New hope for bipolar disorder
New Hope for People with Bipolar Disorder: Your Friendly, Authoritative Guide to the Latest in Traditional and Complementar y Solutions, Including: Proper ... Depression & Manic-Depressive ... by Jan Fawcett
Jan Fawcett, Bernard Golden
Rate this book
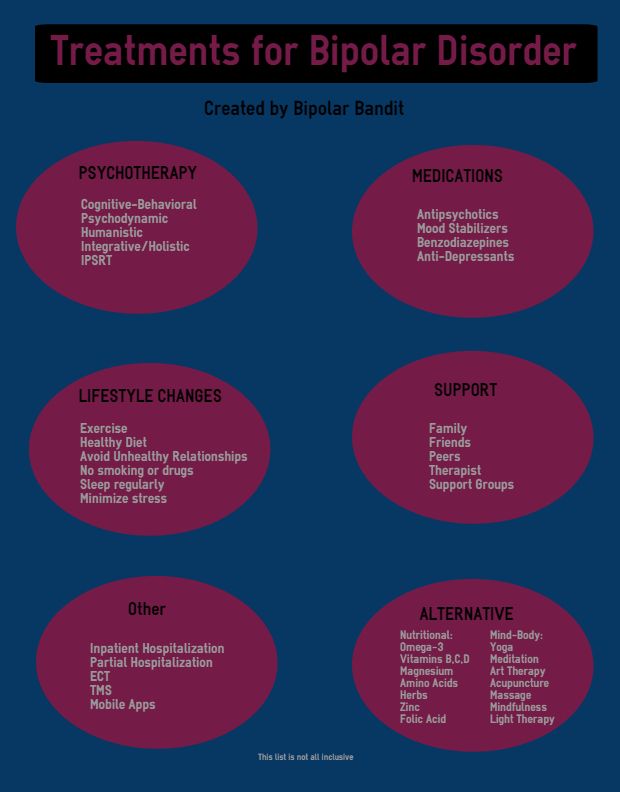
The second edition of this groundbreaking guidebook provides up-to-date treatments and compassionate guidance for anyone affected by bipolar disorder—from the recently diagnosed to chronic sufferers and their families. You’ll receive tips from world-renowned experts—including coauthor Nancy Rosenfeld, herself a bipolar survivor—and learn about vital new options and innovations in bipolar treatment and research, such as:
•New precautions: why some patients can get worse rather than better when taking antidepressant medication
•The inside story on atypical antipsychotic medications, antidepressants, and other medications that affect neurotransmitters
•New genetic research, studies on serotonin, studies into childhood and adolescent bipolar disorder, and results of neuron imaging and neuropsychological testing
•Advice on making instant, effective lifestyle changes, coping with stigma, and deciding whether or not—and how—to disclose your illness to others.
•A guide to the many evolving forms of psychotherapy
352 pages, Paperback
First published September 14, 2000
About the author
What do you think?
Rate this book
Search review text
Displaying 1 - 7 of 7 reviews
July 10, 2020This, along with dyslexia and ADHD, is in my gene pool. Good read. I like the 'new hope' part. If this is in your gene pool, I would encourage you to read. The reviews in Good Reads and Amazon are pretty much spot on for me.
- 2016 health
February 29, 2020
A must read for newbie Bipolars. You need to know all the inter-community lingo and information. I have my own copy.
September 21, 2012
This book was one of the most comprehensive books I have read so far on bipolar disorder. I have read many books on this topic which I suffer but this book is about the best to date. I found the book to have a lot of useful and informative which I believe will help me anf countless others. A lot of books on bipolar only discusses the illness itself. As this is a self-help book for bipolar patients, anyone who reads it can get good information of how to improve their lives and live with the disorder.
I have read many books on this topic which I suffer but this book is about the best to date. I found the book to have a lot of useful and informative which I believe will help me anf countless others. A lot of books on bipolar only discusses the illness itself. As this is a self-help book for bipolar patients, anyone who reads it can get good information of how to improve their lives and live with the disorder.
- self-help
June 24, 2016
This was the first book I read about the topic of bipolar disorder, shortly after my diagnosis. The use of actual people with bipolar disorder as contributors to this book lends it a credence that many books on the topic lack. I felt a kinship with those people. I was more than a patient as I read this. It was more than clinical. I appreciate the fact that this book kept in mind that people with bipolar disorder are still people first and mentally ill second.
August 9, 2013
Very helpful book in understanding bipolar disorder.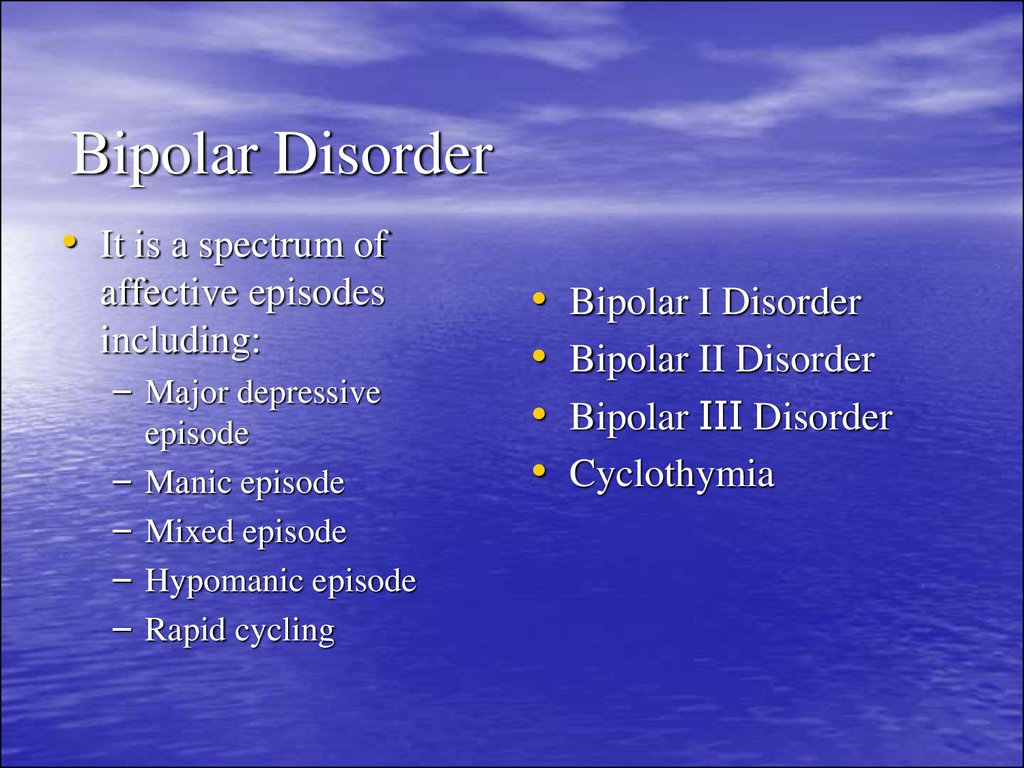 It addresses many different aspects including symptoms, treatment, support systems, living with someone with the disorder, etc.
It addresses many different aspects including symptoms, treatment, support systems, living with someone with the disorder, etc.
The only thing was I wish it went deeper into some of the self-help techniques. Overall a great book for someone recently diagnosed or a family member of someone with bipolar disorder.
July 27, 2010
Great book for understanding and support.
April 24, 2012
A must read for those with or around those with Bi Polar young or old. Comforting how to live with those with bipolar. Hugs
Displaying 1 - 7 of 7 reviews
New Hope for Patients with Treatment-resistant Bipolar Disorder
Study uses advanced imaging to identify targets for deep brain stimulation in severe cases of the disease
UH Neurological Institute - Winter 2018
Neurosurgeon, Division of Functional & Stereotactic Neurosurgery, UH Cleveland Medical Center; Assistant Professor of Neurosurgery, Case Western Reserve University School of Medicine
Deep brain stimulation (DBS) has long been used to treat movement disorders – such as Parkinson’s disease, essential tremor and dystonia – as well as obsessive-compulsive disorder and severe Tourette’s syndrome.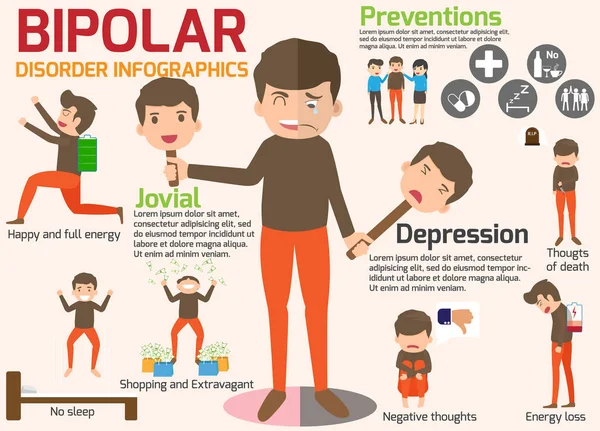 While more doctors have begun using DBS to treat depression, to our knowledge, none have examined its use in treating bipolar patients cycling between mania and depression, says Jennifer Sweet, MD, a neurosurgeon in the Division of Functional & Stereotactic Neurosurgery at University Hospitals Cleveland Medical Center.
