primary school age, tics usually subside by the end of puberty. However, such disorders can also be more persistent, persist for many years and only partially change in manifestations. nine0003
The course of obsessive-compulsive disorder.
Unfortunately, chronization must be indicated as the most characteristic trend in the OCD dynamics. Cases of episodic manifestations of the disease and complete recovery are relatively rare. However, in many patients, especially with the development and preservation of one type of manifestation (agoraphobia, obsessive counting, ritual handwashing, etc.), a long-term stabilization of the condition is possible. In these cases, there is a gradual (usually in the second half of life) mitigation of psychopathological symptoms and social readaptation. For example, patients who experienced fear of traveling on certain types of transport, or public speaking, cease to feel flawed and work along with healthy people. In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation. nine0003
In mild forms of OCD, the disease usually proceeds favorably (on an outpatient basis). The reverse development of symptoms occurs after 1 year - 5 years from the moment of manifestation. nine0003
More severe and complex OCDs such as phobias of infection, pollution, sharp objects, contrasting performances, multiple rituals, on the other hand, may become persistent, resistant to treatment, or show a tendency to recur with disorders that persist despite active therapy. Further negative dynamics of these conditions indicates a gradual complication of the clinical picture of the disease as a whole.
DIFFERENTIAL DIAGNOSIS
It is important to distinguish OCD from other disorders that involve compulsions and rituals. In some cases, obsessive-compulsive disorder must be differentiated from schizophrenia, especially when the obsessive thoughts are unusual in content (eg, mixed sexual and blasphemous themes) or the rituals are exceptionally eccentric. The development of a sluggish schizophrenic process cannot be ruled out with the growth of ritual formations, their persistence, the emergence of antagonistic tendencies in mental activity (inconsistency of thinking and actions), and the uniformity of emotional manifestations. Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.
Prolonged obsessional states of a complex structure must be distinguished from the manifestations of paroxysmal schizophrenia. Unlike neurotic obsessive states, they are usually accompanied by a sharply increasing anxiety, a significant expansion and systematization of the circle of obsessive associations, which acquire the character of obsessions of "special significance": previously indifferent objects, events, random remarks of others remind patients of the content of phobias, offensive thoughts and thereby acquire in their view a special, menacing significance. In such cases, it is necessary to consult a psychiatrist in order to exclude schizophrenia. It can also be difficult to differentiate between OCD and conditions with a predominance of generalized disorders, known as Gilles de la Tourette's syndrome. Tics in such cases are localized in the face, neck, upper and lower extremities and are accompanied by grimaces, opening the mouth, sticking out the tongue, and intense gesticulation.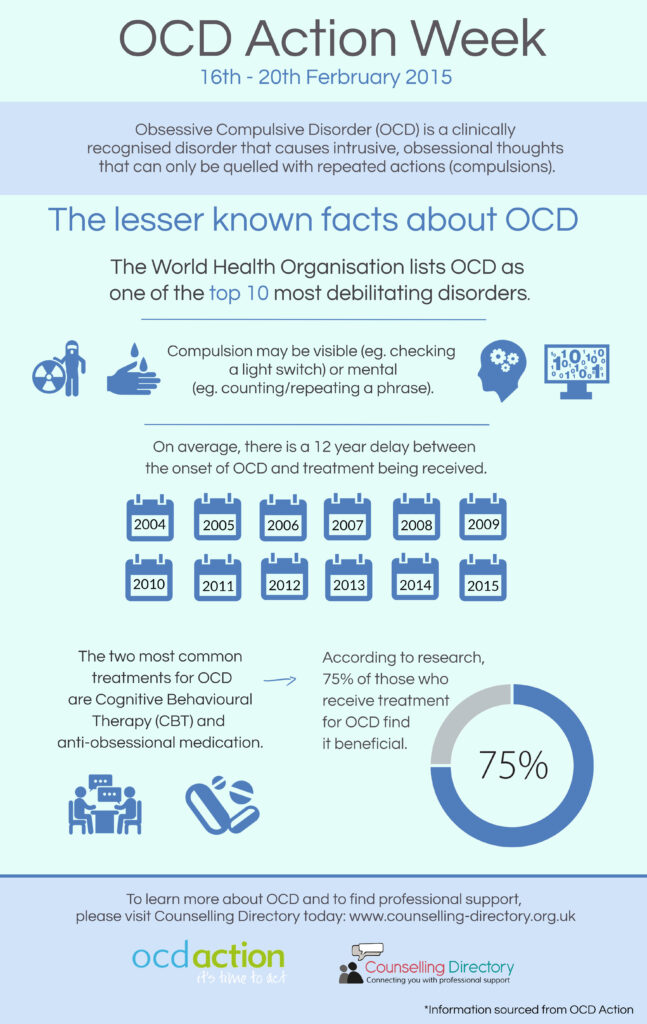 In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders. nine0003
In these cases, this syndrome can be excluded by the coarseness of movement disorders characteristic of it and more complex in structure and more severe mental disorders. nine0003
Genetic factors
Speaking about hereditary predisposition to OCD, it should be noted that obsessive-compulsive disorders are found in approximately 5-7% of parents of patients with such disorders. Although this figure is low, it is higher than in the general population. While the evidence for a hereditary predisposition to OCD is still uncertain, psychasthenic personality traits can be largely explained by genetic factors.
