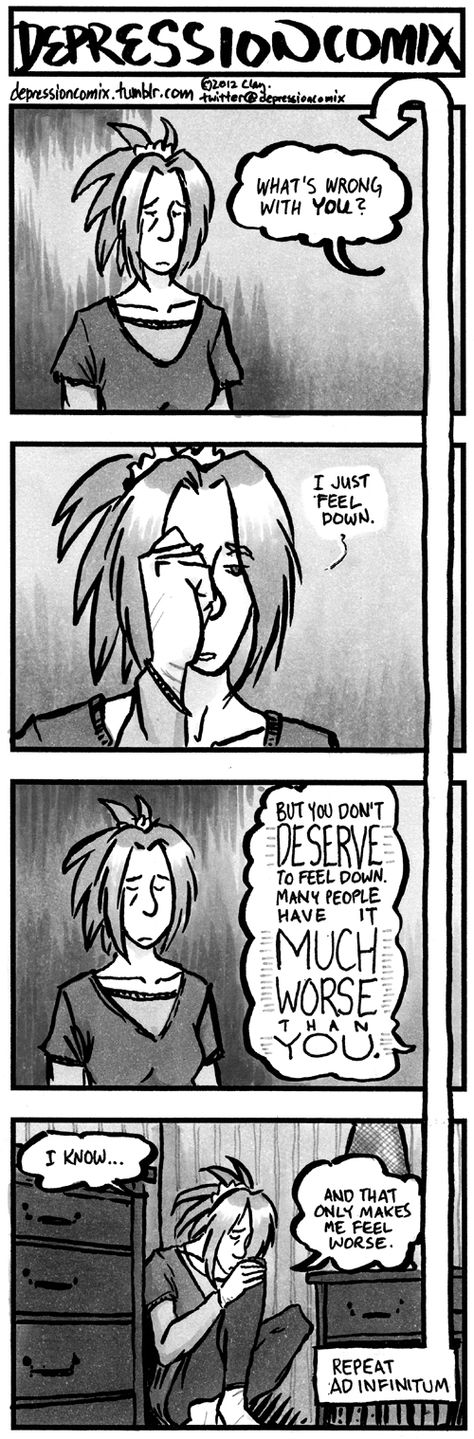
Misconception of depression
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly.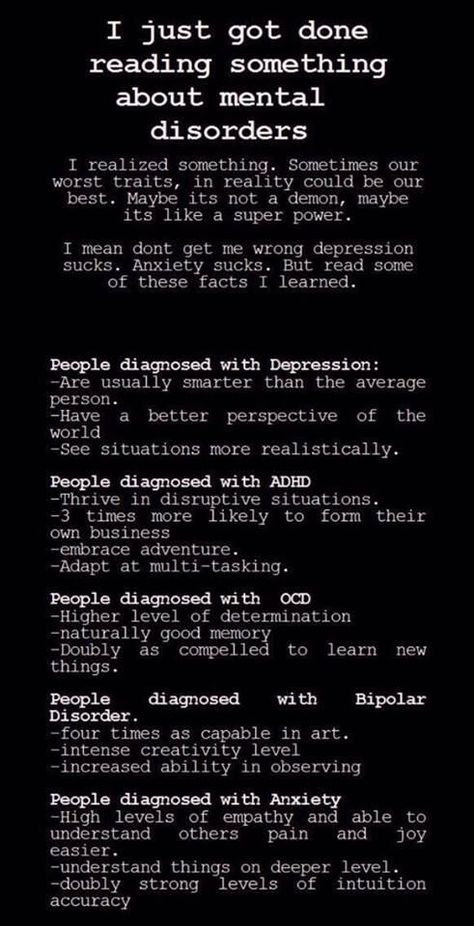 Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Depression
Basic Facts
- Depression is one of the most common mental disorders. It is estimated that more than 300 million people from all age groups suffer from it.
- Depression is the world's leading cause of disability and a significant "contributor" to the global burden of disease.
- Women are more susceptible to depression than men.
- In the worst case, depression can lead to suicide.
- Effective treatments for depression are available.
Review
Depress is common throughout the world: according to estimates, more than 300 million people suffer from it. Depression is different from normal mood changes and short-term emotional responses to problems in everyday life. Depression can become a serious health problem, especially if it lingers and becomes moderate or severe. It can lead to significant human suffering and poor functioning at work, school and family. In the worst cases, it can lead to suicide. Approximately 800,000 people die each year by suicide, the second leading cause of death among people aged 15-29years.
Depression is different from normal mood changes and short-term emotional responses to problems in everyday life. Depression can become a serious health problem, especially if it lingers and becomes moderate or severe. It can lead to significant human suffering and poor functioning at work, school and family. In the worst cases, it can lead to suicide. Approximately 800,000 people die each year by suicide, the second leading cause of death among people aged 15-29years.