While more doctors have begun using DBS to treat depression, to our knowledge, none have examined its use in treating bipolar patients cycling between mania and depression, says Jennifer Sweet, MD, a neurosurgeon in the Division of Functional & Stereotactic Neurosurgery at University Hospitals Cleveland Medical Center.
Dr. Sweet leads a team at University Hospitals in Cleveland, Ohio, that is studying the possible use of DBS to improve the lives of patients with severe treatment-resistant bipolar disorder. Funded by a National Institutes of Health grant, the study is using a special kind of brain imaging known as tractography to learn whether the neural pathways of patients with bipolar disorder are fundamentally different from others.
“Magnetic resonance imaging in these patients looks normal, but we suspect they have abnormal ‘wiring’ that underlies their disorder,” she says.
She and her colleagues have been using tractography to compare the brains of bipolar sufferers with a healthy control group and ultimately identify an area of abnormality that could be targeted with DBS.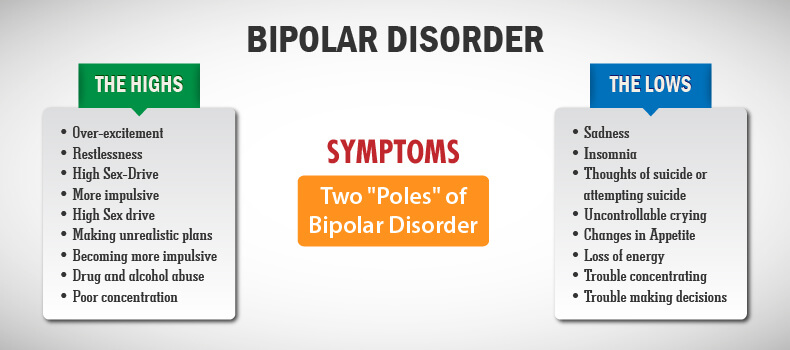 MRI images are put through computational models that manipulate findings and help doctors visualize pathways.
MRI images are put through computational models that manipulate findings and help doctors visualize pathways.
“We can see some of the white matter pathways in the brain with existing technology, but it’s very hard to see the more complex and specific circuitry,” Dr. Sweet explains. “We know that there are numerous interconnected networks regulating mood and thought in the brain, and we are trying to figure out exactly how those networks play a role in various disorders so that we can use neuromodulation to modify aberrant activity.”
NEW HOPE FOR PATIENTS
The overall goal of the UH DBS study is to help bipolar patients who are resistant to medication and other therapies to stop the cycling between mania and depression.
“For many patients, the cycling between mood states makes bipolar disorder a chronic and recurrent illness,” Dr. Sweet says. “If we can stop the cycling, it may be curative, rather than the current approach of treating the symptoms of mania and/or depression.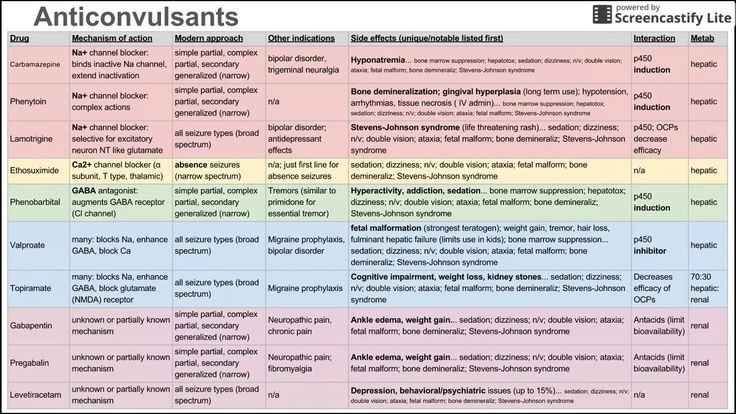 We do not know of any other centers in the country that are focusing on this approach to bipolar disorder.”
We do not know of any other centers in the country that are focusing on this approach to bipolar disorder.”
The study has already exceeded enrollment goals for the initial imaging phase, which examined healthy volunteers, treatment-resistant bipolar patients and treatment-responder bipolar patients. Data analysis is expected to continue for the next several months, and Dr. Sweet hopes to start recruiting patients for the treatment portion in late 2018.
She says only a small group of patients who are found to have abnormal imaging – and who have failed at least four types of FDA-approved treatments, including electroconvulsive therapy and medications – will be treated first to demonstrate the efficacy of the approach.
“We have been doing DBS for decades so we know it’s a safe therapy, but our question is if it will be effective in a new location in the brain for the treatment of a new disease – bipolar disorder,” Dr. Sweet says.
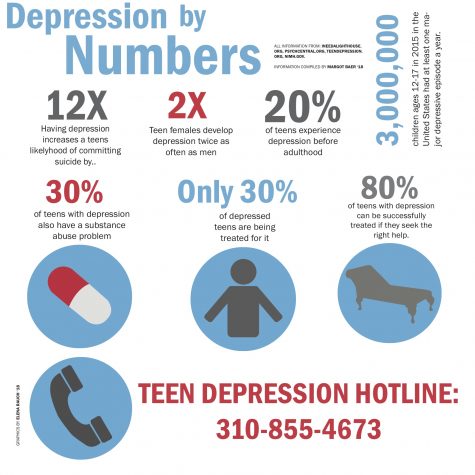
Bipolar disorder is a particularly burdensome condition in that it disproportionately affects younger people.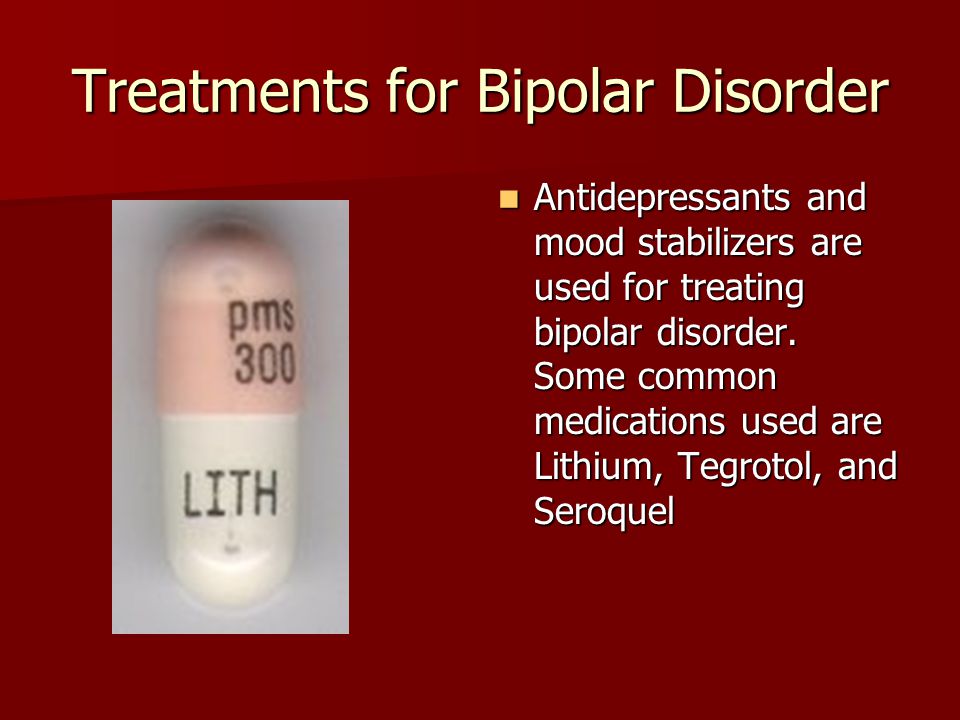 About half of all sufferers are diagnosed by 14 years of age, with up to three-quarters diagnosed by age 24.
About half of all sufferers are diagnosed by 14 years of age, with up to three-quarters diagnosed by age 24.