FORECAST
Approximately two-thirds of OCD patients improve within a year, more often by the end of this period. If the disease lasts more than a year, fluctuations are observed during its course - periods of exacerbations are interspersed with periods of improvement in health, lasting from several months to several years. The prognosis is worse if we are talking about a psychasthenic personality with severe symptoms of the disease, or if there are continuous stressful events in the patient's life. Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later. nine0003
Severe cases can be extremely persistent; for example, a study of hospitalized patients with OCD found that three-quarters of them remained symptom-free 13 to 20 years later. nine0003
TREATMENT: BASIC METHODS AND APPROACHES
Despite the fact that OCD is a complex group of symptom complexes, the principles of treatment for them are the same. The most reliable and effective method of treating OCD is considered to be drug therapy, during which a strictly individual approach to each patient should be manifested, taking into account the characteristics of the manifestation of OCD, age, gender, and the presence of other diseases. In this regard, we must warn patients and their relatives against self-treatment. If any disorders similar to mental ones appear, it is necessary, first of all, to contact the specialists of the psycho-neurological dispensary at the place of residence or other psychiatric medical institutions to establish the correct diagnosis and prescribe competent adequate treatment. At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation. nine0003
At the same time, it should be remembered that at present a visit to a psychiatrist does not threaten with any negative consequences - the infamous "accounting" was canceled more than 10 years ago and replaced by the concepts of consultative and medical care and dispensary observation. nine0003
When treating, it must be borne in mind that obsessive-compulsive disorders often have a fluctuating course with long periods of remission (improvement). The apparent suffering of the patient often seems to call for vigorous effective treatment, but the natural course of the condition must be kept in mind in order to avoid the typical error of over-intensive therapy. It is also important to consider that OCD is often accompanied by depression, the effective treatment of which often leads to an alleviation of obsessional symptoms. nine0003
The treatment of OCD begins with an explanation of the symptoms to the patient and, if necessary, with reassurance that they are the initial manifestation of insanity (a common concern for patients with obsessions). Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients. nine0003
Those suffering from certain obsessions often involve other family members in their rituals, so relatives need to treat the patient firmly, but sympathetically, mitigating the symptoms as much as possible, and not aggravating it by excessive indulgence in the sick fantasies of patients. nine0003
Drug therapy
The following therapeutic approaches exist for the currently identified types of OCD. Of the pharmacological drugs for OCD, serotonergic antidepressants, anxiolytics (mainly benzodiazepine), beta-blockers (to stop autonomic manifestations), MAO inhibitors (reversible) and triazole benzodiazepines (alprazolam) are most often used. Anxiolytic drugs provide some short-term relief of symptoms, but should not be given for more than a few weeks at a time. If anxiolytic treatment is required for more than one to two months, small doses of tricyclic antidepressants or small antipsychotics sometimes help. The main link in the treatment regimen for OCD, overlapping with negative symptoms or ritualized obsessions, are atypical antipsychotics - risperidone, olanzapine, quetiapine, in combination with either SSRI antidepressants or other antidepressants - moclobemide, tianeptine, or with high-potency benzodiazepine derivatives ( alprazolam, clonazepam, bromazepam). nine0003
nine0003
Any comorbid depressive disorder is treated with antidepressants at an adequate dose. There is evidence that one of the tricyclic antidepressants, clomipramine, has a specific effect on obsessive symptoms, but the results of a controlled clinical trial showed that the effect of this drug is insignificant and occurs only in patients with distinct depressive symptoms.