Although effective treatments for depression are known, less than half of the world's sufferers receive such treatment (less than 10% in many countries). Barriers to receiving effective treatment include a lack of resources, a lack of trained health care providers, and social stigma associated with mental disorders. Another hurdle is imprecise estimation. In all countries, people with depression are often misdiagnosed, while other people who do not have the disorder are sometimes misdiagnosed and prescribed antidepressants.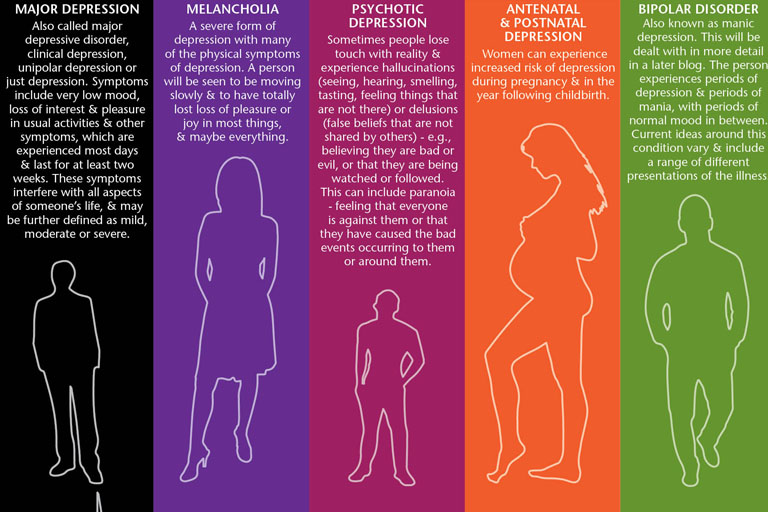
The burden of depression and other mental health problems is growing globally. In May 2013, the World Health Assembly adopted a resolution calling for a comprehensive, coordinated national response to mental disorders.
Types and symptoms
Depending on the number of symptoms and their severity, a depressive episode can be classified as mild, moderate or severe.
One major distinction is also made between depression in people who have already had a manic episode and depression in people who have not had a manic episode before. Both types of depression can be chronic (that is, over a long period of time) and relapse, especially if left untreated.
Recurrent depressive disorder: are recurrent depressive episodes. During such episodes, a person is in a depressed mood, loses interest and does not feel a sense of joy, and a decrease in vital energy leads to a decrease in his activity for at least two weeks. Many people with depression also suffer from anxiety symptoms, sleep and appetite disturbances, and may experience guilt or low self-esteem, poor concentration, and even medically unexplainable symptoms.
Depending on the number of symptoms and their severity, a depressive episode can be classified as mild, moderate or severe. A person with a mild depressive episode will have some difficulty in performing normal work and social activities, but in all likelihood will not stop functioning completely. During a major depressive episode, it is extremely unlikely that a person will be able to continue social life, work, and household chores except for a very limited range of activities.
Bipolar affective disorder: this type of depression usually consists of both manic and depressive episodes interrupted by periods of normal life. Manic episodes include an agitated or irritable mood, excessive activity, pressure of speech, inflated self-esteem, and decreased need for sleep.
Factors contributing to the development of depression and its prevention
Depression develops as a result of a complex interaction of social, psychological and biological factors. People who have experienced some kind of adverse event (job loss, bereavement, psychological trauma) are more likely to develop depression. Depression, in turn, can increase stress, disrupt normal functioning, worsen the living situation of the person suffering from it, and lead to even more severe depression.
People who have experienced some kind of adverse event (job loss, bereavement, psychological trauma) are more likely to develop depression. Depression, in turn, can increase stress, disrupt normal functioning, worsen the living situation of the person suffering from it, and lead to even more severe depression.
There is a relationship between depression and physical health. For example, cardiovascular disease can lead to depression and vice versa.
Prevention programs have been found to reduce the burden of depression. Effective community-based approaches to depression prevention include school-based positive thinking programs for children and adolescents.
Interventions for parents of children with behavioral problems may help reduce depressive symptoms in parents and improve outcomes in their children. Exercise programs for the elderly are also effective in preventing depression.
Diagnosis and treatment
There are effective treatments for moderate and severe depression.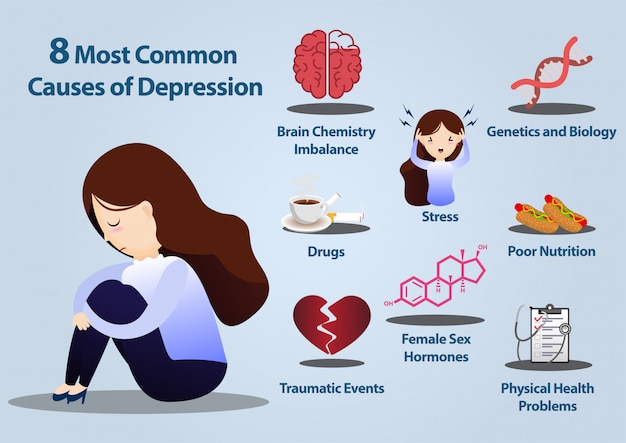 Health care providers may offer psychological treatments (such as behavioral activation, cognitive behavioral therapy [CBT], and interpersonal psychotherapy [IPT]) or antidepressants (such as selective serotonin reuptake inhibitors [SSRIs] and tricyclic antidepressants [TCAs]).