“This is a highly functioning group of people and yet they can become so debilitated by the disease that they can no longer work or have healthy relationships,” Dr. Sweet says. “We hope to help them overcome these obstacles.”
A COLLABORATIVE EFFORT
The NIH grant that is funding this work is a 4-year K grant, designed to help early-career investigators. It is currently in its third year, and Dr. Sweet is applying for additional grant money as well as philanthropic support to continue this work.
She says she is deeply appreciative of the world-renowned experts available to collaborate with her, including:
- Keming Gao, MD, PhD, psychiatrist and Clinical Director, Mood Disorder, and Medical Director, Electroconvulsive Therapy, UH Cleveland Medical Center; Professor of Psychiatry, Case Western Reserve University School of Medicine
- Jonathan Miller, MD, neurosurgeon and Director, Functional and Restorative Neurosurgery Center and Vice Chairman, Educational Affairs, UH Cleveland Medical Center; Associate Professor, Neurosurgery, the School of Medicine
- Joseph Calabrese, MD, psychiatrist and Director, Mood Disorders Program, UH Cleveland Medical Center; Professor of Psychiatry, the School of Medicine
- Cameron McIntyre, PhD, Professor, Department of Biomedical Engineering, the School of Medicine.
We ensure continuity of care from referring physician to specialist by providing prompt communication after each patient visit and carefully coordinated perioperative management. To refer a patient, call 216-844-2724.
Faith and hope: how an Orthodox Christian woman with bipolar disorder lives
Due to illness, I lost hope in God for the first time
– Now there are many jokes about “bipolar”. You open the Internet, it seems that every second person has this disorder. Such is the "fashionable" diagnosis. How about really?
- I dropped out of two colleges, graduated from the third with grief in half and tried three times to get a higher education, without success. I stayed at each workplace for an average of a month. She was in a psychiatric hospital. Got a disability. No, jokes about “fashionable bipolar” do not seem funny to me!
I have Bipolar Affective Disorder (BAD) type II - it is dominated by depressive periods, and manias are not very bright (they are called hypomanias - mild manias).
Depression can be of different depths, it's a spectrum. It happens that everything seems to be fine, but the head does not work, you have to deal with purely everyday things or kill time on the Internet. Such days are painful, you begin to blame yourself for being relaxed. It happens that you can’t even go outside, at best you sleep. Or you sit, swing, wander around the apartment. You don’t remember what was better, and you don’t believe that it will end.
This summer was very difficult. I did not feel alive and did not see the point in my torment.
“Everyone who is dear to me will die, I will die, why then all this?” - the sick mind told me. I was as if driven into a trap and from impotence could only cry. It was the first time in my life when, due to illness, I lost hope in God, and it was very scary.
I was in the hospital. Thanks to the doctors who were there and brought me out of this hell. In general, in depressive episodes, patients often have suicidal thoughts and intentions, and I am grateful to God that I never had them.
Depression in bipolar disorder is replaced by mania. People take out huge loans, spend a lot of money, drop everything and travel, engage in promiscuous sex - in the hospital I met girls who manifested their mania in this way.
I have hypomanias, they are easier - general excitement, a lot of ideas, creativity, passion, a lot of energy. But this is only in words everything is great, but in practice there are a lot of “buts”: you jump on top, nothing is brought to the end, one idea replaces another, and there is no result as such. Well, the ideas themselves are far from always adequate and realistic. For example, in my dacha I wanted to move a giant boulder that even my dad would not have lifted, and make a flower bed around it. I slept for a couple of hours, at night I came up with ideas for books and wrote notes, at dawn I walked with a camera. In this phase, I have a great need for communication, accelerated speech, a tendency to rash purchases.
Sometimes, if I feel like I'm going to be carried away, I give my bank card to my mother - "you'll return it in a week.
"
I came to a psychiatrist by chance, and my confessor advised me to go to the hospital
– How did it all start? Did something foreshadow illness?
– I had mood swings, trouble concentrating at school. And for the first time I got to a psychiatrist by accident. At the age of 16, something happened to my jaw, my mouth did not open completely, I got to the maxillofacial surgeons, and they treated me for six years: braces, plates, washing the joints. When they tried everything, they said: “In our department, nothing can hurt anymore, this is probably already psychosomatic.” And by the hand they took me to a psychiatrist. I was then 22 years old. I also read that some kind of trigger situation can trigger the disorder, and I experienced psychological abuse a couple of years earlier.
The following process was going on in parallel. I went to the temple since childhood, and at the age of 18–20 I almost stopped. Kind of a belated teenage rebellion. Much in the church (not in the faith!), began to confuse, it seemed a formality.
Much in the church (not in the faith!), began to confuse, it seemed a formality.
At some point, my mother began to think that my condition was due to the fact that I did not go to church. I began to go to the temple again, but then it became clear that these were just health problems.
The psychiatrist said that I had mild depression and prescribed an antidepressant. I drank it for only a few days, because because of it, as I later realized, I had a manic rise. The drug was changed, a few more “light” ones were added. But then I had a feeling that the pills made it worse. It was as if they opened some kind of floodgates inside me, and what was hiding inside broke out. And this is the worst thing for me - to lose control of myself.
Then I became interested in psychiatry and began to read articles and books. Self-diagnosis is a thankless task, but I decided that my condition was similar to cyclothymia. The doctor, oddly enough, confirmed my suspicions.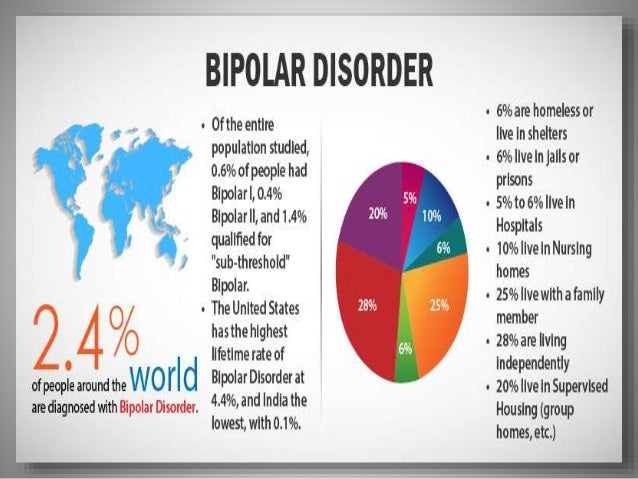 Cyclothymia is, as it were, a mild form of bipolar disorder, when the amplitude of mood swings is less (and some experts consider it a variant of the norm).
Cyclothymia is, as it were, a mild form of bipolar disorder, when the amplitude of mood swings is less (and some experts consider it a variant of the norm).
I remember, during my first hospitalization, I read Masha Pushkina's book Bipolar People and thought, "poor people, how hard it is for them, it's good that I don't have this." But I myself had exactly “this”, they just “forgot” to tell me when I was discharged that they had diagnosed me with bipolar II disorder.
I thought that the pills were picked up, which means that everything is over and you can continue to live a normal life. I just have cyclothymia! A year later, when I was hospitalized for the second time, I already suspected that I had BAD, but again I was told about it only when I asked myself. So for sure I found out my diagnosis only two years ago.
Mental hospital and disability: not so scary?
– People are usually very afraid of “going to a mental hospital”.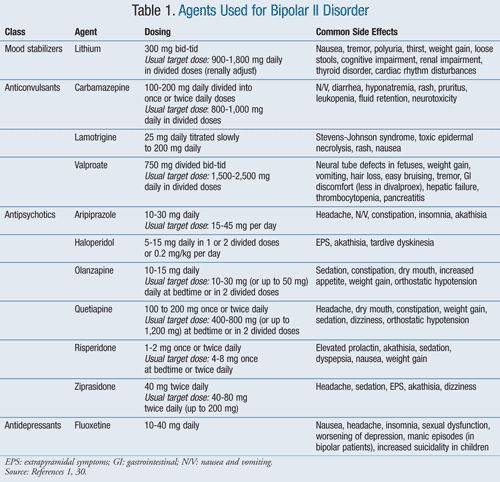 What is it really like to be in a psychiatric hospital?
What is it really like to be in a psychiatric hospital?
- Coming to a psychiatric hospital - what could be worse? I thought so too. From the first appointment at the clinic where I am now being observed, I was advised to be hospitalized. But my mother and I were not ready for this, stereotypes interfered, although we could not pick up pills on an outpatient basis.
Confessor helped me to decide on hospitalization. He said that the hospital is very good, you can take laptops and phones there: “If you lie down, watch a movie, everything will be fine,” and I agreed.
