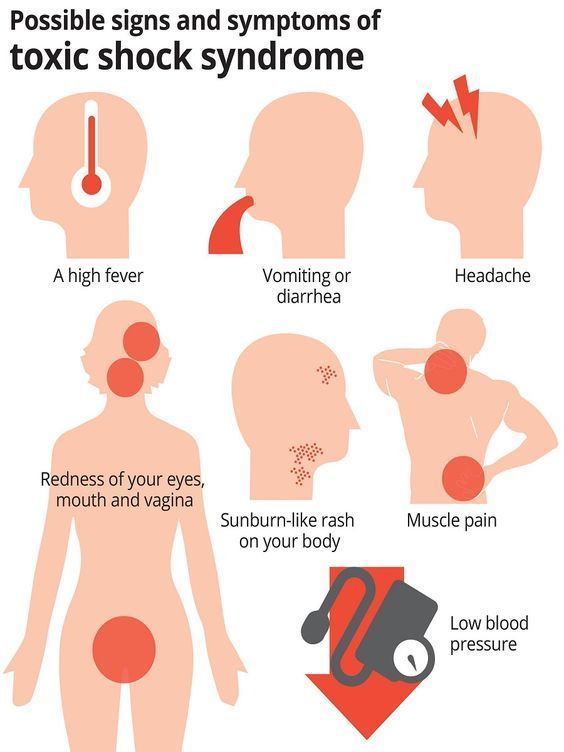
Sign and symptoms of lithium toxicity
What Causes Lithium Toxicity? Accidental Overdose and its Effects
Written by WebMD Editorial Contributors
In this Article
- What Is Lithium Used For
- Side Effects of Lithium
- Types of Lithium Poisoning
- Early Signs of Lithium Toxicity
- Treating Lithium Toxicity Early
You may take lithium as a treatment for bipolar disorder. It’s the most common form of treatment for this condition. Lithium toxicity can be caused by underlying health issues, changes to medication, or incorrect dosage.
What Is Lithium Used For
Lithium is commonly prescribed by psychiatrists to manage recurrent bipolar illness. Lithium was approved in the 1970s by the U.S. Food and Drug Administration (FDA) as a mood stabilizer and a treatment for mania.
Lithium is a powerful medication that has antimanic properties. Though lithium has been approved as a treatment, its effects on the brain aren’t completely understood. Researchers believe lithium makes the brain less responsive to stimulation that causes manic episodes. It’s also thought to reduce the responsiveness to neurotransmitters.
Lithium can become dangerous when it’s taken in excess. When excessive amounts are taken intentionally or accidentally, it can cause acute or acute-on-chronic overdose symptoms.
Side Effects of Lithium
To determine whether you’re experiencing lithium toxicity, you first need to know the common side effects of prescribed lithium. They include:
- Headache
- Nausea or vomiting
- Dizziness or drowsiness
- Diarrhea
- Changes in appetite
- Hand tremors
- Dry mouth
- Increased thirst
- Increased urination
- Thinning of hair or hair loss
- Acne-like rash
Some signs of lithium toxicity are similar to its side effects, but more severe. Symptoms of lithium toxicity include severe nausea and vomiting, severe hand tremors, confusion, and vision changes. If you experience these, you should seek immediate medical attention to check your lithium levels.
Types of Lithium Poisoning
There are three types of lithium toxicity. They range from mild and uncomfortable to severe and dangerous if left untreated.
Acute lithium toxicity. Symptoms commonly include feeling weak, having a worsening tremor, feeling unbalanced or uncoordinated, poor concentration, diarrhea.
Acute-on-chronic lithium toxicity. With this level of poisoning, you could experience gastrointestinal (GI) problems. You may also experience neurological problems.
Chronic lithium toxicity. At this level, you will mostly experience neurological symptoms. Severity will depend on the levels of lithium in your body.
Early Signs of Lithium Toxicity
If you have one or more of the following symptoms, you may be experiencing early lithium toxicity:
- Loss of appetite, or vomiting
- Blurred vision
- Excessive thirstiness
- Needing to pee frequently
- Uncontrollable urination and bowel movements
- A lightheaded or drowsy feeling
- Confusion and blackouts
- Shaking, muscle weakness, twitches, jerks, or spasms affecting your face, tongue, eyes, or neck
- Trouble speaking
Lithium toxicity mostly affects your kidneys and central nervous system.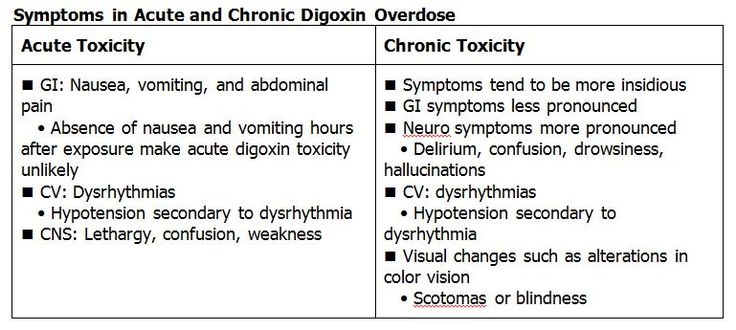 In acute lithium toxicity, your GI tract will be affected too. In more severe cases, you may experience neurological or cardiovascular problems. In early lithium toxicity, you may have mild confusion. As the toxicity worsens, you may feel delirious or even have seizures or go into a coma.
In acute lithium toxicity, your GI tract will be affected too. In more severe cases, you may experience neurological or cardiovascular problems. In early lithium toxicity, you may have mild confusion. As the toxicity worsens, you may feel delirious or even have seizures or go into a coma.
In very rare cases, lithium toxicity may cause diabetes insipidus. This condition leads to large amounts of urine in your body, regardless of how much fluid you drink. You’ll also experience a significant amount of thirst.
If you're experiencing any of these symptoms or side effects, you should seek immediate medical attention. Left untreated, lithium toxicity can progress and worsen. Lithium poisoning can be life-threatening and should be monitored and treated promptly.
