Mdma schizophrenia treatment
MDMA for the Treatment of Negative Symptoms in Schizophrenia
Review
. 2022 Jun 7;11(12):3255.
doi: 10.3390/jcm11123255.
Mitchell D Arnovitz 1 , Andrew J Spitzberg 1 , Ashkhan J Davani 1 , Nehal P Vadhan 1 2 3 , Julie Holland 4 , John M Kane 1 2 3 , Timothy I Michaels 1 2
Affiliations
Affiliations
- 1 Department of Psychiatry, The Zucker Hillside Hospital, Northwell Health, Queens, NY 11004, USA.
- 2 Department of Psychiatry, The Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY 11549, USA.
- 3 Institute of Behavioral Science, Feinstein Institutes for Medical Research, Manhasset, NY 11030, USA.
- 4 Private Practice, New York City, NY 10016, USA.
- PMID: 35743326
- PMCID: PMC9225098
- DOI: 10.3390/jcm11123255
Free PMC article
Review
Mitchell D Arnovitz et al. J Clin Med. .
J Clin Med. .
Free PMC article
. 2022 Jun 7;11(12):3255.
doi: 10.3390/jcm11123255.
Authors
Mitchell D Arnovitz 1 , Andrew J Spitzberg 1 , Ashkhan J Davani 1 , Nehal P Vadhan 1 2 3 , Julie Holland 4 , John M Kane 1 2 3 , Timothy I Michaels 1 2
Affiliations
- 1 Department of Psychiatry, The Zucker Hillside Hospital, Northwell Health, Queens, NY 11004, USA.
- 2 Department of Psychiatry, The Donald and Barbara Zucker School of Medicine at Hofstra/Northwell, Hempstead, NY 11549, USA.
- 3 Institute of Behavioral Science, Feinstein Institutes for Medical Research, Manhasset, NY 11030, USA.
- 4 Private Practice, New York City, NY 10016, USA.
- PMID: 35743326
- PMCID: PMC9225098
- DOI: 10.3390/jcm11123255
Abstract
The profound economic burden of schizophrenia is due, in part, to the negative symptoms of the disease, which can severely limit daily functioning. There is much debate in the field regarding their measurement and classification and there are no FDA-approved treatments for negative symptoms despite an abundance of research. 3,4-Methylenedioxy methamphetamine (MDMA) is a schedule I substance that has emerged as a novel therapeutic given its ability to enhance social interactions, generate empathy, and induce a state of metaplasticity in the brain. This review provides a rationale for the use of MDMA in the treatment of negative symptoms by reviewing the literature on negative symptoms, their treatment, MDMA, and MDMA-assisted therapy. It reviews recent evidence that supports the safe and potentially effective use of MDMA to treat negative symptoms and concludes with considerations regarding safety and possible mechanisms of action.
There is much debate in the field regarding their measurement and classification and there are no FDA-approved treatments for negative symptoms despite an abundance of research. 3,4-Methylenedioxy methamphetamine (MDMA) is a schedule I substance that has emerged as a novel therapeutic given its ability to enhance social interactions, generate empathy, and induce a state of metaplasticity in the brain. This review provides a rationale for the use of MDMA in the treatment of negative symptoms by reviewing the literature on negative symptoms, their treatment, MDMA, and MDMA-assisted therapy. It reviews recent evidence that supports the safe and potentially effective use of MDMA to treat negative symptoms and concludes with considerations regarding safety and possible mechanisms of action.
Keywords: MDMA; negative symptoms; psychedelic-assisted therapy; psychosis; schizophrenia.
Conflict of interest statement
J.M.K. has received honoraria for lectures or consulting fees from Alkermes, Allergan, Boehringer Ingelheim, Cerevel, Click Therapeutics, Dainippon Sumitomo, HLS, Indivior, IntraCellular Therapies, Janssen/J&J, Karuna, LB Pharmaceuticals, Lundbeck, Merck, Minerva, Neumora, Neurocrine, Newron, Novartis, Otsuka, Reviva, Roche, Saladax Biomedical, Sunovion, Takeda, and Teva. He is a shareholder of The Vanguard Research Group, and LB Pharma NPV is a paid research consultant to Sunnyside/Cutback Coach, LLC, an online alcohol moderation platform. J.H. is on the scientific advisory board for Apotheca, CB1 Capital, MycoMedica, Palo Santo, and Tactogen. She is a Medical Advisor for Cardea and MAPS.
Figures
Figure 1
Actionable factors that cause or…
Figure 1
Actionable factors that cause or contribute to secondary negative symptoms.
Actionable factors that cause or contribute to secondary negative symptoms.
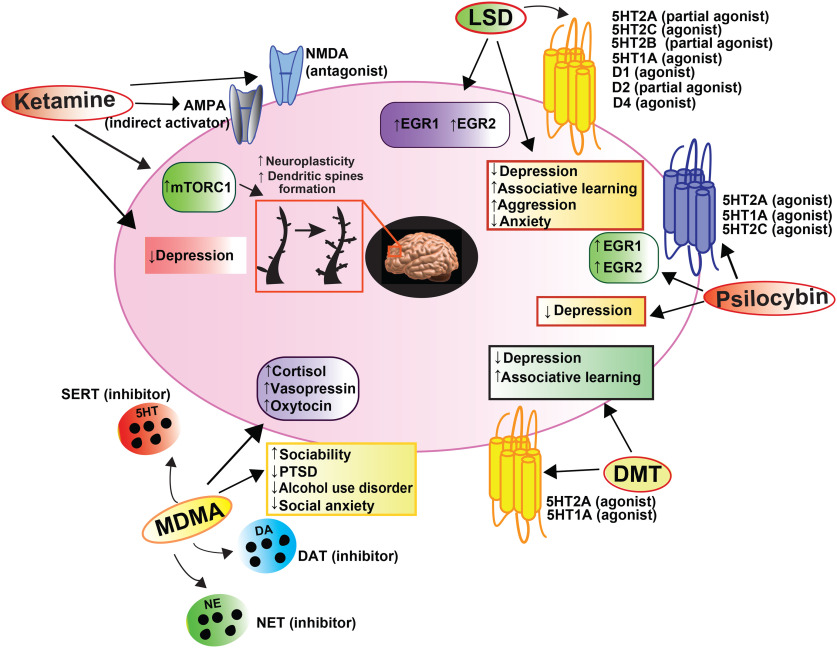
Figure 2
Main mechanisms of action of…
Figure 2
Main mechanisms of action of MDMA in humans. Image obtained from https://commons.wikimedia.org/wiki/File:Main_mechanisms_of_action_of_MDMA_in_humans.svg (accessed…
Figure 2Main mechanisms of action of MDMA in humans. Image obtained from https://commons.wikimedia.org/wiki/File:Main_mechanisms_of_action_of_MDMA_in_humans.svg (accessed on 1 May 2022) and reproduced with permission under the Creative Commons CC0 1.0 Universal Public Domain Dedication.