Health care providers may offer psychological treatments (such as behavioral activation, cognitive behavioral therapy [CBT], and interpersonal psychotherapy [IPT]) or antidepressants (such as selective serotonin reuptake inhibitors [SSRIs] and tricyclic antidepressants [TCAs]).
Health care providers need to be aware of the possible side effects of antidepressants, the options available for a given treatment (in terms of expertise and/or drug availability), and individual preferences. In the format of various types of psychological treatment, individual and / or group types of face-to-face psychological treatment carried out by specialists and volunteers under the supervision of specialists should be considered.
Psychosocial therapy is effective and should be the first line of treatment for mild depression. Antidepressants can be an effective form of treatment for moderate to severe depression, but they are not first-line treatment for mild depression. They should not be used to treat depression in children, and they are not first-line therapy for adolescents, among whom they should be used with caution.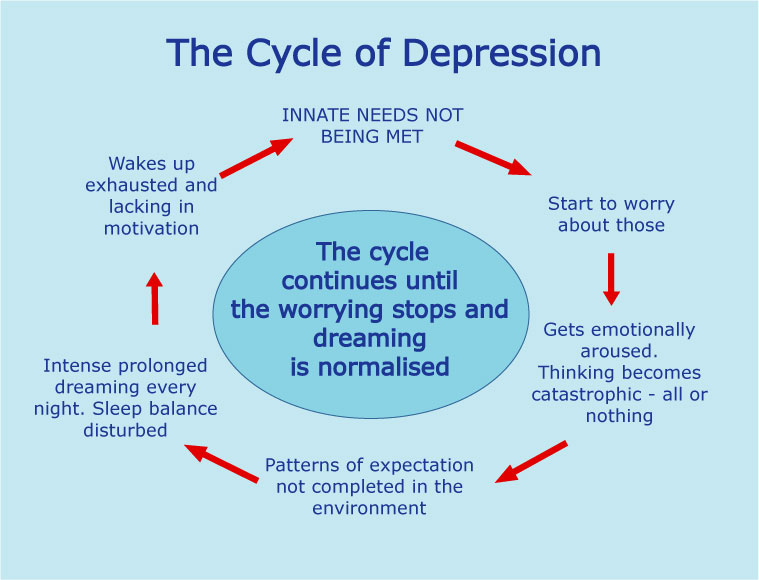
WHO activities
Depression is one of the priority conditions covered by the WHO Mental Health Action Program (mhGAP). The aim of the Program is to help countries scale up services for the treatment of people with mental, neurological, drug and substance use problems by non-mental health professionals.
The program recognizes that with proper care, psychosocial support and medication, tens of millions of people with mental disorders, including depression, could lead normal lives, even in resource-poor settings.
Campaign Brief
Celebrated every year on 7 April, the founding day of WHO, World Health Day is a unique opportunity to mobilize action on a health topic of concern to people around the world.
The theme of the 2017 World Health Day campaign will be depression.
Depression affects people of all ages, all population groups and in all countries. Depression causes mental distress, affects a person's ability to perform even the simplest daily tasks, and can sometimes be disastrous for a person's relationships with loved ones and friends, as well as a person's ability to earn a living.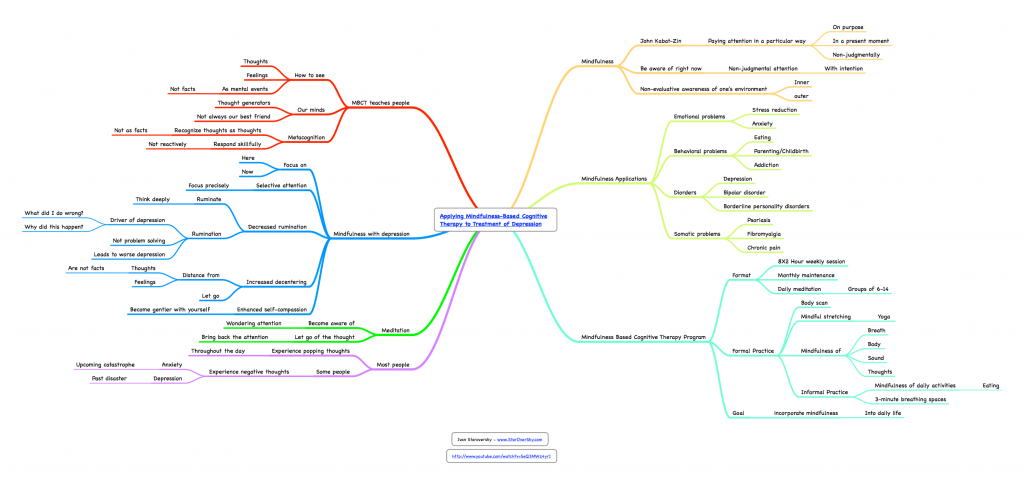 In extreme cases, depression can lead to suicide - today the second leading cause of death among people aged 15-29years.