By noticing the early signs of lithium toxicity, you can get the help you need. Contact your doctor or psychiatrist if you feel like you're experiencing any side effects from your medication. You can also have them check your lithium levels to find out if they're too high.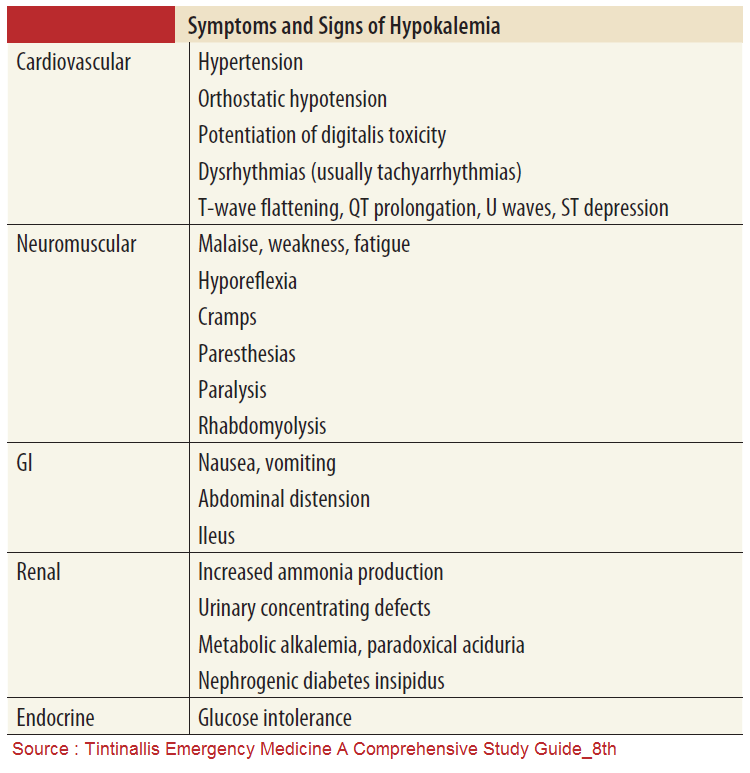
Treating Lithium Toxicity Early
When caught early, lithium toxicity can be treated by keeping or reducing your lithium levels to the low to medium range. If you notice a lithium-induced tremor, you may be treated with beta-blockers.
Diligent monitoring is the best way to avoid lithium toxicity. You’ll also need to make sure other medications you're on don't affect your lithium excretion. If your body excretes too much lithium, it can also create toxic levels in your body.
Medications that can interfere with this include:
- ACE inhibitors (used to treat high blood pressure and heart failure)
- Nonsteroidal anti-inflammatory medications (NSAIDs)
- COX-2 inhibitors (a type of NSAID)
Your doctor should monitor you closely to ensure you're taking the right levels of lithium. It's also important that you tell them about any side effects. Since lithium toxicity can happen through your body's excretion, you might not know initially whether you have high levels in your body.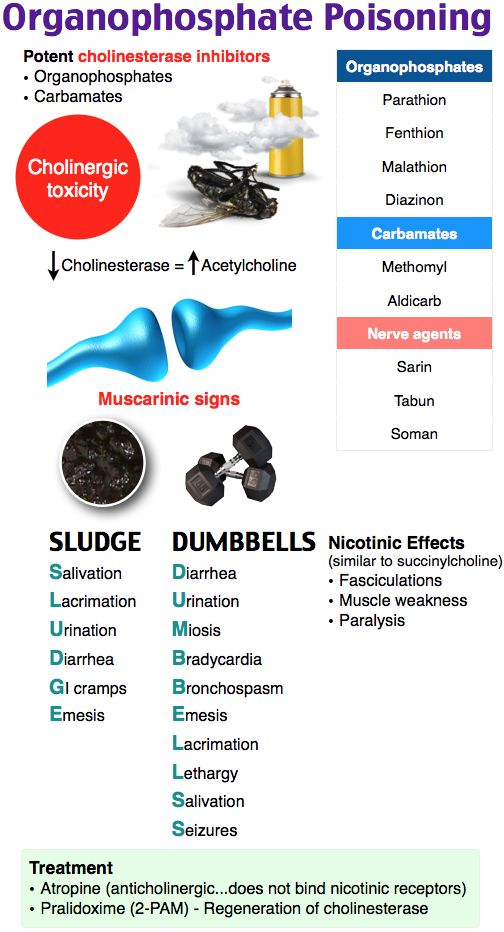
Lithium Toxicity - StatPearls - NCBI Bookshelf
Continuing Education Activity
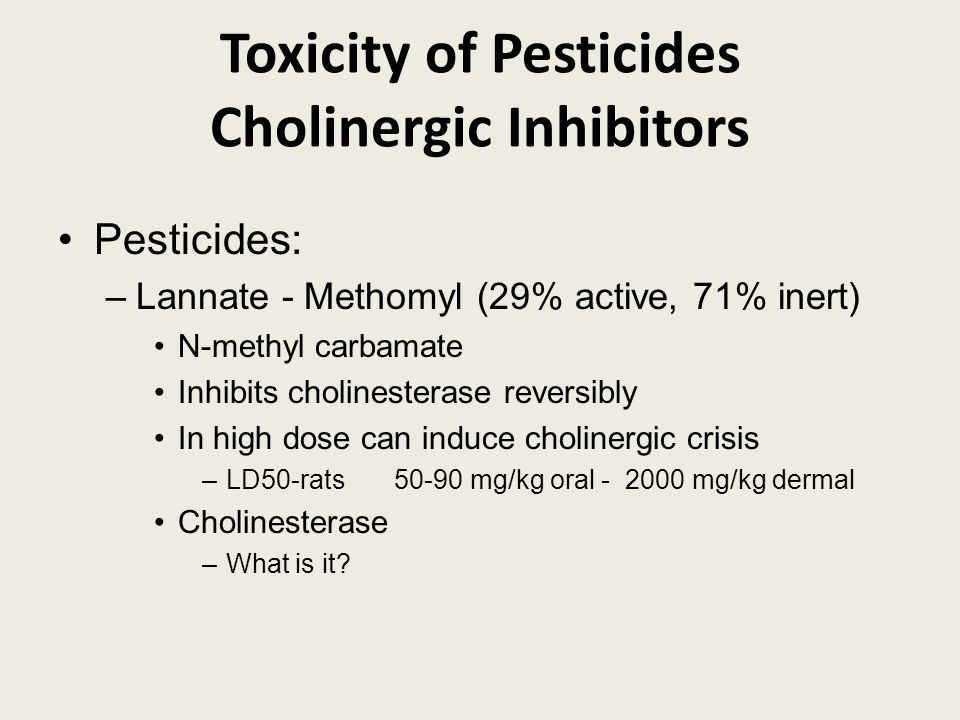
Lithium, a monovalent cation similar to sodium with an unknown mechanism, was first approved by the U.S. Food and Drug Administration (FDA) as a mood-stabilizing medication for the treatment of mania in the 1970s. Lithium is a very powerful, antimanic medication with a narrow therapeutic index. This activity reviews the indications, mode of action, the toxicity of lithium and highlights the role of the interprofessional team in the management of patients with drug toxicity.
Objectives:
Describe the pathophysiology of lithium toxicity.
Review lithium toxicokinetics.
Summarize the treatment of lithium toxicity.
Outline interprofessional team strategies for improving care coordination and communication to advance care bundle approaches to manage lithium toxicity and improve patient outcomes.
Access free multiple choice questions on this topic.
Introduction
The drug of choice for recurrent bipolar illness management remains to be lithium[1]. Lithium, a monovalent cation similar to sodium with an unknown mechanism, was first approved by the U.S. Food and Drug Administration (FDA) as a mood-stabilizing medication for the treatment of mania in the 1970s[2]. Lithium is a very powerful, antimanic medication with a narrow therapeutic index[3].
PharmacodynamicsLithium's physiologic role is unknown, and its mechanism is not well understood; however, some proposed mechanisms include:
Producing brain inositol depletion, leading to reduced responsiveness to alpha-adrenergic stimulation [4].
Reducing neuronal responsiveness to neurotransmitters due to inhibitory effects on adenylate cyclase and G proteins vital for ion channel opening[5].
