Severe dissociation symptoms
Dissociative disorders - NHS
Dissociative disorders are a range of conditions that can cause physical and psychological problems.
Some dissociative disorders are very shortlived, perhaps following a traumatic life event, and resolve on their own over a matter of weeks or months. Others can last much longer.
Symptoms of a dissociative disorder
Symptoms of dissociative disorder can vary but may include:
- feeling disconnected from yourself and the world around you
- forgetting about certain time periods, events and personal information
- feeling uncertain about who you are
- having multiple distinct identities
- feeling little or no physical pain
Dissociation is a way the mind copes with too much stress.
Periods of dissociation can last for a relatively short time (hours or days) or for much longer (weeks or months).
It can sometimes last for years, but usually if a person has other dissociative disorders.
Many people with a dissociative disorder have had a traumatic event during childhood.
They may dissociate and avoid dealing with it as a way of coping with it.
Types of dissociative disorder
There are several different types of dissociative disorder.
The 3 main types are:
- depersonalisation-derealisation disorder
- dissociative amnesia
- dissociative identity disorder
Depersonalisation-derealisation disorder
Depersonalisation is where you have the feeling of being outside yourself and observing your actions, feelings or thoughts from a distance.
Derealisation is where you feel the world around is unreal. People and things around you may seem "lifeless" or "foggy".
You can have depersonalisation or derealisation, or both together. It may last only a few moments or come and go over many years.
Dissociative amnesia
Someone with dissociative amnesia will have periods where they cannot remember information about themselves or events in their past life.
They may also forget a learned talent or skill.
These gaps in memory are much more severe than normal forgetfulness and are not the result of another medical condition.
Some people with dissociative amnesia find themselves in a strange place without knowing how they got there.
They may have travelled there on purpose, or wandered in a confused state.
These blank episodes may last minutes, hours or days. In rare cases, they can last months or years.
In rare cases, they can last months or years.
Dissociative identity disorder
Dissociative identity disorder (DID) used to be called multiple personality disorder.
Someone diagnosed with DID may feel uncertain about their identity and who they are.
They may feel the presence of other identities, each with their own names, voices, personal histories and mannerisms.
The main symptoms of DID are:
- memory gaps about everyday events and personal information
- having several distinct identities
Associated conditions
Someone with a dissociative disorder may also have other mental health conditions, such as:
- medically unexplained symptoms
- post-traumatic stress disorder
- depression
- mood swings
- anxiety and panic attacks
- suicidal tendencies or self-harm
- phobias
- an eating disorder
- obsessive compulsive disorder
They may also have problems sleeping (insomnia).
Causes of dissociative disorder
The causes of dissociative disorders are not well understood.
They may be related to a previous traumatic experience, or a tendency to develop more physical than psychological symptoms when stressed or distressed.
Someone with a dissociative disorder may have experienced physical, sexual or emotional abuse during childhood.
Some people dissociate after experiencing war, kidnapping or even an invasive medical procedure.
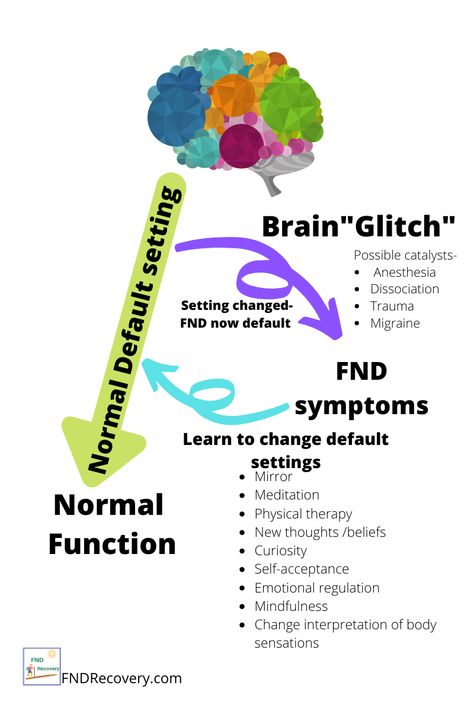
Switching off from reality is a normal defence mechanism that helps the person cope during a traumatic time.
It's a form of denial, as if "this is not happening to me".
It becomes a problem when the environment is no longer traumatic but the person still acts and lives as if it is, and has not dealt with or processed the event.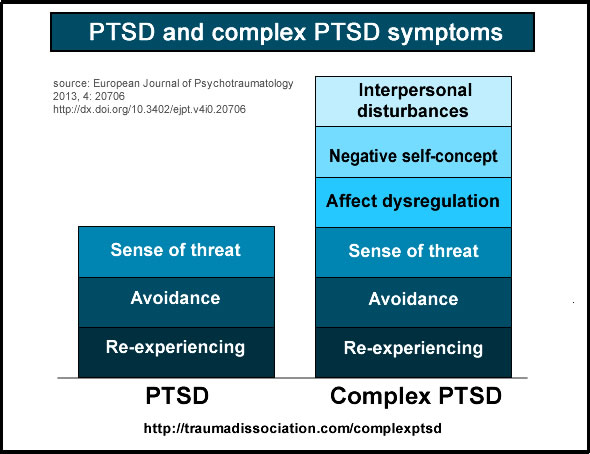
Diagnosing dissociative disorders
A GP may examine you and do some tests to check if another illness might be the cause of your symptoms.
