Major depressive diagnosis
Depression (major depressive disorder) - Diagnosis and treatment
Diagnosis
Your doctor may determine a diagnosis of depression based on:
- Physical exam. Your doctor may do a physical exam and ask questions about your health. In some cases, depression may be linked to an underlying physical health problem.
- Lab tests. For example, your doctor may do a blood test called a complete blood count or test your thyroid to make sure it's functioning properly.
- Psychiatric evaluation. Your mental health professional asks about your symptoms, thoughts, feelings and behavior patterns. You may be asked to fill out a questionnaire to help answer these questions.
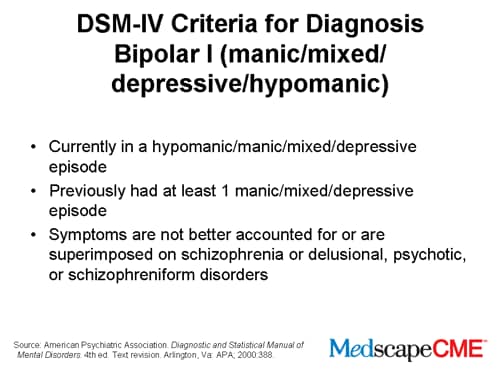
- DSM-5. Your mental health professional may use the criteria for depression listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
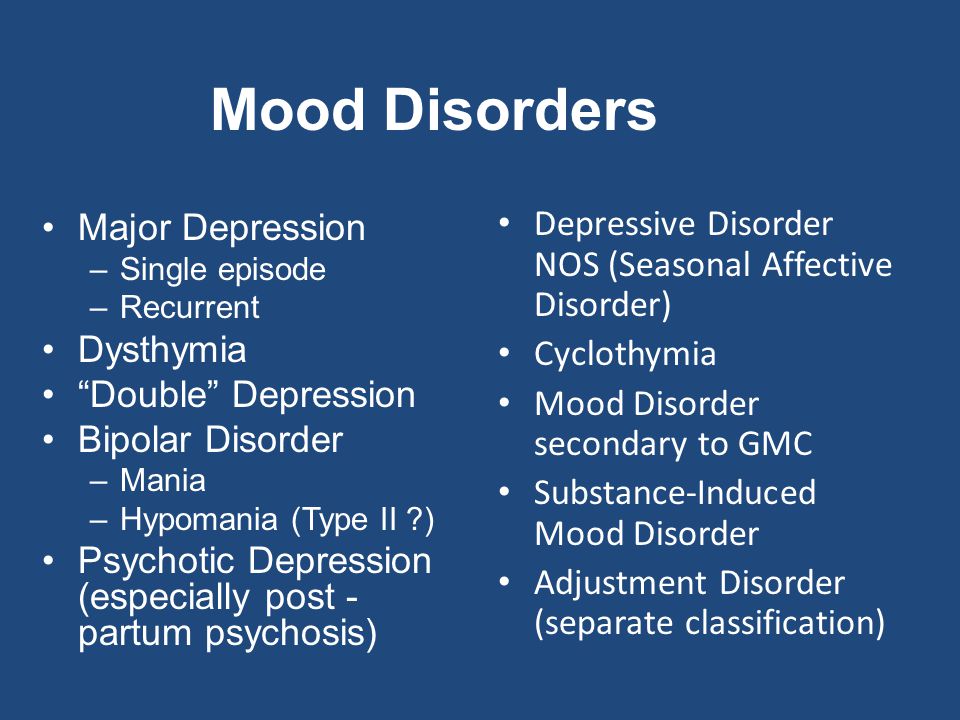
Types of depression
Symptoms caused by major depression can vary from person to person. To clarify the type of depression you have, your doctor may add one or more specifiers. A specifier means that you have depression with specific features, such as:
- Anxious distress — depression with unusual restlessness or worry about possible events or loss of control
- Mixed features — simultaneous depression and mania, which includes elevated self-esteem, talking too much and increased energy
- Melancholic features — severe depression with lack of response to something that used to bring pleasure and associated with early morning awakening, worsened mood in the morning, major changes in appetite, and feelings of guilt, agitation or sluggishness
- Atypical features — depression that includes the ability to temporarily be cheered by happy events, increased appetite, excessive need for sleep, sensitivity to rejection, and a heavy feeling in the arms or legs
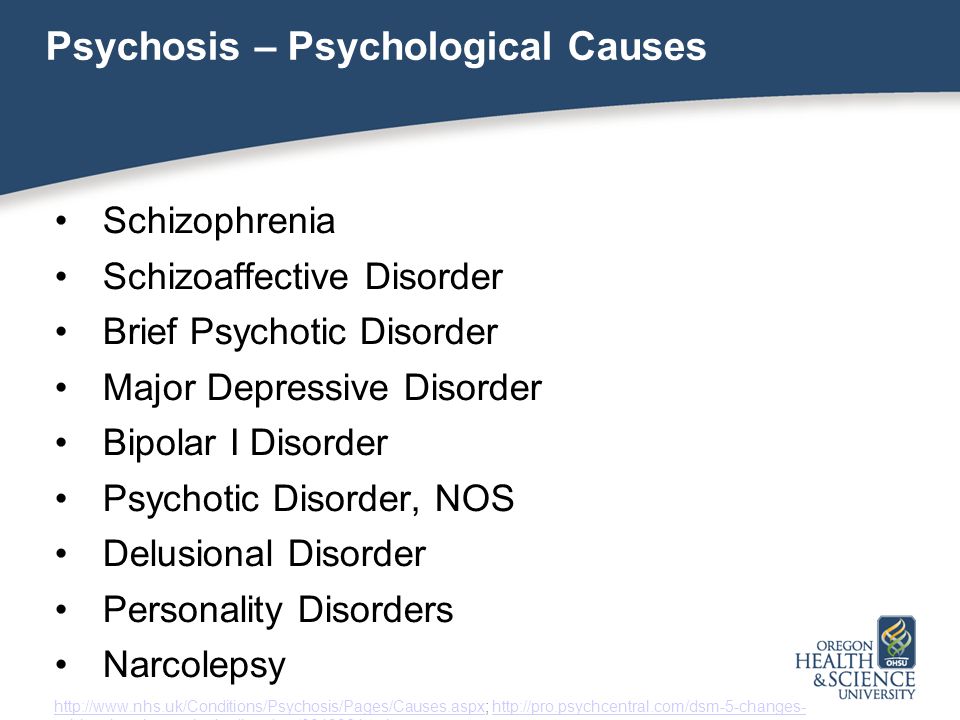
- Psychotic features — depression accompanied by delusions or hallucinations, which may involve personal inadequacy or other negative themes
- Catatonia — depression that includes motor activity that involves either uncontrollable and purposeless movement or fixed and inflexible posture
- Peripartum onset — depression that occurs during pregnancy or in the weeks or months after delivery (postpartum)
- Seasonal pattern — depression related to changes in seasons and reduced exposure to sunlight
Other disorders that cause depression symptoms
Several other disorders, such as those below, include depression as a symptom. It's important to get an accurate diagnosis, so you can get appropriate treatment.
It's important to get an accurate diagnosis, so you can get appropriate treatment.
- Bipolar I and II disorders. These mood disorders include mood swings that range from highs (mania) to lows (depression). It's sometimes difficult to distinguish between bipolar disorder and depression.
- Cyclothymic disorder. Cyclothymic (sy-kloe-THIE-mik) disorder involves highs and lows that are milder than those of bipolar disorder.
- Disruptive mood dysregulation disorder. This mood disorder in children includes chronic and severe irritability and anger with frequent extreme temper outbursts. This disorder typically develops into depressive disorder or anxiety disorder during the teen years or adulthood.
- Persistent depressive disorder. Sometimes called dysthymia (dis-THIE-me-uh), this is a less severe but more chronic form of depression. While it's usually not disabling, persistent depressive disorder can prevent you from functioning normally in your daily routine and from living life to its fullest.

- Premenstrual dysphoric disorder. This involves depression symptoms associated with hormone changes that begin a week before and improve within a few days after the onset of your period, and are minimal or gone after completion of your period.
- Other depression disorders. This includes depression that's caused by the use of recreational drugs, some prescribed medications or another medical condition.
Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your depression (major depressive disorder)-related health concerns Start Here
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Complete blood count (CBC)
Treatment
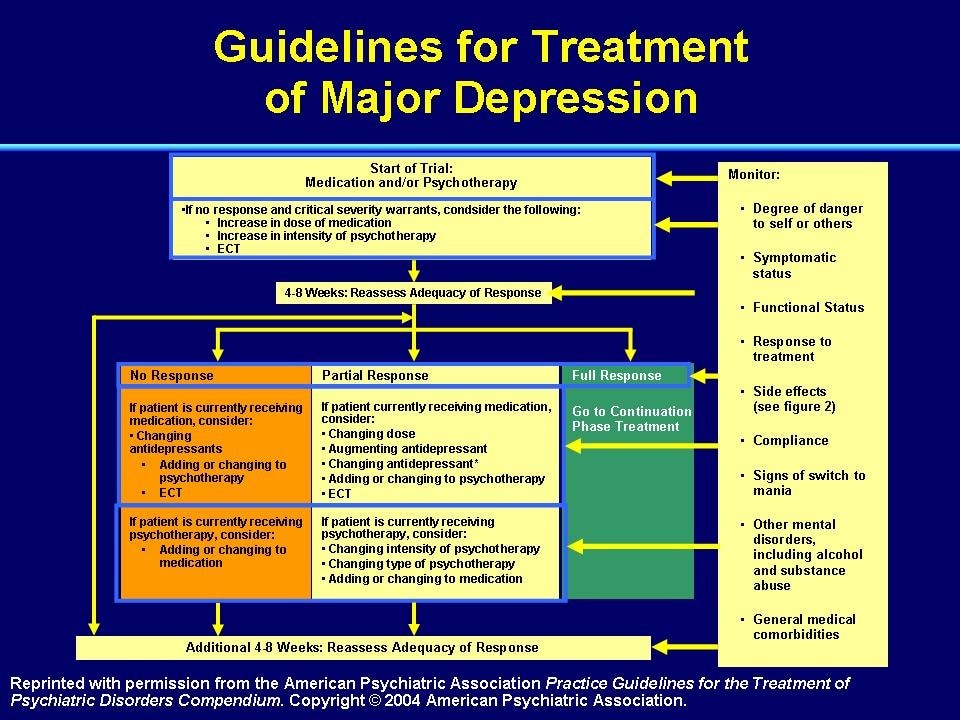
Medications and psychotherapy are effective for most people with depression. Your primary care doctor or psychiatrist can prescribe medications to relieve symptoms.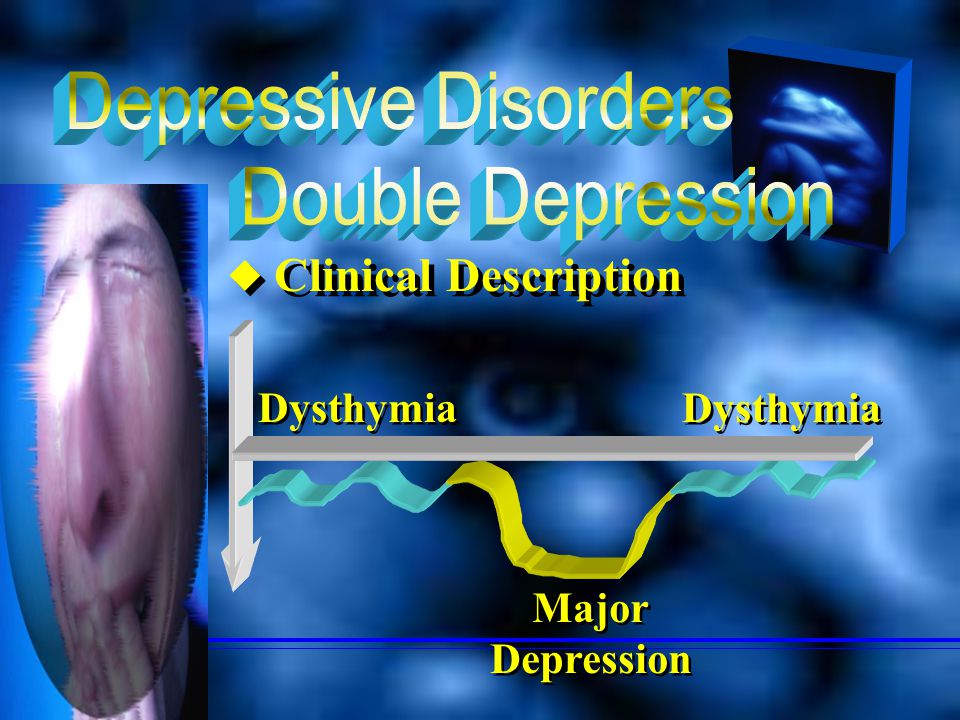 However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
However, many people with depression also benefit from seeing a psychiatrist, psychologist or other mental health professional.
If you have severe depression, you may need a hospital stay, or you may need to participate in an outpatient treatment program until your symptoms improve.
Here's a closer look at depression treatment options.
Medications
Many types of antidepressants are available, including those below. Be sure to discuss possible major side effects with your doctor or pharmacist.
- Selective serotonin reuptake inhibitors (SSRIs). Doctors often start by prescribing an SSRI. These drugs are considered safer and generally cause fewer bothersome side effects than other types of antidepressants. SSRIs include citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil, Pexeva), sertraline (Zoloft) and vilazodone (Viibryd).
- Serotonin-norepinephrine reuptake inhibitors (SNRIs). Examples of SNRIs include duloxetine (Cymbalta), venlafaxine (Effexor XR), desvenlafaxine (Pristiq, Khedezla) and levomilnacipran (Fetzima).
- Atypical antidepressants. These medications don't fit neatly into any of the other antidepressant categories. They include bupropion (Wellbutrin XL, Wellbutrin SR, Aplenzin, Forfivo XL), mirtazapine (Remeron), nefazodone, trazodone and vortioxetine (Trintellix).
- Tricyclic antidepressants. These drugs — such as imipramine (Tofranil), nortriptyline (Pamelor), amitriptyline, doxepin, trimipramine (Surmontil), desipramine (Norpramin) and protriptyline (Vivactil) — can be very effective, but tend to cause more-severe side effects than newer antidepressants. So tricyclics generally aren't prescribed unless you've tried an SSRI first without improvement.
- Monoamine oxidase inhibitors (MAOIs). MAOIs — such as tranylcypromine (Parnate), phenelzine (Nardil) and isocarboxazid (Marplan) — may be prescribed, typically when other drugs haven't worked, because they can have serious side effects. Using MAOIs requires a strict diet because of dangerous (or even deadly) interactions with foods ― such as certain cheeses, pickles and wines ― and some medications and herbal supplements.
 Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs.
Selegiline (Emsam), a newer MAOI that sticks on the skin as a patch, may cause fewer side effects than other MAOIs do. These medications can't be combined with SSRIs. - Other medications. Other medications may be added to an antidepressant to enhance antidepressant effects. Your doctor may recommend combining two antidepressants or adding medications such as mood stabilizers or antipsychotics. Anti-anxiety and stimulant medications also may be added for short-term use.
Finding the right medication
If a family member has responded well to an antidepressant, it may be one that could help you. Or you may need to try several medications or a combination of medications before you find one that works. This requires patience, as some medications need several weeks or longer to take full effect and for side effects to ease as your body adjusts.
Inherited traits play a role in how antidepressants affect you. In some cases, where available, results of genetic tests (done by a blood test or cheek swab) may offer clues about how your body may respond to a particular antidepressant.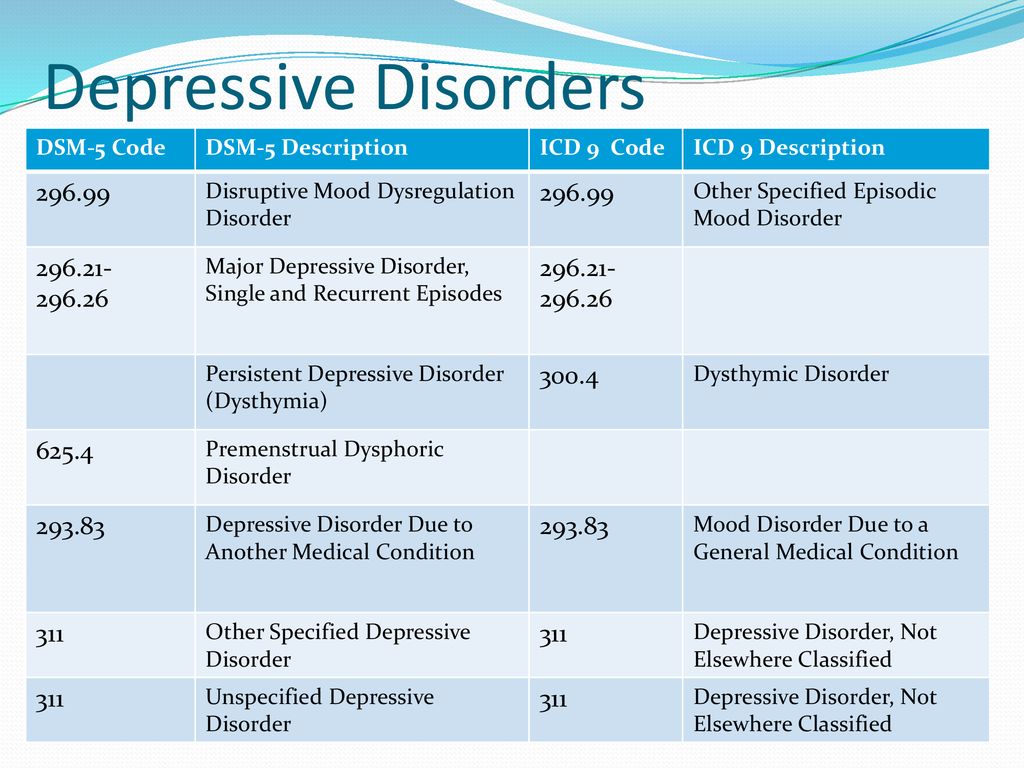 However, other variables besides genetics can affect your response to medication.