In extreme cases, depression can lead to suicide - today the second leading cause of death among people aged 15-29years.
However, depression is preventable and treatable. A deeper understanding of what depression is and how it can be prevented or treated will help dispel the negative stereotypes associated with depression and encourage more people to seek help.
This guide is for you
If you are reading this guide, you might also be interested in becoming a campaigner. This is great, because we need your support to achieve the goals of the campaign.
Whether you work for government, an NGO or the media, whether you are a doctor, teacher, journalist, blogger, parent, or just someone who has heard of the campaign and would like to get involved, this is guide for you.
What we want to achieve
The overall goal of this one-year campaign, which will be launched on World Mental Health Day on October 10, 2016, is to reach as many people with depression as possible in all countries asked for help and received it.
More specifically, we want to achieve the following goals:
- the general public will have a better understanding of depression, its causes and possible consequences, including suicide, as well as what types of help exist or can be available to prevent and treat depression;
- people with untreated depression decide to seek help;
- family members, friends and colleagues of people with depression will be able to support them.
What is depression?
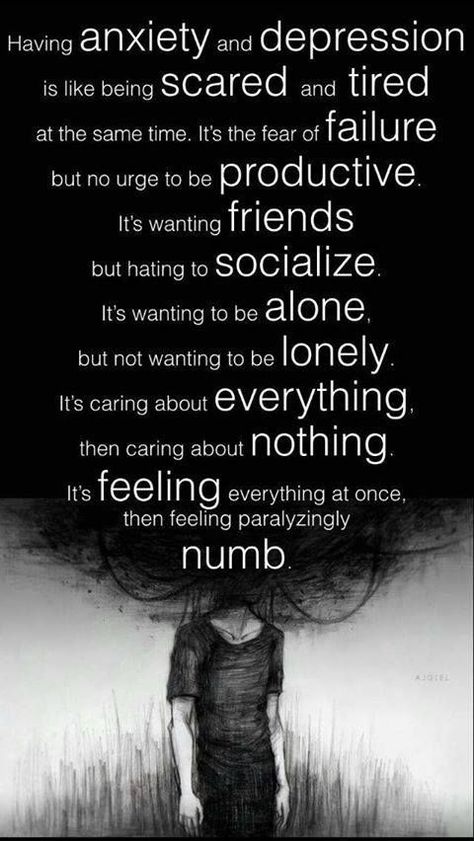
Depression is an illness characterized by a persistent state of despondency and loss of interest in activities that would normally bring satisfaction, as well as an inability to do daily activities for at least two weeks. In addition, people with depression usually have several of the following symptoms: lack of energy, decreased appetite, drowsiness or insomnia, anxiety, decreased concentration, indecision, restlessness, feelings of worthlessness, guilt or despair, and thoughts of hurting oneself harm or suicide.
Central element of the campaign
The focus of the campaign is the question of the great importance of discussing the problem with patients as an essential condition for recovery. Around the world, negative stereotypes associated with mental illness, including depression, continue to prevent people from seeking help. Discussing depression with a family member, friend, or health care professional; in larger groups of people, such as at school, in the workplace and at social events; in society, in the news media, blogs or social networks, all help to break down negative stereotypes and encourage more and more people to finally seek help.
Motto
Campaign motto: "Depression: let's talk."
Who is our target audience
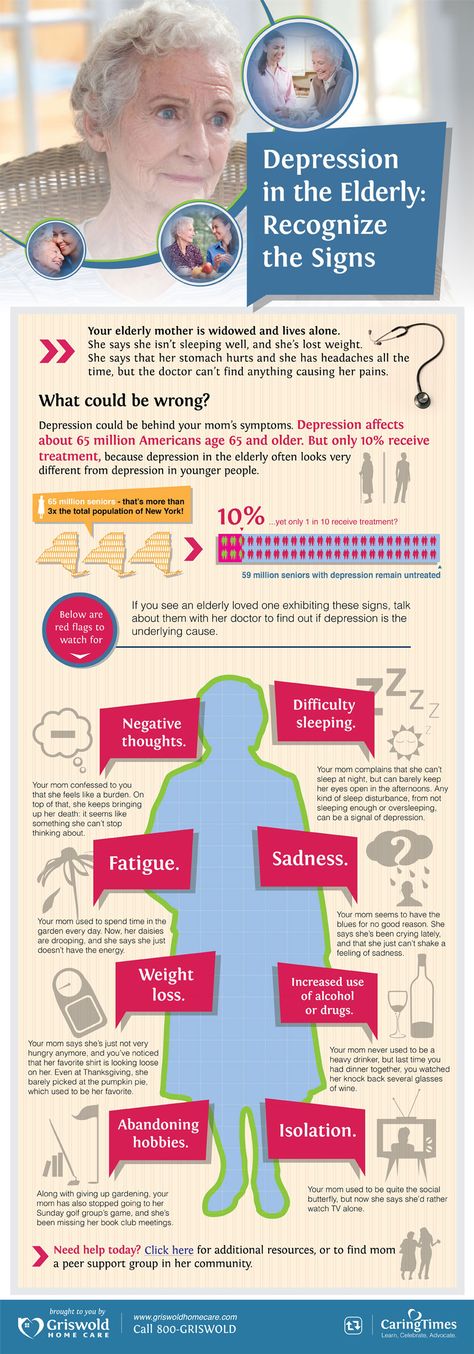