They may also refer you to a mental health specialist for a full assessment.
Assessment
The specialist who carries out your assessment should have a good understanding of dissociative disorders.
The assessment may include:
- a physical examination to rule out things like a head injury or drug or alcohol misuse
- questions about your thoughts, feelings, behaviour and your symptoms
It's important to be honest about your symptoms and not to feel ashamed or embarrassed, so you can receive the help and support you need.
Treatments for dissociative disorders
Many people with a dissociative disorder make a full recovery with treatment and support.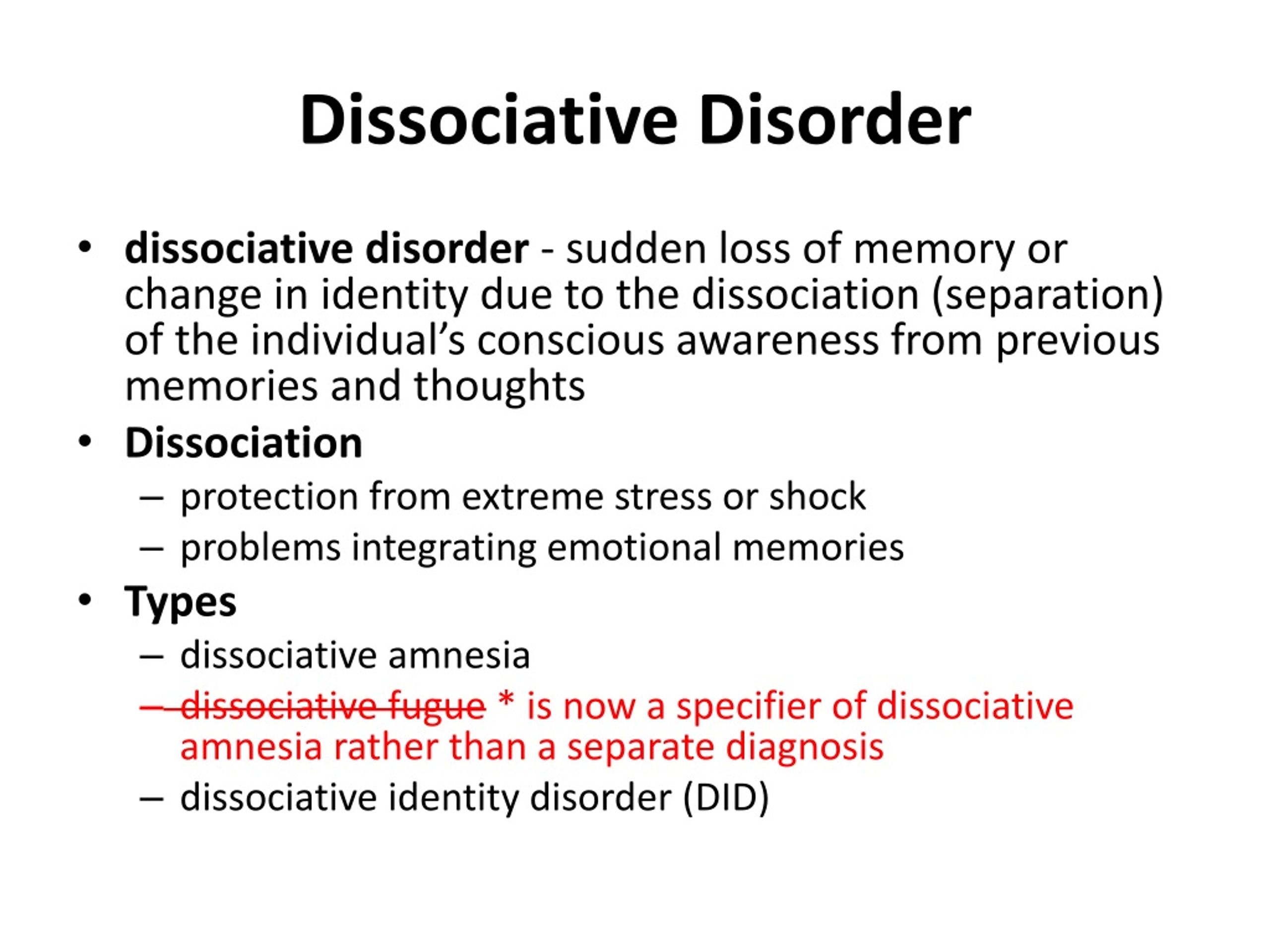
Talking therapies
Talking therapies are often recommended for dissociative disorders.
The aim of talking therapies such as counselling is to help you cope with the underlying cause of your symptoms, and to learn and practise techniques to manage the periods of feeling disconnected.
Medicines
There's no specific medicine to treat dissociation, but medicines like antidepressants may be prescribed to treat associated conditions like depression, anxiety and panic attacks.
If you're feeling suicidal
If you have thoughts about taking your life, it's important you ask someone for help.
It's probably difficult for you to see it at this time, but you're not alone or beyond help.
There are people you can talk to who want to help:
- speak to a friend, family member or someone you trust, as they may be able to help you calm down and find some breathing space
- call the Samaritans free 24-hour support service on 116 123
- go to your nearest A&E and tell the staff how you're feeling
- contact NHS 111
- make an urgent appointment to see a GP
Find out more about getting help if you're feeling suicidal
What to do if you're worried about someone
If you're worried that someone you know may be considering suicide, try to encourage them to talk about how they're feeling.