However, other variables besides genetics can affect your response to medication.
Risks of abruptly stopping medication
Don't stop taking an antidepressant without talking to your doctor first. Antidepressants aren't considered addictive, but sometimes physical dependence (which is different from addiction) can occur.
Stopping treatment abruptly or missing several doses can cause withdrawal-like symptoms, and quitting suddenly may cause a sudden worsening of depression. Work with your doctor to gradually and safely decrease your dose.
Antidepressants and pregnancy
If you're pregnant or breast-feeding, some antidepressants may pose an increased health risk to your unborn child or nursing child. Talk with your doctor if you become pregnant or you're planning to become pregnant.
Antidepressants and increased suicide risk
Most antidepressants are generally safe, but the Food and Drug Administration (FDA) requires all antidepressants to carry a black box warning, the strictest warning for prescriptions.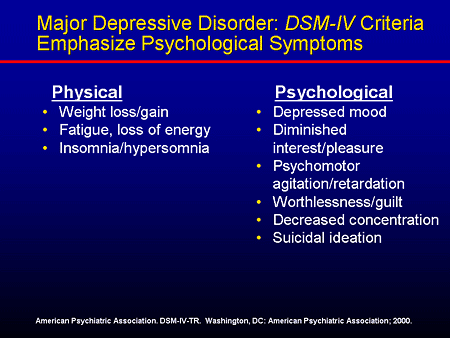 In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
In some cases, children, teenagers and young adults under age 25 may have an increase in suicidal thoughts or behavior when taking antidepressants, especially in the first few weeks after starting or when the dose is changed.
Anyone taking an antidepressant should be watched closely for worsening depression or unusual behavior, especially when starting a new medication or with a change in dosage. If you or someone you know has suicidal thoughts when taking an antidepressant, immediately contact a doctor or get emergency help.
Keep in mind that antidepressants are more likely to reduce suicide risk in the long run by improving mood.
Psychotherapy
Psychotherapy is a general term for treating depression by talking about your condition and related issues with a mental health professional. Psychotherapy is also known as talk therapy or psychological therapy.
Different types of psychotherapy can be effective for depression, such as cognitive behavioral therapy or interpersonal therapy.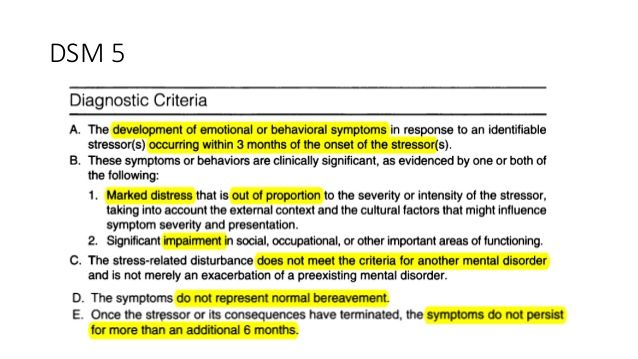 Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
Your mental health professional may also recommend other types of therapies. Psychotherapy can help you:
- Adjust to a crisis or other current difficulty
- Identify negative beliefs and behaviors and replace them with healthy, positive ones
- Explore relationships and experiences, and develop positive interactions with others
- Find better ways to cope and solve problems
- Identify issues that contribute to your depression and change behaviors that make it worse
- Regain a sense of satisfaction and control in your life and help ease depression symptoms, such as hopelessness and anger
- Learn to set realistic goals for your life
- Develop the ability to tolerate and accept distress using healthier behaviors
Alternate formats for therapy
Formats for depression therapy as an alternative to face-to-face office sessions are available and may be an effective option for some people. Therapy can be provided, for example, as a computer program, by online sessions, or using videos or workbooks.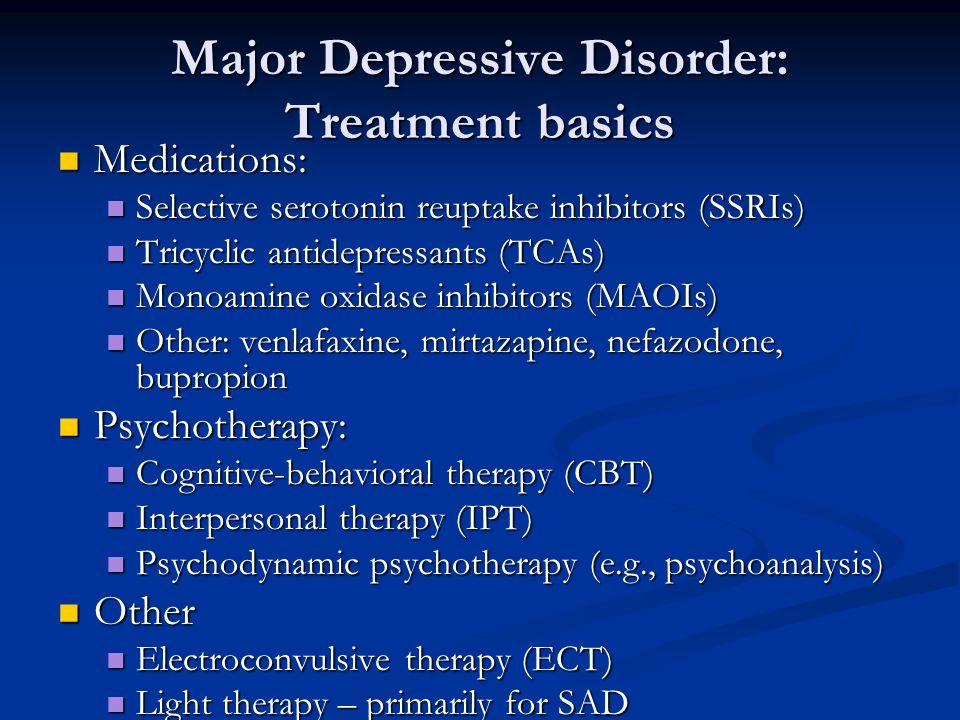 Programs can be guided by a therapist or be partially or totally independent.
Programs can be guided by a therapist or be partially or totally independent.
Before you choose one of these options, discuss these formats with your therapist to determine if they may be helpful for you. Also, ask your therapist if he or she can recommend a trusted source or program. Some may not be covered by your insurance and not all developers and online therapists have the proper credentials or training.
Smartphones and tablets that offer mobile health apps, such as support and general education about depression, are not a substitute for seeing your doctor or therapist.
Hospital and residential treatment
In some people, depression is so severe that a hospital stay is needed. This may be necessary if you can't care for yourself properly or when you're in immediate danger of harming yourself or someone else. Psychiatric treatment at a hospital can help keep you calm and safe until your mood improves.
Partial hospitalization or day treatment programs also may help some people. These programs provide the outpatient support and counseling needed to get symptoms under control.
These programs provide the outpatient support and counseling needed to get symptoms under control.
Other treatment options
For some people, other procedures, sometimes called brain stimulation therapies, may be suggested:
- Electroconvulsive therapy (ECT). In ECT, electrical currents are passed through the brain to impact the function and effect of neurotransmitters in your brain to relieve depression. ECT is usually used for people who don't get better with medications, can't take antidepressants for health reasons or are at high risk of suicide.
- Transcranial magnetic stimulation (TMS). TMS may be an option for those who haven't responded to antidepressants. During TMS, a treatment coil placed against your scalp sends brief magnetic pulses to stimulate nerve cells in your brain that are involved in mood regulation and depression.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Antidepressants: Selecting one that's right for you
- Antidepressants: Side effects
- Atypical antidepressants
- Monoamine oxidase inhibitors (MAOIs)
- Selective serotonin reuptake inhibitors (SSRIs)
- Serotonin and norepinephrine reuptake inhibitors (SNRIs)
- Treatment-resistant depression
- Tricyclic antidepressants and tetracyclic antidepressants
- Antidepressant withdrawal: Is there such a thing?
- Antidepressants and alcohol: What's the concern?
- Antidepressants and weight gain: What causes it?
- Antidepressants: Can they stop working?
- MAOIs and diet: Is it necessary to restrict tyramine?
- Electroconvulsive therapy (ECT)
- Psychotherapy
- Transcranial magnetic stimulation
- Vagus nerve stimulation
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.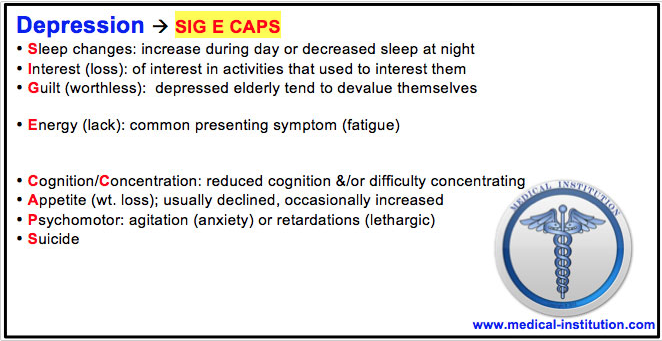
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.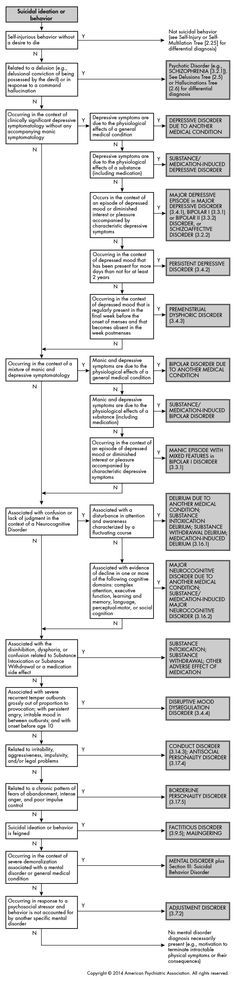
Lifestyle and home remedies
Depression generally isn't a disorder that you can treat on your own. But in addition to professional treatment, these self-care steps can help:
- Stick to your treatment plan. Don't skip psychotherapy sessions or appointments. Even if you're feeling well, don't skip your medications. If you stop, depression symptoms may come back, and you could also experience withdrawal-like symptoms. Recognize that it will take time to feel better.
- Learn about depression. Education about your condition can empower you and motivate you to stick to your treatment plan. Encourage your family to learn about depression to help them understand and support you.
- Pay attention to warning signs. Work with your doctor or therapist to learn what might trigger your depression symptoms. Make a plan so that you know what to do if your symptoms get worse. Contact your doctor or therapist if you notice any changes in symptoms or how you feel.
 Ask relatives or friends to help watch for warning signs.
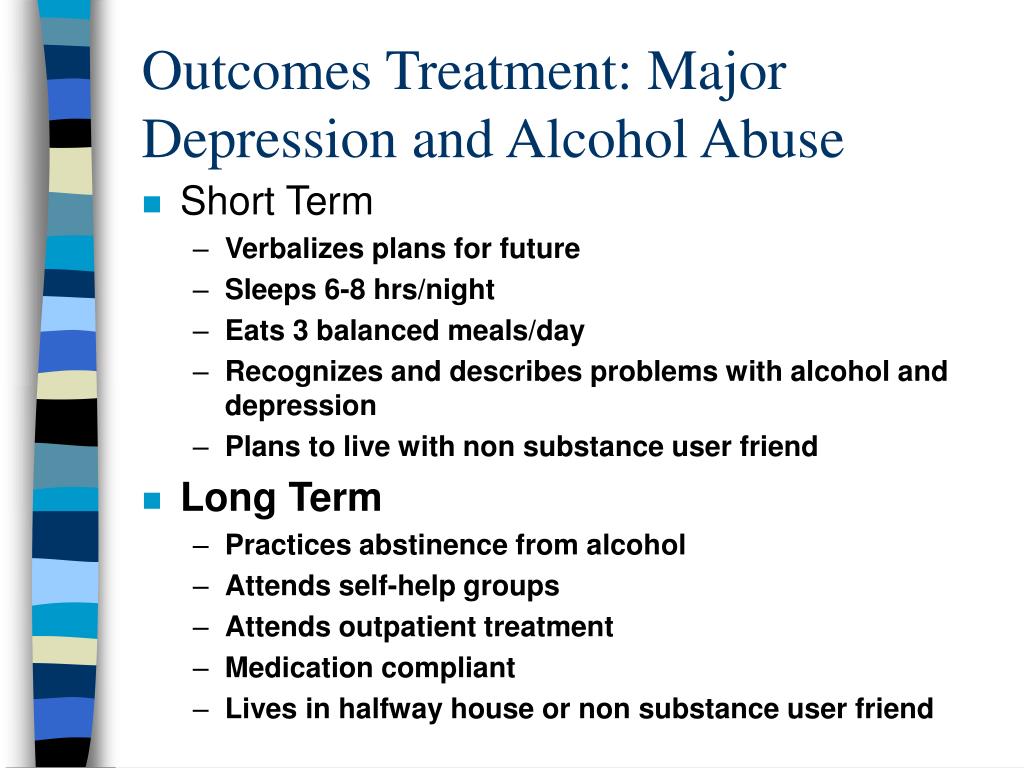
Ask relatives or friends to help watch for warning signs. - Avoid alcohol and recreational drugs. It may seem like alcohol or drugs lessen depression symptoms, but in the long run they generally worsen symptoms and make depression harder to treat. Talk with your doctor or therapist if you need help with alcohol or substance use.
- Take care of yourself. Eat healthy, be physically active and get plenty of sleep. Consider walking, jogging, swimming, gardening or another activity that you enjoy. Sleeping well is important for both your physical and mental well-being. If you're having trouble sleeping, talk to your doctor about what you can do.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Depression, anxiety and exercise
Alternative medicine
Alternative medicine is the use of a nonconventional approach instead of conventional medicine. Complementary medicine is a nonconventional approach used along with conventional medicine — sometimes called integrative medicine.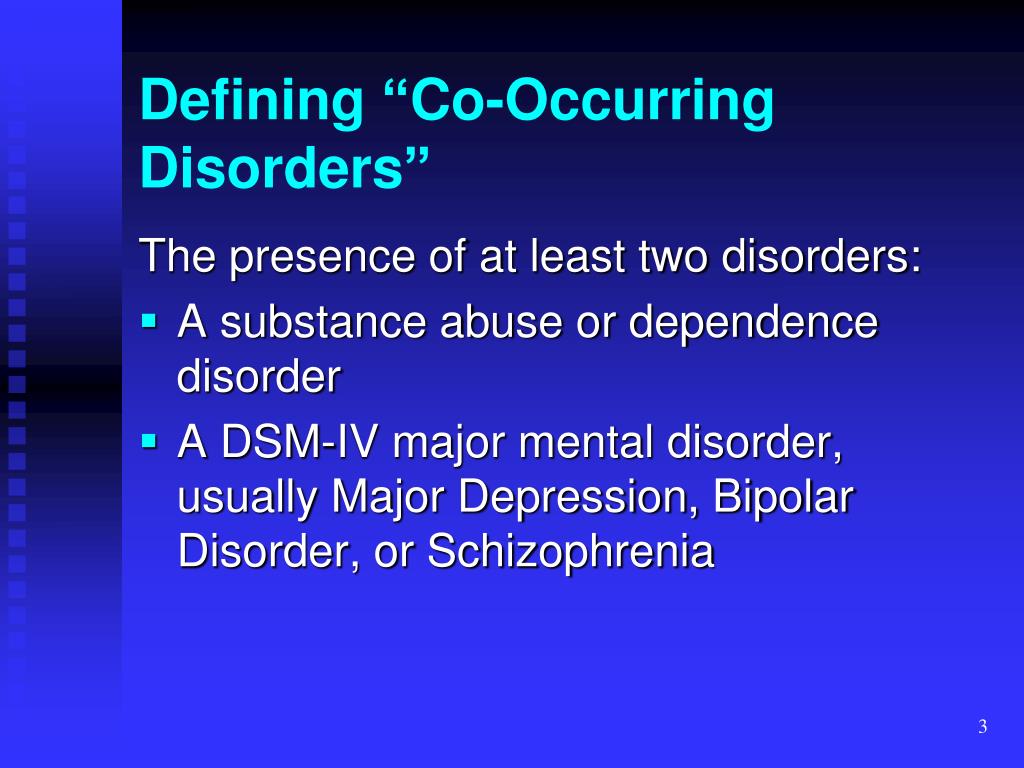
Make sure you understand the risks as well as possible benefits if you pursue alternative or complementary therapy. Don't replace conventional medical treatment or psychotherapy with alternative medicine. When it comes to depression, alternative treatments aren't a substitute for medical care.
Supplements
Examples of supplements that are sometimes used for depression include:
- St. John's wort. Although this herbal supplement isn't approved by the Food and Drug Administration (FDA) to treat depression in the U.S., it may be helpful for mild or moderate depression. But if you choose to use it, be careful — St. John's wort can interfere with a number of medications, such as heart drugs, blood-thinning drugs, birth control pills, chemotherapy, HIV/AIDS medications and drugs to prevent organ rejection after a transplant. Also, avoid taking St. John's wort while taking antidepressants because the combination can cause serious side effects.
- SAMe.
 Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder.
Pronounced "sam-E," this dietary supplement is a synthetic form of a chemical that occurs naturally in the body. The name is short for S-adenosylmethionine (es-uh-den-o-sul-muh-THIE-o-neen). SAMe isn't approved by the FDA to treat depression in the U.S. It may be helpful, but more research is needed. SAMe may trigger mania in people with bipolar disorder. - Omega-3 fatty acids. These healthy fats are found in cold-water fish, flaxseed, flax oil, walnuts and some other foods. Omega-3 supplements are being studied as a possible treatment for depression. While considered generally safe, in high doses, omega-3 supplements may interact with other medications. More research is needed to determine if eating foods with omega-3 fatty acids can help relieve depression.
