Mental disorder screening test
SAMHSA’s National Helpline | SAMHSA
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Main page content
-
SAMHSA’s National Helpline is a free, confidential, 24/7, 365-day-a-year treatment referral and information service (in English and Spanish) for individuals and families facing mental and/or substance use disorders.
Also visit the online treatment locator.
SAMHSA’s National Helpline, 1-800-662-HELP (4357) (also known as the Treatment Referral Routing Service), or TTY: 1-800-487-4889 is a confidential, free, 24-hour-a-day, 365-day-a-year, information service, in English and Spanish, for individuals and family members facing mental and/or substance use disorders.
This service provides referrals to local treatment facilities, support groups, and community-based organizations.
Also visit the online treatment locator, or send your zip code via text message: 435748 (HELP4U) to find help near you. Read more about the HELP4U text messaging service.
The service is open 24/7, 365 days a year.
English and Spanish are available if you select the option to speak with a national representative. Currently, the 435748 (HELP4U) text messaging service is only available in English.
In 2020, the Helpline received 833,598 calls. This is a 27 percent increase from 2019, when the Helpline received a total of 656,953 calls for the year.
The referral service is free of charge. If you have no insurance or are underinsured, we will refer you to your state office, which is responsible for state-funded treatment programs. In addition, we can often refer you to facilities that charge on a sliding fee scale or accept Medicare or Medicaid. If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
If you have health insurance, you are encouraged to contact your insurer for a list of participating health care providers and facilities.
The service is confidential. We will not ask you for any personal information. We may ask for your zip code or other pertinent geographic information in order to track calls being routed to other offices or to accurately identify the local resources appropriate to your needs.
No, we do not provide counseling. Trained information specialists answer calls, transfer callers to state services or other appropriate intake centers in their states, and connect them with local assistance and support.
-
Suggested Resources
What Is Substance Abuse Treatment? A Booklet for Families
Created for family members of people with alcohol abuse or drug abuse problems. Answers questions about substance abuse, its symptoms, different types of treatment, and recovery. Addresses concerns of children of parents with substance use/abuse problems.
Addresses concerns of children of parents with substance use/abuse problems.It's Not Your Fault (NACoA) (PDF | 12 KB)
Assures teens with parents who abuse alcohol or drugs that, "It's not your fault!" and that they are not alone. Encourages teens to seek emotional support from other adults, school counselors, and youth support groups such as Alateen, and provides a resource list.After an Attempt: A Guide for Taking Care of Your Family Member After Treatment in the Emergency Department
Aids family members in coping with the aftermath of a relative's suicide attempt. Describes the emergency department treatment process, lists questions to ask about follow-up treatment, and describes how to reduce risk and ensure safety at home.Family Therapy Can Help: For People in Recovery From Mental Illness or Addiction
Explores the role of family therapy in recovery from mental illness or substance abuse. Explains how family therapy sessions are run and who conducts them, describes a typical session, and provides information on its effectiveness in recovery.
For additional resources, please visit the SAMHSA Store.
Last Updated: 08/30/2022
SAMHSA Behavioral Health Treatment Services Locator
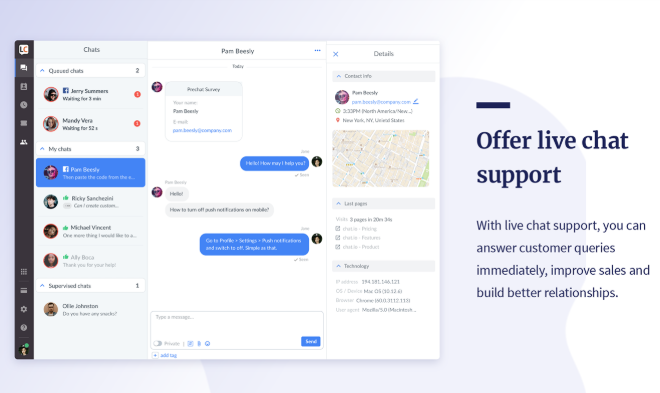
HomeWelcome to the Behavioral Health Treatment Services Locator, a confidential and anonymous source of information for persons seeking treatment facilities in the United States or U.S. Territories for substance use/addiction and/or mental health problems.
PLEASE NOTE: Your personal information and the search criteria you enter into the Locator is secure and anonymous. SAMHSA does not collect or maintain any information you provide.
Please enter a valid location.
please type your address
-
FindTreatment.
 gov
gov Millions of Americans have a substance use disorder. Find a treatment facility near you.