Listening is the best way to help. Try to avoid offering solutions and try not to judge.
If they have previously been diagnosed with a mental health condition, such as depression, you can speak to a member of their care team for help and advice.
Further help and support
If you have a dissociative disorder, getting help and support is an important part of the recovery process.
Talking to your partner, family and friends about how your past experiences have affected you can help you come to terms with what happened, as well as helping them understand how you feel.
Mental health charity Mind has more information on dissociative disorders and a list of support organisations.
Reading about other people with similar experiences may also help.
You can read people's personal accounts of living with a number of different mental health conditions on healthtalk. org.
org.
Dissociative disorders - Symptoms and causes
Overview
Dissociative disorders are mental disorders that involve experiencing a disconnection and lack of continuity between thoughts, memories, surroundings, actions and identity. People with dissociative disorders escape reality in ways that are involuntary and unhealthy and cause problems with functioning in everyday life.
Dissociative disorders usually develop as a reaction to trauma and help keep difficult memories at bay. Symptoms — ranging from amnesia to alternate identities — depend in part on the type of dissociative disorder you have. Times of stress can temporarily worsen symptoms, making them more obvious.
Treatment for dissociative disorders may include talk therapy (psychotherapy) and medication. Although treating dissociative disorders can be difficult, many people learn new ways of coping and lead healthy, productive lives.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms
Signs and symptoms depend on the type of dissociative disorders you have, but may include:
- Memory loss (amnesia) of certain time periods, events, people and personal information
- A sense of being detached from yourself and your emotions
- A perception of the people and things around you as distorted and unreal
- A blurred sense of identity
- Significant stress or problems in your relationships, work or other important areas of your life
- Inability to cope well with emotional or professional stress
- Mental health problems, such as depression, anxiety, and suicidal thoughts and behaviors
There are three major dissociative disorders defined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association:
- Dissociative amnesia.
 The main symptom is memory loss that's more severe than normal forgetfulness and that can't be explained by a medical condition. You can't recall information about yourself or events and people in your life, especially from a traumatic time. Dissociative amnesia can be specific to events in a certain time, such as intense combat, or more rarely, can involve complete loss of memory about yourself. It may sometimes involve travel or confused wandering away from your life (dissociative fugue). An episode of amnesia usually occurs suddenly and may last minutes, hours, or rarely, months or years.
The main symptom is memory loss that's more severe than normal forgetfulness and that can't be explained by a medical condition. You can't recall information about yourself or events and people in your life, especially from a traumatic time. Dissociative amnesia can be specific to events in a certain time, such as intense combat, or more rarely, can involve complete loss of memory about yourself. It may sometimes involve travel or confused wandering away from your life (dissociative fugue). An episode of amnesia usually occurs suddenly and may last minutes, hours, or rarely, months or years. - Dissociative identity disorder. Formerly known as multiple personality disorder, this disorder is characterized by "switching" to alternate identities. You may feel the presence of two or more people talking or living inside your head, and you may feel as though you're possessed by other identities. Each identity may have a unique name, personal history and characteristics, including obvious differences in voice, gender, mannerisms and even such physical qualities as the need for eyeglasses.
 There also are differences in how familiar each identity is with the others. People with dissociative identity disorder typically also have dissociative amnesia and often have dissociative fugue.
There also are differences in how familiar each identity is with the others. People with dissociative identity disorder typically also have dissociative amnesia and often have dissociative fugue. - Depersonalization-derealization disorder. This involves an ongoing or episodic sense of detachment or being outside yourself — observing your actions, feelings, thoughts and self from a distance as though watching a movie (depersonalization). Other people and things around you may feel detached and foggy or dreamlike, time may be slowed down or sped up, and the world may seem unreal (derealization). You may experience depersonalization, derealization or both. Symptoms, which can be profoundly distressing, may last only a few moments or come and go over many years.
When to see a doctor
Some people with dissociative disorders present in a crisis with traumatic flashbacks that are overwhelming or associated with unsafe behavior. People with these symptoms should be seen in an emergency room.
If you or a loved one has less urgent symptoms that may indicate a dissociative disorder, call your doctor.
Suicidal thoughts or behavior
If you have thoughts of hurting yourself or someone else, call 911 or your local emergency number immediately, go to an emergency room, or confide in a trusted relative or friend. Or contact a suicide hotline. In the U.S., call or text 988 to reach the 988 Suicide & Crisis Lifeline, available 24 hours a day, seven days a week. Or use the Lifeline Chat. Services are free and confidential.
Request an appointment
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health. Click here for an email preview.
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Causes
Dissociative disorders usually develop as a way to cope with trauma. The disorders most often form in children subjected to long-term physical, sexual or emotional abuse or, less often, a home environment that's frightening or highly unpredictable. The stress of war or natural disasters also can bring on dissociative disorders.
Personal identity is still forming during childhood. So a child is more able than an adult to step outside of himself or herself and observe trauma as though it's happening to a different person. A child who learns to dissociate in order to endure a traumatic experience may use this coping mechanism in response to stressful situations throughout life.
A child who learns to dissociate in order to endure a traumatic experience may use this coping mechanism in response to stressful situations throughout life.
Risk factors
People who experience long-term physical, sexual or emotional abuse during childhood are at greatest risk of developing dissociative disorders.