Nutritional and dietary products aren't monitored by the FDA the same way medications are. You can't always be certain of what you're getting and whether it's safe. Also, because some herbal and dietary supplements can interfere with prescription medications or cause dangerous interactions, talk to your doctor or pharmacist before taking any supplements.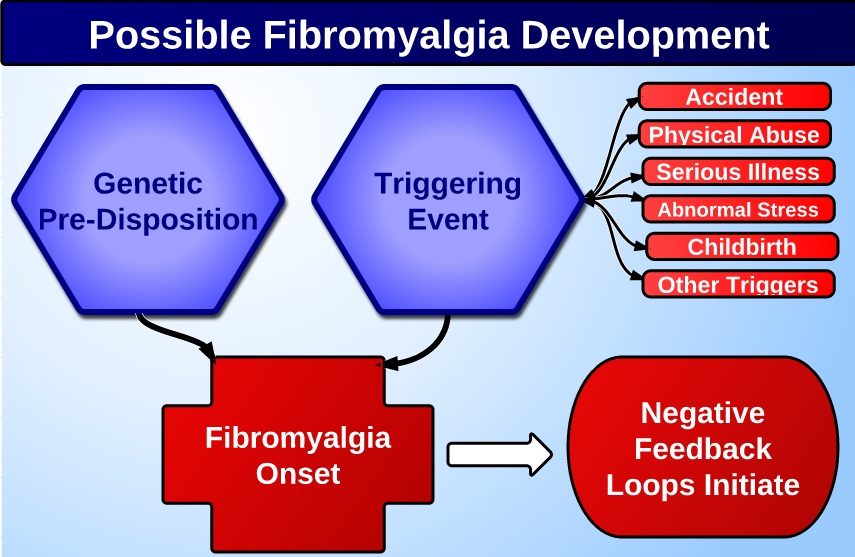
Mind-body connections
Integrative medicine practitioners believe the mind and body must be in harmony for you to stay healthy. Examples of mind-body techniques that may be helpful for depression include:
- Acupuncture
- Relaxation techniques such as yoga or tai chi
- Meditation
- Guided imagery
- Massage therapy
- Music or art therapy
- Spirituality
- Aerobic exercise
Relying solely on these therapies is generally not enough to treat depression. They may be helpful when used in addition to medication and psychotherapy.
More Information
- Depression (major depressive disorder) care at Mayo Clinic
- Natural remedies for depression: Are they effective?
Coping and support
Talk with your doctor or therapist about improving your coping skills, and try these tips:
- Simplify your life. Cut back on obligations when possible, and set reasonable goals for yourself.
 Give yourself permission to do less when you feel down.
Give yourself permission to do less when you feel down. - Write in a journal. Journaling, as part of your treatment, may improve mood by allowing you to express pain, anger, fear or other emotions.
- Read reputable self-help books and websites. Your doctor or therapist may be able to recommend books or websites to read.
- Locate helpful groups. Many organizations, such as the National Alliance on Mental Illness (NAMI) and the Depression and Bipolar Support Alliance, offer education, support groups, counseling and other resources to help with depression. Employee assistance programs and religious groups also may offer help for mental health concerns.
- Don't become isolated. Try to participate in social activities, and get together with family or friends regularly. Support groups for people with depression can help you connect to others facing similar challenges and share experiences.
- Learn ways to relax and manage your stress. Examples include meditation, progressive muscle relaxation, yoga and tai chi.
- Structure your time. Plan your day. You may find it helps to make a list of daily tasks, use sticky notes as reminders or use a planner to stay organized.
- Don't make important decisions when you're down. Avoid decision-making when you're feeling depressed, since you may not be thinking clearly.
Preparing for your appointment
You may see your primary care doctor, or your doctor may refer you to a mental health professional. Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, make a list of:
- Any symptoms you've had, including any that may seem unrelated to the reason for your appointment
- Key personal information, including any major stresses or recent life changes
- All medications, vitamins or other supplements that you're taking, including dosages
- Questions to ask your doctor or mental health professional
Take a family member or friend along, if possible, to help you remember all of the information provided during the appointment.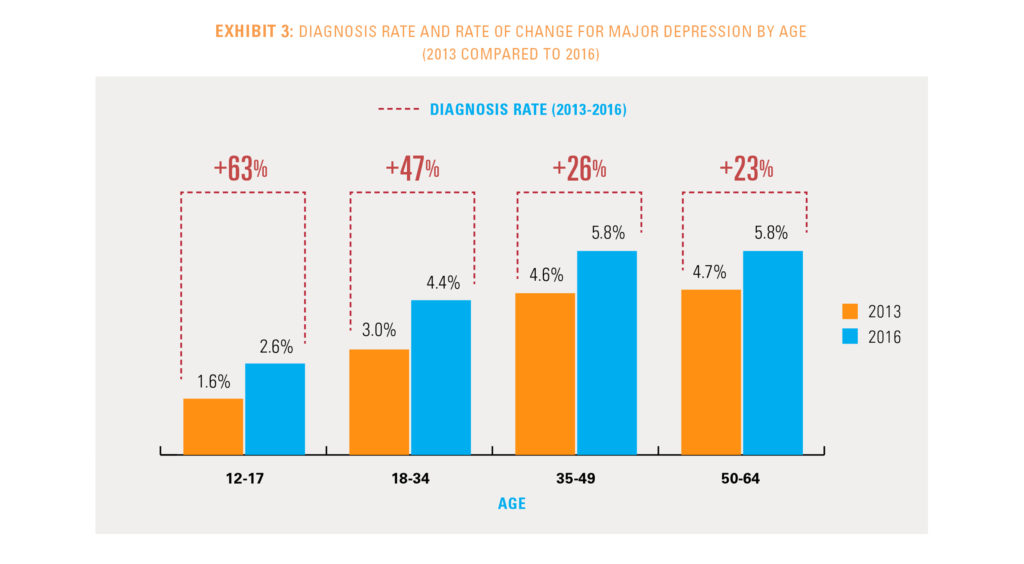
Some basic questions to ask your doctor include:
- Is depression the most likely cause of my symptoms?
- What are other possible causes for my symptoms?
- What kinds of tests will I need?
- What treatment is likely to work best for me?
- What are the alternatives to the primary approach that you're suggesting?
- I have these other health conditions. How can I best manage them together?
- Are there any restrictions that I need to follow?
- Should I see a psychiatrist or other mental health professional?
- What are the main side effects of the medications you're recommending?
- Is there a generic alternative to the medicine you're prescribing?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your doctor will likely ask you a number of questions.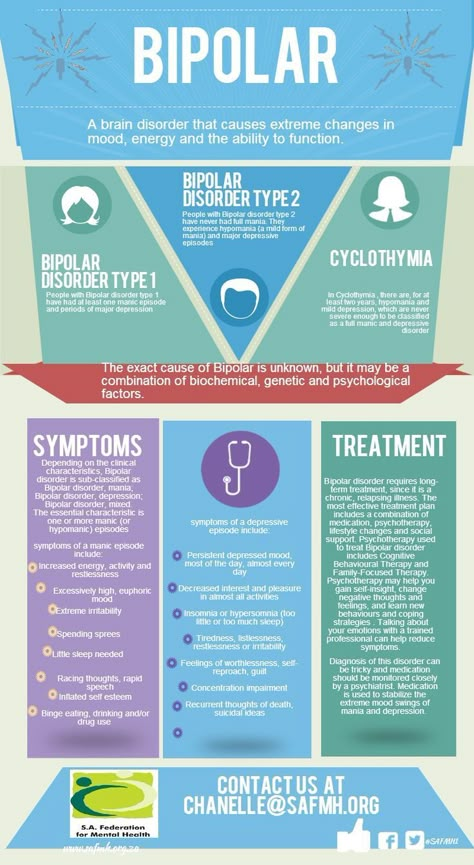 Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
Be ready to answer them to reserve time to go over any points you want to focus on. Your doctor may ask:
- When did you or your loved ones first notice your symptoms of depression?
- How long have you felt depressed? Do you generally always feel down, or does your mood fluctuate?
- Does your mood ever swing from feeling down to feeling intensely happy (euphoric) and full of energy?
- Do you ever have suicidal thoughts when you're feeling down?
- Do your symptoms interfere with your daily life or relationships?
- Do you have any blood relatives with depression or another mood disorder?
- What other mental or physical health conditions do you have?
- Do you drink alcohol or use recreational drugs?
- How much do you sleep at night? Does it change over time?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to worsen your symptoms?
By Mayo Clinic Staff
Major Depressive Disorder - StatPearls
Continuing Education Activity
Major depressive disorder (MDD) has been ranked as the third cause of the burden of disease worldwide in 2008 by WHO, which has projected that this disease will rank first by 2030. It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. This activity reviews the evaluation and management of major depressive disorder which is one of the main causes of disability in the world and highlights the role of the interprofessional team.
It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. This activity reviews the evaluation and management of major depressive disorder which is one of the main causes of disability in the world and highlights the role of the interprofessional team.
Objectives:
Identify the etiology of major depressive disorder.
Review the appropriate management of major depressive disorder.
Outline the typical presentation of a patient with major depressive disorder.
Review the importance of improving care coordination among interprofessional team members to improve outcomes for patients affected by major depressive disorder.
Access free multiple choice questions on this topic.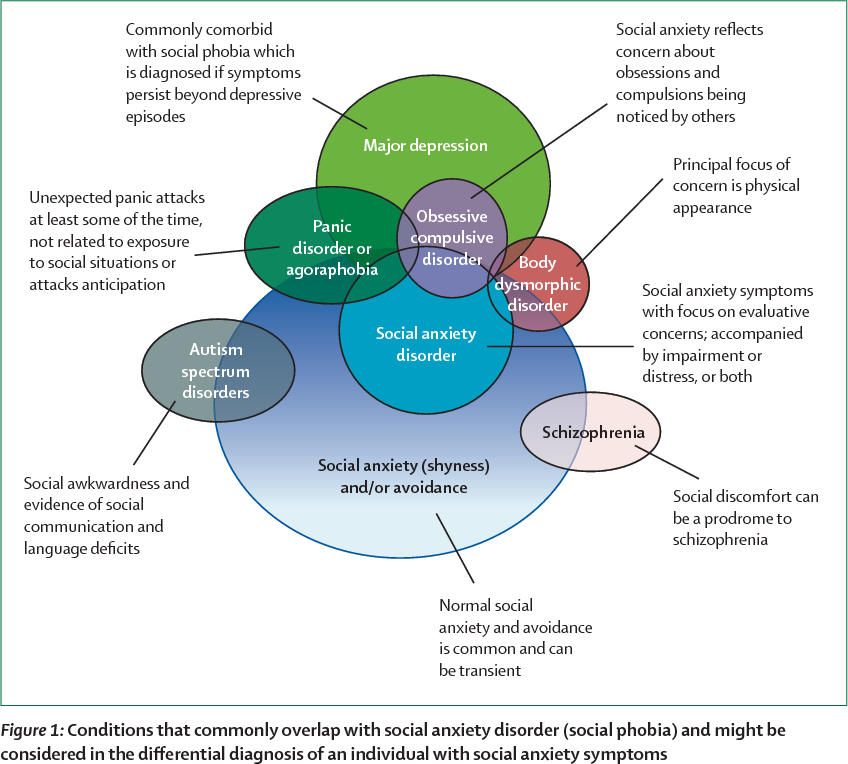
Introduction
Major depressive disorder (MDD) has been ranked as the third cause of the burden of disease worldwide in 2008 by WHO, which has projected that this disease will rank first by 2030.[1] It is diagnosed when an individual has a persistently low or depressed mood, anhedonia or decreased interest in pleasurable activities, feelings of guilt or worthlessness, lack of energy, poor concentration, appetite changes, psychomotor retardation or agitation, sleep disturbances, or suicidal thoughts. Per the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5), an individual must have five of the above-mentioned symptoms, of which one must be a depressed mood or anhedonia causing social or occupational impairment, to be diagnosed with MDD. History of a manic or hypomanic episode must be ruled out to make a diagnosis of MDD. Children and adolescents with MDD may present with irritable mood.
Per DSM-5, other types of depression falling under the category of depressive disorders are:
Persistent depressive disorder, formerly known as dysthymia
Disruptive mood dysregulation disorder
Premenstrual dysphoric disorder
Substance/medication-induced depressive disorder
Depressive disorder due to another medical condition
Unspecified depressive disorder
Etiology
The etiology of Major depressive disorder is believed to be multifactorial, including biological, genetic, environmental, and psychosocial factors.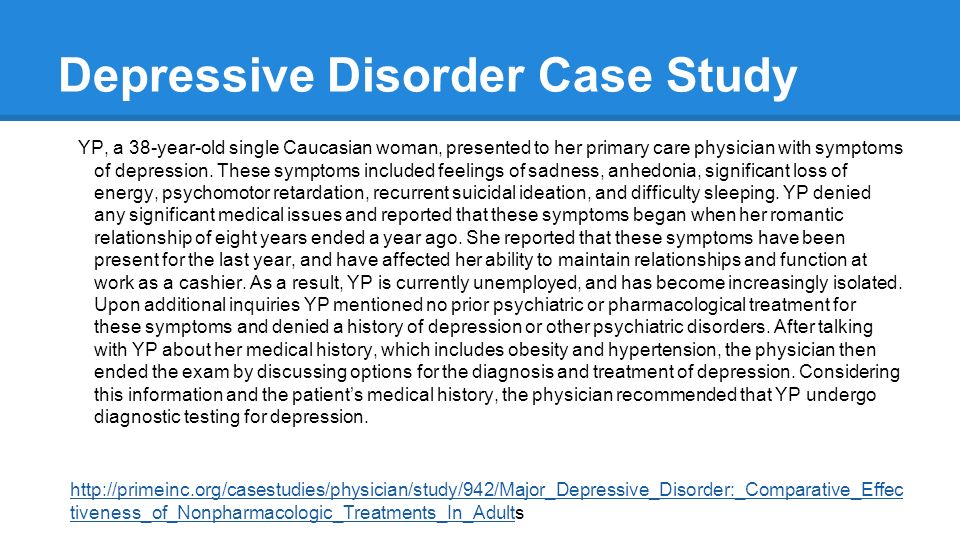 MDD was earlier considered to be mainly due to abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine. This has been evidenced by the use of different antidepressants such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, dopamine-norepinephrine receptor inhibitors in the treatment of depression. People with suicidal ideations have been found to have low levels of serotonin metabolites. However, recent theories indicate that it is associated primarily with more complex neuroregulatory systems and neural circuits, causing secondary disturbances of neurotransmitter systems.
MDD was earlier considered to be mainly due to abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine. This has been evidenced by the use of different antidepressants such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, dopamine-norepinephrine receptor inhibitors in the treatment of depression. People with suicidal ideations have been found to have low levels of serotonin metabolites. However, recent theories indicate that it is associated primarily with more complex neuroregulatory systems and neural circuits, causing secondary disturbances of neurotransmitter systems.
GABA, an inhibitory neurotransmitter, and glutamate and glycine, both of which are major excitatory neurotransmitters are found to play a role in the etiology of depression as well. Depressed patients have been found to have lower plasma, CSF, and brain GABA levels. GABA is considered to exert its antidepressant effect by inhibiting the ascending monoamine pathways, including mesocortical and mesolimbic systems.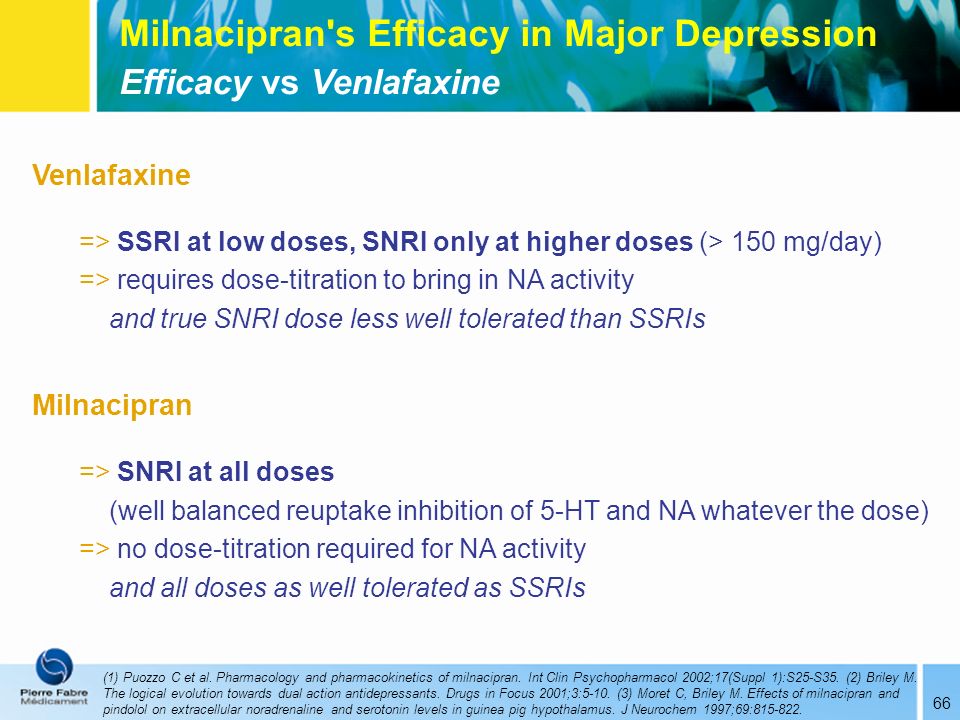 Drugs that antagonize NMDA receptors have been researched to have antidepressant properties. Thyroid and growth hormonal abnormalities have also been implicated in the etiology of mood disorders. Multiple adverse childhood experiences and trauma are associated with the development of depression later in life.[2][3]
Drugs that antagonize NMDA receptors have been researched to have antidepressant properties. Thyroid and growth hormonal abnormalities have also been implicated in the etiology of mood disorders. Multiple adverse childhood experiences and trauma are associated with the development of depression later in life.[2][3]
Severe early stress can result in drastic alterations in neuroendocrine and behavioral responses, which can cause structural changes in the cerebral cortex, leading to severe depression later in life. Structural and functional brain imaging of depressed individuals has shown increased hyperintensities in the subcortical regions, and reduced anterior brain metabolism on the left side, respectively. Family, adoption, and twin studies have indicated the role of genes in the susceptibility of depression. Genetic studies show a very high concordance rate for twins to have MDD, particularly monozygotic twins.[4] Life events and personality traits have shown to play an important role, as well. The learned helplessness theory has associated the occurrence of depression with the experience of uncontrollable events. Per cognitive theory, depression occurs as a result of cognitive distortions in persons who are susceptible to depression.