See this image and copyright information in PMC
Similar articles
-
Prescription of Controlled Substances: Benefits and Risks.

Preuss CV, Kalava A, King KC. Preuss CV, et al. 2022 Sep 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 Sep 21. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 30726003 Free Books & Documents.
-
A proposed mechanism for the MDMA-mediated extinction of traumatic memories in PTSD patients treated with MDMA-assisted therapy.
Sottile RJ, Vida T. Sottile RJ, et al. Front Psychiatry. 2022 Oct 12;13:991753. doi: 10.3389/fpsyt.2022.991753. eCollection 2022. Front Psychiatry. 2022. PMID: 36311515 Free PMC article. Review.
-
Review of potential psychedelic treatments for PTSD.
Henner RL, Keshavan MS, Hill KP.
 Henner RL, et al. J Neurol Sci. 2022 Aug 15;439:120302. doi: 10.1016/j.jns.2022.120302. Epub 2022 May 30. J Neurol Sci. 2022. PMID: 35700643 Review.
Henner RL, et al. J Neurol Sci. 2022 Aug 15;439:120302. doi: 10.1016/j.jns.2022.120302. Epub 2022 May 30. J Neurol Sci. 2022. PMID: 35700643 Review. -
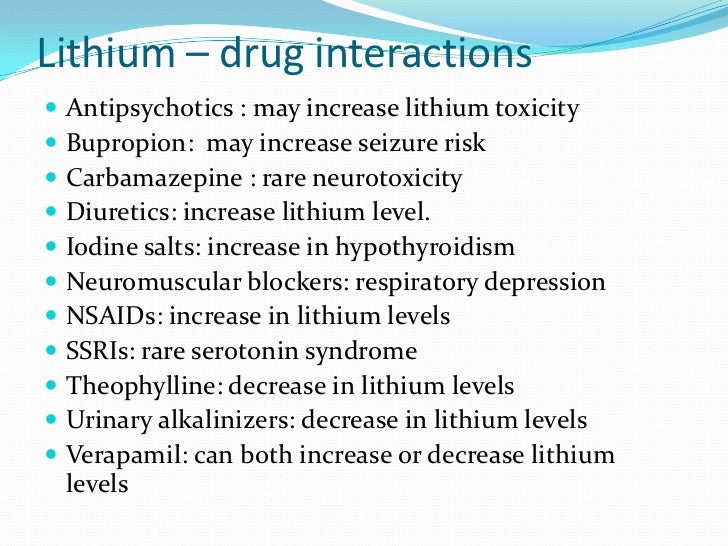
Effects of Selective Serotonin Reuptake Inhibitor Use on 3,4-Methylenedioxymethamphetamine-Assisted Therapy for Posttraumatic Stress Disorder: A Review of the Evidence, Neurobiological Plausibility, and Clinical Significance.
Price CM, Feduccia AA, DeBonis K. Price CM, et al. J Clin Psychopharmacol. 2022 Sep-Oct 01;42(5):464-469. doi: 10.1097/JCP.0000000000001595. Epub 2022 Aug 20. J Clin Psychopharmacol. 2022. PMID: 36018231 Review.
-
Suicidal Ideation.
Harmer B, Lee S, Duong TVH, Saadabadi A. Harmer B, et al. 2022 May 18. In: StatPearls [Internet].
 Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 May 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33351435 Free Books & Documents.
Treasure Island (FL): StatPearls Publishing; 2022 Jan–. 2022 May 18. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 33351435 Free Books & Documents.
See all similar articles
References
-
- Schultz S.H., North S.W., Shields C.G. Schizophrenia: A review. Am. Fam. Physician. 2007;75:1821–1829. - PubMed
-
- Charlson F.J., Ferrari A.J., Santomauro D., Diminic S., Stockings E., Scott J.G., McGrath J., Whiteford H.A. Global Epidemiology and Burden of Schizophrenia: Findings from the Global Burden of Disease Study 2016. Schizophr. Bull. 2018;44:1195–1203.
 doi: 10.1093/schbul/sby058. - DOI - PMC - PubMed
doi: 10.1093/schbul/sby058. - DOI - PMC - PubMed
- Charlson F.J., Ferrari A.J., Santomauro D., Diminic S., Stockings E., Scott J.G., McGrath J., Whiteford H.A. Global Epidemiology and Burden of Schizophrenia: Findings from the Global Burden of Disease Study 2016. Schizophr. Bull. 2018;44:1195–1203.
-
- Olfson M., Gerhard T., Huang C., Crystal S., Stroup T.S. Premature Mortality Among Adults with Schizophrenia in the United States. JAMA Psychiatry. 2015;72:1172–1181. doi: 10.1001/jamapsychiatry.2015.1737. - DOI - PubMed
-
- Palmer B.
 A., Pankratz V.S., Bostwick J.M. The lifetime risk of suicide in schizophrenia: A reexamination. Arch. Gen. Psychiatry. 2005;62:247–253. doi: 10.1001/archpsyc.62.3.247. - DOI - PubMed
A., Pankratz V.S., Bostwick J.M. The lifetime risk of suicide in schizophrenia: A reexamination. Arch. Gen. Psychiatry. 2005;62:247–253. doi: 10.1001/archpsyc.62.3.247. - DOI - PubMed
- Palmer B.