Children and adults who experience other traumatic events, such as war, natural disasters, kidnapping, torture, or extended, traumatic, early-life medical procedures, also may develop these conditions.
Complications
People with dissociative disorders are at increased risk of complications and associated disorders, such as:
- Self-harm or mutilation
- Suicidal thoughts and behavior
- Sexual dysfunction
- Alcoholism and drug use disorders
- Depression and anxiety disorders
- Post-traumatic stress disorder
- Personality disorders
- Sleep disorders, including nightmares, insomnia and sleepwalking
- Eating disorders
- Physical symptoms such as lightheadedness or non-epileptic seizures
- Major difficulties in personal relationships and at work
Prevention
Children who are physically, emotionally or sexually abused are at increased risk of developing mental health disorders, such as dissociative disorders. If stress or other personal issues are affecting the way you treat your child, seek help.
If stress or other personal issues are affecting the way you treat your child, seek help.
- Talk to a trusted person such as a friend, your doctor or a leader in your faith community.
- Ask for help locating resources such as parenting support groups and family therapists.
- Look for churches and community education programs that offer parenting classes that also may help you learn a healthier parenting style.
If your child has been abused or has experienced another traumatic event, see a doctor immediately. Your doctor can refer you to a mental health professional who can help your child recover and adopt healthy coping skills.
By Mayo Clinic Staff
Related
Associated Procedures
Products & Services
Dissociative disorders - causes, symptoms, diagnosis and treatment
Dissociative disorders - mental disorders accompanied by unconscious disintegration of certain mental functions (memory, consciousness, sense of personal identity, etc. ). They are a protective reaction of the psyche to intolerable acute or chronic stress. They can be manifested by the loss of individual memories and one's own identity, a feeling of alienation of one's own body, or peculiar changes in consciousness. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. In the process of diagnosis, other diseases that can cause such disorders are carefully excluded. Treatment - psychotherapy, drug therapy.
). They are a protective reaction of the psyche to intolerable acute or chronic stress. They can be manifested by the loss of individual memories and one's own identity, a feeling of alienation of one's own body, or peculiar changes in consciousness. The diagnosis is exposed on the basis of the anamnesis and clinical manifestations. In the process of diagnosis, other diseases that can cause such disorders are carefully excluded. Treatment - psychotherapy, drug therapy.
General information
Dissociative disorders are a group of rather heterogeneous mental disorders characterized by unconscious alienation of some mental processes. For the first time the term "dissociation" was used by the French psychiatrist, psychologist and neurologist Pierre Janet. This phenomenon is mostly known to the general public from films about multiple personality disorders (The Color of the Night, Sybil) and dissociative fugues (The Long Kiss Goodnight), but in real life these disorders are less common than other types of dissociation: dissociative amnesia , depersonalization and dissociation in trance states.
Cases of mild dissociation are familiar to everyone. Such states include a “strange” perception of oneself and the world around after a sleepless night, meditation, “leaving” for an alternative fictional world or one’s own thoughts while reading an interesting book or a long bus ride, and other similar situations. In clinically significant dissociative disorders, the "gap" between various mental functions becomes more pronounced, certain mental processes become completely isolated. Most dissociative disorders occur once, are completely reversible, and end in recovery. Treatment is carried out by specialists in the field of psychiatry.
Dissociative disorders
Causes of dissociative disorders
An acute or chronic psychotraumatic situation becomes the direct cause of the development of a pathological condition. Dissociative disorders are often observed in circumstances associated with an immediate threat to the patient's life: natural and man-made disasters, car accidents, train wrecks, violence during criminal incidents, etc. which the patient forms an idea of his own personality, its integrity and significance.
which the patient forms an idea of his own personality, its integrity and significance.
Dissociative disorders can provoke the death of loved ones (along with the loss of a loved one, the patient also loses a part of himself - as a husband, father, wife, mother, etc.), breaks in significant relationships, dismissals, especially with uncertain or unfavorable prospects for further employment ( a blow to professional identification, a drop in personal value in society), bankruptcy, loss of one's own home, and other significant traumatic events. Sometimes, due to the discrepancy between the patient's personal value system and the value systems of other people, events that are not significant to others become the cause of the disorder.
There are three groups of factors that increase the risk of developing a dissociative disorder. The first is the individual characteristics of the patient, the tendency to easily enter into trance states. Usually this ability is detected in sensitive, impressionable people with a rich imagination. At the same time, the presence of normal adaptive mechanisms is important. If such a person lives in a supportive environment during childhood, he develops healthy ways of adapting to changing external conditions, and the likelihood of developing a dissociative disorder is reduced.
At the same time, the presence of normal adaptive mechanisms is important. If such a person lives in a supportive environment during childhood, he develops healthy ways of adapting to changing external conditions, and the likelihood of developing a dissociative disorder is reduced.
The second is unfavorable living conditions in childhood: early loss of a loved one, serious illness, physical and psychological violence in the family or at school, especially in case of emotional isolation, lack of support and understanding from adults. The third is a previous traumatic experience. Dissociative disorders are more likely to develop in people who have fought in the past or were in the territory of hostilities, were subjected to torture or prolonged forced suggestion, as victims of terrorists or members of a cult.