Stimulating serotonin release from the hippocampus [6].
Being a cation, acting similar to potassium and sodium, thus affecting ion transport and cell membrane potential [7].
Etiology
Too much lithium can cause lithium toxicity. Factors increasing lithium concentration in the body include excessive intake and impaired excretion[8].
Epidemiology
A study evaluated a group of patients treated with lithium between 1997 and 2013 and the recurrence of lithium intoxication along with changes in renal functionality was to be assessed. 96 patients out of 1340 experienced at least one episode of lithium levels greater than 1.5 mmol/L. a cohort of seventy-seven participants had experienced 91 episodes, of whom 34% needed intensive care and 13% required hemodialysis with no deaths. Acute kidney injury occurred, but renal function at baseline was not different from renal function after the episode [9].
Pathophysiology
Excessive intake or impaired excretion can result in lithium accumulation.
Excessive Intake
Suicidal intent or accidental ingestion of excessive amounts of lithium tablets result in acute or acute-on-chronic overdose settings [10]. Moreover, excessive intake might arise from dose modifications for the patient chronically administering lithium [11].
Moreover, excessive intake might arise from dose modifications for the patient chronically administering lithium [11].
Impaired Excretion
Several factors might lead to impairment in lithium secretion. Sodium and volume depletion due to any conditions like vomiting, diarrhea, febrile illness, renal insufficiency, excessive exercise, water restriction, excessive sweating, low sodium diet, and congestive heart failure may enhance lithium reabsorption in the kidneys [11]. Furthermore, drugs reducing the glomerular filtration rate might inflict chronic toxicity.
Chronic therapy with lithium can precipitate nephrogenic diabetes insipidus, which might elicit a cascade of symptoms and signs of lithium toxicity. This can be attributed to the diminished urinary concentrating capacity of the kidneys[12].
Noteworthy, a vicious cycle of lithium toxicity might result from the concomitant existence of intercurrent illness with the reduced kidney concentrating capacity precipitated by lithium.
For example, reduced clearance and excretion of lithium in case of sodium and volume depletion will result in increased lithium concentration in the serum, which in turn continues to affect the kidneys’ ability to concentrate urine negatively.
Toxicokinetics
Different types of lithium formulations are present including sustained-release preparations[3].
Lithium is neither metabolized nor protein-bound, thus its bioavailability usually is close to 100%. Moreover, lithium absorption is rapid[3].
Serum lithium levels reflect only the extracellular lithium concentration. However, lithium exerts its effects once it has moved to its intracellular compartment. This phenomenon illustrates the reason why patients with significantly elevated serum levels might be asymptomatic[12].
Lithium is more susceptible to accumulation in the liver, bone, muscle, or thyroid with brain and kidney showing the highest levels[13].

The kidneys are responsible for 95% of lithium excretion, and the rest is removed through sweat and feces. The kidneys treat lithium and sodium similarly which is the reason sodium depletion can significantly elevate lithium reabsorption[14].
Volume depletion from diuretics, dehydration, febrile illness, or gastrointestinal loss can lead to elevated lithium levels in the serum[9].
The serum elimination half-life of lithium can vary from 12 to 27 hours. In patients with chronic intoxication, the half-life can be prolonged up to 48 hours[15].
The renal clearance of lithium is usually 10 to 40 mL/ min. However, the clearance may be decreased to 15 mL/min, and the elimination half-life can be as long as 58 hours in elder patients[16].
Lithium freely crosses the placenta and is also excreted in breast milk. It is labeled as pregnancy class D and has been implicated in the increased risk of congenital cardiac defects, particularly the Ebstein anomaly.
 Breastfeeding infants of mothers taking lithium have been reported to have signs of cyanosis, hypotonia, and lethargy[14].
Breastfeeding infants of mothers taking lithium have been reported to have signs of cyanosis, hypotonia, and lethargy[14].
History and Physical
History
In the late 1800s, lithia water was first introduced as a mania and gout treatment [17]. Afterward, lithium tablets with higher lithium concentration largely replaced lithia water. However, the higher lithium concentration found in the tablets was associated with tremors and weakness, and in 1898 lithium toxicity was first described. To determine the extent of lithium toxicity, one must determine the ingested amount, time of ingestion, whether there are co-ingestants, and if the ingestion was intentional or unintentional. It is worth noting that lithium toxicity signs do not often conform to the measured lithium level[18].
Physical
Neurologic Effects
Symptoms of intoxication include coarse tremor, hyperreflexia, nystagmus, and ataxia. Patients often show varying consciousness levels, ranging from mild confusion to delirium. Although the neurological symptoms are mostly reversible, some reports indicate that symptoms might persist for 12 months never resolve[9].
Although the neurological symptoms are mostly reversible, some reports indicate that symptoms might persist for 12 months never resolve[9].
Renal Toxicity
Renal toxicity is more common in patients on chronic lithium treatment. Toxicity includes impaired urinary concentrating ability, nephrogenic diabetes insipidus (the most common cause of drug-induced NDI), sodium-losing nephritis, nephrotic syndrome along with other manifestations is prescribed[19].
Cardiovascular Effects
These are usually mild and non-specific. Almost all patients treated with lithium will develop T wave flattening. Sinus node dysfunction is the most common reported conduction defect followed by QT prolongation, intraventricular conduction defects, and U waves. These findings are reversible[20].
Gastrointestinal Effects
Symptoms typically occur within 1 hour of ingestion and are more common in the acute overdose setting [15].
Endocrine Effects
Lithium administration leads to the inhibition of thyroid hormone synthesis and subsequent release, resulting in hypothyroidism.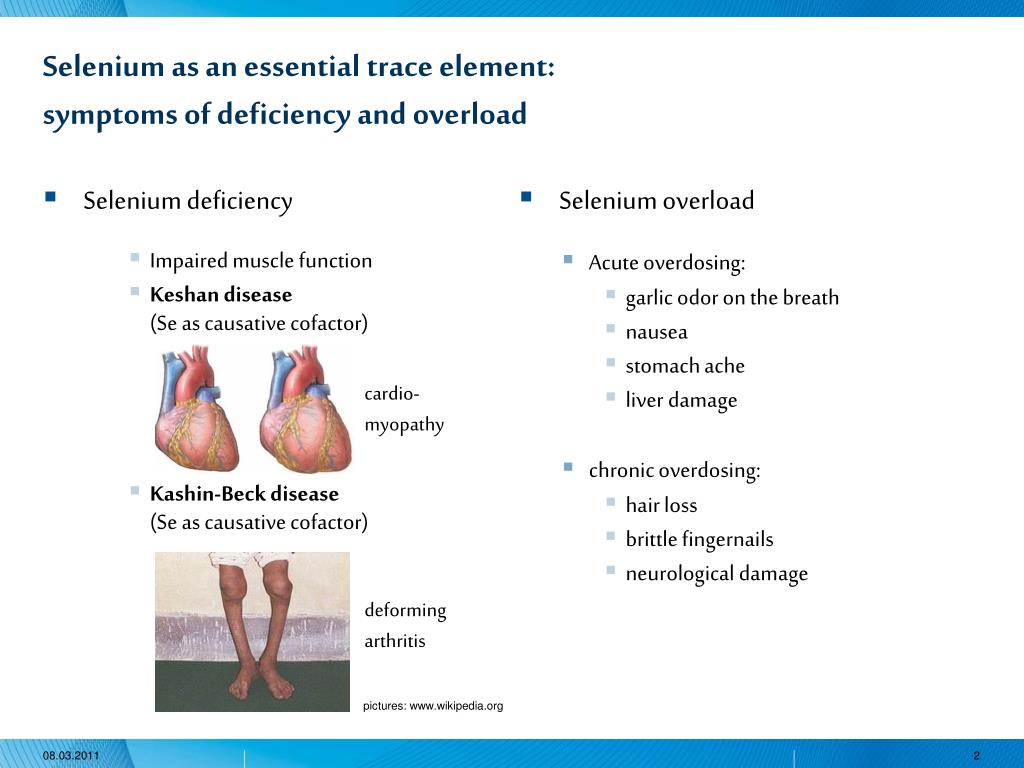 Hyperthyroidism is less commonly manifested, which can mask symptoms of lithium toxicity and boost its toxicity by prompting cellular unresponsiveness and altered renal tubular handling of lithium [21].