-
988 Suicide & Crisis Lifeline
Call or text 988
Free and confidential support for people in distress, 24/7.
-
National Helpline
1-800-662-HELP (4357)
Treatment referral and information, 24/7.

-
Disaster Distress Helpline
1-800-985-5990
Immediate crisis counseling related to disasters, 24/7.
- Overview
- Locator OverviewLocator Overview
- Locator OverviewLocator Overview
- Finding Treatment
- Find Facilities for VeteransFind Facilities for Veterans
- Find Facilities for VeteransFind Facilities for Veterans
- Facility Directors
- Register a New FacilityRegister a New Facility
- Register a New FacilityRegister a New Facility
- Other Locator Functionalities
- Download Search ResultsDownload Search Results
- Use Google MapsUse Google Maps
- Print Search ResultsPrint Search Results
- Use Google MapsUse Google Maps
- Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
 Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers).
Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). - Icon from Find practitioners and treatment programs providing buprenorphine for opioid addiction (heroin or pain relievers). Find programs providing methadone for the treatment of opioid addiction (heroin or pain relievers).
The Locator is authorized by the 21st Century Cures Act (Public Law 114-255, Section 9006; 42 U.S.C. 290bb-36d). SAMHSA endeavors to keep the Locator current. All information in the Locator is updated annually from facility responses to SAMHSA’s National Substance Use and Mental Health Services Survey (N-SUMHSS). New facilities that have completed an abbreviated survey and met all the qualifications are added monthly. Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Updates to facility names, addresses, telephone numbers, and services are made weekly for facilities informing SAMHSA of changes. Facilities may request additions or changes to their information by sending an e-mail to [email protected], by calling the BHSIS Project Office at 1-833-888-1553 (Mon-Fri 8-6 ET), or by electronic form submission using the Locator online application form (intended for additions of new facilities).
Take a depression test. Rate the severity of the disorder
2017-08-29
The presented test was developed on the basis of the "Hospital Anxiety and Depression Scale" to identify and assess the severity of anxiety disorder, depression. This test is usually used as a screening test, while for a more detailed study of the identified violations, an examination by a psychotherapist or psychiatrist is recommended.
note
Test results are approximate, indicative. An experienced doctor can both confirm them and refute them. If you are concerned about your mental state, do not put off a visit to a psychotherapist or psychiatrist.
If you are concerned about your mental state, do not put off a visit to a psychotherapist or psychiatrist.
| No. | Question | Your reply | |
|---|---|---|---|
| one. | Something that brought me great pleasure and now makes me feel the same way. | Definitely so Probably so Only to a very small extent so Not so at all | |
| 2. | I am able to laugh and see the funny in this or that event. | Definitely so Probably so Only to a very small extent so Not so at all | |
| 3. | I feel cheerful. | Not at all Very rarely Sometimes All the time | |
| four. | It seems to me that I began to do everything very slowly. | Most of the time Often Sometimes Very often | |
| 5. | I don't care about my appearance. | It's so I don't pay as much attention to it as I should Maybe I pay less attention to it I take care of myself the same way as before | |
| 6. | I believe that my activities (occupations, hobbies) can bring me a sense of satisfaction. | Same as usual Yes, but not to the same extent as before Significantly less than usual I don't think so at all | |
| 7. | I can enjoy a good book, radio or TV program. | Often Sometimes Rarely Very rarely | |
Author: Specialist of the Alliance Mental Health Center
TsMZ "Alliance"
Specialists
Gonopolskaya
Victoria Nikolaevna
Deputy Head of the Center, psychotherapist, psychiatrist
over 30 years experience
92 positive reviews
- Individual psychotherapy
- Family therapy
- Psychopharmacotherapy
- Rational psychotherapy
Sign up for an appointment
Ashmeib
Nino Anatolyevna
Psychotherapist, Psychiatrist
The highest category
Experience for more than 15 years
37 Positive reviews
- SUGESTIVAL CENTERS
- Reconstructive personality psychotherapy
- Rational psychotherapy
- Individual psychotherapy
make an appointment
Fastovets
Elena Vladimirovna
Psychotherapist, psychiatrist
work experience over 15 years
59 positive reviews
- Individual psychotherapy
- Family therapy
- Cognitive behavioral therapy
- Reconstructive personality psychotherapy
make an appointment
Depression - more information
- Depression
- Recurrent depressive disorder
- Anxiety depressive disorder
- How to get rid of depression and stress: a step-by-step guide
Screening for cognitive impairment - Neurology - LiveJournal
Relevance . Cognitive functions (CF) are the most complex (higher) functions of the brain, with the help of which the process of rational cognition of the world and interaction with it are carried out. Being the most complexly organized, CPs are at the same time very vulnerable in various pathological conditions. CF disorders are observed both in primary organic brain damage (for example, neurodegeneration processes in Parkinson's disease) and in encephalopathy secondary to various somatic or endocrine diseases (for example, Hashimoto's encephalopathy [more]). Therefore, CF disorders are an interdisciplinary problem that is regularly encountered not only by neurologists and psychiatrists, but also by general practitioners, endocrinologists, cardiologists, and doctors of other specialties.