Classification of dissociative disorders
There are different approaches to the classification of dissociative disorders. Psychiatrists traditionally use the term to refer to three pathological conditions: dissociative fugue, dissociative amnesia, and dissociative identity disorder (multiple personality). The American Guidelines for the Diagnosis of Mental Disorders, along with the listed conditions, include depersonalization. The ICD-10 reflects seven dissociative states:
Psychiatrists traditionally use the term to refer to three pathological conditions: dissociative fugue, dissociative amnesia, and dissociative identity disorder (multiple personality). The American Guidelines for the Diagnosis of Mental Disorders, along with the listed conditions, include depersonalization. The ICD-10 reflects seven dissociative states:
- Dissociative Fugue
- Dissociative amnesia
- Dissociative movement and sensation disorders
- Dissociative stupor
- Dissociative convulsions
- Trance and possession.
Forms of dissociative disorders
Dissociative identity disorder
The cause of development is intense or prolonged psychotraumatic impact in childhood. The critical factors are: early attachment disorder (lack of contact with the mother before the age of 2 years), violence, abandonment and neglect of the child. Dissociative disorder is manifested by the presence of several personalities in one person. Personalities can be of different gender, age and nationality, each has its own history. The transition from one subpersonality to another is carried out suddenly, each subpersonality does not know about the existence of the others and has no idea what happened during its "absence".
Personalities can be of different gender, age and nationality, each has its own history. The transition from one subpersonality to another is carried out suddenly, each subpersonality does not know about the existence of the others and has no idea what happened during its "absence".
The main goal of the treatment of dissociative disorder is to bring together different personalities - this approach allows for the normal existence of the patient, his safety and integration into society. Various psychotherapeutic techniques are used, including cognitive psychotherapy, hypnosis, psychodynamic therapy, family therapy. With concomitant depressive disorders and severe anxiety, antidepressants are prescribed. Dissociative identity disorder requires long-term therapy. The literature describes cases of successful integration even with a large number of subpersonalities, however, much is determined by the age of the patient, his ability and willingness to endure the stress associated with the association of "alter ego", and other factors.
Dissociative amnesia
Dissociative amnesia is a fairly common disorder. Represents a partial or complete loss of memory for events that caused severe psychological stress. At the same time, the patient is conscious, recognizes amnesia, is oriented in his own personality and retains memories of other events. This form of dissociative disorder is more often detected in young women who have been injured during a natural disaster or who were in the area of military operations. Short-term episodes of dissociative amnesia often occur with the loss of loved ones and other tragic events.
Treatment - creating a favorable psychological atmosphere, psychotherapy, in some cases in combination with drug therapy. Lost memories can be restored using hypnosis, however, sometimes they can cause a deterioration in the condition of a patient with a dissociative disorder, so the decision to use this technique is made individually. To develop more adaptive ways of responding to traumatic situations, cognitive behavioral therapy and psychodynamic therapy are used; various types of creative psychotherapy are used to facilitate the patient's contact with his feelings and the safe expression of experiences.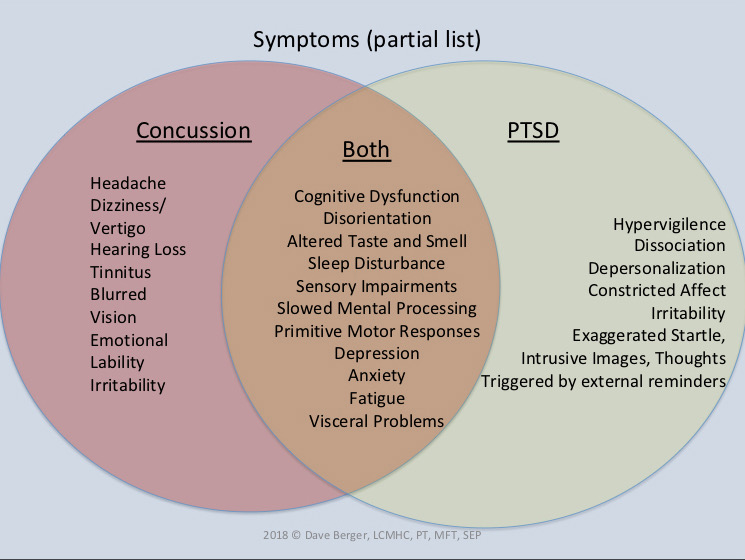 The prognosis is favorable, usually there is a complete recovery.
The prognosis is favorable, usually there is a complete recovery.
Dissociative fugue
Dissociative fugue is a dissociative disorder in which patients suddenly leave home with no memory of their former identity. Some patients are at a loss, others create a new personality, sometimes very believable. The emergence of a new personality is accompanied by a change in behavior. With a prolonged dissociative fugue, patients can get a job in another specialty and create new families. Subsequently, the old personality returns, and the patient, suffering from a dissociative disorder, finds himself in an unfamiliar place with a new life unknown to him. Memories of existence are lost during the fugue.
As a rule, psychiatrists and psychotherapists work with patients who have already experienced a return to their former personality, because during the fugue, patients are not bothered by anything, and they do not turn to specialists. Treatment of dissociative disorder - help in processing the traumatic situation that provoked the fugue. If the fugue is prolonged, assistance may be required to adjust to the old life, as many patients find it hard to bear the changes that have occurred during their absence. The prognosis is favorable, usually there is a complete recovery.