Before that, all I had heard about psychiatric hospitals was that they strip you down to your underpants, give you a hospital gown, and you go there for several months. Turns out it's not like that everywhere!
I am not in the acute department, but, one might say, in the lightest one. The situation there is like in a sanatorium or pioneer camp. The atmosphere is friendly, everyone communicates when someone leaves - they take pictures, hug, exchange contacts.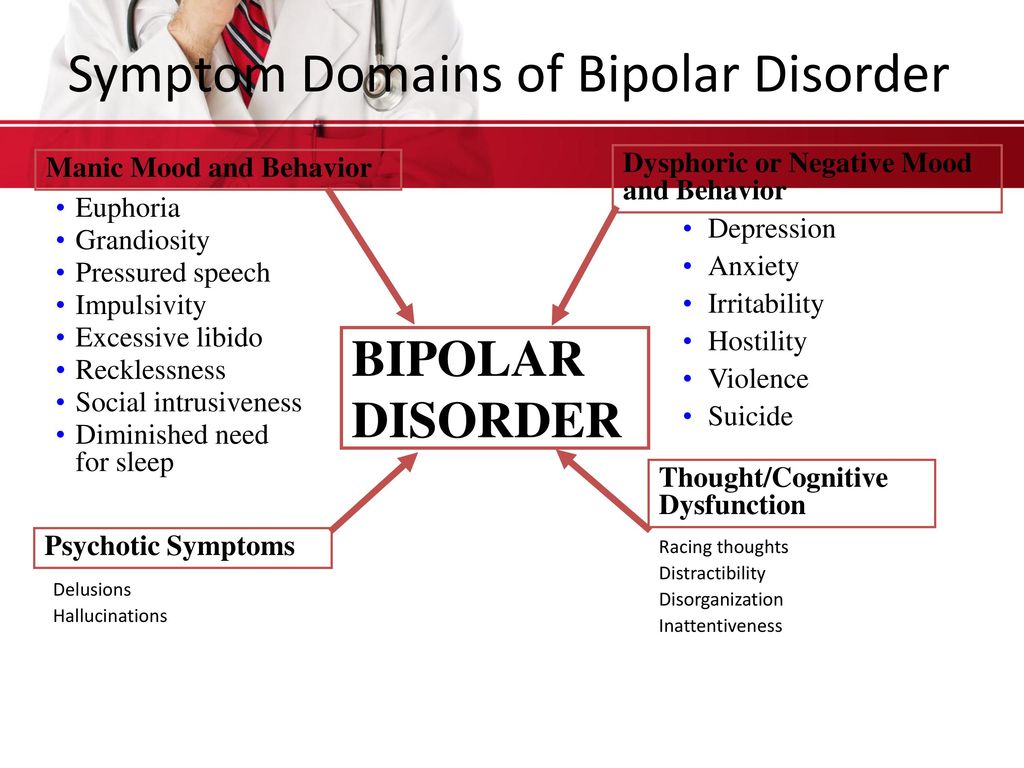 There are a lot of teenagers there. There are restrictions, for example, there are no plugs in the dining room, but there are sockets in the wards, showers according to a schedule, walks according to a schedule and with the doctor’s permission, periodic “search” of things in the wards, you show everything that you brought from the street. Yes, it hurts you a little as a person, but you quickly get used to it.
There are a lot of teenagers there. There are restrictions, for example, there are no plugs in the dining room, but there are sockets in the wards, showers according to a schedule, walks according to a schedule and with the doctor’s permission, periodic “search” of things in the wards, you show everything that you brought from the street. Yes, it hurts you a little as a person, but you quickly get used to it.
Since mid-October I have had my first remission in a long time. Slowly I forget how bad it was in depression. When I remember - just God forbid back into it.
Mental disorders are the same diseases as physical ones. They are also from the word "pain". Only when the soul hurts, you can’t hide from it anywhere, and no painkiller will help.
– Applying for disability due to mental illness is also a difficult step. Was it difficult to decide?
- I did not refuse this opportunity, because my parents are pensioners, I do not work, and the status of a disabled person gives me the right to free travel, medicines (and they now cost about 15,000 a month) and a pension - all this won't bother us.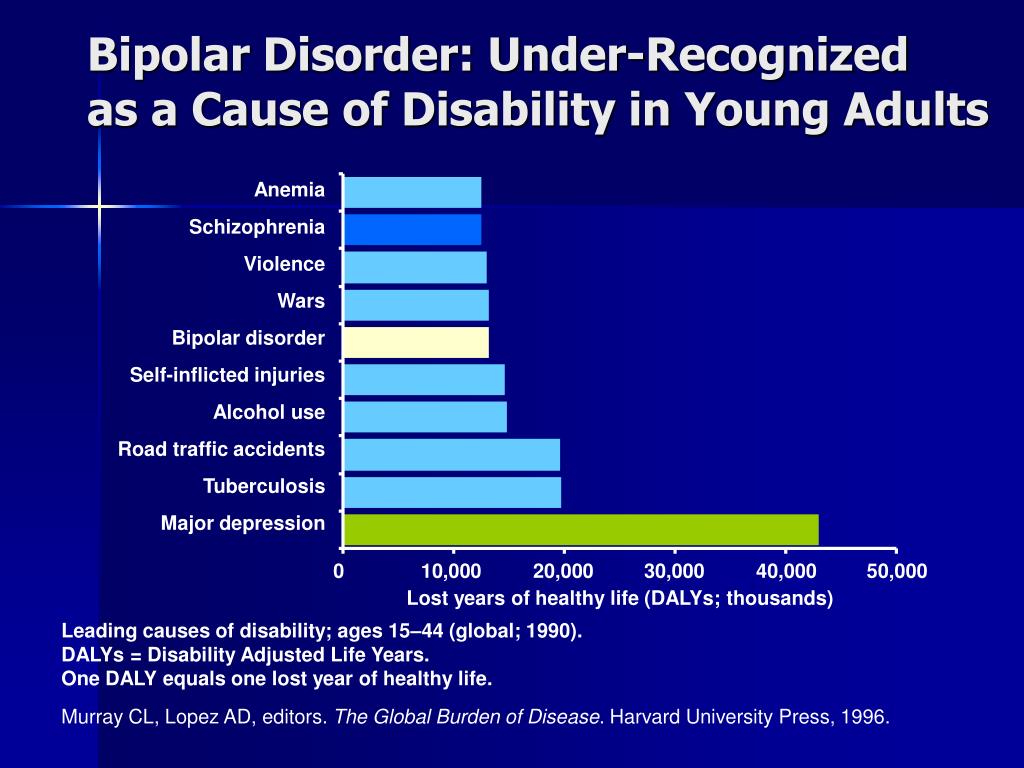
Disability is registered through the district neuropsychiatric dispensary. You need to be observed there for at least six months, go to the local psychiatrist every month, so that the doctor sees that you really can neither work nor study. At the same time, I am treated by my doctor, and I am only observed in the PND. And then - a lot of papers and commissions.
Psychiatric disability does impose some limitations. They definitely won’t give permission for a weapon and, it seems, a driver’s license, but this is not at all relevant to me now.
Life with a diagnosis: resentment against God, then acceptance
– And after you finally got the diagnosis, did something change in your life? Have new restrictions appeared or, on the contrary, has it become easier to live, knowing what is happening?
– I began to treat myself more carefully, to listen. I know where I can go and where I can't. Study, work - this is not for me yet.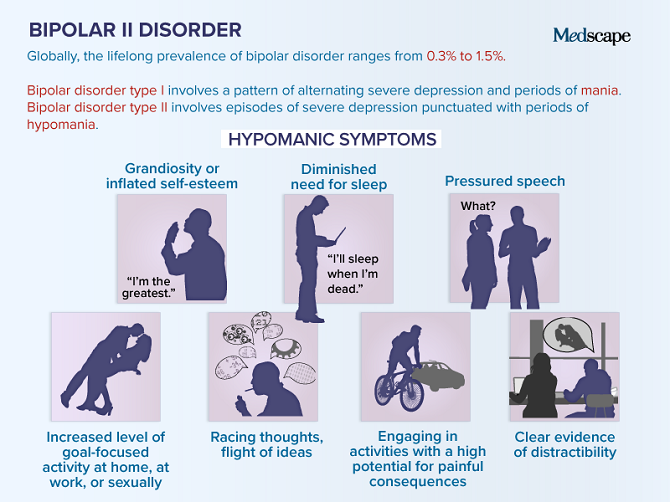
Strangely enough, even though I know that I am sick, the feeling of guilt or “it just seems to me” does not disappear anywhere. You still blame yourself for everything, even when you have a diagnosis, disability and everything else.