In cases where obsessive-phobic symptoms are observed within the framework of schizophrenia, intensive psychopharmacotherapy with proportional use of high doses of serotonergic antidepressants (fluoxetine, fluvoxamine, sertraline, paroxetine, citalopram) has the greatest effect. In some cases, it is advisable to connect traditional antipsychotics (small doses of haloperidol, trifluoperazine, fluanxol) and parenteral administration of benzodiazepine derivatives. nine0003
Psychotherapy
Behavioral psychotherapy
One of the main tasks of the specialist in the treatment of OCD is to establish fruitful cooperation with the patient.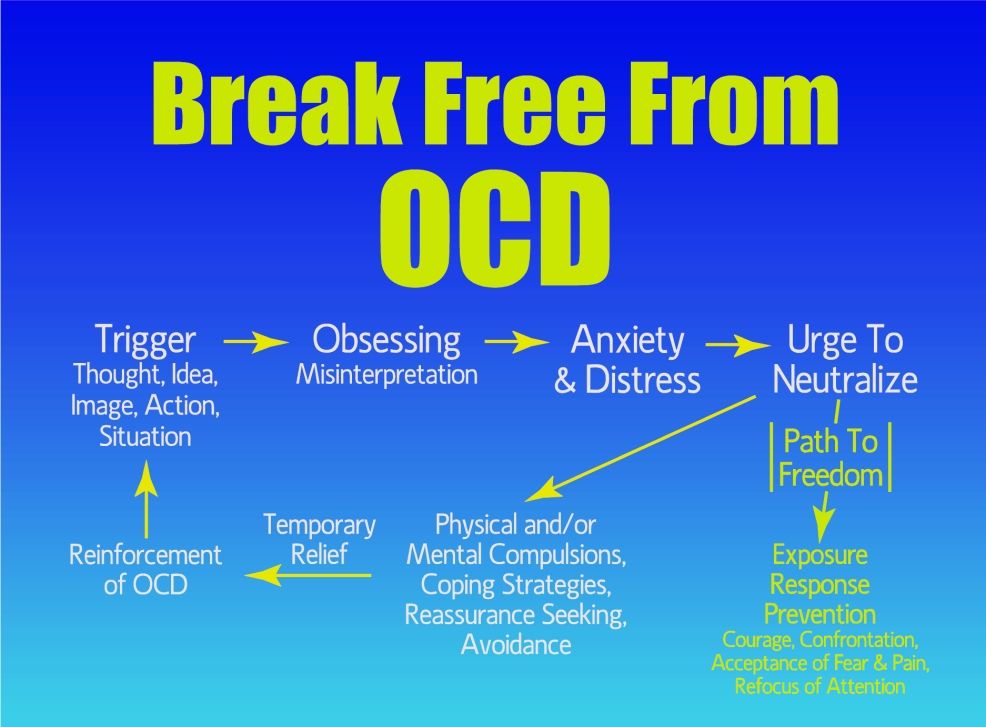 It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.
It is necessary to instill in the patient faith in the possibility of recovery, to overcome his prejudice against the "harm" caused by psychotropic drugs, to convey his conviction in the effectiveness of treatment, subject to the systematic observance of the prescribed prescriptions. The patient's faith in the possibility of healing must be supported in every possible way by the relatives of the OCD sufferer. If the patient has rituals, it must be remembered that improvement usually occurs when using a combination of the method of preventing a reaction with placing the patient in conditions that aggravate these rituals. Significant but not complete improvement can be expected in about two-thirds of patients with moderately heavy rituals. If, as a result of such treatment, the severity of rituals decreases, then, as a rule, the accompanying obsessive thoughts also recede. In panphobia, predominantly behavioral techniques are used to reduce sensitivity to phobic stimuli, supplemented by elements of emotionally supportive psychotherapy.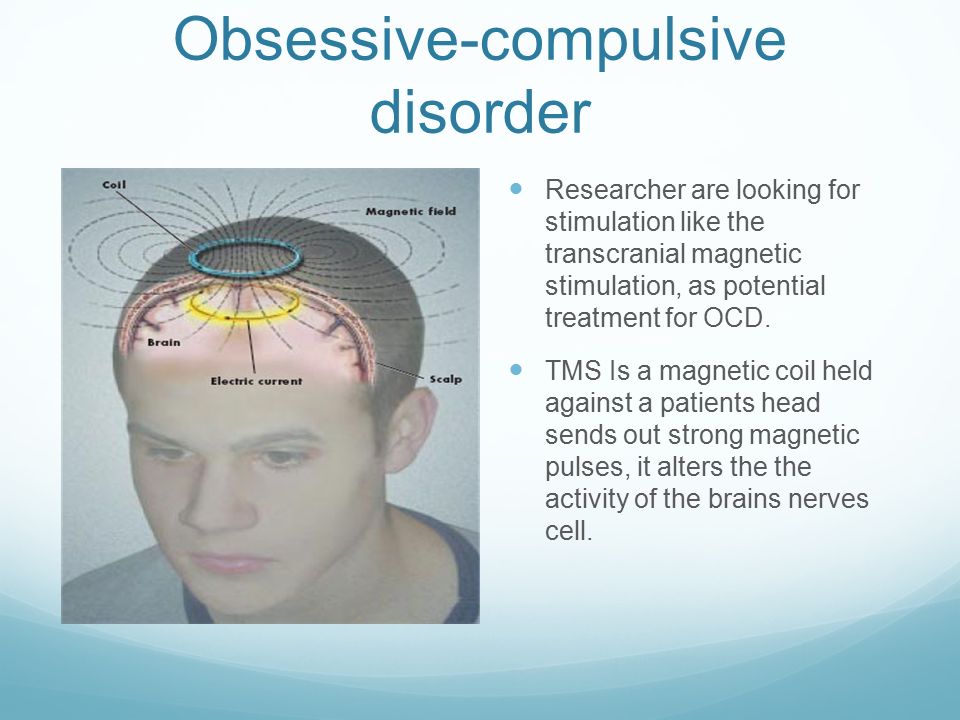 In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven. nine0003