If the fugue is prolonged, assistance may be required to adjust to the old life, as many patients find it hard to bear the changes that have occurred during their absence. The prognosis is favorable, usually there is a complete recovery.
Depersonalization disorder
Depersonalization is a dissociative disorder, manifested by a feeling of alienation of one's own body or one's own mental processes. It can be periodic or constant, accompanied by the effects of distortion of space and time, the perception of oneself as a robot or as a person living in dreams. The patient does not seem to live, but observes his life from the outside, not being able to control it. Depersonalization is often combined with derealization - a feeling of unreality of the surrounding world.
Distinguish between depersonalization in various mental disorders (schizophrenia, depression, bipolar affective disorder, panic disorder) and depersonalization-derealization syndrome as an independent dissociative disorder caused by intolerable stress. The reason for the development of this syndrome can be natural disasters, accidents, violence, childhood abuse, etc. It has been established that all types of depersonalization are associated with an increased level of anxiety, therefore, tranquilizers and antidepressants are used in the treatment of this disorder. The prognosis for depersonalization-derealization syndrome is favorable, with symptomatic depersonalizations, the condition is determined by the course of the underlying disease.
The reason for the development of this syndrome can be natural disasters, accidents, violence, childhood abuse, etc. It has been established that all types of depersonalization are associated with an increased level of anxiety, therefore, tranquilizers and antidepressants are used in the treatment of this disorder. The prognosis for depersonalization-derealization syndrome is favorable, with symptomatic depersonalizations, the condition is determined by the course of the underlying disease.
Trance and possession
Trance and possession are dissociative disorders accompanied by a temporary change in consciousness, a decrease in the ability to be aware of one's own personality and ongoing events. Arise among mediums and ministers of some cults. In everyday life, it can be observed in drivers, pilots and representatives of other professions associated with prolonged monotonous stress, combined with high speeds and the monotony of visual sensations. Trance states can cause plane crashes and car accidents.
In trance dissociative disorders caused by religious and occult rituals, psychotherapeutic treatment (Gestalt therapy, psychoanalysis, rational psychotherapy) may be required while taking tranquilizers. In trances associated with the performance of professional duties, the main role is played by preventive measures: regular rest (if stopping is not possible - replacing the control of the vehicle with another driver or pilot), stopovers and short sleep.
Other dissociative disorders
Dissociative convulsions are pseudo-seizures that can quite accurately mimic seizures in epilepsy, but are not accompanied by complete loss of consciousness, involuntary urination and biting of the tongue. Dissociative disorders of movement and sensation are temporary loss of sensation or movement disorders. Dissociative stupor is manifested by temporary complete or almost complete immobility and lack of response to external stimuli while maintaining consciousness. Treatment for all of these dissociative disorders is psychotherapy, sometimes in combination with drug therapy.
Treatment for all of these dissociative disorders is psychotherapy, sometimes in combination with drug therapy.
Borderline personality disorder: what it is, symptoms and signs of BPD
Borderline personality disorder is characterized by emotional instability, impulsive behavior and low self-control. Forbes Life figured out what causes this disease, how to diagnose borderline personality disorder and how to help people who have experienced it
Mental personality disorders differ from other types of disorders in their intensity. They cannot be treated like an ordinary illness, as a temporary mental disorder, because personality disorders affect a set of personal characteristics formed in childhood. There are a number of problems with diagnosing such diseases: their symptoms are quite individual, although there are a number of common signs. For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
For borderline personality disorder (BPD), these may include difficulties with self-image, extreme mood swings, risky behavior, and self-harm. The good news is that personality disorders can still be managed—there is a cure.
Now officially: BPD is a diagnosis
Borderline personality disorder is one of ten types of personality disorders in modern psychotherapy, which is expressed in problems of awareness and formation of personal identity. Psychologist, Gestalt therapist Valentin Oskin notes that this mental illness is associated with strong, uncontrollable and often painful emotions that lead to a distorted sense of self and unstable interpersonal relationships.
People with BPD are vice versa solipsists: they are convinced of the inviolability of the surrounding world, but doubt the reality of their own existence - their image of the inner “I” is so mobile and unstable. In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
In addition to depersonalization, "borderguards" are characterized by impulsiveness, dependence on other people, unstable behavior, a tendency to a chaotic life, and even a need to harm themselves and injure themselves. "Border guards" are characterized by chronic suicidality: 75% of people with BPD try to commit suicide, of which about 10% die as a result of suicide. Moreover, a third of all completed suicides were committed by those suffering from borderline personality disorder.