When I first heard the diagnosis of bipolar disorder from a doctor, I was stunned. This is a terrible, difficult, life-long diagnosis! “What, does that change anything?” the doctor asked. And I realized, but really - no. The disease did not start a minute ago, in her words. I have been living with her for a long time. And somehow I manage. So, I can continue to cope, and nothing terrible has happened.
When the diagnosis was made, at some point there was resentment against God. I thought that the disease had robbed me of the life I dreamed of, cut off opportunities. But then I saw that it was the disease that helped me to open up, to become myself.
The diagnosis gave me the right to vote. I became part of the community and could now speak on its behalf and do something good, help, enlighten.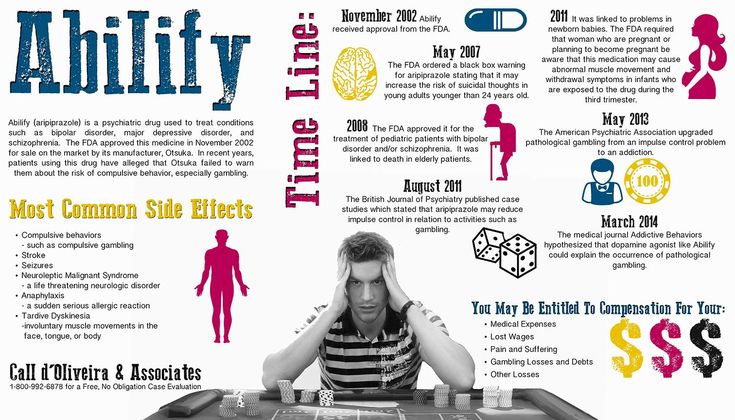 When I found out about BAR, I had about 800 subscribers on my blog. And the first thing I did after calling my mom was to write a post about my bipolar disorder. Then I also wrote psycho-activist posts, and people reacted very interestedly, supported me. I realized that such a blog can be useful. But then I deleted everything. When I am severely depressed, it becomes uncomfortable for me that information about me is on the Internet. So I created and deleted many blogs already, but like a phoenix revived them from the ashes. I hope that the current blog will still be the last one.
When I found out about BAR, I had about 800 subscribers on my blog. And the first thing I did after calling my mom was to write a post about my bipolar disorder. Then I also wrote psycho-activist posts, and people reacted very interestedly, supported me. I realized that such a blog can be useful. But then I deleted everything. When I am severely depressed, it becomes uncomfortable for me that information about me is on the Internet. So I created and deleted many blogs already, but like a phoenix revived them from the ashes. I hope that the current blog will still be the last one.
I am also writing a book. This is an insider novel about the everyday life of a psychiatric hospital, which we look at through the eyes of a young patient diagnosed with bipolar disorder and bulimia. This is autofiction based on my experience, but the heroine is not me. In writing courses, they said that such a book is very necessary, I hope that everything will work out with it.
Of course, there are downsides to my position. For example, on medications, I gained 20 kilograms in just a couple of months and still have not come to terms with the “new” me. It is also very difficult to plan something with BAR: meetings, vacations, training courses, and so on. You never know when depression will hit you. Well, do not forget that bipolar disorder is considered one of the most dangerous mental illnesses.
For example, on medications, I gained 20 kilograms in just a couple of months and still have not come to terms with the “new” me. It is also very difficult to plan something with BAR: meetings, vacations, training courses, and so on. You never know when depression will hit you. Well, do not forget that bipolar disorder is considered one of the most dangerous mental illnesses.
Bipolar disorder is the 12th most common cause of disability in the world
Bipolar affective disorder (BAD) is a mental disorder characterized by alternating
patient's two phases of mood: manic (or
hypomanic) and depressive.
Such phases are called affective, that is, bearing signs of affect -
manifestation of emotions beyond control.
In the International Classification of Diseases ICD-11, bipolar disorder is distinguished I
type and bipolar disorder type II.
In case of BAD type I, during the course of the disease there are necessarily pronounced manic phases
, when the patient feels high spirits, motor
excitement, and acceleration of thinking. Behavior becomes impulsive and often
Behavior becomes impulsive and often
reckless. Until the 1990s, this type of disorder was known as manic-depressive psychosis.
In bipolar II patients, manic episodes are smoothed out, they are called hypomania
(mild mania), and the depressive phases are deeper and longer.
Bipolar disorder is the 12th most common cause of disability according to the World Health Organization. BAD is considered one of the most dangerous
mental illnesses. Between 20 and 60 percent of patients with bipolar disorder have attempted suicide.
Now I am learning to live with BAD, trying to be useful to society and people like me. This is a very important experience for me, this is my way, my voice and my way of talking to the world.
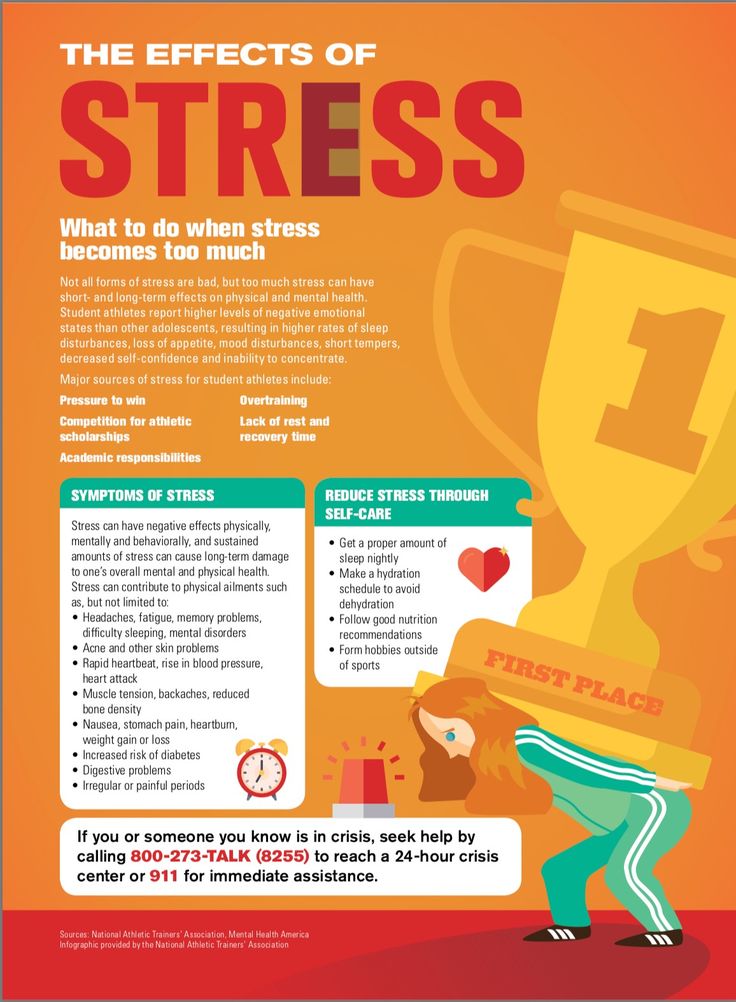
– And what, besides drugs, helps to alleviate the condition?
– Psychotherapy helps a lot. I recently discovered it for myself, before I doubted it. Well, expensive, of course. Now I see the result, because most of the psychological problems that worsen my condition are not directly related to bipolar disorder.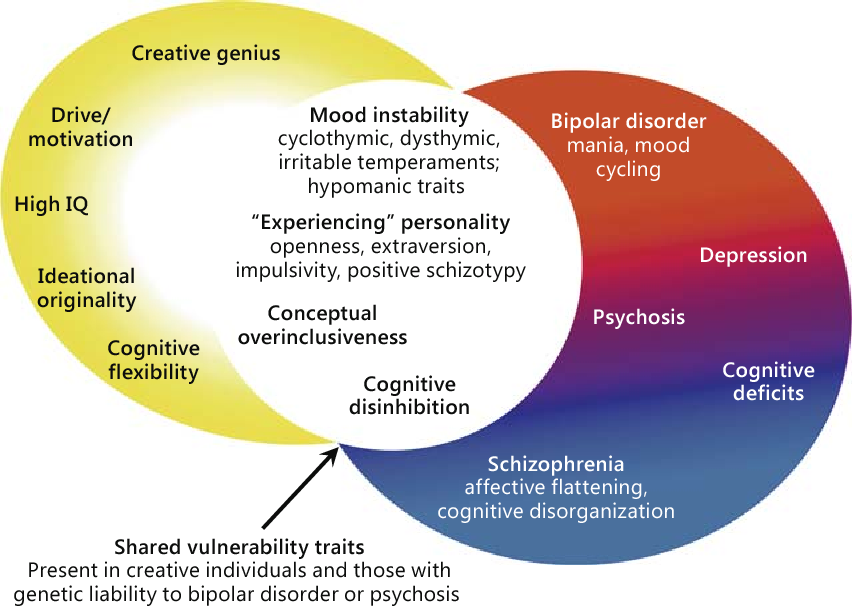 These are some kind of traps of thinking or everyday trifles when you poison your own life. Two things that run like a thread through my therapy are the inner critic and personal boundaries.