The learned helplessness theory has associated the occurrence of depression with the experience of uncontrollable events. Per cognitive theory, depression occurs as a result of cognitive distortions in persons who are susceptible to depression.
Epidemiology
Major depressive disorder is a highly prevalent psychiatric disorder. It has a lifetime prevalence of about 5 to 17 percent, with the average being 12 percent. The prevalence rate is almost double in women than in men.[5] This difference has been considered to be due to the hormonal differences, childbirth effects, different psychosocial stressors in men and women, and behavioral model of learned helplessness. Though the mean age of onset is about 40 years, recent surveys show trends of increasing incidence in younger population due to the use of alcohol and other drugs of abuse.
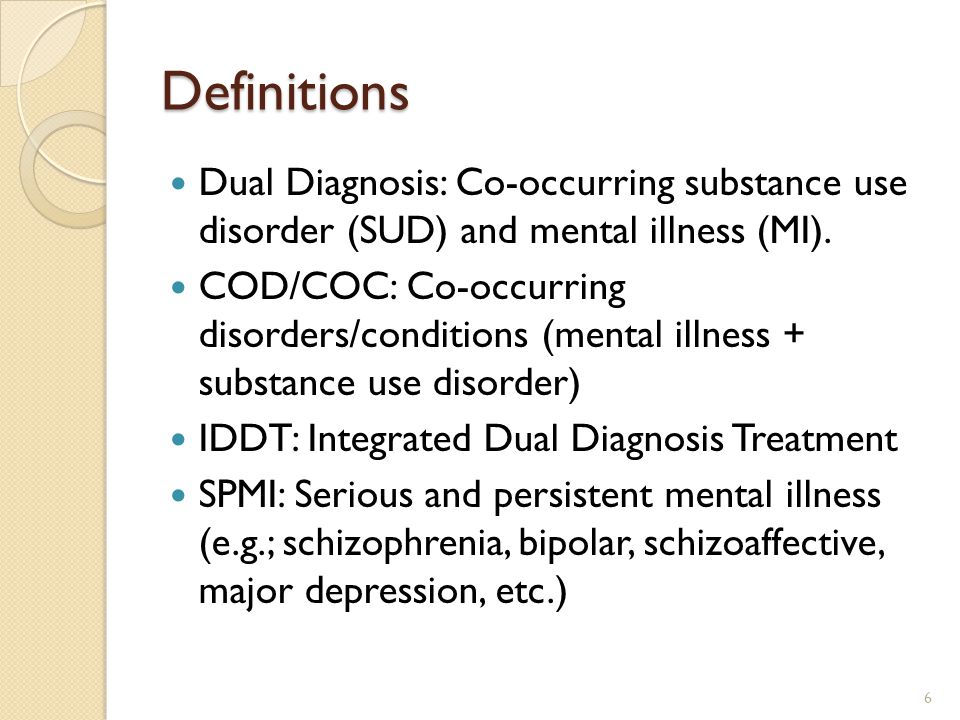
MDD is more common in people without close interpersonal relationships, and who are divorced or separated, or widowed. No difference in the prevalence of MDD has been found among races and socioeconomic status.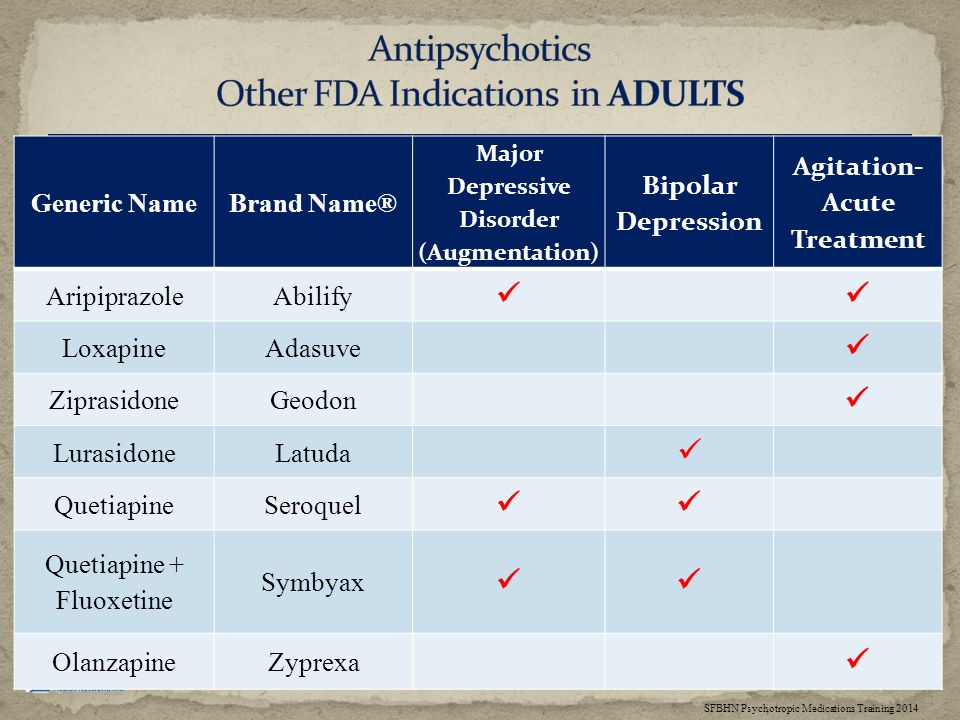 Individuals with MDD often have comorbid disorders such as substance use disorders, panic disorder, social anxiety disorder, and obsessive-compulsive disorder. The presence of these comorbid disorders in those diagnosed with MDD increases their risk of suicide. In older adults, depression is prevalent among those with comorbid medical illnesses.[6] Depression is found to be more prevalent in rural areas than in urban areas.
Individuals with MDD often have comorbid disorders such as substance use disorders, panic disorder, social anxiety disorder, and obsessive-compulsive disorder. The presence of these comorbid disorders in those diagnosed with MDD increases their risk of suicide. In older adults, depression is prevalent among those with comorbid medical illnesses.[6] Depression is found to be more prevalent in rural areas than in urban areas.
History and Physical
Major depressive disorder is a clinical diagnosis; it is mainly diagnosed by the clinical history given by the patient and mental status examination. The clinical interview must include medical history, family history, social history, and substance use history along with the symptomatology. Collateral information from a patient's family/friends is a very important part of psychiatric evaluation.
A complete physical examination, including neurological examination, should be performed. It is important to rule out any underlying medical/organic causes of a depressive disorder.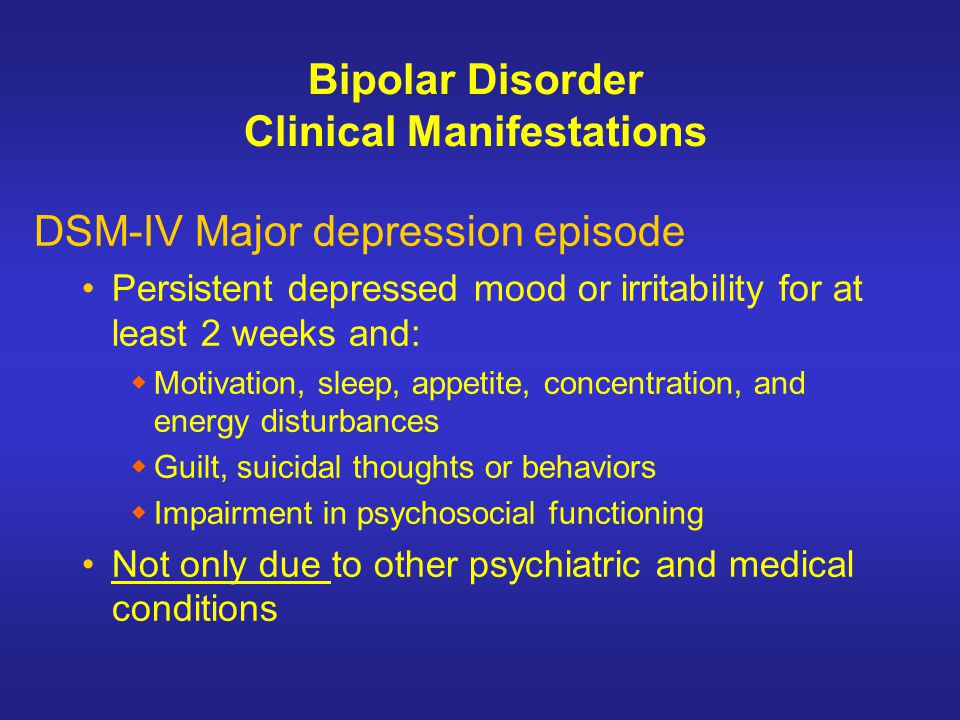 A full medical history, along with the family medical and psychiatric history, should be assessed. Mental status examination plays an important role in the diagnosis and evaluation of MDD.
A full medical history, along with the family medical and psychiatric history, should be assessed. Mental status examination plays an important role in the diagnosis and evaluation of MDD.
Evaluation
Although there is no objective testing available to diagnose depression, routine laboratory work including complete blood account with differential, comprehensive metabolic panel, thyroid-stimulating hormone, free T4, vitamin D, urinalysis, and toxicology screening is done to rule out organic or medical causes of depression.
Individuals with depression often present to their primary care physicians for somatic complaints stemming from depression, rather than seeing a mental health professional. In almost half of the cases, patients deny having depressive feelings, and they are often brought for treatment by the family or sent by the employer to be evaluated for social withdrawal and decreased activity. It is very important to evaluate a patient for suicidal or homicidal ideations at each visit.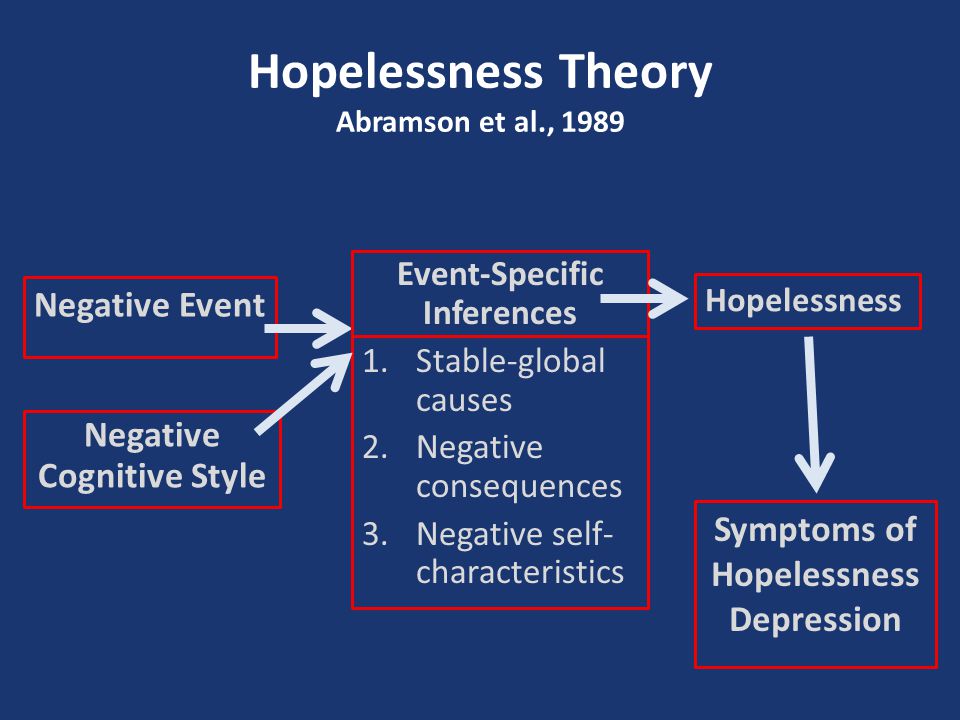
In primary care settings, the Patient Health Questionnaire-9 (PHQ-9), which is a self-report, standardized depression rating scale is commonly used for screening, diagnosing, and monitoring treatment response for MDD.[7] The PHQ-9 uses 9 items corresponding to the DSM-5 criteria for MDD and also assesses for psychosocial impairment. The PHQ-9 scores 0 to 27, with scores of equal to or more than 10, indicate a possible MDD.
In most hospital settings, the Hamilton Rating Scale for Depression (HAM-D), which is a clinician-administered depression rating scale is commonly used for the assessment of depression. The original HAM-D uses 21 items about symptoms of depression, but the scoring is based only on the first 17 items.
Other scales include the Montgomery-Asberg Depression Rating Scale (MADRS), the Beck Depression Inventory (BDI), the Zung Self-Rating Depression Scale, the Raskin Depression Rating Scale, and other questionnaires.
Treatment / Management
Major depressive disorder can be managed with various treatment modalities, including pharmacological, psychotherapeutic, interventional, and lifestyle modification.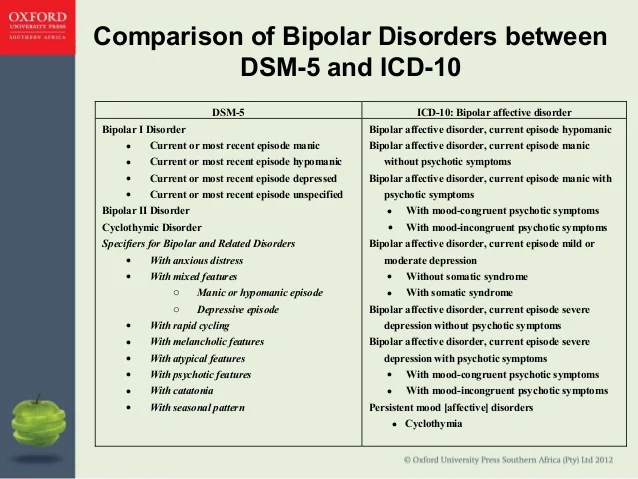 The initial treatment of MDD includes medications or/and psychotherapy. Combination treatment, including both medications and psychotherapy, has been found to be more effective than either of these treatments alone.[8][9] Electroconvulsive therapy is found to be more efficacious than any other form of treatment for severe major depression.[10]
The initial treatment of MDD includes medications or/and psychotherapy. Combination treatment, including both medications and psychotherapy, has been found to be more effective than either of these treatments alone.[8][9] Electroconvulsive therapy is found to be more efficacious than any other form of treatment for severe major depression.[10]
FDA-approved medications for the treatment of MDD are as follows: All antidepressants are equally effective but differ in side-effect profiles.
Selective serotonin reuptake inhibitors (SSRIs) include fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine. They are usually the first line of treatment and the most widely prescribed antidepressants.
Serotonin-norepinephrine reuptake inhibitors (SNRIs) include venlafaxine, duloxetine, desvenlafaxine, levomilnacipran, and milnacipran. They are often used for depressed patients with comorbid pain disorders.
Serotonin modulators are trazodone, vilazodone, and vortioxetine.
Atypical antidepressants include bupropion and mirtazapine. They are often prescribed as monotherapy or as augmenting agents when patients develop sexual side-effects due to SSRIs or SNRIs.
Tricyclic antidepressants (TCAs) are amitriptyline, imipramine, clomipramine, doxepin, nortriptyline, and desipramine.
Monoamine oxidase inhibitors (MAOIs) available are tranylcypromine, phenelzine, selegiline, and isocarboxazid. MAOIs and TCAs are not commonly used due to the high incidence of side-effects and lethality in overdose.
Other medications include mood-stabilizers, antipsychotics which may be added to enhance antidepressant effects.