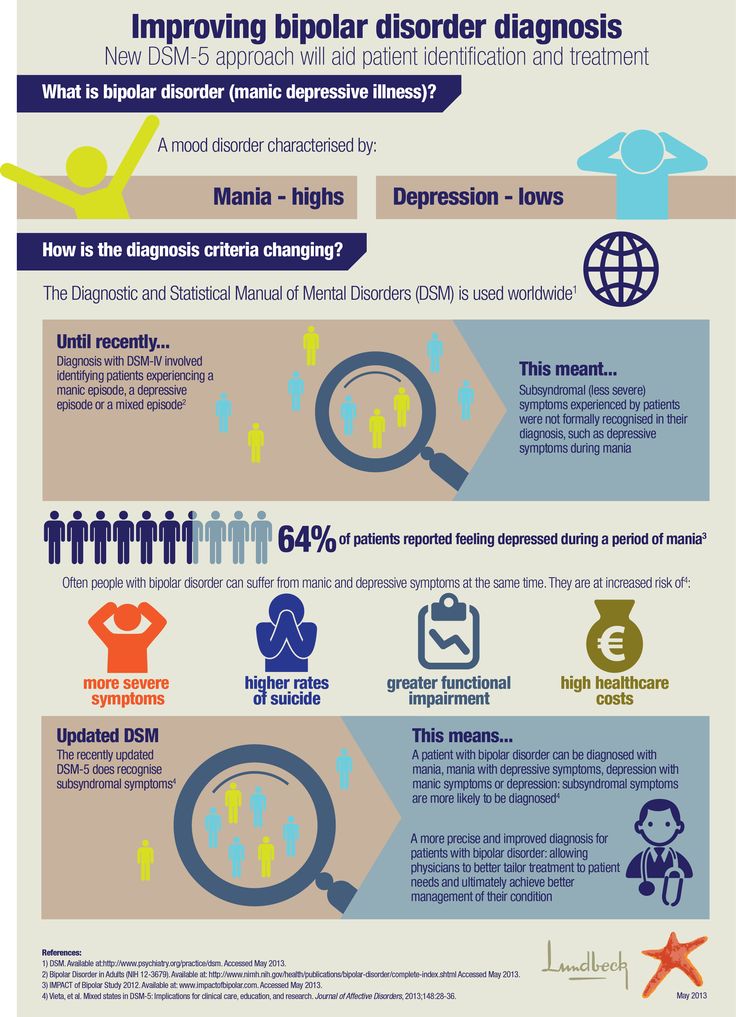
Despite the statistics, until 2022 the diagnosis of BPD in Russia could not be officially diagnosed - borderline personality disorder in psychiatry was defined as a disease only in foreign classifications of diseases. It was often called impulsive personality disorder or generally diagnosed as sluggish schizophrenia: the diseases are similar in symptoms, among the signs of BPD there are no hallucinations and delusions. BPD also resembles bipolar affective disorder (up to 40% of "border guards" get an erroneous diagnosis of bipolar disorder), only periods of depressive and elated mood are replaced with bipolar disorder less often. The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
The transition to the International Classification of Diseases of the 11th revision will finally allow doctors to make an accurate diagnosis for Russian citizens and prescribe the appropriate treatment.
Diagnosis is not a sentence, the boundary between the norm and pathology is very flexible: “Each of us has borderline responses. For some, they are deeply hidden and appear only in crises, traumas, stressful situations. And for some, life as such is stressful, and therefore the ways of responding turn into what psychologists could call the borderline organization of the personality,” notes Irina Mlodik, Candidate of Psychological Sciences, in the book “House of Cards. Psychotherapeutic assistance to clients with borderline disorders.
Related material
Ghost hints
Most people with BPD are unaware of their diagnosis and do not seek medical attention. And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
And it's not just that BPD in psychology does not have a clear definition. The disease does not allow you to objectively assess your mental state and understand that the indomitable monster inside is raging not because of the permanent retrograde Mercury and the fatal force of circumstances. The absence of obvious mental abnormalities like hallucinations makes it possible to attribute emotional behavior to character traits. Colleagues, friends and relatives often believe that behind the disgusting behavior of such a person is hysteria and selfishness. Therefore, systematic treatment of borderline personality disorder begins in most cases after a suicide attempt.
The most striking and obvious sign of borderline personality disorder is a craving for auto-aggression, or self-harm. This is not only the infliction of bodily harm (cuts, blows or burns), but also the intention to deprive oneself of sleep, nutrition. This practice is not necessarily a consequence of suicidal behavior: physical pain serves as a way to drown out inner pain, to switch attention from uncontrollable emotions to those that have become the result of an effort of will. The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
The problem is that self-harm is either carefully hidden by people with BPD because it is not normal in our culture, or they perceive it as controlled behavior (eg, exhausting workouts in the gym, striving to do work tasks in their free time).
Borderline personality disorder may be accompanied by alcohol, drug, gambling and a number of other diseases. “For example, depression, anxiety disorders, eating disorders are common in people with BPD. Often, a history of PTSD or CPTSD is found, ”notes Valentin Oskin. That is, constant panic attacks or overeating in the evenings can be a sign of more serious mental disorders than just a reaction to stress.
Mind, a British mental health resource, highlights the following symptoms that may indicate borderline personality disorder. If they last long enough and have a negative impact on your life, it makes sense to consult a psychotherapist or psychiatrist:
- Fear of being alone.
 You constantly worry about people leaving you and are ready to do everything to prevent this from happening.
You constantly worry about people leaving you and are ready to do everything to prevent this from happening. - Impulsivity and affectivity. You are overcome by strong emotions that last from several hours to several days and can change quickly (for example, from feelings of happiness and confidence to sudden depression and sadness). This is especially evident in a state of anger, which is difficult to control. In a state of severe stress, you may also experience paranoia or dissociation (as if everything is not happening to you, but to someone else).
- Depersonalization. There is no clear idea of who you really are: the sense of self and behavior changes radically depending on where and with whom you are. As an option - a constant feeling of emptiness inside, boredom, misunderstanding of one's true desires and values.
- Communication problems. It is very difficult for you to create and maintain stable relationships, you are prone to masochistic communication, cyclically idealize and devalue even the closest people, and do not always correctly interpret the motives of the actions of others.