-
- Schoenbaum M., Sutherland J.M., Chappel A., Azrin S., Goldstein A.B., Rupp A., Heinssen R.K. Twelve-Month Health Care Use and Mortality in Commercially Insured Young People with Incident Psychosis in the United States. Schizophr. Bull. 2017;43:1262–1272. doi: 10.1093/schbul/sbx009. - DOI - PMC - PubMed
Publication types
Grant support
This research received no external funding.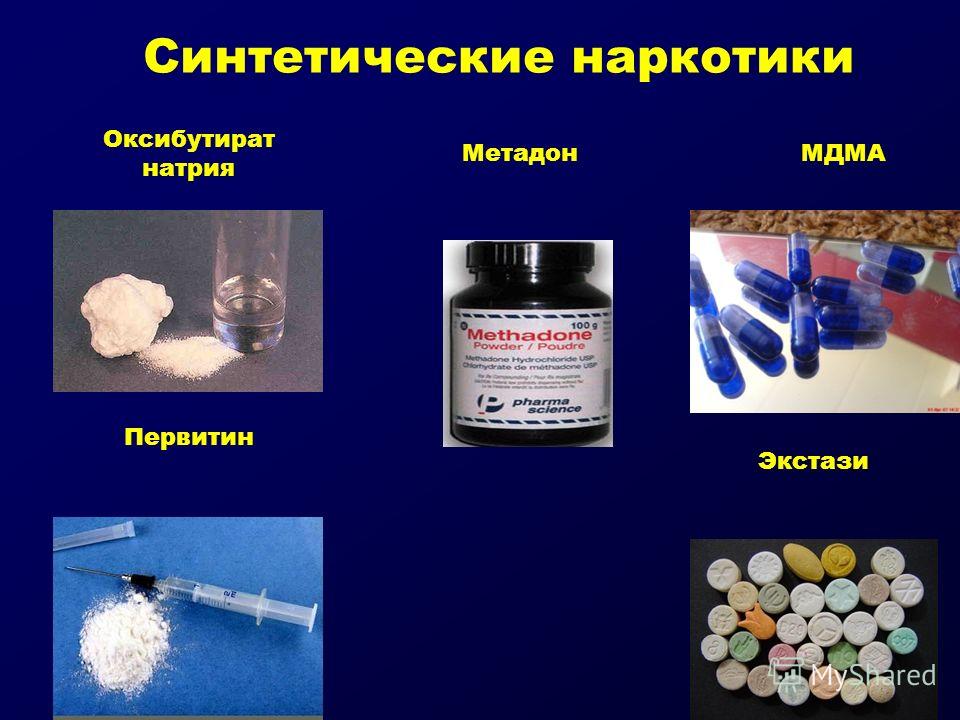
|
MDMA in a Severely Disturbed Man with Psychosis, Administered by his Brother It has been eighteen years since the governing powers made MDMA a Schedule 1 substance, and rendered it unavailable to the millions of people who could benefit from its use. In 1984 I wrote a paper detailing what this letter will again describe. My brother had a history of acute alcoholism and drug use. Our family had sent him down to Sarasota from Indianapolis to my wife and I, in frustration, hoping we could help him out. We tried, but after several months of getting nowhere, having him living with us, we asked him to seek his own means. I had not seen him for six months or so.
One afternoon after work I sat down in my easy chair, ready to watch the news and relax, when I had a sudden urge to go see if this pod of dolphins I was trying to establish a relationship with was around.
I don't know if it was angels, Divine intervention, dolphins, some extra-sensory phenomenon or what. Whatever it was, it was miraculous. For just as I approached the bridge, I saw my brother. He was walking at a fast pace, head down, shoulders slumped. I pulled over, got out of the car, and spoke to him. He seemed confused. He did not recognize me at first. I was able to get him into the car, which was no easy task. He was frightened, paranoid, and seemed to be hallucinating. As I crossed the bridge to get to where I could turn around, the pod of dolphins I thought would be there passed under the bridge and swam off into the sunset. Had they called me in time to save my brother's life? You see, as we drove back to my house, he was able to explain he had injected some very bad bathtub meth, had been awake for about a week, and was going to jump off the bridge. When I got him home, it became clear he was not only depressed, but having fits of rage. He came in and out. He would forget what he was saying, who he was, who I was. He was very paranoid, and tried to escape. My brother, unlike myself, is a very big guy. He frightened me. My wife came home with our little baby, and my concern grew. I called our mother and she said "Commit him." I took him to the exclusive Palms Hospital, a rehab hospital just blocks from our home. I had a friend in rehab there, a famous musician, and figured he could help my brother.
After two weeks there and at an expense to our mother of nearly twenty thousand dollars, we had to make other arrangements. He was doing no better. There was a hearing, and we committed him to the state facility.
Shortly thereafter, Rick Doblin told me about the work he was doing with MDMA, which was prior to its scheduling. He asked if I would be interested in trying it and writing a paper about my experience. My brother had been in the state hospital for five weeks when I called his doctors to see how his progress was coming along. "To be honest, he's no better," one of his doctors explained. "He is still hallucinating, definitely suicidal and most likely homicidal. He can't hold a conversation. He doesn't even know his own name most of the time." I asked the doctor if he had ever heard of MDMA. He responded, "Yes, I'm very familiar with it. We all are here." "What do you think it could do for my brother?" I asked him.
"At this point," and this is verbatim as I still remember this conversation well, "it couldn't hurt him. But we can't administer it to him here. I asked him if he had heard of Rick and his work, and he said yes. I asked how he felt about it. He told me he supported Rick, and MDMA. He said all the doctors out there wished they could give it to their patients, that they all felt it would help many of them. I asked what he would think of Rick and I giving it to my brother. He said he could sign him out for the weekend if I had him back by Monday, warning me to be very careful and not to let him leave my sight. With that, I drove the hour and a half to retrieve my poor spaced out brother. I strapped him into the car and said, "I'm taking you home to get you high, but you have to be good." He didn't say three words the entire trip home. I explained MDMA to him, and he seemed ready to try it.
I did everything according to the methods suggested by Rick and other therapists. My brother was given about 130 mg., after not eating for four hours. In forty minutes, the MDMA kicked in, and he got up and went out on the lawn. We talked for nearly four hours. I gave him another half dose, as suggested for therapy. We looked at our childhood years, we talked about many things. He went to sleep clear and at peace. The next morning I drove him back to the hospital, and he was like his old self again. On Monday morning, his doctor called me and said, "You can come get him Wednesday. He doesn't need to be here." What more can one say? Who knows what his fate would have been had it not been for MDMA. How long would he have suffered? Would he ever have made it back? He has never injected drugs since, however, he has had a very bad time with alcohol. Would he if he could have had ongoing therapy with MDMA under controlled environments with qualified therapists?
MDMA is a healing instrument beyond any other we know of in psychotherapy. I'll never forget the peace it brought to our dying friend, John Major, before cancer took him.