These are some kind of traps of thinking or everyday trifles when you poison your own life. Two things that run like a thread through my therapy are the inner critic and personal boundaries.
I also use an app on my phone, a mood diary. You mark the mood for the day, plus you can additionally enter your state or feelings - anxiety, drowsiness, and so on. This helps to notice the beginning deterioration or to trace the effect when changing drugs.
I also want to try support groups, I'm going to visit one at the Just People Foundation.
Depression, bipolar disorder, schizophrenia fund guide
Read more
“You make everything up!”
– Is it easy to relate to people with bipolar disorder? How do friends and relatives accept the diagnosis? Can they help with something or is it better not to touch a person when he feels bad?
- It's hard to communicate in the depressive phase, but friends know that if I "merge", it means that I'm just "not in the resource" at the moment. At normal times, I'm always happy to meet and chat. And you can help a depressed person in simple ways - bring groceries from the store, cook something, take a walk around the yard.
At normal times, I'm always happy to meet and chat. And you can help a depressed person in simple ways - bring groceries from the store, cook something, take a walk around the yard.
If a person has opened up to you, this is already a very big step for him. Try not to hurt him, do not devalue his problems.
In depression, a person sometimes does not have the strength even to brush his teeth, but this is not a reason to blame him. This is the most important thing for friends and family to remember - do not blame. The disease is not his fault, although outwardly it looks like laziness, or a person may seem rude or something else. It's hard and painful for him. He, like a sick person with a physical ailment, deserves compassion.
My relatives are very supportive. Mom is just a hero, she went through a lot with me. In the summer I was in the hospital for two months, and every day she came to walk with me in the hospital park for an hour. True, sometimes my mother says that I am her cross. And I don’t want to be a cross, I want to be support and support for my loved ones.
And I don’t want to be a cross, I want to be support and support for my loved ones.
Faith and BAR
: “In the temple I can rest from the struggle”– How to live in the Church with BAR, isn't it hard to go to church, pray, fast?
– Due to BAD, sometimes I don't go to church for a month. It’s also hard for me in crowded places, so on Christmas and Easter, if I feel bad, I don’t go to the night service. I need to take medicine four times a day, so I don't go to the temple in the morning on an empty stomach. But I have a very understanding confessor. In general, I feel good in the temple, this is a place where, as if there is no time and you can pause, take a break from the eternal struggle with yourself, with the disease.
Otherwise, I'm not much different from other parishioners. I read prayer rules, when I can’t read, I listen. Progress works wonders, there are audio prayer books! There are usually no problems with fasting, food restrictions do not affect my mental health, but here, I think, this is an individual matter.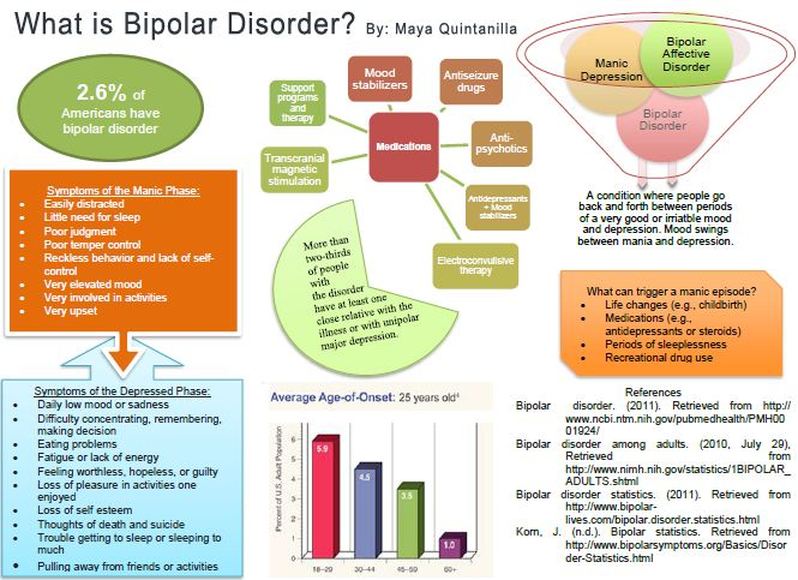
I try to understand and accept my limitations. For a long time I considered some weaknesses as sins, but then it turned out that you just need to come to terms with this.
I regard BAR as an experience, painful, difficult, but sent to me for something, and therefore necessary and necessary. It gives me a different vision of the world. But not in the moment, but when you step aside.
It's like a tattoo or wood carving. When you are depressed, you get a tattoo, it is painful and unpleasant, but when everything is over and you look at it from the side, you will see a drawing.
Unnecessary happiness
Bipolar affective disorder. Accompanied deviations in the biochemical processes of the brain. Word "bipolar" means two extremes - mania and depression replace each other while the person is just trying to live.
“Fifteen years ago I wrote a book about my struggle with mania and depression, about a suicide attempt that almost became for me fatal, about a stubborn unwillingness to take the medicines that I were needed.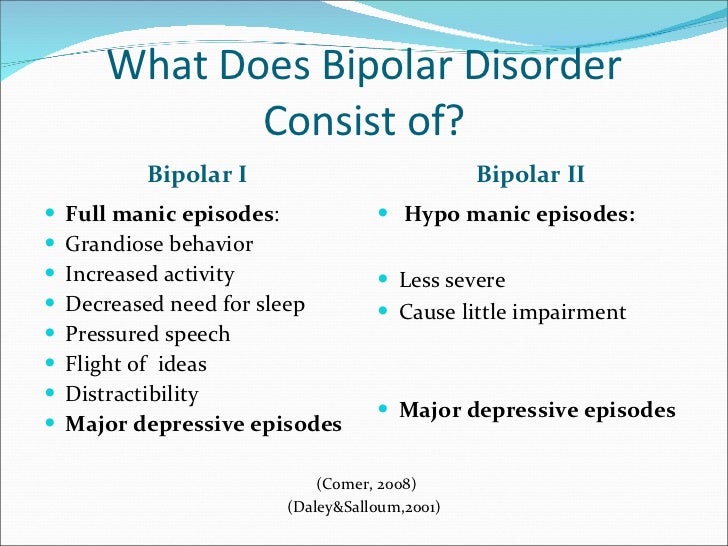 It was a heavy book, plunging into a heavy the reality of bipolar disorder. But it was also a story. about the saving power of love, friendship, family, about the gift of a doctor, able to heal, ”so begins the afterword of the clinical psychologist Kay Jamison to his book on bipolar disorder.
It was a heavy book, plunging into a heavy the reality of bipolar disorder. But it was also a story. about the saving power of love, friendship, family, about the gift of a doctor, able to heal, ”so begins the afterword of the clinical psychologist Kay Jamison to his book on bipolar disorder.
This afterword to A Restless Mind reflects both pain and the hope of people suffering from bipolar affective disorder. IN The world of such people is approximately from 1% to 4%. Of course, count impossible, but even 4% is 320 million people. This is despite that BAD is difficult to diagnose and not everyone goes to the doctor. On in fact, this number could be much higher.
The words "depression" and "bipolar disorder" only in March 2021 years searched in Yandex about a million times. For the same period in 2020 - 700,000 times, and in 2019year - 500,000. And although the tendency to take care of oneself and one's health, including psychological, recently gaining momentum - mental diseases are still shrouded in a fog of obscurity for many, myths, rumors and stereotypes.
Terminology.
BAD - bipolar affective disorder, pathology, accompanied by deviations in the biochemical processes of the brain brain. This disease is chronic, and life expectancy in people with bipolar disorder by an average of 9years less.
The word "bipolar" means two extremes. Disorder manifests itself in sudden changes in emotions, mood and level energy. These changes do not happen all at once, they usually last for several days or weeks.
In general characteristics, suppressed depressive state - depressive episode . He identical to the condition in the associated disorder - unipolar depression. People feel despair, despondency, lack of energy and mental concentration. This condition may appear physically - in lack or excess of sleep or food.