“Borderline personality disorder can manifest itself in a wide range of signs,” says Valentin Oskin, “the symptoms of borderline personality disorder are most fully described in the DSM-5 and ICD-11 reference books. If grouped together, the symptoms will reflect a lack of control in the emotional, behavioral, cognitive spheres, as well as a distortion of the sense of self and a violation of interpersonal relationships. According to the psychologist, it is extremely difficult for people with BPD to break off relationships, even those that need to be broken off. Instead, they may go to great lengths to keep the people who matter to them around them.
At the same time, “border guards” tend to involuntarily throw out their emotions on those who are dear to them: “Often this ends with interruption of communication, because not everyone is able to endure such a bolt from the blue. And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
And even more so if this thunder rumbles once every couple of months, ”Ksenia Ivanenko notes in her Telegram channel, where she describes her personal experience in dealing with BPD.
Related material
To determine if you are at risk, you can take several tests for borderline personality disorder that are publicly available. It is important to understand that the result obtained is not a final diagnosis, it can only be made by a qualified doctor after analyzing the symptoms.
The Root of the Problem: What Causes Borderline Personality Disorder
Effective treatment for most mental illnesses requires the cause to be identified. Borderline personality disorder is problematic in that it arises from a number of factors and affects the basic components of the personality. That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
That is, there is simply no specific reason that triggers the PRL processes. “While BPD is one of the most researched personality disorders, there is no consensus on what exactly causes it. Severe stresses experienced by children and adolescents, such as neglect, prolonged painful separation, loss of a parent, violence, are common in people with BPD. There is also evidence of a genetic predisposition: among first-line relatives of a person with borderline disorder, the likelihood of developing a similar disorder is 3-5 times higher when compared with the general population,” notes Valentin Oskin.
Any person can be at risk, especially if he is going through a difficult stressful situation. It is known that this diagnosis is made more often in women than in men, and that in almost all cases of BPD it is driven by a deep emotional shock. Most researchers agree that the development of BPD is promoted by a combination of two groups of factors:
- Stress and traumatic life situations.
 For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder.
For example, sexual, physical or emotional abuse, persistent feelings of fear or abandonment in childhood, family problems, repressed feelings of anger, anxiety, and sadness. Stress or trauma in adulthood can trigger the onset of borderline personality disorder. - Genetic predisposition and environmental influences. The disease can be inherited, but more often borderline occurs as a pattern of behavior unconsciously borrowed from parents or close people, reactions to external stimuli.
Related material
No reason to break ties
If there is a “border guard” in your environment, you can build constructive communication with him, although this will require a lot of effort. “It is important to understand that a person with borderline personality disorder takes criticism extremely hard, for him it sounds like rejection, which he is terribly afraid of. At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
At the same time, emotional jumps do not allow him to get the desired intimacy. Relations with such a person are usually like a swing between the poles "I love you, don't leave me - I hate you, I'll leave you." It is important to understand that with borderline personality disorder it is impossible to consciously change your behavior, thinking, emotional reactions and response patterns to certain situations, ”says Valentin Oskin.
Many "border guards" live with a constant oppressive feeling of guilt, they feel broken, bad and unworthy of normal communication, which they badly need. They are unable to correctly read the reactions of others and the motives of their actions. This determines their strange behavior and repels potential partners and friends. Often, people with borderline personality disorder have a Favorite Person - a person on whom the "borderguard" is extremely dependent and who replaces not only everyone around him, but also himself. If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
If this person is busy or there is a conflict with him, the “border guard” literally collapses the world: he drowns in a storm of emotions, reflects on death and looks for thousands of reasons why he was rejected.
There are a number of rules that psychologists have developed for those who seek to communicate as "border guards", minimizing chaos, conflicts and the possibility of a tragic denouement: could end in disaster.
 Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”.
Take care of yourself: specify the time you spend separately, and try to logically explain why you are doing this or that and do not intend to devalue or leave the “border guard”. Related material
How to get rid of BPD
The main way to deal with borderline personality disorder is psychotherapy, in which work is done on the accompanying manifestations of an unstable mental state (depression, addictions, eating disorders, etc.) and syndromes (it is often necessary to treat alcohol withdrawal symptoms). syndrome). This is a long and complicated process, but statistics show that 70% of the “border guards” get rid of the main symptoms during therapy within six years, and remission occurs in a third of patients after two years.
“In therapy, people with BPD are primarily trained in emotional control, responsibility, and interpersonal skills. Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Dialectico-behavioral psychotherapy, a specially developed method for the treatment of BPD based on cognitive behavioral therapy, is well suited for this. No less effective is schema therapy, which also has special developments for the treatment of BPD. In the course of treatment, pharmacotherapy can also be prescribed, for example, for the treatment of associated depression or anxiety disorder, ”says Valentin Oskin.
Comprehensive treatment may include the following therapies:
- Dialectical Behavioral Therapy (DBT). Allows the "border guard" to realize that problems can be viewed from different angles, eliminates black and white thinking.
- Mentalization (MBT). It helps to explain to oneself the behavior of other people, logically argue their motives and work to improve interpersonal interaction.
- Transference Psychotherapy (TFP) teaches you to perceive positive and negative qualities at the same time, to get out of the “deification/devaluation” paradigm.
Learn more