My wife is the director of grief support services for a hospice. I wish we could give it to so many of the dying clients and their tormented families. To the children who have watched parents die, murdered, or who have suffered abuse. So many people in pain in this world. MDMA can help them in so many ways. My opinion? It's lobbying from the big drug companies who want their drugs like Prozac to stay on the market. If you can heal a patient with $5 worth of MDMA every month, who needs Prozac? There go mllions of dollars of profit. Thank you Rick, and thank God, for MDMA in 1984. It saved my brother's life. And mine too! Sincerely,
David A. Goodman
|
Schizophrenia and psychosis due to drug use
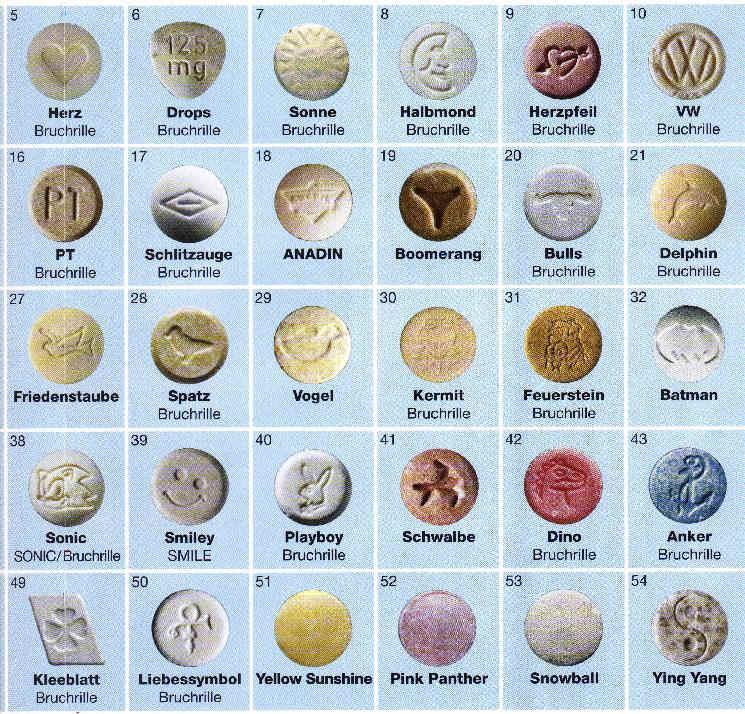
From October 1, 2020 to Petersburg started the month of anti-drug events dedicated to International Day Against Drug Abuse and Drug Abuse illegal traffic.
Events traditionally held in April have been rescheduled for October.
The goal is to expand the forms of participation of the population in prevention of non-medical consumption and drug trafficking drugs and psychotropic substances, as well as the formation of public opinion, motivating for a healthy lifestyle and the resistance of adolescents and youth to drug pressure.
Within the framework of the month of anti-drug activities from 1 to 31 October in St. Petersburg GBUZ "Psychoneurological Dispensary No. 1 planned a set of anti-drug outreach activities, which will be implemented in cooperation with the administration of Vasileostrovsky district, subordinate institutions of education, healthcare, social defense and local governments.
Petersburg GBUZ "Psychoneurological Dispensary No. 1 planned a set of anti-drug outreach activities, which will be implemented in cooperation with the administration of Vasileostrovsky district, subordinate institutions of education, healthcare, social defense and local governments.
Activities will be carried out subject to current restrictions, related to the spread of a new coronavirus infection, and in compliance with all safety standards.
Is it possible to develop schizophrenia as a result of addiction?
Drug addiction, like Alcoholism today is one of the main social problems of society. Any addiction is a disease, no matter what substance it is caused by, the most important thing is that people suffer at the same time, their environment, their families are in dysfunctional connections. Children from these families do not receive proper education. Today this is a big scourge for Russia.
Is it possible to develop schizophrenia "from drug addiction"? It is difficult to answer the question unambiguously, each case considered by psychiatrists individually.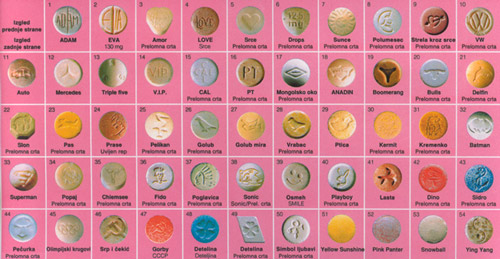 The brain is a fine structure, it is the balance of a large the amount of neurotransmitters. When you interfere with this structure, the consequences may be the most unpredictable.
The brain is a fine structure, it is the balance of a large the amount of neurotransmitters. When you interfere with this structure, the consequences may be the most unpredictable.
Drugs, especially synthetic production, have a strongly negative effect on the nervous human system. Such drugs can not only destroy brain cells, but and cause mental disorders. Schizophrenia and drug addiction are linked in complex ways. relationships, so, after taking drugs, it is possible to develop symptoms similar to those of schizophrenia (perceptual disturbances, hallucinatory states). At the same time, anyone who decides to “try” the drug must understand that that even a single use can lead to dire consequences for psyche. Is it worth experimenting with with your psyche?
Drugs with psychedelic effect (LSD, spices, amphetamines, etc.) can easily provoke the debut of schizophrenia in a healthy person, if his genes already predisposition to this disease. Scientists have proven that the amphetamines against the background of schizophrenia leads to an aggravation of the clinical picture and significant deterioration in the patient's condition. If the diagnosis has already been made, but the patient continues to use psychoactive substances, the prognosis is extremely adverse. The processes of destruction of brain cells, as well as degradation personality under the influence of drugs occur much faster. high risk the onset of psychosis, which are much more severe than outside the reception narcotic substances.
If the diagnosis has already been made, but the patient continues to use psychoactive substances, the prognosis is extremely adverse. The processes of destruction of brain cells, as well as degradation personality under the influence of drugs occur much faster. high risk the onset of psychosis, which are much more severe than outside the reception narcotic substances.
Many schizophrenics are under the influence of drugs become socially dangerous. They can kill or cripple others without feeling any remorse (even after coming out of a state of narcotic intoxication). Another danger is the possibility of suicide of the patient, who in such a state can imagine numerous dangers, enemies or vice versa - instead of a balcony of the 15th floor a person can see a green lawn and strive to get into it.