Cognitive functions (CF) are the most complex (higher) functions of the brain, with the help of which the process of rational cognition of the world and interaction with it are carried out. Being the most complexly organized, CPs are at the same time very vulnerable in various pathological conditions. CF disorders are observed both in primary organic brain damage (for example, neurodegeneration processes in Parkinson's disease) and in encephalopathy secondary to various somatic or endocrine diseases (for example, Hashimoto's encephalopathy [more]). Therefore, CF disorders are an interdisciplinary problem that is regularly encountered not only by neurologists and psychiatrists, but also by general practitioners, endocrinologists, cardiologists, and doctors of other specialties.
At the same time, an analysis of the patient's CF status is necessary both to establish a diagnosis (including to establish the stage of the disease, for example, in chronic cerebral ischemia) and to clarify the characteristics of the disease, and to develop optimal patient management tactics (therapeutic and medical social). It should also be remembered that in the absence of timely prescribed therapy, acute CI can eventually turn into a chronic form - dementia and become a heavy burden for the patient's relatives ([9].0200!!! ] an individually developed plan for the management of patients with CI in many cases can reduce the severity of existing disorders and prevent or delay the onset of dementia).
It should also be remembered that in the absence of timely prescribed therapy, acute CI can eventually turn into a chronic form - dementia and become a heavy burden for the patient's relatives ([9].0200!!! ] an individually developed plan for the management of patients with CI in many cases can reduce the severity of existing disorders and prevent or delay the onset of dementia).
Please note ! Impaired CP (or cognitive impairment [CI]) can occur at any age, but is most common in the elderly. In this regard, brief screening for CI is necessary in [all] patients (especially hospitalized) in the older age group. In the outpatient (polyclinic) link, the basis for analyzing the patient's CF status is complaints of memory loss or a decrease in mental performance, which (complaints) can come from both the patient himself and his relatives, friends, colleagues (information from this circle of people is important diagnostic feature, since the patient's assessment of the state of his CF is not always objective).
Investigation of KN is usually carried out in two stages. [ 1 ] At the first stage, the attending physician, regardless of the specialty, conducts a brief screening (from the English “screening” is a concept that includes a number of measures to detect and prevent diseases), the purpose of which is to identify patients who are likely to have CI. [ 2 ] At the second stage [of CI research], a [detailed] neuropsychological study is carried out, for which a neuropsychologist is usually involved - he evaluates various cognitive functions and makes a conclusion about the degree and qualitative features of the identified disorders, as well as their impact on the patient's daily life . These data allow the diagnosis of dementia or moderate CI (MCI) to be established.
One of the most widely used tests for assessing cognitive functions is the Mini-mental State Examination (MMSE), which consists of 9 tasks, 30 questions. The test is conditionally divided into 2 parts: the first evaluates orientation, attention, perception and memory, the second - speech. The maximum score on the test is 30 points, the boundary value, according to different authors, is 24 - 25 points. The disadvantages of MMSE include the fact that it does not include an assessment of executive functions, its implementation takes an average of about 8 minutes, among the tasks there are those that require drawing, which is problematic for visual impairments, muscle weakness; it is of little use in diagnosing MCI (a more sensitive tool for diagnosing MCI is the Montreal Cognitive Assessment Scale - MoCA [instruction]). There are reports that very low MMSE scores (less than 10 points out of 30) in patients who did not suffer from overt dementia before hospitalization indicate the development of acute CI within the framework of delirium.