Anyone can get depressed. Therefore, our campaign is aimed at every person, regardless of age, gender or social status. At the World Health Organization, we have decided to pay special attention to the three populations most affected by this problem to a much greater extent than others: young people aged 15-24 years, women of childbearing age (especially young mothers), and older people (over 60 years).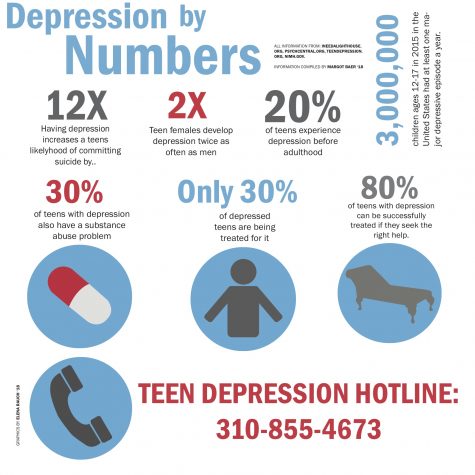 On the occasion of the campaign, information materials were prepared especially for these categories of the population.
On the occasion of the campaign, information materials were prepared especially for these categories of the population.
Campaign messages
- Depression is a common mental disorder that affects people of all ages and social groups in all countries of the world.
- The risk of depression is exacerbated by poverty, unemployment, life events such as the loss of a loved one or the breakup of a relationship, physical illness, and alcohol or drug problems.
- Depression causes mental distress, affects a person's ability to carry out even the simplest daily tasks, and can sometimes be disastrous for a person's relationships with loved ones and friends.
- Untreated depression can prevent a person from working and participating in family and community life.
- In extreme cases, depression can lead to suicide.
- There are effective ways to prevent and treat depression. Typically, depression is treated with either talk therapy, antidepressants, or a combination of the two.

- Overcoming the negative stereotypes associated with depression will help more people seek help.
- Talking to people you trust can be the first step to getting rid of depression.
How does depression affect your well-being?
Each of us has heard the word "depression". But do we fully understand what it is? Let's try to understand the essence of this disease and how it affects our psychological and physical well-being.
Contents
- What is depression?
- Symptoms of depression: psychological state
- Symptoms of depression: physical condition
- How can a mental disorder cause pain?
- Why does depression occur and who is at risk?
- How to make a diagnosis?
- How to treat?
What is depression?
In many people's minds, the word "depression" is synonymous with bad mood and depression. To some extent this corresponds to the truth, but in reality everything is much more complicated.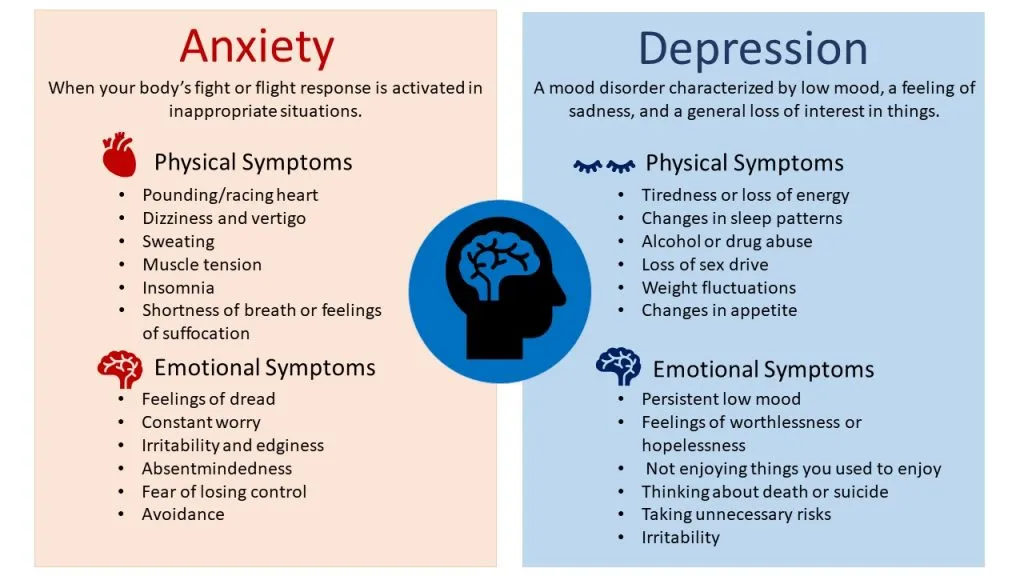
Depression, or major depressive disorder, is an illness that causes persistent feelings of sadness, loss of interest in life, and a host of other symptoms. It affects how a person feels, thinks and behaves and can lead to a variety of both emotional and physical problems. It is important to understand that depression is a serious mental disorder that requires treatment and observation by a specialist, and not to be confused with other problems.