The development of schizophrenia can provoke strong psychoactive substances used in large quantities that have a strong hallucinogenic effect. One of the studies confirms the fact of the development of acute psychoses against the background of cannabis use.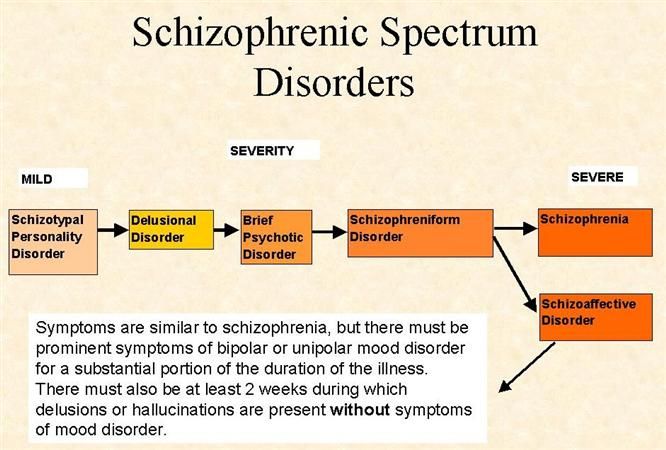
Psychoses against the backdrop of addiction. Synthetic drugs cause mental disorders that are extremely difficult to treat. Long-term use of synthetic drugs causes severe anxiety, panic attacks and depression. Substance use causes irritability, sleep and appetite disorders, behavioral and sexual violations.
Drugs lead to affective disorders that can "flow" under the guise of dysthymia, depression, bipolar disorder.
Also among drug addicts many patients suffering from paranoid schizophrenia, which is observed in lovers of synthetic analogues of cocaine: amphetamine, pervitin, methamphetamine. Symptoms manifest as delusional, auditory, visual, and tactile hallucinations. Patients with these disorders have aggressive behavior, they are often involved in criminal situations.
Regular the use of the mixture in demand today, acute hallucinations are added to delusional ideas, impaired thinking, gross changes are clearly visible personality. Spice addicts, usually after a certain amount of time end up in a psychiatric ward, because they become dangerous for a healthy society.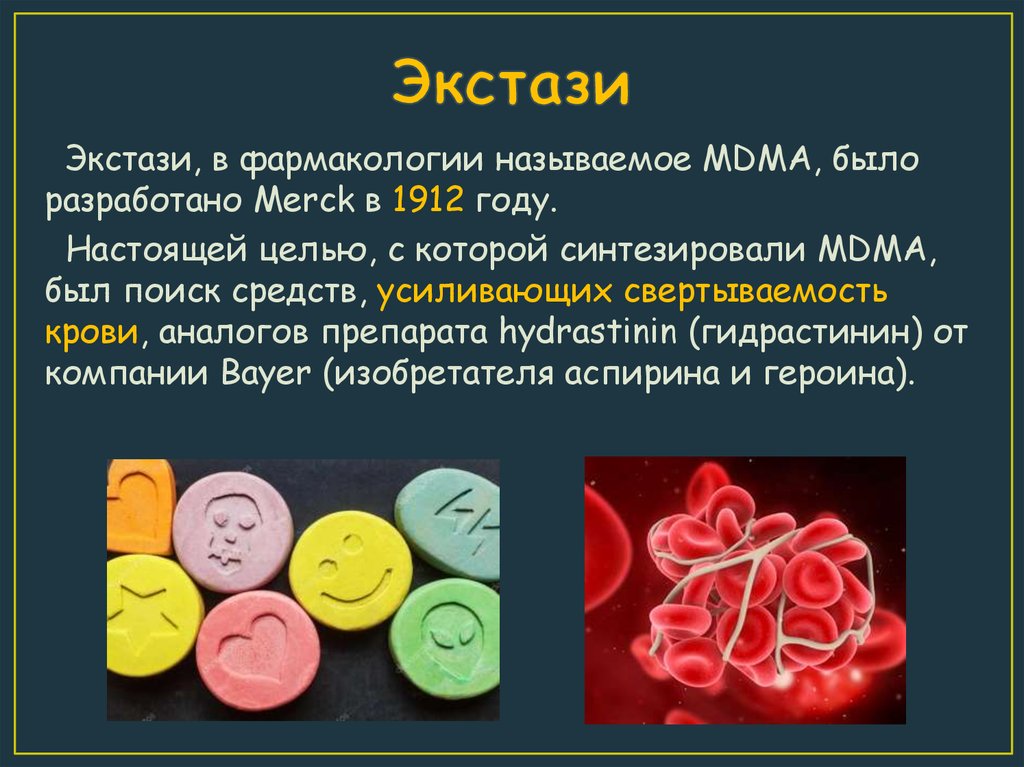 Then doctors may suspect the progression of schizophrenia, creeping unnoticed under the influence of synthetic cannabinoids, to to which the prohibited drug belongs.
Then doctors may suspect the progression of schizophrenia, creeping unnoticed under the influence of synthetic cannabinoids, to to which the prohibited drug belongs.
In addition to being provokes a significant decrease in the cortical content of dopamine, at the same time by increasing its content in the midbrain, the drug leads to extremely rapid development of a debilitating mental disorder. If a person is prone to the emergence of a mental disorder, indulging in drugs, he reaches the fact that the hidden illness is transformed into schizophrenia with all the consequences consequences. Progressing by leaps and bounds, it completely cuts off person from normal life.
Mental drug treatment . Therapy drug-induced psychosis significantly complicated, synthetic psychoactive substances strongly bind to brain receptors and accumulate in body tissues. This condition is treated primarily in a psychiatric hospital, psycho-neurological dispensary by qualified specialists - narcologist, psychiatrist, psychotherapist.
We are still not completely understand how to treat it. You need to select a drug regimen. Often this is the selection of drugs in order to a little bit to restore the psyche. Often the process takes several years (!!!) Treatment drug addiction is a complex process that requires a lot of effort and takes a lot of time.
The best way to fight long-term psychotherapy can be with harmful dependence. As in healthy and in sick people, the cause of cravings for alcohol and drugs is most often an increased level of anxiety, which helps to remove work with a competent a psychotherapist who knows how to interact with mentally ill patients, knows the peculiarities of their thinking and ways of influencing specific altered consciousness of a patient with schizophrenia.