The maximum score on the test is 30 points, the boundary value, according to different authors, is 24 - 25 points. The disadvantages of MMSE include the fact that it does not include an assessment of executive functions, its implementation takes an average of about 8 minutes, among the tasks there are those that require drawing, which is problematic for visual impairments, muscle weakness; it is of little use in diagnosing MCI (a more sensitive tool for diagnosing MCI is the Montreal Cognitive Assessment Scale - MoCA [instruction]). There are reports that very low MMSE scores (less than 10 points out of 30) in patients who did not suffer from overt dementia before hospitalization indicate the development of acute CI within the framework of delirium.
read also post: Delirium in somatic medicine (on laesus-de-liro.livejournal.com) [read]
Pay attention ! In acute CI, the use of short scales, such as the Confusion Assessment Method for Intensive Care Units (ICU), together with the history, objective and laboratory and instrumental studies, is usually sufficient.
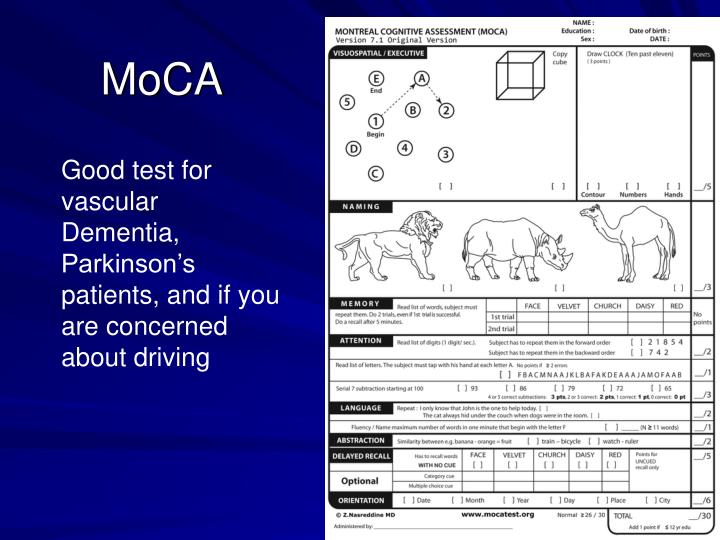
As noted, the use of MMSE (and MoCA) requires a relatively long time (8 - 10 minutes), which is not always possible in outpatient practice. In this regard, it is important for the doctor to know shorter scales for assessing CI, the use of which takes 2-3 minutes (including which can be used in the hospital at the patient's bedside without interrupting the usual bypass).
To detect gross (pronounced) cognitive impairment (that is, dementia) in general somatic practice, the optimal screening tool is the Mini-Cog test (Mini-Cog), proposed by S. Borson et al. (2000) and includes simple memory tasks and a clock drawing test.
There is also the following interpretation of the test results [Mini-Cog]: [ 1 ] if the patient remembered all three words, then there are no gross cognitive impairments; if he did not remember any, that is; [ 2 ] if the patient remembered two or one word, then at the next stage the clock pattern is analyzed; [ 3 ] if the drawing is correct, then there are no gross cognitive impairments;
The main advantage of the Mini-Cog technique lies in its high information content, while being simple and fast, which is very important for non-core specialists. The sensitivity of the test is 99%, the specificity is 93%. It takes about 3 minutes for the patient to complete the test, and the interpretation of the results is extremely simple - the test results are evaluated qualitatively, in other words [ + ] whether the patient has disorders or [ - ] does not. The technique does not provide for a scoring, as well as gradation of cognitive impairment according to the severity, which is not the task of endocrinologists and general practitioners. The Mini-Cog technique can be used to diagnose both vascular and primary degenerative cognitive impairments, as it includes memory tests and "frontal" functions (clock drawing test). The test can be used quite easily in people with speech disorders, a language barrier. The main disadvantage of this technique is its low sensitivity in relation to mild and moderate cognitive impairment. For their diagnosis, more sophisticated tools should be used, such as the MMSE or MoCA scale.
The sensitivity of the test is 99%, the specificity is 93%. It takes about 3 minutes for the patient to complete the test, and the interpretation of the results is extremely simple - the test results are evaluated qualitatively, in other words [ + ] whether the patient has disorders or [ - ] does not. The technique does not provide for a scoring, as well as gradation of cognitive impairment according to the severity, which is not the task of endocrinologists and general practitioners. The Mini-Cog technique can be used to diagnose both vascular and primary degenerative cognitive impairments, as it includes memory tests and "frontal" functions (clock drawing test). The test can be used quite easily in people with speech disorders, a language barrier. The main disadvantage of this technique is its low sensitivity in relation to mild and moderate cognitive impairment. For their diagnosis, more sophisticated tools should be used, such as the MMSE or MoCA scale.
You can read about all brief methods for screening for CI that can be used by a therapist in everyday practice in the article “Identification of cognitive deficits in the practice of a therapist: a review of screening scales” by M.