Hyperthyroidism is less commonly manifested, which can mask symptoms of lithium toxicity and boost its toxicity by prompting cellular unresponsiveness and altered renal tubular handling of lithium [21].
Evaluation
Initially, the studies should include cardiac monitoring, electrocardiogram, assessment of oxygenation and monitoring of urine output, serum electrolytes, calcium, renal function, glucose, serum lithium level, and thyroid-stimulating hormone [22]. Moreover, both therapeutic lithium usage and intoxication can be accompanied by leukocytosis. Furthermore, interference by the carbonate anion after lithium carbonate acute ingestion in the calculation of anion gap might lead to a low anion gap[23].
Patients are susceptible to renal insufficiency with elevated blood urea nitrogen and creatinine in case of chronic intoxication [24].
If the initial diagnosis is unclear, brain imaging may be required[25].
Lithium serum levels normally range from approximately 0.
 6 to 1.2 mEq/L. Measurement of the serum levels should be carried out at least 6 to 12 hours after the last therapeutic dose to avoid misinterpretation of pre-distributional levels.
6 to 1.2 mEq/L. Measurement of the serum levels should be carried out at least 6 to 12 hours after the last therapeutic dose to avoid misinterpretation of pre-distributional levels.
Of note, lithium heparin is used as an anticoagulant in some specimen tubes which can falsely increase results of serum lithium [26].
Treatment / Management
Decontamination
In-vitro studies showed that lithium does not adhere effectively to activated charcoal [27]; however, if co-ingestants are unknown, charcoal should be administered [8].
Gastric lavage should be considered, particularly in the case of regular-release preparations and patients presenting early to the emergency department. On the other hand, in case of sustained-release preparations, administration, or massive ingestion of regular-release products, whole-bowel irrigation should also be considered [8].
Elimination
The most appropriate method of lithium removal is hemodialysis, particularly if the patient demonstrates signs and symptoms of severe lithium poisoning or is having a renal failure due to its small volume of distribution and marginal protein binding [28].
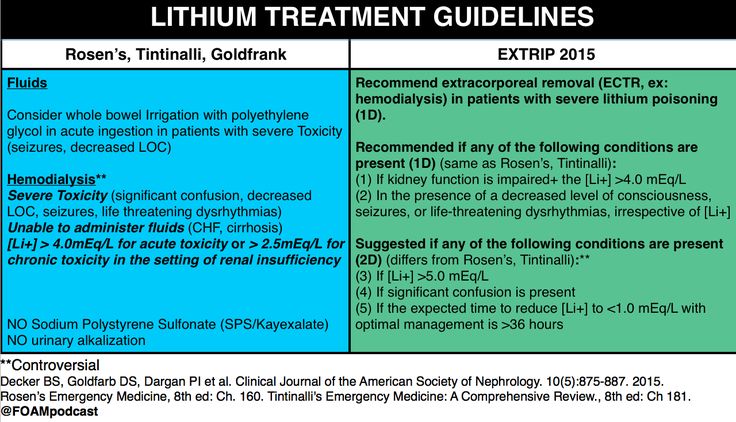
Peritoneal dialysis should not replace hemodialysis; however, if the hemodialysis facilities are not available (e.g., in remote areas), peritoneal dialysis can be initiated[28].
Disposition
All patients with toxicity signs and symptoms, even those with normal serum lithium levels, should be admitted for monitoring in the hospital.
In case of moderate or severe symptoms, the patient has to be admitted to an intensive care unit.
Serial levels of lithium in the serum should be obtained every 6 hours in case of asymptomatic patients after acute ingestion. This should be continued until a descending drift has been established.
Patients should not be discharged until they are asymptomatic and have a serum lithium level less than 1.5 mEq/L.
Differential Diagnosis
Acute hypoglycemia
Alcohol toxicity
Delirium
Dementia
Depression
Mercury toxicity
Stroke, ischemic
Staging
Lithium toxicity can be classified into three major categories:
Acute overdose in a lithium-naive patient [9].
Acute overdose in a patient on chronic therapy (acute-on-chronic)[29].
Chronic over-medication or drug accumulation (associated with the most serious toxicity) [30].
Prognosis
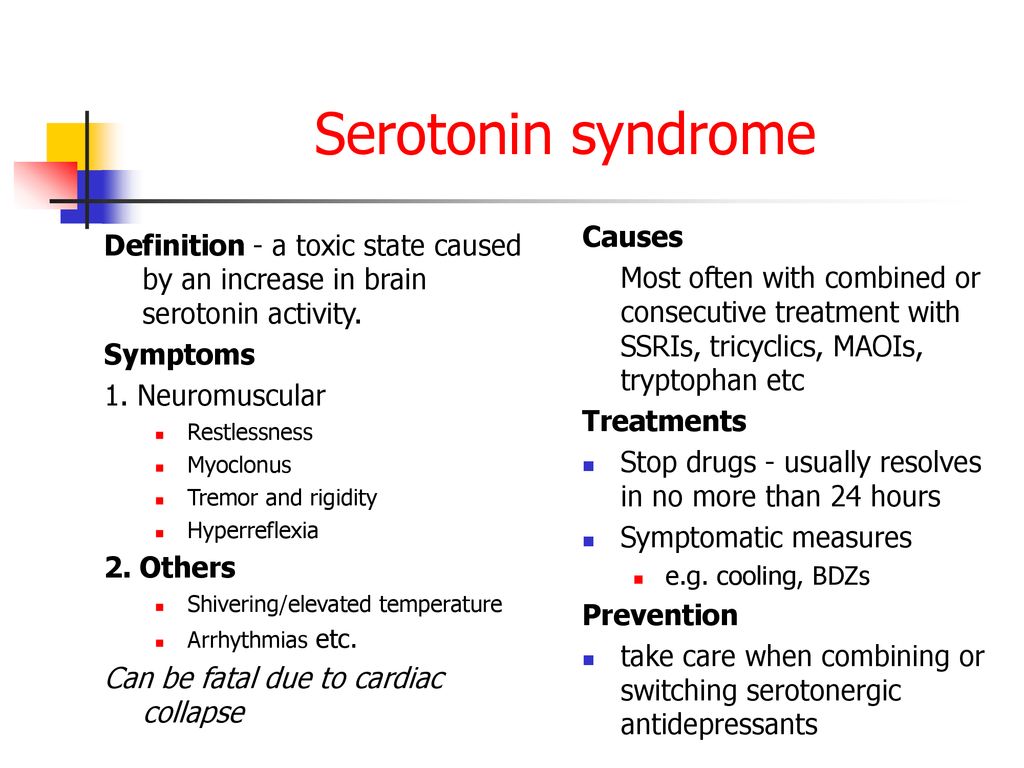
Lithium toxicity signs are obvious and can be identified and managed easily; however, ignoring it can be fatal. Indeed, in some cases, lithium toxicity can lead to coma, brain damage, or even death. Moreover, lithium can induce serotonin syndrome, a potentially fatal and life-threatening condition[31]. The use of serotonergic drugs or drugs inhibiting serotonin metabolism concomitantly with lithium will increase the risk of lithium precipitating serotonin syndrome[32].