For example, constant fatigue and unwillingness to get out of bed in the morning may indicate a lack of vitamins, iron, magnesium or other trace elements.
Although it is possible to take tests for the level of these substances on your own, you should not do this: it will be better if the necessary checks are prescribed and carried out by a doctor - this will save you unnecessary anxiety and expenses.
If you feel bad, experience negative emotions and do not find strength for everyday activities, then this is also not a reason to immediately suspect depression.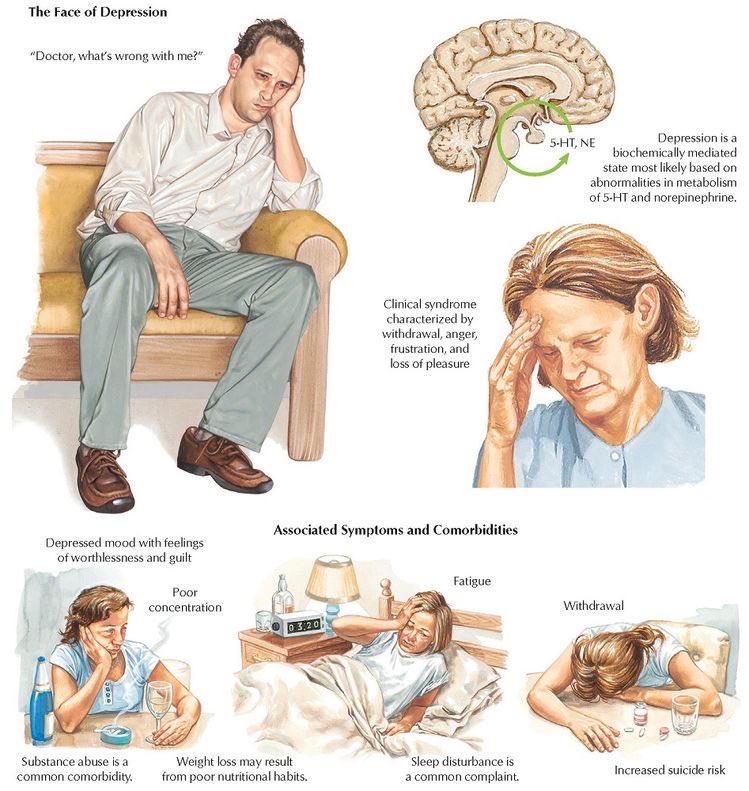 It is likely that the lowering of mood is a reaction to severe stress or bad events that have occurred in your life. Experts point out the following differences between "natural" negative emotions and depression:
It is likely that the lowering of mood is a reaction to severe stress or bad events that have occurred in your life. Experts point out the following differences between "natural" negative emotions and depression:
- If a strong grief has occurred in a person's life (for example, the death of a loved one), then painful feelings come in waves, often mixed with positive memories. With depression, the mood and interest in life are constantly reduced, for two or more weeks.
- In severe sadness or grief, a person's self-esteem is at the same level, and in depression, feelings of worthlessness and self-loathing are common.
- In severe grief, thoughts of one's own death may appear sporadically when a person thinks about "joining" with a deceased loved one. In a depressive disorder, such thoughts arise from a sense of the meaninglessness of one's life or from an inability to cope with problems.
In any case, the symptoms of true depression are not limited to those listed above.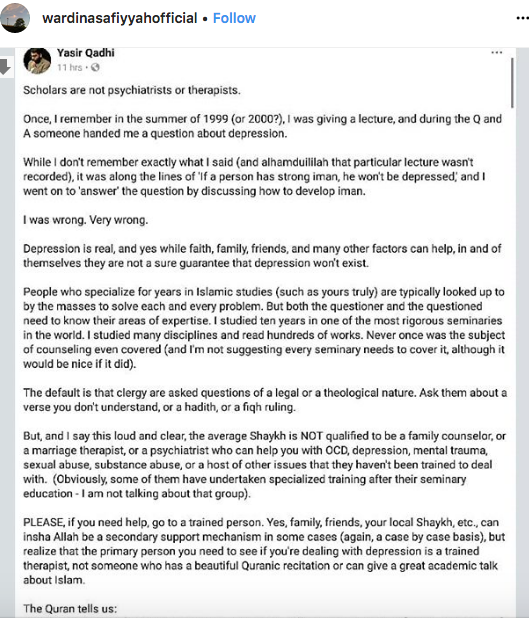 They can be divided into psychological and physical.
They can be divided into psychological and physical.
Symptoms of depression: psychological state
Symptoms of depression affecting the psychological state of a person include:
● Feelings of sadness, hopelessness, emptiness.
● Outbursts of anger and irritability even for minor reasons.
● Loss of interest and pleasure in activities that normally bring joy (sports, hobbies, meeting loved ones).