Conclusion: Mandatory a condition for successful therapy is compliance with the rehabilitation period, which can last from 6 months to several years. The most difficult is search for an incentive to continue life without drugs.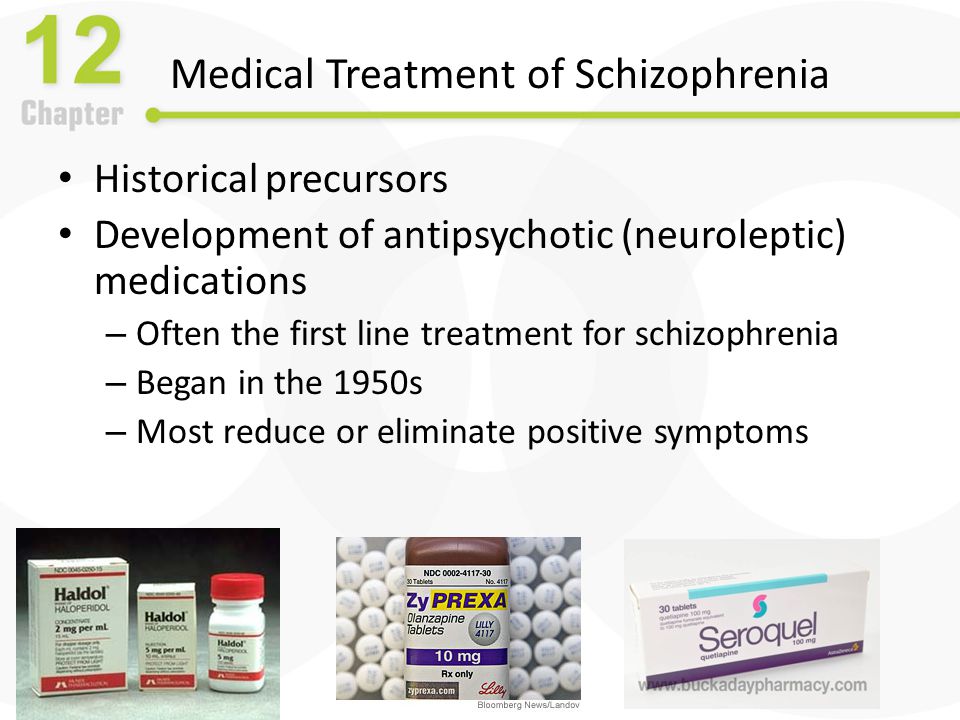 In this case, it is required help of professional psychotherapists, psychologists and support of relatives. Any pathological addiction schizophrenia is dangerous for the patient and can aggravate the course of the disease. Unfortunately, science does not know of a "magic pill" that can instantly rid the patient of drug addiction. Long-term work with specialists, trust doctor and careful intake of prescribed medications will help the patient cope with dangerous habits for him, and with the underlying disease, in order to return again to a normal (or almost normal) life in society.
In this case, it is required help of professional psychotherapists, psychologists and support of relatives. Any pathological addiction schizophrenia is dangerous for the patient and can aggravate the course of the disease. Unfortunately, science does not know of a "magic pill" that can instantly rid the patient of drug addiction. Long-term work with specialists, trust doctor and careful intake of prescribed medications will help the patient cope with dangerous habits for him, and with the underlying disease, in order to return again to a normal (or almost normal) life in society.
SPb GBUZ "Psycho-neurological dispensary No. 1" social work specialist Vysotskaya V.P.
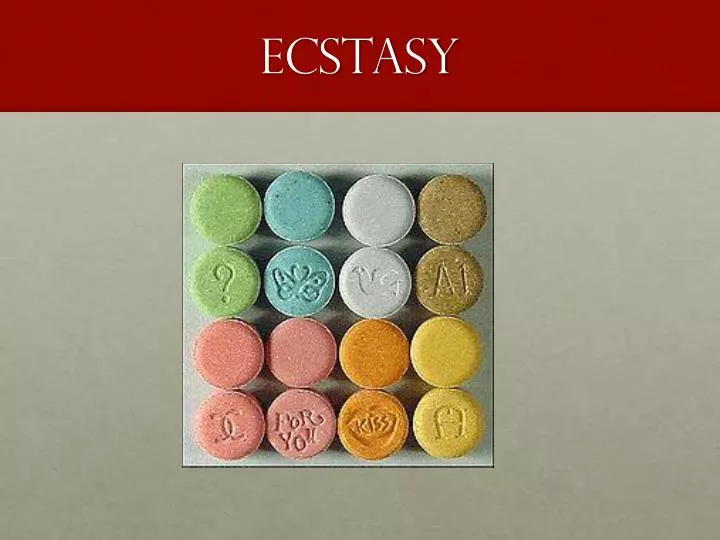
MDMA Club drug showed the effectiveness in the treatment of mental disorders
Club drug MDMA, better known as ecstasy or Molly, according to experts, is able to enhance the feelings of emotional closeness and empathize. Now, a new study by scientists from England has shown that this drug does affect how people feel and act in relation to others.
According to the information at the disposal of IA Express-Novosti, as a result of the work carried out, the researchers found that MDMA makes people more sociable, but only in relation to those they know well. In other words, the drug doesn't make people trust others, the researchers say. The work also showed that the use of MDMA leads to an increase in the activity of those areas of the brain that are believed to be involved in social interaction and understanding the thoughts and intentions of other people. And since MDMA is also being studied as a treatment for post-traumatic stress disorder (PTSD), the new results are "an important and timely step" leading to a better understanding of the drug's social and emotional effects.
IA Express-Novosti informs that MDMA is illegal in the United States, as in many other countries, because it increases the activity of chemical reactions in areas of the brain associated with behavior and mood, including dopamine and serotonin .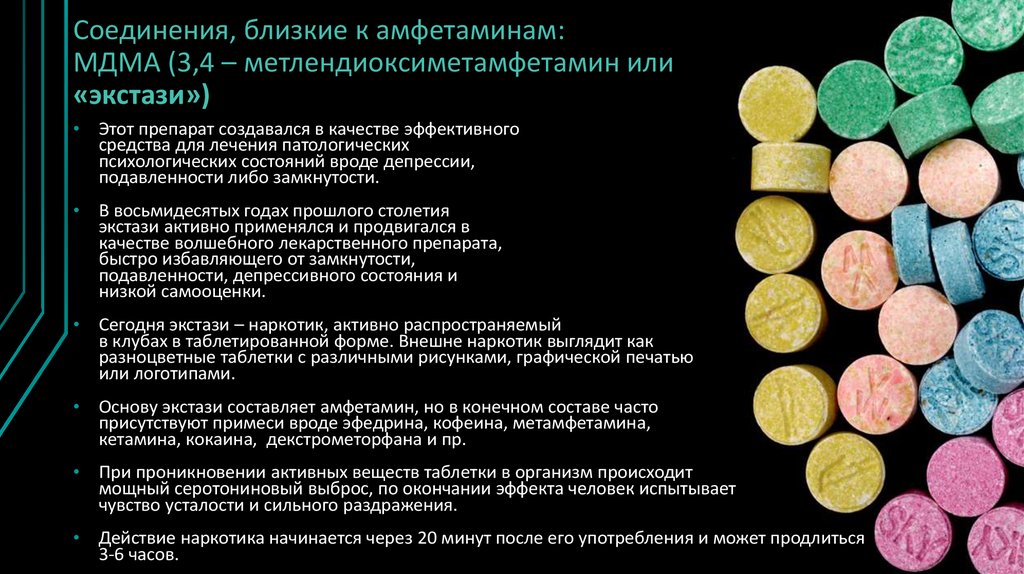 In addition, little is known about how the various chemical exchange systems in the brain contribute to complex social behavior. And just to shed some light on the mystery, in their new study, the researchers recruited 20 healthy male volunteers, aged 20 to 30, who didn't have a mental or substance use disorder, but who were at least used to take MDMA.