Complications
Intoxication degree is of utmost importance for understanding lithium toxicity diagnosis and management.
The severity of lithium toxicity is often divided into the following three grades: mild, moderate, and severe.
Mild symptoms: nausea, vomiting, lethargy, tremor, and fatigue (Serum lithium concentration between 1.
 5-2.5 mEq/L)[33] [34].
5-2.5 mEq/L)[33] [34].Moderate intoxication: confusion, agitation, delirium, tachycardia, and hypertonia (serum lithium concentration between 2.5-3.5 mEq/L)[33] [34].
Severe intoxication: Coma, seizures, hyperthermia, and hypotension (serum lithium concentration (more than 3.5 mEq/L)[33] [34].
Enhancing Healthcare Team Outcomes
During lithium treatment, the healthcare team including physicians and nurses should make sure serum levels are checked regularly to make sure of the treatment course. Lithium is classified as pregnancy category D which means that there is positive evidence of human fetal risk. Therefore, the nurses or clinician should educate the patient on a proper contraceptive method during treatment with lithium. If any signs of early toxicity appear, the patient should stop the medication and seek medical counsel. Extra care should be taken if any activity, illness, or medication might precipitate a profound loss of water and/or salt is taken in a patient administering lithium. [Level 5]
[Level 5]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Vieta E, Sanchez-Moreno J. Acute and long-term treatment of mania. Dialogues Clin Neurosci. 2008;10(2):165-79. [PMC free article: PMC3181868] [PubMed: 18689287]
- 2.
Gajwani P, Kemp DE, Muzina DJ, Xia G, Gao K, Calabrese JR. Acute treatment of mania: an update on new medications. Curr Psychiatry Rep. 2006 Dec;8(6):504-9. [PubMed: 17094930]
- 3.
Ware K, Tillery E, Linder L. General pharmacokinetic/pharmacodynamic concepts of mood stabilizers in the treatment of bipolar disorder. Ment Health Clin. 2016 Jan;6(1):54-61. [PMC free article: PMC6009247] [PubMed: 29955448]
- 4.
Oruch R, Elderbi MA, Khattab HA, Pryme IF, Lund A. Lithium: a review of pharmacology, clinical uses, and toxicity. Eur J Pharmacol. 2014 Oct 05;740:464-73. [PubMed: 24991789]
- 5.
Risby ED, Hsiao JK, Manji HK, Bitran J, Moses F, Zhou DF, Potter WZ. The mechanisms of action of lithium. II. Effects on adenylate cyclase activity and beta-adrenergic receptor binding in normal subjects. Arch Gen Psychiatry. 1991 Jun;48(6):513-24. [PubMed: 1645514]
- 6.
Treiser SL, Cascio CS, O'Donohue TL, Thoa NB, Jacobowitz DM, Kellar KJ. Lithium increases serotonin release and decreases serotonin receptors in the hippocampus. Science. 1981 Sep 25;213(4515):1529-31. [PubMed: 6269180]
- 7.
Jakobsson E, Argüello-Miranda O, Chiu SW, Fazal Z, Kruczek J, Nunez-Corrales S, Pandit S, Pritchet L. Towards a Unified Understanding of Lithium Action in Basic Biology and its Significance for Applied Biology. J Membr Biol. 2017 Dec;250(6):587-604. [PMC free article: PMC5696506] [PubMed: 29127487]
- 8.
Haussmann R, Bauer M, von Bonin S, Grof P, Lewitzka U. Treatment of lithium intoxication: facing the need for evidence. Int J Bipolar Disord.
 2015 Dec;3(1):23. [PMC free article: PMC4615994] [PubMed: 26493348]
2015 Dec;3(1):23. [PMC free article: PMC4615994] [PubMed: 26493348]- 9.
Ott M, Stegmayr B, Salander Renberg E, Werneke U. Lithium intoxication: Incidence, clinical course and renal function - a population-based retrospective cohort study. J Psychopharmacol. 2016 Oct;30(10):1008-19. [PMC free article: PMC5036078] [PubMed: 27307388]
- 10.
Fiaccadori E, Maggiore U, Parenti E, Greco P, Cabassi A. Sustained low-efficiency dialysis (SLED) for acute lithium intoxication. NDT Plus. 2008 Oct;1(5):329-32. [PMC free article: PMC4421258] [PubMed: 25983926]
- 11.
Chien SC, Liu KT, Wu YH. Lithium intoxication presenting as altered consciousness and arrhythmia with cardiogenic shock: A case report. Medicine (Baltimore). 2018 Nov;97(45):e13129. [PMC free article: PMC6250446] [PubMed: 30407335]
- 12.
Erden A, Karagöz H, Başak M, Karahan S, Cetinkaya A, Avci D, Bugǧday I. Lithium intoxication and nephrogenic diabetes insipidus: a case report and review of literature.
 Int J Gen Med. 2013;6:535-9. [PMC free article: PMC3704402] [PubMed: 23861592]
Int J Gen Med. 2013;6:535-9. [PMC free article: PMC3704402] [PubMed: 23861592]- 13.
Horton S, Tuerk A, Cook D, Cook J, Dhurjati P. Maximum Recommended Dosage of Lithium for Pregnant Women Based on a PBPK Model for Lithium Absorption. Adv Bioinformatics. 2012;2012:352729. [PMC free article: PMC3369391] [PubMed: 22693500]
- 14.
Kishore BK, Ecelbarger CM. Lithium: a versatile tool for understanding renal physiology. Am J Physiol Renal Physiol. 2013 May 01;304(9):F1139-49. [PMC free article: PMC3651632] [PubMed: 23408166]
- 15.
Mohandas E, Rajmohan V. Lithium use in special populations. Indian J Psychiatry. 2007 Jul;49(3):211-8. [PMC free article: PMC2902097] [PubMed: 20661390]
- 16.