In cases where ritualized phobias predominate, along with desensitization, behavioral training is actively used to help overcome avoidant behavior. Behavioral therapy is significantly less effective for obsessive thoughts that are not accompanied by rituals. Thought-stopping has been used by some experts for many years, but its specific effect has not been convincingly proven. nine0003
Social rehabilitation
We have already noted that obsessive-compulsive disorder has a fluctuating (fluctuating) course and over time the patient's condition may improve regardless of which particular methods of treatment were used. Until recovery, patients can benefit from supportive conversations that provide continued hope for recovery. Psychotherapy in the complex of treatment and rehabilitation measures for patients with OCD is aimed at both correcting avoidant behavior and reducing sensitivity to phobic situations (behavioral therapy), as well as family psychotherapy to correct behavioral disorders and improve family relationships.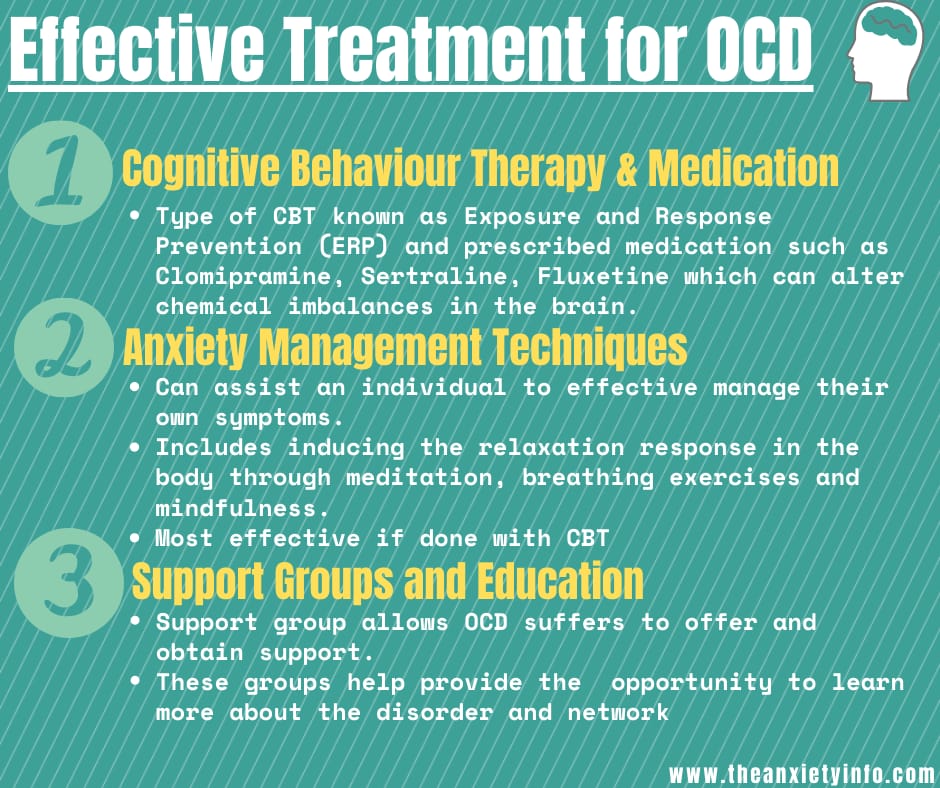 If marital problems aggravate the symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.
If marital problems aggravate the symptoms, joint interviews with the spouse are indicated. Patients with panphobia (at the stage of the active course of the disease), due to the intensity and pathological persistence of symptoms, need both medical and social and labor rehabilitation. In this regard, it is important to determine adequate terms of treatment - long-term (at least 2 months) therapy in a hospital with subsequent continuation of the course on an outpatient basis, as well as taking measures to restore social ties, professional skills, family relationships. Social rehabilitation is a set of programs for teaching OCD patients how to behave rationally both at home and in a hospital setting. Rehabilitation is aimed at teaching social skills to properly interact with other people, vocational training, as well as skills necessary in everyday life. Psychotherapy helps patients, especially those who experience a sense of their own inferiority, treat themselves better and correctly, master ways to solve everyday problems, and gain confidence in their strength.