Psychotherapy
Cognitive-behavioral therapy
Interpersonal therapy
Electroconvulsive Therapy (ECT)
Acute suicidality
Severe depression during pregnancy
Refusal to eat/drink
Catatonia
Severe psychosis
Transcranial Magnetic Stimulation (TMS)
FDA-approved for treatment-resistant/refractory depression; for patients who have failed at least one medication trial
Vagus Nerve Stimulation (VNS)
FDA-approved as a long-term adjunctive treatment for treatment-resistant depression; for patients who have failed at least 4 medication trials
Esketamine
Nasal spray to be used in conjunction with an oral antidepressant in treatment-resistant depression; for patients who have failed other antidepressant medications
Differential Diagnosis
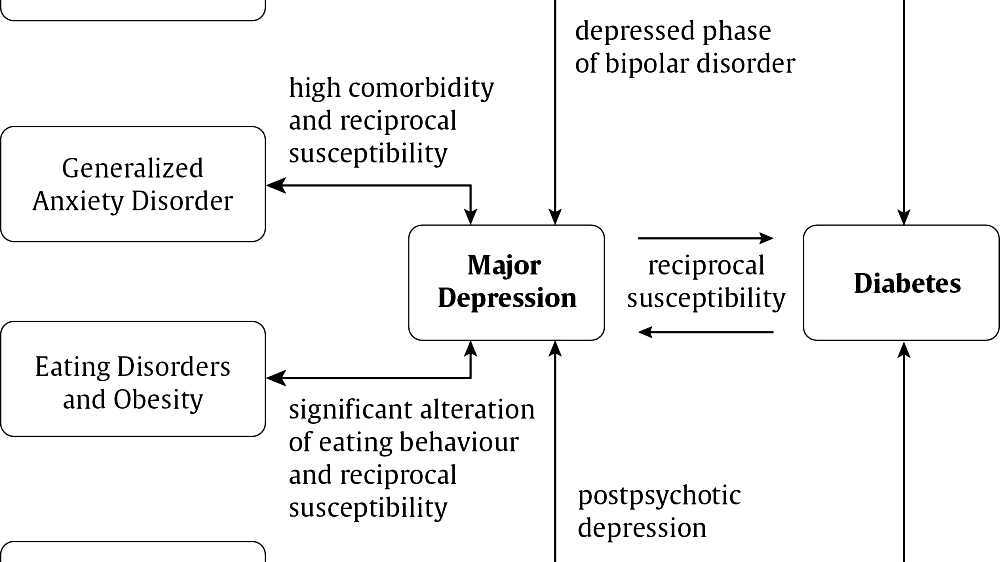
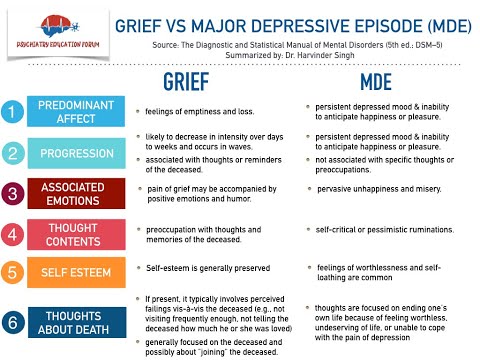
While evaluating for MDD, it is important to rule out depressive disorder due to another medical condition, substance/medication-induced depressive disorder, dysthymia, cyclothymia, bereavement, adjustment disorder with depressed mood, bipolar disorder, schizoaffective disorder, schizophrenia, anxiety disorders, and eating disorders for the appropriate management.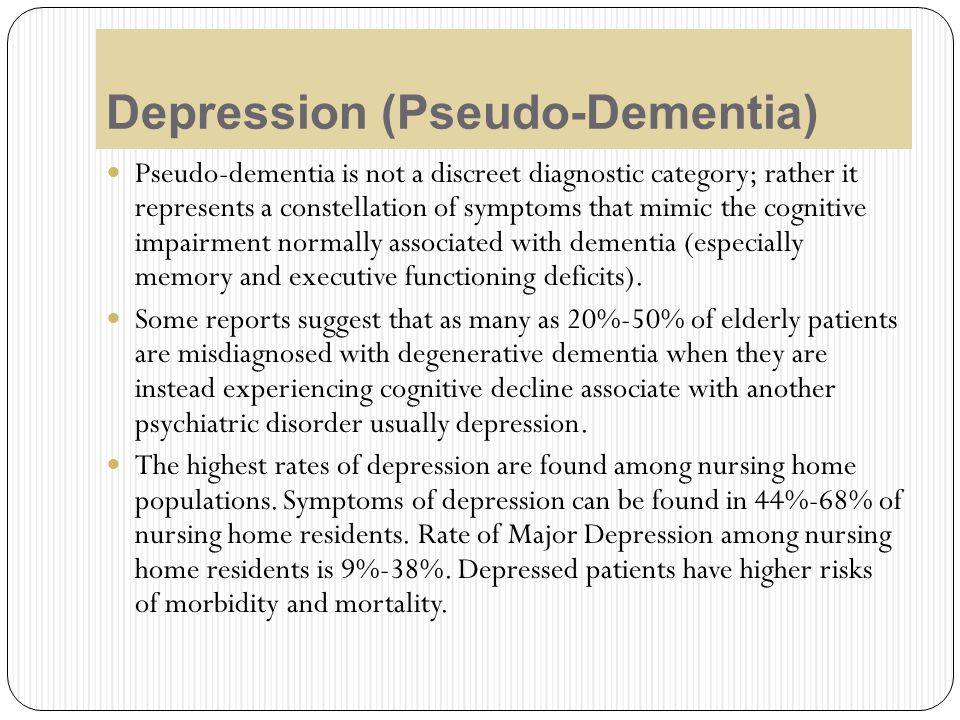 Depressive symptoms can be secondary to the following causes:
Depressive symptoms can be secondary to the following causes:
Neurological causes such as cerebrovascular accident, multiple sclerosis, subdural hematoma, epilepsy, Parkinson disease, Alzheimer disease
Endocrinopathies such as diabetes, thyroid disorders, adrenal disorders
Metabolic disturbances such as hypercalcemia, hyponatremia
Medications/substances of abuse: steroids, antihypertensives, anticonvulsants, antibiotics, sedatives, hypnotics, alcohol, stimulant withdrawal
Nutritional deficiencies such as vitamin D, B12, B6 deficiency, iron or folate deficiency
Infectious diseases such as HIV and syphilis
Malignancies
Prognosis
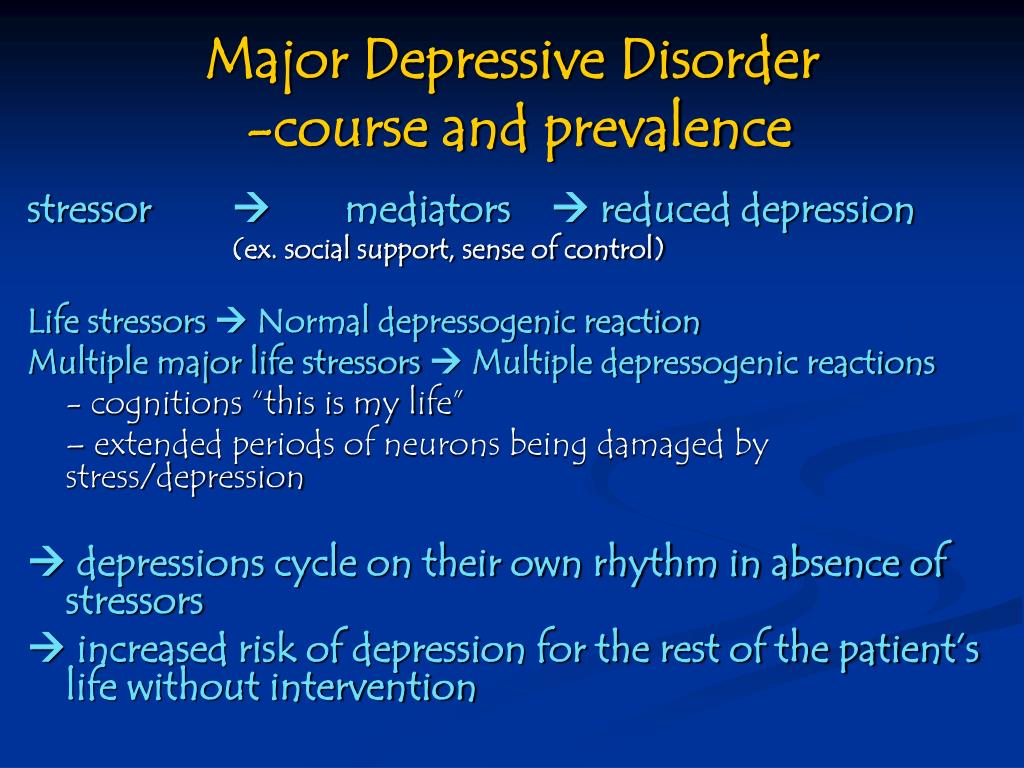
Untreated depressive episodes in major depressive disorder can last from 6 to 12 months. About two-thirds of the individuals with MDD contemplate suicide, and about 10 to 15 percent commit suicide. MDD is a chronic, recurrent illness; the recurrence rate is about 50% after the first episode, 70% after the second episode, and 90% after the third episode. About 5 to 10 percent of the patients with MDD eventually develop bipolar disorder.[11] The prognosis of MDD is good in patients with mild episodes, the absence of psychotic symptoms, better treatment compliance, a strong support system, and good premorbid functioning. The prognosis is poor in the presence of a comorbid psychiatric disorder, personality disorder, multiple hospitalizations, and advanced age of onset.
About 5 to 10 percent of the patients with MDD eventually develop bipolar disorder.[11] The prognosis of MDD is good in patients with mild episodes, the absence of psychotic symptoms, better treatment compliance, a strong support system, and good premorbid functioning. The prognosis is poor in the presence of a comorbid psychiatric disorder, personality disorder, multiple hospitalizations, and advanced age of onset.
Complications
MDD is one of the leading causes of disability worldwide. It not only causes a severe functional impairment but also adversely affects the interpersonal relationships, thus lowering the quality of life. Individuals with MDD are at a high risk of developing comorbid anxiety disorders and substance use disorders, which further increases their risk of suicide. Depression can aggravate medical comorbidities such as diabetes, hypertension, chronic obstructive pulmonary disease, and coronary artery disease. Depressed individuals are at high risk of developing self-destructive behavior as a coping mechanism.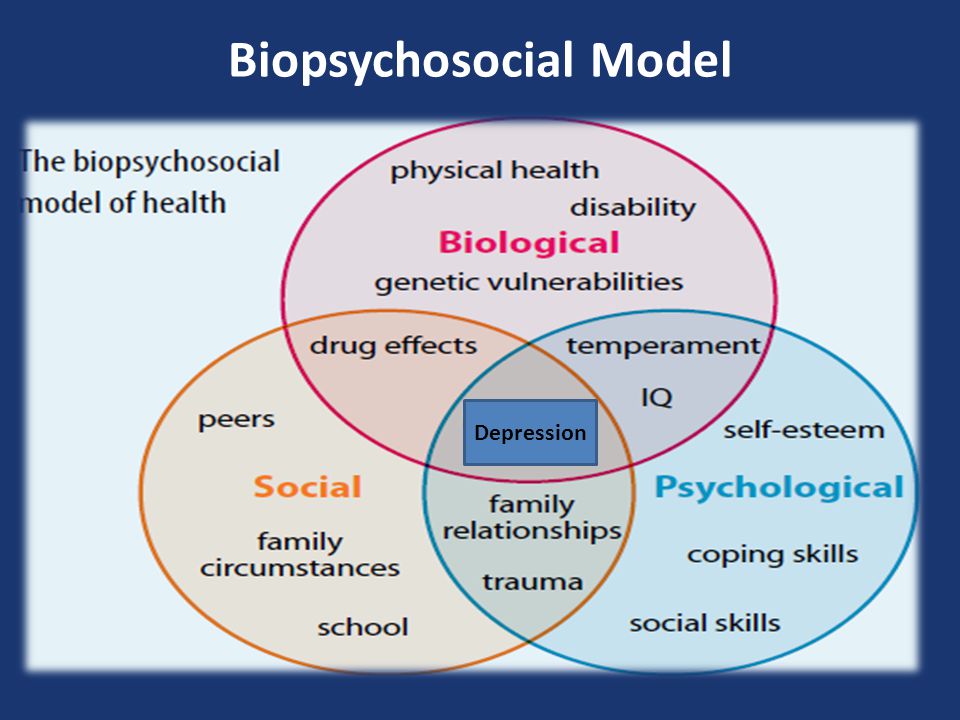 MDD is often very debilitating if left untreated.
MDD is often very debilitating if left untreated.
Deterrence and Patient Education
Patient education has a profound impact on the overall outcome of major depressive disorder. Since MDD is one of the most common psychiatric disorders causing disability worldwide and people in different parts of the world are hesitant to discuss and seek treatment for depression due to the stigma associated with mental illness, educating patients is very crucial for their better understanding of the mental illness and better compliance with the mental health treatment. Family education also plays an important role in the successful treatment of MDD.
Enhancing Healthcare Team Outcomes
An interdisciplinary approach is essential for the effective and successful treatment of MDD. Primary care physicians and psychiatrists, along with nurses, therapists, social workers, and case managers, form an integral part of these collaborated services. In the majority of cases, PCPs are the first providers to whom individuals with MDD present mostly with somatic complaints.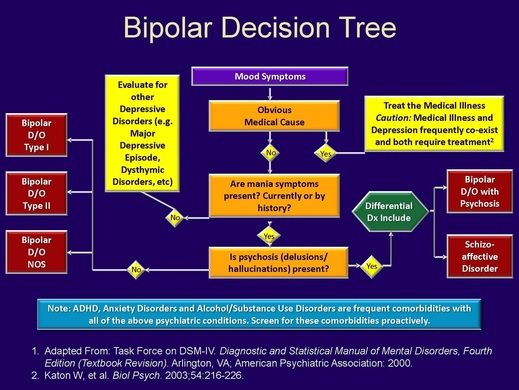 Depression screening in primary care settings is very imperative. The regular screening of the patients using depression rating scales such as PHQ-9 can be very helpful in the early diagnosis and intervention, thus improving the overall outcome of MDD. Psychoeducation plays a significant role in improving patient compliance and medication adherence. Recent evidence also supports that lifestyle modification, including moderate exercises, can help to improve mild-to-moderate depression. Suicide screening at each psychiatric visit can be helpful to lower suicide incidence. Since patients with MDD are at increased risk of suicide, close monitoring, and follow up by mental health workers becomes necessary to ensure safety and compliance with mental health treatment. The involvement of families can further add to a better outcome of the overall mental health treatment. Meta-analyses of randomized trials have shown that depression outcomes are superior when using collaborative care as compared with usual care.
Depression screening in primary care settings is very imperative. The regular screening of the patients using depression rating scales such as PHQ-9 can be very helpful in the early diagnosis and intervention, thus improving the overall outcome of MDD. Psychoeducation plays a significant role in improving patient compliance and medication adherence. Recent evidence also supports that lifestyle modification, including moderate exercises, can help to improve mild-to-moderate depression. Suicide screening at each psychiatric visit can be helpful to lower suicide incidence. Since patients with MDD are at increased risk of suicide, close monitoring, and follow up by mental health workers becomes necessary to ensure safety and compliance with mental health treatment. The involvement of families can further add to a better outcome of the overall mental health treatment. Meta-analyses of randomized trials have shown that depression outcomes are superior when using collaborative care as compared with usual care. [12]
[12]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Malhi GS, Mann JJ. Depression. Lancet. 2018 Nov 24;392(10161):2299-2312. [PubMed: 30396512]
- 2.
Bradley RG, Binder EB, Epstein MP, Tang Y, Nair HP, Liu W, Gillespie CF, Berg T, Evces M, Newport DJ, Stowe ZN, Heim CM, Nemeroff CB, Schwartz A, Cubells JF, Ressler KJ. Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry. 2008 Feb;65(2):190-200. [PMC free article: PMC2443704] [PubMed: 18250257]
- 3.
Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010 Feb;67(2):113-23. [PMC free article: PMC2822662] [PubMed: 20124111]
- 4.
Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000 Oct;157(10):1552-62. [PubMed: 11007705]
- 5.
Pedersen CB, Mors O, Bertelsen A, Waltoft BL, Agerbo E, McGrath JJ, Mortensen PB, Eaton WW. A comprehensive nationwide study of the incidence rate and lifetime risk for treated mental disorders. JAMA Psychiatry. 2014 May;71(5):573-81. [PubMed: 24806211]
- 6.
Lyness JM, Niculescu A, Tu X, Reynolds CF, Caine ED. The relationship of medical comorbidity and depression in older, primary care patients. Psychosomatics. 2006 Sep-Oct;47(5):435-9. [PubMed: 16959933]
- 7.
Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003 Nov;41(11):1284-92. [PubMed: 14583691]
- 8.
Cuijpers P, Dekker J, Hollon SD, Andersson G. Adding psychotherapy to pharmacotherapy in the treatment of depressive disorders in adults: a meta-analysis.
 J Clin Psychiatry. 2009 Sep;70(9):1219-29. [PubMed: 19818243]
J Clin Psychiatry. 2009 Sep;70(9):1219-29. [PubMed: 19818243]- 9.
Cuijpers P, van Straten A, Warmerdam L, Andersson G. Psychotherapy versus the combination of psychotherapy and pharmacotherapy in the treatment of depression: a meta-analysis. Depress Anxiety. 2009;26(3):279-88. [PubMed: 19031487]
- 10.
Pagnin D, de Queiroz V, Pini S, Cassano GB. Efficacy of ECT in depression: a meta-analytic review. J ECT. 2004 Mar;20(1):13-20. [PubMed: 15087991]
- 11.
Ratheesh A, Davey C, Hetrick S, Alvarez-Jimenez M, Voutier C, Bechdolf A, McGorry PD, Scott J, Berk M, Cotton SM. A systematic review and meta-analysis of prospective transition from major depression to bipolar disorder. Acta Psychiatr Scand. 2017 Apr;135(4):273-284. [PubMed: 28097648]
- 12.
Sighinolfi C, Nespeca C, Menchetti M, Levantesi P, Belvederi Murri M, Berardi D. Collaborative care for depression in European countries: a systematic review and meta-analysis.
 J Psychosom Res. 2014 Oct;77(4):247-63. [PubMed: 25201482]
J Psychosom Res. 2014 Oct;77(4):247-63. [PubMed: 25201482]
Major depressive disorders (clinical depression)
Depression is different from normal mood swings and short-term emotional responses to everyday problems. Prolonged moderate to severe depression can become a serious illness. This results in patients suffering greatly and doing poorly at work, at school and have problems in their families. At its worst, depression can lead to suicide.
Depression is a common illness worldwide, affecting more than 264 million people. Major depressive disorder is one of the most common forms of mental illness, affecting approximately one in six men and one in four women in their lives.