Grandjean EM, Aubry JM. Lithium: updated human knowledge using an evidence-based approach. Part II: Clinical pharmacology and therapeutic monitoring. CNS Drugs. 2009;23(4):331-49. [PubMed: 19374461]
- 17.
López-Muñoz F, Shen WW, D'Ocon P, Romero A, Álamo C.
 A History of the Pharmacological Treatment of Bipolar Disorder. Int J Mol Sci. 2018 Jul 23;19(7) [PMC free article: PMC6073684] [PubMed: 30041458]
A History of the Pharmacological Treatment of Bipolar Disorder. Int J Mol Sci. 2018 Jul 23;19(7) [PMC free article: PMC6073684] [PubMed: 30041458]- 18.
Foulser P, Abbasi Y, Mathilakath A, Nilforooshan R. Do not treat the numbers: lithium toxicity. BMJ Case Rep. 2017 Jun 02;2017 [PMC free article: PMC5534930] [PubMed: 28576914]
- 19.
Davis J, Desmond M, Berk M. Lithium and nephrotoxicity: a literature review of approaches to clinical management and risk stratification. BMC Nephrol. 2018 Nov 03;19(1):305. [PMC free article: PMC6215627] [PubMed: 30390660]
- 20.
Canan F, Kaya A, Bulur S, Albayrak ES, Ordu S, Ataoglu A. Lithium intoxication related multiple temporary ecg changes: A case report. Cases J. 2008 Sep 17;1(1):156. [PMC free article: PMC2566567] [PubMed: 18799007]
- 21.
Kibirige D, Luzinda K, Ssekitoleko R. Spectrum of lithium induced thyroid abnormalities: a current perspective. Thyroid Res. 2013 Feb 07;6(1):3.
 [PMC free article: PMC3568739] [PubMed: 23391071]
[PMC free article: PMC3568739] [PubMed: 23391071]- 22.
Maddala RNM, Ashwal AJ, Rao MS, Padmakumar R. Chronic lithium intoxication: Varying electrocardiogram manifestations. Indian J Pharmacol. 2017 Jan-Feb;49(1):127-129. [PMC free article: PMC5351227] [PubMed: 28458438]
- 23.
Kelleher SP, Raciti A, Arbeit LA. Reduced or absent serum anion gap as a marker of severe lithium carbonate intoxication. Arch Intern Med. 1986 Sep;146(9):1839-40. [PubMed: 3092758]
- 24.
Gitlin M. Lithium side effects and toxicity: prevalence and management strategies. Int J Bipolar Disord. 2016 Dec;4(1):27. [PMC free article: PMC5164879] [PubMed: 27900734]
- 25.
Forester BP, Streeter CC, Berlow YA, Tian H, Wardrop M, Finn CT, Harper D, Renshaw PF, Moore CM. Brain lithium levels and effects on cognition and mood in geriatric bipolar disorder: a lithium-7 magnetic resonance spectroscopy study. Am J Geriatr Psychiatry. 2009 Jan;17(1):13-23.
 [PMC free article: PMC4085782] [PubMed: 18626002]
[PMC free article: PMC4085782] [PubMed: 18626002]- 26.
Biancotto A, Feng X, Langweiler M, Young NS, McCoy JP. Effect of anticoagulants on multiplexed measurement of cytokine/chemokines in healthy subjects. Cytokine. 2012 Nov;60(2):438-46. [PMC free article: PMC3449030] [PubMed: 22705152]
- 27.
Favin FD, Klein-Schwartz W, Oderda GM, Rose SR. In vitro study of lithium carbonate adsorption by activated charcoal. J Toxicol Clin Toxicol. 1988;26(7):443-50. [PubMed: 3148035]
- 28.
Amdisen A. Clinical features and management of lithium poisoning. Med Toxicol Adverse Drug Exp. 1988 Jan-Dec;3(1):18-32. [PubMed: 3285125]
- 29.
Bretaudeau Deguigne M, Hamel JF, Boels D, Harry P. Early digestive tract decontamination in acute-on-chronic lithium poisoning does not call conventional therapy into question. Clin Toxicol (Phila). 2013 Sep-Oct;51(8):809. [PubMed: 23902331]
- 30.
Mégarbane B, Hanak AS, Chevillard L.
 Lithium-related neurotoxicity despite serum concentrations in the therapeutic range: risk factors and diagnosis. Shanghai Arch Psychiatry. 2014 Aug;26(4):243-4. [PMC free article: PMC4194008] [PubMed: 25317012]
Lithium-related neurotoxicity despite serum concentrations in the therapeutic range: risk factors and diagnosis. Shanghai Arch Psychiatry. 2014 Aug;26(4):243-4. [PMC free article: PMC4194008] [PubMed: 25317012]- 31.
Netto I, Phutane VH. Reversible lithium neurotoxicity: review of the literatur. Prim Care Companion CNS Disord. 2012;14(1) [PMC free article: PMC3357580] [PubMed: 22690368]
- 32.
Adan-Manes J, Novalbos J, López-Rodríguez R, Ayuso-Mateos JL, Abad-Santos F. Lithium and venlafaxine interaction: a case of serotonin syndrome. J Clin Pharm Ther. 2006 Aug;31(4):397-400. [PubMed: 16882112]
- 33.
Boltan DD, Fenves AZ. Effectiveness of normal saline diuresis in treating lithium overdose. Proc (Bayl Univ Med Cent). 2008 Jul;21(3):261-3. [PMC free article: PMC2446416] [PubMed: 18628924]
- 34.
Dunne FJ. Lithium toxicity: the importance of clinical signs. Br J Hosp Med (Lond). 2010 Apr;71(4):206-10. [PubMed: 20393430]
📖 Acute lithium poisoning, Diagnosis and treatment of intoxication caused by an increase in the concentration of lithium in the blood plasma, Chapter 4.
 Normotimics (mood stabilizers). Guide to psychopharmacotherapy. Arana D. Page 34. Read online
Normotimics (mood stabilizers). Guide to psychopharmacotherapy. Arana D. Page 34. Read online For mild intoxication, should temporarily stop taking lithium until the concentration normalizes. If the cause of the increase in concentration is not found, the function of the kidneys should be checked conduct a urinalysis and determine the creatinine clearance.
In case of moderate and severe intoxication, the patient must be hospitalized. It is necessary to prescribe sodium and measure the concentration of lithium in the blood plasma several times a day. In the absence of heart and kidney failure, intravenous saline at a rate of 150–200 ml per hour is often effective in rapidly lowering lithium concentrations. This method is safe with adequate diuresis.
Acute lithium poisoning.