They also distinguish an elevated state, which replaces depressive - manic episode . In that difference between bipolar disorder and unipolar depression. IN in this state, a person feels full of energy, happiness and optimism. Euphoria and high self-esteem are also companions of this stages.
IN in this state, a person feels full of energy, happiness and optimism. Euphoria and high self-esteem are also companions of this stages.
In depression, suicidal thoughts come to a person, he is gnawing feeling of guilt, self-flagellation begins, certain addictions – food cravings, for example. And in mania people don't just feel good, they feel good literally invincible, in every way. Can invest everything savings in a risky business, carelessly engage in dangerous sports. At this stage, the person may become delirious or manifestations of megalomania - to feel like a messenger of God or with supernatural powers.
Classification
Yes, we all go through certain stages in the "middle" intensity, even when healthy people. In case of bipolar disorder to describe these episodes fit the word "too". Classification disorder depends on the nature of its manifestation. (Fig. 1)
Fig. 1. Classification of disorders and the nature of their manifestations in comparison
A person suffering from unipolar depression may have "average" ups but downs can be crushing and last long enough for a long time.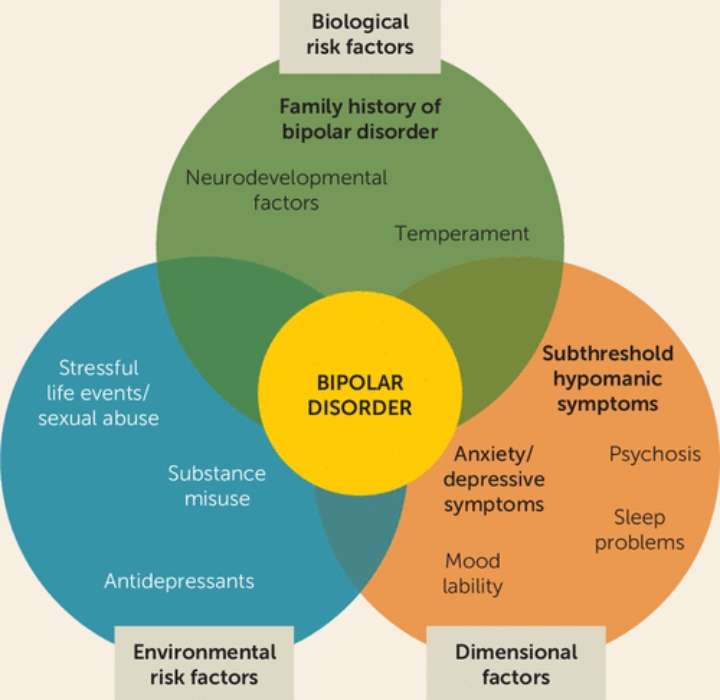 People with bipolar disorder-1 experience severe downturns that last at least two weeks, and then - a steep climb that lasts at least a week. If such manic episodes are not treated, they can last from 3 to 6 months. Bipolar disorder-2 is different from type 1 that a person does not reach such a high level instability in the stage of mania. This is called hypomania. AND it can last at least four days, but, as a rule, such episodes last weeks or months. With cyclothymia, ups and downs less peak, but they continue alternately for at least for two years.
People with bipolar disorder-1 experience severe downturns that last at least two weeks, and then - a steep climb that lasts at least a week. If such manic episodes are not treated, they can last from 3 to 6 months. Bipolar disorder-2 is different from type 1 that a person does not reach such a high level instability in the stage of mania. This is called hypomania. AND it can last at least four days, but, as a rule, such episodes last weeks or months. With cyclothymia, ups and downs less peak, but they continue alternately for at least for two years.
There are also other options. For example, sometimes a person may experience symptoms characteristic of both stages at the same time. Or these phases can change very often - 4 or more episodes depression or mania during the year.
Causes
The cause of bipolar disorder is not yet known, as is the case with many other mental illnesses. However, scientific research has achieved some results.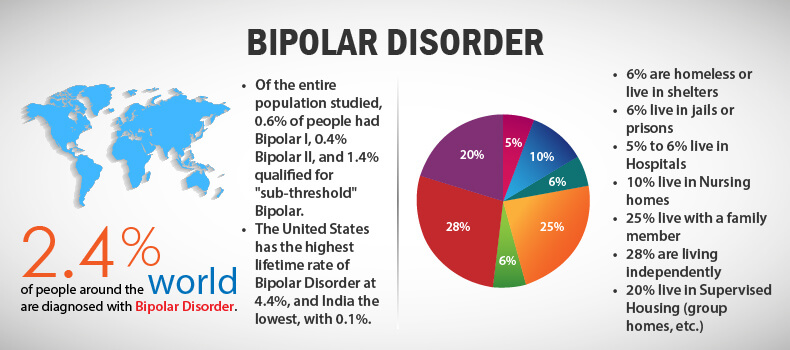 It was found, that the dynamic interplay between genetic, neurochemical and environmental factors play a role in the onset and progression of BAD. (Fig. 2)
It was found, that the dynamic interplay between genetic, neurochemical and environmental factors play a role in the onset and progression of BAD. (Fig. 2)
Fig. 2. Causes of Bipolar Disorder
It is assumed that the level of heredity is approximately 70-80%. Scientists explain such high numbers by two factors: genetic transmission and "inherited" family environment, which potentially impaired if parents have psychopathology. "Bipolar gene" was not found, but found that some interaction between certain genes affects the likelihood of developing disorders.
A genome-wide association study conducted in 2019, found 30 locations on the chromosome - loci that contain genes encoding ion channels, transporters neurotransmitters and synaptic components. Their analysis revealed nine highly enriched sets of genes that affect BAR development. According to the results of the study, scientists found that bipolar disorder-1 is highly genetically correlated with schizophrenia due to psychosis, while bipolar disorder-2 is more strongly correlated with major depressive disorder disorder.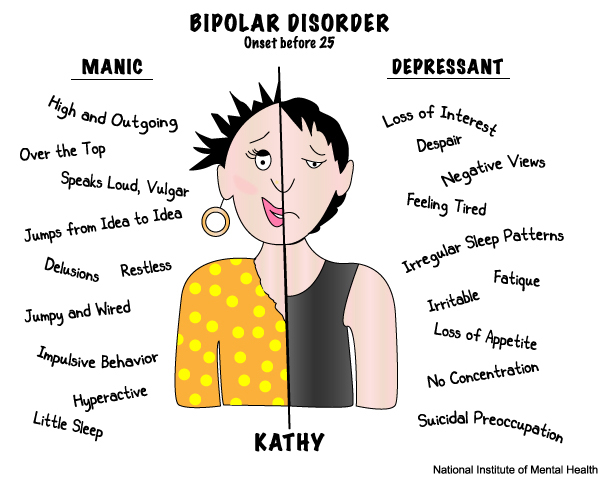
Another study of the DNA genome in the post-mortem hippocampus in humans revealed a decrease in the number of copies of mitochondrial DNA (mtDNA), which are located in the mitochondria. Mitochondria are like "energy" stations for all body cells - including and brain. Scientists believe that the preservation of mitochondria and their proper work affects life expectancy. Many research over the past 50 years has proven mitochondrial dysfunction in people with bipolar disorder and this is considered a pathological factor.
In the same study, researchers found a strong correlation between the number of mtDNA copies and the length of telomeres, which are the "tips" chromosomes, and their length is closely related to the duration life. They also found a significant correlation between acceleration epigenetic aging and telomere length. So the scientists proved accelerated biological aging of the hippocampus in people with bipolar disorder. By According to the same scientists, it may underlie neurocognitive dysfunctions in people with bipolar disorder.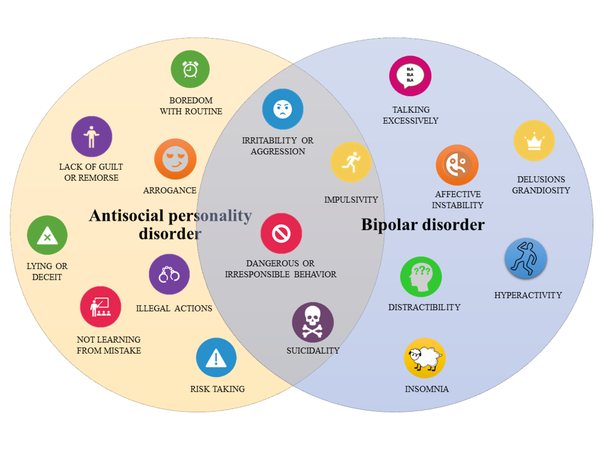
Scientists have repeatedly proven that a person in one way or another At the stage of disorder, the brain works differently.