Major depressive disorder (MDD) is a severe condition characterized by low mood, decreased interests, poor cognitive function, and autonomic symptoms such as disturbed sleep or eating. MDD can develop in one in six adults during their lifetime and affects about twice as many women as men.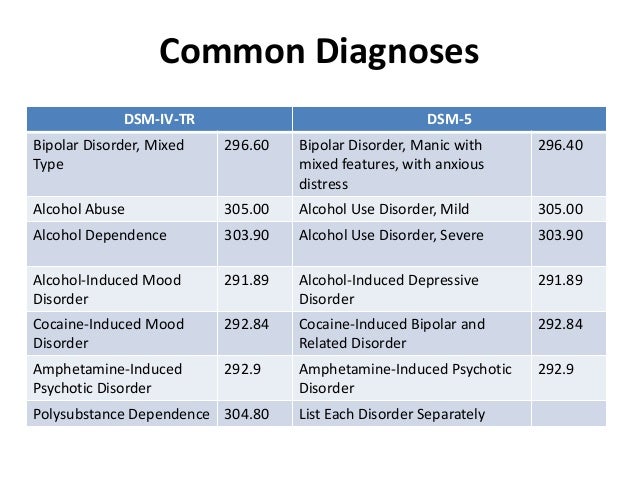
Main symptoms of depressive disorder
Symptoms of major depressive disorder (MDD) may include:
- depression almost every day
- loss of interest in activities you once enjoyed
- changes in appetite or weight
- sleep problems
- feeling lazy or restless
- low energy
- feelings of hopelessness or worthlessness
- trouble concentrating
- frequent thoughts of death or suicide
Recurrent depression:
This is a highly relapsing condition: at least 50% of people recovering from a first episode of depression have at least one additional episode in their lifetime, and about 80% of people have a history of two recurrent episodes.
Episodes typically recur within five years of the first episode, and the average person with a history of depression will have five to nine depressive episodes in their lifetime.
Symptoms of recurrent depression:
- difficulty concentrating
- disturbed sleep
- reduced energy level
- constant light alarm
Major depression in adults:
Depression is a common adult disorder that often leads to poor quality of life and impaired role functioning.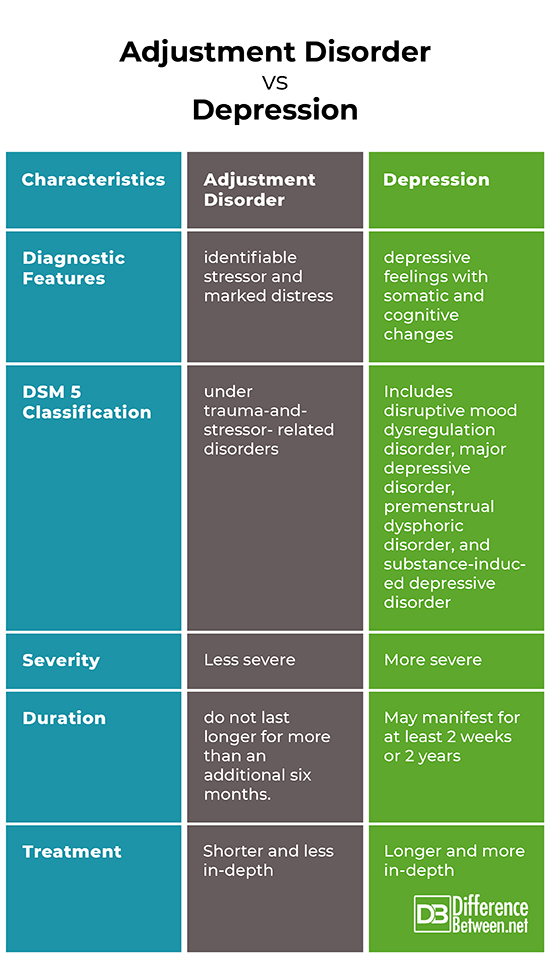 Depression is also associated with high rates of suicidal behavior and death. When depression occurs in the context of a medical illness, it is associated with increased healthcare costs, longer hospital stays, poor collaboration in treatment, etc.
Depression is also associated with high rates of suicidal behavior and death. When depression occurs in the context of a medical illness, it is associated with increased healthcare costs, longer hospital stays, poor collaboration in treatment, etc.
Causes of depression in adults may be related to the difficulty of changing roles:
- low education and low income
- early pregnancy and childbirth
- divorces
- unstable work
- highly competitive and hard work
Major symptoms of depression in adults include:
- Mostly sad or depressed mood
- Loss of interest or pleasure and avoidance of social gatherings
- Decreased energy and frequent fatigue
- Decreased concentration and attention
- Decreased self-esteem and self-confidence
- Thoughts on guilt and unworthiness
- A gloomy and pessimistic view of the future
- Thoughts or actions of harming oneself or suicidal thoughts
- Sleep disturbance or insomnia
- Pronounced or reduced appetite
DSM-5 Criteria for Major Depressive Disorder
According to the DSM-5, the following criteria must be met for a diagnosis of major depression:
At least five of the following symptoms must have been present for at least two weeks and reflect a change in previous functionality. In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
In addition, at least one of the symptoms is a low mood or loss of interest or pleasure.
- The person is depressed most of the day, almost every day, as noted by himself or others.
- He or she is not interested in all or most activities most of the day, almost every day.
- Every day a person gains or loses a large amount of weight or has a decreased or increased appetite.
- Almost every day he or she suffers from insomnia or hypersomnia.
- Every day a person experiences psychomotor disturbances that are visible to others and can also be reported.
- Almost every day he or she feels exhausted or tired.
- Almost every day a person has thoughts of worthlessness or guilt.
- Every day a person's ability to think, concentrate, or make judgments deteriorates.
- He or she has recurrent suicidal thoughts, suicidal thoughts (without a definite plan), a suicide attempt, or a definite plan to commit suicide.
- Symptoms listed above cause clinical distress or interfere with daily activities.
- The episode of depression is not associated with the physiological effect of the drug or other disease.
- The onset of the episode is not better explained by specific or unspecified schizophrenia spectrum illness or other psychotic disorders.
- The person has never had a manic or hypomanic episode.
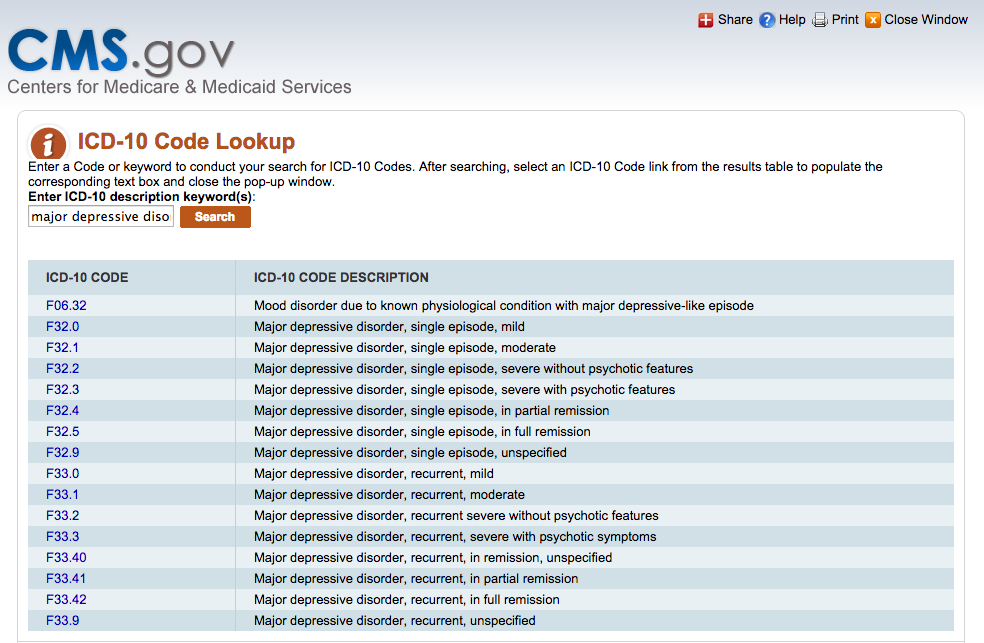
The diagnostic code for major depressive disorder is based on the frequency of recurrent episodes, the severity of the episodes, the presence of psychotic characteristics, and the state of remission. Below are the varieties of depression:
Severity of depression:
- Minor
- Moderate
- Heavy
- Psychotic
- In partial remission
- In complete remission
- Undefined
Epidemiology
Major depressive illness is a common mental illness. Its lifetime prevalence ranges from 5 to 17 percent.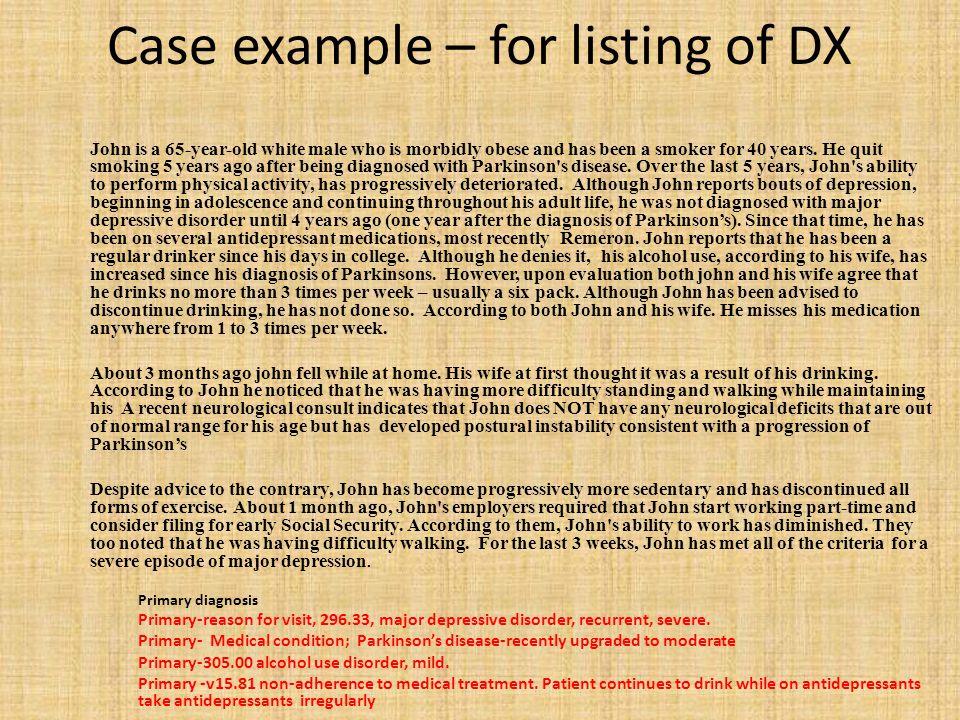 The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
The incidence in women is about twice as high as in men. This is due to hormonal variations, the consequences of childbearing, different psychological pressures in men and women, and a behavioral model of learned helplessness. Although the median age of onset is around 40 years old, new studies show an increase in the incidence among younger populations due to the use of alcohol and other psychoactive substances.
MDD is more common in divorced, separated, or bereaved individuals who do not have meaningful interpersonal interactions. There is no difference in the prevalence of MDD between races or socioeconomic status. People with MDD often have comorbidities such as substance abuse, panic disorder, social anxiety disorder, and obsessive-compulsive disorder.
The presence of these comorbidities in people with MDD increases the risk of suicide. Depression is more common in older people with underlying medical problems. Depression is more common in rural areas than in cities.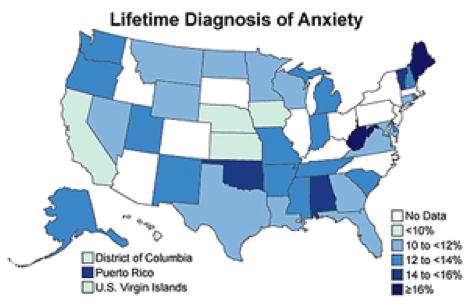
Pathophysiology of major depressive disorder
The genesis of major depressive disorder is believed to be multifaceted, with biological, genetic, environmental and psychological factors at play. It used to be thought that MDD was caused mainly by abnormalities in neurotransmitters, especially serotonin, norepinephrine, and dopamine.
This has been demonstrated by the use of several antidepressants in the treatment of depression, such as selective serotonin receptor inhibitors, serotonin-norepinephrine receptor inhibitors, and dopamine-norepinephrine receptor inhibitors. Serotonin metabolites have been found to decrease in people who have had suicidal thoughts. However, recent hypotheses suggest that this is largely due to more complex neuroregulatory systems and brain circuits, leading to subsequent disruption of the neurotransmitter systems.
GABA, an inhibitory neurotransmitter, as well as glutamate and glycine, important excitatory neurotransmitters, have been shown to play a role in the genesis of depression.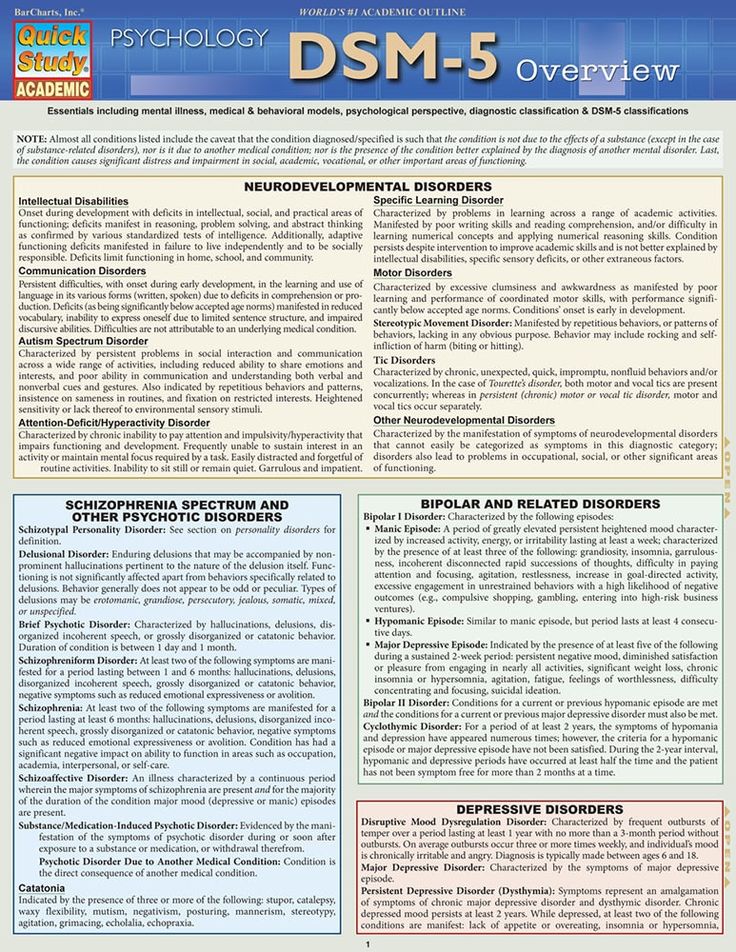 Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
Depressed people have reduced plasma, cerebrospinal fluid, and brain levels of GABA. GABA is believed to act as an antidepressant by blocking the ascending monoamine pathways, including the mesocortical and mesolimbic systems.
The antidepressant properties of drugs that oppose NMDA receptors have been investigated. Thyroid and growth hormone imbalances have also been linked to mood disorders. Numerous adversity and trauma in childhood have been linked to the development of depression later in life.
Severe early stress can cause dramatic changes in neuroendocrine and behavioral responses, leading to anatomical abnormalities in the cerebral cortex and severe depression later in life. Structural functional tomography of the brain in people with depression revealed greater hyperintensity in the subcortical regions and a decrease in the metabolism of the anterior brain regions on the left.
Family, adoption and twin studies have shown that genes play a role in the risk of depression.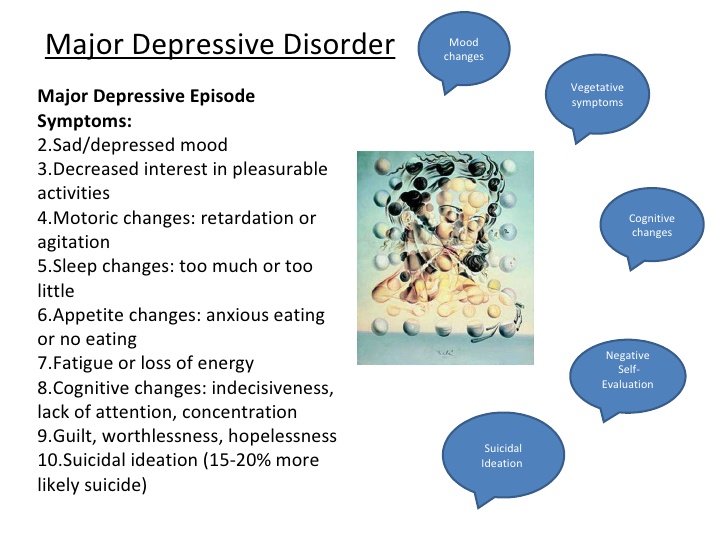 According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to genetic studies, twins with MDD have a very high level of concordance, especially monozygotic twins. Life experience and personal qualities also have an impact.
According to the theory of learned helplessness, the onset of depression is associated with the experience of uncontrollable events. Depression, according to cognitive theory, results from cognitive errors in those who are predisposed to depression.
Somatic illnesses associated with depression
Somatic sensations are especially common in depression and other mental illnesses. Although somatic symptoms are common in depressed individuals, they are of much lesser importance than major depressive symptoms in the diagnosis of depression.
The clinical stages of sad mood are characterized by both painful and non-painful bodily symptoms.