Acute lithium poisoning is a critical condition that manifests itself with a characteristic clinical syndrome and develops at a lithium concentration above 3.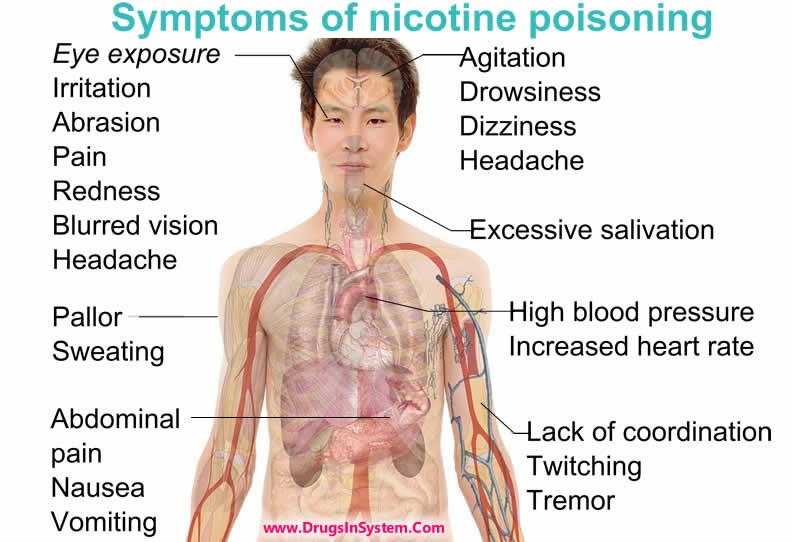 0 mmol / l. The severity and reversibility of intoxication are determined by the concentration of lithium and the duration of high doses of the drug. Therefore, even in the absence of clinical manifestations, emergency treatment is necessary. Indeed, in the early stages of poisoning, despite the high levels of lithium, the clinical manifestations can be relatively mild, so the doctor may underestimate the danger of the situation. Severe poisoning is characterized by both general and neurological symptoms: nausea, vomiting, diarrhea, renal failure, increased neuromuscular excitability or muscle weakness, ataxia, dysarthria, gross tremor, confusion, delirium, hallucinations, epileptic seizures and stupor. Cases of prolonged coma and glucose intolerance have been described. Severe lithium poisoning can also cause death. Patients who survive severe lithium poisoning may develop prolonged cerebellar ataxia and severe anterograde amnesia.
0 mmol / l. The severity and reversibility of intoxication are determined by the concentration of lithium and the duration of high doses of the drug. Therefore, even in the absence of clinical manifestations, emergency treatment is necessary. Indeed, in the early stages of poisoning, despite the high levels of lithium, the clinical manifestations can be relatively mild, so the doctor may underestimate the danger of the situation. Severe poisoning is characterized by both general and neurological symptoms: nausea, vomiting, diarrhea, renal failure, increased neuromuscular excitability or muscle weakness, ataxia, dysarthria, gross tremor, confusion, delirium, hallucinations, epileptic seizures and stupor. Cases of prolonged coma and glucose intolerance have been described. Severe lithium poisoning can also cause death. Patients who survive severe lithium poisoning may develop prolonged cerebellar ataxia and severe anterograde amnesia.
Psychology bookap
In the treatment of acute lithium intoxication, the main goal is to remove lithium from the body as soon as possible. It is necessary to do a toxicological examination in order to find out what other drugs the patient was taking. This is especially important in case of deliberate overdose. If the patient is in a state of coma or stupor, first of all it is necessary to provide airway patency (if necessary with intubation) and cardiorespiratory care. If less than 4 hours have passed since the moment of poisoning, in patients who are conscious, it is necessary to stimulate vomiting, and in patients in a coma, gastric lavage should be done. Since a high concentration of lithium is often found in the gastric juice, prolonged aspiration of the stomach is indicated.
It is necessary to do a toxicological examination in order to find out what other drugs the patient was taking. This is especially important in case of deliberate overdose. If the patient is in a state of coma or stupor, first of all it is necessary to provide airway patency (if necessary with intubation) and cardiorespiratory care. If less than 4 hours have passed since the moment of poisoning, in patients who are conscious, it is necessary to stimulate vomiting, and in patients in a coma, gastric lavage should be done. Since a high concentration of lithium is often found in the gastric juice, prolonged aspiration of the stomach is indicated.
Although lithium toxicity is now rare, precautions must be taken. If the lithium concentration does not exceed 3 mmol / l and signs of intoxication are mild, it is possible to correct water and electrolyte imbalance and normalize diuresis by injecting saline at a rate of 150-200 ml / h (with adequate diuresis). In cases where the concentration of lithium exceeds 3 mmol / l and signs of intoxication are pronounced, as well as in cases of reduced diuresis or renal failure, dialysis should be performed immediately.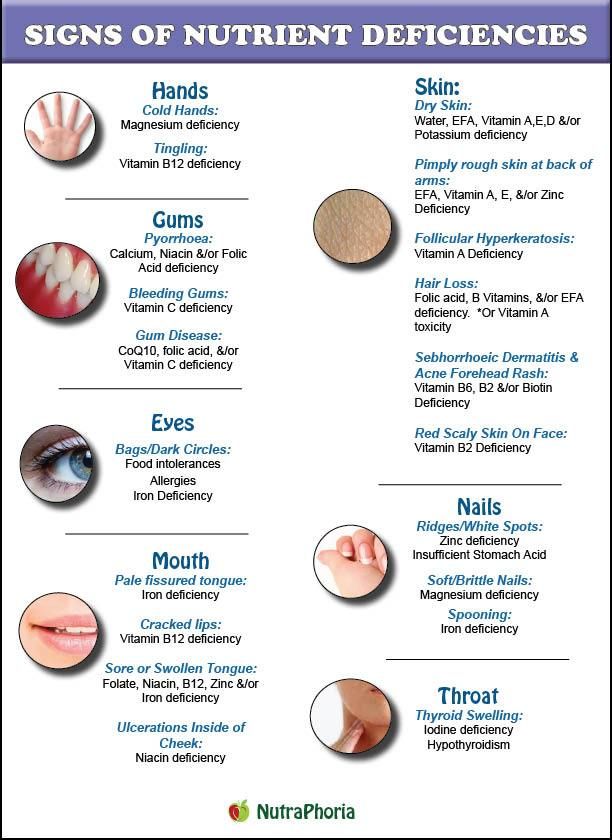 If the lithium concentration is above 4 mmol/l and does not decrease within a few hours at a saline infusion rate of 250 ml/h, dialysis is performed regardless of clinical manifestations. The most effective method is hemodialysis, but peritoneal dialysis can also be used. After dialysis, lithium enters the blood from the tissues, so it is necessary to determine the concentration of lithium in the blood plasma. If 6 hours after dialysis, the lithium concentration has decreased to 1.0 mmol / l or less, you can stop dialysis.
If the lithium concentration is above 4 mmol/l and does not decrease within a few hours at a saline infusion rate of 250 ml/h, dialysis is performed regardless of clinical manifestations. The most effective method is hemodialysis, but peritoneal dialysis can also be used. After dialysis, lithium enters the blood from the tissues, so it is necessary to determine the concentration of lithium in the blood plasma. If 6 hours after dialysis, the lithium concentration has decreased to 1.0 mmol / l or less, you can stop dialysis.
Causes of intoxication.