● Attacks of restlessness, agitation, nervousness.
● Feelings of worthlessness or guilt, obsession with past failures.
● Problems with concentration and memory.
● Recurrent thoughts about one's own death, attempts to hurt oneself or otherwise harm oneself.
In children and adolescents, psychological symptoms are generally the same as those listed above, but they may be accompanied by a decrease in school performance, unwillingness to attend classes, avoidance of communication with classmates and friends, tearfulness.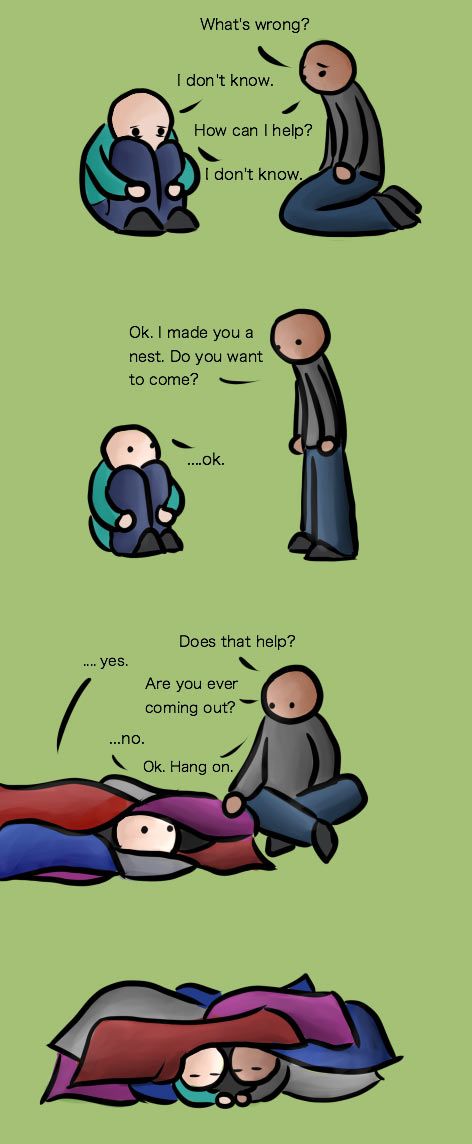
Symptoms of depression: physical condition
The physical manifestations of depressive disorder include the following symptoms:
● Sleep disorders: insomnia or drowsiness.
● Constant fatigue and lack of energy, due to which even ordinary daily activities (cleaning, showering) require significant physical effort.
● Disorders of appetite: its decrease or, conversely, its increase. The result is weight loss or gain.
● Pain for no apparent reason.
● Convulsions.
● Digestive problems.
How can a mental disorder cause pain?
Experts say that disturbances in the normal functioning of the body and pain of unknown origin - that is, occurring without an apparent physical cause - are often a symptom of depression. Pain can occur in the joints, in the limbs, in the back and head; in addition, a person may experience problems with the gastrointestinal tract, fatigue, sleep and appetite disorders, changes in psychomotor activity.
Experts say that both types of symptoms are related - the more pain, the more severe the depressive disorder. In addition, pain can be a kind of "indicator" - according to one study, which studied data from more than 1,000 people diagnosed with depression from 14 countries, 69% of patients first came to the doctor because of unclear pain and other physiological problems. This connection between pain and depression can interfere with diagnosis: first, the doctor, of course, will send the patient with a headache or indigestion for further specialized examinations, but if they do not show anything, and the doctor does not have enough knowledge, he may not suspect depression and be in a diagnostic impasse.
Why is this happening? Physical pain and depression have a deep biological connection. In our body there are biologically active substances called neurotransmitters - they transmit electrochemical impulses from nerve cells and neurons to muscles and other cells of the body. Neurotransmitters that affect both pain and mood include serotonin and norepinephrine.
Neurotransmitters that affect both pain and mood include serotonin and norepinephrine.
Changes in the function and effect of these neurotransmitters, and how they interact with neurons and nerve cells involved in maintaining mood stability, may play an important role in the onset of depression.
The reasons why neurotransmitters start to work "wrong" are very complex, and scientists continue to study them.
Why does depression occur and who is at risk?
According to experts, women are more prone to depression than men, and the median age of onset is 32 years (this means that half of the people who receive a diagnosis of depression in their lifetime will already have their first depressive episode by this age) . However, this is all - experts cannot give a more detailed portrait of a “typical patient”, because anyone can become a victim of the disease.
However, there are a number of factors that increase the risk of developing a depressive disorder:
- Genetics.
 Depression can be inherited: studies show that genetics can contribute up to about 40% to the development of depression, and the likelihood that the twin of a person suffering from depression will also receive this diagnosis is about 70%. In 2019, scientists conducted a meta-analysis of data on more than 800 thousand people and found 102 genetic variants associated with the development of depression.