Major depressive disorder diagnosis
Major depressive disorder is a clinical diagnosis; this is mainly determined by the patient's medical history and assessment of mental status.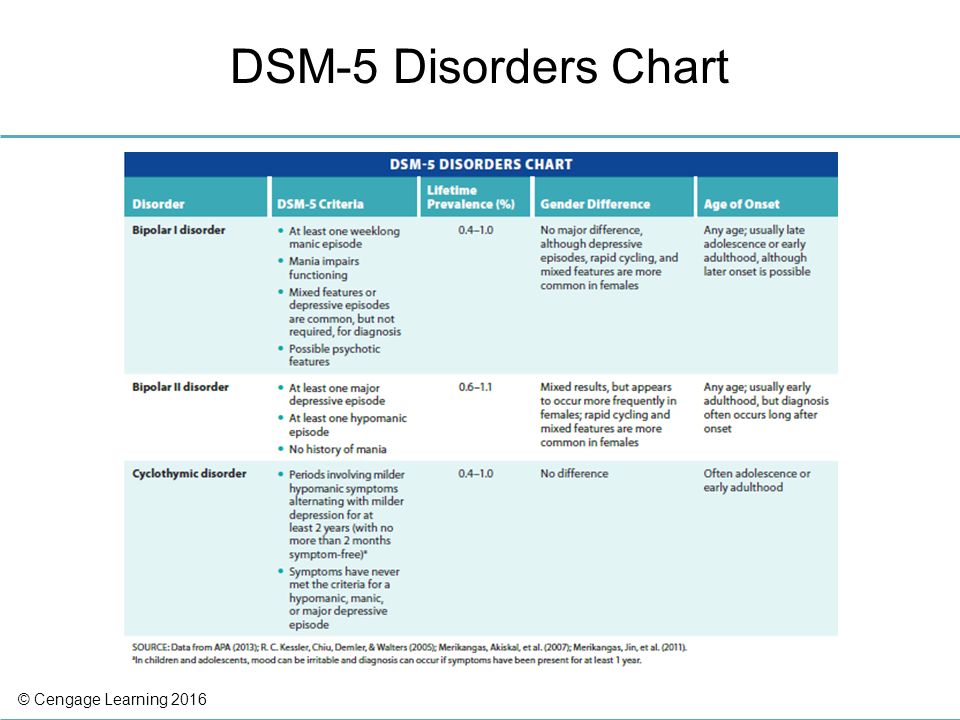 Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Along with symptomatology, the clinical interview should include medical history, family history, social history, and history of drug use. Related information from the patient's family/friends is an important component of the psychiatric evaluation.
Although there are no objective tests to diagnose depression, routine laboratory tests such as CBC with a differential diagnosis, a comprehensive metabolic panel, thyroid-stimulating hormone, free T4, vitamin D, urinalysis, and toxicology screening are done to rule out organic or medical diseases. causes of depression.
People with depression often see their primary care physicians for medical problems related to their depression rather than seeking a mental health professional. In nearly half of the cases, patients deny experiencing depressive symptoms and are often referred to therapy by family members or sent by employers to be tested for social isolation and decreased activity. At each visit, it is critical to assess the patient for thoughts of suicide or murder.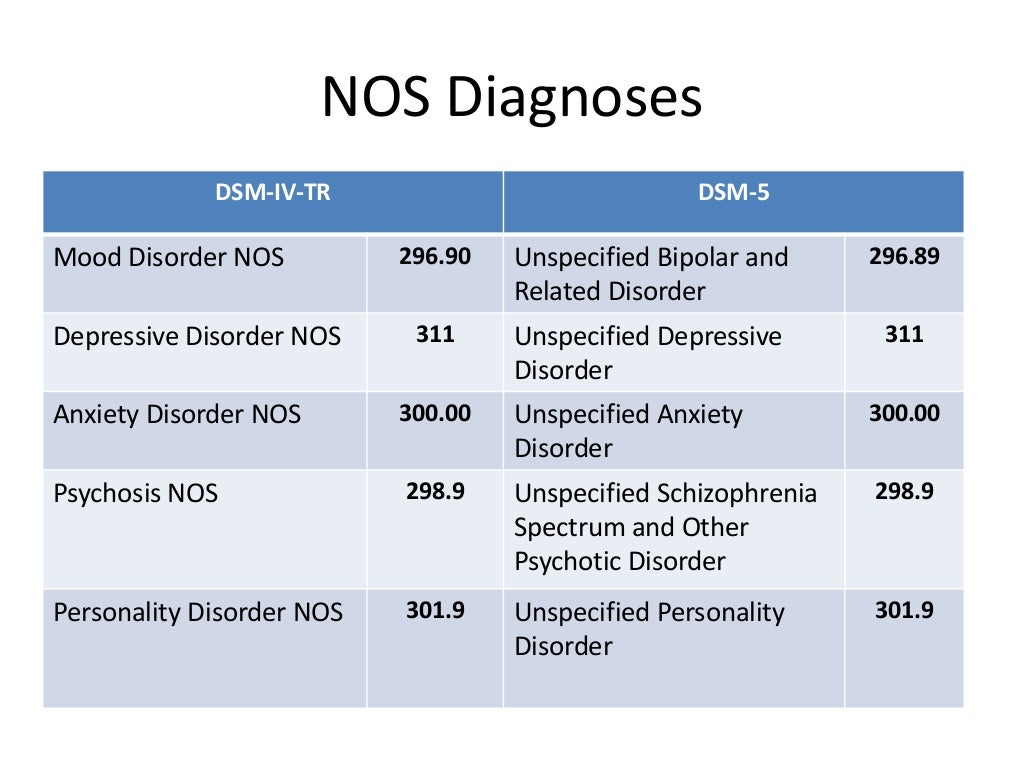
Being in a bad mood or feeling tense is common for all of us. When these feelings persist, you may suffer from depression or anxiety—or both. The self-assessment quizzes contain relevant questions to help you assess your current situation and develop a strategy to help you feel better sooner.
When you are going through a difficult moment, it is natural to feel depressed for a while; feelings like melancholy and loss help define who we are. However, if you feel sad or uncomfortable most of the time for an extended period of time, you may be suffering from depression.
Take a self-test to see if you are showing any warning signs of depression. This won't give you a diagnosis, but it will help you determine what to do next.
Major depressive disorder with psychotic features
Psychotic depression, also known as major depressive disorder with psychotic features, is a serious medical or mental illness that requires prompt treatment and constant monitoring by a physician or mental health professional.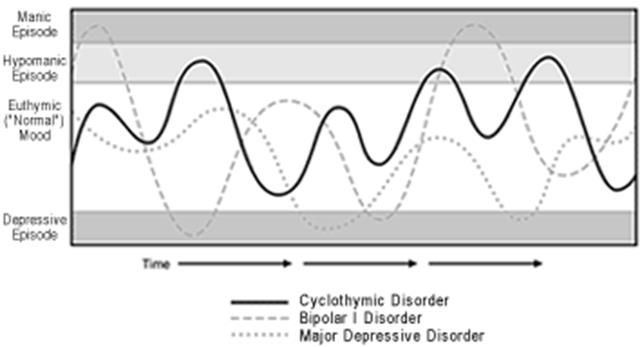
Major depression is a common mental condition that can have a detrimental effect on many aspects of a person's life. It affects mood and behavior as well as various bodily processes such as eating and sleeping. People who are severely depressed often lose interest in things they used to love and have difficulty doing daily activities. Sometimes they may even feel that life is not worth living.
Bipolar disorder (BD)
Depression in patients with bipolar disorder (BD) is a significant clinical problem. Since schizophrenia dominates even in the treatment of BD, depression is associated not only with schizophrenia, but also with BD and comorbid medical disorders with a high risk of suicide.
Diagnosis of bipolar disorder (BD) and risk factors:
Approximately 12-17% of cases of bipolar disorder are not recognized until the mood "transforms" into hypomania or mania, either spontaneously or under the influence of substances uplifting mood.
Factors suggesting a diagnosis of BD:
- Family mania, psychosis, "nervous breakdown" or psychiatric hospitalization
- Early onset, often with depressive symptoms
- Cyclothymic mood
- Multiple relapses (eg 4 episodes of depression in 10 years)
- Depression with characteristic agitation, anger, insomnia, irritability, talkativeness.
- Other features are "mixed" or hypomanic or psychotic symptoms.
- Clinically "worsens", especially with mixed properties, during antidepressant treatment.
- Suicidal thoughts and actions
- Alcohol or drug abuse
Major depressive disorder in children and adolescents:
Major depressive disorder (MDD) can have a significant impact onset during childhood and adolescence. Associated with this are poor school performance, interpersonal problems later in life, early parenthood, and an increased risk of other psychiatric and substance use disorders.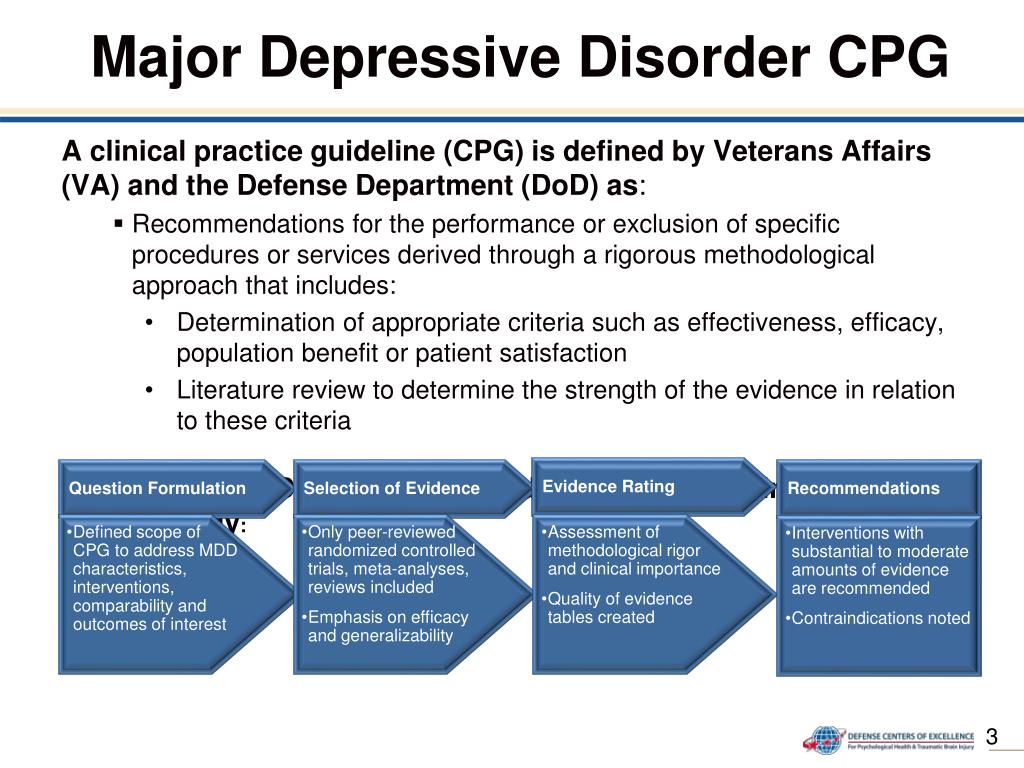 Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Diagnosing MDD in childhood is difficult. Children with MDD are often underdiagnosed and undertreated, and only 50% of adolescents are diagnosed before reaching adulthood.
Symptoms of depression in children aged 3-8 years include:
- unsubstantiated claims.
- irritability
- less signs of depression
- anxiety
- behavioral changes
As the child becomes a teenager and adult, the presentation of symptoms meets the criteria for the Diagnostic and Statistical Manual of Mental Disorders (DSM-5):
- Irritability.
- Expected weight gain.
- Lethargy or inner restlessness.
- May be delusional and not limited to feelings of guilt.
Postpartum depression
Postpartum depression affects one in seven women (PPD). While most women recover quickly from childhood blues, PPD lasts much longer and has a significant impact on women's ability to return to normal activities.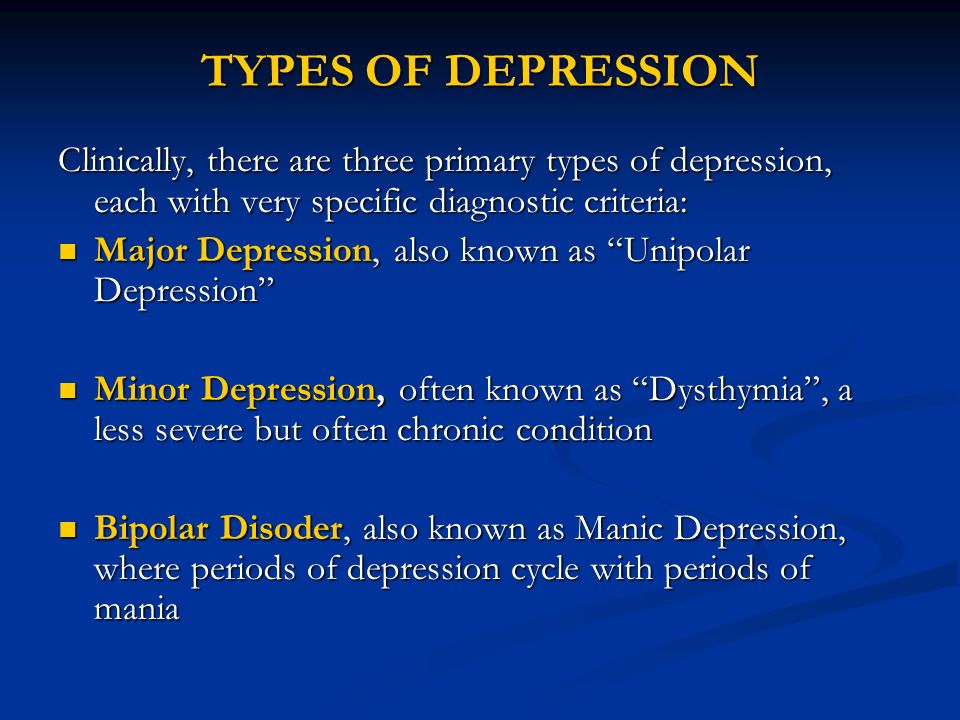
PDD affects the mother and her relationship with the child. PRD impairs maternal brain response and behavior. Postpartum depression most often occurs within 6 weeks after delivery. PDD affects 6.5 to 20% of women. It is more common in teenage girls, mothers who have given birth prematurely, and women living in cities.
In one study, African American and Hispanic mothers reported onset of symptoms within 2 weeks of birth, while white mothers reported onset of symptoms later.
Premenstrual dysphoric disorder
Premenstrual symptoms are a group of psychological, behavioral and physical symptoms that cyclically occur before menstruation and subsequently resolve after menstruation in women of reproductive age. Most women experience relatively mild pain and the symptoms do not interfere with their personal, social, or professional lives; however, 5% to 8% of women experience moderate or severe symptoms that can cause significant distress and functional impairment.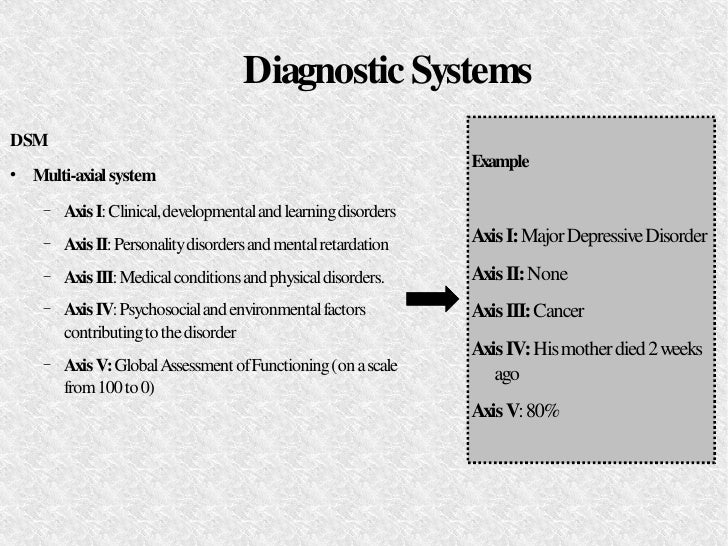
All women of reproductive age, from menarche to menopause, may have premenstrual symptoms. Premenstrual symptoms are a common problem for women of reproductive age. In the United States, 70 to 90 percent of women of reproductive age report at least some premenstrual pain.
Approximately one third of these women have symptoms severe enough to warrant a diagnosis of PMS. PMDD, the most severe type of premenstrual symptom complex, occurs in 3-8% of these women.
Treatment of major depressive disorder
Treatment of major depressive disorder (MDD) in adults:
Treatment options for major depressive disorder include medication, psychological, interventional, and lifestyle changes. Medications and/or psychotherapy are used initially to treat MDD.
Combination treatment, including both drugs and psychotherapy, has been shown to be more effective than either treatment alone. Electroconvulsive therapy has been shown to be more effective than any other treatment for severe major depression.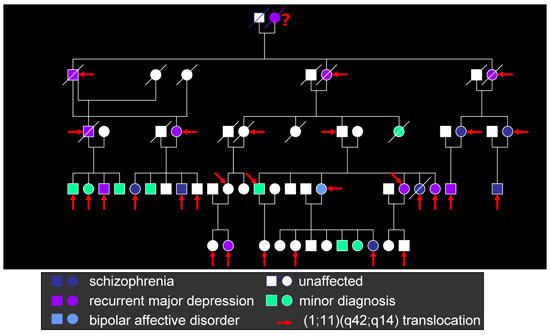
Patient psychotherapy:
Depression education and treatment can be provided to all patients. When appropriate, education may be provided to eligible family members.
Information about available treatment options will help patients make informed decisions, anticipate side effects, and follow prescribed treatment. Another important aspect of education was informing patients and concerned family members about the delayed duration of antidepressant onset of action.
Pharmacotherapy and acute treatment:
Antidepressants may be used as the primary treatment for patients with moderate or severe depression.
Clinical features that may indicate that the drug is a preferred therapeutic agent include a history of previous positive response to antidepressants, severity of symptoms, significant sleep disturbance and appetite disturbance.