Although an increase in concentration can occur as a result of an overdose, more often this occurs as a result of imbalance of sodium . Any cause that causes sodium depletion, such as dehydration, a change in diet (either to restrict salt or to reduce weight), or the use of diuretics that cause sodium loss, can cause an increase in lithium concentration. It has been suggested that lithium intoxication may occur with increased sweating due to heavy exercise or heat.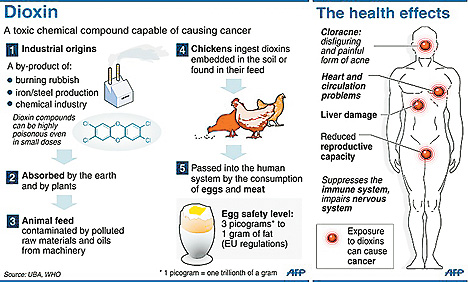 However, a sufficient amount of lithium is excreted in sweat, so increased sweating does not increase the concentration of lithium. Lithium is retained in the body as a result of impaired renal blood flow, which can be caused by taking large amounts of NSAIDs (except aspirin) in susceptible patients, patients with kidney disease and systemic diseases (heart failure and cirrhosis).
However, a sufficient amount of lithium is excreted in sweat, so increased sweating does not increase the concentration of lithium. Lithium is retained in the body as a result of impaired renal blood flow, which can be caused by taking large amounts of NSAIDs (except aspirin) in susceptible patients, patients with kidney disease and systemic diseases (heart failure and cirrhosis).
Lithium poisoning
The most common sources of lithium are drugs lithium carbonate And lithium citrate . The action of lithium is largely due to its similarity with sodium . In particular, it inhibits the activation adenylate cyclase , reduces release norepinephrine and activity Na+,K+-ATPase .
Lithium is rapidly absorbed from the gastrointestinal tract. Its serum concentration reaches maximum 2-4 hours after ingestion (with overdose and ingestion long-acting drugs - later). With plasma proteins, it is almost contacts. Its volume of distribution is about 0.6 l/kg.
Lithium is 95% excreted in the urine, the remaining 5% - with sweat and (minor quantity) with feces.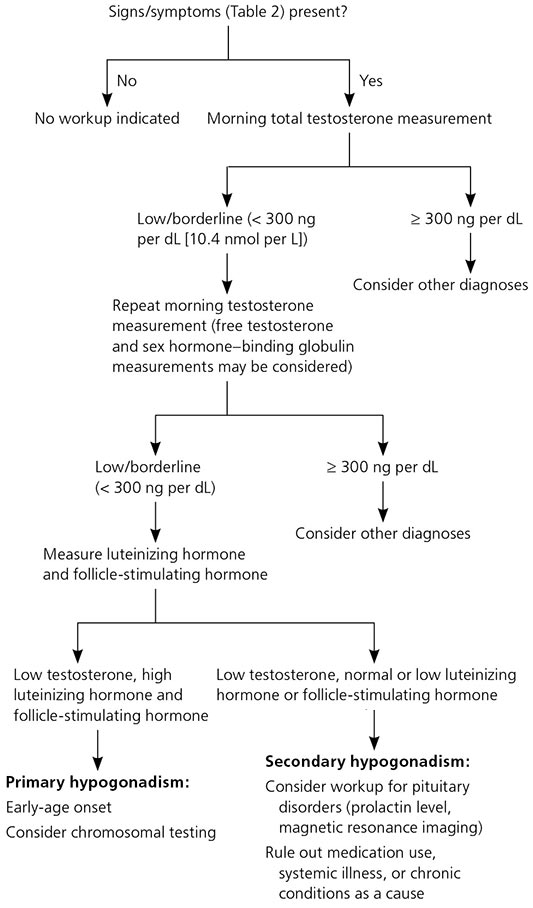 In the kidneys, after filtration, lithium is reabsorbed by 80%. in the proximal tubules. Lithium excretion increases with alkalization urine and decreases with hypovolemia And hyponatremia . T1 / 2 is 18-36 hours, therapeutic serum concentration - 0.6-1.2 mmol / l.
In the kidneys, after filtration, lithium is reabsorbed by 80%. in the proximal tubules. Lithium excretion increases with alkalization urine and decreases with hypovolemia And hyponatremia . T1 / 2 is 18-36 hours, therapeutic serum concentration - 0.6-1.2 mmol / l.
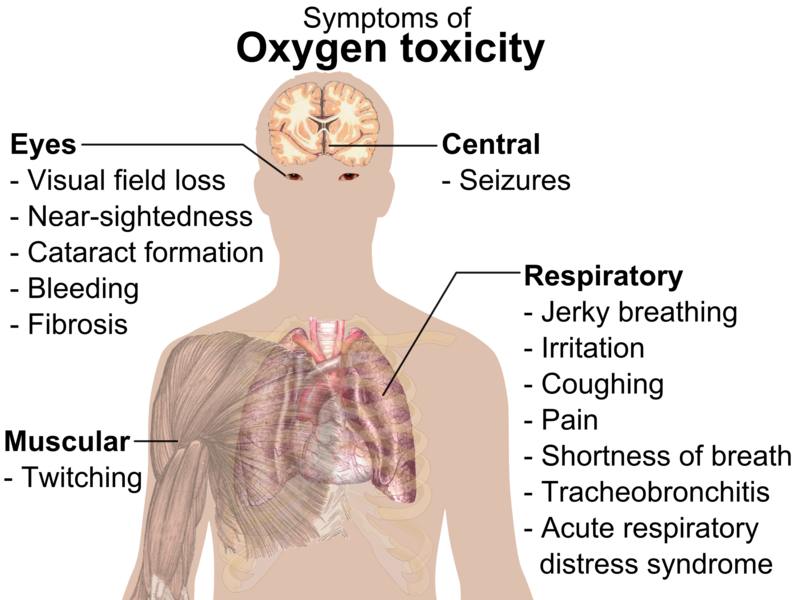
clinical picture. Symptoms appear 1-4 hours after ingestion. Arise nausea , vomit And diarrhea . Characteristic neuromuscular disorders ( weakness , muscle twitching ), neurological disorders ( ataxia , tremor , myoclonus , choreoathetosis , epileptic seizures , confusion , coma ) And cardiovascular disorders ( arterial hypotension , cardiac arrhythmias ). Possible hypothermia .
In a laboratory study, they find leukocytosis , hyperglycemia , albuminuria , glycosuria , and polyuria And urine hypoosmolality (signs nephrogenic diabetes insipidus ). On ECG visible sinus tachycardia or bradycardia , flattened or inverted T waves , AV block , prolongation of the QT interval .
In chronic poisoning, symptoms may develop gradually, but with lower serum lithium concentrations.
Diagnostics. In standard toxicology testing, lithium does not is detected, and therefore the determination of its serum concentration is necessary order specially. In chronic poisoning, severe symptoms observed already at a serum lithium concentration of about 3-4 mmol / l, and in acute it can be scarce even at a concentration of 8 mmol / l and above. Since the absorption of lithium may be slowed down during poisoning, it serum concentration should be determined several times.
TREATMENT. If no more than 4 hours have passed after taking lithium, measures to remove the toxic substance from the gastrointestinal tract. Activated carbon poorly adsorbs lithium. Vomit usually occurs spontaneously, and therefore, first of all, carry out lavage of the stomach and intestines (especially in case of poisoning with drugs long term). At epileptic seizures , CNS depression , arterial hypotension And arrhythmias treatment is usual.