In addition, little is known about how the various chemical exchange systems in the brain contribute to complex social behavior. And just to shed some light on the mystery, in their new study, the researchers recruited 20 healthy male volunteers, aged 20 to 30, who didn't have a mental or substance use disorder, but who were at least used to take MDMA.
Participants were randomized to receive either 100 milligrams of pure MDMA (the chemical 3,4-methylenedioxymethamphetamine) or placebo. They were then invited to play a game while scientists scanned their brains. In a game called the Prisoner's Dilemma, participants choose to either compete or cooperate with another player. If both players choose to cooperate, they both receive points. But if one of the players chooses to cooperate and the others compete, then the one who chooses to compete gets all the points. Participants were told they were playing against real people, but were actually playing against a computer with pre-programmed responses. The researchers programmed the computer to be "trustworthy". That is, he either cooperated in most games or competed (for each group).
The researchers programmed the computer to be "trustworthy". That is, he either cooperated in most games or competed (for each group).
The study found that participants who took MDMA were more likely to partner with trusted players compared to participants who took placebo. But MDMA did not affect their cooperation with unreliable players: both MDMA and placebo cooperated with unreliable players at the same rate.
"MDMA did not force participants to cooperate with unreliable players any more than it was required," study leader Mitul Mehta, Professor of Neuroimaging and Psychopharmacology at King's College London, said in a statement. He also noted that the study showed that when participants chose to cooperate but their opponent chose to compete, it reduced their willingness to cooperate during the next game. But those who took MDMA re-established joint behavior with trusted players more quickly than those who took placebo.
"This trend of rebuilding relationships has led to higher overall levels of collaboration with trusted partners," said lead researcher Anthony Gabay, a neuroscientist at the University of Oxford.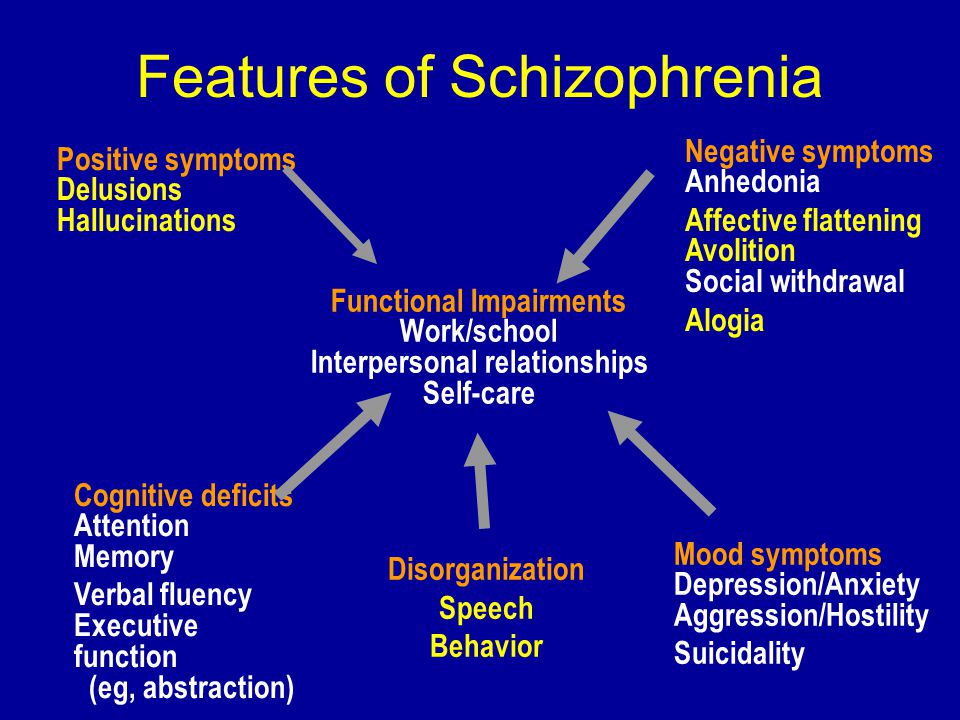
 I had the funny feeling they would be near the bridge on Siesta Drive. The urge became so strong, I bolted out of the chair and drove swiftly to the bridge.
I had the funny feeling they would be near the bridge on Siesta Drive. The urge became so strong, I bolted out of the chair and drove swiftly to the bridge.
 I agreed. My first night of MDMA was one of the most profound of my life. It unlocked feelings of love I had never known, and I was able to view several incidences of my life, especially my childhood, with renewed compassion and understanding, forgiveness and release.
I agreed. My first night of MDMA was one of the most profound of my life. It unlocked feelings of love I had never known, and I was able to view several incidences of my life, especially my childhood, with renewed compassion and understanding, forgiveness and release.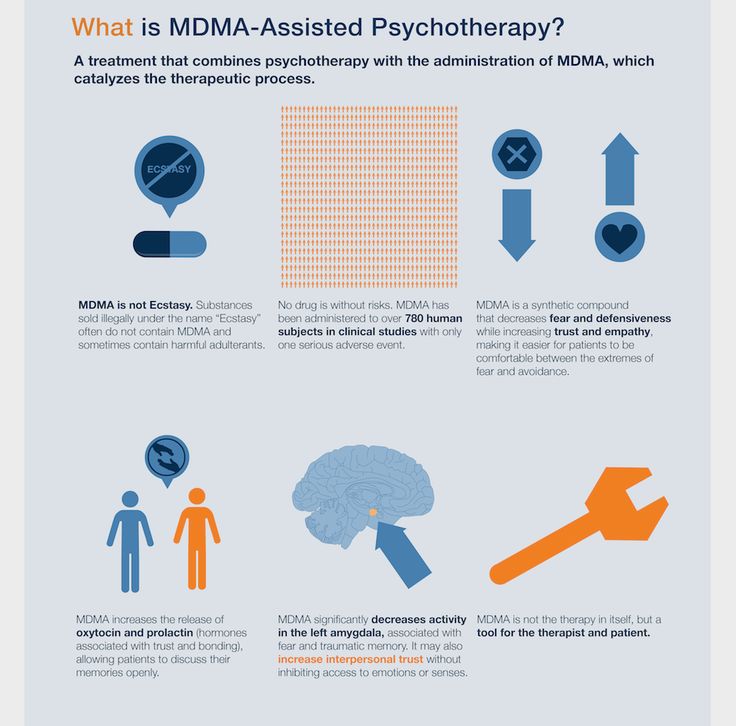 "
" By the way, I did not take it. I told my wife that if he left the yard she was to call the police. He didn't leave, though. He sat down and put his head on his knees for a while, then I saw him lift his head and he was in meditation. I joined him, and we began to talk. He was back!