In a healthy brain, strong relationship, there is a constant process of renewal. Unnecessary connections that a person does not use are erased, and new ones - grow up. In patients with bipolar disorder, the ability updated is broken, there are too many connections and the brain is already unable to navigate them. And since he cannot to navigate, people have abnormal thoughts or behavior.
Neurotrophin BDNF, which is involved in all processes preservation of neuronal cells and the creation of synapses, is considered the most studied in bipolar disorder. Such an interest in him and also in several neutrophins due to the discovery that antidepressants and mood stabilizers can act on these molecules, modulating their signaling pathways.
The amount of BDNF neutrophin in patients with bipolar disorder is underestimated in brain and blood, and preclinical studies have shown that chronic use of certain antidepressants and mood stabilizers such as lithium and valproic acid can increase its level in the brain of rats.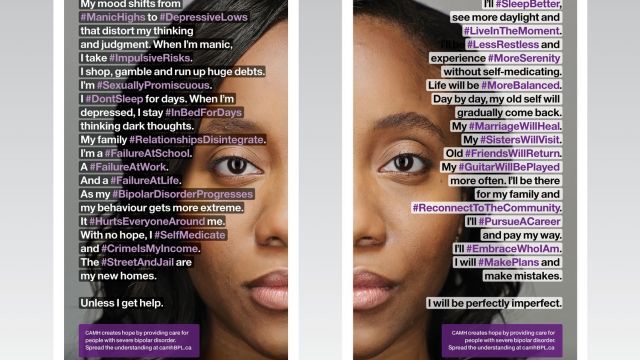 There are studies which confirm the underestimation of the level of nerve growth factor NGF in plasma in patients with bipolar disorder. Lithium also increases NGF and GDNF - glial neurotrophic factor in hippocampus, frontal cortex, occipital region and striatum. The neutrophins NGF and GDNF promote survival, regeneration of neurons and the emergence of new neural connections.
There are studies which confirm the underestimation of the level of nerve growth factor NGF in plasma in patients with bipolar disorder. Lithium also increases NGF and GDNF - glial neurotrophic factor in hippocampus, frontal cortex, occipital region and striatum. The neutrophins NGF and GDNF promote survival, regeneration of neurons and the emergence of new neural connections.
Fig. 3. Brain reactions during risky decision making in patients with mania, patients with depression and healthy people.
In 2001, scientists conducted an experiment where they asked people to decide neuropsychological task (Fig. 3). The people were divided into three groups - patients with mania, patients with depression and healthy People. We watched the reaction of the brain when making risky decisions. The subjects were told that there was a token that was hidden under one of six boxes, which are presented in different colors. The subjects had to guess whether the token was hidden under the red or blue box to win points. Less likely option blue in this example is also associated with a higher value gain to create conflict between reward and uncertainty.
Less likely option blue in this example is also associated with a higher value gain to create conflict between reward and uncertainty.
Patients with mania had increased activity in the area of the brain which is responsible for emotionality, and in the area that participates in strategic processes and management functions – on the contrary, it is underestimated. Patients with depression did not have significant differences in the activation of brain regions.
It is also known that psychosocial stress can also provoke the development of bipolar disorder.
With the clinical course of BAD, scientists have identified abnormalities in the axis hypothalamic-pituitary-adrenal (HPA), which is major mediator of the biological response to stress. This system releases hormones such as glucocorticoids and epinephrine. Glucocarticoids are steroid hormones that are released adrenal glands in response to any stress. Their production is strictly controlled and they affect all three neurotransmitter systems brain - serotonin, norepinephrine and dopamine, which are considered "depressive triad". The production of these hormones affects the synthesis neurotransmitters, their breakdown, the number of receptors (which convert neurotransmitters into a nerve impulse) and their correct work.
The production of these hormones affects the synthesis neurotransmitters, their breakdown, the number of receptors (which convert neurotransmitters into a nerve impulse) and their correct work.
In response to stress, the brain sends a command: to work out some kind of glucocorticoid that prepares the body for counter this stress by stimulating the production of neurotransmitters. To do this, in response to stress, the hypothalamus uses corticotropin-releasing hormone. That one is sent to the pituitary gland, where it causes it to produce adrenocorticotropic a hormone that is already sent to the adrenal glands for increased production of glucocorticoids. And glucocorticoids are already in in turn stimulate the production of the desired neurotransmitter. On this stage, as soon as the body feels that the glucocorticoid got into the blood, the hypothalamus and pituitary stop working, the body comes to a state of rest and the production of a neurotransmitter stops.
Anomalies occur when the negative feedback of the glucocorticoid cortisol to the hypothalamus and pituitary gland, which leads to permanent activation of the HPA axis and excessive release of cortisol. Violation of the negative feedback means that cortisol is not produced stops, its receptors become resistant to constant signals, which leads to an increase in the activity of pro-inflammatory immune mediators and downregulation of neurotrophic factors such as BDNF. The brain simply does not receive information about the fact that cortisol has developed and does not stop sending “impulses stress."
This process is also considered one of the theories of the origin clinical depression. Failures in this system lead to deterioration in sleep patterns, impaired fat burning, disruption in emotions and mood, decreased production of sex hormones, imbalance neurotransmitters, increased inflammation, and many other consequences. (fig.4)
Fig.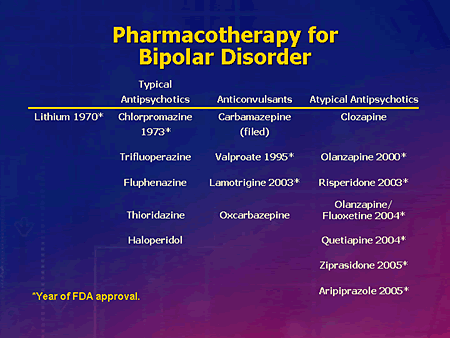 4. Visual reflection of the totality of recent studies of the neurobiological mechanisms of bipolar disorder. Biochemical pathways causing cell damage.
4. Visual reflection of the totality of recent studies of the neurobiological mechanisms of bipolar disorder. Biochemical pathways causing cell damage.
Summary
There is a lot of research in the field of neurobiological mechanisms of bipolar disorder, but it is still not clear what is the root cause and what is consequence. Several biochemical processes, not all of which shown in the figure above, interact at the same time, causing cell damage. A vicious circle in which numerous systems and mechanisms exacerbate and accelerate cell damage, synoptic dysfunction and impaired neurogenesis. It leads to progressive structural changes in the brain and cognitive decline, which scientists believe contributes to neuroprogression of bipolar disorder.
Bipolar affective disorder is not just the inability to take self-control or excessive emotionality. Like depression is mental illness that affects the work of everything organism.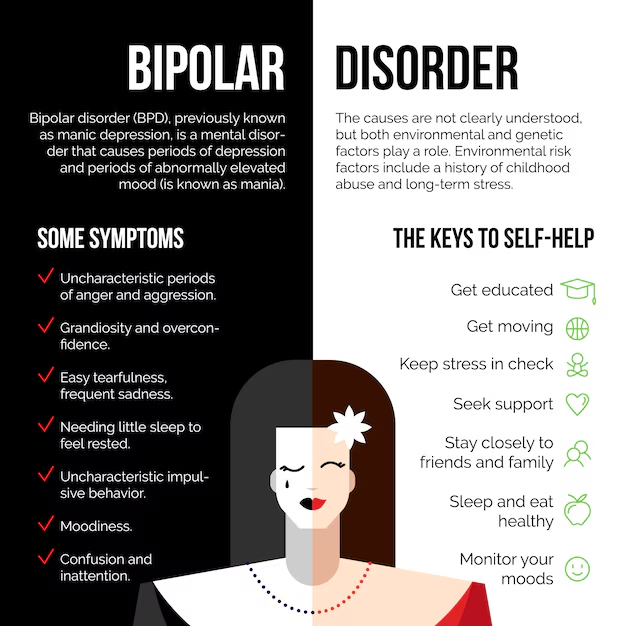
Sources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6282906/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7524405/#B18
- https://pubmed.ncbi.nlm.nih.gov/31746071/
- https://pubmed.ncbi.nlm.nih.gov/31043756/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3181872/
- https://pubmed.ncbi.nlm.nih.gov/11701607/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6489983/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4552246/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1525098/
- https://ironman.ru/news.php?id=5692
- https://www.youtube.com/watch?v=ShsJ6Jr53JI
- https://www.youtube.com/watch?v=RrWBhVlD1H8
Illustrations:
- https://www.healthshots.com/mind/mental-health/what-is-bipolar-disorder/
- https://www.