Patients with severe depression with psychotic features will require antidepressant and antipsychotic and/or electroconvulsive therapy (ECT).
All antidepressants are effective, although their side effects vary. The following drugs have been approved by the FDA for the treatment of MDD:
- Fluoxetine, sertraline, citalopram, escitalopram, paroxetine, and fluvoxamine are examples of selective serotonin reuptake inhibitors (SSRIs). They are commonly used as first line therapy and are the most commonly prescribed antidepressants.
- Venlafaxine, duloxetine, desvenlafaxine, levomilnacipran and milnacipran are examples of serotonin and norepinephrine reuptake inhibitors (SNRIs). They are often used to treat depressed people who also have pain problems.
- Trazodone, vilazodone and vortioxetine are serotonin modulators.
- Bupropion and mirtazapine are examples of atypical antidepressants. When patients experience sexual side effects from SSRIs or SNRIs, they are often recommended as monotherapy or as adjunctive drugs.
- Amitriptyline, imipramine, clomipramine, doxepin, nortriptyline and desipramine are tricyclic antidepressants (TCAs).
- Tranylcypromine, phenelzine, selegiline, and isocarboxazid are examples of monoamine oxidase inhibitors (MAOIs). Due to the high prevalence of side effects and death in overdose, MAOIs and TCAs are not commonly used.
- Other drugs that can be used to improve the effectiveness of antidepressants include mood stabilizers and antipsychotics.
The role of yoga and meditation in managing depression:
Originating in ancient India, yoga is recognized as a form of alternative medicine using mind-body practice. Yoga philosophy is based on 8 elements that are best described as the ethical principles of a meaningful and purposeful life. Yoga can help with depression through the following mechanisms:
- Muscle relaxation resulting in less pain
- Creating Balanced Energy
- Decreased breathing and heart rate
- Lowering blood pressure and cortisol levels
- Increase blood flow
- Reducing stress and anxiety through tranquility
- Improve pre-existing ailments such as arthritis, cancer, mental illness and more.
Treatment of major depressive disorder (MDD) in children and adolescents
Psychotherapy is important for both patients and their families, so everyone knows about the plan and goals of treatment. When the patient receives information, the severity of symptoms decreases. Mental education may include knowledge about the signs and symptoms of depression, the clinical course of the illness, the risk of exacerbation, treatment options, and parental advice on how to interact with depressed young people.
According to research by Sandra Mullen, psychotherapy, along with medication, is often recommended for the treatment of major depressive disorder (MDD) in children and adolescents diagnosed with depression, suicidal ideation, and transient hypomania/mania.
Treatment of bipolar depression
Bipolar depression remains a clinical problem. Treatment options are limited, especially in the treatment of the acute phase of bipolar depression. There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
There are currently only three approved drugs: OFC, quetiapine (immediate or extended release) and lurasidone (lithium monotherapy or adjuvant therapy or valproate). All three agents have similar efficacy profiles. They differ in duration.
Non-approved agents and treatments
Non-pharmacological drugs such as lamotrigine, antidepressants, modafinil, pramipexole, ketamine, and electroconvulsive therapy (ECT) are often prescribed for the treatment of acute bipolar depression.
Treatment of recurrent depression:
Some patients may experience recurrent episodes of depression throughout their lives unless supportive care is used to prevent relapse. Treatment should include psychotherapy and pharmacotherapy, and the dose should generally not be reduced after remission has been achieved.
Differential
Critical to rule out depressive disorder due to another medical condition, depressive disorder due to psychoactive substances/drugs, dysthymia, cyclothymia, bereavement, adjustment disorder with depressed mood, bipolar disorder, schizoaffective disorder, schizophrenia, anxiety disorders and eating disorders when assessed for DMD. Depressive symptoms can develop as a result of the following factors:
Depressive symptoms can develop as a result of the following factors:
- Neurological causes such as cerebrovascular accident, multiple sclerosis, epilepsy, Parkinson's disease and Alzheimer's disease.
- Endocrine diseases such as diabetes, thyroid disease and adrenal disease.
- Metabolic disorders such as hypercalcemia, hyponatremia
- Drugs/substances causing dependence: steroids, antihypertensives, anticonvulsants, antibiotics, sedatives, sleeping pills, alcohol, stimulant withdrawal.
- Nutrient deficiencies such as vitamin D, B12, B6, iron or folate deficiency
- Infectious diseases such as HIV and syphilis
- Malignant neoplasms
Prognosis
Episodes of depression in untreated major depressive disorder can last 6 to 12 months. Approximately two-thirds of people with MDD think about suicide, and 10 to 15% commit suicide. MDD is a chronic relapsing disease; the recurrence rate after the first episode is about 50%, 70% after the second episode and 90% after the third episode.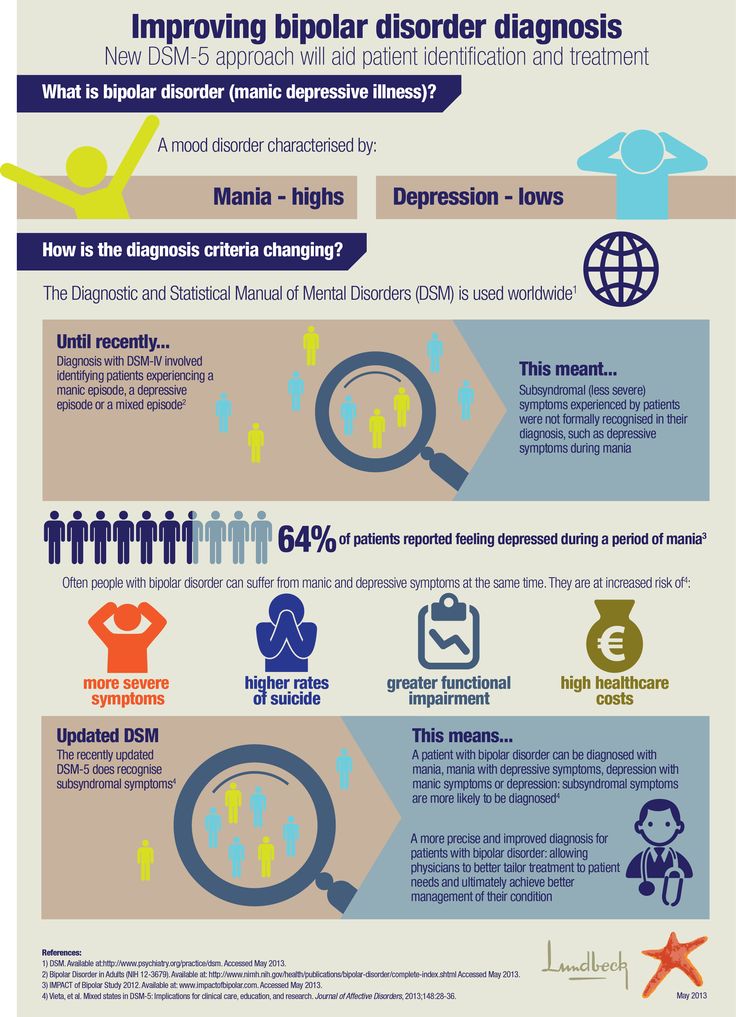 Approximately 5-10% of people with MDD develop bipolar disorder.
Approximately 5-10% of people with MDD develop bipolar disorder.
Patients with mild episodes, no psychotic symptoms, improved adherence, a reliable support system, and adequate premorbid functioning have a positive prognosis for MDD. In the presence of a concomitant mental disorder, personality disorder, multiple hospitalizations and advanced age, the prognosis is poor.
Complications
MDD is one of the leading causes of disability in the world. This not only causes severe functional impairment, but also negatively affects interpersonal relationships, reducing the quality of life. Individuals with MDD are at significant risk of developing comorbid anxiety and drug use disorders, which increase the risk of suicide.
Diabetes, hypertension, chronic obstructive pulmonary disease and coronary heart disease may be aggravated by depression. People who are depressed are more likely to engage in self-destructive behavior as a coping method. Left untreated, MDD can be quite debilitating.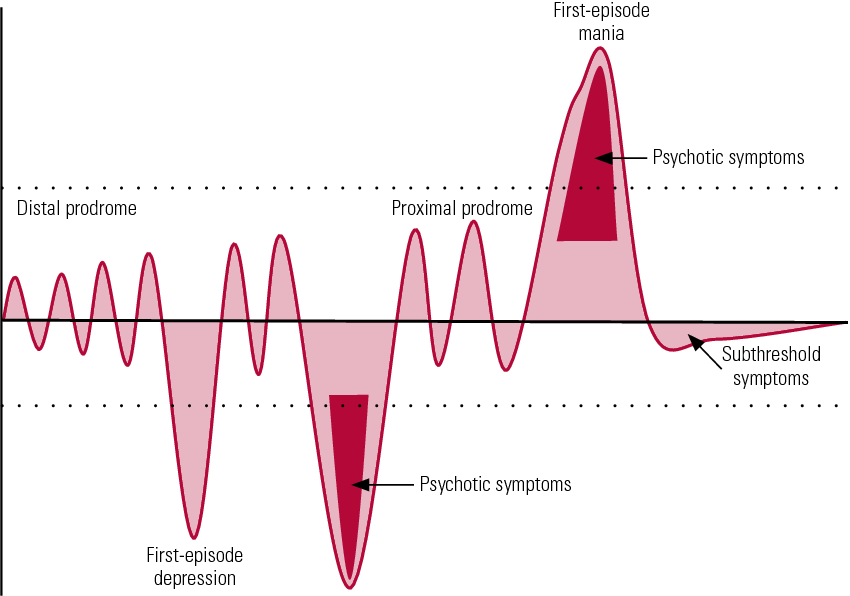
Findings
In 2008, WHO classified major depressive disorder (MDD) as the third leading cause of disease burden worldwide and is expected to be number one by 2030.
Diagnosis is made when a person has a persistently low or depressed mood, anhedonia (loss of interest in pleasure), feelings of guilt or worthlessness, lack of energy, poor concentration, changes in appetite, psychomotor retardation or agitation, trouble sleeping, or suicidal thoughts.
Effective and successful treatment of MDD requires a multidisciplinary approach. These collaborative services include primary care physicians and psychiatrists, as well as nurses, therapists, social workers and caregivers. Screening for depression in primary care settings is critical.
Types of depression - iFightDepression [EN]
There are different types of depression, which are different.
Signs and symptoms vary in number, time, severity and frequency, but are generally very similar. Because different types of depression are treated differently, it is important to pinpoint the type of depression. Depending on gender, age and cultural characteristics, people have different symptoms and severity of depression.
Because different types of depression are treated differently, it is important to pinpoint the type of depression. Depending on gender, age and cultural characteristics, people have different symptoms and severity of depression.
Neurotic, reactive (minor) depression is treated with psychotherapy.
Somatic and psychotic - medication. These terms are used by psychiatrists.
Studies have shown that depression has a phasic course. Periods of normal mood alternate with depressive episodes. Sometimes, instead of a depressive phase,
there may be a manic phase, which is manifested by irritability and high mood. If so, then it is not depression, but bipolar disorder (a more serious illness).
1. Depressive episode
The most common and typical form of depression is the depressive episode. An episode lasts from a few weeks to a year, but is always longer than 2 weeks. A single depressive episode is called a unipolar episode. Approximately one third of affected people experience only one episode, or "phase", during their lifetime.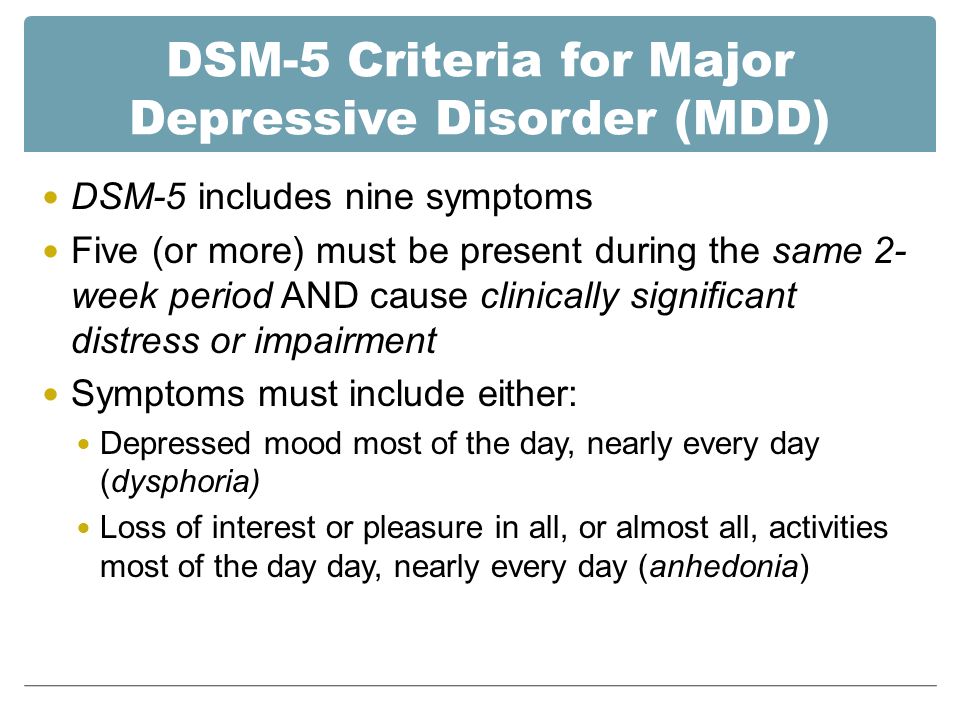 However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
However, if a person does not receive appropriate treatment for depression, there is a risk of recurrent depressive episodes in the future. Depressive episodes always affect a person's performance to one degree or another.
2. Intermittent (recurrent) depressive disorder
When a depressive episode recurs, it is recurrent depressive disorder or major depressive disorder, which usually begins in adolescence or early adulthood. With this kind of depression, depressive phases, which can last from several months to several years, alternate with phases of normal mood. This type of depressive disorder can seriously affect performance and is unipolar in nature (no manic or hypomanic phase). This is the so-called "classic" or "clinical" depression.
3. Dysthymia
Dysthymia presents with milder and less severe symptoms than a depressive episode or recurrent depression. However, the disorder is permanent, with symptoms lasting much longer, at least 2 years, sometimes decades, which is why it is called "chronic depression".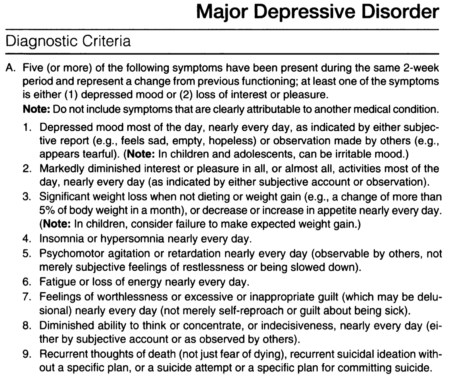 This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
This disorder is unipolar and also affects performance. This type of depression sometimes develops into a more severe form (major depressive episode) and if this happens it is called double depression.
4. Bipolar depression, type I
This is the type of depression in bipolar disorder, formerly called manic-depressive illness, and is less common than unipolar depression. It consists of alternating depressive phases, phases of normal mood and so-called manic phases.
Manic phases are characterized by excessively high mood associated with hyperactivity, anxiety, and decreased need for sleep.
Mania affects thinking, judgment and social behavior causing serious problems and difficulties. When a person is in a manic phase, he makes frequent casual unsafe sex, makes unwise financial decisions. After a manic episode, such people often experience depression.
The best way to describe these "emotional upheavals" is "to be on top of the world and fall into the depths of despair".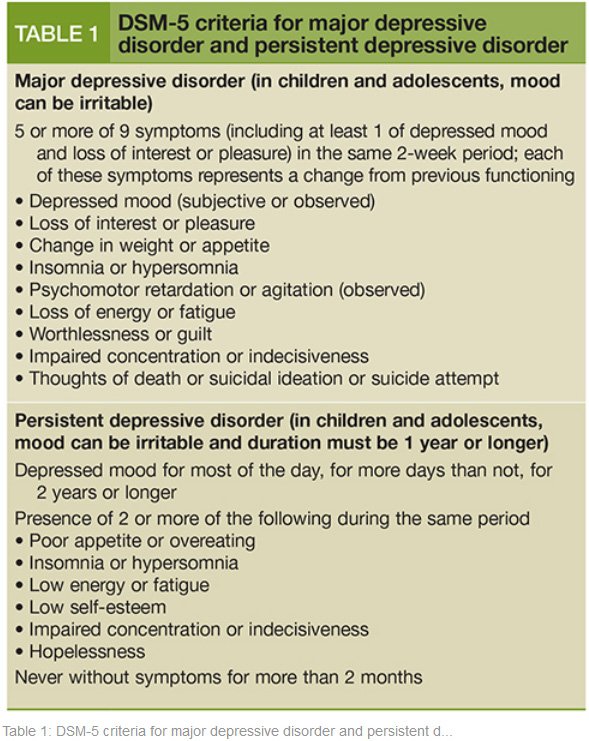
Symptoms of the phases of depression in bipolar disorder are sometimes difficult to distinguish from unipolar depression.
5. Bipolar depression type II
More like recurrent depressive disorder than bipolar disorder. In this disorder, multiple depressive phases alternate with phases of mania, but with less pronounced euphoria. During these phases, family and loved ones may even mistakenly assume that the person is doing well.
6. Mixed anxiety-depressive disorder
In anxiety-depressive disorder, the clinical picture is very similar to depression, however, in depression, depressive syndromes always come first. In this case, both anxious and depressive symptoms are evenly combined.
7. Depressive psychotic episode
A special form of depressive episode is psychotic or delusional depression. Psychosis is a condition in which people see or hear things that do not exist (hallucinations) and/or have false ideas or beliefs (delusions).