By the way, I did not take it. I told my wife that if he left the yard she was to call the police. He didn't leave, though. He sat down and put his head on his knees for a while, then I saw him lift his head and he was in meditation. I joined him, and we began to talk. He was back!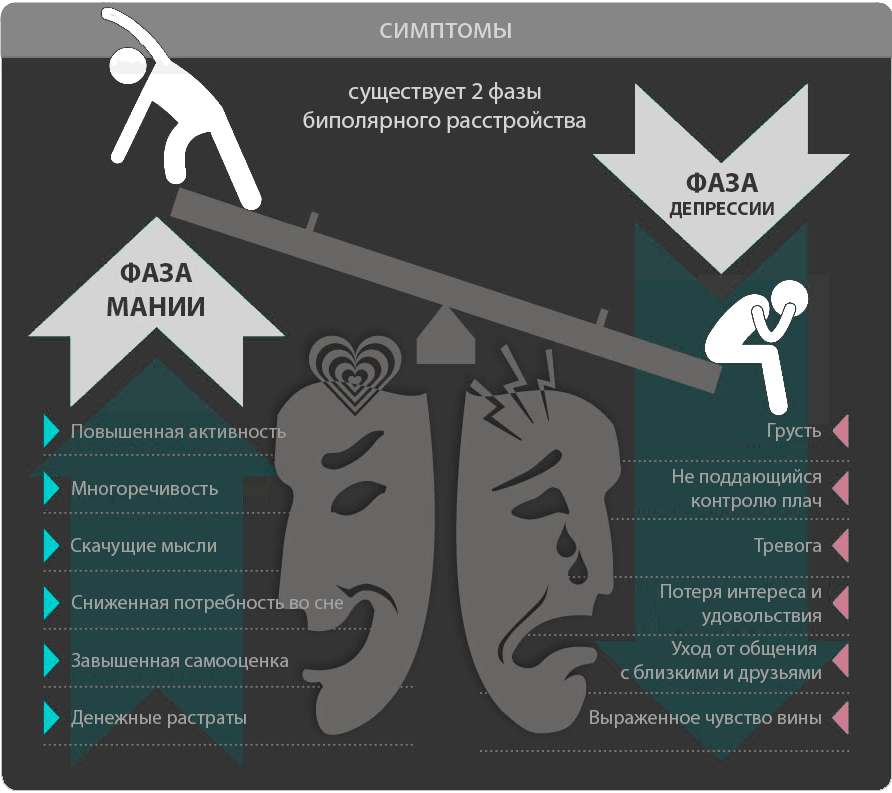 I'm not a therapist, but my wife is. She is not pro use of drugs except in severe cases, but because of the ban on MDMA, she has had no exposure to it, so she has no opinion currently. That's a shame. My friend Rick Doblin does. He has been dedicated to this cause for over twenty years. I am amazed at his commitment and I am equally amazed at the stupidity of the ruling institutions who have kept this drug from those who could benefit.
I'm not a therapist, but my wife is. She is not pro use of drugs except in severe cases, but because of the ban on MDMA, she has had no exposure to it, so she has no opinion currently. That's a shame. My friend Rick Doblin does. He has been dedicated to this cause for over twenty years. I am amazed at his commitment and I am equally amazed at the stupidity of the ruling institutions who have kept this drug from those who could benefit.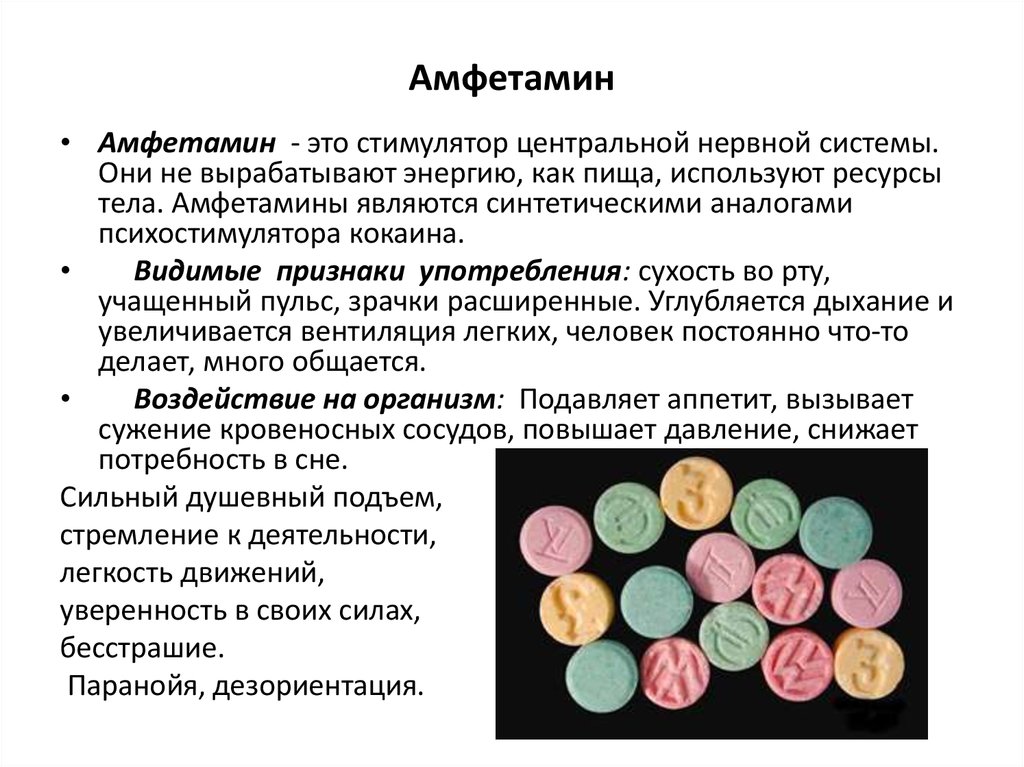 So, what do you think is going to happen?
So, what do you think is going to happen?