Depression can be inherited: studies show that genetics can contribute up to about 40% to the development of depression, and the likelihood that the twin of a person suffering from depression will also receive this diagnosis is about 70%. In 2019, scientists conducted a meta-analysis of data on more than 800 thousand people and found 102 genetic variants associated with the development of depression. - Environmental factors. If a person has experienced severe stress or psychological trauma in his life (for example, a child had a difficult childhood, he was subjected to violence, lived in conditions of extreme poverty), then the likelihood of developing a depressive disorder increases.
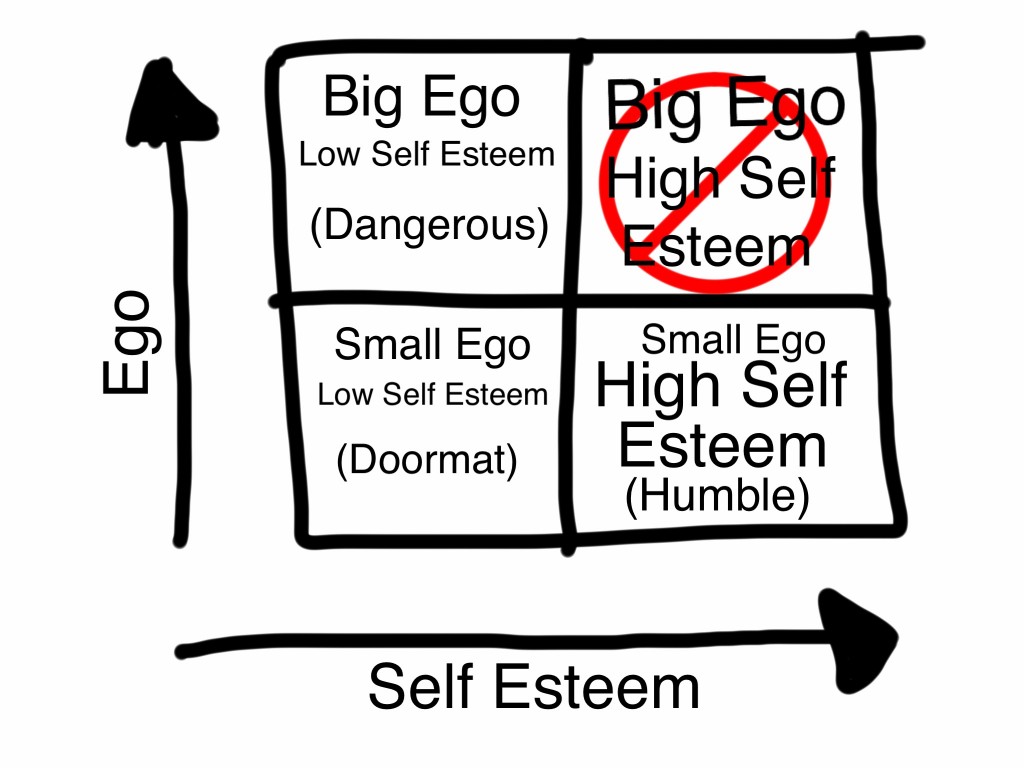
- Personal qualities of a person. People with low self-esteem, easily succumbed to stress, and prone to pessimism are at greater risk.
- Hormonal changes due to pregnancy, postpartum, menopause, and thyroid disorders.
- Other serious health problems: Parkinson's disease, diabetes, heart disease, cancer.
How to make a diagnosis?
Not only the well-being of a person, but also his life can depend on the correct diagnosis and timely treatment. To diagnose a depressive disorder, doctors must conduct a set of studies.
- First of all, a psychiatrist should talk to a person about his state of health, thoughts, behavior. The patient may be asked to fill out a special questionnaire that contains various signs of depression. For a diagnosis to be made, the patient must experience a certain amount of these symptoms for two or more weeks over most of the day.
- General medical examination to find out whether the pain or other disturbances of the body - of course, if present - are of a physical nature.
How to treat?
Despite the seriousness of the disease, do not despair when making a diagnosis. Depressive disorder is treated using different methods:
- Antidepressants - these drugs affect the biochemical processes in the brain, the work of neurotransmitters.
 It is important to know that antidepressants may not have an effect for several weeks after the start of treatment - the patient may not notice improvement within 2-3 months. Sometimes the doctor is not immediately able to choose the right dosage or drug, in addition, antidepressants can have side effects, so they should never be taken on their own, without prescription and constant monitoring by the doctor.
It is important to know that antidepressants may not have an effect for several weeks after the start of treatment - the patient may not notice improvement within 2-3 months. Sometimes the doctor is not immediately able to choose the right dosage or drug, in addition, antidepressants can have side effects, so they should never be taken on their own, without prescription and constant monitoring by the doctor. - Psychotherapy. In cases of mild depression, psychotherapy can be used as the main treatment, in more severe cases, in addition to antidepressants. Usually, specialists use cognitive behavioral therapy - it is focused on helping a person to focus on the present, solve current problems, recognize thoughts and behavior distorted by depression and correct them. This treatment may take several weeks or months.
- Depression is usually treated with medication and psychotherapy. But in extremely severe cases, when the previous treatment has not helped, the method of electroconvulsive (or electroconvulsive) therapy can be used.